Health technology assessment of medical devices
Health technology assessment of medical devices
Health technology assessment of medical devices
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Health</strong> <strong>technology</strong><strong>assessment</strong> <strong>of</strong><strong>medical</strong> <strong>devices</strong>WHO Medical device technical series
Preface<strong>Health</strong> technologies are essential for a functioning health system. Medical <strong>devices</strong> inparticular are crucial in the prevention, diagnosis, and treatment <strong>of</strong> illness and disease,as well as patient rehabilitation. Recognizing this important role <strong>of</strong> health technologies,the World <strong>Health</strong> Assembly adopted resolution WHA60.29 in May 2007. The resolutioncovers issues arising from the inappropriate deployment and use <strong>of</strong> health technologies,and the need to establish priorities in the selection and management <strong>of</strong> healthtechnologies, specifically <strong>medical</strong> <strong>devices</strong>. By adopting this resolution, delegationsfrom Member States acknowledged the importance <strong>of</strong> health technologies for achievinghealth-related development goals; urged expansion <strong>of</strong> expertise in the field <strong>of</strong> healthtechnologies, in particular <strong>medical</strong> <strong>devices</strong>; and requested that the World <strong>Health</strong>Organization (WHO) take specific actions to support Member States.One <strong>of</strong> WHO’s strategic objectives is to “ensure improved access, quality and use <strong>of</strong><strong>medical</strong> products and technologies.” This objective, together with the World <strong>Health</strong>Assembly resolution, formed the basis for establishing the Global Initiative on <strong>Health</strong>Technologies (GIHT), with funding from the Bill & Melinda Gates Foundation. GIHTaims to make core health technologies available at an affordable price, particularlyto communities in resource-limited settings, to effectively control important healthproblems. It has two specific objectives:• to challenge the international community to establish a framework for thedevelopment <strong>of</strong> national essential health <strong>technology</strong> programmes that will have apositive impact on the burden <strong>of</strong> disease and ensure effective use <strong>of</strong> resources;• to challenge the business and scientific communities to identify and adaptinnovative technologies that can have a significant impact on public health.To meet these objectives, WHO and partners have been working towards devising anagenda, an action plan, tools and guidelines to increase access to appropriate <strong>medical</strong><strong>devices</strong>. This document is part <strong>of</strong> a series <strong>of</strong> reference documents being developed foruse at the country level. The series will include the following subject areas:• policy framework for health <strong>technology</strong>• <strong>medical</strong> device regulations• health <strong>technology</strong> <strong>assessment</strong>• health <strong>technology</strong> management››needs <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>››<strong>medical</strong> device procurement››<strong>medical</strong> equipment donations››<strong>medical</strong> equipment inventory management››<strong>medical</strong> equipment maintenance››computerized maintenance management systems• <strong>medical</strong> device data››<strong>medical</strong> device nomenclature››<strong>medical</strong> <strong>devices</strong> by health-care setting››<strong>medical</strong> <strong>devices</strong> by clinical procedures• <strong>medical</strong> device innovation, research and development.WHO Medical device technical series3
These documents are intended for use by bio<strong>medical</strong> engineers, health managers,donors, nongovernmental organizations and academic institutions involved in health<strong>technology</strong> at the district, national, regional or global levels.MethodologyThe documents in this series were written by international experts in their respectivefields, and reviewed by members <strong>of</strong> the Technical Advisory Group on <strong>Health</strong> Technology(TAGHT). The TAGHT was established in 2009 to provide a forum for both experiencedpr<strong>of</strong>essionals and country representatives to develop and implement the appropriatetools and documents to meet the objectives <strong>of</strong> the GIHT. The group has met on threeoccasions. The first meeting was held in Geneva in April 2009 to prioritize which toolsand topics most required updating or developing. A second meeting was held in Rio deJaneiro in November 2009 to share progress on the health <strong>technology</strong> management toolsunder development since April 2009, to review the current challenges and strategiesfacing the pilot countries, and to hold an interactive session for the group to presentproposals for new tools, based on information gathered from the earlier presentationsand discussions. The last meeting was held in Cairo in June 2010 to finalize thedocuments and to help countries develop action plans for their implementation. Inaddition to these meetings, experts and advisers have collaborated through an onlinecommunity to provide feedback on the development <strong>of</strong> the documents. The conceptswere discussed further during the First WHO Global Forum on Medical Devices inSeptember 2010. Stakeholders from 106 countries made recommendations on howto implement the information covered in this series <strong>of</strong> documents at the country level. 1All meeting participants and persons involved in the development <strong>of</strong> these documentswere asked to complete a declaration <strong>of</strong> interest form, and no conflicts were identified.1 First WHO Global Forum on Medical Devices: context, outcomes, and future actions is available at: http://www.who.int/<strong>medical</strong>_<strong>devices</strong>/gfmd_report_final.pdf (accessed March 2011)4<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
DefinitionsRecognizing that there are multiple interpretations for the terms listed below, they aredefined as follows for the purposes <strong>of</strong> this technical series.<strong>Health</strong> <strong>technology</strong>: The application <strong>of</strong> organized knowledge and skills in the form <strong>of</strong><strong>devices</strong>, medicines, vaccines, procedures and systems developed to solve a healthproblem and improve quality <strong>of</strong> life. 2 It is used interchangeably with health-care<strong>technology</strong>.Medical device: An article, instrument, apparatus or machine that is used in theprevention, diagnosis or treatment <strong>of</strong> illness or disease, or for detecting, measuring,restoring, correcting or modifying the structure or function <strong>of</strong> the body for some healthpurpose. Typically, the purpose <strong>of</strong> a <strong>medical</strong> device is not achieved by pharmacological,immunological or metabolic means. 3Medical equipment: Medical <strong>devices</strong> requiring calibration, maintenance, repair, usertraining, and decommissioning – activities usually managed by clinical engineers.Medical equipment is used for the specific purposes <strong>of</strong> diagnosis and treatment <strong>of</strong>disease or rehabilitation following disease or injury; it can be used either alone or incombination with any accessory, consumable, or other piece <strong>of</strong> <strong>medical</strong> equipment.Medical equipment excludes implantable, disposable or single-use <strong>medical</strong> <strong>devices</strong>.2 World <strong>Health</strong> Assembly resolution WHA60.29, May 2007 (http://www.who.int/<strong>medical</strong>_<strong>devices</strong>/resolution_wha60_29-en1.pdf, accessed March 2011).3 Information document concerning the definition <strong>of</strong> the term “<strong>medical</strong> device”. Global Harmonization Task Force, 2005 (http://www.ghtf.org/documents/sg1/sg1n29r162005.pdf, accessed March 2011).WHO Medical device technical series5
Acknowledgements<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong> was developed under the primaryauthorship <strong>of</strong> Reiner Banken, Institut national d’excellence en santé et en servicessociaux (INESSS), Montréal, Canada, and Donald Juzwishin, Alberta <strong>Health</strong> Services,Edmonton, Canada, and produced under the overall direction <strong>of</strong> Adriana Velazquez-Berumen, World <strong>Health</strong> Organization, Geneva, Switzerland as part <strong>of</strong> the Global Initiativeon <strong>Health</strong> Technologies (GIHT) project funded by the Bill & Melinda Gates Foundation.The draft was reviewed by Jennifer Barragan, Maria Benkhalti, Stephen Bornstein,Lisa Farrell, Janet Hatcher-Roberts , Janet Hiller, Mira Johri, Egon Jonsson, ArmineeKazanjian, Guy Maddern, Logan Mardhani-Bayne, Joseph L Mathew, Craig Mitton,Laura Sampietro-Colom, Dima Samaha, Julian Stedman, and edited by Cathy Needham.We would like to thank Aditi A Sharma for assistance in pro<strong>of</strong>reading and Karina Reyes-Moya and Gudrun Ingolfsdottir for administrative support throughout the development<strong>of</strong> this document.Declarations <strong>of</strong> interestsConflict <strong>of</strong> interest statements were collected from all contributors to and reviewers <strong>of</strong> thedocument. Donald Juzwishin declared his employment at the Alberta <strong>Health</strong> Servicesand as a consultant with McMaster University as remuneration from an organizationwith an interest related to the subject. Maria Benkhalti declared her position withKnowledge Transition and <strong>Health</strong> Technology Assessment in <strong>Health</strong> Equity, University<strong>of</strong> Ottawa as representation <strong>of</strong> interests related to the subject. Janet Hatcher-Robertsdeclared receipt <strong>of</strong> funding for a global conference on health equity which was unrelatedto health <strong>technology</strong> <strong>assessment</strong>. Joseph L Mathew declared the <strong>Health</strong> TechnologyAssessment International (HTAi) travel grant award to participate in the annual meeting<strong>of</strong> the scientific society as well as his interest in the publication <strong>of</strong> the report in questionto benefit health care pr<strong>of</strong>essionals and people in developing countries with whom hehas substantial pr<strong>of</strong>essional interests. None <strong>of</strong> these declared conflicts influenced thecontent <strong>of</strong> the document.6<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
Acronyms and abbreviationsTAGHTCOHREDCSIHDALYEUnetHTAEVIPNetGIHTHTAHTAiHTMHTRINAHTAISGQALYSIGWHOTechnical Advisory Group on <strong>Health</strong> TechnologyCouncil on <strong>Health</strong> Research for DevelopmentCanadian Society for International <strong>Health</strong>disability-adjusted life yearEuropean network for <strong>Health</strong> Technology AssessmentEvidence-Informed Policy NetworkGlobal Initiative on <strong>Health</strong> Technologieshealth <strong>technology</strong> <strong>assessment</strong><strong>Health</strong> Technology Assessment internationalhealth/health-care <strong>technology</strong> managementhealth <strong>technology</strong> regulationInternational Network <strong>of</strong> Agencies for <strong>Health</strong> Technology Assessmentinterest sub-groupquality-adjusted life yearspecial interest groupWorld <strong>Health</strong> OrganizationWHO Medical device technical series7
Executive summary<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> (HTA) has emerged as an important tool for supportingthe core functions <strong>of</strong> an effective global health system. 1 Actions by the World <strong>Health</strong>Organization (WHO) and other global health organizations are necessary to supportregional and national initiatives for the advancement <strong>of</strong> HTA in developing and emergingcountries (i.e. nations in the process <strong>of</strong> rapid growth and industrialization). Thisdocument describes an approach for how the multiple players in the global communitycan come together to advance the knowledge and effective uptake <strong>of</strong> health <strong>technology</strong><strong>assessment</strong> in local settings.HTA is the systematic evaluation <strong>of</strong> properties, effects, and/or impacts <strong>of</strong> health<strong>technology</strong>. Its main purpose is to inform <strong>technology</strong>-related policy-making in healthcare, and thus improve the uptake <strong>of</strong> cost-effective new technologies and preventthe uptake <strong>of</strong> technologies that are <strong>of</strong> doubtful value for the health system. It is one<strong>of</strong> three complementary functions to ensure the appropriate introduction and use <strong>of</strong>health <strong>technology</strong>. The other two components are regulation, which is concerned withsafety and efficacy, and <strong>assessment</strong> <strong>of</strong> all significant intended as well as unintendedconsequences <strong>of</strong> <strong>technology</strong> use, including clinical and cost-effectiveness; andmanagement, which is concerned with the procurement and maintenance <strong>of</strong> the<strong>technology</strong> during its life-cycle. The performance <strong>of</strong> health systems is strengthenedwhen the linkages and exchange among these elements are clearly differentiated butmutually supportive.This document integrates health <strong>technology</strong> <strong>assessment</strong> into the WHO framework forevidence-informed policy-making (2). <strong>Health</strong> systems are strengthened when HTA isintegrated into the human and material resources, data, transparent decision- andpolicy-making, and linked to the overall vision <strong>of</strong> equity and accountability. Goodgovernance can rely on health <strong>technology</strong> <strong>assessment</strong> to provide a policy approachthat is accountable for its decisions to the population.Organizations specializing in health <strong>technology</strong> <strong>assessment</strong> are becoming institutionalizedelements <strong>of</strong> health systems, not only to help identify health-care interventions that maynot be effective, but also to identify promising technologies that can stimulate innovation.There are several international agencies supporting the advancement <strong>of</strong> HTA on theglobal stage. <strong>Health</strong> Technology Assessment international (HTAi) and the InternationalNetwork <strong>of</strong> Agencies in <strong>Health</strong> Technology Assessment (INAHTA) have a demonstratedcommitment to advance and collaborate on health <strong>technology</strong> <strong>assessment</strong> with WHOand any country or community that is interested. WHO collaborating centres and theirglobal network – specifically the Global Network <strong>of</strong> WHO Collaborating Centres forHTA – have made a commitment to promote international dialogue, collaboration andstrengthen existing projects.1 The global health system has been defined as the constellation <strong>of</strong> actors (individuals and/or organizations) “whose primary purpose is to promote, restore or maintain health” and “the persistent andconnected sets <strong>of</strong> rules (formal or informal), that prescribe behavioral roles, constrain activity, and shape expectations” among them. Such actors may operate at the community, national or globallevels, and may include governmental, intergovernmental, private for-pr<strong>of</strong>it, and/or non-pr<strong>of</strong>it entities (1).8<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
There are several strategies for overcoming challenges and advancing health <strong>technology</strong><strong>assessment</strong> in developing and emerging countries. In all, sensitivity for contextualizingto the resource capacity and capability is encouraged. One approach for advancing HTAis to build on the 1990 report <strong>of</strong> the Commission on <strong>Health</strong> Research for Developmentand the 2003 commentary by the Council on <strong>Health</strong> Research for Development, both <strong>of</strong>which encourage the strengthening <strong>of</strong> national institutions supported through regionaland international networking.The strategy <strong>of</strong> introducing focal points for health <strong>technology</strong> <strong>assessment</strong> in a developingor emerging country will be dependent on many factors – appropriate location, humanresource capability, and organization capacity to name a few. Good governance, funding,and effective collaboration with partners will be essential ingredients for building HTAcapacity. This document demonstrates that there are many international organizationsand pr<strong>of</strong>essionals willing to work with WHO and developing and emerging countries toadvance HTA to strengthen health systems. Alignment <strong>of</strong> HTA capacity building initiativeswith the WHO strategy on research for health will create synergies for promotingevidence-informed decision-making to improve health systems and population health.WHO Medical device technical series9
1 Introduction<strong>Health</strong> systems throughout the world,whether in developed or developingcountries, are struggling with the challenge<strong>of</strong> how to manage health-care delivery inconditions <strong>of</strong> resource constraint. <strong>Health</strong>carepolicy, practice and decisions areneeded to maximize the positive impact<strong>of</strong> health-care interventions on populationhealth, while maximizing the value fromthe cost <strong>of</strong> providing the interventions.This document explores how health<strong>technology</strong> <strong>assessment</strong> can be adoptedand adapted in developing and emergingcountries in an attempt to foster healthequity.2 Purpose<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong><strong>devices</strong> provides a background to theconcept and programme <strong>of</strong> health<strong>technology</strong> <strong>assessment</strong> (HTA) aroundthe world, and highlights the contributionthat HTA can make to informed policyanddecision-making, particularly fordeveloping and emerging countries. Itaims to describe strategic actions foradvancing HTA into developing andemerging countries, and to support informeddecision-making on the introduction<strong>of</strong> HTA into the health systems <strong>of</strong> thesecountries.This document was commissioned byWHO for the advancement <strong>of</strong> health <strong>technology</strong><strong>assessment</strong> in developing andemerging countries.3 ApproachThis document builds on the work <strong>of</strong> theWHO Department <strong>of</strong> Essential <strong>Health</strong>Technologies, the Global Initiative on<strong>Health</strong> Technologies (GIHT), the GlobalNetwork <strong>of</strong> WHO Collaborating Centres for<strong>Health</strong> Technology Assessment, <strong>Health</strong>Technology Assessment international(HTAi), the International Network<strong>of</strong> Agencies for <strong>Health</strong> TechnologyAssessment (INAHTA), and otherscommitted to the use <strong>of</strong> high-qualityevidence to inform health-care policy anddecision-making. The authors have basedtheir work on a personal knowledge <strong>of</strong> theinternational literature on the conceptsand practice <strong>of</strong> health <strong>technology</strong><strong>assessment</strong> (HTA) as well as on theavailable literature and past experiences<strong>of</strong> introducing HTA into developing andemerging countries. Consultations withkey groups and international experts inHTA have contributed to the text.10<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
4 Definition <strong>of</strong> health <strong>technology</strong> <strong>assessment</strong>The paradigm <strong>of</strong> HTA emerged as aresponse to decision-makers’ questionsabout the uncontrolled diffusion <strong>of</strong> costly<strong>medical</strong> equipment. HTA began in theearly 1970s, when the rapid demandfor computer-assisted tomography (CTscans)became a public policy issue dueto the very high cost per unit, <strong>of</strong>ten inexcess <strong>of</strong> US$ 300 000 (3).In February 1975 the US SenateCommittee on Labor and Public Welfare(on behalf <strong>of</strong> its Subcommittee on <strong>Health</strong>)invited the recently established Office<strong>of</strong> Technology Assessment to conducta study <strong>of</strong> the justifications requiredbefore the implementation <strong>of</strong> costly new<strong>medical</strong> technologies and procedures.The concepts <strong>of</strong> health technologies andHTA have developed very broadly since.A health <strong>technology</strong> is “any interventionthat may be used to promote health, toprevent, diagnose or treat disease or forrehabilitation or long-term care” (4). It thusencompasses <strong>medical</strong> <strong>devices</strong> rangingfrom simple wooden tongue depressorsand assistive <strong>devices</strong>, to the mostsophisticated implants, <strong>medical</strong> imagingsystems, drugs, <strong>medical</strong> and surgicalprocedures, and the organizational andsupportive systems within which suchcare is provided.HTA is “the systematic evaluation <strong>of</strong>properties, effects, and/or impacts <strong>of</strong>health-care <strong>technology</strong>. It may addressthe direct, intended consequences <strong>of</strong>technologies as well as their indirect,unintended consequences. Its mainpurpose is to inform <strong>technology</strong>-relatedpolicy-making in health care. HTA isconducted by interdisciplinary groupsusing explicit analytical frameworksdrawing from a variety <strong>of</strong> methods”(4).Depending on the issues involved, thetime frame <strong>of</strong> decision-making, and theavailability <strong>of</strong> resources, HTAs can takedifferent forms such as a full-scale HTAreport, contextualization <strong>of</strong> HTA reportsproduced elsewhere, rapid reviews,health <strong>technology</strong> information services orhorizon scanning reports. HTA is alwayspolicy-oriented, context-embedded andmethodologically sound (5).As outlined in a document from theOrganisation for Economic Co-operationand Development (6), countries cansuccessfully manage the opportunitiesand challenges arising from healthrelated<strong>technology</strong> by optimizing decisionmakingprocesses, recognizing the value<strong>of</strong> innovation, dealing with uncertainty,and producing and coordinating HTA.WHO Medical device technical series11
5 Methods in health <strong>technology</strong> <strong>assessment</strong>As stated in a policy brief by the EuropeanObservatory on <strong>Health</strong> Systems and Policies,“in order to give an evidence-basedsolution to the problems outlined in thepolicy question, the researchers undertakingthe <strong>assessment</strong> will need to specifythe policy question in terms <strong>of</strong> safety, efficacy,effectiveness, psychological, social,ethical, organizational, pr<strong>of</strong>essional andeconomic aspects. These research questionsdetermine how the rest <strong>of</strong> the <strong>assessment</strong>will be conducted, the aspectsthat will be evaluated and those that willnot ... Formulating research questions is acrucial part <strong>of</strong> the <strong>assessment</strong>, since theytranspose the original decision-makingproblem, the policy question, into questionsthat can be answered by evaluatingscientific evidence”(5). Depending on thespecific context <strong>of</strong> the decision-making,the dimensions needed by the decisionmakermay vary. For example, hospitalbasedHTA tends to focus much moreon specific organizational dimensions,compared with HTA for decision-makingby a ministry <strong>of</strong> health.The <strong>Health</strong> <strong>technology</strong> <strong>assessment</strong>handbook by the Danish Centre for<strong>Health</strong> Technology Assessment providesan excellent overview <strong>of</strong> most <strong>of</strong> themethods needed and used internationallyin HTA (7). It is important to note thatan economic analysis is <strong>of</strong>ten, but notalways, part <strong>of</strong> an HTA. The economicdimensions may include cost-benefitanalysis, cost-utility analysis, costeffectivenessanalysis, cost-minimizationanalysis, and also budget impactanalysis and other forms <strong>of</strong> economic<strong>assessment</strong>s. As always in HTA, themethod must be appropriate for thedecision-making process to be informedby the HTA. Quality-adjusted life years(QALYs) and disability-adjusted life years(DALYs), as used in cost-utility analyses,are <strong>of</strong>ten seen as the hallmarks <strong>of</strong> HTA,but in many situations budget impactis much more important and useful fordecision-makers.Formal methods for using HTAs producedin one setting and putting them into thecontext <strong>of</strong> another setting are receivingincreasing attention. One example isthe HTA adaptation toolkit developed aspart <strong>of</strong> the European Network for HTA(EUnetHTA) collaboration (8).12<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
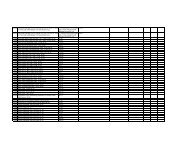
6 Links between health <strong>technology</strong> regulation,health <strong>technology</strong> management and health<strong>technology</strong> <strong>assessment</strong><strong>Health</strong> <strong>technology</strong> regulation (HTR),health <strong>technology</strong> <strong>assessment</strong> (HTA) andhealth <strong>technology</strong> management (HTM)are complementary functions to ensurethe appropriate introduction and use <strong>of</strong><strong>medical</strong> <strong>devices</strong>.While the regulatory processes concernall <strong>medical</strong> <strong>devices</strong> and drugs to somedegree, HTA is usually reserved for complexproblems. Table 1 summarizes some<strong>of</strong> the differences and complementaryroles <strong>of</strong> health <strong>technology</strong> regulationand HTA.Table 1. Comparison <strong>of</strong> health <strong>technology</strong> regulationand health <strong>technology</strong> <strong>assessment</strong>CharacteristicsPerspective<strong>Health</strong><strong>technology</strong>regulationSafety andefficacy<strong>Health</strong><strong>technology</strong><strong>assessment</strong>Efficacy,effectiveness andappropriatenessRequirement Mandatory Recommendationon complextechnologiesRole Prevent harm Maximizeclinical and costeffectivenessPractitioners from HTM and HTA have hadonly very limited interactions in the past.However, as requested in the World <strong>Health</strong>Assembly resolution WHA60.29 on healthtechnologies, Member States are urged“to formulate as appropriate nationalstrategies and plans for the establishment<strong>of</strong> systems for the <strong>assessment</strong>, planning,procurement and management <strong>of</strong> healthtechnologies in particular <strong>medical</strong><strong>devices</strong>, in collaboration with personnelinvolved in health-<strong>technology</strong> <strong>assessment</strong>and bio<strong>medical</strong> engineering”(9).It is useful to compare the dimensions<strong>of</strong> HTM and HTA to gain an appreciation<strong>of</strong> their respective contribution to policydecisions that ensure the most appropriatediffusion <strong>of</strong> health-care technologies,such as <strong>medical</strong> <strong>devices</strong>. Table 2compares HTM and HTA along severalvery broad dimensions. Understandingand supporting the synergy between HTMand HTA will be a major factor for thesuccess <strong>of</strong> national health <strong>technology</strong>policies.Table 2. Comparison <strong>of</strong> health <strong>technology</strong>management and health <strong>technology</strong> <strong>assessment</strong>Dimension<strong>Health</strong><strong>technology</strong>management<strong>Health</strong><strong>technology</strong><strong>assessment</strong>Perspective <strong>Health</strong> facility SocietalOrientation Community served Population healthMethodCriteriaProjectmanagement,<strong>technology</strong> lifecycleNeeds analysis,alternatives,specificationsSystematic criticalreview, metaanalysisClinicaleffectiveness, costeffectiveness,appropriatenessOutcome Decision Policy/decision/practiceHTR, HTA and HTM are distinctactions for enabling the best use <strong>of</strong>health technologies, especially <strong>medical</strong><strong>devices</strong>, for better health care and betterpopulation health. Close links need tobe established between the three, butit is essential to keep these activitiesseparate. For example, in order to supportdecision-making for complex problems,HTA examines all significant intendedas well as unintended consequences <strong>of</strong>WHO Medical device technical series13
<strong>technology</strong> use through multidisciplinaryanalysis, whereas the regulation processfocuses on safety and effectiveness.Therefore, the timing, procedures,objectives and resources needed aredifferent for each <strong>of</strong> them. Regardless, itis important that the outcome from eachis considered as part <strong>of</strong> decision-makingin national health <strong>technology</strong> policies.Very close links between regulation andHTA on a country level will lead to a verysuperficial use <strong>of</strong> HTA not conduciveto evidence-informed decision-making.Furthermore, as described on page 21,HTA cannot support innovation if it isamalgamated with regulation. HTR, HTA,clinical engineering and surveillance areall essential, but have specific roles in thislife-cycle <strong>of</strong> technologies (10). Figure 1illustrates the distinction <strong>of</strong> the regulatoryand management <strong>of</strong> health technologiesfor drugs and <strong>devices</strong>, and the position <strong>of</strong>HTA being independent <strong>of</strong> both.The complementary function <strong>of</strong> HTRand HTA is related to a set <strong>of</strong> questionsthat must be answered for the coherentintroduction <strong>of</strong> technologies, especially<strong>medical</strong> <strong>devices</strong>, into health systems(Figure 2).Figure 1. Domains <strong>of</strong> health <strong>technology</strong> regulation, <strong>assessment</strong> and management for drugs and <strong>devices</strong><strong>Health</strong> <strong>technology</strong>regulationSafetyPerformance(<strong>devices</strong>)Efficacy (drugs)<strong>Health</strong> <strong>technology</strong><strong>assessment</strong>Clinical effectivenessEthicsSocial issuesOrganizational<strong>Health</strong> <strong>technology</strong>managementProcurementSelectionTrainingUseFigure 2. From performance to use in health care: layers <strong>of</strong> questionsHow should the <strong>technology</strong> beimplemented in this setting?Should the <strong>technology</strong> beimplemented in this setting?Can the <strong>technology</strong> workin this setting?ImplementationAppropriatenessEffectivenessEfficacy<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong>Can the <strong>technology</strong> work?TechnicalperformanceRegulation14<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
7 <strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> for evidenceinformedcontext-based decision-makingDifferent concepts and processes havebeen promoted to increase the contribution<strong>of</strong> science to decision-making.Over the last 20 years, the concept <strong>of</strong>evidence-based and evidence-informeddecision-making has received ever increasingattention.The technical rigour <strong>of</strong> the evidence mustbe matched to the policy relevance asillustrated in Figure 3.Figure 3 underscores the importance <strong>of</strong>the need for those who create informationand knowledge to be accessible, reliableand effective in the communication anddissemination <strong>of</strong> the facts. On the otherhand, those who use the information anddata must demonstrate a commitmentto use the evidence and create policyframeworks that incentivize appropriatebehaviour and practice (11).Figure 3. Good quality evidence. Matching technical rigour to policy relevanceData providers(statisticians, evaluators,researchers)Data users(policy-makers)Need to improve dialogueHow?What?Why?WhenReliable andtrustworthyevidenceImproving‘usability’ <strong>of</strong>evidenceEffectivedisseminationWide accessGettingappropriatebuy-inIncentive touse evidenceSource: (11)WHO Medical device technical series15
Figure 4. Framework for evidence-informed policy-makingWider enabling environmentNational contextEvidence-informed (national) policy-makingInfluencesOrganizations FunctionsOrganizationalcapacityResearchpriority-settingFundingbodiesLeadership andgovernanceKnowledgegeneration anddisseminationResearchinstitutionsMediaAdvocacyorganizationsResourcesEvidencefiltering andamplificationThink tanksPolicy messagesCommunicationand networksPolicy-makingprocessesGovernmentbodiesDecision and research culture, regulations and legislationExternal fundersExternal researchinstitutionsExternal advocacyorganizationsTechnical capacity for<strong>Health</strong> Policy andSystems ResearchSource: (2)The WHO Alliance for <strong>Health</strong> Policy andSystems Research proposes a modelthat takes into account the multipleinteracting dimensions for enhancingcapacity for evidence-informed healthpolicy (Figure 4).As depicted in Figure 4, the nationalcontext plays an important role inpatterning the overall conditions forevidence-informed policy. For example,“the policy environment may vary froma closed and corrupted society to anopen, accountable and transparent one.Political and social systems influenceuse <strong>of</strong> evidence. Issues such as thetiming <strong>of</strong> evidence and availability <strong>of</strong>resources; values, beliefs and ideologyaffect its use”(2). Many countries arelabelled as “vicious circle countries”where “evidence is weak and policymakersmake little use <strong>of</strong> it. Evidencebasedpolicy-making is not practiced,which results in poor policy decisionsand poor development outcomes. In thiscase, it is necessary to adopt measureswhich will simultaneously increase boththe demand and supply <strong>of</strong> evidence, aswell as improve the dialogue betweenproducers and users <strong>of</strong> evidence” (2).If a “knowledge pull” from decisionmakersis present, HTA has shown thepotential <strong>of</strong> informing decision-makingunder a great variety <strong>of</strong> conditions.Introducing HTA into a health systemcan change the decision-makingdynamics over time. For example, inThailand, HTA has developed from beinga provider <strong>of</strong> technical information tohaving a transforming role in decisionmakingwhere “experience gained amongacademics, health <strong>of</strong>ficials, and civilsociety organizations [was] helpful notonly in sustaining the momentum butalso in improving formal HTA systems inthe future” (12).16<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
8 <strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> in healthsystems8.1 Decision-making andgovernanceThe policy-oriented nature <strong>of</strong> HTA callsfor a close integration into the functioningand governance <strong>of</strong> health systems.Strengthening the health systems <strong>of</strong>the global health community is one <strong>of</strong>the prime objectives <strong>of</strong> the CanadianSociety for International <strong>Health</strong> (CSIH).The health system model <strong>of</strong> the CSIHemphasizes the central role <strong>of</strong> evidencebaseddecision-making, both on the level<strong>of</strong> service delivery/community interventionas well as for planning and policy-making.The CSIH framework is reproduced inFigure 5.The best practice <strong>of</strong> HTA draws upon anumber <strong>of</strong> elements <strong>of</strong> this model.• HTA contextualizes global knowledgeinto the different elements <strong>of</strong> thehealth system such as human andmaterial resources, as well as relevantdata from the health system setting.• HTA supports transparent decisionmaking,and therefore participationfrom all stakeholders including civilsociety.• Equity and needs-based HTA enablesdecisions to be linked to the overallvision <strong>of</strong> equity and accountability.Figure 5. Canadian Society for International <strong>Health</strong> (CSIH) framework for strengthening health systemsVision: equity and accountabilitySocial determinants <strong>of</strong> health framework<strong>Health</strong> human resourcesStewardship and leadership<strong>Health</strong> financing andresource allocationResource for development(evidence-based planning and policy-making)<strong>Health</strong> information systemsdata for decision-makingEvidence-based decision-making(clinical and community-based)Service delivery –treatments and programmesCommunity interventionsand health promotion“<strong>Health</strong> in all policies”Strong and vibrant civil societyTransparent and accountable public/private sectorSource: (13©JHR/CSIH 2004WHO Medical device technical series17
Decision-making in health systems ispatterned by governance. For example,in health systems with hospital autonomy,an important part <strong>of</strong> new technologiesare introduced at the hospital level onthe basis <strong>of</strong> decision-making by hospitalauthorities. In such health systems, itcan be valuable for some form <strong>of</strong> HTAto be used not only at the national level,but also at the hospital level. The samereasoning applies to regionalized healthsystems. If HTA is to maximize populationhealth impact, it must take into accountthe governance structure <strong>of</strong> the specifichealth system.8.2 Institutionalized health<strong>technology</strong> <strong>assessment</strong>HTA agencies have emerged in responseto the need for a formal organizationto structure and undertake reviews <strong>of</strong>the safety, efficacy and effectiveness <strong>of</strong>health technologies. The agencies are<strong>of</strong>ten established with a mission, andprovided with financial and human resourcesto undertake systematic <strong>assessment</strong>s<strong>of</strong> public policy questions witha defined set <strong>of</strong> objectives. Most HTAactivity in high-income countries is linkedto such agencies – most being members<strong>of</strong> the International Network <strong>of</strong> Agenciesin <strong>Health</strong> Technology Assessment(INAHTA). This non-pr<strong>of</strong>it organizationhas grown to 46 member agencies from26 countries including Australia, NewZealand, and countries in North and LatinAmerica, and Europe. All members arenon-pr<strong>of</strong>it organizations producing HTAs,and are linked to regional or nationalgovernments. HTA agencies are, however,not limited to non-pr<strong>of</strong>it organizations;there are also HTA agencies that operatein the for-pr<strong>of</strong>it sectors.Over the last few years, other models<strong>of</strong> institutionalized HTA have emerged,such as hospital-based HTA (14) or HTAin regional health authorities. These morelocalized forms <strong>of</strong> HTA are following theprinciple <strong>of</strong> a close linkage <strong>of</strong> HTA to thelevels <strong>of</strong> decision-making as patternedby the governance mechanisms <strong>of</strong> thehealth system.One <strong>of</strong> the authors <strong>of</strong> this documenthas developed a framework for thedevelopment and introduction <strong>of</strong> HTAto inform practice and governancedecisions in local health authorities (15).In addition to a framework, the authorhas developed a screening procedurefor determining which technologies areworthy <strong>of</strong> consideration for a HTA (16).HTA institutions are <strong>of</strong>ten linked touniversities. For instance, in Canada,the Newfoundland and Labrador Centrefor Applied <strong>Health</strong> Research is linked tothe Memorial University <strong>of</strong> Newfoundlandand is an innovative example <strong>of</strong> explicitlycontextualizing existing researchsynthesis from HTA or other sources. As adirect result <strong>of</strong> the ever increasing role <strong>of</strong>HTA in health decision-making, industryalso harbours an increasing number <strong>of</strong>HTA-related activities.8.3 <strong>Health</strong> <strong>technology</strong><strong>assessment</strong> and innovationThe processes <strong>of</strong> HTA and innovation areintertwined. HTA started as a responseto the technological breakthrough <strong>of</strong>computer-assisted tomography (CTscans)in the early 1970s. HTA is still verymuch used to inform the decision-makingprocess concerning the introduction <strong>of</strong>new technologies to a health system.Figure 6 captures the natural life-cycle<strong>of</strong> technologies in health care.HTA is aimed at improving the uptake<strong>of</strong> cost-effective new technologies,preventing the uptake <strong>of</strong> technologiesthat are <strong>of</strong> doubtful value for the health18<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
Figure 6. <strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> and diffusion <strong>of</strong> health technologiesUseHTAMedical devicelicensingHTAHTATimeResearch anddevelopmentExperimental<strong>technology</strong>Innovative<strong>technology</strong>General useObsolescence/replacementsystem, and slowing the uptake <strong>of</strong>technologies that seem promising buthave persistent uncertainties.For some, especially industry, HTA isperceived as a hurdle to the introduction<strong>of</strong> innovative technologies into thehealth system. In this perspective, HTAis sometimes classified as the “fourthhurdle”, after the <strong>assessment</strong> <strong>of</strong> safety,efficacy and quality that are part <strong>of</strong>the regulatory requirements in manycountries (17). This view <strong>of</strong> HTA as anadditional hurdle is sometimes used asa synonym for an additional requirement<strong>of</strong> demonstrating cost-effectivenessfor coverage decisions (18). The term“fourth hurdle” is most commonly usedin relation to the coverage <strong>of</strong> new drugs,where it becomes increasingly evidentthat not only cost-effectiveness, but alsobudget impact is an important dimensionin decision-making (19). However, it isbecoming increasingly clear that HTA canbe a highly beneficial additional step formoving technologies from the laboratoryto the bedside (20).There is general concern among <strong>medical</strong>device manufacturers about the timing<strong>of</strong> HTAs in relation to the innovationprocess. The 2008 Eucomed positionpaper on HTA states that:Policy makers should considerthe implications <strong>of</strong> HTA on theenvironment needed to fosterinnovation <strong>of</strong> <strong>medical</strong> <strong>devices</strong>. IfHTA introduces significant newchallenges to market entry then thereis a potential that this may impact onthe rate <strong>of</strong> innovation in the <strong>devices</strong>ector which already faces a number<strong>of</strong> challenges. Intellectual propertyassociated with <strong>medical</strong> <strong>devices</strong>is less well protected than patentson new <strong>medical</strong> compounds. Inaddition to this, <strong>medical</strong> devicedevelopment is characterized byiterative improvement <strong>of</strong> technologiesresulting in a more rapid life-cycleand increased competition (21).Indeed, industry is one <strong>of</strong> the maincontributors to innovation in health<strong>technology</strong>. However, the innovationprocess goes beyond the development<strong>of</strong> a new device for regulatory approval.Innovation comprises both invention andexploitation, meaning an invention onlyWHO Medical device technical series19
ecomes an innovation if it is somehowadapted by the market and integrated intoa <strong>technology</strong>, process or organizationallandscape. Any innovation comprisesthree dimensions.1. Kind <strong>of</strong> innovation: What is new?Product, process, input, organizational,social.2. Subjectivity <strong>of</strong> innovation: New forwhom? Individual, group, organization,industry, society.3. Degree <strong>of</strong> innovation: How new?Market, <strong>technology</strong>, organization,environment.The Global Forum for <strong>Health</strong> Researchproposes this very short working definition<strong>of</strong> innovation: “Innovation encompassesthe entire process from the generation<strong>of</strong> new ideas to the transformation<strong>of</strong> those ideas into useful things(health services, products, methods,management practices and policies) totheir implementation” (22). In accordancewith this concept <strong>of</strong> innovation, HTA playsa major role in innovation by shaping theconditions <strong>of</strong> successful implementationin health systems.Overall, the use <strong>of</strong> HTA to inform nationalcoverage policies leads to a more explicitand transparent resource-allocationprocess, improving not only technical orallocative efficiency, but also health equity.A case study <strong>of</strong> Argentina illustratesthe importance <strong>of</strong> HTA for transparentresource allocation in countries withfragmented health systems (23). Acontext-oriented concept <strong>of</strong> innovationmay also explain the increasing use<strong>of</strong> HTA in different levels <strong>of</strong> decisionmakingwithin health systems, includinghospitals. In order to support innovation,HTA must support decision-making notonly on what to implement, but also onhow to implement a new <strong>technology</strong>.It is valuable for any discussion <strong>of</strong>innovation to take into account theoverall objective <strong>of</strong> the use <strong>of</strong> healthtechnologies for a population. In a casestudy <strong>of</strong> the Israeli health system, theinvestigators state, “Innovation playsa key role in <strong>medical</strong> progress, andcontributes significantly to public health.Reimbursement provides a significantincentive for innovation, with the tw<strong>of</strong>orming a feedback cycle. Nevertheless,it should be kept in mind that it is healththat people desire, and health <strong>technology</strong>utilization is merely the means to achieveit” (24).8.4 <strong>Health</strong> <strong>technology</strong><strong>assessment</strong> as part <strong>of</strong> goodhealth governanceIn their 2008 book Access: how dogood health technologies get to poorpeople in poor countries? Laura Frostand Michael Reich from the HarvardCentre for Population and DevelopmentStudies illustrate a number <strong>of</strong> barriersto an equitable access to beneficialhealth technologies. Their case studies“highlight the importance <strong>of</strong> expertconsensus, both within the directlyinvolved international technical agenciesand the broader international publichealth community” (25). The vision <strong>of</strong>HTA as an interdisciplinary, contextinformedapproach for evidence-basedconsensus building should be promoted.This will help build a stronger community<strong>of</strong> practice and discourse between theproducers <strong>of</strong> HTA and the policy anddecision-makers who use the information.This sets the stage for the need for goodgovernance and leadership.Arminee Kazanjian and Carolyn Green,from the University <strong>of</strong> British Columbia,Canada, pointed out that health<strong>technology</strong> <strong>assessment</strong> is a necessarypart <strong>of</strong> the public accountabilityframework in a health system (26). TheWorld Bank recently released a reportstating that “good governance as an entrypoint can help to focus on performance in20<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
health care delivery, and in turn, providepolicymakers and program managerswith a basis upon which to raiseperformance” (27). The report goes onto describe the importance <strong>of</strong> standards,incentives, information and accountabilityto ensure strong system governance andperformance (27). HTA is a standardsbasedpractice built on the foundation<strong>of</strong> the highest quality evidence and canbe held up to and be accountable for itsclaims. HTA is an essential ingredientin any health system that is seeking apolicy approach that is accountable for itsdecisions to the population <strong>of</strong> the country.WHO’s Good Governance for Medicinesprogramme has identified that theft,extortion and abuse contribute to a hugeloss <strong>of</strong> value in health services worldwide.Corruption has been identified as thesingle greatest obstacle to economic andsocial development. The programmeis raising awareness <strong>of</strong> abuse in thepharmaceutical sector and promotinggood governance. Its ultimate aim is toensure that essential medicines reachpeople – not the black market. Buildingon the momentum <strong>of</strong> WHO’s GoodGovernance for Medicines programme,HTA can become an effective processand tool for helping prevent such abuses.HTA takes a practical approach, free <strong>of</strong>bias, to objectively identifying the clinicalor economic effectiveness <strong>of</strong> a health<strong>technology</strong> (28).WHO Medical device technical series21
9 International collaboration in health<strong>technology</strong> <strong>assessment</strong>There are several international agenciessupporting the advancement <strong>of</strong> HTA onthe global stage. The following sectionreviews each <strong>of</strong> these agencies in turn toprovide an appreciation <strong>of</strong> their mission,goals and activities.9.1 <strong>Health</strong> TechnologyAssessment international(HTAi)HTAi is the global scientific and pr<strong>of</strong>essionalsociety for all those who produce, use,or encounter HTA. HTAi embraces allstakeholders, including researchers,agencies, policy-makers, industry,academia, health service providers, andpatients/consumers, and acts as a neutralforum for collaboration and the sharing <strong>of</strong>information and expertise. HTAi has over1200 members from 59 countries.The mission <strong>of</strong> HTAi is to support andpromote the development, communication,understanding and use <strong>of</strong> HTAaround the world, as a scientifically-basedand multidisciplinary means <strong>of</strong> informingdecision-making regarding the introduction<strong>of</strong> effective innovations and theefficient use <strong>of</strong> resources in health care.HTAi serves as a hub for a range <strong>of</strong>collaborative work. Its major activitiesinclude:• annual international meetings, whichserve as a major gathering pointfor global networking, informationsharing, and dissemination <strong>of</strong> latestadvances in policy, methods, andother areas <strong>of</strong> HTA research;• the HTAi Policy Forum, whichprovides a venue for open discussionbetween global leaders from HTAbodies and industry in areas <strong>of</strong>shared strategic interest;• in a number <strong>of</strong> interest sub-groups(ISGs), acting as international networksfor information exchange inspecific focus areas;• active collaborations with WHO andrelated international societies;• maintenance <strong>of</strong> a web site (www.htai.org) to share information andresources and to act as an onlinework platform for ISGs and othercollaborations;• publication <strong>of</strong> regular onlineresources, including a newsletter andwebcasts;• publication <strong>of</strong> the InternationalJournal <strong>of</strong> Technology Assessment in<strong>Health</strong> Care, HTAi’s <strong>of</strong>ficial academicjournal.Through its ISG on HTA in developingcountries, and through collaborationwith INAHTA, HTAi has made a clearcommitment to explore and promotestrategies and tools to advance accessto, and application <strong>of</strong>, HTA in developingcountries. In 2005, the HTAi specialinterest group (SIG) <strong>of</strong> experts in HTAproduced a report with INAHTA, whichwas presented to WHO as an expression<strong>of</strong> support. In the report, the authorsstate:One <strong>of</strong> the most importantchallenges to improving the quality<strong>of</strong> health systems worldwide is theneed to establish mechanisms fortransferring knowledge to action,(i.e. for bridging the “know-do”gap). Such mechanisms require22<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
the involvement <strong>of</strong> many differentconstituencies, all <strong>of</strong> whom arecommitted to achieving evidencebasedhealth policy and practice.The HTA community, with itsagencies, associations, andresearchers, has developed its rolearound contributing to this effort (29).This statement <strong>of</strong> commitment has been<strong>of</strong>fered to WHO and other agencieswishing to extend HTA into theirjurisdictions. The authors <strong>of</strong> the reportalso recognized the need for respectinglocal contextual settings and advancingthe field <strong>of</strong> HTA at a pace that is mostappropriate for the recipient country,stating:HTA aims to “globalize the evidence,localize the decision”, and, therefore,involves 2 steps. The first comprisesa systematic synthesis <strong>of</strong> the globalevidence base (i.e. systematicreviews). The second involves anappraisal <strong>of</strong> this evidence withina local or jurisdictional context,engaging local experts and decisionmakerswho play important roles inthe dissemination and utilization <strong>of</strong>the intervention. It may also includean examination <strong>of</strong> the intervention’spotential impact on the higherpopulation and policy levels (29).The authors provided a graphicalrepresentation <strong>of</strong> how HTA can be usedto inform different levels <strong>of</strong> practice,policy and decisions (Figure 7), whichshows how the chain <strong>of</strong> evidence can beoperationalized along an iterative loop <strong>of</strong>continual learning.9.2 International Network<strong>of</strong> Agencies in <strong>Health</strong>Technology Assessment(INAHTA)The International Network <strong>of</strong> Agencies in<strong>Health</strong> Technology Assessment (INAH-TA), established in 1993, is a non-pr<strong>of</strong>itorganization that in 2010 had grown to52 member agencies from 26 countries.Figure 7. Knowledge chains and learning loops: health <strong>technology</strong> <strong>assessment</strong> as a toolPolicyinterventionsResearchSynthesisAppraisalDisseminationUtilizationEvaluationPopulationinterventions(public health)ResearchSynthesisAppraisalDisseminationUtilizationEvaluationIndividualinterventions(clinical practice)ResearchSynthesisAppraisalDisseminationUtilizationEvaluationTechnologies(drugs, <strong>devices</strong>, etc.)ResearchSynthesisAppraisalDisseminationUtilizationEvaluation(Primary)researchinnovationSynthesis/<strong>assessment</strong>(global)Impact andapplicabilityappraisal(local)Dissemination Utilization EvaluationmonitoringSource: (29)WHO Medical device technical series23
All members are non-pr<strong>of</strong>it making organizationsproducing HTAs, and are linkedto regional or national governments. MostINAHTA activities are coordinated by asecretariat. The membership meets yearlyand participates in various workinggroups throughout the year. The annualmeeting is held in conjunction with theHTAi conference. The Executive Committeeand Board are elected for two-yearterms.INAHTA’s key communication forum isthe Internet. The INAHTA web site atwww.inahta.org includes informationabout ongoing activities and HTA reports.INAHTA Briefs are published regularly onthe site, and are intended as a forum formember agencies to present overviews<strong>of</strong> recently published reports. Also onthe web site are HTA checklists, whichare an aid to furthering a consistent andtransparent approach to HTA.The web site also has information on jointprojects that involve member agencies incollaborative efforts to evaluate <strong>medical</strong>technologies <strong>of</strong> mutual interest. As anexample, the INAHTA report on positronemission tomography (PET) was updatedand published in the International Journal<strong>of</strong> Technology Assessment in <strong>Health</strong>Care in 2006 (30, 31). A synthesis reportwas published in 2000 and contains asummary and analysis <strong>of</strong> five reports onpreoperative evaluation from INAHTAagencies (32). A members-only section<strong>of</strong> the site provides a platform for ongoingwork <strong>of</strong> the membership.INAHTA also produces a newsletter,which includes news on current initiativesand activities among member agencies,new projects within the Network, recentdevelopments and trends in healthpolicy research, publications in the field,and upcoming events. Other means <strong>of</strong>dissemination include participation ininternational conferences, workshops,exhibitions, and educational activities andseminars.9.3 WHO collaborating centresand their global networkWHO collaborating centres areinstitutions such as units in ministries <strong>of</strong>health, research institutes, universitiesor academies, which are designatedby the WHO Director-General to carryout activities in support <strong>of</strong> WHO’sprogrammes. In 2010, there were over800 WHO collaborating centres in 90Member States working with WHO onareas such as nursing, occupationalhealth, communicable diseases, nutrition,mental health, chronic diseases andhealth technologies.In 2009, the Global Network <strong>of</strong> WHOCollaborating Centres for HTA waslaunched during the HTAi annual meetingin Singapore. This is a network <strong>of</strong> WHOcollaborating centres involved in researchand implementation <strong>of</strong> HTA worldwide.The aim <strong>of</strong> the network is to connect thevarious collaborating centres across theworld involved directly or indirectly inHTA to promote international dialogueand collaboration and to strengthenexisting projects. This networking willlead to increased capacity for using HTAas a key tool in decision-making andpolicy-making processes, especially indeveloping and emerging countries.The network holds annual meetings <strong>of</strong>members in conjunction with the HTAiannual meetings. It also facilitatescommunication between its membersvia its web site hosted by the University<strong>of</strong> Ottawa (http://www.cgh.uottawa.ca/htanet/) and newsletters. In addition,it actively seeks opportunities forcollaboration between its members viaprojects and internships.24<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
There are currently 14 WHO collaboratingcentres with full membership to thenetwork whose work is either directly orindirectly linked to HTA.• National Center for <strong>Health</strong> TechnologyExcellence (CENETEC), Ministry <strong>of</strong><strong>Health</strong> – WHO Collaborating Centrein <strong>Health</strong> Technology in Mexico.• Fudan University Shanghai – WHOCollaborating Centre for <strong>Health</strong> TechnologyAssessment and Managementin China.• Catalan Agency for <strong>Health</strong> TechnologyAssessment and Research (CAHTA)– WHO Collaborating Centre for<strong>Health</strong> Technology Assessment inSpain.• Swedish Council on TechnologyAssessment in <strong>Health</strong> Care (SBU) –WHO Collaborating Centre for <strong>Health</strong>Technology Assessment in Sweden.• Fundação Oswaldo Cruz InstitutoOswaldo Cruz (FIOCRUZ) – WHOCollaborating Centre for Education <strong>of</strong><strong>Health</strong> Technicians in Brazil.• Institute <strong>of</strong> Population <strong>Health</strong> – WHOCollaborating Centre for KnowledgeTranslation and <strong>Health</strong> TechnologyAssessment in <strong>Health</strong> Equity inCanada.• WHO Collaborating Centre for Oral<strong>Health</strong> Research in Ireland.• WHO Collaborating Centre for Mental<strong>Health</strong> Research and Training inEgypt.• Emergency Care Research Institute –WHO Collaborating Centre for PatientSafety, Risk Management and <strong>Health</strong>Care Technology in the United States<strong>of</strong> America.• College <strong>of</strong> Nursing at Ribeirao PretoUniversity <strong>of</strong> São Paulo – WHOCollaborating Centre for NursingResearch Development in Brazil.• DHI Water and Environment and<strong>Health</strong> – WHO Collaborating Centrefor Water and <strong>Health</strong> in Denmark.• Norwegian Centre for Telemedicine(NST), University Hospital <strong>of</strong> NorthNorway – WHO Collaborating Centrefor Telemedicine in Norway.• Curtin University <strong>of</strong> Technology –WHO Collaborating Centre for Environmental<strong>Health</strong> Impact Assessmentin Australia.• CES University – WHO CollaboratingCentre for <strong>Health</strong> Technology inColombia.The network also aims to work in synergywith other existing HTA networks,including HTAi and INAHTA, in orderto galvanize the international HTAcommunity as a whole.9.4 European network for <strong>Health</strong>Technology Assessment(EUnetHTA)EUnetHTA is a European collaborationlaunched in November 2008 with 25founding partners from 15 Europeancountries. Focusing on HTA collaborationin Europe, EUnetHTA:• facilitates efficient use <strong>of</strong> resourcesavailable for HTA;• creates sustainable systems <strong>of</strong> HTAknowledge sharing;• promotes good practices in HTAmethods and processes.In addition, EUnetHTA implementsproject tools and processes, exploresrelative effectiveness principles andmethodology, and develops transparentand broad balanced engagement withidentified HTA stakeholder groups. In2009, the EUnetHTA collaboration joinedforces with European Union MemberStates and the European Commission toimplement the results <strong>of</strong> the EUnetHTAproject through a Joint Action on HTA2010–2012 (33).WHO Medical device technical series25
10 Challenges for using health <strong>technology</strong><strong>assessment</strong> in developing and emergingcountriesThe institutional dimensions are essentialfor enhancing the use <strong>of</strong> knowledge bydecision-makers. A multi-method casestudy by Lavis et al. examined theseinstitutional dimensions <strong>of</strong> evidenceinformedhealth policy in developingcountries. The authors point out:Seven recommendations emergedfor those involved in establishingor leading organizations thatsupport the use <strong>of</strong> researchevidence in developing healthpolicy: 1) collaborate with otherorganizations; 2) establish stronglinks with policymakers and involvestakeholders in the work; 3) beindependent and manage conflicts<strong>of</strong> interest among those involved inthe work; 4) build capacity amongthose working in the organization;5) use good methods and betransparent in the work; 6) startsmall, have a clear audience andscope, and address importantquestions; and 7) be attentive toimplementation considerations, evenif implementation is not a remit (34).The <strong>Health</strong> Technology Assessmentinternational interest sub-group (HTAiISG) on the use <strong>of</strong> HTA in developingcountries highlighted in their 2005 paperthe special challenges <strong>of</strong> advancing HTAfor policy, decision-making and practicein developing countries (29). The authors<strong>of</strong> the paper state:Whether within or among countries,HTA should be context-specific.Although it originated in and hasbeen used mostly in the wealthiernations, HTA is increasingly usedin low- and high-resource nationsto provide findings to inform healthcarepolicies and decisions. Further,there is increasing internationalsharing <strong>of</strong> HTA expertise,information, methods, and findings.It is also an aim among HTA agenciesand scientists in the developedcountries to assist low-incomecountries by “adopting” future localHTA activities and helping to buildup local expertise (29).For many health-care interventions,the <strong>medical</strong> evidence on safety andefficacy is applicable across populationsin different communities or countries.Indeed, evidence used in HTA can berapidly and easily shared around much<strong>of</strong> the world. However, the desirable oracceptable levels <strong>of</strong> safety, effectiveness,cost-effectiveness, and other attributes<strong>of</strong> a <strong>technology</strong>, as well as acceptabletrade-<strong>of</strong>fs among these, may vary indifferent communities, countries, or othercircumstances. As such, in HTA, it can beuseful to “globalize the evidence, localizethe decision” (35).In a presentation at the 2009 HTAiconference in Singapore, entitledNational planning and regulation underpressure, Akiko Maeda from the WorldBank presented the following conclusionsconcerning the challenges for applyingHTA in developing countries.• HTA <strong>of</strong>fers critical information on<strong>technology</strong> solutions but to date,most HTA applications have been26<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
developed for high-income countrieswith relatively well-establishedplanning and regulatory systems inplace.• To be useful for developing countries,there is a need to:››find ways to lower the cost <strong>of</strong>establishing and maintaining HTAfunctions and capacities;››better link HTA with governanceand organizational reforms indeveloping countries to generateappropriate demand (36).At the opening ceremony <strong>of</strong> the HTAi2009 meeting, the Minister <strong>of</strong> <strong>Health</strong> <strong>of</strong>Singapore, Khaw Boon Wan, stressed theimportance for developing countries toadapt global knowledge to local contexts.He urged participants to “not re-inventthe wheel’ and reaffirmed that:Asians welcome such objective,authoritative <strong>assessment</strong>s <strong>of</strong>health <strong>technology</strong>. Many do nothave as many resources for suchresearch, but this is where theglobal collaborative approach canbenefit us. We can adapt your<strong>technology</strong> <strong>assessment</strong>s for our localcontext. And some Asian countriesin a position to do so, should alsocontribute to this body <strong>of</strong> knowledge.I hope that this conference will be auseful forum for mutual learning indeveloping and enhancing decisionmakingsystems which integrateevidence from HTA, and that aresensitive to local factors (37).The HTAi ISG on HTA in developingcountries was aware <strong>of</strong> the sensitivityand different challenges <strong>of</strong> advancingthe application <strong>of</strong> HTA in developingcountries. The authors <strong>of</strong> the paperrecognized this challenge by observingthat:Certainly, implementing healthinterventions in developing countriesthat have been proven in wealthiernations has been difficult and <strong>of</strong>tendisappointing. In the completion <strong>of</strong>HTA and the transfer <strong>of</strong> findings fromone country to another, there can besubstantial differences in:• epidemiological environments (e.g.relative prevalence <strong>of</strong> communicablevs. noncommunicabledisease; acute vs. chronic disease);• physical environments;• financial resources;• health-care financing anddistribution mechanisms;• cultural acceptance <strong>of</strong> healthcareinterventions;• values for personal choice,efficiency, and equity;• <strong>technology</strong> maintenancecapacity;• civil and health-care infrastructure;• skilled human resources;• training and education;• regulatory environment;• health pr<strong>of</strong>essional standards;pr<strong>of</strong>itability <strong>of</strong> health-caremarkets (e.g. for <strong>technology</strong>companies) (29).HTAi has made an explicit commitmentto collaborate on advancing HTA aroundthe globe. In the paper from the HTAiISG on developing countries, the authorsstate, “Partnership – HTAi welcomes theopportunity to work in partnership withother agencies to develop resources forpromot(ing) the use <strong>of</strong> HTA around theworld” (29). The challenge is now for theglobal community to work with HTAi toadvance scientific evidence to informhealth practice, and to facilitate policyanddecision-making for the benefit<strong>of</strong> people in developing and emergingcountries.WHO Medical device technical series27
The Global Network <strong>of</strong> WHO CollaboratingCentres for HTA also recognizes many <strong>of</strong>these challenges and has come forwardwith approaches and next steps toaddress them. In addition, some WHOcollaborating centres have developedtoolkits that will assist in capacity buildingto incorporate HTA into decision-makingand allocate resources within local healthsystems. One such example is the Equityorientedtoolkit for HTA (38) developedby the WHO Collaborating Centre forKnowledge Translation and HTA in <strong>Health</strong>Equity, which assesses existing HTA toolsby their capability to detect differencesin impact by taking into considerationvulnerable populations.28<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
11 Strategies for developing health<strong>technology</strong> <strong>assessment</strong>11.1 Adapting the strategy to thespecific context<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> can beused and introduced in countries basedon their capability, capacity and need.Any country can access HTA knowledgethrough the international HTA database(39), but networking is essential forfinding ongoing HTA research. Thebiggest challenge however is not t<strong>of</strong>ind information, but rather to developthe capacity to use HTA information.Institutional capacity for assessing theneed for HTA, finding the information,analysing this information in relationto the specific context, and supportingdecision-makers to use the informationwill be described in this section.The appropriate use <strong>of</strong> health <strong>technology</strong><strong>assessment</strong> in a country matched againstits resource capacity can be thought <strong>of</strong>as being located along a continuum <strong>of</strong>development:i. researchers, scientists and policymakersbecome familiar with theinternational scientific literature;ii. researchers, scientists and policymakersbecome familiar with theappraisal, interpretation and potentialapplication(s) <strong>of</strong> scientific literature inthe local settings;iii. a critical mass <strong>of</strong> pr<strong>of</strong>essionals isdeveloped so that the country hasthe capacity and capability to createnew knowledge in HTA;iv. formalized mechanisms areestablished for linking the creation<strong>of</strong> knowledge to decision-makingprocesses, eventually leading t<strong>of</strong>ormal organizations.The foundation for advancing health<strong>technology</strong> <strong>assessment</strong> to developingcountries can be signalled with the 1990report <strong>of</strong> the Commission on <strong>Health</strong>Research for Development, entitled<strong>Health</strong> research: essential link to equity indevelopment (40). The report states, “Forthe health field, international functionscan be better achieved by strengtheningnational institutions within developingcountries to play both national andinternational roles, buttressed by regionaland international networking, rather thanby creating new autonomous internationalhealth research centres”(40). Whendeveloping HTA in a specific country orregion it is important to identify existingreputable and autonomous nationalresearch organizations in the country todevelop the HTA capacity.<strong>Health</strong> research systems should beconsidered as part <strong>of</strong> the country’shealth system and take into account thelarge variety <strong>of</strong> stakeholders within thecountry’s national context. A commentaryby the Council on <strong>Health</strong> Research forDevelopment (COHRED) reflects thissentiment in their statement:Furthermore, by defining a healthresearch system as “the people,institutions and activities whose aimis to generate detailed and reliableknowledge”, its boundaries arerestricted to research producers.This retrogressive definition iscontrary to the broad thrust forinclusiveness that has characterizedthe movement for health researchfor development during the lasttwo decades: by moving towardsa demand-driven model <strong>of</strong> healthresearch, decision-makers, users <strong>of</strong>WHO Medical device technical series29
esearch, civil society and mediatorshave been acknowledged as equallyimportant actors (41).The most current and importantcontribution to the advancement <strong>of</strong>health research on the internationalstage is the WHO strategy on researchfor health, which was approved by theWorld <strong>Health</strong> Assembly in May 2010.The strategy focuses on the managementand organization <strong>of</strong> research activitieswithin WHO and on support provided tocountries in organizing health researchwhen required (42). Since this is such animportant piece <strong>of</strong> work it is being usedto inform the structure and approach fordeveloping country HTA capacity.11.2 Priority setting for health<strong>technology</strong> <strong>assessment</strong>Making choices <strong>of</strong> resource allocationin health care is a complex andcontested matter. Approaches usingcost-effectiveness, QALYs, programmebudgeting marginal analysis, anddeliberative discourse are recommended.The optimal approach for priority settingin health care however is far from clear,as each technique has its own strengthsand weaknesses. A deliberative approachusing summaries <strong>of</strong> costs and benefits <strong>of</strong>options as a basis for discussion may bepreferable as it is inclusive <strong>of</strong> a wide array<strong>of</strong> participants.A balance sheet approach has beenshown to be very promising in study <strong>of</strong>a low-income setting. The authors <strong>of</strong> thepaper Combining evidence and valuesin priority setting: testing the balancesheet method in a low-income country(43) concluded that evidence-based anddeliberative decision-making does changepriorities significantly in an experimentalsetting. Their use <strong>of</strong> the balance sheetmethod was meant as a demonstrationproject but could, if properly developed,be feasible for health planners, expertsand health workers; although morework is needed before it can be used bylaypersons (43, 44).11.3 A strategy <strong>of</strong> health<strong>technology</strong> <strong>assessment</strong> focalpointsHTA could be introduced gradually byidentifying individuals with a capacityfor accessing and understanding HTAsand making these individuals the “focalpoints” <strong>of</strong> HTA and scientific evidence <strong>of</strong>effectiveness <strong>of</strong> health-care interventions.Focal points could be located in anational research organization, a nationalgovernment department, a university orother non-pr<strong>of</strong>it agencies concernedwith advancing the use <strong>of</strong> HTA for goodgovernance in policy- and decisionmaking.These individuals – hereafterreferred to as “HTA focal points” –would serve as knowledge mobilizers orambassadors <strong>of</strong> the relevant informationthat they would bring to the attention <strong>of</strong>policy- or decision-makers.The basic role <strong>of</strong> the HTA focal pointwould be to develop awareness <strong>of</strong> health<strong>technology</strong> <strong>assessment</strong> and increasethe uptake and use <strong>of</strong> HTA within adesignated country by:• developing and supporting a network<strong>of</strong> HTA stakeholders within thecountry that find HTA useful in thepolicy- and decision-making;• facilitating the flow <strong>of</strong> HTAinformation from the internationalHTA community to the country;• acting as the primary contact inthe country for HTA resources andinformation;• organizing or facilitating meetings,providing presentations andconducting workshops to helppotential users <strong>of</strong> HTA to interpretand disseminate HTA information;30<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
• identifying and articulating the HTAneeds and priorities <strong>of</strong> key audiences;• facilitating interaction betweenHTA producers and HTA users todevelop an ongoing relationship,and maintaining linkages to theinternational HTA community.The HTA focal point can also takehealth <strong>technology</strong> <strong>assessment</strong>s from theinternational literature and customizethem for appropriate utilization in theircommunities. They would work withthe data and information in the HTAsand with the country-specific data andinformation, and then merge the two sothat they provide a credible source <strong>of</strong>information to inform the policy question.Another strategy would be to introduceand develop HTA capacity within an existingorganization, such as a university orgovernment, or to establish an independentagency with the capacity to undertakehealth <strong>technology</strong> <strong>assessment</strong>s. The elementsthat contribute to an independenthigh functioning HTA agency have beenidentified and described elsewhere in theliterature (45).11.4 Building on synergisticlinkagesOn page 24, synergies were identifiedbetween and among HTAi and INAHTAinitiatives in advancing the internationalcommunity’s advancement <strong>of</strong> HTA. Thesewill be important partners and linkagesavailable to WHO at all levels as wellas the national research organizations,which function in support <strong>of</strong> the countryhealth systems.The WHO strategy on research for health(42) focuses on the management andorganization <strong>of</strong> research activities withinWHO and on support provided to countriesin organizing health research whenrequired. A fundamental component<strong>of</strong> the strategy is that WHO becomesmore familiar with using evidencebaseddecision-making methods suchas health <strong>technology</strong> <strong>assessment</strong>, at itsheadquarters, and in its regional andcountry <strong>of</strong>fices. This demonstrates asubstantive committment to HTA andevidence-based policy-making, andincreases the likelihood <strong>of</strong> HTA gainingtraction in the lower-income countries.The commitment <strong>of</strong> WHO to healthresearch and to HTA will support capacitybuilding in health research and health<strong>technology</strong> <strong>assessment</strong>, and strengthenthe advocacy for these fields. It willalso provide an improved platform forcommunicating its involvement in thecommitment to health research andhealth <strong>technology</strong> <strong>assessment</strong>.For the HTA projects to be successfuland for the WHO infrastructure to beappropriately aligned and supportive,four ingredients are necessary.Figure 9 illustrates the importance <strong>of</strong>these ingredients – good governance,funding, adequate staffing and goodcollaboration with partners – for asuccessful implementation <strong>of</strong> HTAprojects at the country level.Disseminating knowledge and skills inHTA should be based on a progressivestrategy, starting with raising awarenessby attending workshops to becomefamiliar with the concept, methods andresults <strong>of</strong> HTA, and participating in HTAand policy networks. As experience andunderstanding is gained, the next stepwill be toward improving individuals’capability in accessing, assessing,applying and contextualizing the HTA forthe country setting. The next stage wouldbe an attempt to build self-sufficiencyin the knowledge and skills by capacitybuilding with individuals in the countrythrough mentorships, distance education,in situ graduate study or post-doctoralwork. Implementation involves gainingWHO Medical device technical series31
Figure 8. Building health <strong>technology</strong> <strong>assessment</strong> awareness and capacity in WHO and in countriesEvidence-informedpolicy-makingWHOregional<strong>of</strong>ficeWHOcountry<strong>of</strong>ficeCountryexploringHTA as apolicy toolWHOheadquartersFigure 9. Ingredients for successful implementation <strong>of</strong> health <strong>technology</strong> <strong>assessment</strong> projectsGoodgovernanceFundingSuccessfulHTA projectsGoodcollaborationand partnersAdequatestaffing32<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
the experience, knowledge and skillsthat would permit countries to beginconsidering the introduction <strong>of</strong> agenciesto undertake HTAs to solve local healthcareissues. Significant experiencehas been gained by INAHTA memberagencies on mentoring individuals fromdeveloping countries who are interestedin learning HTA. One study demonstratedthat success in implementing an HTApresence in a country setting depends onfactors such as local political, economic,and educational support (46).<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> works inconcert with, and relies on, many scientificdisciplines to advance its work– epidemiology, bio<strong>medical</strong> sciences, behaviouralsciences, clinical effectivenessstudies, health economics, implementationscience, health impact analysis andevaluation are a few <strong>of</strong> many. The multidisciplinaryand interdisciplinary nature<strong>of</strong> HTA is what gives it its strength in beinga valuable tool to inform health-caredecisions and policy about what worksand what does not. This character andstrength is commensurate with the call toaction that the WHO research for healthstrategy has articulated (42). Figure 10shows how health research spans fivegeneric areas <strong>of</strong> activity, all <strong>of</strong> which aresupported by HTA.The WHO research strategy (42) has fiveinterrelated goals.1. Organization – strengthening theresearch culture across WHO.2. Priorities – reinforcing research asessential (at national, regional andglobal levels, and within WHO) inresponse to priority health needs.Figure 10. WHO call to action on health research: the five generic areas <strong>of</strong> activityImplement ordeliver solutionsthrough policiesand programmesEvaluate impacton level anddistribution <strong>of</strong> theproblemWHOresearchfor healthstrategyUnderstandcauses-biological,behavioral, social,environmentalSource: (42)Solutions forinterventions toprevent or mitigatethe problemMeasure themagnitude anddistribution <strong>of</strong> thehealth problemWHO Medical device technical series33
3. Capacity – providing support to thestrengthening <strong>of</strong> national systems forhealth research.4. Standards – promoting good practicein research, drawing on WHO’score function <strong>of</strong> setting norms andstandards.5. Translation – strengthening the linksbetween the policy, practice andproducts <strong>of</strong> research.Figure 11 illustrates the relationshipbetween the five goals <strong>of</strong> the researchfor health strategy and how they convergewith HTA to support WHO’s objectives inhealth research.The actions identified in the WHO researchfor health strategy are commensurate andsupported by the approach <strong>of</strong> HTA toinform practice, policy and decisions.HTA can help to achieve the goals andobjectives <strong>of</strong> WHO’s research for healthstrategy through specific initiativesestablished within the country projects.Regional WHO-supported networkssupporting evidence-informed decisionmaking,such as the Evidence-InformedPolicy Network (EVIPN: http://www.who.int/rpc/evipnet/) should be linked to HTAprojects.Figure 11. Convergence <strong>of</strong> the goals <strong>of</strong> WHO’s research for health strategy and the goals <strong>of</strong> health <strong>technology</strong><strong>assessment</strong>Source: adapted from (42)34<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
12 Concluding remarksOver the last decades, HTA has emerged asa powerful paradigm for institutionalizingevidence-based and evidence-informeddecision-making for health policies.Appropriate HTA strategies enabledeveloping and emerging countries tocontextualize global knowledge, supporttransparent and accountable decisionmaking,and promote health equity.Linking knowledge with action is one <strong>of</strong>the greatest challenges <strong>of</strong> the global healthsystem. This linkage is <strong>of</strong>ten achievedthrough innovations, which commonlystart with basic research that is translatedinto new health technologies. Thesetechnologies must be delivered to thosein need <strong>of</strong> them (47). HTA is an importanttool for supporting these core functions<strong>of</strong> an effective global health system.Actions by WHO and other global healthorganizations are needed to support theeffective development <strong>of</strong> HTA.WHO Medical device technical series35
References1. Szlezák NA et al. The global health system: actors, norms, and expectations intransition. PLoS Medicine, 2010, 7(1): e1000183.2. Green A, Bennett S, eds. Sound choices: enhancing capacity for evidenceinformedhealth policy. Geneva, World <strong>Health</strong> Organization, 2007.3. Jonsson E, Banta D. Management <strong>of</strong> health technologies: an international view.British Medical Journal, 1999, 319(7220):1293.4. HTA glossary. International Network <strong>of</strong> Agencies for <strong>Health</strong> Technology Assessmentand <strong>Health</strong> Technology Assessment international (http://www.htaglossary.net/,accessed November 2010).5. Velasco-Garrido M, Busse R. <strong>Health</strong> <strong>technology</strong> <strong>assessment</strong>: an introduction toobjectives, role <strong>of</strong> evidence, and structure in Europe. Copenhagen, World <strong>Health</strong>Organization Regional Office for Europe, on behalf <strong>of</strong> the European Observatoryon <strong>Health</strong> Systems and Policies, 2005.6. <strong>Health</strong> technologies and decision making. Paris, Organisation for Economic Cooperationand Development (OECD), 2005.7. Børlum Kristensen F, Sigmund H, eds. <strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> handbook.Copenhagen, National Board <strong>of</strong> <strong>Health</strong>, 2008 (http://www.sst.dk/publ/Publ2008/MTV/Metode/HTA_Handbook_net_final.pdf, accessed November 2010).8. Chase D et al. Development <strong>of</strong> a toolkit and glossary to aid in the adaptation <strong>of</strong>health <strong>technology</strong> <strong>assessment</strong> (HTA) reports for use in different contexts. <strong>Health</strong>Technology Assessment, 2009, 13:59.9. Resolution WHA60.29. <strong>Health</strong> technologies. In: Sixtieth World <strong>Health</strong> Assembly.Resolutions and decisions. Geneva, World <strong>Health</strong> Organization, 2007.10. Mytton O et al. Introducing new <strong>technology</strong> safely. Quality and Safety in <strong>Health</strong>Care, 2010, 19(Suppl.2):i9.11. Segone M ed. Country-led monitoring and evaluation systems: better evidence,better policies, better development results. New York, UNICEF, 2009.12. Teerawattananon Y et al. Historical development <strong>of</strong> health <strong>technology</strong> <strong>assessment</strong>in Thailand. International Journal <strong>of</strong> Technology Assessment in <strong>Health</strong> Care, 2009,25(S1):241–252.36<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
13. Canadian Society for International <strong>Health</strong> web site (http://csih.org/en/, accessedNovember 2010).14. McGregor M, Brophy J. End-user involvement in health <strong>technology</strong> <strong>assessment</strong>(HTA) development: a way to increase impact. International Journal <strong>of</strong> TechnologyAssessment in <strong>Health</strong> Care, 2005, 21(02):263–267.15. Juzwishin D. Framework for regional health authorities to make optimal use<strong>of</strong> health <strong>technology</strong> <strong>assessment</strong>. Edmonton, Alberta Heritage Foundation forMedical Research, 2000.16. Juzwishin D, Schneider W. Screening procedure for use when considering theimplementation <strong>of</strong> health <strong>technology</strong>. Edmonton, Alberta Heritage Foundation forMedical Research, 2002.17. Managing the fourth hurdle: small medtech companies addressing the issue <strong>of</strong>reimbursement. Stockholm, Karolinska Institutet, 2008 (http://www.ideon.se/fileadmin/uploads/Pdf_er/Ideonaktuellt/2009/Managing_the_Fourth_Hurdle.pdf,accessed November 2010).18. Taylor R et al. Inclusion <strong>of</strong> cost effectiveness in licensing requirements <strong>of</strong> newdrugs: the fourth hurdle. British Medical Journal, 2004, 329(7472):972.19. Cohen J, Stolk E, Niezen M. The increasingly complex fourth hurdle forpharmaceuticals. Pharmacoeconomics, 2007, 25(9):727–734.20. Rogowski WH, Hartz SC, John JH. Clearing up the hazy road from bench tobedside: a framework for integrating the fourth hurdle into translational medicine.BMC <strong>Health</strong> Services Research, 2008, 8:194.21. Eucomed HTA Position Paper. Brussels, Eucomed, 2008.22. Gardner C. What is innovation? Dgroups: development through dialogue.2009 (http://dgroups.org/ViewDiscussion.aspx?c=74761344-a1cc-4b5a-ad08-d5126a480b62&i=9b475979-a01e-4120-a7b4-bccd0df82f35, accessedNovember 2010).23. Rubinstein A, Pichon-Riviere A, Augustovski F. Development and implementation<strong>of</strong> health <strong>technology</strong> <strong>assessment</strong> in Argentina: two steps forward and one stepback. International Journal <strong>of</strong> Technology Assessment in <strong>Health</strong> Care, 2009,25(S1):260–269.24. Shavit O. Utilization <strong>of</strong> health technologies – do not look where there is a light;shine your light where there is a need to look! Relating national health goals withresource allocation decision-making; illustration through examining the Israelihealthcare system. <strong>Health</strong> Policy, 2009, 92(2–3):268–275.25. Frost L, Reich MR. Access: how do good health technologies get to poor people inpoor countries? Harvard Center for Population and Development Studies, 2008.WHO Medical device technical series37
26. Kazanjian A, Green C. <strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> within a public accountabilityframework. Clinical Governance: An International Journal, 2004, 9(1):51–58.27. Lewis M, Pettersson G, Bank W. Governance in health care delivery: raisingperformance. Washington, World Bank, 2009.28. Good governance for medicines. Geneva, World <strong>Health</strong> Organization (http://www.who.int/medicines/ggm/en/, accessed November 2010).29. Resources for health <strong>technology</strong> <strong>assessment</strong>. <strong>Health</strong> Technology Assessmentinternational and the International Network <strong>of</strong> Agencies for <strong>Health</strong> TechnologyAssessment, 2005 (http://www.inahta.org/upload/HTA_resources/AboutHTA_Resources_for_HTA.pdf, accessed November 2010).30. Hastings J, Adams EJ. Joint project <strong>of</strong> the International Network <strong>of</strong> Agencies for<strong>Health</strong> Technology Assessment part 1: survey results on diffusion, <strong>assessment</strong>,and clinical use <strong>of</strong> positron emission tomography. International Journal <strong>of</strong>Technology Assessment in <strong>Health</strong> Care, 2006, 22(2):143–8.31. Adams EJ et al. Joint project <strong>of</strong> the International Network <strong>of</strong> Agencies for<strong>Health</strong> Technology Assessment part 2: managing the diffusion <strong>of</strong> positronemission tomography with health <strong>technology</strong> <strong>assessment</strong>. International Journal<strong>of</strong> Technology Assessment in <strong>Health</strong> Care, 2006, 22(2):149–54.32. Asua J, López-Argumedo M. Preoperative evaluation in elective surgery.International Journal <strong>of</strong> Technology Assessment in <strong>Health</strong> Care, 2000, 16:673–683.33. EUnetHTA Joint Action 2010–12, EUnetHTA (http://www.eunethta.net/Public/Work_Packages/EUnetHTA-Joint-Action-2010-12/, accessed November 2010).34. Lavis J et al. Evidence-informed health policy synthesis <strong>of</strong> findings from amulti-method study <strong>of</strong> organizations that support the use <strong>of</strong> research evidence.Implementation Science, 2008, 3:53.35. Eisenberg J. Globalize the evidence, localize the decision: evidence-basedmedicine and international diversity. <strong>Health</strong> Affairs, 2002, 21(3):166.36. Maeda A. National planning and regulation under pressure: application <strong>of</strong> HTA indeveloping countries. Presentation at the 6th HTAi annual meeting, 2009 (http://www.htai2009.org/slides/Plenaries%20and%20Breakout%20Sessions/PL1%20-%20Globalization%20and%20HTA-How%20Much%20Impact%20does%20Globalization%20H/Akiko%20MAEDA.pdf, accessed November 2010).37. Wan KB. Costlier care, better health? Opening speech at the 6th HTAi annualmeeting, 2009 (http://www.moh.gov.sg/mohcorp/speeches.aspx?id=22234,accessed November 2010).38<strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> <strong>of</strong> <strong>medical</strong> <strong>devices</strong>
38. Equity oriented toolkit. Ottawa, WHO Collaborating Centre for Knowledge Translationand <strong>Health</strong> Technology Assessment in <strong>Health</strong> Equity (http://www.cgh.uottawa.ca/whocc/projects/eo_toolkit/index.htm, accessed December 2010).39. <strong>Health</strong> <strong>technology</strong> <strong>assessment</strong> (HTA) database [online database] National Institutefor <strong>Health</strong> Research, Centres for Review and Dissemination (http://www.crd.york.ac.uk/crdweb/Home.aspx?DB=HTA, accessed November 2010).40. <strong>Health</strong> research: essential link to health equity. Cambridge, Commission on <strong>Health</strong>Research for Development, 1990.41. Jacobs M, Haan S. <strong>Health</strong> research systems: an evolving framework. Bulletin <strong>of</strong>the World <strong>Health</strong> Organization, 2003, 81:624–624.42. WHO’s role and responsibilities in health research: Draft WHO strategy on researchfor health. Report by the Secretariat to the Sixty-third World <strong>Health</strong> Assembly,Geneva, World <strong>Health</strong> Organization, 2010.43. Makundi E, Kapiriri L, Norheim O. Combining evidence and values in prioritysetting: testing the balance sheet method in a low-income country. BMC <strong>Health</strong>Services Research, 2007, 7(1):152.44. Noorani H et al. Priority setting for health <strong>technology</strong> <strong>assessment</strong>s: A systematicreview <strong>of</strong> current practical approaches. International Journal <strong>of</strong> TechnologyAssessment in <strong>Health</strong> Care, 2007, 23:310–315.45. Hailey D. Elements <strong>of</strong> effectiveness for health <strong>technology</strong> <strong>assessment</strong> programs.Edmonton, Alberta Heritage Foundation for Medical Research, 2003.46. Corabian P et al. Mentoring a developing health <strong>technology</strong> <strong>assessment</strong> initiativein Romania: an example for countries with limited experience <strong>of</strong> assessing health<strong>technology</strong>. International Journal <strong>of</strong> Technology Assessment in <strong>Health</strong> Care, 2005,21:522–525.47. Keusch G et al. The global health system: linking knowledge with action—learningfrom malaria. PLoS Medicine, 2010, 7(1):e1000193.WHO Medical device technical series39
Department <strong>of</strong> Essential <strong>Health</strong> TechnologiesWorld <strong>Health</strong> Organization20 Avenue AppiaCH-1211 Geneva 27SwitzerlandTel: +41 22 791 21 11E-mail: <strong>medical</strong><strong>devices</strong>@who.inthttp://www.who.int/<strong>medical</strong>_<strong>devices</strong>/en/ISBN 978 92 4 150136 1