WHO Guidelines on Drawing Blood: Best Practices in Phlebotomy
WHO Guidelines on Drawing Blood: Best Practices in Phlebotomy
WHO Guidelines on Drawing Blood: Best Practices in Phlebotomy
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es<br />
<strong>on</strong> draw<strong>in</strong>g blood:<br />
best practices <strong>in</strong><br />
phlebotomy
<str<strong>on</strong>g>WHO</str<strong>on</strong>g> Library Catalogu<strong>in</strong>g-<strong>in</strong>-Publicati<strong>on</strong> Data<br />
<str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy.<br />
1.<strong>Blood</strong>lett<strong>in</strong>g – standards. 2.<strong>Phlebotomy</strong> – standards. 3.Needlestick <strong>in</strong>juries – preventi<strong>on</strong> and<br />
c<strong>on</strong>trol. 4.<str<strong>on</strong>g>Guidel<strong>in</strong>es</str<strong>on</strong>g>. I.World Health Organizati<strong>on</strong>.<br />
ISBN 978 92 4 159922 1 (NLM classificati<strong>on</strong>: WB 381)<br />
© World Health Organizati<strong>on</strong> 2010<br />
All rights reserved. Publicati<strong>on</strong>s of the World Health Organizati<strong>on</strong> can be obta<strong>in</strong>ed from <str<strong>on</strong>g>WHO</str<strong>on</strong>g><br />
Press, World Health Organizati<strong>on</strong>, 20 Avenue Appia, 1211 Geneva 27, Switzerland<br />
(tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: bookorders@who.<strong>in</strong>t). Requests for<br />
permissi<strong>on</strong> to reproduce or translate <str<strong>on</strong>g>WHO</str<strong>on</strong>g> publicati<strong>on</strong>s – whether for sale or for n<strong>on</strong>commercial<br />
distributi<strong>on</strong> – should be addressed to <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Press, at the above address (fax: +41 22 791 4806;<br />
e-mail: permissi<strong>on</strong>s@who.<strong>in</strong>t).<br />
The designati<strong>on</strong>s employed and the presentati<strong>on</strong> of the material <strong>in</strong> this publicati<strong>on</strong> do not<br />
imply the expressi<strong>on</strong> of any op<strong>in</strong>i<strong>on</strong> whatsoever <strong>on</strong> the part of the World Health Organizati<strong>on</strong><br />
c<strong>on</strong>cern<strong>in</strong>g the legal status of any country, territory, city or area or of its authorities, or<br />
c<strong>on</strong>cern<strong>in</strong>g the delimitati<strong>on</strong> of its fr<strong>on</strong>tiers or boundaries. Dotted l<strong>in</strong>es <strong>on</strong> maps represent<br />
approximate border l<strong>in</strong>es for which there may not yet be full agreement.<br />
The menti<strong>on</strong> of specific companies or of certa<strong>in</strong> manufacturers’ products does not imply that<br />
they are endorsed or recommended by the World Health Organizati<strong>on</strong> <strong>in</strong> preference to others<br />
of a similar nature that are not menti<strong>on</strong>ed. Errors and omissi<strong>on</strong>s excepted, the names of<br />
proprietary products are dist<strong>in</strong>guished by <strong>in</strong>itial capital letters.<br />
All reas<strong>on</strong>able precauti<strong>on</strong>s have been taken by the World Health Organizati<strong>on</strong> to verify<br />
the <strong>in</strong>formati<strong>on</strong> c<strong>on</strong>ta<strong>in</strong>ed <strong>in</strong> this publicati<strong>on</strong>. However, the published material is be<strong>in</strong>g<br />
distributed without warranty of any k<strong>in</strong>d, either expressed or implied. The resp<strong>on</strong>sibility for the<br />
<strong>in</strong>terpretati<strong>on</strong> and use of the material lies with the reader. In no event shall the World Health<br />
Organizati<strong>on</strong> be liable for damages aris<strong>in</strong>g from its use.<br />
Pr<strong>in</strong>ted by the <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Document Producti<strong>on</strong> Services, Geneva, Switzerland
C<strong>on</strong>tents<br />
Acknowledgements.........................................................................................................................vii<br />
Acr<strong>on</strong>yms..........................................................................................................................................xi<br />
Executive summary.........................................................................................................................xiii<br />
PART I BACKGROUND...................................................................................................................... 1<br />
1 Introducti<strong>on</strong> ............................................................................................................................... 3<br />
1.1 Overview ..................................................................................................................................... 3<br />
1.1.1 Issues <strong>in</strong> phlebotomy........................................................................................................ 3<br />
1.1.2 The need for guidel<strong>in</strong>es.................................................................................................... 4<br />
1.1.3 Def<strong>in</strong>iti<strong>on</strong>s........................................................................................................................ 4<br />
1.2 Purpose and scope....................................................................................................................... 5<br />
1.3 Objectives..................................................................................................................................... 5<br />
1.4 Target audience............................................................................................................................ 5<br />
1.5 Indicati<strong>on</strong>s for blood sampl<strong>in</strong>g and blood collecti<strong>on</strong>................................................................... 5<br />
1.6 Structure of document................................................................................................................. 6<br />
PART II ASPECTS OF PHLEBOTOMY................................................................................................... 7<br />
2 <strong>Best</strong> practices <strong>in</strong> phlebotomy....................................................................................................... 9<br />
2.1 Background <strong>in</strong>formati<strong>on</strong> <strong>on</strong> best practices <strong>in</strong> phlebotomy.......................................................... 9<br />
2.1.1 Plann<strong>in</strong>g ahead................................................................................................................. 9<br />
2.1.2 Us<strong>in</strong>g an appropriate locati<strong>on</strong>.......................................................................................... 9<br />
2.1.3 Quality c<strong>on</strong>trol.................................................................................................................. 9<br />
2.1.4 Quality care for patients and health workers................................................................. 10<br />
2.1.5 Quality of laboratory sampl<strong>in</strong>g....................................................................................... 11<br />
2.2 Practical guidance <strong>on</strong> best practices <strong>in</strong> phlebotomy.................................................................. 12<br />
2.2.1 Provisi<strong>on</strong> of an appropriate locati<strong>on</strong>.............................................................................. 12<br />
2.2.2 Provisi<strong>on</strong> of clear <strong>in</strong>structi<strong>on</strong>s........................................................................................ 12<br />
2.2.3 Procedure for draw<strong>in</strong>g blood.......................................................................................... 12<br />
2.3 Illustrati<strong>on</strong>s for best practices <strong>in</strong> phlebotomy............................................................................ 18<br />
3 <strong>Blood</strong>-sampl<strong>in</strong>g systems .............................................................................................................21<br />
3.1 Background <strong>in</strong>formati<strong>on</strong> <strong>on</strong> blood-sampl<strong>in</strong>g systems................................................................ 21<br />
3.1.1 Closed systems............................................................................................................... 21<br />
3.1.2 Open systems................................................................................................................. 22<br />
3.2 Practical guidance <strong>on</strong> blood-sampl<strong>in</strong>g systems.......................................................................... 22<br />
3.2.1 Needle and syr<strong>in</strong>ge......................................................................................................... 22<br />
3.2.2 Choice of gauge ............................................................................................................. 22<br />
3.3 Illustrati<strong>on</strong>s for blood-sampl<strong>in</strong>g systems.................................................................................... 23<br />
4 Venepuncture for blood d<strong>on</strong>ati<strong>on</strong> ..............................................................................................25<br />
4.1 Background <strong>in</strong>formati<strong>on</strong> <strong>on</strong> venepuncture for blood d<strong>on</strong>ati<strong>on</strong>................................................. 25<br />
4.1.1 M<strong>in</strong>imum requirements for venepuncture for blood d<strong>on</strong>ati<strong>on</strong> ..................................... 25<br />
4.1.2 Before a blood d<strong>on</strong>ati<strong>on</strong>................................................................................................. 26<br />
4.2 Practical guidance <strong>on</strong> venepuncture for blood d<strong>on</strong>ati<strong>on</strong>........................................................... 27<br />
4.2.1 Collect<strong>in</strong>g blood.............................................................................................................. 27<br />
4.2.2 After a blood d<strong>on</strong>ati<strong>on</strong>................................................................................................... 28<br />
4.2.3 Adverse events <strong>in</strong> blood d<strong>on</strong>ati<strong>on</strong>.................................................................................. 29<br />
5 Arterial blood sampl<strong>in</strong>g .............................................................................................................31<br />
5.1 Background <strong>in</strong>formati<strong>on</strong> <strong>on</strong> arterial blood sampl<strong>in</strong>g ................................................................ 31<br />
5.1.1 Choice of site.................................................................................................................. 31<br />
5.1.2 Complicati<strong>on</strong>s related to arterial blood sampl<strong>in</strong>g.......................................................... 31<br />
5.1.3 Sampl<strong>in</strong>g errors............................................................................................................... 32<br />
5.2 Practical guidance <strong>on</strong> arterial blood sampl<strong>in</strong>g........................................................................... 32<br />
5.2.1 Equipment and supplies................................................................................................. 32<br />
5.2.2 Procedure for arterial blood sampl<strong>in</strong>g us<strong>in</strong>g radial artery ............................................. 32<br />
5.3 Illustrati<strong>on</strong>s for arterial blood sampl<strong>in</strong>g..................................................................................... 33<br />
<br />
iii
6 Paediatric and ne<strong>on</strong>atal blood sampl<strong>in</strong>g.....................................................................................35<br />
6.1 Background <strong>in</strong>formati<strong>on</strong> <strong>on</strong> paediatric and ne<strong>on</strong>atal blood sampl<strong>in</strong>g....................................... 35<br />
6.1.1 Choice of procedure and site ......................................................................................... 35<br />
6.2 Practical guidance <strong>on</strong> paediatric and ne<strong>on</strong>atal blood sampl<strong>in</strong>g................................................. 35<br />
6.2.1 Patient identificati<strong>on</strong> ..................................................................................................... 35<br />
6.2.2 Venepuncture................................................................................................................. 36<br />
6.2.3 F<strong>in</strong>ger and heel-prick ..................................................................................................... 37<br />
6.3 Illustrati<strong>on</strong>s for paediatric and ne<strong>on</strong>atal blood sampl<strong>in</strong>g........................................................... 37<br />
7 Capillary sampl<strong>in</strong>g......................................................................................................................41<br />
7.1 Background <strong>in</strong>formati<strong>on</strong> <strong>on</strong> capillary sampl<strong>in</strong>g.......................................................................... 41<br />
7.1.1 Choice of site ................................................................................................................. 41<br />
7.1.2 Select<strong>in</strong>g the length of lancet......................................................................................... 42<br />
7.1.3 Order of draw................................................................................................................. 42<br />
7.1.4 Complicati<strong>on</strong>s................................................................................................................. 42<br />
7.2 Practical guidance <strong>on</strong> capillary sampl<strong>in</strong>g.................................................................................... 43<br />
7.2.1 Selecti<strong>on</strong> of site and lancet............................................................................................. 43<br />
7.2.2 Procedure for capillary sampl<strong>in</strong>g.................................................................................... 43<br />
7.3 Illustrati<strong>on</strong>s for capillary sampl<strong>in</strong>g............................................................................................. 45<br />
PART III IMPLEMENTATION, EVALUATION AND MONITORING..........................................................47<br />
8 Implement<strong>in</strong>g best phlebotomy practices...................................................................................49<br />
8.1 Sett<strong>in</strong>g policies and standard operat<strong>in</strong>g procedures.................................................................. 49<br />
8.2 Procurement.............................................................................................................................. 49<br />
8.2.1 <strong>Blood</strong>-sampl<strong>in</strong>g equipment............................................................................................ 50<br />
8.2.2 Protecti<strong>on</strong>....................................................................................................................... 50<br />
8.3 <strong>Phlebotomy</strong> tra<strong>in</strong><strong>in</strong>g................................................................................................................... 51<br />
8.4 Safe waste and sharps disposal.................................................................................................. 51<br />
8.5 Preventi<strong>on</strong> and management of <strong>in</strong>cidents and adverse events................................................. 52<br />
8.5.1 Patient related................................................................................................................ 52<br />
8.5.2 Health-worker related.................................................................................................... 53<br />
8.5.3 Risk assessment and risk reducti<strong>on</strong> strategies................................................................ 54<br />
9 M<strong>on</strong>itor<strong>in</strong>g and evaluati<strong>on</strong>.........................................................................................................55<br />
PART IV REFERENCES......................................................................................................................57<br />
PART V ANNEXES............................................................................................................................63<br />
Annex A: Methods and evidence base...........................................................................................65<br />
Annex B: Infecti<strong>on</strong> preventi<strong>on</strong> and c<strong>on</strong>trol, safety equipment and best practice............................69<br />
Annex C:<br />
Devices available for draw<strong>in</strong>g blood................................................................................71<br />
Annex D: Manag<strong>in</strong>g occupati<strong>on</strong>al exposure to hepatitis B, hepatitis C and HIV...............................73<br />
Annex E: Tra<strong>in</strong><strong>in</strong>g course c<strong>on</strong>tent for phlebotomists .....................................................................77<br />
Annex F:<br />
Expla<strong>in</strong><strong>in</strong>g the procedure to a patient.............................................................................79<br />
Annex G: Disassembly of needle from syr<strong>in</strong>ge or other devices......................................................81<br />
Annex H: <strong>Blood</strong> spillage ................................................................................................................83<br />
Annex I:<br />
Annex J:<br />
Modified Allen test.........................................................................................................85<br />
Cochrane review.............................................................................................................87<br />
Annex references...........................................................................................................................103<br />
Glossary ........................................................................................................................................105<br />
iv<br />
<str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Tables<br />
Table 2.1 Elements of quality assurance <strong>in</strong> phlebotomy.................................................................... 10<br />
Table 2.2 Infecti<strong>on</strong> preventi<strong>on</strong> and c<strong>on</strong>trol practices......................................................................... 12<br />
Table 2.3 Recommended order of draw for plastic vacuum tubes..................................................... 16<br />
Table 3.1 Recommended needle gauge, length and device for rout<strong>in</strong>e <strong>in</strong>jecti<strong>on</strong> and<br />
phlebotomy procedures for different age groups............................................................... 22<br />
Table 4.1 Adverse events <strong>in</strong> blood d<strong>on</strong>ati<strong>on</strong> ..................................................................................... 29<br />
Table 7.1 C<strong>on</strong>diti<strong>on</strong>s <strong>in</strong>fluenc<strong>in</strong>g the choice of heel or f<strong>in</strong>ger-prick................................................... 41<br />
Table 8.1 Summary of risks and risk-reducti<strong>on</strong> strategies.................................................................. 54<br />
Table B.1 Recommendati<strong>on</strong>s for <strong>in</strong>fecti<strong>on</strong> preventi<strong>on</strong> and c<strong>on</strong>trol, safety equipment<br />
and best practice................................................................................................................. 69<br />
Table C.1 Devices for draw<strong>in</strong>g blood.................................................................................................. 71<br />
Table D.1 Recommendati<strong>on</strong>s for HBV post-exposure prophylaxis, accord<strong>in</strong>g to immune status....... 74<br />
Table D.2 Recommended two and three-drug post-exposure prophylaxis regimens......................... 75<br />
<br />
v
Acknowledgements<br />
The World Health Organizati<strong>on</strong> (<str<strong>on</strong>g>WHO</str<strong>on</strong>g>) Injecti<strong>on</strong> Safety and Related Infecti<strong>on</strong> C<strong>on</strong>trol<br />
programme and the Safe Injecti<strong>on</strong> Global Network (SIGN) Secretariat <strong>in</strong> the <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Department<br />
of Essential Health Technologies (EHT) wish to express their thanks to the people listed below<br />
for their c<strong>on</strong>tributi<strong>on</strong> to the development of these phlebotomy guidel<strong>in</strong>es. The authors and<br />
reviewers are experts <strong>in</strong> the field of <strong>in</strong>jecti<strong>on</strong> safety and related <strong>in</strong>fecti<strong>on</strong> c<strong>on</strong>trol. Particular<br />
thanks go to Shaheen Mehtar of Stellenbosch University, South Africa, who prepared<br />
background documents for the c<strong>on</strong>sultati<strong>on</strong>, and wrote the <strong>in</strong>itial and f<strong>in</strong>al drafts.<br />
Development of this publicati<strong>on</strong> was supported by Cooperative Agreement CDC-RFA-CI09-903<br />
from:<br />
• the Department of Health and Human Services/Centers for Disease C<strong>on</strong>trol and Preventi<strong>on</strong><br />
(CDC), Atlanta, United States of America (USA);<br />
• the Nati<strong>on</strong>al Center for HIV, Viral Hepatitis, STD, and TB Preventi<strong>on</strong>, Global AIDS<br />
Program (GAP).<br />
Technical authors and ma<strong>in</strong> reviewers<br />
Internal authors and reviewers (<str<strong>on</strong>g>WHO</str<strong>on</strong>g>)<br />
Dr Neelam Dh<strong>in</strong>gra<br />
Coord<strong>in</strong>ator<br />
<strong>Blood</strong> Transfusi<strong>on</strong> Safety (BTS)<br />
<str<strong>on</strong>g>WHO</str<strong>on</strong>g> Headquarters (<str<strong>on</strong>g>WHO</str<strong>on</strong>g>/HQ), Health Systems and Services, Department of Essential Health<br />
Technologies (HSS/EHT)<br />
Dr Michel<strong>in</strong>e Diepart<br />
Antiretroviral Treatment and HIV Care<br />
<str<strong>on</strong>g>WHO</str<strong>on</strong>g>/HQ, Department of HIV/AIDS (<str<strong>on</strong>g>WHO</str<strong>on</strong>g>/HQ/HTM/HIV)<br />
Dr Gerald Dziekan<br />
Program Manager<br />
<str<strong>on</strong>g>WHO</str<strong>on</strong>g> Patient Safety Program (PSP)<br />
<str<strong>on</strong>g>WHO</str<strong>on</strong>g>/HQ, Department of Informati<strong>on</strong>, Evidence and Research (IER)<br />
Dr Selma Khamassi, MD, MSc<br />
Injecti<strong>on</strong> Safety and Related Infecti<strong>on</strong> C<strong>on</strong>trol<br />
SIGN Secretariat<br />
<str<strong>on</strong>g>WHO</str<strong>on</strong>g>/HQ/HSS/EHT/Diagnostic Imag<strong>in</strong>g and Medical Devices (DIM)<br />
Dr Fernando Otaiza, MD, MSc, Infecti<strong>on</strong> Preventi<strong>on</strong> and C<strong>on</strong>trol <strong>in</strong> Health Care<br />
Biorisk Reducti<strong>on</strong> for Dangerous Pathogens<br />
<str<strong>on</strong>g>WHO</str<strong>on</strong>g> Department of Epidemic and Pandemic Alert and Resp<strong>on</strong>se<br />
Mrs Susan Wilburn<br />
<str<strong>on</strong>g>WHO</str<strong>on</strong>g>, Department of Occupati<strong>on</strong>al and Envir<strong>on</strong>mental Health (OEH)<br />
Acknowledgements<br />
vii
External authors and reviewers<br />
Dr Rana Al-Abdulrazzak<br />
Head of D<strong>on</strong>ati<strong>on</strong> Department & Hospital Liais<strong>on</strong> Department<br />
Kuwait Central <strong>Blood</strong> Bank<br />
Kuwait<br />
Ms Patricia K Bertsche<br />
Manager, Global Occupati<strong>on</strong>al Health Services<br />
Abbott Laboratories<br />
USA<br />
Dr Nizam Damani<br />
Internati<strong>on</strong>al Federati<strong>on</strong> of Infecti<strong>on</strong> C<strong>on</strong>trol<br />
Northern Ireland<br />
Dr Che-Kit L<strong>in</strong><br />
Hospital Chief Executive<br />
H<strong>on</strong>g K<strong>on</strong>g Red Cross <strong>Blood</strong> Transfusi<strong>on</strong> Service<br />
H<strong>on</strong>g K<strong>on</strong>g<br />
Dr Lawrence Marum<br />
Team Leader Medical Transmissi<strong>on</strong><br />
Global AIDS Program, HIV Preventi<strong>on</strong> Branch<br />
CDC, Atlanta, USA<br />
Professor Shaheen Mehtar<br />
Head of Academic Unit for Infecti<strong>on</strong> Preventi<strong>on</strong> and C<strong>on</strong>trol<br />
Tygerberg Hospital and Stellenbosch University, Cape Town<br />
South Africa<br />
Dr Joseph Perz<br />
Act<strong>in</strong>g Team Leader, Research and Field Investigati<strong>on</strong>s<br />
Epidemiology and Surveillance Branch<br />
Divisi<strong>on</strong> of Healthcare Quality Promoti<strong>on</strong> (DHQP)<br />
CDC, Atlanta, USA<br />
Dr Ruby Pietersz<br />
Manager of Department of Research and Educati<strong>on</strong><br />
Plesmanlaan 125, 1066 CX<br />
Amsterdam<br />
The Netherlands<br />
Dr Christie Reed<br />
HIV Preventi<strong>on</strong> Branch<br />
Global AIDS Program<br />
CDC, Atlanta, USA<br />
Dr Dejana Selenic<br />
HIV Preventi<strong>on</strong> Branch<br />
Global AIDS Program<br />
CDC, Atlanta, USA<br />
Dr Steven Wiersma<br />
Divisi<strong>on</strong> of Viral Hepatitis<br />
CDC, Atlanta, USA<br />
viii<br />
<str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Experts who c<strong>on</strong>tributed to the development of the recommendati<strong>on</strong><br />
<strong>on</strong> sk<strong>in</strong> dis<strong>in</strong>fecti<strong>on</strong> before blood collecti<strong>on</strong> for transfusi<strong>on</strong> purposes<br />
Dr Michael Bell<br />
Associate Director for Infecti<strong>on</strong> C<strong>on</strong>trol, Divisi<strong>on</strong> of Healthcare Quality Promoti<strong>on</strong>, NCPDCID<br />
CDC, Atlanta, USA<br />
Dr Barry Cooks<strong>on</strong><br />
Director, Laboratory of HealthCare Associated Infecti<strong>on</strong>,<br />
Centre for Infecti<strong>on</strong>s, Health Protecti<strong>on</strong> Agency, L<strong>on</strong>d<strong>on</strong>, United K<strong>in</strong>gdom (UK)<br />
Dr Peter Hoffman<br />
C<strong>on</strong>sultant Cl<strong>in</strong>ical Scientist, Central Public Health Laboratory<br />
Laboratory of HealthCare Associated Infecti<strong>on</strong>,<br />
Centre for Infecti<strong>on</strong>s, Health Protecti<strong>on</strong> Agency, L<strong>on</strong>d<strong>on</strong>, UK<br />
Dr Carl McD<strong>on</strong>ald<br />
Head of Bacteriology, Nati<strong>on</strong>al Bacteriology Laboratory<br />
Nati<strong>on</strong>al Health Service <strong>Blood</strong> and Transplant, L<strong>on</strong>d<strong>on</strong>, UK<br />
Dr Ziad Memish<br />
Director, Gulf Cooperati<strong>on</strong> Council States Center for Infecti<strong>on</strong> C<strong>on</strong>trol<br />
Head, Adult Infectious Diseases Secti<strong>on</strong><br />
Dept of Medic<strong>in</strong>e and Infecti<strong>on</strong> Preventi<strong>on</strong> and C<strong>on</strong>trol Program<br />
Nati<strong>on</strong>al Guard Health Affairs<br />
K<strong>in</strong>g Fahad Nati<strong>on</strong>al Guard Hospital, Saudi Arabia<br />
Adjunct Professor Department of Medic<strong>in</strong>e<br />
Divisi<strong>on</strong> of Infectious Diseases, University of Ottawa, Canada<br />
Dr Shirley Pat<strong>on</strong> MN, RN<br />
Senior Advisor, Health Care Associated Infecti<strong>on</strong>s<br />
Centre for Communicable Diseases and Infecti<strong>on</strong> C<strong>on</strong>trol<br />
Public Health Agency of Canada<br />
Peer review<br />
Dr Michael Borg<br />
Chair, Internati<strong>on</strong>al Federati<strong>on</strong> of Infecti<strong>on</strong> C<strong>on</strong>trol<br />
Infecti<strong>on</strong> C<strong>on</strong>trol Unit<br />
Mater Dei Hospital<br />
Msida MSD2090<br />
Malta<br />
Dr Mary Catl<strong>in</strong> BSN, BA, MPH<br />
4210 Midvale Ave N.<br />
Seattle, WA 98103<br />
Editorial work<br />
Dr Hilary Cadman<br />
Editor <strong>in</strong> the Life Sciences (Board of Editors <strong>in</strong> the Life Sciences, USA), Biotext, Canberra,<br />
Australia<br />
The EHT Department of <str<strong>on</strong>g>WHO</str<strong>on</strong>g> developed this document and Dr Selma Khamassi coord<strong>in</strong>ated<br />
the work.<br />
Acknowledgements<br />
ix
Declarati<strong>on</strong> of <strong>in</strong>terests<br />
C<strong>on</strong>flict of <strong>in</strong>terest statements were collected from all c<strong>on</strong>tributors to the guidel<strong>in</strong>e development,<br />
the c<strong>on</strong>sultant c<strong>on</strong>tracted to undertake background reviews and the peer reviewers of the f<strong>in</strong>al<br />
document. No c<strong>on</strong>flict of <strong>in</strong>terest was declared by any of those listed above.<br />
x<br />
<str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Acr<strong>on</strong>yms<br />
CDC<br />
EHT<br />
HBV<br />
HCV<br />
HIV<br />
HSS<br />
PEP<br />
SIGN<br />
<str<strong>on</strong>g>WHO</str<strong>on</strong>g><br />
Centers for Disease C<strong>on</strong>trol and Preventi<strong>on</strong>, Atlanta, USA<br />
Department of Essential Health Technologies (<str<strong>on</strong>g>WHO</str<strong>on</strong>g>)<br />
hepatitis B virus<br />
hepatitis C virus<br />
human immunodeficiency virus<br />
Health Systems and Services (<str<strong>on</strong>g>WHO</str<strong>on</strong>g>)<br />
post-exposure prophylaxis<br />
Safe Injecti<strong>on</strong> Global Network<br />
World Health Organizati<strong>on</strong><br />
Acr<strong>on</strong>yms<br />
xi
Executive summary<br />
<strong>Phlebotomy</strong> – the draw<strong>in</strong>g of blood – has been practised for centuries and is still <strong>on</strong>e of the most<br />
comm<strong>on</strong> <strong>in</strong>vasive procedures <strong>in</strong> health care. Each step <strong>in</strong> the process of phlebotomy affects the<br />
quality of the specimen and is thus important for prevent<strong>in</strong>g laboratory error, patient <strong>in</strong>jury and<br />
even death. For example, the touch of a f<strong>in</strong>ger to verify the locati<strong>on</strong> of a ve<strong>in</strong> before <strong>in</strong>serti<strong>on</strong> of<br />
the needle <strong>in</strong>creases the chance that a specimen will be c<strong>on</strong>tam<strong>in</strong>ated. This can cause false blood<br />
culture results, prol<strong>on</strong>g hospitalizati<strong>on</strong>, delay diagnosis and cause unnecessary use of antibiotics.<br />
Jostl<strong>in</strong>g and jarr<strong>in</strong>g of test tubes <strong>in</strong> transit can lyse or break open red blood cells, caus<strong>in</strong>g false<br />
laboratory results. Clerical errors <strong>in</strong> complet<strong>in</strong>g forms and identify<strong>in</strong>g patients are comm<strong>on</strong>,<br />
costly and preventable. Other adverse effects for patients are comm<strong>on</strong>; they <strong>in</strong>clude bruis<strong>in</strong>g<br />
at the site of puncture, fa<strong>in</strong>t<strong>in</strong>g, nerve damage and haematomas. These guidel<strong>in</strong>es outl<strong>in</strong>e the<br />
simple but important steps that can make phlebotomy safer for patients.<br />
<strong>Phlebotomy</strong> also poses risks for health workers. It is still comm<strong>on</strong> to see a phlebotomist carry<br />
out dangerous practices known to <strong>in</strong>crease the risk of needle-stick <strong>in</strong>jury and transmissi<strong>on</strong> of<br />
disease. Dangerous practices <strong>in</strong>clude:<br />
• recapp<strong>in</strong>g used needles us<strong>in</strong>g two hands;<br />
• recapp<strong>in</strong>g and disassembl<strong>in</strong>g vacuum-c<strong>on</strong>ta<strong>in</strong><strong>in</strong>g tubes and holders;<br />
• reus<strong>in</strong>g tourniquets and vacuum-tube holders that may be c<strong>on</strong>tam<strong>in</strong>ated with bacteria and<br />
sometimes blood;<br />
• work<strong>in</strong>g al<strong>on</strong>e with c<strong>on</strong>fused or disoriented patients who may move unexpectedly,<br />
c<strong>on</strong>tribut<strong>in</strong>g to needle-sticks.<br />
<strong>Phlebotomy</strong> <strong>in</strong>volves the use of large, hollow needles that have been <strong>in</strong> a blood vessel. The<br />
needles can carry a large volume of blood that, <strong>in</strong> the event of an accidental puncture, may<br />
be more likely to transmit disease than other sharps. <strong>Blood</strong>borne organisms that have been<br />
transmitted after needle-sticks <strong>in</strong>clude viruses such as hepatitis B and human immunodeficiency<br />
virus (HIV), bacteria such as syphilis and parasites such as malaria.<br />
Produc<strong>in</strong>g the guidel<strong>in</strong>es<br />
These guidel<strong>in</strong>es were produced to improve the quality of blood specimens and the safety of<br />
phlebotomy for health workers and patients, by promot<strong>in</strong>g best practices <strong>in</strong> phlebotomy.<br />
In April 2008, the <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Injecti<strong>on</strong> Safety programme – part of the Department of Essential<br />
Health Technologies (EHT) at <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Headquarters <strong>in</strong> Geneva – c<strong>on</strong>vened a c<strong>on</strong>sultati<strong>on</strong> <strong>on</strong> best<br />
practices for phlebotomy and blood collecti<strong>on</strong>. The c<strong>on</strong>sultati<strong>on</strong> <strong>in</strong>cluded special categories, such<br />
as arterial blood sampl<strong>in</strong>g, capillary blood sampl<strong>in</strong>g and paediatric blood collecti<strong>on</strong>. A work<strong>in</strong>g<br />
group of <strong>in</strong>ternati<strong>on</strong>al experts and colleagues from <str<strong>on</strong>g>WHO</str<strong>on</strong>g> departments identified the need for<br />
phlebotomy guidel<strong>in</strong>es, and this document was produced <strong>in</strong> resp<strong>on</strong>se.<br />
This document provides guidance <strong>on</strong> the steps recommended for safe phlebotomy, and reiterates<br />
the accepted pr<strong>in</strong>ciples for draw<strong>in</strong>g and collect<strong>in</strong>g blood. The guidel<strong>in</strong>es are based <strong>on</strong> a literature<br />
review that focused <strong>on</strong> identify<strong>in</strong>g systematic literature reviews and evidence relat<strong>in</strong>g specifically<br />
to phlebotomy practices <strong>in</strong> develop<strong>in</strong>g countries. Draft guidel<strong>in</strong>es and evidence were reviewed by<br />
an expert panel, who reached c<strong>on</strong>sensus <strong>on</strong> the recommendati<strong>on</strong>s.<br />
Executive summary<br />
xiii
Protect<strong>in</strong>g patients<br />
To reduce the risk of adverse effects for patients, health workers undertak<strong>in</strong>g phlebotomy need<br />
to be tra<strong>in</strong>ed <strong>in</strong> procedures specific to the types of specimen they collect. Such procedures may<br />
<strong>in</strong>clude arterial sampl<strong>in</strong>g, capillary sampl<strong>in</strong>g, blood culture collecti<strong>on</strong> and venous blood draws.<br />
Health workers who collect specimens from children and <strong>in</strong>fants will need special tra<strong>in</strong><strong>in</strong>g and<br />
practice for these procedures. Phlebotomists work<strong>in</strong>g <strong>in</strong> sett<strong>in</strong>gs with more technology may be<br />
tra<strong>in</strong>ed <strong>in</strong> techniques for plasma and red cell exchange, photophoresis, stem cell collecti<strong>on</strong> and<br />
cord blood collecti<strong>on</strong>. Health workers may need to collect specimens from <strong>in</strong>-dwell<strong>in</strong>g central<br />
l<strong>in</strong>es or arterial l<strong>in</strong>es. Tra<strong>in</strong><strong>in</strong>g should <strong>in</strong>clude techniques that ensure that the specimen collected<br />
will be adequate, and measures that reduce the risk of c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong>, clerical error, <strong>in</strong>fecti<strong>on</strong><br />
and <strong>in</strong>jury.<br />
When tak<strong>in</strong>g blood, health workers should wear well-fitt<strong>in</strong>g, n<strong>on</strong>-sterile gloves, and should also<br />
carry out hand hygiene before and after each patient procedure, before putt<strong>in</strong>g <strong>on</strong> gloves and<br />
after remov<strong>in</strong>g them. The blood should be taken <strong>in</strong> a dedicated locati<strong>on</strong> that ensures patient<br />
comfort and privacy. To remove the risk of envir<strong>on</strong>mental c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> with pathogens,<br />
counter and work surfaces, and chair arms should be cleaned with dis<strong>in</strong>fectant at the start<br />
of each shift and when visibly dirty. To prevent <strong>in</strong>fecti<strong>on</strong>s and other adverse events, health<br />
workers should follow the guidel<strong>in</strong>es <strong>on</strong> patient identificati<strong>on</strong>, hand hygiene, use of gloves, sk<strong>in</strong><br />
dis<strong>in</strong>fecti<strong>on</strong>, use of appropriate blood-sampl<strong>in</strong>g devices and safe transportati<strong>on</strong> of laboratory<br />
samples.<br />
Patient c<strong>on</strong>sent and cooperati<strong>on</strong> are important comp<strong>on</strong>ents of respect<strong>in</strong>g patient rights. A<br />
patient <strong>in</strong>formati<strong>on</strong> leaflet or poster that expla<strong>in</strong>s the procedure <strong>in</strong> simple terms is helpful.<br />
Protect<strong>in</strong>g health workers<br />
<strong>Best</strong> practices <strong>in</strong> phlebotomy protect health workers as well as patients. One way to reduce<br />
accidental <strong>in</strong>jury and blood exposure am<strong>on</strong>g health workers is to use safety (i.e. eng<strong>in</strong>eered)<br />
devices such as retractable lancets, syr<strong>in</strong>ges with needle covers or retractable needles and, when<br />
appropriate, plastic laboratory tubes. Another approach is to elim<strong>in</strong>ate two-handed needle<br />
recapp<strong>in</strong>g and manual device disassembly, and <strong>in</strong>stead dispose of the sharps <strong>in</strong>to a punctureresistant<br />
sharps c<strong>on</strong>ta<strong>in</strong>er (i.e. a safety c<strong>on</strong>ta<strong>in</strong>er) immediately after use. The best practice is<br />
to discard the needle and syr<strong>in</strong>ge, or needle and tube holder, as a s<strong>in</strong>gle unit, <strong>in</strong>to a sharps<br />
c<strong>on</strong>ta<strong>in</strong>er that is clearly visible and with<strong>in</strong> arm’s reach. The size of the c<strong>on</strong>ta<strong>in</strong>er should permit<br />
disposal of the entire device rather than just the needle.<br />
Instituti<strong>on</strong>s should c<strong>on</strong>duct surveillance <strong>on</strong> sharps <strong>in</strong>juries and accidental exposure to blood, so<br />
that preventable factors can be identified. Support services should also be available for health<br />
workers accidentally exposed to blood. These should <strong>in</strong>clude immunizati<strong>on</strong> with hepatitis B<br />
before assum<strong>in</strong>g duties that <strong>in</strong>clude potential exposure to blood and body fluids, and postexposure<br />
prophylaxis for HIV and hepatitis B. All health-care facilities should display clear<br />
<strong>in</strong>structi<strong>on</strong>s for procedures to follow <strong>in</strong> case of accidental exposure to blood and body fluids.<br />
These guidel<strong>in</strong>es also outl<strong>in</strong>e the resp<strong>on</strong>sibilities of managerial staff, <strong>in</strong>clud<strong>in</strong>g provisi<strong>on</strong> of:<br />
• gloves <strong>in</strong> multiple sizes, s<strong>in</strong>gle-use disposable needles, and syr<strong>in</strong>ges or lanc<strong>in</strong>g devices <strong>in</strong><br />
sufficient numbers to ensure that each patient has a sterile needle and collecti<strong>on</strong> device or<br />
equivalent for each blood sampl<strong>in</strong>g;<br />
• sufficient laboratory sample tubes to prevent reuse and manual wash<strong>in</strong>g.<br />
xiv<br />
<str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
<strong>Best</strong> practice <strong>in</strong> dis<strong>in</strong>fecti<strong>on</strong><br />
After review<strong>in</strong>g the evidence <strong>on</strong> best practice <strong>in</strong> phlebotomy, the expert panel found that further<br />
evidence was needed <strong>on</strong> the best method for sk<strong>in</strong> preparati<strong>on</strong> before blood collecti<strong>on</strong> for the<br />
purpose of blood transfusi<strong>on</strong>. The panel commissi<strong>on</strong>ed a systematic review from the Cochrane<br />
group to <strong>in</strong>vestigate the literature <strong>on</strong> whether “alcohol al<strong>on</strong>e” or “any sk<strong>in</strong> dis<strong>in</strong>fectant followed<br />
by alcohol for sk<strong>in</strong> preparati<strong>on</strong>” is more effective <strong>in</strong> reduc<strong>in</strong>g the risk of blood c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> or<br />
bacteraemia.<br />
The Cochrane group found that no research had been c<strong>on</strong>ducted to compare these two methods,<br />
and commented that, until better evidences emerges, decisi<strong>on</strong>s would probably need to be based<br />
<strong>on</strong> c<strong>on</strong>venience and cost.<br />
In l<strong>in</strong>e with <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es for the development of recommendati<strong>on</strong>s, additi<strong>on</strong>al <strong>in</strong>fecti<strong>on</strong><br />
c<strong>on</strong>trol experts were c<strong>on</strong>sulted. Based <strong>on</strong> expert op<strong>in</strong>i<strong>on</strong>, <strong>in</strong>clud<strong>in</strong>g c<strong>on</strong>siderati<strong>on</strong>s of<br />
c<strong>on</strong>venience and cost, these guidel<strong>in</strong>es recommend a <strong>on</strong>e-step procedure for sk<strong>in</strong> preparati<strong>on</strong>.<br />
Health workers should clean the sk<strong>in</strong> with a comb<strong>in</strong>ati<strong>on</strong> of 2% chlorhexid<strong>in</strong>e gluc<strong>on</strong>ate <strong>in</strong> 70%<br />
isopropyl alcohol, cover<strong>in</strong>g the whole area and ensur<strong>in</strong>g that the sk<strong>in</strong> area is <strong>in</strong> c<strong>on</strong>tact with the<br />
dis<strong>in</strong>fectant for at least 30 sec<strong>on</strong>ds; they should then should allow the area to dry completely<br />
(about 30 sec<strong>on</strong>ds).<br />
Implement<strong>in</strong>g and revis<strong>in</strong>g the guidel<strong>in</strong>es<br />
In some countries, these guidel<strong>in</strong>es will be adapted to meet local needs, although key steps<br />
and recommendati<strong>on</strong>s will be ma<strong>in</strong>ta<strong>in</strong>ed. The <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Injecti<strong>on</strong> Safety programme can also<br />
provide technical support for adapt<strong>in</strong>g and implement<strong>in</strong>g the guidel<strong>in</strong>es at regi<strong>on</strong>al and<br />
country levels, if requested. The feasibility of recommended practices and the impact of the<br />
guidel<strong>in</strong>e <strong>on</strong> phlebotomy practices will be evaluated by the <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Injecti<strong>on</strong> Safety programme, <strong>in</strong><br />
collaborati<strong>on</strong> with <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Regi<strong>on</strong>al Offices. The recommendati<strong>on</strong>s <strong>in</strong> this document are expected<br />
to rema<strong>in</strong> valid until 2014, when they will be reviewed.<br />
Executive summary<br />
xv
PART I BACKGROUND
1 Introducti<strong>on</strong><br />
1.1 Overview<br />
<strong>Phlebotomy</strong> – the draw<strong>in</strong>g of blood – has been practiced for centuries and is still <strong>on</strong>e of the<br />
most comm<strong>on</strong> <strong>in</strong>vasive procedures <strong>in</strong> health care (1). However, practice varies c<strong>on</strong>siderably<br />
between countries, and between <strong>in</strong>stituti<strong>on</strong>s and <strong>in</strong>dividuals with<strong>in</strong> the same country (2). These<br />
differences <strong>in</strong>clude variati<strong>on</strong>s <strong>in</strong> blood-sampl<strong>in</strong>g technique, tra<strong>in</strong><strong>in</strong>g (both formal and “<strong>on</strong>-thejob”),<br />
use of safety devices, disposal methods, reuse of devices and availability of hepatitis B<br />
vacc<strong>in</strong>e.<br />
The methods and the evidence base used to develop this document are given <strong>in</strong> Annex A.<br />
1.1.1 Issues <strong>in</strong> phlebotomy<br />
By its nature, phlebotomy has the potential to expose health workers and patients to blood<br />
from other people, putt<strong>in</strong>g them at risk from bloodborne pathogens. These pathogens <strong>in</strong>clude<br />
human immunodeficiency virus (HIV), hepatitis B virus (HBV), hepatitis C virus (HCV), and<br />
those caus<strong>in</strong>g viral haemorrhagic fevers (Crimean C<strong>on</strong>go haemorrhagic fever, Ebola, Lassa and<br />
Marburg) and dengue (3). For example, outbreaks of hepatitis B have been reported with the use<br />
of glucometers (devices used to determ<strong>in</strong>e blood glucose c<strong>on</strong>centrati<strong>on</strong>) (4, 5). Diseases such as<br />
malaria and syphilis may also be transmitted via c<strong>on</strong>tam<strong>in</strong>ated blood (6, 7), and poor <strong>in</strong>fecti<strong>on</strong>c<strong>on</strong>trol<br />
practices may lead to bacterial <strong>in</strong>fecti<strong>on</strong> where the needle is <strong>in</strong>serted and c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong><br />
of specimens.<br />
If a blood sample is poorly collected, the results may be <strong>in</strong>accurate and mislead<strong>in</strong>g to the<br />
cl<strong>in</strong>ician, and the patient may have to undergo the <strong>in</strong>c<strong>on</strong>venience of repeat test<strong>in</strong>g. The three<br />
major issues result<strong>in</strong>g from errors <strong>in</strong> collecti<strong>on</strong> are haemolysis, c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> and <strong>in</strong>accurate<br />
labell<strong>in</strong>g.<br />
Factors that <strong>in</strong>crease the risk of haemolysis <strong>in</strong>clude:<br />
• use of a needle of too small a gauge (23 or under), or too large a gauge for the vessel;<br />
• press<strong>in</strong>g the syr<strong>in</strong>ge plunger to force the blood <strong>in</strong>to a tube, thus <strong>in</strong>creas<strong>in</strong>g the shear force<br />
<strong>on</strong> the red blood cells;<br />
• draw<strong>in</strong>g blood specimens from an <strong>in</strong>travenous or central l<strong>in</strong>e;<br />
• underfill<strong>in</strong>g a tube so that the ratio of anticoagulant to blood is greater than 1:9;<br />
• reus<strong>in</strong>g tubes that have been refilled by hand with <strong>in</strong>appropriate amounts of anticoagulants;<br />
• mix<strong>in</strong>g a tube too vigorously;<br />
• fail<strong>in</strong>g to let alcohol or dis<strong>in</strong>fectant dry;<br />
• us<strong>in</strong>g too great a vacuum; for example, us<strong>in</strong>g too large a tube for a paediatric patient, or<br />
us<strong>in</strong>g too large a syr<strong>in</strong>ge (10–20 ml).<br />
Serious adverse events l<strong>in</strong>ked with phlebotomy are rare, but may <strong>in</strong>clude loss of c<strong>on</strong>sciousness<br />
with t<strong>on</strong>ic cl<strong>on</strong>ic seizures. Less severe events <strong>in</strong>clude pa<strong>in</strong> at the site of venepuncture, anxiety<br />
and fa<strong>in</strong>t<strong>in</strong>g. The best documented adverse events are <strong>in</strong> blood transfusi<strong>on</strong> services, where<br />
poor venepuncture practice or anatomical abnormality has resulted <strong>in</strong> bruis<strong>in</strong>g, haematoma<br />
and <strong>in</strong>jury to anatomical structures <strong>in</strong> the vic<strong>in</strong>ity of the needle entry. For example, <strong>on</strong>e study<br />
reported bruis<strong>in</strong>g and haematoma at the venepuncture site <strong>in</strong> 12.3% of blood d<strong>on</strong>ors (8). Nerve<br />
<strong>in</strong>jury and damage to adjacent anatomical structures occurred <strong>in</strong>frequently, and syncope<br />
occurred <strong>in</strong> less than 1% of <strong>in</strong>dividuals (8). Vasovagal attacks occurred occasi<strong>on</strong>ally, vary<strong>in</strong>g<br />
from mild to severe; fa<strong>in</strong>t<strong>in</strong>g was reported <strong>in</strong> 5.3% of cases and usually occurred <strong>in</strong> first-time<br />
female blood d<strong>on</strong>ors (8-11).<br />
1 Introducti<strong>on</strong> 3
Injuries from sharps (i.e. items such as needles that have corners, edges or projecti<strong>on</strong>s capable of<br />
cutt<strong>in</strong>g or pierc<strong>in</strong>g the sk<strong>in</strong>) comm<strong>on</strong>ly occur between the use and disposal of a needle or similar<br />
device (12, 13). One way to reduce accidental <strong>in</strong>jury and blood exposure am<strong>on</strong>g health workers<br />
is to replace devices with safety (i.e. eng<strong>in</strong>eered) devices (14–16). Safety devices can avoid up to<br />
75% of percutaneous <strong>in</strong>juries (17); however, if they are disassembled or manually recapped, or<br />
if the needle safety feature is not activated, exposure to blood becomes more likely. Elim<strong>in</strong>at<strong>in</strong>g<br />
needle recapp<strong>in</strong>g and <strong>in</strong>stead immediately dispos<strong>in</strong>g of the sharp <strong>in</strong>to a puncture-resistant<br />
sharps c<strong>on</strong>ta<strong>in</strong>er (i.e. a safety c<strong>on</strong>ta<strong>in</strong>er) markedly reduces needle-stick <strong>in</strong>juries (18, 19).<br />
Report<strong>in</strong>g of accidental exposure to blood and body fluids is more frequent from wellestablished<br />
health-care systems; however, it is thought that the <strong>in</strong>cidence of such exposures is<br />
actually higher <strong>in</strong> systems that are not so well equipped (20, 21).<br />
Home-based care is a grow<strong>in</strong>g comp<strong>on</strong>ent of health delivery, and current global trends suggest<br />
that home-based phlebotomy will become <strong>in</strong>creas<strong>in</strong>gly comm<strong>on</strong>. In this situati<strong>on</strong>, str<strong>on</strong>ger<br />
protecti<strong>on</strong> of community-based health workers and the community will be needed. This can<br />
be achieved by improv<strong>in</strong>g sharps disposal, and by us<strong>in</strong>g safety needles with needle covers or<br />
retractable needles to m<strong>in</strong>imize the risk of exposure to needles (22) and lancets.<br />
1.1.2 The need for guidel<strong>in</strong>es<br />
<strong>Phlebotomy</strong> services are available worldwide <strong>in</strong> a range of health-care facilities (e.g. hospitals,<br />
outpatient facilities and cl<strong>in</strong>ics), and are usually performed by both medical and n<strong>on</strong>medical<br />
pers<strong>on</strong>nel. Laboratory staff or members of phlebotomy teams appear to achieve lower rates of<br />
c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> than staff who have broader resp<strong>on</strong>sibilities, even if both have the same tra<strong>in</strong><strong>in</strong>g<br />
(23). For example, for obta<strong>in</strong><strong>in</strong>g a blood sample for rout<strong>in</strong>e genetic screen<strong>in</strong>g of babies, the use<br />
of capillary heel-pricks by a tra<strong>in</strong>ed phlebotomist was found to be the most successful and pa<strong>in</strong>free<br />
blood-sampl<strong>in</strong>g procedure (capillary sampl<strong>in</strong>g is undertaken for rapid tests that require<br />
small quantities of blood) (24).<br />
<strong>Phlebotomy</strong> practice varies am<strong>on</strong>g health-care pers<strong>on</strong>nel, even though percepti<strong>on</strong>s of risk are<br />
similar and there are guidel<strong>in</strong>es for such practice (20, 25). To help standardize practice, several<br />
countries have established formal tra<strong>in</strong><strong>in</strong>g that phlebotomists must undertake before they can<br />
practice cl<strong>in</strong>ically, but physicians can often practice phlebotomy without formal tra<strong>in</strong><strong>in</strong>g (26).<br />
Dur<strong>in</strong>g phlebotomy procedures, the greatest c<strong>on</strong>cern is the safety of health workers and patients;<br />
therefore, guidance for staff <strong>on</strong> best practice is critical (27, 28). Tra<strong>in</strong><strong>in</strong>g <strong>on</strong>, and adherence to,<br />
the guidance presented here should substantially reduce the risks to both patients and staff, and<br />
will improve blood collecti<strong>on</strong> for laboratory tests and from blood d<strong>on</strong>ors.<br />
1.1.3 Def<strong>in</strong>iti<strong>on</strong>s<br />
For the purposes of this document, the term “phlebotomy” covers the terms:<br />
• blood sampl<strong>in</strong>g for purposes of laboratory tests;<br />
• blood collecti<strong>on</strong> for d<strong>on</strong>ati<strong>on</strong>.<br />
4 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
1.2 Purpose and scope<br />
The aim of these guidel<strong>in</strong>es is to summarize best practices <strong>in</strong> phlebotomy, to improve outcomes<br />
for health workers and patients.<br />
These guidel<strong>in</strong>es recommend best practices for all levels of health care where phlebotomy is<br />
practised. They extend the scope of the exist<strong>in</strong>g guidel<strong>in</strong>es from the World Health Organizati<strong>on</strong><br />
(<str<strong>on</strong>g>WHO</str<strong>on</strong>g>) and the Safe Injecti<strong>on</strong> Global Network (SIGN), which is a <str<strong>on</strong>g>WHO</str<strong>on</strong>g>-hosted network. These<br />
exist<strong>in</strong>g guidel<strong>in</strong>es are:<br />
• <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Aide-memoire for a nati<strong>on</strong>al strategy for the safe and appropriate use of <strong>in</strong>jecti<strong>on</strong><br />
(29);<br />
• <strong>Best</strong> <strong>in</strong>fecti<strong>on</strong> c<strong>on</strong>trol practices for <strong>in</strong>tradermal, subcutaneous, and <strong>in</strong>tramuscular needle<br />
<strong>in</strong>jecti<strong>on</strong>s (30).<br />
This document also discusses best practices for venous and arterial blood sampl<strong>in</strong>g, and blood<br />
collecti<strong>on</strong> for transfusi<strong>on</strong> for adult and paediatric populati<strong>on</strong>s. The document does not discuss<br />
collecti<strong>on</strong> from <strong>in</strong>-dwell<strong>in</strong>g central l<strong>in</strong>es, arterial l<strong>in</strong>es or cord blood; also, it does not cover stem<br />
cell collecti<strong>on</strong>.<br />
1.3 Objectives<br />
The objectives of these guidel<strong>in</strong>es are to:<br />
• improve knowledge and awareness of the risks associated with phlebotomy am<strong>on</strong>g all<br />
health workers <strong>in</strong>volved <strong>in</strong> the practice;<br />
• <strong>in</strong>crease safe practices and reduce bloodborne virus exposure and transmissi<strong>on</strong>;<br />
• improve patient c<strong>on</strong>fidence and comfort;<br />
• improve the quality of laboratory tests.<br />
1.4 Target audience<br />
This document is aimed at:<br />
• people who perform or supervise phlebotomy <strong>in</strong> the private and public sectors, <strong>in</strong> hospitals,<br />
community cl<strong>in</strong>ics and other health-care facilities, <strong>in</strong>clud<strong>in</strong>g those <strong>in</strong>volved <strong>in</strong> home-based<br />
care;<br />
• health tra<strong>in</strong>ers and educators;<br />
• procurement officials (who need to be aware of which equipment and supplies are safe and<br />
cost effective).<br />
1.5 Indicati<strong>on</strong>s for blood sampl<strong>in</strong>g and blood collecti<strong>on</strong><br />
The most comm<strong>on</strong> use of blood sampl<strong>in</strong>g is for laboratory tests for cl<strong>in</strong>ical management and<br />
health assessment. Categories that require specialist tra<strong>in</strong><strong>in</strong>g <strong>in</strong>clude:<br />
• arterial blood gases for patients <strong>on</strong> mechanical ventilati<strong>on</strong>, to m<strong>on</strong>itor blood oxygenati<strong>on</strong>;<br />
• ne<strong>on</strong>atal and paediatric blood sampl<strong>in</strong>g<br />
––<br />
heel-prick (i.e. capillary sampl<strong>in</strong>g);<br />
––<br />
scalp ve<strong>in</strong>s <strong>in</strong> paediatrics;<br />
1 Introducti<strong>on</strong> 5
• capillary sampl<strong>in</strong>g (i.e. f<strong>in</strong>ger or heel-pricks or, rarely, an ear lobe puncture) for analysis of<br />
capillary blood specimens for all ages; examples <strong>in</strong>clude test<strong>in</strong>g of ir<strong>on</strong> levels before blood<br />
d<strong>on</strong>ati<strong>on</strong>, blood glucose m<strong>on</strong>itor<strong>in</strong>g, and rapid tests for HIV, malaria and syphilis.<br />
<strong>Blood</strong> collecti<strong>on</strong> is used to obta<strong>in</strong> blood from d<strong>on</strong>ors for various therapeutic purposes.<br />
1.6 Structure of document<br />
This document is divided <strong>in</strong>to five parts:<br />
• Part I <strong>in</strong>troduces the topic and the document.<br />
• Part II covers different aspects of phlebotomy. Each chapter <strong>in</strong> this part is divided <strong>in</strong>to<br />
secti<strong>on</strong>s that give background <strong>in</strong>formati<strong>on</strong>, practical guidance and illustrati<strong>on</strong>s (where<br />
applicable). Part 2 <strong>in</strong>cludes<br />
––<br />
the steps recommended for safe phlebotomy, <strong>in</strong>clud<strong>in</strong>g accepted pr<strong>in</strong>ciples for draw<strong>in</strong>g<br />
and collect<strong>in</strong>g blood (Chapter 2);<br />
––<br />
the various open and closed systems available for phlebotomy (Chapter 3);<br />
––<br />
collecti<strong>on</strong> of blood for transfusi<strong>on</strong> (Chapter 4);<br />
––<br />
collecti<strong>on</strong> of arterial blood, for determ<strong>in</strong>ati<strong>on</strong> of blood gases (Chapter 5);<br />
––<br />
aspects of blood sampl<strong>in</strong>g specific to paediatric and ne<strong>on</strong>atal patients (Chapter 6);<br />
––<br />
capillary sampl<strong>in</strong>g (Chapter 7)<br />
• Part III deals with implementati<strong>on</strong>, m<strong>on</strong>itor<strong>in</strong>g and evaluati<strong>on</strong>; it covers<br />
––<br />
ways to implement best practices <strong>in</strong> phlebotomy (Chapter 8);<br />
––<br />
use of a m<strong>on</strong>itor<strong>in</strong>g and evaluati<strong>on</strong> system to document improvements <strong>in</strong> phlebotomy<br />
practice (Chapter 9).<br />
• Part IV lists the references.<br />
• Part V c<strong>on</strong>ta<strong>in</strong>s a set of annexes that provide additi<strong>on</strong>al <strong>in</strong>formati<strong>on</strong> <strong>on</strong> specific topics; it<br />
also <strong>in</strong>cludes a glossary.<br />
6 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
PART II ASPECTS<br />
OF PHLEBOTOMY
2 <strong>Best</strong> practices <strong>in</strong> phlebotomy<br />
This chapter covers all the steps recommended for safe phlebotomy and reiterates the accepted<br />
pr<strong>in</strong>ciples for blood draw<strong>in</strong>g and blood collecti<strong>on</strong> (31). The chapter <strong>in</strong>cludes background<br />
<strong>in</strong>formati<strong>on</strong> (Secti<strong>on</strong> 2.1), practical guidance (Secti<strong>on</strong> 2.2) and illustrati<strong>on</strong>s (Secti<strong>on</strong> 2.3)<br />
relevant to best practices <strong>in</strong> phlebotomy.<br />
The <strong>in</strong>formati<strong>on</strong> given <strong>in</strong> this secti<strong>on</strong> underp<strong>in</strong>s that given <strong>in</strong> the rema<strong>in</strong>der of Part II for specific<br />
situati<strong>on</strong>s. Chapter 4 also provides <strong>in</strong>formati<strong>on</strong> relevant to the procedure for draw<strong>in</strong>g blood<br />
given below <strong>in</strong> Secti<strong>on</strong> 2.2, but focuses <strong>on</strong> blood collecti<strong>on</strong> from d<strong>on</strong>ors.<br />
Instituti<strong>on</strong>s can use these guidel<strong>in</strong>es to establish standard operat<strong>in</strong>g procedures. Such<br />
procedures should clearly state the risks to patients and health workers, as well as the means to<br />
reduce those risks – discussed below <strong>in</strong> Secti<strong>on</strong>s 2.1.4 and 2.2.<br />
2.1 Background <strong>in</strong>formati<strong>on</strong> <strong>on</strong> best practices <strong>in</strong> phlebotomy<br />
<strong>Best</strong> practices <strong>in</strong> phlebotomy <strong>in</strong>volve the follow<strong>in</strong>g factors:<br />
• plann<strong>in</strong>g ahead;<br />
• us<strong>in</strong>g an appropriate locati<strong>on</strong>;<br />
• quality c<strong>on</strong>trol;<br />
• standards for quality care for patients and health workers, <strong>in</strong>clud<strong>in</strong>g<br />
––<br />
availability of appropriate supplies and protective equipment;<br />
––<br />
availability of post-exposure prophylaxis (PEP);<br />
––<br />
avoidance of c<strong>on</strong>tam<strong>in</strong>ated phlebotomy equipment;<br />
––<br />
appropriate tra<strong>in</strong><strong>in</strong>g <strong>in</strong> phlebotomy;<br />
––<br />
cooperati<strong>on</strong> <strong>on</strong> the part of patients;<br />
• quality of laboratory sampl<strong>in</strong>g.<br />
2.1.1 Plann<strong>in</strong>g ahead<br />
This is the most important part of carry<strong>in</strong>g out any procedure, and is usually d<strong>on</strong>e at the start of<br />
a phlebotomy sessi<strong>on</strong>.<br />
2.1.2 Us<strong>in</strong>g an appropriate locati<strong>on</strong><br />
The phlebotomist should work <strong>in</strong> a quiet, clean, well-lit area, whether work<strong>in</strong>g with outpatients<br />
or <strong>in</strong>patients.<br />
2.1.3 Quality c<strong>on</strong>trol<br />
Quality assurance is an essential part of best practice <strong>in</strong> <strong>in</strong>fecti<strong>on</strong> preventi<strong>on</strong> and c<strong>on</strong>trol (1). In<br />
phlebotomy, it helps to m<strong>in</strong>imize the chance of a mishap. Table 2.1 lists the ma<strong>in</strong> comp<strong>on</strong>ents of<br />
quality assurance, and expla<strong>in</strong>s why they are important.<br />
2 <strong>Best</strong> practices <strong>in</strong> phlebotomy 9
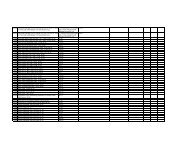
Table 2.1<br />
Elements of quality assurance <strong>in</strong> phlebotomy<br />
Element<br />
Educati<strong>on</strong> and tra<strong>in</strong><strong>in</strong>g<br />
Standard operat<strong>in</strong>g<br />
procedures (SOPs)<br />
Correct identificati<strong>on</strong> of<br />
the patient<br />
The c<strong>on</strong>diti<strong>on</strong> of the<br />
sample<br />
Safe transportati<strong>on</strong><br />
An <strong>in</strong>cident report<strong>in</strong>g<br />
system<br />
Notes<br />
Educati<strong>on</strong> and tra<strong>in</strong><strong>in</strong>g is necessary for all staff carry<strong>in</strong>g out phlebotomy. It should<br />
<strong>in</strong>clude an understand<strong>in</strong>g of anatomy, awareness of the risks from blood exposure,<br />
and the c<strong>on</strong>sequences of poor <strong>in</strong>fecti<strong>on</strong> preventi<strong>on</strong> and c<strong>on</strong>trol.<br />
SOPs are required for each step or procedure. They should be written and be<br />
readily available to health workers.<br />
Identificati<strong>on</strong> should be through match<strong>in</strong>g to the laboratory request form.<br />
• For blood d<strong>on</strong>ati<strong>on</strong>, the identity of the d<strong>on</strong>or should be accurately matched to<br />
the results of screen<strong>in</strong>g tests.<br />
• For blood sampl<strong>in</strong>g, after samples have been taken from a patient or d<strong>on</strong>or, a<br />
system of identificati<strong>on</strong> and track<strong>in</strong>g is essential to ensure that the sample is<br />
correctly matched with the result and with the patient or d<strong>on</strong>or.<br />
The c<strong>on</strong>diti<strong>on</strong> of the sample should be such that the quality of the results is<br />
satisfactory.<br />
Mak<strong>in</strong>g safe transportati<strong>on</strong> of blood or blood products part of best practices will<br />
improve the quality of results from laboratory test<strong>in</strong>g (32).<br />
A system is required for report<strong>in</strong>g all adverse events. A log book or register<br />
should be established with accurate details of the <strong>in</strong>cident, possible causes and<br />
management of adverse events (27).<br />
2.1.4 Quality care for patients and health workers<br />
Several factors can improve safety standards and quality of care for both patients and health<br />
workers, and laboratory tests. These factors, discussed below, <strong>in</strong>clude:<br />
Availability of appropriate supplies and protective equipment<br />
Procurement of supplies is the direct resp<strong>on</strong>sibility of the adm<strong>in</strong>istrative (management)<br />
structures resp<strong>on</strong>sible for sett<strong>in</strong>g up phlebotomy services. Management should:<br />
• provide hand-hygiene materials (soap and water or alcohol rub), well-fitt<strong>in</strong>g n<strong>on</strong>-sterile<br />
gloves, s<strong>in</strong>gle-use disposable needles, and syr<strong>in</strong>ges or lanc<strong>in</strong>g devices <strong>in</strong> sufficient numbers<br />
to ensure that each patient has a sterile needle and syr<strong>in</strong>ge or equivalent for each blood<br />
sampl<strong>in</strong>g;<br />
• make available sufficient laboratory sample tubes to prevent dangerous practices<br />
(e.g. decant<strong>in</strong>g blood to recycle laboratory tubes).<br />
Several safety-eng<strong>in</strong>eered devices are available <strong>on</strong> the market; such devices reduce exposure to<br />
blood and <strong>in</strong>juries. However, the use of such devices should be accompanied by other <strong>in</strong>fecti<strong>on</strong><br />
preventi<strong>on</strong> and c<strong>on</strong>trol practices, and tra<strong>in</strong><strong>in</strong>g <strong>in</strong> their use. Not all safety devices are applicable<br />
to phlebotomy. Before select<strong>in</strong>g a safety-eng<strong>in</strong>eered device, users should thoroughly <strong>in</strong>vestigate<br />
available devices to determ<strong>in</strong>e their appropriate use, compatibility with exist<strong>in</strong>g phlebotomy<br />
practices, and efficacy <strong>in</strong> protect<strong>in</strong>g staff and patients (12, 33). Annex B provides further<br />
<strong>in</strong>formati<strong>on</strong> <strong>on</strong> <strong>in</strong>fecti<strong>on</strong> preventi<strong>on</strong> and c<strong>on</strong>trol, safety equipment and best practice; Annex C<br />
provides a comprehensive guide to devices available for draw<strong>in</strong>g blood, <strong>in</strong>clud<strong>in</strong>g safetyeng<strong>in</strong>eered<br />
equipment.<br />
For sett<strong>in</strong>gs with low resources, cost is a driv<strong>in</strong>g factor <strong>in</strong> procurement of safety-eng<strong>in</strong>eered<br />
devices.<br />
Where safety-eng<strong>in</strong>eered devices are not available, skilled use of a needle and syr<strong>in</strong>ge is<br />
acceptable.<br />
10 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Availability of post-exposure prophylaxis<br />
Accidental exposure and specific <strong>in</strong>formati<strong>on</strong> about an <strong>in</strong>cident should be recorded <strong>in</strong> a register.<br />
Support services should be promoted for those who undergo accidental exposure. PEP can help<br />
to avert HIV and hepatitis B <strong>in</strong>fecti<strong>on</strong>s (13, 27). Hepatitis B immunizati<strong>on</strong> should be provided<br />
to all health workers (<strong>in</strong>clud<strong>in</strong>g cleaners and waste handlers), either up<strong>on</strong> entry <strong>in</strong>to health-care<br />
services or as part of PEP (34). Annex D has details of PEP for hepatitis B and HIV.<br />
Avoidance of c<strong>on</strong>tam<strong>in</strong>ated phlebotomy equipment<br />
Tourniquets are a potential source of methicill<strong>in</strong>-resistant Staphylococcus aureus (MRSA),<br />
with up to 25% of tourniquets c<strong>on</strong>tam<strong>in</strong>ated through lack of hand hygiene <strong>on</strong> the part of the<br />
phlebotomist or reuse of c<strong>on</strong>tam<strong>in</strong>ated tourniquets (35). In additi<strong>on</strong>, reusable f<strong>in</strong>ger-prick<br />
devices and related po<strong>in</strong>t-of-care test<strong>in</strong>g devices (e.g. glucometers) c<strong>on</strong>tam<strong>in</strong>ated with blood<br />
have been implicated <strong>in</strong> outbreaks of hepatitis B (4, 5, 36).<br />
To avoid c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong>, any comm<strong>on</strong>-use items, such as glucometers, should be visibly clean<br />
before use <strong>on</strong> a patient, and s<strong>in</strong>gle-use items should not be reused.<br />
Tra<strong>in</strong><strong>in</strong>g <strong>in</strong> phlebotomy<br />
All staff should be tra<strong>in</strong>ed <strong>in</strong> phlebotomy, to prevent unnecessary risk of exposure to blood and<br />
to reduce adverse events for patients.<br />
• Groups of health workers who historically are not formally tra<strong>in</strong>ed <strong>in</strong> phlebotomy should be<br />
encouraged to take up such tra<strong>in</strong><strong>in</strong>g; lax <strong>in</strong>fecti<strong>on</strong> preventi<strong>on</strong> and c<strong>on</strong>trol practices result <strong>in</strong><br />
poor safety for staff and risk to patients (20, 37).<br />
• The length and depth of tra<strong>in</strong><strong>in</strong>g will depend <strong>on</strong> local c<strong>on</strong>diti<strong>on</strong>s; however, the tra<strong>in</strong><strong>in</strong>g<br />
should at least cover the essentials (see Annex E) (38).<br />
• Supervisi<strong>on</strong> by experienced staff and structured tra<strong>in</strong><strong>in</strong>g is necessary for all health workers,<br />
<strong>in</strong>clud<strong>in</strong>g physicians, who undertake blood sampl<strong>in</strong>g.<br />
Patient cooperati<strong>on</strong><br />
One of the essential markers of quality of care <strong>in</strong> phlebotomy is the <strong>in</strong>volvement and cooperati<strong>on</strong><br />
of the patient; this is mutually beneficial to both the health worker and the patient.<br />
Clear <strong>in</strong>formati<strong>on</strong> – either written or verbal – should be available to each patient who undergoes<br />
phlebotomy. Annex F provides sample text for expla<strong>in</strong><strong>in</strong>g the blood-sampl<strong>in</strong>g procedure to a<br />
patient.<br />
2.1.5 Quality of laboratory sampl<strong>in</strong>g<br />
Factors that <strong>in</strong>fluence the outcome of laboratory results dur<strong>in</strong>g collecti<strong>on</strong> and transportati<strong>on</strong><br />
<strong>in</strong>clude:<br />
• knowledge of staff <strong>in</strong>volved <strong>in</strong> blood collecti<strong>on</strong>;<br />
• use of the correct gauge of hypodermic needle (see Table 3.1 <strong>in</strong> Chapter 3) to prevent<br />
haemolysis or abnormal results;<br />
• the anatomical <strong>in</strong>serti<strong>on</strong> site for venepuncture;<br />
• the use of recommended laboratory collecti<strong>on</strong> tubes;<br />
• patient–sample match<strong>in</strong>g (i.e. labell<strong>in</strong>g);<br />
• transportati<strong>on</strong> c<strong>on</strong>diti<strong>on</strong>s;<br />
• <strong>in</strong>terpretati<strong>on</strong> of results for cl<strong>in</strong>ical management.<br />
2 <strong>Best</strong> practices <strong>in</strong> phlebotomy 11
2.2 Practical guidance <strong>on</strong> best practices <strong>in</strong> phlebotomy<br />
2.2.1 Provisi<strong>on</strong> of an appropriate locati<strong>on</strong><br />
• In an outpatient department or cl<strong>in</strong>ic, provide a dedicated phlebotomy cubicle c<strong>on</strong>ta<strong>in</strong><strong>in</strong>g:<br />
––<br />
a clean surface with two chairs (<strong>on</strong>e for the phlebotomist and the other for the patient);<br />
––<br />
a hand wash bas<strong>in</strong> with soap, runn<strong>in</strong>g water and paper towels;<br />
––<br />
alcohol hand rub.<br />
• In the blood-sampl<strong>in</strong>g room for an outpatient department or cl<strong>in</strong>ic, provide a comfortable<br />
recl<strong>in</strong><strong>in</strong>g couch with an arm rest.<br />
• In <strong>in</strong>patient areas and wards:<br />
––<br />
at the patient’s bedside, close the bed curta<strong>in</strong> to offer privacy<br />
––<br />
ensure that blood sampl<strong>in</strong>g is d<strong>on</strong>e <strong>in</strong> a private and clean manner.<br />
2.2.2 Provisi<strong>on</strong> of clear <strong>in</strong>structi<strong>on</strong>s<br />
Ensure that the <strong>in</strong>dicati<strong>on</strong>s for blood sampl<strong>in</strong>g are clearly def<strong>in</strong>ed, either <strong>in</strong> a written protocol or<br />
<strong>in</strong> documented <strong>in</strong>structi<strong>on</strong>s (e.g. <strong>in</strong> a laboratory form).<br />
2.2.3 Procedure for draw<strong>in</strong>g blood<br />
At all times, follow the strategies for <strong>in</strong>fecti<strong>on</strong> preventi<strong>on</strong> and c<strong>on</strong>trol listed <strong>in</strong> Table 2.2.<br />
Table 2.2 Infecti<strong>on</strong> preventi<strong>on</strong> and c<strong>on</strong>trol practices<br />
Do<br />
DO carry out hand hygiene (use soap and water or<br />
alcohol rub), and wash carefully, <strong>in</strong>clud<strong>in</strong>g wrists and<br />
spaces between the f<strong>in</strong>gers for at least 30 sec<strong>on</strong>ds<br />
(follow <str<strong>on</strong>g>WHO</str<strong>on</strong>g>’s ‘My 5 moments for hand hygiene’ a )<br />
DO use <strong>on</strong>e pair of n<strong>on</strong>-sterile gloves per procedure<br />
or patient<br />
DO use a s<strong>in</strong>gle-use device for blood sampl<strong>in</strong>g and<br />
draw<strong>in</strong>g<br />
DO dis<strong>in</strong>fect the sk<strong>in</strong> at the venepuncture site<br />
DO discard the used device (a needle and syr<strong>in</strong>ge<br />
is a s<strong>in</strong>gle unit) immediately <strong>in</strong>to a robust sharps<br />
c<strong>on</strong>ta<strong>in</strong>er<br />
Where recapp<strong>in</strong>g of a needle is unavoidable, DO use<br />
the <strong>on</strong>e-hand scoop technique (see Annex G)<br />
DO seal the sharps c<strong>on</strong>ta<strong>in</strong>er with a tamper-proof lid<br />
DO place laboratory sample tubes <strong>in</strong> a sturdy rack<br />
before <strong>in</strong>ject<strong>in</strong>g <strong>in</strong>to the rubber stopper<br />
DO immediately report any <strong>in</strong>cident or accident<br />
l<strong>in</strong>ked to a needle or sharp <strong>in</strong>jury, and seek<br />
assistance; start PEP as so<strong>on</strong> as possible, follow<strong>in</strong>g<br />
protocols<br />
Do not<br />
DO NOT forget to clean your hands<br />
DO NOT use the same pair of gloves for more than<br />
<strong>on</strong>e patient<br />
DO NOT wash gloves for reuse<br />
DO NOT use a syr<strong>in</strong>ge, needle or lancet for more<br />
than <strong>on</strong>e patient<br />
DO NOT touch the puncture site after dis<strong>in</strong>fect<strong>in</strong>g it<br />
DO NOT leave an unprotected needle ly<strong>in</strong>g outside<br />
the sharps c<strong>on</strong>ta<strong>in</strong>er<br />
DO NOT recap a needle us<strong>in</strong>g both hands<br />
DO NOT overfill or decant a sharps c<strong>on</strong>ta<strong>in</strong>er<br />
DO NOT <strong>in</strong>ject <strong>in</strong>to a laboratory tube while hold<strong>in</strong>g it<br />
with the other hand<br />
DO NOT delay PEP after exposure to potentially<br />
c<strong>on</strong>tam<strong>in</strong>ated material; bey<strong>on</strong>d 72 hours, PEP is NOT<br />
effective<br />
PEP, post-exposure prophylaxis; <str<strong>on</strong>g>WHO</str<strong>on</strong>g>, World Health Organizati<strong>on</strong>.<br />
a<br />
http://www.who.<strong>in</strong>t/gpsc/5may/background/5moments/en/<strong>in</strong>dex.html<br />
12 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Step 1 – Assemble equipment<br />
Collect all the equipment needed for the procedure and place it with<strong>in</strong> safe and easy reach <strong>on</strong> a<br />
tray or trolley, ensur<strong>in</strong>g that all the items are clearly visible. The equipment required <strong>in</strong>cludes:<br />
• a supply of laboratory sample tubes, which should be stored dry and upright <strong>in</strong> a rack;<br />
blood can be collected <strong>in</strong><br />
––<br />
sterile glass or plastic tubes with rubber caps (the choice of tube will depend <strong>on</strong> what is<br />
agreed with the laboratory);<br />
––<br />
vacuum-extracti<strong>on</strong> blood tubes; or<br />
––<br />
glass tubes with screw caps;<br />
• a sterile glass or bleed<strong>in</strong>g pack (collapsible) if large quantities of blood are to be collected;<br />
• well-fitt<strong>in</strong>g, n<strong>on</strong>-sterile gloves;<br />
• an assortment of blood-sampl<strong>in</strong>g devices (safety-eng<strong>in</strong>eered devices or needles and<br />
syr<strong>in</strong>ges, see below), of different sizes;<br />
• a tourniquet;<br />
• alcohol hand rub;<br />
• 70% alcohol swabs for sk<strong>in</strong> dis<strong>in</strong>fecti<strong>on</strong>;<br />
• gauze or cott<strong>on</strong>-wool ball to be applied over puncture site;<br />
• laboratory specimen labels;<br />
• writ<strong>in</strong>g equipment;<br />
• laboratory forms;<br />
• leak-proof transportati<strong>on</strong> bags and c<strong>on</strong>ta<strong>in</strong>ers;<br />
• a puncture-resistant sharps c<strong>on</strong>ta<strong>in</strong>er.<br />
Ensure that the rack c<strong>on</strong>ta<strong>in</strong><strong>in</strong>g the sample tubes is close to you, the health worker, but away<br />
from the patient, to avoid it be<strong>in</strong>g accidentally tipped over.<br />
Step 2 – Identify and prepare the patient<br />
Where the patient is adult and c<strong>on</strong>scious, follow the steps outl<strong>in</strong>ed below.<br />
• Introduce yourself to the patient, and ask the patient to state their full name.<br />
• Check that the laboratory form matches the patient’s identity (i.e. match the patient’s<br />
details with the laboratory form, to ensure accurate identificati<strong>on</strong>).<br />
• Ask whether the patent has allergies, phobias or has ever fa<strong>in</strong>ted dur<strong>in</strong>g previous <strong>in</strong>jecti<strong>on</strong>s<br />
or blood draws.<br />
• If the patient is anxious or afraid, reassure the pers<strong>on</strong> and ask what would make them more<br />
comfortable.<br />
• Make the patient comfortable <strong>in</strong> a sup<strong>in</strong>e positi<strong>on</strong> (if possible).<br />
• Place a clean paper or towel under the patient’s arm.<br />
• Discuss the test to be performed (see Annex F) and obta<strong>in</strong> verbal c<strong>on</strong>sent. The patient has a<br />
right to refuse a test at any time before the blood sampl<strong>in</strong>g, so it is important to ensure that<br />
the patient has understood the procedure.<br />
For paediatric or ne<strong>on</strong>atal patients, see Chapter 6.<br />
2 <strong>Best</strong> practices <strong>in</strong> phlebotomy 13
Step 3 – Select the site<br />
General<br />
• Extend the patient’s arm and <strong>in</strong>spect the antecubital fossa or forearm.<br />
• Locate a ve<strong>in</strong> of a good size that is visible, straight and clear. The diagram <strong>in</strong> Secti<strong>on</strong> 2.3,<br />
shows comm<strong>on</strong> positi<strong>on</strong>s of the vessels, but many variati<strong>on</strong>s are possible. The median<br />
cubital ve<strong>in</strong> lies between muscles and is usually the most easy to puncture. Under the basilic<br />
ve<strong>in</strong> runs an artery and a nerve, so punctur<strong>in</strong>g here runs the risk of damag<strong>in</strong>g the nerve or<br />
artery and is usually more pa<strong>in</strong>ful. DO NOT <strong>in</strong>sert the needle where ve<strong>in</strong>s are divert<strong>in</strong>g,<br />
because this <strong>in</strong>creases the chance of a haematoma.<br />
• The ve<strong>in</strong> should be visible without apply<strong>in</strong>g the tourniquet. Locat<strong>in</strong>g the ve<strong>in</strong> will help <strong>in</strong><br />
determ<strong>in</strong><strong>in</strong>g the correct size of needle.<br />
• Apply the tourniquet about 4–5 f<strong>in</strong>ger widths above the venepuncture site and re-exam<strong>in</strong>e<br />
the ve<strong>in</strong>.<br />
Hospitalized patients<br />
In hospitalized patients, do not take blood from an exist<strong>in</strong>g peripheral venous access site<br />
because this may give false results. Haemolysis, c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> and presence of <strong>in</strong>travenous fluid<br />
and medicati<strong>on</strong> can all alter the results (39). Nurs<strong>in</strong>g staff and physicians may access central<br />
venous l<strong>in</strong>es for specimens follow<strong>in</strong>g protocols. However, specimens from central l<strong>in</strong>es carry a<br />
risk of c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> or err<strong>on</strong>eous laboratory test results.<br />
It is acceptable, but not ideal, to draw blood specimens when first <strong>in</strong>troduc<strong>in</strong>g an <strong>in</strong>-dwell<strong>in</strong>g<br />
venous device, before c<strong>on</strong>nect<strong>in</strong>g the cannula to the <strong>in</strong>travenous fluids.<br />
Step 4 – Perform hand hygiene and put <strong>on</strong> gloves<br />
• Perform hand hygiene; that is<br />
––<br />
wash hands with soap and water, and dry with s<strong>in</strong>gle-use towels; or<br />
––<br />
if hands are not visibly c<strong>on</strong>tam<strong>in</strong>ated, clean with alcohol rub – use 3 ml of alcohol rub<br />
<strong>on</strong> the palm of the hand, and rub it <strong>in</strong>to f<strong>in</strong>gertips, back of hands and all over the hands<br />
until dry.<br />
• After perform<strong>in</strong>g hand hygiene, put <strong>on</strong> well-fitt<strong>in</strong>g, n<strong>on</strong>-sterile gloves.<br />
Step 5 – Dis<strong>in</strong>fect the entry site<br />
• Unless draw<strong>in</strong>g blood cultures, or prepp<strong>in</strong>g for a blood collecti<strong>on</strong>, clean the site with a 70%<br />
alcohol swab for 30 sec<strong>on</strong>ds and allow to dry completely (30 sec<strong>on</strong>ds) (40–42).<br />
Note: alcohol is preferable to povid<strong>on</strong>e iod<strong>in</strong>e, because blood c<strong>on</strong>tam<strong>in</strong>ated with povid<strong>on</strong>e<br />
iod<strong>in</strong>e may falsely <strong>in</strong>crease levels of potassium, phosphorus or uric acid <strong>in</strong> laboratory test<br />
results (6, 7).<br />
• Apply firm but gentle pressure. Start from the centre of the venepuncture site and work<br />
downward and outwards to cover an area of 2 cm or more.<br />
• Allow the area to dry. Failure to allow enough c<strong>on</strong>tact time <strong>in</strong>creases the risk of<br />
c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong>.<br />
• DO NOT touch the cleaned site; <strong>in</strong> particular, DO NOT place a f<strong>in</strong>ger over the ve<strong>in</strong> to guide<br />
the shaft of the exposed needle. It the site is touched, repeat the dis<strong>in</strong>fecti<strong>on</strong>.<br />
14 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Step 6 – Take blood<br />
Venepuncture<br />
Perform venepuncture as follows.<br />
• Anchor the ve<strong>in</strong> by hold<strong>in</strong>g the patient’s arm and plac<strong>in</strong>g a thumb BELOW the<br />
venepuncture site.<br />
• Ask the patient to form a fist so the ve<strong>in</strong>s are more prom<strong>in</strong>ent.<br />
• Enter the ve<strong>in</strong> swiftly at a 30 degree angle or less, and c<strong>on</strong>t<strong>in</strong>ue to <strong>in</strong>troduce the needle<br />
al<strong>on</strong>g the ve<strong>in</strong> at the easiest angle of entry.<br />
• Once sufficient blood has been collected, release the tourniquet BEFORE withdraw<strong>in</strong>g<br />
the needle. Some guidel<strong>in</strong>es suggest remov<strong>in</strong>g the tourniquet as so<strong>on</strong> as blood flow is<br />
established, and always before it has been <strong>in</strong> place for two m<strong>in</strong>utes or more.<br />
• Withdraw the needle gently and apply gentle pressure to the site with a clean gauze or<br />
dry cott<strong>on</strong>-wool ball. Ask the patient to hold the gauze or cott<strong>on</strong> wool <strong>in</strong> place, with the<br />
arm extended and raised. Ask the patient NOT to bend the arm, because do<strong>in</strong>g so causes a<br />
haematoma.<br />
Step 7 – Fill the laboratory sample tubes<br />
• When obta<strong>in</strong><strong>in</strong>g multiple tubes of blood, use evacuated tubes with a needle and tube<br />
holder. This system allows the tubes to be filled directly. If this system is not available, use a<br />
syr<strong>in</strong>ge or w<strong>in</strong>ged needle set <strong>in</strong>stead.<br />
• If a syr<strong>in</strong>ge or w<strong>in</strong>ged needle set is used, best practice is to place the tube <strong>in</strong>to a rack before<br />
fill<strong>in</strong>g the tube. To prevent needle-sticks, use <strong>on</strong>e hand to fill the tube or use a needle shield<br />
between the needle and the hand hold<strong>in</strong>g the tube.<br />
• Pierce the stopper <strong>on</strong> the tube with the needle directly above the tube us<strong>in</strong>g slow, steady<br />
pressure. Do not press the syr<strong>in</strong>ge plunger because additi<strong>on</strong>al pressure <strong>in</strong>creases the risk of<br />
haemolysis.<br />
• Where possible, keep the tubes <strong>in</strong> a rack and move the rack towards you. Inject downwards<br />
<strong>in</strong>to the appropriate coloured stopper. DO NOT remove the stopper because it will release<br />
the vacuum.<br />
• If the sample tube does not have a rubber stopper, <strong>in</strong>ject extremely slowly <strong>in</strong>to the tube<br />
as m<strong>in</strong>imiz<strong>in</strong>g the pressure and velocity used to transfer the specimen reduces the risk of<br />
haemolysis. DO NOT recap and remove the needle.<br />
• Before dispatch, <strong>in</strong>vert the tubes c<strong>on</strong>ta<strong>in</strong><strong>in</strong>g additives for the required number of times (as<br />
specified by the local laboratory).<br />
Step 8 – Draw samples <strong>in</strong> the correct order<br />
Draw blood collecti<strong>on</strong> tubes <strong>in</strong> the correct order, to avoid cross-c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of additives<br />
between tubes. As colour cod<strong>in</strong>g and tube additives may vary, verify recommendati<strong>on</strong>s with local<br />
laboratories. For illustrati<strong>on</strong> purposes, Table 2.3 shows the revised, simplified recommended<br />
order of draw for vacuum tubes or syr<strong>in</strong>ge and needle, based <strong>on</strong> United States Nati<strong>on</strong>al<br />
Committee Cl<strong>in</strong>ical Laboratory Standards c<strong>on</strong>sensus <strong>in</strong> 2003 (43).<br />
2 <strong>Best</strong> practices <strong>in</strong> phlebotomy 15
Table 2.3<br />
Order<br />
of use a<br />
Recommended order of draw for plastic vacuum tubes<br />
Type of tube/usual Additive c Mode of acti<strong>on</strong> Uses<br />
colour b<br />
1 <strong>Blood</strong> culture bottle<br />
(yellow-black striped<br />
tubes)<br />
Broth mixture<br />
Preserves viability of<br />
microorganisms<br />
Microbiology –<br />
aerobes, anaerobes,<br />
fungi<br />
2 N<strong>on</strong>-additive tube<br />
3 Coagulati<strong>on</strong> tube d<br />
(light blue top)<br />
Sodium citrate<br />
Forms calcium salts to<br />
remove calcium<br />
Coagulati<strong>on</strong> tests<br />
(protime and<br />
prothromb<strong>in</strong> time),<br />
requires full draw<br />
4 Clot activator (red top) Clot activator <strong>Blood</strong> clots, and the<br />
serum is separated by<br />
centrifugati<strong>on</strong><br />
Chemistries,<br />
immunology and<br />
serology, blood bank<br />
(cross-match)<br />
5 Serum separator tube<br />
(red-grey tiger top or<br />
gold)<br />
N<strong>on</strong>e<br />
C<strong>on</strong>ta<strong>in</strong>s a gel at the<br />
bottom to separate<br />
blood from serum <strong>on</strong><br />
centrifugati<strong>on</strong><br />
Chemistries,<br />
immunology and<br />
serology<br />
6 Sodium hepar<strong>in</strong> (dark<br />
green top)<br />
Sodium hepar<strong>in</strong> or<br />
lithium hepar<strong>in</strong><br />
Inactivates thromb<strong>in</strong> and<br />
thromboplast<strong>in</strong><br />
For lithium level use<br />
sodium hepar<strong>in</strong>, for<br />
amm<strong>on</strong>ia level use<br />
either<br />
7 PST (light green top) Lithium hepar<strong>in</strong><br />
anticoagulant and a<br />
gel separator<br />
Anticoagulants with<br />
lithium, separates<br />
plasma with PST gel at<br />
bottom of tube<br />
Chemistries<br />
8 EDTA (purple top) EDTA Forms calcium salts to<br />
remove calcium<br />
Haematology, <strong>Blood</strong><br />
Bank (cross-match)<br />
requires full draw<br />
9 <strong>Blood</strong> tube (pale yellow<br />
top)<br />
Acid-citrate-dextrose<br />
(ACD, ACDA or<br />
ACDB)<br />
Complement <strong>in</strong>activati<strong>on</strong><br />
HLA tissue typ<strong>in</strong>g,<br />
paternity test<strong>in</strong>g,<br />
DNA studies<br />
10 Oxalate/fluoride<br />
(light grey top)<br />
Sodium fluoride and<br />
potassium oxalate<br />
Antiglycolytic agent<br />
preserves glucose up to<br />
five days<br />
Glucoses, requires<br />
full draw (may cause<br />
haemolysis if short<br />
draw)<br />
ACD, acid-citrate-dextrose; DNA, deoxyrib<strong>on</strong>ucleic acid; EDTA, ethylenediam<strong>in</strong>etetraacetic acid; HLA, human leucocyte antigen; PST, plasma<br />
separat<strong>in</strong>g tube.<br />
a<br />
“1” <strong>in</strong>dicates draw first, and “10” draw last (if used).<br />
b<br />
Verify with local laboratory <strong>in</strong> case local colour codes differ.<br />
c<br />
Gently <strong>in</strong>vert tubes with additives to mix thoroughly; err<strong>on</strong>eous test results may be obta<strong>in</strong>ed when the blood is not thoroughly mixed with the<br />
additive.<br />
d<br />
If a rout<strong>in</strong>e coagulati<strong>on</strong> assay is the <strong>on</strong>ly test ordered, then a s<strong>in</strong>gle light blue top tube may be drawn. If there is a c<strong>on</strong>cern about<br />
c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> by tissue fluids or thromboplast<strong>in</strong>s, then a n<strong>on</strong>-additive tube can be drawn before the additive tube. The PST tube c<strong>on</strong>ta<strong>in</strong>s<br />
lithium hepar<strong>in</strong> anticoagulant and a gel separator; if used, draw <strong>in</strong> the order shown.<br />
Source: Table adapted with permissi<strong>on</strong> from WebPath, Mercer University, United States (http://library.med.utah.edu/WebPath/webpath.html).<br />
Order is based <strong>on</strong> United States Nati<strong>on</strong>al Committee for Cl<strong>in</strong>ical Laboratory Standards c<strong>on</strong>sensus (43).<br />
16 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Step 9 – Clean c<strong>on</strong>tam<strong>in</strong>ated surfaces and complete patient procedure<br />
• Discard the used needle and syr<strong>in</strong>ge or blood sampl<strong>in</strong>g device <strong>in</strong>to a puncture-resistant<br />
sharps c<strong>on</strong>ta<strong>in</strong>er.<br />
• Check the label and forms for accuracy. The label should be clearly written with the<br />
<strong>in</strong>formati<strong>on</strong> required by the laboratory, which is typically the patient’s first and last names,<br />
file number, date of birth, and the date and time when the blood was taken.<br />
• Discard used items <strong>in</strong>to the appropriate category of waste. Items used for phlebotomy that<br />
would not release a drop of blood if squeezed (e.g. gloves) may be discarded <strong>in</strong> the general<br />
waste, unless local regulati<strong>on</strong>s state otherwise.<br />
• Perform hand hygiene aga<strong>in</strong>, as described above.<br />
• Recheck the labels <strong>on</strong> the tubes and the forms before dispatch.<br />
• Inform the patient when the procedure is over.<br />
• Ask the patient or d<strong>on</strong>or how they are feel<strong>in</strong>g. Check the <strong>in</strong>serti<strong>on</strong> site to verify that it is not<br />
bleed<strong>in</strong>g, then thank the patient and say someth<strong>in</strong>g reassur<strong>in</strong>g and encourag<strong>in</strong>g before the<br />
pers<strong>on</strong> leaves.<br />
Step 10 – Prepare samples for transportati<strong>on</strong><br />
• Pack laboratory samples safely <strong>in</strong> a plastic leak-proof bag with an outside compartment<br />
for the laboratory request form. Plac<strong>in</strong>g the requisiti<strong>on</strong> <strong>on</strong> the outside helps avoid<br />
c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong>.<br />
• If there are multiple tubes, place them <strong>in</strong> a rack or padded holder to avoid breakage dur<strong>in</strong>g<br />
transportati<strong>on</strong>.<br />
Step 11 – Clean up spills of blood or body fluids<br />
If blood spillage has occurred (e.g. because of a laboratory sample break<strong>in</strong>g <strong>in</strong> the phlebotomy<br />
area or dur<strong>in</strong>g transportati<strong>on</strong>, or excessive bleed<strong>in</strong>g dur<strong>in</strong>g the procedure), clean it up. An<br />
example of a safe procedure is given below.<br />
• Put <strong>on</strong> gloves and a gown or apr<strong>on</strong> if c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> or bleach<strong>in</strong>g of a uniform is likely <strong>in</strong> a<br />
large spill.<br />
• Mop up liquid from large spills us<strong>in</strong>g paper towels, and place them <strong>in</strong>to the <strong>in</strong>fectious<br />
waste.<br />
• Remove as much blood as possible with wet cloths before dis<strong>in</strong>fect<strong>in</strong>g.<br />
• Assess the surface to see whether it will be damaged by a bleach and water soluti<strong>on</strong>.<br />
• For cement, metal and other surfaces that can tolerate a str<strong>on</strong>ger bleach soluti<strong>on</strong>, flood the<br />
area with an approximately 5000 parts per milli<strong>on</strong> (ppm) soluti<strong>on</strong> of sodium hypochlorite<br />
(1:10 diluti<strong>on</strong> of a 5.25% chlor<strong>in</strong>e bleach to water). This is the preferred c<strong>on</strong>centrati<strong>on</strong> for<br />
large spills (44). Leave the area wet for 10 m<strong>in</strong>utes.<br />
• For surfaces that may be corroded or discoloured by a str<strong>on</strong>g bleach, clean carefully to<br />
remove all visible sta<strong>in</strong>s. Make a weaker soluti<strong>on</strong> and leave it <strong>in</strong> c<strong>on</strong>tact for a l<strong>on</strong>ger period<br />
of time. For example, an approximately 525 ppm soluti<strong>on</strong> (1:100 diluti<strong>on</strong> of 5.25% bleach)<br />
is effective.<br />
• Prepare bleach soluti<strong>on</strong> fresh daily and keep it <strong>in</strong> a closed c<strong>on</strong>ta<strong>in</strong>er because it degrades<br />
over time and <strong>in</strong> c<strong>on</strong>tact with the sun.<br />
If a pers<strong>on</strong> was exposed to blood through n<strong>on</strong><strong>in</strong>tact sk<strong>in</strong>, mucous membranes or a puncture<br />
wound, complete an <strong>in</strong>cident report, as described <strong>in</strong> <str<strong>on</strong>g>WHO</str<strong>on</strong>g> best practices for <strong>in</strong>jecti<strong>on</strong>s and<br />
related procedures toolkit. For transportati<strong>on</strong> of blood samples outside a hospital, equip the<br />
transportati<strong>on</strong> vehicle with a blood spillage kit. Annex H has further <strong>in</strong>formati<strong>on</strong> <strong>on</strong> deal<strong>in</strong>g with<br />
a blood spillage.<br />
2 <strong>Best</strong> practices <strong>in</strong> phlebotomy 17
2.3 Illustrati<strong>on</strong>s for best practices <strong>in</strong> phlebotomy<br />
Figure 2. 1 Venepuncture <strong>in</strong> adults<br />
1. Assemble equipment and <strong>in</strong>clude needle and syr<strong>in</strong>ge or vacuum tube, depend<strong>in</strong>g <strong>on</strong> which is to be used.<br />
2. Perform hand hygiene (if us<strong>in</strong>g soap and water, 3. Identify and prepare the patient.<br />
dry hands with s<strong>in</strong>gle-use towels).<br />
Ulnar nerve<br />
Median<br />
cubital ve<strong>in</strong><br />
Ulnar artery<br />
Basilic ve<strong>in</strong><br />
4. Select the site, preferably at the antecubital<br />
area (i.e. the bend of the elbow). Warm<strong>in</strong>g the<br />
arm with a hot pack, or hang<strong>in</strong>g the hand down<br />
may make it easier to see the ve<strong>in</strong>s. Palpate<br />
the area to locate the anatomic landmarks.<br />
DO NOT touch the site <strong>on</strong>ce alcohol or other<br />
antiseptic has been applied.<br />
5. Apply a tourniquet, about 4–5 f<strong>in</strong>ger widths<br />
above the selected venepuncture site.<br />
18 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
6. Ask the patient to form a fist<br />
so that the ve<strong>in</strong>s are more<br />
prom<strong>in</strong>ent.<br />
7. Put <strong>on</strong> well-fitt<strong>in</strong>g, n<strong>on</strong>-sterile<br />
gloves.<br />
8. Dis<strong>in</strong>fect the site us<strong>in</strong>g 70%<br />
isopropyl alcohol for 30 sec<strong>on</strong>ds<br />
and allow to dry completely<br />
(30 sec<strong>on</strong>ds).<br />
9. Anchor the ve<strong>in</strong> by hold<strong>in</strong>g<br />
the patient’s arm and<br />
plac<strong>in</strong>g a thumb BELOW the<br />
venepuncture site.<br />
10. Enter the ve<strong>in</strong> swiftly at a<br />
30 degree angle.<br />
11. Once sufficient blood has been<br />
collected, release the tourniquet<br />
BEFORE withdraw<strong>in</strong>g the needle.<br />
12. Withdraw the needle gently<br />
and then give the patient a<br />
clean gauze or dry cott<strong>on</strong>-wool<br />
ball to apply to the site with<br />
gentle pressure.<br />
13. Discard the used needle and<br />
syr<strong>in</strong>ge or blood-sampl<strong>in</strong>g<br />
device <strong>in</strong>to a punctureresistant<br />
c<strong>on</strong>ta<strong>in</strong>er.<br />
14. Check the label and forms for<br />
accuracy.<br />
15. Discard sharps and broken<br />
glass <strong>in</strong>to the sharps<br />
c<strong>on</strong>ta<strong>in</strong>er. Place items that can<br />
drip blood or body fluids <strong>in</strong>to<br />
the <strong>in</strong>fectious waste.<br />
16. Remove gloves and place<br />
them <strong>in</strong> the general waste.<br />
Perform hand hygiene. If us<strong>in</strong>g<br />
soap and water, dry hands<br />
with s<strong>in</strong>gle-use towels.<br />
2 <strong>Best</strong> practices <strong>in</strong> phlebotomy 19
Figure 2. 2 Fill<strong>in</strong>g tubes<br />
1. If the tube does not have a<br />
rubber stopper, press the<br />
plunger <strong>in</strong> slowly to reduce<br />
haemolysis (this is safer than<br />
remov<strong>in</strong>g the needle).<br />
2. Place the stopper <strong>in</strong> the tube. 3. Follow<strong>in</strong>g laboratory <strong>in</strong>structi<strong>on</strong>s,<br />
<strong>in</strong>vert the sample gently to mix<br />
the additives with the blood<br />
before dispatch.<br />
20 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
3 <strong>Blood</strong>-sampl<strong>in</strong>g systems<br />
Users of these guidel<strong>in</strong>es should read Chapter 2 before read<strong>in</strong>g the <strong>in</strong>formati<strong>on</strong> given below.<br />
This chapter covers background <strong>in</strong>formati<strong>on</strong> (Secti<strong>on</strong> 3.1), practical guidance (Secti<strong>on</strong> 3.2) and<br />
illustrati<strong>on</strong>s (Secti<strong>on</strong> 3.3) relevant to closed and open blood-sampl<strong>in</strong>g systems.<br />
Several blood-sampl<strong>in</strong>g systems are available for phlebotomy. The system most appropriate<br />
for the procedure should be chosen. Annex C provides detailed <strong>in</strong>formati<strong>on</strong> <strong>on</strong> all the systems<br />
available for draw<strong>in</strong>g blood, and outl<strong>in</strong>es the advantages and disadvantages of each device.<br />
3.1 Background <strong>in</strong>formati<strong>on</strong> <strong>on</strong> blood-sampl<strong>in</strong>g systems<br />
3.1.1 Closed systems<br />
Closed systems for blood sampl<strong>in</strong>g are preferable because they have proven to be safer than open<br />
systems (23).<br />
Needle and syr<strong>in</strong>ge<br />
The use of a hypodermic needle and syr<strong>in</strong>ge is the most comm<strong>on</strong> means of blood sampl<strong>in</strong>g.<br />
Choice of gauge<br />
If the needle is too large for the ve<strong>in</strong> for which it is <strong>in</strong>tended, it will tear the ve<strong>in</strong> and cause<br />
bleed<strong>in</strong>g (haematoma); if the needle is too small, it will damage the blood cells dur<strong>in</strong>g sampl<strong>in</strong>g,<br />
and laboratory tests that require whole blood cells, or haemoglob<strong>in</strong> and free plasma, will be<br />
<strong>in</strong>valid.<br />
<strong>Blood</strong> collecti<strong>on</strong> for transfusi<strong>on</strong> requires a larger gauge than is used for blood draw<strong>in</strong>g.<br />
Vacuum extracti<strong>on</strong> systems<br />
The use of vacuum extracti<strong>on</strong> tube systems as closed systems for blood collect<strong>in</strong>g reduces the<br />
risk of direct exposure to blood and has made it easier to take multiple samples from a s<strong>in</strong>gle<br />
venepuncture.<br />
Vacuum extracti<strong>on</strong> systems are widely available <strong>in</strong> most well-resourced countries. These are<br />
recommended, but users should check their own country’s recommendati<strong>on</strong>s. Although vacuum<br />
extracti<strong>on</strong> systems are safe, tra<strong>in</strong><strong>in</strong>g and skill is required for their use.<br />
Double-ended needles are available <strong>in</strong> several recommended gauge sizes. The end covered by<br />
a rubber cuff is screwed <strong>in</strong>to the barrel (also known as the tube holder, evacuated tube needle<br />
holder or bulldog). A thread separates the two ends, and this is where the barrel is screwed <strong>in</strong>to<br />
place. The barrel holds the sample collecti<strong>on</strong> tube <strong>in</strong> place and protects the phlebotomist from<br />
direct c<strong>on</strong>tact with blood. The sample tube is under vacuum. Once the needle is <strong>in</strong> the ve<strong>in</strong>, the<br />
tube is pressed <strong>on</strong> to the needle and the blood is drawn automatically <strong>in</strong>to the sample tube by<br />
vacuum until the required amount is collected. This system comes complete with needle, barrel<br />
and the laboratory sample tubes with appropriately coloured tops for different types of samples.<br />
Tubes for adult and paediatric specimens are available.<br />
Discard the barrel and syr<strong>in</strong>ge as a s<strong>in</strong>gle entity where possible. If there is a need to reuse the<br />
barrel, use a <strong>on</strong>e-hand scoop technique (Annex G) to cover the sharp end of the needle and thus<br />
to safely remove the needle from the barrel. Alternately, use a sharps c<strong>on</strong>ta<strong>in</strong>er with a needle<br />
removal hold, aga<strong>in</strong> employ<strong>in</strong>g a <strong>on</strong>e-handed technique.<br />
3 <strong>Blood</strong>-sampl<strong>in</strong>g systems 21
Some systems have a mechanism that can be activated <strong>on</strong>ce the needle has been used; the<br />
mechanism retracts the used needle <strong>in</strong>to the barrel and snaps it shut. Others have a quickrelease<br />
mechanism to dislodge the used needle <strong>in</strong>to the sharps c<strong>on</strong>ta<strong>in</strong>er.<br />
Vacuum systems may also be used with a w<strong>in</strong>ged butterfly needle and luer-lock c<strong>on</strong>nectors.<br />
W<strong>in</strong>ged butterfly needles are also available with safety-eng<strong>in</strong>eered devices.<br />
The sharps c<strong>on</strong>ta<strong>in</strong>er must be with<strong>in</strong> arm’s reach and clearly visible, to ensure safe disposal of<br />
sharps.<br />
3.1.2 Open systems<br />
Open systems <strong>in</strong>clude hypodermic needle and syr<strong>in</strong>ges, as well as w<strong>in</strong>ged steel needles attached<br />
to a syr<strong>in</strong>ge.<br />
3.2 Practical guidance <strong>on</strong> blood-sampl<strong>in</strong>g systems<br />
3.2.1 Needle and syr<strong>in</strong>ge<br />
To use a needle and syr<strong>in</strong>ge system:<br />
• open the packag<strong>in</strong>g of the hypodermic needle from the hub end (back of the needle),<br />
keep<strong>in</strong>g it capped;<br />
• open the sterile packag<strong>in</strong>g of the syr<strong>in</strong>ge from the plunger end (back of the syr<strong>in</strong>ge),<br />
keep<strong>in</strong>g the nozzle protected <strong>in</strong> the packag<strong>in</strong>g;<br />
• carefully remove the syr<strong>in</strong>ge from the packag<strong>in</strong>g and <strong>in</strong>sert the nozzle of the syr<strong>in</strong>ge firmly<br />
<strong>in</strong>to the exposed hub of the capped hypodermic needle;<br />
• leave the needle and syr<strong>in</strong>ge <strong>in</strong> place until ready for use.<br />
3.2.2 Choice of gauge<br />
Choose the gauge of hypodermic needle that fits comfortably <strong>in</strong>to the most prom<strong>in</strong>ent ve<strong>in</strong> with<br />
little discomfort (Table 3.1).<br />
Table 3.1<br />
Recommended needle gauge, length and device for rout<strong>in</strong>e <strong>in</strong>jecti<strong>on</strong> and phlebotomy<br />
procedures for different age groups<br />
Needle<br />
gauge<br />
Adult<br />
Patient populati<strong>on</strong><br />
Paediatric,<br />
elderly, small ve<strong>in</strong>s Ne<strong>on</strong>atal Procedure<br />
16–18 <strong>Blood</strong> d<strong>on</strong>ati<strong>on</strong><br />
19–20 NA NA NA<br />
21 (1–1.5 <strong>in</strong>ch or<br />
2.54 cm)<br />
22 (1 <strong>in</strong>ch or<br />
2.54 cm)<br />
23 (1–1.5 <strong>in</strong>ch or<br />
2.54 cm)<br />
NA, not applicable.<br />
NA<br />
(1 <strong>in</strong>ch or<br />
2.54 cm)<br />
(W<strong>in</strong>ged set<br />
[butterfly]; 0.5 <strong>in</strong>ch<br />
or 0.75 cm)<br />
NA<br />
NA<br />
(W<strong>in</strong>ged set<br />
[butterfly]; 0.5 <strong>in</strong>ch<br />
or 0.75 cm)<br />
22 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
3.3 Illustrati<strong>on</strong>s for blood-sampl<strong>in</strong>g systems<br />
Figure 3.1 <strong>Blood</strong>-sampl<strong>in</strong>g systems<br />
Needle and syr<strong>in</strong>ge system<br />
Remove the syr<strong>in</strong>ge from the<br />
packag<strong>in</strong>g and <strong>in</strong>sert the nozzle<br />
of the syr<strong>in</strong>ge firmly <strong>in</strong>to the<br />
exposed hub of the capped<br />
hypodermic needle.<br />
Vacuum extracti<strong>on</strong> system<br />
The barrel holds the sample<br />
collecti<strong>on</strong> tube <strong>in</strong> place and<br />
protects the phlebotomist from<br />
direct c<strong>on</strong>tact with blood. Do not<br />
push the laboratory tube <strong>on</strong>to the<br />
needle <strong>in</strong>side the barrel until the<br />
needle is <strong>in</strong> the blood vessel, or<br />
the vacuum will be lost.<br />
W<strong>in</strong>ged butterfly system<br />
(vacuum extracti<strong>on</strong>)<br />
A vacuum system comb<strong>in</strong>ed with<br />
a w<strong>in</strong>ged butterfly needle.<br />
Do not push the laboratory tube<br />
<strong>on</strong>to the needle <strong>in</strong>side the barrel<br />
until the w<strong>in</strong>ged needle is <strong>in</strong>side<br />
the blood vessel or the vacuum<br />
will be lost.<br />
W<strong>in</strong>ged butterfly system<br />
(syr<strong>in</strong>ge)<br />
A syr<strong>in</strong>ge comb<strong>in</strong>ed with a<br />
w<strong>in</strong>ged butterfly needle.<br />
3 <strong>Blood</strong>-sampl<strong>in</strong>g systems 23
4 Venepuncture for blood d<strong>on</strong>ati<strong>on</strong><br />
The <strong>in</strong>formati<strong>on</strong> given here supplements that given <strong>in</strong> Chapters 2 and 3. Users of these<br />
guidel<strong>in</strong>es should read Chapters 2 and 3 before read<strong>in</strong>g the <strong>in</strong>formati<strong>on</strong> given below. This<br />
chapter covers background <strong>in</strong>formati<strong>on</strong> (Secti<strong>on</strong> 4.1) and practical guidance (Secti<strong>on</strong> 4.2)<br />
relevant to venepuncture for blood d<strong>on</strong>ati<strong>on</strong>.<br />
4.1 Background <strong>in</strong>formati<strong>on</strong> <strong>on</strong> venepuncture for blood<br />
d<strong>on</strong>ati<strong>on</strong><br />
<strong>Blood</strong> banks use various processes to try to prevent <strong>in</strong>fecti<strong>on</strong>s that can be transmitted by<br />
<strong>in</strong>fected blood d<strong>on</strong>ati<strong>on</strong>. One important measure to prevent <strong>in</strong>fecti<strong>on</strong> is to recruit d<strong>on</strong>ors from<br />
populati<strong>on</strong>s that are known to have low rates of <strong>in</strong>fecti<strong>on</strong> for bloodborne diseases, such as<br />
voluntary, unpaid d<strong>on</strong>ors and people with no history of <strong>in</strong>travenous drug use. A sec<strong>on</strong>d measure<br />
is to ask d<strong>on</strong>ors a series of additi<strong>on</strong>al screen<strong>in</strong>g questi<strong>on</strong>s (these will vary by regi<strong>on</strong>) to help<br />
identify those who may be at higher risk of <strong>in</strong>fecti<strong>on</strong>. Phlebotomists must adhere strictly to the<br />
rules for <strong>in</strong>clud<strong>in</strong>g and exclud<strong>in</strong>g blood d<strong>on</strong>ors. A third measure is to test d<strong>on</strong>ated blood for<br />
<strong>in</strong>fecti<strong>on</strong>s comm<strong>on</strong> <strong>in</strong> the area before process<strong>in</strong>g it for use for various therapeutic purposes.<br />
The process for collect<strong>in</strong>g blood from d<strong>on</strong>ors is similar to that used for blood sampl<strong>in</strong>g; however,<br />
a few additi<strong>on</strong>al measures are required for collecti<strong>on</strong> of d<strong>on</strong>ated blood. These measures are<br />
primarily to ensure patient safety, but also to m<strong>in</strong>imize exogenous c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of a d<strong>on</strong>ated<br />
blood unit or its derived comp<strong>on</strong>ents, particularly c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> from the sk<strong>in</strong> flora of the<br />
d<strong>on</strong>or’s arm. Because of the volume or blood collected and the length of storage, pathogens can<br />
multiply dur<strong>in</strong>g storage. Safe collecti<strong>on</strong> ensures that the blood products are safe for therapeutic<br />
use throughout their shelf life.<br />
Sk<strong>in</strong> flora is a comm<strong>on</strong> source of c<strong>on</strong>tam<strong>in</strong>ants; it is therefore important to use an effective<br />
antiseptic <strong>on</strong> the d<strong>on</strong>or’s arm before blood d<strong>on</strong>ati<strong>on</strong>. Transfusi<strong>on</strong> with blood comp<strong>on</strong>ents that<br />
are c<strong>on</strong>tam<strong>in</strong>ated with exogenous bacteria or other agents can cause fatal complicati<strong>on</strong>s<br />
(30, 45). Studies <strong>on</strong> the topic have been <strong>in</strong>c<strong>on</strong>clusive (46); however, based <strong>on</strong> available literature<br />
and expert op<strong>in</strong>i<strong>on</strong>, the recommended opti<strong>on</strong> for sk<strong>in</strong> antisepsis for blood d<strong>on</strong>ati<strong>on</strong> is the <strong>on</strong>estep<br />
applicati<strong>on</strong> of a comb<strong>in</strong>ati<strong>on</strong> of 2% chlorhexid<strong>in</strong>e gluc<strong>on</strong>ate and 70% isopropyl alcohol for<br />
30 sec<strong>on</strong>ds, followed by 30 sec<strong>on</strong>ds dry<strong>in</strong>g time (47–49).<br />
<strong>Blood</strong> d<strong>on</strong>ati<strong>on</strong>s should be collected <strong>on</strong>ly by tra<strong>in</strong>ed and qualified blood transfusi<strong>on</strong> services<br />
pers<strong>on</strong>nel.<br />
4.1.1 M<strong>in</strong>imum requirements for venepuncture for blood d<strong>on</strong>ati<strong>on</strong><br />
The relevant guidance given <strong>in</strong> Chapter 2 <strong>on</strong> plann<strong>in</strong>g, locati<strong>on</strong> and <strong>in</strong>fecti<strong>on</strong> preventi<strong>on</strong> and<br />
c<strong>on</strong>trol practices should be followed, as should the guidance <strong>in</strong> Chapter 3 <strong>on</strong> closed systems.<br />
Additi<strong>on</strong>al requirements for a collecti<strong>on</strong> system for blood d<strong>on</strong>ati<strong>on</strong> are listed below.<br />
• Equipment:<br />
––<br />
All equipment used for collecti<strong>on</strong> of blood d<strong>on</strong>ati<strong>on</strong>s should be regularly calibrated,<br />
ma<strong>in</strong>ta<strong>in</strong>ed and serviced, as required. Such equipment <strong>in</strong>cludes blood pressure<br />
m<strong>on</strong>itors, scales, d<strong>on</strong>or couches or chairs, blood collecti<strong>on</strong> m<strong>on</strong>itors or mixers, blood<br />
bag tube sealers, blood transportati<strong>on</strong> boxes and blood bank refrigerators.<br />
– – Furniture and equipment <strong>in</strong> the area of blood d<strong>on</strong>ati<strong>on</strong> and process<strong>in</strong>g should be made<br />
of cleanable surfaces (e.g. v<strong>in</strong>yl rather than fabric). C<strong>on</strong>ta<strong>in</strong>ers used to transport supplies<br />
and specimens should also be cleanable by dis<strong>in</strong>fectants such as sodium hypochlorite<br />
bleach soluti<strong>on</strong>s. Fabric or textile carriers should be mach<strong>in</strong>e washable.<br />
4 Venepuncture for blood d<strong>on</strong>ati<strong>on</strong> 25
––<br />
A closed collecti<strong>on</strong> system with a sterile blood collecti<strong>on</strong> bag c<strong>on</strong>ta<strong>in</strong><strong>in</strong>g anticoagulant,<br />
and with an <strong>in</strong>tegrally attached tube and needle should be used. Some bags <strong>in</strong>clude<br />
diversi<strong>on</strong> pouches to sequester the first 20 ml of blood collected, to m<strong>in</strong>imize<br />
c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> from sk<strong>in</strong> flora and the sk<strong>in</strong> core (50). If blood for haemoglob<strong>in</strong> test<strong>in</strong>g is<br />
gathered with a capillary stick, a s<strong>in</strong>gle-use sterile lancet should be used and then placed<br />
immediately <strong>in</strong> a safety box.<br />
• Locati<strong>on</strong>:<br />
––<br />
Premises should be of sufficient size for efficient operati<strong>on</strong>s, with separate areas for<br />
clean and dirty processes, clean runn<strong>in</strong>g water, and surfaces cleanable by dis<strong>in</strong>fectants.<br />
––<br />
Floors should not be carpeted.<br />
––<br />
Wait<strong>in</strong>g areas should be outside the collecti<strong>on</strong> area, to m<strong>in</strong>imize the risk of respiratory<br />
pathogens for workers.<br />
––<br />
All fixed and mobile blood d<strong>on</strong>ati<strong>on</strong> sites should be safe, clean, hygienic and tidy, and<br />
should meet def<strong>in</strong>ed standards of envir<strong>on</strong>mental safety.<br />
––<br />
The d<strong>on</strong>ati<strong>on</strong> sites should be organized <strong>in</strong> a way that ensures the safety of blood d<strong>on</strong>ors,<br />
staff and d<strong>on</strong>ated blood units, and avoids errors <strong>in</strong> the blood d<strong>on</strong>ati<strong>on</strong> process.<br />
4.1.2 Before a blood d<strong>on</strong>ati<strong>on</strong><br />
<str<strong>on</strong>g>WHO</str<strong>on</strong>g> has developed a set of basic requirements for blood transfusi<strong>on</strong> services, which cover the<br />
steps to take before d<strong>on</strong>ati<strong>on</strong> (51). <strong>Blood</strong> d<strong>on</strong>ati<strong>on</strong> should be voluntary; it should not <strong>in</strong>volve<br />
duress, coerci<strong>on</strong> or remunerati<strong>on</strong>. Also, potential blood d<strong>on</strong>ors should be selected carefully,<br />
accord<strong>in</strong>g to the nati<strong>on</strong>al criteria for d<strong>on</strong>or selecti<strong>on</strong>.<br />
Before a pers<strong>on</strong> d<strong>on</strong>ates blood (52):<br />
• the potential d<strong>on</strong>or should be given pre-d<strong>on</strong>ati<strong>on</strong> <strong>in</strong>formati<strong>on</strong>, advice and counsell<strong>in</strong>g<br />
about the process of blood d<strong>on</strong>ati<strong>on</strong>;<br />
• a relevant history of the d<strong>on</strong>or should be taken, cover<strong>in</strong>g health and high-risk behaviour,<br />
and <strong>in</strong>clud<strong>in</strong>g<br />
––<br />
history of mastectomy (blood should be taken from the arm opposite the site of surgery)<br />
(48, 53);<br />
––<br />
current and recent medicati<strong>on</strong>s or chr<strong>on</strong>ic <strong>in</strong>fecti<strong>on</strong>s;<br />
––<br />
history of prol<strong>on</strong>ged bleed<strong>in</strong>g or a past diagnosis of bleed<strong>in</strong>g disorders;<br />
––<br />
history of previous d<strong>on</strong>ati<strong>on</strong>s, to ensure the wait<strong>in</strong>g period is respected;<br />
• a prelim<strong>in</strong>ary physical check-up of the d<strong>on</strong>or should be d<strong>on</strong>e, <strong>in</strong>clud<strong>in</strong>g weight, blood<br />
pressure, signs of <strong>in</strong>fecti<strong>on</strong> or scarr<strong>in</strong>g at potential sites;<br />
• the d<strong>on</strong>or should be offered fluids, to help reduce the risk of fa<strong>in</strong>t<strong>in</strong>g after blood d<strong>on</strong>ati<strong>on</strong><br />
(54);<br />
• the pers<strong>on</strong> should provide <strong>in</strong>formed written c<strong>on</strong>sent, based <strong>on</strong> the nati<strong>on</strong>al requirements.<br />
26 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
4.2 Practical guidance <strong>on</strong> venepuncture for blood d<strong>on</strong>ati<strong>on</strong><br />
4.2.1 Collect<strong>in</strong>g blood<br />
For collecti<strong>on</strong> of blood for d<strong>on</strong>ati<strong>on</strong>, use the procedure detailed <strong>in</strong> Chapter 2 for blood sampl<strong>in</strong>g<br />
(e.g. for hand hygiene and glove use), as far as it is relevant, and follow the six steps given below.<br />
Step1 – Identify d<strong>on</strong>or and label blood collecti<strong>on</strong> bag and test tubes<br />
• Ask the d<strong>on</strong>or to state their full name.<br />
• Ensure that:<br />
––<br />
the blood collecti<strong>on</strong> bag is of the correct type;<br />
––<br />
the labels <strong>on</strong> the blood collecti<strong>on</strong> bag and all its satellite bags, sample tubes and d<strong>on</strong>or<br />
records have the correct patient name and number;<br />
––<br />
the <strong>in</strong>formati<strong>on</strong> <strong>on</strong> the labels matches with the d<strong>on</strong>or’s <strong>in</strong>formati<strong>on</strong>.<br />
Step 2 – Select the ve<strong>in</strong><br />
• Select a large, firm ve<strong>in</strong>, preferably <strong>in</strong> the antecubital fossa, from an area free from sk<strong>in</strong><br />
lesi<strong>on</strong>s or scars.<br />
• Apply a tourniquet or blood pressure cuff <strong>in</strong>flated to 40–60 mm Hg, to make the ve<strong>in</strong> more<br />
prom<strong>in</strong>ent.<br />
• Ask the d<strong>on</strong>or to open and close the hand a few times.<br />
• Once the ve<strong>in</strong> is selected, release the pressure device or tourniquet before the sk<strong>in</strong> site is<br />
prepared.<br />
Step 3 – Dis<strong>in</strong>fect the sk<strong>in</strong><br />
• If the site selected for venepuncture is visibly dirty, wash the area with soap and water, and<br />
then wipe it dry with s<strong>in</strong>gle-use towels.<br />
• One-step procedure (recommended – takes about <strong>on</strong>e m<strong>in</strong>ute):<br />
––<br />
use a product comb<strong>in</strong><strong>in</strong>g 2% chlorhexid<strong>in</strong>e gluc<strong>on</strong>ate <strong>in</strong> 70% isopropyl alcohol;<br />
––<br />
cover the whole area and ensure that the sk<strong>in</strong> area is <strong>in</strong> c<strong>on</strong>tact with the dis<strong>in</strong>fectant for<br />
at least 30 sec<strong>on</strong>ds;<br />
––<br />
allow the area to dry completely, or for a m<strong>in</strong>imum of 30 sec<strong>on</strong>ds by the clock.<br />
• Two-step procedure (if chlorhexid<strong>in</strong>e gluc<strong>on</strong>ate <strong>in</strong> 70% isopropyl alcohol is not available,<br />
use the follow<strong>in</strong>g procedure – takes about two m<strong>in</strong>utes):<br />
––<br />
step 1 – use 70% isopropyl alcohol;<br />
––<br />
cover the whole area and ensure that the sk<strong>in</strong> area is <strong>in</strong> c<strong>on</strong>tact with the dis<strong>in</strong>fectant for<br />
at least 30 sec<strong>on</strong>ds;<br />
––<br />
allow the area to dry completely (about 30 sec<strong>on</strong>ds);<br />
––<br />
step 2 – use t<strong>in</strong>cture of iod<strong>in</strong>e (more effective than povid<strong>in</strong>e iod<strong>in</strong>e) or chlorhexid<strong>in</strong>e<br />
(2%);<br />
––<br />
cover the whole area and ensure that the sk<strong>in</strong> area is <strong>in</strong> c<strong>on</strong>tact with the dis<strong>in</strong>fectant for<br />
at least 30 sec<strong>on</strong>ds;<br />
––<br />
allow the area to dry completely (about 30 sec<strong>on</strong>ds).<br />
• Whichever procedure is used, DO NOT touch the venepuncture site <strong>on</strong>ce the sk<strong>in</strong> has been<br />
dis<strong>in</strong>fected.<br />
4 Venepuncture for blood d<strong>on</strong>ati<strong>on</strong> 27
Step 4 – Perform the venepuncture<br />
Perform venepuncture us<strong>in</strong>g a smooth, clean entry with the needle, as described <strong>in</strong> step 6 of<br />
Secti<strong>on</strong> 2.2.3. Take <strong>in</strong>to account the po<strong>in</strong>ts given below, which are specific to blood d<strong>on</strong>ati<strong>on</strong>.<br />
• In general, use a 16-gauge needle (see Table 3.1 <strong>in</strong> Chapter 3), which is usually attached to<br />
the blood collecti<strong>on</strong> bag. Use of a retractable needle or safety needle with a needle cover is<br />
preferred if available, but all should be cut off at the end of the procedure (as described <strong>in</strong><br />
step 6, below) rather than recapped.<br />
• Ask the d<strong>on</strong>or to open and close the fist slowly every 10–12 sec<strong>on</strong>ds dur<strong>in</strong>g collecti<strong>on</strong>.<br />
• Remove the tourniquet when the blood flow is established or after 2 m<strong>in</strong>utes, whichever<br />
comes first.<br />
Step 5 – M<strong>on</strong>itor the d<strong>on</strong>or and the d<strong>on</strong>ated unit<br />
• Closely m<strong>on</strong>itor the d<strong>on</strong>or and the <strong>in</strong>jecti<strong>on</strong> site throughout the d<strong>on</strong>ati<strong>on</strong> process – look<br />
for:<br />
––<br />
sweat<strong>in</strong>g, palor or compla<strong>in</strong>ts of feel<strong>in</strong>g fa<strong>in</strong>t that may precede fa<strong>in</strong>t<strong>in</strong>g;<br />
––<br />
development of a haematoma at the <strong>in</strong>jecti<strong>on</strong> site;<br />
––<br />
changes <strong>in</strong> blood flow that may <strong>in</strong>dicate the needle has moved <strong>in</strong> the ve<strong>in</strong>, and needs to<br />
be repositi<strong>on</strong>ed.<br />
• About every 30 sec<strong>on</strong>ds dur<strong>in</strong>g the d<strong>on</strong>ati<strong>on</strong>, mix the collected blood gently with the<br />
anticoagulant, either manually or by c<strong>on</strong>t<strong>in</strong>uous mechanical mix<strong>in</strong>g.<br />
Step 6 – Remove the needle and collect samples<br />
• Cut off the needle us<strong>in</strong>g a sterile pair of scissors.<br />
• Collect blood samples for laboratory test<strong>in</strong>g.<br />
4.2.2 After a blood d<strong>on</strong>ati<strong>on</strong><br />
D<strong>on</strong>or care<br />
After the blood has been collected:<br />
• ask the d<strong>on</strong>or to rema<strong>in</strong> <strong>in</strong> the chair and relax for a few m<strong>in</strong>utes;<br />
• <strong>in</strong>spect the venepuncture site; if it is not bleed<strong>in</strong>g, apply a bandage to the site; if it is<br />
bleed<strong>in</strong>g, apply further pressure;<br />
• ask the d<strong>on</strong>or to sit up slowly and ask how the pers<strong>on</strong> is feel<strong>in</strong>g;<br />
• before the d<strong>on</strong>or leaves the d<strong>on</strong>ati<strong>on</strong> room, ensure that the pers<strong>on</strong> can stand up without<br />
dizz<strong>in</strong>ess and without a drop <strong>in</strong> blood pressure;<br />
• offer the d<strong>on</strong>or some refreshments.<br />
<strong>Blood</strong> unit and samples<br />
• Transfer the blood unit to a proper storage c<strong>on</strong>ta<strong>in</strong>er accord<strong>in</strong>g to the blood centre<br />
requirements and the product (55–58).<br />
• Ensure that collected blood samples are stored and delivered to the laboratory with<br />
completed documentati<strong>on</strong>, at the recommended temperature, and <strong>in</strong> a leak-proof, closed<br />
c<strong>on</strong>ta<strong>in</strong>er (55, 57, 58).<br />
28 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
4.2.3 Adverse events <strong>in</strong> blood d<strong>on</strong>ati<strong>on</strong><br />
Be aware of possible adverse events, and the acti<strong>on</strong>s to take if these occur (Table 4.1).<br />
Table 4.1 Adverse events <strong>in</strong> blood d<strong>on</strong>ati<strong>on</strong><br />
Adverse<br />
event Incidence Cause Management Remarks<br />
Haematoma 2–3% • Poor or failed<br />
venepuncture<br />
Vasovagal<br />
reacti<strong>on</strong><br />
or fa<strong>in</strong>t,<br />
due to a<br />
hypothalamic<br />
resp<strong>on</strong>se<br />
result<strong>in</strong>g <strong>in</strong><br />
bradycardia,<br />
vomit<strong>in</strong>g,<br />
sweat<strong>in</strong>g,<br />
arterial<br />
dilatati<strong>on</strong> and<br />
a low blood<br />
pressure<br />
1% of all<br />
d<strong>on</strong>ati<strong>on</strong>s<br />
(but more<br />
frequent <strong>in</strong><br />
first-time<br />
d<strong>on</strong>ors –<br />
1.7% versus<br />
0.19%)<br />
• Sk<strong>in</strong> pierced at too<br />
great an angle – and<br />
exit<strong>in</strong>g ve<strong>in</strong><br />
• Needle punctur<strong>in</strong>g<br />
the ve<strong>in</strong> twice dur<strong>in</strong>g<br />
the d<strong>on</strong>ati<strong>on</strong><br />
• Inadequate pressure<br />
after the d<strong>on</strong>ati<strong>on</strong><br />
• Anxiety<br />
• Lowered blood<br />
volume and other<br />
associated causes:<br />
––<br />
hypoglycaemia<br />
––<br />
lack of fluids<br />
––<br />
poor sleep<br />
• Atmosphere <strong>in</strong><br />
d<strong>on</strong>ati<strong>on</strong> room (hot<br />
or humid)<br />
Signs and symptoms<br />
• Star<strong>in</strong>g<br />
• Sigh<strong>in</strong>g<br />
• Pallor or sweat<strong>in</strong>g<br />
• Slow pulse<br />
• Drop <strong>in</strong> blood<br />
pressure<br />
• Vomit<strong>in</strong>g<br />
• Loss of c<strong>on</strong>sciousness<br />
(occasi<strong>on</strong>ally)<br />
• C<strong>on</strong>vulsi<strong>on</strong>s (rare)<br />
• Apply pressure and a firm<br />
bandage<br />
• Advise d<strong>on</strong>or to move arm<br />
freely but to avoid heavy<br />
lift<strong>in</strong>g<br />
• Apologize, and reassure<br />
the d<strong>on</strong>or<br />
Mild vasovagal reacti<strong>on</strong><br />
• Disc<strong>on</strong>t<strong>in</strong>ue d<strong>on</strong>ati<strong>on</strong><br />
• Recl<strong>in</strong>e chair<br />
• Loosen clothes<br />
• M<strong>on</strong>itor blood pressure<br />
and pulse<br />
• Reassure d<strong>on</strong>or<br />
• Give fluids to the d<strong>on</strong>or to<br />
dr<strong>in</strong>k (recovery is usually<br />
rapid)<br />
Severe vasovagal reacti<strong>on</strong><br />
• Call physician<br />
• If the d<strong>on</strong>or becomes<br />
unc<strong>on</strong>scious, put the<br />
pers<strong>on</strong> <strong>in</strong> recovery<br />
positi<strong>on</strong> (i.e. head to the<br />
side and ch<strong>in</strong> up) and<br />
ensure that airways are<br />
clear<br />
• Occasi<strong>on</strong>ally, severe fa<strong>in</strong>t<br />
with delayed recovery, or<br />
epileptiform episode with<br />
or without <strong>in</strong>c<strong>on</strong>t<strong>in</strong>ence,<br />
might occur; this is<br />
usually an anoxic fit<br />
rather than epilepsy<br />
• In the case of an<br />
epileptiform fit, generally,<br />
do not report to d<strong>on</strong>or<br />
because it may cause<br />
unnecessary anxiety<br />
• If <strong>in</strong>c<strong>on</strong>t<strong>in</strong>ence occurs,<br />
then <strong>in</strong>form the d<strong>on</strong>or and<br />
deal with privately<br />
Fa<strong>in</strong>ts<br />
• These are usually self<br />
limit<strong>in</strong>g and do not require<br />
<strong>in</strong>vestigati<strong>on</strong> because<br />
they have no underly<strong>in</strong>g<br />
pathology<br />
Give relevant<br />
c<strong>on</strong>tact <strong>in</strong>formati<strong>on</strong><br />
to d<strong>on</strong>or <strong>in</strong> case<br />
the d<strong>on</strong>or has any<br />
further <strong>in</strong>quiries<br />
Care of the d<strong>on</strong>or<br />
The physician will:<br />
• expla<strong>in</strong> to the<br />
d<strong>on</strong>or the nature<br />
of what has<br />
happened<br />
• reassure the<br />
pers<strong>on</strong> that this is<br />
<strong>on</strong>ly related to the<br />
d<strong>on</strong>ati<strong>on</strong> process<br />
Future d<strong>on</strong>ati<strong>on</strong>s<br />
• Severe fa<strong>in</strong>ts –<br />
pers<strong>on</strong> should not<br />
d<strong>on</strong>ate aga<strong>in</strong><br />
• Mild fa<strong>in</strong>ts –<br />
pers<strong>on</strong> may<br />
d<strong>on</strong>ate, but<br />
defer if develops<br />
another fa<strong>in</strong>t<strong>in</strong>g<br />
attack<br />
4 Venepuncture for blood d<strong>on</strong>ati<strong>on</strong> 29
Table 4.1 c<strong>on</strong>t<strong>in</strong>ued<br />
Adverse<br />
event Incidence Cause Management Remarks<br />
Delayed fa<strong>in</strong>t<br />
(syncope)<br />
Arterial<br />
puncture<br />
Nerve<br />
damage<br />
Sources: (8–10, 54).<br />
1 <strong>in</strong> 10,000<br />
d<strong>on</strong>ors<br />
1 <strong>in</strong><br />
30,000–<br />
50,000<br />
• Physical stress<br />
• Inadequate fluid<br />
<strong>in</strong>take<br />
• Cause unknown<br />
Occurs 1–4 hours<br />
after d<strong>on</strong>ati<strong>on</strong>, usually<br />
outside the blood bank<br />
• Brachial artery<br />
sometimes lies<br />
anatomically very<br />
close to the ve<strong>in</strong><br />
• Detected by<br />
observ<strong>in</strong>g that the<br />
blood collected is<br />
bright red and has a<br />
rapid flow<br />
• May result <strong>in</strong> late<br />
complicati<strong>on</strong>s such as<br />
arteriovenous fistulae<br />
• Nerve end<strong>in</strong>gs<br />
brushed dur<strong>in</strong>g<br />
venepuncture<br />
• Pressure from<br />
haematoma<br />
Symptoms and signs<br />
• Pa<strong>in</strong> or parasthesia<br />
• Motor or sensory loss<br />
Hot dr<strong>in</strong>ks or water before<br />
d<strong>on</strong>at<strong>in</strong>g blood; sitt<strong>in</strong>g <strong>in</strong><br />
a sup<strong>in</strong>e positi<strong>on</strong>, audio<br />
or visual distracti<strong>on</strong>; and<br />
m<strong>in</strong>imal pa<strong>in</strong> and stress<br />
dur<strong>in</strong>g blood d<strong>on</strong>ati<strong>on</strong><br />
• Disc<strong>on</strong>t<strong>in</strong>ue d<strong>on</strong>ati<strong>on</strong><br />
or c<strong>on</strong>t<strong>in</strong>ue if identified<br />
towards the completi<strong>on</strong> of<br />
the d<strong>on</strong>ati<strong>on</strong><br />
• Call the d<strong>on</strong>or care<br />
physician<br />
• Apply firm pressure (by<br />
the nurse or medical<br />
staff), for at least 15<br />
m<strong>in</strong>utes<br />
• Apply pressure bandage<br />
and check the radial pulse<br />
• Inform and reassure<br />
d<strong>on</strong>or, and expla<strong>in</strong><br />
that the puncture is<br />
unlikely to have serious<br />
c<strong>on</strong>sequences, but that<br />
bad bruis<strong>in</strong>g may occur,<br />
and heal<strong>in</strong>g takes about<br />
10–14 days<br />
• Recovery is usually<br />
sp<strong>on</strong>taneous and rapid<br />
with<strong>in</strong> 24 hours (<strong>in</strong> rare<br />
cases, up to 6 m<strong>on</strong>ths)<br />
• Refer the d<strong>on</strong>or to the<br />
physician to expla<strong>in</strong><br />
and reassure the d<strong>on</strong>or,<br />
and refer the d<strong>on</strong>or to a<br />
neurologist if the damage<br />
is severe<br />
Try to f<strong>in</strong>d cause<br />
Future d<strong>on</strong>ati<strong>on</strong>s<br />
May d<strong>on</strong>ate, but if<br />
develops a sec<strong>on</strong>d<br />
time, then defer<br />
Give relevant<br />
c<strong>on</strong>tact <strong>in</strong>formati<strong>on</strong><br />
to d<strong>on</strong>or <strong>in</strong> case<br />
the pers<strong>on</strong> has any<br />
further <strong>in</strong>quiries<br />
Give relevant<br />
c<strong>on</strong>tact <strong>in</strong>formati<strong>on</strong><br />
to d<strong>on</strong>or <strong>in</strong> case<br />
the d<strong>on</strong>or has any<br />
further <strong>in</strong>quiries<br />
30 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
5 Arterial blood sampl<strong>in</strong>g<br />
The <strong>in</strong>formati<strong>on</strong> given here supplements that given <strong>in</strong> Chapters 2 and 3. Users of these<br />
guidel<strong>in</strong>es should read Chapters 2 and 3 before read<strong>in</strong>g the <strong>in</strong>formati<strong>on</strong> given below. This<br />
chapter covers background <strong>in</strong>formati<strong>on</strong> (Secti<strong>on</strong> 5.1), practical guidance (Secti<strong>on</strong> 5.2) and<br />
illustrati<strong>on</strong>s (Secti<strong>on</strong> 5.3) relevant to arterial blood sampl<strong>in</strong>g.<br />
5.1 Background <strong>in</strong>formati<strong>on</strong> <strong>on</strong> arterial blood sampl<strong>in</strong>g<br />
An arterial blood sample is collected from an artery, primarily to determ<strong>in</strong>e arterial blood gases.<br />
Arterial blood sampl<strong>in</strong>g should <strong>on</strong>ly be performed by health workers for whom the procedure<br />
is <strong>in</strong> the legal scope of practice for their positi<strong>on</strong> <strong>in</strong> their country and who have dem<strong>on</strong>strated<br />
proficiency after formal tra<strong>in</strong><strong>in</strong>g.<br />
The sample can be obta<strong>in</strong>ed either through a catheter placed <strong>in</strong> an artery, or by us<strong>in</strong>g a needle<br />
and syr<strong>in</strong>ge to puncture an artery. These syr<strong>in</strong>ges are pre-hepar<strong>in</strong>ized and handled to m<strong>in</strong>imize<br />
air exposure that will alter the blood gas values. This chapter describes <strong>on</strong>ly the procedure for a<br />
radial artery blood draw.<br />
5.1.1 Choice of site<br />
Several different arteries can be used for blood collecti<strong>on</strong>. The first choice is the radial artery,<br />
which is located <strong>on</strong> the thumb side of the wrist; because of its small size, use of this artery<br />
requires extensive skill <strong>in</strong> arterial blood sampl<strong>in</strong>g. Alternative sites for access are brachial or<br />
femoral arteries, but these have several disadvantages <strong>in</strong> that they:<br />
• may be harder to locate, because they are less superficial than the radial artery;<br />
• have poor collateral circulati<strong>on</strong>;<br />
• are surrounded by structures that could be damaged by faulty technique.<br />
5.1.2 Complicati<strong>on</strong>s related to arterial blood sampl<strong>in</strong>g<br />
There are several potential complicati<strong>on</strong>s related to arterial blood sampl<strong>in</strong>g. The po<strong>in</strong>ts below<br />
list some of the complicati<strong>on</strong>s related to the procedure, and how they can be prevented (59).<br />
• Arteriospasm or <strong>in</strong>voluntary c<strong>on</strong>tracti<strong>on</strong> of the artery may be prevented simply by help<strong>in</strong>g<br />
the patient relax; this can be achieved, for example, by expla<strong>in</strong><strong>in</strong>g the procedure and<br />
positi<strong>on</strong><strong>in</strong>g the pers<strong>on</strong> comfortably.<br />
• Haematoma or excessive bleed<strong>in</strong>g can be prevented by <strong>in</strong>sert<strong>in</strong>g the needle without<br />
punctur<strong>in</strong>g the far side of the vessel and by apply<strong>in</strong>g pressure immediately after blood is<br />
drawn. Due to the higher pressure present <strong>in</strong> arteries, pressure should be applied for a<br />
l<strong>on</strong>ger time than when sampl<strong>in</strong>g from a ve<strong>in</strong>, and should be supervised more closely, to<br />
check for cessati<strong>on</strong> of bleed<strong>in</strong>g.<br />
• Nerve damage can be prevented by choos<strong>in</strong>g an appropriate sampl<strong>in</strong>g site and avoid<strong>in</strong>g<br />
redirecti<strong>on</strong> of the needle.<br />
• Fa<strong>in</strong>t<strong>in</strong>g or a vasovagal resp<strong>on</strong>se can be prevented by ensur<strong>in</strong>g that the patient is sup<strong>in</strong>e<br />
(ly<strong>in</strong>g down <strong>on</strong> their back) with feet elevated before beg<strong>in</strong>n<strong>in</strong>g the blood draw. Patients<br />
requir<strong>in</strong>g arterial blood sampl<strong>in</strong>g are usually <strong>in</strong>patients or <strong>in</strong> the emergency ward, so will<br />
generally already be ly<strong>in</strong>g <strong>in</strong> a hospital bed. Children may feel a loss of c<strong>on</strong>trol and fight<br />
more if placed <strong>in</strong> a sup<strong>in</strong>e positi<strong>on</strong>; <strong>in</strong> such cases, it may be preferable to have the child<br />
sitt<strong>in</strong>g <strong>on</strong> the parent’s lap, so that the parent can gently restra<strong>in</strong> the child.<br />
• Other problems can <strong>in</strong>clude a drop <strong>in</strong> blood pressure, compla<strong>in</strong>ts of feel<strong>in</strong>g fa<strong>in</strong>t, sweat<strong>in</strong>g<br />
or pallor that may precede a loss of c<strong>on</strong>sciousness.<br />
5 Arterial blood sampl<strong>in</strong>g 31
5.1.3 Sampl<strong>in</strong>g errors<br />
Inappropriate collecti<strong>on</strong> and handl<strong>in</strong>g of arterial blood specimens can produce <strong>in</strong>correct results.<br />
Reas<strong>on</strong>s for an <strong>in</strong>accurate blood result <strong>in</strong>clude:<br />
• presence of air <strong>in</strong> the sample;<br />
• collecti<strong>on</strong> of venous rather than arterial blood;<br />
• an improper quantity of hepar<strong>in</strong> <strong>in</strong> the syr<strong>in</strong>ge, or improper mix<strong>in</strong>g after blood is drawn;<br />
• a delay <strong>in</strong> specimen transportati<strong>on</strong>.<br />
5.2 Practical guidance <strong>on</strong> arterial blood sampl<strong>in</strong>g<br />
5.2.1 Equipment and supplies<br />
Assemble the relevant items described <strong>in</strong> Secti<strong>on</strong> 2.2.3, plus the follow<strong>in</strong>g specimen collecti<strong>on</strong><br />
equipment and supplies:<br />
• pre-hepar<strong>in</strong>ized syr<strong>in</strong>ge;<br />
• needles (20, 23 and 25 gauge, of different lengths) – choose a size that is appropriate for the<br />
site (smaller gauges are more likely to lyse the specimen);<br />
• a safety syr<strong>in</strong>ge with a needle cover that allows the syr<strong>in</strong>ge to be capped before transport,<br />
without manually recapp<strong>in</strong>g (this is best practice for radial blood sampl<strong>in</strong>g);<br />
• a bandage to cover the puncture site after collecti<strong>on</strong>;<br />
• a c<strong>on</strong>ta<strong>in</strong>er with crushed ice for transportati<strong>on</strong> of the sample to the laboratory (if the<br />
analysis is not d<strong>on</strong>e at the po<strong>in</strong>t of care);<br />
• where applicable, local anesthetic and an additi<strong>on</strong>al s<strong>in</strong>gle-use sterile syr<strong>in</strong>ge and needle.<br />
5.2.2 Procedure for arterial blood sampl<strong>in</strong>g us<strong>in</strong>g radial artery<br />
For sampl<strong>in</strong>g from the radial artery us<strong>in</strong>g a needle and syr<strong>in</strong>ge, follow the steps outl<strong>in</strong>ed below.<br />
1. Approach the patient, <strong>in</strong>troduce yourself and ask the patient to state their full name.<br />
2. Place the patient <strong>on</strong> their back, ly<strong>in</strong>g flat. Ask the nurse for assistance if the patient’s<br />
positi<strong>on</strong> needs to be altered to make them more comfortable. If the patient is clench<strong>in</strong>g<br />
their fist, hold<strong>in</strong>g their breath or cry<strong>in</strong>g, this can change breath<strong>in</strong>g and thus alter the test<br />
result.<br />
3. Locate the radial artery by perform<strong>in</strong>g an Allen test (see Annex I) for collateral circulati<strong>on</strong>.<br />
If the <strong>in</strong>itial test fails to locate the radial artery, repeat the test <strong>on</strong> the other hand. Once<br />
a site is identified, note anatomic landmarks to be able to f<strong>in</strong>d the site aga<strong>in</strong>. If it will be<br />
necessary to palpate the site aga<strong>in</strong>, put <strong>on</strong> sterile gloves.<br />
4. Perform hand hygiene, clear off a bedside work area and prepare supplies. Put <strong>on</strong> an<br />
impervious gown or apr<strong>on</strong>, and face protecti<strong>on</strong>, if exposure to blood is anticipated.<br />
5. Dis<strong>in</strong>fect the sampl<strong>in</strong>g site <strong>on</strong> the patient with 70% alcohol and allow it to dry.<br />
6. If the needle and syr<strong>in</strong>ge are not preassembled, assemble the needle and hepar<strong>in</strong>ized<br />
syr<strong>in</strong>ge and pull the syr<strong>in</strong>ge plunger to the required fill level recommended by the local<br />
laboratory.<br />
7. Hold<strong>in</strong>g the syr<strong>in</strong>ge and needle like a dart, use the <strong>in</strong>dex f<strong>in</strong>ger to locate the pulse aga<strong>in</strong>,<br />
<strong>in</strong>form the patient that the sk<strong>in</strong> is about to be pierced then <strong>in</strong>sert the needle at a 45 degree<br />
angle, approximately 1 cm distal to (i.e. away from) the <strong>in</strong>dex f<strong>in</strong>ger, to avoid c<strong>on</strong>tam<strong>in</strong>at<strong>in</strong>g<br />
the area where the needle enters the sk<strong>in</strong>.<br />
32 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
8. Advance the needle <strong>in</strong>to the radial artery until a blood flashback appears, then allow the<br />
syr<strong>in</strong>ge to fill to the appropriate level. DO NOT pull back the syr<strong>in</strong>ge plunger.<br />
9. Withdraw the needle and syr<strong>in</strong>ge; place a clean, dry piece of gauze or cott<strong>on</strong> wool over the<br />
site and have the patient or an assistant apply firm pressure for sufficient time to stop the<br />
bleed<strong>in</strong>g. Check whether bleed<strong>in</strong>g has stopped after 2–3 m<strong>in</strong>utes. Five m<strong>in</strong>utes or more<br />
may be needed for patients who have high blood pressure or a bleed<strong>in</strong>g disorder, or are<br />
tak<strong>in</strong>g anticoagulants.<br />
10. Activate the mechanisms of a safety needle to cover the needle before plac<strong>in</strong>g it <strong>in</strong> the ice<br />
cup. In the absence of a safety-eng<strong>in</strong>eered device, use a <strong>on</strong>e-hand scoop technique (as<br />
expla<strong>in</strong>ed <strong>in</strong> Annex G) to recap the needle after removal.<br />
11. Expel air bubbles, cap the syr<strong>in</strong>ge and roll the specimen between the hands to gently mix<br />
it. Cap the syr<strong>in</strong>ge to prevent c<strong>on</strong>tact between the arterial blood sample and the air, and to<br />
prevent leak<strong>in</strong>g dur<strong>in</strong>g transport to the laboratory.<br />
12. Label the sample syr<strong>in</strong>ge.<br />
13. Dispose appropriately of all used material and pers<strong>on</strong>al protective equipment.<br />
14. Remove gloves and wash hands thoroughly with soap and water, then dry us<strong>in</strong>g s<strong>in</strong>gle-use<br />
towels; alternatively, use alcohol rub soluti<strong>on</strong>.<br />
15. Check the patient site for bleed<strong>in</strong>g (if necessary, apply additi<strong>on</strong>al pressure) and thank the<br />
patient.<br />
16. Transport the sample immediately to the laboratory, follow<strong>in</strong>g laboratory handl<strong>in</strong>g<br />
procedures.<br />
5.3 Illustrati<strong>on</strong>s for arterial blood sampl<strong>in</strong>g<br />
Figure 5.1 Arterial blood sampl<strong>in</strong>g<br />
Locate artery and take a sample<br />
5 Arterial blood sampl<strong>in</strong>g 33
6 Paediatric and ne<strong>on</strong>atal blood sampl<strong>in</strong>g<br />
The <strong>in</strong>formati<strong>on</strong> given here supplements that given <strong>in</strong> Chapters 2 and 3. Users of these<br />
guidel<strong>in</strong>es should read Chapters 2 and 3 before read<strong>in</strong>g the <strong>in</strong>formati<strong>on</strong> given below. This<br />
chapter covers background <strong>in</strong>formati<strong>on</strong> (Secti<strong>on</strong> 6.1), practical guidance (Secti<strong>on</strong> 6.2) and<br />
illustrati<strong>on</strong>s (Secti<strong>on</strong> 6.3) relevant to paediatric and ne<strong>on</strong>atal blood sampl<strong>in</strong>g.<br />
6.1 Background <strong>in</strong>formati<strong>on</strong> <strong>on</strong> paediatric and ne<strong>on</strong>atal blood<br />
sampl<strong>in</strong>g<br />
This chapter discusses aspects specific to paediatric and ne<strong>on</strong>atal blood sampl<strong>in</strong>g (60, 61).<br />
Any<strong>on</strong>e tak<strong>in</strong>g blood from children and ne<strong>on</strong>ates must be well tra<strong>in</strong>ed and practiced <strong>in</strong><br />
venepuncture techniques. A uniform sampl<strong>in</strong>g technique is important to reduce pa<strong>in</strong> and<br />
psychological trauma.<br />
6.1.1 Choice of procedure and site<br />
The choice of site and procedure (venous site, f<strong>in</strong>ger-prick or heel-prick – also referred to as<br />
“capillary sampl<strong>in</strong>g” or “sk<strong>in</strong> puncture”) will depend <strong>on</strong> the volume of blood needed for the<br />
procedure and the type of laboratory test to be d<strong>on</strong>e. Venepuncture is the method of choice<br />
for blood sampl<strong>in</strong>g <strong>in</strong> term ne<strong>on</strong>ates (62, 63); however, it requires an experienced and tra<strong>in</strong>ed<br />
phlebotomist. If a tra<strong>in</strong>ed phlebotomist is not available, the physician may need to draw the<br />
specimen. Secti<strong>on</strong> 7.1 provides <strong>in</strong>formati<strong>on</strong> <strong>on</strong> when a capillary blood specimen from a f<strong>in</strong>gerprick<br />
or a heel-prick is appropriate. The blood from a capillary specimen is similar to an arterial<br />
specimen <strong>in</strong> oxygen c<strong>on</strong>tent, and is suitable for <strong>on</strong>ly a limited number of tests because of its<br />
higher likelihood of c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> with sk<strong>in</strong> flora and smaller total volume.<br />
F<strong>in</strong>ger and heel-prick<br />
Whether to select a f<strong>in</strong>ger-prick or a heel-prick will depend <strong>on</strong> the age and weight of the child.<br />
Secti<strong>on</strong> 7.1 expla<strong>in</strong>s which procedure to select, based <strong>on</strong> these two elements.<br />
Patient immobilizati<strong>on</strong> is crucial to the safety of the paediatric and ne<strong>on</strong>atal patient undergo<strong>in</strong>g<br />
phlebotomy, and to the success of the procedure. A helper is essential for properly immobiliz<strong>in</strong>g<br />
the patient for venepuncture or f<strong>in</strong>ger-prick, as described <strong>in</strong> Secti<strong>on</strong> 6.2.<br />
6.2 Practical guidance <strong>on</strong> paediatric and ne<strong>on</strong>atal blood<br />
sampl<strong>in</strong>g<br />
6.2.1 Patient identificati<strong>on</strong><br />
For paediatric and ne<strong>on</strong>atal patients, use the methods described below to ensure that patients<br />
are correctly identified before tak<strong>in</strong>g blood.<br />
• Use a wrist or foot band <strong>on</strong>ly if it is attached to the patient; DO NOT use the bed number or<br />
a wrist band that is attached to the bed or cot.<br />
• If a parent or legal guardian is present, ask that pers<strong>on</strong> for the child’s first and last names.<br />
• Check that the name, date of birth and hospital or file number are written <strong>on</strong> the laboratory<br />
form, and match them to the identity of the patient.<br />
6 Paediatric and ne<strong>on</strong>atal blood sampl<strong>in</strong>g 35
6.2.2 Venepuncture<br />
Preparati<strong>on</strong><br />
Venepuncture is the preferred method of blood sampl<strong>in</strong>g for term ne<strong>on</strong>ates, and causes less pa<strong>in</strong><br />
than heel-pricks (64).<br />
Equipment and supplies for paediatric patients.<br />
• Use a w<strong>in</strong>ged steel needle, preferably 23 or 23 gauge, with an extensi<strong>on</strong> tube (a butterfly):<br />
––<br />
avoid gauges of 25 or more because these may be associated with an <strong>in</strong>creased risk of<br />
haemolysis;<br />
––<br />
use a butterfly with either a syr<strong>in</strong>ge or an evacuated tube with an adaptor; a butterfly can<br />
provide easier access and movement, but movement of the attached syr<strong>in</strong>ge may make it<br />
difficult to draw blood.<br />
• Use a syr<strong>in</strong>ge with a barrel volume of 1–5 ml, depend<strong>in</strong>g <strong>on</strong> collecti<strong>on</strong> needs; the vacuum<br />
produced by draw<strong>in</strong>g us<strong>in</strong>g a larger syr<strong>in</strong>ge will often collapse the ve<strong>in</strong>.<br />
• When us<strong>in</strong>g an evacuated tube, choose <strong>on</strong>e that collects a small volume (1 ml or 5 ml) and<br />
has a low vacuum; this helps to avoid collapse of the ve<strong>in</strong> and may decrease haemolysis.<br />
• Where possible, use safety equipment with needle covers or features that m<strong>in</strong>imize blood<br />
exposure. Auto-disable (AD) syr<strong>in</strong>ges are designed for <strong>in</strong>jecti<strong>on</strong>, and are not appropriate for<br />
phlebotomy.<br />
Ask whether the parent would like to help by hold<strong>in</strong>g the child. If the parent wishes to help,<br />
provide full <strong>in</strong>structi<strong>on</strong>s <strong>on</strong> how and where to hold the child; if the parent prefers not to help,<br />
ask for assistance from another phlebotomist.<br />
Immobilize the child as described below.<br />
• Designate <strong>on</strong>e phlebotomist as the technician, and another phlebotomist or a parent to<br />
immobilize the child.<br />
• Ask the two adults to stand <strong>on</strong> opposite sides of an exam<strong>in</strong>ati<strong>on</strong> table.<br />
• Ask the immobilizer to:<br />
––<br />
stretch an arm across the table and place the child <strong>on</strong> its back, with its head <strong>on</strong> top of the<br />
outstretched arm;<br />
––<br />
pull the child close, as if the pers<strong>on</strong> were cradl<strong>in</strong>g the child;<br />
––<br />
grasp the child’s elbow <strong>in</strong> the outstretched hand;<br />
––<br />
use their other arm to reach across the child and grasp its wrist <strong>in</strong> a palm-up positi<strong>on</strong><br />
(reach<strong>in</strong>g across the child anchors the child’s shoulder, and thus prevents twist<strong>in</strong>g or<br />
rock<strong>in</strong>g movements; also, a firm grasp <strong>on</strong> the wrist effectively provides the phlebotomist<br />
with a “tourniquet”).<br />
If necessary, take the follow<strong>in</strong>g steps to improve the ease of venepuncture.<br />
• Ask the parent to rhythmically tighten and release the child’s wrist, to ensure that there is<br />
an adequate flow of blood.<br />
• Keep the child warm, which may <strong>in</strong>crease the rate of blood flow by as much as sevenfold<br />
(65), by remov<strong>in</strong>g as few of the child’s clothes as possible and, <strong>in</strong> the case of an <strong>in</strong>fant, by:<br />
––<br />
swaddl<strong>in</strong>g <strong>in</strong> a blanket; and<br />
––<br />
hav<strong>in</strong>g the parent or caregiver hold the <strong>in</strong>fant, leav<strong>in</strong>g <strong>on</strong>ly the extremity of the site of<br />
venepuncture exposed.<br />
• Warm the area of puncture with warm cloths to help dilate the blood vessels.<br />
• Use a transillum<strong>in</strong>ator or pocket pen light to display the dorsal hand ve<strong>in</strong>s and the ve<strong>in</strong>s of<br />
the antecubital fossa.<br />
36 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
<strong>Draw<strong>in</strong>g</strong> blood<br />
• Follow the procedures given <strong>in</strong> Secti<strong>on</strong> 2.2.3 for:<br />
––<br />
hand hygiene;<br />
––<br />
advance preparati<strong>on</strong>;<br />
––<br />
patient identificati<strong>on</strong> and positi<strong>on</strong><strong>in</strong>g;<br />
––<br />
sk<strong>in</strong> antisepsis (but DO NOT use chlorhexid<strong>in</strong>e <strong>on</strong> children under 2 m<strong>on</strong>ths of age).<br />
• Once the <strong>in</strong>fant or child is immobilized, puncture the sk<strong>in</strong> 3–5 mm distal to (i.e. away from)<br />
the ve<strong>in</strong> (66); this allows good access without push<strong>in</strong>g the ve<strong>in</strong> away.<br />
• If the needle enters al<strong>on</strong>gside the ve<strong>in</strong> rather than <strong>in</strong>to it, withdraw the needle slightly<br />
without remov<strong>in</strong>g it completely, and angle it <strong>in</strong>to the vessel.<br />
• Draw blood slowly and steadily.<br />
6.2.3 F<strong>in</strong>ger and heel-prick<br />
See Secti<strong>on</strong> 7.2, which describes the steps for both f<strong>in</strong>ger and heel-pricks, for paediatric and<br />
ne<strong>on</strong>atal patients, and for adults.<br />
Select the proper lancet length for the area of puncture, as described <strong>in</strong> Secti<strong>on</strong> 7.2.<br />
6.3 Illustrati<strong>on</strong>s for paediatric and ne<strong>on</strong>atal blood sampl<strong>in</strong>g<br />
Figure 6.1 Paediatric and ne<strong>on</strong>atal venepuncture<br />
1. Use a w<strong>in</strong>ged steel needle,<br />
usually 23 or 25 gauge, with<br />
an extensi<strong>on</strong> tube (butterfly).<br />
Keep the tube and needle<br />
separate until the needle is <strong>in</strong><br />
the ve<strong>in</strong>.<br />
2. Collect supplies and equipment. 3. Perform hand hygiene (if<br />
us<strong>in</strong>g soap and water, dry<br />
hands with s<strong>in</strong>gle-use towels).<br />
6 Paediatric and ne<strong>on</strong>atal blood sampl<strong>in</strong>g 37
4. Immobilize the baby or child. 5. Put the tourniquet <strong>on</strong> the<br />
patient about two f<strong>in</strong>ger widths<br />
above the venepuncture site.<br />
6. Put <strong>on</strong> well-fitt<strong>in</strong>g, n<strong>on</strong>-sterile<br />
gloves.<br />
7. Attach the end of the w<strong>in</strong>ged<br />
<strong>in</strong>fusi<strong>on</strong> set to the end of the<br />
vacuum tube and <strong>in</strong>sert the<br />
collecti<strong>on</strong> tube <strong>in</strong>to the holder<br />
until the tube reaches the<br />
needle.<br />
8. Remove the plastic sleeve<br />
from the end of the butterfly.<br />
9. Dis<strong>in</strong>fect the collecti<strong>on</strong> site<br />
and allow to dry.<br />
10. Use a thumb to draw the sk<strong>in</strong><br />
tight, about two f<strong>in</strong>ger widths<br />
below the venepuncture site.<br />
11. Push the vacuum tube<br />
completely <strong>on</strong>to the needle.<br />
12. <strong>Blood</strong> should beg<strong>in</strong> to flow <strong>in</strong>to<br />
the tube.<br />
13. Fill the tube until it is full or until<br />
the vacuum is exhausted; if<br />
fill<strong>in</strong>g multiple tubes, carefully<br />
remove the full tube and replace<br />
with another tube, tak<strong>in</strong>g care<br />
not to move the needle <strong>in</strong> the<br />
ve<strong>in</strong>.<br />
14. After the required amount<br />
of blood has been collected,<br />
release the tourniquet.<br />
38 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
15. Place dry gauze over the<br />
venepuncture site and slowly<br />
withdraw the needle.<br />
16. Ask the parent to c<strong>on</strong>t<strong>in</strong>ue<br />
apply<strong>in</strong>g mild pressure.<br />
17. Remove the butterfly from the<br />
vacuum tube holder.<br />
18. Dispose of the butterfly <strong>in</strong> a<br />
sharps c<strong>on</strong>ta<strong>in</strong>er.<br />
19. Properly dispose of all<br />
c<strong>on</strong>tam<strong>in</strong>ated supplies.<br />
20. Label the tube with the patient<br />
identificati<strong>on</strong> number and date.<br />
21. Put an adhesive bandage <strong>on</strong><br />
the patient if necessary.<br />
22. Remove gloves, dispose<br />
of them appropriately and<br />
perform hand hygiene (if us<strong>in</strong>g<br />
soap and water, dry hands<br />
with s<strong>in</strong>gle-use towels).<br />
6 Paediatric and ne<strong>on</strong>atal blood sampl<strong>in</strong>g 39
7 Capillary sampl<strong>in</strong>g<br />
The <strong>in</strong>formati<strong>on</strong> given here supplements that given <strong>in</strong> Chapter 2. Users of these guidel<strong>in</strong>es<br />
should read Chapter 2 before read<strong>in</strong>g the <strong>in</strong>formati<strong>on</strong> given below. This chapter covers<br />
background <strong>in</strong>formati<strong>on</strong> (Secti<strong>on</strong> 7.1), practical guidance (Secti<strong>on</strong> 7.2) and illustrati<strong>on</strong>s<br />
(Secti<strong>on</strong> 7.3) relevant to capillary sampl<strong>in</strong>g.<br />
Capillary sampl<strong>in</strong>g from a f<strong>in</strong>ger, heel or (rarely) an ear lobe may be performed <strong>on</strong> patients of<br />
any age, for specific tests that require small quantities of blood. However, because the procedure<br />
is comm<strong>on</strong>ly used <strong>in</strong> paediatric patients, Secti<strong>on</strong>s 7.1.1 and 7.1.2 focus particularly <strong>on</strong> paediatric<br />
capillary sampl<strong>in</strong>g.<br />
7.1 Background <strong>in</strong>formati<strong>on</strong> <strong>on</strong> capillary sampl<strong>in</strong>g<br />
7.1.1 Choice of site<br />
Adult patients<br />
The f<strong>in</strong>ger is usually the preferred site for capillary test<strong>in</strong>g <strong>in</strong> an adult patient. The sides of the<br />
heel are <strong>on</strong>ly used <strong>in</strong> paediatric and ne<strong>on</strong>atal patients. Ear lobes are sometimes used <strong>in</strong> mass<br />
screen<strong>in</strong>g or research studies.<br />
Paediatric and ne<strong>on</strong>atal patients<br />
Selecti<strong>on</strong> of a site for capillary sampl<strong>in</strong>g <strong>in</strong> a paediatric patient is usually based <strong>on</strong> the age<br />
and weight of the patient. If the child is walk<strong>in</strong>g, the child’s feet may have calluses that h<strong>in</strong>der<br />
adequate blood flow. Table 7.1 shows the c<strong>on</strong>diti<strong>on</strong>s <strong>in</strong>fluenc<strong>in</strong>g the choice of heel or f<strong>in</strong>ger-prick.<br />
Table 7.1<br />
C<strong>on</strong>diti<strong>on</strong>s <strong>in</strong>fluenc<strong>in</strong>g the choice of heel or f<strong>in</strong>ger-prick<br />
C<strong>on</strong>diti<strong>on</strong> Heel-prick F<strong>in</strong>ger-prick<br />
Age Birth to about 6 m<strong>on</strong>ths Over 6 m<strong>on</strong>ths<br />
Weight From 3–10 kg, approximately Greater than 10 kg<br />
Placement of lancet<br />
On the medial or lateral plantar<br />
surface<br />
On the side of the ball of the f<strong>in</strong>ger<br />
perpendicular to the l<strong>in</strong>es of the<br />
f<strong>in</strong>gerpr<strong>in</strong>t<br />
Recommended f<strong>in</strong>ger Not applicable Sec<strong>on</strong>d and third f<strong>in</strong>ger (i.e. middle<br />
and r<strong>in</strong>g f<strong>in</strong>ger); avoid the thumb<br />
and <strong>in</strong>dex f<strong>in</strong>ger because of calluses,<br />
and avoid the little f<strong>in</strong>ger because the<br />
tissue is th<strong>in</strong><br />
Specimens requir<strong>in</strong>g a sk<strong>in</strong> puncture are best obta<strong>in</strong>ed after ensur<strong>in</strong>g that a baby is warm, as<br />
discussed <strong>in</strong> Secti<strong>on</strong> 6.2.2.<br />
7 Capillary sampl<strong>in</strong>g 41
7.1.2 Select<strong>in</strong>g the length of lancet<br />
Adult patients<br />
A lancet slightly shorter than the estimated depth needed should be used because the pressure<br />
compresses the sk<strong>in</strong>; thus, the puncture depth will be slightly deeper than the lancet length. In<br />
<strong>on</strong>e study of 52 subjects, pa<strong>in</strong> <strong>in</strong>creased with penetrati<strong>on</strong> depth, and thicker lancets were slightly<br />
more pa<strong>in</strong>ful than th<strong>in</strong> <strong>on</strong>es (67). However, blood volumes <strong>in</strong>creased with the lancet penetrati<strong>on</strong><br />
and depth.<br />
Lengths vary by manufacturer (from 0.85 mm for ne<strong>on</strong>ates up to 2.2 mm). In a f<strong>in</strong>ger-prick, the<br />
depth should not go bey<strong>on</strong>d 2.4 mm, so a 2.2 mm lancet is the l<strong>on</strong>gest length typically used.<br />
Paediatric and ne<strong>on</strong>atal patients<br />
In heel-pricks, the depth should not go bey<strong>on</strong>d 2.4 mm. For premature ne<strong>on</strong>ates, a 0.85 mm<br />
lancet is available.<br />
The distance for a 7 pound (3 kg) baby from outer sk<strong>in</strong> surface to b<strong>on</strong>e is:<br />
• medial and lateral heel – 3.32 mm;<br />
• posterior heel – 2.33 mm (this site should be avoided, to reduce the risk of hitt<strong>in</strong>g b<strong>on</strong>e);<br />
• toe – 2.19 mm.<br />
The recommended depth for a f<strong>in</strong>ger-prick is:<br />
• for a child over 6 m<strong>on</strong>ths and below 8 years – 1.5 mm;<br />
• for a child over 8 years – 2.4 mm.<br />
Too much compressi<strong>on</strong> should be avoided, because this may cause a deeper puncture than is<br />
needed to get good flow.<br />
7.1.3 Order of draw<br />
With sk<strong>in</strong> punctures, the haematology specimen is collected first, followed by the chemistry<br />
and blood bank specimens. This order of draw<strong>in</strong>g is essential to m<strong>in</strong>imize the effects of platelet<br />
clump<strong>in</strong>g. The order used for sk<strong>in</strong> punctures is the reverse of that used for venepuncture<br />
collecti<strong>on</strong>. If more than two specimens are needed, venepuncture may provide more accurate<br />
laboratory results.<br />
7.1.4 Complicati<strong>on</strong>s<br />
Complicati<strong>on</strong>s that can arise <strong>in</strong> capillary sampl<strong>in</strong>g <strong>in</strong>clude:<br />
• collapse of ve<strong>in</strong>s if the tibial artery is lacerated from punctur<strong>in</strong>g the medial aspect of the<br />
heel;<br />
• osteomyelitis of the heel b<strong>on</strong>e (calcaneus) (68);<br />
• nerve damage if the f<strong>in</strong>gers of ne<strong>on</strong>ates are punctured (69);<br />
• haematoma and loss of access to the venous branch used;<br />
• scarr<strong>in</strong>g;<br />
• localized or generalized necrosis (a l<strong>on</strong>g-term effect);<br />
• sk<strong>in</strong> breakdown from repeated use of adhesive strips (particularly <strong>in</strong> very young or very<br />
elderly patients) – this can be avoided if sufficient pressure is applied and the puncture site<br />
is observed after the procedure.<br />
42 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
7.2 Practical guidance <strong>on</strong> capillary sampl<strong>in</strong>g<br />
7.2.1 Selecti<strong>on</strong> of site and lancet<br />
• Us<strong>in</strong>g the guidance given <strong>in</strong> Secti<strong>on</strong> 7.1, decide whether to use a f<strong>in</strong>ger or heel-prick, and<br />
decide <strong>on</strong> an appropriate size of lancet.<br />
• DO NOT use a surgical blade to perform a sk<strong>in</strong> puncture.<br />
• DO NOT puncture the sk<strong>in</strong> more than <strong>on</strong>ce with the same lancet, or use a s<strong>in</strong>gle puncture<br />
site more than <strong>on</strong>ce, because this can lead to bacterial c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> and <strong>in</strong>fecti<strong>on</strong>.<br />
7.2.2 Procedure for capillary sampl<strong>in</strong>g<br />
Adult patients<br />
Prepare the sk<strong>in</strong><br />
• Apply alcohol to the entry site and allow to air dry (see Secti<strong>on</strong> 2.2.3).<br />
• Puncture the sk<strong>in</strong> with <strong>on</strong>e quick, c<strong>on</strong>t<strong>in</strong>uous and deliberate stroke, to achieve a good flow<br />
of blood and to prevent the need to repeat the puncture.<br />
• Wipe away the first drop of blood because it may be c<strong>on</strong>tam<strong>in</strong>ated with tissue fluid or debris<br />
(slough<strong>in</strong>g sk<strong>in</strong>).<br />
• Avoid squeez<strong>in</strong>g the f<strong>in</strong>ger or heel too tightly because this dilutes the specimen with tissue<br />
fluid (plasma) and <strong>in</strong>creases the probability of haemolysis (60).<br />
• When the blood collecti<strong>on</strong> procedure is complete, apply firm pressure to the site to stop the<br />
bleed<strong>in</strong>g.<br />
Take laboratory samples <strong>in</strong> the correct order to m<strong>in</strong>imize err<strong>on</strong>eous test results<br />
• With sk<strong>in</strong> punctures, collect the specimens <strong>in</strong> the order below, start<strong>in</strong>g with haematology<br />
specimens:<br />
––<br />
haematology specimens;<br />
––<br />
chemistry specimens;<br />
––<br />
blood bank specimens.<br />
Paediatric and ne<strong>on</strong>atal patients<br />
Immobilize the child<br />
• First immobilize the child by ask<strong>in</strong>g the parent to:<br />
Prepare the sk<strong>in</strong><br />
––<br />
sit <strong>on</strong> the phlebotomy chair with the child <strong>on</strong> the parent’s lap;<br />
––<br />
immobilize the child’s lower extremities by positi<strong>on</strong><strong>in</strong>g their legs around the child’s <strong>in</strong> a<br />
cross-leg pattern;<br />
––<br />
extend an arm across the child’s chest, and secure the child’s free arm by firmly tuck<strong>in</strong>g<br />
it under their own;<br />
––<br />
grasp the child’s elbow (i.e. the sk<strong>in</strong> puncture arm), and hold it securely;<br />
––<br />
use his or her other arm to firmly grasp the child’s wrist, hold<strong>in</strong>g it palm down.<br />
• Prepare the sk<strong>in</strong> as described above for adult patients.<br />
• DO NOT use povid<strong>on</strong>e iod<strong>in</strong>e for a capillary sk<strong>in</strong> puncture <strong>in</strong> paediatric and ne<strong>on</strong>atal<br />
patients; <strong>in</strong>stead, use alcohol, as stated <strong>in</strong> the <strong>in</strong>structi<strong>on</strong>s for adults.<br />
7 Capillary sampl<strong>in</strong>g 43
Puncture the sk<strong>in</strong><br />
• Puncture the sk<strong>in</strong> as described above for adult patients.<br />
• If necessary, take the follow<strong>in</strong>g steps to improve the ease of obta<strong>in</strong><strong>in</strong>g blood by f<strong>in</strong>ger-prick<br />
<strong>in</strong> paediatric and ne<strong>on</strong>atal patients:<br />
––<br />
ask the parent to rhythmically tighten and release the child’s wrist, to ensure that there<br />
is sufficient flow of blood;<br />
––<br />
keep the child warm by remov<strong>in</strong>g as few clothes as possible, swaddl<strong>in</strong>g an <strong>in</strong>fant <strong>in</strong> a<br />
blanket, and hav<strong>in</strong>g a mother or caregiver hold an <strong>in</strong>fant, leav<strong>in</strong>g <strong>on</strong>ly the extremity of<br />
the site of capillary sampl<strong>in</strong>g exposed.<br />
• Avoid excessive massag<strong>in</strong>g or squeez<strong>in</strong>g of f<strong>in</strong>gers because this will cause haemolysis and<br />
impede blood flow (60).<br />
Take laboratory samples <strong>in</strong> the order that prevent cross-c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of sample tube additives<br />
• As described above for adult patients, collect the capillary haematology specimen first,<br />
followed by the chemistry and blood bank specimens.<br />
• Clean up blood spills.<br />
• Collect all equipment used <strong>in</strong> the procedure, be<strong>in</strong>g careful to remove all items from the<br />
patient’s bed or cot; to avoid accidents, DO NOT leave anyth<strong>in</strong>g beh<strong>in</strong>d.<br />
Give follow-up care<br />
There are two separate steps to patient follow-up care – data entry (i.e. completi<strong>on</strong> of<br />
requisiti<strong>on</strong>s), and provisi<strong>on</strong> of comfort and reassurance.<br />
Data entry or completi<strong>on</strong> of requisiti<strong>on</strong>s<br />
• Record relevant <strong>in</strong>formati<strong>on</strong> about the blood collecti<strong>on</strong> <strong>on</strong> the requisiti<strong>on</strong> and specimen<br />
label; such <strong>in</strong>formati<strong>on</strong> may <strong>in</strong>clude:<br />
––<br />
date of collecti<strong>on</strong>;<br />
––<br />
patient name;<br />
––<br />
patient identity number;<br />
––<br />
unit locati<strong>on</strong> (nursery or hospital room number);<br />
––<br />
test or tests requested;<br />
––<br />
amount of blood collected (number of tubes);<br />
––<br />
method of collecti<strong>on</strong> (venepuncture or sk<strong>in</strong> puncture);<br />
––<br />
phlebotomist’s <strong>in</strong>itials.<br />
Comfort and reassurance<br />
Show the child that you care either verbally or physically. A simple gesture is all it takes to leave<br />
the child <strong>on</strong> a positive note; for example, give verbal praise, a handshake, a fun sticker or a<br />
simple pat <strong>on</strong> the back.<br />
A small amount of sucrose (0.012–0.12 g) is safe and effective as an analgesic for newborns<br />
undergo<strong>in</strong>g venepuncture or capillary heel-pricks (70).<br />
Unsuccessful attempts <strong>in</strong> paediatric patients<br />
Adhere strictly to a limit <strong>on</strong> the number of times a paediatric patient may be stuck. If no<br />
satisfactory sample has been collected after two attempts, seek a sec<strong>on</strong>d op<strong>in</strong>i<strong>on</strong> to decide<br />
whether to make a further attempt, or cancel the tests.<br />
44 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
7.3 Illustrati<strong>on</strong>s for capillary sampl<strong>in</strong>g<br />
Figure 7.1 Capillary sampl<strong>in</strong>g<br />
1. Lancet and collecti<strong>on</strong> tube. 2. Assemble equipment and<br />
supplies.<br />
3. Perform hand hygiene (if us<strong>in</strong>g<br />
soap and water, dry hands<br />
with s<strong>in</strong>gle-use towels).<br />
4. Put <strong>on</strong> well-fitt<strong>in</strong>g, n<strong>on</strong>-sterile<br />
gloves.<br />
5. Select the site. Apply 70%<br />
isopropyl alcohol and allow to<br />
air dry.<br />
6. Puncture the sk<strong>in</strong>.<br />
7. Wipe away the first drop of<br />
blood.<br />
8. Avoid squeez<strong>in</strong>g the f<strong>in</strong>ger too<br />
tightly.<br />
9. Dispose of all sharps<br />
appropriately.<br />
10. Dispose of waste materials<br />
appropriately.<br />
11. Remove gloves and place <strong>in</strong> general waste.<br />
Perform hand hygiene (if us<strong>in</strong>g soap and<br />
water, dry hands with s<strong>in</strong>gle-use towels).<br />
7 Capillary sampl<strong>in</strong>g 45
PART III IMPLEMENTATION,<br />
EVALUATION AND<br />
MONITORING
8 Implement<strong>in</strong>g best phlebotomy practices<br />
8.1 Sett<strong>in</strong>g policies and standard operat<strong>in</strong>g procedures<br />
As expla<strong>in</strong>ed <strong>in</strong> Chapter 1, these best practice guidel<strong>in</strong>es for phlebotomy extend the scope of the<br />
two <str<strong>on</strong>g>WHO</str<strong>on</strong>g>/SIGN documents <strong>on</strong> related topics that are currently available (29, 30). At the heart<br />
of the document are three pr<strong>in</strong>ciples.<br />
• Standards of safe practice globally should be governed by evidence-based pr<strong>in</strong>ciples.<br />
• Each phlebotomy service should, with<strong>in</strong> its capacity, ultimately strive to achieve best<br />
practices.<br />
• Health workers should be protected and allowed to work <strong>in</strong> a safe envir<strong>on</strong>ment, armed with<br />
knowledge that reduces harm to themselves, patients and the community.<br />
This chapter provides recommendati<strong>on</strong>s (<strong>in</strong> boxes) and gives further <strong>in</strong>formati<strong>on</strong> for each<br />
recommendati<strong>on</strong> (text below the boxes).<br />
8.2 Procurement<br />
Recommendati<strong>on</strong> <strong>on</strong> procurement (<strong>in</strong> c<strong>on</strong>juncti<strong>on</strong> with the <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guid<strong>in</strong>g<br />
pr<strong>in</strong>ciple for <strong>in</strong>jecti<strong>on</strong> device security (71)<br />
Procurement agencies must ensure that all health-care facilities have<br />
sufficient supplies of phlebotomy and pers<strong>on</strong>al protective equipment. Such<br />
equipment must meet at least the m<strong>in</strong>imum standards of sterility, quality and<br />
safety to prevent complicati<strong>on</strong>s related to unsafe practices.<br />
To prevent the complicati<strong>on</strong>s related to unsafe practices discussed <strong>in</strong> Parts I and II of this<br />
document, equipment (<strong>in</strong>clud<strong>in</strong>g materials for hand hygiene) and pers<strong>on</strong>al protective cloth<strong>in</strong>g<br />
must be rout<strong>in</strong>ely available <strong>in</strong> sufficient quantities. Items needed <strong>in</strong>clude:<br />
• pers<strong>on</strong>al protective equipment;<br />
• safe blood-sampl<strong>in</strong>g equipment of high quality, based <strong>on</strong> a cost–effectiveness analysis of<br />
the country’s needs and f<strong>in</strong>ances;<br />
• antiseptics.<br />
All items to be used <strong>on</strong> more than <strong>on</strong>e patient should be designed so that they can be cleaned<br />
and dis<strong>in</strong>fected. Such items <strong>in</strong>clude laboratory transport boxes or trays, tourniquets, evacuated<br />
tube holders, scissors and so <strong>on</strong>. Also, it is best to buy high-quality items even if they are more<br />
expensive. Try<strong>in</strong>g to save m<strong>on</strong>ey by purchas<strong>in</strong>g cheap items that are of poor quality can be more<br />
costly <strong>in</strong> the l<strong>on</strong>g run; for example, if items have to be replaced more frequently.<br />
Governments and procurement agencies should work to ensure that appropriate products are<br />
available <strong>in</strong> the country, by:<br />
• provid<strong>in</strong>g detailed technical specificati<strong>on</strong>s to companies wish<strong>in</strong>g to enter the market – such<br />
specificati<strong>on</strong>s should <strong>in</strong>clude detailed m<strong>in</strong>imum standards acceptable for safety, quality and<br />
usability;<br />
• work<strong>in</strong>g with manufactures to communicate def<strong>in</strong>ed needs to improve products;<br />
• work<strong>in</strong>g with nati<strong>on</strong>al or <strong>in</strong>ternati<strong>on</strong>al regulatory authorities to test products before<br />
importati<strong>on</strong>, to ensure they meet their stated claims and are more effective than cheaper<br />
products available <strong>on</strong> the market;<br />
8 Implement<strong>in</strong>g best phlebotomy practices 49
• work<strong>in</strong>g together to ensure fair, transparent competiti<strong>on</strong> and <strong>in</strong>put of end users dur<strong>in</strong>g<br />
product selecti<strong>on</strong>;<br />
• c<strong>on</strong>duct<strong>in</strong>g post-market<strong>in</strong>g surveillance to track defects and adverse events associated with<br />
products.<br />
Facilities that cannot afford the supplies needed to m<strong>in</strong>imize risk to staff and patients, or<br />
supplies of the quality necessary for valid and reliable laboratory test results, should reassess<br />
whether they should offer phlebotomy or the related laboratory services.<br />
8.2.1 <strong>Blood</strong>-sampl<strong>in</strong>g equipment<br />
Recommendati<strong>on</strong> <strong>on</strong> blood-sampl<strong>in</strong>g equipment (Annex C)<br />
Safety-eng<strong>in</strong>eered evacuated tube systems or w<strong>in</strong>ged needle sets are<br />
safer than a hypodermic needle and syr<strong>in</strong>ge, but all are effective for blood<br />
sampl<strong>in</strong>g. Safety features (e.g. needle covers, needleless transfer systems<br />
or adaptors, and retractable lancets) can further reduce the risks associated<br />
with manual recapp<strong>in</strong>g, needle removal, disassembly and transfer of blood<br />
from syr<strong>in</strong>ges to tubes.<br />
• A needle and syr<strong>in</strong>ge is the most comm<strong>on</strong> tool for withdraw<strong>in</strong>g large quantities of blood.<br />
• A sterile s<strong>in</strong>gle-use needle and syr<strong>in</strong>ge should be used for each patient, and should be<br />
placed, as a s<strong>in</strong>gle unit, <strong>in</strong>to a sharps c<strong>on</strong>ta<strong>in</strong>er immediately after use.<br />
• Safety-eng<strong>in</strong>eered equipment offers better protecti<strong>on</strong> to the health worker, but should be<br />
appropriate for the specific task. Some devices designed to prevent reuse (e.g. auto-disable<br />
syr<strong>in</strong>ges) are not appropriate for phlebotomy. Safety devices are more expensive, so if<br />
resources are limited, their use may need to be restricted to procedures associated with the<br />
greatest rates or risk of sharps <strong>in</strong>jury.<br />
• Capillary punctures should be performed us<strong>in</strong>g a sterile device – preferably with safety<br />
features that automatically retract the lancet – to help prevent both reuse and sharps<br />
<strong>in</strong>juries.<br />
8.2.2 Protecti<strong>on</strong><br />
Recommendati<strong>on</strong> <strong>on</strong> pers<strong>on</strong>al protecti<strong>on</strong><br />
Health workers should wear well-fitt<strong>in</strong>g, n<strong>on</strong>-sterile gloves when tak<strong>in</strong>g<br />
blood; they should also carry out hand hygiene before and after each patient<br />
procedure, before putt<strong>in</strong>g <strong>on</strong> and after remov<strong>in</strong>g gloves.<br />
Clean, n<strong>on</strong>-sterile exam<strong>in</strong>ati<strong>on</strong> gloves <strong>in</strong> multiple sizes should be available for pers<strong>on</strong>nel who<br />
carry out phlebotomy. It is recommended that:<br />
• well-fitt<strong>in</strong>g gloves are worn for each procedure, irrespective of the site of blood sampl<strong>in</strong>g or<br />
the status of the patient; these gloves can be latex or latex-free, and should be n<strong>on</strong>-sterile<br />
(i.e. exam<strong>in</strong>ati<strong>on</strong> gloves);<br />
• the gloves are changed between patients;<br />
• masks, visors and eye protecti<strong>on</strong> may also be needed if additi<strong>on</strong>al blood exposure is<br />
anticipated; for example, dur<strong>in</strong>g arterial blood sampl<strong>in</strong>g.<br />
50 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
8.3 <strong>Phlebotomy</strong> tra<strong>in</strong><strong>in</strong>g<br />
Recommendati<strong>on</strong> <strong>on</strong> phlebotomy tra<strong>in</strong><strong>in</strong>g (Annex E)<br />
All health workers undertak<strong>in</strong>g phlebotomy must be tra<strong>in</strong>ed <strong>in</strong> <strong>in</strong>fecti<strong>on</strong><br />
preventi<strong>on</strong> and c<strong>on</strong>trol procedures. Staff should receive tra<strong>in</strong><strong>in</strong>g and<br />
dem<strong>on</strong>strate proficiency <strong>on</strong> the specific methods that they will use <strong>on</strong> the<br />
job; for example, adult and paediatric sampl<strong>in</strong>g; and venous, arterial and<br />
capillary blood sampl<strong>in</strong>g.<br />
• Regular <strong>in</strong>-service tra<strong>in</strong><strong>in</strong>g and supportive supervisi<strong>on</strong> should be provided.<br />
• The tra<strong>in</strong><strong>in</strong>g programme should provide theoretical and practical knowledge <strong>in</strong> blood<br />
sampl<strong>in</strong>g and blood draw<strong>in</strong>g (31).<br />
• A certificate of competence should be issued up<strong>on</strong> successful dem<strong>on</strong>strati<strong>on</strong> of phlebotomy<br />
after completi<strong>on</strong> of the tra<strong>in</strong><strong>in</strong>g programme.<br />
8.4 Safe waste and sharps disposal<br />
Recommendati<strong>on</strong> <strong>on</strong> safe disposal of sharps (72)<br />
The blood-sampl<strong>in</strong>g device – a needle and syr<strong>in</strong>ge, evacuated needle and<br />
tube holder, or w<strong>in</strong>ged butterfly – should be disposed of immediately after<br />
use as a s<strong>in</strong>gle unit. It should be placed <strong>in</strong> a puncture-proof, leak-proof,<br />
closable sharps c<strong>on</strong>ta<strong>in</strong>er that is clearly visible and is placed with<strong>in</strong> arm’s<br />
reach of the health worker.<br />
• The safe disposal of sharps is <strong>on</strong>e of the major challenges, particularly <strong>in</strong> poorly resourced<br />
countries.<br />
• Shortage of sharps c<strong>on</strong>ta<strong>in</strong>ers can result <strong>in</strong> <strong>in</strong>creases <strong>in</strong> needle-stick <strong>in</strong>juries due to:<br />
––<br />
needle recapp<strong>in</strong>g;<br />
––<br />
decant<strong>in</strong>g of used sharps c<strong>on</strong>ta<strong>in</strong>ers;<br />
––<br />
recycl<strong>in</strong>g of c<strong>on</strong>ta<strong>in</strong>ers;<br />
––<br />
overfill<strong>in</strong>g of sharps c<strong>on</strong>ta<strong>in</strong>ers.<br />
• Another issue is that staff may separate a needle and syr<strong>in</strong>ge as a cost-sav<strong>in</strong>g exercise and<br />
discard the two parts <strong>in</strong> different waste systems.<br />
• The immediate discard of used sharps <strong>in</strong>to a puncture-resistant sharps c<strong>on</strong>ta<strong>in</strong>er that can<br />
be closed is an essential part of manag<strong>in</strong>g waste without needle-stick <strong>in</strong>juries (73).<br />
8 Implement<strong>in</strong>g best phlebotomy practices 51
8.5 Preventi<strong>on</strong> and management of <strong>in</strong>cidents and adverse<br />
events<br />
Recommendati<strong>on</strong> <strong>on</strong> <strong>in</strong>fecti<strong>on</strong> c<strong>on</strong>trol (Annex B)<br />
Infecti<strong>on</strong> c<strong>on</strong>trol procedures that help to prevent health-care associated<br />
<strong>in</strong>fecti<strong>on</strong>s <strong>in</strong>clude:<br />
• hand hygiene;<br />
• glove use;<br />
• sk<strong>in</strong> antisepsis;<br />
• sterile, s<strong>in</strong>gle-use blood-sampl<strong>in</strong>g devices;<br />
• sharps c<strong>on</strong>ta<strong>in</strong>ers;<br />
• dis<strong>in</strong>fecti<strong>on</strong> of surfaces and chairs;<br />
• clean<strong>in</strong>g and dis<strong>in</strong>fecti<strong>on</strong> of tourniquets;<br />
• transportati<strong>on</strong> of laboratory samples <strong>in</strong> labelled, washable c<strong>on</strong>ta<strong>in</strong>ers.<br />
Annex B summarizes the recommendati<strong>on</strong>s for best <strong>in</strong>fecti<strong>on</strong> c<strong>on</strong>trol practices <strong>in</strong> phlebotomy.<br />
The po<strong>in</strong>ts listed below c<strong>on</strong>tribute to <strong>in</strong>fecti<strong>on</strong> c<strong>on</strong>trol.<br />
• The workplace should be clean, tidy and uncluttered. There should be no sign of blood<br />
c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> <strong>on</strong> the chairs, counters or walls. The work<strong>in</strong>g surface should be visibly clean.<br />
• Hand hygiene (hand wash<strong>in</strong>g or use of an alcohol rub) should be carried out before wellfitt<strong>in</strong>g,<br />
n<strong>on</strong>-sterile gloves are put <strong>on</strong> and after they are removed (45).<br />
• Only sterile, s<strong>in</strong>gle-use blood-sampl<strong>in</strong>g devices should be used to take blood.<br />
• Sk<strong>in</strong> at the venepuncture site should be dis<strong>in</strong>fected, tak<strong>in</strong>g <strong>in</strong>to c<strong>on</strong>siderati<strong>on</strong> the type of<br />
specimen, the age and the allergy history of the patient (40–42).<br />
• Once the procedure has been completed and the blood sample or samples have been put<br />
<strong>in</strong>to the laboratory sampl<strong>in</strong>g tubes, the used devices should be discarded immediately <strong>in</strong>to a<br />
sharps c<strong>on</strong>ta<strong>in</strong>er.<br />
• Specimens should be transported <strong>in</strong> c<strong>on</strong>ta<strong>in</strong>ers that help to prevent breakage or spillage of<br />
blood.<br />
8.5.1 Patient related<br />
Recommendati<strong>on</strong> <strong>on</strong> <strong>in</strong>creas<strong>in</strong>g patient c<strong>on</strong>fidence (Annex F)<br />
Health-care facilities should provide a patient <strong>in</strong>formati<strong>on</strong> leaflet or poster<br />
expla<strong>in</strong><strong>in</strong>g the procedure <strong>in</strong> simple terms, to <strong>in</strong>crease patient c<strong>on</strong>fidence.<br />
• Patient <strong>in</strong>formati<strong>on</strong> (leaflets or posters) is recommended. In a busy cl<strong>in</strong>ic, there may not be<br />
time to expla<strong>in</strong> the procedure to the patient, or the reas<strong>on</strong> for the blood sample be<strong>in</strong>g taken.<br />
• Informati<strong>on</strong> should be provided to a fully c<strong>on</strong>scious patient <strong>in</strong> such a way that the pers<strong>on</strong><br />
can make an <strong>in</strong>formed decisi<strong>on</strong>. Be<strong>in</strong>g well <strong>in</strong>formed also helps the patient to relax and may<br />
reduce discomfort dur<strong>in</strong>g the procedure.<br />
• If the patient is mentally <strong>in</strong>capacitated (e.g. through mental illness, organic impairment,<br />
or traumatic or drug-associated loss of c<strong>on</strong>sciousness), essential blood sampl<strong>in</strong>g may be<br />
carried out without permissi<strong>on</strong>, <strong>in</strong> accordance with the <strong>in</strong>stituti<strong>on</strong>al or nati<strong>on</strong>al policy.<br />
However, the status of the patient should be clearly documented <strong>in</strong> the patient’s cl<strong>in</strong>ical<br />
notes.<br />
52 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
• If the patient is unc<strong>on</strong>scious or unable to give <strong>in</strong>formed c<strong>on</strong>sent, the next of k<strong>in</strong> or legal<br />
guardian (which can be a court of law) can give permissi<strong>on</strong> for a blood sample to be taken.<br />
• When carry<strong>in</strong>g out blood sampl<strong>in</strong>g <strong>on</strong> a m<strong>in</strong>or, verbal or written permissi<strong>on</strong> from the<br />
parent or legal guardian, or a court of law may be necessary for medicolegal reas<strong>on</strong>s.<br />
8.5.2 Health-worker related<br />
Recommendati<strong>on</strong> <strong>on</strong> health worker and patient safety policies<br />
A post-exposure prophylaxis protocol must be available <strong>in</strong> all health-care<br />
facilities and phlebotomy areas, provid<strong>in</strong>g clear <strong>in</strong>structi<strong>on</strong>s to follow <strong>in</strong> case<br />
of accidental exposure to blood or body fluids.<br />
• Should an exposure occur, health workers should be aware of the policy <strong>on</strong> PEP. Ideally,<br />
this policy should offer support for exposure to HIV, HBV and HCV (27).<br />
• Worksites should have clear notices giv<strong>in</strong>g the po<strong>in</strong>t of c<strong>on</strong>tact (both dur<strong>in</strong>g the day and at<br />
night) where staff may receive assistance, support and care, <strong>in</strong>clud<strong>in</strong>g PEP and the benefits<br />
of prompt report<strong>in</strong>g for prevent<strong>in</strong>g <strong>in</strong>fecti<strong>on</strong>. This applies to potentially exposed patients as<br />
well.<br />
• Occupati<strong>on</strong>al <strong>in</strong>juries should be reported <strong>in</strong> a system that allows medical management and<br />
track<strong>in</strong>g of exposed <strong>in</strong>dividuals, but also allows an<strong>on</strong>ymous analysis of <strong>in</strong>cidents, to identify<br />
factors that can be modified to prevent accidents. Some facilities supplement requests for<br />
medical management with periodic an<strong>on</strong>ymous surveys to improve report<strong>in</strong>g of exposures<br />
and near misses.<br />
• The benefits of PEP for HIV may be greatest if it is started as so<strong>on</strong> as possible; certa<strong>in</strong>ly, it<br />
should be started no later than 72 hours after exposure (27). Both the source patient and<br />
the exposed <strong>in</strong>dividual should undergo rapid test<strong>in</strong>g to avoid unnecessary treatment. Based<br />
<strong>on</strong> the test result or if the risk assessment requires it, antiretroviral therapy prophylaxis<br />
should be proposed as so<strong>on</strong> as possible; ideally with<strong>in</strong> the first hours, and certa<strong>in</strong>ly no later<br />
than 72 hours after the exposure.<br />
• Hepatitis B immunizati<strong>on</strong> should be offered to all those work<strong>in</strong>g <strong>in</strong> health-care facilities,<br />
and especially to phlebotomists. One to two m<strong>on</strong>ths after complet<strong>in</strong>g the three-dose<br />
series, the health worker should be tested to verify seroprotecti<strong>on</strong> (i.e. a c<strong>on</strong>centrati<strong>on</strong> of<br />
antibodies to hepatitis B surface antigen of at least 10 milli-<strong>in</strong>ternati<strong>on</strong>al units per millilitre<br />
[10 mIU/ml]). This is important because follow-up – <strong>in</strong>clud<strong>in</strong>g repeat serology test<strong>in</strong>g after<br />
exposure to a patient positive for hepatitis B surface antigen – is unnecessary if the exposed<br />
pers<strong>on</strong> was known to have resp<strong>on</strong>ded to the vacc<strong>in</strong>e. Titres will decrease over time, even<br />
<strong>in</strong> those who are seroprotected, but the vacc<strong>in</strong>ated pers<strong>on</strong> rema<strong>in</strong>s protected. In case of<br />
exposure, nati<strong>on</strong>al guidel<strong>in</strong>es <strong>on</strong> PEP for HBV exposure should be c<strong>on</strong>sulted. If n<strong>on</strong>e are<br />
available, detailed <strong>in</strong>structi<strong>on</strong>s <strong>on</strong> the use of hepatitis B immune serum globul<strong>in</strong> (HBIG)<br />
and immunizati<strong>on</strong> aga<strong>in</strong>st HBV are available from <str<strong>on</strong>g>WHO</str<strong>on</strong>g> (27).<br />
• A fourth dose of hepatitis B vacc<strong>in</strong>e should be offered to those who have completed their<br />
immunizati<strong>on</strong> but were tested 1–2 m<strong>on</strong>ths after complet<strong>in</strong>g the vacc<strong>in</strong>ati<strong>on</strong> and had a<br />
hepatitis B surface antibody titre below 10 mIU/ml. If fewer than three doses of hepatitis B<br />
immunizati<strong>on</strong> have been given, a course of hepatitis B immunizati<strong>on</strong> should be provided or<br />
completed.<br />
• There is no recommended PEP for exposure to HCV. If feasible, test<strong>in</strong>g of the source<br />
patient and health worker may be helpful to ensure workers compensati<strong>on</strong> <strong>in</strong> the case that<br />
occupati<strong>on</strong>ally acquired <strong>in</strong>fecti<strong>on</strong> is dem<strong>on</strong>strated. Research <strong>on</strong> PEP for HCV is <strong>on</strong>go<strong>in</strong>g to<br />
determ<strong>in</strong>e whether a regimen <strong>in</strong>volv<strong>in</strong>g peg<strong>in</strong>terfe<strong>on</strong> alfa-2b is effective. However, at least<br />
<strong>on</strong>e recent trial failed because n<strong>on</strong>e of the 213 workers exposed to HCV developed <strong>in</strong>fecti<strong>on</strong>,<br />
whether they received PEP or not (74).<br />
8 Implement<strong>in</strong>g best phlebotomy practices 53
8.5.3 Risk assessment and risk reducti<strong>on</strong> strategies<br />
There is a risk to both patients (or blood d<strong>on</strong>ors) and health workers if the phlebotomist is not<br />
well <strong>in</strong>formed of the patient’s risks. A short cl<strong>in</strong>ical history from the patient is essential.<br />
Risk can be reduced by follow<strong>in</strong>g best practices <strong>in</strong> <strong>in</strong>fecti<strong>on</strong> preventi<strong>on</strong> and c<strong>on</strong>trol, after<br />
obta<strong>in</strong><strong>in</strong>g <strong>in</strong>formed c<strong>on</strong>sent from the patient and blood d<strong>on</strong>ors (Table 8.1).<br />
Table 8.1<br />
Summary of risks and risk-reducti<strong>on</strong> strategies<br />
Risk Type of risk Risk reducti<strong>on</strong> strategy<br />
Patient/<br />
blood d<strong>on</strong>ors<br />
Health worker<br />
Exposure to bloodborne<br />
viruses through reuse of<br />
needles, syr<strong>in</strong>ges and lancets,<br />
c<strong>on</strong>tam<strong>in</strong>ated work surfaces<br />
Infecti<strong>on</strong> at blood sampl<strong>in</strong>g site<br />
Pa<strong>in</strong> at blood sampl<strong>in</strong>g site<br />
Haematoma or thrombus<br />
Extensive bleed<strong>in</strong>g<br />
Nerve damage (8, 10)<br />
Vasovagal reacti<strong>on</strong><br />
Syncope, fa<strong>in</strong>t<strong>in</strong>g (8, 10)<br />
Allergies<br />
Needle or sharps <strong>in</strong>jury dur<strong>in</strong>g<br />
or after the procedure<br />
Breakage of blood c<strong>on</strong>ta<strong>in</strong>ers<br />
Splashes (rare)<br />
Exposure to blood<br />
• Hepatitis B vacc<strong>in</strong>e for workers<br />
• Sterile s<strong>in</strong>gle-use devices <strong>on</strong>ly<br />
• Safety-eng<strong>in</strong>eered devices<br />
• Clean work surfaces with dis<strong>in</strong>fectant<br />
• Perform hand hygiene<br />
• Clean patient’s sk<strong>in</strong> with 70% isopropyl alcohol and<br />
allow to dry<br />
• Use sterile needle and syr<strong>in</strong>ge removed from the<br />
packag<strong>in</strong>g just before use<br />
• Well-tra<strong>in</strong>ed pers<strong>on</strong> should take the blood sample<br />
• Venepuncture is less pa<strong>in</strong>ful than heel-pricks <strong>in</strong><br />
ne<strong>on</strong>ates<br />
• Use needle of smaller gauge than the selected ve<strong>in</strong><br />
• Enter vessel at an angle of 30 degrees or less<br />
• Use gauge of needle smaller than the ve<strong>in</strong><br />
• Apply pressure to a straight arm for 3–5 m<strong>in</strong>utes after<br />
draw<strong>in</strong>g blood<br />
• Take a history to identify patients <strong>on</strong> anticoagulants<br />
and with a history of bleed<strong>in</strong>g<br />
• Use a gauge of needle smaller than the ve<strong>in</strong><br />
• Avoid f<strong>in</strong>ger-pricks for children<br />
• Use antecubital vessels when possible<br />
• Avoid prob<strong>in</strong>g<br />
• Hydrate patient, take postural blood pressure if<br />
dehydrated<br />
• Reduce anxiety<br />
• Have patient lie down if the pers<strong>on</strong> expresses c<strong>on</strong>cern<br />
• Provide audio-visusal distracti<strong>on</strong><br />
• Ask about allergies to latex, iod<strong>in</strong>e and alcohol before<br />
start<strong>in</strong>g the procedure<br />
• Use safety devices such as needle covers, tube holders<br />
that release needles with <strong>on</strong>e hand and safety lancets<br />
• Avoid two-handed recapp<strong>in</strong>g and disassembly<br />
• Place sharps c<strong>on</strong>ta<strong>in</strong>er <strong>in</strong> sight and with<strong>in</strong> arm’s reach<br />
• Dispose of used sharps immediately<br />
• Hepatitis B vacc<strong>in</strong>ati<strong>on</strong><br />
• Wear gloves<br />
• Use evacuated tubes and transfer devices when<br />
draw<strong>in</strong>g multiple tubes<br />
• Follow protocol for exposure to body fluids and report<br />
<strong>in</strong>cident, even if post-exposure prophylaxis is not<br />
desired<br />
• Cover broken sk<strong>in</strong> area with a waterproof dress<strong>in</strong>g<br />
54 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
9 M<strong>on</strong>itor<strong>in</strong>g and evaluati<strong>on</strong><br />
A m<strong>on</strong>itor<strong>in</strong>g and evaluati<strong>on</strong> system should be <strong>in</strong> place to offer surveillance of management of<br />
phlebotomy services and adverse events, and to document improvements. The <strong>in</strong>dicators to use<br />
<strong>in</strong>clude:<br />
• number and rate per 100 full-time workers of sharps exposures and other occupati<strong>on</strong>al<br />
<strong>in</strong>juries occurr<strong>in</strong>g am<strong>on</strong>g health workers <strong>in</strong> the past 12 m<strong>on</strong>ths;<br />
• number and rate of patients with adverse events <strong>in</strong> resp<strong>on</strong>se to phlebotomy such as<br />
haematoma, syncope, <strong>in</strong>fecti<strong>on</strong> or nerve damage;<br />
• number of reported cases of bloodborne pathogens transmitted dur<strong>in</strong>g phlebotomy (disease<br />
surveillance for hepatitis B and C, and HIV) as part of a public health surveillance system<br />
that is capable of receiv<strong>in</strong>g and resp<strong>on</strong>d<strong>in</strong>g to reports of cases and clusters of <strong>in</strong>fecti<strong>on</strong>s;<br />
• number (and percentage) of phlebotomy sessi<strong>on</strong>s where essential equipment was not<br />
available and phlebotomy sessi<strong>on</strong>s were cancelled;<br />
• number (and percentage) of laboratory test results lost due to errors or poor quality; for<br />
example<br />
––<br />
blood culture c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> rate;<br />
––<br />
blood transfusi<strong>on</strong> adverse events;<br />
––<br />
haemolysis;<br />
––<br />
number of specimens with illegible or miss<strong>in</strong>g paperwork or labels;<br />
––<br />
number of specimens that could not be processed due to <strong>in</strong>adequate sample volumes;<br />
• number (and percentage) of tra<strong>in</strong>ed staff <strong>in</strong> the health-care facility work<strong>in</strong>g <strong>in</strong> phlebotomy;<br />
• number (and proporti<strong>on</strong>) of juniors who are supervised by tra<strong>in</strong>ed staff.<br />
9 M<strong>on</strong>itor<strong>in</strong>g and evaluati<strong>on</strong> 55
PART IV REFERENCES
References<br />
1 Lavery I, Ingram P. <strong>Blood</strong> sampl<strong>in</strong>g: best practice. Nurs<strong>in</strong>g Standard, 2005, 19:55–65.<br />
2 Shahangian S et al. Results of a survey of hospital coagulati<strong>on</strong> laboratories <strong>in</strong> the United<br />
States. Archives of Pathology and Laboratory Medic<strong>in</strong>e, 2005, 129:47–60.<br />
3 Wagner D et al. Nosocomial acquisiti<strong>on</strong> of dengue. Emerg<strong>in</strong>g Infectious Diseases, 2004,<br />
10:1872–1873.<br />
4 Dreesman JB, A et al. Outbreak of hepatitis B <strong>in</strong> a nurs<strong>in</strong>g home associated with capillary<br />
blood sampl<strong>in</strong>g. Epidemiology and Infecti<strong>on</strong>, 2006, 134(5):1102–1113.<br />
5 Centers for Disease C<strong>on</strong>trol and Preventi<strong>on</strong>. Transmissi<strong>on</strong> of hepatitis B virus am<strong>on</strong>g pers<strong>on</strong>s<br />
undergo<strong>in</strong>g blood glucose m<strong>on</strong>itor<strong>in</strong>g <strong>in</strong> l<strong>on</strong>g-term care facilities – Mississippi, North<br />
Carol<strong>in</strong>a and Los Angeles County, California, 2003–2004. Morbidity and Mortality Weekly<br />
Report, 2004, 54:220–223.<br />
6 Chiavetta J et al. Estimated risk of transfusi<strong>on</strong> transmitted <strong>in</strong>fecti<strong>on</strong> <strong>in</strong> the Canadian blood<br />
supply (1987–1996). Vox Sangu<strong>in</strong>is, 2000, 78(Suppl 1):360.<br />
7 Moor ACE et al. Transfusi<strong>on</strong>-transmitted diseases: risks, preventi<strong>on</strong> and perspectives.<br />
European Journal of Haematology, 1999, 62(1):1–8.<br />
8 Galena H. Complicati<strong>on</strong>s occurr<strong>in</strong>g from diagnostic venepuncture. Journal of Family<br />
Practice, 1992, 34(5):582–584.<br />
9 Newman B et al. The effect of whole-blood d<strong>on</strong>or adverse events <strong>on</strong> blood d<strong>on</strong>or return rates.<br />
Transfusi<strong>on</strong>, 2006, 46:1374–1379.<br />
10 Eder A. The American Red Cross d<strong>on</strong>or haemovigilance program: complicati<strong>on</strong>s of blood<br />
d<strong>on</strong>ati<strong>on</strong> reported <strong>in</strong> 2006. Transfusi<strong>on</strong>, 2008, 48<br />
11 Barker L. Venipuncture syncope – <strong>on</strong>e occupati<strong>on</strong>al health cl<strong>in</strong>ic’s experience. Journal of the<br />
American Associati<strong>on</strong> of Occupati<strong>on</strong>al Health Nurses, 2008, 56(4):139–140.<br />
12 Centers for Disease C<strong>on</strong>trol and Preventi<strong>on</strong>. Evaluati<strong>on</strong> of safety devices for prevent<strong>in</strong>g<br />
percutaneous <strong>in</strong>juries am<strong>on</strong>g health-care pers<strong>on</strong>nel dur<strong>in</strong>g phlebotomy procedures 1993–<br />
1995. Morbidity and Mortality Weekly Report, 1997, 46:21–25.<br />
http://www.cdc.gov/mmwr/preview/mmwrhtml/00045648.htm<br />
13 Guidance for cl<strong>in</strong>ical health care pers<strong>on</strong>nel: protecti<strong>on</strong> aga<strong>in</strong>st <strong>in</strong>fecti<strong>on</strong> with blood-borne<br />
viruses. Recommendati<strong>on</strong>s of the Expert Advisory Group <strong>on</strong> AIDS and the Advisory Group<br />
<strong>on</strong> Hepatitis. Wetherby, UK Department of Health, 1998.<br />
14 Perry J, Jagger J. EPINet data report: <strong>in</strong>juries from phlebotomy needles. Advances <strong>in</strong><br />
Exposure Preventi<strong>on</strong>, 2003, 6(4):43–45.<br />
15 Cullen B et al. Potential for reported needlestick <strong>in</strong>jury preventi<strong>on</strong> am<strong>on</strong>g healthcare<br />
pers<strong>on</strong>nel through safety device usage and improvement of guidel<strong>in</strong>e adherence: expert panel<br />
assessment. Journal of Hospital Infecti<strong>on</strong>, 2006, 63:445–451.<br />
16 ALERT, Prevent<strong>in</strong>g needlestick <strong>in</strong>juries <strong>in</strong> health care sett<strong>in</strong>gs. Nati<strong>on</strong>al Institute for<br />
Occupati<strong>on</strong>al Safety and Health, 1999.<br />
17 Lam<strong>on</strong>tagne F et al. Role of safety-eng<strong>in</strong>eered devices <strong>in</strong> prevent<strong>in</strong>g needlestick <strong>in</strong>juries <strong>in</strong> 32<br />
French hospitals. Infecti<strong>on</strong> C<strong>on</strong>trol and Hospital Epidemiology, 2007, 28:18–23.<br />
18 Wilburn SE, Eijkemans G. Prevent<strong>in</strong>g needlestick <strong>in</strong>juries am<strong>on</strong>g healthcare workers: a<br />
<str<strong>on</strong>g>WHO</str<strong>on</strong>g>/ICN collaborati<strong>on</strong>. Internati<strong>on</strong>al Journal of Occupati<strong>on</strong>al and Envir<strong>on</strong>mental Health,<br />
2004, 10:451–456.<br />
References 59
19 Wilburn S, Eijkemans G. Protect<strong>in</strong>g health workers from occupati<strong>on</strong>al exposure to HIV,<br />
hepatitis, and other bloodborne pathogens: from research to practice. Asian-Pacific<br />
Newsletter <strong>on</strong> Occupati<strong>on</strong>al Health and Safety, 2007, 13:8–12.<br />
20 Sacar S et al. Poor hospital <strong>in</strong>fecti<strong>on</strong> c<strong>on</strong>trol practice <strong>in</strong> hand hygiene, glove utilizati<strong>on</strong>, and<br />
usage of tourniquets American Journal of Infecti<strong>on</strong> C<strong>on</strong>trol, 2006, 34(9):606–609.<br />
21 Castellaa A et al. Preventability of percutaneous <strong>in</strong>juries <strong>in</strong> healthcare pers<strong>on</strong>nel: a year-l<strong>on</strong>g<br />
survey <strong>in</strong> Italy. Journal of Hospital Infecti<strong>on</strong>, 2003, 55:290–294.<br />
22 Infecti<strong>on</strong> c<strong>on</strong>trol – preventi<strong>on</strong> of healthcare-associated <strong>in</strong>fecti<strong>on</strong>s <strong>in</strong> primary and<br />
community care. L<strong>on</strong>d<strong>on</strong>, Nati<strong>on</strong>al Institute for Health and Cl<strong>in</strong>ical Excellence, 2003.<br />
http://www.nice.org.uk/page.aspxo=CG002fullguidel<strong>in</strong>e<br />
23 Berkeris L et al. Trends <strong>in</strong> blood culture c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong>. A College of American Pathologist<br />
Q-tracks study of 356 <strong>in</strong>stituti<strong>on</strong>s. Archives of Pathology and Laboratory Medic<strong>in</strong>e, 2005,<br />
123:1222–1226.<br />
24 Jewell SM, J et al. Implementati<strong>on</strong> and evaluati<strong>on</strong> of a best practice <strong>in</strong>itiative: venepuncture<br />
<strong>in</strong> the well baby. Advances <strong>in</strong> Ne<strong>on</strong>atal Care, 2007, 7(5):222–229.<br />
25 Little M et al. Percutaneous blood sampl<strong>in</strong>g practice <strong>in</strong> a large urban hospital. Cl<strong>in</strong>ical<br />
Medic<strong>in</strong>e, 2007, 7:243–249.<br />
26 Scerbo M et al. The efficacy of a medical virtual reality simulator for tra<strong>in</strong><strong>in</strong>g phlebotomy.<br />
Human Factors: The Journal of the Human Factors and Erg<strong>on</strong>omics Society, 2006,<br />
48(1):72–84.<br />
27 <str<strong>on</strong>g>Guidel<strong>in</strong>es</str<strong>on</strong>g> <strong>on</strong> post exposure prophylaxis (PEP) to prevent human immunodeficiency virus<br />
(HIV) <strong>in</strong>fecti<strong>on</strong>. Geneva, World Health Organizati<strong>on</strong> and Internati<strong>on</strong>al Labour Organizati<strong>on</strong>,<br />
2008.<br />
http://www.who.<strong>in</strong>t/hiv/pub/guidel<strong>in</strong>es/PEP/en/<strong>in</strong>dex.html<br />
28 Eye of the needle – surveillance of significant occupati<strong>on</strong>al exposure to blood-borne viruses<br />
<strong>in</strong> healthcare pers<strong>on</strong>nel. L<strong>on</strong>d<strong>on</strong>, Health Protecti<strong>on</strong> Authority, 2005.<br />
29 Aide-memoire for a nati<strong>on</strong>al strategy for the safe and appropriate use of <strong>in</strong>jecti<strong>on</strong>s. Geneva,<br />
World Health Organizati<strong>on</strong>.<br />
http://www.path.org/files/SIGN-Aide-Memoire.pdf<br />
30 Hut<strong>in</strong> Y et al. <strong>Best</strong> <strong>in</strong>fecti<strong>on</strong> c<strong>on</strong>trol practices for <strong>in</strong>tradermal, subcutaneous and<br />
<strong>in</strong>tramuscular needle <strong>in</strong>jecti<strong>on</strong>s. Bullet<strong>in</strong> of the World Health Organizati<strong>on</strong>, 2003,<br />
81(7):491–500.<br />
31 So you’re go<strong>in</strong>g to collect a blood specimen: an <strong>in</strong>troducti<strong>on</strong> to phlebotomy, 12th ed. USA,<br />
College of American Pathologists, 2007.<br />
32 Lippi G et al. <strong>Phlebotomy</strong> issues and quality improvement <strong>in</strong> results of laboratory test<strong>in</strong>g.<br />
Cl<strong>in</strong>ical Laboratory, 2006, 52:217–230.<br />
33 Ford J. How to evaluate sharp safety-eng<strong>in</strong>eered devices. Nurs<strong>in</strong>g Times, 2008,<br />
104(36):42–45.<br />
34 Nati<strong>on</strong>al Audit Office. A safer place to work – improv<strong>in</strong>g the management of health and<br />
safety risks to staff <strong>in</strong> NHS trusts. L<strong>on</strong>d<strong>on</strong>, NDA, 2003.<br />
35 Leitch A et al. Reduc<strong>in</strong>g the potential for phlebotomy tourniquets to act as a reservoir for<br />
meticill<strong>in</strong>-resistant Staphylococcus aureus. Journal of Hospital Infecti<strong>on</strong>, 2006,<br />
63:428–431.<br />
36 Louie R et al. Multicenter study of the prevalence of blood c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> <strong>on</strong> po<strong>in</strong>t-of-care<br />
glucose meters and recommendati<strong>on</strong>s for c<strong>on</strong>troll<strong>in</strong>g c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong>. Po<strong>in</strong>t of Care, 2005,<br />
4:158–163.<br />
60 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
37 Rourke C, Bates C, Read R. Poor hospital <strong>in</strong>fecti<strong>on</strong> c<strong>on</strong>trol practice <strong>in</strong> blood sampl<strong>in</strong>g and use<br />
of tourniquets. Journal of Hospital Infecti<strong>on</strong>, 2001, 49:59–61.<br />
38 Kermode M. Health worker safety is a prerequisite for <strong>in</strong>jecti<strong>on</strong> safety <strong>in</strong> develop<strong>in</strong>g<br />
countries. Internati<strong>on</strong>al Journal of Infectious Diseases, 2004, 8:325–327.<br />
39 Norberg A et al. C<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> rates of blood cultures obta<strong>in</strong>ed by dedicated phlebotomy vs<br />
<strong>in</strong>tra venous catheter. Journal of the American Medical Associati<strong>on</strong>, 2003, 289(6):726–729.<br />
40 From AAALAC’s perspective, alcohol as a dis<strong>in</strong>fectant. AAALAC Internati<strong>on</strong>al, 2001.<br />
http://www.aaalac.org/publicati<strong>on</strong>s/C<strong>on</strong>necti<strong>on</strong>/Us<strong>in</strong>g_Alcohol_Dis<strong>in</strong>fectant.pdf<br />
41 Calfee D, Farr B. Comparis<strong>on</strong> of four antiseptic preparati<strong>on</strong>s for sk<strong>in</strong> <strong>in</strong> the preventi<strong>on</strong><br />
of c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of percutaneously drawn blood cultures: a randomized trial. Journal of<br />
Cl<strong>in</strong>ical Microbiology, 2002, 40(5):1660–1665.<br />
42 de Vries J, van Dorp W, van Barneveld P. A randomized c<strong>on</strong>trol trial of alcohol 70% versus<br />
alcoholic iod<strong>in</strong>e 2% <strong>in</strong> sk<strong>in</strong> dis<strong>in</strong>fecti<strong>on</strong> before <strong>in</strong>serti<strong>on</strong> of peripheral <strong>in</strong>fusi<strong>on</strong> catheters.<br />
Journal of Hospital Infecti<strong>on</strong>, 1997, 36:317–320.<br />
43 Procedures for the collecti<strong>on</strong> of diagnostic blood specimens by venipuncture. Approved<br />
standard, H3-A5. Wayne, PA, Nati<strong>on</strong>al Committee for Cl<strong>in</strong>ical Laboratory Standards, 2003.<br />
44 Rutala W, Weber D, Committee HICPA. <str<strong>on</strong>g>Guidel<strong>in</strong>es</str<strong>on</strong>g> for dis<strong>in</strong>fecti<strong>on</strong> and sterilizati<strong>on</strong> <strong>in</strong><br />
healthcare facilities 2008. Atlanta, GA, Centers for Disease C<strong>on</strong>trol and Preventi<strong>on</strong>, 2008.<br />
http://www.cdc.gov/ncidod/dhap/pdf/guidesl<strong>in</strong>es/Dis<strong>in</strong>fecti<strong>on</strong>_nov_2008.pdf<br />
45 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> hand hygiene <strong>in</strong> healthcare. Geneva, World Health Organizati<strong>on</strong>, 2009.<br />
http://whqlibdoc.who.<strong>in</strong>t/publicati<strong>on</strong>s/2009/9789241597906_eng.pdf<br />
46 Webster J, Bell-Syer S, Foxlee R. Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed<br />
by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of blood for transfusi<strong>on</strong>.<br />
Cochrane Database of Systematic Reviews, 2009, Issue 3. Art. No.: CD007948. DOI:<br />
10.1002/14651858.CD007948.<br />
http://mrw.<strong>in</strong>terscience.wiley.com/cochrane/clsysrev/articles/CD007948/frame.html<br />
47 Pratt RJ et al. epic2: Nati<strong>on</strong>al evidence-based guidel<strong>in</strong>es for prevent<strong>in</strong>g healthcare-associated<br />
<strong>in</strong>fecti<strong>on</strong>s <strong>in</strong> NHS hospitals <strong>in</strong> England. Journal of Hospital Infecti<strong>on</strong>, 2007, 65(Suppl 1):S1–<br />
S59.<br />
48 McD<strong>on</strong>ald C et al. Relative values of the <strong>in</strong>terventi<strong>on</strong>s of diversi<strong>on</strong> and improved d<strong>on</strong>orarm<br />
dis<strong>in</strong>fecti<strong>on</strong> to reduce the bacterial risk from blood transfusi<strong>on</strong>. Vox Sangu<strong>in</strong>is, 2004,<br />
86(3):178–182.<br />
49 McD<strong>on</strong>ald C. Bacterial risk reducti<strong>on</strong> by improved d<strong>on</strong>or arm dis<strong>in</strong>fecti<strong>on</strong>, diversi<strong>on</strong> and<br />
bacterial screen<strong>in</strong>g. Transfusi<strong>on</strong> Medic<strong>in</strong>e, 16(6):381–396.<br />
50 Liumbruno G et al. Reducti<strong>on</strong> of the risk of bacterial c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of blood comp<strong>on</strong>ents<br />
through diversi<strong>on</strong> of the first part of the d<strong>on</strong>ati<strong>on</strong> of blood and blood comp<strong>on</strong>ents. <strong>Blood</strong><br />
Transfusi<strong>on</strong>, 2009, 7(2):86–93.<br />
51 <strong>Blood</strong> transfusi<strong>on</strong> safety. Geneva, World Health Organizati<strong>on</strong>, 2009.<br />
http://www.who.<strong>in</strong>t/bloodsafety/en/<strong>Blood</strong>_Transfusi<strong>on</strong>_Safety.pdf<br />
52 Basic requirements for blood transfusi<strong>on</strong> services. Geneva, World Health Organizati<strong>on</strong>,<br />
2009.<br />
53 McLaughl<strong>in</strong> S et al. Prevalence of lymphedema <strong>in</strong> women with breast cancer 5 years after<br />
sent<strong>in</strong>el lymph node biopsy or axillary dissecti<strong>on</strong>: objective measurements. Journal of<br />
Cl<strong>in</strong>ical Oncology, 2008, 26(32):5213–5219.<br />
54 Newman B et al. The effect of a 473-ml (16-oz) water dr<strong>in</strong>k <strong>on</strong> vasovagal d<strong>on</strong>or reacti<strong>on</strong> rates<br />
<strong>in</strong> high school students. Transfusi<strong>on</strong>, 2007, 47(8):1524–1533.<br />
References 61
55 Hillyer C et al. Bacterial c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of blood comp<strong>on</strong>ents : risks, strategies and<br />
regulati<strong>on</strong>. American Society of Hematology. Educati<strong>on</strong> Program, 2003:575–589.<br />
56 Dh<strong>in</strong>gra-Kumar N, Sharma A, Madan N. Analysis <strong>in</strong> quality assurance programme for HIV<br />
screen<strong>in</strong>g <strong>in</strong> blood transfusi<strong>on</strong> centres <strong>in</strong> Delhi. Bullet<strong>in</strong> of the World Health Organizati<strong>on</strong>,<br />
1997, 75(3):223–228.<br />
57 Blajchman M. Bacterial c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> and proliferati<strong>on</strong> dur<strong>in</strong>g the storage of cellular blood<br />
products. Vox Sangu<strong>in</strong>is, 1998, 74:155–159.<br />
58 Blajchman M. Incidence and significance of the bacterial c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of blood<br />
comp<strong>on</strong>ents. Developmental Biology, 2002, 108:59–67.<br />
59 American Associati<strong>on</strong> for Respiratory Care. AARC cl<strong>in</strong>ical practice guidel<strong>in</strong>e. Sampl<strong>in</strong>g for<br />
arterial blood gas analysis. Respiratory Care, 1992, 8(37):891–897.<br />
60 Meites S. Sk<strong>in</strong>-puncture and blood-collect<strong>in</strong>g techniques for <strong>in</strong>fants: updates and problems.<br />
Cl<strong>in</strong>ical Chemistry, 1998, 34(9):1890–1894.<br />
61 Kristen M, Buckbee K. Implement<strong>in</strong>g a pediatric phlebotomy protocol. 1994.<br />
http://f<strong>in</strong>darticles.com/p/articles/mi_m3230/is_n4_v26/ai_15410785<br />
62 Shah V et al. Topical amethoca<strong>in</strong>e gel 4% for <strong>in</strong>tramuscular <strong>in</strong>jecti<strong>on</strong> <strong>in</strong> term ne<strong>on</strong>ates: A<br />
double-bl<strong>in</strong>d, placebo-c<strong>on</strong>trolled, randomized trial. Cl<strong>in</strong>ical Therapeutics, 2008, 30(1):166–<br />
174.<br />
63 Ogawa S et al. Venepuncture is preferable to heel lance for blood sampl<strong>in</strong>g <strong>in</strong> term ne<strong>on</strong>ates.<br />
Archives of Disease <strong>in</strong> Childhood. Fetal and Ne<strong>on</strong>atal Editi<strong>on</strong>, 2005, 90(5):F432–F436.<br />
64 Shah V, Ohlss<strong>on</strong> A. Venepuncture versus heel lance for blood sampl<strong>in</strong>g <strong>in</strong> term ne<strong>on</strong>ates.<br />
Cochrane Database of Systematic Reviews, 2007, Issue 4:CD001452.<br />
65 Blumenfeld T, Hertelendy W, Ford S. Simultaneously obta<strong>in</strong>ed sk<strong>in</strong>-puncture serum, sk<strong>in</strong>puncture<br />
plasma, and venous serum compared, and effects of warm<strong>in</strong>g the sk<strong>in</strong> before<br />
puncture. Cl<strong>in</strong>ical Chemistry, 1997, 23(9):1705–1710.<br />
66 Clagg M. Venous sample collecti<strong>on</strong> from ne<strong>on</strong>ates us<strong>in</strong>g dorsal hand ve<strong>in</strong>s. Laboratory<br />
Medic<strong>in</strong>e, 1989, 20(4):248–250.<br />
67 Fruhstorfer H, Schmelzeisen-Redeker G, Weiss T. Capillary blood sampl<strong>in</strong>g: relati<strong>on</strong> between<br />
lancet diameter, lanc<strong>in</strong>g pa<strong>in</strong> and blood volume. European Journal of Pa<strong>in</strong>, 1999,<br />
3(3):283–286.<br />
68 Lilien L et al. Ne<strong>on</strong>atal osteomyelitis of the calcaneus: complicati<strong>on</strong> of heel puncture. Journal<br />
of Pediatrics, 1976, 88(3):478–480.<br />
69 Pendergraph G. Handbook of phlebotomy, 3rd ed. Philadelphia, Lea & Febiger, 1992.<br />
70 Stevens B, Yamada J, Ohlss<strong>on</strong> A. Sucrose for analgesia <strong>in</strong> newborn <strong>in</strong>fants undergo<strong>in</strong>g pa<strong>in</strong>ful<br />
procedures. Cochrane Database of Systematic Reviews, 2004, Issue 3:CD001069.<br />
71 Guid<strong>in</strong>g pr<strong>in</strong>ciples to ensure <strong>in</strong>jecti<strong>on</strong> device security. Geneva, World Health Organizati<strong>on</strong>,<br />
2003.<br />
http://apps.who.<strong>in</strong>t/medic<strong>in</strong>edocs/en/d/Js4886e/<br />
72 Management of solid health-care waste at primary health-care centres: a decisi<strong>on</strong>-mak<strong>in</strong>g<br />
guide. Geneva, World Health Organizati<strong>on</strong>, 2007.<br />
http://www.who.<strong>in</strong>t/water_sanitati<strong>on</strong>_health/medicalwaste/hcwdmguide/en/<br />
73 Performance specificati<strong>on</strong> for sharps c<strong>on</strong>ta<strong>in</strong>ers. Geneva, World Health Organizati<strong>on</strong>, 2007.<br />
http://www.who.<strong>in</strong>t/immunizati<strong>on</strong>_standards/vacc<strong>in</strong>e_quality/who_pqs_e10_sb01.pdf<br />
74 Corey K et al. Pilot study of postexposure prophylaxis for hepatitis C virus <strong>in</strong> healthcare<br />
workers. Infecti<strong>on</strong> C<strong>on</strong>trol and Hospital Epidemiology, 2009, 30(10):1000–1005.<br />
62 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
PART V ANNEXES
Annex A: Methods and evidence base<br />
A1 C<strong>on</strong>sultati<strong>on</strong> with experts and scope of recommendati<strong>on</strong>s<br />
In April 2008, the <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Injecti<strong>on</strong> Safety programme – which is part of the Department<br />
of Essential Health Technologies (EHT) at <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Headquarters <strong>in</strong> Geneva – c<strong>on</strong>vened a<br />
c<strong>on</strong>sultati<strong>on</strong> <strong>on</strong> best practices for phlebotomy and blood collecti<strong>on</strong>. The c<strong>on</strong>sultati<strong>on</strong> <strong>in</strong>cluded<br />
special categories such as arterial blood sampl<strong>in</strong>g, capillary blood sampl<strong>in</strong>g and paediatric blood<br />
collecti<strong>on</strong>.<br />
A work<strong>in</strong>g group was c<strong>on</strong>vened, compris<strong>in</strong>g <strong>in</strong>ternati<strong>on</strong>al experts and colleagues from <str<strong>on</strong>g>WHO</str<strong>on</strong>g><br />
departments <strong>in</strong>volved <strong>in</strong> <strong>in</strong>fecti<strong>on</strong> c<strong>on</strong>trol and safety of health-care practices.<br />
The specific objectives of the c<strong>on</strong>sultati<strong>on</strong> were to:<br />
• review the first draft of this document, which had been developed <strong>in</strong> resp<strong>on</strong>se to cl<strong>in</strong>ical<br />
questi<strong>on</strong>s and a suggested scope developed by SIGN <strong>in</strong> c<strong>on</strong>sultati<strong>on</strong> with other <str<strong>on</strong>g>WHO</str<strong>on</strong>g><br />
experts and the Centres for Disease C<strong>on</strong>trol and Preventi<strong>on</strong>;<br />
• identify critical steps <strong>in</strong> phlebotomy procedure as a basis for mak<strong>in</strong>g recommendati<strong>on</strong>s.<br />
The focus of the c<strong>on</strong>sultati<strong>on</strong> was primarily <strong>on</strong> the needs of develop<strong>in</strong>g and transiti<strong>on</strong>al<br />
countries, <strong>in</strong> which <strong>in</strong>jecti<strong>on</strong> safety programmes are not yet well developed or <strong>in</strong> which quality<br />
systems are lack<strong>in</strong>g. The c<strong>on</strong>sultati<strong>on</strong> identified the need for guidel<strong>in</strong>es <strong>on</strong> best phlebotomy<br />
practices <strong>in</strong> policy and organizati<strong>on</strong>al issues, and <strong>in</strong> technical and scientific aspects of blood<br />
collecti<strong>on</strong>.<br />
Recommendati<strong>on</strong>s of the work<strong>in</strong>g group<br />
C<strong>on</strong>tent of guidel<strong>in</strong>es<br />
<str<strong>on</strong>g>Guidel<strong>in</strong>es</str<strong>on</strong>g> should <strong>in</strong>clude <strong>in</strong>formati<strong>on</strong> <strong>on</strong> the importance of:<br />
• safe practices <strong>in</strong> phlebotomy;<br />
• an un<strong>in</strong>terrupted supply of s<strong>in</strong>gle-use devices <strong>in</strong> situati<strong>on</strong>s where safetyeng<strong>in</strong>eered<br />
devices are unaffordable;<br />
• tra<strong>in</strong><strong>in</strong>g <strong>in</strong> phlebotomy, to avoid adverse effects to the patient and the<br />
health worker, and blood samples of poor quality.<br />
Evidence base<br />
Recommendati<strong>on</strong>s should be evidence based.<br />
C<strong>on</strong>sistency and flexibility<br />
Recommendati<strong>on</strong>s should be designed to:<br />
• promote a c<strong>on</strong>sistent approach to ensur<strong>in</strong>g phlebotomy safety and<br />
quality of blood drawn;<br />
• be sufficiently flexible to allow for variati<strong>on</strong>s <strong>in</strong> device selecti<strong>on</strong> and<br />
tra<strong>in</strong><strong>in</strong>g curricula.<br />
Annex A: Methods and evidence base 65
A2 Evidence base<br />
An <strong>in</strong>itial literature search was c<strong>on</strong>ducted by the guidel<strong>in</strong>e writer – Professor Mehtar (chair<br />
of the work<strong>in</strong>g group) – us<strong>in</strong>g PubMed, MedL<strong>in</strong>e, the <str<strong>on</strong>g>WHO</str<strong>on</strong>g> library database and regi<strong>on</strong>al<br />
databases. Particular efforts were made to identify systematic literature reviews and evidence<br />
that related specifically to phlebotomy practices <strong>in</strong> develop<strong>in</strong>g countries.<br />
The panel reviewed the draft guidel<strong>in</strong>es and the evidence retrieved, and reached c<strong>on</strong>sensus <strong>on</strong><br />
all but <strong>on</strong>e of the recommendati<strong>on</strong>s. It found that further evidence was needed to determ<strong>in</strong>e the<br />
effect of “alcohol al<strong>on</strong>e” versus “any sk<strong>in</strong> dis<strong>in</strong>fectant followed by alcohol for sk<strong>in</strong> preparati<strong>on</strong>”<br />
before blood collecti<strong>on</strong> for the purpose of blood transfusi<strong>on</strong>. The panel commissi<strong>on</strong>ed a<br />
systematic review with evidence tables based <strong>on</strong> GRADE 1 from the Cochrane group. The overall<br />
f<strong>in</strong>d<strong>in</strong>g from the review, which is given <strong>in</strong> Annex J (1), was as follows:<br />
In c<strong>on</strong>clusi<strong>on</strong> there is currently no evidence of a difference <strong>in</strong> either blood<br />
c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> or bacteraemia when d<strong>on</strong>or sk<strong>in</strong> is cleansed pre-venepuncture with<br />
a <strong>on</strong>e-step alcohol based process or a two-step alcohol plus antiseptic process. This<br />
lack of evidence for a difference however results from a complete absence of research<br />
and therefore a real difference cannot be discounted. Until better evidence emerges,<br />
decisi<strong>on</strong>s about which mode of pre-blood d<strong>on</strong>ati<strong>on</strong> sk<strong>in</strong> cleans<strong>in</strong>g to use are likely to be<br />
driven by c<strong>on</strong>venience and cost.<br />
This c<strong>on</strong>clusi<strong>on</strong> was circulated to the guidel<strong>in</strong>e development group, with a request for advice <strong>on</strong><br />
the best recommendati<strong>on</strong> to <strong>in</strong>corporate <strong>in</strong>to the guidel<strong>in</strong>e. Additi<strong>on</strong>al <strong>in</strong>fecti<strong>on</strong> c<strong>on</strong>trol experts<br />
(see list of additi<strong>on</strong>al reviewers) were c<strong>on</strong>sulted by e-mail, <strong>in</strong> l<strong>in</strong>e with the <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>e<br />
development procedure which notes that, when evidence is lack<strong>in</strong>g, a recommendati<strong>on</strong> should<br />
be based <strong>on</strong> expert op<strong>in</strong>i<strong>on</strong> as well as <strong>on</strong> c<strong>on</strong>venience and cost. C<strong>on</strong>sensus was reached by ask<strong>in</strong>g<br />
the experts to vote <strong>on</strong> the f<strong>in</strong>al recommendati<strong>on</strong>.<br />
The group was able to make a recommendati<strong>on</strong> <strong>on</strong> best practice for sk<strong>in</strong> dis<strong>in</strong>fecti<strong>on</strong> <strong>in</strong> blood<br />
transfusi<strong>on</strong> (see Secti<strong>on</strong> 4.2.1). Due to lack of evidence, the recommendati<strong>on</strong> was based <strong>on</strong><br />
expert op<strong>in</strong>i<strong>on</strong>.<br />
A3 Peer review and technical edit<strong>in</strong>g<br />
Follow<strong>in</strong>g the <strong>in</strong>ternal and external review and revisi<strong>on</strong>, an advanced draft of the document was<br />
sent to Dr Mary Catl<strong>in</strong> and Dr Michael Borg for a thorough peer review. The guidel<strong>in</strong>e was then<br />
submitted to the guidel<strong>in</strong>e development group and to additi<strong>on</strong>al experts who c<strong>on</strong>tributed to<br />
the development of the recommendati<strong>on</strong> <strong>on</strong> sk<strong>in</strong> dis<strong>in</strong>fecti<strong>on</strong> before blood d<strong>on</strong>ati<strong>on</strong>. The expert<br />
group amended the guidel<strong>in</strong>es <strong>in</strong> light of the comments received and agreed.<br />
The technical edit<strong>in</strong>g of this document was undertaken by Dr Hilary Cadman, under the<br />
technical guidance of Dr Selma Khamassi.<br />
A4 Implementati<strong>on</strong> and evaluati<strong>on</strong> plans<br />
The f<strong>in</strong>al phlebotomy guidel<strong>in</strong>es will be translated <strong>in</strong>to all United Nati<strong>on</strong>s languages, and<br />
pr<strong>in</strong>ted for distributi<strong>on</strong> <strong>in</strong> all six <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Regi<strong>on</strong>al Offices and <strong>in</strong> many different countries. It<br />
will also be made available through the <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Injecti<strong>on</strong> Safety Website. A CD-ROM c<strong>on</strong>ta<strong>in</strong><strong>in</strong>g<br />
the phlebotomy document, posters illustrat<strong>in</strong>g each of the practices described and a tra<strong>in</strong><strong>in</strong>g<br />
package will be produced and translated. The document will also be adapted to local needs <strong>in</strong><br />
some countries, although key steps and recommendati<strong>on</strong>s will be ma<strong>in</strong>ta<strong>in</strong>ed.<br />
1 The Grad<strong>in</strong>g of Recommendati<strong>on</strong>s Assessment, Development and Evaluati<strong>on</strong> (GRADE) Work<strong>in</strong>g Group is an <strong>in</strong>formal<br />
collaborati<strong>on</strong> that has developed a comm<strong>on</strong>, sensible and transparent approach to grad<strong>in</strong>g quality of evidence and strength<br />
of recommendati<strong>on</strong>s (http://www.gradework<strong>in</strong>ggroup.org).<br />
66 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Up<strong>on</strong> request, the <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Injecti<strong>on</strong> Safety programme will provide technical support for adapt<strong>in</strong>g<br />
and implement<strong>in</strong>g the guidel<strong>in</strong>e at regi<strong>on</strong>al and country levels.<br />
The feasibility of recommended practices and the impact of the guidel<strong>in</strong>e <strong>on</strong> phlebotomy<br />
practices will be evaluated by the <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Injecti<strong>on</strong> Safety programme, <strong>in</strong> collaborati<strong>on</strong> with <str<strong>on</strong>g>WHO</str<strong>on</strong>g><br />
Regi<strong>on</strong>al Offices. Feasibility and impact will be evaluated us<strong>in</strong>g the revised <strong>in</strong>jecti<strong>on</strong> safety<br />
assessment tool C, developed by the <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Injecti<strong>on</strong> Safety programme (2).<br />
A5 Review and updat<strong>in</strong>g of the recommendati<strong>on</strong>s<br />
The recommendati<strong>on</strong>s <strong>in</strong> this document are expected to rema<strong>in</strong> valid for five years; that is, until<br />
2014. The <str<strong>on</strong>g>WHO</str<strong>on</strong>g> Injecti<strong>on</strong> Safety programme will <strong>in</strong>itiate a review of these recommendati<strong>on</strong>s at<br />
that time.<br />
A6 M<strong>on</strong>itor<strong>in</strong>g and evaluati<strong>on</strong> of the implementati<strong>on</strong><br />
The <strong>in</strong>dicators listed <strong>in</strong> Chapter 9 should be used to m<strong>on</strong>itor and evaluate the implementati<strong>on</strong> of<br />
these guidel<strong>in</strong>es.<br />
Annex A: Methods and evidence base 67
Annex B: Infecti<strong>on</strong> preventi<strong>on</strong> and c<strong>on</strong>trol,<br />
safety equipment and best practice<br />
Table B.1 Recommendati<strong>on</strong>s for <strong>in</strong>fecti<strong>on</strong> preventi<strong>on</strong> and c<strong>on</strong>trol, safety equipment and best practice<br />
Item <strong>Best</strong> practice Rati<strong>on</strong>ale<br />
Pers<strong>on</strong>al protecti<strong>on</strong> and hygiene<br />
Hand hygiene a<br />
Before and after each patient c<strong>on</strong>tact, as<br />
well as between procedures <strong>on</strong> the same<br />
patient<br />
Reduces risk of cross-c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong><br />
between patients<br />
Gloves a<br />
A pair of well-fitt<strong>in</strong>g, clean, disposable<br />
latex or latex-free gloves per patient or<br />
per procedure<br />
Reduces the health-care worker’s<br />
potential exposure to blood and reduces<br />
the patient’s risk of cross-c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong><br />
between patients<br />
Masks, visors or<br />
goggles<br />
Not <strong>in</strong>dicated<br />
Apr<strong>on</strong>/gown or cover<br />
Not <strong>in</strong>dicated<br />
Safe blood-sampl<strong>in</strong>g equipment<br />
Tourniquet<br />
Clean elastic tourniquet reprocessed<br />
between patients<br />
C<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> with nosocomial bacteria<br />
has been documented <strong>on</strong> tourniquets<br />
DO NOT use latex gloves as a tourniquet<br />
if patients have an history of latex<br />
allergy<br />
Some patients may have latex allergy<br />
Sharps c<strong>on</strong>ta<strong>in</strong>ers<br />
Puncture and leak-proof c<strong>on</strong>ta<strong>in</strong>ers, that<br />
are sealed after use<br />
Keep c<strong>on</strong>ta<strong>in</strong>er visible and with<strong>in</strong> arms’<br />
reach<br />
Prevents needle-stick <strong>in</strong>jury to patients,<br />
health workers and the community at<br />
large<br />
Sk<strong>in</strong> preparati<strong>on</strong><br />
Inspect sk<strong>in</strong>, clean if visibly dirty<br />
Apply 70% alcohol with s<strong>in</strong>gle-use swab<br />
or clean cott<strong>on</strong>-wool ball<br />
Prevents <strong>in</strong>serti<strong>on</strong>-site <strong>in</strong>fecti<strong>on</strong> and<br />
c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of the blood collected<br />
Cott<strong>on</strong> wool that is pre-torn with bare<br />
hands is c<strong>on</strong>tam<strong>in</strong>ated and bacteria can<br />
multiply over time<br />
Do not leave c<strong>on</strong>ta<strong>in</strong>ers of cott<strong>on</strong><br />
saturated alcohol and cott<strong>on</strong>; dampen<br />
cott<strong>on</strong> immediately before use without<br />
c<strong>on</strong>tam<strong>in</strong>at<strong>in</strong>g the primary c<strong>on</strong>ta<strong>in</strong>er<br />
<strong>Blood</strong> sampl<strong>in</strong>g<br />
<strong>Draw<strong>in</strong>g</strong> venous blood<br />
For blood d<strong>on</strong>ati<strong>on</strong>, a <strong>on</strong>e-step<br />
comb<strong>in</strong>ati<strong>on</strong> of 2% chlorhexid<strong>in</strong>e<br />
gluc<strong>on</strong>ate <strong>in</strong> 70% isopropyl alcohol is<br />
recommended; allow to air dry<br />
Closed vacuum extracti<strong>on</strong> tubes with<br />
s<strong>in</strong>gle-use needle and needle holder<br />
Reduces c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of the blood<br />
collected<br />
Reduces exposure to blood and<br />
likelihood of c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong><br />
If needleholders must be reused due to<br />
cost, they should be removed with <strong>on</strong>e<br />
hand; some safety boxes have slots for<br />
this purpose<br />
W<strong>in</strong>ged needles with needle cover<br />
Safety syr<strong>in</strong>ges with retractable needles<br />
Safer for health workers and patients –<br />
reduces exposure to blood and sharps<br />
<strong>in</strong>juries<br />
Annex B: Infecti<strong>on</strong> preventi<strong>on</strong> and c<strong>on</strong>trol, safety equipment and best practice 69
Table B.1 c<strong>on</strong>t<strong>in</strong>ued<br />
Item <strong>Best</strong> practice Rati<strong>on</strong>ale<br />
<strong>Blood</strong> sampl<strong>in</strong>g<br />
Small quantities of<br />
capillary blood<br />
S<strong>in</strong>gle-use lancet<br />
Retractable lancet<br />
Lancet platform or glucometer is<br />
dedicated to <strong>on</strong>e patient dur<strong>in</strong>g hospital<br />
stay, or platform or device is cleaned<br />
of all visible dirt and dis<strong>in</strong>fected with<br />
alcohol between uses<br />
Hypodermic needles should be used with<br />
care as they may enter deeper than is<br />
desirable; they should never be used for<br />
heel-pricks<br />
Hepatitis <strong>in</strong>fecti<strong>on</strong>s have been<br />
transmitted to patients when lancet<br />
platforms or glucometers were used <strong>on</strong><br />
several patients without reprocess<strong>in</strong>g<br />
(i.e. without clean<strong>in</strong>g and dis<strong>in</strong>fecti<strong>on</strong>)<br />
<strong>Blood</strong>-sampl<strong>in</strong>g<br />
system<br />
<strong>Blood</strong>-sampl<strong>in</strong>g tubes or c<strong>on</strong>ta<strong>in</strong>ers<br />
(s<strong>in</strong>gle use)<br />
Vacuum-extracti<strong>on</strong> sampl<strong>in</strong>g reduces<br />
exposure to blood<br />
<strong>Blood</strong>-draw<strong>in</strong>g system<br />
Sterile blood collecti<strong>on</strong> bag (s<strong>in</strong>gle or<br />
multiple bag systems) with <strong>in</strong>tegrated<br />
needle and needle protecti<strong>on</strong><br />
<strong>Blood</strong> collected <strong>in</strong> these systems should<br />
be stored and transported accord<strong>in</strong>g to<br />
blood-bank procedures and the product<br />
(i.e. warm or cold stored) 150–500 ml<br />
sterile bag or bags for blood (medical or<br />
blood d<strong>on</strong>ati<strong>on</strong>)<br />
Reduces bacterial c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong><br />
Protects the health worker and patient<br />
Platelets may be stored at room<br />
temperature<br />
Some sterile blood bags may have<br />
a diversi<strong>on</strong> pouch to separate the<br />
first 10 ml or so of blood to reduce<br />
c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong><br />
Transportati<strong>on</strong> of<br />
laboratory samples<br />
Closed system that keeps samples<br />
upright and snugly fitted <strong>in</strong> stackable<br />
trays or racks<br />
Clearly labelled blood sample c<strong>on</strong>ta<strong>in</strong>ers<br />
(Some samples – such as cold<br />
agglut<strong>in</strong><strong>in</strong>s – may need to be<br />
transported <strong>in</strong> a warm transportati<strong>on</strong><br />
system)<br />
Closed system keeps blood samples<br />
c<strong>on</strong>ta<strong>in</strong>ed <strong>in</strong> case of breakage or spillage<br />
Clearly labelled sample c<strong>on</strong>ta<strong>in</strong>ers with<br />
track<strong>in</strong>g system allows samples to be<br />
traced<br />
Request forms<br />
A legible completed form must<br />
accompany blood sample to laboratory<br />
Form is stored with samples but <strong>in</strong> a<br />
separate compartment of the laboratory<br />
transport system<br />
Provides accurate <strong>in</strong>formati<strong>on</strong> <strong>on</strong> tests<br />
required and patient identificati<strong>on</strong><br />
Some facilities use a plastic bag with<br />
an outer pouch that keeps the paper<br />
with the specimen but protects it from<br />
c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong><br />
Specimen storage and<br />
blood sampl<strong>in</strong>g area<br />
Storage <strong>in</strong> a cool, separate area;<br />
temperature regulated to around 25 o C<br />
Keeps samples secure and away from<br />
the general public<br />
Patient <strong>in</strong>formati<strong>on</strong><br />
Verbal explanati<strong>on</strong> and c<strong>on</strong>sent<br />
(<strong>in</strong>formati<strong>on</strong> leaflet)<br />
Helps to ensure patient cooperati<strong>on</strong> and<br />
respect of patient rights<br />
a<br />
Source for <strong>in</strong>formati<strong>on</strong> <strong>on</strong> hand hygiene and gloves: (3, 4).<br />
70 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Annex C: Devices available for draw<strong>in</strong>g blood<br />
The <strong>in</strong>formati<strong>on</strong> given <strong>in</strong> this appendix is based <strong>on</strong> advice from the Centers for Disease C<strong>on</strong>trol<br />
and Preventi<strong>on</strong> (5).<br />
Table C.1<br />
Devices for draw<strong>in</strong>g blood<br />
Type of device Advantages Disadvantages<br />
C<strong>on</strong>venti<strong>on</strong>al devices<br />
Hypodermic s<strong>in</strong>gle-use needle and<br />
syr<strong>in</strong>ge<br />
Vacuum-tube systems<br />
W<strong>in</strong>ged steel needles (butterfly)<br />
Safety-eng<strong>in</strong>eered devices<br />
Passive<br />
Auto-disable (AD) syr<strong>in</strong>ges<br />
NOT recommended for blood<br />
draw<strong>in</strong>g<br />
Lancets<br />
Widely available<br />
Least expensive<br />
Comes <strong>in</strong> wide range of needle<br />
lengths and gauges<br />
Does not require special tra<strong>in</strong><strong>in</strong>g<br />
Can be used for blood draw<strong>in</strong>g <strong>in</strong><br />
paediatric populati<strong>on</strong><br />
For patient with small or difficult<br />
ve<strong>in</strong>s, blood draw<strong>in</strong>g can be easier<br />
than an evacuated tube system<br />
If hepar<strong>in</strong>ized, can be used for<br />
arterial blood draw<strong>in</strong>g<br />
Safer than us<strong>in</strong>g hypodermic<br />
needle and syr<strong>in</strong>ge<br />
Elim<strong>in</strong>ates blood transfer<br />
Allows numerous blood samples<br />
to be collected through s<strong>in</strong>gle<br />
venepuncture<br />
Good for blood draw<strong>in</strong>g from<br />
paediatric populati<strong>on</strong> or patient<br />
with small or difficult ve<strong>in</strong>s<br />
Allows better precisi<strong>on</strong> than<br />
hypodermic needle or evacuated<br />
tube needle<br />
Not recommended for phlebotomy<br />
Designed to prevent reuse, does<br />
not reduce the risks of needlesticks<br />
Retractable; prevent needle-stick<br />
<strong>in</strong>juries<br />
Requires blood transfer, creat<strong>in</strong>g<br />
additi<strong>on</strong>al risk for needle-stick<br />
<strong>in</strong>juries or blood splash<strong>in</strong>g<br />
Difficult to draw large or multiple<br />
blood samples<br />
A smaller syr<strong>in</strong>ge and paediatric<br />
laboratory tube should be used for<br />
paediatric patients<br />
Requires user to be skilled <strong>in</strong> its<br />
use<br />
Reuse of needle holder (tube<br />
holder) creates risk for needlestick<br />
<strong>in</strong>juries dur<strong>in</strong>g disassembly<br />
Mix<strong>in</strong>g comp<strong>on</strong>ents from different<br />
manufactures can create a<br />
problem dur<strong>in</strong>g use<br />
A smaller tube with a reduced<br />
vacuum should be used for<br />
paediatric patients<br />
Higher cost<br />
Because of the air <strong>in</strong> the tub<strong>in</strong>g,<br />
first tube must be collected<br />
without additive or discarded<br />
Difference <strong>in</strong> w<strong>in</strong>ged steel needles<br />
for evacuated system tubes and<br />
w<strong>in</strong>ged <strong>in</strong>fusi<strong>on</strong> set can create<br />
c<strong>on</strong>fusi<strong>on</strong><br />
Higher cost<br />
Dur<strong>in</strong>g prob<strong>in</strong>g, safety mechanism<br />
can be activated, requir<strong>in</strong>g new<br />
venepuncture<br />
Requires blood transfer, creat<strong>in</strong>g<br />
risk of needle-stick <strong>in</strong>juries<br />
Difficult to draw large or multiple<br />
blood samples<br />
Does NOT offer needle-stick<br />
preventi<strong>on</strong><br />
Air <strong>in</strong> the syr<strong>in</strong>ge can affect test<br />
results<br />
Requires additi<strong>on</strong>al tra<strong>in</strong><strong>in</strong>g<br />
Annex C: Devices available for draw<strong>in</strong>g blood 71
Table C.1 c<strong>on</strong>t<strong>in</strong>ued<br />
Type of device Advantages Disadvantages<br />
Safety-eng<strong>in</strong>eered devices<br />
Active<br />
Manually retractable syr<strong>in</strong>ges<br />
Self re-sheath<strong>in</strong>g needles and<br />
syr<strong>in</strong>ges<br />
W<strong>in</strong>ged steel needles with passive<br />
or active safety mechanism<br />
Manually retractable evacuated<br />
tube systems<br />
Safety mechanism retracts the<br />
needle <strong>in</strong>to the syr<strong>in</strong>ge, reduc<strong>in</strong>g<br />
the hazard of needle-stick<br />
exposure and the possibility of<br />
reuse<br />
Sleeve forwarded over the needle<br />
provides guard around the used<br />
needle, reduc<strong>in</strong>g the risk of<br />
needle-stick <strong>in</strong>jury; also prevents<br />
reuse<br />
Needle-lock<strong>in</strong>g mechanism helps<br />
to reduce the risk of needle-stick<br />
<strong>in</strong>jury and prevents reuse<br />
If syr<strong>in</strong>ge is used for blood<br />
draw<strong>in</strong>g, allows for safer transfer<br />
of blood<br />
Safer than us<strong>in</strong>g hypodermic<br />
needle and syr<strong>in</strong>ge because does<br />
not require blood transfer<br />
Allows numerous blood samples<br />
to be collected through s<strong>in</strong>gle<br />
venepuncture<br />
Safety mechanism prevents reuse<br />
and helps to reduce the risk of<br />
needle-stick <strong>in</strong>juries<br />
Safety mechanism cannot be<br />
activated when syr<strong>in</strong>ge is full of<br />
blood and dur<strong>in</strong>g blood transfer<br />
Requires health worker to use it as<br />
recommended<br />
Requires blood transfer, creat<strong>in</strong>g<br />
risk of needle-stick <strong>in</strong>juries<br />
Difficult to draw large or multiple<br />
blood samples<br />
High cost<br />
Needle cannot be covered when<br />
syr<strong>in</strong>ge is full of blood or dur<strong>in</strong>g<br />
blood transfer<br />
Requires user’s compliance<br />
Additi<strong>on</strong>al tra<strong>in</strong><strong>in</strong>g<br />
High cost<br />
If used <strong>in</strong> c<strong>on</strong>necti<strong>on</strong> with vacuum<br />
tubes, because of the air <strong>in</strong><br />
tub<strong>in</strong>g, the first tube is either<br />
without additive or discarded<br />
Requires additi<strong>on</strong>al tra<strong>in</strong><strong>in</strong>g<br />
High cost<br />
Requires skill <strong>in</strong> its use<br />
Reuse of needle (or tube) holders<br />
creates risk of needle-stick <strong>in</strong>juries<br />
dur<strong>in</strong>g disassembly<br />
Comp<strong>on</strong>ents from different<br />
manufacturers may be<br />
<strong>in</strong>compatible<br />
Smaller volume (1–5 ml) tube<br />
with lower vacuum should be used<br />
for paediatric patients to reduce<br />
haemolysis<br />
Requires additi<strong>on</strong>al tra<strong>in</strong><strong>in</strong>g<br />
High cost<br />
72 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Annex D: Manag<strong>in</strong>g occupati<strong>on</strong>al exposure to<br />
hepatitis B, hepatitis C and HIV<br />
Health workers may occasi<strong>on</strong>ally be accidentally exposed to blood and other body fluids that<br />
are potentially <strong>in</strong>fected with HIV, hepatitis virus or other bloodborne pathogens. Occupati<strong>on</strong>al<br />
exposure may occur through direct c<strong>on</strong>tact from splashes <strong>in</strong>to the eyes or mouth, or through<br />
<strong>in</strong>jury with a used needle or sharp <strong>in</strong>strument. Post-exposure prophylaxis (PEP) can help to<br />
prevent the transmissi<strong>on</strong> of pathogens after a potential exposure (6).<br />
This annex describes the steps <strong>in</strong> manag<strong>in</strong>g exposure to blood or other fluids that are potentially<br />
<strong>in</strong>fected with hepatitis B virus (HBV); hepatitis C virus (HCV) or HIV.<br />
Step 1 – Provide immediate first-aid care to the exposure site<br />
Provide immediate first-aid care as follows.<br />
• Wash wounds and sk<strong>in</strong> with soap and water. Do not use alcohol or str<strong>on</strong>g dis<strong>in</strong>fectants.<br />
• Let the wound bleed freely.<br />
• Do not put <strong>on</strong> a dress<strong>in</strong>g.<br />
• Flush eyes, the nose, the mouth and mucous membranes with water for at least 10 m<strong>in</strong>utes.<br />
Step 2 – Determ<strong>in</strong>e the risk associated with the exposure<br />
Determ<strong>in</strong>e the risk associated with the exposure by c<strong>on</strong>sider<strong>in</strong>g:<br />
• the type of fluid; for example, blood, visibly bloody fluid, other potentially <strong>in</strong>fectious fluid,<br />
or tissue and c<strong>on</strong>centrati<strong>on</strong> of virus;<br />
• the type of exposure; for example, there is a higher risk associated with percutaneous <strong>in</strong>jury<br />
with a large, hollow-bore needle, a deep puncture, visible blood <strong>on</strong> the device, a needle<br />
used <strong>in</strong> an artery or ve<strong>in</strong>, and exposure to a large volume of blood or semen, and less risk<br />
associated with exposure of mucous membranes or n<strong>on</strong><strong>in</strong>tact sk<strong>in</strong>, or exposure to a small<br />
volume of blood, semen or a less <strong>in</strong>fectious fluid (e.g. cerebrosp<strong>in</strong>al fluid).<br />
Step 3 – Evaluate the source of the potential exposure<br />
To evaluate the source of the potential exposure:<br />
• assess the risk of <strong>in</strong>fecti<strong>on</strong>, us<strong>in</strong>g available <strong>in</strong>formati<strong>on</strong>;<br />
• test the source pers<strong>on</strong> whenever possible, and <strong>on</strong>ly with his or her <strong>in</strong>formed c<strong>on</strong>sent; but<br />
• do not test discarded needles or syr<strong>in</strong>ges for virus c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong>.<br />
Annex D: Manag<strong>in</strong>g occupati<strong>on</strong>al exposure to hepatitis B, hepatitis C and HIV 73
Step 4 – Manage <strong>in</strong>dividuals exposed to HBV and HIV<br />
There is no PEP regimen recommended for HCV; however, there are specific steps that can be<br />
taken to reduce the risk of <strong>in</strong>fecti<strong>on</strong> for those exposed to HBV and HIV, as described below.<br />
Post-exposure prophylaxis for HBV<br />
A pers<strong>on</strong>’s resp<strong>on</strong>se to exposure to HBV depends <strong>on</strong> his or her immune status, as determ<strong>in</strong>ed by<br />
the history of hepatitis B vacc<strong>in</strong>ati<strong>on</strong> and vacc<strong>in</strong>e resp<strong>on</strong>se if tested 1–2 m<strong>on</strong>ths after vacc<strong>in</strong>ati<strong>on</strong><br />
(see Table D.1), and whether the exposure poses a risk of <strong>in</strong>fecti<strong>on</strong>. HBV PEP is safe for women<br />
who are pregnant or breastfeed<strong>in</strong>g.<br />
Table D.1 Recommendati<strong>on</strong>s for HBV post-exposure prophylaxis, accord<strong>in</strong>g to immune status<br />
HBV immune status<br />
Unvacc<strong>in</strong>ated<br />
Previously vacc<strong>in</strong>ated, known resp<strong>on</strong>der<br />
(anti-hepatitis B surface antigen positive)<br />
Previously vacc<strong>in</strong>ated, known n<strong>on</strong>resp<strong>on</strong>der<br />
Antibody resp<strong>on</strong>se unknown<br />
Post-exposure prophylaxis<br />
HBV vacc<strong>in</strong>ati<strong>on</strong> and HBIg<br />
N<strong>on</strong>e<br />
HBV vacc<strong>in</strong>ati<strong>on</strong> and HBIg<br />
Test; if antibody resp<strong>on</strong>se is < 10 IU/ml, give HBV<br />
vacc<strong>in</strong>ati<strong>on</strong> and HBIg<br />
HBIg, hepatitis B immunogobul<strong>in</strong>; HBV, hepatitis B virus.<br />
Source: CDC (7).<br />
Post-exposure prophylaxis for HIV<br />
Check the current nati<strong>on</strong>al guidel<strong>in</strong>es. This secti<strong>on</strong> is based <strong>on</strong> the <str<strong>on</strong>g>WHO</str<strong>on</strong>g>/ILO <str<strong>on</strong>g>Guidel<strong>in</strong>es</str<strong>on</strong>g> <strong>on</strong><br />
post exposure prophylaxis prophylaxis (PEP) to prevent human immunodeficiency virus<br />
(HIV) <strong>in</strong>fecti<strong>on</strong> (6). In additi<strong>on</strong> to first-aid care and evaluati<strong>on</strong> of exposure and risk, PEP for<br />
HIV <strong>in</strong>cludes counsell<strong>in</strong>g, HIV test<strong>in</strong>g based <strong>on</strong> <strong>in</strong>formed c<strong>on</strong>sent, and – depend<strong>in</strong>g <strong>on</strong> the<br />
risk assessment – the provisi<strong>on</strong> of a short course (28 days) of antiretroviral (ARV) drugs, with<br />
follow-up and support.<br />
The recommendati<strong>on</strong> for HIV PEP is based <strong>on</strong> an evaluati<strong>on</strong> of the risk of <strong>in</strong>fecti<strong>on</strong> described <strong>in</strong><br />
step 2.<br />
If the source pers<strong>on</strong> is identified, it is important to obta<strong>in</strong> <strong>in</strong>formati<strong>on</strong> <strong>on</strong> that pers<strong>on</strong>’s<br />
serostatus and, if positive, an evaluati<strong>on</strong> of the cl<strong>in</strong>ical status and treatment history.<br />
Test<strong>in</strong>g and counsell<strong>in</strong>g<br />
If test<strong>in</strong>g is available, the exposed pers<strong>on</strong> should be offered the chance to be tested for HIV and<br />
receive appropriate counsell<strong>in</strong>g. The pers<strong>on</strong> should always have the choice to refuse test<strong>in</strong>g.<br />
Perform HIV-antibody test<strong>in</strong>g at basel<strong>in</strong>e, and at 6–12 weeks and 6 m<strong>on</strong>ths after exposure. If the<br />
pers<strong>on</strong> develops HIV antibodies, he or she should be referred for treatment, care and support.<br />
Whenever possible, the source patient should also be tested, with his or her <strong>in</strong>formed c<strong>on</strong>sent.<br />
Antiretroviral drugs for post-exposure prophylaxis<br />
ARV drugs should be started as so<strong>on</strong> as possible, and certa<strong>in</strong>ly with<strong>in</strong> 72 hours of exposure.<br />
The drugs should be taken c<strong>on</strong>t<strong>in</strong>uously for 28 days. Health workers should not wait for tests<br />
results before tak<strong>in</strong>g or adm<strong>in</strong>ister<strong>in</strong>g PEP. If the test results show that the source pers<strong>on</strong> is<br />
negative, the prophylaxis can be stopped. Counsell<strong>in</strong>g should <strong>in</strong>clude provisi<strong>on</strong> of <strong>in</strong>formati<strong>on</strong><br />
<strong>on</strong> the importance of adher<strong>in</strong>g to treatment, and <strong>in</strong>formati<strong>on</strong> <strong>on</strong> HIV preventi<strong>on</strong> <strong>in</strong> general<br />
and <strong>in</strong> the workplace. The pers<strong>on</strong> should be advised to use c<strong>on</strong>doms, and not to d<strong>on</strong>ate blood<br />
74 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
or organs for up to 6 m<strong>on</strong>ths after exposure. Women of childbear<strong>in</strong>g age should be advised to<br />
use c<strong>on</strong>tracepti<strong>on</strong>, and alternatives to breastfeed<strong>in</strong>g should be discussed with women currently<br />
feed<strong>in</strong>g their <strong>in</strong>fants, because there is a high risk of transmitt<strong>in</strong>g HIV to the <strong>in</strong>fant if the mother<br />
becomes <strong>in</strong>fected dur<strong>in</strong>g breastfeed<strong>in</strong>g.<br />
Based <strong>on</strong> <str<strong>on</strong>g>WHO</str<strong>on</strong>g> recommendati<strong>on</strong>s, a two-drug PEP regimen should be used (see Table D.2),<br />
unless there is suspici<strong>on</strong> or evidence of drug resistance. The standard regimen c<strong>on</strong>sists of two<br />
nucleotide reverse transcriptase <strong>in</strong>hibitors (NRTIs). When there is suspici<strong>on</strong> that the virus could<br />
be resistant to <strong>on</strong>e or more of the drugs <strong>in</strong>cluded <strong>in</strong> the standard PEP regimen, a third drug – a<br />
protease <strong>in</strong>hibitor – should be added to the two chosen NRTIs (see Table D.2). In this situati<strong>on</strong>,<br />
it is best to c<strong>on</strong>sult an HIV expert.<br />
Table D.2<br />
Recommended two and three-drug post-exposure prophylaxis regimens<br />
Two-drug regimens<br />
Preferred regimens<br />
Alternative regimen<br />
Three-drug regimens<br />
Preferred regimen<br />
Alternative regimens<br />
1. ZDV + 3TC<br />
2. d4T + 3TC<br />
3. TDF + 3TC<br />
1. ZDV + 3TC + LPV/r<br />
2. ZDV + 3TC plus SQV/r or ATV/r or FPV/r<br />
3. TDF + 3TC plus SQV/r or ATV/r or FPV/r<br />
4. TDF + FTC plus SQV/r or ATV/r or FPV/r<br />
5. (d4T) + 3TC plus SQV/r or ATV/r or FPV/r<br />
3TC, lamivud<strong>in</strong>e; ATV/r, atazanavir/rit<strong>on</strong>avir; d4T, stavud<strong>in</strong>e; FPV/r, Fosamprenavir/rit<strong>on</strong>avir; FTC, emtricitab<strong>in</strong>e; LPV/r, lop<strong>in</strong>avir/rit<strong>on</strong>avir; SQV/r,<br />
siqu<strong>in</strong>avir/rot<strong>in</strong>avir; TDF, tenofovir; ZDV, zidovud<strong>in</strong>e.<br />
Follow-up<br />
Women of childbear<strong>in</strong>g age should not be prescribed medicati<strong>on</strong>s such as the comb<strong>in</strong>ati<strong>on</strong><br />
didanos<strong>in</strong>e plus stavud<strong>in</strong>e. They should be offered a pregnancy test before start<strong>in</strong>g the PEP<br />
regimen. Lactat<strong>in</strong>g women should be aware that ARVs are excreted <strong>in</strong> breast milk, and that the<br />
virus itself can be transmitted through breastfeed<strong>in</strong>g. When and where feasible, alternatives<br />
opti<strong>on</strong>s to breastfeed<strong>in</strong>g should be discussed with the mother.<br />
Follow-up visits should aim to support the pers<strong>on</strong>’s adherence to PEP, prevent or treat adverse<br />
effects of the medic<strong>in</strong>es, and detect seroc<strong>on</strong>versi<strong>on</strong>, if it occurs.<br />
Advise those who have been exposed to take precauti<strong>on</strong>s to prevent sec<strong>on</strong>dary transmissi<strong>on</strong><br />
dur<strong>in</strong>g the follow-up period. Such precauti<strong>on</strong>s <strong>in</strong>clude:<br />
• avoid<strong>in</strong>g pregnancy and seek<strong>in</strong>g safe alternatives to breastfeed<strong>in</strong>g;<br />
• avoid<strong>in</strong>g d<strong>on</strong>at<strong>in</strong>g blood, tissue or sperm;<br />
• us<strong>in</strong>g c<strong>on</strong>doms dur<strong>in</strong>g sexual <strong>in</strong>tercourse, until the test at 6 m<strong>on</strong>ths c<strong>on</strong>firms that the<br />
exposed pers<strong>on</strong> rema<strong>in</strong>s ser<strong>on</strong>egative.<br />
PEP for HIV and hepatitis B is not <strong>in</strong>dicated:<br />
• if the exposed pers<strong>on</strong> is already HIV-positive from a previous exposure;<br />
• <strong>in</strong> the c<strong>on</strong>text of chr<strong>on</strong>ic exposure (e.g. repeated exposure to HIV from unprotected sexual<br />
<strong>in</strong>tercourse with a known HIV-positive partner); or<br />
• if the exposure poses no risk of transmissi<strong>on</strong>; for example, <strong>in</strong> the case of<br />
––<br />
exposure of <strong>in</strong>tact sk<strong>in</strong> to potentially <strong>in</strong>fectious body fluids;<br />
– – exposure to body fluids that are not known to transmit HIV or HBV (faeces, saliva, ur<strong>in</strong>e<br />
or sweat); or<br />
Annex D: Manag<strong>in</strong>g occupati<strong>on</strong>al exposure to hepatitis B, hepatitis C and HIV 75
––<br />
exposure to body fluids from a pers<strong>on</strong> known to be HIV-negative, unless the source<br />
pers<strong>on</strong> is identified as be<strong>in</strong>g at high risk of hav<strong>in</strong>g been recently <strong>in</strong>fected and is currently<br />
with<strong>in</strong> the w<strong>in</strong>dow period for seroc<strong>on</strong>versi<strong>on</strong>.<br />
Step 5 – Report the <strong>in</strong>cident<br />
After the <strong>in</strong>cident, refer the exposed pers<strong>on</strong> to a tra<strong>in</strong>ed service provider who can give<br />
counsell<strong>in</strong>g, evaluate the risk of transmissi<strong>on</strong> of bloodborne pathogens hav<strong>in</strong>g occurred, and<br />
decide <strong>on</strong> the need to prescribe ARV drugs or hepatitis B vacc<strong>in</strong>e to prevent <strong>in</strong>fecti<strong>on</strong> with HIV<br />
or HBV, respectively.<br />
Both the <strong>in</strong>cident report and the evaluati<strong>on</strong> of the risk of exposure should lead to quality c<strong>on</strong>trol<br />
and evaluati<strong>on</strong> of the safety of work<strong>in</strong>g c<strong>on</strong>diti<strong>on</strong>s.<br />
Take correcti<strong>on</strong>al measures to prevent exposure to HIV and other bloodborne pathogens.<br />
76 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Annex E: Tra<strong>in</strong><strong>in</strong>g course c<strong>on</strong>tent for<br />
phlebotomists<br />
Before undertak<strong>in</strong>g phlebotomy, health workers should be tra<strong>in</strong>ed <strong>in</strong>, and dem<strong>on</strong>strate<br />
proficiency for, the blood collecti<strong>on</strong> procedures <strong>on</strong> the patient populati<strong>on</strong> that will be with<strong>in</strong><br />
their scope of practice.<br />
Tra<strong>in</strong><strong>in</strong>g should cover paediatric, ne<strong>on</strong>atal and <strong>in</strong>tensive care, and blood transfusi<strong>on</strong>, as<br />
appropriate.<br />
Competence <strong>in</strong> phlebotomy practices should be an essential part of the f<strong>in</strong>al evaluati<strong>on</strong> of those<br />
tra<strong>in</strong><strong>in</strong>g as health workers.<br />
The outcome of the course should be safety of patients, adequacy of the laboratory specimens,<br />
and safety of health workers and the community.<br />
Course c<strong>on</strong>tents<br />
• Anatomy of the phlebotomy sites from which the worker is authorized to access blood.<br />
• Infecti<strong>on</strong> preventi<strong>on</strong> and c<strong>on</strong>trol:<br />
––<br />
elements of standard precauti<strong>on</strong>s relevant to venepuncture (hand hygiene, wear<strong>in</strong>g<br />
n<strong>on</strong>-sterile gloves);<br />
––<br />
use of antiseptics – sk<strong>in</strong> dis<strong>in</strong>fecti<strong>on</strong>;<br />
––<br />
clean<strong>in</strong>g and dis<strong>in</strong>fecti<strong>on</strong> of materials used <strong>on</strong> more than <strong>on</strong>e patient, <strong>in</strong>clud<strong>in</strong>g<br />
tourniquets, scissors and specimen carriers;<br />
––<br />
disposal of used equipment, especially sharps.<br />
• Protecti<strong>on</strong> of the patient:<br />
––<br />
patient identificati<strong>on</strong>, <strong>in</strong>clud<strong>in</strong>g children and c<strong>on</strong>fused patients;<br />
––<br />
awareness of the <strong>in</strong>stituti<strong>on</strong>’s rule to halt and seek help after a def<strong>in</strong>ed number of<br />
unsuccessful draws;<br />
––<br />
<strong>in</strong>formed c<strong>on</strong>sent and patient rights;<br />
––<br />
manag<strong>in</strong>g supplies for patients <strong>in</strong> isolati<strong>on</strong>;<br />
––<br />
awareness of c<strong>on</strong>tra<strong>in</strong>dicati<strong>on</strong>s to blood draws <strong>in</strong>clud<strong>in</strong>g draw<strong>in</strong>g <strong>on</strong> the same side as<br />
a mastectomy, through <strong>in</strong>fected or scarred tissues, and through <strong>in</strong>-dwell<strong>in</strong>g vascular<br />
devices (per <strong>in</strong>stituti<strong>on</strong>al policy).<br />
• Protecti<strong>on</strong> of the health worker:<br />
––<br />
immunizati<strong>on</strong> with hepatitis B;<br />
––<br />
awareness of high risk devices and practices;<br />
––<br />
ability to state who and when to c<strong>on</strong>tact for support <strong>in</strong> the event of exposure to blood<br />
and body fluids;<br />
––<br />
awareness of the benefits of PEP and the need to have source patients tested and HIV<br />
PEP started, preferably with<strong>in</strong> hours;<br />
––<br />
avoidance of two-handed needle recapp<strong>in</strong>g, disassembly of devices, removal of needles<br />
prior to <strong>in</strong>ject<strong>in</strong>g blood <strong>in</strong>to tube;<br />
––<br />
placement and use of sharps c<strong>on</strong>ta<strong>in</strong>er with<strong>in</strong> arm’s reach;<br />
––<br />
appropriate use of pers<strong>on</strong>al protective equipment, <strong>in</strong>clud<strong>in</strong>g gloves.<br />
Annex E: Tra<strong>in</strong><strong>in</strong>g course c<strong>on</strong>tent for phlebotomists 77
• Types of equipment available for blood sampl<strong>in</strong>g, and procurement and use of equipment.<br />
• Practice tak<strong>in</strong>g blood samples, <strong>in</strong>clud<strong>in</strong>g blood sampl<strong>in</strong>g and simulated blood sampl<strong>in</strong>g<br />
(capillary blood, arterial blood, venous blood from adults and children accord<strong>in</strong>g to<br />
resp<strong>on</strong>sibilities.<br />
• Practice <strong>on</strong> artificial arms and cl<strong>in</strong>ical skills development.<br />
• Special techniques:<br />
––<br />
capillary puncture<br />
▪ ▪ heel and f<strong>in</strong>ger-pricks<br />
▪▪<br />
▪▪<br />
lancets<br />
capillary tubes (filter paper, capillary blood tubes, rapid test strips, etc.)<br />
––<br />
venous blood<br />
▪▪<br />
▪▪<br />
▪▪<br />
▪▪<br />
large volume (blood lett<strong>in</strong>g – aware that this must be d<strong>on</strong>e under direct physician<br />
order and management)<br />
w<strong>in</strong>ged needles<br />
evacuated tubes<br />
blood cultures.<br />
• Adverse events and management.<br />
• Occupati<strong>on</strong>al exposure and management:<br />
––<br />
the country’s relevant occupati<strong>on</strong>al health regulati<strong>on</strong>s, <strong>in</strong>clud<strong>in</strong>g PEP for preventi<strong>on</strong> of<br />
HIV and hepatitis B;<br />
––<br />
the procedure for, and benefits of, report<strong>in</strong>g occupati<strong>on</strong>al exposure to blood;<br />
––<br />
first aid after exposure (see management);<br />
––<br />
PEP (importance of timely resp<strong>on</strong>se);<br />
––<br />
surveillance and use of data for preventi<strong>on</strong> of occupati<strong>on</strong>al exposure.<br />
• Waste management, <strong>in</strong>clud<strong>in</strong>g disposal of waste and sharps, and procedures for spillage<br />
and breakage.<br />
• Laboratory practices, <strong>in</strong>clud<strong>in</strong>g type of samples, forms, labell<strong>in</strong>g and transportati<strong>on</strong>.<br />
• Standards of practice.<br />
• Susta<strong>in</strong>ability of tra<strong>in</strong><strong>in</strong>g programme.<br />
• Career path.<br />
• Skill-based <strong>in</strong>centives.<br />
78 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Annex F: Expla<strong>in</strong><strong>in</strong>g the procedure to a patient<br />
Introducti<strong>on</strong>:<br />
Hello, I am ________________ I work at this health-care facility.<br />
What is your name (Health-care worker checks first and last name aga<strong>in</strong>st order for tests and<br />
the patient’s name band if present).<br />
I am tra<strong>in</strong>ed to take blood for laboratory tests (or medical reas<strong>on</strong>s) and I have experience <strong>in</strong><br />
tak<strong>in</strong>g blood.<br />
I will <strong>in</strong>troduce a small needle <strong>in</strong>to your ve<strong>in</strong> and gently draw some blood for ________ tests.<br />
(Tell the patient the specific tests to be drawn).<br />
Then I will label them with your name and c<strong>on</strong>tact details and send them off for tests to the<br />
laboratory. The results will be returned to Dr ________ (menti<strong>on</strong> the name of the cl<strong>in</strong>ician<br />
who ordered the tests).<br />
Do you have any questi<strong>on</strong>s Did you understand what I expla<strong>in</strong>ed to you Are you will<strong>in</strong>g to be<br />
tested<br />
Please sit down and make yourself comfortable.<br />
Now, I will ask you a few questi<strong>on</strong>s so that both of us feel comfortable about the procedure.<br />
• Have you ever had blood taken before<br />
• (If yes) How did it feel How l<strong>on</strong>g ago was that<br />
• Are you scared of needles<br />
• Are you allergic to anyth<strong>in</strong>g (Ask specifically about latex, povid<strong>on</strong>e iod<strong>in</strong>e, tape.)<br />
• Have you ever fa<strong>in</strong>ted when your blood was drawn<br />
• Have you eaten or drunk anyth<strong>in</strong>g <strong>in</strong> the past two hours<br />
• How are you feel<strong>in</strong>g at the moment<br />
Shall we start If you feel unwell or uncomfortable, please let me know at <strong>on</strong>ce.<br />
Annex F: Expla<strong>in</strong><strong>in</strong>g the procedure to a patient 79
Annex G: Disassembly of needle from syr<strong>in</strong>ge or<br />
other devices<br />
Safe methods of remov<strong>in</strong>g the needle from the syr<strong>in</strong>ge or other devices are necessary to protect<br />
health workers from <strong>in</strong>jury.<br />
This procedure must be carried out close to a sharps c<strong>on</strong>ta<strong>in</strong>er, and the needle must be<br />
discarded immediately.<br />
NEVER disassemble an exposed, used needle with your bare hands.<br />
If the needle has to be disassembled from the barrel or syr<strong>in</strong>ge, re-sheath us<strong>in</strong>g a <strong>on</strong>e-hand<br />
scoop technique, then remove the needle us<strong>in</strong>g a removal device. Both of these procedures are<br />
expla<strong>in</strong>ed below.<br />
One-hand scoop technique<br />
1. Leave the needle cap <strong>on</strong> the surface and guide the tip of the used needle tip <strong>in</strong>to it us<strong>in</strong>g<br />
<strong>on</strong>ly <strong>on</strong>e hand. Clean the surface with dis<strong>in</strong>fectant afterward to avoid leav<strong>in</strong>g blood.<br />
2. Place the needle cap aga<strong>in</strong>st a firm upright surface with its open<strong>in</strong>g towards the<br />
phlebotomist, and place the used needle tip <strong>in</strong>to it.<br />
3. Lift the needle and syr<strong>in</strong>ge vertically and, <strong>on</strong>ce the tip is covered, use the other hand to fix<br />
the cap <strong>in</strong>to place.<br />
Use of a removal device<br />
• Needle pliers – Hold the needle with pliers or artery forceps. Dislodge the needle by<br />
unscrew<strong>in</strong>g or pull<strong>in</strong>g it off. Discard immediately <strong>in</strong>to a sharps c<strong>on</strong>ta<strong>in</strong>er.<br />
• Needle guard (mushroom) – Place the cap <strong>in</strong> the device. Us<strong>in</strong>g <strong>on</strong>e hand, <strong>in</strong>sert the needle<br />
tip <strong>in</strong>to the cap vertically and turn firmly to fix the needle <strong>in</strong> the cap. Lift the syr<strong>in</strong>ge or<br />
barrel and removed the covered needle. Discard immediately.<br />
Annex G: Disassembly of needle from syr<strong>in</strong>ge or other devices 81
Annex H: <strong>Blood</strong> spillage<br />
<strong>Blood</strong> spillage may occur because a laboratory sample breaks <strong>in</strong> the phlebotomy area or dur<strong>in</strong>g<br />
transportati<strong>on</strong>, or because there is excessive bleed<strong>in</strong>g dur<strong>in</strong>g the procedure. In this situati<strong>on</strong>,<br />
clean up the spillage and record the <strong>in</strong>cident, us<strong>in</strong>g the follow<strong>in</strong>g procedure.<br />
1. Wear a pair of n<strong>on</strong>-sterile gloves.<br />
2. Use t<strong>on</strong>gs or a pan and brush to sweep up as much of the broken glass (or c<strong>on</strong>ta<strong>in</strong>er) as<br />
possible. Do not pick up pieces with your hands.<br />
3. Discard the broken glass <strong>in</strong> a sharps c<strong>on</strong>ta<strong>in</strong>er. If this is not possible due to the size of the<br />
broken glass, wrap the glass or c<strong>on</strong>ta<strong>in</strong>er <strong>in</strong> several layers of paper and discard it carefully<br />
<strong>in</strong> a separate c<strong>on</strong>ta<strong>in</strong>er. Do not place it <strong>in</strong> the regular waste c<strong>on</strong>ta<strong>in</strong>er.<br />
4. Use disposable paper towels to absorb as much of the body fluids as possible.<br />
5. Wipe the area with water and detergent until it is visibly clean.<br />
6. Saturate the area aga<strong>in</strong> with sodium hypochlorite 0.5% (10 000 ppm available chlor<strong>in</strong>e).<br />
This is a 1:10 diluti<strong>on</strong> of 5.25% sodium hypochlorite bleach, which should be prepared<br />
daily.<br />
7. R<strong>in</strong>se off the t<strong>on</strong>gs, brush and pan, under runn<strong>in</strong>g water and place to dry.<br />
8. Remove gloves and discard them.<br />
9. Wash hands carefully with soap and water, and dry thoroughly with s<strong>in</strong>gle-use towels.<br />
10. Record the <strong>in</strong>cident <strong>in</strong> the <strong>in</strong>cident book if a specimen was lost, or pers<strong>on</strong>s were exposed to<br />
blood and body fluids.<br />
Annex H: <strong>Blood</strong> spillage 83
Annex I:<br />
Modified Allen test<br />
A modified Allen test measures arterial competency, and should be performed before tak<strong>in</strong>g an<br />
arterial sample. The procedure for perform<strong>in</strong>g the test is as follows (see Figure I.1, below).<br />
1. Instruct the patient to clench his or her fist; if the patient is unable to do this, close the<br />
pers<strong>on</strong>’s hand tightly.<br />
2. Us<strong>in</strong>g your f<strong>in</strong>gers, apply occlusive pressure to both the ulnar and radial arteries, to obstruct<br />
blood flow to the hand.<br />
3. While apply<strong>in</strong>g occlusive pressure to both arteries, have the patient relax his or her hand,<br />
and check whether the palm and f<strong>in</strong>gers have blanched. If this is not the case, you have not<br />
completely occluded the arteries with your f<strong>in</strong>gers.<br />
Figure I.1<br />
Allen test<br />
Thumbs occlude radial and ulnar arteries.<br />
Pallor is produced by clenched fist.<br />
Thumb occludes radial artery while ulnar artery is<br />
released and patent. Unclenched hand returns to<br />
basel<strong>in</strong>e colour because of ulnar artery and c<strong>on</strong>nect<strong>in</strong>g<br />
arches.<br />
Source: http://fitsweb.uchc.edu/student/selectives/TimurGraham/Modified_Allen%27s_Test.html<br />
Release the occlusive pressure <strong>on</strong> the ulnar artery <strong>on</strong>ly to determ<strong>in</strong>e whether the modified Allen<br />
test is positive or negative.<br />
• Positive modified Allen test – If the hand flushes with<strong>in</strong> 5–15 sec<strong>on</strong>ds it <strong>in</strong>dicates that the<br />
ulnar artery has good blood flow; this normal flush<strong>in</strong>g of the hand is c<strong>on</strong>sidered to be a<br />
positive test.<br />
• Negative modified Allen test – If the hand does not flush with<strong>in</strong> 5–15 sec<strong>on</strong>ds, it <strong>in</strong>dicates<br />
that ulnar circulati<strong>on</strong> is <strong>in</strong>adequate or n<strong>on</strong>existent; <strong>in</strong> this situati<strong>on</strong>, the radial artery<br />
supply<strong>in</strong>g arterial blood to that hand should not be punctured.<br />
Annex I: Modified Allen test 85
Annex J: Cochrane review<br />
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of ...<br />
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for<br />
prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of blood for transfusi<strong>on</strong>.<br />
Review <strong>in</strong>formati<strong>on</strong><br />
Authors<br />
Joan Webster 1 , Sally EM Bell-Syer 2 , Ruth Foxlee 2<br />
1 Centre for Cl<strong>in</strong>ical Nurs<strong>in</strong>g, Royal Brisbane and Women's Hospital, Herst<strong>on</strong>, Australia<br />
2 Department of Health Sciences, University of York, York, UK<br />
Citati<strong>on</strong> example: Webster J, Bell-Syer SEM, Foxlee R. Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by<br />
any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of blood for transfusi<strong>on</strong>.. Cochrane Database of<br />
Systematic Reviews , Issue . Art. No.: . DOI: .<br />
C<strong>on</strong>tact pers<strong>on</strong><br />
Joan Webster<br />
Nurs<strong>in</strong>g Director, Research<br />
Centre for Cl<strong>in</strong>ical Nurs<strong>in</strong>g<br />
Royal Brisbane and Women's Hospital<br />
Level 2, Build<strong>in</strong>g 34<br />
Butterfield Street<br />
Herst<strong>on</strong><br />
QLD<br />
4029<br />
Australia<br />
E-mail: joan_webster@health.qld.gov.au<br />
Dates<br />
Assessed as Up-to-date:10 March 2009<br />
Date of Search: 10 March 2009<br />
Next Stage Expected: 4 April 2011<br />
Protocol First Published: Not specified<br />
Review First Published: Not specified<br />
Last Citati<strong>on</strong> Issue: Not specified<br />
What's new<br />
Date Event Descripti<strong>on</strong><br />
History<br />
Date Event Descripti<strong>on</strong><br />
Abstract<br />
Background<br />
<strong>Blood</strong> for transfusi<strong>on</strong> may become c<strong>on</strong>tam<strong>in</strong>ated at any po<strong>in</strong>t between collecti<strong>on</strong> and transfusi<strong>on</strong> and may result<br />
<strong>in</strong> bacteraemia (the presence of bacteria <strong>in</strong> the blood), severe illness or even death for the blood recipient. D<strong>on</strong>or<br />
arm sk<strong>in</strong> is <strong>on</strong>e potential source of blood c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong>, so it is usual to cleanse the sk<strong>in</strong> with an antiseptic<br />
before blood d<strong>on</strong>ati<strong>on</strong>. One-step and two-step alcohol based antiseptic regimens are both comm<strong>on</strong>ly advocated<br />
but there is uncerta<strong>in</strong>ty as to which is most effective.<br />
Objectives<br />
To assess the effects of cleans<strong>in</strong>g the sk<strong>in</strong> of blood d<strong>on</strong>ors with alcohol <strong>in</strong> a <strong>on</strong>e-step compared with alcohol <strong>in</strong> a<br />
two-step procedure to prevent c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of collected blood or bacteraemia <strong>in</strong> the recipient.<br />
Search strategy<br />
We searched the Cochrane Wounds Group Specialised Register (March 10 2009); The Cochrane Central Register<br />
of C<strong>on</strong>trolled Trials (CENTRAL) The Cochrane Library 2009, Issue 1; Ovid MEDLINE - (1950 to February Week 4<br />
2009); Ovid EMBASE - (1980 to 2009 Week 9); and EBSCO CINAHL - (1982 to February Week 4 2009). We also<br />
searched the reference lists of key papers.<br />
Selecti<strong>on</strong> criteria<br />
All randomised trials (RCTs) compar<strong>in</strong>g alcohol based d<strong>on</strong>or sk<strong>in</strong> cleans<strong>in</strong>g <strong>in</strong> a <strong>on</strong>e-step versus a two-step<br />
1 / 15<br />
Annex J: Cochrane review 87
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of ...<br />
process that <strong>in</strong>cludes alcohol and any other antiseptic for pre-venepuncture sk<strong>in</strong> cleans<strong>in</strong>g were c<strong>on</strong>sidered.<br />
Quasi randomised trials were to have been c<strong>on</strong>sidered <strong>in</strong> the absence of RCTs.<br />
Data collecti<strong>on</strong> and analysis<br />
Two review authors <strong>in</strong>dependently assessed studies for <strong>in</strong>clusi<strong>on</strong>.<br />
Ma<strong>in</strong> results<br />
No studies (RCTs or quasi RCTs) met the <strong>in</strong>clusi<strong>on</strong> criteria.<br />
Authors' c<strong>on</strong>clusi<strong>on</strong>s<br />
We did not identify any eligible studies for <strong>in</strong>clusi<strong>on</strong> <strong>in</strong> this review. It is therefore unclear whether a two-step,<br />
alcohol followed by antiseptic sk<strong>in</strong> cleans<strong>in</strong>g process prior to blood d<strong>on</strong>ati<strong>on</strong> c<strong>on</strong>fers any reducti<strong>on</strong> <strong>in</strong> the risk of<br />
blood c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> or bacteraemia <strong>in</strong> blood recipients, or c<strong>on</strong>versely whether a <strong>on</strong>e-step process <strong>in</strong>creases risk<br />
above that associated with a two-step process.<br />
Pla<strong>in</strong> language summary<br />
Alcohol, with or without an antiseptic, for prepar<strong>in</strong>g the sk<strong>in</strong> before blood collecti<strong>on</strong>, to prevent<br />
bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of blood for transfusi<strong>on</strong>.<br />
When blood is collected from blood d<strong>on</strong>ors for transfusi<strong>on</strong> it may become c<strong>on</strong>tam<strong>in</strong>ated dur<strong>in</strong>g collecti<strong>on</strong>,<br />
storage or transfusi<strong>on</strong>. <strong>Blood</strong> c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> can cause bacteraemia (the presence of bacteria <strong>in</strong> the blood),<br />
severe illness or even death <strong>in</strong> the blood recipient. When blood is be<strong>in</strong>g taken from d<strong>on</strong>ors, the sk<strong>in</strong> <strong>on</strong> the arm<br />
of the d<strong>on</strong>or is <strong>on</strong>e potential source of c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong>, so it is usual to cleanse the arm with an antiseptic first,<br />
and both <strong>on</strong>e-step and two-step alcohol based regimens are comm<strong>on</strong>ly used, however there is uncerta<strong>in</strong>ty about<br />
which regimen is the most effective for reduc<strong>in</strong>g the microbial load (the number of microscopic bacterial<br />
organisms) <strong>on</strong> the d<strong>on</strong>or arm. We looked for studies that compared the use of alcohol al<strong>on</strong>e versus the use of<br />
alcohol followed by another antiseptic to clean the arm before the needle is <strong>in</strong>serted to draw blood, but we did<br />
not f<strong>in</strong>d any relevant studies. It is currently unclear whether d<strong>on</strong>or sk<strong>in</strong> cleans<strong>in</strong>g with a <strong>on</strong>e-step alcohol based<br />
regimen reduces the risk of blood c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> compared with a two-step alcohol based regimen dur<strong>in</strong>g blood<br />
d<strong>on</strong>ati<strong>on</strong>.<br />
Background<br />
Complicati<strong>on</strong>s associated with the <strong>in</strong>fusi<strong>on</strong> of blood and blood-related products have reduced <strong>in</strong> recent years,<br />
due to c<strong>on</strong>siderable advances <strong>in</strong> detect<strong>in</strong>g transfusi<strong>on</strong>-related viral pathogens, such as human immunodeficiency<br />
virus (HIV) and hepatitis C and B virus (HCV and HBV). In c<strong>on</strong>trast, bacteraemia, result<strong>in</strong>g from bacterial<br />
c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of blood products c<strong>on</strong>t<strong>in</strong>ues to be an <strong>on</strong>go<strong>in</strong>g problem (Sandler 2003; Wagner 2004). Exogenous<br />
c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of d<strong>on</strong>or blood may occur at any po<strong>in</strong>t dur<strong>in</strong>g collecti<strong>on</strong>, storage and transfusi<strong>on</strong> (McD<strong>on</strong>ald 2001<br />
). One of the sources of c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> is thought to be the d<strong>on</strong>or's sk<strong>in</strong>, as a result of <strong>in</strong>adequate sk<strong>in</strong> cleans<strong>in</strong>g<br />
(de Korte 2006; McD<strong>on</strong>ald 2006).<br />
Descripti<strong>on</strong> of the c<strong>on</strong>diti<strong>on</strong><br />
Bacteraemia, or the presence of bacteria <strong>in</strong> the blood, is a potentially fatal c<strong>on</strong>diti<strong>on</strong>. It is associated with high<br />
rates of morbidity (Hakim 2007; Sligl 2006). Microorganisms may enter the blood stream through almost any<br />
organ (for example the lungs follow<strong>in</strong>g pneum<strong>on</strong>ia), through a surgical site, or via an implanted device such as<br />
an <strong>in</strong>travenous catheter. Prognosis is related to the virulence of the <strong>in</strong>fective organism, severity of the sepsis at<br />
diagnosis and the underly<strong>in</strong>g health of the patient (Herchl<strong>in</strong>e 1997). Although the aetiology of bacteraemia is<br />
often difficult to identify, transfusi<strong>on</strong>-transmitted <strong>in</strong>fecti<strong>on</strong> is a rare cause. The <strong>in</strong>cidence of bacterial<br />
transmissi<strong>on</strong> through d<strong>on</strong>ated blood is estimated at between 1 per 100,000 and 1 per 1,000,000 units for<br />
packed red blood cells, and between 1 per 900 and 1 per 100,000 units for platelets (Walther-Wenke 2008).<br />
Fatalities are associated with 1 <strong>in</strong> 8,000,000 red cell units and 1 <strong>in</strong> 50,000 to 500,000 white cell units (Wagner<br />
2004). The reas<strong>on</strong> for higher rates <strong>in</strong> platelet transfusi<strong>on</strong> is thought to be because frozen platelets are thawed<br />
and stored at room temperature before <strong>in</strong>fusi<strong>on</strong> and if they are not used immediately there is an opportunity for<br />
any organisms that may be present to multiply before the product is transfused. Further reducti<strong>on</strong> of <strong>in</strong>fecti<strong>on</strong><br />
rates depends <strong>on</strong> ensur<strong>in</strong>g that blood for transfusi<strong>on</strong> is free of c<strong>on</strong>tam<strong>in</strong>ants. One way of achiev<strong>in</strong>g this is<br />
through careful preparati<strong>on</strong> and cleans<strong>in</strong>g of the d<strong>on</strong>or's sk<strong>in</strong> at the collecti<strong>on</strong> site.<br />
Descripti<strong>on</strong> of the <strong>in</strong>terventi<strong>on</strong><br />
There is no standard method for cleans<strong>in</strong>g the site <strong>on</strong> the blood d<strong>on</strong>or's sk<strong>in</strong> from which the blood will be taken<br />
(generally the cubital fossa, or the <strong>in</strong>ner aspect of the elbow). However, alcohol, followed by an applicati<strong>on</strong> of<br />
povid<strong>on</strong>e iod<strong>in</strong>e has been traditi<strong>on</strong>ally used (Shahar 1990; Kiyoyama 2009). C<strong>on</strong>sequently, the <strong>in</strong>terventi<strong>on</strong>s of<br />
<strong>in</strong>terest for this review are sk<strong>in</strong> cleans<strong>in</strong>g with alcohol (usually 70% isopropyl alcohol) for sk<strong>in</strong> preparati<strong>on</strong> <strong>in</strong> a<br />
<strong>on</strong>e-step process, compared with a two-step process <strong>in</strong>volv<strong>in</strong>g alcohol followed by povid<strong>on</strong>e iod<strong>in</strong>e or other<br />
antiseptic soluti<strong>on</strong>. Antiseptics are antimicrobial substances that are applied to liv<strong>in</strong>g tissue or sk<strong>in</strong> to reduce the<br />
possibility of <strong>in</strong>fecti<strong>on</strong>, sepsis or putrefacti<strong>on</strong>. They should generally be dist<strong>in</strong>guished from antibiotics that<br />
destroy bacteria with<strong>in</strong> the body, and from dis<strong>in</strong>fectants, which destroy microorganisms found <strong>on</strong> n<strong>on</strong>-liv<strong>in</strong>g<br />
objects. Alcohol is widely used prior to venepuncture and is available from a number of manufacturers as easyto-use<br />
dis<strong>in</strong>fecti<strong>on</strong> wipes. Isopropyl alcohol is a flammable, colourless liquid; also known as 2-propanol (MSDS<br />
2 / 15<br />
88 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of ...<br />
2006).<br />
How the <strong>in</strong>terventi<strong>on</strong> might work<br />
Alcohol kills most bacteria and fungi by act<strong>in</strong>g <strong>on</strong> lipid and prote<strong>in</strong> comp<strong>on</strong>ents of the cell. It is less effective<br />
aga<strong>in</strong>st viruses (Adams 2007). Isopropyl alcohol has some advantages over other products because it requires a<br />
shorter c<strong>on</strong>tact time to achieve antisepsis. For example some two-step procedures take up to two m<strong>in</strong>utes to<br />
perform, which is c<strong>on</strong>sidered too l<strong>on</strong>g for some blood bank services (McD<strong>on</strong>ald 2006). Antiseptics are toxic to<br />
liv<strong>in</strong>g tissues as well as bacterial cells, some antiseptics are true germicides, capable of destroy<strong>in</strong>g microbes<br />
(bacteriocidal), whilst others are bacteriostatic and <strong>on</strong>ly prevent or <strong>in</strong>hibit their growth (Morgan 1993).<br />
Why it is important to do this review<br />
Although a range of antiseptics has been used to cleanse the sk<strong>in</strong> of the d<strong>on</strong>or arm, a two-step process,<br />
<strong>in</strong>clud<strong>in</strong>g alcohol and iod<strong>in</strong>e is widely used (Shahar 1990; Kiyoyama 2009). The effectiveness of this regimen, and<br />
other forms of cleans<strong>in</strong>g has been evaluated <strong>in</strong> a number of studies by measur<strong>in</strong>g the microbial load <strong>on</strong> the<br />
d<strong>on</strong>or arm (Cid 2003; Follea 1997; Goldman 1997; McD<strong>on</strong>ald 2001; W<strong>on</strong>g 2004) and any c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of<br />
platelet c<strong>on</strong>centrates de Korte 2006; Lee 2002) however it rema<strong>in</strong>s unclear whether isopropyl alcohol al<strong>on</strong>e is as<br />
effective as alcohol plus povid<strong>on</strong>e iod<strong>in</strong>e (or any other antiseptic) <strong>in</strong> prevent<strong>in</strong>g the cl<strong>in</strong>ical c<strong>on</strong>sequences of<br />
c<strong>on</strong>tam<strong>in</strong>ated blood. This review questi<strong>on</strong> was brought to us by the World Health Organisati<strong>on</strong> (<str<strong>on</strong>g>WHO</str<strong>on</strong>g>) and a<br />
scop<strong>in</strong>g search did not identify any exist<strong>in</strong>g systematic review which had previously addressed this questi<strong>on</strong>.<br />
Objectives<br />
To assess the effects of cleans<strong>in</strong>g the d<strong>on</strong>or arm with alcohol <strong>in</strong> a <strong>on</strong>e-step regimen compared with a two-step<br />
regimen <strong>in</strong>clud<strong>in</strong>g alcohol followed by any other antiseptic to prevent d<strong>on</strong>or blood c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> or recipient<br />
bacteraemia.<br />
Methods<br />
Criteria for c<strong>on</strong>sider<strong>in</strong>g studies for this review<br />
Types of studies<br />
All randomised c<strong>on</strong>trolled trials (RCTs) compar<strong>in</strong>g a <strong>on</strong>e-step alcohol regimen with any two-step regimen that<br />
<strong>in</strong>cludes alcohol followed by another antiseptic for pre-venepuncture sk<strong>in</strong> cleans<strong>in</strong>g were c<strong>on</strong>sidered. Cluster<br />
randomised trials and crossover trials were also eligible for <strong>in</strong>clusi<strong>on</strong>. Quasi randomised trials were to have been<br />
c<strong>on</strong>sidered <strong>in</strong> the absence of RCTs.<br />
Types of participants<br />
Studies enroll<strong>in</strong>g people of any age and <strong>in</strong> any sett<strong>in</strong>g, hav<strong>in</strong>g venepuncture and blood collecti<strong>on</strong> were eligible,<br />
irrespective of whether the venepuncture was for the purpose of blood d<strong>on</strong>ati<strong>on</strong>. Studies should also <strong>in</strong>clude<br />
follow up from the recipients of the d<strong>on</strong>ated blood <strong>in</strong> order to measure outcomes occurr<strong>in</strong>g <strong>in</strong> the recipient.<br />
Types of <strong>in</strong>terventi<strong>on</strong>s<br />
Studies which compared <strong>on</strong>e-step d<strong>on</strong>or sk<strong>in</strong> cleans<strong>in</strong>g with alcohol (any c<strong>on</strong>centrati<strong>on</strong> or applicati<strong>on</strong> method)<br />
with a two-step method which <strong>in</strong>volved alcohol (any strength or applicati<strong>on</strong> method) followed by any other<br />
antiseptic (any c<strong>on</strong>centrati<strong>on</strong> or applicati<strong>on</strong> method) were eligible.<br />
Types of outcome measures<br />
At least <strong>on</strong>e of the primary outcomes was to have been reported for the study to be c<strong>on</strong>sidered for <strong>in</strong>clusi<strong>on</strong> <strong>in</strong><br />
the review.<br />
Primary outcomes<br />
Bacteraemia <strong>in</strong> the blood recipient (the presence of bacteria <strong>in</strong> the blood stream) as measured by blood<br />
culture.<br />
<strong>Blood</strong> product c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> (blood products <strong>in</strong>clude whole blood, platelets, red blood cells or any other<br />
product derived from the blood collecti<strong>on</strong>) at any time between collecti<strong>on</strong> and transfusi<strong>on</strong> as detected most<br />
comm<strong>on</strong>ly by blood culture.<br />
Proxy outcome measures, such as sk<strong>in</strong> c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> or sk<strong>in</strong> col<strong>on</strong>isati<strong>on</strong>, were not c<strong>on</strong>sidered for several<br />
reas<strong>on</strong>s. Namely, any antiseptic will reduce levels of microflora <strong>on</strong> the sk<strong>in</strong> and swabb<strong>in</strong>g sk<strong>in</strong> for bacteria is<br />
really a 'sampl<strong>in</strong>g procedure' which is subject to <strong>in</strong>c<strong>on</strong>sistencies <strong>in</strong> sampl<strong>in</strong>g. In additi<strong>on</strong>, a positive sk<strong>in</strong> culture<br />
does not automatically mean that the blood collected for transfusi<strong>on</strong> will be positive for bacteria (<strong>in</strong> the same way<br />
that a positive sk<strong>in</strong> culture before surgery does not mean the pers<strong>on</strong> will develop a surgical site <strong>in</strong>fecti<strong>on</strong>).<br />
Sec<strong>on</strong>dary outcomes<br />
Death of the blood recipient, attributed to the transfusi<strong>on</strong>.<br />
Any adverse effects <strong>in</strong> the blood recipient associated with the transfusi<strong>on</strong>. This may <strong>in</strong>clude sepsis (a group<strong>in</strong>g<br />
of signs such as fever, chills, or hypotensi<strong>on</strong>), septic shock (severe disturbances of temperature, respirati<strong>on</strong>,<br />
heart rate or white blood cell count) or multiple organ dysfuncti<strong>on</strong> syndrome (altered organ functi<strong>on</strong> <strong>in</strong> a<br />
severely ill patient that requires medical <strong>in</strong>terventi<strong>on</strong> to prevent death).<br />
3 / 15<br />
Annex J: Cochrane review 89
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of ...<br />
Search methods for identificati<strong>on</strong> of studies<br />
Electr<strong>on</strong>ic searches<br />
We searched the follow<strong>in</strong>g databases:<br />
Cochrane Wounds Group Specialised Register (Searched March 10 2009);<br />
The Cochrane Central Register of C<strong>on</strong>trolled Trials (CENTRAL) -The Cochrane Library 2009, Issue 1;<br />
Ovid MEDLINE - 1950 to February Week 4 2009;<br />
Ovid EMBASE - 1980 to 2009 Week 9;<br />
EBSCO CINAHL - 1982 to February Week 4 2009.<br />
The Cochrane Central Register of C<strong>on</strong>trolled Trials (CENTRAL) was searched us<strong>in</strong>g the follow<strong>in</strong>g strategy:<br />
#1 MeSH descriptor <strong>Blood</strong> Specimen Collecti<strong>on</strong> explode all trees<br />
#2 MeSH descriptor <strong>Blood</strong> Transfusi<strong>on</strong> explode all trees<br />
#3 MeSH descriptor <strong>Blood</strong> D<strong>on</strong>ors explode all trees<br />
#4 (blood NEXT collecti<strong>on</strong>*) or (blood NEXT d<strong>on</strong>or*) or (blood NEXT d<strong>on</strong>ati<strong>on</strong>*):ti,ab,kw<br />
#5 (collecti<strong>on</strong> NEAR/1 blood) or (d<strong>on</strong>ati<strong>on</strong> NEAR/1 blood):ti,ab,kw<br />
#6 ven*puncture NEXT site*:ti,ab,kw<br />
#7 (#1 OR #2 OR #3 OR #4 OR #5 OR #6)<br />
#8 MeSH descriptor Antisepsis explode all trees<br />
#9 MeSH descriptor Anti-Infective Agents, Local explode all trees<br />
#10 MeSH descriptor Iod<strong>in</strong>e Compounds explode all trees<br />
#11 MeSH descriptor Povid<strong>on</strong>e-Iod<strong>in</strong>e explode all trees<br />
#12 MeSH descriptor Alcohols explode all trees<br />
#13 MeSH descriptor Dis<strong>in</strong>fectants explode all trees<br />
#14 MeSH descriptor Dis<strong>in</strong>fecti<strong>on</strong> explode all trees<br />
#15 sk<strong>in</strong> NEXT preparati<strong>on</strong>:ti,ab,kw<br />
#16 dis<strong>in</strong>fect*:ti,ab,kw<br />
#17 (“alcohol” or “alcohols” or iod<strong>in</strong>e or povid<strong>on</strong>e-iod<strong>in</strong>e or chlorhexid<strong>in</strong>e):ti,ab,kw<br />
#18 (#8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17)<br />
#19 (#7 AND #18)<br />
The search strategies for Ovid MEDLINE, Ovid EMBASE and EBSCO CINAHL can be found <strong>in</strong> Appendix 2, Appendix<br />
3 and Appendix 4 respectively. The Ovid MEDLINE search was comb<strong>in</strong>ed with the Cochrane Highly Sensitive<br />
Search Strategy for identify<strong>in</strong>g randomised trials <strong>in</strong> MEDLINE: sensitivity- and precisi<strong>on</strong>-maximiz<strong>in</strong>g versi<strong>on</strong><br />
(2008 revisi<strong>on</strong>) (Lefebvre 2008). The Ovid EMBASE and EBSCO CINAHL searches were comb<strong>in</strong>ed with the trial<br />
filters developed by the Scottish Intercollegiate <str<strong>on</strong>g>Guidel<strong>in</strong>es</str<strong>on</strong>g> Network (SIGN 2008). There was no restricti<strong>on</strong> <strong>on</strong> the<br />
basis of date or language of publicati<strong>on</strong>.<br />
Search<strong>in</strong>g other resources<br />
Reference lists of articles retrieved <strong>in</strong> full were searched.<br />
Data collecti<strong>on</strong> and analysis<br />
Selecti<strong>on</strong> of studies<br />
Titles and abstracts identified through the search process were <strong>in</strong>dependently reviewed by two review authors.<br />
Full reports of all potentially relevant studies were retrieved for further assessment of eligibility based <strong>on</strong> the<br />
<strong>in</strong>clusi<strong>on</strong> criteria. Differences of op<strong>in</strong>i<strong>on</strong> were settled by c<strong>on</strong>sensus or referral to a third review author. There was<br />
no bl<strong>in</strong>d<strong>in</strong>g to study authorship when we did these assessments.<br />
Data extracti<strong>on</strong> and management<br />
We had planned to extract the follow<strong>in</strong>g data, where available (to be extracted by <strong>on</strong>e review author and checked<br />
by a sec<strong>on</strong>d review author):<br />
details of the trial/study (first author, year of publicati<strong>on</strong>, journal, publicati<strong>on</strong> status, period);<br />
sett<strong>in</strong>g and country of study;<br />
source of fund<strong>in</strong>g;<br />
<strong>in</strong>clusi<strong>on</strong> and exclusi<strong>on</strong> criteria;<br />
basel<strong>in</strong>e characteristics of participants (age, sex);<br />
aspects of morbidity of the blood recipients, e.g. predictors of susceptibility to bacteraemia;<br />
number of participants <strong>in</strong> each arm of the trial;<br />
descripti<strong>on</strong> of <strong>in</strong>terventi<strong>on</strong> (type, durati<strong>on</strong>);<br />
descripti<strong>on</strong> of c<strong>on</strong>trol <strong>in</strong>terventi<strong>on</strong> (type, durati<strong>on</strong>);<br />
details and durati<strong>on</strong> of follow up;<br />
primary and sec<strong>on</strong>dary outcomes (by group);<br />
design / methodological quality data as per risk of bias criteria;<br />
unit of randomisati<strong>on</strong> (where relevant);<br />
unit of analysis;<br />
results and primary statistical analysis.<br />
4 / 15<br />
90 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of ...<br />
Assessment of risk of bias <strong>in</strong> <strong>in</strong>cluded studies<br />
Two review authors were to <strong>in</strong>dependently assess study risk of bias us<strong>in</strong>g the Cochrane Collaborati<strong>on</strong> tool (<br />
Higg<strong>in</strong>s 2008a).This tool addresses six specific doma<strong>in</strong>s, namely sequence generati<strong>on</strong>, allocati<strong>on</strong> c<strong>on</strong>cealment,<br />
bl<strong>in</strong>d<strong>in</strong>g, <strong>in</strong>complete outcome data, selective outcome report<strong>in</strong>g and other issues (e.g. co-<strong>in</strong>terventi<strong>on</strong>s)(see<br />
Appendix 1 for details of criteria <strong>on</strong> which the judgements were to have been based). Bl<strong>in</strong>d<strong>in</strong>g and completeness<br />
of outcome data would have been assessed for each outcome separately and we had planned to complete a risk<br />
of bias table for each eligible study.<br />
We planned to c<strong>on</strong>tact <strong>in</strong>vestigators of <strong>in</strong>cluded studies to resolve any ambiguities. We also planned to <strong>in</strong>clude<br />
data from duplicate publicati<strong>on</strong>s <strong>on</strong>ly <strong>on</strong>ce, but to retrieve all publicati<strong>on</strong>s perta<strong>in</strong><strong>in</strong>g to a s<strong>in</strong>gle study to enable<br />
full data extracti<strong>on</strong> and risk of bias quality assessment.<br />
For any eligible study, we planned to present assessment of risk of bias us<strong>in</strong>g a 'risk of bias summary figure',<br />
which presents the judgments <strong>in</strong> a cross-tabulati<strong>on</strong> of study by entry. This display of <strong>in</strong>ternal validity <strong>in</strong>dicates<br />
the weight the reader may give the results of each study.<br />
Measures of treatment effect<br />
For <strong>in</strong>dividual trials, effect measures for categorical outcomes (e.g. rates of bacteraemia) would have <strong>in</strong>cluded<br />
relative risk (RR) with its 95% c<strong>on</strong>fidence <strong>in</strong>terval (CI). For c<strong>on</strong>t<strong>in</strong>uous outcomes, we planned to use the mean<br />
difference (MD) or, if the scale of measurement differed across trials, standardized mean difference (SMD), each<br />
with its 95% CI. For any meta-analyses (see below), for categorical outcomes the typical estimates of RR with their<br />
95% CI would have been calculated; and for c<strong>on</strong>t<strong>in</strong>uous outcomes the weighted mean difference (WMD) or a<br />
summary estimate for SMD, each with its 95% CI, would have been calculated.<br />
We planned to analyse data us<strong>in</strong>g The Cochrane Collaborati<strong>on</strong>'s Review Manager 5 software.<br />
Deal<strong>in</strong>g with miss<strong>in</strong>g data<br />
If outcome data had rema<strong>in</strong>ed miss<strong>in</strong>g despite our attempts to obta<strong>in</strong> complete outcome data from authors, we<br />
would have performed an available-case analysis, based <strong>on</strong> the numbers of patients for whom outcome data<br />
were known. If standard deviati<strong>on</strong>s were miss<strong>in</strong>g, we would have imputed them from other studies or, where<br />
possible, computed them from standard errors us<strong>in</strong>g the formula SD = SE x √¯N , where these were available (<br />
Higg<strong>in</strong>s 2008b).<br />
Assessment of heterogeneity<br />
Heterogeneity would have been assessed visually and by us<strong>in</strong>g the chi-squared statistic with significance be<strong>in</strong>g<br />
set at p < 0.10. In additi<strong>on</strong>, the degree of heterogeneity would have been <strong>in</strong>vestigated by calculat<strong>in</strong>g the I 2<br />
statistic (Deeks 2008). If evidence of significant heterogeneity had been identified (I 2 >50%), we would have<br />
explored potential causes and a random-effects approach to the analysis would have been used if a metaanalysis<br />
had been appropriate.<br />
Assessment of report<strong>in</strong>g biases<br />
Report<strong>in</strong>g bias would have been assessed us<strong>in</strong>g guidel<strong>in</strong>es <strong>in</strong> the Cochrane Handbook for Systematic Reviews of<br />
Interventi<strong>on</strong>s (Sterne 2008).<br />
Data synthesis<br />
Where appropriate, results of comparable trials would have been pooled and the pooled estimate together with<br />
its 95% CI would have been reported. We planned to c<strong>on</strong>duct a narrative review of eligible studies if statistical<br />
synthesis of data from more than <strong>on</strong>e study was not possible or c<strong>on</strong>sidered not appropriate.<br />
Subgroup analysis and <strong>in</strong>vestigati<strong>on</strong> of heterogeneity<br />
We planned to analyse potential sources of heterogeneity us<strong>in</strong>g the follow<strong>in</strong>g subgroup analysis: c<strong>on</strong>cealment of<br />
allocati<strong>on</strong> (adequate versus not reported).<br />
Sensitivity analysis<br />
We planned to undertake a sensitivity analysis to explore the effect of exclud<strong>in</strong>g studies where c<strong>on</strong>cealment of<br />
allocati<strong>on</strong> was unclear<br />
Results<br />
Descripti<strong>on</strong> of studies<br />
We did not f<strong>in</strong>d any randomised or quasi-randomised c<strong>on</strong>trolled trials that met the <strong>in</strong>clusi<strong>on</strong> criteria.<br />
Results of the search<br />
Our <strong>in</strong>itial search identified 457 citati<strong>on</strong>s of which 19 were c<strong>on</strong>sidered potentially relevant. Full copies of these<br />
papers were obta<strong>in</strong>ed and reviewed <strong>in</strong>dependently by two review authors, however, n<strong>on</strong>e met the <strong>in</strong>clusi<strong>on</strong><br />
criteria.<br />
Included studies<br />
5 / 15<br />
Annex J: Cochrane review 91
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of ...<br />
No studies were <strong>in</strong>cluded.<br />
Excluded studies<br />
The Table: Characteristics of excluded studies c<strong>on</strong>ta<strong>in</strong>s reas<strong>on</strong>s for exclud<strong>in</strong>g 19 potentially eligible studies. In<br />
summary, two citati<strong>on</strong>s were for unsystematic literature reviews (Blajchman 2004; Wendel 2002) eight trials did<br />
not compare the eligible <strong>in</strong>terventi<strong>on</strong>s (Calfee 2002; Choudhuri 1990; Little 1999; Mimoz 1999; Schifman 1993;<br />
Sutt<strong>on</strong> 1999; Suwanpimolkul 2008; Trautner 2002). Eight studies were not randomised or quasi randomised<br />
c<strong>on</strong>trolled trials (Kiyoyama 2009; de Korte 2006; Goldman 1997; Lee 2002; McD<strong>on</strong>ald 2006; Pleasant 1994<br />
Shahar 1990; W<strong>on</strong>g 2004). One study exam<strong>in</strong>ed techniques for quantify<strong>in</strong>g bacterial reducti<strong>on</strong> (Follea 1997).<br />
Risk of bias <strong>in</strong> <strong>in</strong>cluded studies<br />
No studies were <strong>in</strong>cluded.<br />
Effects of <strong>in</strong>terventi<strong>on</strong>s<br />
We did not identify any eligible randomised or quasi randomised c<strong>on</strong>trolled trials, nor were we able to identify<br />
any <strong>on</strong>go<strong>in</strong>g trials.<br />
Discussi<strong>on</strong><br />
We have been unable to identify any trials address<strong>in</strong>g the effectiveness of alcohol al<strong>on</strong>e compared with alcohol<br />
followed by any other antiseptic to prevent bacteraemia from transfused blood or blood products. This may be<br />
because <strong>in</strong>fusi<strong>on</strong> related bacteraemia is a relatively rare event and very large trials would be needed to<br />
<strong>in</strong>vestigate the effect of d<strong>on</strong>or-arm cleans<strong>in</strong>g. Sepsis rates for platelet transfusi<strong>on</strong>s are around 1:50,000 and for<br />
red cell transfusi<strong>on</strong>s around 1:500,000 (Sandler 2003). Therefore mount<strong>in</strong>g a trial large enough to detect<br />
differences <strong>in</strong> cl<strong>in</strong>ical outcomes, based <strong>on</strong> products used for arm cleans<strong>in</strong>g, would be prohibitively expensive and<br />
lengthy.<br />
Because of this, surrogate measures, such as c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of stored blood have been used to evaluate<br />
antisepsis efficacy. However, aga<strong>in</strong>, we found no trials that compared alcohol al<strong>on</strong>e with alcohol followed by any<br />
other antiseptic for cleans<strong>in</strong>g the d<strong>on</strong>or sk<strong>in</strong>. A number of studies used the surrogate outcome of post-cleans<strong>in</strong>g<br />
sk<strong>in</strong> microbial load at the venepuncture site however we excluded such studies a priori <strong>on</strong> the grounds that this<br />
is a surrogate outcome of unproven validity; it is not known how sk<strong>in</strong> c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> relates to blood recipient<br />
outcomes. Moreover n<strong>on</strong>e of these trials compared a <strong>on</strong>e-step with a two-step cleans<strong>in</strong>g process (de Korte 2006;<br />
Follea 1997; Goldman 1997).<br />
Whilst we did identify two studies that compared the effects of the eligible <strong>in</strong>terventi<strong>on</strong>s they were otherwise<br />
<strong>in</strong>eligible for important methodological reas<strong>on</strong>s and did not meet our pre-specified study design eligibility<br />
criteria. The first compared blood culture c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> follow<strong>in</strong>g pre-venepuncture cleans<strong>in</strong>g with 70% alcohol<br />
for <strong>on</strong>e m<strong>in</strong>ute followed by povid<strong>on</strong>e iod<strong>in</strong>e soluti<strong>on</strong> for an additi<strong>on</strong>al m<strong>in</strong>ute with brief swabb<strong>in</strong>g of the sk<strong>in</strong><br />
three to five times with 70% alcohol. Patients who were suspected of hav<strong>in</strong>g bacteraemia had two blood samples<br />
taken; <strong>on</strong>ce us<strong>in</strong>g the two-step method and <strong>on</strong>ce with the standard method. Unfortunately it appeared from the<br />
report that the order <strong>in</strong> which the methods were used was not randomised and samples may have been taken<br />
from the same or a closely adjacent site with an unreported time lapse between sampl<strong>in</strong>g. Of the 181 cultures<br />
tested <strong>in</strong> each group, eight (4.4%) were positive <strong>in</strong> the two-step group compared with six (3.3%) <strong>in</strong> the <strong>on</strong>e-step<br />
preparati<strong>on</strong> group (no statistically significant difference) (Shahar 1990). The sec<strong>on</strong>d study potentially suffers<br />
from important selecti<strong>on</strong> bias <strong>in</strong> that the treatment groups were <strong>in</strong> different sett<strong>in</strong>gs as well as receiv<strong>in</strong>g different<br />
modes of sk<strong>in</strong> cleans<strong>in</strong>g and compared blood culture c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> rates between patients <strong>in</strong> whom blood had<br />
been drawn <strong>in</strong> the emergency department and who received a <strong>on</strong>e-step 70% alcohol cleans<strong>in</strong>g with <strong>in</strong>patients<br />
who received a two-step 70% alcohol followed by povid<strong>on</strong>e iod<strong>in</strong>e procedure. Although there was a statistically<br />
significant difference <strong>in</strong> positive culture rates <strong>in</strong> favour of the <strong>on</strong>e step process (189 (6.6%) positive cultures <strong>in</strong><br />
the <strong>on</strong>e-step group versus 248 (8.9%) <strong>in</strong> the two step, alcohol plus iod<strong>in</strong>e group (p = 0.0015) (Kiyoyama 2009)<br />
this study was not eligible for <strong>in</strong>clusi<strong>on</strong> <strong>in</strong> the review due to the <strong>in</strong>herent risk of selecti<strong>on</strong> bias (<strong>in</strong>patients and<br />
emergency department patients may well be at different levels of risk of positive blood culture). Thus whilst the<br />
authors presented additi<strong>on</strong>al data to suggest that basel<strong>in</strong>e positive blood culture rates were similar between<br />
<strong>in</strong>patients and emergency department patients the risk of selecti<strong>on</strong> bias rema<strong>in</strong>s and this study was excluded (<br />
Kiyoyama 2009).<br />
In c<strong>on</strong>clusi<strong>on</strong> there is currently no evidence of a difference <strong>in</strong> either blood c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> or bacteraemia when<br />
d<strong>on</strong>or sk<strong>in</strong> is cleansed pre-venepuncture with a <strong>on</strong>e-step alcohol based process or a two-step alcohol plus<br />
antiseptic process. This lack of evidence for a difference however results from a complete absence of research<br />
and therefore a real difference cannot be discounted. Until better evidence emerges, decisi<strong>on</strong>s about which mode<br />
of pre-blood d<strong>on</strong>ati<strong>on</strong> sk<strong>in</strong> cleans<strong>in</strong>g to use are likely to be driven by c<strong>on</strong>venience and cost. It is also important<br />
to note that arm cleans<strong>in</strong>g is <strong>on</strong>ly <strong>on</strong>e of the po<strong>in</strong>ts at which blood c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> may occur. Careful collecti<strong>on</strong><br />
and storage of blood and blood products, and systematic surveillance to detect bacterial c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> can all<br />
c<strong>on</strong>tribute to the safety of patients requir<strong>in</strong>g blood transfusi<strong>on</strong>s. Elim<strong>in</strong>at<strong>in</strong>g all bacteria from stored blood may<br />
not be possible. So, follow<strong>in</strong>g relevant cl<strong>in</strong>ical guidel<strong>in</strong>es (for example UK BTS <str<strong>on</strong>g>Guidel<strong>in</strong>es</str<strong>on</strong>g> 2005) for collecti<strong>on</strong> and<br />
for detect<strong>in</strong>g bacterial c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> <strong>in</strong> stored blood, both at the time of collecti<strong>on</strong> and at the time of issue, may<br />
be the most effective way of reduc<strong>in</strong>g <strong>in</strong>fusi<strong>on</strong> related bacteraemia (Yomtovian 2006).<br />
Summary of ma<strong>in</strong> results<br />
6 / 15<br />
92 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of ...<br />
We did not identify any eligible studies for <strong>in</strong>clusi<strong>on</strong> <strong>in</strong> this review. It is therefore unclear whether a two-step,<br />
alcohol followed by antiseptic sk<strong>in</strong> cleans<strong>in</strong>g process prior to blood d<strong>on</strong>ati<strong>on</strong> c<strong>on</strong>fers any reducti<strong>on</strong> <strong>in</strong> the risk of<br />
blood c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> or bacteraemia <strong>in</strong> blood recipients (or c<strong>on</strong>versely whether a <strong>on</strong>e-step process <strong>in</strong>creases risk<br />
above that associated with a two-step process).<br />
Potential biases <strong>in</strong> the review process<br />
Biases <strong>in</strong> the review process were m<strong>in</strong>imised as far as possible by adher<strong>in</strong>g to the guidance provided by the<br />
Cochrane Handbook ( Higg<strong>in</strong>s 2008). We believe that publicati<strong>on</strong> bias is unlikely <strong>in</strong> this case; whilst no trials met<br />
the <strong>in</strong>clusi<strong>on</strong> criteria , this is probably due to the difficulty and expense associated with mount<strong>in</strong>g a trial large<br />
enough to answer the questi<strong>on</strong>.<br />
Authors' c<strong>on</strong>clusi<strong>on</strong>s<br />
Implicati<strong>on</strong>s for practice<br />
We did not f<strong>in</strong>d any eligible randomised or quasi randomised c<strong>on</strong>trolled trials. Until further research emerges,<br />
decisi<strong>on</strong>s about which mode of pre-blood d<strong>on</strong>ati<strong>on</strong> sk<strong>in</strong> cleans<strong>in</strong>g to use are likely to be driven by c<strong>on</strong>venience<br />
and cost. It is also important to note that arm cleans<strong>in</strong>g is <strong>on</strong>ly <strong>on</strong>e of the po<strong>in</strong>ts at which blood c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong><br />
may occur.<br />
Implicati<strong>on</strong>s for research<br />
Cleans<strong>in</strong>g the d<strong>on</strong>or sk<strong>in</strong> before tak<strong>in</strong>g blood for transfusi<strong>on</strong> is important, but c<strong>on</strong>duct<strong>in</strong>g a trial to compare the<br />
effects of us<strong>in</strong>g specific antiseptics <strong>on</strong> bacteraemia rates would be logistically difficult given the relatively rare<br />
event rate. It may be possible to estimate the effects of dis<strong>in</strong>fect<strong>in</strong>g with alcohol al<strong>on</strong>e versus alcohol plus other<br />
antiseptics <strong>on</strong> blood c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> rates but this would still require very large sample sizes to detect cl<strong>in</strong>ically<br />
important differences. Alternatively, high quality observati<strong>on</strong>al studies may provide additi<strong>on</strong>al <strong>in</strong>formati<strong>on</strong> to<br />
guide practice. A future comprehensive evidence synthesis that summarised the evidence for all compet<strong>in</strong>g<br />
alternative approaches to pre-blood d<strong>on</strong>ati<strong>on</strong> sk<strong>in</strong> cleans<strong>in</strong>g would be worthwhile.<br />
Acknowledgements<br />
The authors would like to acknowledge the peer referees: Mart<strong>in</strong> Bland, Julie Bruce, Mike Clarke, Jo Dumville,<br />
Carmel Hughes, Susan O'Meara, Ian Roberts and David Tovey. Nicky Cullum provided editorial <strong>in</strong>put throughout<br />
the review process and checked the search results.<br />
C<strong>on</strong>tributi<strong>on</strong>s of authors<br />
Joan Webster: designed the review, checked the search results and all papers retrieved <strong>in</strong> full, wrote the review<br />
draft, resp<strong>on</strong>ded to the peer referee feedback, made an <strong>in</strong>tellectual c<strong>on</strong>tributi<strong>on</strong> to the review and approved the<br />
f<strong>in</strong>al review prior to submissi<strong>on</strong>. Guarantor of the review<br />
Sally Bell-Syer: coord<strong>in</strong>ated the review, edited the review draft, resp<strong>on</strong>ded to the peer referee feedback, made an<br />
<strong>in</strong>tellectual c<strong>on</strong>tributi<strong>on</strong> to the review and approved the f<strong>in</strong>al review prior to submissi<strong>on</strong>.<br />
Ruth Foxlee: designed the search strategy, c<strong>on</strong>ducted the literature searches and retrieved papers. Edited the<br />
search methods secti<strong>on</strong> and resp<strong>on</strong>ded to the peer referee feedback and approved the f<strong>in</strong>al review prior to<br />
submissi<strong>on</strong>.<br />
Declarati<strong>on</strong>s of <strong>in</strong>terest<br />
n<strong>on</strong>e known<br />
Differences between protocol and review<br />
Nil<br />
Published notes<br />
This rapid review was undertaken at the request of the World Health Organisati<strong>on</strong> (<str<strong>on</strong>g>WHO</str<strong>on</strong>g>). This organisati<strong>on</strong><br />
framed the review questi<strong>on</strong> but they did not provide fund<strong>in</strong>g or <strong>in</strong>fluence its publicati<strong>on</strong>.<br />
Characteristics of studies<br />
Characteristics of <strong>in</strong>cluded studies<br />
Footnotes<br />
Characteristics of excluded studies<br />
Blajchman 2004<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
Narrative, n<strong>on</strong>-systematic literature review<br />
Calfee 2002<br />
7 / 15<br />
Annex J: Cochrane review 93
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of ...<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
N<strong>on</strong>e of the four study arms <strong>in</strong>volved a two-step sk<strong>in</strong> preparati<strong>on</strong> process.<br />
Choudhuri 1990<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
Comparis<strong>on</strong> of two <strong>on</strong>e-step processes; alcohol swab compared with iod<strong>in</strong>e<br />
swab.<br />
de Korte 2006<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
S<strong>in</strong>gle arm study evaluat<strong>in</strong>g a double-swab isopropyl alcohol dis<strong>in</strong>fecti<strong>on</strong><br />
process.<br />
Follea 1997<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
Exam<strong>in</strong>ed techniques for quantify<strong>in</strong>g bacterial reducti<strong>on</strong> by compar<strong>in</strong>g a threestep<br />
process with no sk<strong>in</strong> dis<strong>in</strong>fecti<strong>on</strong>.<br />
Goldman 1997<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
Abstract <strong>on</strong>ly available and it was unclear how patients where allocated to<br />
groups. Though this was not likely to have been randomised or quasirandomised<br />
because <strong>on</strong>e group was treated <strong>in</strong> a particular way <strong>on</strong> the basis<br />
that they were allergic to iod<strong>in</strong>e. Also there was no <strong>on</strong>e-step, alcohol-<strong>on</strong>ly sk<strong>in</strong><br />
preparati<strong>on</strong> group.<br />
Kiyoyama 2009<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
Not a randomised or quasi-randomised c<strong>on</strong>trolled trial. Two <strong>in</strong>dependent<br />
groups were c<strong>on</strong>sidered; <strong>on</strong>e group from an <strong>in</strong>patient ward was treated with<br />
isopropyl alcohol + povid<strong>on</strong>e-iod<strong>in</strong>e and the other from an emergency<br />
department was treated with isopropyl alcohol al<strong>on</strong>e.<br />
Lee 2002<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
Not a randomised or quasi-randomised c<strong>on</strong>trolled trial. Comparis<strong>on</strong> of two<br />
two-step processes <strong>in</strong> c<strong>on</strong>secutive time periods. Cetrimide/ chlorhexid<strong>in</strong>e<br />
soluti<strong>on</strong> + isopropyl alcohol compared with povid<strong>on</strong>e-iod<strong>in</strong>e + isopropyl<br />
alcohol.<br />
Little 1999<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
Povid<strong>on</strong>e-iod<strong>in</strong>e was compared with iod<strong>in</strong>e t<strong>in</strong>cture, i.e. not a comparis<strong>on</strong> of a<br />
<strong>on</strong>e-step with a two-step sk<strong>in</strong> preparati<strong>on</strong>.<br />
McD<strong>on</strong>ald 2006<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
An unc<strong>on</strong>trolled before and after evaluati<strong>on</strong> of a two-step process <strong>in</strong>volv<strong>in</strong>g<br />
isopropyl alcohol + t<strong>in</strong>cture of iod<strong>in</strong>e.<br />
Mimoz 1999<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
Povid<strong>on</strong>e-iod<strong>in</strong>e compared with chlorhexid<strong>in</strong>e, i.e. not a comparis<strong>on</strong> of a <strong>on</strong>estep<br />
with a two-step sk<strong>in</strong> preparati<strong>on</strong>.<br />
Pleasant 1994<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
Only available <strong>in</strong> abstract form; no <strong>in</strong>formati<strong>on</strong> to suggest this was a<br />
randomised c<strong>on</strong>trolled trial; attempts to c<strong>on</strong>tact the authors were<br />
unsuccessful.<br />
8 / 15<br />
94 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of ...<br />
Schifman 1993<br />
Reas<strong>on</strong> for exclusi<strong>on</strong> Comparis<strong>on</strong> of two two-step processes, namely, isopropyl alcohol pads +<br />
povid<strong>on</strong>e-iod<strong>in</strong>e swabs compared with isopropyl alcohol/acet<strong>on</strong>e scrub +<br />
povid<strong>on</strong>e-iod<strong>in</strong>e dispenser.<br />
Shahar 1990<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
Not a randomised or quasi-randomised c<strong>on</strong>trolled trial; the venepuncture site<br />
was cleansed with a two-step process after which a culture was taken, at a<br />
later time po<strong>in</strong>t the venepuncture site was cleansed with a <strong>on</strong>e-step process<br />
after which a culture was taken. The two samples were collected from the<br />
same pers<strong>on</strong> but it is not clear from the report if the two venepuncture sites<br />
were different, if there was a possibility of cross c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> between sites<br />
and what time period separated the sampl<strong>in</strong>g process..<br />
Sutt<strong>on</strong> 1999<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
Isopropyl alcohol (IPA) compared with no IPA sk<strong>in</strong> preparati<strong>on</strong>, i.e. not a<br />
comparis<strong>on</strong> of a <strong>on</strong>e-step with a two-step sk<strong>in</strong> preparati<strong>on</strong>.<br />
Suwanpimolkul 2008<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
Chlorhexid<strong>in</strong>e <strong>in</strong> alcohol compared with povid<strong>on</strong>e-iod<strong>in</strong>e, i.e. not a<br />
comparis<strong>on</strong> of a <strong>on</strong>e-step with a two-step sk<strong>in</strong> preparati<strong>on</strong>.<br />
Trautner 2002<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
Chlorhexid<strong>in</strong>e gluc<strong>on</strong>ate compared with iod<strong>in</strong>e t<strong>in</strong>cture, i.e. not a comparis<strong>on</strong><br />
of a <strong>on</strong>e-step with a two-step sk<strong>in</strong> preparati<strong>on</strong> .<br />
Wendel 2002<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
Narrative, n<strong>on</strong>-systematic literature review.<br />
W<strong>on</strong>g 2004<br />
Reas<strong>on</strong> for exclusi<strong>on</strong><br />
An unc<strong>on</strong>trolled before and after study of a <strong>on</strong>e-step process <strong>in</strong>volv<strong>in</strong>g<br />
chlorhexid<strong>in</strong>e gluc<strong>on</strong>ate.<br />
Footnotes<br />
Characteristics of studies await<strong>in</strong>g classificati<strong>on</strong><br />
Footnotes<br />
Characteristics of <strong>on</strong>go<strong>in</strong>g studies<br />
Footnotes<br />
Summary of f<strong>in</strong>d<strong>in</strong>gs tables<br />
Additi<strong>on</strong>al tables<br />
References to studies<br />
Included studies<br />
Excluded studies<br />
Blajchman 2004<br />
Blajchman MA, Goldman M, Baeza F. Improv<strong>in</strong>g the bacteriological safety of platelet transfusi<strong>on</strong>s. Transfusi<strong>on</strong><br />
Medic<strong>in</strong>e Reviews 2004;18(1):11-24.<br />
Calfee 2002<br />
Calfee DP, Farr BM. Comparis<strong>on</strong> of four antiseptic preparati<strong>on</strong>s for sk<strong>in</strong> <strong>in</strong> the preventi<strong>on</strong> of c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of<br />
percutaneously drawn blood cultures: a randomized trial. Journal of Cl<strong>in</strong>ical Microbiology 2002;40(5):1660-5.<br />
9 / 15<br />
Annex J: Cochrane review 95
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of ...<br />
Choudhuri 1990<br />
Choudhuri M, McQueen R, Inoue S, Gord<strong>on</strong> RC. Efficiency of sk<strong>in</strong> sterilizati<strong>on</strong> for a venipuncture with the use of<br />
commercially available alcohol or iod<strong>in</strong>e pads. American Journal of Infecti<strong>on</strong> C<strong>on</strong>trol 1990;18(2):82-5.<br />
de Korte 2006<br />
de Korte D, Curvers J, de Kort WL, Hoekstra T, van der Poel CL, Beckers EA, et al. Effects of sk<strong>in</strong> dis<strong>in</strong>fecti<strong>on</strong><br />
method, deviati<strong>on</strong> bag, and bacterial screen<strong>in</strong>g <strong>on</strong> cl<strong>in</strong>ical safety of platelet transfusi<strong>on</strong>s <strong>in</strong> the Netherlands.<br />
Transfusi<strong>on</strong> 2006;46(3):476-85.<br />
Follea 1997<br />
Folléa G, Sa<strong>in</strong>t-Laurent P, Bigey F, Gayet S, Bientz M, Cazenave JP. Quantitative bacteriological evaluati<strong>on</strong> of a<br />
method for sk<strong>in</strong> dis<strong>in</strong>fecti<strong>on</strong> <strong>in</strong> blood d<strong>on</strong>ors. Transfusi<strong>on</strong> Cl<strong>in</strong>ique et Biologique 1997;4(6):523-31.<br />
Goldman 1997<br />
Goldman M, Roy G, Fréchette N, Décary F, Massicotte L, Delage G. Evaluati<strong>on</strong> of d<strong>on</strong>or sk<strong>in</strong> dis<strong>in</strong>fecti<strong>on</strong> methods.<br />
Transfusi<strong>on</strong> 1997;37(3):309-12.<br />
Kiyoyama 2009<br />
Kiyoyama T, Tokuda Y, Shiiki S, Hachiman T, Shimasaki T, Endo K. Isopropyl alcohol compared with isopropyl<br />
alcohol plus povid<strong>on</strong>e-iod<strong>in</strong>e as sk<strong>in</strong> preparati<strong>on</strong> for preventi<strong>on</strong> of blood culture c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong>. Journal of<br />
Cl<strong>in</strong>ical Microbiology 2009;47(1):54-8.<br />
Lee 2002<br />
Lee CK, Ho PL, Chan NK, Mak A, H<strong>on</strong>g J, L<strong>in</strong> CK. Impact of d<strong>on</strong>or arm sk<strong>in</strong> dis<strong>in</strong>fecti<strong>on</strong> <strong>on</strong> the bacterial<br />
c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> rate of platelet c<strong>on</strong>centrates. Vox Sangu<strong>in</strong>is 2002;83(3):204-8.<br />
Little 1999<br />
Little JR, Murray PR, Traynor PS, Spitznagel E. A randomized trial of povid<strong>on</strong>e-iod<strong>in</strong>e compared with iod<strong>in</strong>e<br />
t<strong>in</strong>cture for venipuncture site dis<strong>in</strong>fecti<strong>on</strong>: effects <strong>on</strong> rates of blood culture c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong>. American Journal of<br />
Medic<strong>in</strong>e 1999;107(2):119-25.<br />
McD<strong>on</strong>ald 2006<br />
McD<strong>on</strong>ald CP. Bacterial risk reducti<strong>on</strong> by improved d<strong>on</strong>or arm dis<strong>in</strong>fecti<strong>on</strong>, diversi<strong>on</strong> and bacterial screen<strong>in</strong>g.<br />
Transfusi<strong>on</strong> Medic<strong>in</strong>e 2006;16(6):381-96.<br />
Mimoz 1999<br />
Mimoz O, Karim A, Mercat A, Cosser<strong>on</strong> M, Falissard B, Parker F, et al. Chlorhexid<strong>in</strong>e compared with povid<strong>on</strong>eiod<strong>in</strong>e<br />
as sk<strong>in</strong> preparati<strong>on</strong> before blood culture. A randomized, c<strong>on</strong>trolled trial. Annals of Internal Medic<strong>in</strong>e<br />
1999;131(11):834-7.<br />
Pleasant 1994<br />
Pleasant H, Mar<strong>in</strong>i J, Stehl<strong>in</strong>g L. Evaluati<strong>on</strong> of three sk<strong>in</strong> preps for use prior to phlebotomy. Tranfusi<strong>on</strong><br />
1994;34(Supp):14S.<br />
Schifman 1993<br />
Schifman RB, P<strong>in</strong>dur A. The effect of sk<strong>in</strong> dis<strong>in</strong>fecti<strong>on</strong> materials <strong>on</strong> reduc<strong>in</strong>g blood culture c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong>.<br />
American Journal of Cl<strong>in</strong>ical Pathology 1993;99(5):536-8.<br />
Shahar 1990<br />
Shahar E, Wohl-Gottesman BS, Shenkman L. C<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of blood cultures dur<strong>in</strong>g venepuncture: fact or myth<br />
Postgraduate Medical Journal 1990;66(782):1053-8.<br />
Sutt<strong>on</strong> 1999<br />
Sutt<strong>on</strong> CD, White SA, Edwards R, Lewis MH. A prospective c<strong>on</strong>trolled trial of the efficacy of isopropyl alcohol<br />
wipes before venesecti<strong>on</strong> <strong>in</strong> surgical patients. Annals of the Royal Collegeof Surge<strong>on</strong>s of England<br />
1999;81(3):183-6.<br />
Suwanpimolkul 2008<br />
Suwanpimolkul G, P<strong>on</strong>gkumpai M, Suankratay C. A randomized trial of 2% chlorhexid<strong>in</strong>e t<strong>in</strong>cture compared with<br />
10% aqueous povid<strong>on</strong>e-iod<strong>in</strong>e for venipuncture site dis<strong>in</strong>fecti<strong>on</strong>: Effects <strong>on</strong> blood culture c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> rates.<br />
The Journal of Infecti<strong>on</strong> 2008;56(5):354-9.<br />
Trautner 2002<br />
Trautner BW, Clarridge JE, Darouiche RO. Sk<strong>in</strong> antisepsis kits c<strong>on</strong>ta<strong>in</strong><strong>in</strong>g alcohol and chlorhexid<strong>in</strong>e gluc<strong>on</strong>ate or<br />
t<strong>in</strong>cture of iod<strong>in</strong>e are associated with low rates of blood culture c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong>. Infecti<strong>on</strong> C<strong>on</strong>trol and Hospital<br />
Epidemiology 2002;23(7):397-401.<br />
10 / 15<br />
96 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of ...<br />
Wendel 2002<br />
Wendel S. Chemoprophylaxis of transfusi<strong>on</strong>-transmitted agents <strong>in</strong> labile blood comp<strong>on</strong>ents. Revista da Sociedade<br />
Brasileira de Medic<strong>in</strong>a Tropical 2002;35(4):275-81.<br />
W<strong>on</strong>g 2004<br />
W<strong>on</strong>g P-Y, Colville VL, White V, Walker HM, Morris RA. Validati<strong>on</strong> and assessment of a blood-d<strong>on</strong>or arm<br />
dis<strong>in</strong>fectant c<strong>on</strong>ta<strong>in</strong><strong>in</strong>g chlorhexid<strong>in</strong>e and alcohol. Transfusi<strong>on</strong> 2004;44(8):1238-42.<br />
Studies await<strong>in</strong>g classificati<strong>on</strong><br />
Ongo<strong>in</strong>g studies<br />
Other references<br />
Additi<strong>on</strong>al references<br />
Adams 2007<br />
Adams D, Elliot TS. Sk<strong>in</strong> antiseptics used prior to <strong>in</strong>travascular catheter <strong>in</strong>serti<strong>on</strong>. British Journal of Nurs<strong>in</strong>g<br />
2007;16(5):278-80.<br />
Cid 2003<br />
Cid J, Ortín X, Ardanuy C, C<strong>on</strong>treras E, Elies E, Martín-Vega C. Bacterial persistence <strong>on</strong> blood d<strong>on</strong>ors' arms after<br />
phlebotomy site preparati<strong>on</strong>: analysis of risk factors. Haematologica 2003;88(7):839-40.<br />
Deeks 2008<br />
Deeks, JJ , Higg<strong>in</strong>s JPT, Altman DG <strong>on</strong> behalf of the Cochrane Statistical Methods Group and the Cochrane Bias<br />
Methods Group (Editors). Chapter 9: Analys<strong>in</strong>g data and undertak<strong>in</strong>g meta-analyses. In: Higg<strong>in</strong>s JPT, Green S<br />
(editors), Cochrane Handbook for Systematic Reviews of Interventi<strong>on</strong>s Versi<strong>on</strong> 5.0.0 (updated February 2008).The<br />
Cochrane Collaborati<strong>on</strong>, 2008. Available from www.cochrane-handbook.org.<br />
Hakim 2007<br />
Hakim H, Mylotte JM, Faden H. Morbidity and mortality of Staphylococcal bacteremia <strong>in</strong> children. Americal Journal<br />
of Infecti<strong>on</strong> C<strong>on</strong>trol 2007;35(2):102-5.<br />
Herchl<strong>in</strong>e 1997<br />
Herchl<strong>in</strong>e T, Gros S. Improv<strong>in</strong>g cl<strong>in</strong>ical outcome <strong>in</strong> bacteremia. Journal of Evaluati<strong>on</strong> <strong>in</strong> Cl<strong>in</strong>ical Practice<br />
1997;4(3):191-5.<br />
Higg<strong>in</strong>s 2008<br />
Higg<strong>in</strong>s JPT, Green S (editors) . Cochrane Handbook for Systematic Reviews of Interventi<strong>on</strong>s Versi<strong>on</strong> 5.0.1 (<br />
updated September 2008 ) . The Cochrane Collaborati<strong>on</strong>. Available from www.cochrane-handbook.org , 2008 .<br />
Higg<strong>in</strong>s 2008a<br />
Higg<strong>in</strong>s JPT, Altman DG <strong>on</strong> behalf of the Cochrane Statistical Methods Group and the Cochrane Bias Methods<br />
Group (Editors). Chapter 8: Assess<strong>in</strong>g risk of bias <strong>in</strong> <strong>in</strong>cluded studies. In: Higg<strong>in</strong>s JPT, Green S (editors), Cochrane<br />
Handbook for Systematic Reviews of Interventi<strong>on</strong>s Versi<strong>on</strong> 5.0.0 (updated February 2008).The Cochrane<br />
Collaborati<strong>on</strong>, 2008. Available from www.cochrane-handbook.org.<br />
Higg<strong>in</strong>s 2008b<br />
Higg<strong>in</strong>s JPT, Deeks JJ, Altman DG <strong>on</strong> behalf of the Cochrane Statistical Methods Group and the Cochrane Bias<br />
Methods Group (Editors). Chapter 16: Special topics <strong>in</strong> statistics. Higg<strong>in</strong>s JPT, Green S (editors), Cochrane<br />
Handbook for Systematic Reviews of Interventi<strong>on</strong>s Versi<strong>on</strong> 5.0.0 (updated February 2008).The Cochrane<br />
Collaborati<strong>on</strong>, 2008. Available from www.cochrane-handbook.org.<br />
Lefebvre 2008<br />
Lefebvre C, Manheimer E, Glanville J. Chapter 6: Search<strong>in</strong>g for studies. In: Higg<strong>in</strong>s JPT, Green S (editors). Cochrane<br />
Handbook for Systematic Reviews of Interventi<strong>on</strong>s Versi<strong>on</strong> 5.0.0 (updated February 2008). The Cochrane<br />
Collaborati<strong>on</strong>, 2008. Available from www.cochrane-handbook.org.<br />
McD<strong>on</strong>ald 2001<br />
McD<strong>on</strong>ald CP, Lowe P, Roy A, Robb<strong>in</strong>s S, Hartley S, Harris<strong>on</strong> JF, et al. Evaluati<strong>on</strong> of d<strong>on</strong>or arm dis<strong>in</strong>fecti<strong>on</strong><br />
techniques. Vox Sangu<strong>in</strong>is 2001;80(3):135-41.<br />
Morgan 1993<br />
Morgan D . Is there still a role for antiseptics . Journal of Tissue Viability 1993 ; 3 : 80-4 .<br />
MSDS 2006<br />
Material Safety Data Sheet (MSDS). Safety data for 2-propanol. http://msds.chem.ox.ac.uk/PR/2-propanol.html<br />
2006.<br />
11 / 15<br />
Annex J: Cochrane review 97
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of ...<br />
Sandler 2003<br />
Sandler SG, Yu H, Rassai N. Risks of blood transfusi<strong>on</strong> and their preventi<strong>on</strong>. Cl<strong>in</strong>ical Advances <strong>in</strong> Hematology and<br />
Oncology 2003;1(5):307-13.<br />
SIGN 2008<br />
Scottish Intercollegiate <str<strong>on</strong>g>Guidel<strong>in</strong>es</str<strong>on</strong>g> Network (SIGN). Search filters.<br />
http://www.sign.ac.uk/methodology/filters.html#random accessed 2 June 2008).<br />
Sligl 2006<br />
Sligl W, Taylor G, Br<strong>in</strong>dley PG. Five years of nosocomial Gram-negative bacteremia <strong>in</strong> a general <strong>in</strong>tensive care<br />
unit: epidemiology, antimicrobial susceptibility patterns, and outcomes. Internati<strong>on</strong>al Journal of Infectious<br />
Diseases 2006;10(4):320-5.<br />
Sterne 2008<br />
Sterne JAC, Egger M, Moher D <strong>on</strong> behalf of the Cochrane Bias Methods Group (Editors). Chapter 10: Address<strong>in</strong>g<br />
report<strong>in</strong>g biases. In: Higg<strong>in</strong>s JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventi<strong>on</strong>s<br />
Versi<strong>on</strong> 5.0.0 (updated February 2008).The Cochrane Collaborati<strong>on</strong>, 2008. Available from www.cochranehandbook.org.<br />
UK BTS <str<strong>on</strong>g>Guidel<strong>in</strong>es</str<strong>on</strong>g> 2005<br />
Virge James (Editor). Collecti<strong>on</strong> of a blood d<strong>on</strong>ati<strong>on</strong>. In: <str<strong>on</strong>g>Guidel<strong>in</strong>es</str<strong>on</strong>g> for the <strong>Blood</strong> Transfusi<strong>on</strong> Services <strong>in</strong> the<br />
United K<strong>in</strong>gdom. 7th editi<strong>on</strong>. L<strong>on</strong>d<strong>on</strong>: TSO (The Stati<strong>on</strong>ery Office), 2005:33-39.<br />
Wagner 2004<br />
Wagner SJ. Transfusi<strong>on</strong>-transmitted bacterial <strong>in</strong>fecti<strong>on</strong>: risks, sources and <strong>in</strong>terventi<strong>on</strong>s. Vox Sangu<strong>in</strong>is<br />
2004;86(3):157-63.<br />
Walther-Wenke 2008<br />
Walther-Wenke G. Incidence of bacterial transmissi<strong>on</strong> and transfusi<strong>on</strong> reacti<strong>on</strong>s by blood comp<strong>on</strong>ents. Cl<strong>in</strong>ical<br />
Chemistry and Laboratory Medic<strong>in</strong>e 2008;46(7):919-25.<br />
Yomtovian 2006<br />
Yomtovian RA, Palavec<strong>in</strong>o EL, Dysktra AH, Downes KA, Morrissey AM, Bajaksouzian S, et al. Evoluti<strong>on</strong> of<br />
surveillance methods for detecti<strong>on</strong> of bacterial c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of platelets <strong>in</strong> a university hospital, 1991 through<br />
2004. Transfusi<strong>on</strong> 2006;46(5):719-30.<br />
Other published versi<strong>on</strong>s of this review<br />
Classificati<strong>on</strong> pend<strong>in</strong>g references<br />
Data and analyses<br />
Figures<br />
Sources of support<br />
Internal sources<br />
Department of Health Sciences, University of York, UK<br />
External sources<br />
No sources of support provided<br />
Feedback<br />
Appendices<br />
1 Criteria for a judgment of 'yes' for the sources of bias<br />
1. Was the allocati<strong>on</strong> sequence randomly generated<br />
Yes, low risk of bias<br />
A random (unpredictable) assignment sequence.<br />
Examples of adequate methods of sequence generati<strong>on</strong> are computer-generated random sequence, co<strong>in</strong> toss (for<br />
studies with two groups), roll<strong>in</strong>g a dice (for studies with two or more groups), draw<strong>in</strong>g of balls of different<br />
colours, deal<strong>in</strong>g previously shuffled cards.<br />
No, high risk of bias<br />
- Quasi-randomised approach: Examples of <strong>in</strong>adequate methods are: alternati<strong>on</strong>, birth date, social<br />
<strong>in</strong>surance/security number, date <strong>in</strong> which they are <strong>in</strong>vited to participate <strong>in</strong> the study, and hospital registrati<strong>on</strong><br />
number<br />
- N<strong>on</strong>-random approaches: Allocati<strong>on</strong> by judgement of the cl<strong>in</strong>ician; by preference of the participant; based <strong>on</strong><br />
12 / 15<br />
98 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of ...<br />
the results of a laboratory test or a series of tests; by availability of the <strong>in</strong>terventi<strong>on</strong>.<br />
Unclear<br />
Insufficient <strong>in</strong>formati<strong>on</strong> about the sequence generati<strong>on</strong> process to permit judgement<br />
2. Was the treatment allocati<strong>on</strong> adequately c<strong>on</strong>cealed<br />
Yes, low risk of bias<br />
Assignment must be generated <strong>in</strong>dependently by a pers<strong>on</strong> not resp<strong>on</strong>sible for determ<strong>in</strong><strong>in</strong>g the eligibility of the<br />
participants. This pers<strong>on</strong> has no <strong>in</strong>formati<strong>on</strong> about the pers<strong>on</strong>s <strong>in</strong>cluded <strong>in</strong> the trial and has no <strong>in</strong>fluence <strong>on</strong> the<br />
assignment sequence or <strong>on</strong> the decisi<strong>on</strong> about whether the pers<strong>on</strong> is eligible to enter the trial. Examples of<br />
adequate methods of allocati<strong>on</strong> c<strong>on</strong>cealment are: Central allocati<strong>on</strong>, <strong>in</strong>clud<strong>in</strong>g teleph<strong>on</strong>e, web-based, and<br />
pharmacy c<strong>on</strong>trolled,randomisati<strong>on</strong>; sequentially numbered drug c<strong>on</strong>ta<strong>in</strong>ers of identical appearance; sequentially<br />
numbered, opaque, sealed envelopes.<br />
No, high risk of bias<br />
Examples of <strong>in</strong>adequate methods of allocati<strong>on</strong> c<strong>on</strong>cealment are: alternate medical record numbers, unsealed<br />
envelopes; date of birth; case record number; alternati<strong>on</strong> or rotati<strong>on</strong>; an open list of random numbers any<br />
<strong>in</strong>formati<strong>on</strong> <strong>in</strong> the study that <strong>in</strong>dicated that <strong>in</strong>vestigators or participants could <strong>in</strong>fluence the <strong>in</strong>terventi<strong>on</strong> group.<br />
Unclear<br />
Randomisati<strong>on</strong> stated but no <strong>in</strong>formati<strong>on</strong> <strong>on</strong> method of allocati<strong>on</strong> used is available.<br />
3. Bl<strong>in</strong>d<strong>in</strong>g was knowledge of the allocated <strong>in</strong>terventi<strong>on</strong>s adequately prevented dur<strong>in</strong>g the study<br />
Was the participant bl<strong>in</strong>ded to the <strong>in</strong>terventi<strong>on</strong><br />
Yes, low risk of bias<br />
The treatment and c<strong>on</strong>trol groups are <strong>in</strong>dist<strong>in</strong>guishable for the participants or if the participant was described as<br />
bl<strong>in</strong>ded and the method of bl<strong>in</strong>d<strong>in</strong>g was described.<br />
No, high risk of bias<br />
- Bl<strong>in</strong>d<strong>in</strong>g of study participants attempted, but likely that the bl<strong>in</strong>d<strong>in</strong>g could have been broken; participants<br />
were not bl<strong>in</strong>ded, and the n<strong>on</strong>bl<strong>in</strong>d<strong>in</strong>g of others likely to <strong>in</strong>troduce bias.<br />
Unclear<br />
Was the care provider bl<strong>in</strong>ded to the <strong>in</strong>terventi<strong>on</strong><br />
Yes, low risk of bias<br />
The treatment and c<strong>on</strong>trol groups are <strong>in</strong>dist<strong>in</strong>guishable for the care/treatment providers or if the care provider<br />
was described as bl<strong>in</strong>ded and the method of bl<strong>in</strong>d<strong>in</strong>g was described.<br />
No, high risk of bias<br />
Bl<strong>in</strong>d<strong>in</strong>g of care/treatment providers attempted, but likely that the bl<strong>in</strong>d<strong>in</strong>g could have been broken;<br />
care/treatment providers were not bl<strong>in</strong>ded, and the n<strong>on</strong>bl<strong>in</strong>d<strong>in</strong>g of others likely to <strong>in</strong>troduce bias.<br />
Unclear<br />
Was the outcome assessor bl<strong>in</strong>ded to the <strong>in</strong>terventi<strong>on</strong><br />
Yes, low risk of bias<br />
Adequacy of bl<strong>in</strong>d<strong>in</strong>g should be assessed for the primary outcomes. The outcome assessor was described as<br />
bl<strong>in</strong>ded and the method of bl<strong>in</strong>d<strong>in</strong>g was described.<br />
No, high risk of bias<br />
No bl<strong>in</strong>d<strong>in</strong>g or <strong>in</strong>complete bl<strong>in</strong>d<strong>in</strong>g, and the outcome or outcome measurement is likely to be <strong>in</strong>fluenced by lack<br />
of bl<strong>in</strong>d<strong>in</strong>g<br />
Unclear<br />
4. Were <strong>in</strong>complete outcome data adequately addressed<br />
Was the drop-out rate described and acceptable<br />
The number of participants who were <strong>in</strong>cluded <strong>in</strong> the study but did not complete the observati<strong>on</strong> period or were<br />
not <strong>in</strong>cluded <strong>in</strong> the analysis must be described and reas<strong>on</strong>s given.<br />
Yes, low risk of bias<br />
If the percentage of withdrawals and drop-outs does not exceed 20% for short-term follow-up and 30% for l<strong>on</strong>gterm<br />
follow-up and does not lead to substantial bias. (N.B. these percentages are arbitrary, not supported by<br />
literature);<br />
No miss<strong>in</strong>g outcome data;<br />
Reas<strong>on</strong>s for miss<strong>in</strong>g outcome data unlikely to be related to true outcome (for survival data, censor<strong>in</strong>g unlikely to<br />
be <strong>in</strong>troduc<strong>in</strong>g bias);<br />
Miss<strong>in</strong>g outcome data balanced <strong>in</strong> numbers across <strong>in</strong>terventi<strong>on</strong> groups, with similar reas<strong>on</strong>s for miss<strong>in</strong>g data<br />
across groups;<br />
Miss<strong>in</strong>g data have been imputed us<strong>in</strong>g appropriate methods.<br />
No, high risk of bias<br />
13 / 15<br />
Annex J: Cochrane review 99
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of ...<br />
Reas<strong>on</strong> for miss<strong>in</strong>g outcome data likely to be related to true outcome, with either imbalance <strong>in</strong> numbers or<br />
reas<strong>on</strong>s for miss<strong>in</strong>g data across <strong>in</strong>terventi<strong>on</strong> groups;<br />
Unclear<br />
Were all randomised participants analysed <strong>in</strong> the group to which they were allocated (ITT analysis)<br />
Yes, low risk of bias<br />
Specifically reported by authors that ITT was undertaken and this was c<strong>on</strong>firmed <strong>on</strong> study assessment, or not<br />
stated but evident from study assessment that all randomised participants are reported/analysed <strong>in</strong> the group<br />
they were allocated to for the most important time po<strong>in</strong>t of outcome measurement (m<strong>in</strong>us miss<strong>in</strong>g values)<br />
irrespective of n<strong>on</strong>-compliance and co-<strong>in</strong>terventi<strong>on</strong>s.<br />
No, high risk of bias<br />
Lack of ITT c<strong>on</strong>firmed <strong>on</strong> study assessment (patients who were randomised were not <strong>in</strong>cluded <strong>in</strong> the analysis<br />
because they did not receive the study <strong>in</strong>terventi<strong>on</strong>, they withdrew from the study or were not <strong>in</strong>cluded because<br />
of protocol violati<strong>on</strong>) regardless of whether ITT reported or not<br />
‘As-treated’ analysis d<strong>on</strong>e with substantial departure of the <strong>in</strong>terventi<strong>on</strong> received from that assigned at<br />
randomisati<strong>on</strong>; potentially <strong>in</strong>appropriate applicati<strong>on</strong> of simple imputati<strong>on</strong>.<br />
Unclear<br />
Described as ITT analysis, but unable to c<strong>on</strong>firm <strong>on</strong> study assessment, or not reported and unable to c<strong>on</strong>firm by<br />
study assessment.<br />
5. Are reports of the study free of suggesti<strong>on</strong> of selective outcome report<strong>in</strong>g<br />
Yes, low risk of bias<br />
If all the results from all pre-specified outcomes have been adequately reported <strong>in</strong> the published report of the<br />
trial. This <strong>in</strong>formati<strong>on</strong> is either obta<strong>in</strong>ed by compar<strong>in</strong>g the protocol and the f<strong>in</strong>al trial report, or <strong>in</strong> the absence of<br />
the protocol, assess<strong>in</strong>g that the published report <strong>in</strong>cludes enough <strong>in</strong>formati<strong>on</strong> to make this judgment.<br />
Alternatively a judgement could be made if the trial report lists the outcomes of <strong>in</strong>terest <strong>in</strong> the methods of the<br />
trial and then reports all these outcomes <strong>in</strong> the results secti<strong>on</strong> of the trial report.<br />
No, high risk of bias<br />
Not all of the study’s pre-specified primary outcomes have been reported;<br />
One or more primary outcomes is reported us<strong>in</strong>g measurements, analysis methods or subsets of the data (e.g.<br />
sub scales) that were not prespecified;<br />
One or more reported primary outcomes were not pre-specified (unless clear justificati<strong>on</strong> for their report<strong>in</strong>g is<br />
provided, such as an unexpected adverse effect);<br />
One or more outcomes of <strong>in</strong>terest <strong>in</strong> the review are reported <strong>in</strong>completely so that they cannot be entered <strong>in</strong> a<br />
meta-analysis;<br />
The study report fails to <strong>in</strong>clude results for a key outcome that would be expected to have been reported for such<br />
a study.<br />
Unclear<br />
6. Other sources of potential bias:<br />
Were co-<strong>in</strong>terventi<strong>on</strong>s avoided or similar<br />
There were no co-<strong>in</strong>terventi<strong>on</strong>s or there were co-<strong>in</strong>terventi<strong>on</strong>s but they were similar between the treatment and<br />
c<strong>on</strong>trol groups.<br />
Was the compliance acceptable <strong>in</strong> all groups<br />
The review author determ<strong>in</strong>es if the compliance with the <strong>in</strong>terventi<strong>on</strong>s is acceptable, based <strong>on</strong> the reported<br />
<strong>in</strong>tensity, durati<strong>on</strong>, number and frequency of sessi<strong>on</strong>s for both the treatment <strong>in</strong>terventi<strong>on</strong> and c<strong>on</strong>trol<br />
<strong>in</strong>terventi<strong>on</strong>(s). For example, ultrasound treatment is usually adm<strong>in</strong>istered over several sessi<strong>on</strong>s; therefore it is<br />
necessary to assess how many sessi<strong>on</strong>s each participant attended or if participants completed the course of an<br />
oral drug therapy. For s<strong>in</strong>gle-sessi<strong>on</strong> <strong>in</strong>terventi<strong>on</strong>s (for example: surgery), this item is irrelevant.<br />
2 Ovid MEDLINE search strategy<br />
1 exp <strong>Blood</strong> Specimen Collecti<strong>on</strong>/<br />
2 exp <strong>Blood</strong> Transfusi<strong>on</strong>/<br />
3 exp <strong>Blood</strong> D<strong>on</strong>ors/<br />
4 (blood collecti<strong>on</strong>$ or blood d<strong>on</strong>or$ or blood d<strong>on</strong>ati<strong>on</strong>$).ti,ab.<br />
5 ((collect$ adj1 blood) or (d<strong>on</strong>at$ adj1 blood)).ti,ab.<br />
6 venpuncture site$.ti,ab.<br />
7 or/1-6<br />
8 exp Antisepsis/<br />
9 exp Anti-Infective Agents, Local/<br />
10 exp Iod<strong>in</strong>e Compounds/<br />
11 exp Povid<strong>on</strong>e-Iod<strong>in</strong>e/<br />
12 exp Alcohols/<br />
14 / 15<br />
100 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of ...<br />
13 exp Dis<strong>in</strong>fectants/<br />
14 exp Dis<strong>in</strong>fecti<strong>on</strong>/<br />
15 sk<strong>in</strong> preparati<strong>on</strong>.ti,ab.<br />
16 dis<strong>in</strong>fect$.ti,ab.<br />
17 (alcohol$1 or iod<strong>in</strong>e or povid<strong>on</strong>e-iod<strong>in</strong>e or chlorhexid<strong>in</strong>e).ti,ab.<br />
18 or/8-17<br />
19 7 and 18<br />
3 Ovid EMBASE search strategy<br />
1 exp <strong>Blood</strong> Sampl<strong>in</strong>g/<br />
2 exp <strong>Blood</strong> Transfusi<strong>on</strong>/<br />
3 exp <strong>Blood</strong> D<strong>on</strong>or/<br />
4 (blood collecti<strong>on</strong>$ or blood d<strong>on</strong>or$ or blood d<strong>on</strong>ati<strong>on</strong>$).ti,ab.<br />
5 ((collect$ adj1 blood) or (d<strong>on</strong>at$ adj1 blood)).ti,ab.<br />
6 exp Ve<strong>in</strong> Puncture/<br />
7 venpuncture site$.ti,ab.<br />
8 or/1-7<br />
9 exp Antisepsis/<br />
10 exp Topical Anti<strong>in</strong>fective Agent/<br />
11 exp Iod<strong>in</strong>e/<br />
12 exp Povid<strong>on</strong>e Iod<strong>in</strong>e/<br />
13 exp Chlorhexid<strong>in</strong>e/<br />
14 exp Alcohol/<br />
15 exp Dis<strong>in</strong>fectant Agent/<br />
16 exp Dis<strong>in</strong>fecti<strong>on</strong>/<br />
17 sk<strong>in</strong> preparati<strong>on</strong>.ti,ab.<br />
18 dis<strong>in</strong>fect$.ti,ab.<br />
19 (alcohol$1 or iod<strong>in</strong>e or povid<strong>on</strong>e-iod<strong>in</strong>e or chlorhexid<strong>in</strong>e).ti,ab.<br />
20 or/9-19<br />
21 8 and 20<br />
4 EBSCO CINAHL search strategy<br />
S19 S9 and S18<br />
S18 S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17<br />
S17 TI ( alcohol or alcohols or iod<strong>in</strong>e or povid<strong>on</strong>e-iod<strong>in</strong>e or chlorhexid<strong>in</strong>e ) or AB ( alcohol or alcohols or iod<strong>in</strong>e<br />
or povid<strong>on</strong>e-iod<strong>in</strong>e or chlorhexid<strong>in</strong>e )<br />
S16 TI dis<strong>in</strong>fect* or AB dis<strong>in</strong>fect*<br />
S15 TI sk<strong>in</strong> preparati<strong>on</strong> or AB sk<strong>in</strong> preparati<strong>on</strong><br />
S14 (MH "Dis<strong>in</strong>fectants")<br />
S13 (MH "Alcohols+")<br />
S12 (MH "Povid<strong>on</strong>e-Iod<strong>in</strong>e")<br />
S11 (MH "Iod<strong>in</strong>e")<br />
S10 (MH "Anti<strong>in</strong>fective Agents, Local+")<br />
S9 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8<br />
S8 TI venepuncture site* or AB venepuncture site*<br />
S7 (MH "Venipuncture+")<br />
S6 TI blood d<strong>on</strong>ati<strong>on</strong>* or AB blood d<strong>on</strong>ati<strong>on</strong>*<br />
S5 TI blood d<strong>on</strong>or* or AB blood d<strong>on</strong>or*<br />
S4 TI blood collecti<strong>on</strong>* or AB blood collecti<strong>on</strong>*<br />
S3 (MH "<strong>Blood</strong> D<strong>on</strong>ors")<br />
S2 (MH "<strong>Blood</strong> Transfusi<strong>on</strong>+")<br />
S1 (MH "<strong>Blood</strong> Specimen Collecti<strong>on</strong>+")<br />
15 / 15<br />
Annex J: Cochrane review 101
Annex references<br />
1 Webster J, Bell-Syer S, Foxlee R. Sk<strong>in</strong> preparati<strong>on</strong> with alcohol versus alcohol followed<br />
by any antiseptic for prevent<strong>in</strong>g bacteraemia or c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong> of blood for transfusi<strong>on</strong>.<br />
Cochrane Database of Systematic Reviews, 2009, Issue 3. Art. No.: CD007948. DOI:<br />
10.1002/14651858.CD007948.<br />
http://mrw.<strong>in</strong>terscience.wiley.com/cochrane/clsysrev/articles/CD007948/frame.html<br />
2 Revised <strong>in</strong>jecti<strong>on</strong> safety assessment tool (tool C revised). Geneva, World Health<br />
Organizati<strong>on</strong>, 2008.<br />
http://www.who.<strong>in</strong>t/<strong>in</strong>jecti<strong>on</strong>_safety/en<br />
3 Sacar S et al. Poor hospital <strong>in</strong>fecti<strong>on</strong> c<strong>on</strong>trol practice <strong>in</strong> hand hygiene, glove utilizati<strong>on</strong>, and<br />
usage of tourniquets. American Journal of Infecti<strong>on</strong> C<strong>on</strong>trol, 2006, 34(9):606–609.<br />
4 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> hand hygiene <strong>in</strong> healthcare. Geneva, World Health Organizati<strong>on</strong>, 2009.<br />
http://whqlibdoc.who.<strong>in</strong>t/publicati<strong>on</strong>s/2009/9789241597906_eng.pdf<br />
5 Centers for Disease C<strong>on</strong>trol and Preventi<strong>on</strong>. Transmissi<strong>on</strong> of hepatitis B virus am<strong>on</strong>g pers<strong>on</strong>s<br />
undergo<strong>in</strong>g blood glucose m<strong>on</strong>itor<strong>in</strong>g <strong>in</strong> l<strong>on</strong>g-term care facilities – Mississippi, North<br />
Carol<strong>in</strong>a and Los Angeles County, California, 2003–2004. Morbidity and Mortality Weekly<br />
Report, 2004, 54:220–223.<br />
6 <str<strong>on</strong>g>Guidel<strong>in</strong>es</str<strong>on</strong>g> <strong>on</strong> post exposure prophylaxis prophylaxis (PEP) to prevent human<br />
immunodeficiency virus (HIV) <strong>in</strong>fecti<strong>on</strong>. Geneva, World Health Organizati<strong>on</strong> and<br />
Internati<strong>on</strong>al Labour Organizati<strong>on</strong>, 2008.<br />
http://www.who.<strong>in</strong>t/hiv/pub/guidel<strong>in</strong>es/PEP/en/<strong>in</strong>dex.html<br />
7 Centres for Diseases C<strong>on</strong>trol and Preventi<strong>on</strong>. Treatment guidel<strong>in</strong>es: hepatitis B. Morbidity<br />
and Mortality Weekly Report, 2006, 55(TT-11).<br />
http://www.cdc.gov/STD/treatment/2006/hepatitis-b.htm<br />
8 Jo<strong>in</strong>t ILO/<str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> health services and HIV/AIDS: Fact sheet No. 4. Geneva,<br />
Internati<strong>on</strong>al Labour Organizati<strong>on</strong>, 2005.<br />
Annex references 103
Glossary<br />
Acquired immunodeficiency syndrome (AIDS)<br />
Morbidity result<strong>in</strong>g from <strong>in</strong>fecti<strong>on</strong> with the human immunodeficiency virus.<br />
Adm<strong>in</strong>istrative c<strong>on</strong>trols to reduce exposure<br />
A method of m<strong>in</strong>imiz<strong>in</strong>g patient or employee exposures through enforcement of policies and<br />
procedures, modificati<strong>on</strong> of work assignment, tra<strong>in</strong><strong>in</strong>g <strong>in</strong> specific work practices, and other<br />
adm<strong>in</strong>istrative measures designed to reduce the exposure.<br />
Alcohol-based hand rub<br />
An alcohol-c<strong>on</strong>ta<strong>in</strong><strong>in</strong>g preparati<strong>on</strong> (liquid, gel or foam) designed for applicati<strong>on</strong> to the hands<br />
to reduce the growth of microorganisms. Such preparati<strong>on</strong>s may c<strong>on</strong>ta<strong>in</strong> <strong>on</strong>e or more types of<br />
alcohol with excipient (a relatively <strong>in</strong>ert substance used as a carrier for the active <strong>in</strong>gredients of a<br />
medicati<strong>on</strong>), or other active <strong>in</strong>gredients and humectants.<br />
Antiseptic handwash<strong>in</strong>g<br />
Wash<strong>in</strong>g hands with water and soap or other detergents c<strong>on</strong>ta<strong>in</strong><strong>in</strong>g an antiseptic agent.<br />
Recommended when carry<strong>in</strong>g out an aseptic technique.<br />
Antiseptics<br />
Antimicrobial substances applied to liv<strong>in</strong>g tissue or sk<strong>in</strong> to prevent <strong>in</strong>fecti<strong>on</strong>. They differ from<br />
antibiotics, which destroy bacteria with<strong>in</strong> the body, and from dis<strong>in</strong>fectants, which are used <strong>on</strong><br />
n<strong>on</strong>liv<strong>in</strong>g objects. Some antiseptics are true germicides, capable of destroy<strong>in</strong>g microbes whereas<br />
others are bacteriostatic and <strong>on</strong>ly prevent or <strong>in</strong>hibit their growth.<br />
Aseptic technique<br />
The manner of c<strong>on</strong>duct<strong>in</strong>g procedures to prevent microbial c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong>. An aseptic technique<br />
alters the method of hand hygiene, PPE worn, the locati<strong>on</strong> and physicial characteristics where<br />
a procedure is c<strong>on</strong>ducted, the use of sk<strong>in</strong> antisepsis and dis<strong>in</strong>fectants <strong>in</strong> the envir<strong>on</strong>ment, the<br />
manner of open<strong>in</strong>g of packages and the use of sterile supplies.<br />
Auto-disable (AD) syr<strong>in</strong>ge<br />
A syr<strong>in</strong>ge designed to prevent reuse by lock<strong>in</strong>g or disabl<strong>in</strong>g after giv<strong>in</strong>g a s<strong>in</strong>gle <strong>in</strong>jecti<strong>on</strong>, Several<br />
types of AD syr<strong>in</strong>ges are commercially available.<br />
Biohazard (biological hazard)<br />
A risk to the health of humans caused by exposure to harmful bacteria, viruses or other<br />
dangerous biological agents, or by a material produced by such an organism.<br />
<strong>Blood</strong>borne pathogens<br />
Pathogenic microorganisms <strong>in</strong> human blood that are transmitted through exposure to blood<br />
or blood products, and cause disease <strong>in</strong> humans. Comm<strong>on</strong> pathogens of occupati<strong>on</strong>al c<strong>on</strong>cern<br />
<strong>in</strong>clude hepatitis B virus, hepatitis C virus and human immunodeficiency virus.<br />
Capillary blood collecti<strong>on</strong><br />
<strong>Blood</strong> collected from capillaries, the smallest of a body’s blood vessels, measur<strong>in</strong>g 5–10 μm <strong>in</strong><br />
diameter, which c<strong>on</strong>nect arterioles and venules. <strong>Blood</strong> collected by this method is usually by heel<br />
or f<strong>in</strong>ger-prick.<br />
Cross-c<strong>on</strong>tam<strong>in</strong>ati<strong>on</strong><br />
The act of spread<strong>in</strong>g microbes (bacteria and viruses) from <strong>on</strong>e surface to another. S<strong>in</strong>ce<br />
bloodborne viruses can live <strong>on</strong> objects and surfaces for up to a week, and other pathogens<br />
for m<strong>on</strong>ths or more, microbes could be spread when surfaces are not dis<strong>in</strong>fected correctly or<br />
equipment is not cleaned and sterilized between patients.<br />
Glossary 105
Dis<strong>in</strong>fecti<strong>on</strong><br />
Kill<strong>in</strong>g of <strong>in</strong>fectious agents outside the body by direct exposure to chemical or physical agents.<br />
Dis<strong>in</strong>fecti<strong>on</strong> is necessary <strong>on</strong>ly for diseases spread by <strong>in</strong>direct c<strong>on</strong>tact.<br />
Disposal<br />
Intenti<strong>on</strong>al burial, deposit, discharge, dump<strong>in</strong>g, plac<strong>in</strong>g or release of any waste material <strong>in</strong>to<br />
or <strong>on</strong> any air, land or water. In the c<strong>on</strong>text of this document, disposal refers to the storage and<br />
subsequent destructi<strong>on</strong> of <strong>in</strong>jecti<strong>on</strong> or blood sampl<strong>in</strong>g equipment to avoid reuse or <strong>in</strong>jury.<br />
Eng<strong>in</strong>eer<strong>in</strong>g c<strong>on</strong>trols<br />
Methods of isolat<strong>in</strong>g or remov<strong>in</strong>g hazards from the workplace. Examples <strong>in</strong>clude sharps disposal<br />
c<strong>on</strong>ta<strong>in</strong>ers and safer medical devices (e.g. sharps with eng<strong>in</strong>eered sharps-<strong>in</strong>jury protecti<strong>on</strong>s<br />
and needleless systems), laser scalpels and ventilati<strong>on</strong>, <strong>in</strong>clud<strong>in</strong>g the use of ventilated biological<br />
cab<strong>in</strong>ets (laboratory fume hoods). In the c<strong>on</strong>text of sharps <strong>in</strong>jury preventi<strong>on</strong>, eng<strong>in</strong>eer<strong>in</strong>g<br />
c<strong>on</strong>trols means c<strong>on</strong>trol that isolates or removes the bloodborne pathogens from the workplace.<br />
F<strong>in</strong>ger-prick<br />
A method of capillary sampl<strong>in</strong>g. In medic<strong>in</strong>e, some blood tests are c<strong>on</strong>ducted <strong>on</strong> venous blood<br />
obta<strong>in</strong>ed by f<strong>in</strong>ger-prick. There are ways of open<strong>in</strong>g a small wound that produces no more than<br />
a few drops of blood. The procedure can be pa<strong>in</strong>ful, but can also be quicker and less distress<strong>in</strong>g<br />
than venepuncture.<br />
Hand hygiene<br />
Any type of hand cleans<strong>in</strong>g.<br />
Handwash<strong>in</strong>g<br />
Wash<strong>in</strong>g hands with soap and water, and dry<strong>in</strong>g thoroughly afterwards with s<strong>in</strong>gle-use towels.<br />
Hepatitis B <strong>in</strong>fecti<strong>on</strong><br />
Hepatitis caused by hepatitis B virus (HBV) and transmitted by exposure to blood or blood<br />
products, or dur<strong>in</strong>g sexual <strong>in</strong>tercourse. It causes acute and chr<strong>on</strong>ic hepatitis. Chr<strong>on</strong>ic hepatitis B<br />
can cause liver disease, cirrhosis and liver cancer.<br />
Hepatitis C <strong>in</strong>fecti<strong>on</strong><br />
Hepatitis caused by a hepatitis C virus (HCV) and transmitted by exposure to blood or blood<br />
products. Hepatitis C is usually chr<strong>on</strong>ic and can cause cirrhosis and primary liver cancer.<br />
Hierarchy of c<strong>on</strong>trols<br />
A c<strong>on</strong>cept developed <strong>in</strong> occupati<strong>on</strong>al health <strong>in</strong>dustrial hygiene to emphasize preventi<strong>on</strong>. The<br />
hierarchy, <strong>in</strong> order of priority for their efficacy <strong>in</strong> c<strong>on</strong>troll<strong>in</strong>g exposure to hazards and prevent<strong>in</strong>g<br />
<strong>in</strong>jury or illness result<strong>in</strong>g from exposure hazards, is as follows:<br />
• elim<strong>in</strong>ati<strong>on</strong> of the hazard;<br />
• eng<strong>in</strong>eer<strong>in</strong>g c<strong>on</strong>trols;<br />
• adm<strong>in</strong>istrative c<strong>on</strong>trols;<br />
• work practice c<strong>on</strong>trols; and<br />
• use of pers<strong>on</strong>al protective equipment.<br />
See also Annex 4 of Jo<strong>in</strong>t ILO/<str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> health services and HIV/AIDS (Annex<br />
reference 8) for the applicati<strong>on</strong> of the hierarchy of c<strong>on</strong>trols to the hazard of bloodborne pathogen<br />
exposure and needle-stick <strong>in</strong>juries.<br />
106 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Human immunodeficiency virus (HIV)<br />
A virus ma<strong>in</strong>ly transmitted dur<strong>in</strong>g sexual <strong>in</strong>tercourse or through exposure to blood or blood<br />
products. HIV causes acquired immunodeficiency syndrome (AIDS).<br />
Infecti<strong>on</strong> c<strong>on</strong>trol<br />
A health-care organizati<strong>on</strong>’s program, <strong>in</strong>clud<strong>in</strong>g policies and procedures, for the surveillance,<br />
preventi<strong>on</strong> and c<strong>on</strong>trol of health-care associated <strong>in</strong>fecti<strong>on</strong>s. Such a program <strong>in</strong>cludes all patient<br />
care and patient care support departments and services. Examples of <strong>in</strong>fecti<strong>on</strong> c<strong>on</strong>trol measures<br />
<strong>in</strong>clude immunizati<strong>on</strong>, hand hygiene, antimicrobial stewardship, review of facility c<strong>on</strong>structi<strong>on</strong>s,<br />
supervisi<strong>on</strong> of dis<strong>in</strong>fecti<strong>on</strong> and sterilizati<strong>on</strong>, surveillance, use of protective cloth<strong>in</strong>g and<br />
isolati<strong>on</strong>.<br />
Injecti<strong>on</strong><br />
Percutaneous <strong>in</strong>troducti<strong>on</strong> of a medic<strong>in</strong>al substance, fluid or nutrient <strong>in</strong>to the body. This may<br />
be accomplished most comm<strong>on</strong>ly by a needle and syr<strong>in</strong>ge, but also by jet <strong>in</strong>jectors, transdermal<br />
patches, micro-needles and other newer devices. The <strong>in</strong>jecti<strong>on</strong>s are comm<strong>on</strong>ly classified by the<br />
target tissue (e.g. <strong>in</strong>tradermal, subcutaneous, <strong>in</strong>tramuscular, <strong>in</strong>travenous, <strong>in</strong>traosseous, <strong>in</strong>traarterial,<br />
perit<strong>on</strong>eal).<br />
Intradermal <strong>in</strong>jecti<strong>on</strong><br />
A shallow <strong>in</strong>jecti<strong>on</strong> given between the layers of the sk<strong>in</strong>, creat<strong>in</strong>g a “weal” <strong>on</strong> the sk<strong>in</strong>.<br />
Intramuscular <strong>in</strong>jecti<strong>on</strong><br />
An <strong>in</strong>jecti<strong>on</strong> given <strong>in</strong>to the body of a muscle.<br />
Intravenous <strong>in</strong>jecti<strong>on</strong><br />
An <strong>in</strong>jecti<strong>on</strong> given <strong>in</strong>to a ve<strong>in</strong>.<br />
Intravascular<br />
With<strong>in</strong> a blood vessel.<br />
Jet <strong>in</strong>jector<br />
A needle-free device that allows the <strong>in</strong>jecti<strong>on</strong> of a substance through the sk<strong>in</strong> under high<br />
pressure.<br />
Lancet<br />
A blood-sampl<strong>in</strong>g device to obta<strong>in</strong> a capillary sample of blood for test<strong>in</strong>g. It is most comm<strong>on</strong>ly<br />
used by people with diabetes dur<strong>in</strong>g blood glucose m<strong>on</strong>itor<strong>in</strong>g. The depth of sk<strong>in</strong> penetrati<strong>on</strong><br />
can be adjusted by select<strong>in</strong>g lancets of different lengths.<br />
Needle-stick<br />
Penetrat<strong>in</strong>g stab wound caused by a needle.<br />
Occupati<strong>on</strong>al exposure<br />
Exposure to materials that results from the performance of an employee’s duties.<br />
Glossary 107
Other potentially <strong>in</strong>fectious materials<br />
Body fluids that are potentially <strong>in</strong>fectious for HIV, HBV and HBC <strong>in</strong>clud<strong>in</strong>g:<br />
• semen, vag<strong>in</strong>al secreti<strong>on</strong>s, cerebrosp<strong>in</strong>al fluid, synovial fluid, pleural fluid, pericardial fluid,<br />
perit<strong>on</strong>eal fluid, amniotic fluid, saliva <strong>in</strong> dental procedures, any body fluid that is visibly<br />
c<strong>on</strong>tam<strong>in</strong>ated with blood, and all body fluids <strong>in</strong> situati<strong>on</strong>s where it is difficult or impossible<br />
to differentiate between body fluids;<br />
• any unfixed tissue or organ (other than <strong>in</strong>tact sk<strong>in</strong>) from a human (liv<strong>in</strong>g or dead);<br />
• cell or tissue cultures, or organ cultures c<strong>on</strong>ta<strong>in</strong><strong>in</strong>g HIV;<br />
• culture medium or other soluti<strong>on</strong>s c<strong>on</strong>ta<strong>in</strong><strong>in</strong>g HIV, HBV or HCV;<br />
• blood, organs or other tissues from experimental animals <strong>in</strong>fected with HIV, HBV or HCV.<br />
Parenteral<br />
Pierc<strong>in</strong>g mucous membranes or the sk<strong>in</strong> barrier through subcutaneous, <strong>in</strong>tramuscular,<br />
<strong>in</strong>travenous or arterial routes; for example, through <strong>in</strong>jecti<strong>on</strong>s, needle-stick, cuts or abrasi<strong>on</strong>s.<br />
Pathogen<br />
A microorganism capable of caus<strong>in</strong>g disease.<br />
Pers<strong>on</strong>al protective equipment<br />
Specialized equipment worn by an employee to protect aga<strong>in</strong>st a def<strong>in</strong>ed hazard. Such<br />
equipment <strong>in</strong>cludes gloves, lab coats, gowns, apr<strong>on</strong>s, shoe covers, goggles, glasses with side<br />
shields, masks, respirators and resuscitati<strong>on</strong> bags. The purpose of pers<strong>on</strong>al protective equipment<br />
is to prevent hazardous materials from reach<strong>in</strong>g the workers’ sk<strong>in</strong>, mucous membranes or<br />
pers<strong>on</strong>al cloth<strong>in</strong>g. The equipment must create an effective barrier between the exposed worker<br />
and the hazard.<br />
<strong>Phlebotomy</strong><br />
The act of draw<strong>in</strong>g or remov<strong>in</strong>g blood from the circulatory system through an <strong>in</strong>cisi<strong>on</strong> or<br />
puncture to obta<strong>in</strong> a sample for analysis and diagnosis.<br />
Post-exposure care and prophylaxis for HIV<br />
Preventive <strong>in</strong>terventi<strong>on</strong>s offered to manage the specific aspects of exposure to HIV, and prevent<br />
HIV <strong>in</strong>fecti<strong>on</strong> <strong>in</strong> exposed <strong>in</strong>dividuals. The services <strong>in</strong>clude counsell<strong>in</strong>g, risk assessment, HIV<br />
test<strong>in</strong>g (based <strong>on</strong> <strong>in</strong>formed c<strong>on</strong>sent), first care and, when needed, the provisi<strong>on</strong> of short-term<br />
(28 days) antiretroviral drugs, with follow-up and support.<br />
Post-exposure prophylaxis (PEP)<br />
A medical resp<strong>on</strong>se given to prevent the transmissi<strong>on</strong> of bloodborne pathogens after potential<br />
exposure. It is available for HIV and hepatitis B.<br />
Quality c<strong>on</strong>trol<br />
A management functi<strong>on</strong> whereby c<strong>on</strong>trol of the quality of raw materials, assemblies, produced<br />
materials and comp<strong>on</strong>ents; services related to producti<strong>on</strong>; and management, producti<strong>on</strong><br />
and <strong>in</strong>specti<strong>on</strong> processes is exercised for the purpose of prevent<strong>in</strong>g undetected producti<strong>on</strong> of<br />
defective material or the render<strong>in</strong>g of faulty services.<br />
Recapp<strong>in</strong>g<br />
The act of replac<strong>in</strong>g a protective sheath <strong>on</strong> a needle. Recapp<strong>in</strong>g needles us<strong>in</strong>g two-handed<br />
methods <strong>in</strong>creases the risk of needle-stick <strong>in</strong>juries and is not recommended. However, where<br />
such acti<strong>on</strong> is unavoidable, the <strong>on</strong>e-hand scoop technique reduces the risk of needle-sticks.<br />
108 <str<strong>on</strong>g>WHO</str<strong>on</strong>g> guidel<strong>in</strong>es <strong>on</strong> draw<strong>in</strong>g blood: best practices <strong>in</strong> phlebotomy
Safe <strong>in</strong>jecti<strong>on</strong><br />
An <strong>in</strong>jecti<strong>on</strong> that does no harm to the recipient, does not expose the health worker to any risk<br />
and does not result <strong>in</strong> waste that puts the community at risk.<br />
Sharp<br />
Any object that can penetrate the sk<strong>in</strong>; sharps <strong>in</strong>clude needles, scalpels, broken glass, broken<br />
capillary tubes and exposed ends of dental wires.<br />
Sharps c<strong>on</strong>ta<strong>in</strong>er<br />
A puncture-resistant, rigid, leak-resistant c<strong>on</strong>ta<strong>in</strong>er designed to hold used sharps safely dur<strong>in</strong>g<br />
collecti<strong>on</strong>, disposal and destructi<strong>on</strong>. Sometimes referred to as a “sharps box” or “safety box”.<br />
Sharps <strong>in</strong>jury<br />
An exposure event occurr<strong>in</strong>g when any sharp penetrates the sk<strong>in</strong>.<br />
Sharps protecti<strong>on</strong> device<br />
A sharp or needle device used for withdraw<strong>in</strong>g body fluids, access<strong>in</strong>g a ve<strong>in</strong> or artery, or<br />
adm<strong>in</strong>ister<strong>in</strong>g medicati<strong>on</strong>s or other fluids. The device has a built-<strong>in</strong> safety feature or mechanism<br />
that effectively reduces the risk of an exposure <strong>in</strong>cident.<br />
S<strong>in</strong>gle-use syr<strong>in</strong>ge<br />
A sterile syr<strong>in</strong>ge <strong>in</strong>tended for the aspirati<strong>on</strong> of fluids or for the <strong>in</strong>jecti<strong>on</strong> of fluids immediately<br />
after fill<strong>in</strong>g (ISO 7886-1).<br />
Solid sharp<br />
A sharp that does not have a lumen through which material can flow; for example, a suture<br />
needle, scalpel or lancet.<br />
Standard precauti<strong>on</strong>s<br />
A set of practices designed to prevent the spread of <strong>in</strong>fecti<strong>on</strong> between health workers and<br />
patients from c<strong>on</strong>tact with <strong>in</strong>fectious agents <strong>in</strong> recognized and unrecognized sources of <strong>in</strong>fecti<strong>on</strong>.<br />
Such precauti<strong>on</strong>s are recommended for use with all patients, regardless of patient diagnoses or<br />
presumed <strong>in</strong>fectious status. Key elements <strong>in</strong>clude hand hygiene, clean<strong>in</strong>g of the envir<strong>on</strong>ment,<br />
reprocess<strong>in</strong>g of equipment between patients, use of pers<strong>on</strong>al protective equipment, placement<br />
of patients with known <strong>in</strong>fecti<strong>on</strong> or col<strong>on</strong>izati<strong>on</strong> <strong>in</strong>to isolati<strong>on</strong>, laundry management, <strong>in</strong>jecti<strong>on</strong><br />
safety, prevent<strong>in</strong>g exposure to bloodborne pathogens, waste management and respiratory<br />
hygiene.<br />
Sterile<br />
Free from liv<strong>in</strong>g microorganisms.<br />
Subcutaneous <strong>in</strong>jecti<strong>on</strong><br />
An <strong>in</strong>jecti<strong>on</strong> delivered under the sk<strong>in</strong>.<br />
Syr<strong>in</strong>ge with reuse preventi<strong>on</strong> feature<br />
A sterile s<strong>in</strong>gle-use hypodermic syr<strong>in</strong>ge of a design such that it can be rendered unusable after<br />
use (ISO 7886-4).<br />
Work practice c<strong>on</strong>trols<br />
Techniques that reduce the likelihood of exposure by chang<strong>in</strong>g the way a task is performed.<br />
Glossary 109