(IPHS) Guidelines - NRHM Manipur
(IPHS) Guidelines - NRHM Manipur
(IPHS) Guidelines - NRHM Manipur
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Indian Public Health Standards (<strong>IPHS</strong>)<strong>Guidelines</strong> forCommunity Health CentresRevised 2012Directorate General of Health ServicesMinistry of Health & Family WelfareGovernment of India
Indian Public Health Standards (<strong>IPHS</strong>)<strong>Guidelines</strong> forCommunity Health CentresRevised 2012Directorate General of Health ServicesMinistry of Health & Family WelfareGovernment of India
ContentsMessageForewordPrefaceAcknowledgementsvviviiviiiExecutive Summary 1Indian Public Health Standards (<strong>IPHS</strong>) for Community Health Centres 3Introduction 3Objectives of Indian Public Health Standards (<strong>IPHS</strong>) for CHCs 3Service Delivery in CHCs 3Manpower 8Equipment 11Drugs 11Physical Infrastructure 11Quality Assurance in Service Delivery 16Patient Safety and Infection Control 17Statutory and Regulatory Compliance 18Record Maintenance 18Checklists 18AnnexuresAnnexure 1: Newborn Care Facilities at Chc 20Annexure 1A: Newborn Corner in OT/Labour Room 20Annexure 1B: Newborn Care Stabilization Unit 22Annexure 2: Requirements with Regard to Revised National TB Control Programme 24Annexure 3: National Aids Control Programme: <strong>Guidelines</strong> 26Annexure 4: National Vector Borne Disease Control Programme 27
Annexure 5: National Leprosy Eradication Programme 29Annexure 6: National Programme for Control of Blindness 30Annexure 7: Integrated Disease Surveillance Project 31Annexure 7A: Form P (Weekly Reporting Format-IDSP) 32Annexure 7B: Form L (Weekly Reporting Format-IDSP) 33Annexure 7C: Format for Instantaneous Reporting of Early Warning Signal/Outbreaks as soon as it is Detected 34Annexure 8: Facility Based Maternal Death Review Form 35Annexure 9: List of Equipment in CHC 39Annexure 10: List of Drugs 47Annexure 11: Extracts from National <strong>Guidelines</strong> on Blood Storage Facilities at FRUs 65Annexure 12: List of Diagnostic Services 68Annexure 13: Model Citizen’s Charter 71Annexure 14: List of Statutory Compliances 73Annexure 15: Steps for Safety in Surgical Patients (in the Pre-operative Ward) 74Annexure 16: List of Abbreviations 76References 78Members of Task Force for Revision of <strong>IPHS</strong> 79
MESSAGENational Rural Health Mission (<strong>NRHM</strong>) was launched to strengthen the Rural Public HealthSystem and has since met many hopes and expectations. The Mission seeks to provide effectivehealth care to the rural populace throughout the country with special focus on the States andUnion Territories (UTs), which have weak public health indicators and/or weak infrastructure.Towards this end, the Indian Public Health Standards (<strong>IPHS</strong>) for Sub-Centres, Primary HealthCentres (PHCs), Community Health Centres (CHCs), Sub-District and District Hospitals werepublished in January/February, 2007 and have been used as the reference point for public healthcare infrastructure planning and up-gradation in the States and UTs. <strong>IPHS</strong> are a set of uniform standards envisagedto improve the quality of health care delivery in the country.The <strong>IPHS</strong> documents have been revised keeping in view the changing protocols of the existing programmes andintroduction of new programmes especially for Non-Communicable Diseases. Flexibility is allowed to suit thediverse needs of the states and regions.Our country has a large number of public health institutions in rural areas from sub-centres at the most peripherallevel to the district hospitals at the district level. It is highly desirable that they should be fully functional and deliverquality care. I strongly believe that these <strong>IPHS</strong> guidelines will act as the main driver for continuous improvement inquality and serve as the bench mark for assessing the functional status of health facilities.I call upon all States and UTs to adopt these <strong>IPHS</strong> guidelines for strengthening the Public Health Care Institutionsand put in their best efforts to achieve high quality of health care for our people across the country.New Delhi23.11.2011(Ghulam Nabi Azad)
ForewordAs envisaged under National Rural Health Mission (<strong>NRHM</strong>), the public health institutions in ruralareas are to be upgraded from its present level to a level of a set of standards called “IndianPublic Health Standards (<strong>IPHS</strong>)”. The Indian Public Health Standards are the benchmarks forquality expected from various components of Public health care organizations and may be usedfor assessing performance of health care delivery system.The Community Health Centres (CHCs) which constitute the secondary level of health carewere designed to provide referral as well as specialist health care to the rural population.Indian Public Health Standards (<strong>IPHS</strong>) for CHCs were first released under National Rural Health Mission (<strong>NRHM</strong>) in early 2007.As setting standards is a dynamic process, need was felt to update the <strong>IPHS</strong> keeping in view the changing protocolsof existing National Health Programmes, development of new programmes especially for non-communicablediseases and the prevailing epidemiological situation in the country. The <strong>IPHS</strong> for CHC has been revised by a taskforce comprising of various stakeholders under the Chairmanship of Director General of Health Services. Subjectexperts, NGOs, State representatives and health workers working in the health facilities have also been consultedat different stages of revision.The newly revised <strong>IPHS</strong> (CHC) has considered the services, infrastructure, manpower, equipment and drugs in twocategories of Essential (minimum assured services) and Desirable (the ideal level services which the states and UTsshall try to achieve). Unlike Sub-centre and PHCs, CHCs will be of one type only and will act as Block level healthadministrative unit and Gatekeeper for referrals to higher level of facilities.I would like to acknowledge the efforts put by the Directorate General of Health Services in preparing theguidelines. It is hoped that this document will be useful to all the stakeholders. Comments and suggestions forfurther improvements are most welcome.(P.K.Pradhan)
PrefaceStandards are a means of describing a level of quality that the health care organizations areexpected to meet or aspire to achieve. For the first time under National Rural Health Mission(<strong>NRHM</strong>), an effort had been made to develop Indian Public Health Standards (<strong>IPHS</strong>) for a vastnetwork of peripheral public health institutions in the country and the first set of standards wasreleased in early 2007 to provide optimal specialized care to the community and achieve andmaintain an acceptable standard of quality of care.The <strong>IPHS</strong> for Community Health Centres has been revised keeping in view the resourcesavailable with respect to functional requirements for a Community Health Centre with minimum standards forsuch as building, manpower, instruments and equipment, drugs and other facilities etc. The revised <strong>IPHS</strong> hasalso incorporated the changed protocols of the existing health programmes and new programmes and initiativesespecially in respect of Non-Communicable Diseases. The task of revision was completed as a result of consultationsheld over many months with task force members, programme officers, Regional Directors of Health and FamilyWelfare, experts, health functionaries, representatives of Non-Government organizations, development partnersand State/Union Territory Government representatives after reaching a consensus. The contribution of all of themis well appreciated. Several innovative approaches have been incorporated in the management process to ensurecommunity and Panchayati Raj Institutions’ involvement and accountability.Under the revised <strong>IPHS</strong>, CHC serves as a First Referral Unit, Block level Administrative Unit and Block level PublicHealth Unit. This document prescribes the essential requirements for a minimum functional grade of a CommunityHealth Centre and the desirable requirements needed for an ideal situation.Setting standards is a dynamic process and this document is not an end in itself. Further revision of the standardsshall be undertaken as and when the Community Health Centres will achieve a minimum functional grade. Itis hoped that this document will be of immense help to the States/Union Territories and other stakeholders inbringing up the Community Health Centres to the level of Indian Public Health Standards.(Dr. Jagdish Prasad)
AcknowledgementsThe revision of the existing guidelines for Indian Public Health Standards (<strong>IPHS</strong>) for different levels of HealthFacilities from Sub-Centre to District Hospitals was started with the formation of a Task Force under theChairmanship of Director General of Health Services (DGHS). This revised document is a concerted effort madepossible by the advice, assistance and cooperation of many individuals, Institutions, government and nongovernmentorganizations.I gratefully acknowledge the valuable contribution of all the members of the Task Force constituted to reviseIndian Public Health Standards (<strong>IPHS</strong>). The list of Task Force Members is given at the end of this document. I amthankful to them individually and collectively.I am truly grateful to Mr. P.K. Pradhan, Secretary (H & FW) for the active encouragement received from him.I also gratefully acknowledge the initiative, inspiration and valuable guidance provided by Dr. Jagdish Prasad,Director General of Health Services, Ministry of Health and Family Welfare, Government of India. He has alsoextensively reviewed the document while it was being developed.I sincerely thank Miss K. Sujatha Rao, Ex-Secretary (H&FW) for her valuable contribution and guidancein rationalizing the manpower requirements for Health Facilities. I would specially like to thank Ms. Anuradha Gupta, Additional Secretary and Mission Director <strong>NRHM</strong>, Mr. Manoj Jhalani Joint Secretary(RCH), Mr. Amit Mohan Prasad, Joint Secretary (<strong>NRHM</strong>), Dr. R.S. Shukla Joint Secratary (PH), Dr. ShivLal, former Special DG and Advisor (Public Health), Dr. Ashok Kumar, DDG Dr. N.S. Dharm Shaktu, DDG,Dr. C.M. Agrawal DDG, Dr. P.L. Joshi former DDG, experts from NHSRC namely Dr. T. Sunderraman, Dr. J.N. Sahai, Dr. P. Padmanabhan, Dr. J.N. Srivastava, experts from NCDC Dr. R.L. Ichhpujani, Dr. A.C. Dhariwal,Dr. Shashi Khare, Dr. S.D. Khaparde, Dr. Sunil Gupta, Dr. R.S. Gupta, experts from NIHFW Prof. B. Deoki Nandan,Prof. K. Kalaivani, Prof. M. Bhattacharya, Prof. J.K. Dass, Dr. Vivekadish, programme officers from Ministry ofHealth Family welfare and Directorate General of Health Services especially Dr. Himanshu Bhushan, Dr. ManishaMalhotra, Dr. B. Kishore, Dr. Jagdish Kaur, Dr. D.M. Thorat and Dr. Sajjan Singh Yadav for their valuable contributionand guidance in formulating the <strong>IPHS</strong> documents. I am grateful to the following State level administrators,health functionaries working in the health facilities and NGO representatives who shared their field experienceand greatly contributed in the revision work; namely:viiiIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Dr. Manohar Agnani, MD <strong>NRHM</strong> from Government of MP Dr. Junaid Rehman from Government of Kerala.Dr. Kamlesh Kumar Jain from Government of Chhattisgarh.Dr. Y.K. Gupta, Dr. Kiran Malik, Dr. Avdesh Kumar, Dr. Naresh Kumar, Smt. Prabha Devi Panwar, ANM and Ms. Pushpa Devi, ANM from Government of Uttar Pradesh.Dr. P.N.S. Chauhan, Dr. Jayashree Chandra, Dr. S.A.S. Kazmi, Dr. L.B. Asthana, Dr. R.P. Maheshwari, Dr. (Mrs.) Pushpa Gupta, Dr. Ramesh Makwana and Dr. (Mrs.) Bhusan Shrivastava from Government of Madhya Pradesh.Dr. R.S. Gupta, Dr. S.K. Gupta, Ms. Mamta Devi, ANM and Ms. Sangeeta Sharma, ANM from Government ofRajasthan.Dr. Rajesh Bali from Government of Haryana.NGO representatives: Dr. P.K. Jain from RK Mission and Dr. Sunita Abraham from Christian Medical Associationof India.Tmt. C. Chandra, Village Health Nurse, and Tmt. K. Geetha, Village Health Nurse from Government of Tamil Nadu.I express my sincere thanks to Architects of Central Design Bureau namely Sh. S. Majumdar, Dr. Chandrashekhar,Sh. Sridhar and Sh. M. Bajpai for providing inputs in respect of physical infrastructure and building norms.I am also extremely grateful to Regional Directors of Health and Family Welfare, State Health Secretaries, StateMission directors and State Directors of Health Services for their feedback.I shall be failing in my duty if I do not thank Dr. P.K. Prabhakar, Deputy Commissioner, Ministry of Health andFamily Welfare for providing suggestions and support at every stage of revision of this document.Last but not the least the assistance provided by my secretarial staff and the team at Macro Graphics Pvt. Ltd.is duly acknowledged.(Dr. Anil Kumar)Member Secretary-Task forceCMO (NFSG)Directorate General of Health ServicesJune 2012Ministry of Health & Family WelfareNew Delhi Government of IndiaIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centresix
Executive SummaryThe Community Health Centres (CHCs) constitutethe secondary level of health care, were designed toprovide referral as well as specialist health care to therural population. Indian Public Health Standards (<strong>IPHS</strong>)for CHCs have been prescribed under National RuralHealth Mission (<strong>NRHM</strong>) since early 2007 to provideoptimal specialized care to the community and achieveand maintain an acceptable standard of quality of care.As setting standards is a dynamic process, the need wasfelt to update the <strong>IPHS</strong> keeping in view the changingprotocols of existing National Health Programmes,development of new programmes especially for noncommunicablediseases and prevailing epidemiologicalsituation in the country and different States/UTs of thecountry; accordingly the revision has been carried out.These standards would act as benchmarks and helpmonitor and improve the functioning of the CHCs.Service DeliveryUnlike Sub-centre and PHCs, CHCs have beenenvisaged as only one type and will act bothas Block level health administrative unit andgatekeeper for referrals to higher level offacilities.The revised <strong>IPHS</strong> (CHC) has consideredthe services, infrastructure, manpower,equipment and drugs in two categories ofEssential (minimum assured services) andDesirable (the ideal level services which thestates and UT shall try to achieve).All essential services as envisaged in the CHCshould be made available, which includesroutine and emergency care in Surgery,Medicine, Obstetrics and Gynaecology,Paediatrics, Dental and AYUSH in addition toall the National Health Programmes.Standards of services under existingprogrammes were updated and standardsadded for newly developed non communicabledisease programmes based on the inputs fromvarious programme divisions.Standards for Newborn stabilization unit,MTP facilities for second trimester pregnancy(desirable), The Integrated Counselling andTesting Centre (ICTC), Blood storage and linkAnti Retroviral Therapy centre have beenadded.Minimum Requirement forDelivery of the Above-MentionedServicesThe following requirements are being projectedbased on the assumption that there will be averagebed occupancy of 60%. The strength may be furtherincreased if the occupancy increases with subsequentup gradation. With regards to Manpower, 2 specialists,namely, Anesthetist and Public Health Specialist willbe provided in addition to the available specialists,namely, Surgery, Medicine, Obstetrics and Gynecologyand Pediatrics.A Block Public Health Unit is envisaged at the CHC havinga Block Medical Officer/Medical superintendent, oneIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Public Health specialist and at least one Public HealthNurse. The support manpower will include a DentalAssistant, Multi Rehabilitation Worker, Cold Chain andVaccine Logistic Assistant in addition to the existing staff.The manpower at CHC has been rationalized in order toensure optimal utilization of scarce manpower.FacilitiesThe lists of equipment and essential drugs have beenupdated; the drug list for obstetric care and sicknewborn & child care (for First Referral Unit (FRU)/CHC)has been incorporated in these guidelines.Physical Infrastructure will be remodeled or rearrangedto make best possible use for optimal utilization as pergiven guidelines in the relevant section.Human Resource ManagementCapacity Building will be ensured at all levels by periodictraining of all cadres.AccountabilityIt is mandatory for every CHC to have functional“Rogi Kalyan Samiti” (RKS) to ensure accountabilityand also shall have the Charter of Patients’ Rightsdisplayed prominently at the entrance. A grievanceredressal mechanism under the overall supervisionof RKS would also be set up.Quality of ServicesStandard Operating Procedures and Standard TreatmentProtocols for common ailments and the National HealthProgrammes should be available and followed. Tomaintain quality of services, external monitoring throughPanchayati Raj Institutions and internal monitoring atappropriate intervals is advocated. <strong>Guidelines</strong> are beingprovided for management of routine and emergencycases under the National Health Programmes so as tomaintain uniformity in Management in tune with theNational Health Policy.Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Indian Public Health Standards (<strong>IPHS</strong>) for Community Health CentresIntroductionHealth care delivery in India has been envisaged atthree levels namely primary, secondary and tertiary.The secondary level of health care essentially includesCommunity Health Centres (CHCs), constituting theFirst Referral Units (FRUs) and the Sub-district andDistrict Hospitals. The CHCs were designed to providereferral health care for cases from the Primary HealthCentres level and for cases in need of specialist careapproaching the centre directly. 4 PHCs are includedunder each CHC thus catering to approximately 80,000populations in tribal/hilly/desert areas and 1,20,000population for plain areas. CHC is a 30-bedded hospitalproviding specialist care in Medicine, Obstetrics andGynecology, Surgery, Paediatrics, Dental and AYUSH.There are 4535 CHCs functioning in the country ason March 2010 as per Rural Health Statistics Bulletin2010. These centres are however fulfilling the tasksentrusted to them only to a limited extent. Thelaunch of the National Rural Health Mission (<strong>NRHM</strong>)gives us the opportunity to have a fresh look at theirfunctioning.<strong>NRHM</strong> envisages bringing up the CHC services to thelevel of Indian Public Health Standards. Although thereare already existing standards as prescribed by theBureau of Indian Standards for 30-bedded hospital, theseare at present not achievable as they are very resourceintensive.Under the <strong>NRHM</strong>, the Accredited Social HealthActivist (ASHA) is being envisaged in each village topromote the health activities. With ASHA in place, thereis bound to be a groundswell of demands for healthservices and the system needs to be geared to face thechallenge. Not only does the system require up-gradationto handle higher patient load, but emphasis also needsto be given to quality aspects to increase the level ofpatient satisfaction. In order to ensure quality of services,the Indian Public Health Standards (<strong>IPHS</strong>) are being setup for CHCs so as to provide a yardstick to measure theservices being provided there. This document providesthe essential requirements for a Minimum FunctionalGrade of a Community Health Centre and the desirablerequirements needed for an ideal situation.Objectives of Indian Public HealthStandards (<strong>IPHS</strong>) for CHCsTo provide optimal expert care to thecommunity.To achieve and maintain an acceptablestandard of quality of care.To ensure that services at CHC arecommensurate with universal best practicesand are responsive and sensitive to the clientneeds/expectations.Service Delivery in CHCsOPD Services and IPD Services: General,Medicine, Surgery, Obstetrics & Gynaecology,Paediatrics, Dental and AYUSH services.Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Eye Specialist services (at one for every 5 CHCs).Emergency ServicesLaboratory ServicesNational Health ProgrammesEvery CHC has to provide the following services whichhave been indicated as Essential and Desirable. AllStates/UTs must ensure the availability of all Essentialservices and aspire to achieve Desiable services whichare the ideal that should be available.I. Care of Routine and Emergency Casesin SurgeryEssentialII.This includes dressings, incision anddrainage, and surgery for Hernia, Hydrocele,Appendicitis, Haemorrhoids, Fistula, andstitching of injuries.Handling of emergencies like IntestinalObstruction, Haemorrhage, etc.Other management including nasal packing,tracheostomy, foreign body removal etc.Fracture reduction and putting splints/plastercast.Conducting daily OPD.Care of Routine and Emergency Casesin MedicineEssential Specific mention is being made of handlingof all emergencies like Dengue HaemorrhagicFever, Cerebral Malaria and others like Dog &snake bite cases, Poisonings, Congestive HeartFailure, Left Ventricular Failure, Pneumonias,meningoencephalitis, acute respiratoryconditions, status epilepticus, Burns, Shock,acute dehydration etc. In case of NationalHealth Programmes, appropriate guidelinesare already available, which should befollowed. Conducting daily OPD.III. Maternal HealthEssential Minimum 4 ANC check ups includingRegistration & associated services : As someantenatal cases may directly register with CHC,the suggested schedule of antenatal visits isreproduced below.1 st visit: Within 12 weeks—preferablyas soon as pregnancy is suspected—forregistration of pregnancy and first antenatalcheck-up.2 nd visit: Between 14 and 26 weeks3 rd visit: Between 28 and 34 weeks4 th visit: Between 36 weeks and term24-hour delivery services including normaland assisted deliveries.Managing labour using Partograph.All referred cases of Complications inpregnancy, labour and post-natal period mustbe adequately treated.Ensure post-natal care for 0 & 3 rd day at thehealth facility both for the mother and newbornand sending direction to the ANM of theconcerned area for ensuring 7 th & 42 nd daypost-natal home visits.Minimum 48 hours of stay after delivery,3-7 days stay post delivery for managingComplications.Proficiency in identification and Managementof all complications including PPH, Eclampsia,Sepsis etc. during PNC.Essential and Emergency Obstetric Careincluding surgical interventions like CaesareanSections and other medical interventions.Provisions of Janani Suraksha Yojana (JSY) andJanani Shishu Suraksha Karyakram (JSSK) asper guidelines.IV. Newborn Care and Child HealthEssential Essential Newborn Care and Resuscitation byproviding Newborn Corner in the Labour Roomand Operation Theatre (where caessariantakes place). Details of Newborn Corner givenat Annexure 1A.i. Early initiation of breast feeding with in onehour of birth and promotion of exclusivebreast-feeding for 6 months. Newborn Stabilization Unit (Details given atAnnexure 1B). Counseling on Infant and young child feedingas per IYCF guidelines. Routine and emergency care of sick childrenincluding Facility based IMNCI strategy. Full Immunization of infants and childrenagainst Vaccine Preventable Diseases andIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Vitamin-A prophylaxis as per guidelines ofGovt. of India. Tracking of vaccination dropouts and left outs.Prevention and management of routinechildhood diseases, infections and anemia etc.Management of Malnutrition cases.Provisions of Janani Shishu Suraksha Karyakram(JSSK) as per guidelines.V. Family PlanningEssential Full range of family planning services includingIEC, counseling, provision of Contraceptives,Non Scalpel Vasectomy (NSV), LaparoscopicSterilization Services and their follow up. Safe Abortion Services as per MTP act andAbortion care guidelines of MOHFW.Desirable MTP Facility approved for 2 nd trimester ofpregnancy.VI. Other National Health Programmes(NHP): (Essential Except as Indicated)All NHPs should be delivered through the CHCs.Integration with the existing programmes isvital to provide comprehensive services. Therequirements for the important NHPs are beingannexed as separate guidelines and following arethe assured services under each NHP.Communicable Diseases Programmes RNTCP: CHC should provide diagnosticservices through the microscopy centreswhich are already established in the CHCsand treatment services as per the Technicaland Operational <strong>Guidelines</strong> for TuberculosisControl (Annexure 2). HIV/AIDS Control Programme: Theservices to be provided at the CHC levelare (Annexure 3). Integrated Counselling and TestingCentre.Blood Storage Centre .Sexually Transmitted Infection clinic.Desirable Link Anti Retroviral Therapy Centre.Blood storage units should have at least number of units of Blood equalto double of the average daily requirement/consumption. National Vector Borne Disease ControlProgramme: The CHCs are to providediagnostic/linkages to diagnosis andtreatment facilities for routine and complicatedcases of Malaria, Filaria, Dengue, JapaneseEncephalitis and Kala-azar in the respectiveendemic zones (Annexure 4). National Leprosy Eradication Programme(NLEP): The minimum services that are tobe available at the CHCs are for diagnosisand treatment of cases and complicationsincluding reactions of leprosy along withconselling of patients on prevention ofdeformity and cases of uncomplicated ulcers(Annexure 5). National Programme for Control ofBlindness: The eye care services that shouldbe made available at the CHC are as givenbelow.Essential Vision Testing with Vision drum/VisionCharts. Refraction The early detection of visual impairmentand their referral. Awareness generation throughappropriate IEC strategies and involvingcommunity for primary prevention andearly detection of impaired vision andother eye conditions.Desirable Intraocular pressure measurement byTonometers. Syringing and probing. The provision for removal of ForeignBody. Provision of Basic services for Diagnosisand treatment of common eye diseases. Surgical services including cataract by IOLimplantation.One ophthalmologist is being envisaged for every 5 lakhpopulation i.e. one ophthalmologist will cater to 5 CHCs.(Annexure 6). Under Integrated Disease SurveillanceProject, CHC will function as peripheralsurveillance unit and collate, analyse andreport information to District SurveillanceIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Unit on selected epidemic prone diseases. Inoutbreak situations, appropriate action willbe initiated (Annexure 7).National Programme for Prevention and Control ofDeafness (NPPCD)CHC will provide following services: The early detection of cases of hearingimpairment and deafness and referral. Provision of Basic Diagnosis and treatmentservices for common ear diseases. Awareness generation through appropriateIEC strategies and greater participation/role of community in primary preventionand early detection of hearing impairment/deafness.National Mental Health Programme (NMHP)EssentialEarly identification, Diagnosis and treatmentof common mental disorders (anxiety,depression, psychosis, schizophrenia, ManicDepressive Psychosis).IEC activities for prevention, removal of stigmaand early detection of mental disorders.Follow up care of detected cases who are ontreatment.Desirable With short term training the medicalofficers would be trained to deliver basicmental health care using limited numberof drugs and to provide referral service.This would result in early identification andtreatment of common mental illnesses inthe community.National Programme for Prevention and Controlof Cancer, Diabetes, Cardiovascular Diseases andStroke (NPCDCS)Cancer ControlEssential Facilities for early detection and referral ofsuspected cancer cases. Screening for Cervical, Breast & Oral Cancers. Education about Breast Self Examination andOral Self Examination. PAP smear for Cancer CervixDesirable Basic equipment (Magna Visualiser, IndirectLaryngoscope, Punch biopsy forceps) andconsumables for early detection of commoncancers. Public private partnership for laboratoryinvestigations (biochemical, pathological(including biopsy), microbiological, tumormarkers, mammography etc. which are relatedto cancer diagnosis). Investigations to confirm diagnosis of cancerin patients with early warning signals throughPublic Private Partnership mode.Diabetes, CVD and StrokesEssentialPromotion & PreventionHealth Promotion: Focus will be onhealthy population.Modify individual, group and communitybehaviour through intervention like,• Promotion of Healthy Dietary Habits.• Promotion of physical activity.• Avoidance of tobacco and alcohol.• Stress Management.Treatment & Timely Referral (Complicatedcases) of Diabetes Mellitus, Hypertension,IHD, CHF etc. Assured investigations: Urine Albuminand Sugar, Blood Sugar, Blood Lipid Profile,KFT (Blood urea, creatinine) ECG.DesirableEarly detectionSurvey of population through simplemeasures like history taking of symptoms,measuring blood pressure, checking for sugarin urine and blood etc. and their segregationinto normal, vulnerable, high risk and thosesuffering from disease.National Iodine Deficiency Disorders ControlProgramme (NIDDCP) IEC activities in the form of posters,pamphlets, Interpersonal communicationIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
to promote the consumption of iodised saltby the people and monitoring of iodised saltthrough salt testing kits.National Programme for Prevention and Controlof Fluorosis (NPPCF) Essential in Fluorosis affectedVillages Clinical examination and preliminarydiagnostic parameters assessment for casesof Fluorosis if facilities are available. Monitoring of village/community levelFluorosis surveillance and IEC activities. Referral Services. IEC activities in theform of posters, pamphlets, Interpersonalcommunication to prevent Fluorosis.National Tobacco Control Programme (NTCP)Essential Health education and IEC activities regardingharmful effects of tobacco use and secondhand smoke. Promoting quitting of tobacco in thecommunity and offering brief advice to allsmokers and tobacco users. Making the premises of CHC tobacco free anddisplay of mandatory signages.DesirableSetting up a Tobacco cessation Clinic, by trainingthe couselor in tobacco cessation.National Programme for Health Care of ElderlyDesirable Medical rehabilitation services. Compilation of elderly data from PHC& forwarding the same to district nodalofficers. Visits to the Homes of disabled/bed riddenpersons by rehabilitation worker on receivinginformation from PHC/Sub-centre. Geriatric Clinic: twice a week.Physical Medicine and Rehabilitation (PMR)EssentialPrimary prevention of Disabilities.Screening, early identification and detectionCounselling.DesirableOral HealthIssue of Disability Certificate for obviousDisabilities by CHC doctors.Community based Rehabilitation Services.Basic treatments like Exercise and Heattherapy, ROM exercises, cervical and LumbarTraction, referral to higher centers and followup.Essential Dental care and Dental Health educationservices as well as root canal treatment andfilling/extraction of routine and emergencycases. Oral Health education in collaboration withother activities e.g. Nutritional education,school health and adolescent health.VII. Other ServicesSchool Health:Teachers screen students on a continuous basis andANMs/HWMs (a team of 2 workers) visit the schools(one school every week) for screening, treatment ofminor ailments and referral. Doctor from CHC/PHC will also visit one school per week based on thescreening reports submitted by the teams. Overallservices to be provided under school health shallincludeEssentialHealth service provision:Screening, health care and referral:• Screening of general health, assessmentof Anaemia/Nutritional status, visualacuity, hearng problems, dental checkup, common skin conditions, Heartdefects, physical disabilities, learningdisorders, behavior problems, etc.• Basic medicines to take care of commonailments, prevalent among young schoolgoing children.• Referral Cards for priority services atDistrict / Sub-District hospitals.Immunization:• As per national schedule• Fixed day activityIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
• Coupled with education about theissueMicronutrient (Vitamin A & IFA)management:• Weekly supervised distribution ofIron-Folate tablets coupled witheducation about the issue• Administration of Vitamin-A in needycases.De-worming• Biannually supervised schedule• Prior IEC• Siblings of students also to becoveredCapacity buildingMonitoring & EvaluationMid Day MealDesirableHealth Promoting Schools• Counseling services• Regular practice of Yoga, Physicaleducation, health education• Peer leaders as health educators.• Adolescent health education-existingin few places• Linkages with the out of schoolchildren• Health clubs, Health cabinets• First Aid room/corners or clinics.Adolescent Health CareTo be provided preferably through adolescent friendlyclinic for 2 hours once a week on a fixed day. Servicesshould be comprehensive i.e. a judicious mix ofpromotive, preventive, curative and referral servicesCore package (Essential) Adolescent and Reproductive Health:Information, counseling and services relatedto sexual concerns, pregnancy, contraception,abortion, menstrual problems etc. Services for tetanus immunization ofadolescentsNutritional Counseling, Prevention andmanagement of nutritional anemiaSTI/RTI managementReferral Services for VCTC and PPTCT servicesand services for Safe termination of pregnancy,if not available at PHCOptional/additional services (desirable): as per localneedOutreach services in schools (essential) and communityCamps (desirable)EssentialPeriodic Health check ups and healtheducation activities, awareness generationand Co-curricular activitiesBlood Storage FacilityDiagnostic Services (Annexure 12) In addition to the lab facilities and X-ray, ECGshould be made available in the CHC withappropriate training to a nursing staff/Lab.Technician. All necessary reagents, glass ware andfacilities for collecting and transport ofsamples should be made available.Referral (transport) ServicesMaternal Death Review (MDR).Facility Based MDR form is at Annexure 8.Minimum Requirement forDelivery of the Above-mentionedServicesThe following requirements are being projectedbased on the assumption that there will be averagebed occupancy of 60%. The strength may be furtherincreased if the occupancy increases with subsequentupgradation.ManpowerIn order to provide round the clock clinical services,there is likelihood of shortage of doctors in 8-hourlyshift duties. This shortage can be compensated byresource pooling (Block Pooling Concept) of availabledoctors posted at Primary Health Centres coveredunder the CHC.Under the present scenario of shortage of clinicalmanpower, it is suggested that doctors of PHCs, inaddition to attending to routine OPD duties at PHCsmay also do shift duties to provide emergency servicesat CHCs.Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
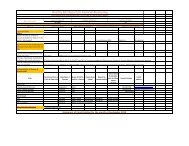
Manpower: CHCPersonnel Essential Desirable Qualifications RemarksBlock MedicalOfficer/MedicalSuperintendentBlock Public Health Unit1 Senior most specialist/GDMO preferablywith experience inPublic Health/Trainedin ProfessionalDevelopment Course(PDC)Public Health Specialist 1 MD (PSM)/MD (CHA)/MD CommunityMedicine or PostGraduation Degreewith MBA/DPH/MPHPublic Health Nurse(PHN) #1 +1Specialty ServicesGeneral Surgeon 1 MS/DNB, (GeneralSurgery)Physician 1 MD/DNB, (GeneralMedicine)Obstetrician &1 DGO /MD/DNBGynaecologistPaediatrician 1 DCH/MD (Paediatrics)/DNBAnaesthetist 1 MD (Anesthesia)/DNB/DA/LSAS trained MOGeneral Duty OfficersDental Surgeon 1 BDSGeneral Duty Medical2 MBBSOfficerMedical Officer -1 Graduate in AYUSHAYUSHNurses and ParamedicalStaff Nurse 10Pharmacist 1 +1Pharmacist – AYUSH 1Will be responsible forcoordination of NHPs,management of ASHAsTraining and otherresponsibilities under<strong>NRHM</strong> apart fromoverall administration/Management ofCHC etc. He willbe responsible forquality & protocols ofservice delivery beingdelivered in CHC.Essential for utilizationof the surgicalspecialities. They maybe on contractualappointment or hiringof services fromprivate sectors on percase basisIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Personnel Essential Desirable Qualifications RemarksLab. Technician 2Radiographer 1Dietician 1Ophthalmic Assistant 1Dental Assistant 1Cold Chain & Vaccine1Logistic AssistantOT Technician 1Multi Rehabilitation/1 +1Community BasedRehabilitation workerCounsellor 1Administrative StaffRegistration Clerk 2Statistical Assistant/2Data Entry OperatorAccount Assistant 1AdministrativeAssistant1Group D StaffDresser (certified1by Red Cross/JohnsAmbulance)Ward Boys/Nursing5OrderlyDriver* 1* 3Total 46 52Note:If patient load increases, then number of General Duty Doctors may be increased.Funds would be provided for out-sourcing and providing support services as per need.One of nursing orderlies could be trained in CSSD procedures.Budget to be provided for outsourcing Class IV services like Mali, Aya, Peon, OPD Attendant, Security and Sanitary workers.* May be outsourced.# Graduate or Diploma in Nursing and will be trained for 6 months in Public Health.Note:12345.6As a short term arrangement, MBBS doctors who have received short term training or having experience of at least two years inthe particular speciality can be utilized against the spciality post. However, in such cases a specific order after posting such doctorsmust be issued.One of the Class IV employees can be identified as a helper to Cold Chain & Vaccine Logistic Assistant and trained as Cold ChainHandler.States shall as per provision under <strong>NRHM</strong> explore keeping part time/contractual staff wherever deficient. Outsourcing of servicesmay be done as per State’s policy.One nursing staff/Lab technician may be trained for ECG.One Ophthalmologist is recommended for 5 CHCs.The Health Educator at PHC should work in coordination with block public health unit for organizing health education services.10Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
EquipmentDrugsThe list of equipment provided under theCSSM may be referred to as they are deemedto be adequate for providing all services in theCHC (Annexure 9). Before ordering new sets,the existing equipment should be properlyassessed.For ophthalmic equipment wherever theservices are available, Annexure no. 6 may bereferred to.Maintenance of equipment. It is estimatedthat 10-15% of the annual budget is necessaryfor maintenance of euipments.Refrigerators [3(Essential), 4 (Desirable)], onefor each ward, one for OT, One for laboratory,should be available in the CHC. No Sharing ofRefrigerator with the lab should be done.Appropriate standards for equipment arealready available in the Bureau of IndianStandards. If standards for any equipment arenot available, technical specifications for theequipment may be prepared by the technicalcommittee of the State for the process oftendering and procurement.The list of essential drugs and emergency drugs areprovided at Annexure 10.Programme specific drugs are detailed in the <strong>Guidelines</strong>under each programme. AYUSH drugs are beingincluded.Physical InfrastructureThe CHC should have 30 indoor beds with one Operationtheatre, labour room, X-ray, ECG and laboratory facility.In order to provide these facilities, following are theguidelines.Location of the centre: All the guidelines as belowunder this sub-head may be applicable only to centresthat are to be newly established and priority is to begiven to operationalise the existing CHCs. To the extent possible, the centre shouldbe located at the centre of the blockheadquarter in order to improve access tothe patients.The area chosen should have the facility forelectricity, all weather road communication,adequate water supply, telephone etc.It should be well planned with the entirenecessary infrastructure. It should be well litand ventilated with as much use of naturallight and ventilation as possible.CHC should be away from garbage collection,cattle shed, water logging area, etc.Disaster Prevention Measures: (For all new upcomingfacilities in seismic zone 5 or other disaster proneareas).Building structure and the internal structure shouldbe made disaster proof especially earthquake proof,flood proof and equipped with fire protectionmeasures.Earthquake proof measures: Structural and nonstructuralelements should be built in to withstandquake as per geographical/state govt. guidelines. Nonstructuralfeatures like fastening the shelves, almirahs,equipment etc are even more essential than structuralchanges in the buildings. Since it is likely to increase thecost substantially, these measures may especially betaken on priority in known earthquake prone areas.CHC should not be located in low lying area to preventflooding.CHC should have dedicated, intact boundary wall witha gate. Name of the CHC in local language should beprominently displayed at the entrance which is readablein night too.Fire fighting equipment: Fire extinguishers, sandbuckets, etc. should be available and maintained tobe readily available when needed. Staff should betrained in using fire fighting equipment. Each CHCshould develop a fire fighting and fire exit plan withthe help of Fire Department. Regular mock drillsshould be conducted.All CHCs should have a Disaster Management Plan in linewith the District Disaster management Plan. All healthstaff should be trained and well conversant with disasterprevention and management aspects Surprise mockdrills should be conducted at regular intervals. Aftereach drill the efficacy of the Disaster Plan, preparednessof the CHC, and the competence of the staff should beIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 11
evaluated followed by necessary changes in the Planand training of the staff.The CHC should be, as far as possible, environment friendlyand energy efficient. Rain-Water harvesting, solar energyuse and use of energy-efficient CFL bulbs/equipment should be encouraged. Provision should be made for horticulture services including herbal garden.The building should have areas/space marked for thefollowing:Entrance ZoneSignage Prominent display boards in local languageproviding information regarding the servicesavailable and the timings of the institute. Directional and layout signages for all thedepartments and utilities (toilets, drinkingwater etc.) shall be appropriately displayed foreasy access. All the signages shall be bilingualand pictorial. Citizen charter shall be displayed at OPD andEntrance in local language including patient’srights and responsibilities. On-the-way signages of the CHC & locationshould be displayed on all the approachroads. Safety, hazards and caution signs shall bedisplayed prominently at relevant places, e.g. radiation hazards for pregnant woman inX-Ray. Fluroscent Fire-Exit signages at strategiclocations. Barrier free access environment for easyaccess to non-ambulant (wheel-chairstretcher), semi-ambulant, visually disabledand elderly persons as per “<strong>Guidelines</strong>and Space Standards for barrier-free builtenvironment for Disabled and Elderly Persons”of Government of India. Ramp as per specification, Hand-railing,proper lightning etc must be provided in allhealth facilities and retrofitted in older onewhich lack the same. Registration cum Inquiry counters. Pharmacy for drug dispensing and storage.Clean Public utilities separate for males andfemales.Suggestion/complaint boxes for the patients/visitors and also information regardingthe person responsible for redressal ofcomplaints.Outpatient DepartmentThe facility shall be planned keeping in mind themaximum peak hour load and shall have scope forfuture expansion.Name of Department and doctor, timings and user fees/charges shall be displayed.Layout of the Out Patient Department shall follow thefunctional flow of the patients: e.g.Enquiry→Registration→Waiting→SubWating→Clinic→Dressing room/Injection Room→Billing→Dignostics (lab/X-ray)→pharmacy→ExitClinics for Various Medical Disciplines : These clinicsinclude general medicine, general surgery, dental,obstetric and gynaecology, paediatrics and familywelfare. Separate cubicles for general medicine andsurgery with separate area for internal examination(privacy) can be provided if there are no separaterooms for each. The cubicles for consultation andexamination in all clinics should provide for doctor’stable, chair, patient’s stool, follower’s seat, washbasin with hand washing facilities, examinationcouch and equipment for examination. Room shall have, for the admission of lightand air, one or more apertures, such aswindows and fan lights, opening directly tothe external air or into an open verandah.The windows should be in two oppositewalls. Family Welfare Clinic : The clinic shouldprovide educative, preventive, diagnosticand curative facilities for maternal, childhealth, school health and health education.Importance of health education is beingincreasingly recognized as an effective toolof preventive treatment. People visitinghospital should be informed of personal andenvironmental hygiene, clean habits, need fortaking preventive measures against epidemics,family planning, non-communicable diseasesetc. Treatment room in this clinic should actas operating room for IUCD insertion andinvestigation, etc. It should be in close proximity12Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
to Obstetric & Gynaecology. Family Welfarecounselling room should be provided.Waiting room for patients.The Pharmacy should be located in an areaconveniently accessible from all clinics.The dispensary and compounding roomshould have two dispensing windows,compounding counters and shelves. Thepattern of arranging the counters andshelves shall depend on the size of theroom. The medicines which require cold storage and blood required for operations andemergencies may be kept in refrigerators.Emergency Room/Casualty: At the moment,the emergency cases are being attendedin OPD during OPD hours and in inpatientunits afterwards. It is recommended tohave a separate earmarked emergency areato be located near the entrance of hospitalpreferalbly having 4 rooms (one for doctor,one for minor OT, one for plaster/dressing)and one for patient observation (At least 4beds).Treatment RoomMinor OTInjection Room and Dressing RoomObservation RoomWards: Separate for Males and FemalesNursing Station : The nursing station shallbe centered such that it serves all the clinicsfrom that place. The nursing station should bespacious enough to accommodate a medicinechest/a work counter (for preparing dressings,medicines), hand washing facilities, sinks,dressing tables with screen in between andcolour coded bins (as per IMEP guidelinesfor community health centres). It shouldhave provision for Hub cutters and needledestroyers.Examination and dressing table.Patient AreaEnough space between beds.Toilets; separate for males and females.Separate space/room for patients needingisolation.Ancillary roomsNurses rest room.There should be an area separating OPDand Indoor facility.Operation theatre/Labour roomPatient waiting Area.Pre-operative and Post-operative(recovery) room.Staff area.Changing room separate for males andfemales.Storage area for sterile supplies.Operating room/Labour room.Scrub area.Instrument sterilization area.Disposal area.Newborn care Corner (Annexure 1A).Newborn Care Stabilization Unit: Annexure 1BPublic utilities: Separate for males and female; forpatient as well as for paramedical & Medical staff.Disabled friendly, WC with wash basins as specifiedunder <strong>Guidelines</strong> for disabled friendly environmentshould be provided.Physical Infrastructure for Support ServicesCentral Steritization Supply Department (CSSD):Sterilization and Sterile storage.Laundry: Storage should be separate for dirtylinen and clean linen.Outsourcing is recommended afterappropriate training of washer man regardingsegregation and separate treatment forinfected and non-infected linen.Engineering Services: Electricity/telephones/water/civil Engineering may be outsourced.Maintenance of proper sanitation in toiletsand other public utilities should be givenutmost attention. Sufficient funding for thispurpose must be kept and the services maybe outsourced.Water Supply : Arrangements shall be madeto supply 10,000 litres of potable water perday to meet all the requirements (includinglaundry) except fire fighting. Storage capacityIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 13
for 2 days requirements should be on thebasis of the above consumption. Round theclock water supply shall be made available toall wards and departments of the hospital.Separate reserve emergency overhead tankshall be provided for operation theatre.Necessary water storage overhead tankswith pumping/boosting arrangement shallbe made. The laying and distribution ofthe water supply system shall be accordingto the provisions of IS: 2065-1983 (a BISstandard). Cold and hot water supplypiping should be run in concealed formembedded into wall with full precautionsto avoid any seepage. Geyser in O.T./L.R.and one in ward also should be provided. Wherever feasible solar installations shouldbe promoted.Emergency Lighting : Emergency portable/fixed light units should also be providedin the wards and departments to serve asalternative source of light in case of powerfailure. Generator back-up should be availablein all facilities. Generator should be of goodcapacity. Solar energy wherever feasible maybe used.Generator : 5 KVA with POL for ImmunizationCold Chain maintenance.Telephone: minimum two direct lines withintercom facility should be available.Administrative zoneSeparate rooms should be available for:OfficeStoresResidential ZoneMinimum 8 quarters for Doctors.Minimum 8 quarters for staff nurses/paramedical staff.Minimum 2 quarters for ward boys.Minimum 1 quarter for driver.If the accommodation can not be provided due toany reason, then the staff may be paid house rentallowance, but in that case they should be staying innear vicinity of CHC so that they are available for 24 x7 in case of need.Function & Space Requirement forCommunity Health CentreIt is suggested considering the land cost & availability ofland, CHC building may be constructed in two floors.Function & Space Requirement for Different ZonesZone Functions Size for Each Sub-functionin Mtrs.Entrance ZoneRegistration & Recordstorage, Pharmacy (Issuecounter/Formulation/Drugstorage) Public utilities &circulation spaceRegistration/Record Room3.2 X 3.2 X 2Queue area outsideregistration room 3.5 X 3Pharmacy cum store 6.4 X 3.2Pharmacy cum store forAYUSH 6.4 X 3.2Total Areas in Sq Mtrs20.48 Sq Mtrs10.5 Sq Mtrs20.48 Sq Mtrs20.48 Sq MtrsAmbulatory Zone (OPD)Examination & Workup(Examination Room, subwaiting), Consultation(consultation room Toilets,sub waiting) Nursing station(Nurses desk, clean utility,Space for 4 General DoctorRoom 3.2 X 3.2 X 4Space for 2 AYUSH doctorsRoom 3.2 X 3.2 X 28 specialist room with attachtoilets = 3.7 X 3.2 X 840.96 Sq Mtrs20.48 Sq Mtrs94.72 Sq Mtrs14Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Zone Functions Size for Each Sub-functionin Mtrs.Diagnostic Zonedirty utility, treatmentrooms, injection & dressingroom), Cold Chain, Vaccinesand Logistics area, ECG(with sub waiting) Casualty/Emergency, public utilities,circulation spacePathology (Optional)Laboratory, samplecollection, bleeding room,washing disinfectantsstorage, sub waiting, Imaging(radiology, radiography, ultrasound),Preparation, room,change room, toilet, control,Dark room, treatment room,sub waiting, public utilitiesTreatment room 3.7 X 3.2Refraction room 3.2 X 3.2Nursing Station 6.4 X 3.2Casualty 6.4 X 6.4Dress Room 3.2 X 3.2Injection Room 3.2 X 3.2Female injection room 3.2 X 3.2Public Utility/CommonToiletsWaiting AreaCold Chain Room 3.5 x 3Vaccine and Logistics Room3.5 x 3Area specification isrecommendedTotal Areas in Sq Mtrs11.84 Sq Mtrs10.24 Sq Mtrs20.48 Sq Mtrs40.96 Sq Mtrs10.24 Sq Mtrs10.24 Sq Mtrs10.24 Sq Mtrs9.5 Sq Mtrs31.5 Sq Mtrs10.5 Sq Mtrs10.5 Sq Mtrs180 Sq MtrsZone Functions Area Requirementfor Each Sub-functionIntermediateZone(inpatientNursingunits)Critical Zone (OperationalTheater/Labour roomNursing station (Nursedesk,clean utility, treatmentroom, pantry, store, sluiceroom, trolly bay) patientarea (bed space, toilets,Day space, Isolation Space)Ancillary rooms (Doctor’srest room, Nurses dutyroom, Public utilities,circulation space.Patient area (Preparation,Preanaesthesia, postoperative resting) Staff area(Changing Resting) Suppliesarea (trolley bay, equipmentstorage, sterile storage) OT/Lr area (Operating/Labourroom, scrub, instrumentsterilization, Disposal) publicutilities, circulation spaceNursing station 6.4 X 6.44 wards each with 6 beds( 2 male wards & 2 femalewards) size (6.2 X 6.2 ) X 44 private room (2 each formale & females) with toilets6.2 X 3.2 X 4 2isolation rooms with toilet(one each for male & female)6.2 X 3.2 X 2Area specification isrecommendedTotal Areas in Sq Mtrs40.96 Sq Mtrs 153.76 Sq Mtrs79.36 Sq Mtrs39.68 Sq Mts240 Sq MtrsIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 15
Zone Functions Area Requirementfor Each Sub-functionService ZoneAdministrative zoneTotal Circulation Area/CorridorsTotal AreaDietary (Dry Store, DayStore, Preparation, Cooking,Delivery, pot wash, Utensilwash, Utensil store, trolleypark) C.S.S.D. (Receipt, wash,assembly, sterilization, sterilestorage, Issue) Laundry(Receipt, weigh, sluice/wash,Hydro extraction, tumble,calender, press) Laundry(clean storage, Issue),Civil engineering (Buildingmaintenance, Horticulture,water supply, drainageand sanitation), Electricalengineering (sub station &generation, Illumination,ventilation), Mechanicalengineering, Space forother services like gas store,telephone, intercom, fireprotection, waste disposal,Mortuary.General Administration,general store, public utilitiescirculation spaceServices like Electricalengineering /Mechanicalengineering & Civilengineering can be privatelyhired to avoid permanentspace in the CHC buildingArea specification isrecommendedTotal Areas in Sq MtrsArea specification isrecommended60 Sq Mtrs191.15 Sq Mtrs1503.32 Sq MtrsCapacity BuildingTraining of all cadres of worker at periodic intervals is anessential component. Multi skill training for Doctors, StaffNurses and paramedical workers is recommended.Quality Assurance in ServiceDeliveryQuality of Service Should be Maintained atall LevelsStandard Treatment protocol is the “Heart” ofquality and cost of care. Standard treatmentprotocol for all national programmes and locallycommon diseases should be made available atall CHCs. All the efforts that are being made toimprove “hardware i.e. infrastructure” and “software i.e. human resource” are necessary but not sufficient.These need to be guided by Standard TreatmentProtocols. Some of the states have already preparedthese guidelines. For all ailments covered byNational Health Programmes an agreed treatment/case management protocol need to be adhered tovoluntarily by the physicians.Diet: Diet may either be outsourced or adequate spacefor cooking should be provided in a separate space. Thediet within the budget/funds and affordability shouldbe healthy food, nutritious and full of minerals andvitamins.CSSD: Adequate space and standard procedures forsterilization and Sterile storage should be available. Apractical protocol for quality assurance of CSSD maybe developed in coordination with District Hospital lab and implemented to ensure sterilization quality.16Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
LaundryStorage: Separate for dirty linen and cleanlinen.Outsourcing is recommended after appropriatetraining of washer man regarding separatetreatment for infected and non-infected linen.Services: Maintenance of Electricity/telephones/watersupply/civil engineering etc. may be outsourced.Blood Storage Units: The GOI guidelines as given inAnnexure 11 may be referred to.Waste Disposal: “<strong>Guidelines</strong> for Health Care Workersfor Waste Management and Infection Control inCommunity Health Centres” are to be followed. Acentral storage point should be made for biomedicalwaste collected from all points of CHC which should belocated away from OPD & IPD.Charter of Patient Rights: It is mandatory for everyCHC to have the Charter of Patient Rights prominentlydisplayed at the entrance. Details are provided in theAnnexure 13.Quality ControlInternal MonitoringRoutine Monitoring by District Health Authority at leastonce in a month..Social Audit: Through Rogi Kalyan Samitis/PanchayatiRaj Institution etc.Medical auditOthers like Death audit, technical audit, economic audit,disaster preparedness audit etc.Patient Satisfaction SurveysOut Patient care: This shall include:Access to patientsRegistration and admission procedures.ExaminationInformation exchange: complaints &suggestions and their remedical measures byhospital, authorities.TreatmentOther facilities: waiting, toilets, drinkingwater.In Patient CareLinen/bedsStaying facilities for relatives with respect toDiet, drinking water and Toilets.External Monitoring Gradation of the centre by PRI (Zilla Parishad)/Rogi Kalyan Samitis. Community monitoring.Monitoring of laboratory: Internal Quality Assessment scheme. External Quality Assessment scheme.Patient Safety and InfectionControlEssential1 Hand washing facilities in all OPD clinics, wards,emergency and OT areas.2 Safe clinical practices as per standard protocolsto prevent health care associated infectionsand other harms to patients.3 There shall be proper written handing oversystem between health care staff.4 Safe Injection administration practices as perthe prescribed protocol.5. Safe Blood transfusion practices need to beimplemented by the hospital administrators.6 Ensuring Safe disposal of Bio-medical Waste asper rules (National <strong>Guidelines</strong> to be followed).7 Regular Training of Health care workers inPatient safety, infection control and Bio-medicalwaste management.Desirable1 Use of safe Surgery check lists in the ward andoperation Theatre to minimize the errors duringsurgical procedures. (for the detailed checklistrefer to Annexure 15.)2. Antibiotic Policy : CHC shall develop its ownantibiotic policy to check indiscriminate useof antibiotics and reduce the emergence ofresistant strains.Health Care Workers Safety1Provision of Protective gears like gloves, masks,gowns, caps, personal protective equipment,lead aprons, dosimeters etc and their useby Health Care workers as per standardprotocols.Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 17
234Desirable12Display Standard operating procedures atstrategic locations in the hospitals.Implementation of Infection control practicesand Safe BMW Management.Regular Training of Health care workersin Universal precautions, Patient safety, infection control and Bio-medical wastemanagement.Immunization of Health care workers againstTetanus and Hepatitis B.Provision of round the clock Post exposureprophylaxis against HIV in cases of needle sticksinjuries.Statutory and RegulatoryCompliancesCHC shall fulfil all the statuary and regulatoryrequirements and comply to all the regulations issued by local bodies, state, and union of India. CHCshall have copy of these regulations/acts. List of statuaryand regulatory compliances is given in Annexure 14.Record MaintenanceIt is desirable that Computers should be used foraccurate record maintenance.ChecklistChecklist for Minimum Requirement of CHCsServices Existing RemarksPopulation coveredSpecialist services availableMedicineSurgeryOBGPaediatricsNHPsEmergency servicesLaboratoryBlood StorageInfrastructure(As per Specifications)Area of the BuildingOPD rooms/cubiclesWaiting room for patientsNo. of beds: MaleNo. of beds: FemaleOperation theatreLabour roomLaboratoryX-ray RoomBlood StoragePharmacyWater supplyElectricityGardenTransport facilitiesExistingRemarks18Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Checklist for EquipmentEquipment(As per List)Available Functional RemarksChecklist for DrugsDrugs(As per Essential Drug list)ExistingRemarksChecklist for AuditParticulars Available Whether Functional as per NormsPatient's charterRogi Kalyan SamitiInternal monitoringExternal MonitoringAvailability of SOPs/STPs**Standard Operating Procedures/ Standard Treatment Protocols.Checklist for Monitoring Maternal HealthANCMinimum 4 ANCHigh Risk pregnancyCases with Danger sign and symptoms treated.No of Caesarian Section (CS) doneProportion of Caesarian sections out of total deliveriesPNC VisitMinimum 3 PNC Visits within 1 st week of delivery i.e. on 0,3,7 th day.Are deliveries being monitored through Partograph?Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 19
AnnexuresAnnexure 1 Newborn Care Facilities at ChcAnnexure 1A: Newborn Corner in OT/Labour RoomDelivery rooms in Operation Theatres (OT) and in Labourrooms are required to have separate resuscitationspace and outlets for newborns. Some term infants andmost pre-term infants are at greater thermal risk andoften require additional personnel (Human Resource),equipment and time to optimize resuscitation. An appropriate resuscitation/stabilization environmentshould be provided as provision of appropriatetemperature for delivery room & resuscitation of highriskpre-term infants is vital to their stabilization.Services at the CornerThis space provides an acceptable environment formost uncomplicated term infants, but may not supportthe optimal management of newborns who may requirereferral to SNCU. Services provided in the Newborn CareCorner are:Care at birth.Resuscitation.Provision of warmth.Early initiation of breast feeding.Weighing the neonate.Configuration of the CornerClear floor area shall be provided for in theroom for newborn corner. It is a space withinthe labour room, 20-30 sq ft in size, where aradiant warmer will be kept.Oxygen, suction machine and simultaneouslyaccessibleelectrical outlets shall be providedfor the newborn infant in addition to thefacilities required for the mother.Clinical procedures: Standard operatingprocedures including administration ofoxygen, airway suction would be put in place.Resuscitation kit should be placed as part ofradiant warmer.Provision of hand washing and containmentof infection control if it is not a part of thedelivery room.The area should be away from draught ofair, and should have power connection forplugging in the radiant warmer.20Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Equipment and Consumables Required for the CornerItemNo.Item DescriptionEssentialDesirableQuantityInstallationTrainingCivilMechanicalElectrical12Open care system: radiant warmer, fixed height, with trolley,drawers, O2-bottlesResuscitator (silicone resuscitation bag and mask withreservoir) hand-operated, neonate, 500 mlE 1 X X X X XE 1 X3 Weighing Scale, spring E 1 X4 Pump suction, foot operated E 1 X5 Thermometer, clinical, digital, 32-34 0 C E 26 Light examination, mobile, 220-12 V E 1 X X7 Hub Cutter, syringe E 1 XConsumables8 I/V Cannula 24 G, 26 G E9 Extractor, mucus, 20 ml, ster, disp Dee Lee E10 Tube, feeding, CH07, L40 cm, ster, disp E11 Oxygen catheter 8 F, Oxygen Cylinder E12 Sterile Gloves EIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 21
Annexure - 1 B: Newborn Care Stabilization UnitSetting of Stabilization Unit atFirst Referral UnitsEvery first referral unit, whether or not care of sickbabies is undertaken, must have clearly establishedarrangements for the prompt, safe and effectiveresuscitation of babies and for the care of babiestill stabilized, either in the maternity ward or by safetransfer elsewhere.Services at the Stabilization UnitFRUs are not intended to provide any intensive care,a newborn that has problems identified immediatelyafter birth, or who becomes ill subsequently, mayhave a requirement for one or more of the followingservices. These should therefore be available to ensuresafe care of the baby prior to appropriate transfer:Provision of warmth.Resuscitation.Supportive care including oxygen, drugs, IV fluids.Monitoring of vital signs, including bloodpressure.Breast feeding/feeding support.Referral Services.Configuration of the StabilizationUnitStabilization unit should be located within or inclose proximity of the emergency ward where sickand low birth weight newborns and children canbe cared.Space of approximately 40-50 sq ft per bedis needed, where 4 radiant warmers will bekept.Provision of hand washing and containmentof infection control.Human ResourceStaffingONE STAFF NURSE SHOULD PROVIDE COVER FORNEONATES AND CHILDREN ROUND THE CLOCKAdditional nursing staff may be required for newborn care at the Stabilization Unit. Pediatricianposted at FRU will be in charge of the StabilizationUnit.TrainingDoctors and Nurses posted at Stabilization Unit willundergo Facility based care training.Referral ServicesEach Unit accepting neonatal and sick child referralsshould have, or have access to, an appropriately staffedand equipped transport service.22Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Equipment and Consumables Required for the Stabilization UnitItemNo.Item DescriptionEssentialDesirableQuantityInstallationTrainingCivilMechanicalElectrical1Open care system: radiant warmer, fixed height, with trolley,drawers, O 2 -bottlesE 4 X X X X X2 Resuscitator, hand-operated, neonate and child, 500 ml E 2 X3 Laryngoscope set E 2 X4 Scale, baby, electronic, 10 kg E 1 X5 Pump suction, foot operated E 1 X6 Thermometer, clinical, digital, 32-34 C E 47 Light examination, mobile, 220-12 V E 4 X X8 Hub Cutter, syringe E 1 XConsumables9 I/V Cannula 24 G, 26 G E10 Extractor, mucus, 20 ml, ster, disp Dee Lee E11 Tube, feeding, CH07, L40 cm, ster, disp E12 Oxygen cylinder 8 F E13 Sterile Gloves E14 Tube, suction, CH 10, L50 cm, ster, disp E15 Cotton wool, 500 g, roll, non-ster E16 Disinfectant, chlorhexidine, 20% EIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 23
Annexure 2Requirements with regard to Revised NationalTB Control ProgrammeDiagnostic ServicesA Microscopy Centre (MC) is established for 1,00,000population. For hilly, tribal and difficult areas MC isestablished for 50,000 populations. The MicroscopyCentres are established at PHC, CHC or District Hospital.Inputs1123RNTCP has provided inputs to upgrade theinfrastructure through minor civil works of theexisting laboratories to be able to come up tothe minimum standard required to carry outsputum microscopy. At present, entire countryis covered under RNTCP.Manpower: Existing Laboratory Technicians(LTs) are provided training and they function asLTs to carry out sputum microscopy. For up to20% of the requirements of the LTs at designatedMicroscopy Centres at the District level, LTs areprovided by RNTCP on contractual basis.Equipment: Binocular Microscopes areprovided to the Microscopy Centres for sputummicroscopy.Laboratory Consumables: Funds are providedto the District TB Control Societies forprocurement and supply of all the consumablesrequired to carry out sputum microscopy. Forlist of Laboratory consumables, refer to RNTCPguidelines.Treatment Servicesi.Medical Officers: All Medical Officers are trainedin RNTCP to suspect chest symptomatics, referthem for sputum microscopy and be able tocategorize the patients and handle side effectsof anti TB drugs.DOTS Centres: All sub-centres, PHCs, CHCsand District Hospitals work as DOTS Centres.In addition, the community DOTS providers arealso trained to deliver DOTS. A room of the CHCis used to function as DOTS centre. Facilities forseating and making available drinking waterto the patients for consumption of drugs areprovided under the Programme.DOTS Providers: The Multi Purpose Workers(MPWs), Pharmacists and Staff Nurses aretrained in to monitor consumption of anti TBdrugs by the patients.All the DOTS providers to deliver treatmentas per treatment guidelines. All the doctorsto categorize patients as per treatmentguidelines (refer Technical <strong>Guidelines</strong>).Drugs in patient wise boxes and loosedrugs are provided at DOT Centres throughDistrict TB Centre (DTC). Details of thedrugs given in RNTCP guidelines.Recording and reporting to be done as perOperational <strong>Guidelines</strong> (refer Operational<strong>Guidelines</strong>).Treatment of Complicated Cases1ii.iii.a.bcFor patients who require admission (PleuralEffusion, Emphysema etc.) drugs are providedin the form of prolongation pouches throughDistrict TB Centre for indoor treatment.24Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
2The common complications of TB can be treatedby the Medical Officers/Specialists at CHC andside effects of drugs can also be handled by thedoctors at CHC.Quality Assurancei.Diagnosis: The diagnostic services aresupervised by Senior TB Laboratory Supervisorii.(STLS) for all the Microscopy Centres at thesub-district level (5,00,000 population or2,50,000 population in the hilly, difficult andtribal areas).Treatment: All major drugs are procured atthe Centre through World Bank recommendedprocedures and provided to the States, therebyassuring quality of the drugs.Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 25
Annexure 3National Aids Control Programme: <strong>Guidelines</strong>At present the preventive and care interventions forthe control of HIV/AIDS are being provided belowdistrict level through integrated Health Care Systemusing the available staff. There is also a provisionof training of health care providers and generatingawareness through intensive IEC campaign. Theprogramme is being further strengthened byconverging the activities under NACP with RCHprogramme, which is underway. The followingactivities are being proposed to be integrated at CHClevel.Consumables/Logistics3000 Nos Whole Blood Finger Prick HIV Rapid Test andSTI Screening Test each; STI syndromic drug kit.IEC/Job aidsCounseling Flip Chart, Posters etc.ReportingRegisters and Monthly formats as per NACO guidelines.Sl.ActivitiesProposedNo.1 STI clinic: RTI/STD management services Expansion of services up to CHC & 24 hours PHC. Basicscreening test for RTI/STD to be made available at the CHCs.2 Integrated Counseling and Testing Centre (ICTC), LinkART Centre & youth information centresExpansion of services up to CHCs in all States3 Prevention of parent-to-Child Transmission (PPTCT) Services to be provided at all CHCs4 Behaviour Change Communication (BCC) Joint communication strategy messages & mediumdevelopment to be done5 Condom promotion Joint condom procurement & distribution of condoms tomeet the needs of sexually active women and men as amethod of dual protection6 Blood safety Blood storage centres planned at FRUs will procure bloodfrom licensed blood banks but will be supported by RCH7 Trainings A specific plan will be developed jointly by both thedepartments to train the peripheral staff at CHC8 Management Information System All facilities to report service performance on RTI/STI, ICTC,Link ART services, PPTCT as a part of routine reporting9 Operationalisation A convergence facilitator to be appointed under NACPto ensure coordinated inputs between the activitiesimplemented by NACP and RCH26Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Annexure 4National Vector Borne Disease ControlProgrammeThe National Vector Borne Disease Control Programme(NVBDCP), erstwhile National Anti Malaria Programme(NAMP) is the country’s most comprehensive and multifacetedpublic health activity. Directorate of NVBDCP isthe nodal agency for prevention and control of majorvector borne diseases of public health importancenamely Malaria, Filariasis, Japanese Encephalitis (JE),Kala-Azar, Chikungunya and Dengue.Following are the strategies for control of thesediseases:Malaria Early Diagnosis and prompt treatment ofmalaria cases.Integrated vector control.Early Detection and Containment of malariaoutbreak. Information, Education and Communication(IEC) for personal protection and communityinvolvement for malaria control. Training and Capacity Building of Medical andPara-medical workers. Monitoring and evaluation of EfficientManagement Information System (MIS).Dengue: Epidemiological Surveillance of Dengue cases. Entomological surveillance of Aedes aegyptimosquitoes. Clinical management of reported cases. Control of mosquitoes through IntegratedVector Management including sourcereduction, use of larvivorous fishes,impregnated bednets and selective foggingwith Pyrethrum.Behaviour change communication to changebehavior of the community about preventionof breeding of mosquitoes.Kala-azar Early diagnosis & complete treatment throughPrimary Health Care System. Interruption of transmission through vectorcontrol by undertaking residual insecticidalspraying in affected areas . Health Education and communityparticipation.Japanese Encephalitis Vector control by insecticidal sprayingwith appropriate insecticide for outbreakcontainment. Early diagnosis and prompt clinicalmanagement to reduce fatality. Health Education. Training of Medical Personnel andProfessionals.FilariasisFor elimination of Lymphatic Filariasis, following are thestrategies: Annual Mass Drug Administration (MDA) withsingle dose of DEC to all eligible population atrisk of Lymphatic Filariasis.Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 27
Home based management of Lymphodemacases.Hydrocelectomy.The diagnosis, treatment and examination are performedat CHCs as per the pattern of PHC. In addition, CHCsare the first referral units for treatment of severe andcomplicated malaria cases.Services to be provided are: Diagnosis of malaria cases, microscopicconfirmation and treatment. Cases of suspected JE and Dengue tobe provided symptomatic treatment,hospitalization and case managements. Complete treatment to Kala-azar cases in Kalaazarendemic areas. Complete treatment of micro-filaria positivecases with DEC and participation & arrangementfor Mass Drug Administration (MDA) alongwith preparedness of management of sidereactions.StandardsThe CHC Medical Officer should be well-trained inprevention and control of the Vector Borne. Diseasesand should carry out the following activities: He will refer all fever cases to malarialaboratory for blood smear collection andexamination before giving final prescription/medicines. He will supervise all Malaria Clinics and PHClaboratory in his area, see the quality ofblood smear collection, staining, efficiency ofmicroscopic examination and check whetherthe stain is filtered daily. He will also ensure/supervise that all positivecases get radical treatment within 48 hours ofexamination.DrugsHe will also ensure that sufficient stocks ofAntimalarial including Quinine tablets andinjectable Quinine and Artemisenine areavailable in CHC and also PHCs.He will ensure that malaria laboratory is keptin proper condition along with microscopeand other equipment.He will provide referral services to severecases of malaria.He will refer severe and complicated casesto District Hospital in case of emergency anddrug failure.He will also ensure that Filaria cases aremanaged at CHC and the Hydrocele cases areoperated.Chloroquine, Primaquine, SulphadoxinPyremethamine Combination, ArtemisinineDerivatives, Quinine Injections, Quinine tabletsand 5% Dextrose saline and DEC tablets.EquipmentMicroscope, Slides, Pricking Needles, Cotton,Stains, Staining Jars, Filter paper, Glassmarking pencil, Lint cloth and Glass wares forpreparation of stains and storage.IEC Material Display material like posters, banners andpermanent hoardings etc. Distribution material like handbills, pamphlets,booklets display cards etc. Training Materials like <strong>Guidelines</strong> on programmestrategies, dose-schedule cards etc.Diagnosis and Management of Vector borne Diseasesis to be done as per NVBDCP guidelines for PHC/CHC.28Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Annexure 5National Leprosy Eradication ProgrammeMinimum Services to be Availableat Community Health Centres(CHC)Diagnosis of Leprosy.Treatment.Management of Reactions.Counselling of patient on treatment, possibleside effects & lepra reactions.Advise to Patient on prevention of disabilitiesand self care.Manpower RequiredMedical Officer trained in leprosy diagnosis.Pharmacist to issue medicine and manageMDT Stock.Health Worker trained in identificationof leprosy lesions, its complications andmaintenance of records/reports.Diagnosis, classification and treatment of Leprosyshould be made according to programme guidelines.Standard MDT RegimensMDT should be is available in separate blister packs forMulti Bacillary (MB)- Adult, MB -Child, Pauci Bacillary (PB) -Adult & PB-Child. Each Blister Pack contains treatment for 4 weeks.Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 29
Annexure 6National Programme for Control of BlindnessStandards at Community HealthCentresPhysical Structure for Eye Care at CHCa.bEquipmentRefraction Room.Eye OT with Eye Ward, only if eye surgeonis posted. (number of beds based onworkload).For IOL SurgeryOperating microscopeA-Scan BiometerKeratometerSlit LampAutoRefractometerFlash AutoclaveStreak RetinoscopeTonometers (Schiotz)Direct OphthalmoscopeFor Primary Eye Care & Vision TestingTonometers (Schiotz)Direct OphthalmoscopeIlluminated Vision Testing DrumTrial Lens Sets with Trial FramesSnellen & Near Vision ChartsBattery Operated Torch (2)DrugsEye OintmentsAtropine (1%)Local antibiotic: Framycetin/Gentamicin etc.Local antibiotic steroid ointmentOphthalmic DropsXylocaine 4% (30 ml)Local antibiotic: Framycetin/Gentamicin etc.Local antibiotic steroid dropsPilocarpine Nitrate 2%Timolol 0.5%Homatropine 2%Tropicamide 1%InjectionsXylocaine 2% (30 ml)Inj Hyalase (Hyaluronidase)GentamycinBetamethasone/DexamethasoneInj. Maracaine (0.5%) (For regoinal anesthesia)Inj. AdrenalineRinger Lacate (540 ml) from reputed firmSurgical AccessoriesGauzeGreen ShadesBlades (Carbon Steel)Opsite surgical gauze (10 x 14 c. m.)Double needle Suture (commodity asstt. GOI)Visco-elastics from reputed firm30Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Annexure 7Integrated Disease Surveillance ProjectServices and Standards atCommunity Health CentresCHC will function as peripheral surveillance unit andcoallate, analyse and report information to DistrictSurveillance Unit as per IDSP reporting format atAnnexure 7A, 7B and 7C. In out-break situations,appropriate action will also be initiated.Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 31
Annexure 7 A: Form P (Weekly Reporting Format-IDSP)Name of Reporting Institution:I.D. No.:State: District: Block/Town/City:Officer-in-Charge Name: Signature:IDSP Reporting Week: Start Date: End Date: Date of Reporting:__/__/____ __/__/____ __/__/____Sl. No. Diseases/Syndromes No. of cases1 Acute Diarrhoeal Disease (including acute gastroenteritis)2 Bacillary Dysentery3 Viral Hepatitis4 Enteric Fever5 Malaria6 Dengue/DHF/DSS7 Chikungunya8 Acute Encephalitis Syndrome9 Meningitis10 Measles11 Diphtheria12 Pertussis13 Chicken Pox14 Fever of Unknow Origin (PUO)15 Acute Respiratory Infection (ARI) Influenza Like lllness (ILI)16 Pneumonia17 Leptospirosis18 Acute Flaccid Paralysis < 15 year of Age19 Dog bite20 Snake bite21 Any other State Specific Disease (Specify)22 Unusual Syndromes NOT Captured Above (Specify clinical diagnosis)Total New OPD attendance (Not to be filled up when data collected for indoor cases)Action taken in brief if unusual increase noticed in cases/deaths for any of the abovediseases32Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Annexure 7 B: Form L (Weekly Reporting Format-IDSP)Name of the Laboratory:Institution:State: District: Block/Town/City:Officer-in-Charge Name: Signature:IDSP Reporting Week: Start Date: End Date: Date of Reporting:__/__/____ __/__/____ __/__/____Diseases No. Samples Tested No. Found PositiveDengue/DHF/DSSChikungunyaJEMeningococcal MeningitisTyphoid FeverDiphtheriaCholeraShigella DysenteryViral Hepatitis AViral Hepatitis ELeptospirosisMalaria PV: PF:Other (Specify)Other (Specify)Line List of Positive Cases (Except Malaria cases)NameAge(Yrs)Sex(M/F)Address:Village/TownName ofTest DoneDiagnosis(Lab confirmed)Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 33
Annexure 7 C: Format for instantaneous reporting of EarlyWarning Signal/outbreaks as soon as it isdetectedState: District: Date of reporting:Is there any unusual increase in Cases/Deaths or unusual event in any area?If yes, provide the following information:yes/noDisease/Syndrome (Provisional/Confirmed)Area affected (Block, PHC, Sub-centre, Village)No. of casesNo. of deathsDate of start of the outbreakTotal population of affected area (Village)Salient epidemiological observationsLab results (type of sample, number of samples collected and tested, What test,where, results)Control measures undertaken (Investigated by RRT or not)Present statusAny other information* State SSU need to report instantaneously as well as weekly compilation on every Monday to the CSU including NIL reports.34Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Annexure 8Facility Based Maternal Death Review FormNote: This form must be completed for all deaths, including abortions and ectopic gestation related deaths, inpregnant women or within 42 days after termination of pregnancy irrespective of duration or site of pregnancy.Attach a copy of the case records to this form.Complete the form in duplicate within 24 hours of a maternal death. The original remains at the institution wherethe death occurred and the copy is sent to the person responsible for maternal health in the State.FB-MDR no:For Office use Only:Year:1. General InformationAddress of Contact Person at District and State:Residential Address of Deceased Woman:Address where Died:Name and Address of facility:Block:District:State:Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 35
2. Details of Deceased Womani.Name: /Age (years) : /Sex: /Inpatient Number:ii. Gravida: /Live Births(Para): /Abortions: /No. of Living children:iii. Timing of death: During pregnancy/ during delivery/ within 42 days of delivery/iv. Days since delivery/abortion:v. Date and time of admission:vi. Date/Time of death:3. Admission at Institution Where Death Occurred or from Where It was Reportedi .Type of facility where died:PHC 24 x 7 PHC SDH/RURALHOSPITALdistricthospitalmedicalcollege/tertiaryhospitalprivatehospitalPvt Clinicotherii.Stage of pregnancy/delivery at admission:Abortion Ectopic Pregnancy Not In Labour In Labour Postpartumiii.Stage of pregnancy/delivery when died:Abortion Ectopic Pregnancy Not In Labour In Labour Postpartumiv.Duration of time from onset of complication to admission:v. Condition on Admission: Stable/Unconscious/Serious/Brought dead/vi. Referral history: Referred from another centre ? How many centres?Type of centre?4. Antenatal CareReceived Antenatal care or not/Reasons for not receiving care/Type of antenatal care provided/High risk pregnancy : aware of risk factors?/what risk factors?36Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
5. Delivery, Puerperium and Neonatal Informationi. Details of labor :had labor pains or not stage of labor when died duration of labor.ii.iii.Details of delivery: undelivered/normal/assisted (forceps or vacuum) surgical intervention (C-section)Puerperium: Uneventful/Eventful (PPH/Sepsis etc.).Comments on labour, delivery and puerperium. (in box below)iv.Neonatal Outcome : stillborn/neonatal death immediately after birth/alive at birth/alive at 7 days.Comments on baby outcomes (in box below)6. InterventionsSpecific medical/surgical procedures/rescuscitation procedures undertaken7. Cause of Deatha.b.c.d.8. FactorsProbable direct obstetric (underlying) cause of death: Specify:Indirect Obstetric cause of death: Specify:Other Contributory (or antecedent) cause/s: Specify:Final Cause of Death: (after analysis)(other than medical causes listed above)a.b.c.d.Personal/FamilyLogisticsFacilities availableHealth personnel related9. Comments on Potential Avoidable Factors, Missed Opportunities and SubstandardcareIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 37
10. AutopsyPerformed/Not PerformedIf performed please report the gross findings and send the detailed report later11. Case Summary(please supply a short summary of the events surrounding the death):12. Form filled by13. Name14. Designation15. Institution and location16. Signature and Stamp17. Date38Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Annexure 9List Of Equipment In ChcStandard Surgical Set - I (Instruments) FRU (Essential)1 Tray, instrument/dressing with cover, 310 x 200 x 600 mm-ss 12 Gloves surgeon, latex sterilizable, size 6 123 Gloves surgeon, latex sterilizable, size 6-1/2 124 Gloves surgeon, latex sterilizable, size 7 125 Gloves surgeon, latex sterilizable, size 7-1/2 126 Gloves surgeon, latex sterilizable, size 8 127 Forceps, backhaus towel, 130 mm 48 Forceps, sponge holding, 228 mm 69 Forceps, artery, pean straight, 160 mm, stainless steel 410 Forceps hysterectomy, curved, 22.5 mm 411 Forceps, hemostatic, halsteads mosquito, straight, 125 mm-ss 612 Forceps, tissue, all/is 6x7 teeth, straight, 200 mm-ss 613 Forceps, uterine, tenaculum, 280 mm, stainless steel 114 Needle holder, mayo, straight, narrow jaw, 175 mm-ss 115 Knife-handle surgical for minor surgery # 3 116 Knife-handle surgical for major surgery # 4 117 Knife-blade surgical, size 11, for minor surgery, pkt of 5 318 Knife-blade surgical, size 15 for minor surgery, pkt of 5 419 Knife blade surgical, size 22, for major surgery, pkt of 5 320 Needles, suture triangular point, 7.3 cm, pkt of 6 221 Needles, suture, round bodied, 3/8 circle No. 12 pkt of 6 222 Retractor, abdominal, Deavers, size 3, 2.5 cm x 22.5 cm 123 Retactor, double-ended abdominal, Beltouis, set of 2 224 Scissors, operating curved mayo-blunt pointed 170 mm 125 Retractor abdominal, Balfour 3 blade self-retaining 126 Scissors, operating, straight, blunt point, 170 mm 127 Scissors, gauze, straight, 230 mm, stainless steel 1Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 39
28 Suction tube, 225 mm, size 23 F 129 Clamp intestinal, Doyen, curved, 225 mm, stainless steel 230 Clamp intestinal, Doyen straight, 225 mm, stainless steel 231 Forceps, tissue spring type, 160 mm, stainless steel 232 Forceps , tissue spring type, 250 mm, stainless steel. 1Standard Surgical Set – II (Essential)1 Forceps, tissue, 6 x 7 teeth, Thomas-Allis, 200 mm- ss 12 Forceps, backhaus towel, 130 mm, stainless steel 43 Syringe, anaesthetic (control), 10 ml, luer-glass 14 Syringe, hypodermic, 10 ml glass, spare for item 3 45 Needles, hypodermic 20G x 1-1/2” box of 12 16 Forceps, tissue, spring type, 145 mm, stainless steel 17 Forceps, tissue spring type 1 x 2 teeth, Semkins, 250 mm 18 Forceps, tissue spring type, 250 mm, stainless steel 19 Forceps, hemostat curved mosquito halsteads, 130 mm 610 Forceps, artery, straight pean, 160 mm, stainless steel 311 Forceps artery, curved pean, 200 mm, stainless steel 112 Forceps, tissue, Babcock, 195 mm, stainless steel 213 Knife handle for minor surgery No. 3 114 Knife blade for minor surgery No. 10, pkt of 5 815 Needle holder, straight narrow-jaw Mayo-Heger, 175 mm 116 Needle suture straight, 5.5 mm, triangular point, pkt of 6 217 Needle, Mayo, % circle, taper point, size 6, pkt of 6 2 218 Catheter urethral Nelaton solid-tip one-eye 14 Fr 119 Catheter urethral Nelaton solid-tip one-eye 16 Fr 120 Catheter urethral Nelaton solid-tip one-eye 18 Fr 121 Forceps uterine tenaculum duplay dbl-cvd, 280 mm 122 Uterine elevator (Ranathlbod), stainless steel 123 Hook, obstetric, Smellie, stainless steel 124 Proctoscope Mcevedy complete with case 125 Bowl, sponge, 600 ml, stainless steel 126 Retractor abdominal Richardson-Eastman, dbl-ended, set 2 127 Retractor abdominal Deaver, 25 mm x 3 cm, stainless steel 128 Speculum vaginal bi-valve graves, medium, stainless steel 129 Scisssors ligature, spencer straight, 130 mm, stainless steel 130 Scissors operating straight, 140 mm, blunt/blunt ss 131 Scissors operating curved, 170 mm, blunt/blunt ss 232 Tray instrument curved, 225 x 125 x 50 mm, stainless steel 133 Battery cells for item 24 2IUD Insertion Kit (Essential)1 Setal sterilization tray with cover size 300 x 220 x 70 mm, S/S, Ref IS:3993 12 Gloves Surgeon, latex, size 6-1/2 Ref. 4148 63 Gloves surgeon latex, size 7-1/2 Ref. 4148 64 Bowl, metal sponge, 600 ml, Ref. IS: 5782 15 Speculum vaginal bi-valve cusco’s graves small ss 140Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
6 Forceps sponge holding, straight 228 MMH Semken 200 mm 17 Sound uterine simpson, 300 mm graduated UB 20 mm 18 Forceps uterine tenaculum duplay DBL-CVD, 280 mm 19 Forceps tissue - 160 mm 110 Anterior vaginal wall retractor stainless 111 Torch without batteries 112 Gloves surgeon, latex, size 7, Ref: 4148 613 Gloves surgeon, latex size 6 Ref. IS: 4148 614 Battery dry cell 1.5 V ‘D’ Type for Item 7 G 115 Speculum vaginal bi-valve cusco’s/Grea Ves Medium ss 116 Forceps artery, straight, Pean, 160 mm 117 Scissors operating, straight, 145 mm, Blunt/Blunt 118 Forceps uterine vulsellum curved, Museux, 240 mm 119 Speculum vaginal double-ended #3 1CHC Standard Surgical Set – III (Essential)Tray, instrument/dressing with cover, 310 x 195 x 63 mm 1Forceps, backhaus towel, 130 mm, stainless steel 4Forceps, hemostat, straight, Kelly, 140 mm, stainless steel 4Forceps, hemostat, curved, Kelly, 125 mm, stainless steel 2Forceps, tissue Allis, 150 mm, stainless steel, 4 x 5 teeth 2Knife handle for minor surgery No. 3 1Knife blade for minor surgery, size 11, pkt of 5 10Needle hypodermic, Luer 22G x 11/4”, box of 12 1Needle hypodermic, Luer 250G x 3/4”, box of 12 1Needle, suture straight 5.5 cm, triangular point, pkt of 6 2Needle, suture, Mayo circle, taper point No. 6, pkt of 6 2Scissors, ligature, angled on flat, 140 mm, stainless steel 1Syringe anaesthetic control, Luer - 5 ml, glass 4Syringe 5 ml, spare for item 13 4Sterilizer, instrument 200 x 100 x 60 mm with burner ss 1Syringe, hypodermic, Luer 5 ml, glass 4Forceps, sterilizer, Cheatle, 265 mm, stainless steel 1Normal Delivery Kit (Essential)Trolley, dressing carriage size 76C, long x 46 cm wide and 84 cm high. Ref. IS 4769/1968 1Towel, trolley 84 cm x 54 cm 2Gown, operation, cotton 1Cap. operation, surgeon’s 36 x 46 cm 2Gauze absorbent non-sterile 200 mm x 6 m as per IS: 171/1985 2Tray instrument with cover 450 mm (L) x 300 mm (W) x 80 mm (H) 1Macintosh, operation, plastic 2Mask, face, surgeon’s cap of rear ties: B) Beret type with elastic hem 2Towel, glove 3Cotton wool absorbent non-sterilize 500 G 2Drum, sterilizing cylindrical - 275 mm Dia x 132 mm, ss as per IS: 3831/1979 2Table instrument adjustable type with tray ss 1Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 41
Standard Surgical Set – IV (Essential)Vaccum extractor, Malastrom 1Forceps obstetric, Wrigley's, 280 mm, stainless steel 1Forceps, obstetric, Barnes-Neville, with traction, 390 mm 1Forceps, sponge holding, straight 228 mm, stainless steel 4Forceps, artery, Spencer-Wells, straight, 180 mm-ss 2Forceps, artery, Spencer-Wells, straight, 140 mm-ss 2Holder, needle straight, Mayo-Hegar, 175 mm-ss 1Scissors, ligature, Spencer, 130 mm, stainless steel 1Scissors, episiotomy, angular, Braun, 145 mm, stainless steel 1Forceps, tissue, spring-type, 1 x 2 teeth, 160 mm-ss 1Forceps, tissue, spring-type, serrated ups, 160 mm-ss 1Catheter, urethral, rubber, Foley's 14 ER 1Catheter, urethral, Nelaton, set of five (Fr 12-20) rubber 1Forceps, backhaus towel -130 mm-ss 4Speculum, vaginal, Sim's, double-ended # 3-ss 1Speculum, vaginal, Hamilton-Bailey 1Standard Surgical Set – V (Essential)Forceps, obstetric, Neville-Barnes, W/traction 390 mm 1Hook, decapitation, Braun, 300 mm, stainless steel 1Hook, crochet, obstetric 300 mm, Smellie, stainless steel 1Bone, forceps, Mesnard 280 mm, stainless steelPerforator, Smellie, 250 mm, stainless steel 1Forceps, cranial, Gouss, straight, 295 mm-ss 1Cranioclast, Braun, stainless steel, 365 mm long 1Scissors ligature Spencer 130 mm, stainless steel 1Forceps sponge holding, 22.5 cm straight - ss 1Forceps, tissue, spring-type, 1 x 2 teeth, 160 mm, stainless steel 1Forceps, tissue, spring-type, serrated tips, 160 mm-ss 1Forceps, artery, Spencer-Wells, straight, 180 mm-ss 2Forceps, artery, Spencer-Wells, straight, 140 mm-ss 2Forceps, scalp flap, Willet's 190 mm -ss 4Forceps, Vulsellum, duplay double curved, 280 mm-ss 4Forceps, Vulsellum, duplay double curved, 240 mm-ss 1Catheter, urethral, 14 Fr. solid tip, one eye, soft rubber 3Holder, needle, Mayo-Hegar, narrow jaw, straight, 175 mm-ss 1Speculum vaginal bi-valve, Cusco-medium, stainless steel 1Speculum, vaginal sim's double-ended, size # 3-ss 1Forceps, backhaus towel, 130 mm, stainless steel 4Standard Surgical Set – VI (Essential)Forceps, sponge holding, straight, 225 mm, stainless steel 4Speculum, vaginal, Sim's double-ended size # 3 - ss 1Speculum, vaginal, weighted Auvard, 38 x 75 mm blade - ss 1Forceps, tenaculum, Teale's, 230 mm-ss 3 x 42Sound, uterine, Simpson, 300 mm with 200 mm graduations 142Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Dilator, uterine, double - ended hegar, set of 5 - ss 1Curette, uterine, sim's blunt, 26 cm x 11 mm size # 4-ss 2Curette, uterine, sim's sharp, 26 cm x 9 mm size # 3-ss 2Forceps, artery, Spencer-Well's straight, 140 mm-ss 1Forceps, tissue, spring-type, serrated tips, 160 mm-ss 1Forceps, ovum, Krantz, 290 mm, stainless steel 1MiscellaneousNSV Kit 2Laproscope 1Nebuliser 1Peak Expiratory Flow Rate (PEFR) Meter (Desirable) 1Equipment for Anaesthesia (Essential)Face mask, plastic w/rubber cushion & headstrap, set of 4 4Airway Guedel or Berman, autoclavable rubber, set of 6 2Laryngoscope, set with infant, child, adolescent blades 3Catheter, endotracheal w/cuff, rubber set of 4 3Catheter, urethral, stainless steel, set of 8 in case 2Forceps, catheter, Magill, adult and child sizes, set of 2 1Connectors, catheter, straight/curved, 3, 4, 5 mm (set of 6) 3Cuffs for endotracheal catheters, spare for item 4 4Breathing tubes, hoses, connectors for item 1, anti-static 4Valve, inhaler, chrome-plated brass, Y-shape 3Bag, breathing, self inflating, anti-static rubber, set of 4 2Vaporiser, halothane, dial setting 2Vaporiser, ether or methoxyflurane, wick type 2Intravenous set in box 6Needle, spinal, stainless set of 4 2Syringe, anesthetic, control 5 ml Luer mount glass 2Cells for item 3 2Equipment for Neo-natal Resuscitation (Essential)Catheter, mucus, rubber, open ended tip, size 14FR 2Catheter, nasal, rubber, open tip, funnel end, size 8Fr 2Catheter, endotracheal, open tip, funnel end rubber, 12Fr 3Stilette, curved, for stiffening tracheal catheter SS 1Catheter, suction, rubber, size 8Fr 3Laryngoscope, infant, w/three blades and spare bulbs. 1Lateral mask, with ventillatory bag, infant size 2Resuscitator, automatic, basinet type 1Lamp, ultra-violet (heat source) with floor stand 1Cells for item 6 (Laryngoscope) 2Oxygen Cylinders 1Nasal Prongs 5Thermometers 5Infantometer: Measuring range 33-100 cm 2Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 43
Stadiometer: Measuring range 60-200 cm 1Photo therapy Unit 1Radiant warmers 2Dextromsticks100 sticksNebulisers/MDI 1IV Canulas (22 G and 24 G)100 eachScalp vein set No. 22 and 24100 eachNasogastric tube ( 8,10,12 FG) 20Oropharyngeal airway (000-4 Guydel size)Plastic/disposable syringes including tuberculin 100IV infusion sets (adult and pediatric) 100Materials Kit for Blood Transfusion (Essential)Bovine albumin 20% testing agent, box of 10 X 5 ml vials 5Centrifuge, angle head for 6 X 1 5 ml tubes, 240 volt 1Bath, water, serological, with racks, cover, thermostat, 240 v 1Pipette, volumetric, set of six 1 mol/2 ml/3 ml/5 ml/10 ml/20 ml 1Test-tube without rim 75 X 12 mm HRG 12Test-tube without rim 1 50 X 16 mm, HRG 12Cuff, sphygmomanometer, set of two sizes – Child/Adult 1Needle, blood collection disposable, 1 7 g X 1-1/3 box of 100 1Ball, donor squeeze, rubber, dia, 60 mm 1Forceps, artery, Spencer-Wells, straight 140 mm, stainless steel 1Scissors, operating, straight 140 mm, blunt/jpoints, ss 1CPDA anti-coagulent, pilot bottle 350 mil for collection 20Microscope, binocular, inclined, 10 X 40 X 100 X magnificent 1Illuminator 1Slides, microscope, plain 25 X 75 mm, clinical, box of 100 1Equipment for Operation Theatre(Essential)Diathermy machineDressing drum all sizesLamps shadow less:Ceiling lampPortable typeSterilizerSuction ApparatusStand with wheel for single basinTable operation, hydraulic:MajorMinorTrolley for patientsTrolley for instrumentsX-ray view boxWheel chairsEquipment for Labour RoomAprons rubberCradles babyWheel ChairCabinet InstrumentDressing drumShadow less lampsTable forObstetric labourExamination44Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Trolley forPatientsDressingTorch (flash light)TraysVacuum ExtractorWeighing machine babyWheel chairsEquipment for RadiologyAprons lead ribberDiagnostic X-ray Unit 20 C 7300 m A with automaticdeviceDark room accessoriesDark room timerFilm clipsLead sheetsX-ray view boxX-ay protection screenX-ray film processing tankImmunization Equipment (Essential)ILR (Large) & DF (Large) with Voltage Stabilizer1 Assuming 30,000 population directly servedby CHC, 25/1000 live birth, 19.5 mixedantigens, 25% wastage & 25% buffer stock,80.6 cubic cm per child, and 33% space for aircirculation, the ILR storage volume requiredis =11.4 L.2 Ice pack making by DF.3 Stabilizer to protect the Cold Chain Equipmentfrom voltage fluctuation.4 However considering contingency plan LargeILR & ILR DF may be provided to the CHC.Cold Boxes (Large & Small):Small – one, Large – twoVaccine Carriers with Ice packsTwo per SC (maximum 2 per booth) + 1 forCHC: Transport of vaccines to session sites. For campaign, more vaccine carrier will berequiredSpare ice Pack Box8, 25 & 60 ice pack boxs per vaccine carrier, 5L cold box& 20L cold box respectivelyRoom Heater/Cooler for immunization clinic withelectrical fittingsThermometers Alcohol (stem) 2AD syringes AD syringes (0.5 ml & 0.1 ml) - need basedReconstitution syringes Reconstitution syringes (5ml)- need basedFull size steel Almirah for FW Clinic For storage ofregisters and reports and LogisticsFreeze Tag :Monitoring Freezing of vaccineWaste disposal twin bucket, hypochlorite solution/bleachChair for new staffs proposed-4Dustbin with lid-2Water receptacle-1Hub cutters-2Computer with Modem with UPS, Printer with InternetconnectionImmunization schedule printed on a tin platePosters/Paintings on key messagesRecords and ReportsImmunization register-1Vaccine stock & issue register-1Tally sheetsTemperature monitoring registers/chartAD syringes, Reconstitution syringes, other logistic stock& issue registerMonthly UIP reportsRI Monitoring ChartWeekly surveillance reports (AFP, Measles)Serious AEFI reportsOutbreak reportsTracking Bag and Tickler BoxIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 45
Equipment and Renewable required for the Newborn Corner and Newborn Stabilization Unit (Essential): givenin Annexure 1A and 1B respectivelyEquipment Required for Non- Communicable Diseases (Essential wherever the Programme is Being Implemented)NPPCDNationalProgrammefor Preventionand Control ofCancer, Diabetes,CardiovascularDiseases & Stroke(NPCDCS)PMROral Health••••••••••••••••••••••••••••••••••••Head LightEar speculaEar SyringeOtoscopeJobson Horne ProbeTuning forkNoise MakerConsumable for screening of cervical cancerDisposable tongue depressorPAP smear kitECG machine ordinary 1Cardiac Monitor with defibrillator 1Pulse Oximeter 1Infusion pump 1Ophthalmoscope (direct) 1Slit Lamp 1B.P.apparatus table model 4Stethoscope 4Shot wave diathermyUltra sound therapyInfra-red lamp (therapy)Neuromuscular StimulatorPocket TENSParaffin Wax bathHot packs with hydro collators.Exercise Table – 2 nosStatic CycleShoulder WheelCervical & Lumber tractionMedicine ballQuadriceps ExerciserCoordinator boardHand grips strength measurement kit.Kit for Neuro- Development assessment.CBR ManualsAssorted toys like sound making/colorfulgadgets/building blocks/peg boards/pictorialcharts and manualsDental Unit consisting of Dental Chair and set ofdental Equipment for examination, extractionand management of Dental & related problems.••••For screening of patients of hearingimpairment/deafnessFor diagnosis of common ear ProblemsFor early detection of hearing lossRemoval of foreign body from ear and noseFor early detection of common cancersPAP smearFor screening of patientsFor diagnosis and early detection of CVD, DM,StrokeAs PMR services would be provided with theposting of qualified paramedical these are allrequired equipmentNecessary for dental care servicesEquipment under National Health Programmes (as listed under each NHP) and Blood Storage equipment as atAnnexure - 11.46Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Annexure 10List of DrugsList of the drugs given under is not exhaustive and exclusive but has been provided for delivery of minimumassured services.Emergency Obstetric Care Drugs Kit for CHC/FRU (Essential)Sl. No. Name of the Drug/Form Dosage Quantity/Kit1 Halothane BP Containing 0.01 % w/w thymol IP; 200 mlin each Bottles2 Atropine Injection IP Atropine Sulphate IP 600 mg/ml; 02 ml ineach ampoule3 Thiopentone Injection IP Each vial containing Thiopentone SodiumIP 500 mg ; Capacity of vial 20 ml4 Bupivacaine Injection IP Bupivacaine Hydrochloride IP eq. toBupivaine hydrochloride anhydrous 5 mg/ml; 20 ml in each vial5 Lignocaine Injection IP Lignocaine Hydrochloride IP 5% w/v; 02 mlin each ampoule6 Lignocaine Injection IP Lignocaine Hydrochloride IP 2% w/v; 30 mlin each vial7 Diazepam Injection IP Diazepam IP 5 mg/ml; 2 ml in eachampoule8 Pentazocine Injection IP Pentazocine Lactate IP eq. to Pentazocine30 mg/ml; 01 ml in each ampoule9 Dexmethasone Injection IP Dexamethasone Sodium Phosphate IP eq.to Dexamethasone Phosphate, 4 mg/ml.;02 ml in each ampoule10 Promethazine Injection IP Promethazine hydrochloride IP, 25 mg/ml;02 ml in each ampoule5 Bottles50 ampoules100 Vials50 vials50 ampoules50 vials100 ampoules100 ampoules100 ampoules50 ampoules11 Nifedipine Capsules IP Nifedipine IP 10 mg 500 capsules12 Dopamine Injection USP Dopamine Hydrochloride USP 40 mg/ml; 25 vials05 ml in each vialIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 47
Sl. No. Name of the Drug/Form Dosage Quantity/Kit13 Digoxin Tablets IP Digoxin IP 250 mg/tab 500 tablets14 Methyldopa Tablets IP Methyldopa IP eq. to Methyldopa500 tabletsanhydrous 250 mg15 Frusemide Tablets IP Frusemide IP 40 mg 500 tablets16 Frusemide Injection IP Frusemide IP 10 mg/ml; 02 ml in each 100 ampoulesampoule17 Ampicillin Injection IP Ampicillin Sodium IP eq. to Ampicillin 1000 vialsanhydrous 250 mg /vial18 Gentamycin Injection IP Gentamycin Sulphate eq. to gentamycin 1000 vials40 mg/ml; 02 ml in each vial19 Amoxycillin Capsules IP Amoxycylline Trihydrate IP eq. to2000 capsulesamoxycylline 250 mg20 Norfloxacin Tablets IP Norfloxacin IP 400 mg 2000 tablets21 Doxycycline Capsules IP Doxycycline Hydrochloride eq. to1000 capsulesDoxycycline100 mg22 Metronidazole Tablets IP Metronidazole IP 400 mg 2000 tablets23 Methylergometrine Injection IP Methylergometrine maleate IP, 0.2 mg /ml; 500 ampoules01 ml in each ampoule24 Oxytocin Injection IP Oxytocin IP 5.0 I.U./ml; 02 ml in each 500 ampoulesampoule25 Etofylline BP plus Anhydrous Theophylline Etofylline BP 84.7 mg/ml & Theophylline IP 100 ampoulesIP Combination Injection (As per standardsprovided)eq. to Theophylline anhydrous, 25.3 mg/ml; 02 ml in each ampoule26 Hydrocortisone Acetate Injection IP Hydrocortisone Acetate IP 25 mg/ml; 02 ml 100 vialsin each vial27 Salbutamol Tablets IP Salbutamol sulphate eq. to Salbutamol 1000 tablets2 mg28 Adrenaline Injection IP 0.18% w/v of Adrenaline Tartrate or 100 ampoulesAdrenaline Tartrate IP eq. to adrenaline 1 mg/ml; 01 ml in each ampoule29 Succinylcholine Injection IP Succinylcholine Chloride IP 50 mg/ml; 30 vials10 ml in each vial30 Ketamine Injection IP Ketamine Hydrochloride eq. to Ketamine 50 vialsbase 10 mg/ml; 10 ml in each vial31 Diazepam Tablets IP Diazepam IP 5 mg 250 tablets32 Vecuronium Bromide Injection (as perstandards provided)Vecuronium Bromide USP 4 mg perampoule33 Pancuronium Bromide Injection BP Pancuronium Bromide BP 2 mg/ml; 02 mlin each ampoules34 Neostigmine Injection IP Neostigmine methylsulphate 0.5 mg/ml(??); 01 ml in each ampoule35 Benzylpenicillin Injection IP Benzylpenicillin Sodium IP eq. toBenzylpenicillin 300 mg/vial.36 Fortified Procaine Penicillin Injection IP Procaine Penicillin IP 300 mg andBenzylpenicillin Sodium/Potassium salt IPeq. to Benzylpenicillin 60 mg per vial37 Benzathine Penicillin Injection IP Benzathine penicillin IP 450 mg (6 lakh units)/vial500 ampoules500 ampoules500 ampoules2000 vials1000 vials100 vials48Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Sl. No. Name of the Drug/Form Dosage Quantity/Kit38 Trimethoprim & Sulphamethoxazole Trimethoprim IP 80 mg/Sulphamethoxzole 5000 tabletsTablets IPIP 400 mg39 Phenoxymethylpenicillin Potassium Phenoxymethylpenicillin Potassium 3000 tabletsTablets IP250 mg40 Fluconazole Tablets Fluconazole USP 150 mg1500 tablets(as per the standards provided)41 Cloxacillin Injection IP Cloxacillin Sodium IP 250 mg/vial 100 vials42 Metronidazole Injection IP (IV infusion) Metronidazole IP 5 mg/ml: 100 ml in each 100 bottlesbottle43 Ergometrine Tablets IP Ergometrine maleate IP 250 mcg 2000 tablets44 Phenytoin Tablets IP Phenytoin Sodium IP 100 mg 150 tablets45 Hydroxyprogestrone Injection IP Hydroxyprogesterone Hexanoate IP 100 vials250 mg/ml; 02 ml in each vial46 Norethisterone Acetate Tablets Norethisterone Acetate BP 5 mg1000 tablets(as per the standards provided)47 Insulin Injection IP Insulin IP (porcine/bovine/human) 20 vials40 units/ml; 10 ml in each vial48 Insulin Zinc Suspension Injection IP Insulin Zinc Suspension eq. to Insulin 10 vials40 units/ml; 10 ml in each vial49 Sodium Bicarbonate Injection IP Sodium Bicarbonate 7.5 % w/v; 10 ml in 100 ampoules(IV infusion)each ampoule50 Magnesium Sulphate Injection IP Magnesium Sulphate 50% w/v ; 02 ml in 50 vialseach vial51 Phenytoin Injection BP Phenytoin Sodium IP 50 mg/ml; 02 ml in 50 ampoules.each ampoule52 Oxygen IP Medical Oxygen in steel or aluminium, 2 Cylinderscylinder (10 litres water cap).with gasspecific PIN system53 Sodium Chloride Injection IP (I.V. Solution) Sodium Chloride IP 0.9 % w/v; 500 ml ineach bottle/pouch1000 FFS pouches/BFSbottles54 Dextrose Injection IP (I.V.Solution) Dextrose eq. to Dextrose anhydrous 5% w/v250 FFS pouches/BFSbottles55 Nitrous Oxide Gas IP Medical Nitrous Oxide B Type in steel or 2 Cylindersaluminium, Cylinder (10 litres water cap.)with gas specific PIN system56 Dextran 40 Injection IP (Plasma Volume expander)Dextrans 10 w/v; 500 ml in each bottle 10 bottles57 Sterile Water for injections IP 05 ml in each ampoule 1000 ampoules58 Infusion Equipment BIS IV set with hypodermic needle 21 G of 1.5” 900 nos.length59 Intracath Cannulas for Single useGauze 18, length 45 mm, Flow rate 90 ml/ 12 nos.(Intravascular Catheters) BISminute60 Intracath Cannula for Single useSize 22, Length 25 mm, Flow rate 35 ml/ 12 nos.(Intravascular Catheters) BISminute61 Hypodermic Syringe for Single use - 2 ml Cap. 2 ml + - 1.5%500 nos.BP/BIS62 Hypodermic Syringe for Single use - 5 mlBP/BISCap. 5 ml + - 1.5%500 nos.Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 49
Sl. No. Name of the Drug/Form Dosage Quantity/Kit63 Hypodermic Syringe for Single use - 10 ml Cap. 10 ml + - 1.5%500 nos.BP/BIS64 Hypodermic Syringe for Single use - 50 ml Cap. 50 ml + - 1.5%20 nos.BP/BIS65 Hypodermic Needle for Single use – Gauze Length, 25 +1/-2550 nos.22 BIS66 Hypodermic Needle for Single use – Gauze Length, 25 +1/-2500 nos.23 BIS67 Hypodermic Needle for Single use – Gauze Length, 25 +1/-2500 nos.24 BIS68 Compound Sodium Lactate Injection IP 0.24 % V/V of Lactic Acid (eq. to 0.32%w/v of Sodium Lactate), 0.6 % w/v Sodium1000 FFS pouches/BFSbottlesChloride, 0.04 % w/v Potassium Chlorideand 0.027 % w/v Calcium Chloride; 500 mlin each bottle/pouch.69 Surgical Gloves, Sterile BIS Size 6 500 pairs.70 Surgical Gloves, Sterile BIS Size 6.5 500 pairs71 Surgical Gloves, Sterile BIS Size 7 100 pairs.Drug Kit for Sick Newborn & Child Care - FRU/CHC1 Diazepam Inj. IP 5 mg per ml Inj. 2 ml Ampoule 60 Ampoules (For perrectally use only)2 Inj. Cefotaxime 1 gm Vial 100 Vial3 Inj. Cloxacillin 1 gm Vial 100 Vial4 Dexamethasone Sodium 4 mg per ml Inj. 2 ml ampoule 300 AmpoulesPhosphate inj. IP5 Aminophylline Inj. BP 25 mg per ml Inj. 10 ml Ampoule 60 Ampoules6 Adrenaline Bitartrate 1 mg per ml (1:1000 Inj. 1 ml Ampoule60 mpoulesInj. IPdilution)7 Ringer Lactate 500 ml 500 ml plastic pouch 300 Pouches8 Doxycycline Hydrochloride dispersible Tablets 300 Tablets9 Vit. K3 (Menadione Inj.) IP Inj. 10 mg per ml Inj. 1 ml ampoule 100 Ampoules10 Phenytoin 50 mg per ml Inj. 2 ml Ampoule 60 Ampoules11 Dextrose Inj. IP I.V. Solution 5% Inj. 500 ml plastic pouch 60 Plastic pouches12 Inj. Gentamycin 10 mg/ml Ampoule 150 Ampoules13 Water for injection 2 ml/ 5 ml Ampoule 300 Ampoules14 Inj. Lasix 20 mg/2ml 2 ml Ampoule 300 Ampoule15 Inj. Phenobarbitone 100 mg/ml 2 ml Ampoule 60 Ampoule16 Inj. Quinine 150 mg/ml 2 ml Ampoule 60 Ampoule17 Normal Saline 500 ml 500 mg Plastic pouch 60 Plastic pouches18 Inj. Ampicillin 500 mg/ 5ml Vial 150 Vial19 Inj. Chloramphenicol 1 gm/10 ml Vial 150 Vial20 Inj. Calcium Gluconate 10% 10 ml Ampoule 60 Ampoules21 Ciprofloxacin 100 mg dispersible Tablet 500 tablets22 Nebulisable Salbutamolnebusol solution (to beused with nebuliser)15 ml 100 (Nebuliser equipmentto be provided withNubulisable Salbutamol)50Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
23 Inj. Dopamine 200 mg/5 ml Ampoule 20 Ampoule24 Needles 23 G 75025 Disposable Syringe 1 ml/ 2ml/5 ml 1 ml-2002 ml-5005 ml-500List of Other Essential Drugs for ChcSl. No. Name of the Drug Route of administration/dosageform1 Lignocaine Hydrochloride Topical Forms 2-5%Strength2 Acetyl Salicylic Acid Tablets 75 mg, 100 mg 300 mg 350 mg3 Ibuprofen Tablets 200 mg, 400 mg4 Paracetamol Injection 150 mg/mlSyrupTablets125 mg/5 ml500 mg5 Chloroquine Phosphate Tablets 150 mgInjectionSyrup40 mg/ml6 Chlorpheniramine Maleate Tablets 4 mg50 ml/5 ml7 Prednisolone Tablets 5 mg, 10 mg8 Promethazine HCL Tablets 25 mg9 Phenobarbitone Tablets 30 mg. 60 mg10 Phenytoin Sodium Capsules or Tablets 50 mg, 100 mgSyrup25 mg/ml11 Albendazole Tablets 400 mgSuspension200 mg/ 5 ml12 Amoxicillin Powder for suspension 125 mg/5 ml13 Ciprofloxacin Hydrochloride Tablets 250 mg, 500 mgSuspension40 +200 mg/5 ml14 Clotrimazole Pessaries 100 mg, 200 mgGel 2%15 Sulfadoxine + Pyrimethamine Tablets 500 mg + 25 mg16 Ferrous Salt Tablets 60 mgOral solution25 mg17 Folic Acid Tablets 1 mg, 5 mg18 Isosorbide Mononitrate/Dinitrate Tablets 10 mg, 20 mg19 Amlodipine Tablets 2.5 mg, 5 mg, 10 mg20 Digoxin Injection 0.25 mg/mlElixir0.05 mg/ml21 Benzoic Acid + Salicylic Acid Ointment or Cream 6% + 3%22 Miconazole Ointment or Cream 2%23 Neomycin + Bacitracin Ointment 5 mg + 500 IU24 Silver Sulphadiazine Cream 1%Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 51
Sl. No. Name of the Drug Route of administration/dosageform25 Benzyl Benzoate Lotion 25%26 Acriflavin + Glycerin Solution27 Gentian Violet Paint 0.5%, 1%28 Hydrogen Peroxide Solution 6%29 Povidone Iodine Solution 5%, 10%30 Bleaching Powder Powder31 Potassium Permanganate Crystals for solution32 Aluminium Hydroxide + MagnesiumHydroxideTabletSuspension33 Domperidone Tablets 10 mg34 Local Anaesthetic, Astringent andAnti inflammatory MedicineSyrupOintment/suppository1 mg/ml35 Dicyclomine Hydrochloride Tablets 10 mgInjection10 mg/ml36 Oral Rehydration Salts Powder for solution As per IP37 Ciprofloxacin Hydrochloride Drops/Ointment 0.3%38 Tetracycline Hydrochloride Ointment 1%39 Alprozolam Tab 0.25 mg40 Salbutamol Sulphate Tablets 4 mgSyrupInhalation2 mg/5 ml100 mg/dose41 Glucose Injection 50% hypertonic42 Glucose with Sodium Chloride Injection 5% + 0.9%43 Ringer Lactate Injection44 Ascorbic Acid Tablets 100 mg, 500 mg45 Calcium salts Tablets 250 mg, 500 mgStrength46 Multivitamins (As per Schedule V) Tablets47 Atenolol Tablets 50 mg48 Fluoxetine Tablets 20 mg49 Amitryptiline Hcl Tablets 25 mg50 Bisacodyl Tablets 05 mg51 Tinidazole Tablets 300 mg,52 Daonil Tablets 5 mg53 Haloperidol Tablets 1, 2, 5 mg54 Sulphacetamide eye drops Drops55 Tab. MetoprololTablets12.5, 25 mg, 100 mgHydrochlorthiazide56 Tab Captopril Tablets 25 mg57 Glyceryl Trinitrate Inj. Inj58 Carbamazepine Tabs, syrup 100 mg, 200 mg59 Tab. Methyldopa Tablets 250 mg52Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Sl. No. Name of the Drug Route of administration/dosageform60 Tab. Enalapril Tablets 2.5/5mg61 Atorvastatin Tab Tablets 10 mg62 Inj. Streptokinase 15 lac vialInj. Streptokinase 7.5 lac vialInj.Inj.15 lac vial7.5 lac vial63 Inj. Heparin sod. 1000 IU Inj. 1000 IU64 Inj. Insulin RegularInsulin IntermediateInj.Inj.65 Tab. Metformin Tablets 500 mg66 Inj. Crocin Inj.67 Inj. Potassium chloride Inj.68 Inj. Buscopan Inj.69 Inj. Duvadilan Inj.70 Inj. Chlormycetin Inj.71 Inj. Manitol Inj.72 Inj. Chloroquine Inj.73 Inj. Pethidine Inj.74 Inj. Chlorpromazine Inj.75 Inj. Pheniramine (Avil) Inj.76 Inj. Dextrose (10%) Inj.77 Inj. Salbutamol MDI Inj.78 Inj. Anti Rabies Vaccine Inj. 1 ml79 Inj. Anti Rabies Senem Inj.80 Inj. Anti Snake Venom (Polyvalent) Inj. 10mlStrengthApart from drugs mentioned above, Drugs under various National Health Programmes and Vaccines as underImmunization Programme are to be provided.Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 53
List of Ayurvedic Medicines for Chcs1 Sanjivani Vati2 Godanti Mishran3 AYUSH-644 Lakshmi Vilas Rasa (Naradeeya)5 Khadiradi Vati6 Shilajatwadi Louh7 Swas Kuthara rasa8 Nagarjunabhra rasa9 Sarpagandha Mishran10 Punarnnavadi Mandura11 Karpura rasa12 Kutajaghan Vati13 Kamadudha rasa14 Laghu Sutasekhar rasa15 Arogyavardhini Vati16 Shankha Vati17 Lashunadi Vati18 Kankayana Vati19 Agnitundi Vati20 Vidangadi louh21 Brahmi Vati22 Sirashooladi Vajra rasa23 Chandrakant rasa24 Smritisagara rasa25 Kaishora guggulu26 Simhanad guggulu27 Yograj guggulu28 Gokshuradi guggulu29 Gandhak Rasayan30 Rajapravartini Vati31 Triphala guggulu32 Saptamrit Louh33 Kanchanara guggulu34 Ayush Ghutti35 Talisadi Churna36 Panchanimba Churna37 Avipattikara Churna38 Hingvashtaka Churna39 Eladi Churna40 Swadishta Virechan Churna41 Pushyanuga Churna42 Dasanasamskara Churna43 Triphala Churna44 Balachaturbhadra Churna45 Trikatu Churna46 Sringyadi Churna47 Gojihwadi kwath Churna48 Phalatrikadi kwath Churna49 54. Maharasnadi kwath Churna50 Pashnabhedadi kwath Churna51 Dasamoola Kwath Churna52 Eranda paka53 Haridrakhanda54 Supari pak55 Soubhagya Shunthi56 Brahma Rasayana57 Balarasayana58 Chitraka Hareetaki59 Amritarishta60 Vasarishta61 Arjunarishta62 Lohasava63 Chandanasava64 Khadirarishta65 Kutajarishta66 Rohitakarishta67 Ark ajwain68 Abhayarishta69 Saraswatarishta70 Balarishta71 Punarnnavasav72 Lodhrasava73 Ashokarishta74 Ashwagandharishta75 Kumaryasava76 Dasamoolarishta77 Ark Shatapushpa (Sounf)78 Drakshasava79 Aravindasava80 Vishagarbha Taila54Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
81 Pinda Taila82 Eranda Taila83 Kushtarakshasa Taila84 Jatyadi Taila/Ghrita85 Anu Taila86 Shuddha Sphatika87 Shuddha Tankan88 Shankha Bhasma89 Abhraka Bhasma90 Shuddha Gairika91 Jahar mohra Pishti92 Ashwagandha Churna93 Amrita (Giloy) Churna94 Shatavari Churna95 Mulethi Churna96 Amla Churna97 Nagkesar Churna98 Punanrnava Churna99 Dadimashtak Churna100 Chandraprabha Vati.101 Dhanwantara Taila102 Balaswagandhadi Taila103 Mahanarayana Taila104 Sahacharadi Taila105 Ksheerabala Taila106 Kaseesadi Taila107 Kolakulatthadi Udvarthana Churna108 Jatamayadi Udvarthana Churna109 Upanaha Churna110 Shadpala Ghrita111 Panchthiktha Guggulu Ghrita112 Panchagavya Ghrita113 Madanapippali Churna114 Saindhava Lavana115 Madhu116 Pippali Churna117 Shuddha Ghrita118 Trivrit Leha119 Dashmoola or Ransnadi Kwath Churna120 Manibhadra Guda121 Gandharvahastadi Kwath Churna122 Balaguluchyadi Kwath Churna123 Aragwadadi Kwath Churna124 Pure Ghrita125 Icchabhedi RasaList of Unani Medicines for CHCs1 Arq-e-Ajeeb2 Arq-e-Gulab3 Arq-e-Kasni4 Arq-e-Mako5 Barshasha6 Dawaul Kurkum Kabir7 Dawaul Misk Motadil Sada8 Habb-e-Aftimoon9 Habb-e-Bawasir Damiya10 Habb-e-Bukhars11 Habb-e-Dabba-e-Atfal12 Habb-e-Gule Pista13 Habb-e-Hamal14 Habb-e-Hilteet15 Habb-e-Hindi Qabiz16 Habb-e-Hindi Sual17 Habb-e-Hindi Zeeqi18 Habb-e-Jadwar19 Habb-e-Jawahir20 Habb-e-Jund21 Habb-e-Kabid Naushadri22 Habb-e-karanjwa23 Habb-e-Khubsul Hadeed24 Habb-e-Mubarak25 Habb-e-Mudirr26 Habb-e-Mumsik27 Habb-e-Musaffi28 Habb-e-Nazfuddam29 Habb-e-Nazla30 Habb-e-Nishat31 Habb-e-Raal32 Habb-e-Rasaut33 Habb-e-Shaheeqa34 Habb-e-ShifaIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 55
35 Habb-e-Surfa36 Habb-e-Tabashir37 Habb-e-Tankar38 Habb-e-Tursh Mushtahi39 Itrifal Shahatra40 Itrifal Ustukhuddus41 Itrifal Zamani42 Jawahir Mohra43 Jawarish Jalinoos44 Jawarish Kamooni45 Jawarish Mastagi46 Jawarish Tamar Hindi47 Khamira Gaozaban Sada48 Khamira Marwareed49 Kushta Marjan Sada50 Laooq Katan51 Laooq Khiyarshanbari52 Laooq Sapistan53 Majoon Arad Khurma54 Majoon Dabeedulward55 Majoon Falasifa56 Majoon Jograj Gugal57 Majoon Kundur58 Majoon Mochras59 Majoon Muqawwi-e-Reham60 Majoon Nankhwah61 Majoon Panbadana62 Majoon Piyaz63 Majoon Seer Alwikhani64 Majoon Suhag Sonth65 Majoon Suranjan66 Majoon Ushba67 Marham Hina68 Marham Kafoor69 Marham Kharish70 Marham Quba71 Marham Ral Safaid72 Qurs Aqaqia73 Qurs Dawaul Shifa74 Qurs Deedan75 Qurs Ghafis76 Qurs Gulnar77 Qurs Habis78 Qurs Kafoor79 Qurs Mulaiyin80 Qurs Sartan Kafoori81 Qurs Zaranbad82 Qurs Ziabetus Khaas83 Qurs Ziabetus Sada84 Qurs-e-Afsanteen85 Qurs-e-Sartan86 Qutoor-e-Ramad87 Raughan Baiza-e-Murgh88 Raughan Bars89 Raughan Kahu90 Raughan Kamila91 Raughan Qaranful92 Raughan Surkh93 Raughan Turb94 Roghan Luboob Saba95 Roghan Malkangni96 Roghan Qust97 Safoof Amla98 Safoof Chutki99 Safoof Dama Haldiwala100 Safoof Habis101 Safoof Muqliyasa102 Safoof Mustehkam Dandan103 Safoof Naushadar104 Safoof Sailan105 Safoof Teen106 Sharbat Anjabar107 Sharbat Buzoori Motadil108 Sharbat Faulad109 Sharbat Khaksi110 Sharbat Sadar111 Sharbat Toot Siyah112 Sharbat Zufa113 Sunoon Mukhrij-e-Rutoobat114 Tiryaq Nazla115 Tiryaq pechish116 Zuroor-e-Qula56Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
List of Siddha Medicines for Chcs1 Amai otu parpam For diarrhoea in childrenand indigestion2 Amukkarac curanam For general debility,insomnia3 Anna petic centuram For anaemia4 Antat Tailam For febrile convulsions5 Appirakac centuram Diabetes mellitus6 Arakkut Tailam Headache and sinusinfection7 Arumukac Centuram Arthritis8 Atotataik kuti nir cough and cold9 Atatotai manappaku cough and cold10 Atatotai nei cough and wheeze11 Aya jampirac karpam anaemia12 Aya Kantac centuram aneamia13 Canku parpam anti allergic14 Cantamarutac Centuram arthritis15 Canta cantirotayam fevers and jaundice16 Carapunka Vilvati ilakam nervine tonic17 Cati Campirak Kulampu Nausea and vomiting18 Cempu Parpam peptic ulcer19 Cilacattu Parpam Urinary infection, whitedischarge20 Cilntil Curanam Diabetes mellitus21 Ciropara Nivarana Tailam Headache and sinus22 Cirra Muttit Tailam Neuritis, uterineproblems23 Civanar Amirtam Anti-allergic, bronchialasthma24 Comput Tinir Indigestion, loss ofappetite25 Cukkut Tailam Headache and earache26 Cuvacakkutori mathiral Asthma and cough27 Elatic curanam Allergy, fever in primarycomplex28 IIaku Viamuttit Tailam Hemiplegia29 Impural IIakam Bleedings30 Impural Vatakam Blood vomiting31 Inicic Curanam Indigestion, flatulence32 Iraca Kanti Meluku Skin infections, venerealinfections33 Iti Vallati Venereal uncer34 Kaiyan Tailam Cough with expectoration35 Kantaka Racayanam Skin diseases and urinaryinfections36 Kapa Curak Kutinir Fevers37 Karappan Tailam Eczema38 Karunai Ilakam Piles39 Kasturik karuppu Fever, cough, allergicbronchitis40 Kauri CintamanicCenturamLiver disorders, fever,fistula41 Kecari Ilakam Dropsy, amoebicdysentery42 Kilanellit Tailam Jaundice, giddiness,neuritis43 Kilincil Meluku Cracks on the heel andsole44 Korocanai mattirai Sinus, fits45 Kunkiliya parpam Urinary infection, whitedischarge46 Kunkumappu Mattirai Peptic ulcer, habitualconstipation47 Kunkiliya Vennay External application forpiles and scalps48 Kumak Kutori Peptic ulcer49 Kuntarikat Tailam Swelling andinflammation50 Man Kompup Parpam Chest pain51 Manturati Ataik Kutinir Anaemia52 Mattan Tailam Ulers, carbuncle andgangrence53 Matulai Manappaku Nausea, vomiting,anaemia54 Mayanat Tailam Swelling, inflammation55 Mayilirakatic Curanam Hiccup56 Mekanatak Kulikai Constipation57 Murukkan Vitai Mattirai Intestinal worms58 Muttuc cippi Parpam Diarrhea in children59 Naciroka Nacat Tailam Nasal problems60 Naka Parpam Diuretic61 Nantukkal Parpam Diuretic62 Nattai Parpam Bleeding piles63 Nellikkai Ilakam TonicIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 57
64 Neruncik Kutinir Diuretic65 Nilavakaic Curanam Constipation66 Nila Vempuk Kutinir Fever67 Noccit Tailam Sinus68 Omat Tinir Indigestion69 Palacancivi mattirai Fever in children,indigestion70 Palakarai Parpam Anti-allergic71 Panca Lavana Parpam Hyper acidity72 Parankip pattaicSkin diseasesCuranam73 Paankip PattaiSkin diseasesIracayanam74 Parankip Pattaip Skin diseasesPatankam75 Patikara parpam Urinary infection,stomatitis76 Pattuk karuppu DUB, painfulmenstruation77 Pavala Parapam Cough and fever78 Peranta Parpam No.1 Fits79 Pinacat tailam Sinus80 Pirami Ney Nervine tonic81 Pirammanta pairavam Fevers82 Punkat Tailam Injury and ulcers83 Talampu mattirai Toxic fever84 Talicati Vatakam Cough85 Tayirc Cuntic Curanam Diarrhea, used as ORS86 Terran kottai Ilakam Tonic, used in bleedingpiles87 Tiripalaic Curanam Styptic and tonic88 Tipplili Iracayanam Cough89 Uluntut Tailam Musclar atrophy,deafness90 Vacanta Kucumakaram Fever, cough, and cold inchild91 Veti Anna PeticCenturamDropsy92 Vilvati Ilakam Tonic93 Visnu Cakkaram PleurisyPatent & Proprietary Drug1 777 Oil for PsoriasisList of Homeopathy Medicines for CHCsSl. No. Name of Medicine Potency1 Abrotanum 302 Abrotanum 2003 Absinthium Q4 Aconite Nap. 65 Aconite Nap. 306 Aconite Nap. 2007 Aconite Nap. 1M8 Actea Racemosa 309 Actea Racemosa 20010 Aesculus Hip 3011 Aesculus Hip 20012 Aesculus Hip 1M13 Agaricus musca. 3014 Agaricus musca 20015 Allium cepa 616 Allium cepa 3017 Allium cepa 20018 Aloe soc. 619 Aloe soc. 3020 Aloe soc. 200Sl. No. Name of Medicine Potency21 Alumina 3022 Alumina 20023 Ammon Carb 3024 Ammon Carb 20025 Ammon Mur 3026 Ammon Mur 20027 Ammon Phos 3028 Ammon phos 20029 Anacardium Ori. 3030 Anacardium Ori. 20031 Anacardium Ori. 1M32 Angustura vera Q33 Anthracinum 20034 Anthracinum 1M35 Antim Crud 3036 Antim Crud 20037 Antim Crud 1M39 Antimonium Tart 3X40 Antimonium Tart 641 Antimonium Tart 3058Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Sl. No. Name of Medicine Potency42 Antimonium Tart 20043 Apis mel 3044 Apis mel 20045 Apocynum Can Q46 Apocynum Can 3047 Arg. Met 3048 Arg Met. 20049 Arg. Nit. 3050 Arg. Nit. 20051 Arnica Mont. Q52 Arnica Mont 3053 Arnica Mont 20054 Arnica Mont 1M55 Arsenicum Alb. 656 Arsenicum Alb. 3057 Arsenicum Alb. 20058 Arsenicum Alb. 1M59 Aurum Met. 3060 Aurum Met. 20061 Bacillinum 20062 Bacillinum 1M63 Badiaga 3064 Badiaga 20065 Baptisia Tinct. Q66 Baptisia Tinct 3067 Baryta Carb. 3068 Baryta Carb. 20069 Baryta Carb. 1M70 Baryta Mur. 3X71 Belladonna 3072 Belladonna 20073 Belladonna 1M74 Bellis Perennis Q75 Bellis Perennis 3076 Benzoic Acid 3077 Benzoic Acid 20078 Berberis Vulgaris Q79 Berberis Vulgaris 3080 Berberis Vulgaris 20081 Blatta Orientalis Q82 Blatta Orientalis 3083 Blumea Odorata Q84 Borax 30Sl. No. Name of Medicine Potency85 Bovista 3086 Bromium 3087 Bryonia Alba 3X88 Bryonia Alba 689 Bryonia Alba 3090 Bryonia Alba 20091 Bryonia Alba 1M92 Bufo rana 3093 Carbo veg 3094 Carbo veg 20095 Cactus G. Q96 Cactus G. 3097 Calcarea Carb 3098 Calcarea Carb 20099 Calcarea Carb 1M100 Calcarea Fluor 30101 Calcarea Fluor 200102 Calcarea Fluor 1M103 Calcarea Phos 30104 Calcarea Phos 200105 Calcarea Phos 1M106 Calendula Off Q107 Calendula Off 30108 Calendula Off 200109 Camphora 6110 Camphora 200111 Cannabis Indica 6112 Cannabis Indica 30113 Cantharis Q114 Cantharis 30115 Cantharis 200116 Capsicum 30117 Capsicum 200118 Carbo Animalis 30119 Carbo Animalis 200120 Carbolic Acid 30121 Carbolic Acid 200122 Carduus Mar Q123 Carduus Mar 6124 Carduus Mar 30125 Carcinosinum 200126 Carcinosinum 1M127 Cassia sophera QIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 59
Sl. No. Name of Medicine Potency128 Caulophyllum 30129 Caulophyllum 200130 Causticum 30131 Causticum 200132 Causticum 1M133 Cedron 30134 Cedron 200135 Cephalendra Indica Q136 Chamomilla 6137 Chamomilla 30138 Chamomilla 200139 Chamomilla 1M140 Chelidonium Q141 Chelidonium 30142 Chin Off Q143 Chin Off 6144 Chin Off 30145 Chin Off 200146 Chininum Ars 3X147 Chininum Sulph 6148 Cicuta Virosa 30149 Cicuta Virosa 200150 Cina Q151 Cina 3X152 Cina 6153 Cina 30154 Cina 200155 Coca 200156 Cocculus Indicus 6157 Cocculus Indicus 30158 Coffea Cruda 30159 Coffea Cruda 200160 Colchicum 30161 Colchicum 200162 Colocynthis 6163 Colocynthis 30164 Colocynthis 200165 Crataegus Oxy Q166 Crataegus Oxy 3X167 Crataegus Oxy 30168 Crataegus Oxy 200169 Crotalus Horridus 200170 Croton Tig. 6Sl. No. Name of Medicine Potency171 Croton Tig. 30172 Condurango 30173 Condurango 200174 Cuprum met. 30175 Cuprum met. 200176 Cynodon Dactylon Q177 Cynodon Dactylon 3X178 Cynodon Dactylon 30179 Digitalis Q180 Digitalis 30181 Digitalis 200182 Dioscorea 30183 Dioscorea 200184 Diphtherinum 200185 Drosera 30186 Drosera 200187 Dulcamara 30188 Dulcamara 200189 Echinacea Q190 Echinacea 30191 Equisetum 30192 Equisetum 200193 Eupatorium Perf. 3X194 Eupatorium Perf. 30195 Eupatorium Perf. 200196 Euphrasia Q197 Euphrasia 30198 Euphrasia 200199 Ferrum Met. 200200 Flouric Acid 200201 Formica Rufa 6202 Formica Rufa 30203 Gelsimium 3X204 Gelsimium 6205 Gelsimium 30206 Gelsimium 200207 Gelsimium 1M208 Gentiana Chirata 6209 Glonoine 30210 Glonoine 200211 Graphites 30212 Graphites 200213 Graphites 1M60Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Sl. No. Name of Medicine Potency214 Guaiacum 6215 Guaiacum 200216 Hamamelis Vir Q217 Hamamelis Vir 6218 Hamamelis Vir 200219 Helleborus 6220 Helleborus 30221 Hepar Sulph 6222 Hepar Sulph 30223 Hepar Sulph 200224 Hepar Sulph 1M225 Hippozaenium 6226 Hydrastis Q227 Hydrocotyle As. Q228 Hydrocotyle As. 3X229 Hyocyamus 200230 Hypericum Q231 Hypericum 30232 Hypericum 200233 Hypericum 1M234 Ignatia 30235 Ignatia 200236 Ignatia 1M237 Iodium 30238 Iodium 200239 Iodium 1M240 Ipecacuanha Q241 Ipecacuanha 3X242 Ipecacuanha 6243 Ipecacuanha 30244 Ipecacuanha 200245 Iris Tenax 6246 Iris Veriscolor 30247 Iris Veriscolor 200248 Jonosia Ashoka Q249 Justicia Adhatoda Q250 Kali Bromatum 3X251 Kali Carb 30252 Kali Carb 200253 Kali Carb 1M254 Kali Cyanatum 30255 Kali Cyanatum 200256 Kali lod 30Sl. No. Name of Medicine Potency257 Kali lopd 200258 Kali Mur 30259 Kali Mur 200260 Kal Sulph 30261 Kalmia Latifolium 30262 Kalmia Latifolium 200263 Kalmia Latifolium 1M264 Kreosotum Q265 Kreosotum 30266 Kreosotum 200267 Lae Defloratum 30268 Lae Defloratum 200269 Lac Defloratum 1M270 Lac Can 30271 Lac Can 200272 Lachesis 30273 Lachesis 200274 Lachesis 1M275 Lapis Albus 3X276 Lapis Albus 30277 Ledum Pal 30278 Ledum Pal 200279 Ledum Pal 1M280 Lillium Tig. 30281 Lillium Tig. 200282 Lillium Tig. 1M283 Lobella inflata Q284 Lobella inflata 30285 Lycopodium 30286 Lycopodium 200287 Lycopodium 1M288 Lyssin 200289 Lyssin 1M290 Mag.Carb 30291 Mag.Carb 200292 Mag Phos 30293 Mag Phos 200294 Mag Phos 1M295 Medorrhinum 200296 Medorrhinum 1M297 Merc Cor 6298 Merc Cor 30299 Merc Cor 200Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 61
Sl. No. Name of Medicine Potency300 Merc Sol 6301 Merc Sol 30302 Merc Sol 200303 Merc Sol 1m304 Mezerium 30305 Mezerium 200306 Millefolium Q307 Millefolium 30308 Muriatic Acid 30309 Muriatic Acid 200310 Murex 30311 Murex 200312 Mygale 30313 Naja Tri 30314 Naja Tri 200315 Natrum Ars 30316 Natrum Ars 200317 Natrum Carb 30318 Natrum Carb 200319 Natrum Carb 1M320 Natrum Mur 6321 Natrum Mur 30322 Natrum Mur 200323 Natrum Mur 1M324 Natrum Phos 30325 Natrum Sulph 30326 Natrum Sulph 200327 Natrum Sulph 1M328 Nitric Acid 30329 Nitric Acid 200330 Nitric Acid 1M331 Nux Vomica 6332 Nux Vomica 30333 Nux Vomica 200334 Nux Vomica 1M335 Nyctenthus Arbor Q336 Ocimum Sanctum Q337 Oleander 6338 Petroleum 30339 Petroleum 200340 Petroleum 1M341 Phosphoric Acid Q342 Phosphoric Acid 30Sl. No. Name of Medicine Potency343 Phosphoric Acid 200344 Phosphoric Acid 1M345 Phosphorus 30346 Phosphorus 200347 Phosphorus 1M348 Physostigma 30349 Physostigma 200350 Plantago Major Q351 Plantago Major 6352 Plantago Major 30353 Platina 200354 Platina 1M355 Plumbum Met 200356 Plumbum Met 1M357 Podophyllum 6358 Podophyllum 30359 Podophyllum 200360 Prunus Spinosa 6361 Psorinum 200362 Psorinum 1M363 Pulsatilla 30364 Pulsatilla 200365 Pulsatilla 1M366 Pyrogenium 200367 Pyrogenium 1M368 Ranunculus bulbosus 30369 Ranunculus bulbosus 200370 Ranunculus repens 6371 Ranunculus repens 30372 Ratanhia 6373 Ratanhia 30374 Rauwolfia serpentina Q375 Rauwolfia serpentina 6376 Rauwolfia serpentina 30377 Rhododendron 30378 Rhododendron 200379 Rhus tox 3X380 Rhus tox 6381 Rhus tox 30382 Rhus tox 200383 Rhus tox 1M384 Robinia 6385 Robinia 3062Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Sl. No. Name of Medicine Potency386 Rumex crispus 6387 Rumex crispus 30388 Ruta gr 30389 Ruta gr 200390 Sabal serreulata Q391 Sabal serreulata 6392 Sabina 3X393 Sabina 6394 Sabina 30395 Sang.can 30396 Sang.can 200397 Sarsaprilla 6398 Sarsaprilla 30399 Secalecor 30400 Secalecor 200401 Selenium 30402 Selenium 200403 Senecio aureus 6404 Sepia 30405 Sepia 200406 Sepia 1M407 Silicea 30408 Silicea 200409 Silicea 1M410 Spigellia 30411 Spongia tosta 6412 Spongia tosta 30413 Spongia tosta 200414 Stannum 30415 Stannum 200416 Staphisagria 30417 Staphisagria 200418 Staphisagria 1M419 Sticta pulmonaria 6420 Sticta pulmonaria 30421 Stramonium 30422 Stramonium 200423 Sulphur 30424 Sulphur 200Sl. No. Name of Medicine Potency425 Sulphur 1M426 Sulphuric acid 6427 Sulphuric acid 30428 Syphilinum 200429 Syphilinum 1M430 Tabacum 30431 Tabacum 200432 Tarentula cubensis 6433 Tarentula cubensis 30434 Tellurium 6435 Tellurium 30436 Terebinthina 6437 Terebinthina 30438 Terminalia arjuna Q439 Terminalia arjuna 3X440 Terminalia arjuna 6441 Thuja occidentalis Q442 Thuja occidentalis 30443 Thuja occidentalis 200444 Thuja occidentalis 1M445 Thyroidinum 200446 Thyroidinum 1M447 Tuberculinum bov 200448 Uran.Nit 3X449 Urtica urens Q450 Urtica urens 6451 Ustilago 6452 Verat alb 6453 Viburnan opulus 6454 Viburnan opulus 30455 Viburnan opulus 200456 Vipera tor 200457 Vipera tor 1M458 Verat viride 30459 Verat viride 200460 Viscum album 6461 Wyethia 6462 Wyethia 30463 Wyethia 200Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 63
Sl. No. Name of Medicine Potency464 Zinc met 200465 Zinc met 1M466 Zink phos 200467 Zink phos 1M468 Globules 20 no.469 Sugar of milk470 Glass Piles 5 ml471 Glass Piles 10 ml472 Butter Paper473 Blank Sticker Ointments 1/2*3/2 inch474 Aesculus HipSl. No. Name of Medicine Potency475 Arnica476 Calendula477 Cantharis478 Hamamelis Vir479 Rhus tox480 Twelve BiochemicMedicines481 Cineraria Eye Drop482 Euphrasia Eye Drop483 Mullein Oil ( Ear Drop )6x & 12x64Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Annexure 11Extracts from National <strong>Guidelines</strong> on BloodStorage Facilities at FRUsRequirementsSpace: The area required for setting up the facility is only10 square meters, well-lighted, clean and preferablyair-conditioned.Manpower: One of the existing doctors and techniciansshould be designated for this purpose. They should betrained in the operation of blood storage centers andother basic procedures like storage, grouping, crossmatchingand release of blood.The medical officer designated for this purpose will beresponsible for overall working of the storage center.Electricity: 24 hours supply is essential. Provision ofback-up generator is required.Equipment: Each FRU should have the following:1234.Blood Bank refrigerators having a storagecapacity of 50 units of blood.Deep freezers for freezing ice packs requiredfor transportation. The deep freezersavailable in the FRUs under the ImmunizationProgramme can be utilized for this purpose.Insulated carrier boxes with ice packs formaintaining the cold chain during transportationof blood bags.Microscope and centrifuge: since these are anintegral part of any existing laboratory, thesewould already be available at the FRUs. Theseshould be supplied only if they are not alreadyavailable.Consumables: There should be adequate provisionfor consumables and blood grouping reagents.The following quantities would suffice the annualrequirement of an FRU with up to 50 beds.Consumables QuantityPasteur pipette 12 dozens/yearGlass tubes 7.5 to 10 mm - 100 dozens/yearGlass slides 1” x 2” boxes of 20 or 25 each/yearTest tube racks 6 racks, each for 24 tablesRubber teats 6 dozens/yearGloves Disposable rubber gloves 500 pairs per yearBlotting tissue paper As requiredMarker pencil (alcohol based) As requiredTooth picks As requiredReagents: All the reagents should come from theMother Blood Bank.Anti-A 2-vials each per monthAnti-B 2-vials each per monthAnti-AB 2-vials each per monthAnti-D (Blend of IgM & IgG) 2 vials each per monthAntihuman Globulin 1 vial per month(Polyclonal IgG & Complement)Since quality of the reagents is an important issue, thesupplies of these should be made from the same bloodIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 65
ank/centre from where blood is obtained. For thispurpose, State Governments/Union Territories shouldprovide the additional budgetary requirements to themother blood bank/centre.Disinfectants: Bleach & Hypochlorite Solution - Asrequired.Suggested Quantities of WholeBlood Units to he Available at aBlood Storage Unit5 units each of A, B, O (Positive)2 units of AB (Positive)1 units each of A, B & O (Negative)This can be modified according to the actualrequirement.Storage & TransportationCold chain: It is necessary to maintain the cold chainat all levels i.e. from the mother centre to the bloodstorage centre to the issue of blood. This can beachieved by using insulated carrier boxes. Duringtransportation, the blood should be properly packedinto cold boxes surrounded by the ice packs. Ice, if usedshould be clean and should not come in direct contactwith the blood bags. The blood should be kept in bloodbank refrigerator at 4°- 6°c ± 2°c. The temperature ofthe blood should be monitored continuously.Storage: The storage center should check the conditionof blood on receipt from the mother center and alsoduring the period of storage. The responsibility of anyproblem arising from storage, cross matching, issueand transfusion will be of the storage center. Any unitof blood showing hemolysis, turbidity or change incolour should not be taken on stock for transfusion. Duecare should be taken to maintain sterility of blood bykeeping all storage areas clean. The expiry of the bloodis normally 35/42 days depending on the type of bloodbags used. The Medical Officer in-charge should ensurethat unused blood bags should be returned to themother center at least 10 days before the expiry of theblood and fresh blood obtained in its place. The bloodstorage centers are designed to ensure rapid and safedelivery of whole blood in an emergency. The detail ofstorage of packed cells, fresh frozen plasma and plateletsconcentrate are therefore not given in these guidelines.In case, however, these are required to be stored, thestorage procedures of the mother blood bank shouldbe followed.Issue of BloodPatients blood grouping and cross matching shouldinvariably be carried out before issue of blood. A properrecord of this should be kept.First In and First Out (FIFO) policy, whereby blood closerto expiry date is used first, should be followed.DisposalSince all the blood bags will already be tested by themother center, disposal of empty blood bags should bedone by landfill. Gloves should be cut and put in bleachfor at least one hour and then disposed as normalwaste.Documentation & RecordsThe center should maintain proper records forprocurement, cross matching and issue of blood andblood components. These records should be kept for atleast 5 years.TrainingTraining of doctors and technicians, who will beresponsible for the Blood Storage Center, should becarried out for 3 days in an identified center as per theguidelines. Training will include:Pre-transfusion checking. i.e. patient identityand grouping.Cross matching.Compatibility.Problems in grouping and cross matching.Troubleshooting.Issue of blood.Transfusion reactions and its management.Disposal of blood bags.66Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
The states will have to identify the institutions wheretraining of the staff responsible for running the bloodstorage centre is to be held. These could be the bloodbanks at Medical Colleges, Regional Blood Banks,Indian Red Cross Blood Banks, or any other well setuplicensed Blood Bank, provided they have the necessaryinfrastructure for undertaking training.The training will be for three-days duration duringwhich the Medical Officer and the technician fromthe identified FRUs will be posted at the traininginstitution.A “Standard Operating Procedures Manual” (SOPM)has been developed and is part of these guidelines.This SOPM will be used as the training material.A copy of this SOPM will be made available to theMedical Officer for use in his Blood Storage Center forundertaking storage, grouping, cross matching andtransfusion.In addition to the training of the above Medical Staff,it is considered necessary that the clinicians whowill be responsible for prescribing the use of bloodare also sensitized on the various parameters ofblood transfusion. For this the “Clinician’s Guide toAppropriate Use of Blood” has been developed. Itis suggested that one-day sensitization programmefor the clinicians may be organized at the DistrictHospital/Medical College.Government of India will make the expenditure for theabove-mentioned trainings, available as per the normsof training under the RCH Programme. This training will,however, be coordinated by the Training Division ofDepartment of Family Welfare. The states are requiredto include training as part of the overall State ActionPlan for establishing Blood Storage Centers.Equipment for Laboratory Tests & BloodTransfusionRod, flint-glass, 1000 x 10 mm dia, set of two 2.Cylinder, measuring, graduated W/pouring lip, glass, 50 ml 2.Bottle, wash, polyethylene W/angled delivery tube, 250 ml 1.Timer, clock, interval, spring wound, 60 minutes x 1 minute 1.Rack, slide drying nickel/silver, 30 slide capacity 1.Tray, staining, stainless steel 450 x 350 x 25 mm 1.Chamber, counting, glass, double neubauer ruling 2.Pipette, serological glass, 0.05 ml x 0.0125 ml 6.Pipette, serological glass, 1.0 ml x 0.10 ml 6.Counter, differential, blood cells, 6 unit 1.Centrifuge, micro-hematocrit, 6 tubes, 240v 1.Cover glass for counting chamber (item 7), Box of 12 1.Tube, capillary, heparinized, 75 mm x 1.5 mm, vial of100 10.Lamp, spirit W/screw cap. Metal 60 ml 1.Lancet, blood (Hadgedorn needle) 75 mm pack of 10 ss 10.Benedict’s reagent qualitative dry components forsoln 1.Pipette measuring glass, set of two sizes 10 ml,20 ml 2 Test tube, w/o rim, heat resistant glass, 100 x13 mm 24.Clamp, test-tube, nickel plated spring wire, standardtype 3.Beaker, HRG glass, low form, set of two sizes, 50 ml, 150 ml 2.Rack, test-tube wooden with 12 x 22 mm dia holes 1.Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 67
Annexure 12List of Diagnostic ServicesList of Diagnostic ServicesSl. No. Speciality Diagnostic Services/TestsI CLINICAL PATHOLOGYa) Haematology Haemoglobin estimationTotal Leucocyte countDifferential Leucocyte countAbsolute Eosinophil countReticulocyte countTotal RBC countE.S.R.Peripheral Blood SmearMalaria/Filaria ParasitePlatelet countPacked Cell volumeBlood groupingRh typingBlood Cross matchingb) Urine Analysis Urine for Albumin, Sugar, Deposits, bile salts, bile pigments, acetone,specific gravity, Reaction (pH)c) Stool Analysis Stool for Ovacyst (Eh)Hanging drop for V. CholeraOccult bloodII PATHOLOGYa) Sputum Sputum cytologyIII MICROBIOLOGY Smear for AFB, KLBGrams Stain for Throat swab, sputum etc.68Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Sl. No. Speciality Diagnostic Services/TestsIV SEROLOGY VDRLPregnancy test (Urine gravindex)WIDAL testV BIOCHEMISTRY Blood SugarBlood ureaLiver function testsKidney function testsBlood lipid profileVI CARDIAC INVESTIGATIONS a) ECGVII OPHTHALMOLOGY a) Refraction by using Snellen's chartRetinoscopyOphthalmoscopyIX RADIOLOGY a) X ray for Chest, Skull, Spine, Abdomen, bonesb) Dental X rayc) Ultrasonography (Desirable)Physical Structure for Laboratory at CHCSl. No. Item No. at CHC Level1 Marble/Stone Table Top for Platform 12 Wash-basins (Steel/Porcelain) 13 Water Taps 14 Electric Fittings As per requirement5 Office Table 16 Office Chairs 37 Revolving Stools 28 Almirah (Steel/Wooden) 19 Wooden/Steel Racks 1Laboratory Equipment1 Binocular Microscope with oil immersion2 Lancet3 Ice box4 Stool transport carrier5 Test tube rack6 Table top centrifuge7 Refrigerator8 Spirit lamp9 Smear transporting box10 Sterile leak proof containersIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 69
Laboratory Supplies1 Clean slides2 Slide markers3 Gloves4 Transport medium (Cary Blair)5 Sterile test tubes6 Plastic vials7 Sterile cotton wool swabs8 Rapid Diagnostic Kit Typhoid9 Rapid test kit for faecal contamination10 Blood culture bottles with broth11 Zeil Neelsen Acid fast stain12 Aluminium Foil13 Cotton14 Sealing material15 Extra plastic vials for70Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Annexure 13Model Citizen’s CharterMission StatementAccess to servicesThis CHC provides medical care to all patientswithout any discrimination of gender/cast/religion/status. Emergency services are available 24 x 7. Themanagement of this hospital is responsible for ensuringthe delivery of services.Standards of ServicesThis hospital provides quality minimum assured servicesset by Indian Public Health Standards (<strong>IPHS</strong>).Your Rights in the Hospital1Right to access to all the services provided bythe Hospital.2345.67Right to Information - including informationrelating to your treatment.Right of making decision regarding treatment.Right for privacy and confidentiality.Right to religious and cultural freedom.Right for Safe and Secure Treatment.Right for grievance redressal.General InformationNo. of Beds.....................................................................No. and specialization of Doctors....................................No. of Nurses...................................................................No. of Ambulances..........................................................Services AvailableOPD Indoor Treatment/Wards 24 hrs Emergency andMedicolegalRadiologyX-Ray, Ultrasound (if available)MCH Services(including High Risk Pregnancy& Newborn stabilization unit)Laboratory Pharmacy DentistryFamily Planning Services Immunization Blood storage Operation TheatreAYUSH ECG 24 Hrs AmbulanceIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 71
Enquiries and InformationEnquiry counter is located at...............Timings for working counter are............Phone no. for telephonic enquiry (24 hours service)......Location guide maps and directional signages have beenput up at strategic points in the hospital.Casualty & Emergency ServicesFacilities All Emergency Services are available roundthe clock.Medico legal services are available.Referral Services to higher centre in casefacilities for treatment are not available in thehospital.Round the clock ambulance services withbasic life support.In serious cases, treatment/management getspriority over paper work like registration andmedico-legal requirements. The decision restswith the treating doctor.OPD ServicesOPD services are available on all working days excludingSundays and Gazetted Holidays.Timings -Morning - ............am to.......... am/pmEvening - .............pm to.......... pm.Various outpatient services available in the CHC aredetailed below (as available):Department Room no. TimingsGeneral MedicineGeneral SurgeryObstetrics & GynaecologyPaediatricsEyeDentistryAYUSH ServicesHomeopathicAyurvedicOthersMedical Facilities Not AvailableDiagnostic ServicesTimingsLists of tests and charges are available in the respectivedepartment.X-RaysUltrasoundECGComplaints & GrievancesEvery complaint will be duly acknowledged.We aim to settle your complaints within ..........days of its receipt.Suggestions/Complaint boxes are alsoprovided at enquiry counter and........... in thehospital.If we cannot, we will explain the reasons andthe time we will take to resolve.You can address your complaints toName …………………….Designation…………….Tele(O)………………(R)…………………(M)................Meeting Hours………….....… to ……………………Your ResponsibilitiesPlease do not inconvenience other patients.Please help us in keeping the hospital and itssurroundings neat and clean.Beware of Touts. If you find any such person inpremises tell the hospital authorities.The Hospital is a “No Smoking Zone” andsmoking is a Punishable Offence.Please refrain from demanding undue favoursfrom the staff and officials as it encouragescorruption.Please provide useful feedback & constructivesuggestions. These may be addressed to theMedical Superintendent of the Hospital.72Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Annexure 14List of Statutory Compliances1. No objection certificate from the CompetentFire Authority.2. Authorisation under Bio-medical Waste(Management and Handling) Rules, 1998.3. Authorisation from Atomic Energy RegulationBoard.4. Excise permit to store Spirit.5. Vehicle registration certificates for Ambulances.6. Consumer Protection Act.7. Drug & Cosmetic Act 1950.8. Fatal Accidents Act 1855.9. Indian Lunacy Act 1912.10. Indian Medical Council Act and code of MedicalEthics.11. Indian Nursing Council Act.12. Maternity Benefit Act 1961.13. Boilers Act as amended in 2007.14. MTP Act 1971.15. Persons with Disability Act 1995.16. Pharmacy Act 1948.17. PNDT Act 1996.18. Registration of Births and Deaths Act 1969.19. License for Blood Bank or Authorisation forBlood Storage facility.20. Right to Information act.21. Narcotics and psychotropic substances Act 1985.22. Clinical Establishments (Registration andRegulation) Act 2010.Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 73
Annexure 15Steps for Safety in Surgical Patients (in the Pre-operative Ward)To be done by SurgeonTo be done by Staff NurseTo be done by AnesthetistHistory, examination and investigationsPre-op ordersCheck and reconfirm PAC findingsAssess and mention any co-morbid conditionRecord boldly on 1 st page of case sheetHistory of drug allergiesBlood transfusionSample for grouping and crossmatchingto be sentCheck availability & donationRisk of transfusion to be explainedto relativesPatient’s consent to be taken(Counter sign by surgeon)Part preparation as orderedIdentification tag on patient wristName/Age/Sex/C.R. No/Surgical unit/DiagnosisFollow pre-op ordersAntibiotic sensitivity test doneSignature of Staff NurseCheck PAC findingsAssess co morbid conditionsH/O any drug allergyCheck ConsentSignature of AnaesthetistWritten well informed consent from patient(Counter sign by surgeon)Sister in charge of O.T. to be informed inadvance regarding the need for specialequipmentSignature of Surgeon74Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Surgical Safety Check List in the Operation TheatreSIGN IN (Period before induction ofanesthesia)TIME OUT (Period after induction & beforesurgical incision)SIGN OUT (Period from wound closure tilltransfer of patient from OT room)Patient has confirmedIdentitySiteProcedureConsentSite marked/Not ApplicableAnesthesia Safety Check CompletedAnesthesia EquipmentA B C D EPulse Oxymeter on Patient and functioningConfirm all team members haveintroduced themselves by name & roleSurgeon, Anesthetist & Nurse verballyConfirmPatientSiteProcedureANTICIPATED CRITICAL EVENTS Surgeons reviews: What are the critical orunexpected steps, operative duration &anticipated blood lossNurse Verbally confirm with the team :The name of the procedure recordedThat instrument, sponge, needle countsare correct (or not applicable)How the specimen is labeled(including Patient name)Whether there are any equipmentproblems to be addressed?DOES PATIENT HAVE A:Known Allergy No YesDifficult Airway/Aspiration Risk? No Yes, and assistance availableRisk of >500 ml Blood loss(7 ml/kg in children) No Yes and adequate I.V. access & Blood/Fluids Planned.Anesthetist reviews: Are there any patientspecific concernsNursing Team reviews: Has sterility beenconfirmed? Is there equipment issue orany concern?Has Antibiotic prophylaxis been given within the last 60 minutes? YesNot ApplicableIs Essential Imaging Displayed? YesNot ApplicableSurgeon, Anesthetist & Nurse reviewthe key concerns for recovery andmanagement of patient & post-op ordersto be given accordinglyInformation to patients attendant aboutprocedure performed, condition of thepatient & specimen to be shownHistopathology form to be filled properly& return all the records & investigation toattendant/patientSignature of AnesthetistSignature of NurseSignature of SurgeonIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 75
Annexure 16List of AbbreviationsAD : Auto DisabledANC : Ante Natal CareANM : Auxiliary Nurse MidwifeASHA : Accredited Social Health ActivistAYUSH : Ayurveda, Yoga & Naturopathy, Unani, Siddha and HomoeopathyBCC : Behaviour Change CommunicationBP : Blood PressureCBR : Community Based RehabilitationCHC : Community Health CentresCS : Caesarian SectionCSSD : Central Sterile Supply DepartmentCSSM : Child Survival and Safe MotherhoodDEC : Di Ethyl CarbamazineDF : Deep FreezerDOTS : Directly Observed Treatment Short CourseDTC : District Tuberculosis CentreECG : Electro Cardio GraphyESR : Erythrocyte Sedimentation RateFRU : First Referral UnitICTC : Integrated Counselling and Testing CentreIEC : Information, Education and CommunicationILR : Ice Lined RefrigeratorInj : Injection<strong>IPHS</strong> : Indian Public Health StandardsI/V : IntravenousIUCD : Intra-urine Contraceptive Devise76Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
IYCF : Infant and Young Child FeedingJE : Japanese EncephalitisLR : Labour RoomLTs : Laboratory TechniciansMC : Microscopic CentreMDT : Multi Drug TherapyMIS : Management Information SystemMO : Medical OfficerMPWs : Multi Purpose WorkersNACP : National AIDS Control ProgrammeNAMP : National Anti Malaria ProgrammeNHP : National Health ProgrammeNLEP : National Leprosy Eradication ProgrammeNPCDCS : National Programme for Prevention and Control of Cancer, Diabetes,Cardiovascular Diseases & Stroke<strong>NRHM</strong> : National Rural Health MissionNSV : Non Scalpel VasectomyNVBDCP : National Vector Borne Disease Control ProgrammeOPD : Out Patient DepartmentOT : Operation TheatrePDC : Professional Development CoursePHC : Primary Health CentrePMR : Physical Medicine and RehabilitationPNC : Post Natal CarePOL : Petrol Oil and LubricantPPH : Post Partum HaemorrhagePPTCT : Prevention of Parent to Child TransmissionPRI : Panchayati Raj InstitutionRCH : Reproductive & Child HealthRNTCP : Revised National Tuberculosis Control ProgrammeRTI/STI : Reproductive Tract Infections/Sexual Tract InfectionsSNCU : Special Newborn Care UnitSOPs : Standard Operating ProceduresSTLS : Senior Tuberculosis Laboratory SupervisorSTPs : Standard Treatment ProtocolsTENS : Transcutaneous Electrical Nerve StimulationUT : Union TerritoryWC : Water Closet (i.e. a flush toilet)Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 77
REFERENCES1. National Rural Health Mission 2005-2012 – Reference Material (2005), Ministry of Health & Family Welfare,Government of India.2. Bulletin on Rural Health Statistics in India (2005), Infrastructure Division, Department of Family Welfare;Ministry of Health & Family Welfare, Government of India.3. <strong>Guidelines</strong> for Operationalising 24 x 7 PHC (2005) (unpublished), Maternal Health Division, Department ofFamily Welfare, Ministry of Health & Family Welfare, Government of India.4. <strong>Guidelines</strong> for Ante-Natal Care and Skilled Attendance at Birth by ANMs and LHVs (2005), Maternal HealthDivision, Department of Family Welfare, Ministry of Health & Family Welfare, Government of India.5. RCH Phase II, National Programme Implementation Plan (PIP) (2005), Ministry of Health & Family Welfare,Government of India.6. <strong>Guidelines</strong> for Setting up of Rogi Kalyan Samiti/Hospital Management Committee (2005), Ministry ofHealth & Family Welfare, Government of India.7. Indian Standard: Basic Requirements for Hospital Planning, Part-1 up to 30 Bedded Hospital, IS: 12433(Part 1)-1988, Bureau of Indian Standards, New Delhi.8. Indian Public Health Standards (<strong>IPHS</strong>) for Community Health Centre (April 2005), Directorate General ofHealth Services, Ministry of Health & Family Welfare, Government of India.78Indian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres
Members of Task Force for Revision of <strong>IPHS</strong>(As per order No. T 21015/55/09 – NCD, Dte.GHS, dated 29-1-2010 and minutes ofmeeting of Task Force held on 12-2-2010)12345.678910Dr. R.K. Srivastava, Director General of HealthServices – ChairmanDr. Shiv Lal, Special DG (PH), Dte.GHS, NirmanBhawan, New Delhi – Co-Chairman.Sh. Amarjit Sinha, Joint Secretary, <strong>NRHM</strong>,Ministry of Health & F.W., Nirman Bhawan, NewDelhi.Dr. Amarjit Singh, Executive Director,Jansankhya Sthirata Kosh, Bhikaji Cama Place, New Delhi - 110066.Dr. B. Deoki Nandan, Director National Instituteof Health & Family Welfare, Baba Gang NathMarg, Munirka, New Delhi – 110067Dr. T. Sunderraman, Executive Director, NationalHealth Systems Resource Centre, NIHFWCampus, Baba Gang Nath Marg, Munirka, New Delhi – 110067.Dr. N.S. Dharmshaktu, DDG (NSD), Dte.G.H.S.,Nirman Bhawan, New Delhi.Dr. S.D. Khaparde, DC (ID), Ministry of Health &F.W., Nirman Bhawan, New Delhi.Dr. A.C. Dhariwal, Additional Director (PH)and NPO, National Centre for Disease Control(NCDC), 22, Sham Nath Marg, New Delhi –110054.Dr. C.S. Pandav, Prof. and Head, CommunityMedicine, AIIMS, New Delhi.1112131415.1617181920Dr. J.N. Sahay, Advisor on Quality improvement,National Health Systems Resource Centre,NIHFW Campus, Baba Gang Nath Marg, Munirka, New Delhi – 110067.Dr. Bir Singh, Prof. Department of CommunityMedicine, AIIMS and Secretary General.Indian Association of Preventive and SocialMedicine.Dr. Jugal Kishore, Professor of CommunityMedicine, Maulana Azad Medical College,Bahadur Shah Zafar Marg, New Delhi – 110002Mr. J.P. Mishra, Ex. Programme Advisor,European Commission, New DelhiDr. S. Kulshreshtha, ADG, Dte. GHS., NirmanBhawan, New Delhi.Dr. A.C. Baishya, Director, North Eastern RegionalResource Centre, Guwahati, Assam.Dr. S. K. Satpathy, Public Health Foundation ofIndia, Aadi School Building, Ground Floor, 2Balbir Saxena Marg, New Delhi – 110016.Dr. V.K. Manchanda, World Bank, 70, LodhiEstate, New Delhi – 110003.Sh. Dilip Kumar, Nursing Advisor, Dte. G.H.S.,Nirman Bhawan, New Delhi.Dr. Anil Kumar, CMO (NFSG), Dte.G.H.S, NirmanBhawan, New Delhi- Member SecretaryIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres 79
82Directorate General of Health ServicesMinistry of Health & Family WelfareGovernment of IndiaIndian Public Health Standards (<strong>IPHS</strong>) <strong>Guidelines</strong> for Community health centres