Procedural Sedation Administered by Non-Anesthesiologist Providers
Procedural Sedation Administered by Non-Anesthesiologist Providers
Procedural Sedation Administered by Non-Anesthesiologist Providers
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
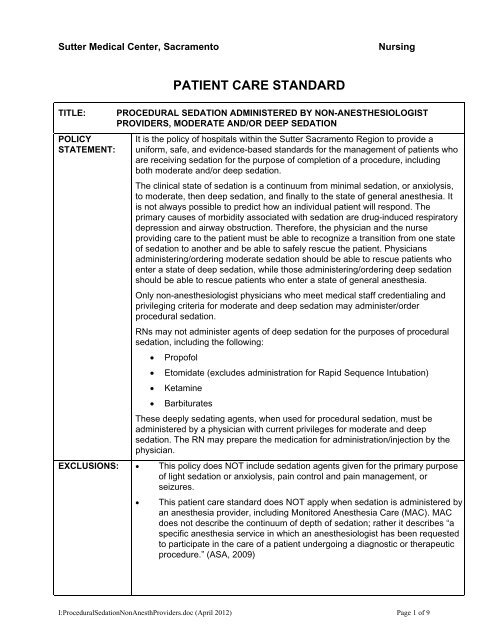
Sutter Medical Center, SacramentoNursingTITLE:POLICYSTATEMENT:PATIENT CARE STANDARDPROCEDURAL SEDATION ADMINISTERED BY NON-ANESTHESIOLOGISTPROVIDERS, MODERATE AND/OR DEEP SEDATIONIt is the policy of hospitals within the Sutter Sacramento Region to provide auniform, safe, and evidence-based standards for the management of patients whoare receiving sedation for the purpose of completion of a procedure, includingboth moderate and/or deep sedation.The clinical state of sedation is a continuum from minimal sedation, or anxiolysis,to moderate, then deep sedation, and finally to the state of general anesthesia. Itis not always possible to predict how an individual patient will respond. Theprimary causes of morbidity associated with sedation are drug-induced respiratorydepression and airway obstruction. Therefore, the physician and the nurseproviding care to the patient must be able to recognize a transition from one stateof sedation to another and be able to safely rescue the patient. Physiciansadministering/ordering moderate sedation should be able to rescue patients whoenter a state of deep sedation, while those administering/ordering deep sedationshould be able to rescue patients who enter a state of general anesthesia.Only non-anesthesiologist physicians who meet medical staff credentialing andprivileging criteria for moderate and deep sedation may administer/orderprocedural sedation.RNs may not administer agents of deep sedation for the purposes of proceduralsedation, including the following:• Propofol• Etomidate (excludes administration for Rapid Sequence Intubation)• Ketamine• BarbituratesThese deeply sedating agents, when used for procedural sedation, must beadministered <strong>by</strong> a physician with current privileges for moderate and deepsedation. The RN may prepare the medication for administration/injection <strong>by</strong> thephysician.EXCLUSIONS: • This policy does NOT include sedation agents given for the primary purposeof light sedation or anxiolysis, pain control and pain management, orseizures.• This patient care standard does NOT apply when sedation is administered <strong>by</strong>an anesthesia provider, including Monitored Anesthesia Care (MAC). MACdoes not describe the continuum of depth of sedation; rather it describes “aspecific anesthesia service in which an anesthesiologist has been requestedto participate in the care of a patient undergoing a diagnostic or therapeuticprocedure.” (ASA, 2009)I:<strong>Procedural</strong><strong>Sedation</strong><strong>Non</strong>Anesth<strong>Providers</strong>.doc (April 2012) Page 1 of 9
PATIENT CARE STANDARDTITLE:PROCEDURAL SEDATION ADMINISTERED BY NON-ANESTHESIOLOGISTPROVIDERS, MODERATE AND/OR DEEP SEDATIONDEFINITIONS: • <strong>Procedural</strong> <strong>Sedation</strong>: Moderate or deep sedation provided duringdiagnostic or therapeutic procedures.• <strong>Non</strong>-<strong>Anesthesiologist</strong> providers of procedural sedation: Physicians whoare not anesthesia specialists• Minimal sedation/Light sedation (anxiolysis) is a drug-induced stateduring which patients respond normally to verbal commands. Althoughcognitive function and physical coordination may be impaired, airwayreflexes, and ventilation and cardiovascular function are unaffected. (ASA,2002).• Moderate sedation is a drug-induced depression of consciousness duringwhich patients respond purposefully** to verbal commands, either alone oraccompanied <strong>by</strong> light tactile stimulation. No interventions are required tomaintain a patent airway, and spontaneous ventilation is adequate.Cardiovascular function is usually maintained. ** Reflex withdrawal from apainful stimulus is NOT considered a purposeful response. (ASA, 2002).• Deep sedation is a drug-induced depression of consciousness during whichpatients cannot be easily aroused but respond purposefully** followingrepeated or painful stimulation. The ability to independently maintainventilatory function may be impaired. Patients may require assistance inmaintaining a patent airway, and spontaneous ventilation may beinadequate. Cardiovascular function is usually maintained. ** Reflexwithdrawal from a painful stimulus is NOT considered a purposefulresponse. (ASA, 2002).• General Anesthesia is a drug-induced loss of consciousness during whichpatients are not arousable, even <strong>by</strong> painful stimulation. The ability toindependently maintain ventilatory function is often impaired. Patients oftenrequire assistance in maintaining a patent airway, and positive pressureventilation may be required because of depressed spontaneous ventilationor drug-induced depression of neuromuscular function. Cardiovascularfunction may be impaired. (ASA, 2009)I:<strong>Procedural</strong><strong>Sedation</strong><strong>Non</strong>Anesth<strong>Providers</strong>.doc (April 2012) Page 2 of 9
PATIENT CARE STANDARDTITLE:PROCEDURAL SEDATION ADMINISTERED BY NON-ANESTHESIOLOGISTPROVIDERS, MODERATE AND/OR DEEP SEDATIONContinuum of Depth of <strong>Sedation</strong>2002, Practice Guidelines for <strong>Sedation</strong> and Analgesia <strong>by</strong> <strong>Non</strong>-<strong>Anesthesiologist</strong>sMinimal (Light) Moderate <strong>Sedation</strong><strong>Sedation</strong>(Anxiolysis)ResponsivenessNormal responseto verbalstimulationPurposeful responseto verbal or tactilestimulationAirway Unaffected No interventionrequiredSpontaneousventilationCardiovascularfunctionDeep<strong>Sedation</strong>Purposeful responseafter repeated orpainful stimulationIntervention may berequiredGeneralAnesthesiaUnarousable,even withpainful stimulusInterventionoften requiredUnaffected Adequate May be inadequate FrequentlyinadequateUnaffected AdequateMay be inadequate May beUsually maintained Usually maintained impairedLEVEL OF SEDATION SCALE:The patient’s level of sedation will be documented using a sedation scale. Various sedation scales areused within the region as identified in Appendix A.Pre-<strong>Procedural</strong> NPO Guidelines (Recommendations from the Department of Anesthesia*)(SMCS): See Medical Staff Policy for Department of Anesthesia Statement Adult and Pediatric NPOGuidelinesInfants(0-6months)Children(7 months –12 months)Children(13 monthsto 12 years)Solids 8 hours 8 hours 8 hoursBreast MilkandFormulaClearLiquids4 hours 6 hours 8 hoursProcedure before1200No solids after 2300the night before2 hours 2 hours 2 hours Procedure before1200Nothing after 2300the night beforeChildren and Adults(13 years and up)Procedure after1200No solids after 2400 thenight beforeProcedure after1200May have clear liquidsup to 4 hours beforescheduled procedure.For all patients, regardless of age: Maximum of 4 ounces (1/2 cup) clear liquids during the onehour prior to beginning complete NPO status.*Please note: these are guidelines only. For purposes of clarification, pediatric clear liquids includewater, Pedialyte, Koolaid, Gatorade, grape juice, cranberry juice, apple juice, pulp-free popsicles. Nocarbonated drinks, no 7-Up or ginger ale, no gelatin (jello), no broth.I:<strong>Procedural</strong><strong>Sedation</strong><strong>Non</strong>Anesth<strong>Providers</strong>.doc (April 2012) Page 3 of 9
PATIENT CARE STANDARDTITLE:CLINICALLOCATIONS FORSEDATIONADMINISTRATION:REQUIREDEQUIPMENT ANDSUPPLIES:PROCEDURAL SEDATION ADMINISTERED BY NON-ANESTHESIOLOGISTPROVIDERS, MODERATE AND/OR DEEP SEDATION<strong>Procedural</strong> sedation may be administered in areas where the patient can beadequately and safely monitored as outlined in this policy. See Appendix B.To ensure patient safety and the rapid ability to rescue patients, the followingequipment and supplies must be readily available:• Crash crash/defibrillator – age appropriate• Oxygen source and equipment/supplies for administering supplementaloxygen (cannula, mask) – age appropriate• Emergency advanced airway/intubation equipment – age appropriate• Bag-valve mask – age appropriate• Working suction source and equipment/supplies required for suctioning• Patient monitoring equipment: cardiac monitor, non-invasive bloodpressure monitor, pulse oximetry, and end-tidal CO2 monitor• <strong>Sedation</strong> medications and appropriate antagonists/reversal agents.SMCS: Procedure FlowsheetREQUIREMENTS/RESPONSIBILITES:NON-ANESTHESIOLOGIST PHYSICIAN PROVIDER REQUIREMENTS:The physician ordering/overseeing/administering sedation must:• Hold current medical staff credentials for procedural sedation.• Hold a valid DEA license to prescribe the selected sedatives andanalgesics.RN COMPETENCY REQUIREMENTS:• For adult patients: Completion of hospital sponsored <strong>Sedation</strong> Trainingcourse.• For pediatric patients less than 14 years of age: Completion of hospitalsponsored Adult and Pediatric <strong>Sedation</strong> Training.• Current certification in an age appropriate advanced cardiac life supportcourse, such as ACLS, PALS, NRP. NICU: RN must also have ALSdesignation.REQUIRED PERSONNEL REQUIRED FOR PROCEDURAL SEDATION:In addition to the practitioner performing the procedure, sufficient numbers ofqualified personnel must be present for all procedures requiring moderate ordeep sedation.• One health care provider (an RN or physician who is competent insedation management and is not the physician performing theprocedure) must have the primary responsibility of monitoring thepatient, including vital signs and level of consciousness. This personcannot leave the room/suite during the procedure.• For the adult patient, a second health care provider may be required toassist as directed with sedation monitoring. This person must be BLScertified.I:<strong>Procedural</strong><strong>Sedation</strong><strong>Non</strong>Anesth<strong>Providers</strong>.doc (April 2012) Page 4 of 9
PATIENT CARE STANDARDTITLE:REQUIREMENTS/RESPONSIBILITESCONTINUED:PROCEDURAL SEDATION ADMINISTERED BY NON-ANESTHESIOLOGISTPROVIDERS, MODERATE AND/OR DEEP SEDATIONrecommended NPO guidelines, notify the physician.6. Review the patient’s current medications, allergies, age, weight, generalhealth history including pregnancy status when applicable. Ask thepatient about their anesthesia history including prior complications andpersonal or family history of malignant hyperthermia.7. Verify patent IV access.8. Explain the procedure to the patient and provide patient/ parent/caregiver education.9. Provide verbal and/or written objectives of the sedation and procedure.10. Discuss anticipated changes before and after sedation and procedure.11. Assure availability of a responsible person to accompany the outpatienthome, if necessary.12. Obtain baseline assessment to include the following:a. Vital signs – blood pressure, heart rate, respiratory rate, and O2saturation.b. Heart rhythm.c. Physical exam including evaluation of the patient’s heart, lungs,airway and adequacy of ventilation.d. Baseline end tidal CO2 or TCM.13. Document baseline assessment findings on the appropriate proceduralsedation tool.PATIENT MONITORING REQUIREMENTS:Summarized in Addenda C:1. The RN can administer/give drugs for moderate sedation when theprocedural physician is present and at the bedside and all preproceduralsedation requirements as described above have been met.The RN cannot administer/inject agents of deep sedation, includingpropofol, etomidate, and ketamine, for the purposes of completing aprocedure. The RN may prepare the medication foradministration/injection <strong>by</strong> the physician.2. The RN will be in attendance during all phases of the procedure tomonitor the patient. Continuous assessment and monitoring (prolonged,without interruption at any time): Pulse oximetry, heart rate, heartrhythm, airway patency, adequacy of ventilation, and end tidal CO2 ortranscutaneous monitor (TCM). .3. Every 5 minutes during the procedure, the following will beI:<strong>Procedural</strong><strong>Sedation</strong><strong>Non</strong>Anesth<strong>Providers</strong>.doc (April 2012) Page 6 of 9
PATIENT CARE STANDARDTITLE:REQUIREMENTS/RESPONSIBILITESCONTINUED:PROCEDURAL SEDATION ADMINISTERED BY NON-ANESTHESIOLOGISTPROVIDERS, MODERATE AND/OR DEEP SEDATIONdocumented:a. Blood pressure, pulse oximetry, end tidal CO2 or TCM, respiratoryrate, heart rate and level of sedation.4. If assessing level of sedation compromises and/or disrupts theprocedure, the reason must be documented.5. It is the responsibility of the RN to keep the physician informed ofpatient status throughout the duration of the sedation. This includes:a. Patient assessment information.b. Loss of protective reflexes.c. Inability to maintain a patent airway.d. Variations in vital signs indicating potential change in patientstatus.e. Amount of medication given per physician order.6. The RN is to notify the physician immediately if the patient experiences:a. Baseline oxygen saturation of less than 93%, a decrease in oxygensaturation from a low saturation baseline, or a fall in oxygensaturation of 5% or greater.b. Inadequate ventilation and/or inability to maintain a patent airway.c. Inability to respond appropriately to physical stimulation/verbalcommands.d. Hemodynamic instability, as evidenced <strong>by</strong> hypotension, arrhythmia,chest pain, shortness of breath.e. Other adverse reactions to drugs administered.7. Should any of the above changes occur, implement the followingmeasures:a. Give supplemental oxygen as ordered <strong>by</strong> the physician.8. If saturation does not improve:a. Stimulate the patient.b. Halt procedure.c. Attempt to improve the airway with jaw thrust and/ororal/nasopharyngeal airway.d. Initiate or assist ventilation with bag/valve/mask and oxygen.e. Administer reversal agents as ordered.f. Initiate cardiopulmonary resuscitation procedures as needed.1) If endotracheal intubation is employed, determine correct tubeplacement <strong>by</strong> carbon dioxide detection, presence of equalbreath sounds and presence of chest rise. When appropriate,tube position should be verified <strong>by</strong> x-ray.PHYSICIAN REQUIREMENTS FOLLOWING PROCEDURAL SEDATIONI:<strong>Procedural</strong><strong>Sedation</strong><strong>Non</strong>Anesth<strong>Providers</strong>.doc (April 2012) Page 7 of 9
PATIENT CARE STANDARDTITLE:REQUIREMENTS/RESPONSIBILITESCONTINUED:PROCEDURAL SEDATION ADMINISTERED BY NON-ANESTHESIOLOGISTPROVIDERS, MODERATE AND/OR DEEP SEDATIONADMINISTRATION:1. At the conclusion of the procedure, the physician ordering theprocedural sedation reviews and signs the sedation record. Physiciansignature indicates agreement with information recorded on the form,including medication and dosages given for sedation.2. The physician documents a post-sedation, post-procedure note toinclude diagnosis, procedure findings, complications, blood loss orspecimen removal, and plan of care.3. The physician must document criteria for discharge from the hospital, ifoutpatient.RN REQUIREMENTS FOLLOWING PROCEDURAL SEDATION:1. Following the completion of the procedure, the patient remainscontinuously monitored and immediately enters the recovery phase ofcare.2. Document at a minimum of every 15 minutes: pulse oximetry, heartrate, heart rhythm, airway patency, adequacy of ventilation, end tidalCO2 or TCM and blood pressure until the patient returns to his/herbaseline level of consciousness and is able to independently maintaintheir airway and oxygen saturation, follow verbal commands, and vitalsigns are consistent with pre-procedure vital signs.3. If the patient required reversal of sedation, (i.e. use of narcan(nalaxone) and/or romazicon (flumazenil), recovery time is extended <strong>by</strong>one additional hour to monitor for re-sedation.4. For outpatients, provide written post-sedation discharge instructionsthat indicate:a. Potential/anticipated sedation effect.b. Activity limitations.c. Dietary precautions.d. 24-hour emergency and follow-up contact numbers.REPORTABLECONDITIONS:REPORTABLEReportable conditions include any of the following:1. Unexpected intubation or need for mechanical ventilation2. Cardiac arrest3. Unplanned transfer to higher level of care, including inpatient admission4. Suspected aspiration5. Use of reversal agents6. Adverse medication reaction7. Patient, family, or staff complaint regarding quality of sedationI:<strong>Procedural</strong><strong>Sedation</strong><strong>Non</strong>Anesth<strong>Providers</strong>.doc (April 2012) Page 8 of 9
PATIENT CARE STANDARDTITLE:CONDITIONSCONTINUED:PROCEDURAL SEDATION ADMINISTERED BY NON-ANESTHESIOLOGISTPROVIDERS, MODERATE AND/OR DEEP SEDATION8. Inappropriate level of sedation (too high or too low)9. Hemodynamic instability, chest painEVALUATION OFPATIENTOUTCOMES:REFERENCES:The Department of Anesthesia is responsible for reviewing aggregate datarelated to procedural sedation with indicators identified through thecontinuous quality improvement process.Standards for Basic Anesthetic Monitoring 2011 PDF filehttp://www.rn.ca.gov/pdfs/regulations/npr-b-06.pdfContinuum Of Depth Of <strong>Sedation</strong>: Definition Of General Anesthesia And LevelsOf <strong>Sedation</strong>/Analgesia, Asa, 2007.http://www.csahq.org/pdf/news/Deep<strong>Sedation</strong>_06_08_final.pdf, CaliforniaSociety of <strong>Anesthesiologist</strong>s: GUIDELINES FOR DEEP SEDATION BY NON-ANESTHESIOLOGISTS, 2008Gross JB et al. (2002). Practice Guidelines for <strong>Sedation</strong> and Analgesia <strong>by</strong><strong>Non</strong>-<strong>Anesthesiologist</strong>s: An updated report <strong>by</strong> the American Society of<strong>Anesthesiologist</strong>s task force on sedation and analgesia <strong>by</strong> nonanesthesiologists.Origination Date: March 2011Revision Date: 04/12Written <strong>by</strong>:Revised <strong>by</strong>:Brenda McCulloch, CNSBrenda McCulloch, CNSInformation Only:Critical Care CommitteeOb/Gyn Administrative CommitteeSurgery Administrative CommitteeCardiovascular Disease Administrative CommitteePediatric Administrative CommitteeMedicine Administrative CommitteeFamily Medicine Administrative CommitteePharmacy Therapeutic TeamEmergency Medicine Administrative CommitteeD.I.R.O. Administrative CommitteeApproval Date:February 26, 2012March 27, 2012April 13, 2012Approved <strong>by</strong>:Anesthesia Administration CommitteeMedical Executive CommitteeShelly McGriff, Chief Nurse ExecutiveI:<strong>Procedural</strong><strong>Sedation</strong><strong>Non</strong>Anesth<strong>Providers</strong>.doc (April 2012) Page 9 of 9
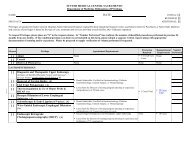
PROCEDURAL SEDATION ADMINISTERED BYNON-ANESTHESIOLOGIST PROVIDERSADDENDA ASEDATION SCALES IN USE IN THE REGIONLevel of <strong>Sedation</strong> (LOS)1 Awake and alert2 Awake but sleepy3 Asleep, easily arouses4 Asleep, not easily arousable5 Asleep, not arousableUsed at SMCSRamsey <strong>Sedation</strong> ScaleUsed at SRMC1 Patient awake, anxious and agitated; or both2 Patient awake, cooperative, oriented, and tranquil.3 Patient awake but drowsy, sleepy, tranquil, responds toverbal commands only. Eyes may be closed butresponds to commands without tactile stimulation.Patient will still be able to answer questions about painor discomfort to determine need for analgesia.4 Patient asleep but briskly responds to loud auditorystimulus gently shaking or light glabellar tap (light tapbetween the eyes). Drifts back to sleep duringconversation.5 Patient asleep and responds only to noxious stimuli orhas sluggish response to loud auditory stimulus or lightglabellar tap (light tap between the eyes).6 Patient asleep and has no response to firm nail bedpressure or other noxious stimuli.Richmond Agitation <strong>Sedation</strong> Scale (RASS) Used at SDHTarget RASS Description+4 Combative, violent, danger to staff+3 Pulls or removes tube(s) or catheters, aggressive+2 Frequent non-purposeful movement, fights ventilator+1 Anxious, apprehensive, but not aggressive0 Alert and calm-1 Awakens to voice (eye opening/contact) > 10 seconds-2 Light sedation, briefly awakens to voice (eyeopening/contact) < 10 seconds-3 Moderate sedation, movement or eye opening???, noeye contact-4 Deep sedation, no response to voice, but movement oreye opening to physical stimulation-5 Unarousable, no response to voice or physicalstimulationI:<strong>Procedural</strong><strong>Sedation</strong><strong>Non</strong>Anesth<strong>Providers</strong>.doc (April 2012)
PROCEDURAL SEDATION ADMINISTERED BYNON-ANESTHESIOLOGIST PROVIDERSSAFH – Sutter Auburn Faith Hospital• Special Procedures/OR/PACU• ICU/CCU/TCU• Emergency Department• Diagnostic Imaging Services• Cardiac Cath Lab• Cardiopulmonary ServicesADDENDA BLOCATIONS WHERE SEDATION MAY BE ADMINISTEREDSDH – Sutter Davis Hospital• Special Procedures/Bronchoscopy Procedure Room• Critical Care Nursing Units• Emergency Department• Endoscopy Room• Diagnostic Imaging (ED patients only/monitored <strong>by</strong> ED staff)SMCS – Sutter Medical Center Sacramento• –<strong>Procedural</strong> sedation can be provided in clinical locations where all requirements of this patientcare standard can be met.SRMC – Sutter Roseville Medical Center• Special Procedures and Bronchoscopy Procedure Room• Telemetry and Critical Care Units• Emergency Departments• Diagnostic Imaging Services• Outpatient Services• Operating Room, Post Anesthesia Care Unit, Surgical Preparation Area (SPA)• Endoscopy Laboratory• Angiography and Cardiac Catheterization LaboratorySSMC – Sutter Solano Medical Center• Surgical Services• Endoscopy• PACU• ICU• ED• RadiologyI:<strong>Procedural</strong><strong>Sedation</strong><strong>Non</strong>Anesth<strong>Providers</strong>.doc (April 2012)
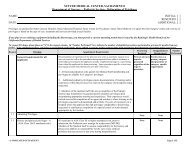
PROCEDURAL SEDATION ADMINISTERED BYNON-ANESTHESIOLOGIST PROVIDERSADDENDA CPATIENT MONITORING REQUIREMENTSModerate<strong>Sedation</strong>Deep<strong>Sedation</strong>DuringprocedureAfterprocedureDuringprocedureAfterprocedureB/P Heart Rate RespiratoryRateMonitor Documentcontinuously every 5Document minutesevery 5minutesDocumentevery 5minutesDocumentevery 15minutesDocumentevery 5minutesDocumentevery 15minutesMonitorcontinuouslyDocumentevery 15minutesMonitorcontinuouslyDocumentevery 5minutesMonitorcontinuouslyDocumentevery 15minutesDocumentevery 15minutesDocumentevery 5minutesDocumentvery 15minutesSa0202 satMonitorcontinuouslyDocumentevery 5minutesMonitorcontinuouslyDocumentevery 15minutesMonitorcontinuouslyDocumentevery 5minutesMonitorcontinuouslyDocumentevery 15minutesEnd TidalC02Documentevery 5minutes-MonitorcontinuouslyDocumentevery 5minutesMonitorcontinuouslyDocumentevery 15minutes<strong>Sedation</strong>ScoreDocumentevery 5minutesDocumentevery 15minutesDocumentevery 5minutesDocumentevery 15minutesI:<strong>Procedural</strong><strong>Sedation</strong><strong>Non</strong>Anesth<strong>Providers</strong>.doc (April 2012)