View June's Board Pack - Royal Bournemouth Hospital
View June's Board Pack - Royal Bournemouth Hospital
View June's Board Pack - Royal Bournemouth Hospital
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
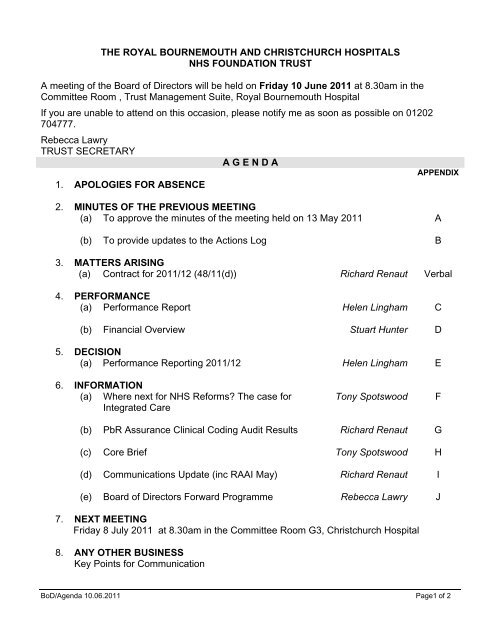
THE ROYAL BOURNEMOUTH AND CHRISTCHURCH HOSPITALSNHS FOUNDATION TRUSTA meeting of the <strong>Board</strong> of Directors will be held on Friday 10 June 2011 at 8.30am in theCommittee Room , Trust Management Suite, <strong>Royal</strong> <strong>Bournemouth</strong> <strong>Hospital</strong>If you are unable to attend on this occasion, please notify me as soon as possible on 01202704777.Rebecca LawryTRUST SECRETARYA G E N D AAPPENDIX1. APOLOGIES FOR ABSENCE2. MINUTES OF THE PREVIOUS MEETING(a) To approve the minutes of the meeting held on 13 May 2011 A(b) To provide updates to the Actions Log B3. MATTERS ARISING(a) Contract for 2011/12 (48/11(d)) Richard Renaut Verbal4. PERFORMANCE(a) Performance Report Helen Lingham C(b) Financial Overview Stuart Hunter D5. DECISION(a) Performance Reporting 2011/12 Helen Lingham E6. INFORMATION(a) Where next for NHS Reforms? The case forIntegrated CareTony SpotswoodF(b) PbR Assurance Clinical Coding Audit Results Richard Renaut G(c) Core Brief Tony Spotswood H(d) Communications Update (inc RAAI May) Richard Renaut I(e) <strong>Board</strong> of Directors Forward Programme Rebecca Lawry J7. NEXT MEETINGFriday 8 July 2011 at 8.30am in the Committee Room G3, Christchurch <strong>Hospital</strong>8. ANY OTHER BUSINESSKey Points for CommunicationBoD/Agenda 10.06.2011 Page1 of 2
9. COMMENTS QUESTIONS FROM THE GOVERNORS<strong>Board</strong> Members will be available for 10-15 minutes after the end of the Part I meeting totake comments or questions from the Governors.10. EXCLUSION OF PRESS AND PUBLIC AND OTHERSTo resolve that under the provision of Section 1, Sub-Section 2, of the Public BodiesAdmission to Meetings Act 1960, representatives of the press, members of the public andothers not invited to attend be excluded on the grounds that publicity would proveprejudicial to the public interest by reason of the confidential nature of the business to betransacted.BoD/Agenda 10.06.2011 Page2 of 2
THE ROYAL BOURNEMOUTH AND CHRISTCHURCH HOSPITALSNATIONAL HEALTH SERVICE FOUNDATION TRUSTMinutes of a Meeting of the <strong>Royal</strong> <strong>Bournemouth</strong> and Christchurch <strong>Hospital</strong>s National HealthService Foundation Trust <strong>Board</strong> of Directors held on Friday 13 May 2011 in the CommitteeRoom, <strong>Royal</strong> <strong>Bournemouth</strong> <strong>Hospital</strong>Present:Mrs J StichburyMr T SpotswoodMrs H LinghamMrs K AllmanMr B FordMr S HunterMr S PeacockMr R RenautMs B AtkinsonMr P DavéMr K TullettMr D BennettDr M ArmitageMrs A Pike(JS)(TS)(HL)(KA)(BF)(SH)(SP)(RR)(BA)(PD)(KT)(DB)(MA)(AP)Chairman (in the chair)Chief ExecutiveChief Operating OfficerDirector of Human ResourcesNon-Executive DirectorDirector of Finance and ITNon-Executive DirectorDirector of Service DevelopmentDirector of Nursing and MidwiferyNon-Executive DirectorNon-Executive DirectorNon-Executive DirectorMedical DirectorNon-Executive DirectorIn attendance:Apologies:Mrs R LawryMr L FoordMrs T HallMr S BungeyMs J BakerMrs M Ray(RL)(LF)(TH)(SB)(JB)(MR)Trust SecretaryGovernorCommunicationsGovernorGovernorReporter New Milton Advertiser46/11 MINUTES OF MEETING 8 April 2011 (Appendix A)The minutes of the meeting held on the 8 April 2011 were received,accepted as a true record and signed accordingly by the Chairman.47/11 Actions Log (Appendix B)(a)Performance updateHL gave a verbal update and advised that she is currently workingon some further development of the performance report and willincorporate suggested items and also ensure that it reflects therequirements of the compliance framework. Next month she willbring back recommendations on what the performance reportshould look like going forward to ensure <strong>Board</strong> assurance.HL(b)Strategy trackerRR advised some amendments have been made but the tracker isnow complete._____________________________________________________________________________________BOD/PT 1 MINS 13.05.11 PAGE 1 OF 6
48/11 MATTERS ARISING(a)New Director of Nursing Update (38/11(b))TS noted 4 strong candidates have been selected and interviewswill take place with an outside assessor in June.(b)Staff Survey (Management Skills) (41/11(b)KA was unable to provide the comparator data but verbally wasable to confirm that training session for managers will beintroduced and agreed to bring further detail back in June.KA(c) Contract for 2011/12RR noted the Heads of Terms have been agreed and we nowhave the direction of travel for QIPP which is positive. He notedthat we are still working on the actual legal contracts, and aim tocomplete this work by the end of May. TS asked for a report onhow we have ameliorated some of the more punitiverequirements.RR49/11 PERFORMANCE(a) Performance Report (Appendix C)HL confirmed overall good performance for the year. She notedthat we have delivered exceptional quality and performance. No MRSA to report in April 3 C-Diff cases which is minimal Will measure MSSA and E-Coli cases in future but we areawaiting a national steer Cancer - green throughout our performance on allstandards. She noted that we have been asked how wehave managed to achieve these levels and advised that thishas been through our consultants’ flexibility. ED - Monitor are currently interested in figures for total timespent in A&E, but for Q2 we will be measured on all 5areas. HL noted that the figures will not include the eyeunit, these will be input manually,DToC numbers are steady and we will be monitoring this ona daily basis to fulfil the contractual requirements. Strong 18 week performance, we are moving to a new setof measures when we benchmark, we are the strongestperforming 18 wk Trust in the South West. VTE assessment – we are upper quartile and engagingmedical staff to ensure it is maintained. Sickness – we are monitoring the monthly and cumulativeposition and we have put in place a trajectory to get us to_____________________________________________________________________________________BOD/PT 1 MINS 13.05.11 PAGE 2 OF 6
50/11 DECISION3% by the 4 th quarter. GP referrals are down for ophthalmology and we arelooking at how to realign this. There has been a decrease inOrthopaedics referrals and we need to determine if this is atrue decline, or simply patients being delayed, longer termtrends would not at this stage support a sustainablereduction in referrals.AP noted that performance has been outstanding given a verydifficult year. She noted that the assurance and clarity NEDs getfrom this is commendable. HL suggested putting something out tothank people. TS noted we will also be holding an evening eventto thank the individuals involved which will be held on Monday20th June. TS thanked HL for her continued effort.KT suggested that we should not lose historic figures from thereports as this provides trend lines for the <strong>Board</strong>. TS suggestedlooking at this in the annual report.PD asked how we ensure sustainability. HL advised that it isculturally embedded within this trust and she noted that we areknown as a very high performing trust nationally.(b) Financial Overview (Appendix D)SH confirmed the following key points from the report: It has been an excellent year for the financial performance,and we ended 0.2% above contract value which is goodnews for the health economy Expenditure has been well managed EBITDA improved on last year which highlights operationalefficiency. A 1.7% surplus will allow us to continue to invest in thecapital plan. There has been a capital slippage, but part ofthis will be recovered. Monitor risk indicators returned to green with a risk rating of4 by year end.TS commended in particular the performance against thetransformation programme which saw the savings targetcomfortably exceeded.(a) Consultation on Annual Plan – Next Steps (Appendix E)RR noted the comprehensive report and that we have been veryhappy with the quality of the feedback.He noted that even some of the most ardent critics agreed that ourconsultation process was extensive. We have had very good_____________________________________________________________________________________BOD/PT 1 MINS 13.05.11 PAGE 3 OF 6
51/11 DISCUSSIONengagement, with people wanting feedback.Emerging themes - option 1 for Christchurch <strong>Hospital</strong> wassupported. By the end of the process there was a high level ofunderstanding. The dental surgery has opened and has had 2500patients registered in the first month.RR added that instead of maintaining we want to increaseservices at Christchurch.AP noted that the process is a great credit to the team. The levelof participation means we have a robust outcome.RR noted that the business case is due to go to FinanceCommittee in October and back to <strong>Board</strong> in November. TSsuggested adding in some flexibility to ensure we don’t end up inan all or nothing situation.SP asked if there is a risk that the proposals could be delayed. TSnoted we are talking about natural progression and evolutionarysteps. He suggested we do some more work with LionelCartwright to ensure local GPs fully understand our plans, withinChristchurch there is strong support for the proposals.BF asked about Paul Sly’s letter and HL advised we areundertaking a piece of work looking at primary care at the frontdoor. There is a lot of work being done and we may be able totake some views on that to see if it is for the benefit of thepatients.TS noted that TMB raised out of hours services becoming morerobust. If there is more extensive GP provision support for out ofhours service, the view was there would be a more appropriateuse of secondary care services.(a)The Pause – The Listening Opportunity for the NHS Reform(Appendix F)TS noted that the <strong>Board</strong> and the Governors engaged in anextensive joint exercise yesterday on this point and relayed thekey feedback:Choice and competition - there should be as much collaborationas possible, if there is competition this must not jeopardise theprovision of local emergency services.Accountability – there is a need for far greater transparency in howprimary care and GPs are using resources. There should be morepatient involvement in decision making._____________________________________________________________________________________BOD/PT 1 MINS 13.05.11 PAGE 4 OF 6
52/11 INFORMATIONClinical advice - integrating working with a multi-professionalapproach.Education and Training - there was support for development of alocalised setup to reflect the needs of local employers.RL and TS will put a response back to the DOH.KA noted that it is disappointing that some believe that withdevolvement of the training monies, we will use it for propping upservices - we must stop this mistaken belief. Partnership boardswill be too big for small to medium organisations to have their say.This will be picked up by Workforce Committee to ensure we areheard.(a)NHS Institute for Innovation and Improvement – EnhancingEngagement in Medical Leadership (Appendix G)TS noted that many recognise our success is due to high qualitymedical engagement.MA added that in other organisations, staff feel much moreisolated.KT commended the leadership of TS and the executive team. Healso noted that this is a really good example of the sharing of bestpractice. TS noted other opportunities to do this will come up.TS noted that the strong clinical engagement has fostered this.MA agreed that 18 years of clinical engagement has helped.Furthermore, continuity of CEO has helped, also the strongsupport of the CDs.(b) Monitor Compliance Framework Changes (Appendix H)HL noted that this needs to be read, but had nothing further toadd.(c) Core Brief (Appendix I)The report was noted for information.(d) Communications Update (inc RAAI April) (Appendix J)The report was noted for information.(e) <strong>Board</strong> of Directors Forward Programme (Appendix K)_____________________________________________________________________________________BOD/PT 1 MINS 13.05.11 PAGE 5 OF 6
The report was noted for information.53/11 DATE OF NEXT MEETINGFriday 10 June 2011 at 08.30am in the Committee Room <strong>Royal</strong><strong>Bournemouth</strong> <strong>Hospital</strong>54/11 ANY OTHER BUSINESS3 Communications points for staff1. Performance to include finance and operations2. The Pause3. The decision to move ahead for Option 1 with ChristchurchSky news exposeTS noted Saxon Square was focussed on in the Sky News expose howeverhe emphasised that we have no responsibility for Saxon Square - there isno link at all to this Trust.55/11 QUESTIONS FROM GOVERNORS1. SB reiterated the excellent quality of the consultation and thefeedback from constituencies is great.2. LF asked if the sickness absence information could appear in CoGpapers - HL agreed._____________________________________________________________________________________BOD/PT 1 MINS 13.05.11 PAGE 6 OF 6
THE ROYAL BOURNEMOUTH AND CHRISTCHURCH HOSPITALSNATIONAL HEALTH SERVICE FOUNDATION TRUSTActions carried forward from a Meeting of the <strong>Royal</strong> <strong>Bournemouth</strong> and Christchurch <strong>Hospital</strong>s National Health Service FoundationTrust <strong>Board</strong> of Directors held on Friday 13 May 2011.47/11 Actions Log (Appendix B)(a)Performance update48/11 MATTERS ARISINGHL gave a verbal update and advised that she is currently workingon some further development of the performance report and willincorporate suggested items and also ensure that it reflects therequirements of the compliance framework. Next month she willbring back recommendations on what the performance reportshould look like going forward to ensure <strong>Board</strong> assurance.(c) Staff Survey (Management Skills) (41/11(b)HLAgenda ItemKA was unable to provide the comparator data but verbally wasable to confirm that training session for managers will beintroduced and agreed to bring further detail back in June.KA Agenda Item Part 2(d) Contract for 2011/12RR noted the Heads of Terms have been agreed and we nowhave the direction of travel for QIPP which is positive. He notedthat we are still working on the actual legal contracts, and aim tocomplete this work by the end of May. TS asked for a report onhow we have ameliorated some of the more punitiverequirements.RRMatters Arising__________________________________________________________________________________________________________________BOD/11.03.11 PAGE 1 OF 1
THE ROYAL BOURNEMOUTH AND CHRISTCHURCH HOSPITALSNHS FOUNDATION TRUSTBOARD OF DIRECTORSMeeting Date and Part: 10 June 2011 (Part 1)Subject:Performance ReportSection:PerformanceExecutive Director with overallresponsibility:Helen Lingham, Chief OperatingOfficerAuthor of Paper:David Mills, Head of InformationSummary:Monthly review of performanceagainst DoH targetsStandards for Better Healthdomain:GovernanceAction required by <strong>Board</strong> ofDirectors:Note for information
<strong>Board</strong> of Directors10 June 20111 Purpose of the ReportPerformance MonitoringThe report outlines the Trust’s position against key access and performance targetsfor the month of April 2011 as set out in the Monitor Compliance Framework andQuality Care Commission requirements.2 Cancer Waiting TimesThis report illustrates the Cancer Waiting Times performance figures for March2011. The targets are as follows: Maximum 14 day wait from urgent GP referral for suspected cancer Maximum 14 day wait for symptomatic breast patients Maximum 31 day wait from diagnosis to treatment for all cancers Maximum 31 day subsequent treatment Maximum 62 day wait from urgent referral to treatment for all cancers Maximum 62 day consultant upgrade Maximum 62 day screening patientsTable 1 illustrates the March 2011 figures against the new thresholds.Table 1 Thresholds Mar-11 Quarter 42 week wait 93% 93.4% 93.4%2 week wait for symptomatic breast patients 93% 98.8% 99.5%31 Day – 1 st treatment 96% 100.0% 99.7%31 Day – subsequent treatment 94% 100.0% 100.0%62 Day – 1 st treatment 85% 88.3% 89.5%62 day – Consultant upgrade 90% 83.3% 91.7%62 day – screening patients 90% 87.5% 95.5%All the Cancer standards were achieved in Quarter 4. The reasons for patientswaiting longer than the target in March were:SCREENINGTumour SiteColorectalReason for BreachBowel Screening Programme capacity issue for the 1 stseen appointment caused delay to the pathway.Performance Monitoring Page 1 of 11For Information
<strong>Board</strong> of Directors10 June 2011CONSULTANT UPGRADETumour Site Reason for BreachPatient needed thoracoscopy but was not keen to haveLungit, later changed mind and was then referred to SGHfor surgical thoracoscopy.3 18 Weeks Referral To TreatmentMaximum wait of 18 weeks from GP referral to treatment (90% for admitted. 95% fornon-admitted)Admitted Pathways (Target 90%)The Trust achieved 96.6% for the aggregate admitted performance in April withalmost all specialities achieving the 90% target. Orthopaedics achieved 89.5%.Part 1a - Total Admitted Patients Clock StoppedCodeSpecialtyRTT Performance TotalNo's % No's100 General Surgery 454 96.8% 469101 Urology 374 100.0% 374110 Trauma & Orthopaedics 552 89.5% 617120 ENT 0 - 0130 Ophthalmology 659 97.8% 674140 Oral surgery 18 100.0% 18150 Neurosurgery 0 - 0160 Plastic surgery 0 - 0170 Cardiothoracic Surgery 0 - 0300 General medicine 368 99.7% 369301 Gastroenterology 0 - 0320 Cardiology 268 99.3% 270330 Dermatology 234 98.3% 238340 Thoracic Med 2 100.0% 2400 Neurology 0 - 0410 Rheumatology 54 100.0% 54430 Eld Med 0 - 0502 Gynaecology 121 93.8% 129Other 93 96.9% 96Total 3197 96.6% 3310Non-Admitted Pathways (Target 95%)The Trust achieved 99.7% for the aggregate non-admitted performance in March. Allspecialities achieved the 95% target.Performance Monitoring Page 2 of 11For Information
<strong>Board</strong> of Directors10 June 2011Part 1b - Total Non-Admitted Patients Clock StoppedCodeSpecialty CodeRTT Performance TotalNo's % No's100 General Surgery 403 99.5% 405101 Urology 90 100.0% 90110 Trauma & Orthopaedics 158 99.4% 159120 ENT 121 98.4% 123130 Ophthalmology 420 100.0% 420140 Oral surgery 86 100.0% 86150 Neurosurgery 0 - 0160 Plastic surgery 0 - 0170 Cardiothoracic Surgery 0 - 0300 General medicine 320 100.0% 320301 Gastroenterology 0 - 0320 Cardiology 142 100.0% 142330 Dermatology 236 100.0% 236340 Thoracic Med 163 100.0% 163400 Neurology 75 97.4% 77410 Rheumatology 178 98.9% 180430 Eld Med 0 - 0502 Gynaecology 222 99.6% 223Other 671 100.0% 671Total 3285 99.7% 3295Median and 95 th Percentile RTT PerformanceThe Trust is performing well against both median and 95 th percentiles for admittedand non admitted patients in April. The aggregate 95 th percentile will become aMonitor and SHA target from April 2011 with the SHA also monitoring the medianwait.Target(wks) Feb-11 Mar-11 Apr-1195th Percentile 23 17.6 17.6 17.4Admitted Median Wait 11.1 5.2 5.4 5.4Non 95th Percentile 18.3 13.1 13.6 13.2Admitted Median Wait 6.6 3.8 3.5 3.6RTT Data Completeness IndicatorThis measure has been removed from the DoH reporting requirements as analternative more appropriate indicator is being sought.4 4 Hour Emergency TargetEmergency accessPerformance Monitoring Page 3 of 11For Information
<strong>Board</strong> of Directors10 June 201195% of patients to wait 4 hours or less in Emergency Department from arrival toadmission, discharge or transfer, across the local health communityFor the month of April the Trust achieved 96.1% overall against the 4 hourturnaround target. The year to date performance is 96.1%.Weekly Emergency Department 4 hour Performance from April 10100%99%98%97%96%95%94%93%92%91%90%04/04/1004/05/1004/06/1004/07/1004/08/1004/09/10Percentage04/10/1004/11/1004/12/1004/01/1104/02/1104/03/1104/04/1104/05/11Data 95% Threshold 98% ThresholdThe table below highlights the additional pressure the emergency department wasunder during April 2011 compared to April 2010.Apr‐10 Apr‐11 % ChangeMain ED Attendances 4238 4393 3.7%Admissions via RBCDU 1656 1952 17.9%The table below illustrates April’s performance against the new A&E qualityindicators. In 2011/12 the Monitor Compliance Framework requires the Total Time inA&E indicator to be met in quarter one and the remaining four indicators fromquarter two.Performance Monitoring Page 4 of 11For Information
<strong>Board</strong> of Directors10 June 2011Emergency Department Quality IndicatorPerformanceTotal time in A&E (95th percentile) - 4hrsTime to initial assessment (95th percentile) - 15minsTime to Treatment decision (median) - 60minsUnplanned re-attendance rate - 5%Left without being seen - 5%April 2011positionAmbulance handover delaysHandover timesAmbulance Crews should take no more then 15 minutes to off load and handoverpatients to the Emergency DepartmentThe graph below illustrates the latest validated performance in ambulance handovertimes over 15 minutes compared to the total number of ambulance handovers.500Patient Handovers -Over 15 Minute Trajectory (NB/ from 24.01.11 ">15 minute actual" ="Validated >15 mins")45040035030025020015010050020/04/0927/07/0902/11/0908/02/1017/05/1023/08/1029/11/1007/03/11w.c>15 Minute Actual >15 Minute Trajectory Validated >15 minutes Total HandoversPerformance Monitoring Page 5 of 11For Information
<strong>Board</strong> of Directors10 June 20115 Infection ControlMRSAIn April there were no hospital acquired bacteraemia and there were no communityacquired bacteraemia. This year the Trust has a de minimis target of 6 (Monitor).Local PCT / SHA targets remain under discussion.MRSA Monitoring 2011/127654MRSA cases pre 48 hrsMRSA cases post 48 hrsCumulative casesTarget - Contract3210Apr-11 May-11 Jun-11 Jul-11 Aug-11 Sep-11 Oct-11 Nov-11 Dec-11 Jan-12 Feb-12 Mar-12MRSA ScreeningThe Trust continues to meet the MRSA screening target for elective patients.Achievement over 100% occurs as this target is calculated by dividing the number ofadmissions by the number of screens. Some admitted patients receive more thanone screen.MRSA Apr-11 May-11 Jun-11 Jul-11 Aug-11 Sep-11 Oct-11 Nov-11 Dec-11 Jan-12 Feb-12 Mar-12Elective Admissions 3323No of MRSA Screens 4018% MRSA Screening 121%Internal audit of the new non elective screening shows good compliance.C.DifficileThe C.Difficile target and trajectory for 2011/12 is 87. The graph below shows theposition for April with performance well within target.Performance Monitoring Page 6 of 11For Information
<strong>Board</strong> of Directors10 June 2011C.Difficile Monitoring - 2011/12C.Difficile cases10090807060504030C.Diff cases - post 48 hrsCumulative - post 48 HrsTarget20100Apr-11 May-11 Jun-11 Jul-11 Aug-11 Sep-11 Oct-11 Nov-11 Dec-11 Jan-12 Feb-12 Mar-126 StrokeStroke target80% of stroke patients treated on a dedicated stroke ward for 90% of theirspell60% of high risk TIA cases investigated and treated within 24 hours by April2011April’s performance against the Stroke targets remains good. 84% of stroke patientswere treated on a dedicated stroke unit for 90% of their spell. This is a PCT target,Monitor has yet to confirm the Stroke target & threshold for 2011/12.Performance Monitoring Page 7 of 11For Information
<strong>Board</strong> of Directors10 June 2011In April the Trust achieved 64% of high risk TIA cases being investigated and treatedwithin 24 hours.PeriodIndicator Key Performance Indicators Target Apr-11 May-11 Jun-11 Jul-11Stroke Stroke patients are treated on a dedicated stroke ward for 90% of spell 80% 84.0%High risk TIA cases investigated and treated within 24hrs 60% 62%7 Cancelled OperationsCancelled operationsAll patients cancelled on the day of admission or after admission for nonmedicalreason to be admitted for treatment within 28 days or have theirtreatment funded at the time and hospital of the patient’s choiceTarget:
<strong>Board</strong> of Directors10 June 20118 15 Key Diagnostic TestsThe table below reflects the patients currently waiting for one of the 15 keydiagnostic tests. At the end of April there were 9 patients waiting over 6 weeks whichresulted from an increase in fast track referrals requiring urgent procedures. This is asignificant improvement from the March position (60 patients waiting over 6 weeks).April 2011 15 Key Diagnostic TestsCategoryImagingPhysiologicalMeasurementEndoscopyDiagnostic Test< 06Weeks06 < 07Weeks07 < 08Weeks08 < 09Weeks09 < 10Weeks10 < 11Weeks11 < 12Weeks12 < 13Weeks13 plusWeeksMagnetic Resonance Imaging 622 0 0 0 0 0 0 0 0Computed Tomography 266 0 0 0 0 0 0 0 0Non-obstetric ultrasound 874 0 0 0 0 0 0 0 0Barium Enema 6 0 0 0 0 0 0 0 0DEXA Scan 231 0 0 0 0 0 0 0 0Audiology - Audiology Assessments 0 0 0 0 0 0 0 0 0Cardiology - echocardiography 345 0 0 0 0 0 0 0 0Cardiology - electrophysiology 2 0 0 0 0 0 0 0 0Neurophysiology - peripheral neurophysiology 0 0 0 0 0 0 0 0 0Respiratory physiology - sleep studies 0 0 0 0 0 0 0 0 0Urodynamics - pressures & flows 91 0 0 0 0 0 0 0 0Colonoscopy 132 1 1 2 1 0 0 0 0Flexi sigmoidoscopy 120 0 1 0 1 0 1 0 0Cystoscopy 109 0 0 0 0 0 0 0 0Gastroscopy 181 1 0 0 0 0 0 0 0Total 2979 2 2 2 2 0 1 0 09 Delayed Transfers of CareDelayed transfers of care to be maintained at a minimal levelNumber of patients whose transfer of care was delayed as a proportion of thetotal numbers of patients admitted, reported on a weekly basisThe position for April is 1% of acute patients were reported with delayed transfers ofcare.Performance Monitoring Page 9 of 11For Information
<strong>Board</strong> of Directors10 June 2011Weekly Delayed Discharges Occupancy Ratefor 2011.125.0%4.5%4.0%3.5%3.0%2.5%2.0%1.5%1.0%0.5%0.0%DTOC Actual for Week3.5% TrajectoryDTOC Actual YTDThe table below shows the site split for all delayed transfers of care patients.RBHChristchurch3530252015105028/02/11‐06/03/1107/03/11‐13/03/1114/03/11‐20/03/1121/03/11‐27/03/1128/03/11‐03/04/1104/04/11 ‐ 10/04/1111/04/11 ‐ 17/04/1118/04/11 ‐ 24/04/1124/04/11 ‐ 01/05/1102/05/11 ‐ 08/05/1109/05/11 ‐ 15/05/1116/05/11 ‐ 22/05/1128/03/2011-03/04/201104/04/2011-10/04/201111/04/2011-17/04/201118/04/2011-24/04/201125/04/2011-01/05/201102/05/2011-08/05/201109/05/2011-15/05/201116/05/2011-22/05/2011Performance Monitoring Page 10 of 11For Information
<strong>Board</strong> of Directors10 June 2011The table below shows the breakdown of April SITREP reportable delayed transfersof care by reason.Acute Delayed Discharges byReason for Delay: Health Social ServicesA) Completion of AssessmentB) Public FundingC) Further non acute NHS care(including intermediate care,4rehabilitation etc)D) Care Home placement i) Residential Home 1ii) Nursing HomeE) Care package in own home 1F) Community Equipment/adaptionsG) Patient or family choiceH) DisputesI) Housing - patients not covered byNHS and Community Care Act1TOTAL 6 110 Venous Thromboembolism (VTE)Prevention of Venous Thromboembolism (VTE)The number of adult hospital admissions who are being risk assessed forVenous Thromboembolism (VTE) to allow appropriate prophylaxis based onnational guidance from NICE (Target 90%)This is a new target which started in June 10. Performance continues to beexcellent; the Trust achieved 94.5% of patients being risk assessed for VTE in April.Venous Thromboembolism (VTE)Score Apr-10 May-10 Jun-10 Jul-10 Aug-10 Sep-10 Oct-10 Nov-10 Dec-10 Jan-11 Feb-11 Mar-11 Apr-11VTE Assessments 88.4% 90.6% 90.2% 91.5% 94.3% 91.8% 92.8% 92.8% 94.7% 94.8% 94.5%12 RecommendationThe <strong>Board</strong> of Directors is requested to note performance and theongoing work which will support compliance with the new Monitorregulations from December 2010.HELEN LINGHAMCHIEF OPERATING OFFICERPerformance Monitoring Page 11 of 11For Information
APPENDIX 12011/12 Performance RAG Report for June 2011 TMB and <strong>Board</strong> MeetingsInfectionControlTargetIndicator Key Performance Indicators NationalApril (exceptCancer - March)YTD(2011/12)MRSA Bacteraemias 6 0 0Clostridium difficile year on year reduction 87 3 3Cancer 2 weeks - Maximum wait for urgent suspected cancer referrals from GP 93% 93.4% 93.4%2 week wait for symptomatic breast patients 93% 98.8% 99.5%31 Day – 1st treatment 96% 100.0% 99.7%31 Day – subsequent treatment 94% 100.0% 100.0%62 Day – 1st treatment 85% 88.3% 89.5%62 day – Consultant upgrade 90% 83.3% 91.7%62 day – screening patients 90% 87.5% 95.5%Elective Access18 weeks referral to treatment - Admitted 90% 96.6% 96.6%18 weeks referral to treatment - Non Admitted 95% 99.7% 99.7%Inpatient waits - No. of patients who breached 26 weeks 0 0 0Outpatient waits - No. of patients who breached 13 weeks 0 0 015 Key Diagnostics - Patients who breached 6 weeks 0 9 9Emergency % of patients meeting 4 hour maximum wait in Emergency dept 95% 96.1% 96.1%StrokePeriodStroke patients are treated on a dedicated stroke ward for 90% of spell 80% 84.0% 84.0%% of high risk TIA cases investigated & treated within 24hrs 60% 62.0% 62.0%Cancelled OPs No. of cancelled operations not rebooked within 28 Days
THE ROYAL BOURNEMOUTH AND CHRISTCHURCH HOSPITALSNHS FOUNDATION TRUSTBOARD OF DIRECTORSMeeting Date:10 th June 2011, Part ISubject:Financial PerformanceSections:PerformanceExecutive Director with overallresponsibility:Stuart Hunter, Director of Finance & ITAuthor of Paper:Phil Trevorrow, Deputy Director ofFinanceSummary:Review of the financial performance forApril 2011Standards for Better Health domain:GovernanceAction required by <strong>Board</strong> ofDirectors:Note for Information
<strong>Board</strong> of DirectorsJune 2011Transformation Programme (TP)The recorded savings in month one total £492k against a target of £541k. The ProjectManagement Office continues to work with Directorates to identify and embedadditional schemes.Capital expenditureExpenditure is currently under target, standing at £192k against a plan of £253k.7. WorkforceStaffing numbers continue the previous year’s trend and are currently belowestablishment by 145 WTE’s in the month (4%). Sickness levels were 3.9% in monthone, being below the target of 4%.8. Monitor Risk IndicatorsThese are all green.9. RecommendationThe Trust Management <strong>Board</strong> are invited to consider and note this report.Phil TrevorrowDeputy Director of Finance24 May 2011Financial Performance Page 2 of 2For information
The <strong>Royal</strong> <strong>Bournemouth</strong> & Christchurch <strong>Hospital</strong>s NHS Foundation Trust - Summary Performance Report as at 30 April 2011ACTIVITY 2011/12YTD2010/11Actual YTD Plan YTD ActualYTDVarianceFull yearplanFull yearforecastForecast vsplanvariancePlanned same day / day cases 3,933 3,384 3,745 361 47,382 47,382 0Elective spells 913 768 919 151 10,755 10,755 0Non elective spells 2,260 2,115 2,664 549 25,809 25,809 0Outpatient attendances 19,595 19,120 20,057 937 267,686 267,686 0Outpatient Pre assessment 0 1,405 1,743 338 19,675 19,675 0ED attendances 5,549 5,361 5,463 102 65,401 65,401 0INCOME 2011/12YTD2010/11Actual YTD budget YTD actual VarianceFull yearbudgetFull yearforecastForecast vsbudgetvariance£000 £000 £000 £000 £000 £000 £000Planned same day / day cases 2,899 2,376 2,512 136 33,269 33,269 0Elective spells 2,921 2,396 2,409 13 33,539 33,539 0Non elective spells 4,274 4,281 4,316 35 52,230 52,230 0Outpatient attendances 2,451 2,444 2,473 28 34,222 34,222 0ED attendances 432 410 412 2 5,006 5,006 0Cost and volume 1,855 1,491 1,532 41 20,878 20,878 0Block 1,626 1,634 1,634 -0 19,613 19,613 0MFF 630 771 752 -18 10,242 10,242 0Interest receivable 27 33 25 -9 400 400 0Non contracted 1,638 2,497 2,389 -108 21,005 21,005 0Total 18,752 18,334 18,455 121 230,403 230,403 0EXPENDITURE 2011/12YTD2010/11Actual YTD budget YTD actual VarianceFull yearbudgetFull yearforecastForecast vsbudgetvariance£000 £000 £000 £000 £000 £000 £000Pay 11,468 11,495 11,347 148 137,456 137,456 0Drugs 1,788 1,662 1,653 9 20,681 20,681 0Clinical supplies 2,897 2,562 2,582 -19 31,542 31,542 0Other costs 1,466 1,653 1,651 2 25,662 25,662 0Depreciation 710 748 751 -4 9,594 9,594 0Dividends payable 421 415 425 -10 4,968 4,968 0Total 18,750 18,534 18,409 125 229,902 229,902 0OTHER FINANCIALS 2011/12YTD2010/11Actual YTD plan YTD actual VarianceFull yearplanFull yearforecastForecast vsplanvariance£000 £000 £000 £000 £000 £000 £000EBITDA 1,106 929 1,198 269 14,663 14,663 0EBITDA margin 5.9% 5.8% for Q1 6.5% 7.0% 5.9% 5.9% 0Net surplus / (deficit) 2 -201 46 247 501 501 0Transformation Programme 226 541 492 -49 7,879 7,304 -575Capital expenditure 480 253 192 61 9,611 9,611 0STATEMENT OF FINANCIAL POSITION 2011/12YTD2010/11ActualYTD actualFull yearplanFull yearforecastForecast vsplanvariance£000 £000 £000 £000 £000Non Current Assets 146,354 149,193 150,399 150,399 0Current assets 51,427 48,177 45,267 45,267 0Current and Non Current liabilities -31,808 -19,996 -18,485 -18,485 0Total assets employed 165,973 177,374 177,181 177,181 0Public dividend capital 78,674 78,674 78,674 78,674 0Income and expenditure reserve 15,147 22,373 22,829 22,829 0Revaluation reserve 65,957 69,326 69,325 69,325 0Donated asset reserve 6,195 7,001 6,353 6,353 0Total funds employed 165,973 177,374 177,181 177,181 0WORKFORCE 2011/12YTD2010/11Actual Establish ment Actual VarianceFull yearplanFull yearforecastForecast vsplanvarianceStaff (whole time equivalents) 3,603 3,695 3,550 145 3,678 3,678 0Sickness rate 4.5% 4.0% 3.9% 0.1% 4.0% 4.0% 0.0%Turnover rate 11.4% 9.6%ACTIVITYBelow target 0 to 5%Below target by more than 5%Above target 0 to 5%Above target by more than 5%SUMMARY FINANCIALSEBITDA as per income rulesSurplus as per income rulesCIP as per income rulesCapex as per Monitor rules i.e. 25%The 5% rulesINCOMEEXPENDITUREBelow budget 0 to 5% Below budget 0 to 5%Below budget by more than 5% Below budget by more than 5%Above budget 0 to 5% Above budget 0 to 5%Above budget by more than 5% Above budget by more than 5%BALANCE SHEETWORKFORCEPlan variance 0 to 5% Below target 0 to 5%Below plan by more than 5% Below target by more than 5%Above plan 0 to 5% Above target 0 to 5%Above plan by more than 5% Above target by more than 5%
Proposed indicatorUnplanned decrease in Earnings before Interest,Tax, Depreciation & Amortisation (EBITDA)margin in two consecutive quartersPotential financial weaknessDeteriorating trend in operating performance andcash flow generationQ12011/12PlanQ22011/12PlanQ32011/12PlanQ42011/12Plan2011/12Month 1ActualQuarterly self-certification by trust that theFinancial Risk Rating (FRR) may be less than 3in the next 12 monthsIdentified risk of potential financial breach withinthe next yearFRR 2 for any one quarterIn year deterioration in financial performanceWorking capital facility (WCF) agreementincludes default clause. This will require all truststo review their WCF agreements.Risk that WCF, whilst included in calculation ofliquidity days for the purpose of FRR, may not beavailable if and when required e.g. FRR 1 or 2.Debtors more than 90 days past due account formore than 5% of total debtor balancesPotential for payment / debtor collectionconcernsCreditors more than 90 days past due accountfor more than 5% of total creditor balancesPotential for build up in creditors, resulting infuture liquidity concernsCapital expenditure is less than 75% of plan forthe year to dateCapital expenditure plans are delayed toconserve cashQuarter end cash balance less than 10 days ofoperating expenses or less than £4 million.Potential liquidity concerns and ability to meetliabilities as they fall dueInterim Finance Director in place over more thanone quarter endAbsence of permanent / substantive appointmentto key positionTwo or more changes in Finance Director in atwelve month periodMultiple changes in a short period of leadfinancial officer
THE ROYAL BOURNEMOUTH AND CHRISTCHURCH HOSPITALSNHS FOUNDATION TRUSTBOARD OF DIRECTORSMeeting Date and Part: 10 June 2011 (Part 1)Subject: Performance Reporting 2011/12Section:For decisionExecutive Director with overallresponsibility:Helen Lingham, Chief OperatingOfficerAuthor of Paper:Donna Parker, Deputy ChiefOperating OfficerSummary:Proposed amendments to the Trust’s<strong>Board</strong> performance reporting toreflect the changes made in theOperating Framework 2011/12Standards for Better Healthdomain:GovernanceAction required by <strong>Board</strong> ofDirectors:The <strong>Board</strong> is asked to support theadvised changes to the regularperformance reporting dashboard
<strong>Board</strong> of Directors Part 110 June 20111 BackgroundPerformance Reporting 2011/12The 2011/12 Monitor Compliance Framework was published on 31 March 2011following its earlier consultation exercise and publication of the OperatingFramework for the NHS in England 2011/12. A paper was submitted to the<strong>Board</strong> in May outlining the amendments to the Framework. This includedchanges that had been made to the governance indicators to reflect the2011/12 Operating Framework.In light of these changes and the proposed PCT contract schedules, in order toensure governance of our key national and local indicators, the followingamendments to the Trust’s performance reporting is proposed.2 AdditionsThe following indicators will be added to the Trust <strong>Board</strong> report (a number ofthese have been included within the report in recent months due to theanticipated changes in indicators):Indicator Measure MonitorTargetOperatingFrameworkPCTContractInternalTargetReferral to Treatment Waiting TimesAdmitted (95 th percentile) 18 weeks from GP referral to 1 st 23 wks Yes 23 wks 23 wkstreatment – aggregate levelNon Admitted (95 th percentile) 18 weeks from GP referral to 1 st 18.3 Yes 18.3 wks 18.3 wkstreatment – aggregate level wksAdmitted (median)18 weeks from GP referral to 1 st N/A Yes 11.1 wks 11.1 wkstreatment – aggregate levelNon Admitted (median) 18 weeks from GP referral to 1 sttreatment – aggregate levelN/A Yes 6.6 wks 6.6 wksA&E Quality IndicatorsTotal Time in A&E (95 thpercentile)Percentage of patients spending 4hours or less in A&ETime to Initial Assessment Percentage of patients receiving(95 th percentile) 1 initial assessment in 15 mins orlessTime to Treatment Decision(median) 1Unplanned ReattendanceRate 1Left Department Without BeingSeen 1Ambulatory CareA&E Service ExperienceConsultant Sign-offPercentage of patients seeingdecision making clinician in 1 hr orlessPercentage of patients reattendingA&E within 7 daysPercentage of patients who leftdepartment without being seenAmbulatory care for cellulitis casesand DVT careExperience of 24hr nature ofservice collected and acted uponPercentage of patients presentingat A&E sites in certain high riskcategories who are reviewed by anemergency medicine consultantbefore being discharged< 4 hrs Yes < 4 hrs < 4 hrs< 15minsYes < 15mins< 15 mins< 1 hr Yes < 1 hr < 1 hr< 5 % Yes < 5 % < 5 %< 5 % Yes < 5 % < 5 %N/A Yes tbc tbcN/A Yes tbc tbcN/A Yes tbc tbc1 Note: these measures are not reportable to Monitor until Q. 2Performance Reporting 2011/12 Page 1 of 4For decision
<strong>Board</strong> of Directors Part 110 June 2011Indicator Measure MonitorTargetStroke IndicatorsTIA Low Risk PatientsBrain Imaging – as perindicationsPercentage of low risk patientsseen, assessed and treated by astroke specialist within 7 days ofcontactOperatingFrameworkPCTContractN/A N/A tbc -100%Patients with acute stroke meeting N/A N/A tbc –imaging within 1 hr 2the indications receive brain95%InternalTargettbc - 100%tbc – 95%N/A N/A tbc –Brain Imaging – other stroke Other stroke patients receive braintbc - 100%imaging within 24 hrs 3 N/A N/A tbc -100%Direct Admission to Stroke Patients with suspected stroke aretbc – 90%within 4 hrs of arrival 4Unitadmitted to a specialist stroke unit90%Alteplase (Thrombolysis) Percentage of appropriate patients N/A N/A tbc 100%receiving thrombolysisOther Quality and Performance TargetsMixed Sex AccommodationBreachesNo of patients affected by a breachof the mixed sex sleepingN/A Yes 0 0Bowel Cancer ScreeningWorkforceAttendanceAppraisalsaccommodation requirementTo meet the current minimumstandards set by the BCSPPercentage of monthly andcumulative sickness by directoratePercentage compliance with annualappraisalsN/A N/A QtrlyaudittbcN/A N/A N/A 4% - 3%stretchN/A N/A N/A 90%A summary of hospital activity including relevant elective and non electiveadmissions, outpatient and ED attendances will be provided at the beginning ofthe monthly report to provide context to the Trust’s performance against thegovernance indicators.MSSA, E Coli and Readmission measures will be added during the year iftargets are confirmed.3 AmendmentsIndicator Measure MonitorTargetCancerCancer 62 Day Wait fromConsultant UpgradeOperatingFrameworkPCTContractInternalTargetAlthough this measure is no longer required by Monitor, it remains within the OperatingFramework although the PCT target has yet to be confirmed. This will continue to beincluded in the <strong>Board</strong> report following confirmation of the agreed target .Infection ControlC Difficile and MRSAThe PCT are currently in discussion with the Trust to confirm local targets and anyamendments will be reflected in the Trust <strong>Board</strong> report going forward. The Monitortargets will remain at 87 for C Difficile and 6 (de minimis) for MRSA and achievementagainst these will continue to be reported.Indicator Measure MonitorTargetOperatingFrameworkPCTContractInternalTarget2 The stroke best practice tariff requires imaging within 1hr. Network aspirations are for 30mins and therefore, thePCT target is under discussion.3 The stroke best practice tariff requires imaging within 24 hrs. Network aspirations are for 12 hrs and therefore,the PCT target is under discussion.4 The stroke best practice tariff requires direct admission within 4 hrs. Network aspirations are 45 mins linked tothrombolysis assessment and therefore, the PCT target is under discussion.Performance Reporting 2011/12 Page 2 of 4For decision
<strong>Board</strong> of Directors Part 110 June 2011Stroke Indicators90% Time Spent on StrokeWardPercentage of patients spending90% or more of their time on thestroke ward during their inpatientstayOther Quality and Performance TargetsDelayed Transfers of Care Delayed transfer of care levels asper Heads of Terms (attributable)tbc 5 Yes 80%(90% byApr2012)N/A Yes 10 1080% -increasingin Q.4 to90% Mar124 RemovedThe following measures are no longer required by Monitor or as part of theOperating Framework and will therefore, be removed:MRSA Elective ScreeningAmbulance HandoversCoronary Heart DiseaseHowever, these will continue to be monitored internally (see below for thosereported to the weekly internal Performance Management Group).5 Monitored at Performance Management GroupIn addition to the above and other operational management measures, thefollowing will continue to/be monitored internally at the weekly PerformanceManagement Group meeting:Indicator Measure MonitorTargetOperatingFrameworkPCTContractInternalTargetReferral to Treatment Waiting TimesIncomplete Pathways (95 th Weeks waiting on an incomplete N/A Yes 28 wks 28 wkspercentile)pathwayIncomplete Pathways (median) Weeks waiting on an incomplete N/A Yes 7.2 wks 7.2 wkspathwayRTT waiting times admitted 90% admitted – speciality level N/A N/A 90% 90%RTT waiting times non95% non admitted – speciality level N/A N/A 95% 95%admittedDiagnostics Patients waiting greater than 6 N/A N/A 0 0weeksInfection ControlMRSA elective screening Percentage of total (included) N/A N/A N/A tbcadmissions screenedMRSA non elective screening Percentage of total (included) non N/A N/A N/A tbcelective admissions screenedStroke IndicatorsOther Stroke Indicators NICE and Network measures e.g.rehab, swallow assessment.N/A N/A tbc tbcOther Quality and Performance TargetsAmbulance HandoversNo. of patients waiting >15 minsand >25 minsN/A N/A tbc tbcThe PCT contracting schedules currently remain under discussion. Any furtheradditions or amendments will be notified to the <strong>Board</strong> following conclusion.5 The Monitor and Operating Framework stroke indicator is yet to be confirmed but it is anticipated that thismeasure is likely to feature.Performance Reporting 2011/12 Page 3 of 4For decision
<strong>Board</strong> of Directors Part 110 June 20116 RecommendationThe <strong>Board</strong> of Directors is asked to support the advised changes tothe regular performance reporting dashboard. Any in yearadjustments required through finalisation of the PCT contractdiscussions will be populated as appropriate.HELEN LINGHAMCHIEF OPERATING OFFICERPerformance Reporting 2011/12 Page 4 of 4For decision
THE ROYAL BOURNEMOUTH AND CHRISTCHURCH HOSPITALSNHS FOUNDATION TRUSTBOARD OF DIRECTORSMeeting Date and Part:10 June 2011 Part ISubject:Where next for NHS Reforms? The case forIntegrated CareSections:InformationExecutive Director with overallresponsibility:Tony Spotswood, Chief ExecutiveAuthors of Paper:Tony Spotswood, Chief ExecutiveSummary:Article from the Kings FundStandards for better HealthDomain:Clinical and Cost EffectivenessAccessible and Responsive CareAction required by <strong>Board</strong> ofDirectors:To note for information
<strong>Board</strong> of Directors10 June 2011THE ROYAL BOURNEMOUTH & CHRISTCHURCH HOSPITALSNHS FOUNDATION TRUSTWhere next for the NHS Reforms?The Case for Integrated CareThe attached paper authored by the Kings Fund is provided to the <strong>Board</strong> of Directorsfor information. It provides a thoughtful and thorough assessment of theopportunities The Pause presents for reviewing aspects of the Health Bill. Inparticular, it sets out the case for a more searching diagnosis of the problems/challenges facing the NHS and sets out a new model of integrated care in whichclinicians work together more closely to meet the needs of patients and co-ordinateservices. The model of integrated care focuses more on preventing ill health,supporting self care, embracing primary care, and increasing co-ordination betweenprimary care teams and specialists and between health and social care.There are a number of facets of this approach which would serve Dorset well inresponding to the challenges that lie ahead.This paper is provided for information.Tony SpotswoodChief ExecutiveWhere next for Health Reforms? Page 1 of 1For Information
Where next for the NHS reforms?The case for integrated careAuthors:Chris HamCandace ImisonNick GoodwinAnna DixonPatrick SouthThe King’s Fund11–13 Cavendish SquareLondon W1G OANTel 020 7307 2400Registered charity: 1126980www.kingsfund.org.ukSummaryThis paper sets out the challenges facing the English NHS now and in the futureand identifies the reforms we believe are needed to meet these challenges. It hasbeen written as a contribution to the listening exercise initiated by the coalitiongovernment following the announcement at the beginning of April of a pausein the parliamentary passage of the Health and Social Care Bill. It builds on TheKing’s Fund’s response to the health White Paper published in July 2010 (Dixon andHam 2010), our briefing for the second reading debate on the Bill in the House ofCommons (The King’s Fund 2011a), and our extensive programme of policy analysisand research.The main argument of the paper is that reforms to the NHS must be clearly focusedon, and proportionate to, the challenges it faces. One of the reasons the coalitiongovernment has run into difficulty is that it moved very rapidly to set out radicalchanges to the NHS without having first clarified the problems that these reformswere meant to address. The King’s Fund is in no doubt that in some areas there isscope to improve performance and to move closer to the standards of care achievedin other countries, but we suggest that a clear diagnosis of the state of the NHStoday is needed to inform the design of future reforms.The NHS is faced with the major challenges of using resources more efficiently andof meeting the needs of an ageing population in which chronic medical conditionsare increasingly prevalent. The key task therefore is to implement a new model ofcare in which clinicians work together more closely to meet the needs of patientsand to co-ordinate services. This model of integrated care would focus much moreon preventing ill health, supporting self-care, enhancing primary care, providingcare in people’s homes and the community, and increasing co-ordination betweenprimary care teams and specialists and between health and social care.There are many barriers to the implementation of integrated care, includingorganisational complexity, divisions between GPs and specialists, perversefinancial incentives, and the absence of a single electronic medical record availablethroughout the NHS. The coalition government’s proposed reforms have thepotential to help overcome some of these barriers but they could also make it moredifficult to achieve closer integration of care unless they are modified in a numberof areas. Our paper Liberating the NHS: The right prescription in a cold climate?proposed a series of modifications centred on the argument that well-designedreforms must strike a balance between collaboration in some areas of care andcompetition in others (Dixon and Ham 2010).In this paper, we offer suggestions for revisions to the current Bill and future policydevelopment but we also lay out a more radical model that we believe holds theprospect of greater progress towards the vision of integrated care and a healthsystem sustainable in the longer term.© The King’s Fund 2011
Where next for the NHS reforms in England?Proposed legislation and future policy:summary of recommendationsMany of the changes we outline do not require legislationand should be taken forward as a matter of urgencythrough established policy-making processes. The mainimplication for the Bill is to ensure that its centrepieceproposals for economic regulation do not promote thewrong kind of competition or create further barriers tocollaboration and the development of integrated carewhere this will bring benefits. Monitor must adopt anuanced and proportionate approach that encouragesboth collaboration and competition where appropriate.In our view, the Bill needs to create a regulatoryframework that supports the development of moreintegrated models of care and multi-professionalcollaboration at all levels within the NHS. The frameworkshould enable local innovation and allow the continuingadaptation of service models as medicine advances andthe needs of patients change. While we support theneed to promote patient choice, and competition whereappropriate, we believe that all organisations engagedin regulating, commissioning or providing NHS careshould have the goal of integration ‘hard-wired’ into theircorporate objectives.The key changes that could facilitate integrated includethe following.• Alternatives to the tariff are needed for nonelective,long-term and complex care. Thesealternatives may include bundled payments, pooledor delegated budgets and capitated budgets. Anypayment mechanism adopted needs to ensurethat financial rewards are linked to the quality andoutcomes of care.• There is a need for system leadership at a regionallevel and this should be provided by multiprofessionalclinically led groups or clinical cabinetsworking with the NHS Commissioning <strong>Board</strong>.• Joint working between health and social care needsto be facilitated in order to ensure population healthissues are addressed, including tackling healthinequalities and the needs of unregistered patients.GP commissioning boundaries should, as far aspossible, be aligned to local authority boundaries tosupport this.• At a local level, multi-professional health and socialcare teams that support the needs of high-riskpatients such as frail older people should be a coreelement of service provision, as is already the casefor patients with chronic mental health problems andlearning disabilities.• To support clinical integration and patient-focusedcare, anyone providing or commissioning NHScare should be required as part of their licensingagreement or statutory function to share relevantinformation with patients and professionals.The reforms and the legislation should also allow theevolution of new approaches. At the end of this paperwe lay out one such approach – the integrated carepartnership – that The King’s Fund and others have longadvocated should be piloted (Curry et al 2008; Lewis et al2010). Under this approach the commissioning functionis split between a strategic commissioner and budgetholding,not-for-profit, integrated care partnerships.These integrated care partnerships might include GPsand relevant health and social care specialists formingorganisations that take on a capitated, risk-bearingbudget for a defined population while also being chargedwith the provision of care where appropriate.2 © The King’s Fund 2011
The King’s Fund ResponseIntroductionThroughout the debate on the White Paper and theHealth and Social Care Bill, The King’s Fund has arguedthat the real choice is not between stability andchange but between reforms that are well designedand effectively implemented and those that are poorlyplanned and risk undermining NHS performance. Ourconcerns with the coalition government’s proposalshave centred on a view that they are moving toofar and too fast and that this will make it difficult toachieve the productivity improvements required todeliver the so-called ‘Nicholson challenge’. This paperdescribes how to design and implement the rightreforms for the NHS, starting from where it is now andadopting an evolutionary path of change.How good is the NHS?The NHS has made significant progress over the pastdecade. Our review of NHS performance since 1997,published a year ago (Thorlby and Maybin 2010), identified anumber of notable achievements:• hospital waiting times have been transformed, withmore than 90 per cent of patients waiting less than 18weeks for treatment, with improvements in access to GPservices too• infant mortality has fallen and life expectancy isincreasing for all social groups• smoking rates have fallen, and deaths from cancer andcardiovascular diseases have been steadily declining• infection rates for MRSA and C difficile have beensignificantly reduced, and there are now robustsystems for collecting and analysing information onadverse events• in mental health services, access to specialist earlyintervention and crisis resolution teams is consideredamong the best in Europe and has led to reductions inacute admissions• there is now far more information available to patients,professionals and the public about how services perform.This analysis is reflected in national and internationalsurveys.• According to the British Social Attitudes Survey, 64per cent of people report that they are satisfied withthe NHS, a record high (Appleby et al 2010a).• The UK was ranked second in an assessment ofhealth systems in seven countries published by theCommonwealth Fund in June 2010 (Davis et al 2010).• In November 2010, a Commonwealth Fund survey of11 leading nations found that people in the UK have thehighest levels of confidence in the effectiveness andaffordability of health treatment (Schoen et al 2010).However, while good progress has been made, there are anumber of areas where performance needs to improve beforethe NHS can be deemed truly world class. For example:• although cancer survival rates have improved,international comparisons suggest we still lagbehind other countries in survival rates for severaltypes of cancer• while infant mortality has fallen, recent analysispublished by the BMJ suggests that child mortalityrates in the United Kingdom are higher than in manyother European countries (Wolfe et al 2011)• NHS productivity has declined by an average of 0.2per cent a year since 1995, according to estimatesby the Office for National Statistics (National AuditOffice 2011)• while progress has been made in reducing smoking,alcohol consumption and related hospital admissions areincreasing, and obesity rates have risen significantly• inequalities in life expectancy between rich andpoor have widened, even though life expectancy isincreasing for all groups• support for people with long-term conditions isinconsistent, and people continue to be admittedto hospital for conditions that could be managed inthe community• variations in the quality of general practice and in thetreatment provided in hospitals remain persistent andwidespread (The King’s Fund 2011b; Appleby et al2011).Against this background of substantial progress, albeitwith more work to do, the case for reform is clear,but the nature of reform needs to be focused on and© The King’s Fund 2011 3
Where next for the NHS reforms in England?proportionate to the problems to be addressed.What are the main challenges forthe future?As well as focusing on the areas where the performanceof the NHS needs to improve, any reforms must addressthe future challenges it faces. The most immediate andpressing challenge for the NHS is to continue to improvepatient care in a very difficult financial climate.NHS spending now stands at more than £100 billion ayear. Although the coalition government’s pledge toprotect the health budget meant it fared well comparedto other Whitehall departments in the Spending Review,expenditure will be flat in real terms in the years up to2015. To put this into perspective, the NHS has averagedreal-terms increases of 4 per cent a year since it wasestablished and 7 per cent since the turn of the century.The only similar period of near-zero real-terms growthwas in the early 1950s.In order to maintain the quality of care and meetrising demand for services, the Spending Review alsocommitted the NHS to finding £20 billion in productivityimprovements by 2015 – the so-called ‘Nicholsonchallenge’. This requires it to deliver efficiency savingsof at least 4 per cent a year, unprecedented in its history.Finding these savings must be the overriding priorityfor the NHS over the next few years, and any reformsmust support it in meeting this challenge. The majororganisational changes already under way, includingthe planned abolition of strategic health authorities,the clustering of PCTs, and reductions in managementcosts, risk distracting leaders from the task of improvingfinancial performance and the quality of care.The NHS faces other key challenges.Demographic change: people are living longer and thepopulation is ageing. While many people live both longand healthy lives, increasing numbers are affected byconditions such as dementia that affect their quality oflife and place demands on families, carers and the healthand social care systems.Social change: more people are living in single-personhouseholds and further from their extended family.There will therefore be less marital and family supportfor people as they get older and increased demand onpaid/statutory support.The shifting burden of disease: premature death ratesfrom cardiovascular diseases and cancer have declinedbut chronic conditions such as diabetes, asthma, chronicobstructive pulmonary disease, heart failure, arthritisand dementia have become more prevalent. As thepopulation ages, a high proportion of NHS funds willbe spent on meeting the needs of increasing numbersof older frail people with multiple conditions and comorbidities.Public expectations: increased levels of per capitaincome and educational attainment have contributedto rising public expectations of the NHS. The NHSof the future will need to deliver more personalised,patient-centred services that give people genuinechoice and control.Medical advances: new forms of diagnosis andtreatment have contributed to long-term improvementsin population health, and developments in genomics,stem cell research and other fields hold out promise forthe future but have significant implications for futurespending on health care.A new model of careCurrent models of care reflect the legacy of decisionstaken during the lifetime of the NHS. These models arecentred on the provision of episodic treatment to addressthe main burden of disease in the second half of thetwentieth century, namely cardiovascular diseases andcancer. Acute hospitals have come to play an increasinglyprominent part in the NHS as successive governmentshave sought to make available effective treatment forpeople affected by these life-threatening conditions.Demographic changes and the shifting burden of diseaserequire a re-assessment of the hospital-based modelof care. Meeting the health needs of the increasingnumbers of older people should be a high priority. Whilemany of these people will live long and for the most parthealthy lives, others will require support from both theNHS and social care. This includes services for peoplewith dementia and other chronic conditions to enablethem to live independently in the community for as longas possible.4 © The King’s Fund 2011
The King’s Fund ResponseA new model of care is needed, less oriented to treatingpeople when they become ill and more focused onprevention, accompanied by a progressive shift inresources away from acute hospitals to providing care inand closer to people’s homes. This should seek to achievethe triple aim of improved patient experiences, betterhealth outcomes and more cost-effective care. Moving tothe new model requires a comprehensive approach thatimproves the co-ordination of services for patients andpromotes integration in the delivery of care.Key elements in the new modelPrevention of ill health: action at the population/community level and targeted at individuals to identifypeople at risk, address risk factors and fully engage thepopulation in bringing about further improvement inlife expectancy and in the quality of life. This includesaction to reduce the health gap between more and lessaffluent groups.Supported self-care: action to enable individuals, carersand families to make healthy choices and to continue toplay a key role in looking after themselves when theybecome ill or are diagnosed with a chronic condition. Thisincludes the use of assistive technologies in the homeand training programmes to provide people with theconfidence and skills to manage their conditions.Enhanced primary care: action to reduce variationsin the quality of primary care and to provide additionalservices that help to keep people out of hospital. Thisrequires a network of primary care providers thatpromote and maintain continuity of care with localpeople and act as hubs not only for the provision ofgeneralist care but also for access to diagnostics andchronic disease management. Increased collaborationbetween general practices in federated arrangementswould enable patients to access services closer to home.Co-ordination of care: action to link primary careteams more closely with specialists and with health andsocial care professionals to ensure patients and serviceusers receive care that is effectively co-ordinated. Thisis likely to be facilitated by the development of theelectronic care record and of IT systems that connectdifferent parts of the care system. Responsibility forthe co-ordination of patient care, regardless of wherethat is provided in the system, needs to be taken by theorganisation with whom they register.High-quality, safe specialist care: action to rationaliseacute care in fewer hospitals and to concentratespecialist services in centres of excellence able to deliverthe best outcomes, supported by networks that linktogether expertise in different settings. Some servicescurrently provided in acute hospitals will be increasinglyunbundled, with more diagnostic and outpatient servicesprovided in primary care, and many inpatient servicesdelivered in step-down facilities such as communityhospitals and nursing homes. In some cases, patientscurrently cared for in hospitals will be looked after intheir own homes with support from nurses and others.Consistent standards of care: action to reduceunwarranted variations in health care throughsystematic and routine collection and publication of data,the development of incentives to encourage action totackle unwarranted variation and an emphasis on shareddecision-making to establish the right level of variationbased on patients’ own assessments of their needs andattitudes to risk.The approach we advocate requires a shift in the waycare is delivered, with much less reliance on clinicianspractising autonomously in a ‘cottage industry’ modeland greater emphasis on standardising care around bestpractice guidelines supported by routine monitoringof performance and transparent reporting (Swensenet al 2010). This approach means moving beyondfragmentation between providers and services toeffective co-ordination around the needs of patients.Choice and competition have a part to play in the healthcare system of the future, but applying market principlesin health care needs to be done in a way that improvesthe value and outcomes of care.Towards integrated careAt the heart of the new model of care is the need tobetter integrate services between providers aroundthe individual needs of patients and service users. AsThe King’s Fund’s review of the evidence for integratedcare concluded, significant benefits can arise from theintegration of services (Curry and Ham 2010), particularlywhen these are targeted at those client groups for whomcare is currently poorly co-ordinated.© The King’s Fund 2011 5
Where next for the NHS reforms in England?The integration of care can take on many different forms.A distinction can be drawn between real integration, inwhich organisations merge their services, and virtual orcontractual integration, in which providers work togetherthrough networks and alliances. Studies have shown thatorganisational mergers do not deliver benefits withoutclinical and service integration. Virtual integration basedon networks and alliances may therefore offer greaterpotential to deliver a new model of care if it facilitatesclinical teams to come together to co-ordinate servicesaround the needs of patients.In some cases integration may entail bringing togetherresponsibility for commissioning and provision. This formof integration is important because it allows cliniciansto use budgets either to provide services more directlyor to commission these services from others through‘make or buy’ decisions. Many integrated medical groupsin the United States work in this way, and researchhas highlighted the beneficial impact on both serviceutilisation (for example, reduced use of hospital beds)and quality of care. One of the challenges for theproposed reforms is how to facilitate the emergenceof integrated medical groups able to take ‘make or buy’decisions and we discuss this in more detail below.Examples of integration can be found at the micro levelin the use of multidisciplinary teams to meet the needsof individual service users and carers. They can also befound at the meso level when providers collaborate ormerge to meet the needs of particular care groups likeolder people or populations with the same diseases orconditions. The most ambitious forms of integrationare those that provide the full range of care to thepopulations they serve.Kaiser Permanente in the United States is a well-knownexample, and it exhibits many of the elements of the newmodel of care described above. It is a virtually integratedsystem in which hospitals, the medical group and thehealth plan (or ‘commissioner’ to use NHS terminology)remain distinct organisations and collaborate closely.Kaiser Permanente delivers good outcomes for itsmembers, with studies showing that it makes much lessuse of hospital beds than the NHS. It achieves this resultbecause of its focus on prevention, supported self-care,and pro-active care co-ordination (Feachem et al 2002;Ham et al 2003).Integrated care in the NHSIn the NHS, integrated care is particularly important in meetingthe needs of people with chronic diseases like diabetes andchronic obstructive pulmonary disease; frail older people whomay have several chronic diseases and be in contact with arange of health and social care professionals; and people usingspecialist services – for example, those involved in cardiac andcancer care – where networks linking hospitals that providethese services have contributed to improved outcomes. Thefollowing box illustrates examples of each .Diabetes care in BoltonThe Bolton Diabetes Centre was set up in 1995 and is thebase for a team of community-based specialists. The teamreaches into the local hospital for inpatient care, and out togeneral practices to provide support and undertake sharedconsultations. The vision is of care that is patient centredand delivered in the appropriate place at the appropriatetime by the appropriately trained professional. Boltonaspires to develop a fully integrated diabetes servicewithout gaps or duplication and with smooth and quickreferral from primary care to specialist advice. Patientsand staff have reported high levels of satisfaction withthe service, and in 2005/6 Bolton reported the lowestnumber of hospital bed days per person with diabetes inthe Greater Manchester area (Irani et al 2007).Care for older people in TorbayHealth and social care for older people in Torbay isdelivered through integrated teams, first establishedon a pilot basis in 2004 and since extended throughoutthe area. Each team serves a locality of between 25,000and 40,000 people and is aligned with the generalpractices in the locality. Budgets are pooled and areused flexibly by integrated teams who are involved inmicro commissioning to meet patients’ needs. A majorpriority has been to increase spending on intermediatecare services that enable patients to be supported athome and help avoid inappropriate hospital admissions.The work of integrated teams has been taken forwardthrough the work of the Torbay Care Trust, created in2005. Results include a reduction in the daily averagenumber of occupied beds from 750 in 1998/9 to 502 in2009/10, emergency bed day use in the population aged65 and over that is the lowest in the region, and negligibledelayed transfers of care (Thistlethwaite 2011).6 © The King’s Fund 2011
The King’s Fund ResponseStroke care in Manchester and LondonStroke care in London and Manchester has beenimproved by planning the provision of these servicesacross networks linking hospitals. Manchester usesan integrated hub-and-spoke model that provides onecomprehensive, two primary and six district strokecentres. Results include increasing the number of eligiblepatients receiving thrombolysis within the metropolitanarea from 10 to 69 between 2006 and 2009 (NAO 2010).In London implementation of a pan-London stroke carepathway and the development of eight hyper-acutestroke units has improved access and reduced length ofstay in hospitals: 85 per cent of high-risk patients whohave had a transient ischaemic attack are treated within24 hours, compared with a national average of 56 percent, and 84 per cent of patients spend at least 90 percent of their time in a dedicated stroke unit, comparedto a national average of 68 per cent. Five of the topsix performing hospitals in the National Sentinel Auditfor Stroke are now London hyper-acute stroke units(Intercollegiate Stroke Working Party 2011).The ingredients of effectiveintegrated careAs the above examples illustrate, many differentapproaches can be taken to achieving integrated care.While mergers to create organisations that take fullresponsibility for commissioning and providing servicesfor the populations they serve have been pursued inScotland and Wales, this option is not on the agendain England, and in any case the benefits of this kind oforganisational integration remain a matter of dispute. Amore promising route for the NHS in England is thereforeto encourage virtual or contractual integration betweenproviders, learning from experience in other sectorswhere strategic partnering and integration throughsupply chains and networks are widely used. In our view,the main priority should be to support clinicians to worktogether to deliver co-ordinated care by engaging themeffectively in commissioning.A number of ingredients can be identified thattogether contribute to the outcomes that integratedsystems achieve almost regardless of the particularorganisational form adopted.The core ingredients of integrated careDefined populations that enable health care teamsto develop a relationship over time with a ‘registered’population or local community, and so to targetindividuals who would most benefit from a more coordinatedapproach to the management of their careAligned financial incentives that support providers towork collaboratively by avoiding any perverse effects ofactivity-based payments; promote joint responsibilityfor the prudent management of financial resources; andencourage the management of ill-health in primary caresettings in order to prevent admissions to hospitals andnursing homesShared accountability for performance throughthe use of data to improve quality and account tostakeholders through public reportingInformation technology that supports the deliveryof integrated care, especially via the electronic medicalrecord and the use of clinical decision support systems,and through the ability to identify and target ‘at risk’patientsThe use of guidelines to promote best practice, supportcare co-ordination across care pathways, and reduceunwarranted variations or gaps in careA physician–management partnership that linksthe clinical skills of health care professionals with theorganisational skills of executives, sometimes bringingtogether the skills of purchasers and providers ‘underone roof’Effective leadership at all levels with a focus oncontinuous quality improvementA collaborative culture that emphasises team workingand the delivery of highly co-ordinated and patientcentredcareMulti-specialty groups of health and social careprofessionals in which, for example, generalists workalongside specialists to deliver integrated carePatient engagement in taking decisions about theirown care and support in enabling them to self-care(Source: adapted from Curry and Ham 2010)© The King’s Fund 2011 7
Where next for the NHS reforms in England?There is evidence to suggest that approachesto integrated care work best when some of theresponsibilities for commissioning services are givento those responsible for delivery (Christensen et al2008). Giving providers freedom to take ‘make or buy’decisions means that the redesign of care and servicesis clinically led. Importantly, it promotes collectiveaccountability among providers for the quality, costs andoutcomes of care as incentives to integrate services arealigned and this approach becomes more culturally andsystematically embedded.We would also emphasise that integrated care does notappear to evolve as a natural response to emerging careneeds in any system of care whether this be planned ormarket-driven. Achieving the benefits of integrated carerequires strong system leadership, for example, frompolicy-makers and other system architects, to providea platform to support it. Systemic barriers to integratedcare in England must be addressed if patient-centredintegrated care is to become a reality. It is to this issuethat we now turn.The barriers to integrated care and theimplications of the proposed reformsThe NHS today contains many barriers to integratedcare. Examples of how they have been overcome, suchas those described in the previous section, are fewand far between. As a result, the NHS ranks poorlyin international comparisons examining patientcentredcare where surveys demonstrate comparativeweaknesses in its ability to support care co-ordination(Schoen et al 2008). What then are the main barriers todeveloping a new model of care?Organisational complexity and restructuringThe NHS in England is made up of a large number oforganisations, each with responsibility for differentaspects of commissioning and service provision. Theseorganisations include strategic health authorities,primary care trusts and NHS trusts (most of which arenow foundation trusts) responsible for acute services,specialist services, mental health services, communityservices, and ambulance services. Complexity has beenincreased by the move to enable NHS services to be runas social enterprises and by the encouragement givento independent sector and voluntary sector providersto deliver care to patients. Alongside the NHS, localauthorities are responsible for social care, on which manyof the most vulnerable users depend.As well as organisational complexity, the NHS has beenaffected by frequent restructuring. This has had theeffect of taking managers’ time and attention awayfrom the core business of improving patient care andaddressing weaknesses in performance. In some cases,restructuring has resulted in increased fragmentation.Examples include the separation of responsibility forcommissioning health care and providing services,introduced in 1991, and the requirement that primarycare trusts divest themselves of responsibility fordirectly providing services under the transformingcommunity services policy.The latter policy has resulted in increased integrationin areas where community services have been takenon by NHS trusts providing acute services and mentalhealth services. Paradoxically, in other areas, such asTorbay, progress in integrating care has been adverselyaffected by this policy, in part because of the instabilitycaused by restructuring, and in part because of therequirement that there should be a clear separationbetween commissioning and service provision in thecare trust. Similar challenges have been encountered inareas like the Cumbria, the Isle of Wight and Knowsleywhere the requirement that primary care trusts shoulddivest themselves of responsibility for directly providingservices has put barriers in the way of closer integration.The impact of the proposed reformsThe proposed reforms to the NHS could increaseorganisational complexity as encouragement is givento any willing provider to deliver care to patients andrenewed efforts are made to encourage NHS staff toestablish social enterprises. Also, the proposed abolitionof strategic health authorities and primary care trusts mayhelp in reducing the number and type of organisations inthe NHS, but it will also have the effect of removing thetwo bodies that have the potential to support partnershipworking and provide local system leadership. On the otherhand, the proposed health and wellbeing boards will havea duty to promote integrated care, although their powersto make this happen are weak under current plans.8 © The King’s Fund 2011
The King’s Fund ResponseProfessional divisionsOne of the characteristics of British medicine is thehistorical separation between general practitioners (GPs)and specialists. This separation is in part organisational– GPs work mainly in the community as self-employedcontractors and specialists mainly in hospitals as salariedemployees – and in part cultural. Although the statusand remuneration of GPs has steadily increased duringthe lifetime of the NHS, and the quality of primary carein the UK is widely admired, there remains a perceptionin some quarters that a career in general practice isnot as prestigious as a career in hospital medicine. As aconsequence, it can be difficult for GPs to work on equalterms with specialists.An unintended consequence of the increasing trendtowards specialisation and professionalisation in theroles and tasks performed by health and social careprofessionals has been fragmentation at a clinical andservice level (Ahgren 2010). There is a need to promotethe role of generalist physicians in the workforce –for example, in care of older people – to counter theunintended consequences of sub-specialisation.This becomes more urgent with the increasing numbersof older people in the population, some of whom havemultiple and complex chronic conditions that requirethe expertise of GPs and a range of specialists and theirteam. Integrated delivery systems in other countries,such as Kaiser Permanente, embrace a model of multispecialtymedical practice in which GPs work alongsidespecialists, often in the same facilities.Multi-specialty medical practice (also referred to asintegrated medical groups) is a form of integration thathas been shown to deliver better results compared witharrangements in which doctors work in isolated practices(Curry and Ham 2010). It is relevant to the NHS becauseof the need for specialists and GPs to work togethermuch more closely to help patients remain independentfor as long as possible and to reduce avoidable hospitaladmissions. While there are some examples of specialistswho work in the community alongside GPs (as in theBolton diabetes service described above), these remainthe exception rather than the rule.One reason for this is that the organisation of generalpractice in relatively small units makes it difficult forspecialists to work outside hospitals in a way that is bothefficient and supports the delivery of high-quality care.Also, the lack of appropriate buildings and equipment fordiagnosis and treatment in primary care means that thehospital becomes the default setting for the delivery ofmost forms of specialist care. Proposals such as thoseput forward in London for the development of polyclinicswere intended to address these challenges, but progressin implementation has been slow.The impact of the proposed reformsThe proposed reforms to the NHS could reinforcedivisions between GPs and specialists if current plans forGP commissioning proceed without modification. Theyemphasise that GPs will take the lead on commissioningand are silent on the role of specialists and the part theywill be expected to play in future.Financial incentivesThe main way of paying hospitals for the work theydo, Payment by Results, was introduced in 2003/4 tosupport the aim of cutting waiting lists and waitingtimes for planned hospital care, at a time when the NHSbudget was increasing rapidly. The incentives containedwithin Payment by Results have contributed to theimprovements in access to care in the past decade but alsomake it difficult to develop integrated care. This is becausehospitals may experience a reduction in demand for theirservices and therefore income if greater emphasis is givento prevention and to care closer to home.By setting up hospitals as profit centres seeking togenerate surpluses for investment under the regulatoryregime established by Monitor, recent health reformshave put significant barriers in the way of necessarychanges in clinical practice. Anecdotal evidence ofspecialists being instructed not to undertake workthat reduces hospital activity and income, or that is notremunerated under the Payment by Results tariff, suchas telephone consultations with GPs, offer powerfulevidence of this. In effect, financial incentives serve tolock in an outmoded model of care and provide no rewardfor the integrated models we have argued should be atthe centre of the health care system of the future.In theory, world class commissioning and practice-basedcommissioning were intended to act as a countervailingforce to Payment by Results and the establishment of© The King’s Fund 2011 9
Where next for the NHS reforms in England?foundation trusts, with the aim of moving to the newmodel of care we have outlined. In practice, neitherprimary care trusts nor practice-based commissionersin most parts of the NHS found it easy to challenge thepower of acute hospitals, with the result that activitylevels in hospitals have continued to increase andprogress in developing care in alternative settings hasbeen slow and uneven. The reasons for this can be foundin the inherent difficulties involved in commissioninghealth care services, not just in the NHS but in otherhealth care systems (Ham 2008), and the relatively weakincentives available to commissioners.The impact of the proposed reformsThe financial pressures facing the NHS require an urgentreview of current incentives and how they should bemodified, not least because commissioners will not beable to fund ever-increasing levels of hospital activity.Payment by Results makes sense for planned care as away of supporting choice and competition in the market,and it may also have a role in other areas of care wherethere is a case for encouraging new providers to deliverservices to NHS patients. In the case of unplanned care,where the aim is to reduce avoidable admissions andprovide care outside hospitals wherever appropriate,alternative payment systems are needed. Thesealternatives should create incentives for high-qualityco-ordinated care for people with chronic diseases. Theexperience of integrated systems that have incentivesaligned with their objectives should be used to developthese alternatives.Competition and regulationSuccessive governments over the past 20 years haveused competition as a means of improving performancein the NHS. Studies have pointed to mixed results fromthe use of competition in the NHS, and there are stronglyheld views on how appropriate it is to apply marketprinciples in a publicly funded health care system. One ofthe concerns of critics of competition is that it will resultin increased fragmentation and inefficient duplicationof services that may have adverse effects on the qualityand outcomes of care.Market principles have been applied most extensivelyin the United States. The analysis undertaken byPorter and Teisberg highlights the challenges thatarise when the ‘wrong kind of competition’ is usedin health care (Porter and Teisberg 2006). Thesechallenges include cost-shifting, attempts to capturepatients and restrict choice, efforts to reduce costsby limiting services, and competition to increasebargaining power. The alternative proposed by Porterand Teisberg is value-based competition centred onintegrated practice units defined around medicalconditions rather than medical specialties.The rationale behind this approach – echoing thearguments of this paper – is the need to move beyondfragmented care to an integrated approach in whichpatients receive high-quality co-ordinated services.The implication is that competition itself need not bea barrier to collaboration provided that the risks of thewrong kind of competition are addressed. This meansensuring appropriate regulation of the market to supportthe emergence of value-based competition. Porterand Teisberg’s argument is related to the analysis ofChristensen and colleagues (Christensen et al 2009),who see the solution to the problems of health carein the United States as lying in competition betweenintegrated systems.This analysis indicates that there is no inherentcontradiction between competition and integrationprovided that the complexities of health care areunderstood. The well-known risks of market failureneed to be addressed in the design of the NHS reformsto support the implementation of the new model ofintegrated care we have described.The impact of the proposed reformsThe proposed reforms to the NHS, and in particularthe Health and Social Care Bill, include provisionsfor an economic regulator (Monitor) with a duty topromote competition where appropriate. Monitor willbe expected to work with the Office of Fair Trading, theCompetition Commission and the NHS Commissioning<strong>Board</strong> in discharging its responsibilities. If theseproposals are taken forward, it will be essential thatMonitor recognises the challenges of applying marketprinciples in a way that avoids the problems identifiedby Porter and Teisberg. As we discuss in the finalsection of this paper, this means supporting bothcompetition in the market and competition for themarket. It also means ensuring that Monitor’s duty10 © The King’s Fund 2011
The King’s Fund Responseto promote competition where appropriate does notcreate further barriers to collaboration and integratedcare where this will bring benefits.Functional separation between commissionerand providerThe concept of ‘commissioning’ as developed in Englandencompasses a broad range of activities, includinganalysing the health needs of the population, identifyingcommissioning priorities, planning and designingservices, procuring and then monitoring and evaluatingthe services provided. Despite attempts to strengthenthe commissioning function in England through theworld class commissioning programme, commissioninghas yet to deliver the ambitions set out for it (HCSC2010). Commissioners have struggled in the face oflarge and powerful providers and a major asymmetry ofinformation between commissioner and provider.Even before the general election, there was discussionabout whether PCTs were operating at sufficient scale toundertake commissioning effectively and challenge largeproviders. PCTs were also criticised for lacking clinicalinvolvement despite the existence of a ProfessionalExecutive Committee as part of the governancearrangements. In many areas, they struggled to findways to influence the quality of primary care, encouragethe shift to develop more services in the community, andmanage the volume of care.Practice-based commissioning – that is, the delegation ofbudgets to groups of practices – was seen as the solution.However, these were soft or nominal budgets, small in sizeand scope, and the process for obtaining these delegatedbudgets was often cumbersome and lacking transparency.One of the key lessons from the experience of practicebasedcommissioning and its predecessors was that moreprogress in service redesign and delivery is made when ‘real’budgets are devolved to commissioner–provider groups sothey have autonomy in decision-making (Curry et al 2008).Impact of the proposed reformsWe have noted already the opportunities and threats tointegrated care posed by the transforming communityservices policy. Similar issues arise in relation to thecoalition government’s proposed reforms, especiallythose relating to GP commissioning consortia.While the proposed GP consortia would introducevaluable clinical insight to the commissioning process,the proposal that consortia should be statutorybodies that will only commission care continues theprevious government’s emphasis on the separationof commissioner and provider responsibilities. Publicprocurement rules are likely to make it difficult for GPconsortia to implement the new model of care describedin this paper because GPs will have to decide whetherto be involved in commissioning or to focus mainly ondeveloping new approaches to service provision toovercome concerns about conflicts of interest.Our experience is that many GPs involved in thepathfinder programme see themselves first andforemost as providers and they are enthusiastic aboutcommissioning because of the opportunities it offersto develop new models of provision in which they andother practices will play a part. If regulatory barriersare placed in the way of GPs and other clinicians usingcommissioning as a lever to innovate in service provision,then the current interest in commissioning may rapidlydissipate as has been the case in the past. This willseverely attenuate the potential benefits of engagingclinicians more directly in commissioning, and underpinsour argument for a more radical option set out at the endof the paper.Information technologyThe final barrier to integrated care is informationtechnology. Progress has been made in hospitals and,especially, in primary care in the use of informationtechnology; however, delays in the Connecting forHealth programme mean that the vision of a singlesystem that links hospitals and primary care remainsunfulfilled. The consequence is that patients may beassessed repeatedly, communication between cliniciansis inhibited, co-ordination of care may suffer, and qualityfailures may occur.High-performing integrated systems in other countrieshave made a major commitment to informationtechnology and have been early and effectiveimplementers of the electronic medical record and clinicaldecision support systems. The electronic medical recordis itself an important means of supporting integration byenabling clinicians to access information about patients© The King’s Fund 2011 11
Where next for the NHS reforms in England?wherever they are treated. Likewise, clinical decisionsupport systems facilitate the adoption of best practiceguidelines and the delivery of high-quality, safe healthcare. Patients are able to access their own recordsremotely, communicate with doctors and other cliniciansthrough secure email channels, make appointmentsonline and order repeat prescriptions.The data captured through information technology canalso be used to support comparisons of performanceamong clinicians and hospitals and as a tool forcontinuous quality improvement. This is fundamentallyimportant in moving away from the cottage industrymodel of health care, reducing unwarranted variations incare and promoting greater consistency with recognisedstandards of care. Measurement and benchmarking canalso be used to support informed patient choice andtransparent reporting of performance.What needs to be done to supportintegrated care?Based on this analysis, what actions do we believeare now needed in relation to the legislation beforeparliament and to current health policies to makeintegrated care a reality? In this final section of ourpaper, we set out a range of proposals designed toinform the work going on during the listening exerciseand the decisions the government will take onmodifications to the Health and Social Care Bill whenthe listening exercise is completed. The discussion isorganised around the ways of overcoming the barriersdiscussed in the previous section. We offer suggestionsfor revisions to the current Bill but also lay out anevolutionary path to a more radical model, based on adifferent approach to commissioning that we believewill help move towards the vision of integrated care anda sustainable health system.As we have shown, the NHS does need to change to buildon recent improvements in performance, and proposalsto strengthen choice and competition have a part to playin this process. The imperative now must be to ensurethat future reforms are well designed, appropriate tothe challenges that lie ahead, proportionate to thesechallenges, and effectively implemented. In our view, thetop priority for the current legislation is to adopt a nuancedapproach to economic regulation that avoids promotingthe wrong kind of competition and does not createfurther barriers to collaboration and the development ofintegrated care where this will bring benefits. Such anapproach needs to rebalance the system towards a morecollaborative model while retaining a strong focus onclinical leadership and outcomes.We would also reiterate the need to phase theimplementation of the reforms in a way that supportsdelivery of the Nicholson challenge. As we have arguedelsewhere, integrated care that is focused on the needsof older people and people with chronic conditions hasa major contribution to make in enabling the NHS to riseto this challenge (Appleby et al 2010b). Migration fromthe current system should be calibrated on the basis ofan assessment of the readiness of clinicians to take onthe responsibilities being offered them and in a way thatensures the retention of experienced NHS leaders duringand beyond the transition. This evolutionary path appliesequally to current proposals and our more radical model.Organisational complexity and restructuring:the need for system leadership and coherenceAt a time when organisational complexity is likely toincrease as a consequence of the government’s anywilling provider policy, the key question is how toachieve co-ordination around the needs of patientsamong an increasingly diverse range of providers? Theanswer to this question is unlikely to be through furtherrestructuring to reduce the number and variety of NHSorganisations, not least because of the negative effectsof constant changes to the organisation of the NHS.An alternative is to recognise the need for effectivesystem leadership in support of clinical commissioning,in anticipation of the eventual demise of strategic healthauthorities and primary care trusts.By system leadership we mean the ability to take anoverview of the needs of the population in an area and ofthe role of different organisations in responding to theseneeds. In our response to the White Paper, we arguedthat commissioning consortia were unlikely to be ableto undertake this task and to address complex issuessuch as the organisation of specialised care and thereconfiguration of acute hospitals (Dixon and Ham 2010).Recent work by The King’s Fund on the reorganisation12 © The King’s Fund 2011
The King’s Fund Responseof hospital services in south-east London has reinforcedus in this view (Palmer 2011). In the context of thispaper, system leadership encompasses responsibility forpromoting integrated care where this will bring benefits.The government’s plans envisage that health and wellbeingboards will have a duty to promote integrated care, andwe welcome this. However, their powers are weak undercurrent plans, and the future of health care services willbe decided by commissioning consortia and the NHSCommissioning <strong>Board</strong>. It is likely that consortia will chooseto work with each other to deal with issues that demandexpertise unlikely to be available in every consortium,helping to fill the gap that will be left when strategic healthauthorities and primary care trusts are abolished.Collaboration between consortia is, however, unlikelyto be sufficient to take forward integrated care forspecialist services such as cardiac care and cancer careor to ensure that existing networks are sustained wherethey are functioning well. As the examples of strokeservices in Manchester and London show (see page7), system leadership is needed to agree how somespecialist services should be concentrated in fewercentres able to deliver better outcomes where progresshas not already been made on these issues. For thesereasons, we propose that the NHS Commissioning<strong>Board</strong> should be given an explicit role to work withcommissioning consortia to provide system leadershipand promote integrated care for specialist services.A case can be made for the establishment of clinicalcabinets at a regional level to provide support toconsortia and to ensure that this system leadershiprole has at its heart the best available clinical advice.These clinical cabinets would have a major part to playin promoting integrated care for specialist servicesand in helping to overcome the historical divisions inBritish medicine that create barriers to integration.And by ensuring that clinicians are at the heart ofthis regional role of the NHS Commissioning <strong>Board</strong>, itshould be possible to avoid the reinvention of strategichealth authorities.Under current arrangements, PCTs and local authoritieshave developed numerous ways of working inpartnership, resulting in better co-ordination of services.The loss of co-terminosity achieved between manyauthorities and PCTs may create practical barriers tojoint working, particularly to support public healthinitiatives. It will also make accountability for outcomesmore problematic as it will be significantly harder to linkdemographic and epidemiological data to commissioners’registered populations. There are strong arguments forseeking co-terminosity between commissioners anddefined geographical areas.Recommendations• System leadership is needed at the regional leveland this should be provided by multi-professionalclinically led groups or clinical cabinets.• As far as possible GP commissioning boundariesshould be aligned to geographical and local authorityboundaries in order to address population healthissues including tackling health inequalities,promoting public health and serving the needs ofhard-to-reach groups.Professional divisions: the need forclinical integrationDemographic changes and the shifting burden ofdisease mean that the sharp division between primarycare and secondary care is increasingly unhelpful.Patients who are the most intensive users of careneed to access expertise from generalists as well asspecialists and from different members of the healthand social care team.The implication is that at all levels of the NHS andsocial care there should be a commitment to clinicallyintegrated care. The use of integrated health and socialcare teams aligned with GP practices to meet the needsof older people in Torbay illustrates what this meansat a local level. The example of the integrated diabetesservice in Bolton in which community-based specialistswork closely with GPs and nurses demonstrates howbarriers between professionals can be broken downacross a health community.Building on these examples, commissioning consortiashould include involvement from specialists and otherclinicians. This will help to facilitate the redesign of carepathways and to overcome the fragmentation and lackof co-ordination that prevents the NHS becoming trulyworld class in the delivery of care.© The King’s Fund 2011 13
Where next for the NHS reforms in England?Recommendations• Multi-professional collaboration needs to besupported at all levels within the NHS.• GP consortia should have a ‘duty’ to engage andcollaborate with the other clinicians responsible forthe care of their patients.• Opportunities to develop multi-professional teams tosupport the needs of high-risk patients such as frailolder people should be a core element of services atlocal level, as is already the case for patients withchronic mental health problems.Financial incentives: the need to alignincentives to support integrated careThe financial pressures on the NHS and the need to reorientthe provision of care towards prevention and care outsidehospitals make it imperative that financial incentives aremodified to support integrated care. Payment by Resultshas a continuing role in relation to planned care, includingdiagnostic services, outpatient appointments and electivesurgery, where the emphasis needs to be on competition inthe market. In the case of unplanned care, the provision ofspecialist services, and particularly the needs of older peopleand people with complex needs, the priority should be todevelop ways of paying for care that reward good outcomesand avoid perverse incentives to increase hospital activity.Experience in the United States of new forms ofpayment that go beyond fee-for-service and case-basedreimbursement contains pointers on possible options(Shih et al 2008). These new forms of payment includeepisode-based payments that bundle together paymentsfor a range of services relating to a particular episode ofcare. An example from Geisinger Health System is theuse of a global fee that covers the entire cost of cardiaccare from pre-admission through surgery to follow-upfor 90 days after the operation.There are various ways of adapting the currentmechanisms to better support integrated care;for example (Ham et al 2011):• combining payments to cover an episode of care orcare pathway• exploring the idea of the ‘year of care’ that has beentested in three national pilots for diabetes• contracting with local clinical networks (of primary,secondary, or primary and secondary care clinicians)or foundation trusts to deliver integrated care for aspecific population• using personal health budgets to enable patientswith support from carers and families themselves tocommission care packages• using CQUIN payments across pathways of care toincentivise best practice models and collaborativeworking• increasing use of pooled budgets.A further approach is for commissioners to place a contractwith a lead or prime contractor to provide services forpatients with a specific condition or disease like diabetes.Such an approach is being piloted in the East of Englandthrough work on commissioning integrated pathway hubswhere the chosen provider will work under an agreedbudget. While this work offers the potential to help movebeyond fragmented and episodic care, there is a risk ofcreating new silos centred on conditions and diseases inplace of existing silos.An alternative would be for commissioners to contractfor the provision of care to populations such as frailolder people with complex needs who account for a highproportion of utilisation and expenditure. This woulddraw on the experience of areas like Torbay and mightencompass social care as well as health care. An addedattraction of this approach is that commissioners could usetheir leverage to promote integration of health and socialcare rather than this being achieved through structuralchange. Integrated care focused on populations would mostlikely be funded through capitated budgets that reflect theneeds of these populations.Whatever approach is adopted, it will be important to ensurethat incentives are put in place to reward improvements inthe quality of care and to avoid patients being under-served.Again, experience from the United States is relevant, as in theAlternative Quality Contract being tested by Blue Cross BlueShield Massachusetts (Chernew et al 2011). Under this contract,which has some similarities with the quality and outcomesframework in general practice, medical groups are able to earnextra income based on their performance against a range ofmeasures of quality relating to primary and secondary care.14 © The King’s Fund 2011
The King’s Fund ResponseRecommendations• Alternatives to the tariff are needed for nonelective,long-term and complex care.• These alternatives may include bundled payments,pooled or delegated budgets and capitated budgets.• Any payment mechanism adopted needs to ensurethat financial rewards are linked to the quality andoutcomes of care.Competition and regulation: the need fora nuanced approach that recognises thecomplexity of health careCompetition and collaboration are means not ends.Ministers must ensure that Monitor adopts a nuancedand proportionate approach that encourages bothcollaboration and competition where appropriate. Allorganisations involved in commissioning and providingcare should be required to collaborate where this willbring benefits to ensure that the integration is ‘hardwired’ into the NHS of the future. The primary and soleduty of Monitor should be the protection and promotionof the interests of patients and the public.In promoting competition where appropriate, Monitormust recognise the complexity of health care and the riskof encouraging the wrong kind of competition. Differentservices lend themselves to different approaches withcompetition in the market likely to work best for plannedand elective care and competition for the market beingappropriate for unplanned care and specialist services.Competition for the market can encourage co-operationand information-sharing among providers along a patientpathway as well as for patients with complex needs whodo not fit easily into disease-based pathways.It will be important to determine the most appropriateunit of competition. In some cases this might be thehospital or provider of community services and in othersit could be a provider or co-ordinator of integratedcare. In many cases, services will need to be plannedand delivered across networks, with patients and theirclinicians able to select a provider who can deliverhigh-quality packages of care over time, if necessary incollaboration with other providers.The example of stroke services illustrates this point.Evidence from Manchester and London summarisedearlier demonstrates the benefits that arise whenhospitals work in networks and specialist stroke servicesare concentrated in fewer centres to deliver betteroutcomes. Monitor should support developments of thiskind and not see them as anti-competitive.Monitor and the NHS Commissioning <strong>Board</strong> should alsoensure that there is neither a proliferation of specialistservices nor inefficient duplication as providers competefor market share. The NHS Commissioning <strong>Board</strong> canoffer guidance on how to commission integrated servicesin different areas of care and provide advice and supporton contractual routes, currencies and incentive schemes,and outcome indicators for assessment of progress.Equally, Monitor should guard against the wrong kind ofintegration and the risk that collaboration fails to deliverthe improvements in performance that are needed.Monitor needs to draw on experience in other sectorsas it takes on its new responsibilities. While there areno direct parallels to the health sector, the experienceof regulation of the railways has some relevance,especially in the award of long-term franchises to railoperating companies and in the emphasis placed onnetworks of provision (Walker 2011). Monitor and theNHS Commissioning <strong>Board</strong> can also support yardstickcompetition by the transparent reporting of performancein the market.Recommendations• Monitor and the supporting regulations for NHSprocurement need to promote both competition andcollaboration.• A duty to collaborate should be a requirement for allorganisations providing or commissioning NHS care.• The NHS Commissioning <strong>Board</strong> should provideguidance to support the commissioning of integratedcare and should hold commissioning bodies toaccount against a transparent outcomes framework.Information management and technologyLike financial incentives, information can be a majorenabler or barrier to integrated care. Policy needs tosupport the effective sharing of meaningful informationfor patients, providers and commissioners. The use ofpatient-held records should be actively encouraged.© The King’s Fund 2011 15
Where next for the NHS reforms in England?Recommendations• Anyone providing or commissioning NHS care shouldbe required as part of their licensing agreement orstatutory function to share relevant informationwith patients and professionals.• Monitor should include common protocols, dataprotection policies, data definitions and technologystandards to facilitate the sharing of information inits licence.Functional separation between commissionerand providerProposals for commissioning consortia will helpto ensure that commissioning decisions are ledby clinicians and this is likely to bring benefits. Asdiscussed earlier, consortia will need to collaborate toundertake some functions effectively and they willrequire excellent management support. There is a needto be clear about where in the system some of thestrategic functions of commissioning will take place asnot all of these are appropriately done at the level ofconsortia or consortia working together.The development of clinical cabinets at a regionallevel as part of the NHS Commissioning <strong>Board</strong> asproposed earlier will assist in ensuring that thesestrategic functions are carried out effectively. Thisincludes leading improvements in specialist servicessuch as stroke and trauma care where reconfigurationof services across large populations may be needed.The combination of commissioning consortia andclinical cabinets at a regional level will go some way toovercoming the separation between commissionersand providers and in the final section of this paper weoutline an evolutionary path that could go much further.Recommendations• The NHS Commissioning <strong>Board</strong> should establishclinical cabinets at regional level to take on someof the strategic commissioning functions fromconsortia.• The Bill must retain the flexibilities to allow consortiato cluster together and pool budgets as appropriateto undertake those aspects of commissioning betterdone at a more strategic level.Beyond the current reforms:the case for radical evolutionThe outstanding question is how far will the proposedreforms with the modifications we have outlined help tofacilitate the new model of integrated care focused onthe needs of patients required in the future? Our view isthat while there is potential for commissioning consortiathat involve clinicians from a range of backgrounds tosupport the emergence of new models of provisionincluding federated networks of general practices andintegrated care for people with chronic diseases andcomplex needs, the insistence on there being a continuingseparation between commissioning and provision couldinhibit development in this direction. This is becausecommissioning consortia as statutory bodies will not havethe flexibilities to take the decisions to either provideservices directly or commission them from others thatare needed to implement integrated care. If the outcomeof the listening exercise is to proceed with consortia, andto make modifications to their design along the lines wehave proposed, then what more could be done to supportevolution in the direction towards the new model of care?The answer can be found by returning to the experienceof integrated medical groups in the United Statesworking under capitated budgets as well as theachievements of long-established integrated systemslike Kaiser Permanente. Integrated medical groupsthat have been successful in delivering high-qualityintegrated care to patients combine responsibility forcommissioning and provision (Curry and Ham 2010). Oneof the characteristics of these organisations is that theyenable groups of GPs and specialists to take ‘make or buy’decisions by linking clinical and financial responsibilities.In this way, they create a platform on which doctorswho control budgets are able to provide care directlywhere this is appropriate and to commission from otherproviders where it is not.Integrated medical groups working under capitatedbudgets perform well on a number of indicators andthey have strong incentives both to meet the needs ofpatients (because they compete with other groups) andto use resources efficiently (because they benefit fromany savings made). Evidence from the 1990s onwardsshows that groups were successful in reducing the useof hospital beds, and more recent studies indicate that16 © The King’s Fund 2011
The King’s Fund Responselarger groups are able to provide higher-quality care topatients at lower cost than other types of practices.Integrated medical groups deliver these results becausethey are both providers and commissioners and areable to use the clinical expertise of doctors to deliverimprovements in care.The King’s Fund has recently studied experience inMassachusetts, where integrated medical groupsranging in size and scope have a long tradition of workingin this way. These groups work closely with health plans,which monitor the use of resources by medical groupsto ensure that the financial incentives under which theyoperate do not result in patients being denied access tonecessary care or receiving care of poor quality. Groupsare also rewarded by the plans based on their financialperformance and ability to improve the quality ofcare. Some of the health plans have adopted incentiveschemes that encourage medical groups to workclosely with hospitals to improve quality through closerintegration of care.As this example shows, commissioning involves twodistinct functions: clinical commissioning (or whatwe referred to earlier as micro commissioning) inwhich integrated medical groups use their controlof budgets to improve the provision of care; andstrategic commissioning in which a health plan takesresponsibility for funding for a large population andsupports clinical commissioners to undertake theirfunctions effectively. GPs and other clinicians in theNHS are in our view much more strongly motivatedto engage in clinical commissioning than strategiccommissioning not least because this will enablethem to make rapid improvements in how servicesare delivered. The requirement that commissioningconsortia should only commission care and not beinvolved in providing services is likely to deter some ofthe most innovative clinicians from playing a full part incommissioning because these clinicians are interestedmainly in improving service provision by developing newmodels of care.One way of addressing this challenge would be throughevolution from the reforms currently proposed to whatwe would call integrated care partnerships that involve awider range of health and social care professionals thatboth commission and provide services. Integrated carepartnerships might evolve from federations of generalpractices working in partnership with relevant healthand social care professionals to form organisationsthat take on a capitated risk-bearing budget to deliverservices for a defined population. These organisationswould be in a position to take ‘make or buy’ decisions,including developing networks of providers in which theco-ordination of care to meet the needs of patients isactively encouraged.We would envisage these organisations being not forprofit, for example, social enterprises or communityinterest companies. One of the advantages of thisapproach is that it would be easier to promote mergersand to forge alliances and partnerships than in the caseof commissioning consortia that are statutory bodies.This would help to avoid the destabilising effects oforganisational restructuring that we referred to earlier.The NHS Commissioning <strong>Board</strong> and its clinically ledregional offices could over time take on the higher levelstrategic commissioning functions from consortia andbe accountable for the use of resources. The <strong>Board</strong> andthe clinically led regional offices would retain a strongpopulation and geographical focus. They would leadsignificant service change, for example, around thereconfiguration of hospitals and set commissioningpriorities and goals. A critical role would be to overseehow integrated care partnerships use their resourcesand to provide the appropriate regulatory assurance inassociation with Monitor and professional regulators.They would also have strong relationships with health andwellbeing boards. In urban areas, where there might bemore than one integrated care partnership, patients wouldbe able to choose which partnership they register with.Patients who register with a practice that is part of anintegrated care partnership would be able to exercisechoice of provider within the partnership as well aschoosing to use services outside the partnership wherethese are not provided by the partnership itself. Thepoint to emphasise is that integrated care partnershipswould lever the benefits of collaboration among GPs,specialists and other care professionals and they wouldbe stimulated to provide responsive and high-qualityservices through the knowledge that patients in urbanareas would be able to join another partnership, say onan annual basis, if they were dissatisfied with their care.© The King’s Fund 2011 17
Where next for the NHS reforms in England?In this way, choice and competition would go hand inhand with collaboration.Moving in this direction beyond the current reformswould be a radical step. Many of our proposals have beenset out at a high level and more work is needed on thedetail. It is for these reasons that we have emphasisedthe need for an evolutionary approach that startsfrom the reforms currently proposed, modifies thesereforms in the way we have suggested, and creates abasis for further changes in the light of experience. Thiskind of approach would help to avoid further top-downrestructurings and would encourage experimentationfrom within the NHS led by innovative clinicians andmanagers. In our view, there would be merit in testingthe radical option in one or two regions to explore therisks and benefits of such an approach.Summary and conclusionThe proposals set out in this paper are offered as aconstructive contribution to the listening exercisewith the aim of building on recent progress inimproving the performance of the NHS in England andcreating the foundations on which the NHS can riseto future challenges. The proposals are intended tobe a co-ordinated package of ideas for improving thegovernment’s current plans that need to be acted ontogether. If the government’s response to this paper is totake forward some proposals and ignore others, then it isunlikely that the plans will be strong enough to addressthe concerns we have expressed in recent months. Itis also important to emphasise the need to evolve inthe direction we have proposed rather than to embarkon a rapid process of change, and in doing so to retainexperienced leaders whose involvement is essential todelivery of the Nicholson challenge.We would argue that the proposals are both appropriateand proportionate to the issues that need to beaddressed and that, if executed well, they shouldenable the NHS to meet the Nicholson challenge andabove all to improve outcomes for patients. Some of ourproposals, such as those on economic regulation, requiremodifications to the Bill, but most can and should bedealt with through established policy-making processes.The agenda set out here must be taken forward as amatter of urgency to remove barriers to the delivery ofintegrated care and to tackle the core challenge of anageing population in which chronic medical conditionsrepresent a threat to the sustainability of a universal,comprehensive, tax-funded health care system.18 © The King’s Fund 2011
The King’s Fund ResponseReferencesAhgren B (2010). ‘Dissolving the patient Bermuda Triangle’. InternationalJournal of Care Pathways, vol 14, no 4.Appleby J, Robertson R (2010a). ‘A healthy improvement? Satisfaction withthe NHS under Labour’. In: Park A, Phillips M, Clery E, Curtice J, eds. British SocialAttitudes Survey 2010-2011: Exploring Labour’s legacy—the 27th report.London: Sage.Appleby J, Ham C, Imison C, Jennings M (2010b). Improving NHS Productivity:More with the same not more of the same. London: The King’s Fund. Availableat: www.kingsfund.org.uk/publications/improving_nhs.html (accessed on 20May 2011)Appleby J, Raleigh V, Frosini F, Bevan,F, Gao H, Lyscom T (2011). Variations inHealth Care: The good, the bad and the inexplicable. London: The King’s Fund.Available at www.kingsfund.org.uk/publications/healthcare_variation.html.(accessed on 16 May 2011)Chernew M, Mechanic T Landon B, Safran DG (2011). ‘Private-payer innovationIn Massachusetts: the “Alternative Quality Contract”’. Health Affairs, vol 30, no1, pp51-61.Christensen CM, Grossman JH, Hwang J (2009). The Innovator’s Prescription: Adisruptive solution for health care. New York: McGraw Hill.Curry N, Ham C (2010). Clinical and Service Integration: The route to improvedoutcomes. London: The King’s Fund. Available at: www.kingsfund.org.uk/publications/clinical_and_service.html (accessed on 16 May 2011).Curry N, Goodwin N, Naylor C, Robertson R (2008). Practice-basedCommissioning: Reinvigorate, replace or abandon? London: The King’s Fund.Available at: www.kingsfund.org.uk/publications/pbc.html (accessed 19 May2011).Davis K, Schoen C, Stremikis K (2010). Mirror, Mirror on the Wall: How thePerformance of the U.S. Health Care System Compares Internationally, 2010Update [online]. The Commonwealth Fund website. Available at: www.commonwealthfund.org/Content/Publications/Fund-Reports/2010/Jun/Mirror-Mirror-Update.aspx?page=all (accessed on 30 September 2010).Dixon A, Ham C (2010) Liberating the NHS: The right prescription in a coldclimate? London: The King’s Fund. Available at www.kingsfund.org.uk/current_projects/the_nhs_white_paper/Feachem RGA, Sehri NK, White KL (2002). ‘Getting more for their dollar: acomparison of the NHS with California’s Kaiser Permanente’. British MedicalJournal, vol 324, pp 135–43.Ham C, Smith J, Eastmure E (2011). Commissioning Integrated Care in a LiberatedNHS (in publication).Ham C (2008). ‘World class commissioning: a health policy chimera?’ Journal ofHealth Services Research & Policy, vol 13, no 2, pp 116–21.Ham C, York N, Sutch S, Shaw R (2003). ‘<strong>Hospital</strong> bed utilisation in the NHS,Kaiser Permanente, and the US Medicare programme: analysis of routine data’.British Medical Journal, vol 327, p 1257.House of Commons Health Select Committee (2010). Commissioning. Fourthreport of session. HC 268-1 (2010–11)Intercollegiate Stroke Working Party (2011). National Sentinel Stroke ClinicalAudit 2010 Round 7 Public Report for England, Wales and Northern Ireland.London: <strong>Royal</strong> College of Physicians. Available from www.rcplondon.ac.uk/sites/default/files/national-sentinel-stroke-audit-2010-public-report-andappendices_0.pdf(accessed on 16 May 2011).Irani M, Dixon M, Drinkwater C, Reader P (2007). Specialist Doctors inCommunity Health Services: opportunities and challenges in the modern NHS.London: NHS Alliance, Available at www.networks.nhs.uk/nhs-networks/nhsalliance-specialists-network/documents/Specialist%20Doctors%20in%20Community%20Health%20Services.pdf (accessed on 16 May 2011).Lewis R, Rosen R, Goodwin N, Dixon J (2010). Where Next for Integrated CareOrganisations in the NHS? London: Nuffield Trust.National Audit Office (2010). Progress in Improving Stroke Care. London: TheStationery Office. Available at: www.nao.org.uk/publications/0910/stroke.aspx(accessed on 16 May 2011).National Audit Office (2011). Management of NHS <strong>Hospital</strong> Productivity:, Reportby the Comptroller and Auditor General, Session 2010-11. Department of HealthHC 491. London: The Stationery Office.Palmer K (2011). Reconfiguring <strong>Hospital</strong> Services: Lessons from south eastLondon. London: The King’s Fund. Available at: www.kingsfund.org.uk/publications/reconfiguring.html (accessed on 16 May 2011)Porter M, Teisberg E (2006). Redefining Health Care: Creating Value- BasedCompetition On Results. Harvard Business School Press.Schoen C, Osborn R, Squires D, Doty M, Pierson R, Applebaum S (2010). ‘Howhealth insurance design affects access to care and costs, by income, in elevencountries’. Health Affairs Web First. Available at www.commonwealthfund.org/Content/Publications/In-the-Literature/2010/Nov/How-Health-Insurance-Design-Access-Care-Costs.aspx (accessed on 16 May 2011).Schoen C, Osborn R How S, Doty M, Peugh J (2008). ‘In Chronic condition:experiences of patients with complex health care needs, in eight countries.Health Affairs Web Exclusive, November 13, 2008, w1-w16. Available at: http://content.healthaffairs.org/cgi/content/abstract/hlthaff.28.1.w1?ijkey=cOSQSi1j6fDlo&keytype=ref&siteid=healthaff (accessed on 16 May 2011)Shih A, Davis K, Shoenbaum SC, Gauthier A, Nuzum R, McCarthy D (2008).Organising the US Health Care Delivery System for High Performance. New York:The Commonwealth Fund.Swensen SJ, Meyer GS, Nelson EC, Hunt GC Jr, Pryor DB, Weissberg JI, KaplanGS, Yates GR, Chassin MR, James BC, Berwick DM (2010). ‘Cottage industry topostindustrial care—the revolution in health care delivery’. New England Journalof Medicine , vol 362, no 5:e12(1)-e12(4).The King’s Fund (2011a) .Health and Social Care Bill: Briefing. Available at www.kingsfund.org.uk/document.rm?id=8927 (accessed on 16 May 2011)The King’s Fund (2011b). Improving the Quality of Care in General Practice:Report of an independent inquiry commissioned by The King’s Fund. London:The King’s Fund. Available at: www.kingsfund.org.uk/publications/gp_inquiry_report.html (accessed on 16 May 2010).Thistlethwaite P (2011). Integrating health and social care in Torbay: Improvingcare for Mrs Smith. London: The King’s Fund. Available at: www.kingsfund.org.uk/publications/integrating_health_1.html (accessed on 16 May 2011).Thorlby R, Maybin J, eds (2010) . A high-performing NHS? A review of theevidence 1997-2010. London: The King’s Fund. Available at: www.kingsfund.org.uk/publications/a_highperforming_nh.html (accessed on 30 September2010).Walker A (2011). Speech to The King’s Fund on choice and competition. Audioonline at : www.kingsfund.org.uk/multimedia/anna_walker_on.htmlWolfe I, Cass H, Thompson MJ, Craft A, Peile E, Wiegersma PA, Janson S,Chambers TL, Mckee M (2011). ’ Improving child health services in the UK:insights from Europe and their implications for the NHS reforms’. British MedicalJournal , vol 342, d1277.© The King’s Fund 2011 19
THE ROYAL BOURNEMOUTH AND CHRISTCHURCH HOSPITALSNHS FOUNDATION TRUSTBOARD OF DIRECTORSMeeting Date and Part:Subject:Section:Executive Director with overallresponsibility:Author of Paper:Summary:Standards for Better Healthdomain:Action required by <strong>Board</strong> ofDirectors:10 th June 2011 Part IResults of the 2010/11 PbR AssuranceCoding Audit, by the Audit CommitteeInformationRichard RenautDirector of Service DevelopmentRichard RenautDirector of Service DevelopmentThis report is a summary of the full resultspaper following the audit on Clinical Codingfor 2010/11.Clinical and Cost EffectivenessTo note the report, actions and significantimprovements
<strong>Board</strong> of Directors – Part I10 th June 2011Results of the 2010/11 PbR Assurance Coding Audit,by the Audit Commission1. IntroductionEach year an audit of our PbR coding is undertaken by the Audit Commission, paid forby our host PCT. The full results are attached. This paper summarises the:• Key findings and messages• Updates against the proposed action plan.• Provides context as to impact of the action plan.The audit methodology is based upon a risk assessment of outlier codes and localknowledge from the PCT. This is then used to select areas for attention. 200 casenotes are then audited and used for these results.2. Key findings and messages2.1 Headline messages are that:• Coding accuracy has significantly improved.• There was a 0% financial impact of any inaccuracies.• Changes required in one aspect of cardiac coding will be a feature of the 2012/13contract.2.2 HRG error rateThis is 9.9% versus the national average of 9.1%. However, within this the two mainareas driving the number can easily be rectified (skin site of surgery coding andcoding of cardiac catheters). As a result the underlying accuracy is now much morerobust. This is also a massive improvement from the 24% error rate, which was drivenby our move to HRG4, which was hampered by being in a minority of trusts in our useof READ methodology.2.3 Procedure and diagnosis error rateThese have also massively improved, as the charts on Page 3 of the reportdemonstrate and the report which “commends” the efforts and improvements atnumerous points. These are both better than the known national average. Again theareas for improvement are relatively clearly identified and actionable, and thus havealready been applied.2.4 Key messagesThe really difficult aspects of coding improvement are:1) Widespread clinical engagement.2) Electronic notes including eIDF (Immediate Discharge Form).3) Tackling multiple consultant transfers of emergency inpatients on the system.Results of the 2010/11 PbR Assurance Clinical Coding Audit Page 1 of 3
<strong>Board</strong> of Directors – Part I10 th June 2011These have all been hugely challenging, but we have actually achieved the seachange in each to underpin our coding quality. Therefore the areas in the action planare relatively straight forward in comparison to previous year’s requirements. The onlysignificant changes revolve around IT, which are discussed below, under action plan.However, maintaining the constant attention to improvement in all aspects of coding,along with the two day coding completion deadline (the fastest we know of in the NHS)plus having one of the lowest cost departments using Audit Commission benchmarks,is not easy. Therefore <strong>Board</strong> level recognition of the Coding Department’s staff effortwould be appreciated. This combined with feedback to clinical staff about the positiveimpact of their efforts to improve should create a positive cycle for ongoing accuracy.3. Update on the recommendations and proposed action planThe Coding Department has an accuracy improvement plan that goes far beyond theformal recommendations, as it did last year as well. However this section reflects thesix areas highlighted by the Commission. R6 relating to IT systems, has been carriedover from last year.R1 Angiogram recording. This change has been deferred to April 2012, and isdiscussed further below, as part of the wider context.R2 Skin procedure training has occurred. Action completed.R3 Coding clinic co-morbidity list new widely circulated and embedded. Actioncompleted.R4 Image control recording by clinical staff. Training has been implemented and isbeing monitored, especially in Interventional Radiology. Action completed.R5 Review and share the results with Medical Records User Group. This isunderway, but the Commission recognises this is more good practice rather thanactually being expected to improve accuracy, and is a repeat of last year.R6 Update the system, avoiding READ codes. This is discussed below.As of May 2011 all actions are completed to an agreed outcome, with the exception ofa date for the IT update to allow us to move from READ coding. This is likely to occurin late 2011, following upgrade to the server capacity in the summer. This change willhave numerous benefits including:• Less transcription errors, improving our accuracy scores.• Faster upgrades to OPCS, again improving our coding accuracy.• Less staff time and duplication of entry.• Better ability to audit coding accuracy in house, as part of the coding teams work.Results of the 2010/11 PbR Assurance Clinical Coding Audit Page 2 of 3
<strong>Board</strong> of Directors – Part I10 th June 20114. Wider context for coding accuracy and improvementThe most contentious part of the Audit Commission recommendations is regardingcardiac angiogram recording, as part of another procedure. Our view, and that ofmany Trusts, is that all activity should be coded, and it is for the grouper to assign thisto the right HRG. Therefore the national and local message was to record allprocedures as part of an episode of care.The recommendation is to stop recording angiograms where an angiography isundertaken. Whilst the financial impact of this within the cohort of patients audited isnet neutral, estimates of the Trust wide impact of this change are between £400k and£750k. The PCT and Trust have not agreed a financial impact figure, but have agreedto defer the implementation of the change for 12 months, starting April 2012. This isbalanced by the Trust agreeing to defer the impact of Emergency Departmentattendance tariffs for the same period. Again estimates have not been agreed, but theTrust is confident we will be able to at least, offset the angiogram impact, andpotentially more than offset it.All other changes arising from the results of the audit will though be enacted in2011/12.5. Future plansAn external company will once again undertake a mid year audit using the samemethodology as the Audit Commission. This will be used to give external assuranceregarding the actions and outcomes discussed here. The audit Commission will thenrepeat this exercise in a similar timescale next year, with exact dates still to beconfirmed.The wider work on improving coding accuracy will also continue.The results of the Audit Commission report will be made available to ourcommissioning PCTs, and publicly. The results will also be used to inform our CQCmonthly quality risk report.6. RecommendationsThe <strong>Board</strong> are asked to note the report and actions, and the significantimprovements in performance. An update after future re-audits will beshared with the <strong>Board</strong>.Results of the 2010/11 PbR Assurance Clinical Coding Audit Page 3 of 3
Payment byresults dataassuranceframeworkClinical Coding Audit at The <strong>Royal</strong> <strong>Bournemouth</strong> andChristchurch <strong>Hospital</strong>s NHS Foundation Trust<strong>Bournemouth</strong> and Poole Teaching Primary Care TrustAudit 2010/11
The Audit Commission is an independent watchdog,driving economy, efficiency and effectiveness in localpublic services to deliver better outcomes for everyone.Our work across local government, health, housing,community safety and fire and rescue services meansthat we have a unique perspective. We promote value formoney for taxpayers, auditing the £200 billion spent by11,000 local public bodies.As a force for improvement, we work in partnershipto assess local public services and make practicalrecommendations for promoting a better quality of lifefor local people.
ContentsSummary.............................................................................................................2Introduction...................................................................................................2Summary of overall findings .........................................................................2Audit results..................................................................................................3Key areas for improvements.........................................................................5Recommendations........................................................................................5Next steps.....................................................................................................6Detailed report....................................................................................................7Introduction...................................................................................................7Audit Approach .............................................................................................8Scope of the audit.........................................................................................8Unsafe to Audit (UTA)...................................................................................9Findings ........................................................................................................9Next steps...................................................................................................16Appendix 1 – Action Plan (PCT) .....................................................................18Appendix 2 – Action Plan (Trust)....................................................................19Appendix 3 – Specialty A - General Medicine ...............................................21Appendix 4 – Specialty B - General Medicine ...............................................34Appendix 5 – Chapter - JC Skin......................................................................50Appendix 6 – HRG area EB01Z - Non interventional acquired cardiacconditions 19 years and over .........................................................................67Appendix 7 – Ungrouped original Cardiology results from 2007/08 ...........71Appendix 8 – Error keys..................................................................................72Appendix 9 – Glossary ....................................................................................77Audit Commission Payment by results data assurance framework 1
SummaryIntroduction1 The Payment by Results (PbR) Data Assurance programme (theprogramme) supports the improvement of data quality. Accurate coding datais important as it is the underlying information used, not only for billing bytrusts, but also for information on the health of the local community bycommissioners.2 Since 2007/08, the programme has identified £9 million of incorrectlycoded activity from over £200 million of payments. There have beenimprovements with the accuracy of clinical coding improving from a 16 percent error rate to 11 per cent in 2009/10.3 Under PbR PCTs are charged by trusts according to the HealthcareResource Groups (HRGs) they deliver. The <strong>Royal</strong> <strong>Bournemouth</strong> andChristchurch <strong>Hospital</strong>s NHS Foundation Trust (the Trust) was selected for atargeted audit as the HRG error rates over three years places it in the worstperforming 20 per cent of trusts. We carried out the audit in December 2010using data from 1 April to 30 June 2010.Summary of overall findings4 The aim of the programme is to provide assurance for bothcommissioners and providers that the HRGs used as the basis for charginghave been correctly calculated. At The <strong>Royal</strong> <strong>Bournemouth</strong> andChristchurch <strong>Hospital</strong>s NHS Foundation Trust the error rate measured usingHealthcare Resource Groups (HRGs) has improved since the previousaudit.5 This year the HRG error rate at the Trust is 10 per cent. This is asignificant improvement compared to last year when the HRG error rate was24 per cent. The Trust is performing close to the national average (9.1 percent) when compared to the overall performance of trusts in 2009/10. TheTrust’s HRG error rate has varied over the four year period of theprogramme. However, further improvements in the accuracy of clinicalcoding could be made.6 Overall the Trust is improving the quality of the source document forcoding which in this Trust is a formal electronic discharge summary with thebenefit of in-house computer systems to back this up. The electronicdischarge summary is fairly comprehensive. However, this could beimproved by clinical staff providing more specific information as it stillaccounted for 4.3 per cent of primary diagnosis and 6.5 per cent ofsecondary diagnosis errors.Audit Commission Payment by results data assurance framework 2
Figure 1: HRG, procedure and diagnosis error rate40%HRG error rate Procedure error rate Diagnosis error rate35%30%25%20%15%10%5%0%2007/08 2008/09 2009/10 2010/11 2007/08 2008/09 2009/10 2010/11 2007/08 2008/09 2009/10 2010/11Trust error rateNational averageAudit results7 We measure trust performance using two indicators - HealthcareResource Group (HRG) accuracy and clinical coding accuracy - see Figure1. The performance of the Trust, measured using HRG error rate, is similarto the national average using the 2009/10 full year results. The Trust'saverage HRG error rate is 10 per cent compared to the 2009/10 nationalaverage of 9.1 per cent.8 HRGs are based on diagnosis and procedure codes which generatesthe HRG on which payment is based. Figure 1 shows that the percentage ofdiagnoses and procedures incorrectly coded at the Trust is 9.9 per cent.This is an improvement on the 2009/10 national average of 11 per cent.This year we audited 1,422 diagnoses and procedures and there were 142errors or 9.9 per cent were in correct. The Coding Manager has worked withclinical staff to ensure the content of the electronic discharge summary isrobust enough to support clinical coding. However, ensuring that theelectronic discharge summary contains the right level of detail is an ongoingissue as clinical staff rotate and change regularly.9 The main reasons for the coding errors were:■ non coder errors – leading to 65 errors (45.8 per cent); and■ omission of diagnosis and procedures – leading to 46 errors (32.4 percent)Unsafe to audit - cases excluded from the audit10 The aim of the programme is to provide assurance that the HRGs usedas the basis for charging commissioners have been correctly calculated. Wewere provided with 300 episodes with a value of £342,424. No episodeswere excluded from the audit because they were "unsafe to audit".Audit Commission Payment by results data assurance framework 3
Areas selected for follow up11 As part of the programme this year, two areas were selected for followupso that we could provide assurance for commissioners on the progress ina particular area. Where necessary we "regrouped" the information toenable a direct comparison.12 In 2009/10, the HRG error rate in General Medicine was 35 per centand this year, the HRG error rate was 7 per cent - an improvement of 28percentage points. This indicates that coding in this area has improvedsignificantly following the discussions and agreement between the CodingManager and Clinical Staff. The improvements to the quality of theelectronic discharge summary and the improvement of the informationrecorded on the electronic patient record are evident in the audit results.However, as noted above, ensuring that the electronic discharge summarycontains the right level of detail is an ongoing issue as clinical staff rotateand change regularly.13 In 2007/08, the regrouped HRG error rate in Cardiology was 3 per centand this year, the HRG error rate was 10 per cent - a deterioration of 7percentage points. This indicates that coding in this area is poor as themajority of errors in Cardiology were due to recording codes as instructedby clinical staff or a lack of complete information available on the electronicdischarge summary.Financial impact of errors14 Table 1 below shows the financial impact of the HRG errors acrosseach of the areas audited. The financial value of all of the errors is £152from an audit sample of £342,424 – 4.0 per cent. The net impact of errors isvery small. Based on the sample tested, the Trust is overcharging itscommissioners by £152.Table 1:Table of main findingsAreaauditedSpecialty/Subchapter/HRGNumberof FCEs% ofepisodeschangingHRGPreAuditPaymentPostAuditPaymentNetchange%changeTheme General 100 7.0 £79,712 £79,665 -£47 -0.1MedicineSpecialty Cardiology 100 10.0 £201,825 £197,126 -£4,699 -2.3SubchapterJC - Skin 70 18.6 £46,626 £51,220 £4,594 9.9surgeryHRG EB01Z 30 0.0 £14,261 £14,261 £0 0.0Overall 300 10.0 £342,424 £342,272 -£152 0.0Audit Commission Payment by results data assurance framework 4
Key areas for improvements15 The key areas for the Trust to improve the coding accuracy are:■ removal of the policy regarding the use of a secondary procedure codefor angiograms when an angioplasty is undertaken. These are codeddue to clinical staff insisting these codes are added when an angiogramis done at the same time as an angioplasty;■ provide training to the coders covering how skin procedures should becoded, as these can be coded in two ways depending on the site of thebody that has been operated on;■ reinforce the importance of recording the mandatory co-morbidities fromthe March 2010 Coding Clinic, as omission of secondary diagnoses wasan issue from both the coder and clinical perspective; and■ the clinical staff need to be informed that all information in thecasenotes should be duplicated on the electronic patient record as thisis the source document for coding.Recommendations16 Accurate coding supports accurate data. This information is used notonly for billing purposes, but for planning by both the Trust and allcommissioners. We followed up the progress on the 12 recommendationsfrom our 2009/10 report, including one outstanding since 2008/09. The Trusthas fully implemented 10 of the 12 recommendations, which is satisfactory.Recommendation 6 in 2009/10 on improvements in the standard ofcasenotes has not been implemented but this has little impact on the qualityof coding as casenotes are not used as the source document in the Trust.The coders use the electronic discharge summary with the EPR and thiswould only impact on the few episodes when the coder would need toaccess the information in the casenotes due to poor information held withinthe electronic discharge summary or electronic patient record.17 The PCT and Trust should ensure that all recommendations arefollowed up and implemented in order to support the improvement in coding.The key recommendations for each organisation are noted below.High priority recommendations for the TrustR1 Stop recording Angiogram codes when Angioplasty procedures areundertaken and remove the policy regarding this from the coding Policyand Procedure document. Coders should be instructed to use onlyappropriate codes in cardiology episodes.R2 Train coders to follow the guidance regarding skin procedures at thebeginning of OPCS chapter S and when to use codes from chapter S orspecific body system codes.R3 Recording of co-morbidities from the March 2010 Coding Clinic must befollowed by all coders and clinicians.Audit Commission Payment by results data assurance framework 5
18 A full action plan for the PCT is at appendix 1 with an action plan for theTrust at appendix 2. The detailed report and appendices 3, 4, 5 and 6expand on the audit findings and provide evidence for the actions to supportimprovement. The appendices are aimed primarily at specialist coding staffat the Trust and will be of interest to commissioners where there are specificissues arising from the audit.Next steps19 The findings from this audit will be discussed and agreed with the Trustand PCT on 3 February 2011 and the organisations should use theirestablished arrangements to monitor and follow up the issues andrecommendations agreed in the report. The results of this audit should beshared with other PCTs commissioning services from The <strong>Royal</strong><strong>Bournemouth</strong> and Christchurch <strong>Hospital</strong>s NHS Foundation Trust.20 We will publish a summary of the key results on the Audit Commission’swebsite when all audits in 2010/11 are completed and reported to PCTs andtrusts. Our website also contains details of the other aspects of theprogramme. This includes national briefings, case studies and free accessto the National Benchmarker for NHS organisations.21 Providing assurance over the quality of underpinning data remains akey consideration for the PbR system. This will increase with the plans tomove the PbR tariff into areas such as mental health, community servicesand the further development of linking payments to outcomes. The AuditCommission will continue to undertake this role whilst it and PCTs exist. Wewill work with the Department of Health, the new NHS Commissioning<strong>Board</strong>, Monitor and the Information Centre to ensure these crucial checksremain within the payment system in the future and will be consulting in2011 regarding the future direction of the programme for 2011/12 onwards.Audit Commission Payment by results data assurance framework 6
Detailed reportIntroduction22 The Payment by Results (PbR) Data Assurance programme (theprogramme), commissioned by the Department of Health (DH), is designedto support the improvement of data quality that underpins the accuracy ofcoding and payment. The programme, which is being delivered as part ofPCT audits in 2010/11, is a rolling programme of work developed andmanaged by the Audit Commission, and is delivered by accredited clinicalcoder auditors.23 The programme is now in its fourth year and the inpatient audit hasbeen extended to include audits of Independent Sector providers, as well asNHS Trusts carrying out work under contract to PCTs. Other aspects of theprogramme include:■ reviewing the quality of costing information at all acute trusts in 2010/11,including assessing the accuracy of activity and costing data used bymany PCTs for local pricing and contracting of non-PbR activity. It willalso provide some assurance over the accuracy of national tariffs giventhat reference costs are the basis of most tariffs;■ national reporting and analysis from the audit programme, includingpublication of results and comparative briefings for all SHAs, PCTs andtrusts;■ developing the PbR National Benchmarker online tool, used extensivelyby the NHS;■ following up outpatient arrangements at 30 NHS trusts based on theresults from our work; and■ piloting and reporting extensions to the coverage of the programme,such as our work with independent sector providers and on Accidentand Emergency (A&E).24 Since the start of the full programme in 2007/08, we have audited over£200 million of payments and identified approximately £9 million of financialerrors due to clinical coding errors. The HRG error rate has fallen since thestart of the programme, though increased from 2008/09 to 2009/10 mainlydue to the introduction of HRG4 - for more information see our 2010/11national report. The average HRG error rate in 2009/10 was 9.1 per cent.The accuracy of clinical coding, measured using procedure and diagnosiserror rates is improving year-on-year - from an average of 16 per cent to 11per cent in 2009/10.25 The quality of the data underpinning PbR has wider implications for theNHS as this information is used in all aspects of the service to determinehow and where care is delivered. The clinical coding data that is auditedhere is used for service planning and monitoring; commissioning andepidemiology; research; clinical audit; consultant job planning; patient safetyAudit Commission Payment by results data assurance framework 7
and clinical governance. Good data quality improves and supports gooddecision making at a national and a local level, as well as informingdecisions on patient care and planning.Audit Approach26 This inpatient audit was carried out by accredited clinical codingauditors who are NHS Connecting for Health (CFH) registered auditors.They are required to adhere to the latest version of the NHS CFH Code ofPractice for clinical coding auditors. The coding audits undertaken for theprogramme go beyond the CFH coding audit national methodology v3.1 inthe following respects:■ the use of benchmarking indicators to support the audit;■ grouping the data to HRGs and processing under PbR business rules togauge financial impact of data quality;■ calculating the value and impact on error rate of cases deemed "unsafeto audit"; and■ identification of best practice.27 This approach allows the accuracy of clinical coding to be assessed inthe targeted areas, and to support improvement in coding and associatedarrangements. There is no other toolkit/approach that provides this.28 We consulted with stakeholders in late 2009 on developing theprogramme. Based on this feedback we are moving to a more risk basedapproach focusing resources on the trusts still that need to improve themost. The <strong>Royal</strong> <strong>Bournemouth</strong> and Christchurch <strong>Hospital</strong>s NHS FoundationTrust (the Trust) was selected for audit as the HRG error rates over threeyears places it in the worst performing 20 per cent of trusts.29 The Audit Commission reports to a lead PCT for each trust audit as thecommissioner of services and the acute provider as both haverecommendations that should be implemented. The lead PCT should sharethe findings from this audit with other PCTs who commission services fromthe Trust.Scope of the audit30 The audit was undertaken at The <strong>Royal</strong> <strong>Bournemouth</strong> and Christchurch<strong>Hospital</strong>s NHS Foundation Trust in December 2010. The audit covered 300Finished Consultant Episodes (FCEs), of which 200 were selected from anarea audited as a national theme or specialty in the previous three years.Audit Commission Payment by results data assurance framework 8
31 The remaining 100 FCEs were selected based on local knowledgesupported by the output from the National Benchmarker which identifiesareas where the Trust was an outlier. Table 2 sets out the areas that wereaudited:Table 2:Audit areasAreaauditedSpecialty/Subchapter/HRGGeneralMedicineSample sizeReason forselectionSpec A100 Audited in2009/10Spec B Cardiology 100 Audited in2007/08Sub-chapter JC - Skin 70 Selected fromsurgerybenchHRGEB01Z Noninterventionalacquiredcardiacconditions 19years andovermarking data30 Selected frombench markingdataDetailedfindingsAppendix 3Appendix 4Appendix 5Appendix 6Cases referred to Connecting for Health for arbitration32 In cases where the Coding Auditor and trust are unable to agree thecoding, the case is removed from audit. The Coding Auditor submits thecase to CFH for adjudication and we audit another case to main samplesizes. No cases have been sent to CFH from this audit.Unsafe to Audit (UTA)33 There were no cases judged "unsafe to audit" within the 300 episodesprovided for audit. These are episodes where there is no information withinthe notes for the episode which has been selected for audit.Findings34 The audit findings focus on the following areas:■ coding accuracy;■ follow up area/s;■ financial impact of errors;■ coding arrangements;■ follow up of previous year’s recommendations;■ audit information and data quality; and■ local data definition issues.Audit Commission Payment by results data assurance framework 9
Coding accuracy35 The number of episodes with errors which would have changed theHRG was 30 representing 10 per cent of the total cases tested. There were23 procedure errors (6.5 per cent) and 119 diagnosis coding errors (11.1per cent).36 The area with the largest number of errors was in Chapter JC - Skinwhere there was 42 percent of secondary diagnoses coded incorrectly thiswas mainly due to omission of codes (34 per cent)37 Table 3 shows the coding accuracy in the areas audited:Table 3:AreaauditedCoding accuracy in the areas auditedSpecialty/Subchapter/HRG% ProceduresCoded Incorrectly% Diagnoses CodedIncorrectly% ofepisodeschangingHRG% ofspellschangingHRGPrimary Secondary Primary SecondaryTheme General 11.8 0.0 12.0 9.1 7.0 9.6MedicineSpecialty Cardiology 2.5 0.0 2.0 7.3 10.0 12.5SubchapterJC- Skin 17.1 12.8 12.9 42.0 18.6 18.6surgeryHRG EB01Z Non 0.0 0.0 16.7 20.0 0.0 0.0interventionalacquiredcardiacconditions 19years andoverOverall 9.7 3.0 9.3 11.8 10.0 12.7Key areas for improvements38 The <strong>Royal</strong> <strong>Bournemouth</strong> and Christchurch <strong>Hospital</strong>s NHS FoundationTrust is performing close to the national average when compared to theoverall performance of trusts in 2009/10. The Trust’s HRG error rate hasvaried over the four year period of the programme. However, furtherimprovements in the accuracy of clinical coding could be made.39 The Coding Manager confirmed the electronic discharge summary waspoor in previous years but work has been done to improve this. The CodingManager held awareness sessions and regular meetings with clinical staff toexplain what details the coders need when coding. As the error rate hasimproved this indicated there have been problems in accuracy of the sourcedocument from using the discharge summary in isolation but this has nowimproved. This year clinical coding accuracy at the Trust is slightly higherthan the 2009/10 national average of 9.1 per cent.Audit Commission Payment by results data assurance framework 10
40 The HRG error rate at the Trust is 10 per cent, a significant decreasefrom 24 per cent in 2009/10. This is a considerable improvement from2009/10 error rate in the accuracy of the coded data and the Trust shouldbe commended for this.41 The accuracy of coding diagnosis and procedures, the building blocksof HRG coding, has also improved over the period. The percentage ofinaccurately coded procedures and diagnosis was 9.9 per cent. This issignificantly better than in previous audits and demonstrates the time andeffort that has been invested in improving the quality of the coded data.42 The main reasons for the coding errors were:■ coders and clinicians not following the guidance from the March 2010Coding Clinic regarding coding of mandatory co-morbidities when theinformation was available at the time of coding;■ the use of a secondary procedure code for angiograms when anangioplasty is undertaken in Cardiology. These are coded due to clinicalstaff insisting these codes are added when an angiogram is done at thesame time as an angioplasty. This is against the coding rule whendiagnostic and therapeutic procedures are carried out on the same siteas the same theatre visit and only the therapeutic procedure should berecorded. This was the cause of all of the HRG changes withinCardiology;■ skin procedures are coded in two ways depending on the site of thebody that has been operated on. The coder had not reflected thedifferent site of procedures within the codes allocated and continued touse only codes from chapter ‘S’ when sometimes the correct codesshould be from other specific chapters. For example, skin operation onthe ear should be coded using a code from chapter ‘D’ with a code fromchapter ‘S’ to enhance this. All coders must have this rule re-enforced toensure these are coded correctly; and■ the specific type of image control used was not documented within thecasenotes and the EPR. The coding of Cardiology procedures could bemore specific if this information is available to the coder.Follow up area – General Medicine and Cardiology43 As a measure of progress, the audit revisited coding in GeneralMedicine. In General Medicine in 2009/10 there were 35 per cent of HRGschanging. This year, the HRG error rate was 7 per cent which is aconsiderable improvement on last year and the Trust should be commendedfor this.44 The audit also revisited coding in Cardiology. In Cardiology in 2007/08,3 per cent of HRGs were changing. This year the HRG error rate was 10 percent which is an improvement on the previous audit in 2007/08 however thiscould be improved further if the policy of recording angiograms wasremoved.Audit Commission Payment by results data assurance framework 11
45 As the audit of Cardiology was undertaken in 2007/08 and groupedusing HRGV3.5, we have converted the data from 2007/08 HRG4 to providea more accurate base for comparison with this year’s result.Table 4:General Medicine area progressItem 2009/10 % 2010/11 % Change %HRG errors i 35 7 -28Primary Diagnosis 46.0 12.0 -34errorsSecondary 41.6 9.1 -32.5Diagnosis errorsPrimary13.3 11.8 -1.5procedure errorsSecondary 7.9 0 -7.9procedure errorsNet Financialimpact of errors£2,045 -£47 £2,092Table 5:Cardiology area progressItemRegrouped 2010/11 % Change %2007/08 %HRG errors ii 3 10 7Primary Diagnosis 10.0 2.0 -8errorsSecondary 30.7 24 -6.7Diagnosis errorsPrimary14.4 7.3 -7.1procedure errorsSecondary 11.6 0 -11.6procedure errorsNet Financialimpact of errors£2,418 -£4,699 £2,28146 Coding in General Medicine has improved significantly following theimprovement of the quality of the electronic discharge summary and theimprovement of the information recorded on the electronic patient record.This was the result of joint working between the Coding Manager andclinical staff.47 Coding in Cardiology has deteriorated, however, the majority of errorswere due to recording codes as instructed by clinical staff or to a lack ofcomplete information available at the time of coding.Financial impact of audited errors48 The sample covered 300 FCEs. These episodes were then grouped to221 spells with a total value of £342,424. The total value of all errorsregardless of who they favoured (absolute or gross change) was £13,538.i Only HRGs have been regroupedii Only HRGs have been regroupedAudit Commission Payment by results data assurance framework 12
The net value of the HRGs that changed as a result of the errors identifiedin coding and correction of the spells in the sample would lead to a smalldecrease in total payments due to the Trust of £152. The level and mixtureof errors between those reducing or increasing payments indicates thatcoder error, rather than deliberate miscoding, is at the root of theinaccuracies.49 A summary of the impact of the errors on the HRG allocation andconsequent applicable tariff is given in Table 5 below:Table 6:AreaauditedPayment changes from pre to post auditSpells Pre PostAudit AuditPayment PaymentSpecialty/Subchapter/HRGValue of HRGChanges% change preand post auditGross Net Absolute NetTheme General 52 £79,712 £79,665 £4,245 -£47 5.3 -0.1MedicineSpecialty Cardiology 80 £201,825 £197,126 £4,699 - 2.3 -2.3£4,699SubchapterSkinSurgery70 £46,626 £51,220 £4,594 £4,594 9.9 9.9JCHRG EB01Z 19 £14,261 £14,261 £0 £0 0.0 0.0Overall 221 £342,424 £342,272 £13,538 -£152 4.0 -0.0Coding arrangements50 The coding arrangements are good leading to a decrease in the HRG,procedure and diagnosis error rates.51 The condition of the casenotes has been improved and new folders areissued when the original folder is in poor condition. However it is imperativethat further improvements to the medical record are progressed through theMedical Records User Group. As the coders use the electronic dischargesummary with the EPR this will have little impact on the coded data.52 Coding at the Trust is done using a combination of clinical terminology(READ codes) and then ICD-10 and OPCS 4.5 codes. Clinical terms arechosen first, and maps to the other classifications are then defined. Thismakes coding accuracy more difficult to achieve. This issue was raised inlast year's report and the Trust investigated possible system updates tocode directly to ICD-10 and OPCS 4.5 codes thereby avoiding theintermediate step of using clinical terminology (READ codes). It has beenagreed to update the system to allow the coders to directly code in ICD10and OPCS 4.5, the Trust are waiting for an implementation date.53 The key areas for the Trust to improve the coding accuracy are:■ removal of the policy regarding the use of a secondary procedure codefor angiograms when an angioplasty is undertaken. These are codeddue to clinical staff insisting these codes are added when an angiogramis done at the same time as an angioplasty. This is against the codingrule when diagnostic and therapeutic procedures are carried out on theAudit Commission Payment by results data assurance framework 13
■■■■same site at the same theatre visit, only the therapeutic procedureshould be recorded. This was the cause of all of the HRG changeswithin Cardiology;provide training to the coders covering how skin procedures should becoded, as these can be coded in two ways depending on the site of thebody that has been operated on. The coder had not reflected thedifferent site of procedures within the codes allocated and continued touse only codes from chapter ‘S’ when sometimes the correct codesshould be from other specific chapters. For example skin operation onthe ear should be coded using a code from chapter ‘D’ with a code fromchapter ‘S’ to enhance this. All coders must have this rule re-enforced toensure these are coded correctly;reinforce the importance of recording the mandatory co-morbidities fromthe March 2010 Coding Clinic, as omission of secondary diagnoses wasan issue from both the coder and clinical perspective;the Coding Manager needs to work with clinical staff to re-enforce theneed that all information in the casenotes should be duplicated on theelectronic patient record as this is the source document for coding; andthe specific type of image control needs to be documented within thecasenotes and the EPR. The coding of Cardiology procedures could bemore specific if this information is available to the coder.RecommendationsR1 Stop recording Angiogram codes when Angioplasty procedures areundertaken and remove the policy regarding this from the coding policy andprocedure document. Coders should be instructed to use only appropriatecodes in cardiology episodes.R2 Train Coders to follow the guidance regarding skin procedures at thebeginning of OPCS chapter S and when to use codes from chapter S orspecific body system codes.R3 Recording the co-morbidities from the March 2010 Coding Clinic mustbe followed by all coders and clinicians.R4 Target training to clinical staff on the use of image control to berecorded more accurately to identify the specific type of imaging oncardiology procedures.R5 (R6 in 2009/10) Review and share results with Medical Records UserGroup, the organisation of casenotes to agree on an action plan forimproving record keeping standards (to improve ease of use and so codingaccuracy / speed).R6 (R9 in 2009/10) Update the system to code directly to ICD-10 andOPCS 4.5 codes thereby avoiding the intermediate step of using clinicalTerminology (READ codes).Audit Commission Payment by results data assurance framework 14
Follow up of previous year’s recommendations54 The coding audit for 2010/11 took place in January 2010. Progress onthese recommendations was followed up at the set up meeting and duringthe course of the audit visit. There were 12 recommendations from our2009/10 report, including one outstanding from previous audits. Of theseone had been outstanding since 2008/09. The Trust has fully implemented10 of the 12 recommendations, which is satisfactory. Despite action beingtaken on the remaining recommendations, they had not been fullyimplemented or the issues are still affecting coding.55 <strong>Bournemouth</strong> and Poole Teaching PCT, as lead commissioner for theTrust, should work in partnership with other commissioners to ensure actionis being taken to address the issues raised in this report.Implemented recommendationsR1 in 2009/10 (R2 in 2008/09 report; revised): Include all local codingpolicies within the Policy and Procedure document. Updates to thisdocument should be formally agreed, signed and dated by relevantclinicians. Coders’ awareness of local policies should be assessedregularly.■ Action: All local policies have been reviewed and updated asnecessary and Clinicians have signed relevant statements.R2 in 2009/10: Investigate causes of multiple incorrect episodes beingcreated within spells, and address the issues to ensure transfers of careare recorded accurately.■ Action: A Clinical Data Quality Co-ordinator is now in post toimplement changes in the recording of consultant transfers whichwill reduce errors.R3 in 2009/10: Code from full casenotes for long-stay patients with actualmultiple episodes, in order to identify individual incidents and avoidinaccuracies in coding the component episodes.■ Action: A clinical coder has been placed on the ward to facilitatethis.R4 in 2009/10: Review departmental staffing levels and workloads (in linewith national averages) to improve coding accuracy.■ Action: A review has taken place of the workload and it was foundthat the workload should reduce now the multiple consultanttransfer errors have been resolved.R5 in 2009/10: Carry out internal audits to ensure clinicians are completingsummaries within timeframes, and coders are reading through the entirecontents of the summaries.■ Action: An audit has taken place on the content of dischargesummaries and the timeliness – both are improving. Coders haveAudit Commission Payment by results data assurance framework 15
Implemented recommendationsbeen reminded of attention to detail.R7 in 2009/10: Revise the Trust’s Policy and Procedure manual so that itprovides comprehensive guidance on all clinical coding issues.■ Action: The Policy and Procedure document was reviewed andupdated in August 2010.R8 in 2009/10: Deliver targeted training to address errors noted in theaudit.■ Action: Training has been provided.R10 in 2009/10: Train coders to research the symptoms of disorders andstop coding unnecessary co-morbidities; revise the rehabilitation coderules and apply external cause code rules appropriately.■ Action: Training has been provided.R11 in 2009/10: Organise training by clinical staff on the interpretation ofTOMCAT reports.■ Action: TOMCAT reports have been analysed and training hasbeen provided.R12 in 2009/10: Amend the local policy document, together with thecardiac team, to clarify the image control of cardiac procedures generallyand what form of imagery is used in exceptional cases.■ Action: A review has taken place with the cardiac team and thelocal policy has been amended.56 Action was taken on the remaining recommendations, however theaudit identified that the same issues were still occurring, so theserecommendations have been carried forward to this audit report.Audit information and data quality57 The Trust was able to provide a data file for the audit.Local data definition issues58 There were no local data definition issues identified between the Trustand the lead PCT.Next steps59 The findings from this audit will be discussed and agreed with the Trustand PCT on 3 February 2011. The two organisations should use theirestablished arrangements to monitor and follow up the issues andrecommendations agreed in the report. The PCT should share the findingsfrom this audit with other PCTs commissioning services from The <strong>Royal</strong><strong>Bournemouth</strong> and Christchurch <strong>Hospital</strong>s NHS Foundation Trust.Audit Commission Payment by results data assurance framework 16
60 A summary of the key results will be published on the AuditCommission’s website when all audits in 2010/11 are completed andreported to PCTs and trusts. Our website also contains details of the otheraspects of the programme. This includes national briefings, case studiesand free access to the National Benchmarker for NHS organisations. Formore information see www.audit-commission.gov.uk/pbr.Audit Commission Payment by results data assurance framework 17
Appendix 1 – Action Plan (PCT)RecommendationsRecommendation 1R1: Continue the established mechanism with the Trust to follow up the actions and issuesidentified in this report.ResponsibilityHighPriorityDateCommentsAudit Commission Payment by results data assurance framework 18
Appendix 2 – Action Plan (Trust)RecommendationsRecommendation 1R1: Stop recording Angiogram codes when Angioplasty procedures are undertaken and removethe policy regarding this from the coding Policy and Procedure document. Coders should beinstructed to use only appropriate codes in Cardiology episodes.ResponsibilityHighPriorityDateCommentsRecommendation 2R2: Train coders to follow the guidance regarding skin procedures at the beginning of OPCSchapter S and when to use codes from chapter S or specific body system codes.ResponsibilityHighPriorityDateCommentsRecommendation 3R3: Recording the co-morbidities from the March 2010 Coding Clinic must be followed by all codersand clinicians.ResponsibilityHighPriorityDateCommentsRecommendation 4R4: Target training to clinical staff on the use of image control to be recorded more accurately toidentify the specific type of imaging on cardiology procedures.ResponsibilityMediumPriorityDateCommentsAudit Commission Payment by results data assurance framework 19
Recommendation 5R5 (R6 in 2009/10): Review and share results with Medical Records User Group, the organisationof casenotes to agree on an action plan for improving record keeping standards (to improve ease ofuse and so coding accuracy / speed).ResponsibilityMediumPriorityDateCommentsRecommendation 6R6 (R9 in 2009/10): Update the system to code directly to ICD-10 and OPCS 4.5 codes therebyavoiding the intermediate step of using clinical Terminology (READ codes).ResponsibilityHighPriorityDateCommentsAudit Commission Payment by results data assurance framework 20
Appendix 3 – Specialty A - General Medicine61 At The <strong>Royal</strong> <strong>Bournemouth</strong> and Christchurch <strong>Hospital</strong>s NHSFoundation Trust the follow up area covered was General Medicine whichwas audited in 2009/10. This audit was at a specialty level, covering allHRGs / chapters. A sample of 100 cases was provided for audit and nonewere found to be unsafe to audit as per NHS CFH standards.Table 7: Specialty A General Medicine area: coding errorsPrimarydiagnosisSecondarydiagnosisPrimaryprocedureSecondaryprocedureTotalfromepisodesauditedIncorrectCoderErrorNoncodererrorTotalincorrect% incorrect2010/11 2009/10100 9 3 12 12.0 46.0296 15 12 27 9.1 41.634 2 2 4 11.8 13.39 0 0 0 0.0 7.9Overall 439 26 17 43 9.8 36.9Table 8: Specialty A area: HRG errorsEpisodesSpellsTotal 100 52Total changing HRG 7 5% changing HRG 7.0 9.6Analysis of coding errors62 The audit identified 43 (9.8 per cent) errors in procedure and diagnosescoding, leading to seven HRG changes. The impact of the seven HRGchanges was that the Trust was undercharging its commissioners by £47 onthe sample tested.Audit Commission Payment by results data assurance framework 21
63 The following areas for improvement have been identified:■ reinforcing the importance of recording the mandatory co-morbiditiesfrom the March 2010 Coding Clinic, as omission of secondarydiagnoses was an issue from both the coder and clinical perspective.This accounted for 53.5 per cent of the errors in this area; and■ providing training to the coders to cover the definition of the primarydiagnosis. There were nine coder errors at primary diagnosis level (20.9per cent).64 There were 17 non-coder errors due to the source document not havingall of the information for the coder at the time/point of coding, this affectedthree primary and 12 secondary diagnoses plus two primary procedures.65 The coder errors were in the following areas:■ incorrect coding at the required 3-, 4- and 5- character level affectingseven primary and four secondary diagnoses and two primaryprocedures; and■ omission of diagnosis and procedures – affecting two primary and 11secondary diagnoses.66 There are 10 instances when information not relevant to the episode ofcare has been coded. NHS CFH does not treat this as an error and werethey to have been included they would have accounted for none of the HRGchanges. The Trust should seek to code only relevant information.Follow up of audit in this area from 2009/1067 General Medicine was audited in 2009/10 and was selected as an areafor follow up. It is important to note that different OPCS versions may havebeen in use at the time of the audits. This can have an impact on the overallHRG error rate.Table 9: Follow up of HRG changesEpisodes2010/11 2009/10 ChangeTotal 100 100 -Total changingHRG 7 35 -28% changingHRG 7.0% 35.0% -28.0%68 The HRG and coding error rate have improved considerably since2009/10. This result could be better if training was provided coveringprimary diagnosis definition and the March 2010 Coding Clinic regarding thecoding of relevant mandatory co-morbidities.Audit Commission Payment by results data assurance framework 22
Financial impact of errorsTable 10: Specialty A area: financial impact of errorsPre AuditPaymentPost AuditPaymentGrossChange% GrossChangeNetChange£79,712 £79,665 £4,245 5.3 -£47 -0.1% NetChangeData Issues69 There were no data issues identified within the Specialty A area.Audit Commission Payment by results data assurance framework 23
HRGs and price changes as a result of the audit (General Medicine)Example 1ID Speclty 300 ThemeEpisode Start 16/04/2010 End 19/04/2010TrustCodingAuditCodingError KeyPDiag K20X Oesophagitis K921 Melaena PDODiag1 B378 Candidiasis - Candidiasis K20X Oesophagitisof other sitesDiag2 K259 Gastric ulcer - Gastriculcer, unspecified asacute or chronic, withouthaemorrhage orperforationB378 Candidiasis - Candidiasisof other sitesDiag3 I259 Chronic ischaemic heartdisease - Chronicischaemic heart disease,unspecifiedDiag4 I10X Essential (primary)hypertensionDiag5 J449 Other chronic obstructivepulmonary disease -Chronic obstructivepulmonary disease,unspecifiedI259I10XJ449Chronic ischaemic heartdisease - Chronicischaemic heart disease,unspecifiedEssential (primary)hypertensionOther chronic obstructivepulmonary disease -Chronic obstructivepulmonary disease,unspecifiedDiag6 K259 Gastric ulcer - Gastriculcer, unspecified asacute or chronic, withouthaemorrhage orperforationHRG FZ31A Disorders of theOesophagus with MajorCCSpellHRGFZ31ABasetariffShortstayadj.Specialist TopUpExcessbeddaysTotalPriceCoding SourceDisorders of theOesophagus with MajorCCFZ38AFZ16Z£3,235 £2,295£0 £0£0 £0£0 £0£3,235 £2,295Clinical RecordGastrointestinal Bleedwith Major CCVery Major Proceduresfor Gastrointestinal BleedCodingManual orCodingClinicreferenceThe coder had omitted the primary diagnosis. Episode 1 of 2Audit Commission Payment by results data assurance framework 24
Example 2ID Speclty 300 ThemeEpisode Start 19/04/2010 End 20/04/2010TrustCodingAuditCodingError KeyPDiag K20X Oesophagitis K921 Melaena PDODiag1 B378 Candidiasis - Candidiasis K20X Oesophagitisof other sitesDiag2 K259 Gastric ulcer - Gastriculcer, unspecified asacute or chronic, withouthaemorrhage orperforationB378 Candidiasis - Candidiasisof other sitesDiag3 I259 Chronic ischaemic heartdisease - Chronicischaemic heart disease,unspecifiedDiag4 I10X Essential (primary)hypertensionDiag5 J449 Other chronic obstructivepulmonary disease -Chronic obstructivepulmonary disease,unspecifiedI259I10XJ449Chronic ischaemic heartdisease - Chronicischaemic heart disease,unspecifiedEssential (primary)hypertensionOther chronic obstructivepulmonary disease -Chronic obstructivepulmonary disease,unspecifiedDiag6 K259 Gastric ulcer - Gastriculcer, unspecified asacute or chronic, withouthaemorrhage orperforationProc1 G451 Fibreoptic endoscopicexamination of uppergastrointestinal tract andbiopsy of lesion of uppergastrointestinal tractG451Proc2 Z272 Stomach Z272 StomachHRG FZ31A Disorders of theOesophagus with MajorCCFZ16ZSpellHRGFZ31ABasetariffShortstayadj.Specialist TopUpExcessbeddaysTotalPriceCoding SourceDisorders of theOesophagus with MajorCCFZ16Z£3,235 £2,295£0 £0£0 £0£0 £0£3,235 £2,295Clinical RecordFibreoptic endoscopicexamination of uppergastrointestinal tract andbiopsy of lesion of uppergastrointestinal tractVery Major Proceduresfor Gastrointestinal BleedVery Major Proceduresfor Gastrointestinal BleedCodingManual orCodingClinicreferenceThe coder had omitted the primary diagnosis. Episode 2 of 2Audit Commission Payment by results data assurance framework 25
Example 3ID Speclty 300 ThemeEpisode Start 06/04/2010 End 10/04/2010TrustCodingAuditCodingError KeyPDiag A419 Other septicaemia -Septicaemia, unspecifiedDiag1 N390 Urinary tract infection,site not specifiedDiag2 D479 Other neoplasms ofuncertain or unknownbehaviour of lymphoid,haematopoietic andrelated tissue - Neoplasmof uncertain or unknownbehaviour of lymphoid,haematopoietic andrelated tissue,unspecifiedDiag3 F019 Vascular dementia -Vascular dementia,unspecifiedDiag4 I48X Atrial fibrillation andflutterDiag5 Z867 Personal history ofdiseases of thecirculatory systemD649 Other anaemias -Anaemia, unspecifiedA419 Other septicaemia -Septicaemia, unspecifiedN390 Urinary tract infection,site not specifiedD479 Other neoplasms ofuncertain or unknownbehaviour of lymphoid,haematopoietic andrelated tissue - Neoplasmof uncertain or unknownbehaviour of lymphoid,haematopoietic andrelated tissue,unspecifiedF019 Vascular dementia -Vascular dementia,unspecifiedI48X Atrial fibrillation andflutterDiag6 Z867 Personal history ofdiseases of thecirculatory systemHRG WA03V Septicaemia with MajorCCSpellHRGWA03VSepticaemia with MajorCCSA09ESA09EOther Red Blood CellDisorders withIntermediate CCOther Red Blood CellDisorders withIntermediate CCPDICodingManual orCodingClinicreferenceBase£3,643 £2,437tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£3,643 £2,437PriceCoding SourceClinical RecordThis patient was admitted with recurrent anaemia and given blood transfusions as an in-patient. The dischargesummary in the casenotes records that the patient deteriorated and this is thought to have been secondary sepsisto a urinary tract infection. The main condition treated was the anaemia. The sepsis and urinary tract infection wasAudit Commission Payment by results data assurance framework 26
only mentioned in the discharge summary.Audit Commission Payment by results data assurance framework 27
Example 4ID Speclty 300 ThemeEpisode Start 07/06/2010 End 08/06/2010TrustCodingAuditCodingError KeyPDiag K769 Other diseases of liver -Liver disease,unspecifiedDiag1 F102 Mental and behaviouraldisorders due to use ofalcohol. DependencesyndromeDiag2 J698 Pneumonitis due to solidsand liquids - Pneumonitisdue to other solids andliquidsDiag3 I259 Chronic ischaemic heartdisease - Chronicischaemic heart disease,unspecifiedDiag4 I10X Essential (primary)hypertensionDiag5 J449 Other chronic obstructivepulmonary disease -Chronic obstructivepulmonary disease,unspecifiedR18X Ascites PDIK709 Alcoholic liver disease -Alcoholic liver disease,unspecifiedF102J698I259I10XMental and behaviouraldisorders due to use ofalcohol. DependencesyndromePneumonitis due to solidsand liquids - Pneumonitisdue to other solids andliquidsChronic ischaemic heartdisease - Chronicischaemic heart disease,unspecifiedEssential (primary)hypertensionDiag6 N180 End-stage renal disease J449 Other chronic obstructivepulmonary disease -Chronic obstructivepulmonary disease,unspecifiedDiag7 N180 End-stage renal diseaseProc1 T462 Drainage of ascites NEC PPIHRG GC06B Liver and PancreaticDisorders category 2 withIntermediate CCSpellHRGGC06BLiver and PancreaticDisorders category 2 withIntermediate CCFZ13A General Abdominal -Diagnostic Procedureswith CCFZ13A General Abdominal -Diagnostic Procedureswith CCSDICodingManual orCodingClinicreferenceBase£2,068 £3,914tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£2,068 £3,914PriceCoding SourceClinical RecordThis patient was admitted with general deterioration and known alcoholic liver disease. Ascites were drained on7/6/10. The electronic patient record only states chronic liver disease and does not mention the ascites or drainage.Episode 1 of 2Audit Commission Payment by results data assurance framework 28
Example 5ID Speclty 300 ThemeEpisode Start 08/06/2010 End 25/06/2010TrustCodingAuditCodingError KeyPDiag K769 Other diseases of liver -Liver disease,unspecifiedDiag1 F102 Mental and behaviouraldisorders due to use ofalcohol. DependencesyndromeDiag2 J698 Pneumonitis due to solidsand liquids - Pneumonitisdue to other solids andliquidsDiag3 I259 Chronic ischaemic heartdisease - Chronicischaemic heart disease,unspecifiedDiag4 I10X Essential (primary)hypertensionDiag5 J449 Other chronic obstructivepulmonary disease -Chronic obstructivepulmonary disease,unspecifiedR18X Ascites PDIK709 Alcoholic liver disease -Alcoholic liver disease,unspecifiedF102J698I259I10XMental and behaviouraldisorders due to use ofalcohol. DependencesyndromePneumonitis due to solidsand liquids - Pneumonitisdue to other solids andliquidsChronic ischaemic heartdisease - Chronicischaemic heart disease,unspecifiedEssential (primary)hypertensionDiag6 N180 End-stage renal disease J449 Other chronic obstructivepulmonary disease -Chronic obstructivepulmonary disease,unspecifiedDiag7 N180 End-stage renal diseaseProc1 T462 Drainage of ascites NEC PPIHRG GC06B Liver and PancreaticDisorders category 2 withIntermediate CCSpellHRGGC06BLiver and PancreaticDisorders category 2 withIntermediate CCFZ13A General Abdominal -Diagnostic Procedureswith CCFZ13A General Abdominal -Diagnostic Procedureswith CCSDICodingManual orCodingClinicreferenceBase£2,068 £3,914tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£2,068 £3,914PriceCoding SourceClinical RecordThis patient was admitted with alcoholic liver disease and ascites were drained under aseptic technique on 9/6/10.This was recorded in the patient casenotes. The primary diagnosis recorded on the electronic patient record wasonly chronic liver disease and the drainage of the ascites was not documented.Episode 2 of 2Audit Commission Payment by results data assurance framework 29
Example 6ID Speclty 300 ThemeEpisode Start 07/04/2010 End 07/04/2010TrustCodingAuditCodingError KeyPDiag R101 Pain localized to upper R074 Chest pain, unspecified PD3abdomenProc1 G459 Diagnostic fibreoptic G169 Diagnostic fibreoptic PP3endoscopic examinationof upper gastrointestinaltract - Unspecifiedendoscopic examinationof oesophagus -UnspecifiedProc2 Z241 Pharynx Z271 OesophagusHRG FZ03A Diagnostic andintermediate procedureson the upper GI tract 19years and overCZ02Y Intermediate MouthProcedures 19 years andover without CCSpellHRGFZ03ABasetariffShortstayadj.Specialist TopUpExcessbeddaysTotalPriceCoding SourceDiagnostic andintermediate procedureson the upper GI tract 19years and overCZ02Y£441 £644£0 £0£0 £0£0 £0£441 £644Clinical RecordIntermediate MouthProcedures 19 years andover without CCCodingManual orCodingClinicreferenceThe endoscopy sheet clearly stated the problem was chest pain not abdominal. The procedure only progressed tothe Oesophagus which was also clearly documented.Audit Commission Payment by results data assurance framework 30
Example 7ID Speclty 300 ThemeEpisode Start 08/04/2010 End 09/04/2010TrustCodingAuditCodingError KeyPDiag T432 Poisoning bypsychotropic drugs, NEC- Other and unspecifiedantidepressantsDiag1 X619 Intentional self-poisoningby and exposure toantiepileptic, sedativehypnotic,antiparkinsonism andpsychotropic drugs, notelsewhere classified -Occurrence atT432X619Poisoning bypsychotropic drugs, NEC- Other and unspecifiedantidepressantsIntentional self-poisoningby and exposure toantiepileptic, sedativehypnotic,antiparkinsonism andpsychotropic drugs, notelsewhere classified -Occurrence atunspecified placeunspecified placeDiag2 F319 Bipolar affective disorder- Bipolar affectivedisorder, unspecifiedDiag3 Z915 Personal history of selfharmSDIDiag4 Z720 Tobacco use SDIHRG WA11Y Poisoning, toxic,environmental andunspecified effectswithout CCWA11X Poisoning, toxic,environmental andunspecified effects withIntermediate CCSpellHRGWA11YPoisoning, toxic,environmental andunspecified effectswithout CCWA11XPoisoning, toxic,environmental andunspecified effects withIntermediate CCSDICodingManual orCodingClinicreferenceCodingClinicMarch2010Base£366 £594tariffShort£0 £178stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£366 £416PriceCoding SourceClinical RecordThe co-morbidities for bipolar depression and smoking have been added. These should always be recorded as perlist in Coding Clinic dated March 2010. The patient has a history of self harm which is also relevant to this episode.This information was in the patient casenotes but not on the electronic patient record.Audit Commission Payment by results data assurance framework 31
Analysis of errors – General Medicine:All the acronyms in this table are defined in appendix 8 – error keys.Overall Number %Total Number of 100episodes examinedUTA Unsafe to audit 0Financial value of 0UTA episodes (spelllevel)Actual number of 100episodes examinedNumber of spells this 52representsNumber of episodes 7 7.00where HRG wouldchange as a result ofAuditor's coding.Number of spellswhere HRG wouldchange as a result ofAuditor's coding.5 9.62Primary Diagnosis Number of primary 88 88.00diagnoses correctNon Coder ErrorPDI 3 3.00Coder ErrorPD3 1 1.00PD4 3 3.00PD5 3 3.00PDO 2 2.00Secondary Diagnosis Number of secondary 296diagnosesNumber of secondarydiagnoses correct269 90.88Non Coder ErrorSDI 12 4.05Coder ErrorSD3 4 1.35SDO 11 3.72ECNR 10Primary ProceduresNumber of primaryproceduresNumber of primaryprocedures correct3430 88.24Non Coder ErrorPPI 2 5.88Coder ErrorPP3 2 5.88SecondaryProceduresNumber of secondaryproceduresNumber of secondaryprocedures correct99 100.00Non Coder ErrorCoder ErrorAdditional Fields Number %Pre-audit sample £79,712pricePost-audit sample £79,665pricePrice of gross £4,245 5.33Audit Commission Payment by results data assurance framework 32
changePrice of net change -£47 -0.06Number of spells in 0 0.00pre-audit sampleoutside of PbRPost-audit price of 0 0.00these spellsNumber of spells in 0 0.00post-audit sampleoutside of PbRPre-audit price ofthese spells.0 0.00Audit Commission Payment by results data assurance framework 33
Appendix 4 – Specialty B - Cardiology70 At The <strong>Royal</strong> <strong>Bournemouth</strong> and Christchurch <strong>Hospital</strong>s NHSFoundation Trust the follow up area covered was Cardiology which wasaudited in 2007/08. This audit was at a specialty level, covering all HRGs /chapters. A sample of 100 cases was provided for audit and none werefound to be unsafe to audit as per NHS CFH standards.Table 11: Specialty B area: coding errorsTotalfromepisodesauditedIncorrectCoderErrorNoncodererrorTotalincorrect% incorrect2009/10 2007/08Primary 100 1 1 2 2.0 10.0diagnosisSecondary 327 2 22 24 7.3 30.7diagnosisPrimary 79 2 0 2 2.5 14.4procedureSecondary 118 0 0 0 0.0 11.6procedureOverall 624 5 23 28 4.5 18.4Table 12: Specialty B area: HRG errorsEpisodesSpellsTotal 100 80Total changing HRG 10 10% changing HRG 10.0 12.5Analysis of coding errors71 The audit identified 28 (4.5 per cent) errors in procedure and diagnosescoding, leading to 10 HRG changes. To enable an accurate HRG levelcomparison between the 2007/08 and 2010/11 audits we have regroupedthe 2007/08 audit data to HRG4. The HRG error rate was 3 per cent in2007/08 if HRG4 was in use in 2007/08 and it would show that HRG codinghas not improved. It is important to note that different OPCS versions mayhave been in use at the time of the audits. This can have an impact on theoverall HRG error rate. The impact of the 10 HRG changes was that theTrust was overcharging its commissioners by £4,699 on the sample tested.Audit Commission Payment by results data assurance framework 34
72 The following areas for improvement have been identified:■ removal of the policy regarding the use of a secondary procedure codefor angiograms when an angioplasty is undertaken. These are codeddue to clinical staff insisting these codes are added when an angiogramis done at the same time as an angioplasty. This is against the codingrule when diagnostic and therapeutic procedures are carried out on thesame site at the same theatre visit on the same body site, only thetherapeutic procedure should be recorded. This was the cause of all ofthe HRG changes within Cardiology; and■ documenting the specific type of image control within the casenotes andthe EPR. The coding of Cardiology procedures could be more specific ifthis information is available to the coder.73 There were 23 non-coder errors due to the source document notholding all the relevant information for the coder at the time/point ofcoding this affected one primary and 22 secondary diagnoses. The noncoder errors accounted for 82.1 per cent of the total number of errors inthis area.74 The coder errors were in the following areas:■■incorrect sequencing where the diagnosis or procedure was identifiedbut not coded in the correct order - affecting one primary and twosecondary procedures; andomission of diagnosis and procedures – affecting two secondarydiagnoses.75 There are 11 instances when information not relevant to the episode ofcare has been coded. NHS CFH does not treat this as an error but werethey to have been included they would have accounted for all 10 of the HRGchanges. These are all due to clinical input requesting Angiograms arecoded alongside an Angioplasty procedure. This does not comply withnational standards as diagnostic procedures should not be coded when atherapeutic procedure is undertaken at the same time and on the same site.The Trust should seek to code only relevant information.Follow up of audit in this area from 2007/0876 Cardiology was audited in 2007/08 and was selected as an area forfollow up. To enable an accurate HRG level comparison between the2007/08 and 2010/11 audits we have regrouped the 2007/08 audit data toHRG4. This is what the error rate would have been if HRG4 was in use in2007/08 and shows that HRG coding has improved compared to 2007/08when this area was originally audited. It is important to note that differentOPCS versions may have been in use at the time of the audits. This canhave an impact on the overall HRG error rate.Audit Commission Payment by results data assurance framework 35
Table 13: Follow up of HRG changesEpisodes2010/11 2007/08 ChangeTotal 100 100 -Total changingHRG 10 3 7% changing HRG 10.0% 3.0% 777 The coding error rate has improved since 2007/08 however the HRGrate has deteriorated. This is due to the policy at the Trust regarding theuse of a secondary procedure code for angiograms when an angioplasty isundertaken as this accounted for all of the HRG changes in this area.Financial impact of errorsTable 14: Specialty B area: financial impact of errorsPre AuditPaymentPost AuditPaymentGrossChange% GrossChangeNetChange£201,825 £197,126 £4,699 2.3 -£4,699 -2.3% NetChange78 The sample of spells audited covered £201,825 of activity. The totalvalue of all errors regardless of who they favoured (gross change) was£4,699 (2.3 per cent of total sample tested). If the episodes and thereforespells had been coded according to the auditor coding, the impact wouldhave been a decrease in income (net change) due to the Trust from itscommissioners of £4,699 or 2.3 per cent of payments tested.Data Issues79 There were no data issues identified within the Specialty B area.Audit Commission Payment by results data assurance framework 36
HRGs and price changes as a result of the audit (Cardiology)Example 1ID Speclty 320 SpecialtyEpisode Start 20/05/2010 End 20/05/2010TrustCodingAuditCodingError KeyPDiag I251 Atherosclerotic heartdiseaseDiag1 I209 Angina pectoris - Anginapectoris, unspecifiedProc1 K752 Percutaneoustransluminal balloonangioplasty and insertionof 3 or more drug-elutingstents into coronaryarteryProc2 K632 Angiocardiography ofright side of heart NECProc3 Y539 Approach to organ underimage control -UnspecifiedProc4 Y703 First stage of stagedoperations NOCHRG EA34Z Percutaneous CoronaryInterventions with 3 ormore Stents andCatheterisationSpellHRGEA34ZPercutaneous CoronaryInterventions with 3 ormore Stents andCatheterisationI251I209K752Y539Y703EA33ZEA33ZAtherosclerotic heartdiseaseAngina pectoris - Anginapectoris, unspecifiedPercutaneoustransluminal balloonangioplasty and insertionof 3 or more drug-elutingstents into coronaryarteryApproach to organ underimage control -UnspecifiedFirst stage of stagedoperations NOCPercutaneous CoronaryInterventions with 3 ormore StentsPercutaneous CoronaryInterventions with 3 ormore StentsSPNRCodingManual orCodingClinicreferenceOPCSinstructionManualPage E-6Base£4,565 £3,756tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£4,565 £3,756PriceCoding SourceClinical RecordIt is a Trust Consultant policy always to record the angiogram carried out at the same time. There is a coding rulenot to record a diagnostic procedure as well as a therapeutic procedure.Audit Commission Payment by results data assurance framework 37
Example 2ID Speclty 320 SpecialtyEpisode Start 26/05/2010 End 26/05/2010TrustCodingAuditCodingError KeyPDiag I258 Chronic ischaemic heartdisease - Other forms ofchronic ischaemic heartdiseaseDiag1 I209 Angina pectoris - Anginapectoris, unspecifiedDiag2 Z955 Presence of coronaryangioplasty implant andgraftI258I209Z955Chronic ischaemic heartdisease - Other forms ofchronic ischaemic heartdiseaseAngina pectoris - Anginapectoris, unspecifiedPresence of coronaryangioplasty implant andgraftDiag3 Z720 Tobacco use Z720 Tobacco useProc1 K751 Percutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryK751Proc2 K631 Angiocardiography ofcombination of right andleft side of heartProc3 Y539 Approach to organ underimage control -UnspecifiedHRG EA32Z Percutaneous CoronaryIntervention (0-2 stents)SpellHRGEA32Zand CatheterisationPercutaneous CoronaryIntervention (0-2 stents)and CatheterisationY539EA31ZEA31ZPercutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryApproach to organ underimage control -UnspecifiedPercutaneous CoronaryIntervention (0-2 Stents)Percutaneous CoronaryIntervention (0-2 Stents)SPNRCodingManual orCodingClinicreferenceOPCSinstructionManualPage E-6Base£3,756 £3,306tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£3,756 £3,306PriceCoding SourceClinical RecordThere is a Trust policy always to record the angiogram when carried out at the same time.There is no need torecord the angiocardiography under the therapeutic versus diagnostic procedure rule.Audit Commission Payment by results data assurance framework 38
Example 3ID Speclty 320 SpecialtyEpisode Start 05/05/2010 End 08/05/2010TrustCodingAuditCodingError KeyPDiag I200 Unstable angina I200 Unstable anginaDiag1 I258 Chronic ischaemic heartdisease - Other forms ofchronic ischaemic heartdiseaseI258 Chronic ischaemic heartdisease - Other forms ofchronic ischaemic heartdiseaseDiag2 I10X Essential (primary) I10X Essential (primary)hypertensionDiag3 Z955 Presence of coronaryangioplasty implant andgraftDiag4 E119 Non-insulin-dependentdiabetes mellitus - Noninsulin-dependentdiabetes mellitus withoutcomplicationsDiag5 E785 Hyperlipidaemia,unspecifiedDiag6 E669 Obesity - Obesity,unspecifiedProc1 K751 Percutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryProc2 K631 Angiocardiography ofcombination of right andleft side of heartProc3 Y539 Approach to organ underimage control -UnspecifiedHRG EA32Z Percutaneous CoronaryIntervention (0-2 stents)SpellHRGEA32ZBasetariffShortstayadj.Specialist TopUpExcessbeddaysTotalPriceCoding Sourceand CatheterisationPercutaneous CoronaryIntervention (0-2 stents)and CatheterisationZ955E119E785E669K751Y539EA31ZEA31Z£4,949 £4,428£0 £0£0 £0£0 £0£4,949 £4,428Clinical RecordhypertensionPresence of coronaryangioplasty implant andgraftNon-insulin-dependentdiabetes mellitus - Noninsulin-dependentdiabetes mellitus withoutcomplicationsHyperlipidaemia,unspecifiedObesity - Obesity,unspecifiedPercutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryApproach to organ underimage control -UnspecifiedPercutaneous CoronaryIntervention (0-2 Stents)Percutaneous CoronaryIntervention (0-2 Stents)SPNRCodingManual orCodingClinicreferenceOPCSinstructionManualPage E-6It is incorrect to record an angiogram with an angioplasty. The clinician has instructed the coders to add thesecodes.Audit Commission Payment by results data assurance framework 39
Example 4ID Speclty 320 SpecialtyEpisode Start 24/05/2010 End 24/05/2010TrustCodingAuditCodingError KeyPDiag I251 Atherosclerotic heartdiseaseDiag1 I209 Angina pectoris - Anginapectoris, unspecifiedDiag2 I352 Aortic (valve) stenosiswith insufficiencyDiag3 I739 Other peripheral vasculardiseases - Peripheralvascular disease,unspecifiedProc1 K751 Percutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryProc2 K631 Angiocardiography ofcombination of right andleft side of heartProc3 Y539 Approach to organ underimage control -UnspecifiedHRG EA32Z Percutaneous CoronaryIntervention (0-2 stents)SpellHRGEA32Zand CatheterisationPercutaneous CoronaryIntervention (0-2 stents)and CatheterisationI251I209I352I739K751Y539EA31ZEA31ZAtherosclerotic heartdiseaseAngina pectoris - Anginapectoris, unspecifiedAortic (valve) stenosiswith insufficiencyOther peripheral vasculardiseases - Peripheralvascular disease,unspecifiedPercutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryApproach to organ underimage control -UnspecifiedPercutaneous CoronaryIntervention (0-2 Stents)Percutaneous CoronaryIntervention (0-2 Stents)SPNRCodingManual orCodingClinicreferenceOPCSinstructionManualPage E-6Base£3,756 £3,306tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£3,756 £3,306PriceCoding SourceClinical RecordThere is a consultant Trust rule to always code angiograms when done at the same time. There is no need torecord an angiocardiography under the diagnositic versus therapeutic rule.Audit Commission Payment by results data assurance framework 40
Example 5ID Speclty 320 SpecialtyEpisode Start 01/06/2010 End 01/06/2010TrustCodingAuditCodingError KeyPDiag I251 Atherosclerotic heartdiseaseI251 Atherosclerotic heartdiseaseDiag1 I209 Angina pectoris - Anginapectoris, unspecifiedI209 Angina pectoris - Anginapectoris, unspecifiedDiag2 I48X Atrial fibrillation andflutterI48X Atrial fibrillation andflutterDiag3 I714 Abdominal aorticaneurysm, withoutmention of ruptureI714 Abdominal aorticaneurysm, withoutmention of ruptureDiag4 F03X Unspecified dementia F03X Unspecified dementiaProc1 K751 Percutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryK751 Percutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryProc2 K633 Angiocardiography of leftside of heart NECProc3 Y539 Approach to organ underimage control -UnspecifiedHRG EA32Z Percutaneous CoronaryIntervention (0-2 stents)SpellHRGEA32Zand CatheterisationPercutaneous CoronaryIntervention (0-2 stents)and CatheterisationY539EA31ZEA31ZApproach to organ underimage control -UnspecifiedPercutaneous CoronaryIntervention (0-2 Stents)Percutaneous CoronaryIntervention (0-2 Stents)SPNRCodingManual orCodingClinicreferenceOPCSinstructionManualPage E-6Base£3,756 £3,306tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£3,756 £3,306PriceCoding SourceClinical RecordThe Trust have a consultant signed policy to include the code for Angiogram. Coding diagnostic vs therapeuticrules confirms this is not necessary.Audit Commission Payment by results data assurance framework 41
Example 6ID Speclty 320 SpecialtyEpisode Start 16/06/2010 End 16/06/2010TrustCodingAuditCodingError KeyPDiag I251 Atherosclerotic heartdiseaseDiag1 I209 Angina pectoris - Anginapectoris, unspecifiedProc1 K751 Percutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryProc2 K631 Angiocardiography ofcombination of right andleft side of heartProc3 Y539 Approach to organ underimage control -UnspecifiedHRG EA32Z Percutaneous CoronaryIntervention (0-2 stents)SpellHRGEA32Zand CatheterisationPercutaneous CoronaryIntervention (0-2 stents)and CatheterisationI251I209K751Y539EA31ZEA31ZAtherosclerotic heartdiseaseAngina pectoris - Anginapectoris, unspecifiedPercutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryApproach to organ underimage control -UnspecifiedPercutaneous CoronaryIntervention (0-2 Stents)Percutaneous CoronaryIntervention (0-2 Stents)SPNRCodingManual orCodingClinicreferenceOPCSinstructionManualPage E-6Base£3,756 £3,306tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£3,756 £3,306PriceCoding SourceClinical RecordThere is a trust rule always to record the angiogram when done at the same time. This procedure does not need tobe recorded when carried out at the same time as an angioplasty under the diagnostic versus therapeutic rule.Audit Commission Payment by results data assurance framework 42
Example 7ID Speclty 320 SpecialtyEpisode Start 13/05/2010 End 17/05/2010TrustCodingAuditCodingError KeyPDiag I258 Chronic ischaemic heartdisease - Other forms ofchronic ischaemic heartdiseaseDiag1 I254 Coronary arteryaneurysmDiag2 T818 Complications ofprocedures, NEC - Othercomplications ofprocedures, NECDiag3 T810 Complications ofprocedures, NEC -Haemorrhage andhaematoma complicatinga procedure, NECDiag4 Z955 Presence of coronaryangioplasty implant andgraftDiag5 E119 Non-insulin-dependentdiabetes mellitus - Noninsulin-dependentdiabetes mellitus withoutcomplicationsDiag6 J449 Other chronic obstructivepulmonary disease -Chronic obstructivepulmonary disease,unspecifiedDiag7 Z864 Personal history ofpsychoactive substanceabuseProc1 K752 Percutaneoustransluminal balloonangioplasty and insertionof 3 or more drug-elutingstents into coronaryarteryProc2 K633 Angiocardiography of leftside of heart NECProc3 Y539 Approach to organ underimage control -UnspecifiedProc4 Y711 Subsequent stage ofstaged operations NOCHRG EA34Z Percutaneous CoronaryInterventions with 3 ormore Stents andCatheterisationSpellHRGBasetariffEA34ZPercutaneous CoronaryInterventions with 3 ormore Stents andCatheterisationI258I254T818T810Z955E119J449Z864K752Y539Y711EA33ZEA33Z£4,565 £3,756Chronic ischaemic heartdisease - Other forms ofchronic ischaemic heartdiseaseCoronary arteryaneurysmComplications ofprocedures, NEC - Othercomplications ofprocedures, NECComplications ofprocedures, NEC -Haemorrhage andhaematoma complicatinga procedure, NECPresence of coronaryangioplasty implant andgraftNon-insulin-dependentdiabetes mellitus - Noninsulin-dependentdiabetes mellitus withoutcomplicationsOther chronic obstructivepulmonary disease -Chronic obstructivepulmonary disease,unspecifiedPersonal history ofpsychoactive substanceabusePercutaneoustransluminal balloonangioplasty and insertionof 3 or more drug-elutingstents into coronaryarteryApproach to organ underimage control -UnspecifiedSubsequent stage ofstaged operations NOCPercutaneous CoronaryInterventions with 3 ormore StentsPercutaneous CoronaryInterventions with 3 ormore StentsSPNRCodingManual orCodingClinicreferenceOPCSinstructionManualPage E-6Audit Commission Payment by results data assurance framework 43
Short£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £732beddaysTotal£4,565 £4,488PriceCoding SourceClinical RecordNo need to record angiocardiography as per therapeutic versus diagnostic rule.Audit Commission Payment by results data assurance framework 44
Example 8ID Speclty 320 SpecialtyEpisode Start 09/06/2010 End 10/06/2010TrustCodingAuditCodingError KeyPDiag I251 Atherosclerotic heartdiseaseDiag1 I209 Angina pectoris - Anginapectoris, unspecifiedDiag2 I10X Essential (primary)hypertensionDiag3 Z824 Family history ofischaemic heart diseaseand other diseases of thecirculatory systemDiag4 T812 Complications ofprocedures, NEC -Accidental puncture andlaceration during aprocedure, NECProc1 K751 Percutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryProc2 K631 Angiocardiography ofcombination of right andleft side of heartProc3 Y539 Approach to organ underimage control -UnspecifiedProc4 Y703 First stage of stagedoperations NOCHRG EA32Z Percutaneous CoronaryIntervention (0-2 stents)and CatheterisationSpellHRGEA32ZPercutaneous CoronaryIntervention (0-2 stents)and CatheterisationI251I209I10XZ824T812K751Y539Y703EA31ZEA31ZAtherosclerotic heartdiseaseAngina pectoris - Anginapectoris, unspecifiedEssential (primary)hypertensionFamily history ofischaemic heart diseaseand other diseases of thecirculatory systemComplications ofprocedures, NEC -Accidental puncture andlaceration during aprocedure, NECPercutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryApproach to organ underimage control -UnspecifiedFirst stage of stagedoperations NOCPercutaneous CoronaryIntervention (0-2 Stents)Percutaneous CoronaryIntervention (0-2 Stents)SPNRBase£3,756 £3,306tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£3,756 £3,306PriceCoding SourceClinical RecordThere is a Trust rule to code angiograms. No need to record angiocardiography under diagnostic versustherapeutic ruleCodingManual orCodingClinicreferenceOPCSinstructionManualPage E-6Audit Commission Payment by results data assurance framework 45
Example 9ID Speclty 320 SpecialtyEpisode Start 10/05/2010 End 15/05/2010TrustCodingAuditCodingError KeyPDiag I200 Unstable angina I251 Atherosclerotic heartdiseaseDiag1 I251 Atherosclerotic heart I200 Unstable anginadiseaseDiag2 J841 Other interstitialJ841 Other interstitialpulmonary diseases withpulmonary diseases withfibrosisfibrosisProc1 K751 Percutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryProc2 K631 Angiocardiography ofcombination of right andleft side of heartProc3 Y539 Approach to organ underimage control -UnspecifiedHRG EA32Z Percutaneous CoronaryIntervention (0-2 stents)SpellHRGEA32Zand CatheterisationPercutaneous CoronaryIntervention (0-2 stents)and CatheterisationK751Y539EA31ZEA31ZPercutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryApproach to organ underimage control -UnspecifiedPercutaneous CoronaryIntervention (0-2 Stents)Percutaneous CoronaryIntervention (0-2 Stents)PDISSPNRCodingManual orCodingClinicreferenceOPCSinstructionManualPage E-6Base£4,949 £4,428tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£4,949 £4,428PriceCoding SourceClinical RecordThe auditor has recorded the heart disease in first place as the patient is being treated for this. There is no need torecord the angiocardiography under the therapeutic versus diagnostic rule.Audit Commission Payment by results data assurance framework 46
Example 10ID Speclty 320 SpecialtyEpisode Start 30/04/2010 End 02/05/2010TrustCodingAuditCodingError KeyPDiag I211 Acute transmuralmyocardial infarction ofinferior wallDiag1 I251 Atherosclerotic heartdiseaseDiag2 E780 PurehypercholesterolaemiaI211I251E780Acute transmuralmyocardial infarction ofinferior wallAtherosclerotic heartdiseasePurehypercholesterolaemiaDiag3 Z720 Tobacco use Z720 Tobacco useDiag4 L309 Other dermatitis -Dermatitis, unspecifiedL309 Other dermatitis -Dermatitis, unspecifiedProc1 K751 Percutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryK751 Percutaneoustransluminal balloonangioplasty and insertionof 1-2 drug-eluting stentsinto coronary arteryProc2 K631 Angiocardiography ofcombination of right andleft side of heartProc3 Y539 Approach to organ underimage control -UnspecifiedProc4 U201 TransthoracicechocardiographyHRG EA32Z Percutaneous CoronaryIntervention (0-2 stents)and CatheterisationSpellHRGEA32ZPercutaneous CoronaryIntervention (0-2 stents)and CatheterisationY539U201EA31ZEA31ZApproach to organ underimage control -UnspecifiedTransthoracicechocardiographyPercutaneous CoronaryIntervention (0-2 Stents)Percutaneous CoronaryIntervention (0-2 Stents)SPNRCodingManual orCodingClinicreferenceOPCSinstructionManualPage E-6Base£4,949 £4,428tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£4,949 £4,428PriceCoding SourceClinical RecordThere is no need to record the angiocardiography. Rationale: Diagnostic versus therapeutic rule if a therapeuticprocedure is done at the same time and on the same site as a diagnostic procedure there is no need to code thediagnostic procedure as well. See Clinical Coding Instruction Manual OPCS-4 page E-6Audit Commission Payment by results data assurance framework 47
Analysis of errors – Cardiology:All the acronyms in this table are defined in appendix 8 – error keys.Overall Number %Total Number of 100episodes examinedUTA Unsafe to audit 0Financial value of 0UTA episodes (spelllevel)Actual number of 100episodes examinedNumber of spells this 80representsNumber of episodes 10 10.00where HRG wouldchange as a result ofAuditor's coding.Number of spellswhere HRG wouldchange as a result ofAuditor's coding.10 12.50Primary Diagnosis Number of primary 98 98.00diagnoses correctNon Coder ErrorPDI 1 1.00Coder ErrorPDIS 1 1.00Secondary Diagnosis Number of secondary 327diagnosesNumber of secondarydiagnoses correct303 92.66Non Coder ErrorSDI 22 6.73Coder ErrorSDNR 1SDO 2 0.61Primary ProceduresNumber of primaryproceduresNumber of primaryprocedures correct7977 97.47Non Coder ErrorCoder ErrorPPIS 2 2.53SecondaryProceduresNumber of secondaryproceduresNumber of secondaryprocedures correct118118 100.00Non Coder ErrorCoder ErrorSPNR 10Additional Fields Number %Pre-audit sample £201,825pricePost-audit sample £197,126pricePrice of gross £4,699 2.33changePrice of net change -£4,699 -2.33Number of spells in 0 0.00Audit Commission Payment by results data assurance framework 48
pre-audit sampleoutside of PbRPost-audit price ofthese spellsNumber of spells inpost-audit sampleoutside of PbRPre-audit price ofthese spells.0 0.000 0.000 0.00Audit Commission Payment by results data assurance framework 49
Appendix 5 – Chapter - JC Skin Surgery80 The appendix gives a detailed breakdown of the clinical coding auditfindings in the specific area audited. It is designed as a technical report forthe clinical coding department at the Trust audited. However PCTs will findthe data useful in understanding the cause of the HRG assignment errorsand the coding errors.81 At the set up meeting the Trust and PCT agreed to audit chapter JC -Skin Surgery as suggested in the benchmarking report. A sample of 70cases was provided for audit and no episodes were found unsafe to auditper NHS CFH standards.Table 15: Chapter area: coding errorsTotal fromepisodesauditedIncorrectCoderErrorNon codererrorTotalincorrect%incorrectPrimary 70 4 5 9 12.9diagnosisSecondary 50 18 3 21 42.0diagnosisPrimary 70 12 0 12 17.1procedureSecondary 39 5 0 5 12.8procedureOverall 229 39 8 47 20.5Table 16: Chapter area: HRG errorsEpisodesSpellsTotal 70 70Total changing HRG 13 13% changing HRG 18.6 18.6Analysis of coding errors82 The audit identified 47 (20.5 per cent) errors in procedure anddiagnoses coding, leading to 13 HRG changes. The impact of the 13 HRGchanges was that the Trust was undercharging its commissioners by £4,594on the sample tested.83 The following areas for improvement has been identified:Audit Commission Payment by results data assurance framework 50
■■provide training to the coders covering how skin procedures should becoded, as these can be coded in two ways depending on the site of thebody that has been operated on. The coder had not reflected thedifferent site of procedures within the codes allocated and continued touse only codes from chapter ‘S’ when sometimes the correct codesshould be from other specific chapters. For example skin operation onthe ear should be coded using a code from chapter ‘D’ with a code fromchapter ‘S’ to enhance this. All coders must have this rule re-enforced toensure these are coded correctly; andreinforcing the importance of recording the mandatory co-morbiditiesfrom the March 2010 Coding Clinic, as omission of secondarydiagnoses was an issue from both the coder and clinical perspective.84 There were eight non-coder errors due to the source document notholding all the relevant information for the coder at the time/point of codingaffecting five primary and three secondary diagnoses.85 The coder errors were in the following areas:■ incorrect coding at the required 3-, 4- and 5- character level affectingfour primary and one secondary diagnosis, three primary and twosecondary procedures; and■ omission of diagnosis and procedures – affecting 17 secondarydiagnoses, nine primary and three secondary procedures.Financial impact of errorsTable 16 Chapter area: financial impact of errorsPre AuditPaymentPost AuditPaymentGrossChange% GrossChangeNetChange£46,626 £51,220 £4,594 9.9 £4,594 9.9% NetChange86 The sample of spells audited covered £46,626 of activity. The totalvalue of all errors regardless of who they favoured (gross change) was£4,594 (9.9 per cent of total sample tested). If the episodes and thereforespells had been coded according to the auditor coding, the impact wouldhave been an increase in income (net change) due to the Trust from itscommissioners of £4,594 or 9.9 per cent of payments tested.Data Issues87 There were no data issues identified within the chapter area.Audit Commission Payment by results data assurance framework 51
HRGs and price changes as a result of the audit (Chapter JC - SkinSurgery)Example 1ID Speclty 330 SubchapterEpisode Start 12/05/2010 End 12/05/2010TrustCodingAuditCodingError KeyPDiag L82X Seborrhoeic keratosis L82X Seborrhoeic keratosisProc1 S082 Curettage andcauterisation of lesion ofskin NECE092 Destruction of lesion ofexternal nose NECProc2 Z221 External nose S082 Curettage andcauterisation of lesion ofskin NECHRG JC15Z Skin Therapies level 3 CZ12Y Minor Nose Procedures19 years and overwithout CCSpellHRGJC15Z Skin Therapies level 3 CZ12Y Minor Nose Procedures19 years and overwithout CCCodingManual orCodingClinicreferencePPO OPCS 4.5instructionmanualPage S-5Base£635 £644tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£635 £644PriceCoding SourceClinical RecordThe coder should have selected a code from chapter E and there are specific codes for external nose then addedthe S code for more information.Audit Commission Payment by results data assurance framework 52
Example 2ID Speclty 330 SubchapterEpisode Start 25/06/2010 End 25/06/2010TrustAuditError KeyCodingPDiag C444 Other malignantneoplasms of skin - Skinof scalp and neckCodingC444Other malignantneoplasms of skin - Skinof scalp and neckDiag1 I10X Essential (primary)hypertensionProc1 S069 Other excision of lesion S069 Other excision of lesionof skin - Unspecifiedof skin - UnspecifiedProc2 Z481 Skin of scalp S369 Other autograft of skin -UnspecifiedProc3 Z481 Skin of scalpHRG JC15Z Skin Therapies level 3 JC05B Minor Skin Procedurescategory 3 withIntermediate CCSpellHRGJC15Z Skin Therapies level 3 JC05B Minor Skin Procedurescategory 3 withIntermediate CCSDOSPOCodingManual orCodingClinicreferenceBase£635 £1,533tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£635 £1,533PriceCoding SourceClinical RecordThe procedure carried out was an excision of lesion and graft repair. Hypertension was recorded on the dischargesummary in the casenotes. This is a mandatory co-morbidity as per list in the Coding Clinic March 2010.Audit Commission Payment by results data assurance framework 53
Example 3ID Speclty 330 SubchapterEpisode Start 30/04/2010 End 30/04/2010TrustAuditError KeyCodingPDiag C440 Other malignantneoplasms of skin - Skinof lipDiag1 I10X Essential (primary)hypertensionProc1 S069 Other excision of lesionof skin - UnspecifiedCodingC440I10XOther malignantneoplasms of skin - Skinof lipEssential (primary)CodingManual orCodingClinicreferencehypertensionF021 Excision of lesion of lip PP3 OPCS 4.5instructionmanualPage S-5Proc2 Z251 LipHRG JC15Z Skin Therapies level 3 CZ02X Intermediate MouthProcedures 19 years andover with IntermediateCCSpellHRGJC15Z Skin Therapies level 3 CZ02X Intermediate MouthProcedures 19 years andover with IntermediateCCBase£635 £788tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£635 £788PriceCoding SourceClinical RecordThere is an exclusion note at the beginning of Chapter S in OPCS-4 that codes from this chapter should not beused for certain sites including the site for lip. A code from chapter F should be used.Audit Commission Payment by results data assurance framework 54
Example 4ID Speclty 100 SubchapterEpisode Start 04/05/2010 End 04/05/2010TrustAuditError KeyCodingPDiag L918 Hypertrophic disorders ofskin - Other hypertrophicdisorders of skinProc1 S069 Other excision of lesionof skin - UnspecifiedCodingD24XB353Benign neoplasm ofbreast - Benign neoplasmof breastExtirpation of lesion ofnippleProc2 Z156 Nipple S069 Other excision of lesionof skin - UnspecifiedProc3 Z943 Left sided operation Z943 Left sided operationHRG JC15Z Skin Therapies level 3 JA11C Minor Breast Procedurescategory 1 without CCSpellHRGJC15Z Skin Therapies level 3 JA11C Minor Breast Procedurescategory 1 without CCBase£635 £847tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotalPrice£635 £847PDICodingManual orCodingClinicreferencePPO OPCS 4.5instructionmanualPage S-5Coding SourceClinical RecordThere is an exclusion note at the beginning of Chapter S in OPCS-4 that codes from this chapter should not beused for certain sites including the site for nipple. A code from chapter B should be used.Audit Commission Payment by results data assurance framework 55
Example 5ID Speclty 330 SubchapterEpisode Start 21/04/2010 End 21/04/2010TrustAuditError KeyCodingPDiag C442 Other malignantneoplasms of skin - Skinof ear and externalauricular canalProc1 S068 Other excision of lesionof skin - Other specifiedCodingC442D021Other malignantneoplasms of skin - Skinof ear and externalauricular canalExcision of lesion ofexternal earProc2 Z201 External ear S065 Excision of lesion of skinof head or neck NECProc3 Z943 Left sided operation Z943 Left sided operationHRG JC15Z Skin Therapies level 3 CZ08Y Minor Ear Procedures 19years and over withoutCCSpellHRGJC15Z Skin Therapies level 3 CZ08Y Minor Ear Procedures 19years and over withoutCCCodingManual orCodingClinicreferencePPO OPCS 4.5instructionmanualPage S-5Base£635 £680tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£635 £680PriceCoding SourceClinical RecordThere is an exclusion note at the beginning of Chapter S in OPCS-4 that codes from this chapter should not beused for certain sites including the site for Ear. A code from chapter D should be used.Audit Commission Payment by results data assurance framework 56
Example 6ID Speclty 330 SubchapterEpisode Start 28/04/2010 End 28/04/2010TrustAuditError KeyCodingPDiag C449 Other malignantneoplasms of skin -Malignant neoplasm ofskin, unspecifiedDiag1 I10X Essential (primary)hypertensionDiag2 J459 Asthma - Asthma,unspecifiedProc1 S055 Microscopically controlledexcision of lesion of skinof head or neck NECProc2 S279 Other local flap of skin -UnspecifiedCodingC449I10XJ459E091S055Other malignantneoplasms of skin -Malignant neoplasm ofskin, unspecifiedEssential (primary)hypertensionAsthma - Asthma,unspecifiedExcision of lesion ofexternal noseMicroscopically controlledexcision of lesion of skinof head or neck NECProc3 Z221 External nose S279 Other local flap of skin -UnspecifiedHRG JC17Z Skin Therapies level 5 CZ12V Minor Nose Procedures19 years and over withCCSpellHRGJC17Z Skin Therapies level 5 CZ12V Minor Nose Procedures19 years and over withCCCodingManual orCodingClinicreferencePPO OPCS 4.5instructionmanualPage S-5Base£635 £734tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£635 £734PriceCoding SourceClinical RecordA procedure code from Chapter E OPCS-4 should be selected as per exclusion note at beginning of Chapter S.Audit Commission Payment by results data assurance framework 57
Example 7ID Speclty 330 SubchapterEpisode Start 25/06/2010 End 25/06/2010TrustAuditError KeyCodingPDiag C440 Other malignantneoplasms of skin - Skinof lipProc1 S152 Biopsy of lesion of skinNECCodingC440Other malignantneoplasms of skin - Skinof lipCodingManual orCodingClinicreferenceF021 Excision of lesion of lip PP3 OPCS 4.5instructionmanualPage S-5Proc2 Z251 LipHRG JC15Z Skin Therapies level 3 CZ02Y Intermediate MouthProcedures 19 years andover without CCSpellHRGJC15Z Skin Therapies level 3 CZ02Y Intermediate MouthProcedures 19 years andover without CCBase£635 £644tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£635 £644PriceCoding SourceClinical RecordA procedure code from Chapter F in OPCS-4 should be selected in accordance with exclusion note at chapterheading for Chapter S.Audit Commission Payment by results data assurance framework 58
Example 8ID Speclty 330 SubchapterEpisode Start 14/04/2010 End 14/04/2010TrustAuditError KeyCodingPDiag C440 Other malignantneoplasms of skin - Skinof lipDiag1 I10X Essential (primary)hypertensionDiag2 E109 Insulin-dependentdiabetes mellitus -Insulin-dependentdiabetes mellitus withoutcomplicationsCodingC440I10XE119Other malignantneoplasms of skin - Skinof lipEssential (primary)hypertensionNon-insulin-dependentdiabetes mellitus - Noninsulin-dependentdiabetes mellitus withoutcomplicationsDiag3 J459 Asthma - Asthma,unspecifiedProc1 S065 Excision of lesion of skinof head or neck NECSDISDOCodingManual orCodingClinicreferenceF021 Excision of lesion of lip PP3 OPCS 4.5instructionmanualPage S-5Proc2 S279 Other local flap of skin -UnspecifiedF042 Reconstruction of lipusing skin flapProc3 Z251 LipHRG JC15Z Skin Therapies level 3 CZ03V Major Mouth Procedures19 years and over withCCSpellHRGJC15Z Skin Therapies level 3 CZ03V Major Mouth Procedures19 years and over withCCBase£635 £2,476tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£635 £2,476PriceCoding SourceClinical RecordThere is an exclusion note at the beginning of Chapter S in OPCS-4 that codes from this chapter should not beused for certain sites including the site for lip. A code from chapter F should be used.SP3Audit Commission Payment by results data assurance framework 59
Example 9ID Speclty 330 SubchapterEpisode Start 01/04/2010 End 01/04/2010TrustAuditError KeyCodingPDiag C440 Other malignantneoplasms of skin - Skinof lipProc1 S069 Other excision of lesionof skin - UnspecifiedCodingC440Other malignantneoplasms of skin - Skinof lipCodingManual orCodingClinicreferenceF021 Excision of lesion of lip PPO OPCS 4.5instructionmanualPage S-5Proc2 Z251 Lip F042 Reconstruction of lipusing skin flapHRG JC15Z Skin Therapies level 3 CZ03Y Major Mouth Procedures19 years and overwithout CCSpellHRGJC15Z Skin Therapies level 3 CZ03Y Major Mouth Procedures19 years and overwithout CCBase£635 £1,837tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£635 £1,837PriceCoding SourceClinical RecordThere is an exclusion note at the beginning of Chapter S in OPCS-4 that codes from this chapter should not beused for certain sites including the site for lip. A code from chapter F should be used.SPOAudit Commission Payment by results data assurance framework 60
Example 10ID Speclty 330 SubchapterEpisode Start 27/05/2010 End 27/05/2010TrustCodingAuditCodingError KeyPDiag L82X Seborrhoeic keratosis L82X Seborrhoeic keratosisDiag1 I10X Essential (primary) I10X Essential (primary)hypertensionDiag2 E119 Non-insulin-dependentdiabetes mellitus - Noninsulin-dependentdiabetes mellitus withoutcomplicationsProc1 S081 Curettage andcauterisation of lesion ofskin of head or neckE119E091hypertensionNon-insulin-dependentdiabetes mellitus - Noninsulin-dependentdiabetes mellitus withoutcomplicationsExcision of lesion ofexternal noseProc2 Z221 External nose S081 Curettage andcauterisation of lesion ofskin of head or neckHRG JC15Z Skin Therapies level 3 CZ12V Minor Nose Procedures19 years and over withCCSpellHRGJC15Z Skin Therapies level 3 CZ12V Minor Nose Procedures19 years and over withCCCodingManual orCodingClinicreferencePPO OPCS 4.5instructionmanualPage S-5Base£635 £734tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£635 £734PriceCoding SourceClinical RecordA code from Chapter E should be used for the excision of lesion nose as per the exclusion note at the heading forChapter S.Audit Commission Payment by results data assurance framework 61
Example 11ID Speclty 330 SubchapterEpisode Start 20/05/2010 End 20/05/2010TrustAuditError KeyCodingPDiag D233 Other benign neoplasmsof skin - Skin of other andunspecified parts of faceDiag1 D239 Other benign neoplasmsof skin - Skin, unspecifiedProc1 S139 Punch biopsy of skin -UnspecifiedCodingD233D237E095Other benign neoplasmsof skin - Skin of other andunspecified parts of faceOther benign neoplasmsof skin - Skin of lowerlimb, including hipBiopsy of lesion ofexternal noseProc2 Z221 External nose S139 Punch biopsy of skin -UnspecifiedProc3 Z494 Skin of back Z496 Skin of shoulderHRG JC15Z Skin Therapies level 3 CZ12Y Minor Nose Procedures19 years and overwithout CCSpellHRGJC15Z Skin Therapies level 3 CZ12Y Minor Nose Procedures19 years and overwithout CCSD4CodingManual orCodingClinicreferencePPO OPCS 4.5instructionmanualPage S-5Base£635 £644tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£635 £644PriceCoding SourceClinical RecordThere is an exclusion note at the beginning of Chapter S in OPCS-4 that codes from this chapter should not beused for certain sites including the site for external nose. A code from chapter E should be used.Audit Commission Payment by results data assurance framework 62
Example 12ID Speclty 330 SubchapterEpisode Start 24/05/2010 End 24/05/2010TrustCodingAuditCodingError KeyPDiag L570 Actinic keratosis L570 Actinic keratosisProc1 S081 Curettage andcauterisation of lesion ofskin of head or neckE092Destruction of lesion ofexternal nose NECProc2 Z221 External nose S081 Curettage andcauterisation of lesion ofskin of head or neckHRG JC15Z Skin Therapies level 3 CZ12Y Minor Nose Procedures19 years and overwithout CCSpellHRGJC15Z Skin Therapies level 3 CZ12Y Minor Nose Procedures19 years and overwithout CCCodingManual orCodingClinicreferencePPO OPCS 4.5instructionmanualPage S-5Base£635 £644tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£635 £644PriceCoding SourceClinical RecordThere is an exclusion note at the beginning of Chapter S in OPCS-4 that codes from this chapter should not beused for certain sites including the site for external nose. A code from chapter E should be used and an ‘S’ codebe added to give additional information if requiredAudit Commission Payment by results data assurance framework 63
Example 13ID Speclty 330 SubchapterEpisode Start 23/04/2010 End 23/04/2010TrustAuditError KeyCodingPDiag L989 Other disorders of skinand subcutaneous tissue,NEC - Disorder of skinand subcutaneous tissue,unspecifiedProc1 S149 Shave biopsy of skin -UnspecifiedCodingL989E091Other disorders of skinand subcutaneous tissue,NEC - Disorder of skinand subcutaneous tissue,unspecifiedExcision of lesion ofexternal noseProc2 Z221 External nose S141 Shave biopsy of lesion ofskin of head or neckHRG JC15Z Skin Therapies level 3 CZ12Y Minor Nose Procedures19 years and overwithout CCSpell JC15Z Skin Therapies level 3 CZ12Y Minor Nose ProceduresHRG19 years and overwithout CCBase£635 £644tariffShort£0 £0stayadj.Speciali£0 £0st TopUpExcess£0 £0beddaysTotal£635 £644PriceCodingManual orCodingClinicreferencePPO OPCS 4.5instructionmanualPage S-5SP4Coding SourceClinical RecordThere is an exclusion note at the beginning of Chapter S in OPCS-4 that codes from this chapter should not beused for certain sites including the site for external nose. A code from chapter E should be used and an ‘S’ codebe added to give additional information if required.Audit Commission Payment by results data assurance framework 64
Analysis of errors – Chapter JC - Skin:All the acronyms in this table are defined in appendix 8 – error keys.Overall Number %Total Number of 70episodes examinedUTA Unsafe to audit 0Financial value of 0UTA episodes (spelllevel)Actual number of 70episodes examinedNumber of spells this 70representsNumber of episodes 13 18.57where HRG wouldchange as a result ofAuditor's coding.Number of spellswhere HRG wouldchange as a result ofAuditor's coding.13 18.57Primary Diagnosis Number of primary 61 87.14diagnoses correctNon Coder ErrorPDI 5 7.14Coder ErrorPD3 4 5.71Secondary Diagnosis Number of secondary 50diagnosesNumber of secondarydiagnoses correct29 58.00Non Coder ErrorSDI 3 6.00Coder ErrorSD4 1 2.00SDO 17 34.00Primary ProceduresNumber of primaryproceduresNumber of primaryprocedures correct7058 82.86Non Coder ErrorCoder ErrorPP3 3 4.29PPO 9 12.86SecondaryProceduresNumber of secondaryproceduresNumber of secondaryprocedures correct3934 87.18Non Coder ErrorCoder ErrorSP3 1 2.56SP4 1 2.56SPO 3 7.69Additional Fields Number %Pre-audit sample £46,626pricePost-audit sample £51,220pricePrice of gross £4,594 9.85Audit Commission Payment by results data assurance framework 65
changePrice of net change £4,594 9.85Number of spells in 0 0.00pre-audit sampleoutside of PbRPost-audit price of 0 0.00these spellsNumber of spells in 0 0.00post-audit sampleoutside of PbRPre-audit price ofthese spells.0 0.00Audit Commission Payment by results data assurance framework 66
Appendix 6 – HRG area EB01Z - Noninterventional acquired cardiac conditions 19years and over88 The appendix gives a detailed breakdown of the clinical coding auditfindings in the specific area audited. It is designed as a technical report forthe clinical coding department at the Trust audited. However PCTs will findthe data useful in understanding the cause of the HRG assignment errorsand the coding errors.89 At the set up meeting the Trust and PCT agreed to audit HRG EB01Zas this was an area of concern for commissioners. A sample of 30 caseswas provided for audit and no episodes found unsafe to audit per NHS CFHstandards because there was no evidence of the episode within in thecasenotes.Table 17: HRG EB01Z area: coding errorsTotal fromepisodesauditedIncorrectCoderErrorNon CoderErrorTotalincorrect%incorrectPrimary 30 1 4 5 16.7diagnosisSecondary 95 6 13 19 20.0diagnosisPrimary 2 0 0 0 0.0procedureSecondary 3 0 0 0 0.0procedureOverall 130 7 17 24 18.5Table 18: Table 18 HRG area: HRG errorsEpisodesSpellsTotal 30 19Total changing HRG 0 0% changing HRG 0.0 0.0Analysis of coding errors90 The audit identified 24 (18.5 per cent) errors in procedure anddiagnoses coding, leading to no HRG changes.Audit Commission Payment by results data assurance framework 67
91 The following area for improvement has been identified;■ reinforce the importance of recording the mandatory co-morbidities fromthe March 2010 Coding Clinic, as omission of secondary diagnoses wasan issue from both the coder and clinical perspective.92 There were 17 non-coder errors due to the source document notholding all the relevant information for the coder at the time/point of codingaffecting four primary and 13 secondary diagnoses.93 The coder errors were in the following areas:■■incorrect coding at the required 3- character level affecting one primaryand four secondary diagnoses; andomission of diagnosis and procedures – affecting two secondarydiagnoses.94 There are five instances when information not relevant to the episode ofcare has been coded. NHS CFH does not treat this as an error and werethey to have been included they would have accounted for none of the HRGchanges. The Trust should seek to code only relevant information.Financial impact of errorsTable 19: HRG area: financial impact of errorsPre AuditPaymentPost AuditPaymentGrossChange% GrossChangeNetChange£14,261 £14,261 £0 0.0 £0 0.0% NetChange95 The sample of spells audited covered £14,261 of activity. The errorshad no financial impact on the sample tested.Data Issues96 There were no data issues identified within the HRG area.Audit Commission Payment by results data assurance framework 68
Analysis of errors – HRG EB01Z:All the acronyms in this table are defined in appendix 8 – error keys.Overall Number %Total Number of 30episodes examinedUTA Unsafe to audit 0Financial value of 0UTA episodes (spelllevel)Actual number of 30episodes examinedNumber of spells this 19representsNumber of episodes 0 0.00where HRG wouldchange as a result ofAuditor's coding.Number of spellswhere HRG wouldchange as a result ofAuditor's coding.0 0.00Primary Diagnosis Number of primary 25 83.33diagnoses correctNon Coder ErrorPDI 4 13.33Coder ErrorPD3 1 3.33Secondary Diagnosis Number of secondary 95diagnosesNumber of secondarydiagnoses correct76 80.00Non Coder ErrorSDI 13 13.68Coder ErrorSD3 4 4.21SDNR 4SDO 2 2.11ECNR 1Primary ProceduresNon Coder ErrorCoder ErrorSecondaryProceduresNumber of primaryproceduresNumber of primaryprocedures correctNumber of secondaryproceduresNumber of secondaryprocedures correct22 100.0033 100.00Non Coder ErrorCoder ErrorAdditional Fields Number %Pre-audit sample £14,261pricePost-audit sample £14,261pricePrice of gross £0 0.00changePrice of net change £0 0.00Number of spells in 0 0.00Audit Commission Payment by results data assurance framework 69
pre-audit sampleoutside of PbRPost-audit price ofthese spellsNumber of spells inpost-audit sampleoutside of PbRPre-audit price ofthese spells.0 0.000 0.000 0.00Audit Commission Payment by results data assurance framework 70
Appendix 7 – Ungrouped original Cardiologyresults from 2007/0897 This section shows the finding from the audit of Cardiology completed in2007/08. This was coded using OPCS-4.3 and grouped using HRGv3.5grouper. To enable an accurate HRG level comparison between the2007/08 and 2010/11 audits we have regrouped the 2007/08 audit data toHRG4.Table 20: Original Cardiology area: coding errorsTotal fromepisodesauditedIncorrectTotalincorrect%incorrectCodererrorNon CoderErrorPrimary 100 5 5 10 10.0diagnosisSecondary 153 18 29 47 30.7diagnosisPrimary 90 11 2 13 14.4procedureSecondary 95 4 7 11 11.5procedureOverall 438 38 43 81 18.5Table 21: Original Cardiology area: HRG errorsTotal 100Total changing HRG 2% changing HRG 2.0EpisodesFinancial impact of errorsTable 22: Original Cardiology area: financial impact of errorsPre AuditPaymentPost AuditPaymentGrosschange% GrossChangeNetchange£236,816 £239,234 £3,682 1.5 £2,418 1.0% netchangeAudit Commission Payment by results data assurance framework 71
Appendix 8 – Error keysError Key DescriptionsKEYDESCRIPTIONUTAUNSAFE TO AUDITThe Auditor is unable to audit the coded clinical data against the sourcedocumentation.For example:There is insufficient or no information regarding the episode in theAuditor’s source documentation.Primary Diagnosis error keysCoder errorPD3PRIMARY DIAGNOSISINCORRECT AT THREECHARACTER LEVELThe primary diagnosis code has been allocated to an incorrect threecharacter code.PD4PRIMARY DIAGNOSISINCORRECT AT FOURCHARACTER LEVELThe primary diagnosis code has been allocated to an incorrect fourthcharacter.PD5PRIMARY DIAGNOSISINCORRECT AT FIVECHARACTER LEVELThe primary diagnosis code has been allocated to an incorrect fifthcharacter.PDISPRIMARY DIAGNOSISINCORRECTLY SEQUENCEDThe primary diagnosis code recorded by the Auditor has not beensequenced by the Coder as the primary diagnosis.PDOPRIMARY DIAGNOSIS OMITTEDThe primary diagnosis recorded by the Auditor has not been recorded bythe Coder in any diagnosis field.Non-Coder ErrorPDIINFORMATION AVAILABLE ATTHE TIME OF AUDIT NOTAVAILABLE AT THE TIME OFCODINGInformation available to the Auditors was not available at the time ofAudit Commission Payment by results data assurance framework 72
KEYDESCRIPTIONcoding. This is where information regarding the episode becameavailable after the episode was coded. This error key is not to be used ifthe information was not accessed by the Clinical Coder at the point ofcoding, for example, with histopathology reports.This error key would also be assigned by the Auditor when the sourcedocumentation used at the time of coding did not contain all pertinentinformation required for accurate and complete coding and the Coder didnot have access to this information, for example, coding from proformawith no access to the casenotes.PDDPRIMARY DIAGNOSISDOCUMENTATION ISSUEThe Auditor is unable to code the clinical data from the sourcedocumentation and compare against that of the Trusts due to unclear orinconsistent information.For example:Inconsistency between information recorded by clinical staff contained onthe source documentation and it is not clear which is correct.The source documentation is illegible.PDMPRIMARY DIAGNOSIS CODEDTO MANAGEMENTSPECIFICATIONThere is a clear and documented directive from management tocontravene coding to national standards.For example:by unbundling diagnoses or procedures into component partsby adding or optimising the coded clinical data to alter the derived HRG.PDCPRIMARY DIAGNOSIS CODEDTO CLINICIAN SPECIFICATIONThere is a clear and documented directive from Clinicians to contravenecoding to national standards or capture those instances where a Clinicianhas requested that coding be done in a particular way as it moreaccurately captures the diagnosis.For example:by unbundling diagnoses or procedures into component parts.PDSCPRIMARY DIAGNOSIS CODEDDUE TO SYSTEM CONSTRAINTDue to the system that the Organisation uses the primary diagnosis codesis technically incorrect at some level, omitted or sequenced incorrectly.Secondary diagnosis error key descriptionsCoder ErrorSD3SECONDARY DIAGNOSISINCORRECT AT THREECHARACTER LEVELThe secondary diagnosis code has been allocated to an incorrect threecharacter code.SD4SECONDARY DIAGNOSISINCORRECT AT FOURAudit Commission Payment by results data assurance framework 73
KEYDESCRIPTIONCHARACTER LEVELThe secondary diagnosis code has been allocated to an incorrect fourcharacter code.SD5SECONDARY DIAGNOSISINCORRECT AT FIVECHARACTER LEVELThe secondary diagnosis code has been allocated to an incorrect fivecharacter code.SDNRSECONDARY DIAGNOSIS NOTRELEVANTThe secondary diagnosis code recorded by the Coder is not relevant tothe episode of care.SDOSECONDARY DIAGNOSISOMITTEDDiagnosis that has been recorded by the Auditor as relevant but ismissing from the Organisation’s recorded episode.SDISSECONDARY DIAGNOSISINCORRECT SEQUENCINGThe sequencing of the secondary codes contravenes national standards.This error key can only be assigned for error in the following nationalstandards:Outcome of delivery (Z37 and Z38 if not well baby)Asterisk codes must be preceded by a dagger codeSpecific coding conventions in ICD-10 i.e. use additional codeExtent of body surface in burns (T31, T32).ECIEXTERNAL CAUSE CODEINCORRECTThe external cause code recorded by the Organisation is incorrect at anycharacter level.ECOEXTERNAL CAUSE CODEOMITTEDThe external cause code has been omitted from the Organisation’srecorded episode.Non-Coder ErrorSDISee PDI.SDDSDMSDCSDSCSee PDDSee PDMSee PDCINFORMATION AVAILABLE ATTHE TIME OF AUDIT NOTAVAILABLE AT THE TIME OFCODINGSECONDARY DIAGNOSISDOCUMENTATION ISSUESECONDARY DIAGNOSISCODED TO MANAGEMENTSPECIFICATIONSECONDARY DIAGNOSISCODED TO CLINICIANSPECIFICATIONSECONDARY DIAGNOSISAudit Commission Payment by results data assurance framework 74
KEYSee PDSCDESCRIPTIONCODED DUE TO SYSTEMCONSTRAINTPrimary procedure error key descriptionsCoder ErrorPP3PRIMARY PROCEDUREINCORRECT AT THREECHARACTER LEVELThe primary procedure code has been allocated to an incorrect threecharacter code.PP4PRIMARY PROCEDUREINCORRECT AT FOURCHARACTER LEVELThe primary procedure code has been allocated to an incorrect fourcharacter code.PPISPRIMARY PROCEDUREINCORRECTLY SEQUENCEDThe primary procedure code recorded by the Auditor has not beensequenced by the Coder as the primary procedure.PPOPRIMARY PROCEDUREOMITTEDThe primary procedure recorded by the Auditor has not been recorded bythe Coder in any procedure field.PPNRPRIMARY PROCEDURE NOTRELEVANTThe primary procedure recorded by the Coder is not relevant to theepisode of care.Non-Coder ErrorPPISee PDI.PPDPPMPPCPPSCSee PDSCSee PDDSee PDMSee PDCINFORMATION AVAILABLE ATTHE TIME OF AUDIT NOTAVAILABLE AT THE TIME OFCODINGPRIMARY PROCEDUREDOCUMENTATION ISSUEPRIMARY PROCEDURE CODEDTO MANAGEMENTSPECIFICATIONPRIMARY PROCEDURE CODEDTO CLINICIAN SPECIFICATIONPRIMARY PROCEDURE CODEDDUE TO SYSTEM CONSTRAINTSecondary Procedure error key descriptionsCoder ErrorSP3SECONDARY PROCEDUREINCORRECT AT THREECHARACTER LEVELThe secondary procedure code has been allocated to an incorrect threeAudit Commission Payment by results data assurance framework 75
KEYcharacter code.SP4DESCRIPTIONSECONDARY PROCEDUREINCORRECT AT FOURCHARACTER LEVELThe secondary procedure code has been allocated to an incorrect fourcharacter code.SPISSECONDARY PROCEDUREINCORRECTLY SEQUENCEDThe Organisation has not sequenced the procedure coding according tothe rules and conventions of the classification.For example:See use as secondary code when associated with…SPOSECONDARY PROCEDUREOMITTEDSecondary procedure that has been recorded by the Auditor as relevantbut is missing from the Organisation’s recorded episode.SPNRSECONDARY PROCEDURE NOTRELEVANTThe secondary procedure code recorded by the Coder is not relevant tothe episode of care.Non-Coder ErrorSPISee PDI.SPDSee PDDSPMSPCSPSCSee PDSCSee PDMSee PDCINFORMATION AVAILABLE ATTHE TIME OF AUDIT NOTAVAILABLE AT THE TIME OFCODINGSECONDARY PROCEDUREDOCUMENTATION ISSUESECONDARY PROCEDURECODED TO MANAGEMENTSPECIFICATIONSECONDARY PROCEDURECODED TO CLINICIANSPECIFICATIONSECONDARY PROCEDURECODED DUE TO SYSTEMCONSTRAINTAudit Commission Payment by results data assurance framework 76
Appendix 9 – GlossaryTermExplanationBenchmarkingThe process of measuringstandards of actual performanceagainst those achieved by otherswith broadly similar characteristics.The aim is to improve quality sothat other organisations or servicescan raise their own performance tothat of the best. The process helpspractitioners take a structuredapproach to share, compare,identify and develop the bestpractice.DiagnosisDiagnostic codes are used to groupand identify diseases, disorders,symptoms, and medical signs, andare used to measure morbidity andmortality. Diagnoses codes areaudited against ICD-10 standards,as set by the World HealthOrganisationFinished Consultant Episode (FCE) An FCE or episode of care is acompleted period of care of apatient using an NHS hospital bed,under one consultant within onehealthcare provider. If a patient istransferred from one consultant toanother, even if this is within thesame provider unit, the episodeends and another one beginsGrouperSystem which uses diagnosis andprocedure codes to allocate activityto HRGs for billing purposes.Healthcare Resource Group (HRG) A grouping consisting of patientevents that have been judged toconsume a similar level ofresource. This is the currency usedfor payment under Payment byResultsHRGv3.5 NHS Grouper used until 2008/09HRG4 NHS Grouper used from 2009/10ICD10International Classification ofDisease and Related HealthProblems. An internationallydefined classification of disease,managed by the World HealthOrganisation – 10th Revisions.OPCS-4.5Office of Population Censuses andSurveys version 4.5 (now the OfficeAudit Commission Payment by results data assurance framework 77
TermProceduresSpellExplanationof National Statistics). The standardclassification system used to recordhealthcare procedures andinterventions in England. Version4.5 mandated for use since 1 April2009.Procedure codes are numbers oralphanumeric codes used toidentify specific health interventionstaken by medical professionals.Procedure codes are auditedagainst national standards inOPCS-4.5.A continuous spell of admitted carecomprising one or more finishedconsultant episodes. A hospitalspell is the period from the date ofadmission to the date of discharge.A hospital spell may consist ofmore than one FCE.Audit Commission Payment by results data assurance framework 78
THE ROYAL BOURNEMOUTH AND CHRISTCHURCH HOSPITALSNHS FOUNDATION TRUSTBOARD OF DIRECTORSMeeting Date and Part:10 June Part ISubject:Core BriefSection:InformationExecutive Director with overallresponsibility:Tony Spotswood, Chief ExecutiveAuthor of Paper:Tracey Hall, Head of CommunicationsSummary:The Core Brief distributed within theTrust in May 2011Standards for Better Healthdomain:N/AAction required by <strong>Board</strong> ofDirectorsNote for information
Core BriefMayFrom: Tony Spotswood, Chief Executive2011Your voices heardThe Trust recently held a 12-week public consultationon its draft Annual Plan. The Plan set out proposalsfor improving patient outcomes and achievingefficiency savings, including looking at patientpathways and estate options.There was particular interest in the two options forChristchurch <strong>Hospital</strong>, which we asked you to voteon. The first was to retain current services and usethe remaining space for services such as an NHSdentist, nursing home, GP and pharmacy. Thesecond option was to move all services to the <strong>Royal</strong><strong>Bournemouth</strong> site and use all of the Christchurchsites for the community services mentioned togetherwith a larger nursing home facility.Over 1,500 copies of the plan were sent to staff, thepublic and local groups, including all local authorities,LINks, community and patient groups and healthpartners. The Trust also held a range of meetingswith various staff, community groups and healthpartners as well as three public meetings. Largenotice boards setting out the options for Christchurch<strong>Hospital</strong> were displayed widely across Christchurch.The Trust received a fantastic response. In total2,174 people used the voting slips. 2,142 voted foroption 1 (98.5%) while 32 voted for Option 2. Lettersand emails were also received either giving optionone as their preferred option or writing in with theirgeneral views.The following were the main issues causing youconcern:l The future of Christchurch <strong>Hospital</strong> and ensuringservices remain on the site.l Ensuring sufficient care in the community(particularly following a stroke).l Sufficient support for patients once they have lefthospital (social care).l It was generally felt that the concept should not bereferred to as an ‘older people’s village’. The term‘health village’ will be used for the interim.l A key issue is the need for closer integration ofcommunity and hospital services.l There was a plea from the public to ensure theexcellent Dermatology Service and the MacmillanUnit remained at Christchurch.Both members of the public and some Christchurchcouncillors praised the consultation process and theopportunity to hear our plans and be able to commenton them.Next stepsThe Draft Annual Plan will be updated to reflect thecomments received.Regarding Christchurch <strong>Hospital</strong>, the work ondeveloping a detailed business case will begin,influenced by the detailed comments received.It is expected that this will be produced by theautumn. The Plan will centre on progressing Option1, which includes maintaining existing outpatientdiagnostic and day hospital services andcomplementing these will be GP surgery, NHSdentistry, nursing home and other communityprovision.The remainder of the plan will now be progressed,and regular updates will be provided.For a full copy of the summary log on towww.rbch.nhs.uk or if you would like to be addedto our mailing list to receive regular updatesplease contact us at comments@rbch.nhs.ukor 01202 704271.Tony Spotswood,Chief Executive6 Is our Transformation Programme an appropriate response to the need to find savingsand improve care? (Section 4)7 What are your views on the approach set out in “organising for clinical excellence”?(Section 5)8 In the section “Better use of buildings”, do you have a preference for Option 1 orOption 2 and do you have any comments on the consequences of either option?(Section 6)9 In developing new models of care (Section 7), do you have any comments to add?DraftAnnual Planfor PublicConsultation2011/12ents to add?
Catering UpdateThe first phase of the refurbishmentof the staff dining room is nearingcompletion and I would like to thankour customers for their patienceduring this time. I would also liketo thank the catering staff for theirresilience and support during thischallenging time.Once complete, the refurbishmentswill improve the services availableand provide a separate staff onlydining area called the “Oasis”.Next steps:• We will be transferring the Delibar from its current location to thenew servery. The new DeliCounter will be available from10.30-7.30pm, daily.• A third till will be open. Duringpeak times this would berestricted to staff only.• Re-Introduction of “Hungry staff”pre-ordering service. Orderforms available from the cateringinternet site. This new servicewill enable staff to pre-order fromthe Deli via email for collectionat a specific time. When orderinginclude your loyalty card numberand the transaction will bedebited from your account, noneed to queue at the till.Don’t forget to collect yourrestaurant loyalty card.We have had quite a number ofstaff who have applied for arestaurant loyalty card in theCatering Department.For those who have been notifiedto collect but have not yet done so,can you please pick these up fromthe Shelley Restaurant between thefollowing hours:• 7.30am - 11.00amMonday to Sunday• 2.30pm - 8.30pmMonday to SundayIf you have applied for a card anddo not want it, please let me know,and I will re issue the card.For those who wish to apply for aloyalty card, please contact me formore information at terry.reeves@rbch.nhs.uk. Thank you.Terry Reeves,Catering ManagerThird ThursdayMedicine for ManagersTo remind you that the program for the next few months is:16 June 2011 Dr Khaled Amar, Consultant Physician, Medicine forthe Elderly. “Parkinson’s Disease or not Parkinson’sDisease - that is the question?”.22 September 2011 Mr Andrew Morris, Consultant Ophthalmologist.Retinal Disease.19 October 2011 (Wednesday) Mr Dexter Perry, ConsultantSurgeon. Update on Breast/Skin Cancer.A buffet lunch will be available in the Lakeside Deli from 12.30 pmwith the lecture starting at 1 pm in the Lecture Theatre,Postgraduate Centre (the lectures last 40-45 minutes).Dr Mary Armitage, Medical DirectorSuccess forOrthopaedicTeamThe work of theOrthopaedic Therapy Teamat the <strong>Royal</strong> <strong>Bournemouth</strong><strong>Hospital</strong> has beenrecognised at the 2011Advancing HealthcareAwards for Allied HealthProfessionals andHealthcare Scientists.The team was announcedas Runners Up in the‘Rethinking the PatientCare Pathway’ categoryfor their project entitled‘Using an EnhancedRecovery Pathway to DriveChange in Orthopaedics’.The announcement reflectsthe huge amount of workperformed by the TherapyService to help reducelength of stay and improvepatient outcomes andexperience for Orthopaedicinpatients. This includesthe introduction of a sevenday therapy service, preoperative patient educationand improved patientinformation.This is a wonderfulachievement thatacknowledges the greatefforts of the team overthe past few years. Thiswork will continue to bedeveloped as the teamconstantly strives toimprove patient outcomesand service efficiencies.Jon Swan, Team Leaderand Harriet Sturgess, SeniorOccupational Therapist
Staff Excellence Awards 2011- still time to nominateThe deadline for staff awards nominations is fast approachingand we would like to encourage as many people as possible tonominate.There are seven categories from which you can nominate.For more information about these and to submit a nomination,please visit http://www.rbch.nhs.uk/awards2011_staff/index.php?link=criteria.Hard copies of the nomination forms will also be made availableon request. To request a hard copy or for more information aboutsubmitting a nomination, please contact Andrea Smithson onext 4271.Remember, if your nominee gets shortlisted, then you will beinvited to the awards ceremony at the <strong>Royal</strong> Bath Hotel on the7th September.Good luck and get nominating!Melanie Croydon,Communications OfficerTwilight Walk for WomenOur latest Jigsaw appeal aims to raise £1.5m to transform the Women’sHealth Unit (WHU) at RBH. The new unit will create a better experiencefor the 7,000 patients who visit each year with a lighter, brighterenvironment offering greater privacy and dignity.A ‘Twilight Walk for Women’ is taking place on Friday 3rd June. The walkis suitable for all women of ages and levels of fitness with options for a1km walk, a 5km walk or a 10km walk. All three routes will be guided bya team of Jigsaw marshals and will start and finish at Pier Approach on<strong>Bournemouth</strong> Seafront. We hope to have nearly 300 women participating,and have a number of supporters including Sally Taylor from BBC Southand The Village Hotel taking part.Men are also being asked to show their support for wives, partners andloved ones, by following in the women’s footsteps and doing a men-onlywalk. This will take place at 9.30pm, just half an hour after the women’swalk, following the same 1km, 5km or 10km route.Both walks cost just £15 to enter and participants are encouraged to raisea much sponsorship as possible. Eachparticipant will receive a free T–shirt, awalking number, and a fundraising pack.If you have not already signed up pleasepop down and see anyone fromthe Jigsaw office (locatedin the atrium of the <strong>Royal</strong><strong>Bournemouth</strong> <strong>Hospital</strong>)for an application form.Michelle House,Fundraising Staffand Corporate OfficerJoin Sallyand walkfor womenwalk for womenplusfor the Jigsaw AppealFriday 3rd June - 9pm<strong>Bournemouth</strong> Seafront (women only)Race for Wife 9.30pm (men only)1km, 5km and 10km fundraising walkEntry Fee: £15 per person (includes T-shirt)Please raise as much sponsorship as possibleThe <strong>Royal</strong> <strong>Bournemouth</strong> <strong>Hospital</strong> Jigsaw Appeal aims to raise £1.5 millionto create a new Womens Health Unit for the hospitalRiderSurveyTo help improve cyclingfacilities we are asking all cyclistsfor feedback on how supportedthey feel and how things can beimproved.We would like to know about yourindividual experiences of cyclingto work, good or bad.A survey has been designed tocover all the aspects of cyclingto work with an emphasis onsecurity safety and fitness.It is hoped that highlighting themany benefits that cycling towork has brought to staff willhelp support future funding andencourage more people to takeup cycling to work.The survey is available fromthe blue return post boxes in allthe bike shelters, the changingrooms near the restaurant atRBH and via the intranethttp://rbhintranet/2011pdf/bike_survey.pdf (internal only).Completed surveys will beentered into a raffle on 1st Junewith a draw being made for thechance to win £100 worth ofcycle vouchers.Richard Ford, MedicalEquipment Library ManagerName:Department:Postcode:Age: 16-25 25-35 35-50 50-65 65+Gender: Male FemaleWhat site do you work at? RBH XCH BothHow often in a month do you ride into work?Everyday 10-20 days 5-10 days < 5 daysHow far do you cycle from home?< 2 Miles 2-4 Miles 4-8miles > 8 MilesWhat is the main reason you cycle to work:No Permit Cost Health EnjoymentWhat seasons do you cycle to work?All year Summer All year not WinterDo you cycle to work in wet weather?Yes No SometimesIf you don’t cycle how do you get to work?Car Bus Walk LiftWhat type of bike do you usually use?Mountain Hybrid Step-through Racer ElectricHow do you store your bike at work? Bike shedBike box Bikestands Railings WorkplaceWhat kind of lock do you use?Wire number Wire key Heavywire key D lockHow much is your bike worth?
THE ROYAL BOURNEMOUTH AND CHRISTCHURCH HOSPITALSNHS FOUNDATION TRUSTBOARD OF DIRECTORSMeeting Date and Part: 10 th June, 2011 – Part 1Subject:Communications UpdateSection:InformationExecutive Director with overallresponsibility:Author of Paper:Summary:Standards for Better Healthdomain:Action required by the <strong>Board</strong> ofDirectors:Richard Renaut,Director of Service DevelopmentTracey HallHead of CommunicationsAn overview of communications activity. Theupdate also includes Read All About (mediacoverage for April 2011).Patient focusAccessible and responsive carePublic HealthFor Information
<strong>Board</strong> of Directors – Part I10 th June, 2011Communications activityJune 20111. IntroductionThe June Communications Report focuses on: Media Plan E-Communications update Looking ahead2. Media PlanThe Communications Team has a proactive media plan for the coming monthswhich takes into account events, health campaigns and developments withinthe Trust. These are items that, as well as promoting to local media, will also beincluded in other communications media such as Buzzword, LCD screens andthe website.While this document is constantly updated below is the plan for June toSeptember of planned proactive news releases:MonthTopicMay Work begins on the new Stroke Unit Trust Open Day Cancer Services Open Day Jigsaw Sky DiveJune British Heart Week (7 th -15 th ) Breath Easy Week (13 th -19 th ) Post Twilight Walk Post Cancer Open Day Release Tulip Appeal ‘An evening with Karen Hardy’July Medicine Uncovered Sun Awareness Funds raised from Twilight Walk New Forest Bike Ride Jigsaw Mike Gatting cricket matchAugust National Women’s Month – link with Appeal forWomenSeptember Stroke Week (12 th -16 th ) – progress on new StrokeUnit Post Mike Gatting cricket event Post ‘An Evening with Karen Hardy’Communications activity – June 2011 Page 1 of 2For information
<strong>Board</strong> of Directors – Part I10 th June, 20113. E-CommunicationsJay Gill, Communications Officer is being seconded into a one year e-communications role to develop this area within the Trust. Work streams willinclude for example:Scoping the opportunities for the Trust to increase e-communicationswith patients and the public.Developing the interactive elements the Trust’s websites, e.g. corporateand Jigsaw.Scoping ongoing developments for the Trust’s websites, particular inareas that support QIPP and MAP initiatives.Scoping social networking opportunities for the Trust and a process formanaging content.To scope and produce a clear plan for promoting and increasing traffic tothe Trust’s websites.An action plan is being developed with the Head of IT and will be monitored atthe Marketing Committee.4. Looking aheadAs well as maintaining the day to day publications, enquiries and e-communications development, the Communications and FundraisingDepartment will focus on the following activities over the coming months are:June: (3 rd ) Twilight Walk for the Appeal for Women – just over 300participantsJuly-Sept: Staff Excellence Awards judging, filming and planning for theevening event on 7 th September.Sept:(1 st ) Charity cricket event with Mike Gatting for the Jigsaw Appeal(2 nd ) An Audience with Karen Hardy in aid of the Jigsaw AppealTracey HallHead of CommunicationsJune, 2011Communications activity – June 2011 Page 2 of 2For information
Read All About It...May 2011Asthma awarenessAsthma is a common disease that affects about5.4 million people in the UK. It often starts inchildhood, but it can occur for the first time at anyage - even in people in their 70s and 80s. It isestimated that there is a person with asthma livingin one in five households in Britain.When a person with asthma comes into contactwith something that irritates their airways (anasthma trigger), the muscles around the walls ofThe May media report includes positive coverage about anumber of subjects including the orthopedic team’s success at theAdvancing Healthcare Awards and a number of complimentaryletters about the excellent service patients have recently received.The report also includes a negative letter about the confusionsome patients are experiencing regarding where to returnmedical equipment.he airways tighten. The airways become narrowernd the lining of the airways becomes inflamedd starts to swell. All these reactions make itcult for people to breath, leading to symptomssthma.ugh the specific cause of asthma is unknown,are many factors that contribute. It canetimes difficult to avoid all your triggerse you have identified them, there areions you can take to better control yourThere was also a large positive article which encouraged peopleto make a nomination for the Staff Excellence Awards 2011 andcoverage of a fundraising event that raised money for Jigsaw.er, asthma cannot be cured but it can beso that attacks can be prevented. Mostasthma who take regular treatmentalers have entirely normally livesing time from school or work, and enjoyent in sport and other recreations.ple with asthma spend time inthey shouldn’t have to. If yourr control, you’re more likely to havef life and be more able to do theto.your regular asthma medication,festyle and self-help measuresreduce your symptoms andn asthma attack. Thesea triggers e.g. pet hair,.y in a smoke-freer exercise.eather.e and support onthma.org.uk/.inationte a member ofor Christchurchrd - a rewardxtra mYour voices heardWe recently held a 12-week public consultation onour draft Annual Plan. The Plan set out proposals forimproving patient outcomes and achieving efficiencysavings, including looking at patient pathways andestate options.There was particular interest in the two options forMay 2011 l 1Christchurch <strong>Hospital</strong>, which we asked you to voteon. The first was to retain current services and usethe remaining space for services such as an NHSdentist, nursing home, GP and pharmacy. Thesecond option was to move all services to the <strong>Royal</strong><strong>Bournemouth</strong> site and use all of the Christchurchsites for the community services mentioned togetherwith a larger nursing home facility.We sent over 1,500 copies of our plan to individualsand local groups, including all local authorities, LINks,community and patient groups and health partners.We also held a range of meetings with various staffand community groups and our health partners aswell as three public meetings. Large notice boardssetting out the options for Christchurch <strong>Hospital</strong> weredisplayed widely across Christchurch.We received a fantastic response, particularly frommembers of the public. In total 2,174 people usedthe voting slips. 2,142 voted for option 1 (98.5%)while 32 voted for Option 2. We also received lettersand emails from members of the public either givingoption one as their preferred option or writing in withtheir general views:The following were the main issues you told us werecausing you concern:• The future of Christchurch <strong>Hospital</strong> and ensuringservices remain on the site.• Ensuring sufficient care in the community(particularly following a stroke)• Sufficient support for patients once they have lefthospital (social care)• It was generally felt that the concept should not bereferred to as an ‘older people’s village’. The term‘health village’ will be used for the interim.• A key issue is the need for closer integration ofity and hospital servicesublic to ensure themillanArticles are published with the kind permission of the Daily Echo, Advertiser,the New Milton Advertiser and the Stour and Avon Magazine.Summary of media coverage:May 2011Print 17Radio 0Television 02011 Coverage*Positive 12Negative 2OK 1May 2010 Positive 13 Negative 8 OK 0*This does not include Mary Armitage’s Echo column
DatePublicationInformationTitlePage numberArticle size3 May 2011Daily EchoLetter to Editors regarding healthcare equipmentand where patients can return the equipment to.Why can’t we return it?18Quarter pageDatePublicationInformationTitlePage numberArticle size3 May 2011Daily EchoPicture and caption about the visitof Princess Anne to officially openthe Dorset Heart centre.That was never five years ago!23Sixteenth of a pageDatePublicationInformationTitlePage numberArticle size4 May 2011Daily EchoLetter to editor praising service atthe Derwent Centre at RBH.<strong>Hospital</strong> staff have done me proud19Eighth of a pageMay 2011 l 2
DatePublicationInformationTitlePage numberArticle size7 May 2011Daily EchoLetter to editors regarding theexcellent treatment a patienthad at RBH and other hospitals inDorset.Publish more on the excellent NHS19Eighth of a pageAsthma awarenessAsthma is a common disease that affects about5.4 million people in the UK. It often starts inchildhood, but it can occur for the first time at anyage - even in people in their 70s and 80s. It isestimated that there is a person with asthma livingin one in five households in Britain.When a person with asthma comes into contactwith something that irritates their airways (anasthma trigger), the muscles around the walls ofthe airways tighten. The airways become narrowerand the lining of the airways becomes inflamedand starts to swell. All these reactions make itdifficult for people to breath, leading to symptomsof asthma.Although the specific cause of asthma is unknown,there are many factors that contribute. It canbe sometimes difficult to avoid all your triggersbut once you have identified them, there areprecautions you can take to better control yourasthma.Remember, asthma cannot be cured but it can becontrolled so that attacks can be prevented. Mostpeople with asthma who take regular treatmentsuch as inhalers have entirely normally liveswithout loosing time from school or work, and enjoyfull involvement in sport and other recreations.Too many people with asthma spend time inhospital when they shouldn’t have to. If yourasthma is under control, you’re more likely to havea better quality of life and be more able to do thethings you want to.As well as taking your regular asthma medication,there are simple lifestyle and self-help measuresthat you can take to reduce your symptoms andyour risk of having an asthma attack. Theseinclude:• Avoiding your asthma triggers e.g. pet hair,pollens, or perfumes.• Stop smoking and stay in a smoke-freeenvironment.• Get appropriate regular exercise.• Taking care in the cold weather.• Eating healthy.For more information, advice and support onasthma, please visit www.asthma.org.uk/.May 2011 l 3DatePublicationInformationTitle11 May 2011Daily EchoMedical column.Asthma awarenessMake your nominationRemember, you can now nominate a member ofstaff from the <strong>Royal</strong> <strong>Bournemouth</strong> or Christchurch<strong>Hospital</strong>s for an Unsung Hero award - a rewardthat recognises those who go the extra mile inputting patients first.The deadline for entries is 12.00pm,27th May. For further details on theaward criteria and how to makea nomination please visitwww.rbch.nhs.uk or contact theCommunications Department on01202 704905.Dr Mary Armitage, Medical Director.medical@rbch.nhs.uk
DatePublicationInformationTitlePage numberArticle size12 May 2011Daily EchoArticle promoted the boardmeeting which discussed the resultsof the recent consultation.<strong>Hospital</strong>’s fate to be reviewed4Eighth of a pageDatePublicationInformationTitlePage numberArticle size12 May 2011Daily EchoStory about the OrthopaedicTherapy Team and their recentsuccess at the AdvancingHealthcare Awards 2011.Team is runner up at awards16Sixteenth of a pageMay 2011 l 4
DatePublicationInformationTitlePage numberArticle size12 May 2011Daily EchoArticle promoting the Staff Excellence Awards 2011.Our hero will be a health service tonic22Half pageMay 2011 l 5
DatePublicationInformationPage numberArticle size13 May 2011Stour and Avon MagazineArticle regarding a local dance teacher and herfundraising for the Jigsaw Appeal for Women.21Eighth of a pageDatePublicationInformationTitlePage numberArticle size13 May 2011Stour and Avon MagazineStory about the OrthopaedicTherapy Team and their recentsuccess at the AdvancingHealthcare Awards 2011.Success for orthopaedic team21Sixteenth of a pageDatePublicationInformationTitlePage numberArticle size13 May 2011Stour and Avon MagazineArticle regarding a talk anRBH consultant is doing in<strong>Bournemouth</strong>.Prostate cancer support21Sixteenth of a pageMay 2011 l 6
DatePublicationInformationTitlePage numberArticle size14 May 2011Daily EchoArticle regarding the success ofthe discharge service which iscommissioned by a partnership oflocal councils and RBH.Charity praised for assistance5Eighth of a pageDatePublicationInformationTitle14 May 2011The LancetArticle regarding a 3-yearcollaboration between healthprofessionals in the UK andGhana to improve stroke care ischanging day-to-day managementand improving multidisciplinaryworking. Clare Gordon from RBHwas involved with this team.Collaboration works to improvestroke outcomes in GhanaMay 2011 l 7
DatePublicationInformationTitlePage numberArticle size18 May 2011Daily EchoArticle regarding the theft of a bicycle outside the hospital.Father ‘disgusted’ at hospital bicycle theft3Quarter pageMay 2011 l 8
May 2011 l 9DatePublicationInformationTitle25 May 2011Daily EchoMedical column.Your voices heardYour voices heardWe recently held a 12-week public consultation onour draft Annual Plan. The Plan set out proposals forimproving patient outcomes and achieving efficiencysavings, including looking at patient pathways andestate options.There was particular interest in the two options forChristchurch <strong>Hospital</strong>, which we asked you to voteon. The first was to retain current services and usethe remaining space for services such as an NHSdentist, nursing home, GP and pharmacy. Thesecond option was to move all services to the <strong>Royal</strong><strong>Bournemouth</strong> site and use all of the Christchurchsites for the community services mentioned togetherwith a larger nursing home facility.We sent over 1,500 copies of our plan to individualsand local groups, including all local authorities, LINks,community and patient groups and health partners.We also held a range of meetings with various staffand community groups and our health partners aswell as three public meetings. Large notice boardssetting out the options for Christchurch <strong>Hospital</strong> weredisplayed widely across Christchurch.We received a fantastic response, particularly frommembers of the public. In total 2,174 people usedthe voting slips. 2,142 voted for option 1 (98.5%)while 32 voted for Option 2. We also received lettersand emails from members of the public either givingoption one as their preferred option or writing in withtheir general views:The following were the main issues you told us werecausing you concern:• The future of Christchurch <strong>Hospital</strong> and ensuringservices remain on the site.• Ensuring sufficient care in the community(particularly following a stroke)• Sufficient support for patients once they have lefthospital (social care)• It was generally felt that the concept should not bereferred to as an ‘older people’s village’. The term‘health village’ will be used for the interim.• A key issue is the need for closer integration ofcommunity and hospital services• There was a plea from the public to ensure theexcellent Dermatology Service and the MacmillanUnit remained at Christchurch.• Both members of the public and someChristchurch councillors praised the consultationprocess and the opportunity to hear our plans andbe able to comment on them.Next stepsThe Draft Annual Plan will be updated to reflect thecomments we received. Regarding Christchurch<strong>Hospital</strong>, the work on developing a detailed businesscase will begin, influenced by the detailed commentsreceived. It is expected that this will be produced bythe autumn when further public communication will beundertaken.The remainder of the plan will now be progressed,and regular updates will be provided.For a full copy of the summary log onto www.rbch.nhs.uk or if you wouldlike to be added to our mailing list toreceive regular updates please contactus at comments@rbch.nhs.uk or01202 704271.Dr Mary Armitage, Medical Director.medical@rbch.nhs.uk
DatePublicationInformationTitlePage numberArticle size25 May 2011Daily EchoArticle regarding the brand new stroke unit at RBH.Work begins on new £2.2m stroke unit9Half pageMay 2011 l 10
DatePublicationInformationTitlePage numberArticle size26 May 2011Daily EchoArticle regarding the debate about smoking in public.Is it time we banned smoking in public?10Half pageMay 2011 l 11
THE ROYAL BOURNEMOUTH AND CHRISTCHURCH HOSPITALSNHS FOUNDATION TRUSTBOARD OF DIRECTORSMeeting Date and Part:10 June 2011 Part ISubject:<strong>Board</strong> of Directors Forward ProgrammeSection:InformationExecutive Director with overallresponsibility:Author of Paper:Rebecca Lawry, Trust SecretaryRebecca Lawry, Trust SecretarySummary:Copy of the <strong>Board</strong> of Directors ForwardProgrammeStandards for Better Health domain:GovernanceAction required by <strong>Board</strong> ofDirectors:For Information
<strong>Board</strong> of Directors - Meeting Map 1What Who Where Before Jan Feb Mar Apr May Jun Jul Sep Oct Nov Dec Where AfterAnnual Report & Accounts - Going Concern Statement SH Finance & Audit Report & A/CAnnual Plan - Draft for Public Consultation RR Service DevelopmentAnnual Plan - Feedback from Consultation RR CoGAnnual Plan - Second Draft RR Service DevelopmentAnnual Plan - Final Draft for Approval RR Service Development PublicationAnnual Report - Audit Committee IM Audit N/AAnnual Report - Finance Committee BF Finance N/AAnnual Report - Healthcare Assurance Committee BA HAC N/AAnnual Report & Accounts - Final draft for approval SH Finance & Audit Cttees MonitorAnnual Report & Accounts First Draft SH Finance N/AAssurance Framework BA HAC N/A<strong>Board</strong> Objectives TS Chief Executive N/A<strong>Board</strong> Statement of Commitment to prevention of Healthcare Associated Infection BA Infection Control ?Budget for next financial year SH Finance N/ACapital Plan for next financial year SH CMG & Finance N/ACharitable Funds - Annual Report & Accounts SH Charitable Funds Charities ComChild Protection & Safeguarding Annual Report BA HAC N/AClinical Governance - Annual Report BA HAC N/AClinical Governance - Quarterly Report BA HAC N/ACode of Conduct for Payment by Results RR Service Development N/ACode of Governance Disclosure Statement JD Trust Secretary MonitorCommunications Audit Action Plan RR Marketing ?Constitutional Documents - Annual Review JD Trust Secretary CoGCore Brief RR Comms FinishCQC - Annual Health Check - Results BA HAC ?CQC - Annual Health Check - Final Declaration BA HAC CQCCQC - Annual Health Check - Format for forthcoming year BA HAC ?Dr Foster Mortality Group Report MA Medical Director MADr Foster Quarterly Report BA Medical Director ?Financial Report - Monthly SH DoF N/AForward Programme JD Trust Secretary N/AInfection Control - Annual Report BA Infection Control N/AInfection Control - Quarterly Update BA Infection Control N/AInpatient Annual Survey Results RR Marketing Publication?Local Clinical Excellence Awards SP Remuneration ?Local Clinical Excellence Awards - Annual Report SP Remuneration N/AMarketing & Communications Report RR Service Development N/AMeeting Dates for Next Year JD Trust Secretary N/AMinutes of Audit Committee Cttee Audit N/AMinutes of Charity Committee Cttee Charitable Funds N/AMinutes of Council of Governors JD CoG N/AMinutes of Finance Committee Cttee Finance N/AMinutes of Healthcare Assurance Cttee HAC N/AMinutes of Infection Control Cttee Infection Control N/AMinutes of Marketing Committee Cttee Marketing N/AMinutes of Remuneration Committee Cttee Remuneration N/AMinutes of Trust Management <strong>Board</strong> Cttee TMB N/AMinutes of Workforce Committee Cttee Workforce N/AMonitor Annual Risk Assessment TS External Monitor?
What Who <strong>Board</strong> Where of Directors Before - Meeting Jan Map Feb Mar Apr May Jun Jul Sep Oct Nov Dec Where 2 AfterMonitor Quarter 1 Report HL Director of Ops MonitorMonitor Quarter 3 Report HL Director of Ops MonitorMonitor Quarter 4 Results HL Director of Ops MonitorMonitor Quarter 2 Report HL Director of Ops MonitorMonitor's FT Sector Overview - Annual Risk Assessment TS Chief Executive N/AMonitor Self Certification - <strong>Board</strong> Statements JD Trust Secretary MonitorPCT Contract Sign Off RR Service Development PCTPerformance Report - Monthly HL Director of Ops N/APutting Patients First - Quarterly Progress Report RR Marketing N/AQuality Accounts - First Draft BA Service Development N/AQuality Accounts - Final Draft for Approval BA Service Development PublicationRead All About It RR Service Development N/ARegister of Interests JD Trust Secretary FileStaff Excellence Awards - Chairman's Prize RR Awards Panel Staff AwardsStaff Excellence Awards - Process for current year RR Service Development N/AStaff Survey - Results KA Workforce ?Standards for Better Health - Final Declaration BA HAC ?Strategy Tracker - Quarterly RR Service Development N/ATerms of Reference - Audit Committee IM Audit File - JDTerms of Reference - Charities Committee KT Charitable Funds File - JDTerms of Reference - Finance Committee SH Finance File - JDTerms of Reference - Healthcare Assurance Committee BA HAC File - JDTerms of Reference - Infection Control Committee BA Infection Control File - JDTerms of Reference - Marketing Committee RR Marketing File - JDTerms of Reference - Remuneration Committee SC Remuneration File - JDTerms of Reference - Trust Management <strong>Board</strong> TS TMB File - JDTerms of Reference - Workforce Committee KA Workforce File - JDWorkforce Committee - Quarterly Report KA Workforce N/A
<strong>Board</strong> of Directors Business Programme<strong>Board</strong> of Directors - Meeting Map 1What Who Where Before Jan Feb Mar Apr May Jun Jul Sep Oct Nov Dec Where AfterAnnual Plan<strong>Board</strong> Objectives TS Chief Executive N/AAnnual Plan - BoD approve Draft for Public Consultation RR TMB BoDAnnual Plan - Feedback from Consultation to BoD RR CoG BoDAnnual Plan - Final Draft for BoD Approval RR TMB BoD PublicationStrategy Tracker - Quarterly RR Service Development N/ABudgetBudget for next financial year SH Finance N/ACapital Plan for next financial year SH CMG & Finance N/ACode of Conduct for Payment by Results RR Service Development N/APCT Contract Sign Off RR Service Development PCTAnnual reportAnnual Report & Accounts First Draft SH Finance N/AAnnual Report - Audit Committee SP Audit N/AAnnual Report - Finance Committee BF Finance N/AAnnual Report - Healthcare Assurance Committee BA HAC N/AAnnual Report & Accounts - Final draft for approval SH Finance & Audit Cttees MonitorAnnual Report & Accounts - Going Concern Statement SH Finance & Audit Report & A/CsCQC RegistrationQuality and Risk Profile Update BA HAC CQCCharitable FundsAnnual Report & Accounts SH Charity Cmtte Charities Commission?HealthcareAssurance Framework BA HAC N/AChild Protection & Safeguarding Annual Report BA HAC N/AClinical Governance - Quartency Report BA HAC N/AClinical Governance - Annual Report BA HAC N/ADr Foster Quarterly Report MA Medical Director ?Quality Accounts - First Draft BA Clinical Governance N/AQuality Accounts - Final Draft for Approval BA Clinical Governance PublicationInfection Control<strong>Board</strong> Statement of Commitment to prevention of Healthcare Associated Infection BA Infection Control ?Infection Control - Annual Report BA Infection Control N/AInfection Control - Quarterly Update BA Infection Control N/AMonitorMonitor Quarter 1 Report HL Director of Ops MonitorMonitor Quarter 2 Report HL Director of Ops MonitorMonitor Quarter 3 Report HL Director of Ops MonitorMonitor Quarter 4 Results HL Director of Ops MonitorMonitor Annual Risk Assessment TS External Monitor?Monitor's FT Sector Overview - Annual Risk Assessment TS Chief Executive N/AMonitor Self Certification - <strong>Board</strong> Statements RL Trust Secretary MonitorStaff
What Who Where <strong>Board</strong> Before of Directors - Meeting Jan Map Feb Mar Apr May Jun Jul Sep Oct Nov Dec Where After 2Staff Excellence Awards - Chairman's Prize RR Awards Panel Staff AwardsStaff Excellence Awards - Process for current year RR Service Development N/AStaff Survey - Results KA Workforce ?Workforce Committee - Quarterly Report KA Workforce N/ALocal Clinical Excellence Awards MA Remuneration ?Local Clinical Excellence Awards - Annual Report MA Remuneration N/AGovernanceRegister of Interests RL Trust Secretary FileConstitutional Documents - Annual Review RL Trust Secretary CoGCode of Governance Disclosure Statement RL Trust Secretary MonitorMeeting Dates for Next Year RL Trust Secretary N/AForward Programme RL Trust Secretary N/AMinutes of Subordinate groupsAudit Committee Cttee Audit N/ACharity Committee Cttee Charitable Funds N/ACouncil of Governors RL CoG N/AFinance Committee Cttee Finance N/AHealthcare Assurance Cttee HAC N/AInfection Control Cttee Infection Control N/AMarketing Committee Cttee Marketing N/ARemuneration Committee Cttee Remuneration N/ATrust Management <strong>Board</strong> Cttee TMB N/AWorkforce Committee Cttee Workforce N/AReview Performance & Terms of Reference subordinate GroupsAudit Committee SP Audit File - RLCharities Committee KT Charitable Funds File - RLFinance Committee SH Finance File - RLHealthcare Assurance Committee BA HAC File - RLInfection Control Committee BA Infection Control File - RLMarketing Committee RR Marketing File - RLRemuneration Committee SC Remuneration File - RLTrust Management <strong>Board</strong> TS TMB File - RLWorkforce Committee KA Workforce File - RLCommunicationsCommunications Audit Action Plan RR Marketing ?Inpatient Annual Survey Results RR Marketing Publication?Marketing & Communications Report RR Service Development N/APutting Patients First - Quarterly Progress Report RR Marketing N/ARead All About It RR Service Development N/AService Guide RR Service Development ?