A G E N D A 1. APOLOGIES FOR ABSENCE Ian Metcalfe 2 ...
A G E N D A 1. APOLOGIES FOR ABSENCE Ian Metcalfe 2 ...
A G E N D A 1. APOLOGIES FOR ABSENCE Ian Metcalfe 2 ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
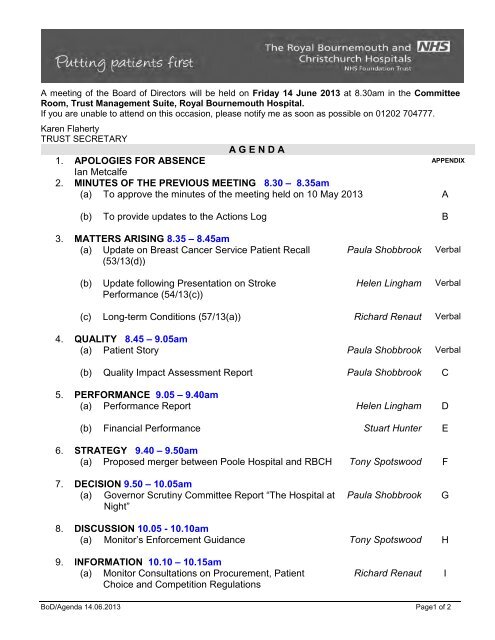
A meeting of the Board of Directors will be held on Friday 14 June 2013 at 8.30am in the CommitteeRoom, Trust Management Suite, Royal Bournemouth Hospital.If you are unable to attend on this occasion, please notify me as soon as possible on 01202 704777.Karen FlahertyTRUST SECRETARYA G E N D A<strong>1.</strong> <strong>APOLOGIES</strong> <strong>FOR</strong> <strong>ABSENCE</strong> APPENDIX<strong>Ian</strong> <strong>Metcalfe</strong>2. MINUTES OF THE PREVIOUS MEETING 8.30 – 8.35am(a) To approve the minutes of the meeting held on 10 May 2013 A(b) To provide updates to the Actions Log B3. MATTERS ARISING 8.35 – 8.45am(a) Update on Breast Cancer Service Patient Recall(53/13(d))Paula ShobbrookVerbal(b)Update following Presentation on StrokePerformance (54/13(c))Helen LinghamVerbal(c) Long-term Conditions (57/13(a)) Richard Renaut Verbal4. QUALITY 8.45 – 9.05am(a) Patient Story Paula Shobbrook Verbal(b) Quality Impact Assessment Report Paula Shobbrook C5. PER<strong>FOR</strong>MANCE 9.05 – 9.40am(a) Performance Report Helen Lingham D(b) Financial Performance Stuart Hunter E6. STRATEGY 9.40 – 9.50am(a) Proposed merger between Poole Hospital and RBCH Tony Spotswood F7. DECISION 9.50 – 10.05am(a) Governor Scrutiny Committee Report “The Hospital atNight”Paula ShobbrookG8. DISCUSSION 10.05 - 10.10am(a) Monitor’s Enforcement Guidance Tony Spotswood H9. IN<strong>FOR</strong>MATION 10.10 – 10.15am(a) Monitor Consultations on Procurement, PatientChoice and Competition RegulationsRichard RenautIBoD/Agenda 14.06.2013 Page1 of 2
(b)Monitor’s Designation Framework for CommissionerRequested Services/ Location Specific ServicesRichard RenautJ(c) Appointment of new Medical Director Tony Spotswood K(d) Core Brief (May) Tony Spotswood L(e) Communications Update (inc RAAI May) Richard Renaut M(f) Board of Directors Forward Programme Karen Flaherty N10. NEXT MEETINGFriday 12 July 2013 at 8.30am in the Committee Room, Royal Bournemouth Hospital1<strong>1.</strong> ANY OTHER BUSINESSKey Points for Communication12. COMMENTS AND QUESTIONS FROM THE GOVERNORS 10.15 – 10.30amBoard Members will be available for 10-15 minutes after the end of the Part I meeting to takecomments or questions from the Governors on items received or considered by the Board ofDirectors at the meeting.13. EXCLUSION OF PRESS AND PUBLIC AND OTHERSTo resolve that under the provision of Section 1, Sub-Section 2, of the Public BodiesAdmission to Meetings Act 1960, representatives of the press, members of the public andothers not invited to attend be excluded on the grounds that publicity would prove prejudicialto the public interest by reason of the confidential nature of the business to be transacted.BoD/Agenda 14.06.2013 Page2 of 2
THE ROYAL BOURNEMOUTH AND CHRISTCHURCH HOSPITALSNHS FOUNDATION TRUSTMinutes of a Meeting of The Royal Bournemouth and Christchurch Hospitals NHS FoundationTrust Board of Directors held on Friday 10 May 2013 in the Committee Room, RoyalBournemouth HospitalPresent:In attendance:Apologies:Jane StichburyTony SpotswoodKaren AllmanMary ArmitageDavid BennettBrian FordStuart HunterHelen Lingham<strong>Ian</strong> <strong>Metcalfe</strong>Steven PeacockAlex PikeRichard RenautPaula ShobbrookKen TullettKaren FlahertyPeter GillDily RufferTracey HallSue LangloisDamian JenkinsonJoseph KwanClare GordonMike AllenJayne BakerDavid BellamyGlenys BrownSue BungeySharon Carr-BrownDerek ChaffeyCarole DeasEric FisherLee FoordDoreen HolfordGraham SwetmanDavid TriplowMargaret NevilleNone(JS)(TS)(KA)(MA)(DB)(BF)(SH)(HL)(IM)(SP)(AP)(RR)(PS)(KT)(KF)(PG)(DR)(TH)(SL)(DJ)(JK)(CG)(MAll)(JB)(DBel)(GB)(SB)(SCB)(DC)(CD)(EF)(LF)(DH)(GS)(DT)(MN)Chairman (in the chair)Chief ExecutiveDirector of Human ResourcesMedical DirectorNon-Executive DirectorNon-Executive DirectorDirector of FinanceChief Operating OfficerNon-Executive DirectorNon-Executive DirectorNon-Executive DirectorDirector of Service DevelopmentDirector of Nursing and MidwiferyNon-Executive DirectorTrust SecretaryDirector of InformaticsGovernor Co-ordinatorHead of CommunicationsSenior Nurse, Medical Directorate (foritem 4(a) only)Consultant, Stroke Unit (for item 5(c) only)Consultant, Stroke Unit (for item 5(c) only)Consultant Stroke Nurse (for item 5(c)only)Public GovernorPublic GovernorPublic GovernorPublic GovernorPublic GovernorPublic GovernorPublic GovernorPublic GovernorPublic GovernorAppointed GovernorPublic GovernorPublic GovernorPublic GovernorMember of the PublicJS welcomed <strong>Ian</strong> <strong>Metcalfe</strong> to his first meeting following his recentappointment by the Board of Directors.BOD/Part 1MINS 10.05.13 PAGE 1 OF 16
50/13 MINUTES OF THE MEETING HELD ON 12 APRIL 2013 (Appendix A)The minutes of the meeting were taken as read and accepted as a truerecord of the meeting, subject to the correction of a couple of typographicalerrors.51/13 ACTIONS LOG (Appendix B)(a)29/13(a) Performance Report52/13 MATTERS ARISING53/13 QUALITYHL noted that this had been included on the agenda for Part 2 ofthe meeting initially.There were no matters arising.(a)Patient Story (Verbal)JS welcomed Sue Langlois to the meeting. PS explained how theway in which staff communicated with patients and their familiesor carers can change their experience while in the Hospital.SL described how an 80 year old patient with Parkinson's Diseaseand dysphasia had had a poor experience in the Trust on aprevious stay due to an issue with their medication which hadlengthened the patient’s stay. She noted that the patient's familywere still very angry but the lead nurse on the Ward had spokenwith the family and asked them to give the Trust an opportunity todemonstrate how it could do better. She described the care thepatient had received, adding that the patient's condition haddeteriorated rapidly and the Trust had managed the patient's endof life care so they got to die at home which was what the patientsand family had wanted. She concluded by noting that the familyhad written to the Trust to say that they would recommend theHospital to anyone and it had been a wonderful experience.PS highlighted that where patients have a bad experience of theHospital their faith and confidence in the Trust could be rebuilt.She commended the lead nurse on the Ward for her proactiveapproach to this and the confidence she had demonstrated in thestaff on the Ward by her commitment knowing that the patientwould need to receive their medication for Parkinson's Diseaseevery two hours. BF supported this, recognising the couragetaken to do this. AP also noted that this was a fantastic exampleof facing into problems and not being defensive and staff need toknow that they have the support of the Trust to deal with situationsin this way.BOD/Part 1MINS 10.05.13 PAGE 2 OF 16
In response to a question from KT about the initial cause forcomplaint, PS acknowledged that the delivery of medication everytwo hours did create pressures for staff but the knowledge fromthis Ward on how best to prioritise this would be shared with otherMedical wards. SP noted that the willingness to share this type ofstory demonstrated the maturity of the patient story format at theTrust. He asked whether staff were given training to deal withthese situations. PS replied that much was down to clinicalleadership in addressing issues immediately to stop theseescalating. She also noted that the Board discussion and supportfor staff to deal this so staff are aware of this.PG added that issues with patients' medication often arose onemergency admissions when the information about the patient'smedication was not always available. He highlighted that theEmergency Department (ED) had access to a Summary CareRecord and can access information from GPs directly. MA notedthat in this case the issue was due to how challenging it was togive the patient the medication on such a frequent basis.RR reported that the Patient Experience and CommunicationsCommittee (PECC) had discussed filming patient stories so thatthese could be shared more widely as they were very powerful. JSnoted the link to the Staff Survey and providing support for staff sothey feel empowered. She thanked SL for sharing the story andalso her contribution during Health Minister Dr Dan Poulter's visitto the Trust the previous day.(b) CQC Quality and Risk Profile (Appendix C)PS presented the paper, pointing out that the Trust remained lowrisk according to the assessment of the Care Quality Commission(CQC). She reported that she and TS had met with Sally Newell,the CQC's Regional Manager, who had explained the CQC's newmethodology for assessments and the new local assessor. Shenoted that the CQC's new inspection regime was to be announcedand the current outcomes would be grouped under five headings.She added that the CQC would be establishing a national team toundertake in-depth reviews of hospitals with significant or longstandingproblems and those applying to be foundation trusts.PS noted that they had raised the issue with the currency of someof the data used by the CQC and the CQC had clarified that thisdata was only part of the picture in terms of the overallassessment of the Trust and the Trust needed to be assured thatit was meeting these standards. In response to a question fromSP as to whether the Trust validated its performance against theCQC outcomes using more current data, PS explained theprocess of assessment of compliance by the responsiblecommittees using the results of audits and other evidence.BOD/Part 1MINS 10.05.13 PAGE 3 OF 16
JS stressed that the Trust should not be complacent and therewere issues that the Board would return to. PS endorsed thesecomments and the need to be vigilant.(c) CQC Inpatient Survey 2012 (Appendix D)PS presented the results of the latest CQC Inpatient Surveysummarising that:• 156 trusts had been surveyed;• the patients surveyed had been in hospital for more thanone night;• the Trust had been rated amber for 60 out of 61 questions,which meant that its performance was about the same asother trusts;• there had been an improvement in 18 areas;• the Trust's performance on the five CQUIN(Commissioning for Quality and Innovation) questions wasabove average; and• the Trust was categorised as red in one area which waswhether patients were given enough privacy whenexamined or treated and was the worst performing trust onthis question.PS noted that the Trust scored much better on its own internalsurvey results but this was not reflected in CQC survey and drewattention to the actions taken since the CQC's survey wasconducted in July 2012. She also noted that the range betweenthe top and bottom scores in the bandings was very narrow.PS explained that the actions to be taken had been discussed bythe PECC which would be driving this work forward. She addedthat the Trust was also looking at the data on a disaggregatedDirectorate level to provide information on areas for improvementwithin each Directorate.BF highlighted that over half the patients surveyed were admittedon an emergency or urgent basis and it was more difficult todeliver privacy and dignity in those areas than it was for plannedadmissions although this should not detract from the need for theTrust to do its best. SP, although noting that he did not want to beoverly critical, felt the presentation focussed on the data ratherthan focussing on the actions required. PS clarified that shewanted to provide all the relevant information to provide a fullunderstanding of the results. DB observed that the results from156 trusts were spread over seven basis points and that while theTrust being last should not be the principal cause for concern, itshould not detract from focus on the underlying issue.HL interjected that patients would be commenting on their wholestay, which would include the ED. She described that work whichhad been done in the ED using screens rather than curtains andBOD/Part 1MINS 10.05.13 PAGE 4 OF 16
how this was being rolled out throughout the Hospital. She alsonoted that there were not enough side rooms, which would alsohave benefits for infection control, and that the Trust needed tofind a way of increasing the number of side rooms butacknowledged that this was very difficult given the levels ofactivity currently.IM asked why there was such a difference in the results of theTrust's own internal surveys and the CQC survey. PS respondedthat the Trust collected its data from the patient comment cardsand real-time patient feedback and the Trust was continuing to rollthis out further to increase the sample size. She added thatpatients were often worried about giving a negative responsewhilst they were in Hospital on the basis that this could potentiallyaffect their treatment. Again, PS highlighted that this data wasprovided to the Wards each month so that improvements could bemade at that level.AP agreed that the sampling technique did have a bearing. Shereported that the results had been discussed at length at PECCwhich they felt were very disappointing and did not reflect the levelof work going on in the Trust in relation to the patient experience,which had a greater focus and drive than at any other time in theseven years she had been at the Trust. She added that the Trustneeded to speak to more patients to understand what they meantby privacy and dignity to get a richer understanding on this andhow to address the issue. JS agreed and added that patients'expectations had also changed over time.(d)Breast Care Service Update (Verbal)PS reported that the Trust had invited a number of patients whohad been seen by a junior doctor between January 2011 andAugust 2012 back to the Trust for a further breast careassessment by a consultant. She wanted to apologise to thepatients as this would obviously be a source of concern for them.She noted that the patients that the Trust had spoken to had beengrateful that the Trust had adopted this proactive stance. Sheadded that the helpline had worked very well with patients giventhe opportunity to speak to a nurse and a breast care specialistShe reported that letters had also been sent to local GPs andcommissioners, the Strategic Health Authority, the CQC and staffhad been briefed so that they were aware of what was happening.She noted that the junior doctor had been referred forinvestigation and the Royal College of Surgeons had been askedto assist with the Trust's internal review. She clarified that this wasunrelated to the national breast screening programme and thepatients affected were symptomatic patients referred by GPs.DB stressed that the investigation must focus on professionalBOD/Part 1MINS 10.05.13 PAGE 5 OF 16
54/13 PER<strong>FOR</strong>MANCEoversight to allow intervention at an earlier stage. PS confirmedthat this would be covered by the review. TS acknowledged thatthere would be questions about the supervision of the individualand the Trust would be able to provide further informationfollowing the review.KT mentioned that he had met two people who had been invitedfor a further assessment and both had been very complimentaryabout the sensitivity with which this has been handled. He addedthat he shared DB’s concerns about the need for a systematicprocess to assess performance. TS confirmed that medical staffwere required to have an appraisal annually but advised that itwould be better to wait for the full report following the review toaddress these concerns. JS underlined the importance of having avery full review.TS thanked PS and John Stevens for the way in which the recallof patients had been conducted operationally by providing theadditional capacity to run the clinics and setting up the helplinesas well as the interaction with the media which had given clearmessages about this being a precautionary measure.In response to a question from SP about the number of patientsseen and the timescale for seeing the remainder of patients, TSreplied that the Trust had seen half the current group of patientsand capacity was the only constraint. He added that the Trust hadmade good progress in a short period and often the weekendswas not the most convenient time for patients.(a) Performance Report (Appendix E)HL presented the report, highlighting:• the increase in emergency activity since March 2012although the Trust was not currently seeing patients in thesame peaks as in 2012/13;• that the Trust was achieving the 4 hour wait in the ED in thepast three weeks even with the high number of patients andthis was a credit to the staff;• that the Trust had achieved an aggregate of 94.8% patientsseen within four hours in April;• that there were 668 more ambulance handovers in ED thanin the previous year, which equates to an additional 50each week;• that there were still a number of patients who should be inMedical beds but who were in beds elsewhere in theorganisation although the numbers had reduced;• a reduction in the number of operations cancelled due tothe shortage of general or critical care beds available evenwith the two additional critical care beds but the Trust wasBOD/Part 1MINS 10.05.13 PAGE 6 OF 16
still challenged at times;• that the Trust had met the 18 week wait target at anaggregate level in April but Orthopaedics, General Surgery,Gynaecology and Urology were not expected to meet thetarget but the primary focus would remain on patient carerather than meeting targets;• that cancer referrals and outpatient activity were alsoputting pressure on Urology;• that there were two C Difficile cases in April and no casesof hospital acquired MRSA;• the 2 week cancer referral target was still challenging withthe upward trend of fast track referrals continuing;• there were a number of breaches for the 62 day cancertargets in Urology illustrating real pressure in the system;• she had visited St Leonards Community Hospital with thedirectors responsible at Dorset Healthcare University NHSFoundation Trust (DHUFT) and they were looking at how toopen up the second ward there in conjunction with theEstates team;• funding for emergency pressures had been allocated by theNHS Dorset Clinical Commissioning Group (CCG) for thefirst six months subject to assessing the widerrecommendations from the recent urgent care review;• the results of the Joint Advisory Group inspection ofEndoscopy, which had commended the team culture andapproach to patients, and although there wasdisappointment that the Trust’s re-accreditation had beendeferred for three months pending the action plan it wasacknowledged that no unit in UK had been givenaccreditation without deferment; and• that sickness levels were on a par with the previous month.TS added that there were some broader issues as DHUFT hadmade a substantial profit under a block contract when there werefacilities which were not available which had been raised withcommissioners.JS thanked HL and her team for their work in achieving apredominantly green position on the Monitor and contractualtargets at the year end, particularly given the levels of activity.In response to a question about the outliers and the number ofpatient moves, HL reported that an audit had been completed atMA’s instigation. She noted that this had revealed an issue withthe data as every move on a patient pathway was counted. Sheconfirmed that there were a small number of patients who hadbeen moved continually and there was very little evidence ofinappropriate moves but the recommendations from the auditwould allow the Trust to focus on any problem areas.BOD/Part 1MINS 10.05.13 PAGE 7 OF 16
KT asked whether there was any evidence of a wider appreciationof the issues with emergency activity among healthcare partnersin community. HL confirmed there were lots of discussions andthat there had been progress and they were working to allowdirect access to the out of hours GP service without anappointment by the end of May. She added that the Trust was stillworking with local GPs to increase their presence in ED Minors inaddition to ED Majors and also to ensure assessments for patientswith ongoing health and social care needs are carried outside ofthe hospital as more efficient.TS added that The King’s Fund had been commissioned toidentify the priorities locally and one of the recommendations waslikely to be that the acute trusts should manage communityhospitals in order to better align the incentives to move patientsout of an acute care setting into a more appropriate one.IM asked whether the performance issues with the 18 weekreferral to treatment targets were likely to continue while activitylevels remained high. HL replied that the Trust had prepared atrajectory for recovery and a capacity plan in order to achievecompliance in a clinically sustainable way between May andOctober in all specialities. She added that some breaches weredue to cancellations and complex pathways.(b) Financial Performance (Appendix F)SH presented the paper, noting that the year-end results weresubject to external audit. He reported that:• EBITDA had fallen due to a reduction in non-operatingexpenditure and a non recurrent increase in operatingexpenditure, the first related to the reduced capitalprogramme and a revaluation of the Trust’s asset base bythe District Valuer and the latter to the initial planning anddesign fees in relation to Christchurch Hospital;• the Trust had met the transformation plan for 2012/13 buthe expressed caution on the outlook for the coming year inparticular in the context of non-recurrent savings.He concluded that the 2012/13 performance had been excellentand there were no concerns relating to any Directorate.JS requested whether additional information on staff vacancylevels could be provided in the report to highlight areas wherevacancy levels were high. SH confirmed that the reporting relatedto unfilled clinical vacancies only and reported at an aggregatelevel across the Trust.SHBOD/Part 1MINS 10.05.13 PAGE 8 OF 16
(c)Stroke Performance (Presentation)Damian Jenkinson, Joseph Kwan and Clare Gordon joined themeeting.DJ commented that the concern shown by the Board and theCouncil of Governors both pleased and troubled him as heappreciated the priority and focus on the performance of theStroke Unit but was aware at the same time that the performancehad created some anxiety.DJ delivered his presentation, explaining that:• the targets for Stroke performance were measures of theprocess of care rather than clinical outcomes but it hadbeen demonstrated that the quality of the process waslinked to good outcomes;• patients’ survival and their ability to live independently washeavily influenced by their condition prior to their stroke;• 100% of patients should be directly admitted to the StrokeUnit and the recent dip in the Trust’s performance and themore recent recovery in performance;• the aspiration for 80% of patients to spend 90% of their stayon the Stroke Unit;• there was a pattern in terms of annual performance and theactions which had been taken had led to an improvementequating to a smaller dip in performance in 2012/13 thanthe previous year;• other performance measures relating to brain imaging andthrombolysis were provided with support from Radiologyand the Trust’s performance was close to the nationalaverage;• the introduction of a weekend service for TIA as it wasimportant to act quickly and prevent strokes in thesepatient;• both he and JK had worked weekends and this wasdelivering an excellent service, with imaging within 20minutes and the results within 25 minutes, although due tocoding issues they did not have data available yet;• the excellent, high quality service provided through EarlySupported Discharge (ESD) work which supported patientsoutside Hospital where they recover better;• the Stroke Unit was looking to expand the communityservice for patients who did not qualify for ESD due to theirmore complex needs;• the reduction in the number of beds when the Stroke Unitwas opened was due to the reduction in delays relating totransfer to Christchurch Hospital, ESD and increasedconsultant ward rounds and the Department of Health’sasset tool had been used to support these calculationswhich were still correct (although a different mix of bedsBOD/Part 1MINS 10.05.13 PAGE 9 OF 16
may be required) but was based on the assumption thatthere would be no delays in transfers out of the Hospital;• the national average length of stay was 20 days and theaverage length of stay on the Stroke Unit was 21 dayscurrently;• nursing levels in the Stroke Unit were slightly belowestablishment with some vacancies and new staff, includinga new Clinical Leader (PS and CG had been reviewingnurse staffing and skill mix on the Stroke Unit as this hadnot been part of the initial Nurse Staffing Review and wasslightly different given that there were both nurses andallied health professionals on the Stroke Unit.);• a Stroke outreach pilot within the Trust had begun whichhad demonstrated improved access to CT scan andswallow assessments but this could not be sustained due tostaffing shortages on the Stroke Unit and a business casewas being prepared to support this;• there was good consultant cover;• the Trust’s performance under the summary measure ofprocess of care in a national audit was above the nationalaverage but not in the top 20%;• the Trust was close to the volume of Stroke patients atwhich it would provide better and more cost-effective carewith better outcomes for patients and it would reach thatlevel with the merger; and• the relevant domains in the NHS Outcomes Framework andthe commissioner strategy for NHS Dorset CCG.He concluded that the priorities for the service were:• an Acute Outreach Team;• weekend specialist ward rounds;• a Stroke specialist community neurology team;• an improvement in stroke specific social care; and• for continuing health care assessments to take place incommunity settings.KT asked about the relationship between the process indicatorsused in the performance measures and outcomes for patients. DJresponded that outcomes were affected by the case mix but theTrust’s mortality rate was close to national average but this datahad not been systematically collected before but was now part ofthe Stroke National Audit Programme.IM asked whether the numbers of beds needed to be increased toaccommodate the issues with discharging patients, however DJnoted that the Trust needed to focus on resolving that issue ratherthan respond by increasing the number of beds.SP summarised the recommendations and asked how the Trustwould respond to these. HL responded that:BOD/Part 1MINS 10.05.13 PAGE 10 OF 16
• nurse staffing was already being reviewed as PS hadalready commented;• the business case for the Acute Outreach Team was beingprepared and needed to consider whether nurses or alliedhealth professionals could deliver this service;• the number of doctors was more difficult and getting to a 7day consultant presence presented a real challenge andneeded to be reviewed in the context of the general medicaltake and required creative thinking about how to do this inorder to make it affordable although it had been consideredin the context of the merger; and• discussions regarding continuing health care assessmentsin community settings had been discussed earlier.SP emphasised the need to reach agreement on what needed tobe done and to do so quickly in order to avoid a further dip inperformance. JS agreed and added that the Trust may need tolook closely at the need for investment.TS/HLTS added that there was a risk when looking at one service inisolation as HL had already stated. He noted that any additionalinvestment would need to be looked at in the and it needed to belooked at in the round in the context of other pressures in Urologyand in the Acute Admissions Unit ensuring the Trust maintained asustainable financial position. SH confirmed that this had not beendiscussed in detail as part of budget-setting.JK added that the Stroke Unit had demonstrated the benefit interms of patient outcomes on mortality, infection rates, venousthromboembolism, Adverse Incident Reports, readmissions andpatient satisfaction despite the process deficiencies highlightedbut maintaining outcomes for patients was causing some strain forthe service. He highlighted that an investment in processimprovement may lead to outcome improvement and also thatthere was a huge seasonal variation which could be reflected infuture funding, and the same was true of Medicine for the Elderly,and the Stroke Unit could also work more closely with Medicine forthe Elderly and the Acute Medical Unit to deliver therecommendations.AP and SCB shared some frustration that these recommendationshad not been discussed in budget-setting meetings.SCB was also concerned that the Board and the Governorspresent were also hearing this for the first time. She asked whatlevers the Trust had around discharge planning. HL added that theTrust was dealing with discharge planning across all areas and notjust the Stroke Unit. She described some of the actions includingthe ability for the Trust to instigate some re-ablement packagesdirectly and having social workers as part of multi-disciplinaryteams and agreed to bring information back to the Board toHLBOD/Part 1MINS 10.05.13 PAGE 11 OF 16
provide greater details on the work which was being done arounddischarge planningGB asked about the impact on outcomes for patients who werenot able to be admitted to the Stroke Unit. DJ acknowledged thatlots had been written about this and had shown that Stroke Unitsimprove the clinical outcomes for patients when compared togeneral medical wards. He added that the data around ESD hadcompared outcomes to patients on a Stroke Unit rather thangeneral medical wards and this demonstrated further improvementin outcomes for patients with ESD with mild to moderate strokes.DJ added that there were tariffs associated with stroke servicesand best practice for admitting patients to a fully specified StrokeUnit for example there was an additional £0.33m payable for theweekend TIA service.JS requested that the Board be provided with more information onthe outcomes measures for the Stroke Unit which had beenreferred to in the discussion. She thanked DJ, JK and CG for thepresentation and noted how she had been encouraged by thenational position.JS acknowledged that the questions which had been submitted bythe Governors would be answered by a subsequent briefing. DJ,JK and CG left the meeting.HLHL55/13 STRATEGY(a)Proposed Merger between Poole Hospital and RBCH(Appendix G)TS reported on the visit to the Hospital from Dr Dan Poulter MPwhich had been arranged after Christopher Chope MP had raisedquestions about the merger in Parliament.He confirmed that the Council of Governors had received adetailed brief on the Competition Commission process followingthe hearing and that there would be a further hearing in June. Herelayed the Competition Commission’s latest thinking in relation towhich services may be affected by a substantial lessening ofcompetition following the merger, which indicated that non-electiveservices, private activity and community activity would not beaffected and there may be a risk of a substantial lessening ofcompetition for outpatients and some elective activity. He notedthat any discussion about remedies would be likely to last throughJuly and August, but it was difficult to gauge at this stage, and theTrusts continued to work towards licensing of the merged trust inApril 2014.BOD/Part 1MINS 10.05.13 PAGE 12 OF 16
(b) Informatics Strategy (Appendix H)PG presented the report describing how the Trust’s InformaticsStrategy was clinically driven and the Trust’s vision. He noted thatthe National Information Strategy published in 2012 recognisedthe paperless hospital for first time. He highlighted the objectivesand drivers of the strategy, including:• the aim for all patient information to be collectedelectronically to allow access for multiple users at any time;• maximising safety and clinical quality;• improving efficiency;• supporting clinical decision-making;• improving digital channels for communicating and deliveringcare to patients;• assisting in the delivery of recommendations in the FrancisReport relating to the electronic patient record (EPR) andelectronic escalation; and• improving the way various organisations involved in apatient’s health and social care worked together, giving theexample the EPR being available to ambulance staff andthe electrocardiogram from the ambulance being availableto the teams in the Hospital.He explained that there were 27 projects and six workstreamswhich included those elements that provided the foundation for thenew tools and the new tools themselves. He concluded that thefunding for the strategy had been approved in principle by theFinance Committee and that this would be reviewed at leastannually and it had also been approved by the Board of Directorsat Poole Hospital on 25 April.In response to a question from SP about the level of resiliencebuilt into the plan, PG replied that innovations were tracked verycarefully and the Trust could look at other countries who werefurther ahead that the UK from an Informatics perspective to gaingreater insight.BF and TS questioned the possible impact of any financialdifficulties at Poole Hospital NHS Foundation Trust on the fundingand delivery of the strategy. PG responded that the delivery of thestrategy was dependent on the capital but that projects could bephased differently if this was an issue and also that someelements of the strategy were dependent on both Trusts workingtogether at same time, giving the example of the scanning ofpaper records.PS noted that the strategy was impressive and demonstrated howInformatics could help improve some of the risks arounddocumentation which the Trust had identified previously andreferred to eNEWS. She asked whether PG had confidence thatBOD/Part 1MINS 10.05.13 PAGE 13 OF 16
56/13 DECISIONthe Trust had the expertise and infrastructure to deliver thestrategy. He acknowledged that the Trust needed to keep thisunder review but the restructure for the new Directorate wascoming to a close and this had increased capacity at less seniorlevels.JS noted that the vision was right and addressed a number ofongoing wider issues within the health economy. She noted thattraining and ensuring the integrity and governance of the systemswas critical to its success.The Board approved the strategy.(a) Code of Governance Disclosure Statement (Appendix I)57/13 DISCUSSIONKF explained the review of compliance with Monitor's FoundationTrust Code of Governance and the need for the Trust to explainthe approach it had adopted in any areas of non-compliance. Sheadded that this would be submitted to Monitor alongside theAnnual Report and Accounts and highlighted the wording whichwould appear in the Annual Report.The Board approved the statement.(a) Long Term Conditions (Appendix J)JS highlighted that there had been a good discussion around longtermconditions at a recent Council of Governors’ seminar relatingto Health Promoting Hospitals. RR reported that theannouncement on the decision for self-care for long-termconditions in Dorset had been delayed but noted that this was theresult of work between all the foundation trusts in Dorset and thelocal charity Help and Care, providing a good example ofpartnership working. RR added that their bid was up againstUnitedHealth and the successor to NHS Direct whichdemonstrated that this was a highly contested area.JS requested that the result of bid be shared when known.RR58/13 IN<strong>FOR</strong>MATION(a)New Emergency Preparedness Resilience and Response(Appendix K)The report was noted for information.BOD/Part 1MINS 10.05.13 PAGE 14 OF 16
(b)Monitor’s Guidance for NHS Providers (Quality Governance)(Appendix L)The report was noted for information.BF added that the paper was one of best Monitor had producedand was something the Board could come back to and use tomeasure its performance against.(c) Core Brief (Appendix M)This was noted for information.(d) Communications Update (Appendix N)The report was noted for information.(e) Board of Directors Forward Programme (Appendix O)The report was noted for information.59/13 DATE OF NEXT MEETINGFriday 14 June 2013 at 8.30am, Committee Room, Royal BournemouthHospital60/13 ANY OTHER BUSINESSThere was no other business.61/13 Key Communications points for staff<strong>1.</strong> End of year performance figures and thanks to staff given thepressures in year2. Stroke3. Patient story and leadership and courage shown4. Informatics Strategy5. Breast care serviceJS referred to the discussions earlier in the meeting relating to theperformance of the Stroke Unit and the recall of breast service patients. Shenoted that the Trust was never complacent despite the high level ofperformance delivered in the previous financial year but it was a mark of anorganisation as to how it got through the more difficult periods. Sheacknowledged PS’s work in particular on the quality of care for patients.62/13 QUESTIONS FROM GOVERNORS<strong>1.</strong> DBel referred to the dignity and privacy issue from the CQC InpatientSurvey. PS added that the Trust was planning to do unannouncedaudits on privacy and dignity throughout the Trust.2. DBel asked how well the IT system at the Trusts would beBOD/Part 1MINS 10.05.13 PAGE 15 OF 16
coordinated with primary care records. PG responded that this wasincorporated in the vision and the ED was already drawinginformation from the Summary Care Record. He noted that theTrusts had a large number of GP practices in common which wouldbe the focus on work to share access to the full patient record withtheir consent. He noted that this would get easier as more progressis made nationally to support this.3. EF endorsed the proactive stance in relation to the patient recall forbreast cancer services. He asked how the Trust had communicatedwith representatives from local cancer charities. PS responded thatthe Trust had informed these local groups but had not needed orrequested their support in connection with the recall as the Trust hadestablished its own helpline. She added that the patients being calledback for a review may not have had cancer and therefore may neverhave been in contact with these groups.4. DH also asked about the recall, noting the good job that PS andother nurses had done with the patients affected. She asked whetherabout the monitoring of junior doctors. JS agreed that the Boardwould come back to this issue when the Trust had the results of theindependent review.5. DT asked whether the average age of Stroke patients in this areahad been take into account when considering the size of the StrokeUnit. MA noted that the number of beds was not necessarily linked tocost and explained that the aim of the London model had been tohave fewer Stroke Units and to provide a better service once thesewere centralised and merged.6. SB asked about IT services and whether there were plans to improvethe IT services for Governors. KF responded that there was aproduct available which had been identified by the IT team at theTrust and a business case was being prepared.7. MAll commented that the NHS appeared to be starting again lookingat the Informatics Strategy and wanted to ensure that the Trust couldwork better with other healthcare providers. PG responded that alltrusts were developing their information systems independentlywhich was now the national strategy and were using the samestandards for systems to ensure inter-operability rather than usingthe same systems. He added that the Royal Colleges also specifiedstandards in terms of what information should be contained withinsystems and records.8. MAll also asked about Never Events. MA noted that the latest datawas published the previous day and the Trust did not appear on thelist as it had no Never Events.There being no further business the meeting was declared closed.BOD/Part 1MINS 10.05.13 PAGE 16 OF 16
THE ROYAL BOURNEMOUTH AND CHRISTCHURCH HOSPITALSNHS FOUNDATION TRUSTActions carried forward from a Meeting of The Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust Board ofDirectors held on Friday 10 May 2013.54/13 PER<strong>FOR</strong>MANCE(b) Financial Performance (Appendix F)JS requested whether additional information on staff vacancy levelscould be provided in the report to highlight areas where vacancylevels were high.SHInformation atDirectorate/Departmentlevel now included infinance papers in Part2.(c)Stroke Performance (Presentation)SP emphasised the need to reach agreement on what needed to bedone and to do so quickly in order to avoid a further dip inperformance. JS agreed and added that the Trust may need to lookclosely at the need for investment.She described some of the actions including the ability for the Trustto instigate some re-ablement packages directly and having socialworkers as part of multi-disciplinary teams and agreed to bringinformation back to the Board to provide greater details on the workwhich was being done around discharge planningJS requested that the Board be provided with more information onthe outcomes measures for the Stroke Unit which had been referredto in the discussion. She thanked DJ, JK and CG for thepresentation and noted how she had been encouraged by thenational position.TS/HLHLHLIncluded on agendaunder Matters ArisingIncluded inPerformance Reportitem on the Boardagenda.Included inPerformance Reportitem on the Boardagenda.__________________________________________________________________________________________________________________BOD Actions Log 10.05.13 PAGE 1 OF 2
57/13 DISCUSSIONJS acknowledged that the questions which had been submitted bythe Governors would be answered by a subsequent briefing. DJ, JKand CG left the meeting.(a) Long Term Conditions (Appendix J)HLIncluded inPerformance Reportitem on the Boardagenda.JS requested that the result of bid be shared when known. RR Included on agendaunder Matters Arising__________________________________________________________________________________________________________________BOD Actions Log 10.05.13 PAGE 2 OF 2
BOARD OF DIRECTORSMeeting Date and Part: 14 th June 2013 – Part 1Subject:Quality Impact AssessmentSection:QualityExecutive Director withoverall responsibility:Author of Paper:Dr Mary Armitage, Medical DirectorPaula Shobbrook, Director of Nursing and MidwiferyJoanne Sims, Associate Director Clinical GovernanceGeraldine Sweeney, Transformation Programme ManagerKey Purpose Assurance x PerformanceAction required by BoDFor discussionPrevious Discussion: Healthcare Assurance Committee - 30 th May 2013Executive Summary:The following paper provides details of the Trust procedures in place to ensure qualityimpact assessments have been completed for all transformation schemes for 2013/14.The paper also outlines the directorate and Trust procedures for the on going review andreporting of progress against initial QIA proposals and metrics.HAC agreed that the new process is robust, although noted that the process only reviewsthe impact on quality and doesn’t comment on the credibility or likelihood of delivery.Strategic Goals &ObjectivesLinks to CQC RegistrationLinks to AssuranceFramework/Key RisksAllAll Essential Standards of Quality and SafetyAllType of Assurance All External – CQC
Quality Impact Assessment Process 2013/14BackgroundThe 2012/13 Operating Framework makes clear the requirement for NHS Trusts to ensure that allCIPS include a quality impact assessment and these are agreed by the Medical Director and Directorof Nursing.The requirement for QIAs is also cited in the following publications: Delivering sustainable cost improvement programmes, Monitor, January 2012 How to Quality Impact Assess Provider Cost Improvement Plans, National Quality Board, July2012Transformation Programme CycleThe Transformation Programme/CIP process can be summarised into the following steps:Budgets setDirectorates identify potential CIPS tomatch budgetsCIPS assessed for financial impactCIPS assessed for quality impact (QIA).Standard framework used, quality metricsidentified and linked to directorate qualitydashboard and clinical governancemonitoring structuresQIAs viewed and approved by MedicalDirector and Director of NursingCIPs and QIAs monitored by directoratesand variance or risks reported byexception at TMB monthlyCIPS adjusted accordingly
Quality Impact Assessments 2013/14The above process has been implemented for all transformation programmes (corporate and clinicalschemes) identified for 2013/14.All individual schemes have been quality impact assessed at directorate meetings. Support for the QIAprocess has been provided to directorates by the Transformation Programme Manager and AssociateDirector Clinical Governance.The QIA template has ensured that each scheme identifies the following: Directorate Project reference Scheme title Area of quality (Patient experience, patient outcome, safety) Quality impact (Improve, Maintain or Reduce quality) Risk rating (Improve = Green, Maintain = Amber, Reduce = Red) Data Source (Drop down menu provided linked to primary quality metrics to included on thenew Board and Directorate quality dashboards)AIRsSUIHSMRFriends and Family TestDelayed Transfer of CareReadmissionsMRSACDiffRTTLength of StayRegulatory ComplianceComplaintsSickness AbsenceStaffingAppraisalsMandatory TrainingMonitoring Forum (i.e. where the above metrics will be routinely discussed in addition to thedirectorate management & clinical governance forums)The three year plans incorporated a total of 145 individual clinical work streams, and include theRBCH 13/14 schemes. These work streams were impact assessed by the directorates andsubsequently reviewed by the Medical Director and Director of Nursing. Of the 145 work streamsreviewed, 11 were not approved and further information and assessment has been requested.
Full details of the QIAs for the clinical schemes is shown in Appendix A. A summary is providedbelow:DirectorateNo ofSchemesSchemes not approved by MedicalDirector and Director of Nursing atfirst reviewAnaesthetics 9 0Trauma and Orthopaedics 12 0Specialist Services 14 0Surgical Specialties 17 0Cardiology 5 0Acute Surgery 16 0PPT 28 PPT006, PPT011, PPT028 3Medicine 6 MED006 1Radiology 13 0Maternity 10 MAT008, MAT015 2Cancer Care 15 CA005, CA020, CA021, CA027, CA030 5Total 145 11Not signed offOngoing Monitoring of QIAsThe following process has been agreed at PMG:• Directorates will review current QIAs and clarify the specific metrics that will be used forongoing monitoring of performance and impact• Directorate will set KPI base lines for identified metrics in order to monitor variance in year andquantify positive or negative impact• Schemes will be monitored at Directorate Team meetings – or other relevant forums• Directorate will formally record status in monthly TMB reporting – TMB template to be amendedto enable reporting by exception• CIPs and QIAs to be reviewed exception at PMG• System for providing independent scrutiny to be devised• Directorate to raise to risk level at CGRC and HAC as appropriateRecommendationHAC agreed to support the QIA process for 2013/14 and recommends this to the Board of Directors
Example of completed QIATransformation Project / Business Case Title: Additional Nursing Template for X WardDescription of Impact (list allapplicable in each section)Reduction in patient complaintsImprovement in patient surveyRTPFAIRSHAIsHarm Free CareMEWS complianceRisk Assessment complianceSepsis managementFluid and HydrationNutritionPrivacy and DignityWaiting time complianceLength of StayReadmissionsSickness absenceMandatory training complianceArea of Quality(patient outcome,patientexperience,safety)PESSSPOPSPOPOPOPEPEPOPOSSQuality Impact(Improve,Maintain,Reduce)IIIIIIIIIIIIIIIIData SourceComplaints/PALSRTPF ResultsF&F CQUINAIRSAIRS/Saving LivesdataSafety ThermometerMEWS AuditAuditHSMRAuditAuditAuditActivity dataActivity dataActivity dataS/A reports(monthly)MT reports (monthly)MonitoringArrangementWardscorecard,CL meetingsWardscorecard,CL meetings,DirectorateRAGGMortality GrpWardscorecard,CL meetings,DirectorateRAGGPMGComment
BOARD OF DIRECTORSMeeting Date and Part:14 th June 2013 Part ISubject:Performance ReportSection:Executive Director withoverall responsibilityPerformanceHelen LinghamAuthor of Paper:David Mills/Donna ParkerDetails of previous discussionand/or dissemination:PMGKey Purpose:PatientSafetyHealth &SafetyPerformanceXStrategyAction required by BoD:InformationExecutive Summary:Strategic Goals & Objectives:Links to CQC Registration:(Outcome reference)Links to AssuranceFramework/Key Risks:This report accompanies the Performance Indicator Matrixand outlines the Trust’s performance exceptions againstkey access and performance targets for the month of April2013, as set out in the Monitor Compliance Framework,Operating Framework and contractual requirements.PerformanceSection 2 – Outcome 4: Care and welfare of people whouse services.Outcome - 6 Co-operating with others.PerformanceType of Assurance:InternalXExternal
Board of Directors Part 114th June 2013Performance Exception Report2012/13 - June1 Purpose of the ReportThis report accompanies the Performance Indicator Matrix and outlines the Trust’sperformance exceptions against key access and performance targets for the monthof April 2013, as set out in Everyone counts: Planning for Patients 2013/14, theMonitor Compliance Framework and in our contracts.2 Accident and EmergencyPerformance against 4 Hour Maximum Waiting TimeThe performance for April was 94.01%, below the threshold of 95%. Following aninitial below threshold performance this has now improved.3 CancerTwo week wait from referral to date first seen for symptomatic breast patientsTwo patients were not seen within two weeks due to patient choice. Due to the lownumber of referrals in the month, this also resulted in a below thresholdperformance, however, the target was achieved across the quarter.4 Stroke IndicatorsPerformance against Stroke Best Practice Tariff and Network indicatorsStrokeTotal Patients(April)Number ofPatients FailingTarget (April)April 2013TIA High Risk Patients 44 17 6<strong>1.</strong>4%TIA Low Risk Patients 22 3 86.4%Performance Monitoring Page 1 of 3For Information
Board of Directors Part 114th June 2013Alteplase (Thrombolysis) 3 0 100%90% Time Spent on Stroke Ward 55 21 6<strong>1.</strong>8%Direct Admission to Stroke Unitwithin 4 hoursBrain Imaging – urgent within 1hourBrain Imaging – other within 24hours50 23 54.0%16 1 93.8%51 5 90.2%TIA High Risk performance improved to 6<strong>1.</strong>4% compared to 40% in March. 17patients failed the target. Of these 7 were due to reduced clinics or clinics full, 2patients had a delay in GP referral, 2 changed appointment times and 1 was due topatient choice. TIA Low Risk performance improved to 86.4% in April compared to81% in March.Performance against the 90% time on the stroke unit target improved in April.6<strong>1.</strong>8% of patients had 90% of their stay on a Stroke Unit compared to 44% inMarch. 21 patients failed the target for various reasons including poor prognosis,treatment required prior to transfer, patients awaiting discharge transferred off of theunit and bed capacity.54% of patients had a Direct Admission to the Stroke Unit within 4 Hours comparedto 43.9% in March. Non compliance was primarily due to bed capacity and delayeddiagnosis, but also included patients with poor prognosis who were appropriatelymanaged on other wards. 64% of patients had a direct admission to the stroke unit(regardless of 4hr) compared to 58% in March.5 Cancelled OperationsPatients not seen within 28 days of cancellation - YTD Cumulative rate (
Board of Directors Part 114th June 20136 AttendanceSickness absence rate (4% current; 3% stretch)Sickness slightly increased in April with an absence rate of 3.58%, compared to3.55% in March. The Trust cumulative absence rate is 3.75%, which continues to bebelow the current target of 4% although above the stretch target of 3%.7 Appraisals90% of appraisals completed within one yearThe Trust achieved 68.51% compliance with the annual appraisal target in Aprilcompared to 70.58% in March. All directorates have developed an action plan andare confirming an indicative trajectory for recovery.8 Admitted RTT – Speciality Level90% of patients on an admitted pathway treated within 18 weeksAs previously anticipated at the Trust Board admitted RTT performance was belowthreshold in General Surgery, Urology, Orthopaedics and Gynaecology. These havebeen predominantly due to elective cancellations as a result of the urgent carepressures and the knock on impact of rebooking patients, as well as the impact offast track referral pathways.9 RecommendationThe TMB are requested to note the performance exceptions to theTrust’s compliance with the 2013/14 Monitor and OperatingFramework requirements.HELEN LINGHAMCHIEF OPERATING OFFICERPerformance Monitoring Page 3 of 3For Information
2013/14 PER<strong>FOR</strong>MANCE INDICATOR MATRIX <strong>FOR</strong> BOARD OF DIRECTORSArea Indicator Measure Target Monitor Jan-13 Feb-13 Mar-13 Apr-13RAG ThresholdsMonitor Governance Targets & IndicatorsInfection MRSA Bacteraemias Number of hospital acquired MRSA cases - Monitor de-minimis 6 <strong>1.</strong>0 00 > 1 trajectory < trajectoryReferral toTreatmentCancerRTT Admitted 18 weeks from GP referral to 1 st treatment – specialty level 90% <strong>1.</strong>0 9<strong>1.</strong>5%90.5% =90%RTT Non Admitted 18 weeks from GP referral to 1st treatment – specialty level 95% <strong>1.</strong>0 98.6%98.6% =95%RTT Incomplete pathway 18 weeks from GP referral to 1st treatment – specialty level 92% <strong>1.</strong>0 95.3%96.3% =92%2 week wait From referral to to date first seen - all urgent referrals 93%0.59<strong>1.</strong>4% 94.5% 93.1% =93%2 week wait From referral to to date first seen - for symptomatic breast patients 93% 93.1% 100.0% 92.0% =93%31 day wait From diagnosis to first treatment 96% 0.5 97.1% 97.1% 97.0% =96%31 day wait For second or subsequent treatment - Surgery 94% 100.0% 100.0% 100.0% =94%31 day wait For second or subsequent treatment - anti cancer drug treatments 98% <strong>1.</strong>0 100.0% 100.0% 100.0% =98%31 day wait For second or subsequent treatment - radiotherapy 94% =94%62 day wait For first treatment from urgent GP referral for suspected cancer 85%<strong>1.</strong>085.6% 86.5% 89.2% =85%62 day wait For first treatment from NHS cancer screening service referral 90% 100.0% 100.0% 100.0% =90%A&E 4 hr maximum waiting time From arrival to admission / transfer / discharge 95% <strong>1.</strong>0 96.8%94.0% =95%LD Patients with a learning disability Compliance with requirements regarding access to healthcare n/a 0.5 YesNo YesIndicators within the Operating Framework / Key Contractual PrioritiesTIA High Risk Patients High risk TIA cases investigated and treated within 24hrs 60% BPT 47% 61% 40% 61% < 50% 50% - 60% > 60%TIA Low Risk Patients % of patients seen, assessed & treated by stroke specialist < 7 days 100% BPT 83% 77% 81% 86% < 80% 80% - 90% >90%StrokeBrain Imaging – as per indicationsPatients with acute stroke meeting the indications receive brain imagingwithin 1 hr95% BPT 82% 71% 95% 94% < 80% 80% - 90% >90%Brain Imaging – other stroke Other stroke patients receive brain imaging within 24 hrs 100% BPT 95% 91% 92% 90% < 80% 80% - 90% >90%Direct admission to stroke unitPercentage of patients with suspected stroke admitted to a specialist strokeunit within 4 hrs of arrival90% BPT 54% 44% 44% 54% < 80% 80% - 90% >90%Alteplase (Thrombolysis) Percentage of appropriate patients receiving thrombolysis 100% BPT 100% 100% 100% 100% < 80% 80% - 90% >90%90% time spent on stroke wardPercentage of patients spending 90% or more of their time on the stroke wardduring their inpatient stay80% BPT 65% 33% 57% 62% < 70% 70% - 80% >80%MSA Mixed Sex Accommodation No of patients breaching the mixed sex accommodation requirement 0 0 0 0 0 > 0 0IC MRSA Bacteraemias Number of hospital acquired MRSA cases - national stretch 0 0 0 0 0 >= 1 0Cancer 62 day – Consultant upgrade Following a consultant’s decision to upgrade the patient priority * 90% 100.0% 100.0% 100.0% < 90% >=90%VTE Venous Thromboembolism Risk assessment of hospital-related venous thromboembolism 90% 93.7% 94.2% 94.2% 90.5%Diagnostics Six week diagnostic tests Less than 1% of patients to wait longer than 6 wks for a diagnostic test = 1% 0.9%-0.99%
Area Indicator Measure Target Monitor Jan-13 Feb-13 Mar-13 Apr-13 RAG ThresholdsE.D. QualityIndicatorsPatient Impact Indicator Achieve at least one of the Patient Impact Indicators Y Y Y No YesTimeliness Indicator Achieve at least one of the Timeliness Indicators Y Y Y No YesAmbulance Handovers No of breaches of the 30 minute handover standard tbc 3.1% 2.6% 3.3% <strong>1.</strong>1%CancelledOperationsWorkforceElective cancelled operations Cancelled Ops on day of admission as % of elective admissions < 0.7% 0.7% 0.6% 0.8% 0.4% >0.7% 0.65%-0.7% 4% 3% - 4% < 3%Appraisals Percentage compliance with annual appraisals 90% 74.71% 73.14% 70.58% 68.51% < 70% 70% - 89.9% >= 90%RTT Admitted 100 - General Surgery 90% 92.9% 88.6% 90.5% 85.5% =90%RTT Admitted 101 - Urology 90% 92.8% 90.0% 85.9% 82.7% =90%RTT Admitted 110 - Orthopaedics 90% 9<strong>1.</strong>5% 86.8% 83.6% 89.4% =90%RTT Admitted 130 - Ophthalmology 90% 9<strong>1.</strong>0% 9<strong>1.</strong>3% 90.5% 92.3% =90%RTT Admitted 140 - Oral surgery 90% 100.0% 92.3% 100.0% 97.2% =90%RTT Admitted 300 - General medicine 90% 98.3% 99.7% 99.2% 97.9% =90%RTT Admitted 320 - Cardiology 90% 92.9% 92.1% 95.1% 94.0% =90%RTT Admitted 330 - Dermatology 90% 94.5% 95.8% 93.3% 96.2% =90%RTT Admitted 410 - Rheumatology 90% 98.1% 94.6% 100.0% 95.8% =90%RTT Admitted 502 - Gynaecology 90% 94.8% 90.2% 85.8% 8<strong>1.</strong>9% =90%RTT Admitted Other 90% 96.9% 98.1% 96.9% 98.3% =90%RTTSpecialtyRTT Non admitted 100 - General Surgery 95% 98.7% 98.3% 96.6% 97.6% =95%RTT Non admitted 101 - Urology 95% 99.0% 99.1% 98.9% 98.8% =95%RTT Non admitted 110 - Orthopaedics 95% 98.1% 98.5% 100.0% 100.0% =95%RTT Non admitted 120 - ENT 95% 99.1% 98.9% 95.3% 99.0% =95%RTT Non admitted 130 - Ophthalmology 95% 100.0% 100.0% 99.8% 100.0% =95%RTT Non admitted 140 - Oral surgery 95% 95.0% 98.3% 95.1% 95.0% =95%RTT Non admitted 300 - General medicine 95% 97.9% 95.9% 96.2% 96.3% =95%RTT Non admitted 320 - Cardiology 95% 98.1% 98.3% 97.8% 97.6% =95%RTT Non admitted 330 - Dermatology 95% 99.7% 99.6% 100.0% 99.2% =95%RTT Non admitted 340 - Thoracic medicine 95% 100.0% 100.0% 98.8% 99.1% =95%RTT Non admitted 400 - Neurology 95% 97.1% 100.0% 98.5% 98.9% =95%RTT Non admitted 410 - Rheumatology 95% 97.1% 97.0% 96.9% 98.0% =95%RTT Non admitted 502 - Gynaecology 95% 99.1% 99.1% 98.9% 99.0% =95%RTT Non admitted Other 95% 99.6% 99.7% 99.3% 100.0% =95%vrbhinfo / performance management / board tmb / 2013-2014 / Performance Indicator Matrix for June 13 Board Final v2 Page 2 of 2
• Trust Balanced Dashboard –• Quality, Performance, Productivity and Efficiency• Reporting Month: Apr 2013• Report produced: 07/06/2013 16:05:24
Trust Performance Dashboard – Quality, Performance, Productivity andEfficiency: Apr 2013QualityProductivity & WorkforceKPI Units Actual PlanLastMonthLastYear12 Month Trend KPI Units Actual PlanLastMonthLastYear12 Month TrendHSMR* Index TBC 100 TBC TBC Medical outliers No. TBC TBC TBC TBC# of Deaths* No. TBC TBC TBC Average length of Stay Days 5.1 4.7 4.2% Harm Free Care (Patient SafetyThermometer)% 88.5% 95.0% 90.0% 90.6% Theatre session utilisation % 85.1% 85.0% 85.6% 86.1%Serious incidents No. 4 TBC 3 1 Outpatient New-to-Follow-Up ratio Ratio 0.60 0.58 0.64Emergency Department Friends &Family TestScore 58 80 52 Sickness absence % 3.6% 3.0% 3.6% 3.2%Inpatient Friends & Family Test Score 78 80 76 Vacancy % 5.6% 6.6% 6.3%Delayed Transfers of Care No. 5 TBC 14 11 Appraisals % 69% 90% 71% 87%30 day readmissions No. 463 569 534 Mandatory training compliance % 80% 78% 71%PerformanceActivity & FinanceKPI Units Actual PlanLastMonthLastYear12 Month Trend KPI Units Actual PlanLastMonthLastYear12 Month TrendMRSA Bacteraemias No. 0 0 0 0 # ED of attendancesED Attendances No. 6,731 6,592 5,665 5,291Clostridium difficile No. 2 2 5 3 Elective admissions No. 5,415 5,145 5,093 4,813RTT metrics (below plan) No. 0 0 0 0 Non-elective admissions No. 2,396 2,264 2,966 2,486Cancer metrics (below plan)* No. 1 0 0 GP OP Referrals No. 5,384 4,718 5,052 4,718Stroke metrics (below plan) No. 3 0 4 2 Risk ratings Rating 3.7 3.4 3.3A&E 4 hr maximum waiting time % 94.0% 95.0% Surplus £000s £ 346 £ 248 £ 312 £ 101Patients with a learning disability(Monitor compliance)Y / N TBC Y Y 100% Transformational plans £000s £ 632 £ 754 £ 726 £ 487• *Metric reported 1 month in arrears in monthly views; quarterly values are unadjusted• Report produced: 07/06/2013 16:05:252
BOARD OF DIRECTORSMeeting Date and Part:14 June 2013 - Part ISubject:Financial PerformanceSection:Executive Director withoverall responsibilityPerformanceStuart Hunter, Director of FinanceAuthor of Paper:Pete Papworth, Deputy Director of FinanceDetails of previous discussionand/or dissemination:Finance Committee and Trust Management BoardKey Purpose:PatientSafetyHealth &SafetyPerformanceXStrategyAction required by BOD:For InformationExecutive Summary:Review of the financial performance for Month 1 2013Strategic Goals & Objectives:Goal 7 – Financial StabilityLinks to CQC Registration:(Outcome reference)Outcome 26 – Financial PositionLinks to AssuranceFramework/Key Risks:Type of Assurance:InternalXExternal
Board of DirectorsJune 2013Financial Performance<strong>1.</strong> IntroductionThis report summarises the Trust’s financial performance for April 2013. A financialoverview is attached at Annex A.2. OverviewThe Trust is planning a cumulative surplus for the year of £<strong>1.</strong>25 million, representing asmall proportion (half a percent) of the Trust’s £250 million turnover. Thisdemonstrates sound and prudent financial planning, allowing the capacity to invest infuture years.This budget plan does however include a further 4% efficiency requirement in order tocover the many cost pressures experienced by the acute sector. As indicated inprevious reports, the achievement of these further efficiencies becomes more difficultin time as the Trust has transformed services over many years and benchmarks well at91% on the reference cost indicator.3. Key FinancialsNet SurplusThe Trust has delivered a net surplus of £347,000 during April, against a budgetedsurplus of £248,000. This represents a favourable variance to plan of £98,000.Earnings Before Interest, Taxation, Depreciation and Amortisation (EBITDA)The EBITDA ratio is one of the key performance indicators the Foundation Trust ismonitored against. April reported a return of 6.7% against a plan of 6.3%. Theforecast for the year is a return of 5.5%.Transformation ProgrammeThe Trust has a strong track record of delivering significant efficiency savings, and asa result, has a Reference Cost Index of 9<strong>1.</strong> This means that the Trust provides a mixof services at lower than the national average cost, indicated by an index of 100.It is recognised, however, that to continue to deliver such levels is becoming ever moredifficult as a single organisation. As a result, all transformation schemes are subject toa comprehensive Quality Impact Assessment. The process of monitoring these planshas been enhanced further in 2013, with a monthly mechanism to measure whetherthere is any potential adverse effect on the quality of the service provided.The savings requirement for 2013/14 is £10.3 million, with savings recorded duringApril amounting to £632,000 against a target of £754,000. Whilst it is expected thatfurther schemes will come on stream throughout the year, some concerns areapparent within a small number of directorates.Financial Performance Page 1 of 3For information
Board of DirectorsJune 2013The Service Improvement and Transformation Team continue to support directoratesin the identification of further savings opportunities.Capital expenditureCapital expenditure in April totalled £169,000 against a plan of £130,000. This smallover spend is due to a number of schemes commencing ahead of plan. The Trust isplanning total capital expenditure of £9.475 million during 2013/14.4. Financial Risk RatingThe Trust’s overall financial risk rating as at 30 April was a rating of 4. This strongperformance reflects the favourable variance to plan for month one; however theexpectation is that the Trust will end the year with a rating of 3. The best possible(lowest risk) rating is a rating of 5.5. ActivityOverall, activity was <strong>1.</strong>9% above budgeted levels in April, continuing the trend seenthroughout 2012/13. The key pressures in relation to non elective activity remain, withactivity above the 2008/09 threshold attracting only 30% of the PbR tariff.Activity in April was 3.3% above that seen in April last year, with elective admissionsand emergency department attendances being the main drivers of this. Outpatient andnon elective activity were both below the same period last year.6. Income and ExpenditureDuring April the Trust earned income of £2<strong>1.</strong>1 million against a budget of £20.6 million,being a favourable variance of £0.5 million. Expenditure during April totalled £20.7million against a budget of £20.4 million, being an adverse variance of £0.4 million.These variances are mainly attributable to a number of additional activities that theTrust has resourced and implemented to support the management of emergencypatient flow given the ongoing pressures experienced. This has been recognisedthrough the agreement of additional income from the Dorset Clinical CommissioningGroup.7. WorkforceUnfilled vacancies within clinical directorates’ year to date stand at 43 Whole TimeEquivalents, equating to a vacancy rate of <strong>1.</strong>5%. Recorded sickness increasedmarginally from 3.55% in March to 3.58% in April, increasing the rolling twelve monthcumulative sickness level to 3.75%.Financial Performance Page 2 of 3For information
Board of DirectorsJune 20138. RecommendationThe Trust is planning the delivery of all financial duties, with a planned surplus of £<strong>1.</strong>25million demonstrating that financial budgetary control is well embedded within the dayto day activities of the organisation.It is recognised, however, that to continue to deliver the level of savings required isbecoming ever more difficult as a single organisation. As a result, directorate savingsplans will need to be closely monitored to ensure that any areas of concern arehighlighted early and addressed promptly.Members are asked to note the Trust’s financial performance for the period to 30 April2013.Pete PapworthDeputy Director of FinanceMay 2013Financial Performance Page 3 of 3For information
ANNEX ATHE ROYAL BOURNEMOUTH AND CHRISTCHURCH HOSPITALS NHS FOUNDATION TRUSTFINANCIAL PER<strong>FOR</strong>MANCE <strong>FOR</strong> THE PERIOD TO 30 APRIL 2013KEY FINANCIALS2012/132013/14 YEAR TO DATE 2013/14 FULL YEARYTD ACTUAL PLAN ACTUAL VARIANCE VARIANCE PLAN <strong>FOR</strong>ECAST VARIANCE VARIANCE£'000 £'000 £'000 £'000 % £'000 £'000 £'000 %NET SURPLUS/ (DEFICIT) 101 248 346 98 40% 1,250 1,250 0 0%EBITDA 1,316 1,288 1,409 121 9% 13,745 13,745 0 0%TRANS<strong>FOR</strong>MATION PROGRAMME 487 754 632 (122) (16%) 10,345 10,345 0 0%CAPITAL EXPENDITURE 374 130 169 39 30% 9,475 9,475 0 0%FINANCIAL RISK RATING2012/132013/14 YEAR TO DATE 2013/14 FULL YEARYTD ACTUAL PLAN ACTUAL RISK WEIGHTED PLAN <strong>FOR</strong>ECAST RISK WEIGHTEDMETRIC METRIC METRIC RATING RATING METRIC METRIC RATING RATINGEBITDA Margin % 6.9% 6.3% 6.7% 3 0.8 5.5% 5.5% 3 0.8EBITDA Achievement of Plan % 102.2% 100.0% 109.4% 5 0.5 94.3% 94.3% 4 0.4Net Return after Financing % 0.3% <strong>1.</strong>4% 2.1% 4 0.8 0.5% 0.5% 3 0.6I&E Surplus Margin % 0.2% <strong>1.</strong>2% <strong>1.</strong>5% 3 0.6 0.5% 0.5% 2 0.4Liquidity Days 55.1 57.9 58 4 <strong>1.</strong>0 56.4 56.4 4 <strong>1.</strong>0FINANCIAL RISK RATING 3.7 3.2ACTIVITY2012/132013/14 YEAR TO DATE 2013/14 FULL YEARYTD ACTUAL PLAN ACTUAL VARIANCE VARIANCE PLAN <strong>FOR</strong>ECAST VARIANCE VARIANCENUMBER NUMBER NUMBER NUMBER % NUMBER NUMBER NUMBER %Elective 4,584 5,146 5,419 273 5% 62,242 62,242 0 0%Outpatients 23,969 22,827 22,974 147 1% 276,102 276,102 0 0%Non Elective 2,487 2,265 2,396 131 6% 27,559 27,559 0 0%Emergency Department Attendances 5,291 6,592 6,731 139 2% 80,203 80,203 0 0%TOTAL PbR ACTIVITY 36,331 36,831 37,520 689 2% 446,107 446,107 0 0%INCOME2012/132013/14 YEAR TO DATE 2013/14 FULL YEARYTD ACTUAL PLAN ACTUAL VARIANCE VARIANCE PLAN <strong>FOR</strong>ECAST VARIANCE VARIANCE£'000 £'000 £'000 £'000 % £'000 £'000 £'000 %Elective 5,446 6,040 6,078 39 1% 73,053 73,053 0 0%Outpatients 2,839 2,840 2,830 (9) (0%) 34,345 34,345 0 0%Non Elective 4,437 4,210 4,197 (13) (0%) 51,227 51,227 0 0%Emergency Department Attendances 514 624 618 (6) (1%) 7,597 7,597 0 0%Non PbR 4,109 4,974 5,171 197 4% 60,156 60,156 0 0%Non Contracted 1,719 1,739 2,011 272 16% 20,137 20,137 0 0%Research 128 153 163 10 7% 1,834 1,834 0 0%Interest 11 33 0 (33) (99%) 400 400 0 0%TOTAL INCOME 19,202 20,613 21,069 456 2% 248,750 248,750 0 0%EXPENDITURE2012/132013/14 YEAR TO DATE2013/14 FULL YEARYTD ACTUAL PLAN ACTUAL VARIANCE VARIANCE PLAN <strong>FOR</strong>ECAST VARIANCE VARIANCE£'000 £'000 £'000 £'000 % £'000 £'000 £'000 %Pay 11,515 12,105 12,301 (196) (2%) 143,719 143,719 0 0%Clinical Supplies 2,547 2,484 2,534 (49) (2%) 33,778 33,778 0 0%Drugs 1,978 1,978 2,077 (99) (5%) 24,004 24,004 0 0%Other Non Pay Expenditure 1,707 2,457 2,460 (3) (0%) 31,086 31,086 0 0%Research 128 153 163 (10) (7%) 1,834 1,834 0 0%Depreciation 801 801 801 0 0% 8,431 8,431 0 0%PDC Dividends Payable 425 387 387 0 0% 4,646 4,646 0 0%TOTAL EXPENDITURE 19,101 20,365 20,723 (358) (2%) 247,500 247,500 0 0%STATEMENT OF FINANCIAL POSITION2012/132013/14 YEAR TO DATE 2013/14 FULL YEARYTD ACTUAL PLAN ACTUAL VARIANCE VARIANCE PLAN <strong>FOR</strong>ECAST VARIANCE VARIANCE£'000 £'000 £'000 £'000 % £'000 £'000 £'000 %Non Current Assets 148,621 144,749 144,782 33 0% 146,266 146,266 0 0%Current Assets 62,319 68,546 67,866 (680) (1%) 67,593 67,593 0 0%Current Liabilities (25,865) (26,853) (25,954) 899 (3%) (26,691) (26,691) 0 0%Non Current Liabilities (3,253) (2,788) (2,789) (1) 0% (2,357) (2,357) 0 0%TOTAL ASSETS EMPLOYED 181,823 183,654 183,905 251 0% 184,811 184,811 0 0%Public Dividend Capital 78,674 78,674 78,674 0 0% 78,674 78,674 0 0%Revaluation Reserve 68,498 64,488 64,485 (3) (0%) 64,488 64,488 0 0%Income and Expenditure Reserve 34,651 40,493 40,746 253 1% 41,649 41,649 0 0%TOTAL TAXPAYERS EQUITY 181,823 183,655 183,905 250 0% 184,811 184,811 0 0%WORK<strong>FOR</strong>CE2012/132013/14 YEAR TO DATE 2013/14 FULL YEARYTD ACTUAL PLAN ACTUAL VARIANCE VARIANCE PLAN <strong>FOR</strong>ECAST VARIANCE VARIANCE% %Staff (Whole Time Equivalents) 3,553 3,694 3,682 12 0.3% 3,633 3,633 0 0.0%Sickness 3.43% 3.00% 3.75% (0.75%) (25.0%) 3.00% 3.50% 0.50% 16.7%
BOARD OF DIRECTORSMeeting Date and Part: 14 June 2013 Part 1Subject:Section:Proposed merger of The Royal Bournemouth andChristchurch Hospitals NHS FT and Poole Hospital NHS FTStrategyExecutive with OverallResponsibilityTony SpotswoodAuthor of Paper:Details of previousdiscussion and/ordissemination:Key Purpose:Tony SpotswoodOngoing discussions regarding the mergerPatient Safety Health & Safety Performance StrategyXXAction required by BoD:To note progressExecutive Summary:Strategic Goals &Objectives:Links to CQCRegistration: (Outcomereference)Links to AssuranceFramework/Key Risks:Type of Assurance:To update the Board on current work regarding the proposedmergerMaintaining local servicesQuality and SafetyQuality and SafetyInternalExternalX
Board of Directors Part 114 June 2013The proposed merger of The Royal Bournemouth and ChristchurchHospitals NHS FT and Poole Hospital NHS FTThe Trusts are due to hold second separate hearings with the CompetitionCommission on 11 June. These discussions will principally focus on the areas ofoverlap between the two organisations, the CC’s attempt to define our market, thecounterfactual, maternity services and the competitive effect on elective services.At this stage the emerging CC papers argue the Trusts provide a range of serviceswhich they do not. This is despite clear evidence to the contrary. It is cruciallyimportant that the lay panel are fully aware of this fact as otherwise the degree ofoverlap is overstated. This has emerged as a result of the CC seeking toreapportion patient activity attributed to general medicine and general surgery. Afull update on the hearing will be given at the Board meeting.Once concluded the Trusts expect to receive, by the end of June, the provisionalfindings of the Competition Commission. This will then generate a series ofdiscussions regarding potential remedies which the CC would see as an importantmeans of mitigating any perceived significant lessening of competition. From thework that has been undertaken to date the areas it is most concerned about relateto elective and maternity services.An important recent development has been an acknowledgement from Monitor thatin the absence of merger and financial support from the CCG, (which they are clearwill not be forthcoming), then Poole will face very significant financial pressures.The Competition Commission had previously argued that this was unlikely to impacton the future of the Trust; Monitor are, however, clear in view of recent informationprovided to them by Poole Hospital, that this will create significant pressure. TheCC will need to weigh this development very carefully in considering any potentiallessening of competition.Work continues now led by Mary Sherry to develop a more detailed set of plansunderpinning the likely savings to accrue as a result of the merger. It is importantthat all directorates are able to complete their Post Transaction Integration Plans(PTIPs) and detail savings/efficiencies that will be generated in 2014/15 and2015/16. The two Trusts are currently working to identify whether the savings aresufficient to maintain a balanced financial position for any new merged organisation.Monitor will want to be satisfied that the new organisation is financially viable. It ispossible that further discussions will be required with commissioners concerning theneed to provide transitional support for the new organisation. These discussionshave not yet taken place but will be important in helping maintain the financial healthof a new organisation. The Cost Improvement Plans of each directorate will bereviewed in detail on 1 and 2 July. This scrutiny is critical to ensure that we haverobust plans going forward and these will be independently tested through KPMGand Monitor’s assessment of the proposed organisation.Work will commence in the Autumn to determine the options to be put forward forconsultation with regard to the future configuration of a range services includingthose previously discussed. It is important for me to emphasise that no decisionshave been taken with regard to the future siting of services and both TMB and HEGProposed Merger Page 1 of 2Strategy
Board of Directors Part 114 June 2013will need to consider and agree both the model of care for various services as wellas options for the siting of reconfigured services, which will be fully consulted onpost-merger. During the Autumn we will also work through the sequencing of capitalinvestment to support the proposed reconfiguration of services.A more detailed update on the merger will be given at the Board meeting.Tony SpotswoodChief ExecutiveProposed Merger Page 2 of 2Strategy
BOARD OF DIRECTORSMeeting Date and Part: 14 June 2013 - Part 1Subject:The Hospital at NightSection:Executive Director withoverall responsibilityAuthor of Paper:Details of previous discussionand/or dissemination:Quality / PerformancePaula ShobbrookThe Governor Scrutiny Committee(David Bellamy and Sharon Carr-Brown)Governor Scrutiny CommitteeKey Purpose:PatientSafetyxHealth &SafetyPerformancexStrategyAction required by BoD:For DecisionExecutive Summary:Strategic Goals & Objectives:Links to CQC Registration:(Outcome reference)Links to AssuranceFramework/Key Risks:The Scrutiny Committee’s remit is to select a topic relevantto patient care or patient services for scrutiny each year.The committee wished to understand better the operationand culture of the Royal Bournemouth Hospital at night - isthere any difference in care offered during the night fromduring the day?• To listen to, support, motivate and develop our staff• To offer patient centred services by providing highquality, responsive, accessible, safe, effective andtimely care• To promote and improve the quality oif life of ourpatients• To strive towards excellence in the services and carewe provide• Outcome 4 – Care and welfare of people who useservices• Outcome 14 – Supporting workersVariousType of Assurance: Internal X External
Board of Directors Part 114 June 2013<strong>1.</strong> IntroductionGovernor Scrutiny Committee Report 2013The Hospital at NightThe Governor Scrutiny Committee is a committee of the Council of Governorsand is accountable to it. The remit of the committee is to select a topicrelevant to patient care or patient services for scrutiny each year. The topic ischosen to address an issue not covered by formal Trust scrutiny or whereGovernors feel further insight would be helpful to understand overallperformance.2. SummaryThe committee wished to understand better the operation and culture of theRoyal Bournemouth Hospital at night. With a drive to provide services 24-hours a day, seven days a week and the hospital under pressure fromunprecedented levels of admissions, it was felt an appropriate time to look atwhether there were any differences in care offered during the night and duringthe day.The committee decided to take an overview of the Royal BournemouthHospital at night during the month of February and the first two weeks ofMarch 2013. This was a period of very high admissions. Previously, theClinical Site Team had been visited during January to give committeemembers a better understanding of how the hospital worked before startingour research. Nine wards were selected: at least five staff (two Health CareAssistants and three registered nurses) and ten patients from each wereinterviewed using a questionnaire.We would like to thank our fellow governors, Derek Dundas, Doreen Holford,Jayne Baker and Sue Bungey for helping us carry out the research.3. Process3.1 Selection of topicAs is usual practice, the topic ideas were discussed with the Director ofNursing at the beginning of the scrutiny cycle and agreed upon as oneswhich fulfilled useful criteria for the Trust, patients and governors. TheCouncil of Governors was consulted before a final decision was taken bythe committee.1The Hospital at NightQuality/Performance
Board of Directors Part 114 June 20133.2 Initial actionOver two nights in January, the scrutiny committee members spent anevening with the Clinical Site Team (CST) to learn how the hospitaloperates at night, how it is staffed and to visit wards. The CST was veryhelpful and open with us and this insight helped us with our latersurveys. We would like to thank BJ Waltho and her team for their help,as well as the CST.We also met the doctors on duty at night, being present for theirhandover at 11pm. During one of our January visits, one of thecommittee witnessed the pressure the single surgical doctor (F1) in thehospital at night feels when they were found visibly upset and worriedabout coping.4. InvestigationNine wards were selected as representative of the hospital and at least fivestaff and ten patients were interviewed from each using a questionnaire. Thequestionnaires were developed with input from the Director of Nursing.Tabulated results for the questionnaires can be found at Appendices A, B, Cand D.The nine wards visited in this survey were:Ward 1Ward 14Ward 2Ward 15Ward 9Ward 22Ward 24AMUStrokeThe following report has been written in two parts - a patient report and a staff report,each including its own conclusions and recommendations.The Governor Scrutiny Committee is grateful to all staff and patients involved inproviding information and support for this report.2The Hospital at NightQuality/Performance
Board of Directors Part 114 June 20135. PATIENT REPORT5.1 Introduction91 patients were interviewed across all 9 wards. Typically 10 patients wereinterviewed from each ward, with the exception of Ward 1, where 11 wereinterviewed. The full, tabulated results for all wards can be found at AppendixA. A ward-by-ward breakdown can be found at Appendix C.5.2 Results and responses5.2.1 Do you think there are enough nursing staff on this ward at night?56% of patients felt there were enough nursing staff on their ward at night.Many of the comments received were very positive about the quality of thenursing at night, although many did also mention they felt the staff wereworking very hard. Ward 9 is typical in this respect with six patients remarkingthat the staff were extremely busy and not always able to attend to those inpain. However, they also felt the staff were professional and caring.Several patients from different wards felt that staffing levels were adequate onquiet nights but very poorly or difficult patients stretched staff. Of the twopatients on the Acute Medical Unit (AMU) who felt there were not enoughstaff, neither felt their personal care had been affected by this, something thatwas echoed across many wards.However, the reasons given by patients on the Stroke Unit for feeling there arenot enough staff at night raise specific concerns around not answering callbells and medication being given late. A patient on this ward also told us thathe had had to wait until day staff came on for something to be done for him aspart of his ongoing care, leaving him in pain during the night.5.2.2 Have you experienced any difference between care during the dayand night?The majority of patients (79%) stated that they had not noticed any differencein care between day and night. The reasons the nineteen patients who saidthey had noticed a difference mirror answers to the previous question. Delaysin giving medication at night meant that patients had to wait to settle down tosleep and with fewer staff on the wards, confused patients and those withdementia were far more disruptive to their fellow patients, with some shoutingand banging tables.Patients on two wards noted difficulties in getting a doctor at night as thereason for finding care different between day and night. There was concernfrom patients on other wards at staff’s ability to cope with emergencies giventheir reduced numbers.However, one patient on AMU felt this ward was more ‘demure’ at night and aclear majority of patients felt the standard of nursing care was very high.3The Hospital at NightQuality/Performance
Board of Directors Part 114 June 20135.2.3 Do you get your night-time medication on time and if you requireany pain medication during the night/early morning, is this givenpromptly?90% (82 people) said they did get their night-time medication in good time,though some qualified this when thinking about whether pain relief at othertimes in the night was as promptly given or easy to access. A couple ofpatients in different wards noted that timed medication was not always givenon time resulting in discomfort.Patients who did require pain medication at night were mostly happy it wasgiven on time and thought that any delays were down to the staff being verybusy. One patient in AMU said it could be worse getting pain medicationduring the day.A general observation around prescribing was accessibility to doctors to dothis. One patient, who thought they might like a sleeping tablet later, asked inpassing about this and was told ‘it was a doctor thing’ and was given theimpression it was not easy to do so she did not ask for it in the end. Staff alsomentioned having to wait for doctors to prescribe and there not being anypharmacy open at night.5.2.4 Do you feel safe in the hospital at night?Only one patient out of 91 reported not feeling safe in the hospital at nightbecause he had vomited one night and it had not been cleaned up promptly.Otherwise, patients universally felt very safe.5.2.5 How long does it take for a call bell to be answered at night?Patients answered this question in various ways and it was also difficult forpatients to always judge accurately the amount of time involved. In reviewingthe answers, the committee felt the following categories were a fair reflectionof what patients had told us:Immediately(up to 1-2minutes)Quickly(2-5minutes)Acceptably(5-10minutes)Unacceptably Had not used(
Board of Directors Part 114 June 2013Medicine for the Elderly on Ward 22 recorded all patients as saying they hadwaited 10-30 minutes for the bell to be answered. It may be that some patientshere were unable to estimate time accurately. This is a concern for this wardbut is not representative of the hospital overall.The patients who did not have call bells said they were unhappy or feltinsecure about it. These patients were in escalation beds. Some patients feltthat the fact they had not needed to use their bell reflected well on the level ofcare they were receiving.5.2.6 Have you been able to sleep well whilst in hospital?41% of patients reported that they had slept well whilst on the wards, with onepatient stating that he had slept better here than at home! Ward 24 didespecially well here, having had a focus on helping patients to have a goodnight's sleep. However, 59% had not slept well (some said they did not sleepwell at home either) and gave a range of reasons with the most common atthe top:Other patients being noisy – e.g. coughing and shouting – andwandering aboutNoise from staff – talking and laughing loudly, moving beds, newadmissionsNoisy equipment – bleeps and buzzers, nebulizers etc.Lights not being dimmed early enough or being too brightGeneral hospital and strange noisesPatient’s own medical symptoms or pain – doctors slow to tend to themEnvironment – cold ward, bad smells, uncomfortable bed clothingBeing away from home and generally unsettled and anxiousNot being tired5The Hospital at NightQuality/Performance
Board of Directors Part 114 June 20135.2.7 Overall, on a scale of 1 to 5 (1 being bad and 5 being excellent),how good is the care at night on this ward?SCALE 1 2 3 4 5Ward 1 0 0 2 5 4Ward 2 0 0 1 5 4Ward 9 0 0 1 3 6Ward 14 0 0 1 7 2Ward 15 0 0 1 8 1Ward 22 0 0 3 7 0Ward 24 0 0 1 2 7AMU 0 0 0 1 9Stroke 1 0 3 5 1Total 1 0 13 43 3437% felt their care was excellent, with AMU performing exceptionally well andWard 24 also doing very well. 47% felt their care was very good, with Wards14,15 and 22 doing well here. Only 14% gave the middle ranking to their wardfor night-time care, with responses spread across most wards and one personthought their care deserved the lowest score of <strong>1.</strong> Six of the wards scoredentirely 4 or 5. On this scale, 99% of our patients thought their care wasfair/good or better.5.2.8 Additional comments from patients:Comments relating to the standard of care receivedI received excellent care for an asthma attack during the night.Amazing, excellent, kind, considerate staff.Willing to do anything for patients.Very attentive at night. Couldn’t have had better treatment.Excellent care from night staff. Good all round. Care at night generallyvery good.Nurses are very caring, treat all patients with care and respect.Night care better than day care teams.Not all staff as committed to patient care as others.“We’re very lucky to have such a good hospital here in Bournemouth”.Enjoyed being here, superb people. Very friendly. Absolutely fantastic.Sensitive to my needs, high level of personal consideration.6The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013Couldn’t fault the care. Pleasantly surprised.“I wouldn’t do their job for double the pay!"RNIB could give training to staff in awareness and difficulties for blindpeople.Comments relating to the facilities on the wardNo ventilation in the shower which creates problems for patients withCOPD as there is a build up of steam.TV is too expensive, particularly for pensioners (two patients said this).Toilet too far away on the orthopaedic ward considering the type ofpatients here and their limited mobility.Need to think about arrangement of bedside areas for those with limitedmobility.An air freshener would be appreciated on some wards where the smellfrom bed pans and incontinent patients can be bad.Lights should be dimmed earlier.Comments relating to food and mealtimesFood always cold, including the plates. Don’t always get what isordered. Food not first class. No food available during the night.“Drug rounds coincide with mealtimes which means I get an injection inmy stomach half-way through a meal. I thought mealtimes wereprotected.”Comments relating to staff uniforms and attireStaff should wear soft-soled shoes.Staff should introduce themselves and uniforms confusing.5.3 ConclusionsThere is a general consensus amongst patients right across all thewards we visited that their care is very good at night with little differencebetween their care during the day and night. Staff are seen as caring,hard-working, friendly and attentive. Some patients preferred their careat night.However, some patients also felt that the staff are too busy. Mostpatients felt their care had not been affected by how busy the staffwere, but where that had occurred, many were understanding that theywere doing their best.In some cases, the fact that staff were so busy had affected patientcare with some drugs given late, procedures not carried out and a veryfew patients left in pain, discomfort or dirty.Most patients felt that wards did have adequate nursing staff providedthere were no emergencies, patients were not too poorly or there wereno confused patients on wards (other than medicine for the elderly7The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013wards). When these situations arose, nursing staff were stretched andthis could have an adverse impact on the care other patients received.Some of the difficulties patients perceived nursing staff as having weredown to a shortage of doctors at night. There is only one Registrar onsite at night with other doctors on call and so patients who are not anemergency may wait hours to see a doctor or have medicationprescribed.A majority of our patients had not slept well whilst with us and the mostcommon reason given was noise - other patients and staff being themain sources. Patients understand that a hospital is a strangeenvironment and noise is inevitable with poorly people around them butsome sources of noise are avoidable, such as staff talking too loudlyand patients being moved late at night. The lights were also a problem,not being dimmed early enough in the evening and being too brighteven when dimmed.One fifth of patients had had to wait in excess of 10 minutes to havetheir call bell answered, with a few waiting up to half an hour. This isworrying for patients, however busy the staff. Three patients had notbeen given a call bell, which they were unhappy about but 14% hadnever needed to use their bell which some remarked reflected thequality of the care they were receiving.6. Recommendations<strong>1.</strong> Ensure night staff are informed of the high esteem patientshold them in.2. Consider providing more nursing and HCA staff in areas withincreased dependency as and when required.3. Medical cover at night needs to be improved.4. Remind staff to keep unnecessary noise to a minimum and todim lights early and low enough.5. Ensure all staff have adequate training in the management ofconfused and disruptive patients wherever they may be in thehospital.6. Where escalation beds are in use an alternative to theelectronic call bell needs to be provided for patients.7. Consideration should be given to an audit of the timeliness ofadministering late night medication to ensure this is being givenon time and when needed.8The Hospital at NightQuality/Performance
Board of Directors Part 114 June 20137. STAFF REPORT7.1 IntroductionNursing staff were interviewed on nine wards throughout the hospital inFebruary and March 2013 with the aim of providing information from acute,specialist medical, surgical and Medicine for the Elderly units.All staff had been on night duty during the previous months and were informedthat the questionnaire was confidential. An average of 5 staff were interviewedper ward with the intention that this should include 3 registered nurses and 2Health Care Assistants (HCAs). Extra staff were interviewed on wards 1 and24.The total number of nursing staff interviewed was 48, which included:17 HCAs (bands 2 and 3)25 Staff nurses (band 5) and6 Sisters (band 6) (who had in several cases been recently promotedbut had been on night duty in the past few months)Length of time in post varied from 6 weeks to 24 years. 18 (37%) of thenursing staff were on permanent night duty. The full, tabulated results for allwards can be found at Appendix B. A breakdown of the staff results by wardcan be found at Appendix D.7.2 General information on night staffing levelsMedicalAcute admissions, covering the Acute Medical Unit (AMU) and GP admissions- 1 medical registrar and 1 Senior House Officer (SHO)Medical wards - 1 F1 (Houseman) and 1 F2 (SHO). Occasionally the medicalregistrar may be called to see a serious ward problem.Surgical wards - 1 F1 with a registrar who was supposed to be mainly in bedas they were working normally the next day.Clinical Site Team (CST)This consists of either two band 6 sisters or a band 6 and a band 7.PortersThere are 4 or 5 porters on duty at night with one permanently in theEmergency Department (ED). All are on a permanent night rota.7.3 Results and responses7.3.1 Appraisals and trainingA majority of 85% of staff had had an appraisal in the last year and severalof those who had not had one had been in post for less than a year. A9The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013large majority of 83% had received all mandatory and necessary updatetraining in the past year.However, there was some feeling that HCAs may struggle to obtain theirpersonal development more than registered staff. A few staff membersseemed unclear about what they should be getting in terms of personaldevelopment. There was no impression that working on a permanentnights rota affected the availability or take-up of training.7.3.2 Staffing levels and skill mixAlmost 80% of staff were happy with the number of staff on their wards atnight. The clear exception was the Acute Medical Unit (AMU) where all 5respondents said more staff were needed particularly HCAs and alsoregistered staff. Ward 15 also felt they needed more staff to cope withelderly confused patients.Recent staffing level increases on several of the wards had made a majorimprovement to working conditions and care at night. We understand thatsince the survey took place, extra staff have been appointed to AMU atnight in line with a request from the clinical lead there and the Society ofAcute Medicine’s guidelines.In terms of skill mix, responses were largely positive but several problemswere of concern to many wards:The use of Agency nurses caused general disharmony as theywere unable to perform drug rounds and a number of practicalprocedures and although being paid as band 5s were effectivelyfunctioning as HCAs.It was suggested that the Trust might more effectively andeconomically employ one or two band 5 nurses to act as a “float”nurse around the hospital to fill gaps where needed instead ofemploying Agency staff. Bank staff were held in a better light butstill had their drawbacks.Medical outliers (general medical and medicine for the elderly acuteadmissions that have not been able to be placed on an appropriateward due to the high pressure of acute admissions) on wards raisedproblems for many staff because of a lack of appropriate training,their acute medical problems and patients’ often high levels ofdependence.Moving staff to other wards during shifts caused the remaining staffto be pressurised and over-worked. Sometimes replacing a staffnurse with an HCA made accomplishing more specialised tasksdifficult, particularly on high dependency wards.10The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013However, there is a need and understanding that nursing staff haveto show flexibility and may occasionally need to change wardswhere an acute problem arises.Some wards reported that band 5 nurses were not prepared toperform more basic tasks, leaving this to HCAs, even when theHCAs were under pressure, which is not good team work.When we asked whether there was ever a time when there was noregistered nurse on the ward, all wards replied that at least one registerednurse is always allocated to every ward at night. Only one member of stafffrom Ward 22 and one from the Stroke Unit said that for very shortperiods, such as toilet breaks, might there not be a registered member ofstaff on the ward at all times.7.3.3 Support and help from the Clinical Site Team (CST)There were high levels of satisfaction for the help and support given by theCST. Answers for a timely response from the CST were also very positivebut some dissatisfaction was aired on a couple of wards.If the CST was under pressure and pushed, wards suffered. It wasgenerally felt that the CST could do with another member of staff, whichcould be the same as the twilight/roving band 5 or 6 previously mentioned.There is usually no dissatisfaction with the time taken for red alert calls tobe answered by the CST and doctor but nursing staff felt that amber callscould take a long time for a doctor to respond.Medical staff were a cause of repeated comment by most wards.Generally in this very busy admission period staff complained that it wasdifficult to get hold of a doctor and they often took far too long to come towards particularly for writing up drugs and intravenous regimes. Mostnursing staff felt there should be another doctor on for the wards at nightpreferably someone more senior. There were some comments that doctorresponse and answering bleeps was particularly bad at the night doctorhandover at 23.00.It is difficult to know what the doctor response times were when thehospital was less busy prior to September but since this increase inadmissions has continued for over six months one may have to concludethat this is the new norm and it would seem there is a strong universalfeeling amongst nursing staff and the CST that current levels of medicalcover are inadequate.Only one third of nursing staff felt there was adequate support for themwhen their ward was under pressure. How often this happens and if thereis any pattern of cause or failure of response was not ascertained.11The Hospital at NightQuality/Performance
Board of Directors Part 114 June 20137.3.4 Staff’s confidence in expressing concerns to managers aboutcareThere was a very strong positive response in 98% of nursing staff. Theystated that managers listened to their comments and views. The role ofthe clinical lead is key as the leader and co-ordinator of the team andbeing approachable and responsive to comments from staff is an essentialpart of the role.7.3.5 Job satisfaction85% of nursing staff said they left work feeling they had done a good job.60% of staff on the Stroke Unit were less happy about their role at night –when busy the essentials are not always done and patients not alwaysmade to feel special. Several staff on the Acute Medical Unit commentedthat a patient’s personal care sometimes took second place to clinicalcare. Because they are always busy, care was sometimes dependent onthe skill mix at the time. Most AMU staff felt they were under-staffed at thetime of the review.When we asked staff whether they ever left work feeling anxious thatpatients had not received optimum care, this produced a 50/50 split. Staffclearly want to perform a really good and caring job and many of theircomments reflect the circumstances of the job, like being too busy. Tosome extent responses depended on how the interviewee interpreted thequestion. The responses were more a reflection of how high a level of carestaff wish to give rather than the reality of the situation.Many wards commented on how well they worked as a team although onsome wards there were comments that band 5 nurses would sometimesnot help out HCAs with their more basic tasks. Some responsesmentioned that acutely ill patients were not being given the best care as ittakes too long to be seen by a doctor.What are the aspects of night working you find frustrating ornegative?The points below reflect general comments made by staff:Not enough nursing staffDoctors slow to respond. Not enough doctorsFood and breaks – when busy don’t always have a meal break.Poor food availabilitySleep pattern disruptionIsolation at nightResponsibility and decision making greaterVery tiring and strenuousStaff talking loudlySecurity staff and porters – calling a porter on the computer systemis slow and time consumingResponse to requested task often very tardy. Lack of porters12The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013Managing aggressive, demented and confused patients can be verydifficultSlow chain of response for sick patients – medicallyGetting hold of equipment can be hard – role of portersWhat are the aspects of night working you find most beneficial orpositive?Being in charge, taking more responsibility, using initiativeMore time to talk to patients, read notes, paperwork and admin, canoffer more care and be compassionateMore time for social careHome life suits night workingBetter team working – like a family7.3.6 What are the food options available at night?Lack of food and meals at night is a universal and strongly held complaint.Nearly all the staff said the current situation is very poor and the two thatdid not answer “no” did so as they usually brought in their own food andaccepted this as the status quo.There is no hot food available as the canteen is closed. Vending machinesare found only outside the restaurant and are generally stocked with junkfood. Sandwiches are said to be stale.The vending machines are also too far away from staff in the oppositewing. When they are very busy they do not have time to walk there andback. Staff can heat food in microwaves on the ward if they bring their ownfood but sometimes these don’t work. Being able to buy plated food fromthe canteen before it closes in order to reheat it later would be an option.Vending machines with good food are needed in both hospital wings.There are also complaints that there is not always a place to take a break.Not all wards have a quiet space nearby to relax in and there are notenough breaks within the long, twelve-hour shifts (currently just one onehourbreak).7.3.7 Name three things that would improve night working on thiswardThere were lots of suggestions, many of which re-iterated some of thecomments above. Below is a short list of common of requests in noparticular order.More staff - HCAs mostly but trained nurses on AMU and perhapsthe CSTQuicker and easier access to doctors13The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013Time for breaks, good food and drink for the breaks andsomewhere away from the ward to take the breaksBetter access to equipment and drugs for emergency use. Morethoughtful planning by staff during the day to ensure night staffhave them readily availableImproved and more rapid porteringMedical outliers on wards increase pressure on staff – please keepthem to a minimumBetter portering and security for confused patientsNot using agency staff wherever possibleMinimising patient and staff transfers during the nightLess noise from staff, phones and lower lights7.3.8Interview with members of the Clinical Site TeamMost of the issues raised by the nursing staff were reaffirmed by thethree members of the CST that we spoke to. Their main pointswere:More doctors are needed – either a medical registrar or SeniorHouse OfficerAnother porter would be extremely helpful. The IT system forsummoning a porter is slow, cumbersome and repetitive andneeds urgently to be modified.More nursing/medical jobs can be done in the day – equipmenttracking, drug charts written up in a more anticipatory fashione.g. night sedation and analgesia, having supplies of emergencytherapy such as antibiotics available on the ward as it can bedifficult to obtain these at night when the pharmacist is only oncall.iPADs for the Clinical Site Team would allow more informationto be given to the team when they are walking the hospital,resulting in more swift and appropriate action.The surgical F1 covering the surgical wards feels isolated. Theirregistrar is in bed on site but seemingly does not like beingdisturbed.14The Hospital at NightQuality/Performance
Board of Directors Part 114 June 20137.4 ConclusionsThe overall impression was that nursing staff worked to the very best oftheir ability and enjoyed their work at night.A high proportion of staff had both an appraisal in the last year andappropriate training. Being on permanent night duty seemed noimpairment to receiving training.The availability and speed of response of doctors were deemedinadequate and some staff commented that it impaired good medicalcare. More doctor cover is required to cope with the busy workload.Despite the current high levels of patient activity in the Trust, 80% of staffinterviewed felt there was adequate nursing staff on their ward.Additional staff appointed in the last few months had made aconsiderable difference on some of the wards. However, AMU felt theywere still under-staffed and ward 15 commented they needed more staffto cope with elderly confused patients.The Clinical Site Team also felt an extra nurse was needed for theirteam.The staff mix was generally satisfactory. The main negative commentsconcerned the limited role of Agency nurses on wards. A smaller degreeof discontent was expressed regarding bank staff. There was moreunhappiness about moving staff to other wards.There is a perception among some HCAs on a few wards that trainednurses are reluctant to help them with administering basic nursing care,even when the HCAs are under pressure.Many nursing staff commented on problems relating to outlier patients ontheir wards. Lack of training in managing elderly and confused patientswith co-morbidities was seen as a barrier to good clinical care. Acutemedical patients on surgical wards may also not receive the level of careexpected where staff are less experienced in delivering a particular typeof care.Nursing staff were generally very happy with both the support andavailability of the Clinical Site Team. Many felt, as did the CST members,that the Team would benefit from a further member.Portering services at night are both slow and inadequate. The current ITsystem for summoning a porter is cumbersome and repetitive and takestoo long. Responses for aggressive or confused patients need to beimproved.Nearly all staff felt happy to discuss concerns with their Team Leader ormanager.15The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013It was highlighted that on rare occasions staff had been unclear how toreport incidents.The total lack and unavailability of food at night was a strongly anduniversally held concern, together with somewhere to take breaks andrelax.The availability of emergency drugs and equipment on wards at nightcould be much better managed by more thoughtful planning by day staffand doctors.Nights are enjoyable for many offering a better balance of home life andchildcare. They also can provide a challenging and stimulatingprofessional environment with greater autonomy.Some staff may feel isolated but this is very infrequent.16The Hospital at NightQuality/Performance
Board of Directors Part 114 June 20138.Recommendations<strong>1.</strong> Strong consideration should be given for the need for extra cover/stafffor:a. The Acute Medical Unit (see earlier note regarding anuplift in staff there since the research was done)b. The Clinical Site Teamc. Doctor cover at nightd. Extra HCAs on some wardse. Portering and security arrangementsThis could be achieved by rostering staff differently or byemploying extra staff, as appropriate.2. An extra nursing post for the CST might involve a twilight shift rota. Aband 5 nurse who is suitably trained could act as a float forpressurised areas, particularly in the evenings. Nurse prescribing bymembers of the CST could also go a long way to alleviating theproblems around access to drugs overnight.3. There needs to be a review of the current IT system for summoningporters and a much faster and more flexible response from them isneeded.4. As far as outliers are concerned a training needs analysis should becarried out in order to allow staff to cope with a more diverse casemix.5. In order to promote better team working, trained nurses need toconsider the level of support given to HCAs in carrying out basicnursing care.6. Better and more considerate daytime planning by medical and nursingstaff in advance could reduce workload at night by making sure drugsand intravenous therapies are written up and equipment is stored onthe ward when likely to be needed. Supplies of emergency drugs needto be made more readily available at night and could perhaps bestored in a locked cupboard in the CST office.7. There is an urgent need to provide better food at night. Plated mealscould be available for staff before the catering team go off duty whichcould be subsequently heated in a microwave if appropriate. Wellstockedvending machines need to be sited on both wings of thehospital with fresh healthy foods. Staff also need somewhere to taketheir breaks away from wards, if possible.8. Wherever possible, no patients should be moved to another ward aftermidnight.17The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013APPENDIX APATIENT QUESTIONNAIRE RESPONSESThere were 91 patients interviewed in all – 43 female respondents (47%) and 48male respondents (53%)Yes % No %Question 1Have you only been on thisward for this hospital stay?Question 2Do you think there areenough nursing staff onthis ward at night?Question 3Have you experienced anydifference between careduring the day and night?Question 4Do you get your night-timemedication on time and ifyou require any painmedication during thenight/morning, is this givenpromptly?Question 5Do you feel safe in thehospital at night?Question 6How long does it take for acall bell to be answered atnight?Question 7Have you been able tosleep well whilst inhospital?Question 8Overall, on a scale of 1 to 5(1 being bad and 5 beingexcellent), how good is thecare at night on this ward?53 58% 38 42%51 56% 38 44% 2 non respondents19 21% 72 79%82 90% 8 10% 1 non respondent90 99% 1 1%37 41% 54 59%Immediately 21%Quickly 32%Acceptably 11%Unacceptably 19%Not used 17%34 scored 5 = 37%43 scored 4 = 47%13 scored 3 = 14%0 scored 2 = 0%1 scored 1 = 1%18The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013APPENDIX BSTAFF QUESTIONNAIRE RESPONSESCombined responses from all 48 nursing staff interviewedYes % No %Question 1Have you had an appraisal in the last year?Question 2Have you had all the training identified –mandatory and personal development?Question 3Are there enough staff on the ward at night?Question 4Do you have the right mix of staff on the ward atnight?Question 5Are there times when there are no registeredstaff on the ward at night?Question 6Do you have enough help or support from theClinical Site Team at night?Question 7Is the response from the CST within anacceptable timescale?41 85% 7 15%40 83% 8 17%38 79% 10 21%39 81% 9 19%2 4% 46 96%45 94% 3 6%42 88% 6 12%Question 828 a 64% 16 36%Do you have enough help / support when ward isunder pressure?Question 9Are you confident about expressing anyconcerns you may have about care tomanagers?Question 10Do you leave work feeling you have done a goodjob?Question 11Do you feel anxious that patients have notreceived optimum care?47 98% 1 2%41 85% 7 15%24 a 50% 24 50%Question 142 4% 46 96%Are the food options available at night for staffadequate?a – several staff answered this question with a yes / no response19The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013APPENDIX CPATIENT QUESTIONNAIRE RESPONSES TABULATED BY WARDWard 1 is a specialist gastroenterology ward which includes a high dependency unitfor acute Gastro-intestinal bleeders and thus needs a higher level of morespecialised nursing care.11 patients 6 female + 5 male Age range 25 – 84Lengths of Stay 2 – 28 nightsQUESTION YES NO<strong>1.</strong> Have you only been on this ward for this hospitalstay?2. Do you think there are enough nursing staff on thisward at night?3. Have you experienced any difference between careduring the day and night?4. Do you get your night-time medication on time andif you require any pain medication during thenight/morning is this given promptly?5. Do you feel safe in the hospital at night? 116. How long does it take for a call bell to be answeredat night?7 48 32 9112-5mins x 1010-20minsx17. Have you been able to sleep well whilst in hospital? 4 78. Overall, on a scale of 1 to 5, how good is the care atnight on this ward?1 – 02 – 03 – 24 – 55 – 420The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013Ward 2 is a 26-bedded respiratory ward which includes a 4-bedded acute lung bay.Most patients are admitted from the Acute Medical Unit although some patients aretransferred from other wards in the hospital.10 patients 5 female + 5 male Age range 55 - 86Lengths of Stay 5 – 18 nightsQUESTION YES NO<strong>1.</strong> Have you only been on this ward for this hospitalstay?2. Do you think there are enough nursing staff on thisward at night?3. Have you experienced any difference between careduring the day and night?4. Do you get your night-time medication on time andif you require any pain medication during thenight/morning is this given promptly?5. Do you feel safe in the hospital at night? 106. How long does it take for a call bell to be answeredat night?4 67 31 98 21-2minsx33-4minsx14-5minsx2>5mins x17. Have you been able to sleep well whilst in hospital? 3 78. Overall, on a scale of 1 to 5, how good is the care atnight on this ward?1 – 02 – 03 – 14 – 55 – 4N/A321The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013Ward 9 is a 29-bedded surgical orthopaedic ward taking the more complex electivesurgical case mix. Patients require a higher level of nursing care and the unit alsooften has medical outliers due to its having seven side rooms.10 patients 10 female Age range 59 – 86Lengths of Stay 3 – 13 nightsQUESTION YES NO<strong>1.</strong> Have you only been on this ward for this hospitalstay?2. Do you think there are enough nursing staff on thisward at night?3. Have you experienced any difference between careduring the day and night?4. Do you get your night-time medication on time andif you require any pain medication during thenight/morning is this given promptly?5. Do you feel safe in the hospital at night? 106. How long does it take for a call bell to be answeredat night?104 60 109 11-2minsx85-10minsx27. Have you been able to sleep well whilst in hospital? 7 38. Overall, on a scale of 1 to 5, how good is the care atnight on this ward?1 – 02 – 03 – 14 – 35 – 622The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013Ward 14 is a Vascular and male Endocrine ward. One patient interviewed is waitingto be re-housed, hence the three-month length of stay.10 patients 5 female + 5 male Age range 30 – 93QUESTION YES NO<strong>1.</strong> Have you only been on this ward for this hospitalstay?2. Do you think there are enough nursing staff on thisward at night?3. Have you experienced any difference between careduring the day and night?4. Do you get your night-time medication on time and ifyou require any pain medication during thenight/morning is this given promptly?5. Do you feel safe in the hospital at night? 106. How long does it take for a call bell to be answered atnight?4 681 not sure11 910 0Not long -510 minsx2Long timex1Varies x 17. Have you been able to sleep well whilst in hospital? 4 68. Overall, on a scale of 1 to 5, how good is the care atnight on this ward?1 – 02 – 03 – 14 – 75 – 21N/A23The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013Ward 15 is a 26-bedded ward taking patients undergoing acute urological surgery.This ward has a high turnover of patients and is very busy.10 patients 1 female + 9 male Age range 48 – 90QUESTION YES NO<strong>1.</strong> Have you only been on this ward for this hospitalstay?2. Do you think there are enough nursing staff onthis ward at night?3. Have you experienced any difference betweencare during the day and night?4. Do you get your night-time medication on timeand if you require any pain medication during thenight/morning is this given promptly?5. Do you feel safe in the hospital at night? 106. How long does it take for a call bell to beanswered at night?7. Have you been able to sleep well whilst inhospital?8. Overall, on a scale of 1 to 5, how good is the careat night on this ward?5 56 42 89 1N/AImmediatelyto a fewminutes x 81 91 – 01 – 03 – 13.5 – 14 – 75 – 12N/A24The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013Ward 22 is an all-male Medicine for the Elderly ward.10 patients 10 male Age range 59 - 91QUESTION YES NO<strong>1.</strong> Have you only been on this ward for this hospitalstay?2. Do you think there are enough nursing staff on thisward at night?3. Have you experienced any difference between careduring the day and night?4. Do you get your night-time medication on time andif you require any pain medication during thenight/morning is this given promptly?5. Do you feel safe in the hospital at night? 106. How long does it take for a call bell to be answeredat night?2 841 declinedto answer53 79 110 – 30mins7. Have you been able to sleep well whilst in hospital? 2 88. Overall, on a scale of 1 to 5, how good is the care atnight on this ward?1 – 02 – 03 – 34 – 75 – 01025The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013Ward 24 is a 25-bedded specialist Cardiology ward which includes high dependencybays for acute patients who need a higher level of nursing care.10 patients 7 female + 3 male Age range 28 – 86Lengths of Stay 4 – 28 nightsQUESTION YES NO<strong>1.</strong> Have you only been on this ward for this hospitalstay?2. Do you think there are enough nursing staff on thisward at night?3. Have you experienced any difference between careduring the day and night?4. Do you get your night-time medication on time andif you require any pain medication during thenight/morning is this given promptly?5. Do you feel safe in the hospital at night? 106. How long does it take for a call bell to be answeredat night?7 35 54 6102-5 minsx7Not usedx37. Have you been able to sleep well whilst in hospital? 7 38. Overall, on a scale of 1 to 5, how good is the care atnight on this ward?1 – 02 – 03 – 14 – 25 – 726The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013The Acute Medical Unit is a large, 52-bedded ward with 42 short stay inpatient bedsand 10 rapid assessment beds that take direct GP and Emergency Departmentreferrals for medical input. The assessment beds take an unpredictable take and theinpatient beds are from admission-72 hours.10 patients 6 female + 4 male Age range 24 – 83Lengths of Stay 2 – 4 nightsQUESTION YES NO<strong>1.</strong> Have you only been on this ward for this hospitalstay?2. Do you think there are enough nursing staff onthis ward at night?3. Have you experienced any difference betweencare during the day and night?4. Do you get your night-time medication on timeand if you require any pain medication during thenight/morning is this given promptly?5. Do you feel safe in the hospital at night? 106. How long does it take for a call bell to beanswered at night?7. Have you been able to sleep well whilst inhospital?8. Overall, on a scale of 1 to 5, how good is the careat night on this ward?8 27 31 99 1Immediatelyto 2 minutesx410 mins x 15 51 – 02 – 03 – 04 – 15 – 94 N/A1 didnothaveone27The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013The Stroke Unit is a 36-bedded specialist stroke ward.10 patients 3 female + 7 male Age range 59 – 91Lengths of Stay 4 – 49 nightsQUESTION YES NO<strong>1.</strong> Have you only been on this ward for this hospitalstay?2. Do you think there are enough nursing staff on thisward at night?3. Have you experienced any difference between careduring the day and night?4. Do you get your night-time medication on time andif you require any pain medication during thenight/morning is this given promptly?6 42 85 57 35. Do you feel safe in the hospital at night? 9 16. How long does it take for a call bell to be answeredat night?7. Have you been able to sleep well whilst inhospital?8. Overall, on a scale of 1 to 5, how good is the careat night on this ward?5-10mins x630mins x14 61 – 12 – 03 – 34 – 55 – 12Didnothaveone28The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013APPENDIX DSTAFF QUESTIONNAIRE RESPONSES TABULATED BY WARDAt night Ward 1 is staffed by three trained band 5 staff nurses and one Health CareAssistant (HCA). Staff levels have recently been increased to the third band 5member and all respondents commented that this has made a big difference inhelping them with their heavy workload during the night.Staff interviewed: 3 Registered - Band 52 HCA - Band 21 Sister - Band 6 (newly appointed)5 staff on internal rotation, 1 HCA on permanent nightsLength of time in current post: 16 months to 11 yearsHandovers are done by tape recorder for all night staff when they come on dutywhich takes about 15 minutes. Then they meet with the nurse in charge of the dayshift for any particular further information that needs to be added.QUESTION YES NO<strong>1.</strong> Have you had an appraisal in the last year? 6 02. Have you had all the training identified – mandatory andCPD?6 03. Do you feel there are enough staff on the ward at night? 5 14. Do you have the right mix of staff at night on this ward? 5 15. Are there times at night when there are no registeredstaff on the ward?6. Do you have enough help/support from the Clinical SiteTeam?7. Is the response from the CST usually within anacceptable timescale?8. Do you have enough help/support when the ward isunder pressure?9. Do you feel confident in expressing any concerns youmay have about care to your managers?0 66 06 041 Yes6 010. Do you leave work feeling you have done a good job? 6 01<strong>1.</strong> Are there instances when you are left feeling anxiousthat patients have not received optimum care?14. Are the food options available for staff at nightadequate?2 40 61& No29The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013At night Ward 2 is staffed by 3 trained staff nurses and 2 HCAs. The ward is currentlynot at full establishment of staff. Bank nursing staff are used to make up thenumbers. Trained agency nursing staff are not used as they are unable to carry outdrug administration.Staff interviewed: 3 Registered - Band 52 HCA - Band 2Length of time in current post: 4 – 11 yearsAll staff work internal rotation with the exception of the clinical leader and deputy whowork only days. No staff work predominantly nights. The staffing template hasrecently been revised and on each shift there are:4 trained nurses and 3 healthcare assistants for a morning shift4 trained nurses and 2 healthcare assistants for the late shift3 trained nurses and 2 healthcare assistants for the night shiftHandovers are predominantly taped. Only if the staff are too busy to be able todictate the handover is verbal handover used. Taping is considered to be thepreferred method as it’s more accurate when staff are arriving for shifts at differenttimes.QUESTION YES NO<strong>1.</strong> Have you had an appraisal in the last year? 5 02. Have you had all the training identified – mandatory andCPD?2 33. Do you feel there are enough staff on the ward at night? 5 04. Do you have the right mix of staff at night on this ward? 5 05. Are there times at night when there are no registeredstaff on the ward?6. Do you have enough help/support from the Clinical SiteTeam?7. Is the response from the CST usually within anacceptable timescale?8. Do you have enough help/support when the ward isunder pressure?9. Do you feel confident in expressing any concerns youmay have about care to your managers?0 54 14 131 N/A15 010. Do you leave work feeling you have done a good job? 5 01<strong>1.</strong> Are there instances when you are left feeling anxiousthat patients have not received optimum care?14. Are the food options available for staff at nightadequate?3 20 530The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013At night Ward 9 is generally staffed by two trained nurses and two HCAs, with theexception of Sundays when there is one less HCA. If patients are very ill, more staffwill be brought in to help.Staff interviewed: 3 Registered - 2 x Band 5 1 x Band 62 HCA - Band 23 staff on internal rotation, 2 predominantly on nightsLength of time in current post: 6 –16 yearsMorning handover is done by tape, lunchtime handover is at the desk and eveninghandovers are done in the office.QUESTION YES NO<strong>1.</strong> Have you had an appraisal in the last year? 5 02. Have you had all the training identified – mandatory andCPD?5 03. Do you feel there are enough staff on the ward at night? 4 14. Do you have the right mix of staff at night on this ward? 5 05. Are there times at night when there are no registeredstaff on the ward?6. Do you have enough help/support from the Clinical SiteTeam?7. Is the response from the CST usually within anacceptable timescale?8. Do you have enough help/support when the ward isunder pressure?9. Do you feel confident in expressing any concerns youmay have about care to your managers?0 54 13 21sometimes45 010. Do you leave work feeling you have done a good job? 5 01<strong>1.</strong> Are there instances when you are left feeling anxiousthat patients have not received optimum care?14. Are the food options available for staff at nightadequate?2 30 531The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013Ward 14 has recently changed its night shift to 7.30pm – 7.30am. There has alsobeen an increase in the number of staff working nights as the clinical lead felt thatthere was a risk with just two trained staff and one HCA. Now there are two trainednurses and two HCAs. This has made a huge difference.However, staff can be called away to assist in other wards if they are short staffed,but this is only for about an hour. There can be a problem if one of the staff is sickand there is not enough time to bring in Bank or Agency staff. Then they have tomanage the situation, but this does not happen very often.Staff interviewed: 3 Registered - Band 5 2 HCA - Bands 2 and 3Length of time in post: 7 months – 13 years4 work permanent nights, 1 occasional nights.Their handovers are verbal with each bay nurse handing over to all night staff. In themorning, all day staff receive a handover from the night staff.QUESTION YES NO<strong>1.</strong> Have you had an appraisal in the last year? 4 1*2. Have you had all the training identified – mandatoryand CPD?3. Do you feel there are enough staff on the ward atnight?4. Do you have the right mix of staff at night on thisward?5. Are there times at night when there are noregistered staff on the ward?6. Do you have enough help/support from the ClinicalSite Team?4 1unsure5 05 00 55 07. Is the response from the CST usually within anacceptable timescale?5mostly08. Do you have enough help/support when the ward isunder pressure?9. Do you feel confident in expressing any concernsyou may have about care to your managers?10. Do you leave work feeling you have done a goodjob?1<strong>1.</strong> Are there instances when you are left feelinganxious that patients have not received optimumcare?14. Are the food options available for staff at nightadequate?*only in post 7 months41 Yes & No5 05 00 50 532The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013Ward 15 is staffed at night by two trained nurses and one HCA. Their band 6 sisterdoes some internal night shift rotation.Staff interviewed: 3 Registered - 2 x Band 5 1 x Band 62 HCA - Band 22 Registered Nurses on internal rotation, 1 on permanent nights2 HCAs on permanent nightsLength of time in current post: 6 months – 20 yearsHandovers are verbal and taped. Formal group handover in the evening is with allstaff. Additional information may also be passed between nurses regarding specificbays. Early morning handover is done by tape by the nurse in charge at about5.30am for the day shift, highlighting any areas of concern.QUESTION YES NO<strong>1.</strong> Have you had an appraisal in the last year? 4 12. Have you had all the training identified – mandatory andCPD?4 13. Do you feel there are enough staff on the ward at night? 3 24. Do you have the right mix of staff at night on this ward? 5 05. Are there times at night when there are no registeredstaff on the ward?6. Do you have enough help/support from the Clinical SiteTeam?7. Is the response from the CST usually within anacceptable timescale?8. Do you have enough help/support when the ward isunder pressure?9. Do you feel confident in expressing any concerns youmay have about care to your managers?0 55 05 03 25 010. Do you leave work feeling you have done a good job? 4 11<strong>1.</strong> Are there instances when you are left feeling anxiousthat patients have not received optimum care?14. Are the food options available for staff at nightadequate?5 00 533The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013At night Ward 22 is staffed by two trained nurses and two HCAs plus one trainednurse working from 3-11pm. This ward operates an early, late and night shift pattern,rather than the longer 12-hour shifts.Staff interviewed: 2 Registered - Band 5 3 HCA - Band 22 staff on internal rotation, 1 predominantly nightsLength of time in current post: 6 weeks – 8 yearsThere is a taped handover from night to day and a verbal handover from day to night.Staff in the main work 12-hour shifts. However, if anyone works a late shift a verbalhandover is then given (otherwise a taped handover would need to be updated andre-recorded).QUESTION YES NO<strong>1.</strong> Have you had an appraisal in the last year? 5 02. Have you had all the training identified – mandatory andCPD?4 13. Do you feel there are enough staff on the ward at night? 5 04. Do you have the right mix of staff at night on this ward? 3 25. Are there times at night when there are no registeredstaff on the ward?6. Do you have enough help/support from the Clinical SiteTeam?7. Is the response from the CST usually within anacceptable timescale?8. Do you have enough help/support when the ward isunder pressure?9. Do you feel confident in expressing any concerns youmay have about care to your managers?1 45 04 13 25 010. Do you leave work feeling you have done a good job? 5 01<strong>1.</strong> Are there instances when you are left feeling anxiousthat patients have not received optimum care?14. Are the food options available for staff at nightadequate?0 50 534The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013Ward 24 at night is staffed by two trained band 5 staff nurses and one HCA. Inaddition, they have a twilight shift for one trained nurse, working from 9.30am to10pm. This allows for extra cover at busy times for giving antibiotics, controlled drugsand additional patient care.Staff interviewed: 5 Registered - Band 5 1 HCA - Band 21 Sister - Band 6 (newly appointed, so will not continue workingat night)6 staff on internal rotation, 1 HCA on permanent nightsLength of time in current post: 4 months – 8 yearsHandovers are done on tape with any updates being done verbally.QUESTION YES NO<strong>1.</strong> Have you had an appraisal in the last year? 5 22. Have you had all the training identified – mandatory andCPD?7 03. Do you feel there are enough staff on the ward at night? 7 04. Do you have the right mix of staff at night on this ward? 6 15. Are there times at night when there are no registeredstaff on the ward?6. Do you have enough help/support from the Clinical SiteTeam?7. Is the response from the CST usually within anacceptable timescale?8. Do you have enough help/support when the ward isunder pressure?9. Do you feel confident in expressing any concerns youmay have about care to your managers?0 77 07 02 57 010. Do you leave work feeling you have done a good job? 7 01<strong>1.</strong> Are there instances when you are left feeling anxiousthat patients have not received optimum care?14. Are the food options available for staff at nightadequate?5 20 735The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013The Acute Medical Unit (AMU) is a 52-bedded unit with 42 short stay inpatient bedsand 10 rapid assessment beds that take direct GP and Emergency Departmentreferrals. The Unit is split into a Left and Right side.During the night, AMU has one registered nurse for both GP bays. In addition, thereis one HCA on the left and one on the right. There are also two trained nurses oneach side plus a co-ordinator (Band 6). The HCAs ward clerk at night. There hasrecently been an increase in staff numbers.Staff interviewed: 3 Registered - 1 - Band 5 2 - Band 62 HCA - Band 2Length of time in post: 15 months – 24 years4 were on permanent nights, 1 had been until recentlyAll have permanent contracts, 1 is part-timeHandovers are done verbally by the nurse looking after each area.QUESTION YES NO<strong>1.</strong> Have you had an appraisal in the last year? 4 12. Have you had all the training identified – mandatory andCPD?4 13. Do you feel there are enough staff on the ward at night? 0 54. Do you have the right mix of staff at night on this ward? 3 25. Are there times at night when there are no registeredstaff on the ward?6. Do you have enough help/support from the Clinical SiteTeam?7. Is the response from the CST usually within anacceptable timescale?8. Do you have enough help/support when the ward isunder pressure?9. Do you feel confident in expressing any concerns youmay have about care to your managers?0 55 05 041 Yes5 00& No10. Do you leave work feeling you have done a good job? 23 Yes & No1<strong>1.</strong> Are there instances when you are left feeling anxiousthat patients have not received optimum care?14. Are the food options available for staff at nightadequate?2 Yes2 33& No36The Hospital at NightQuality/Performance
Board of Directors Part 114 June 2013The Stroke Unit is staffed at night by three trained nurses and three HCAs.Sometimes ‘specials’ are required – extra staff to sit with specific patients all night.Specials are always available when required.Staff interviewed: 3 Registered - Band 5 2 HCA - Band 2Length of time in post: 5 – 27 yearsAll three nurses are on internal rotation; the HCAs are predominantly nights.Handovers are always taped and the one from night to day staff takes place outsidethe clinical area to reduce noise levels.QUESTION YES NO<strong>1.</strong> Have you had an appraisal in the last year? 3 22. Have you had all the training identified – mandatory andCPD?4 13. Do you feel there are enough staff on the ward at night? 4 14. Do you have the right mix of staff at night on this ward? 2 35. Are there times at night when there are no registeredstaff on the ward?6. Do you have enough help/support from the Clinical SiteTeam?7. Is the response from the CST usually within anacceptable timescale?8. Do you have enough help/support when the ward isunder pressure?9. Do you feel confident in expressing any concerns youmay have about care to your managers?1 44 13 24 14 110. Do you leave work feeling you have done a good job? 2 31<strong>1.</strong> Are there instances when you are left feeling anxiousthat patients have not received optimum care?14. Are the food options available for staff at nightadequate?5 00 537The Hospital at NightQuality/Performance
BOARD OF DIRECTORSMeeting Date and Part: 14 June 2013 Part 1Subject:Section:Executive with OverallResponsibilityAuthor of Paper:Details of previousdiscussion and/ordissemination:Key Purpose:Action required by BoD:Monitor’s Enforcement GuidanceDiscussionTony Spotswood, Chief ExecutiveKaren Flaherty, Trust SecretaryN/APatient Safety Health & Safety Performance StrategyXFor informationExecutive Summary:This guidance describes the enforcement powers that Monitor has under the National HealthService Act 2006 in relation to the licensing of providers and also its powers in relation tocompetition law.The powers in relation to licensing include informal action, providers giving enforcementundertakings, imposing discretionary requirements (including monetary penalties up to 10% ofthe provider’s turnover in England), imposing new licence conditions, requiring a trust to remove,suspend or disqualify directors and/or governors and revoking a provider’s licence. Thesepowers may be exercised by Monitor where it finds that a provider is breaching, or hasbreached, one or more of its licence conditions or an enforcement undertaking, or has not met arequirement to hold a licence, or has failed to provide Monitor with information it requires or, inthe case of enforcement undertakings, it has reasonable grounds to suspect that a provider hasdone these things. In relation to compeition law, Monitor’s powers include giving directions tobring an infringement to an end and imposing financial penalties and these powers are heldconcurrently with the Office of Fair Trading.The guidance also sets out how Monitor will prioritise its enforcement action.Strategic Goals & Objectives:AllLinks to CQC Registration:(Outcome reference)Links to AssuranceFramework/Key Risks:Type of Assurance: Internal External
EnforcementGuidance28 March 2013Monitor’s enforcement guidance explains the actionwe can take to enforce compliance with the providerlicence and other regulatory obligations on providersand others required to provide Monitor withinformation needed to perform its functions. It setsout the proposed process for prioritising issues,deciding on the action to take and seeking inputfrom stakeholders on our proposed actions.
ContentsForeword................................................................................................................. 3<strong>1.</strong> Introduction…................................................................................................... 52. Prioritisation..................................................................................................... 133. Imposing discretionary requirements and accepting enforcementundertakings………………………………………………………………………… 174. Enforcement – case procedures……….......................................................... 255. Decision-making for enforcement cases....................................................... 406. Rights of appeal................................................................................................ 42Annex:Monitor’s powers of enforcement under the Health and Social Care Act2012……………………………………………………………………………………… 45Page 2 of 50
ForewordThe Health and Social Care Act 2012 (the Act)makes changes to the way health care isregulated, including expanding Monitor’s role bygiving us a number of additional responsibilities.As part of these changes we are given a newmain duty to protect and promote the interestsof people who use health care services bypromoting the provision of services which iseconomic, efficient and effective, and maintainsor improves the quality of the services.As the foundation of our new role, the Act requires that Monitor issue licences for providers ofNHS services and also gives Monitor powers to enforce this licence. These powers enableMonitor to investigate potential breaches of the licence and then to either impose requirements onNHS service providers where we find actual breaches, or accept undertakings from the provider,to make sure they return to compliance. The requirements we can impose range from obligingproviders to take steps to restore compliance, requiring providers to restore the position beforethe breach or obliging them to pay a financial penalty. In exceptional circumstances, we can alsoconsider revoking a licence.Some of the enforcement powers of the Act can also be exercised against those who are notlicence holders - such as those operating without a licence when required to hold one, and thosein breach of a requirement to provide Monitor with information. The Act separately gives Monitorconcurrent powers with the Office of Fair Trading to apply competition law in the health caresector in England.This document sets out guidance on how we will exercise our enforcement powers. As examples,this guidance will apply to:complaints from a commissioner that a provider has acted unreasonably in refusing tosupply a service as a Commissioner Requested Service, in breach of its licence;complaints that a provider is not charging in line with the national tariff as required by itslicence;complaints that a provider has acted anti-competitively in breach of its licence and/orcompetition law;investigations into whether an NHS foundation trust may be in breach of its licenceconditions about governance; andfailures, by those obliged to do so, to provide information to Monitor.In this document we explain when we may formally investigate potential breaches, the processeswe are likely to follow, and the factors that we may consider when deciding what requirements toimpose should Monitor find a breach of the provider licence.Page 3 of 50
We are very grateful for the support and engagement of stakeholders in helping develop thisguidance through the recent consultation. This is a new enforcement framework which we willdevelop and refine over time as we learn through practice. But we are keen to start with aneffective regime building on regulatory experience to date.Adrian MastersManaging Director of Sector DevelopmentPage 4 of 50
1 IntroductionThe Health and Social Care Act 2012 (the Act) makes changes to the way providers of NHShealth care services will be regulated and gives Monitor new duties and powers. Furtherinformation on our role can be found on our website: www.monitor.gov.ukThis guidance covers the general approach that Monitor will take to using our provider licenceenforcement and competition law powers over health care providers. Parts of it apply to otherswho may be required to supply Monitor with information. This document explains:when Monitor may decide to take action, and what action we might take;how Monitor is likely to decide what kind of sanctions to impose using our powers underthe Act; andthe high-level processes Monitor intends to follow when taking enforcement action.This guidance is designed to provide information about how Monitor generally expects to goabout our enforcement work. The circumstances in some cases may make it appropriate for us todepart from the guidance.We have written this guidance to be as clear as possible, and have tried to use straightforwardlanguage and avoided quoting sections of the Act where possible; this means that, sometimes,we do not use the exact wording used in the Act which would, of course, override this guidance.All of this guidance is relevant to providers of NHS health care services in England. The sectionsthat cover competition law are relevant to all providers of health care services in England. Thesections covering enforcement action under sections 105 and 106 of the Act apply also to otherswhere they may be in breach of a requirement to provide Monitor with information; this applies tothe NHS Commissioning Board and clinical commissioning groups. This guidance does not coverMonitor's approach to using our enforcement powers under the National Health Service(Procurement, Patient Choice and Competition) (No. 2) Regulations 2013.As we move from the current framework of regulating NHS foundation trusts through their termsof Authorisation to regulating them through the licence, we are following a similar approach to thatset out in this guidance in ‘translating’ breaches of terms of the Authorisation into appropriateregulatory action under the licence, to take effect as the licence comes into force. We are workingclosely with the NHS foundation trusts affected by this to achieve a smooth transition.Page 5 of 50
<strong>1.</strong>1 Scope of the guidanceThe Act requires Monitor to introduce a licence for providers of NHS health care services, thestandard conditions for which are available here. The Act gives Monitor associated enforcementpowers under sections 105 and 106. Monitor may use these specific enforcement powers toensure that any provider that should hold a licence does in fact hold one, all licensed providerscomply with their licence conditions and all providers and others who may be obliged to complywith requests from Monitor to provide information.Section 89 of the Act gives Monitor the power to revoke a provider’s licence if we are satisfiedthat the provider has failed to comply with a licence condition. Some of this guidance also appliesto investigations which may result in revocation of a licence under section 89 of the Act.Section 111 of the Act gives Monitor additional specific powers to take action where thegovernance of an NHS foundation trust is such that it is failing, or will fail, to comply with one ormore of the conditions in its licence. These powers are in addition to those described above.Some of this guidance also applies to investigations which may result in an intervention undersection 111 of the Act.When carrying out the above functions, Monitor will seek to ensure that the enforcement actionswe take enable us to best achieve our main duty to protect and promote the interests of peoplethat use health care services (health care service users) by promoting the provision of health careservices which is economic, efficient and effective, and maintains or improves the quality of theservices.The Act gives Monitor concurrent powers with the Office of Fair Trading (OFT) to applycompetition law in relation to the provision of health care services in England meaning that eitherMonitor or the OFT may act in relation to a particular case. Some of this guidance also hasrelevance to investigations that Monitor may carry out under the Competition Act 1998 (theCompetition Act) and the Treaty on the Functioning of the European Union (the TFEU). It gives anoverview of the investigation process we intend to follow and contains links to informationpublished by the OFT. Monitor and the OFT will decide on a case-by-case basis whichorganisation is best placed to investigate an issue. We may, in the future, publish more detailedguidance on Monitor’s procedures around applying competition law.This guidance also describes how we will prioritise our enforcement work in order to make thebest use of resources. We intend to apply the same principles for prioritising all of our decisionsthat potentially involve a significant amount of resource to a case or project.Page 6 of 50
Table <strong>1.</strong>1 Monitor’s enforcement powersHow this guidance applies to Monitor’s different enforcement powers:RegulatoryactionSection ofguidanceInformalactionEnforcementundertakings(section 106)Discretionaryrequirements(section 105)Section 111new licenceconditionSection 111remove,suspend ordisqualifydirectors /governorsRevokingaprovider’slicence(section89)Competitionlaw(section72)2.2 Prioritisation 2.3 Informal orformal action 3.2 to 3.4Imposingdiscretionary requirements3.5 Acceptingenforcementundertakings4.2.1 Caseinitiation 4.2.2Investigations 4.2.3 Caseupdates 4.2.4 Enteringintoenforcementundertakings4.2.5Discretionaryrequirements4.3 Proceduresfor licencerevocation4.4 Actionsunder section111 of the Act(applies to NHSfoundationtrusts)4.5Investigationsundercompetition law5 Decisionmaking 6.2 Rights ofappeal * * Right of appeal for enforcement undertakings is only in relation to a refusal by Monitor to issue acertificate of compliance with undertakings.Page 7 of 50
<strong>1.</strong>2 Monitor’s enforcement powersIn this section we explain the different enforcement powers that the Act gives Monitor. Moredetails of Monitor’s enforcement powers are in the Annex. This section outlines:Licence enforcementwhat discretionary requirements are and when Monitor may impose them - section 105 ofthe Act;what enforcement undertakings are and when Monitor may accept them - section 106 ofthe Act;Monitor’s power to revoke a provider’s licence - section 89 of the Act;Monitor’s powers to impose additional licence conditions on an NHS foundation trust, andto require a foundation trust to remove, suspend or disqualify one or more of its directorsand/or governors - section 111 of the Act; andCompetition law enforcementMonitor’s powers to apply competition law.Page 8 of 50
Licence enforcementDiscretionary requirements under the ActWhere Monitor finds that a provider is breaching, or has breached, one or more of its licenceconditions, or has not met a requirement to hold a licence, or has failed to provide Monitor withinformation we require, Monitor may impose one or more of the ‘discretionary requirements’specified in section 105 of the Act. Monitor may also impose such requirements on others inbreach of a requirement to provide us with information.The discretionary requirements that Monitor may impose are:compliance requirements which require a provider to take such steps as we may specifyto ensure that the breach in question does not continue or recur;restoration requirements which require a provider to take such actions as we mayspecify to restore the situation to what it would have been, absent the breach; andvariable monetary penalties which require a provider to pay a penalty.The Act requires us to explain in guidance how we intend to exercise our powers to imposediscretionary requirements including: when we are likely to impose a discretionary requirement - see Chapter 3; when we may not impose a discretionary requirement - see Chapter 3;the matters we are likely to take into account in determining a variable monetary penalty,including any discounts for voluntary reporting - see Chapter 3; and a provider’s rights to make representations and rights of appeal - see Chapter 6.Enforcement undertakings under the ActIf Monitor has reasonable grounds to suspect that a provider is breaching, or has breached, oneor more of its licence conditions, or has not met a requirement to hold a licence, or has failed toprovide Monitor with information we required, we may also accept ‘enforcement undertakings’, asdescribed in section 106 of the Act. Monitor may also accept such undertakings from others inbreach of a requirement to provide us with information.Enforcement undertakings are actions that providers commit themselves to taking and whichMonitor may decide to accept. They would usually be used as an alternative to investigatingfurther with the attendant possibility of imposing discretionary requirements.An enforcement undertaking may include one or more of the following commitments:Page 9 of 50
action to ensure that the breach does not continue or recur;action to ensure that the position is, so far as possible, restored to what it would havebeen, absent the breach;action, including the payment of a sum of money, to benefit any other licensee affected bythe breach, any provider of NHS health care services affected by the breach, or anycommissioner of NHS health care services affected by the breach; oraction of such a description as may be prescribed.The Act requires us to include in our guidance information about how we intend to exercise ourpowers to accept enforcement undertakings - see Chapters 3 and 4.Revoking a provider’s licenceMonitor may also revoke a provider’s licence if we are satisfied that the provider has failed tocomply with a licence condition, as set out in section 89 of the Act.Powers to impose additional licence conditions on NHS foundation trustsMonitor has additional specific powers to take action where the governance of an NHS foundationtrust is such that it is failing, or will fail, to comply with one or more of the conditions in its licence.There are two parts to these powers:I. where Monitor is satisfied that an NHS foundation trust’s directors and/or governors arefailing to (a) secure compliance with conditions in the foundation trust’s licence, or (b) takesteps to reduce the risk of a breach of a condition in the foundation trust’s licence undersection 111 of the Act, Monitor may include in the licence such conditions relating togovernance as Monitor considers appropriate; andII. where Monitor is satisfied that the NHS foundation trust has breached, or is breaching, anadditional licence condition that was included under section 111 of the Act, we may use ourpowers to require the foundation trust to remove, suspend or disqualify one or more of thefoundation trust’s directors and/or governors or, if the foundation trust does not do so,Monitor may make such changes.Page 10 of 50
Competition lawMonitor has concurrent powers with the OFT to apply UK and European competition law toproviders in the health care sector in England. Where Monitor establishes an infringement of theCompetition Act and/or Articles 101/102 of the TFEU, our enforcement powers include:giving directions to bring an infringement to an end; andimposing financial penalties.Before any finding of infringement, Monitor may accept binding commitments offered to us by anundertaking.Monitor’s powers to apply competition law are not limited to the NHS but apply to all undertakingsinvolved in the provision of health care services in England. Further information on whatconstitutes an ‘undertaking’ can be found here.Overview of Monitor’s formal provider enforcement powers (simplified)Monitor’s findingEnforcement powerMonitor has reasonablegrounds to suspect:breach of a licenceconditionORfailure to give MonitorinformationOREnforcementundertakings (s106)The provider may give an undertaking to:• take steps to bring the breach to an end;• take actions to restore the situation; and/or• any other actionswhere a provider fails to comply with an undertakingBreach of a licence conditionORFailure to give MonitorinformationOperate without a licenceDiscretionaryrequirements (s105)Monitor may oblige the provider to:• take steps to bring the breach to an end;• take actions to restore the situation; and/or• pay a financial penalty.Breach of a licence conditionRevoke licence (s89)Require the NHS foundationThe governance of an NHSfoundation trust is such thatthe trust will fail or is failingto comply with its licenceImpose additionalconditions relating togovernance (s111)And if thoseconditionsare breachedthentrust to remove, suspend,disqualify one or moredirectors or members of thecouncil and if it fails,Monitor can take this actionBreach of competition lawGive directions tobring infringement toan end,impose a fine(The wording of the Health & Social CareAct 2012 and Competition Act 1998 issimplified in this diagram)Page 11 of 50
<strong>1.</strong>3 About this documentChapter 2 explains how Monitor is likely to decide whether to take action, and what kind of actionwe might decide to take.Chapter 3 is about enforcement actions and explains the factors Monitor will take into accountwhen deciding which, if any, discretionary requirements to impose or what, if any, enforcementundertakings we will accept. This chapter also covers the matters Monitor may take into accountwhen imposing a variable monetary penalty.Chapter 4 describes the processes that Monitor will follow if we decide to investigate formally apotential breach. This includes the procedures for gathering information, the information thatparties may receive about the investigation process, and the opportunity for the affected party tomake representations.Chapter 5 outlines the decision-making procedures that Monitor will follow.Chapter 6 explains what rights of appeal exist if the affected party wishes to contest a Monitorenforcement decision or a competition law decision.Page 12 of 50
2 PrioritisationThis chapter sets out the prioritisation framework that we intend to follow to make sure Monitorfocuses on the issues that best enable us to meet our duties and to make use of our resources.2.1 Prioritisation frameworkMonitor intends to apply this prioritisation framework to decisions about whether to pursueenforcement action and to all other significant cases where Monitor has discretion over whether toact. We will use this framework to inform our decisions on whether or not to begin cases, and tocontinue with them once under way. In developing this framework, Monitor has considered theapproaches taken by other regulators, many of which also use prioritisation frameworks.When assessing priorities for enforcement action, we would expect to draw on a range ofinformation, including but not limited to: intelligence and information that Monitor may collectdirectly; information from patient representative bodies and commissioners; any complaints andrepresentations made to Monitor; and information from providers themselves, including, forexample, monitoring information supplied to us.In weighing up the benefits and costs of taking action, we will consider, amongst any otherrelevant factors:The likely benefits to health care service usersOur key consideration will be the expected benefit of our work for health care service users.When we decide whether to devote resources to a matter, we will consider all types of benefitsthat our actions may generate or protect. Such benefits may include:Direct benefits to health care service users. We intend to consider the impact of ouractions on the quality of health care services, access to care and value for money spenton health care. We will consider both the short and longer term impacts of our proposedinterventions.Indirect benefits to health care service users. We will consider whether a particularaction in one area may lead to a wider, more general, benefit to health care service users.This might arise by reducing the likelihood of future breaches by the provider in question.This might also arise, for example, by prompting positive changes in the generalbehaviour of providers, commissioners or health care service users. For example,enforcement action considered appropriate in relation to one provider’s breach of theprovider conditions may also:Page 13 of 50
o deter similar breaches by other providers;o help other providers understand how obligations apply in certain circumstances;o enable commissioners to obtain better information about the strengths andcapabilities of particular providers or effective ways to procure health careservices;o enable health care service users to become better informed about their rights andempowered to make choices;o increase confidence in the functioning of the health care sector more generallywhich may lead to more providers and expansion of the sector; ando help Monitor to identify that certain aspects of the sector may not be working wellfor health care service users, resulting in future policy improvements.In assessing how much an action may benefit health care service users, we will be mindful of thelikelihood of success. When we decide whether Monitor should take action about a suspectedbreach of a licence condition, we may assess, for example, whether there is a risk that Monitormight be unable to gather the evidence to be satisfied that a condition has been breached.In determining the potential benefits of an intervention by Monitor, we will also consider whetherwe can achieve the best outcome for health care service users by ourselves acting or actingtogether with another organisation, or whether another organisation has regulatory tools thatcould tackle an issue more effectively, or is already taking steps that are likely to address thepotential harm. For example, the Care Quality Commission, the Office of Fair Trading, the CharityCommission, the NHS Commissioning Board, the NHS Trust Development Authority, and theAdvertising Standards Authority are all also able to take action within the health care sector.If the breach relates to enabling integrated care, we will also consider the potential for action toreduce inequalities, in line with our duty under the Act.The likely costs of taking actionTo ensure that we make the best possible use of our resources, we will also consider the cost ofany action. We will think about the resources needed to take a particular course of action andcompare them to the potential benefits. We propose to consider staff and non-staff costs, and thelikely duration of the work.Page 14 of 50
We also recognise that the actions we take may be costly for other organisations in the healthcare sector. So we intend to consider the impact of our possible actions on providers, and otherparties, and will pay close attention to whether the burden they would impose is in proportion tothe scale of the problem they aim to correct.Deciding whether to take formal or informal actionWhen called on to act, Monitor may need to choose between taking informal action, formal action,or no action at all. We may also consider responding to a problem in ways that do not involve theuse of our enforcement powers. For example, we may decide to review the situation, review ourown policy approach, or consider addressing the matter by using other powers such as the powerto set prices for some NHS services.Even when a matter could appropriately be addressed by using Monitor’s formal enforcementpowers, it may still be appropriate to deal with it informally and give providers an opportunity toaddress any issues without a formal investigation. Monitor’s decision on whether to take formal orinformal action will take into account the individual circumstances of the matter in hand. We willmake our decisions based on what is in the interests of health care service users in line with ourmain duty. Relevant considerations may include:the impact of the breach or potential breach on health care service users;whether the provider has already taken steps that suggest the breach is unlikely to recur,for example by:oonotifying the breach to Monitor as soon as it was identified; orvoluntarily taking action to end the breach and limit the risk of similar futurebreaches;the context in which the breach has occurred. For example, we might consider: whetherthe conduct involves repeated breaches of the same condition; a provider that isrepeatedly breaching different conditions; whether other regulators or relevantstakeholders have relevant concerns about the provider; a provider’s history of respondingto breaches; the likelihood that the action being considered resulting in compliance andthe speed at which it will result in compliance; whether the type of breach is thought to bewidespread in the health care sector; and/ orwhether any third parties (e.g. other regulators or litigants) are taking relevant action inrelation to the same breach.Page 15 of 50
If Monitor considers that informal action is preferred over formal action, or as a first attempt toresolve a matter before moving to formal action, such informal action may involve one or more ofthe following:providing guidance, or working with providers to support them in maintaining or restoringcompliance. For example, this may include the use of agreed action plans containingspecific milestones and deadlines;issuing an advisory letter to explain a provider’s obligations and what action may beadvisable to maintain compliance; andissuing a warning letter which sets out Monitor’s concerns, and notifying the provider thatif it does not take action Monitor may commence a formal investigation.In choosing the most effective response to a potential issue, we will consider which option is likelyto create the most potential benefit to health care service users, with proportionate potential coststo Monitor and the sector, in line with the principles outlined above.Page 16 of 50
3 Imposing discretionary requirements and accepting enforcementundertakings3.1 IntroductionMonitor may impose discretionary requirements where we are satisfied that a provider is, or was,in breach of a licence condition, or the requirement to hold a licence, or a requirement to supplyMonitor with information. A provider subject to a formal investigation may offer Monitor anenforcement undertaking which Monitor may accept instead of investigating further and,potentially, imposing discretionary requirements. Monitor may also accept enforcementundertakings from, others in breach of a requirement to provide us with information.This chapter outlines:the nature of the discretionary requirements that Monitor may impose;the factors that Monitor may consider in determining what requirements are needed;issues relevant to each requirement and how they may be implemented, including thefactors that Monitor may take into account when setting a variable monetary penalty; andwhen Monitor may accept enforcement undertakings.3.2 Discretionary requirementsDiscretionary requirements are formally specified in the Act and may be a:Compliance requirement: A compliance requirement is an instruction from Monitor to theprovider to take specified steps within a set period to secure that the breach not continueor recur. The principal focus of a compliance requirement is to secure compliance;Restoration requirement: A restoration requirement obliges the provider to take suchsteps within such period as Monitor may specify to secure that the position is, so far aspossible, restored to what it would have been, absent the breach. Restorationrequirements may also be used to compensate any affected party, including health careservice users and other providers. Such a requirement could require, for example, that theprovider gives up any gains it has made from the breach and restores the position of thosewho have suffered harm as a result; andPage 17 of 50
Variable monetary penalty: Variable monetary penalties require a provider to pay afinancial penalty of such amount as Monitor may specify. The variable monetary penaltymust not exceed 10% of the provider’s turnover in England.Discretionary requirements may be used in combination in relation to the same breach, whereappropriate. However, Monitor must not impose discretionary requirements on more than oneoccasion in relation to the same breach.3.3 Deciding what kind of discretionary requirements to imposeIn considering what, if any, discretionary requirements to impose, Monitor’s aim is to ensure thatany action we take promotes compliance and fulfils Monitor’s main duty to protect and promotethe interests of people who use health care services, by promoting the provision of health careservices which is economic, efficient and effective, and maintains or improves the quality of theservices. We will ensure also that we take into account all our other duties as appropriate inexercising our enforcement functions.In deciding what action is most appropriate in the circumstances of the individual case and whichrequirements, if any, to impose, we intend to consider, amongst other relevant considerations:the seriousness of the breach;ensuring provider compliance;deterring similar breaches;restoring the position to what it would have been without the breach; andthe proportionality of the remedy to the nature of the breach.Monitor may decide not to impose a discretionary requirement if we conclude that:the breach caused (or was capable of causing) no harm or harm that is not material;a discretionary requirement is not required to ensure provider compliance;a discretionary requirement is not required to restore the position to what it would havebeen without the breach; anda discretionary requirement is not required to deter similar breaches.Monitor may also decide not to impose a discretionary requirement if we conclude that the onlysuitable discretionary requirement would be disproportionate to the nature of the breach.Page 18 of 50
SeriousnessMonitor will take into account a range of relevant factors in assessing seriousness, including:the nature and the scale of the harm that a breach or potential breach has caused or iscapable of causing to health care service users. Monitor intends to assess:ooooowho has been or is likely to be affected;the extent to which any harm could be reversed or remedied;the number of health care service users affected, or potentially affected,whether directly or indirectly;the actual or potential impact on those health care users;the duration of any harmful effects of potential effects;whether the provider knew or should have known that its actions would risk noncompliance;and/orwhether the provider has committed a breach before.The more serious the breach, the more likely Monitor will be to impose discretionaryrequirements.Ensuring provider complianceMonitor will consider what action may be needed to ensure: that a breach not continue; and/orthat the provider end the breach and not repeat it. Monitor will also consider what forms ofintervention may be needed to deter similar breaches from recurring.In considering whether requirements are needed to ensure that a breach not continue, Monitorproposes to assess, amongst other relevant factors:whether the breach has been brought to an end;if the breach is continuing, what steps the provider has taken and/or proposes to takevoluntarily in order to bring the breach to an end;whether, if the provider has proposed voluntary steps, it would still be beneficial to ensurethat the breach does not continue by imposing requirements relating to those proposedsteps;whether there are other steps which Monitor considers should be taken in order to ensurethat the breach not continue; andPage 19 of 50
whether any third parties (e.g. other regulators or litigants) are taking relevant action inrelation to the same breach.If Monitor considers that discretionary requirements are needed to ensure a breach not continue,it is likely that Monitor will impose a compliance requirement.In considering whether requirements are needed to deter further breaches by the provider,Monitor proposes to assess, amongst other relevant factors:Whether the provider knew, or should have known, that its actions would risk noncompliance;this may include evidence that the breach was genuinely accidental and thatthe provider has already taken steps to avoid non-compliance;How much the provider has gained, or is expected to gain, from the breach - relevantbenefits may include financial and other benefits such as reputational benefits; Whether the provider has taken steps that suggest the breach in question will not recur -this could be, for example, by:oooonotifying the breach to Monitor as soon as it was identified;voluntarily taking effective steps to ensure that the breach is remedied and to limitthe risk of further breaches taking place in future;cooperating generally with Monitor’s enquiries and requirements; ortaking action to compensate those affected.Whether the breach could represent part of a pattern of non-compliance, emerging orotherwise, such that Monitor considers that imposing requirements is necessary toincentivise compliance in the future; andWhether any third parties (e.g. other regulators or litigants) are taking relevant action inrelation to the same breach.Monitor is likely to impose a discretionary requirement if we are satisfied that it is needed to deterfuture breaches. A compliance requirement is likely to be appropriate if there are practical stepswhich Monitor could require of the provider in order to ensure that the breach not recur. Thegreater the risk of future breach, the greater the likelihood that Monitor will impose a variablemonetary penalty (whether instead of or in addition to other discretionary requirements) in orderto deter a recurrence.Page 20 of 50
Deterring similar breaches by other providersIn order to deter similar breaches by other providers, Monitor will consider how the action we takein one case might also affect the incentives on other providers to comply. For example, Monitormay find it appropriate to adjust the severity of the requirements we impose according to:the extent to which the type of breach under consideration is thought to be widespread inthe health care sector;the extent of harm the type of breach has caused (or is capable of causing) to health careservice users; orwhether previous sanctions have been effective or ineffective in deterring others fromtaking similar action.If Monitor considers that it is necessary to adjust the proposed discretionary requirements in orderto deter similar breaches by other providers, it is likely that Monitor would impose (or increase) avariable monetary penalty. However, in appropriate cases the objective of deterring similarbreaches by other providers may be met through the imposition of, or modifications to, acompliance requirement or a restoration requirement.Restoring the position to what it would have been without the breachMonitor will consider whether it would be desirable and feasible to take steps to restore theposition to what it would have been without the breach. If so, Monitor may impose a restorationrequirement.Restoration could require a provider to give up any gains it has made from a breach and restorethe position of those who have suffered harm as a result. Restoration requirements may befinancial or non-financial.Where a breach of a regulatory requirement causes harm to another party, Monitor considers thata restoration requirement may have a number of advantages. It might be used to ensure thatparties do not profit from a breach, and it may deter others from similar conduct in future. It mayalso compensate any affected parties.However, there may be some practical limits to Monitor’s ability to impose restorationrequirements. For example, it may be difficult to establish which parties (whether individuals orcategories of parties) have been harmed by a breach, or the extent of any such harm.Page 21 of 50
ProportionalityMonitor will ensure the action we take is proportionate and reasonable in the circumstances athand, and that we balance the need to deter harmful conduct with the need to ensure thecontinued provision of health care services to health care service users.Before imposing a requirement, Monitor therefore proposes to consider:the specific circumstances of the relevant provider;how any requirement is likely to affect the provider’s delivery of health care services; andIn particular, Monitor will consider the impact of a particular requirement on the provider’s futurefinancial viability. We propose to consider factors such as:the cost of the requirement to the provider;the provider’s current financial position;how much the provider has gained from the relevant breach;whether a requirement is likely to cause the provider financial hardship or distress thatcould:ooothreaten service continuity; orcause further harm to health care service users by reducing competition andchoice in the market; orany wider harm to health care service users that might arise from reducing theresources available to the provider in line with our main duty.3.4 Variable monetary penaltiesThis section sets out the factors which Monitor will consider when deciding on the appropriateamount of a variable monetary penalty.Variable monetary penalties may require a provider to pay a monetary penalty to Monitor whichMonitor must pay into the Government Consolidated Fund. The variable monetary penalty mustnot exceed 10% of the provider’s turnover in England. The Department of Health has publishedits intended definition of ‘turnover’ for these purposes, which is available here.Page 22 of 50
An important objective of imposing a penalty is deterring similar conduct in future. The amount ofany penalty must be sufficient to ensure that it will act as an effective incentive to compliance,having regard to the seriousness of the breach. The factors Monitor will take into account,therefore, include amongst other relevant considerations:the seriousness of the breach;ensuring provider compliance;deterring similar breaches by other providers; andthe proportionality of a variable monetary penalty to the nature of the breach.The factors relevant to each of these considerations are described in section 3.3 above.As well as these matters, Monitor will consider any relevant aggravating and mitigating factors.Penalties are likely to be higher when we identify one or more aggravating factors. Aggravatingfactors could be, but are not limited to, where:Monitor has previously imposed a discretionary requirement on, or accepted anenforcement undertaking from, the relevant provider concerning similar or related matters;there is a positive intent to contravene, in that the provider must have been aware, orcould not reasonably have been unaware, that its conduct would lead to a breach; ora provider has not cooperated with Monitor’s investigation.Penalties are likely to be lower when we identify relevant mitigating factors. Mitigating factorscould be, but are not limited to, where:a provider takes timely and effective action to remedy the effects of a breach, includingaction to restore any actual or potential harm caused;a provider self-reports a breach; ora provider has cooperated fully with Monitor’s investigation and requirements.Page 23 of 50
3.5 Enforcement undertakingsA provider may offer an enforcement undertaking during the course of a formal investigation.Monitor may accept the undertaking if we have reasonable grounds to suspect that the provideris, or was, in breach of a licence condition, the requirement to hold a licence, or a requirement tosupply Monitor with information. An enforcement undertaking may include a commitment to takesteps to secure that the breach in question does not continue or recur. A provider may alsoundertake to restore the position to what it would have been had the breach in question notoccurred, or action (including the payment of a sum of money) to benefit any other licence holderor commissioner affected by the breach.The decision whether to accept an enforcement undertaking, rather than to continue aninvestigation and potentially impose discretionary requirements, is at Monitor’s discretion and willdepend on the circumstances. In considering an enforcement undertaking offered by a provider,Monitor intends to take into account the factors outlined in section 3.3 above.Agreed enforcement undertakings may be less burdensome on the provider than thediscretionary requirements which Monitor would otherwise have imposed. This is in recognition of:the cooperation demonstrated by that provider; andthe fact that Monitor is then able to devote resources to other matters on the basis thatMonitor can stop pursuing an investigation or parts of an investigation.We intend to maintain a register of enforcement undertakings. We are likely to require providersthat have given undertakings report on compliance. Any reporting commitments will be agreed aspart of the agreement of the enforcement undertaking as a whole.If the relevant provider complies with the enforcement undertaking, Monitor cannot take furtheraction in relation to the relevant breach or suspected breach. For example, having acceptedundertakings which are then complied with, Monitor cannot seek to impose additionaldiscretionary requirements or to revoke the provider’s licence in relation to the same breach.Failing, or partially failing, to comply with an enforcement undertaking accepted by Monitor mayresult in the imposition of a discretionary requirement.Page 24 of 50
4 Enforcement - case procedures4.1 IntroductionThis chapter outlines the general procedures that Monitor intends, in general, to follow whenconducting an investigation that may result in us taking formal enforcement action.This chapter focuses first on the procedures relevant to licence enforcement and to imposingdiscretionary requirements or accepting enforcement undertakings. Under schedule 11 of the Act,Monitor is bound to follow certain processes when taking such enforcement action.This chapter also outlines:the processes relevant to licence revocation;the processes Monitor intends to follow when using our additional powers where thegovernance of an NHS foundation trust is such that it is failing, or will fail, to comply withone or more of its licence conditions; andan introduction to the processes relevant to enforcement under competition law.As we explained earlier, we are following a similar approach to that set out in this guidance in‘translating’ breaches of NHS foundation trusts’ terms of Authorisation into appropriate regulatoryaction under the licence, to take effect as the licence comes into force. The processes we follow,however, are likely to be more bespoke than the case procedures set out in this section. Forexample, we do not intend to publish case initiations or consult on draft findings for this transitionactivity. We are currently working closely with the relevant foundation trusts.4.2 Enforcement procedures4.2.1 Case initiationWhen we become aware of a potential breach, we will consider how to proceed in accordancewith our prioritisation principles - see chapter 2. Where we decide to begin an investigation of apotential breach, we will notify the relevant party or parties and set out what Monitor isinvestigating, the key contacts at Monitor, and the expected timetable for the investigation.Information about the investigation will, where appropriate, be published on Monitor’s website.Monitor considers that publication of case details will generally be beneficial, as it will help tohighlight issues that are of concern to Monitor and deter inappropriate conduct, and help ensurethat all interested parties are aware of an issue and can provide relevant information.Page 25 of 50
4.2.2 InvestigationOnce Monitor has decided to start a formal investigation, we may use our powers under the Act togather information – see section 104 of the Act. These powers allow us to ask parties specified inthe Act (licence holders, provider licence applicants, providers who are exempt from requiring alicence, providers who should hold a provider licence, the NHS Commissioning Board and clinicalcommissioning groups) for any information, documents or other items Monitor considers arenecessary or expedient to have in order to perform our regulatory functions.Information includes information, documents or records kept by means of a computer. Monitoralso has the power to require the provision of the information, documents or records in legibleform. The Monitor provider licence will also require licence holders to provide Monitor with suchinformation as we consider necessary to fulfil our licensing functions, which can be used inaddition to or instead of the powers specified in section 104 of the Act.During the course of an investigation, Monitor may need to issue several information requests todetermine whether a provider has breached its obligations or for any other appropriate reason.Monitor will try to limit the burdens placed on parties to an investigation, as much as possible, andensure that our information gathering is focused and proportionate - in line with our obligationsunder section 68 of the Act.At any point during an investigation, Monitor may close a case without further action if, forexample, we consider that there is insufficient evidence of a breach or that a formal investigationshould no longer be prioritised. Where we consider it appropriate, we will also publish our reasonsfor making such decisions on our website.There is no specific time period within which Monitor must complete an investigation, and howlong an investigation lasts will vary depending on the complexity of the issue and how muchrelevant information is available. But when an investigation is opened, we will provide parties withour expected timescales and provide updates to the timescale as appropriate.4.2.3 Case updatesIn longer running cases, we intend to give the relevant parties regular updates about how theinvestigation is progressing, and when key decisions are likely to be taken.We intend to:keep the parties to the investigation informed about the expected timetable and anychanges; andPage 26 of 50
provide regular case updates to parties, for example, each month, by telephone or inwriting.We will also offer providers under investigation the opportunity to meet representatives of thecase team at appropriate intervals, for example every four to six months to ensure that partieshave the opportunity to raise points directly with us and to discuss the progress of aninvestigation.4.2.4 Entering into enforcement undertakingsThis section sets out our proposed procedure for entering into enforcement undertakings, whichwe are required to publish in accordance with schedule 11 of the Act.Where Monitor considers it appropriate we may discuss with the provider the possibility ofaccepting an enforcement undertaking. A provider may offer an enforcement undertaking at anypoint during the course of an investigation, up until a final decision is made as to whether theprovider has acted in breach and as to any discretionary requirement, although the closer aninvestigation is to its conclusion, the smaller the resource saving to be made by acceptingundertakings - see section 3.5.Offering an enforcement undertaking Where a provider wishes to offer an enforcementundertaking, it should first discuss this with the case team. If after this it wishes to do so, it shouldwrite to the case team setting out the commitments it is offering, any timescales for implementingthe commitments and their anticipated impact. If Monitor thinks that an enforcement undertakingmay be an appropriate way to resolve a matter, we may invite a provider to consider making anoffer of an enforcement undertaking. When a provider makes such an offer, Monitor expects thatwe will normally respond by telling the provider that we either:do not consider it appropriate to enter into discussions about undertakings at that time andintend to continue the formal investigation; orconsider it appropriate to enter into discussions about undertakings.In some circumstances, Monitor is likely to wish to continue with an investigation until we can besatisfied that an enforcement undertaking may or may not be an appropriate way forward. In mostcircumstances, Monitor will tell the provider when we expect to be in a position to respond to anoffer of an enforcement undertaking.When undertakings have been offered and Monitor considers they may be an appropriate way toresolve the matter; we are likely to discuss the form and content of the undertaking offered withPage 27 of 50
the provider, and invite the parties to make any changes that we consider necessary. In decidingwhether to accept enforcement undertakings, Monitor will assess the proposed undertaking byreferring to the factors outlined in section 3.3 above.Accepting an enforcement undertaking Where Monitor has received a proposed enforcementundertaking that we think may represent an appropriate resolution of the matter we may seekviews on whether it is appropriate. When we choose to seek views, we will also give reasons whywe propose to accept the draft enforcement undertaking, referring to the factors outlined insection 3.3.Seeking views may range from formal and extensive public engagement to more informal, briefengagement with third parties. The decision on whether to seek views will be made on a case-bycasebasis. In deciding whether to seek views we will consider all relevant matters includingwhether it is in the interests of health care service users to take action quickly, for example wherethere is a concern about patient safety, as well as any benefits of wider engagement. We will alsoconsider the factors outlined in section 3.3.After seeking views, Monitor would then need to decide whether the proposed undertakingsshould be modified, accepted, or rejected.After an enforcement undertaking has been accepted Where Monitor accepts an enforcementundertaking, we are under a legal obligation to publish it. That means Monitor cannot accept anenforcement undertaking on the basis that any of the terms of the undertaking will be keptconfidential. We can only withhold from publication any part of an enforcement undertaking whichcontains information which is:commercial, information whose disclosure would or might significantly harm the legitimatebusiness interests of the affected party; orinformation about the private affairs of an individual, where disclosure would or mightsignificantly harm that person’s interests.The terms of an enforcement undertaking - including, in particular, the action it specifies and theperiod within which the action must be taken - may be varied if both Monitor and the provideragree.Where Monitor is satisfied that a provider has complied with an enforcement undertaking, wemust issue a certificate to that effect – this is called a compliance certificate. A provider who hasgiven an enforcement undertaking can apply to Monitor at any time for a compliance certificate,Page 28 of 50
including in the application evidence to demonstrate that the provider has satisfactorily met thecompliance requirement, and other relevant information to be required and specified by Monitor.Monitor must decide whether or not to issue a compliance certificate, and give notice to theapplicant of the decision within 14 days after the day on which we receive the application. Thereis a right of appeal from a decision to refuse this application.If at any point Monitor considers that a provider who has given an enforcement undertaking hassupplied inaccurate, misleading or incomplete information in relation to the undertaking then wemay treat the provider as having failed to comply with the undertaking. In that case, after givingnotice, Monitor may revoke any compliance certificate given to that provider.Table 4.1 summarises the process for entering into enforcement undertakings1 Monitor informs the provider in writing that we have launched formal enforcement action inrelation to a suspected breach.2 If it wishes, the provider contacts the case team to discuss the possibility of undertakingsand following this it writes to Monitor with an outline of a proposed enforcementundertaking. The provider may also write to Monitor with an outline of a proposedundertaking after an invitation from Monitor to do so.3 Monitor responds to the provider indicating, if necessary, whether the matter is suitable foran enforcement undertaking and the terms and timescales on which discussions mightproceed.4 Discussions on an enforcement undertaking may proceed based on the provider’s offer at2 above and/or alternative suggestions made by Monitor.5 If provisional agreement is reached, Monitor may seek views as set out above if itconsiders this appropriate.6 Following consideration of views if sought Monitor either:accepts the enforcement undertaking – with any necessary and agreedmodifications – and closes our investigation; orrejects the proposed undertakings and continues our investigation.7 Monitor will publish the agreed enforcement undertaking.Page 29 of 50
4.2.5 Discretionary requirementsNotice of IntentUnder schedule 11 of the Act, if Monitor intends to impose a discretionary requirement on aprovider we must issue the provider with a ‘Notice of Intent’ containing the following information:• the proposal to impose a discretionary requirement;• the effect of the discretionary requirement;• the grounds for making the proposal - a statement of the evidence and reasoning behindthe proposal as well as our preliminary conclusion;• an explanation of the effect of section 106 of the Act (enforcement undertakings),including whether we have considered an enforcement undertaking, or may beconsidering them;• the circumstances (if any) in which Monitor may not impose the requirement; and• the period for making representations (‘notice period’).Where Monitor is considering imposing discretionary requirements, we may seek views onwhether they are appropriate. When we choose to seek views, we will also give reasons for ourproposals, referring to the factors outlined in section 3.3.Seeking views may range from formal and extensive public engagement to more informal, briefengagement with third parties. The decision on whether to seek views will be made on a case-bycasebasis. In deciding whether to seek views we will consider all relevant matters includingwhether it is in the interests of health care service users to take action quickly, for example wherethere is a concern about patient safety, as well as any benefits of wider engagement. We will alsoconsider the factors outlined in section 3.3.After seeking views, Monitor would then need to decide whether the proposed requirementsshould be imposed and in the original or modified form.Making representations to MonitorUnder schedule 11 of the Act, on receiving a Notice of Intent, the relevant parties will be invited tosubmit representations to Monitor in writing and in person within a specified period, known as the‘notice period’ of at least 28 days from the day after the Notice of Intent was received.On request, providers may also make oral representations to the relevant decision-makers withinMonitor.Page 30 of 50
In certain circumstances, Monitor may reduce the notice period to a minimum of five days. Thismay be the case, as specified in schedule 11, where:• Monitor is proposing a compliance requirement or restoration requirement; and• Monitor considers that a shorter notice period is necessary to prevent or minimise furtherbreaches.Final noticeUnder schedule 11 of the Act, after the end of the notice period, Monitor must decide whether toimpose the discretionary requirement, with or without modification, or impose any otherdiscretionary requirement.If, after issuing the Notice of Intent, Monitor has become aware of new information which theprovider should in fairness be given an opportunity to comment on before Monitor decideswhether to impose a discretionary requirement, Monitor will make arrangements for the providerto be given that opportunity.If the decision-makers - see chapter 5 - decide to impose a discretionary requirement Monitor willissue a further notice, known as a ‘final notice’. The final notice will contain the followinginformation:• the discretionary requirement which Monitor has decided to impose;• the effect of the discretionary requirement;• the reasons for imposing the requirement;• the consequences of failing to comply with the requirement; and• the right of appeal.Although we are not required by the Act to do so, we expect that Monitor will always publish finalnotices unless the circumstances of the case make this inappropriate. Where appropriate, we willconsider the need to obtain confirmation of factual accuracy prior to publication.If Monitor imposes a variable monetary penalty, the final notice, as specified in schedule 11 of theAct, will also contain the following information:Page 31 of 50
• how to make the payment;• the period within which payment must be made;• any discount for early payment; and• the rate of interest payable for late payment.The provider will have a minimum period of 28 days, as specified in schedule 11 of the Act, fromthe day after the final notice was received to pay a monetary penalty. A monetary penalty may notbe imposed unless the Notice of Intent was issued within five years of the last day of the period inwhich the licensee was in breach.Any financial penalty paid to Monitor will be transferred to the Government Consolidated Fund.Under schedule 11 of the Act, if the provider does not pay a monetary penalty imposed byMonitor within the specified time, interest may be payable and, in addition to any other action torecover these amounts due, Monitor may take action to collect the money, and any interest owed,through the civil courts as a civil debt.After the decisionUnder schedule 11 of the Act, Monitor has some freedom to change a discretionary requirementafter we have given a final notice. At that stage, Monitor may still:• withdraw the requirement;• reduce the amount of any variable monetary penalty;• extend the time allowed for paying the penalty; or• extend the time for taking steps specified in a compliance or restoration requirement.Although we are not required to do so, we expect that where Monitor has decided to take any ofthe above steps, we will always publish notices setting out the steps decided on and our reasonsfor taking any of these steps, unless the circumstances of the case would make thisinappropriate.The provider may appeal a decision to impose a discretionary requirement. This is explained inchapter 6.Page 32 of 50
Non-compliance penaltiesUnder schedule 11 of the Act, if the provider fails to comply with a compliance or restorationrequirement that Monitor has imposed, we may take further action against the provider.Monitor may impose a financial penalty known as a ‘non-compliance penalty’ on the provider.If we decide to take this action, we will first issue a ‘non-compliance notice’, as specified inschedule 11 of the Act, setting out:• the amount of the non-compliance penalty;• the reasons for imposing the non-compliance penalty;• how to pay the non-compliance penalty;• the period within which a provider must pay;• any discount for early payment;• the consequences of late payment; and• the right of appeal.Although we are not required to do so, we expect that Monitor will always publish non-compliancenotices unless the circumstances of the case would make this inappropriate. Where appropriate,we will consider the need to obtain confirmation of factual accuracy prior to publication.If any part of the original payment demanded is not paid by the deadline, Monitor may underschedule 11 of the Act increase the amount payable by up to 50% of the amount of the originalpenalty.As with discretionary requirements, under schedule 11 of the Act Monitor has discretion to reducethe amount of the penalty or extend the payment period of a non-compliance penalty. We maymake such changes at any time in the process after we have imposed a non-compliance penalty.Payments from non-compliance penalties are recoverable as civil debts and we will pay them intothe Government Consolidated Fund.The provider can appeal against Monitor’s decision to impose a non-compliance penalty. Theprocess for appealing is explained in chapter 6.Page 33 of 50
4.3 Procedures for licence revocationAs outlined in section <strong>1.</strong>2, Monitor may revoke a provider’s licence if we are satisfied that theprovider has failed to comply with a licence condition – see section 89 of the Act. In making thedecision that a provider has failed to comply with its licence condition, we intend the followingparts of this proposed guidance to apply:Chapter 2 - deciding whether a matter is a priority;Chapter 4, section 4.2 - case initiation, investigation and case updates;Chapter 5 - decision making; andChapter 6 - appeals.Monitor expects that we would consider revoking a provider’s licence only rarely, as to do sowould prevent a provider from continuing to provide NHS health care services where it is obligedto hold a licence. If Monitor considers it appropriate to do so, we will consider revoking aprovider’s licence.In considering whether to revoke a licence, Monitor’s aim will be to fulfil Monitor’s main duty toprotect and promote the interests of people who use health care services by promoting theprovision of health care services which is economic, efficient and effective, and maintains orimproves the quality of the services. We intend to consider, amongst any other relevant factors,the following factors as set out in section 3.3 above, that is:the seriousness of the breach;ensuring provider compliance;deterring similar breaches; andthe proportionality of the remedy to the nature of the breach.Monitor considers that it would normally only be appropriate to revoke a licence if we are satisfiedthat the objectives could not be met through the imposition of discretionary requirements (or theacceptance of enforcement undertakings).Case initiation, investigation, case updateWe propose that the processes relevant to licence revocation will be as we set out in sections4.2.1, 4.2.2, and 4.2.3.Page 34 of 50
Notice of Intent (section 90)Where Monitor proposes to revoke a licence, we must give notice to the provider setting out ourreasons for proposing to revoke the licence and the time that the licensee has to makerepresentations - see section 90 of the Act. Monitor may take such action only where we aresatisfied that a licence holder has failed to comply with a condition of its licence.Monitor must provide the licence holder with no less than 28 days from date of receipt, withinwhich representations may be made. Providers may, on request, also make oral representationsto relevant decision-makers (see chapter 5 below) within Monitor.Where Monitor is proposing this action, we may seek views on whether it is appropriate. When wechoose to seek views, we will also give reasons for our proposal, referring to the factors outlinedin section 3.3.Seeking views may range from formal and extensive public engagement to more informal, briefengagement with third parties. The decision on whether to seek views will be made on a case-bycasebasis. In deciding whether to seek views we will consider all relevant matters includingwhether it is in the interests of health care service users to take action quickly, for example wherethere is a concern about patient safety, as well as any benefits of wider engagement. We will alsoconsider the factors outlined in section 3.3.After seeking views, Monitor would then need to decide whether to take the proposed action orother action.Notice of Decision (section 91)Having considered the licence holder’s representations Monitor will issue a Notice of Decisionconfirming whether or not the provider’s licence has been revoked. Under section 91 of the Act,the Notice of Decision must explain the provider’s right of appeal (see chapter 6 below).A licence revocation can only have effect once the licensee’s right to appeal has ended or oncean appeal has been confirmed by the First-Tier Tribunal or the appeal has been abandoned – seesections 91 and 92 of the Act (see chapter 6 below).Although we are not required by the Act, we expect that Monitor will always publish final noticesunless the circumstances of the case mean that this would be inappropriate.The licensee can appeal against Monitor’s decision to revoke its licence. The process forappealing is explained in chapter 6.Page 35 of 50
4.4 Procedures for imposing additional licence conditions on NHSfoundation trusts and removing, suspending or disqualifying directors orgovernors of NHS foundation trustsWe intend that the following parts of this proposed guidance apply to Monitor’s actions undersection 111 of the Act:Chapter 2 - deciding whether a matter is a priority;Chapter 4, section 4.2 - case initiation, investigation and case updates; andChapter 5 - decision making.As outlined in section <strong>1.</strong>2, there are two parts to Monitor’s powers under section 111:I. where Monitor is satisfied that an NHS foundation trust’s directors and/or governors arefailing to (a) secure compliance with conditions in the foundation trust’s licence, or (b) takesteps to reduce the risk of a breach of a condition in the foundation trust’s licence undersection 111 of the Act, Monitor may include in the licence such conditions relating togovernance as Monitor considers appropriate; andII. where Monitor is satisfied that the NHS foundation trust has breached or is breaching anadditional licence condition that was included under section 111 of the Act, we may use ourpowers to require the foundation trust to remove, suspend or disqualify one or more of thefoundation trust’s directors and/or governors or, if the foundation trust does not do so,Monitor may make such changes.A separate process must be followed to exercise the second power. The process that Monitorproposes to follow is set out below.Case initiation, investigation, case updateWe propose that the processes relevant to section 111 actions will be as we set out in sections4.2.1, 4.2.2, and 4.2.3.Notice of Intent (section 111)If Monitor is minded to impose an additional licence condition on a foundation trust, Monitor willissue a notice to the foundation trust informing it of:• the proposal to impose additional licence conditions;• the anticipated effect of the additional licence conditions;Page 36 of 50
• any incidental or consequential modifications which may be necessary or expedient toother licence conditions in consequence of the additional licence conditions;• the grounds for making the proposal; and• the period for making representations (‘notice period’).Monitor would follow the same procedure in the event that we were minded to vary any suchlicence condition.Where Monitor is proposing such action, we may seek views on whether it is appropriate. Whenwe choose to seek views, we will also give reasons for our proposals, referring to the factorsoutlined in section 3.3.Seeking views may range from formal and extensive public engagement to more informal, briefengagement with third parties. The decision on whether to seek views will be made on a case-bycasebasis. In deciding whether to seek views we will consider all relevant matters includingwhether it is in the interests of health care service users to take action quickly, for example wherethere is a concern about patient safety, as well as any benefits of wider engagement. We will alsoconsider the factors outlined in section 3.3.After seeking views, Monitor would then need to decide whether the proposed condition shouldbe modified, retained or not included.If Monitor is satisfied that a foundation trust has not complied with additional licence conditionsand Monitor is minded to require a foundation trust to remove, suspend or disqualify one or moreof its directors and/or governors, we will issue a notice to the foundation trust informing it of:• the proposal to require the foundation trust to remove, suspend or disqualify one or moreof its directors and/or governors;• the grounds for making the proposal; and• the period for making representations (‘notice period’).Page 37 of 50
Final notice (section 111)At the end of the notice period, if Monitor has not changed its view following the foundation trust’srepresentations, Monitor would issue a final notice.If the decision-makers - see chapter 5 - decide to impose an additional licence condition, Monitorwill issue a further notice, known as a ‘final notice of additional licence conditions’. This notice willcontain the following information:• the licence conditions which Monitor has decided to impose; any incidental orconsequential modifications which must be made to other licence conditions;• the anticipated effect of the additional licence conditions;• the reasons for imposing the additional licence conditions; and• the consequences of failing to comply with them.Monitor would follow the same procedure in the event that we decided to vary any such licencecondition.If the decision-makers - see chapter 5 - decide to impose governance changes, Monitor will issuea further notice, known as a ‘final notice of governance changes’. It will contain the followinginformation:• the requirements of the foundation trust to remove, suspend or disqualify one or more ofits directors and/or governors and appoint interim governors or directors;• the reasons for imposing them; and• the consequences of failing to comply with them.Although we are not required to do so, we expect that Monitor will always publish final noticesunless the circumstances of the case mean that this would be inappropriate.Should the foundation trust not comply with this notice, Monitor will, if it considers appropriate,itself implement one or more of the requirements set out in the notice.4.5 Procedures for investigations under competition lawWhere Monitor suspects anti-competitive behaviour in the health care sector in England, we maydecide to use our powers under the provider licence, or apply the prohibitions on anti-competitiveagreements and abuse of a dominant position set out in the Competition Act and Articles 101 and102 of the Treaty on the functioning of the European Union.Page 38 of 50
Monitor will have concurrent powers to apply competition law, meaning that either Monitor or theOFT could act in relation to a particular case. Monitor and the OFT will decide which organisationis best placed to investigate an issue on a case-by-case basis.As far as possible, we intend that the procedures Monitor follows are consistent whether takingaction under the Act or the Competition Act or the TFEU. But when Monitor takes action under theCompetition Act, we must adhere to the same statutory rules that the OFT would if it were takingthe case (see Competition Act 1998 (Office of Fair Trading’s Rules) Order 2004 StatutoryInstrument 2751 of 2004 http://www.legislation.gov.uk/uksi/2004/2751/contents/made). Similarly,when enforcing Articles 101 and 102 of the TFEU, Monitor must comply with the requirements inEuropean Union Regulation 1/2003.In any enforcement proceedings under the Competition Act, Monitor will also be required to haveregard to:• the OFT’s guidance on the circumstances in which it may be appropriate to accept bindingcommitments. This is contained in an annex to the OFT’s Enforcement Guidelines, seehttp://www.oft.gov.uk/shared_oft/business_leaflets/ca98_guidelines/oft407.pdf.• the OFT’s guidance as to the appropriate amount of a penalty, seehttp://www.oft.gov.uk/shared_oft/business_leaflets/ca98_guidelines/oft423.pdf.The following sections of this proposed guidance are also relevant to investigations under theCompetition Act or TFEU:Chapter 2 - deciding whether a matter is a priority;Chapter 4, section 4.2 - case initiation and case updates;Chapter 5 - decision making; andChapter 6 - appeals.We may, in the future, publish more detailed guidance on Monitor’s procedures in applyingcompetition law.Page 39 of 50
5 Decision-making for enforcement cases5.1 IntroductionThis chapter sets out Monitor’s proposed approach to taking three key decisions relevant toformal enforcement:I. the decision to formally investigate a potential breach or infringement;II. the decision to provisionally find a breach and to issue, for example, a ‘Notice of Intent’; andIII. the decision to find a breach and to issue, for example, a ‘final notice’.5.2 The decisions to launch a formal investigation and to make aprovisional findingThe first two decisions relevant to a formal investigation are: whether to formally investigate amatter; and whether to make a provisional finding that there has been a breach or infringement.In both cases, Monitor proposes the decisions are taken by a senior staff member in the Monitorgroup, advised by technical experts as appropriate, responsible for the enforcement action. Thisperson will oversee the investigation up to and including any provisional finding, and takedecisions about whether or not enforcement undertakings should be accepted in relation tobreaches of obligations by providers, or commitments in competition law cases.5.3 The decision to find a breach or infringementFor final decisions concerning a breach or an infringement, Monitor proposes that a decisionmakingcommittee comprising a number of Monitor’s senior staff would take the decision as towhether there has been a breach/infringement, and what sanctions, if any, should be imposed.The membership of the decision-making committee will be decided on a case-by-case basis, tosuit the matter in hand and reflect the risk and complexity involved. It may involve staff from anydiscipline throughout Monitor. Monitor’s Board may decide that it forms the decision-makingcommittee in relation to enforcement matters that are of particular significance to health careservice users. In other cases, Monitor’s Executive team may form the decision-making committee,or it may be made up of other members of Monitor’s senior staff.However the final decision-making committee is composed, the majority of the decision makerson the committee would not have had any significant prior involvement in the investigation – thatis, they would bring a ‘fresh pair of eyes’ to the matter. The senior staff member responsible forPage 40 of 50
the first two decision-making points (decision to investigate and provisional finding) and othermembers of the investigating team may participate in the discussions around making the finaldecision, but will not be members of the decision-making committee for the purpose of making thedecision. It is noted in this context that Monitor has processes in place for decision-makers todeclare where necessary any conflicts of interest.If a party offers an enforcement undertaking after a provisional finding, the decision-makingcommittee would take the decision as to whether that undertaking should be accepted.To ensure that parties have the opportunity to make representations directly to decision-makers,members of the decision-making committee would hear any oral representations made inresponse to a provisional finding.Page 41 of 50
6 Rights of appeal6.1 IntroductionThis chapter outlines the decisions that are appealable and the appeal processes as specified bylaw.6.2 Provider enforcementA provider may appeal a decision to impose a discretionary requirement, the imposition of a noncompliancepenalty or the refusal by Monitor to issue a certificate of compliance in relation to anenforcement undertaking to the First-tier Tribunal.The First-tier Tribunal is a specialist judicial body established under the Courts and EnforcementAct 2007. The main function of the First-tier Tribunal is to hear and decide appeals in specifiedareas of law (see http://www.justice.gov.uk/tribunals).Discretionary requirementsA provider has a right of appeal to the First-tier Tribunal against a decision to impose adiscretionary requirement. An appeal may be brought on one or more of the following grounds:• that the decision was based on an error of fact;• that the decision was wrong in law;• that the amount of a variable monetary penalty is unreasonable;• that the nature of a compliance requirement or restoration requirement is unreasonable; or• that the decision was unreasonable for any other reason.Once the provider has lodged an appeal, the discretionary requirement will be suspended untilthe appeal is determined.When the Tribunal reaches a decision on the appeal, it may take any of the following actions:• confirm, vary or withdraw the discretionary requirement;• take such steps as Monitor could take in relation to the breach; or• remit the decision whether to confirm the requirement, or any matter relating to thedecision, to Monitor.Page 42 of 50
Non-compliance penaltiesA provider may appeal to the First-tier Tribunal against one of Monitor’s decisions to impose anon-compliance penalty on any of the following grounds:• that the decision was based on an error of fact;• that the decision was wrong in law; or• that the decision was, or the amount of the penalty is, unfair or unreasonable.If the provider lodges an appeal, the non-compliance penalty will be suspended until the appeal isdetermined.When making a decision on the appeal, the Tribunal may take the following action:• confirm, vary or withdraw the non-compliance penalty; or• remit the decision whether to confirm the penalty, or any matter relating to that decision, toMonitor.Enforcement undertakingsA provider may appeal, to the First-tier Tribunal, a refusal from Monitor to meet a request for acertificate of compliance on the following grounds:• the decision was based on an error of fact;• the decision was wrong in law; or• the decision was unfair or unreasonable.In making a decision on the appeal, the Tribunal may either confirm Monitor’s decision or directthat it is not to have effect.6.3 Licence revocationA licensee has a right of appeal to the First-tier Tribunal against a decision to revoke a licenceunder section 89(b). An appeal may be brought on one or more of the following grounds:• that the decision was based on an error of fact;• that the decision was wrong in law; or• that the decision was unreasonable.Page 43 of 50
Once the provider has lodged an appeal, the licence revocation does not take effect until theappeal is confirmed or abandoned.When making a decision on the appeal, the Tribunal may take any of the following actions:• confirm Monitor’s revocation decision;• direct that Monitor’s revocation decision is not to have effect; or• remit the revocation decision to Monitor.6.4 Competition law enforcementMonitor’s Competition Act and TFEU decisions may be appealed to the Competition AppealTribunal. Appeals can be brought by addressees of Monitor’s decisions and by third parties with asufficient interest. Appealable decisions include decisions as to whether there has been acompetition law infringement; interim measures’ decisions; and decisions on the imposition of, orthe amount of, a penalty (see http://www.catribunal.org.uk/242/About-the-Tribunal.html#Appealunder-CA98).The Competition Appeal Tribunal was created by section 12 and Schedule 2 to the Enterprise Act2002 which came into force on 1 April 2003. The Competition Appeal Tribunal is a specialistjudicial body with cross-disciplinary expertise in law, economics, business and accountancywhose function is to hear and decide cases involving competition or economic regulatory issues.The Competition Appeal Tribunal has wide powers to determine most appeals under competitionlaw on their merits and may:• confirm or set aside all or part of the decision;• remit the matter to Monitor;• impose, revoke or vary the amount of any penalty;• give such directions, or take such other steps as Monitor could have given or taken; or• make any other decision which Monitor could have made.Page 44 of 50
AnnexMonitor’s powers of enforcement under the Health andSocial Care Act 2012<strong>1.</strong> CompetitionFunctions under the Competition Act (section 72)Monitor and the Office of Fair Trading have concurrent functions under Part 1 of the CompetitionAct, relating to the provision of health care services in England where:a) agreements, decisions or concerted practices are anti-competitive (anti-competitivepractices); orb) there are abuses of a dominant position in a market (abuse of dominant position).These powers relate to the Competition Act and the TFEU.Functions under Part 4 of the Enterprise Act 2002 (section 73)Monitor and the Office of Fair Trading have concurrent functions under Part 4 of the EnterpriseAct 2002 (market investigations), relating to activities which concern the provision of health careservices in England.2. Licensing procedureLicence revocation (section 89)Monitor may revoke a provider’s licence on the application of the licensee, or if Monitor is satisfiedthat the licensee has failed to comply with a condition of its licence.Monitor must give notice to the licensee if we propose to revoke its licence. The notice must setout Monitor’s reasons for its proposal; and specify the period (not less than 28 days from the dateof receipt) within which representations about it may be made to Monitor.Right to make representations (section 90)Monitor must give notice to the licensee if we propose to revoke its licence. That notice must:a) set out Monitor’s reasons for our proposal; andb) specify the period (not less than 28 days beginning with the day after that on which thenotice is received), for representations to be made on it to Monitor.Page 45 of 50
Notice of decisions (section 91)If Monitor decides to revoke a licence, we must give notice of our decision to the licensee. Thenotice must explain the right of appeal against that decision.The decision will take effect when we specify, subject to not being a day earlier than:a) the day on which a decision on appeal (if made) is confirmed or the appeal is abandoned;b) the day on which Monitor receives notification that the licensee does not intend to appeal(before the end of the period for bringing an appeal); orc) the day after the period for bringing an appeal.Appeals to the Tribunal (section 92)An appeal may be made to the First-tier Tribunal against Monitor’s decision to revoke a licence.The grounds for an appeal are that the decision was:a) based on an error of fact;b) wrong in law; orc) unreasonable.On hearing the appeal, the First-tier Tribunal may:a) confirm Monitor’s decision;b) direct that the decision is not to have effect; orc) remit the decision to Monitor.3. EnforcementInformation provision (section 104)Monitor may require a person (any provider of NHS health care services in England whetherlicensed or not, the NHS Commissioning Board and a Clinical Commissioning Group) to provideus with any information, documents, records or other items which we consider is necessary orexpedient for our functions. This includes information, documents or records kept by means of acomputer and Monitor has the power to require the provision of the information, documents orrecords in legible form.Discretionary requirements (section 105)Monitor may impose one or more discretionary requirements on a person if Monitor is satisfiedthat the person:Page 46 of 50
a) has provided, or is providing, an NHS health care service without either a licence or anexemption to hold a licence;b) is a provider licensee who is in breach of a licence condition; orc) is in breach of a requirement to provide information.Discretionary requirement means:a) a requirement to pay a monetary penalty to Monitor (a “variable monetary penalty”).The variable monetary penalty must not exceed 10% of the person’s turnover inEngland, such amount to be calculated in the manner set out in regulations by theDepartment of Health. If all or part of a variable monetary penalty is not paid by the timerequired, the unpaid balance carries interest at the rate specified in section 17 of theJudgments Act 1838; subject to the total interest not exceeding the amount of thepenalty;b) a requirement to take such steps, within such period, to secure that the breach inquestion does not continue or recur (a “compliance requirement”); orc) a requirement to take such steps, within such period, to secure that the position is, sofar as possible, restored to what it would have been if the breach in question was notoccurring or had not occurred (a “restoration requirement”).Monitor must not impose discretionary requirements on a person on more than one occasion inrelation to the same breach.Enforcement undertaking requirements (section 106)Monitor may accept an enforcement undertaking from a person if Monitor has reasonablegrounds to suspect that the person:a) has or is providing, an NHS health care service without either a licence or an exemptionto hold a licence:b) is a licensee who has or is providing, an NHS health care service in breach of a licencecondition; orc) is in breach of a requirement to provide information.An enforcement undertaking is that a specified action will be taken within a specified period. Theaction must be:a) to secure that the breach does not continue or recur;Page 47 of 50
) to secure that the position is, so far as possible, restored to what it would have been ifthe breach was not occurring or had not occurred;c) action (including the payment of a sum of money) to benefit:(i)any other licence holder affected by the breach;(ii) any commissioner of NHS health care services which is affected by the breach; ord) action of such a description as may be allowed in regulations to be made by theDepartment of Health.Where Monitor accepts an enforcement undertaking, unless the person has failed to comply withthe undertaking or any part of it:a) Monitor may not impose any discretionary requirement which we would otherwise havepower to impose in respect of the breach; andb) Monitor may not revoke that person’s licence if the breach is a breach of a licencecondition.Where the person has complied with only part of an enforcement undertaking, Monitor must takethe partial compliance into account in deciding whether:a) to impose a discretionary requirement on the person; orb) to revoke the person’s licence, if the breach is a breach of a licence condition.Further provision about enforcement powers (section 107)Monitor must follow schedule 11 provisions about procedures for discretionary requirements andenforcement undertakings.Guidance on use of enforcement powers (section 108)Monitor must publish guidance about how we intend to impose discretionary requirements, acceptenforcement undertakings and the procedures we will follow to do so. Monitor may revise theguidance. Monitor must consult persons we consider appropriate before publishing or revising theguidance.The guidance, in regard to discretionary requirements, must include information about:a) the circumstances in which Monitor is likely to impose a discretionary requirement;b) the circumstances in which Monitor may not impose a discretionary requirement;Page 48 of 50
c) the matters likely to be taken into account by Monitor in determining the amount of anyvariable monetary penalty to be imposed (including, where relevant, any discounts forvoluntary reporting); andd) rights to make representations and rights of appeal.Monitor must have regard to the guidance or revised guidance in imposing discretionaryrequirements and accepting enforcement undertakings.Publication of enforcement action (section 109)Monitor must include, in our annual report, information about:a) cases in which a discretionary requirement has been imposed during the financial year ofthe report (except if it was overturned on appeal); andb) cases in which an enforcement undertaking has been accepted during that financial year.But Monitor must not include information which we are satisfied is:a) commercial information where its disclosure might significantly harm the legitimatebusiness interests of the relevant provider; orb) information relating to the private affairs of an individual where its disclosure mightsignificantly harm that person’s interests.Notification of enforcement action (section 110)As soon as is practicable after imposing a discretionary requirement or accepting an enforcementundertaking, Monitor must notify:a) the NHS Commissioning Board;b) Clinical Commissioning Groups who are likely to be affected by the requirement orundertaking; andc) any person exercising regulatory functions in relation to the relevant provider.4. Imposition of licence conditions on NHS foundation trusts andremoving, suspending or disqualifying directors or governors of NHSfoundation trusts (section 111)Where Monitor is satisfied that the governance of an NHS foundation trust is such that thefoundation trust will fail to comply with the conditions of its licence, Monitor may include agovernance condition(s) in its licence that we consider is appropriate to reduce that risk.Page 49 of 50
This includes where Monitor is satisfied that the council of governors, the board of directors or thecouncil of governors and board of directors together are failing:a) to secure compliance with conditions in the foundation trust’s licence; orb) to take steps to reduce the risk of a breach of a condition in the foundation trust’s licence.Monitor may modify such a condition once it has been included.Such a condition will have effect until the Secretary of State for Health orders that section 111 ofthe Act ceases to have effect.Where Monitor is satisfied that the trust has breached or is breaching this new condition Monitormay by notice require the foundation trust to:a) remove one or more of the directors or members of the council of governors and appointinterim directors or members of the council;b) suspend one or more of the directors or members of the council of governors from officeas a director or member for a set period; orc) disqualify one or more of the directors or members of the council of governors fromholding office as a director or member for a set period.Where Monitor is satisfied that a foundation trust has failed or is failing to comply with such anotice, Monitor may do one or more of the things which we required the foundation trust to do.Where Monitor includes a condition, we may also make such incidental or consequentialmodifications as we consider necessary or expedient to any other condition of the licenceconcerned which is affected.Monitor can also, in relation to such a condition, use the enforcement powers under sections 105and 106 of the Act.Where Monitor includes a condition by modifying a standard condition of the licence concerned,the modification does not prevent any other part of the condition from continuing to be regardedas a standard condition.Page 50 of 50
Monitor, 4 Matthew Parker Street, London SW1H 9NPTelephone: 020 7340 2400Email: enquiries@monitor.gov.ukWebsite: www.monitor.gov.uk© Monitor (28 March 2013)Publication code: IRG 12/13This publication can be made available in a number ofother formats on request. Application for reproduction ofany material in this publication should be made in writingto enquiries@monitor.gov.uk or to the address above.
BOARD OF DIRECTORSMeeting Date and Part:Subject:Section:Executive Director with overallresponsibility:Author of Paper:Details of previous discussionand/or dissemination:Key Purpose:Action required by Board ofDirectors:Executive Summary:14 th June 2013 – Part IMonitor Guidance on Procurement, Patient Choice andCompetition RegulationsInformationRichard Renaut, Director of Service DevelopmentSandy Edington, Associate Director of Service DevelopmentN/APatient Safety Health & Safety Performance Strategy Note for InformationThis report gives an overview of the two draft consultationpapers relating to the National Health Service (Procurement,Patient Choice and Competition) Regulations 2013 (No. 2).recently released by MonitorStrategic Goals & Objectives: 1,4,7Links to CQC Registration:(Outcome reference)Section 1, Outcome 1Links to AssuranceFramework/Key Risks:Type of Assurance:InternalExternal
Board of Directors – Part I14 th June 2013Monitor Guidance on Procurement Patient Choiceand Competition Regulations<strong>1.</strong> IntroductionMonitor has recently released two draft consultation papers relating to the National HealthService (Procurement, Patient Choice and Competition) Regulations 2013 (No. 2).http://www.monitor-nhsft.gov.uk/regulating-health-care-providerscommissioners/cooperation-and-competition/our-cooperation-and-compeBoth of these sets of guidance are for commissioners (CCGs and NHS England). The firstindicates how commissioners can comply with these regulations and the second describesenforcement steps and processes that Monitor will take under the regulations. This paperis therefore split into two components; Compliance and Enforcement.The Board may recall the national debates about competition versus integration and thesedocuments are part of the evolution of that debate.As this is a consultation a number of questions are posed in each document. A completeset of these for the compliance document is at Annex A. The consultation periodconcludes on the 15 th July.The guidance adopts a principles based approach and the intention is that this allowscommissioners to make locally based decisions based on local needs and requirements.The over-arching requirement is that commissioners must;• Adhere to good practice in relation to the procurement of NHS funded healthcareservices• Protect the rights of patients to make choices• Avoid anti-competitive behaviour, unless it is in the interests of NHS health careusersIn terms of application to an NHS FT, the guidance gives an idea of the procurementapproaches that are expected and where we may be able to dispute processes ordecisions that commissioners choose to take. This constitutes the formal procurementguidance to PCTs and therefore is likely to be the document that would guide and supporta challenge by a provider to a commissioner’s clinical procurement process.2. Compliance with the RegulationsThis document sets out the objectives of procurements;• Securing the needs of health care service users• Improving the quality of services and• Improving the efficiency with which services are providedMonitor Guidance on Procurement Patient Choice and Competition Regulations Page 1 of 4For Information
Board of Directors – Part I14 th June 2013There are a number of factors that commissioners are expected to take account ofincluding;• Evaluate and identify the health needs of the population• Take a holistic view of the needs of the health care users• Consider the needs of all users (vulnerable, socially excluded, settings, sustainabilityincluding the impact of a procurement decision on a provider’s capacity to continueother services)• Monitor the quality and efficiency of existing service provision• How health needs might be best secured (including safety, volume of work forclinicians)The above may include consultation processes with local clinicians, out of area expertsand utilise relevant clinical guidelines and best practice, but it does not mention consultinglocal or existing providers. This would therefore be an area to pursue by way ofresponding to their questions.Procurements are expected to be undertaken in a transparent, proportional and nondiscriminatoryway and commissioners should “consider appropriate ways of improvingservices including through services being provided in a more integrated way, enablingproviders to compete to provide services and allowing patients a choice of provider”The section on transparency, as it relates to procurement, indicates that in judgingcommissioner compliance, Monitor would consider the extent to which commissionershave:• Published information on their future procurement strategies and intentions• Taken steps to ensure that providers are aware of their intention to procure particularservicesThese would be of particular interest to us since it has been difficult to get advanceinformation from Commissioners.There is a section which provides guidance as to the interaction between competition,choice and integrated care. –“…commissioners to consider whether introducingcompetition and choice and delivering care in a more integrated way could be used toimprove quality and efficiency.” Enacting the guidance seems to be firmly with thecommissioners and it will be left to them to make judgments based on statements such asthat above. Much of the guidance will inevitably end up being tested by lawyers. A keyissue that arises throughout the guidance on integration and cooperation is that of sharingclinical records.The need to publish contract opportunities for NHS services is examined and inparticular circumstances are described where it may be appropriate to award a contractwithout publishing a contract notice – “single capable provider”.Qualification of providers (e.g. Any Qualified Provider) is covered in a separate sectionand this applies to services other than in the context of a competitive tender. It providedguidance on transparency, non-discrimination and proportionality.Monitor Guidance on Procurement Patient Choice and Competition Regulations Page 2 of 4For Information
Board of Directors – Part I14 th June 2013There are sections in the guidance on record keeping and the opportunity forcommissioners to obtain support from Commissioning Support Units or from othersources such as the private or voluntary sectors.Conflicts of InterestThere is a significant section on conflicts of interest, in particular where individuals areinvolved in commissioning and potentially the provision of a service. The documentrecognises that this can be direct or indirect and financial or non-financial. It alsorecognises that can affect all stages of a procurement process from specificationdevelopment to contract award.Other than excluding conflicted individuals from the procurement process there are otherways suggested, including use of out of area GPs or independent lay persons. It alsosuggests that decisions taken could be subject to an independent review by a third partyand that the processes of how these are being managed should be full recorded.Anti-Competitive BehaviourThere is a short section on anti-competitive behaviour by commissioners. The process forMonitor assessing whether a commissioner has acted anti-competitively envisagesweighing the costs and the benefits of the commissioner’s procurement process andassessing the net effects of these on users of health care services. Monitor may considerwhether a commissioner has:• “…limited the extent to which providers are able to compete by limiting the totalnumber of patients a provider can treat or income a provider can earn…”• “…restricted the ability of providers to differentiate themselves to attract patients,such as, for example, by imposing minimum waiting times that providers must adhereto or restricted opening hours, without objective justification…”The final section of the Compliance document relates to the commissioner responsibility tooffer patient choice. The part of this that affects us relates to maximum waiting times inelective care. This supports existing requirements such that where a patient that hasbeen referred for elective care will not have commenced treatment within 18 weeks of areferral being received the commissioners are required to take all reasonable steps toensure that a patient is offered an appointment with a clinical appropriate alternativeprovider.3. Enforcement of the RegulationsThe other guidance published in addition to the above is the enforcement guidanceassociated with the same Procurement, Patient Choice and Competition Regulations.This covers the steps that Monitor would take on being informed of a potential breach ofthe guidance by a commissioner. These steps include;Monitor Guidance on Procurement Patient Choice and Competition Regulations Page 3 of 4For Information
Board of Directors – Part I14 th June 2013• Prioritisation –which cases Monitor would pursue and to what extent - based on thelikely benefits to health care service users and including the likely costs of takingaction• Making a “Declaration of Ineffectiveness” – this encompasses making “Directions” [toa commissioner] such as varying or withdrawing a tender or otherwise directing acommissioner• Accepting undertakings from commissioners in response to a “Direction” or to avoid a“Declaration of Ineffectiveness”4. RecommendationThe Board is asked to note this report for informationMonitor Guidance on Procurement Patient Choice and Competition Regulations Page 4 of 4For Information
Board of Directors – Part I14 th June 2013Annex AResponse form:Substantive guidance on the Procurement, Patient Choice andCompetition RegulationsWe are consulting on the guidance that we intend to publish about how to comply with theProcurement, Patient Choice and Competition Regulations and with certain requirements relatingto patient choice in the NHS Commissioning Board and Clinical Commissioning Groups(Responsibilities and Standing Rules) Regulations 2012 which Monitor has the power to enforceunder the Procurement, Patient Choice and Competition Regulations.Chapter 3, Question 1:Do you agree with the examples of factors that Monitor may consider when deciding whethercommissioners have complied with their duty to act transparently, proportionately and in a nondiscriminatoryway?Are there other factors that you think we should highlight?Chapter 3, Question 2:Do you agree with the examples of factors that Monitor may consider when deciding whethercommissioners have complied with their duty to procure services from the providers most capableof delivering commissioners’ objective and that provide best value for money?Are there other factors that you consider we should highlight?Chapter 3, Question 3:Do you think that the description of integrated care, choice and competition is helpful?Chapter 3, Question 4:Do you agree with the examples of the factors that Monitor may take into account in decidingwhether commissioners have complied with their general duty to consider appropriate means ofimproving quality and efficiency, including through services being delivered in an integrated way,patient choice and competition?Are there other factors that you consider we should highlight?Chapter 4, Question 1:Do you think the description of the considerations that commissioners should take into accountwhen deciding whether or not to publish a contract opportunity is helpful?Do you think there are other considerations that we should list?Monitor Guidance on Procurement Patient Choice and Competition Regulations Page 1 of 3For Information
Board of Directors – Part I14 th June 2013Annex AChapter 4, Question 2:Do you think that the examples of situations where it may be appropriate for a commissioner toaward a contract without publishing a contract notice and running a competitive tendering processare helpful?Chapter 4, Question 3:Do you think that the description of the circumstances in which a contract will be treated as a newcontract is helpful? Are there other situations where a contract may amount to a new contract thatyou think we should highlight?Chapter 5, Question 1:Do you agree with the examples of the factors that Monitor might take into account in decidingwhether commissioners have complied with their duty to apply and establish transparent,proportionate and non-discriminatory qualification criteria?Are there other factors that you consider we should highlight?Chapter 6, Question 1:Do you agree with the suggestions of the types of information that may be relevant for thepurposes of compiling an adequate record of a contract award decision to demonstrate thatcommissioners have complied with their relevant duties under the National Health Service Act2006?Are there other types of information that may be relevant that you consider we should highlight?Chapter 7, Question 1:Do you agree with the examples of the factors that Monitor might take into account in decidingwhether commissioners have complied with their duty to ensure that any person providingcommissioning support or assistance acts in accordance with the relevant requirements of theProcurement, Patient Choice and Competition Regulations?Are there other factors that you consider we should highlight?Chapter 8, Question 1:Do you agree with the examples of interests in the provision of services that may give rise to aconflict with the interests in commissioning them?Are there other examples that you consider we should highlight?Chapter 8, Question 2:Do you agree with the examples of factors that Monitor may take into account when decidingwhether a conflict affects or appears to affect the integrity of a contract award?Are there other factors that may be relevant that you consider we should highlight?Monitor Guidance on Procurement Patient Choice and Competition Regulations Page 2 of 3For Information
Board of Directors – Part I14 th June 2013Annex AChapter 8, Question 3:Do you agree with the suggestions of the types of information that may be relevant for thepurposes of compiling an adequate record to demonstrate that a conflict of interest has beenappropriately managed?Are there other types of information that may be relevant that you consider we should highlight?Chapter 9, Question 1:The cost/benefit analytical framework is the same as that applied by the Cooperation andCompetition Panel when analysing anti-competitive behaviour under the Principles and Rules.Do you think this description is helpful?Chapter 9, Question 2:Do you agree with the examples of the considerations that Monitor may take into account inassessing whether a commissioner has engaged in anti-competitive conduct that is not in theinterests of patients?Do you think there are other examples that we should highlight?Chapter 10, Question 1:Do you agree that we should include a description of the requirements relating to patient choice inthe Responsibilities and Standing Rules Regulations that Monitor has the power to enforce underthe Procurement, Patient Choice and Competition Regulations?Chapter 10, Question 2:Do you agree with the examples of relevant factors that Monitor may take into account in decidingwhether commissioners have complied with their duties relating to patient choice?Are there other relevant factors that you consider we should highlight?Monitor Guidance on Procurement Patient Choice and Competition Regulations Page 3 of 3For Information
BOARD OF DIRECTORSMeeting Date and Part:Subject:Section:Executive Director with overallresponsibility:Author of Paper:Details of previous discussionand/or dissemination:Key Purpose:Action required by Board ofDirectors:Executive Summary:14 th June 2013 – Part ICommissioner Requested Services and Location SpecificServicesInformationRichard Renaut, Director of Service DevelopmentSandy Edington, Associate Director of Service DevelopmentN/APatient Safety Health & Safety Performance StrategyNote for InformationThis report gives an overview of the new Monitor licensingregime.PPStrategic Goals & Objectives: 1,4,7Links to CQC Registration:(Outcome reference)Section 1, Outcome 1Links to AssuranceFramework/Key Risks:Type of Assurance:InternalExternalP
Board of Directors Part I14 th June 2013<strong>1.</strong> IntroductionCommissioner Requested Servicesand Location Specific ServicesIn the past as part of the previous licensing regime for Foundation Trusts (FTs) andbecause of the quasi-independence that this provides, for each FT certain services weredesignated as “mandatory”. The intention of this was that the Trust could not arbitrarilyclose down services, for example on the basis of an adverse financial position for a givenservice. The new Monitor licensing regime has meant a review of this position and thepublication of guidance for FTs http://www.monitor-nhsft.gov.uk/home/news-eventspublications/our-publications/browse-category/guidance-health-care-providers-and-co-19The guidance uses the term Commissioner Requested Services (CRS) for previouslymandatory services. It also introduces a new term - Location Specific Services (LCS) forservices that “should be maintained by the trust Special Administrator at or close to theprovider”. This latter category is therefore intended to be for services that need to beprovided even if a provider fails financially.2. Key Issues• Services described as mandatory have been transferred entirely to the newcategory of CRS• The CRS designation will apply until April 2016• Commissioners are expected to review the designation of CRS services over thenext three years• There is a 4 stage Designation Framework developed to support the commissionerprocess3. The Designation Framework1) Information gathering – to define the service being assessed and identify keyfeatures of the service;2) Considering suitable alternative provision – to assess the availability, capacity andaccessibility of alternative providers and/or pathways;3) Considering any impact on health inequalities – to assess whether disadvantagedgroups may be significantly adversely affected if the service is withdrawn, includingwhether they might face particular difficulties in accessing alternative providers; and4) Considering interdependent services – to determine whether the safe and effectiveoperation of the service requires co-dependent services to be retained as well, orwhether there are feasible alternative providers for any co-dependent services.Commissioner Requested Services and Location Specific Services Page 1 of 3For Information
Board of Directors Part I14 th June 20134. Implications for RBCH, CC, MergerRBCHThere would seem to be two ways of looking at this guidance and the mandatory categorythat preceded it. Originally it is assumed to have been put in place to ensure that if Trustfound a particular combination of costs and income meant they would lose money, theycould not simply abandon the service. Conversely if a commissioner wanted to abandon aservice with a Trust they could not do so if it was mandated (at least theoretically).The new guidance clarifies that this is a commissioner process, with stakeholder input viaconsultation and the thrust of the guidance is to ensure that Trust do not divest themselvesof services where the commissioners want them to continue. We are moving into an erawhere the PBR regime is likely to be flexed more and more with for example further blockcontract arrangements being put in place. One of the keys issues for any Trust withrespect to a given service is the financial position and a Trust could be boxed in by thisguidance with a CCG unprepared to pay an appropriate rate for a service, but the Trustunable to close it if it is designated as a CRS.The list of CRS for RBCH (attached at Appendix A) appears to include a large proportionof our existing services. Notable perhaps is the designation of CRS to 476 ClinicalHaematology inpatient spells.Competition Commission & RemediesThis Monitor guidance is new and there appears to be relatively little information aboutdebates and decisions relating to FT’s mandatory services in the past. The CC remediesfor the RBCH / Poole merger are as yet unclear, but if they mandate that a service wecurrently operate has to be taken over by another organisation (e.g. DHUFT) to maintaincompetition, it is unclear if this would be trumped or otherwise affected by a service beingdesignated as a CRS.MergerThe impact of the CRS designation on transformation type exercises is uncertain, butimplies that if the CCG wanted a service to continue they would have to ensure that theconsultation process they undertook as part of their review of CRS has this result. If wewish to shed the designation of CRS we would need to get the CCG to review this statusand to agree (perhaps via their consultation process) that the designation no longerapplies. It is also not clear if a merged organisation would assume the designations ofCRS from the two individual trusts. This CRS designation might limit the extent to whichsome transformations were able to take place.If merger did not proceed and services (perhaps particularly at Poole) were substantiallyuneconomic they may not be in a position to reduce or close services if these wereclassified as CRS.Commissioner Requested Services and Location Specific Services Page 2 of 3For Information
Board of Directors Part I14 th June 2013It is likely that the impact of the Commissioner Requested Services and Location SpecificServices will become relevant only when substantial amendments or changes to servicesare being proposed, either by commissioners or by providers. At this point either of theseparties as well as other stakeholders such as members of the public may attempt to invokethis guidance. Inevitably there would follow some legal testing of this and the results of thisare difficult to anticipate.5. RecommendationsThe Board is asked to note this report for informationCommissioner Requested Services and Location Specific Services Page 3 of 3For Information
List of Commissioner Requested ServicesOrganisationThe Royal Bournemouth And Christchurch Hospitals NHS Foundation TrustNHS Code:RDZSector:AcuteOutpatientsA&EFAOutpatients Outpatients Emergency Elective Day ElectiveOutpatient OutpatientFUp Procedures Inpatients Cases Inpatients Best Practice Non-Elective pre-assess exclusionsFollow UpAttendances Treatments Spells Spells Spells Spells Spells Spells SpellsCode DescriptionAttendancesFirstAttendances130 ACCIDENT & EMERGENCY 15,136 - - - - - - - - - -180 ENT 54,958 - - - - - - - - - -100 GENERAL SURGERY - - - - 2,995 4,723 2,059 - 22 - -101 UROLOGY - - - - 1,260 6,365 1,944 - 28 - -110 TRAUMA & ORTHOPAEDICS - - - - 10 4,381 3,421 - 1 - -130 OPHTHALMOLOGY - - - - 228 9,284 700 - - - -140 ORAL SURGERY - - - - 1 264 - - - - -180 ACCIDENT & EMERGENCY - - - - 18,026 - - - - - -190 ANAESTHETICS - - - - 5 1,147 14 - - - -300 GENERAL MEDICINE - - - - - 6,077 696 - 221 - -301 GASTROENTEROLOGY - - - - - 1,339 139 - 2 - -303 CLINICAL HAEMATOLOGY - - - - 299 2,745 177 - 6 - -314 REHABILITATION - - - - 18 - 1 - - - -320 CARDIOLOGY - - - - 1,937 2,768 1,504 - 454 - -330 DERMATOLOGY - - - - - 3,572 - - 1 - -361 NEPHROLOGY - - - - 2 - - - - - -370 MEDICAL ONCOLOGY - - - - 321 1,122 59 - - - -400 NEUROLOGY - - - - - - 1 - - - -410 RHEUMATOLOGY - - - - - 1,488 - - 2 - -430 GERIATRIC MEDICINE - - - - - - 1 - 1 - -502 GYNAECOLOGY - - - - 220 974 613 - 2 - -560 MIDWIFE EPISODE - - - - - - 1 - 1,085 - -810 RADIOLOGY - - - - - 49 13 - - - -100 GENERAL SURGERY - 945 1,007 171 - - - - - 445 -101 UROLOGY - 4,810 7,283 4 - - - - - 1,392 -103 BREAST SURGERY - 2,875 3,034 353 - - - - - 265 -104 COLORECTAL SURGERY - 1,694 2,151 1,050 - - - - - - -105 HEPATOBILIARY & PANCREATIC SURGERY - 90 202 6 - - - - - - -106 UPPER GASTOINTESTINAL SURGERY - 2,045 899 172 - - - - - - -107 VASCULAR SURGERY - 1,415 875 356 - - - - - 175 -110 TRAUMA & ORTHOPAEDICS - 9,912 16,888 1,286 - - - - - 10,111 -120 ENT - 991 1,408 2,889 - - - - - - -130 OPHTHALMOLOGY - 13,313 26,295 1,518 - - - - - 764 -140 ORAL SURGERY - 1,822 1,132 755 - - - - - - -143 ORTHODONTICS - 1,059 1,977 7,970 - - - - - - -190 ANAESTHETICS - 6,005 78 - - - - - - 6,226 -191 PAIN MANAGEMENT - 586 445 8 - - - - - - -300 GENERAL MEDICINE - 2,414 2,411 2 - - - - - 170 -301 GASTROENTEROLOGY - 2,872 3,299 25 - - - - - - -302 ENDOCRINOLOGY - 706 1,789 - - - - - - - -303 CLINICAL HAEMATOLOGY - 1,459 9,460 - - - - - - - -306 HEPATOLOGY - 842 2,187 - - - - - - - -307 DIABETIC MEDICINE - 1,689 7,122 - - - - - - - -320 CARDIOLOGY - 6,839 8,048 - - - - - - 2,955 -329 TRANSIENT ISCHAEMIC ATTACK - 358 53 96 - - - - - - -330 DERMATOLOGY - 4,763 9,990 6,208 - - - - - - -340 RESPIRATORY MEDICINE - 2,841 7,043 - - - - - - - -360 GENITOURINARY MEDICINE - 15,587 8,949 - - - - - - - -370 MEDICAL ONCOLOGY - 679 6,449 1 - - - - - - -410 RHEUMATOLOGY - 3,394 8,344 715 - - - - - - -420 PAEDIATRICS - 311 510 43 - - - - - - -430 GERIATRIC MEDICINE - 1,902 2,422 179 - - - - - - -501 OBSTETRICS - 102 3,737 - - - - - - - -502 GYNAECOLOGY - 5,613 5,137 2,409 - - - - - 377 -560 MIDWIFE EPISODE - 3,024 3,009 - - - - - - - -800 CLINICAL ONCOLOGY (previously RADIOTHERAPY) - 14 43 - - - - - - - -100 GENERAL SURGERY - - - - - - - 235 - - -101 UROLOGY - - - - - - - 250 - - 33104 COLORECTAL SURGERY - - - - - - - - - - 66110 TRAUMA & ORTHOPAEDICS - - - - - - - 227 - - 4130 OPHTHALMOLOGY - - - - - - - 464 - - 634140 ORAL SURGERY - - - - - - - 17 - - -143 ORTHODONTICS - - - - - - - 7 - - -180 ACCIDENT & EMERGENCY - - - - - - - 178 - - 3,351190 ANAESTHETICS - - - - - - - 33 - - 59300 GENERAL MEDICINE - - - - - - - 626 - - 10301 GASTROENTEROLOGY - - - - - - - 23 - - 10303 CLINICAL HAEMATOLOGY - - - - - - - 902 - - 6306 HEPATOLOGY - - - - - - - - - - 6307 DIABETIC MEDICINE - - - - - - - - - - 1311 CLINICAL GENETICS - - - - - - - - - - 113313 CLINICAL IMMUNOLOGY and ALLERGY - - - - - - - 62 - - 5314 REHABILITATION - - - - - - - - - - 205316 CLINICAL IMMUNOLOGY and ALLERGY - - - - - - - - - - 57317 CLINICAL IMMUNOLOGY and ALLERGY - - - - - - - 401 - - 271320 CARDIOLOGY - - - - - - - 100 - - -330 DERMATOLOGY - - - - - - - 129 - - 1340 RESPIRATORY MEDICINE - - - - - - - - - - 1370 MEDICAL ONCOLOGY - - - - - - - 3,514 - - 1400 NEUROLOGY - - - - - - - - - - 1,723410 RHEUMATOLOGY - - - - - - - 58 - - 333501 OBSTETRICS - - - - - - - - - - 1502 GYNAECOLOGY - - - - - - - 82 - - 2654 DIETETICS - - - - - - - - - - 2,750655 ORTHOPTICS - - - - - - - - - - 7,055810 RADIOLOGY - - - - - - - - - - 8Total 70,094 102,971 153,676 26,216 25,322 46,298 11,343 7,308 1,825 22,880 16,706
BOARD OF DIRECTORSMeeting Date and Part: 14 June 2013 Part 1Subject:Appointment of new Medical Director for RBCHSection:InformationExecutive with OverallResponsibilityTony SpotswoodAuthor of Paper:Details of previousdiscussion and/ordissemination:Key Purpose:Action required by BoD:Executive Summary:Strategic Goals &Objectives:Links to CQCRegistration: (Outcomereference)Links to AssuranceFramework/Key Risks:Type of Assurance:Tony SpotswoodNot relevantPatient Safety Health & Safety Performance StrategyXXTo note the arrangement to appoint a new Medical Directorfor the TrustProcess to secure feedback to allow appointment of a newMedical DirectorMaintaining local servicesQuality and LeadershipInternalXExternal
Board of Directors Part 114 June 2013Appointment of a new Medical Director for The RoyalBournemouth and Christchurch Hospitals Foundation TrustAs the Trust Board are aware Dr Mary Armitage is retiring after many years ofoutstanding service in September 2013. The Trust will therefore need to appoint anew Medical Director. This process is not straightforward because at the time wemake such an appointment it will not be clear as to whether we are indeed mergingwith Poole Hospital or will remain as an independent separate organisation. Thedecision of the Competition Commission as to whether two approve or prevent themerger isn’t likely to be known before September.I have therefore invited expressions of interest for the Medical Director role andenclose for information a copy of the Job Description for the Medical Director.Candidates have considered the role in the context that it may be for a period ofseven months, but could conceivably be for a period of three years. Followingvarious discussions I am delighted to confirm that Mr Basil Fozard has put himselfforward as a candidate for the role and discussions with Clinical Directors and othersenior medical colleagues on Basil’s candidature will take place on 7 June. It isclearly important that there is broad support for any candidate appointed MedicalDirector and views are therefore being sought accordingly. Subject to thesediscussions the Board will be asked to move ahead to formally appoint a newMedical Director with a view to a minimum of a month’s overlap between the newappointee starting and Dr Armitage retiring.This paper is provided for informationTony SpotswoodChief ExecutiveAppointment of a new Medical Director Page 1 of 1Discussion
Job DescriptionPOST TITLEREPORTS AND ACCOUNTABLE TOKEY WORKING RELATIONSHIPSMedical DirectorChief ExecutiveBoard of DirectorsTrust Executive and ClinicalManagement BoardConsultant Medical StaffPostgraduate DeanClinical TutorsDirector of Research and DevelopmentMedical Personnel ManagerJOB SUMMARYThe Medical Director is responsible for the leadership of, and management ofprofessional issues associated with the medical workforce and the services providedby doctors.The Medical Director is a member of the Executive Team and the Trust Board and assuch will contribute to the overall development of the Trust’s strategic direction and beaccountable for the Trust’s performance and governance as a statutory organisation.The Medical Director has specific responsibility for providing advice and information onmedical and related clinical issues, including:• Providing strong and effective medical leadership to the organisation• Working closely with the Director of Nursing and Associate Medical Director onClinical Governance• Developing and overseeing the Trust’s strategy on Research and Development(R&D)• Leading on medical education and the management and development of linkswith the Deanery, working closely with the Director of HRThe Medical Director will advise on and help determine medical policy and direction forthe Trust providing a vital link between the medical staff and the Board of Directors.He/she will support and provide professional leadership to Clinical Directors workingclosely with the Chief Operating Officer.The Medical Director will be the responsible officer accountable to the GMC for theprofessional standards of Doctors.All Directors work as part of a cohesive team and where necessary take leadresponsibility for corporate issues outside their immediate sphere of responsibility.TS - June 20131
KEY RESPONSIBILITIESSTRATEGY AND CLINICAL SERVICESContribute as a full member of the Board in the development and implementation ofthe Trust’s strategic direction, corporate planning and policy development and decisionmaking.Input fully to the work underpinning the proposed merger of the Royal Bournemouthand Christchurch Hospitals NHS FT and Poole Hospital NHS FT.Interpret Health policy and guidance for the Board and medical profession, advising onits implications and practical implementation.Ensure that the Trust delivers its corporate clinical targets, influencing and maintainingdeveloping alignment on the part of the Trust’s medical workforce, with the Trust’sgoals and objectives.As the most senior doctor in the Trust, provide strong and effective medical leadershipand advice to inform corporate decisions, and advise on the shape of future clinicalservices.Provide leadership, encouragement and support to enable the medical workforce todevelop and run their services appropriately.Contribute to the development of service policy, particularly relating to national orregional initiatives, directives from NICE, the Care Quality Commission or others areimplemented appropriately and in line with best practice.GOVERNANCEIn conjunction with the Director of Nursing, lead Clinical Governance in the Trustensuring that the Governance structures are appropriate and that development andchanges in clinical practices are appropriately supported and communicated in thehealth community.Chair appropriate committees as agreed through the terms of reference, includingResearch and Clinical Effectiveness, Mortality Group, Drug and Therapeutics andMedicine’s Governance.Lead on clinical governance issues involving doctors, including reviewing SUIs/AIRsand clinical concerns.The Medical Director will support the Clinical Audit lead in ensuring Clinical Audit isundertaken within the Trust in accordance with the agreed plan.TS - June 20132
MEDICAL LEADERSHIPAs Medical Director and Responsible Officer, provide effective professional leadershipof all medical staff working for the Trust, and support to Associate Medical Directorsand Clinical Directors ensuring their development needs are reviewed and supported.Identify and nurture medical leadership potential in the Trust with the aim of havingeffective succession planning.In conjunction with the Director of HR deal appropriately with problems arising from theconduct, performance and health of medical and dental staff.Act as a management side member in meetings and negotiations with the LocalNegotiating Committee for medical and dental staff ensuring all agreements reachedmaintain the commitment and morale of medical staff whilst delivering cost effective,flexible, high quality medical care.Oversee and participate in the process of Consultant appraisal and Revalidation,ensuring both the quality of the process and the robustness of individual appraisalsand appropriate record- keeping.The Medical Director will be managerially responsible for the Chief Pharmacist andResearch and Development structure in the Trust, and will work with relevant staff onthe overall R&D strategy and enhance its reputation and output as a centre of researchexcellence.Oversee processes to review the Trust’s committee governing Clinical ExcellenceAwards.To support Clinical Directors in the job planning process.EDUCATIONWork with Medical Education leads, Medical Personnel and others involved in medicaleducation to provide post-graduate medical education and training and theprofessional development of all doctors in the Trust.Provide guidance on the development and implementation of a medical educationstrategy which supports the Trust and contributes to the wider NHS agenda.Ensure that the Trust meets all its obligations for the training and education of juniormedical staff, and complies with the Royal College and NHDS guidance regulation andrecommendations.Ensure that appropriate action is taken following visits from colleges, PostgraduateDean, etc.EXTERNALDevelop links with Medical Directors of other key Trusts.Promote effective relationships with Royal Colleges and Postgraduate Deans.Develop professional and effective links with key CCG staff.TS - June 20133
OTHERContribute fully to the day to day running of the Trust, including in participating in theExecutive on-call rota.To assume the role of the Caldicott Guardian in accordance with the attached roledescription.NOTE – These functions and the support provided will be reviewed with the successfulappointee.TS - June 20134
PERSON SPECIFICATIONQualifications:Employed at substantive consultant level, working in the acute hospital environmentand registered with GMC or qualified doctor employed in medical managementSatisfactory record of continuous professional developmentEvidence of participation in management development opportunities withdemonstrable management experienceKnowledge and Understanding :Sound knowledge of clinical governance and effective systems of medicalmanagement such as job planning, appraisal, revalidation and clinical assessmentAn understanding of medical recruitment and training mattersEvidence of being involved in improving infection controlDemonstrates good strategic awareness of wider NHS issues and the implication ofNHS drivers on Trust servicesKnowledge of information governance as applicable to the NHSKnowledge of the research and development agendaExperience:Extensive involvement in management rolesConsiderable experience in clinical leadership rolesEvidence of leading service change with consultant colleaguesCredible to medical colleaguesPersonal Skills and QualitiesGood organisational skillsGood team leadership skillsAbility to communicate effectively with staff at all levels and with colleagues within andexternal to the TrustEffective motivator with strong influencing skills and personal credibilityAbility to analyse complex issues and identify potential solutionsTS - June 20135
A clear commitment to delivering quality and patient focused servicesFocused on delivering objectives and improvements to patient servicesUnderstands other functional perspectives e.g. Finance, HRCan take a corporate approach to key issuesInclusive leadership and management styleTS - June 20136
CALDICOTT GUARDIAN ROLE DESCRIPTIONACCOUNTABLE TO: CHIEF EXECUTIVE AS ACCOUNTABLE OFFICERRole Summary:<strong>1.</strong> The role of the guardian is to safeguard and govern patient informationwithin the Trust, and to oversee data flows of patient information to otherNHS and non-NHS organisations. Caldicott Guardianship is a keycomponent of broader information governance.2. The Guardian is responsible for ensuring that procedures are in placegoverning access to, and the use of, person-identifiable patient informationand, where appropriate, the transfer of that information to other bodies.3. The Guardian will also take account of the codes of conduct provided byprofessional bodies, and guidance on the protection and use of patientinformation, including the NHS Confidentiality Code of PracticeWorking relationshipsKey tasksThe Caldicott Guardian will:<strong>1.</strong> be supported by the Information Governance Manager2. liaise and work with Service Managers and the Trust Board in the course ofpromoting the Caldicott principles, which will include attendance at meetingsas appropriate.3. be a member of the Trust’s Information Governance Committee and workwith colleagues from areas represented on that committee.4. contribute to the peer review of relevant policies and procedures and theinterpretation of local or national confidentiality issues..<strong>1.</strong> To oversee development and implementation of procedures to ensure thatall routine uses of person-identifiable patient information are identified,agreed as being justified and documented.2. To oversee development and implementation of processes for dealing withad hoc requests for person-identifiable patient information for non-clinicalpurposes.3. To ensure standard procedures and protocols are in place to govern accessto person-identifiable patient information.4. To work with the Research, Research Ethics and Clinical Audit Committeesand personnel to ensure protocols for releasing information for research andaudit are in line with applicable information governance standards.5. To understand and apply the principles of confidentiality and data protectionas set out in the DH publication ‘Confidentiality: NHS Code of Practice’.6. To ensure that there is a programme in place to raise awareness of theCaldicott principles through training and education.7. To resolve any issues relating to breach of patient confidentiality.8. To ensure that information sharing protocols are in line with guidanceprovided by the Department of Health, and to govern the use and sharing ofpatient-identifiable information between organisations both within andoutside the NHS.TS - June 20137
StrategicReporting<strong>1.</strong> To help ensure that the Trust is implementing the various elements ofCaldicott guidelines in its development of strategy and process. Specficallythis will include but not limited to:• Advising on staff registration and authentication process• Ensuring that confidentiality alerts and audit trails are monitored andeffectively managed2. To keep up-to-date with developments within Connecting for Health<strong>1.</strong> In collaboration with Information Governance Manager to draw to theattention of relevant managers any occasion where the appropriateprocedures, guidelines and protocols may not have been followed.2. On an annual basis to participate in the Information Governance Toolkitassessment.3. To report breaches of confidentiality to the Information GovernanceCommittee.TS - June 20138
BOARD OF DIRECTORSMeeting Date and Part: 14 June 2013 Part 1Subject:Core BriefSection:InformationExecutive Director withoverall responsibility:Author of Paper:Tony Spotswood, Chief ExecutiveTracey Hall, Head of CommunicationsKey PurposePatientSafetyHealth &SafetyPerformanceXStrategyXAction required byBoard of Directors:Note for information.Executive Summary: The Core Brief distributed within the Trust in May 2013Strategic Goals &ObjectivesLinks to CQCRegistration(Outcome reference)Links to AssuranceFramework/Key RisksType of Assurance Internal X External
Core BriefMayFrom: Tony Spotswood, Chief Executive2013Health Minister Dr DanPoulter visits RBHDr Poulter (left) speaks to Tony Spotswoodand Dr Mark SopherHealth Minister Dr Dan Poulter visited theRoyal Bournemouth Hospital on 9 May to seethe excellent work carried out by a number ofdepartments and to meet staff and patients.Accompanied by Trust Chief Executive, TonySpotswood, and Chairman, Jane Stichbury, hefirst visited the Derwent Unit where more than athousand elective primary hip andprimary knee replacements arecarried out each year. RBH is one ofthe leading centres for hip and kneereplacements in the UK and Dr Poulterspoke to two patients to hear first-handabout their experience at the hospital.Dr Poulter was then introduced to theteam in the Cardiac Intervention Unit.RBH’s Dorset Heart Centre providesfirst class specialised adult cardiacservices for much of Dorset and partsof Wiltshire and Hampshire.Consultant Cardiologist Dr Mark Sopher talked himthrough a percutaneous coronary intervention (PCI)procedure - non-surgical procedures used to treatthe narrowed coronary arteries of the heart whichare a key area of speciality for the Trust.Dr Poulter was finally taken to see the Trust’snew GP-led unit where patients who no longerrequire acute medical attention are attended to in aspecialist ward led by GPs. He met representativesfrom the new Dorset Clinical Commissioning Groupand heard about the importance of joint working inensuring that patients receive the best quality ofcare in the most appropriate setting.Tony said: “We were delighted to be able toshowcase some of the many excellent servicesoffered by the Trust. Dr Poulter was impressedwith the cardiac and orthopaedic units andacknowledged the excellent work being done todevelop a more integrated model of care for elderlypatients.”Tony Spotswood,Chief ExecutiveChief operating officer Helen Lingham talks to Dr Poulter and staff in theGP led unit
Transporting sharps containersIn order to comply with an alert from the Department of Health’s Estate and Facilities Departmentthe Trust has entered into an arrangement with the supplier Daniels for special sharpscontainers which will not open by accident during transportation.Please click on the link for further details of this product:www.daniels.co.uk/catalog/product.php?id=635The following two policies are being amended by the Sharps Group (thesubcommittee to the H&S Committee) to incorporate these changes:l Driving at Work Policyl Management of Needlestick Injuries and Accidents Involving Exposure toBlood and Body Fluids PolicyThis item will be on the Powergate system for managers to order. Pleaseensure your staff are made aware of this Alert and the new arrangements.Please can staff also be reminded to report all needlestick incidents on AIR forms.Hospital Open Day -Wednesday 12 June 2013The annual Open Day at the Royal Bournemouth Hospital returns on Wednesday 12 June,giving the public a chance to find out about some of the services available at the Trust.The day runs from 10am - 4pm and will see the return of the popular and informativeconsultant talks:10.30am: Hip Arthritis: NewTreatments and Preventionby Dr Robert Middleton, Consultant OrthopaedicSurgeon1<strong>1.</strong>30am: Understanding Dementiaby Dr Sue Hazel, Consultant in Geriatric Medicine12.30pm: Cherishing the SkinYou’re Inby Dr <strong>Ian</strong> Pearson, Consultant Dermatologist<strong>1.</strong>30pm: Medicine and theNew Mediaby Professor David Kerr, Consultant Physicianin the Bournemouth Diabetes andEndocrine Centre2.45pm: Understanding Arthritisby Dr Neil Hopkinson, Rheumatology ConsultantThe hospital atrium will host informationdisplays from different hospital departments,each with their own interactive stand,including quizzes, challenges, and basichealth checks.We hope to see you on the day.HospitalOpen DayWednesday 12 June 2013l Atrium exhibition l Educational presentationsl Department stands l Competitions...and lots more10am - 4pmA number of presentations will be held throughout the day in the Chapel10.30am: Hip Arthritis: New treatments andPrevention Dr Robert Middleton, Consultant Orthopaedic Surgeon1<strong>1.</strong>30am: Understanding DementiaDr Sue Hazel, Consultant in Geriatric Medicine12.30pm: Cherishing the Skin You’re InDr <strong>Ian</strong> Pearson, Consultant Dermatologist<strong>1.</strong>30pm: Medicine and the New Media Professor DavidKerr, Consultant Physician in the Bournemouth Diabetes and Endocrine Centre2.45pm: Understanding ArthritisDr Neil Hopkinson, Rheumatology ConsultantPlaces at these talks are limited so if you would like to attend,please call: 01202 704271 to book your placeor email: communications@rbch.nhs.uk
Sending emailssecurelyA number of (non-NHS) organisations haverecently received monetary penalties of up to£120,000 from the Information Commissioner’sOffice as a result of inappropriately disclosingsensitive personal information via email.To stop this happening at this Trust, be mindfulof the following when using email:l the security of any emails sent from the Trust’ssecure server to an insecure recipient will bethreatened. Consider whether the content ofany email that you send should be encryptedor password protected - any personalinformation emailed outside of the Trust’ssecure network should be encrypted.Guidance on sending emails securely isavailable at: http://rbhintranet/information_governance/pdf/secure_emailing_update_09_201<strong>1.</strong>pdfl be careful when using a group email address.Check who is in the group and make sure youreally want to send your message to everyonel ensure that you are aware of the contentof an email when forwarding it on - checkattachments and previous emails within thechain to make sure that you are not sharingsomething unintentionally or inappropriatelyl when you start to type in the name of therecipient, some email software will suggestsimilar addresses you have used before. Ifyou have previously emailed several peoplewhose name or address starts the sameway - e.g. “Dave” - the auto-completefunction may bring up several “Daves”.Make sure you choose the right addressbefore you click sendl remember that all emails that you send fromyour Trust email account are a public record,and could therefore be disclosable under theFreedom of Information Act 2000The Trust is obliged by the Data ProtectionAct 1998 to take appropriate technical andorganisational measures to protect thepersonal data that it holds, and could face amonetary penalty of up to £500,000 from theInformation Commissioner’s Office should itbe found to be in breach of this.Jigsaw Building planssubmitted to planningcommitteePlans for the new Jigsaw Building at the RoyalBournemouth Hospital have been submitted forconsideration to Bournemouth Council.Following a detailed feedback period, when thebuilding designers sought comments and viewsfrom hospital staff, patients and the public, the plansfor the new 2000m2 building have now beensubmitted.Richard Renaut, Director of Service Development,said: “We’re really pleased to get to this stage of theprocess. Our staff have worked hard to ensure theplans are right and that they reflect the feedback wehave received.“We’re excited about the design and will continue towork with the public to get their views on the interiorof the building and the garden area.“We are now in a 13 week process and wouldencourage people to either send their support forthe plans to us or to the council.”The Jigsaw Building will be located between the EyeUnit and the Derwent Suite for Orthopaedics at RBH.It will bring together oncology, haematology,gynaecology, breast care and early pregnancy intwo new units.Subject to planning approval, initial work couldstart in September/October with a potentialcompletion date of late 2014.Artist’s impression of what the Jigsaw Building will look like
NHS Winter Heroes recognisedFour members of staff and a wholeward team were named NHS WinterHeroes in April. Staff were nominatedby patients and their families or theirwork colleagues, for the differencethey make to the lives of patients intheir care.The scheme focused on the smallthings that make a huge differencesuch as a hand to hold, or ashoulder to lean on, recognisingwhat NHS Heroes do to make sureevery patient receives the best care.A presentation event took place onTuesday 30 April, where the Heroesenjoyed afternoon tea with theirrelatives and friends and were joinedby their patients and colleagues whohad nominated them for the award.Tony Spotswood, Chief Executive,and Jane Stichbury, Chairman,presented certificates at theceremony.Jane said: “As a Trust, we wantto ensure that patients are ournumber one priority and are at theheart of what we do. Patientsatisfaction doesn’t come byaccident; it is something that theTrust achieves through the hardwork, excellence and commitmentthat staff put in on a daily basis. Weare delighted to celebrate the storiesbehind the nominations and thankthose patients and relatives whoshared their experiences with us.“We would also like to extend thanksto the partners, family and friends ofall our staff, because there are oftenlong hours worked and having asupportive and understandingnetwork around them makes a hugedifference.”The RBCH NHS Winter Heroes are:Clare Bent, ConsultantRadiologistClare was nominated by a patient,who said: “I have had three lots oflung cancer in a year. After goingthrough two operations, Clare dida radiofrequency ablation (RFA)procedure on me which was far lessinvasive. She was there for me everystep of the way, she even came todo my procedure on her day off -that’s dedication and care I havenever seen before and I could neverthank her enough.”Marcus Blake, OrthopaedicTechnicianMarcus was commended for hisfriendly and kind manner. “Marcushas always gone that extra mile,showing genuine concern for mywellbeing and giving his all to easemy distress. When a recent surgeryhad complications and I requiredconstant changes of casts, he satand held my hand through manytimes of tears. Marcus hasexcellent listening skills and tooktime to show empathy for myhusband and this touched us bothdeeply. For me, Marcus is my NHShero as he epitomises everythingthat patient care is about.”Ciaran Dunne, ConsultantRheumatologistCiaran was praised for his highquality of care and attention to hispatients, helping them get back ontheir feet and improving theirquality of life: “Dr Dunne saw thingsthat no other saw I am now fit andwell. He is a true hero.”Jenny House, Senior Nurseof OrthopaedicsA colleague nominated Jenny,saying: “Our Trust has experienceda challenging winter withemergency admissions. As SeniorNurse of Orthopaedics, Jenny hasbeen instrumental in creating extramedical capacity on our wards.A human dynamo of energy andenthusiasm, her personalcontribution has been immense.Her outstanding leadership skillsand exemplary approach get themost out of her colleagues.Completely focused on providingthe best she can for patients, Jennypersonifies all that is good about theNHS. She is a delight and aninspiration to work with and I amproud to call her a friend.”Ward 9A relative of a patient said thefollowing of the Ward 9 team:“My father has had some seriousmedical problems after a hipreplacement operation and all thestaff including day staff, night staffand student nurses have been sodedicated and considerate whilelooking after him. They haveattended to his every need, spendinghours with him helping him to regainhis strength as well as explainingeverything in detail so that he wouldunderstand what was happening tohim. Thank you all from both of us.”
Welcome to ourVirtual NurseMany people have wished theycould be in two places at onetime and for the Director ofNursing and Midwifery at RBCH,this is now a reality.A virtual version of PaulaShobbrook has been placedin the main atrium at RBH toeducate patients and visitorsabout good hand hygiene andto encourage them to use handgel before they go on to wards orclinical areas.Virtual Paula is positionedbetween two hand gel pumps,which will be monitored to assesswhether the use of hand gelgoes up, and if infection levels godown.Paula said: “Our low levels ofinfection are among the bestin the region but we cannotbecome complacent. We activelyencourage our patients andvisitors to wash their handsand this is another tool whichwill hopefully capture people’sattention as soon as they walkthrough the front door.”Separate seasonal messageshave been filmed as well as afilm for Christchurch Hospital,so virtual Paula may soonfind herself on the move andeducating even more peopleabout infection control.Facebookand TwitterRBCH is on Facebook andTwitter. To find out more aboutthe latest news and eventsincluding hot topics on that day,search for us as shown below:RBCH_NHSThe Royal BournemouthHospital(Please note, you will not beable to access these sites via theTrust computers so please sendthe links to your mobile phone orpersonal email address.)For more information,please contactcommunications@rbch.nhs.ukStaffExcellenceAwardsNominations for the StaffExcellence Awards are nowclosed and the judgingprocess will soon begin.All nominees will be notifiedas to whether they have beenshortlisted in their categories.The winners will be announcedat a ceremony in September.Thank you to everyone whotook time to make nominations.x
Leadership programmesSupported by NHS Thames Valley and Wessex LeadershipAcademy, the most far-reaching and comprehensive leadershipdevelopment portfolio the NHS has ever developed launchedon 1 May 2013.Aimed at wide range of NHS staff, a range of leadershipprogrammes have been developed to support leaders in creatingan environment where staff feel supported and encouraged tofocus on providing high-quality health care.Full details of the programmes are available from theNHS Leadership Academy website. Please visitwww.leadershipacademy.nhs.uk.A brief overview of the programmes:The Edward Jenner ProgrammeLeadership Foundation. Leaders in the NHS have a key role toplay in improving the health of their communities. LeadershipFoundation is an open access online learning package designed tosupport anyone looking to gain essential leadership skills. It leadsto an NHS Leadership Academy award in Leadership Foundations.The Mary Seacole ProgrammeLeading Care <strong>1.</strong> This one-year programme combines experientialand online learning, and develops key leadership skills. Theprogramme will be open to all those working in health (nominatedby an individual’s place of work) regardless of professional oracademic background. It leads to an NHS Leadership AcademyAward in Leading on the Frontline and a Postgraduate Certificatein Healthcare Leadership.The Elizabeth Garrett Anderson ProgrammeLeading Care 2. The programme leads to an NHS LeadershipAcademy Award in Senior Healthcare Leadership and an MSc inHealthcare Leadership. The programme is 18 months long, andavailable to all those working in the NHS or in NHS-funded care,regardless of professional background.The Nye Bevan ProgrammeLeading Care 3. The Nye Bevan Programme leads to an NHSLeadership Academy Award in Executive Healthcare Leadership.It combines a significant element of personal and behaviouralleadership development with the knowledge and skills neededto operate successfully at the most senior levels in NHSorganisations.Applications for the majority of the programmes close on Friday14 June, with a start date of September. The exception to this isthe Edward Jenner programme, which is an online course and willbe ready to start during June.If you would like to discuss your application, contactKaren Allman, Director of Human Resources.TwilightWalkThere is still time to jointhe Bournemouth HospitalCharity for an evening walkalong the seafront and raisemoney for women’s health atthe Royal BournemouthHospital (RBH) on Friday7 June.We want to make this ourbiggest year yet so why notget your whole team involvedand pick up a registrationform from the FundraisingOffice in the main entranceat RBH or download a copyat www.bournemouthhospitalcharity.co.ukRegistration costs £15 perperson. Participants willreceive a t-shirt and afundraising pack. Fancydress is optional.2013Twilightwalk for womenFriday 7th June 2013 - 8pmBournemouth Seafront1km, 5km and 10km fundraising walkEntry Fee: £15 per person (includes T-shirt)Please raise as much sponsorship as possible.The event is open to women, men and childrenso why not get a group together and get everybodywalking for women and theΩBournemouth Hospital CharityChildren under 12 walk for freeFor more information please contact:Charity Office, Royal Bournemouth Hospital, Castle Lane East, Bournemouth BH7 7DWTel: 01202 704060 Email: charity@rbch.nhs.ukor book online at: www.bournemouthhospitalcharity.co.uk
BOARD OF DIRECTORSMeeting Date and Part: 14 June 2013 – Part 1Subject:Communications Update and Read All About ItSection:Executive Director withoverall responsibility:InformationRichard Renaut, Director of Service DevelopmentAuthor of Paper:Tracey Hall, Head of Communications and FundraisingDetails of previousdiscussion and/ordissemination:Key Purpose:PatientSafetyHealth &SafetyPerformance StrategyXXAction required by Board ofDirectors:Executive Summary:To note the reportThe Communications Report provides a summary of keycommunication activities over the past month, includingmedia KPIs and a summary of the Trust’s mediacoverage (Read All About It).Strategic Goals &Objectives:Links to CQC Registration:(Outcome reference)Section 1, Outcome 1,Section 4, Outcome 13 and 14Links to AssuranceFramework/Key Risks:Type of Assurance:InternalExternal
Board of Directors – Part I14 June 2013<strong>1.</strong> IntroductionCommunications activitiesJune 2013The following paper sets out:• recent communication and fundraising activities• media relations KPIs2. Recent activitiesTrust achieved patient Information StandardPatients coming to the Royal Bournemouth and Christchurch hospitals can beassured the information they are receiving is of the highest quality. The Trusthas been awarded the Information Standard quality mark for the health andcare information it produces for patients.To achieve the Information Standard accreditation, the Trust underwent arigorous two-day assessment of its patient information process by the RoyalSociety for Public Health, one of the organisations accredited to carry out theassessment. Achieving the accreditation means all information produced cannow carry the Information Standard quality mark – a clear indication that it isaccurate and reliable.Launch of The big askRBCH has joined health organisations across Dorset to ask the public to takepart in The big ask - a unique survey which will help shape NHS services in thefuture.The survey asks for views on a whole range of NHS services, from your localGP and out of hours’ services to community, mental health and hospitalservices. This is the first time that NHS organisations across the county haveworked together on an exercise of this scale. It includes the major hospitals inBournemouth, Christchurch, Dorchester and Poole working together with thenewly-formed Dorset Clinical Commissioning Group, which represents thecounty’s 101 GP practices, and Dorset HealthCare, which provides communityhealth services across a wide range of locations.To ensure the exercise is independent it is being carried out by BournemouthUniversity’s Market Research Group. More than 12,000 people will be sent thesurvey by post but anyone can take part online atwww.bournemouth.ac.uk/thebigaskOther:• RBCH now has over 100 Twitter followers and continues to push socialmedia activity• work has been ongoing for the Trust’s Open Day on 12 June. Theaccompanying consultant talks are fully bookedCommunications activity – June 2013 Page 1 of 3For information
Board of Directors – Part I14 June 2013• Health Minister Dr Dan Poulter visited the Trust in May• work is about to start on two new patient information videos – dementiaand clinical site team• an update is soon to go out on the development at Christchurch Hospital• merger communications continues• Twilight Walk for Women on 7 June3. Future activities• Staff Excellence Awards filming• merger communications• patient films• developing social media plan• developing the Bournemouth Hospital Charity fundraising strategy4. RecommendationThe Board is asked to note the report.Communications activity – June 2013 Page 2 of 3For information
Board of Directors – Part I14 June 2013Media relations - Key Performance Measures 2013(this includes fundraising)2013 No. of proactivenews releasedistributedMay2013April2013March201312 (including virtualnurse, Open Day,Twilight Walk,Winter Heroes, bradonation, Eye Unitaward, HealthMinister visit andInformationStandard)10 (includingpatient legacyurology equipment,Health PromotingHospitals, OpenDay)11 (includingthanks for XCHhospital support,Ortho magnet upfor award, NHSChange Day andRBCH second inquality report)% thatreceivedmediacoveragein thatmonth% ofarticlesrelating toreleases/mediaenquiries• * Any paid for adverts are not included i.e. advertorials• ** Negative articles are not includedTotalnumber ofpieces ofcoverage(includesadverts)Totalpositivemediacoverage(all media)Communications activity – June 2013 Page 3 of 3For informationAdvertising value(for printcoverage)*/**TotalnegativemediacoverageNegativecoveragerebuttedi.e.avoidedMedia enquiries92% 94% 67 40 £23,478 24 0 24 (including anumber ofenquiries andfollow upquestions aboutthe recall ofbreast patients)60% 40% 25 22 N/A needupdatedadvertisingrates1 0 12 (includingpatient filming forBBC programme,weekend staffinglevels, cateringwaste, merger,Jigsaw building)82% 74% 66 59 pieces £57,035 2 0 6 (includingmerger, women’shealth unit, XCHhospital andrequests fromBBC RadioSolent for specialhealth feature)
Read All About It...May 2013May saw a significant increase in the number of media enquiriescompared to April, mainly in relation to the breast patients who wereinvited back to the hospital for consultations. The media enquiriescame from both local and national media and included requests forinterviews. This patient recall led to a higher than average amount ofmedia coverage, which was expected.May also saw a very good level of positive coverage across a rangeof media, including new publications. Positive coverage includedthe celebration of our NHS Winter Heroes, promotion of the TwilightWalk for Women and the Trust Open Day, the Trust achieving theInformation Standard, a visit to the Trust by Health Minister Dr DanPoulter and the Eye Unit being nominated for an award.Articles are published with the kind permission of the Daily Echo, Advertiser,the New Milton Advertiser and the Stour and Avon Magazine.Summary of media coverage:May 2013Online 32Print 30Radio 1Television 42013 coveragePositive 40Negative 24OK 3May 2012 Positive 10 Negative 0 OK 1May 2013 l 1
DatePublicationTitleInformationPage numberArticle sizeValue1 April 2013Daily EchoSo fortunate with hospitalPatient feedback to negative coverage inpress saying what good care she received atRBH from ward 16.19Eighth of a page£845DatePublicationTitleInformationPage numberArticle sizeValue1 April 2013Daily EchoOpen day at hospitalThe Royal Bournemouth hospital will host itsopen day on 12 June from 10am to 4pm.27Sixteenth of a page£635May 2013 l 2
DatePublicationTitleInformationPage numberArticle sizeValue2 May 2013Christchurch AdvertiserPatience to pay offImproving quality of care for patients withlong term health conditions.14Quarter of a page£889.60May 2013 l 3
DatePublicationTitle3 May 2013www.seekernews.co.ukNHS Winter Heroes recognisedMay 2013 l 4
DatePublicationTitleInformationPage numberArticle size4 May 2013Daily EchoBreast cancer scare/Breast consultationpatients called backHundreds of women recalled to hospital asjunior doctor faces investigation.1 and 2One and a half pagesMay 2013 l 5
May 2013 l 6
Negative online coverage of breast cancer screening recall4/5/11 News168.co.uk Royal Bournemouth Hospital: hundreds recalled for breast cancer screening4/5/13 www.dailymail.co.uk Junior doctor ‘wrongly gives cancer all-clear to hundreds of women’4/5/13 metro.co.uk Royal Bournemouth Hospital: hundreds recalled for breast cancer screening4/5/13 www.bbc.co.uk Royal Bournemouth Hospital breast cancer screening recall4/5/13 www.bournemouthecho.co.uk Hundreds of patients recalled after breast cancer consultation fears4/5/13 www.huffingtonpost.co.uk Breast cancer scare for hundreds at Royal Bournemouth Hospital, patients recalledafter concerns over junior doctor4/5/13 www.standard.co.uk Women recalled for breast cancer screening after ‘failings’ of junior doctor5/5/13 vettevoice.com Royal Bournemouth Hospital: 250 women recalled for tests5/5/13 www.covertimes.com Royal Bournemouth Hospital 250 women recalled for tests6/5/13 www.bbc.co.uk Royal Bournemouth Hospital breast cancer re-screenings ‘worrying’, says charity6/5/13 www.dailymail.co.uk Junior doctor ‘wrongly gives cancer all-clear to hundreds of women’7/5/13 www.telegraph.co.uk Scare over breast cancer test recall in Bournemouth7/5/13 www.parentherald.com UK hospital recalls 250 women for re-assessment of breast cancer7/5/13 www.onenewspage.co.uk Royal Bournemouth Hospital’ breast screening recall ‘a concern’7/5/13 www.thisisdorset.co.uk Royal Bournemouth Hospital’ breast screening recall ‘a concern’9/5/13 www.bournemouthecho.co.uk Women advised: don’t be put off breast cancer screening in wake of junior doctor incidentNegative radio coverage of breast cancer screening recall4/5/13 106 Jackfm Hundreds of patients recalled at the Royal Bournemouth HospitalNegative television coverage of breast cancer screening recall4/5/13 ITV News Hundreds recalled for further breast cancer screening4/5/13 ITV Meridian Patients recalled to Royal Bournemouth Hospital4/5/13 Sky News Bournemouth Hospital recalls breast patients5/5/13 news.sky.com Bournemouth Hospital recalls breast patientsMay 2013 l 7
DatePublicationTitleInformationPage numberArticle sizeValue4 May 2013New Milton AdvertiserDoctor to give talk on bowel cancerChristchurch Hospital governors organiseda talk about bowel cancer by a consultantgastroenerologist.22Sixteenth of a page£663DatePublicationTitle7 May 2013www.seekernews.co.ukThe ultimate fashion fix in aid of theBournemouth Hospital Charity’s JigsawAppealMay 2013 l 8
DatePublicationTitleInformationPage numberArticle size9 May 2013Daily EchoWomen advised to keep on screeningBosses of breast cancer charities are urging women not to be putoff breast cancer screening.10Two thirds of a pageMay 2013 l 9
DatePublicationTitleInformationPage numberArticle sizeValue9 May 2013Daily EchoDirectors set to meetThe Royal Bournemouth and ChristchurchHospital Trust’s board of directors will meeton 10 May.14Sixteenth of a page£663DatePublicationTitleIformationPage numberArticle sizeValue10 May 2013Stour & Avon magazineHospital consultants to talk at hospital opendayThe annual Open Day at the RoyalBournemouth Hospital returns onWednesday 12 June.27Eighth of a page£90DatePublicationTitleInformationPage numberArticle size10 May 2013Stour & Avon magazineRoyal Bournemouth Hospital breast screening recall ‘a concern’Recall of patients described as ‘extremely worrying’.27Sixteenth of a pageMay 2013 l 10
DatePublicationTitleInformationPage numberArticle size11 May 2013New Milton AdvertiserWomen recalled for cancer checks overdoctor fearsConcerns about how a junior doctor carriedout breast cancer assessments.1Eighth of a pageDatePublicationTitleInformationPage numberArticle sizeValue11 May 2013New Milton AdvertiserTalks and displays at hospital Open DayOpen day talks from 10am to 4pm on 12June.21Sixteenth of a page£49.88May 2013 l 11
DatePublicationTitleInformationPage numberArticle size11 April 2013Daily EchoFrom ward ro boardAdvertorial feature.17Full pageMay 2013 l 12
DatePublicationTitle13 May 2013www.wiltshirebusinessonline.co.ukSalisbury lawyer commends Dorsethospital in breast cancer scareMay 2013 l 13
DatePublicationTitle13 May 2013www.seekernews.co.ukParliamentary Under Secretary of State forHealth visits Royal Bournemouth HospitalMay 2013 l 14
DatePublicationTitleInformationPage numberArticle size9 May 2013Daily EchoHotline set up over cancer recall fearsExtra clinics and telephone hotline set up for women who areworried.10Two thirds of a pageMay 2013 l 15
DatePublicationTitleInformationPage numberArticle sizeValue9 May 2013Daily EchoHospital’s Winter Heroes honoredVarious teams of staff from RBCH have been named as WinterHeroes.15Two thirds of a page£7005May 2013 l 16
DatePublicationTitleInformationPage numberArticle sizeValue14 May 2013Daily EchoHospital staff so wonderfulPatient comments on how good the staffwere at RBCH and how fortunate he was toreceive a high standard of care.18Eighth of a page£845May 2013 l 17
DatePublicationTitle14 May 2013www.bournemouthecho.co.ukMeet the NHs winter heroesDatePublicationTitleInformationPage numberArticle sizeValue15 May 2013Daily EchoMinister on his roundsHealth minister Dr Dan Poulter vistedthe Royal Bournemouth Hospital tomeet staff and patients.24Eighth of a page£845May 2013 l 18
DatePublicationTitle13 May 2013www.seekernews.co.ukFour weeks to go until the RoyalBournemouth Hospital open dayMay 2013 l 19
DatePublicationTitleInformationPage numberArticle sizeValue17 May 2013Stour & Avon magazineLegacy funds new urology equipment forRoyal Bournemouth HospitalGenerous legacy from a former patient hasfunded new equipment to be used within theUrology department.25Quarter of a page£180DatePublicationTitleInformationPage numberArticle sizeValue17 May 2013Stour & Avon magazineNHS Winter Heroes recognisedFour members and ward team from RBCHhas been named as NHS Winter Heroes.25Eighth of a page£90May 2013 l 20
DatePublicationTitleInformationPage numberArticle sizeValue18 May 2013New Milton AdvertiserBeaulieu fashion show for hospital unitcampaignFundraising fashion show for RoyalBournemouth Hospital Jigsaw Appeal tocreate a new women’s health unit.7Sixteenth of a page£49.88May 2013 l 21
DatePublicationTitle20 May 2013www.seekernews.co.ukFormer patients supports theTwilight walkMay 2013 l 22
DatePublicationTitle22 May 2013www.seekernews.co.ukVirtual Nurse arrives at Royal BournemouthHospitalMay 2013 l 23
DatePublicationTitleInformationPage numberArticle sizeValue23 May 2013Christchurch AdvertiserHospital’s HeroesStaff from RBCH have been named as WinterHeroes.5Eighth of a page£444.80DatePublicationTitleInformationPage numberArticle sizeValue23 May 2013Christchurch AdvertiserThanks for all of the supportA family would like to thank The Macmillan Cancerunit nursing staff and the carers of the day centre inChristchurch Hospital.12Sixteenth of a page£222.40May 2013 l 24
DatePublicationTitle24 May 2013www.dailyecho.co.ukThe ultimate fashion fix in aid of theBournemouth Hospital Charity’s JigsawAppealMay 2013 l 25
DatePublicationTitle24 May 2013www.seekernews.co.ukRoyal Bournemouth Hospital eyespecialists nominated for national awardMay 2013 l 26
DatePublicationTitle24 May 2013www.bournemouthecho.co.ukCancer survivor backs Twilight WalkMay 2013 l 27
DatePublicationTitle24 May 2013www.thisisdorset.co.ukFormer Bournemouth Hospital patientsupports the Twilight WalkDatePublicationTitleInformationPage numberArticle sizeValue24 May 2013Stour and AvonHospital open day and talksOpen day talks are booking up fast.30Sixteenth of a page£45May 2013 l 28
DatePublicationTitleInformationPage numberArticle sizeValue24 May 2013Stour & Avon magazineFormer Bournemouth Hospital patientsupports the Twilight WalkA cancer survivor will be walking with theJigsaw Twilight Walk on the 7 June.30Eighth of a page£90DatePublicationTitleInformationPage numberArticle sizeValue24 May 2013Stour & Avon magazineHospital aims to improve care for chronicconditionsRBCH has launched a new initiative toimprove the quality of care for patients withlong-term conditions.30Eighth of a page£90May 2013 l 29
DatePublicationTitleInformationPage numberArticle sizeValue25 May 2013Daily EchoSurvivor walking in Jigsaw building bidA cancer survivor will be walking with the Jigsaw Twilight Walk onthe 7 June.12Two thirds of a page£7005May 2013 l 30
DatePublicationTitleInformationPage numberArticle sizeValue25 May 2013New Milton AdvertiserCancer patient’s call to join in fundraising walkFormer patient at Royal Bournemouth Hospital is encouragingpeople to join her on a sunset beach walk to raise cash for theJigsaw Appeal.21Eighth of a page£7<strong>1.</strong>25DatePublicationTitleInformation27 May 2013www.itv.com/newsTeam in line for major awardCoverage of the Eye Unit being nominatedfor a national award.May 2013 l 31
DatePublicationTitle27 May 2013www.salisburyjournal.co.ukCancer survivor urging people to join walkMay 2013 l 32
DatePublicationTitle28 May 2013www.seekernews.co.ukFashion show raises funds for theBournemouth Hospital Charity’s JigsawAppealMay 2013 l 33
DatePublicationTitleInformationPage numberArticle size29 May 2013Daily EchoTraffic situationPatient letter regarding worsening traffic situation at RBH.18Two thirds of a pageMay 2013 l 34
DatePublicationTitleInformationPage numberArticle sizeValue30 May 2013Bournemouth AdvertiserSurvivor walks in building bidA cancer survivor will be walking for the Twilight walk to helpraise funds for the new Jigsaw building.12Quarter of a page£2525DatePublicationTitle30 May 2013www.seekernews.co.ukTrust’s patient information gets stampof approvalMay 2013 l 35
DatePublicationTitleInformationPage numberArticle sizeValue31 May 2013Stour & Avon magazineEye Specialists nominated for national awardTeam of eye specialists nominated for a nationalaward after outstanding praise from patients.25Eighth of a page£90DatePublicationTitleInformationPage numberArticle sizeValue31 May 2013Stour and AvonDr Dan Poulter visited the Royal BournemouthHospital.25Sixteenth of a page£45May 2013 l 36
BOARD OF DIRECTORSMeeting Date and Part: 14 June 2013 Part 1Subject:Directors Forward ProgrammeSection:Executive Director withoverall responsibility:Author of Paper:InformationTony Spotswood, Chief ExecutiveKaren Flaherty, Trust SecretaryKey PurposePatientSafetyHealth &SafetyPerformanceXStrategyXAction required byBoard of Directors:Note for information.Executive Summary:Strategic Goals &ObjectivesLinks to CQCRegistration(Outcome reference)Links to AssuranceFramework/Key RisksUpdate of the Board of Directors Forward ProgrammeGovernance of the organisationN/AN/AType of Assurance Internal X External
Board of Directors Business Programme 20131What Who Where Before Jan Feb Mar Apr May Jun Jul Sep Oct Nov Dec Where AfterAnnual PlanBoard Objectives TS Chief Executive Part 1 MonitorAnnual Plan - BoD approve Draft for Public Consultation RR TMB/CoG Part 2 Public ConsultationAnnual Plan - Feedback from Consultation to BoD RR CoG Part 1Annual Plan - Final Draft for BoD Approval RR TMB Part 2 PublicationBudgetBudget for next financial year SH Finance Committee N/ACapital Plan for next financial year SH CMG & Finance N/ACode of Conduct for Payment by Results RR Service Development N/ANational Reference Cost Index SH Finance N/ACCG Contract RR Service Development PCTAnnual FeportAnnual Report & Accounts First Draft SH Finance Committee N/AAnnual Report - Audit Committee SP Audit Committee N/AAnnual Report - Finance Committee BF Finance Committee N/AAnnual Report - Healthcare Assurance Committee PS HAC N/AAnnual Report & Accounts - Final draft for approval SH Finance & Audit Cttees MonitorAnnual Report & Accounts - Going Concern Statement SH Finance & Audit Cttees Report & A/CsCharitable FundsAnnual Report & Accounts SH Charity Cmtte Charity CommissionQualityAcute Trust Quality Dashboard HL External CoGAnnual Inpatient Survey Results PS PEC Publication?Annual Outpatient Survey Results PS PECAdult Safeguarding and Child Protection and Safeguarding Report PS HAC Part 2 N/AClinical Governance Quarterly Report PS HAC N/ACQC Quality and Risk Profile PS HAC N/AMortality Quarterly Report MA Medical Director N/APatient Story PS N/A Part 1 N/AQuality Accounts - First Draft PS HAC N/AQuality Accounts - Final Draft for Approval PS HAC PublicationAnnual Progress Report on Francis Report PS HAC/TMB N/ARisk and Assurance Report (including Assurance Framework) PS HAC N/ASepsis Deaths Case Note Review MA TMB N/AInfection ControlBoard Statement of Commitment to prevention of Healthcare Associated Infection PS Infection Control N/AInfection Control - Annual Report PS Infection Control N/AMonitorMonitor Quarter 1 Report HL COO MonitorMonitor Quarter 2 Report HL COO MonitorMonitor Quarter 3 Report HL COO MonitorMonitor Quarter 4 Results HL COO MonitorMonitor Annual Risk Assessment HL External MonitorMonitor's FT Sector Overview - Annual Risk Assessment HL Chief Executive N/AMonitor Annual Self Certification - Board Statements KF Trust Secretary MonitorStaff
What Who Where Before Jan Feb Mar Apr May Jun Jul Sep Oct Nov Dec Where AfterStaff Excellence Awards - Chairman's Prize RR Awards Panel Staff AwardsStaff Survey - Results KA Workforce CoGLocal Clinical Excellence Awards MA Remuneration Rem ComLocal Clinical Excellence Awards - Annual Report MA Remuneration N/A2GovernanceRegister of Interests KF Trust Secretary Trust SecretaryConstitutional Documents - Annual Review KF Constitution Cttee CoGCode of Governance Disclosure Statement KF Trust Secretary MonitorMeeting Dates for Next Year KF Trust Secretary N/AForward Programme KF Trust Secretary N/ANHS Constitution - Bi-annual Self-Assessment KF Trust Secretary PCTIG Toolkit KF HAC Connecting for HealthAnnual Members' Meeting CoG N/A 10th N/AWinter Plan 2012/13 COO N/A PCT/SHAAnnual Members' MeetingBoard Performance JS N/A CoGMinutes of Subordinate groupsAudit Committee Cttee Audit N/ACharity Committee Cttee Charitable Funds N/ACouncil of Governors KF CoG N/AFinance Committee Cttee Finance N/AHealthcare Assurance Committee Cttee HAC N/AInfection Control Committee Cttee Infection Control N/APatient Experience and Communications Committee Cttee PEC N/ARemuneration Committee Cttee Remuneration N/ATrust Management Board Cttee TMB N/AWorkforce Committee Cttee Workforce N/AReview Performance & Terms of Reference subordinate GroupsAudit Committee SP Audit File - KFCharity Committee KT Charitable Funds File - KFFinance Committee SH Finance File - KFHealthcare Assurance Committee PS HAC File - KFInfection Control Committee PS Infection Control File - KFPatient Experience and Communications Committee RR PEC File - KFRemuneration Committee SC Remuneration File - KFTrust Management Board TS TMB File - KFWorkforce Committee KA Workforce File - KFCommunicationsCore Brief RR N/A N/ADr Foster Hospital Guide RR TMB N/ACommunications Update (including Read All About It) RR Service Development N/A