billing the dmercs and others for infusion pumps - ION Solutions
billing the dmercs and others for infusion pumps - ION Solutions
billing the dmercs and others for infusion pumps - ION Solutions
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
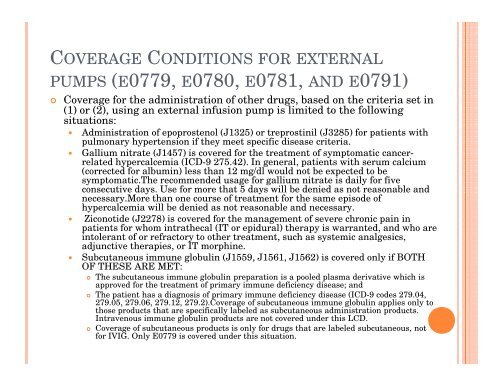
COVERAGE CONDIT<strong>ION</strong>S FOR EXTERNALPUMPS (E0779, E0780, E0781, AND E0791)Coverage <strong>for</strong> <strong>the</strong> administration of o<strong>the</strong>r drugs, based on <strong>the</strong> criteria set in(1) or (2), using an external <strong>infusion</strong> pump is limited to <strong>the</strong> followingsituations:Administration of epoprostenol (J1325) or treprostinil (J3285) <strong>for</strong> patients withpulmonary hypertension if <strong>the</strong>y meet specific disease criteria.Gallium nitrate (J1457) is covered <strong>for</strong> <strong>the</strong> treatment of symptomatic cancerrelatedhypercalcemia (ICD-9 275.42). In general, patients with serum calcium(corrected <strong>for</strong> albumin) less than 12 mg/dl would not be expected to besymptomatic.The recommended usage <strong>for</strong> gallium nitrate is daily <strong>for</strong> fiveconsecutive days. Use <strong>for</strong> more that 5 days will be denied as not reasonable <strong>and</strong>necessary.More than one course of treatment <strong>for</strong> <strong>the</strong> same episode ofhypercalcemia will be denied as not reasonable <strong>and</strong> necessary.Ziconotide (J2278) is covered <strong>for</strong> <strong>the</strong> management of severe chronic pain inpatients <strong>for</strong> whom intra<strong>the</strong>cal (IT or epidural) <strong>the</strong>rapy is warranted, <strong>and</strong> who areintolerant of or refractory to o<strong>the</strong>r treatment, such as systemic analgesics,adjunctive <strong>the</strong>rapies, or IT morphine.Subcutaneous immune globulin (J1559, J1561, J1562) is covered only if BOTHOF THESE ARE MET:The subcutaneous immune globulin preparation is a pooled plasma derivative which isapproved <strong>for</strong> <strong>the</strong> treatment of primary immune deficiency disease; <strong>and</strong> The patient has a diagnosis of primary immune deficiency disease (ICD-9 codes 279.04,279.05, 279.06, 279.12, 279.2).Coverage of subcutaneous immune globulin applies only tothose products that are specifically labeled as subcutaneous administration products.Intravenous immune globulin products are not covered under this LCD.Coverage of subcutaneous products is only <strong>for</strong> drugs that are labeled subcutaneous, not<strong>for</strong> IVIG. Only E0779 is covered under this situation.