Ohio Essential Health Benefits Benchmark Plan Template Page 1 of 7
Ohio Essential Health Benefits Benchmark Plan Template Page 1 of 7
Ohio Essential Health Benefits Benchmark Plan Template Page 1 of 7
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
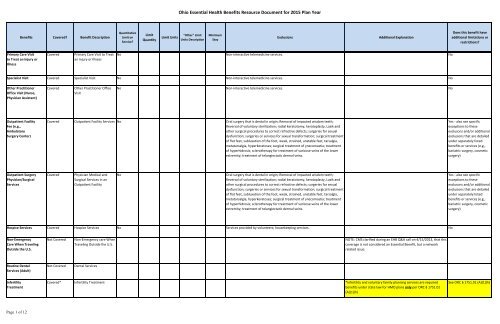
<strong>Ohio</strong> <strong>Essential</strong> <strong>Health</strong> <strong>Benefits</strong> Resource Document for 2015 <strong>Plan</strong> Year<strong>Benefits</strong> Covered? Benefit DescriptionQuantitativeLimit onService?LimitQuantityLimit Units"Other" LimitUnits DescriptionMinimumStayExclusionsAdditional ExplanationDoes this benefit haveadditional limitations orrestrictions?Primary Care Visitto Treat an Injury orIllnessCoveredPrimary Care Visit to Treatan Injury or IllnessNo Non-interactive telemedicine services. NoSpecialist Visit Covered Specialist Visit No Non-interactive telemedicine services. NoOther PractitionerOffice Visit (Nurse,Physician Assistant)CoveredOther Practitioner OfficeVisitNo Non-interactive telemedicine services. NoOutpatient FacilityFee (e.g.,AmbulatorySurgery Center)Covered Outpatient Facility Services No Oral surgery that is dental in origin; Removal <strong>of</strong> impacted wisdom teeth;Reversal <strong>of</strong> voluntary sterilization; radial keratotomy, keratoplasty, Lasik andother surgical procedures to correct refractive defects; surgeries for sexualdysfunction; surgeries or services for sexual transformation; surgical treatment<strong>of</strong> flat feet, subluxation <strong>of</strong> the foot, weak, strained, unstable feet, tarsalgia,metatarsalgia, hyperkeratoses; surgical treatment <strong>of</strong> ynecomastia; treatment<strong>of</strong> hyperhidrosis; sclerotherapy for treatment <strong>of</strong> varicose veins <strong>of</strong> the lowerextremity; treatment <strong>of</strong> telangiectatic dermal veins.Yes - also see specificexceptions to theseexclusons and/or additionalexclusions that are detailedunder separately listedbenefits or services (e.g.,bariatric surgery, cosmeticsurgery)Outpatient SurgeryPhysician/SurgicalServicesCoveredPhysician Medical andSurgical Services in anOutpatient FacilityNoOral surgery that is dental in origin; Removal <strong>of</strong> impacted wisdom teeth;Reversal <strong>of</strong> voluntary sterilization; radial keratotomy, keratoplasty, Lasik andother surgical procedures to correct refractive defects; surgeries for sexualdysfunction; surgeries or services for sexual transformation; surgical treatment<strong>of</strong> flat feet, subluxation <strong>of</strong> the foot, weak, strained, unstable feet, tarsalgia,metatarsalgia, hyperkeratoses; surgical treatment <strong>of</strong> ynecomastia; treatment<strong>of</strong> hyperhidrosis; sclerotherapy for treatment <strong>of</strong> varicose veins <strong>of</strong> the lowerextremity; treatment <strong>of</strong> telangiectatic dermal veins.Yes - also see specificexceptions to theseexclusons and/or additionalexclusions that are detailedunder separately listedbenefits or services (e.g.,bariatric surgery, cosmeticsurgery)Hospice Services Covered Hospice Services No Services provided by volunteers; housekeeping services. NoNon-EmergencyCare When TravelingOutside the U.S.Not CoveredNon-Emergency care WhenTraveling Outside the U.S.NOTE: CMS clarified during an EHB Q&A call on 4/15/2013, that thiscoverage is not considered an <strong>Essential</strong> Benefit, but a networkrelated issue.Routine DentalServices (Adult)Not CoveredDental ServicesInfertilityTreatmentCovered* Infertility Treatment *Infertility and voluntary family planning services are requiredbenefits under state law for HMO plans only per ORC § 1751.01(A)(1)(h)See ORC § 1751.01 (A)(1)(h)<strong>Page</strong> 1 <strong>of</strong> 12
<strong>Ohio</strong> <strong>Essential</strong> <strong>Health</strong> <strong>Benefits</strong> Resource Document for 2015 <strong>Plan</strong> Year<strong>Benefits</strong> Covered? Benefit DescriptionQuantitativeLimit onService?LimitQuantityLimit Units"Other" LimitUnits DescriptionMinimumStayExclusionsAdditional ExplanationDoes this benefit haveadditional limitations orrestrictions?Long-Term/Custodial NursingHome CareNot CoveredLong-Term/CustodialNursing Home CarePrivate-DutyNursingCoveredPrivate duty nursingservicesYes 90 - 110* Visits peryearPrivate duty nursing services in an inpatientsetting.Home nursing services provided through home health care. Limitapplies to Private duty nursing in home setting.*Quantitative Limitrepresents number <strong>of</strong> visitsto meet establishedactuarial equivalent <strong>of</strong>benchmark plan annualdollar limits.Annual and lifetime $ limitswill no longer apply.Routine Eye Exam(Adult)Not Covered Routine Eye Exam Routine eye exam and refraction are not covered, as well as services for visiontraining and orthoptics, eyeglasses and eyewear.Urgent CareCenters orFacilitiesHome <strong>Health</strong> CareServicesCoveredUrgent Care Services in anUrgent Care Center orFacilityCovered Home <strong>Health</strong> Care Services Yes 100 Visits peryearNoFood, housing, homemaker services and home delivered meals; home oroutpatient hemodialysis services; physician charges; helpful environmentalmaterials; Services provided by registered nurses and other health workerswho are not acting as employees or under approved arrangements with acontracting Home <strong>Health</strong> Care Provider; Services provided by a member <strong>of</strong> thepatient's immediate family; Services provided by volunteer ambulanceassociations for which patient is not obligated to pay, visiting teachers,vocational guidance and other counselors, and services related to outside,occupational and social activities; Manipulation therapy services rendered inthe home.Medical treatment provided in the home on a part time orintermittent basis including visits by a licensed health carepr<strong>of</strong>essional, including a nurse, therapist, or home health aide; andphysical, speech, and occupational therapy. When these therapyservices are provided as part <strong>of</strong> home health they are not subject toseparate visit limits for therapy services. 100 visit/year limit notapplicable to home infusion therapy or private duty nursing renderin home setting.NoNoEmergency RoomServicesCovered Emergency Room Services No Care received in and emergency room that is not emergency care. NoEmergencyTransportation/AmbulanceCoveredEmergency Transportation/AmbulanceNoNon covered services for ambulance include but are not limited to, trips to aphysician's <strong>of</strong>fice or clinic, a morgue or a funeral home.Ambulance transportation from home, scene <strong>of</strong> accident or medicalemergency to hospital; between hospitals; between hospital andskilled nursing facility; from hospital or skilled nursing facility topatient's home.No<strong>Page</strong> 2 <strong>of</strong> 12
<strong>Ohio</strong> <strong>Essential</strong> <strong>Health</strong> <strong>Benefits</strong> Resource Document for 2015 <strong>Plan</strong> Year<strong>Benefits</strong> Covered? Benefit DescriptionQuantitativeLimit onService?LimitQuantityLimit Units"Other" LimitUnits DescriptionMinimumStayExclusionsAdditional ExplanationDoes this benefit haveadditional limitations orrestrictions?Inpatient HospitalServices (e.g., HospitalStay)Covered Inpatient Hospital Services No Oral surgery that is dental in origin; Removal <strong>of</strong> impacted wisdom teeth;Reversal <strong>of</strong> voluntary sterilization; radial keratotomy, keratoplasty, Lasik andother surgical procedures to correct refractive defects; surgeries for sexualdysfunction; surgeries or services for sexual transformation; surgical treatment<strong>of</strong> flat feet, subluxation <strong>of</strong> the foot, weak, strained, unstable feet, tarsalgia,metatarsalgia, hyperkeratoses; surgical treatment <strong>of</strong> gynecomastia; treatment<strong>of</strong> hyperhidrosis; sclerotherapy for treatment <strong>of</strong> varicose veins <strong>of</strong> the lowerextremity; treatment <strong>of</strong> telangiectatic dermal veins.Facility billed services while in an inpatient facility. Includes roomand board, nursing services, and ancillary services and supplies.Yes - also see specificexceptions to theseexclusons and/or additionalexclusions that are detailedunder separately listedbenefits or services (e.g.,bariatric surgery, cosmeticsurgery)Inpatient Physicianand SurgicalServicesCoveredInpatient Physician andSurgical ServicesYes 1 Other One (1)Inpatientvisit/day perPhysician orotherPr<strong>of</strong>essionalProviderOral surgery that is dental in origin; Removal <strong>of</strong> impacted wisdom teeth;Reversal <strong>of</strong> voluntary sterilization; radial keratotomy, keratoplasty, Lasik andother surgical procedures to correct refractive defects; surgeries for sexualdysfunction; surgeries or services for sexual transformation; surgical treatment<strong>of</strong> flat feet, subluxation <strong>of</strong> the foot, weak, strained, unstable feet, tarsalgia,metatarsalgia, hyperkeratoses; surgical treatment <strong>of</strong> gynecomastia; treatment<strong>of</strong> hyperhidrosis; sclerotherapy for treatment <strong>of</strong> varicose veins <strong>of</strong> the lowerextremity; treatment <strong>of</strong> telangiectatic dermal veins.Facility billed services while in an inpatient facility. Includes roomand board, nursing services, and ancillary services and supplies.Yes - also see specificexceptions to theseexclusons and/or additionalexclusions that are detailedunder separately listedbenefits or services (e.g.,bariatric surgery, cosmeticsurgery)Bariatric Surgery Not Covered Bariatric Surgery Bariatric surgery, regardless <strong>of</strong> the purpose it is proposed or performed. Thisincludes Roux- en-Y(RNY), Laparoscopic gastric bypass surgery or other gastricbypass surgery (surgical procedures that reduce stomach capacity and divertpartially digested food from the duodenum to the jejunum, the section <strong>of</strong> thesmall intestine extending from the duodenum), or Gastroplasty, (surgicalprocedures that decrease the size <strong>of</strong> the stomach), or gastric bandingprocedures. Complications directly related to bariatric surgery that results inan Inpatient stay or an extended Inpatient stay for the bariatric surgery, asdetermined by Us, are not covered. This exclusion applies when the bariatricsurgery was not a Covered Service under this <strong>Plan</strong> or any previous Anthemplan, and it applies if the surgery was performed while the Member wascovered by a previous carrier/self-funded plan prior to coverage under thisCertificate. Directly related means that the Inpatient stay or extended Inpatientstay occurred as a direct result <strong>of</strong> the bariatric procedure and would not havetaken place in the absence <strong>of</strong> the bariatric procedure.<strong>Page</strong> 3 <strong>of</strong> 12
<strong>Ohio</strong> <strong>Essential</strong> <strong>Health</strong> <strong>Benefits</strong> Resource Document for 2015 <strong>Plan</strong> Year<strong>Benefits</strong> Covered? Benefit DescriptionQuantitativeLimit onService?LimitQuantityLimit Units"Other" LimitUnits DescriptionMinimumStayExclusionsAdditional ExplanationDoes this benefit haveadditional limitations orrestrictions?Cosmetic Surgery Not Covered Cosmetic Surgery For any procedures, services, equipment or supplies provided in connectionwith cosmetic services. Cosmetic services are primarily intended to preserve,change or improve your appearance or are furnished for psychiatric orpsychological reasons. No benefits are available for surgery or treatments tochange the texture or appearance <strong>of</strong> your skin or to change the size, shape orappearance <strong>of</strong> facial or body features (such as your nose, eyes, ears, cheeks,chin, chest or breasts). Complications directly related to cosmetic servicestreatment or surgeries, as determined by Us, are not covered. This exclusionapplies even if the original cosmetic services treatment or surgery wasperformed while the Member was covered by another carrier/self- funded planprior to coverage under this Certificate. Directly related means that thetreatment or surgery occurred as a directresult <strong>of</strong> the cosmetic services treatment or surgery and would not have takenplace in the absence <strong>of</strong> the cosmetic services treatment or surgery.Skilled NursingFacilityCovered Skilled Nursing Facility Yes 90 Days peryearCustodial or residential care in a skilled nursing facility or any other facility isnot covered except as rendered as part <strong>of</strong> Hospice care.Items and services provided as an inpatient in a skilled nursing bed<strong>of</strong> skilled nursing facility or hospital, including room and board insemi-private accommodations; rehabilitative services; and drugs,biologicals, and supplies furnished for use in the skilled nursingfacility and other medically necessary services and supplies.NoPrenatal andPostnatal CareCoveredPrenatal and PostnatalCareNoServices related to surrogacy if member is notthe surrogate.Maternity care, maternity-related checkups, and delivery <strong>of</strong> thebaby in the hospital are covered.NoDelivery and AllInpatient Services forMaternity CareCoveredDelivery and All InpatientFacility and Pr<strong>of</strong>essionalServices for Maternity CareNo 48 Services related to surrogacy if member is notthe surrogate.Maternity care, maternity-related checkups, and delivery <strong>of</strong> thebaby in the hospital are covered. 48 hour minimum length <strong>of</strong> stayfor vaginal delivery; 96 hour minimum length <strong>of</strong> stay for cesareandelivery.No<strong>Page</strong> 4 <strong>of</strong> 12
<strong>Ohio</strong> <strong>Essential</strong> <strong>Health</strong> <strong>Benefits</strong> Resource Document for 2015 <strong>Plan</strong> Year<strong>Benefits</strong> Covered? Benefit DescriptionQuantitativeLimit onService?LimitQuantityLimit Units"Other" LimitUnits DescriptionMinimumStayExclusionsAdditional ExplanationDoes this benefit haveadditional limitations orrestrictions?Mental/Behavioral<strong>Health</strong> OutpatientServicesCoveredMental/Behavioral <strong>Health</strong>Outpatient ServicesYes Other Mental <strong>Health</strong>ParityCustodial or Domiciliary Care. Supervised living or halfway houses. Residential Coverage and limits must comply with state mandate and the paritytreatment centers. Room and board charges unless the treatment provided standards set forth in the federal Mental <strong>Health</strong> Parity andmeets Medical Necessity criteria for Inpatient admission patient's condition. Addiction Equity Act <strong>of</strong> 2008.Services or care provided or billed by a school, halfway house, Custodial Carecenter for the developmentally disabled or outward bound programs, even ifpsychotherapy is included. Services related to non-compliance <strong>of</strong> care if theMember ends treatment for Substance Abuse against the medical advice <strong>of</strong> theProvider. Residential Treatment (individualized and intensive treatment in aresidential setting, including observation and assessment by a psychiatristweekly or more frequently, an individualized program <strong>of</strong> rehabilitation,therapy, education, and recreational or social activities); care provided orbilled by residential treatment centers or facilities, unless those centers orfacilities are required to be covered under state law; residential programs fordrug and alcohol; marital and sexual counseling/ therapy; and wildernesscamps.Mental <strong>Health</strong> Parity andAddiction Equity Act <strong>of</strong>2008Mental/Behavioral<strong>Health</strong> InpatientServicesCoveredMental/Behavioral <strong>Health</strong>Inpatient ServicesYes Other Mental <strong>Health</strong>ParityCustodial or Domiciliary Care. Supervised living or halfway houses. Residential Coverage and limits must comply with state mandate and the paritytreatment centers. Room and board charges unless the treatment provided standards set forth in the federal Mental <strong>Health</strong> Parity andmeets Medical Necessity criteria for Inpatient admission patient's condition. Addiction Equity Act <strong>of</strong> 2008.Services or care provided or billed by a school, halfway house, Custodial Carecenter for the developmentally disabled or outward bound programs, even ifpsychotherapy is included. Services related to non-compliance <strong>of</strong> care if theMember ends treatment for Substance Abuse against the medical advice <strong>of</strong> theProvider. Residential Treatment (individualized and intensive treatment in aresidential setting, including observation and assessment by a psychiatristweekly or more frequently, an individualized program <strong>of</strong> rehabilitation,therapy, education, and recreational or social activities); care provided orbilled by residential treatment centers or facilities, unless those centers orfacilities are required to be covered under state law; residential programs fordrug and alcohol; marital and sexual counseling/ therapy; and wildernesscamps.Mental <strong>Health</strong> Parity andAddiction Equity Act <strong>of</strong>2008<strong>Page</strong> 5 <strong>of</strong> 12
<strong>Ohio</strong> <strong>Essential</strong> <strong>Health</strong> <strong>Benefits</strong> Resource Document for 2015 <strong>Plan</strong> Year<strong>Benefits</strong> Covered? Benefit DescriptionQuantitativeLimit onService?LimitQuantityLimit Units"Other" LimitUnits DescriptionMinimumStayExclusionsAdditional ExplanationDoes this benefit haveadditional limitations orrestrictions?Substance AbuseDisorder OutpatientServicesCoveredSubstance Abuse DisorderOutpatient ServicesYes Other Mental <strong>Health</strong>ParityCustodial or Domiciliary Care. Supervised living or halfway houses. Residential Coverage and limits must comply with state mandate and the paritytreatment centers. Room and board charges unless the treatment provided standards set forth in the federal Mental <strong>Health</strong> Parity andmeets Medical Necessity criteria for Inpatient admission patient's condition. Addiction Equity Act <strong>of</strong> 2008.Services or care provided or billed by a school, halfway house, Custodial Carecenter for the developmentally disabled or outward bound programs, even ifpsychotherapy is included. Services related to non-compliance <strong>of</strong> care if theMember ends treatment for Substance Abuse against the medical advice <strong>of</strong> theProvider. Residential Treatment (individualized and intensive treatment in aresidential setting, including observation and assessment by a psychiatristweekly or more frequently, an individualized program <strong>of</strong> rehabilitation,therapy, education, and recreational or social activities); care provided orbilled by residential treatment centers or facilities, unless those centers orfacilities are required to be covered under state law; residential programs fordrug and alcohol; marital and sexual counseling/ therapy; and wildernesscamps.Mental <strong>Health</strong> Parity andAddiction Equity Act <strong>of</strong>2008Substance AbuseDisorder InpatientServicesCoveredSubstance Abuse DisorderInpatient ServicesYes Other Mental <strong>Health</strong>ParityCustodial or Domiciliary Care. Supervised living or halfway houses. Residential Coverage and limits must comply with state mandate and the paritytreatment centers. Room and board charges unless the treatment provided standards set forth in the federal Mental <strong>Health</strong> Parity andmeets Medical Necessity criteria for Inpatient admission patient's condition. Addiction Equity Act <strong>of</strong> 2008.Services or care provided or billed by a school, halfway house, Custodial Carecenter for the developmentally disabled or outward bound programs, even ifpsychotherapy is included. Services related to non-compliance <strong>of</strong> care if theMember ends treatment for Substance Abuse against the medical advice <strong>of</strong> theProvider. Residential Treatment (individualized and intensive treatment in aresidential setting, including observation and assessment by a psychiatristweekly or more frequently, an individualized program <strong>of</strong> rehabilitation,therapy, education, and recreational or social activities); care provided orbilled by residential treatment centers or facilities, unless those centers orfacilities are required to be covered under state law; residential programs fordrug and alcohol; marital and sexual counseling/ therapy; and wildernesscamps.Mental <strong>Health</strong> Parity andAddiction Equity Act <strong>of</strong>2008Generic Drugs Covered Generic Prescription Drugs No Over the counter drugs and drugs with over the counter equivalents; Drugs forweight loss; Stop smoking aids; Nutritional and/or dietary supplements; drugsfor the treatment <strong>of</strong> sexual or erectile dysfunction or inadequacies; fertilitydrugs; human growth hormone for children born small for gestational age;treatment <strong>of</strong> onchomycosis.Must comply with Regulations at 45 C.F.R. 156.122, providingcoverage for at least the greater <strong>of</strong> (1) one drug in every USPcategory and class, or (2) the same number <strong>of</strong> prescription drugs ineach USP category and class as the state's EHB-benchmark plan.Prescription Drug EHB-<strong>Benchmark</strong> <strong>Plan</strong> <strong>Benefits</strong>by Category and ClassPreferred BrandDrugsCoveredPreferred BrandPrescriptionDrugsNoOver the counter drugs and drugs with over the counter equivalents; Drugs forweight loss; Stop smoking aids; Nutritional and/or dietary supplements; drugsfor the treatment <strong>of</strong> sexual or erectile dysfunction or inadequacies; fertilitydrugs; human growth hormone for children born small for gestational age;treatment <strong>of</strong> onchomycosis.Must comply with Regulations at 45 C.F.R. 156.122, providingcoverage for at least the greater <strong>of</strong> (1) one drug in every USPcategory and class, or (2) the same number <strong>of</strong> prescription drugs ineach USP category and class as the state's EHB-benchmark plan.Prescription Drug EHB-<strong>Benchmark</strong> <strong>Plan</strong> <strong>Benefits</strong>by Category and Class<strong>Page</strong> 6 <strong>of</strong> 12
<strong>Ohio</strong> <strong>Essential</strong> <strong>Health</strong> <strong>Benefits</strong> Resource Document for 2015 <strong>Plan</strong> Year<strong>Benefits</strong> Covered? Benefit DescriptionQuantitativeLimit onService?LimitQuantityLimit Units"Other" LimitUnits DescriptionMinimumStayExclusionsAdditional ExplanationDoes this benefit haveadditional limitations orrestrictions?Non-PreferredBrand DrugsCoveredNon-Preferred BrandPrescription DrugsNoOver the counter drugs and drugs with over the counter equivalents; Drugs forweight loss; Stop smoking aids; Nutritional and/or dietary supplements; drugsfor the treatment <strong>of</strong> sexual or erectile dysfunction or inadequacies; fertilitydrugs; human growth hormone for children born small for gestational age;treatment <strong>of</strong> onchomycosis.Must comply with Regulations at 45 C.F.R. 156.122, providingcoverage for at least the greater <strong>of</strong> (1) one drug in every USPcategory and class, or (2) the same number <strong>of</strong> prescription drugs ineach USP category and class as the state's EHB-benchmark plan.Prescription Drug EHB-<strong>Benchmark</strong> <strong>Plan</strong> <strong>Benefits</strong>by Category and ClassSpecialty Drugs Covered Specialty PrescriptionDrugsNoOver the counter drugs and drugs with over the counter equivalents; Drugs forweight loss; Stop smoking aids; Nutritional and/or dietary supplements; drugsfor the treatment <strong>of</strong> sexual or erectile dysfunction or inadequacies; fertilitydrugs; human growth hormone for children born small for gestational age;treatment <strong>of</strong> onchomycosis.Must comply with Regulations at 45 C.F.R. 156.122, providingcoverage for at least the greater <strong>of</strong> (1) one drug in every USPcategory and class, or (2) the same number <strong>of</strong> prescription drugs ineach USP category and class as the state's EHB-benchmark plan.Prescription Drug EHB-<strong>Benchmark</strong> <strong>Plan</strong> <strong>Benefits</strong>by Category and ClassOutpatientRehabilitationServicesCoveredOutpatient RehabilitationServicesYes 116 Other Combined totalvisits/year forall therapies.*Physical Therapy - Non Covered Services include: maintenance therapy to *Includes physical therapy, occupational therapy, speech therapy,delay or minimize muscular deterioration in patients suffering from a chronic pulmonary therapy and cardiac rehabilitation. Separate 20 visitdisease or illness; repetitive exercise to improve movement, maintain strength limits for PT, OT, ST, Pulmonary Rehab; 36 visit limit for Cardiacand increase endurance (including assistance with walking for weak or Rehab.unstable patients); range <strong>of</strong> motion and passive exercises that are not relatedto restoration <strong>of</strong> a specific loss <strong>of</strong> function, but are for maintaining a range <strong>of</strong>motion in paralyzed extremities; general exercise programs; diathermy,ultrasound and heat treatments for pulmonary conditions; diapulse; workhardening.Occupational Therapy - Does not include coverage for diversional,recreational, vocational therapies (e.g., hobbies, arts and crafts). Non CoveredServices include: supplies (looms, ceramic tiles, leather, utensils); therapy toimprove or restore functions that could be expected to improve as the patientresumes normal activities again; general exercises to promote overall fitnessand flexibility; therapy to improve motivation; suction therapy for newborns(feeding machines); s<strong>of</strong>t tissue mobilization (visceral manipulation or viscerals<strong>of</strong>t tissue manipulation), augmented s<strong>of</strong>t tissue mobilization, my<strong>of</strong>ascial;adaptions to the home such as rampways, door widening, automobileadaptors, kitchen adaptation and other types <strong>of</strong> similar equipment.Cardiac Rehab - Home programs, on-going conditioning and maintenance arenot covered.Pulmonary Rehab - Pulmonary rehabilitation in the acute Inpatientrehabilitation setting is not a Covered Service.General Exclusions - Non-Covered Services for physical medicine andrehabilitation include, but are not limited to: admission to a Hospital mainly forphysical therapy; long term rehabilitation in an Inpatient setting.<strong>Page</strong> 7 <strong>of</strong> 12
<strong>Ohio</strong> <strong>Essential</strong> <strong>Health</strong> <strong>Benefits</strong> Resource Document for 2015 <strong>Plan</strong> Year<strong>Benefits</strong> Covered? Benefit DescriptionQuantitativeLimit onService?LimitQuantityLimit Units"Other" LimitUnits DescriptionMinimumStayExclusionsAdditional ExplanationDoes this benefit haveadditional limitations orrestrictions?HabilitationServicesCovered -Requiredsupplement to<strong>Benchmark</strong> <strong>Plan</strong>benefitsHabilitation ServicesIssuers must include the benefits outlined in the governor’s letterdated December 26, 2012. In addition, issuers must ensure thatproducts are otherwise compliant with all other EHB requirements.<strong>Ohio</strong> Governor's letterdated 12/26/2012ACA Final Rule -Standards Related to<strong>Essential</strong> <strong>Health</strong> <strong>Benefits</strong>,Actuarial Value, andAccreditationChiropractic Care Covered Osteopathic/ChiropracticManipulation TherapyYes 12 Visits peryearManipulation therapy services rendered in thehome as part <strong>of</strong> Home Care Services are not covered.Benefit limit applies forOsteopathic/ChiropracticManipulation Therapy.NoDurable MedicalEquipmentCoveredMedical Equipment andSuppliesNoNon covered services include: Items for personal hygiene, environmentalcontrol or convenience; Exercise equipment;Repairs and replacement - Repair and replacement due to misuse, maliciousbreakage or gross neglect. Replacement <strong>of</strong> lost or stolen items.Medical and Surgical Supplies - Adhesive tape, band aids, cotton tippedapplicators; Arch supports; Doughnut cushions; Hot packs, ice bags; vitamins;medijectors;Durable Medical Equipment - Air conditioners; Ice bags/ coldpack pump;Raised toilet seats; Rental <strong>of</strong> equipment if the Member is in a Facility that isexpected to provide such equipment; Translift chairs; Treadmill exerciser; Tubchair used in shower.Prosthetics - Dentures, replacing teeth or structures directly supporting teeth;Dental appliances; Such non-rigid appliances as elastic stockings, garter belts,arch supports and corsets; Artificial heart implants; Wigs (except followingcancer treatment); Penile prosthesis in men suffering impotency resulting fromdisease or injury;Orthotics - Orthopedic shoes (except therapeutic shoes for diabetics); Footsupport devices, such as arch supports and corrective shoes, unless they are anintegral part <strong>of</strong> a leg brace; Standard elastic stockings, garter belts, and othersupplies not specially made and fitted (except as specified under MedicalSupplies); Garter belts or similar devices.Covered services include: Durable medicalequipment, medical devices and supplies, prosthetics andappliances, including cochlear implants.Limit <strong>of</strong> four (4) surgical bras following mastectomy per benefitperiod; LVAD covered only as bridge to heart transplant.NoHearing Aids Not Covered Hearing Aids See Durable MedicalEquipment benefits re:coverage for cochlearimplants.Diagnostic Test(X-Ray and LabWork)Covered Diagnostic Tests No No<strong>Page</strong> 8 <strong>of</strong> 12
<strong>Ohio</strong> <strong>Essential</strong> <strong>Health</strong> <strong>Benefits</strong> Resource Document for 2015 <strong>Plan</strong> Year<strong>Benefits</strong> Covered? Benefit DescriptionQuantitativeLimit onService?LimitQuantityLimit Units"Other" LimitUnits DescriptionMinimumStayExclusionsAdditional ExplanationDoes this benefit haveadditional limitations orrestrictions?Imaging(CT/PET Scans, MRIs)CoveredAdvanced DiagnosticImaging ServicesNoNoPreventive Care/ CoveredScreening/ ImmunizationPreventive Care/Screeningsand ImmunizationsNoCoverage must include all preventive services described in section2713 <strong>of</strong> the PHS Act, as added by section 1001 <strong>of</strong> the ACA.NoRoutine Foot Care Not Covered Routine Foot Care Routine foot care (including the cutting or removal <strong>of</strong> corns and calluses); Nailtrimming, cutting or debriding; Hygienic and preventive maintenance foot care,including: cleaning and soaking the feet; applying skin creams in order tomaintain skin tone; other services that are performed when there is not alocalized illness, injury or symptom involving the foot; cosmetic foot care.Acupuncture Not Covered Acupuncture Services or supplies related to alternative orcomplementary medicine. Examples <strong>of</strong> services in this category include:acupuncture, holistic medicine, homeopathy, hypnosis, aroma therapy,massage and massagetherapy, reiki therapy, herbal, vitamin ordietary products or therapies, naturopathy, thermograph, orthomoleculartherapy, contact reflex analysis, bioenergial synchronization technique (BEST),iridology- study <strong>of</strong> the iris, auditory integration therapy (AIT), colonic irrigation,magnetic innervation therapy, electromagnetic therapy, and neur<strong>of</strong>eedback.Weight LossProgramsNot Covered Weight Loss Programs Weight loss programs, whether or not theyare pursued under medical or physiciansupervision.Routine Eye Examfor ChildrenCovered Routine eye exam Yes 1 Visits peryearRequired coverage will include benefits specified in the FEDVIP FEPBlue Vision - High Option plan.FEP BlueVision - HighOption2012 <strong>Plan</strong> BenefitBrochureEye Glasses forChildrenCovered Eyeglasses for children Yes 1 Other 1 pair <strong>of</strong>glasses(lenses andframes peryear)Required coverage will include benefits specified in the FEDVIP FEPBlue Vision - High Option plan.FEP BlueVision - HighOption2012 <strong>Plan</strong> BenefitBrochureDental Check-Upfor ChildrenCovered -Requiredsupplement to<strong>Benchmark</strong> <strong>Plan</strong>benefitsDental Exams Yes 1 Other 1 every 6monthsRequired coverage will include benefits specified in the FEDVIPMetLife Federal Dental - High Option <strong>Plan</strong>., which includes basic,intermediate and major dental services and supplies as well asmedically-necessary orthodontia.MetLife Federal Dental <strong>Plan</strong> -High Option 2012 <strong>Plan</strong>Benefit Brochure<strong>Page</strong> 9 <strong>of</strong> 12
<strong>Ohio</strong> <strong>Essential</strong> <strong>Health</strong> <strong>Benefits</strong> Resource Document for 2015 <strong>Plan</strong> Year<strong>Benefits</strong> Covered? Benefit DescriptionQuantitativeLimit onService?LimitQuantityLimit Units"Other" LimitUnits DescriptionMinimumStayExclusionsAdditional ExplanationDoes this benefit haveadditional limitations orrestrictions?Other <strong>Ohio</strong> EHB <strong>Benchmark</strong> <strong>Plan</strong> <strong>Benefits</strong>Other Covered Radiation Therapy No NoOther Covered Chemotherapy No NoOther Covered Infusion Therapy No NoOther Covered Renal Dialysis/HemodialysisNoNoOther Covered Allergy Treatment No NoOther Covered Injectable drugs andother drugs administeredin a provider's <strong>of</strong>fice orother outpatient settingNoNoOther Not Covered Bi<strong>of</strong>eedbackOther Covered Vision Correction AfterSurgery or AccidentNoPrescription, fitting, or purchase <strong>of</strong> eyeglasses or contact lenses except asotherwise specifically stated as a Covered Service.Prescription glasses or contact lenses when required as a result <strong>of</strong>surgery or for the treatment <strong>of</strong> accidental injury.NoOther Covered Medical supplies,equipment, and educationfor diabetes care for alldiabeticsNoMedical supplies, equipment, and education for diabetes care for alldiabetics. Orthopedic/therapeutic shoes.NoOther Covered Accidental Dental Yes 3000* Other Dollars perOccurrence*Damage to teeth due to chewing or biting is not deemed an accidental injuryand is not covered.Dental services resulting from an accidental injury when treatment *Quantitative Limitis performed within 12 months after the injury. The benefit limit will represents establishednot apply to Outpatient facility charges, anesthesia billed by a actuarial equivalent <strong>of</strong>Provider other than the Physician performing the service, or to benchmark plan annualservices that we are required by law to cover. Coverage includes dollar limits. Annual andoral examinations, x-rays, tests and laboratory examinations, lifetime $ limits will norestorations, prosthetic services, oral surgery, mandibular/maxillary longer apply.reconstruction, anesthesia. Other covered dental services includefacility charges for Outpatient services for the removal <strong>of</strong> teeth orfor other dental processes if the patient’s medical condition or thedental procedure requires a Hospital setting to ensure the safety <strong>of</strong>the patient.<strong>Page</strong> 10 <strong>of</strong> 12
<strong>Ohio</strong> <strong>Essential</strong> <strong>Health</strong> <strong>Benefits</strong> Resource Document for 2015 <strong>Plan</strong> Year<strong>Benefits</strong> Covered? Benefit DescriptionQuantitativeLimit onService?LimitQuantityLimit Units"Other" LimitUnits DescriptionMinimumStayExclusionsAdditional ExplanationDoes this benefit haveadditional limitations orrestrictions?Other Covered Human Organ andTissue TransplantServicesNoMedically necessary human organ and tissue transplant services.When a human organ or tissue transplant is provided from a livingdonor to a covered person, both the recipient and the donor mayreceive the benefits <strong>of</strong> the health plan. Additional covered servicesinclude unrelated donor searches and transportation and lodging.YesOther Covered Human Organ andTissue TransplantServices - Transportationand LodgingYes 10000 dollars per transplantbenefit periodNon covered transportation and lodging includes child care; mileage within the The <strong>Plan</strong> will provide assistance with reasonable and necessary Yestransplant city; rental cars, buses, taxis or shuttle service, except as specifically travel expenses when patient is required to travel more than 75approved; frequent flyer miles; coupons, vouchers or travel tickets;miles from residence to reach the facility where the Coveredprepayments or deposits; services for a condition that is not directly related to, Transplant Procedure will be performed. Assistance with travelor a direct result <strong>of</strong>, the transplant; telephone calls; laundry; postage; expenses includes transportation to and from the facility andentertainment; interim visits to a medical facility while waiting for the actual lodging for the patient and one companion. If the Member receivingtransplant procedure; travel expenses for donor companion/ caregiver; return treatment is a minor, then reasonable and necessary expenses forvisits for the donor for a treatment <strong>of</strong> a condition found during evaluation. transportation and lodging may be allowed for two companions.Other Covered Human Organ and Yes 30000 dollars per transplantTissue Transplant Services -benefit periodUnrelated donor searchYesInpatientHospital Services (e.g.,Hospital Stay)CoveredRehab FacilitiesIncluding Room & BoardCharges, Physician Fees,Imaging, Testing, andSuppliesYes 60 Days peryearAdmission to a Hospital mainly for physical therapy; long term rehabilitation inan Inpatient setting.Includes coverage for Day Rehabilitation Program services subjectto combined 60 day limit with inpatient services.YesInpatientPhysician andSurgicalServicesCoveredRehab FacilitiesIncluding Room &Board Charges, PhysicianFees, Imaging, Testing, andSuppliesYes 60 Days peryearAdmission to a Hospital mainly for physical therapy; long term rehabilitation inan Inpatient setting.YesOther Covered -Requiredsupplement to<strong>Benchmark</strong> <strong>Plan</strong>benefitsBasic Dental Care –ChildNoRequired coverage will include benefits specified in the FEDVIPMetLife Federal Dental - High Option <strong>Plan</strong>., which includes basic,intermediate and major dental services and supplies as well asmedically-necessary orthodontia.MetLife Federal Dental <strong>Plan</strong> -High Option 2012 <strong>Plan</strong>Benefit BrochureOther Covered -Requiredsupplement to<strong>Benchmark</strong> <strong>Plan</strong>benefitsMajor Dental Care –ChildNoRequired coverage will include benefits specified in the FEDVIPMetLife Federal Dental - High Option <strong>Plan</strong>., which includes basic,intermediate and major dental services and supplies as well asmedically-necessary orthodontia.MetLife Federal Dental <strong>Plan</strong> -High Option 2012 <strong>Plan</strong>Benefit Brochure<strong>Page</strong> 11 <strong>of</strong> 12
<strong>Ohio</strong> <strong>Essential</strong> <strong>Health</strong> <strong>Benefits</strong> Resource Document for 2015 <strong>Plan</strong> Year<strong>Benefits</strong> Covered? Benefit DescriptionQuantitativeLimit onService?LimitQuantityLimit Units"Other" LimitUnits DescriptionMinimumStayExclusionsAdditional ExplanationDoes this benefit haveadditional limitations orrestrictions?Other Covered -Requiredsupplement to<strong>Benchmark</strong> <strong>Plan</strong>benefitsOrthodontia - Child No Required coverage will include benefits specified in the FEDVIPMetLife Federal Dental - High Option <strong>Plan</strong>., which includes basic,intermediate and major dental services and supplies as well asmedically-necessary orthodontia.MetLife Federal Dental <strong>Plan</strong> -High Option 2012 <strong>Plan</strong>Benefit BrochureOther Covered Temporomandibularor CraniomandibularJoint/Jaw TreatmentNoNoOther Covered Sterilization No NoOther Covered ReconstructiveServicesNoReconstructive services (unless required by law) except: Necessary care andtreatment <strong>of</strong> medically diagnosed congenital defects and birth abnormalities <strong>of</strong>a newborn child; Breast reconstruction resulting from a mastectomy;Hemangiomas, and port wine stains <strong>of</strong> the head and neck areas for childrenages 18 years <strong>of</strong> age or younger; Limb deformities such as club hand, club foot,syndactyly (webbed digits), polydactyly (supernumerary digits), macrodactylia;Otoplasty when performed to improve hearing by directing sound in the earcanal, when ear or ears are absent or deformed from trauma, surgery, disease,or congenital defect; Tongue release for diagnosis <strong>of</strong> tongue-tied; Congenialdisorders that cause skull deformity such as Crouzon's disease; Cleft lip; Cleftpalate.NoOther Covered Off Label PrescriptionDrugsNo Coverage must comply with ORC §§ 3923.60, 3923.61, and 1751.66,as well as Regulations at 45 C.F.R. 156.122.NoOther Covered Specified Non-RoutineDental ServicesNo1) Limited to facility charges for Outpatient Services for the removal<strong>of</strong> teeth or for other dental processes only if the patient’s medicalcondition or the dental procedure requires a Hospital setting toensure the safety <strong>of</strong> the patient; 2) Dental xrays, supplies, &appliances and all associated expenses, including hospitalizationand anesthesia are limited to services/treatments for: transplantpreparation; initiation <strong>of</strong> immunosuppresives; or direct treatment<strong>of</strong> acute traumatic injury, cancer, or cleft palate.NoOther Covered Nutritional Counseling No No<strong>Page</strong> 12 <strong>of</strong> 12