Provider policies & procedures - Contact the Husky Health Program ...
Provider policies & procedures - Contact the Husky Health Program ...
Provider policies & procedures - Contact the Husky Health Program ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
PROVIDER POLICIES &PROCEDURESFOOT ORTHOTICSThe purpose of this Clinical Guideline is to provide guidance to providers enrolled in <strong>the</strong> ConnecticutMedical Assistance <strong>Program</strong> (CMAP <strong>Provider</strong>s) on <strong>the</strong> requirements for prior authorization of footorthotics. This includes both <strong>the</strong> applicable medical necessity criteria for approval of coverage through<strong>the</strong> prior authorization process for HUSKY members and <strong>the</strong> applicable <strong>procedures</strong> and guidelines of <strong>the</strong>prior authorization process.Foot orthotics are removable shoe inserts that do not extend beyond <strong>the</strong> ankle and may include heelwedges and arch supports, which are available commercially or may be custom-made. The goal oftreating conditions with foot orthotics is to decrease pain and increase function by controlling foot motion,reducing shock absorption, and minimizing stress forces. Foot orthotics are placed in a shoe (shoeinserts) to assist in restoring or maintaining normal alignment of <strong>the</strong> foot, relieve stress from strained orinjured soft tissues, bony prominences, deformed bones and joints, and inflamed or chronic bursae. Theymay also correct some foot deformities and provide shock absorption to <strong>the</strong> foot. Foot orthoses may beused to treat conditions including those involving impaired peripheral circulation and sensation, when<strong>the</strong>y are attached to a pros<strong>the</strong>tic shoe or orthosis, for a neurologic or neuromuscular condition and forcongenital or acquired foot conditions.Foot orthotics may be accommodative or functional. Accommodative foot orthoses are custom or noncustominlays fabricated for <strong>the</strong> purpose of providing relief from callosities and pressure points, andmaintaining <strong>the</strong> integrity of <strong>the</strong> longitudinal arch and/or <strong>the</strong> metatarsal heads. The devices can be madeof several different types of materials and can be fabricated from plaster molds of <strong>the</strong> feet or electronic(computer) imaging in a semi-weight bearing or non-weight bearing, neutral position, with correctionsbuilt in to prevent abnormal compensation during <strong>the</strong> gait cycle.A shoe modification is a medically prescribed alteration(s) to a shoe(s) to accommodate minor footdeformities, disabilities, or leg shortening of less than 1 and ½ inches. Shoe modifications, e.g., rockersoles, shoe buildups, metatarsal bars, shoe stretching, Thomas heels, tongue pads, Velcro closures,modified lacers, etc., may be applied to shoes, upon medical determination of need, to compensate forminor foot deformities.CLINICAL GUIDELINEPrior authorization is required for foot orthotics including inserts, arch supports, and modifications toorthopedic shoes. Foot orthotics can be considered medically necessary for members who meet <strong>the</strong>following criteria and for whom o<strong>the</strong>r treatment methods have been ruled out prior to recommending footorthotics.Custom-fabricated foot orthosis (es) are typically considered medically necessary when <strong>the</strong>re is failure,contraindication, or intolerance to a prefabricated foot orthosis for ANY of <strong>the</strong> following conditions:• Impaired peripheral sensation and/or altered peripheral circulation (e.g., diabetic neuropathy andperipheral vascular disease);Please note that authorization is based on medical necessity at <strong>the</strong> time <strong>the</strong> authorization is issued and is not a guarantee of payment.Payment is based on <strong>the</strong> member having active coverage, benefits and <strong>policies</strong> in effect at <strong>the</strong> time of service.1To determine if a service or procedure requires prior authorization, CMAP <strong>Provider</strong>s may refer to <strong>the</strong> Benefit and Authorization Gridssummaries on www.huskyhealth.com by clicking here [See DME/Pros<strong>the</strong>tics and Orthotics].. For a definitive list of benefits and servicelimitations, CMAP <strong>Provider</strong>s may access <strong>the</strong> CMAP provider fee schedules and regulations at www.ctdssmap.com.
• The foot orthosis is an integral part of a leg brace and is necessary for <strong>the</strong> proper functioning of<strong>the</strong> brace;• The foot orthosis is used to compensate for a missing portion of <strong>the</strong> foot (e.g., amputation) and isnecessary for <strong>the</strong> alleviation or correction of illness, injury or congenital defect;• Neurologic or neuromuscular condition (e.g., cerebral palsy, hemiplegia, spina bifida) producingspasticity, mal-alignment or pathological positioning of <strong>the</strong> foot where <strong>the</strong>re is reasonableexpectation of improvement;• Plantar fasciitis, following failure of conservative medical management (e.g.,stretching/streng<strong>the</strong>ning of calf muscles, taping, strapping, nonsteroidal anti-inflammatorymedications, reduced activity and physical <strong>the</strong>rapy) including, unless contraindicated, at least asix-week trial of a prefabricated or custom-fitted orthosis; and• Acquired or congenital foot deformity when ALL of <strong>the</strong> following criteria are met:1. The deformity is <strong>the</strong> result of ONE of <strong>the</strong> following:a. Symptomatic rigid flatfootb. Posterior tibial tendon dysfunctionc. Mid- or hind-foot arthritis2. The deformity is associated with significant pain that interferes with activities of daily livingand <strong>the</strong>re is impaired gait, balance, or mobility as a result of <strong>the</strong> condition.3. Conservative medical management has failed.4. There is a reasonable expectation that <strong>the</strong> condition will improve through <strong>the</strong> use of <strong>the</strong>orthotic device.• O<strong>the</strong>r foot condition or deformity, ei<strong>the</strong>r acquired or congenital, that interferes with activities ofdaily living and has resulted in impaired gait, balance, or mobility where supportive shoes and/oro<strong>the</strong>r intervention has been unsuccessful.Orthopedic footwear including inserts (L3000-L3030), arch supports (L3040-L3090) and o<strong>the</strong>rmodifications to shoes (L3649, L5000) for individuals who do not have diabetes is generally consideredmedically necessary in <strong>the</strong> following circumstances:• Heel replacements, sole replacements and shoe transfers involving shoes on a medicallynecessary lower extremity orthosis(es)• Inserts and o<strong>the</strong>r shoe modifications (e.g., arch supports) if <strong>the</strong>y are on a shoe that is an integralpart of a medically necessary lower extremity orthosis(es) or pros<strong>the</strong>sis(es) and is medicallynecessary for <strong>the</strong> proper functioning of <strong>the</strong> orthosis(es) or pros<strong>the</strong>sis(es)• O<strong>the</strong>r orthotic modifications will be considered on a case-by-case basis in consideration of <strong>the</strong>patient’s ambulation status, sensation, skin integrity, symptoms, and orthopedic alignment.Orthopedic footwear including inserts and modification to shoes for individuals with diabetes is generallyconsidered medically necessary if ALL of <strong>the</strong> following criteria are met:1. The individual has diabetes mellitus; and2. The individual has one or more of <strong>the</strong> following conditions:a. Previous amputation of <strong>the</strong> o<strong>the</strong>r foot or part of ei<strong>the</strong>r foot, orb. History of previous foot ulceration of ei<strong>the</strong>r foot, orc. History of pre-ulcerative calluses of ei<strong>the</strong>r foot, ord. Peripheral neuropathy with evidence of callus formation of ei<strong>the</strong>r foot, ore. Foot deformity of ei<strong>the</strong>r foot, orf. Poor circulation in ei<strong>the</strong>r foot.3. The certifying physician who is managing <strong>the</strong> individual’s systemic diabetic condition has certifiedthat indications (1) and (2) above are met and that he/she is treating <strong>the</strong> individual under aPlease note that authorization is based on medical necessity at <strong>the</strong> time <strong>the</strong> authorization is issued and is not a guarantee of payment.Payment is based on <strong>the</strong> member having active coverage, benefits and <strong>policies</strong> in effect at <strong>the</strong> time of service.2To determine if a service or procedure requires prior authorization, CMAP <strong>Provider</strong>s may refer to <strong>the</strong> Benefit and Authorization Gridssummaries on www.huskyhealth.com by clicking here [See DME/Pros<strong>the</strong>tics and Orthotics].. For a definitive list of benefits and servicelimitations, CMAP <strong>Provider</strong>s may access <strong>the</strong> CMAP provider fee schedules and regulations at www.ctdssmap.com.
comprehensive plan of care for his/her diabetes and that <strong>the</strong> individual needs <strong>the</strong> inserts ormodifications to <strong>the</strong>rapeutic shoes.4. O<strong>the</strong>r orthotic modifications will be considered on a case-by-case basis in consideration of <strong>the</strong>patient’s ambulation status, sensation, skin integrity, symptoms, and orthopedic alignment.A modification of a custom molded or depth shoe is typically considered medically necessary as asubstitute for an insert. Although not intended as a comprehensive list, <strong>the</strong> following are <strong>the</strong> mostcommon shoe modifications:• Rigid rocker bottoms• Roller bottoms• Wedges• Metatarsal bars• Offset heelsThe following orthotic devices are generally NOT considered medically necessary:• Separate orthotic devices for an additional pair of shoes• Orthoses primarily for improved athletic performance or sports participation• Orthoses considered experimental, investigational or unproven (this list may not be all-inclusiveincluding) including:1. Custom-fabricated foot orthosis for <strong>the</strong> treatment of hallux valgus or hallux rigidus footdeformity2. Magnetic insole (i.e., orthosis with magnetic foil)• Foot orthotics not ordered by <strong>the</strong> treating providerCustom-fabricated foot orthoses and orthopedic footwear including inserts, arch supports andmodifications to shoes, that do not meet <strong>the</strong> above criteria are generally not considered medicallynecessary. Additional evidence must be provided for individual consideration to support medicalnecessity in situations that do not meet <strong>the</strong> criteria listed above.COVERAGE:Foot orthotics are a covered benefit for those members who demonstrate medical necessity as definedabove.EFFECTIVE DATEThis Clinical Guideline is effective for prior authorization requests for foot orthotics for HUSKY A, C and Dmembers on or after October 1, 2012.LIMITATIONSFoot orthotics are NOT covered for members enrolled in <strong>the</strong> HUSKY B <strong>Program</strong> <strong>Health</strong> Plan. Band 1and Band 2 HUSKY B members may be eligible for <strong>the</strong>se items under <strong>the</strong> HUSKY Plus <strong>Program</strong>.HUSKY Plus provides supplemental coverage of children with intensive physical health needs forservices not covered under <strong>the</strong> HUSKY B plan, only Band 1 and 2 children may qualify. Call 1-860-837-6200 for more information.Please note that authorization is based on medical necessity at <strong>the</strong> time <strong>the</strong> authorization is issued and is not a guarantee of payment.Payment is based on <strong>the</strong> member having active coverage, benefits and <strong>policies</strong> in effect at <strong>the</strong> time of service.3To determine if a service or procedure requires prior authorization, CMAP <strong>Provider</strong>s may refer to <strong>the</strong> Benefit and Authorization Gridssummaries on www.huskyhealth.com by clicking here [See DME/Pros<strong>the</strong>tics and Orthotics].. For a definitive list of benefits and servicelimitations, CMAP <strong>Provider</strong>s may access <strong>the</strong> CMAP provider fee schedules and regulations at www.ctdssmap.com.
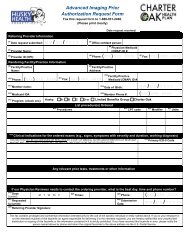
PROCEDUREAll requests for orthotics and pros<strong>the</strong>tics will be reviewed under and all final determinations of medicalnecessity will be made under Connecticut General Statute Section 17b-259b. Coverage determinationswill be based upon a review of requested and/or submitted case-specific information to include evidencebasedevaluations.Information Required for Review:A clinical assessment by <strong>the</strong> patient’s physician (preferably an orthopedist or podiatrist) BEFORE <strong>the</strong>patient is referred for foot orthotics is required. This clinical assessment should also include <strong>the</strong>physician’s specific recommendation for types of orthotics, including additions/modifications andaccompany <strong>the</strong> request for prior authorization for <strong>the</strong> foot orthotics which will also provide <strong>the</strong> necessaryclinical information for appropriate medical review and decision. The assessment can also include <strong>the</strong>o<strong>the</strong>r medical approaches being used to address <strong>the</strong> patient’s needs, including o<strong>the</strong>r DME, medications,and <strong>the</strong>rapies; including <strong>the</strong> following:1. Prescription/ signed letter of medical necessity;2. Completed State of Connecticut, Department of Social Services Outpatient Prior AuthorizationRequest Form;3. Treatment history, including effectiveness of treatment, orthotics, and medications;4. Clinical assessment to include:• Current list of ambulatory aids/orthotics with current skill level for each;• Ambulatory skills with and without orthoisis• Patient’s current health status, functional abilities, level of activity and level of comfort;• Date of purchase, condition, and fit of current orthotics and shoes;• Primary diagnosis(es)• Foot/ankle/forefoot muscle strength, range of motion, and any deformities or asymmetries• Vascular, skin and sensory status• Observational gait assessment (swing and stance phase)5. Documentation confirming that <strong>the</strong> member’s medical condition cannot be addressed viaalternative medical approaches, functional strategies, or o<strong>the</strong>r/existing DME; e.g., muscularstretching, streng<strong>the</strong>ning exercises, taping, NSAIDS, over-<strong>the</strong>-counter insoles, and/or supportiveshoes or athletic shoes. O<strong>the</strong>r forms of treatment have been considered and ruled out. Customfabricatedfoot orthotics are not medically necessary unless <strong>the</strong>re is clinical documentation thatnon-custom, prefabricated foot orthotics are not appropriate for <strong>the</strong> condition or diagnosis.6. O<strong>the</strong>r pertinent information as requested by Medical Management and/or Utilization ManagementDepartments.7. A detailed product description and quotation including manufacturer, model/part number, productdescription, HCPC code, unit(s), quantity, DSS fee schedule allowed amount and retail pricesubmitted by <strong>the</strong> DME vendor.Review Process:1. Requests for foot orthotics must be submitted by <strong>the</strong> billing provider/vendor.2. Requests for items should be submitted to CHNCT via fax at 203-265-3994 using <strong>the</strong> OutpatientPrior Authorization Request Form located on <strong>the</strong> HUSKY <strong>Health</strong> website atwww.huskyhealth.com. Requests for foot orthotics will be reviewed by <strong>the</strong> CHNCT UtilizationManagement Department in accordance with <strong>the</strong> <strong>procedures</strong> and time-frames in place forreviewing requests for DME and medical-surgical supplies. CHNCT has up to 14 calendar daysto notify <strong>the</strong> provider of <strong>the</strong>ir decision. If additional information is requested, <strong>the</strong> provider has upto 14 calendar days to submit <strong>the</strong> requested information.Please note that authorization is based on medical necessity at <strong>the</strong> time <strong>the</strong> authorization is issued and is not a guarantee of payment.Payment is based on <strong>the</strong> member having active coverage, benefits and <strong>policies</strong> in effect at <strong>the</strong> time of service.4To determine if a service or procedure requires prior authorization, CMAP <strong>Provider</strong>s may refer to <strong>the</strong> Benefit and Authorization Gridssummaries on www.huskyhealth.com by clicking here [See DME/Pros<strong>the</strong>tics and Orthotics].. For a definitive list of benefits and servicelimitations, CMAP <strong>Provider</strong>s may access <strong>the</strong> CMAP provider fee schedules and regulations at www.ctdssmap.com.
CODES:CodeL3000L3001L3002L3003L3010L3020L3030L3040L3050L3060L3070L3080L3090L3649L5000DescriptionFoot insert, removable, molded to patient model, UCB type, Berkeley shell, eachFoot insert, removable, molded to patient model, Spenco, eachFoot insert, removable, molded to patient model, Plastazote or equal, eachFoot insert, removable, molded to patient model, silicone gel, eachFoot insert, removable, molded to patient model, longitudinal arch support, eachFoot insert, removable, molded to patient model, longitudinal./metatarsal support, eachFoot insert, removable, formed to patient foot, eachFoot, arch support, removable, premolded, longitudinal, eachFoot, arch support, removable, premolded, metatarsal, eachFoot, arch support, removable, premolded, longitudinal/metatarsal, eachFoot, arch support, nonremovable, attached to shoe, longitudinal, eachFoot, arch support, nonremovable, attached to shoe, metatarsal, eachFoot, arch support, nonremovable, attached to shoe, longitudinal/metatarsal, eachOrthopedic shoe, modification, addition or transfer, not o<strong>the</strong>rwise specifiedPartial foot, shoe insert with longitudinal arch, toe fillerDEFINITIONS1. HUSKY A: Connecticut’s implementation of health insurance under <strong>the</strong> federal Medicaid program(Title XIX) for children, parents or relative caretakers. Eligibility is for families earning below 185% aswell as pregnant women under 250% of <strong>the</strong> federal poverty level and o<strong>the</strong>r groups pursuant toSection 17b-266 of <strong>the</strong> Connecticut General Statutes.2. HUSKY B: The health insurance plan for children and youth, up to <strong>the</strong> age of nineteen, establishedpursuant to Title XXI (CHIP) of <strong>the</strong> Social Security Act, <strong>the</strong> provisions of Sections 17b-289 to 17b-303, inclusive, of <strong>the</strong> Connecticut General Statutes, and Section 16 of Public Act 97-1 of <strong>the</strong> Octoberspecial session. This program provides subsidized health insurance for uninsured children in familiesearning from 185% to 300% of <strong>the</strong> federal poverty level. Unsubsidized coverage is available underHUSKY B for families earning more than 300% of <strong>the</strong> federal poverty level.3. HUSKY C: Connecticut’s implementation of health insurance under <strong>the</strong> federal Medicaid program(Title XIX) for individuals who are aged, blind or disabled (ABD) and certain o<strong>the</strong>r groups such asrefugees.4. HUSKY D: Connecticut’s implementation of health insurance under <strong>the</strong> federal Medicaid program(Title XIX) for low income adults age 19 to 64, also known as Medicaid for Low Income Adults (LIA).5. HUSKY <strong>Health</strong> <strong>Program</strong>: The HUSKY A, HUSKY B, HUSKY C, HUSKY D and HUSKY LimitedBenefit programs, collectively.6. HUSKY Limited Benefit <strong>Program</strong> or HUSKY, LBP: Connecticut’s implementation of limited healthinsurance coverage under Medicaid for individuals with tuberculosis or for family planning purposesand such coverage is substantially less than <strong>the</strong> full Medicaid coverage.7. Medically Necessary or Medical Necessity: (as defined in Connecticut General Statutes § 17b-259b) Those health services required to prevent, identify, diagnose, treat, rehabilitate or amelioratean individual's medical condition, including mental illness, or its effects, in order to attain or maintainPlease note that authorization is based on medical necessity at <strong>the</strong> time <strong>the</strong> authorization is issued and is not a guarantee of payment.Payment is based on <strong>the</strong> member having active coverage, benefits and <strong>policies</strong> in effect at <strong>the</strong> time of service.5To determine if a service or procedure requires prior authorization, CMAP <strong>Provider</strong>s may refer to <strong>the</strong> Benefit and Authorization Grids summarieson www.huskyhealth.com or www.charteroakhealthplan.com by clicking here [See DME/Pros<strong>the</strong>tics and Orthotics].. For a definitive list ofbenefits and service limitations, CMAP <strong>Provider</strong>s may access <strong>the</strong> CMAP provider fee schedules and regulations at www.ctdssmap.com.
<strong>the</strong> individual's achievable health and independent functioning provided such services are: (1)Consistent with generally-accepted standards of medical practice that are defined as standards thatare based on (A) credible scientific evidence published in peer-reviewed medical literature that isgenerally recognized by <strong>the</strong> relevant medical community, (B) recommendations of a physicianspecialtysociety, (C) <strong>the</strong> views of physicians practicing in relevant clinical areas, and (D) any o<strong>the</strong>rrelevant factors; (2) clinically appropriate in terms of type, frequency, timing, site, extent and durationand considered effective for <strong>the</strong> individual's illness, injury or disease; (3) not primarily for <strong>the</strong>convenience of <strong>the</strong> individual, <strong>the</strong> individual's health care provider or o<strong>the</strong>r health care providers; (4)not more costly than an alternative service or sequence of services at least as likely to produceequivalent <strong>the</strong>rapeutic or diagnostic results as to <strong>the</strong> diagnosis or treatment of <strong>the</strong> individual's illness,injury or disease; and (5) based on an assessment of <strong>the</strong> individual and his or her medical condition.8. Prior Authorization: A process for approving covered services prior to <strong>the</strong> delivery of <strong>the</strong> service orinitiation of <strong>the</strong> plan of care based on a determination by CHNCT as to whe<strong>the</strong>r <strong>the</strong> requested serviceis medically necessary.9. Custom-fabricated orthosis: An orthosis that is specifically manufactured for an individual.Custom-fabricated devices may include custom-molded devices (e.g., molded to <strong>the</strong> individual’sspecific body part).10. Prefabricated orthosis: An orthosis manufactured in quantity without a specific individual in mind(e.g., off-<strong>the</strong>-shelf). Prefabricated orthotic devices may include custom-fitted devices (e.g., trimmed,bent or molded for use by a specific individual).11. Foot orthosis: A type of shoe insert that does not extend beyond <strong>the</strong> ankle and may include heelwedges and arch supports. The goal of treating conditions with foot orthoses is to decrease pain andincrease function. They may also correct some foot deformities and provide shock absorption to <strong>the</strong>foot. Foot orthoses may be used to treat conditions such as those involving impaired peripheralcirculation and sensation, when <strong>the</strong>y are attached to a pros<strong>the</strong>tic shoe or brace, for a neurologic orneuromuscular condition and for congenital or acquired foot conditions. HCPCS codes representingfoot orthoses provided to patients without diabetes are L3000–L3090.12. Foot Orthoses Associated with Pros<strong>the</strong>tic Shoes and Braces: Pros<strong>the</strong>tic shoes are used whenall or a portion of <strong>the</strong> foot is missing. A brace may or may not be attached to <strong>the</strong> pros<strong>the</strong>tic shoe. Theabsence of all or a portion of <strong>the</strong> foot may be <strong>the</strong> result of a congenital deformity, illness (amputationsecondary to diabetic foot ulcer) or injury (traumatic amputation). Patients with minor distalamputations typically do not require special shoes. When all digits have been amputated, a forefootfiller orthosis may be used with a commercial shoe. For more extensive partial-foot amputations (e.g.,mid-level Trans metatarsal, Chopart’s amputation), a pros<strong>the</strong>tic may be needed consisting of aconventional shoe with an ankle-foot orthosis (AFO), brace and a forefoot filler. A custom-fitted orcustom-molded foot orthosis may be used as a replacement or substitute for missing parts of <strong>the</strong> foot(e.g., due to amputation) and when it is necessary for <strong>the</strong> alleviation or correction of illness, injury orcongenital defect.13. Metatarsal bars: Exterior bars that are placed behind <strong>the</strong> metatarsal heads in order to removepressure from <strong>the</strong> metatarsal heads. The bars are of various shapes, heights, and constructiondepending on <strong>the</strong> exact purpose14. Offset heel: A heel flanged at its base ei<strong>the</strong>r in <strong>the</strong> middle, to <strong>the</strong> side, or a combination, that is <strong>the</strong>nextended upward to <strong>the</strong> shoe in order to stabilize extreme positions of <strong>the</strong> hind foot.16. Rigid rocker bottoms: Exterior elevations with apex position for 51% to 75% distance measuredfrom <strong>the</strong> back end of <strong>the</strong> heel. The apex is a narrowed or pointed end of an anatomical structure. Theapex must be positioned behind <strong>the</strong> metatarsal heads and taper off sharply to <strong>the</strong> front tip of <strong>the</strong> sole.Apex height helps to eliminate pressure at <strong>the</strong> metatarsal heads. Rigidity is ensured by <strong>the</strong> steel in<strong>the</strong> shoe. The heel of <strong>the</strong> shoe tapers off in <strong>the</strong> back in order to cause <strong>the</strong> heel to strike in <strong>the</strong> middleof <strong>the</strong> heel.Please note that authorization is based on medical necessity at <strong>the</strong> time <strong>the</strong> authorization is issued and is not a guarantee of payment.Payment is based on <strong>the</strong> member having active coverage, benefits and <strong>policies</strong> in effect at <strong>the</strong> time of service.To determine if a service or procedure requires prior authorization, CMAP <strong>Provider</strong>s may refer to <strong>the</strong> Benefit and Authorization Gridssummaries on www.huskyhealth.com by clicking here [See DME/Pros<strong>the</strong>tics and Orthotics].. For a definitive list of benefits and servicelimitations, CMAP <strong>Provider</strong>s may access <strong>the</strong> CMAP provider fee schedules and regulations at www.ctdssmap.com.6