Radiology Benefit Management Program â Prior Authorization for ...
Radiology Benefit Management Program â Prior Authorization for ...
Radiology Benefit Management Program â Prior Authorization for ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
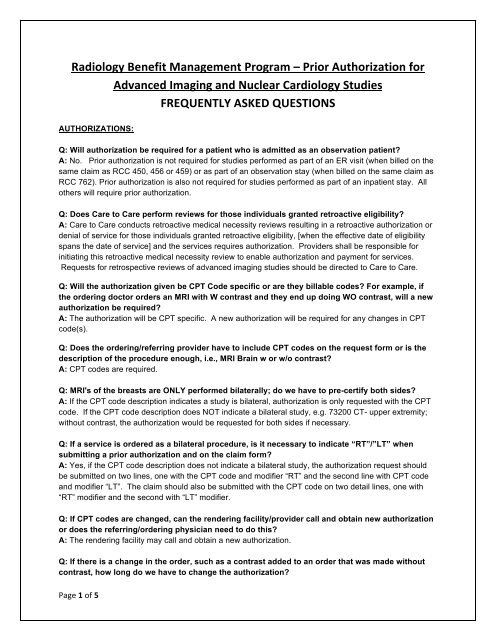
<strong>Radiology</strong> <strong>Benefit</strong> <strong>Management</strong> <strong>Program</strong> – <strong>Prior</strong> <strong>Authorization</strong> <strong>for</strong> Advanced Imaging and Nuclear Cardiology Studies FREQUENTLY ASKED QUESTIONS AUTHORIZATIONS:Q: Will authorization be required <strong>for</strong> a patient who is admitted as an observation patient?A: No. <strong>Prior</strong> authorization is not required <strong>for</strong> studies per<strong>for</strong>med as part of an ER visit (when billed on thesame claim as RCC 450, 456 or 459) or as part of an observation stay (when billed on the same claim asRCC 762). <strong>Prior</strong> authorization is also not required <strong>for</strong> studies per<strong>for</strong>med as part of an inpatient stay. Allothers will require prior authorization.Q: Does Care to Care per<strong>for</strong>m reviews <strong>for</strong> those individuals granted retroactive eligibility?A: Care to Care conducts retroactive medical necessity reviews resulting in a retroactive authorization ordenial of service <strong>for</strong> those individuals granted retroactive eligibility, [when the effective date of eligibilityspans the date of service] and the services requires authorization. Providers shall be responsible <strong>for</strong>initiating this retroactive medical necessity review to enable authorization and payment <strong>for</strong> services.Requests <strong>for</strong> retrospective reviews of advanced imaging studies should be directed to Care to Care.Q: Will the authorization given be CPT Code specific or are they billable codes? For example, ifthe ordering doctor orders an MRI with W contrast and they end up doing WO contrast, will a newauthorization be required?A: The authorization will be CPT specific. A new authorization will be required <strong>for</strong> any changes in CPTcode(s).Q: Does the ordering/referring provider have to include CPT codes on the request <strong>for</strong>m or is thedescription of the procedure enough, i.e., MRI Brain w or w/o contrast?A: CPT codes are required.Q: MRI's of the breasts are ONLY per<strong>for</strong>med bilaterally; do we have to pre-certify both sides?A: If the CPT code description indicates a study is bilateral, authorization is only requested with the CPTcode. If the CPT code description does NOT indicate a bilateral study, e.g. 73200 CT- upper extremity;without contrast, the authorization would be requested <strong>for</strong> both sides if necessary.Q: If a service is ordered as a bilateral procedure, is it necessary to indicate “RT”/”LT” whensubmitting a prior authorization and on the claim <strong>for</strong>m?A: Yes, if the CPT code description does not indicate a bilateral study, the authorization request shouldbe submitted on two lines, one with the CPT code and modifier “RT” and the second line with CPT codeand modifier “LT”. The claim should also be submitted with the CPT code on two detail lines, one with“RT” modifier and the second with “LT” modifier.Q: If CPT codes are changed, can the rendering facility/provider call and obtain new authorizationor does the referring/ordering physician need to do this?A: The rendering facility may call and obtain a new authorization.Q: If there is a change in the order, such as a contrast added to an order that was made withoutcontrast, how long do we have to change the authorization?Page 1 of 5
A: Any changes made to an ordered procedure can take place during the 30-Day approval timeframe ofthe authorization, but it is PREFERRED that any change is indicated within 1 business day prior to theDate of Service (DOS).<strong>Radiology</strong> <strong>Benefit</strong> <strong>Management</strong> <strong>Program</strong> – <strong>Prior</strong> <strong>Authorization</strong> <strong>for</strong> Advanced Imaging and Nuclear Cardiology Studies FREQUENTLY ASKED QUESTIONS Q: For “urgent” studies done after hours, should they be per<strong>for</strong>med without a prior authorizationand a prior authorization request submitted the next business day?A: For urgent studies per<strong>for</strong>med after hours, the study may be per<strong>for</strong>med and an authorization requestsubmitted the following business day. Please Note: urgent requests will still need to meet the definition ofmedical necessity.Q: Are the authorizations date specific? Are they valid <strong>for</strong> 30 days or both?A: <strong>Authorization</strong>s are valid <strong>for</strong> 30 days from the date the request is approved.Q: Is a new authorization needed if there is a change to the date of a previously authorizedservice/ test that is still within the 30 day period?A: NoQ: If an office of the referring/rendering provider fails to obtain prior authorization (PA) <strong>for</strong> aservice that requires a PA, due to having incorrect insurance in<strong>for</strong>mation, do we have a 24-48 hourwindow to get a retroactive authorization?A: Rendering providers are required to ensure that there is a prior authorization approval <strong>for</strong> any hightechradiology services be<strong>for</strong>e they are per<strong>for</strong>med. If the insurance in<strong>for</strong>mation of the member associatedwith the PA is incorrect, you will need to contact the RBM <strong>Program</strong> within two business days, who willthen issue a new authorization.Q: Can we revise an authorization after a procedure has been per<strong>for</strong>med?A: If an authorization is approved and a different procedure is per<strong>for</strong>med, you will need to contact theRBM <strong>Program</strong> <strong>for</strong> a new authorization. Modifications such as with contrast to without contrast will beapprovable, but any modality modifications will require another medical necessity review.Q: As a free standing facility we have multiple providers within the group. When thereferring/ordering provider is trying to prior authorize a procedure, can we provide them with thegroup’s AVRS number?A: Providing a facility’s AVRS number to a provider would be at the group’s discretion.Q: Can the rendering facility change the rendering facility’s address, when there are multiplesites?A: As long as the rendering facility has the appropriate request number and member demographics, theywill be able to request a different rendering facility address, and then a new authorization will be issued.Page 2 of 5
<strong>Radiology</strong> <strong>Benefit</strong> <strong>Management</strong> <strong>Program</strong> – <strong>Prior</strong> <strong>Authorization</strong> <strong>for</strong> Advanced Imaging and Nuclear Cardiology Studies FREQUENTLY ASKED QUESTIONSQ: If an exam is changed at the time of service, such as adding contrast to an exam authorizedwithout contrast, can an update to the authorization be submitted after the exam? If so is thissomething that the rendering provider/facility will be able to do or does the referring/orderingprovider be required to make the change?A: A rendering facility may request a change to the original authorization. The original authorization willbe cancelled and a new authorization with a new authorization number will be given if deemedappropriate and medically necessary Q: Does the criteria based assistance prompt the provider to order the correct exam, i.e. CTabdomen and pelvis <strong>for</strong> abdomen pain, not just abdomen CT.A: The criteria based assistance in the CARE Portal is available <strong>for</strong> indicating major symptoms of thepatient and determining medical necessity. If you wish to discuss proper exams, phone requests will be amore appropriate path.Q: What if there is not an authorization or an authorization is pending when the patient presents,is the client/patient turned away?A: <strong>Authorization</strong> SHOULD be obtained prior to per<strong>for</strong>ming a study. However, <strong>for</strong> urgent studiesper<strong>for</strong>med after hours, the study may be per<strong>for</strong>med and an authorization request submitted the followingbusiness day. Please Note: Urgent requests will still need to meet the definition of medical necessity.Q: Can the rendering facility/provider verify that a prior authorization has been made?A: Yes. <strong>Authorization</strong> status may be viewed in the Care to Care CARE Portal.Q: Can the authorization be printed once it is authorized?A: Once a request is approved, an authorization letter will be faxed to the referring provider. If you wishto print a copy of the <strong>Authorization</strong> Confirmation screen in the CARE Portal, you will have the ability toprint through your ISP.Q: How does a facility find a prior authorization on the website?A: If a facility is registered with the CARE Portal system, they can review prior authorization requests withthe request reference number through the “<strong>Authorization</strong> Inquiry” tab on the home screen.Q: Do we have to register on Care to Care’s (CtC) CARE Portal system in order to submit priorauthorization requests online?A: Yes.Page 3 of 5
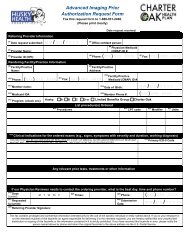
<strong>Radiology</strong> <strong>Benefit</strong> <strong>Management</strong> <strong>Program</strong> – <strong>Prior</strong> <strong>Authorization</strong> <strong>for</strong> Advanced Imaging and Nuclear Cardiology Studies FREQUENTLY ASKED QUESTIONSBILLING/CLAIMS SUBMISSION:Q: If the patient has Medicare or a Medicare Advantage Plan and Medicaid is secondary will a <strong>Prior</strong><strong>Authorization</strong> be needed?A: <strong>Prior</strong> authorization from Care to Care <strong>for</strong> advanced imaging studies is not required <strong>for</strong> members with dual eligibility where traditional Medicare is primary. Please refer to the member’s primary carrier <strong>for</strong> coverage in<strong>for</strong>mation. <strong>Prior</strong> authorization from Care to Care <strong>for</strong> advanced imaging studies is required <strong>for</strong> members with dual eligibility where a Medicare Advantage Plan/Commercial Medicare Plan is primary. Q: If a commercial insurance is the Primary payor, will HUSKY Health <strong>Program</strong> and Charter OakHealth Plan require a prior authorization?A: YesQ: If the patient insists on having a procedure requiring prior authorization but one is notobtained, can the patient be held financially responsible?A: No, a HUSKY Health or Charter Oak client cannot be held financially liable/responsible <strong>for</strong> a coveredservice that is not payable due to the provider’s failure to obtain prior authorization as required under theprogram.Additional balance billing guidelines are found in the Provider Manual, Chapter 2 on the DSS website,www.ctdssmap.com.“A provider shall only charge an eligible Medical Assistance <strong>Program</strong> client, or any financially responsiblerelative or representative of that individual, <strong>for</strong> goods or services which are not coverable under theMedical Assistance <strong>Program</strong>, when the client knowingly elects to receive the goods or services andenters into an agreement in writing or such goods or services prior to receiving them;” CARE PORTAL REGISTRATION:Q: We are a participating facility with the HUSKY Health and Charter Oak <strong>Program</strong>s, howeverwhen I went on line to make sure we were listed, nothing cames up. What do we do?A: In order to register with the CARE Portal system, you will need to verify your facility is registered withthe Connecticut DSS through www.ctdssmap.com. You will then be able to locate your facility using thesite’s NPI or Medicaid ID.Page 4 of 5
GENERAL QUESTIONS:Q: Do radiologists within a group all have an individual AVRS number (Medicaid ID number)?A: Yes, all providers that are successfully enrolled in the CMAP network are issued an AVRS/CMAP IDnumber. If they are enrolled with CMAP, then they have received an AVRS/CMAP ID number.<strong>Radiology</strong> <strong>Benefit</strong> <strong>Management</strong> <strong>Program</strong> – <strong>Prior</strong> <strong>Authorization</strong> <strong>for</strong> Advanced Imaging and Nuclear Cardiology Studies FREQUENTLY ASKED QUESTIONS Q: Where can the group and provider’s AVRS numbers be obtained or found?A: The group/provider AVRS/CMAP ID number can be found on the following:• HP provider enrollment letters issued to the provider upon successfully enrolling in the CMAPnetwork,• Provider secure web site, www.ctdssmap.com,• Provider remittance advice.Q: Where on the HUSKY HEALTH website is the webinar presentation?A: www.huskyhealth.com• Select “For Providers”• Select the Quick link “Provider Training and Events” under Find It Here• Click on “Provider Webinars” - then scroll to the bottom of the screen and click on “download acopy of the <strong>Radiology</strong> <strong>Benefit</strong> <strong>Management</strong> webinar presentation here”.Q: Is there a direct telephone number to reach Care to Care with questions?A: Contact (800) 440.5071Press prompt #2 then;Press prompt #2 <strong>for</strong> Medical <strong>Authorization</strong>s; thenPress prompt #1 <strong>for</strong> <strong>Radiology</strong> <strong>Authorization</strong>sQ: What is the telephone number to call when a change is needed to a prior authorized service?A: Contact (800) 440.5071Press prompt #2 then;Press prompt #2 <strong>for</strong> Medical <strong>Authorization</strong>s; thenPress prompt #1 <strong>for</strong> <strong>Radiology</strong> <strong>Authorization</strong>s.Q: What is the facsimile number to fax the <strong>Prior</strong> <strong>Authorization</strong> Form?A: The number to fax the <strong>Prior</strong> <strong>Authorization</strong> Request Form is 888.931.2468.Page 5 of 5