Inflammations of the nervous system
Inflammations of the nervous system
Inflammations of the nervous system
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
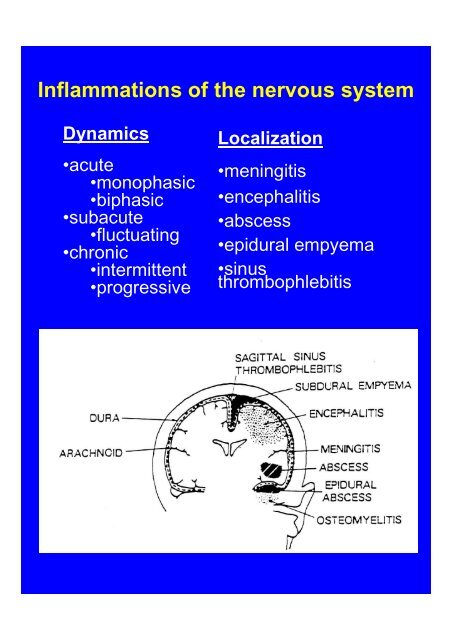
<strong>Inflammations</strong> <strong>of</strong> <strong>the</strong> <strong>nervous</strong> <strong>system</strong>Dynamics•acute•monophasic•biphasic•subacute•fluctuating•chronic•intermittent•progressiveLocalization•meningitis•encephalitis•abscess•epidural empyema•sinusthrombophlebitis
Pathology1. Meningeal infiltration2. Blood-brain barrier damage• perivascular cellular infiltration• extracellular edema3. Glial proliferation4. Damage <strong>of</strong> <strong>the</strong> <strong>nervous</strong> tissue(neuron, axon, oligodendroglia, myelin sheath)The routes <strong>of</strong> infection1. Hematogen (abscess)2. Paranasal sinuses (meningitis)3. Respiratory tract (nose, lung) (meningoencephalitis)4. Scull fracture (abscess, epiduralempyema, meningitis)5. Peripheral nerve (rabies, HSV, VZV)
MENINGITISPathology•Cellular infiltration <strong>of</strong> <strong>the</strong> meningxes•Brain parenchyma is intact, except edemaand radicular/cranial nerve lesionsClinical picture: ("Meningeal syndrome”)• general symptoms (fever, weakness)• signs <strong>of</strong> meningeal irritation (nuchalrigidity, Kernig-, Brudzinsky signs,headache, hyperirritability)• changes in mental status (apathy,somnolence, delirium)• focal neurological signs are absent• "CSF syndrome" (increased cell&protein)
Acute aseptic meningitisPathogens:•virusHERPES (HSV, HZV, EBV, CMV),ENTERO (echo, coxaci, polio, etc.),ARBO (tick-bite encephalitis virus),ADENO, LCMV, HIV, etc.•spirochete (leptospira, borrelia, treponema)Clinical pictureIncubation 7-10 day, "dromedary" courseCSF:•cell count 50-1000/ul, lymphocytes•protein level moderately elevated (0.4-lg/1)•sugar: normal•microbiol. culture: negative Dg: serology(repeated)O<strong>the</strong>rs:EEG, neuroimaging: usually normalTherapy: supportive
Subacute/chronic meningitisPathogens:•mycobacterium, mycoplasma•fungus (candida, cryptococcus, aspergillus)•spirochete (leptospira, borrelia)•virus (LCMV)•toxoplasma•non-infective (leukemia, SLE, tumour cells)Clinical picture (weeks-months)intermittent febrile statesslowly progressive mental changes, mild (orabsent) meningeal signs, progressive cranialnerve palsiesCSF:•50-100/ul cells, lymphocytes•high protein level - 1-3 g/1 (severe BBBdamage)•low sugar level (>2 mmol/l)Dg: need special culture technique, serologyTherapy: for tbc: Isonicid, Rifampycin,Dexamethason. for fungus: Amphotericin B
Purulent meningitisPathogens:•adult: Pnemococcus, N. meningitidis,•child: Hemophylus, EnterobacteriaClinical picture:primary extracranial manifestation (lung,paranasal)severe condition, high fever, prominentmeningeal signs, confusion (high mortality !)residual signs (hydrocephalus, hypacusis,ment. retard., epileptic seizures)CSF: green-like•1000 to several 10,000 cells/ul, granulocytes•high protein level (1-3 g/1)•low sugarDg: microbiol. cultureO<strong>the</strong>r: eradication <strong>of</strong> <strong>the</strong> (respiratory) sourceEEG: generalized slowing CT/MRI: look for"pus-cap”, brain abscess, hydrocephalusTherapy: based on <strong>the</strong> culture. Before:Penicillin + Ampicillin + Ceftriaxon iv., insevere cases + Dexamethason(Steptokinaze)
„Covered syndrome”(pretreated/masked form <strong>of</strong> purulentmeningitis)Clinical pictureheadache, intermittent febrile state, butno prominent meningeal signsantibiotic <strong>the</strong>rapy in <strong>the</strong> recent historyCSF•no more than 1000 cells, granulocytes/mixed•protein elevated >1 g/l•sugar: decreased•negative culture resultDiagnosis based on CSF findingsTherapy should be <strong>the</strong> same as in acutepurulent meningitis (combined antibiotics)Brain abscessEtiol.: direct or haematogenic spreadingClinical picture: focal signs, seizures, risedintracranial pressureDg: CT, MRITH: antibiotics, surgical
ENCEPHALITISPathology:Blood-brain barrier damage+Central <strong>nervous</strong> <strong>system</strong> damageClinically: "Encephalitis syndrome"meningeal syndrome +neurological signs (focal signs <strong>of</strong> motor-,sensory, autonomic <strong>system</strong>s, sings <strong>of</strong>inreased intracranial pressure)seizuresaltered mental stateEEG, MRI, CSF alterationsPolio- leuko- panencephalitis
Polioencephalitis:Herpes simplex encephalitis•Clinical: primary [subclinical] infection withHSV-1, endogenous reactivation,• flu-like phase followed by encephalitislocated to temporal lobe (aphasia, paresis,seizures, psychoorganic syndrome).•Dg: CSF, EEG, MRI, biopsy (PCR),serology.•Treatment with Acyclovir 30mg/bwkg a dayfor weeksTick-born encephalitis•Clinical: tick bite,•flu-like illness followed by meningitis orencephalitis syndrome, predilection forcervical spinal cord motoneurons andtemporal lobe•Dg: typical CSF findings, serology•TH: supportive
HSV
Acute anterior poliomyelitisClinical: gastrointestinal infection, viraemiafollowed by asymmetric flaccid paresis,predilection for large motoneurons in spinalcord and brainstem,Dg: typical CSF findings,Treatment : supportive, prevention withperoral immunization)Lyssa, rabiesClinical: transmitted by bite <strong>of</strong> an rabidanimal {small predators}, week to months <strong>of</strong>incubation period,Stages: 1. Prodrome (fever, fatigue) 2.Excitation (restlessness, hyperirritability,convulsions, 3. Paralytic phase (widespreadparesis, death)Dg. Pathology (Negri-body in hippocampus),CSF, preventive immunization)
CMVNegri
LeukoencephalitisPathology: immune demyelinationClinical picture: acute/subacute, monophasicdisease with widespread white matter lesion,typical CSF (BBB damage +OB)•parainfectious encephalomyelitis(measles, rubella, varicella, smallpox, mumps,infectious mononucleosis)•postvaccination encephalomyelitis(vaccination against smallpox, measles,rabies, tetanus)
Panencephalitis(„slow virus” diseases, progressive course)•SSPE (subacute sclerotising panencephalitis)•CJD (Kreutzfeld-Jakob disease)•PML (progressive multifocalleuko-encephalopathy)
SSPEPathogenesis:childhood infection with measles virusreactivation <strong>of</strong> "defective" virus (5-10y),Clinical pictureno general signs, young patients,progressive dementia (impaired cognitiveperformance in school), ataxia, myoclonicjerks, decerebration, deathEEG: generalized slow waves(Rademecker complex) in every 3-10 sec.CSF: OB, high anti-measles Ab'sTh: symptomatic
CJDEtiology:Prion (sporadic, iatrogenic, familial)Clinical pictureOnset: 35-65 y, personality changes,progressive dementia within few months,extrapyramidal signs, ataxia, dysarthria,myoclonus, death within a yearsEEG: triphasic slow complexes, 1-2 cpsCSF: unremarcableDg: clinical picture, (brain biopsy)Th: symptomatic
GSS(Gertsmann-Straussler-Scheinkerdisease)AD inheritanceOnset: 40-50 y, duration 1-10 yClin.: spinocerebellar degen. + dementiaFFI(Fatal familial insomnia)Degen. <strong>of</strong> <strong>the</strong> medial nucleus <strong>of</strong>thalamusClin: lack <strong>of</strong> sleep + vegetativedisturbancesDg: clinical + EEG/polysomnography
PML(progressive multifocal leukoencephalopathy)Immunsuppression (HIV, cytostatics,leukemia, malignancies)Mechanism: JC papova virus causesoligodendroglia degenerationClinical picture: subacute onset, changingin personality, pramidal signs, ataxia,dementia, death within a few monthsCSF: unremarkableMRI: demyelination (confluent, noenhancement)Dg: brain biopsyTh: stop immunsuppression, symptomatic
NeurosyphilisPathogen: treponema pallidumPrimer genital infection followed byhematogenous spreadingForms:1. Luetic meningitis (early)2. Meningovascular syphilis (months)3. Paralysis progressiva (dementia,psychosis, several years)4. Tabes dorsalis (spinal ataxia)Dg: CSF, serology, MRITh: penicillin
NEUROBORRELIOSISEtiologySpirochetal (Borrelia burgdorferi) infection bybite <strong>of</strong> a vector insect (tick borne)Symptoms and signsRelapsing-remitting course with multipleorgan affection: skin- ECM, heart-carditis,joints- mono-, polyarthritis, and CNS/PNS -neuroborreliosisStages•(acute) flu-Iike symptoms (headache,myalgia, ECM)•(subacute) meningitis, meningoradiculitis,mono-, polyneuritis (+arthritis, andsometimes carditis)•(chronic) meningo-encephalo-myelitis
NEUROBORRELIOSISCharacteristic neurological forms:•Diplegia facialis-most common form <strong>of</strong>neuritis caused by BB. (1-3 weeks)•Bannwarth-Sy. (meningo-polyradiculitis,1-3 months)•Encephalomyelitis (ataxia, memorydisturbances, fatigue, progressivepyramidal signs, disturbances <strong>of</strong> bladderfunctions, neuritis retrobulbaris, peripheralneuritis, tetraparesis, dementia)MRI: focal white matter lesionsCSF: OBDg: Based on clinical picture + serologyTh:Prolonged course with high doses <strong>of</strong>antibiotics (Doxycyclin,Penicillin,Rocephin )
NEUROLOGICAL COMPLICATIONS OFAIDS1. DISEASES WITH DIRECT RELATIONSTO HIV-1•Meningitis (acute, or chronic form)•Encephalopatia (= AIDS-dementiacomplex)•Myelopathy•Neuropathy -symmetric polyneuropathy-mononeuritis multiplex•Myopathy (direct or due to treatment)2. SECONDARY COMPLICATIONS•Opportunistic infections (CMV; Toxopl.,Cryptococcus, PML, HSV, TBC)•Neoplasms (lymphoma, metastases, etc)•Cerebrovascular diseases (vasculitis)•Metabolic disorders (Wernicke, vitamindeficyency)
HIV