Acute Upper Gastrointestinal (UGI) Bleed - Wirral University ...
Acute Upper Gastrointestinal (UGI) Bleed - Wirral University ...
Acute Upper Gastrointestinal (UGI) Bleed - Wirral University ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
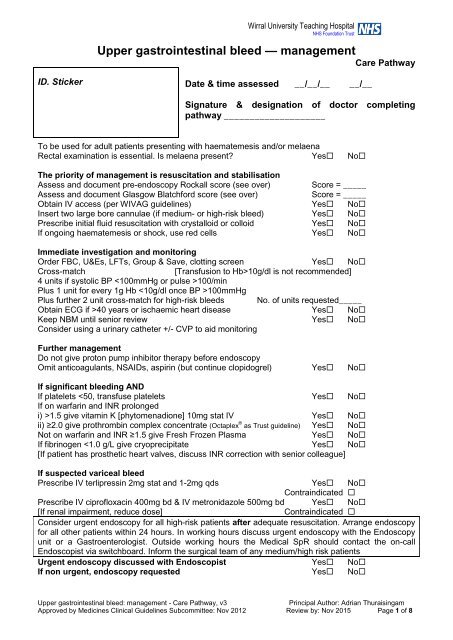
<strong>Wirral</strong> <strong>University</strong> Teaching HospitalNHS Foundation Trust<strong>Upper</strong> gastrointestinal bleed — managementCare PathwayID. StickerDate & time assessed __/__/__ __/__Signature & designation of doctor completingpathway ____________________To be used for adult patients presenting with haematemesis and/or melaenaRectal examination is essential. Is melaena present? Yes NoThe priority of management is resuscitation and stabilisationAssess and document pre-endoscopy Rockall score (see over) Score = _____Assess and document Glasgow Blatchford score (see over)Score = _____Obtain IV access (per WIVAG guidelines) Yes NoInsert two large bore cannulae (if medium- or high-risk bleed) Yes NoPrescribe initial fluid resuscitation with crystalloid or colloid Yes NoIf ongoing haematemesis or shock, use red cells Yes NoImmediate investigation and monitoringOrder FBC, U&Es, LFTs, Group & Save, clotting screen Yes NoCross-match[Transfusion to Hb>10g/dl is not recommended]4 units if systolic BP 100/minPlus 1 unit for every 1g Hb 100mmHgPlus further 2 unit cross-match for high-risk bleeds No. of units requested_____Obtain ECG if >40 years or ischaemic heart disease Yes NoKeep NBM until senior review Yes NoConsider using a urinary catheter +/- CVP to aid monitoringFurther managementDo not give proton pump inhibitor therapy before endoscopyOmit anticoagulants, NSAIDs, aspirin (but continue clopidogrel) Yes NoIf significant bleeding ANDIf platelets 1.5 give vitamin K [phytomenadione] 10mg stat IV Yes Noii) ≥2.0 give prothrombin complex concentrate (Octaplex ® as Trust guideline) Yes NoNot on warfarin and INR ≥1.5 give Fresh Frozen Plasma Yes NoIf fibrinogen
PRE-ENDOSCOPY Rockall ScoreAdd age + shock + co-morbidity (full score requires endoscopy)AgeScorePredicted mortality80 years 2 0 0.2%RiskShock Score 1 2.4% LowNone 0 2 5.6%*Pulse>100 + syst BP > 100 1 3 11.0% MediumSystolic BP 2: Admit to ward 34 (bleed bay if available). Consider HDUIf Pre-Rockall Score ≤ 2: Admit to medical ward (34 if bed available)Glasgow Blatchford ScoreAdd urea + haemoglobin + systolic BP + other markersBlood urea (mmol/L) Score Systolic BP (mmHg) Score
Post-endoscopy managementCalculate Full Rockall score (post endoscopy)Endoscopic diagnosis Score Full Rockall score Predicted mortalityNo lesion or Mallory Weiss tear 0 7 41.1%Follow the management plan determined by the EndoscopistFurther transfusion & correction of clotting abnormalities may be required. Close monitoringand correction of haemodynamic status is required post endoscopy. FBC, clotting and U&Esneed at least daily monitoring if there has been significant bleeding or if there has been largevolume transfusion of blood components.Non-variceal bleedingFollowing endoscopic therapy for non-variceal bleeding patients should be treated by an IVPPI infusion (Hong Kong regimen).Pantoprazole 80mg in 100ml 0.9% sodium chloride over 15 minutes thenPantoprazole 80mg in 250ml 0.9% sodium chloride at 8mg/hr infusion for 72 hoursContinue low-dose aspirin for secondary prevention of vascular events in patients in whomhaemostasis has been achieved. Stop other NSAIDs (including COX-2 inhibitors) during theacute phase. Discuss the risks and benefits of continuing clopidogrel (or any otherthienopyridine antiplatelet agents) with the appropriate specialist (e.g. a cardiologist or astroke specialist) and with the patient.Any evidence of rebleeding should prompt discussion with an Endoscopist. Repeatendoscopy, interventional radiology or surgery may be appropriate for unstable patients whore-bleed after endoscopic treatment. Refer urgently for surgery if interventional radiology isnot promptly available.Variceal bleedingFollowing endoscopy for variceal bleeding, stop IV terlipressin after definitive haemostasishas been achieved or after 5 days. [NICE advise that informed consent for off-label use ofterlipressin (>72 hours) should be obtained and documented.]Continue antibiotics for 1 week. IV ciprofloxacin and metronidazole can be stepped down tooral ciprofloxacin and metronidazole when able to eat.Consider arranging transjugular intrahepatic portosystemic shunts (TIPS) if bleeding fromoesophageal varices is not controlled by band ligation.ReferenceNICE CG 141. <strong>Acute</strong> upper gastrointestinal bleeding: management. June 2012<strong>Upper</strong> gastrointestinal bleed: management - Care Pathway, v3Principal Author: Adrian ThuraisingamApproved by Medicines Clinical Guidelines Subcommittee: Nov 2012 Review by: Nov 2015 Page 3 of 8
Appendix 1Discharge plan for minor upper gastrointestinaI bleeds*Glasgow Blatchford Score = 0Accompanied at home?Has access to transport?Has Telephone?NOADMITYESAnother indication for admission?On warfarin or other oral anticoagulant?Known to have previous varices?Has pacemaker or implantable cardiacdefibrillator?YESADMITNOClinical decision “Is patient suitable foroutpatient gastroscopy?”NOADMITYESComplete “Ambulatory Gastroscopy Request” formWrite contact telephone number on request formGive patient <strong>UGI</strong> bleed, ambulatory gastroscopy &gastroscopy patient information leafletsStop aspirin and NSAIDsAdvise patient to return if passing black tarry stool or faintingKeep NBM from midnight next dayDeliver request form to Endoscopy clerk (out of hours placein Endoscopy “Red Box” [outside Endoscopy reception])Arrange for case-notes to be delivered to the Endoscopy Unitby the AMAU ANPDISCHARGEPost-endoscopy managementA copy of the Endoscopy report will be sent to referring ConsultantIf normal/nil significant, patient will be discharged back to GPIf a repeat gastroscopy is required this will be arranged by EndoscopyIf readmission is required, following Endoscopy, the Endoscopy unit will arrange thisvia bed bureau and inform the Medical Registrar (bleep 2770). Patients will usually bereadmitted via AMAU.Any histology results from Endoscopy are the responsibility of the referring Consultantand will be sent to them as normal.<strong>Upper</strong> gastrointestinal bleed: management - Care Pathway, v3Principal Author: Adrian ThuraisingamApproved by Medicines Clinical Guidelines Subcommittee: Nov 2012 Review by: Nov 2015 Page 4 of 8
Ambulatory Gastroscopy Requestfor minor upper GI bleeds only<strong>Wirral</strong> <strong>University</strong> Teaching HospitalNHS TrustIncomplete forms will be returnedPATIENT DETAILSName:……………….…………………………………..…DOB:…….................Hospital Number:…………………Address:………………………………………..……………………………………………………..……..............................................Post Code:……….……...................... Phone Number:……………………..………................<strong>Upper</strong> GI bleed meeting all following criteriaUrea < 6.5 mmol/LHaemoglobin ≥ 130 g/L (Male)or ≥ 120 g/L (Female)Systolic blood pressure ≥ 110 mm HgPulse < 100 beats per minAbsence of:i. Melaenaii. Syncopeiii. Cardiac failureiv. Liver diseaseConsultant:…………………………...……………………Dr. completing form:……………..……………………….Bleep:………………..Date:……………………………….Leave in Endoscopy Red Box/ReceptionEnsure patient is accompanied at home, hasaccess to a telephone and transportKeep NBM from midnight on next working dayGiven patient information leafletStop aspirin/NSAIDSAdvised to return if black tarry stool or faintingExclusionsPatients on warfarin/dabigatran/LMWHPatients with pacemaker or implantable cardiacdefibrillatorPatients requiring hospital admission for any otherreasonPatients with previous varicesFurther information :……………………………..……………………………………………………………………….……………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………………Follow up Arrangements :Comorbidities (give details)Diabetic Yes/No Diet/Tablet/InsulinHeart disease Yes/No…………………………….Resp diseaseYes/No…………………………….MedicationsIronYes/NoClopidogrel*** Yes/No***Can they be stopped? Yes/No*** When?..................................PPIYes/NoBloods(if available)Hb……………….MCV…………….Plts………………INR………………For Endoscopy Use:Date received …../…../….. Date vetted by Endoscopist …../…../….. Vetted by …………Form complete Yes/No Date of appointment …../…../….. Date letter sent …../…../…..<strong>Upper</strong> gastrointestinal bleed: management - Care Pathway, v3Principal Author: Adrian ThuraisingamApproved by Medicines Clinical Guidelines Subcommittee: Nov 2012 Review by: Nov 2015 Page 5 of 8
Patient Information leafletAmbulatory gastroscopy for upper gastrointestinal bleedingThe clinical assessment and tests we have performed indicate that the bleeding from yourstomach is minor. From previous experience we feel it is best if your case is now managedon an out patient basis and we will now allow you to go home.You have been discharged home with a plan to have a gastroscopy (camera test of thestomach) within 24 hours. This will take place in the Endoscopy Unit, which is situated on the3 rd floor of Arrowe Park Hospital. The Endoscopy Unit should contact you to confirm a time toattend for your gastroscopy (Please note that the Endoscopy unit may appear on yourtelephone as number blocked or withheld). If you have not been contacted by 10.00amtomorrow please contact the Endoscopy unit on 0151 604 7095.PLEASE NOTE THE FOLLOWINGYou must NOT eat or drink anything from midnight the night before your gastroscopy.Stop taking any aspirin or anti-inflammatory drugs, until you are advised otherwise.No alcohol between now and your gastroscopy.<strong>Wirral</strong> <strong>University</strong> Teaching HospitalNHS Foundation TrustIf you are diabetic, do NOT take your normal insulin or diabetes tablets on the morning ofyour gastroscopy.Please bring a list of your normal medication with you when you come for your gastroscopy.If you experience black tarry stool or fainting prior to this appointment it is very important thatyou come back to hospital immediately.If you choose to have sedation for your gastroscopy. it is essential that there is someone whocan take you home afterwards and stay with you for 24 hours.<strong>Upper</strong> gastrointestinal bleed: management - Care Pathway, v3Principal Author: Adrian ThuraisingamApproved by Medicines Clinical Guidelines Subcommittee: Nov 2012 Review by: Nov 2015 Page 6 of 8
Patient Information leafletGastroscopy & therapy for upper gastrointestinal bleedingThe medical team think that you may be bleeding from your oesophagus (gullet), stomach orduodenum (top part of the intestine). There are many causes for bleeding from these areas ofthe body. Depending on the findings at gastroscopy, treatment may be needed to treat orhelp prevent further bleeding.Treatment can include all or any of the following:1) Injection of adrenaline2) Placement of endoscopic clips3) Thermocoagulation with gold probe4) Argon plasma coagulationAll of the above 4 treatments are usually used to treat bleeding from ulcers or any abnormalblood vessels5) Endoscopic banding or injection of varices<strong>Wirral</strong> <strong>University</strong> Teaching HospitalNHS Foundation TrustInjection of adrenalineAn injection needle is passed down the gastroscope once it is in position. Adrenaline isinjected into and/or around a recent or active bleeding point.Placement of endoscopic clipsSmall metal clips are passed down the gastroscope once it is in position. The clips are placedonto and/or around a recent or active bleeding point.Thermocoagulation with gold probeA small probe is passed down the gastroscope once it is in position. The probe is placed ontoand/or around a recent or active bleeding point. The tip of the probe is heated to a hightemperature to help flatten and seal any blood vessels.Argon plasma coagulationA small probe is passed down the gastroscope once it is in position. The probe is placedclose to a possible bleeding point. The tip of the probe fires argon gas which is then heatedto a high temperature to help heat seal any blood vesselsUncommon risks and complications:Injection of adrenaline, placement of endoscopic clips, thermocoagulation with gold probeand argon plasma coagulation are all safe procedures with a low risk of complications, butoccasionally the following can occur:Patients may experience pain particularly after adrenaline injection. This is usuallyshort lasting.The whole purpose of the procedure is to prevent or treat serious bleeding.Occasionally the procedure itself can cause bleeding. The risk is less than 5 in 100cases and it can usually be treated at the time of the gastroscopy procedure.A hole (perforation) in the oesophagus, stomach or duodenum can occur during theprocedure. If a hole is made, you will require further treatment which may includesurgery. The risk is between 0-2 in 100 cases.<strong>Upper</strong> gastrointestinal bleed: management - Care Pathway, v3Principal Author: Adrian ThuraisingamApproved by Medicines Clinical Guidelines Subcommittee: Nov 2012 Review by: Nov 2015 Page 7 of 8
If bleeding or perforation does occur this can be serious and these complications maysometimes result in death, but you are at greater risk of not having the treatment.These treatments have been proved to improve outcomes when needed and arerecommended by national guidelines.Endoscopic banding or injection of varicesVarices are large veins that appear in the oesophagus and stomach. These may burst andcause significant bleeding. If these veins bleed, they can make you vomit blood, (possibly inlarge quantity) and or pass dark, altered blood from your bottom. Therefore it is important totry to reduce or shrink varices and get rid of them, if at all possible.Treatment of oesophageal varicesTreatment of your varices during your gastroscopy can be done either by banding orsometimes by injecting them, but the method chosen will be decided by your doctor.Endoscopic banding (or variceal ligation)Banding of oesophageal varices involves placement of rubber bands over the varices at thetime of endoscopy. This is a method for treating oesophageal varices using a technique thathas also been used for the treatment of haemorrhoids (piles). Several treatments, on morethan one occasion, may be required to achieve complete shrinkage.Injection sclerotherapy of varicesThis procedure is carried out by using an injection needle which can be passed down thegastroscope once it is in position in the oesophagus (gullet). In order to completely shrink theveins several injections, on more than one occasion, may be necessary.Uncommon risks and complications:Banding and injection sclerotherapy are both safe procedures with a low frequency ofcomplications, but occasionally the following can occur:The banded or injected areas can become scarred, causing a narrowing in your gulletand discomfort when you swallow. The risk is less than 1 in 100.Occasionally small ulcers can form in the gullet where the banding or injections havebeen carried out. The risk is less than 5 in 100.The whole purpose of the procedure is to prevent or treat serious bleeding from thedistended veins. Occasionally the procedure itself can cause bleeding from varices.This can be as serious as bleeding from untreated varices. The risk is approximately 3in 100 cases. Once the course of banding is completed the risk of bleeding of any sortis greatly reduced.A hole (perforation) in the oesophagus can occur during the procedure. If a hole ismade, you will be admitted to hospital for further treatment which may include surgery.The risk is less than 1 in 100.If bleeding or perforation does occur this can be serious, as with any procedure, andthese complications may sometimes result in death, but you are at greater risk of nothaving the treatment.ReferencesComplications of <strong>Gastrointestinal</strong> Endoscopy. British Society of Gastroenterology guidelinesNov 2006.<strong>Upper</strong> gastrointestinal bleed: management - Care Pathway, v3Principal Author: Adrian ThuraisingamApproved by Medicines Clinical Guidelines Subcommittee: Nov 2012 Review by: Nov 2015 Page 8 of 8