NCEPOD: Trauma - Who Cares? - London Health Programmes
NCEPOD: Trauma - Who Cares? - London Health Programmes
NCEPOD: Trauma - Who Cares? - London Health Programmes
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
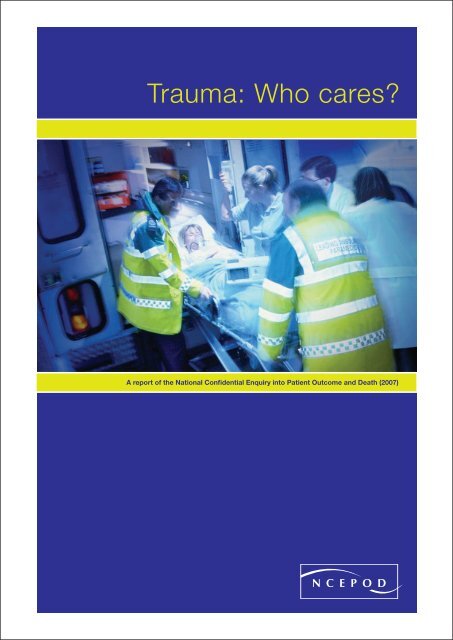
<strong>Trauma</strong>: <strong>Who</strong> cares?A report of the National Confidential Enquiry into Patient Outcome and Death (2007)
<strong>Trauma</strong>: <strong>Who</strong> cares?A report of the National Confidential Enquiry into Patient Outcome and Death (2007)Compiled by:G Findlay MB ChB FRCAI C Martin LLM FRCS FDSRCSS Carter MBBS FRCS FRCS(G) RCPSN Smith BSc PhDD Weyman BScM Mason PhD11
ContentsAcknowledgements 4Foreword 8Summary of findings 10Principal recommendations 12Introduction 14References 16Method 17Chapter 1 – Data overview 21Chapter 2 – Organisational data 25Key fi ndings 33Recommendations 33Chapter 3 – Overall assessment 34Key fi ndings 36Chapter 4 – Prehospital care 37Introduction 37Organisational aspects of care 37Clinical aspects of care 42Airway and ventilation 43Key fi ndings 48Recommendations 48References 49Chapter 5 – Hospital reception 50Introduction 50Results 50<strong>Trauma</strong> team response 51<strong>Trauma</strong> team response – individual cases 52Primary survey and overall assessment 59Key fi ndings 60Recommendations 61References 612
Chapter 6 – Airway and breathing 62Introduction 62Results 62Case study 1 68Key fi ndings 68Recommendations 68References 69Chapter 7 – Management of circulation 70Introduction 70Results 71Case study 2 72Case study 3 76Key fi ndings 81Recommendations 82References 82Chapter 8 – Head injury management 85Introduction 85Results 85Prehospital data 86Hospital data 91Case study 4 97Case study 5 104Key fi ndings 108Recommendations 109References 109Chapter 10 – Transfers 118Introduction 118Results 119Case study 6 123Case study 7 123Key fi ndings 124Recommendations 124References 125Chapter 11 – Incidence of traumaand organisation of trauma services 126Introduction 126Results 126Discussion 128Key fi ndings 131Recommendations 131References 132Appendix A – Glossary 133Appendix B – Injury severity score 134Appendix C – Adult and paediatricGlasgow Coma Scale 135Appendix D – An example of an excellentPatient Report Form (PRF) 138Chapter 9 – Paediatric care 112Organisational data 112Clinical data 114Key fi ndings 116Recommendations 116References 117Appendix E – Level 1 trauma care 140Appendix F – Participation 141Appendix G – Corporate structure 1483
AcknowledgementsThis is the twenty first report published by <strong>NCEPOD</strong> and, as always, could not have beenachieved without the support of a wide range of individuals and organisations.Our particular thanks go to:The Expert Group who advised <strong>NCEPOD</strong>:Dr B WinterConsultant in Adult Critical CareDr C CarneyChief Executive East Anglian Ambulance NHS TrustMr D GilroyConsultant General SurgeonMr K PorterConsultant Orthopaedic SurgeonProfessor P GiannoudisProfessor of <strong>Trauma</strong> and OrthopaedicsMr S Davies<strong>Trauma</strong> Nurse Co-ordinatorProfessor T CoatsProfessor of Emergency MedicineMr T PigottConsultant Spinal SurgeonMs E SymondsLay RepresentativeDr A GrayConsultant AnaesthetistDr A NicholsonConsultant Vascular Radiologist,Clinical Director of RadiologyDr I DoughtyConsultant PaediatricianThe Advisors who reviewed the cases:Dr A WilsonConsultant in Emergency MedicineMiss A Hutchings<strong>Trauma</strong> Nurse Specialist / <strong>Trauma</strong> Co-ordinatorDr A FeazeyConsultant in Emergency MedicineDr A BlackConsultant PaediatricianMiss A McGinleyConsultant NurseDr A SutcliffeConsultant in Intensive CareMr A ArmstrongConsultant Plastic SurgeonMr B WhiteConsultant Neurosurgeon4
AcknowledgementsDr C StevensonSpecialist Registrar in AnaesthesiaDr C GomezConsultant in Intensive CareDr C DeakinConsultant AnaesthetistDr D GardinerConsultant in Intensive CareDr D BrydenConsultant in Intensive CareMr D TeanbyConsultant Orthopaedic SurgeonDr D EsbergerConsultant in Emergency MedicineDr E AbrahamsonConsultant in Emergency MedicineMiss H CattermoleConsultant Orthopaedic SurgeonMr M PerryConsultant Oral and Maxillofacial SurgeonMr M McMonagleSpecialist Registrar in General SurgeryMr N TaiConsultant Vascular SurgeonDr O BagshawConsultant PaediatricianDr R LandauConsultant in Emergency MedicineDr R BanksSpecialist Registrar in Maxillofacial SurgeryMr S MarksConsultant NeurosurgeonDr S SmithConsultant in Emergency MedicineDr S LuneyConsultant AnaesthetistDr J BerridgeConsultant AnaesthetistMr K BrohiConsultant General SurgeonMajor M ButlerSpecialist Registrar in <strong>Trauma</strong> and Orthopaedics5
AcknowledgementsThe organisations that provided funding to cover thecost of this study:The professional organisations that support our workand who constitute our Steering Group:National Patient Safety AgencyDepartment of <strong>Health</strong>, Social Services and Public Safety(Northern Ireland)Aspen <strong>Health</strong>careBenenden HospitalBMI <strong>Health</strong>careBUPACapio GroupCovenant <strong>Health</strong>careCromwell HospitalIsle of Man <strong>Health</strong> and Social Security DepartmentFairfield Independent HospitalHCA InternationalHorder CentreHospital Management TrustHospital of St John and St ElizabethKing Edward VII HospitalKing Edward VIIs Hospital Sister Agnes<strong>London</strong> ClinicMcIndoe Surgical CentreMount Alvernia HospitalNetcare <strong>Health</strong>careNew Victoria HospitalNorth Wales Medical CentreNuffield HospitalsOrchard HospitalSt Anthony’s HospitalSt Joseph’s HospitalSpencer Wing, Queen Elizabeth theQueen Mother HospitalStates of Guernsey, <strong>Health</strong> and Social ServicesStates of Jersey, <strong>Health</strong> and Social ServicesUlster Independent ClinicAssociation of Anaesthetists of Great Britain and IrelandAssociation of Surgeons of Great Britain and IrelandCoroners’ Society of England and WalesFaculty of Dental Surgery of the Royal Collegeof Surgeons of EnglandFaculty of Public <strong>Health</strong> of the Royal Collegeof Physicians of the UKInstitute of <strong>Health</strong>care ManagementRoyal College of AnaesthetistsRoyal College of Child <strong>Health</strong> and PaediatricsRoyal College of General PractitionersRoyal College of NursingRoyal College of Obstetricians and GynaecologistsRoyal College of OphthalmologistsRoyal College of PathologistsRoyal College of Physicians of <strong>London</strong>Royal College of RadiologistsRoyal College of Surgeons of England6
AcknowledgementsThe authors and Trustees of <strong>NCEPOD</strong> wouldparticularly like to thank the <strong>NCEPOD</strong> staff for theirhard work in collecting and analysing the data forthis study:Robert Alleway, Sabah Begg, Philip Brown, HeatherCooper, Karen Protopapa, Sidhaarth Gobin, Clare Holtby,Dolores Jarman, Viki Pepper, and Saba Raza.In addition we thank our scientifi c advisors Dr Martin Utleyand Professor Steve Gallivan for all their assistance.DISCLAIMERThis work was undertaken by <strong>NCEPOD</strong>, which receivedfunding for this report from the National Patient SafetyAgency. The views expressed in this publication are thoseof the authors and not necessarily those of the Agency.7
ForewordSevere injury - a car crash, a fall froma height - accidents such as these arethe commonest causes of loss of life inthe young. The chance of survival andthe completeness of recovery are highlydependent on the care that follows. Someare killed outright but those who survivethe initial impact may still die in the hours,days or weeks that follow. The speedwith which lethal processes are identifiedand halted makes the difference betweenlife and death. The injury sets in trainlife threatening effects of injury on thecirculation, tissue oxygenation and thebrain. The sooner we can halt and reversethese processes, the more likely andcomplete will be the return to health.8
ForewordAs a junior in the emergency and neurosurgical departmentsin Cambridge in the early 1970s we were trained in theserather obvious principles. To use a current catch phrase - it’snot rocket science or another, nearer the point - it doesn’ttake a brain surgeon to work that out! And yet somehow theapparently obvious - or we might see it as “common sense”- was not so commonplace. Then in 1976 an orthopaedicsurgeon James Styner crashed his plane in Nebraska. Hiswife was dead and there he was in a fi eld with three of hisfour children critically injured. He fl agged down a car to getto the nearest hospital - which was closed. Once opened itbecame clear to him that the care available was inadequateand inappropriate.The minutes and fi rst hours after an accident are not thetime to be working out care from fi rst principles. We missthe obvious under pressure; we cannot hope to makeconsistently inspired diagnoses. It is not the time to benegotiating a hierarchy, debating priorities and searchingshelves and drawers for equipment. We need a well workedout process based on getting most things right and very fewthings wrong. Realising this, Styner started to work out asystem of care. From his initial efforts came Acute <strong>Trauma</strong>Life Support (ATLS) and with it a new philosophy of careof the severely injured patient based around well thoughtthrough processes and teams trained in them - all adheringto the same workshop manual.To be effective, all processes, including ATLS and othercomponents of care of severely injured patients, must beembedded in practice at every stage: the scene of theaccident; alerts to the hospital; the journey from the sceneto the emergency department; preparations made there;expertise accessible on arrival and at all subsequent stages,including transfer to specialist services. This <strong>NCEPOD</strong> reporthas studied how well we do - and where we sometimesfail. It is by sympathetically, and analytically, studying wherethings go wrong that we can learn most.Professor T. TreasureChairman9
Summary of fi ndingsThis study shows a rounded picture ofcurrent trauma care provision in England,Wales, Northern Ireland and the OffshoreIslands. It draws on data provided by theclinicians involved in the care of thesepatients (from questionnaires) and dataextracted from the casenotes. However,these data are accompanied by peerreview, by practising clinicians involved inthe day-to-day care of trauma patients, togive a much richer picture than a purelyquantitative assessment would allow.Almost 60% of the patients in this study received a standardof care that was less than good practice. Defi ciencies inboth organisational and clinical aspects of care occurredfrequently.There were diffi culties in identifying those patients with aninjury severity score (ISS) >16. With large costs involved inboth the provision of care and resources for the managementof these patients it is surprising that that there is no currentmethod of identifying the demand for the management ofthese patients.10
Summary of findingsThe organisation of prehospital care, the trauma teamresponse, seniority of staff involvement and immediate inhospitalcare was found to be defi cient in many cases.Lack of appreciation of severity of illness, of urgency ofclinical scenario and incorrect clinical decision making wereapparent. Many of these clinical issues were related to thelack of seniority and experience of the staff involved in theimmediate management of these patients.It was clear that the provision of suitably experienced staffduring evenings and nights was much lower than at othertimes. In the management of trauma, which very oftenpresents at night, this is a major concern. NHS Trustsshould be open about the differences in care by day andnight and look to address this as a matter of urgency. Publicawareness of these differences may be useful in any debateabout the future confi guration of trauma services.Severe trauma is not common and many hospitals see lessthan one severely injured patient per week. This has a directbearing on experience and ability to manage these challengingpatients. Not only does this relate to clinical skills but also tothe feasibility of providing the entire infrastructure required tomanage the trauma patient defi nitively in all centres.11
Principal recommendationsOrganisational dataThere is a need for designated Level 1 trauma centresand a verifi cation process needs to be developedto quality assure the delivery of trauma care (as hasbeen developed in the USA by the American Collegeof Surgeons). (Royal College of Surgeons of England,College of Emergency Medicine)Prehospital careAll agencies involved in trauma management, includingemergency medical services, should be integrated intothe clinical governance programmes of a regional traumaservice. (All healthcare providers)Airway management in trauma patients is oftenchallenging. The prehospital response for these patientsshould include someone with the skill to secure theairway, (including the use of rapid sequence intubation),and maintain adequate ventilation. (Ambulance andhospital trusts)Hospital receptionTrusts should ensure that a trauma team is available 24hours a day, seven days a week. This is an essential partof an organised trauma response system. (Hospital trusts)A consultant must be the team leader for the managementof the severely injured patient. There should be no reasonfor this not to happen during the normal working week.Trusts and consultants should work together to providejob plans that will lead to better consultant presence in theemergency department at all times to provide more uniformconsultant leadership for all severely injured patients.(Hospital trusts and clinical directors)12
Principal recommendationsAirway and breathingThe current structure of prehospital management isinsuffi cient to meet the needs of the severely injuredpatient. There is a high incidence of failed intubationand a high incidence of patients arriving at hospital witha partially or completely obstructed airway. Changeis urgently required to provide a system that reliablyprovides a clear airway with good oxygenation andcontrol of ventilation. This may be through the provisionof personnel with the ability to provide anaesthesiaand intubation in the prehospital phase or the use ofalternative airway devices. (Ambulance trusts)All patients with severe head injury should be transferredto a neurosurgical/critical care centre irrespective of therequirement for surgical intervention. (Strategic healthauthorities, hospital trusts, trauma team leaders)Paediatric careEach receiving unit should have up to date guidelines forchildren which recognise the paediatric skills available onsite and their limitations and include agreed guidelinesfor communication and transfer with specialisedpaediatric services within the local clinical network.(Strategic health authorities and hospital trusts)Management of circulation<strong>Trauma</strong> laparotomy is potentially extremely challengingand requires consultant presence within the operatingtheatre. (Clinical directors)If CT scanning is to be performed, all necessary imagesshould be obtained at the same time. Routine use of‘top to toe’ scanning is recommended in the adulttrauma patient if no indication for immediate interventionexists. (Royal College of Radiology and radiologydepartment heads)TransfersThere should be standardised transfer documentation ofthe patients’ details, injuries, results of investigations andmanagement with records kept at the dispatching andreceiving hospitals. (<strong>Trauma</strong> team leader, Departmentof <strong>Health</strong>)Published guidelines must be adhered to and audits performedof the transfers and protocols. (Hospital trusts)Head injury managementPatients with severe head injury should have a CT headscan of the head performed as soon as possible afteradmission and within one hour of arrival at hospital.(<strong>Trauma</strong> team leader and radiology heads)Incidence of trauma and organisationof trauma servicesGiven the relatively low incidence of severe traumain the UK, it is unlikely that each individual hospitalcan deliver optimum care to this challenging group ofpatients. Regional planning for the effective delivery oftrauma services is therefore essential. (Strategic healthauthorities, hospital trusts)13
Introduction<strong>Trauma</strong> remains the fourth leading cause of death in westerncountries and the leading cause of death in the fi rst fourdecades of life. The incidence of trauma is particularly highin the younger population; an average of 36 life years arelost per trauma death 1 . Furthermore, trauma is also a majorcause of debilitating long-term injuries. For each traumafatality there are two survivors with serious or permanentdisability 2 . <strong>Trauma</strong> is, therefore, not only a leading causeof death but also a large socio-economic burden. In 1998,the estimated cost to the NHS, of treating all injuries, was£1.2 billion per annum 3 . Reducing injuries is, therefore, a keygovernment objective. By 2010, the Department of <strong>Health</strong>aims to have reduced the incidence of accidents by at least20% from the baseline that was set in 1996 3 .Road trauma accounts for over a third of all deaths due toinjury 4 . In 2001-2003, there were (on average) 3,460 traffi crelated fatalities per annum in Great Britain 5 . The incidenceof severe trauma, defi ned as an Injury Severity Score (ISS) of16 or greater, is estimated to be four per million per week 6 .Given that the UK population in mid-2003 was in the regionof 59.5 million 7 , there are approximately 240 severely injuredpatients in the UK each week.In 1988, the working party report by the Royal College ofSurgeons of England highlighted ‘serious defi ciencies in themanagement of severely injured patients’ 8 . Following thisreport, there was increased focus on the care of traumapatients in the UK and consequently the fatality rate oftrauma patients reduced. However, most of the improvementin the outcome of these patients occurred prior to 1995, withno further signifi cant change occurring between 1994 and2000 9 .In 2000, a joint report from the Royal College of Surgeonsof England and the British Orthopaedic Associationrecommended that standards of care for the severelyinjured patient should be nationally co-ordinated and14
Introductionsystematically audited 6 . It was also recommended thatstandards and outcome measures be developed, againstwhich institutions can audit the outcome of treatment. Thestandards of care recommended in the report include theuse of advance warning systems by the ambulance service,the establishment of trauma teams, the involvement ofa senior anaesthetist from the outset and criteria for theactivation of the trauma team. The overall purpose of theserecommendations was to improve the care of severely injuredpatients in terms of reduced mortality and unnecessarymorbidity.A number of UK-based single and multi-centre studieshave addressed specifi c issues relating to the care oftrauma patients 10-15 . The use of ambulance crews to alerthospitals of severely injured patients, the effect of interhospitaltransfers and the determinants affecting outcomehave all been studied. One of the largest UK-based studieslooked at the treatment of neurosurgical trauma patients innon-neurosurgical units 16 . There has not, however, been anational study to examine the overall care of trauma patientsin the UK to date.Much of the research on trauma care in the UK has beencarried out using data from the <strong>Trauma</strong> Audit and ResearchNetwork (TARN), which was established in response tothe Royal College of Surgeons of England’s working partyreport. Approximately 50% of trauma receiving hospitalssubmit data to TARN 17 . The <strong>Trauma</strong> Network Database isnow an important source of epidemiological data and, in2000 it contained information on over 120,000 cases 18 . The<strong>Health</strong>care Commission is working with TARN to increaseparticipation from 50% to 100% of hospitals and to expandthe number of quantitative trauma audits. At a local level, thefeedback provided by TARN to individual hospitals highlights,amongst others, those cases in which patient outcomewas ‘unexpected’. This markedly aids internal audit and thereview of trauma cases by those multi-specialty clinicianswho were involved in the care of particular patients. Togetherwith national evaluations of trauma care, in particular headinjury, processes of trauma care are also analysed andprovide a factual basis for system review.A lack of continued improvement in outcome is coupledwith concern that the quality of care in hospital is not ofa consistently high standard across the UK, despite theavailability of guidelines that indicate referral pathways foroptimum triage, management and access to specialistcare 6,19,20 . Furthermore, owing to the incidence of severetrauma, hospitals are unlikely to treat more than one severelyinjured patient per week. It has been suggested, therefore,that as suffi cient trauma experience cannot be achieved atall hospitals, optimal outcomes may be compromised. Oneof the overall recommendations of the 2000 report was theestablishment of a National <strong>Trauma</strong> Service trauma hub andspoke network between hospitals in each geographic area 6 .The organisation of trauma services in the UK remainshighly topical. The recent report from The Royal Collegeof Surgeons of England (2006) 6 confi rms that high qualitytrauma care is not consistently available within the NHS.Recent public debate and government statements refl ectthe continuing controversies regarding the optimum systemof delivering trauma services within the present resourceconstraints 21 . This study is therefore timely as it exploresthe organisation in trauma services from the perspectiveof the patient journey. <strong>NCEPOD</strong> have identifi ed remediablefactors and made recommendations for improvement in themanagement of the severely injured patient.The Royal College of Surgeons of England <strong>Trauma</strong>Committee proposed this study as part of <strong>NCEPOD</strong>’s topicselection process in February 2004. The <strong>NCEPOD</strong> SteeringGroup selected the topic, which falls under <strong>NCEPOD</strong>’sextended remit.15
IntroductionReferences1. Chaira 0, Cimbanissi S. Organized trauma care: doesvolume matter and do trauma centers save lives?Curr Opin Crit Care 2003; 9:510-42. http://www. tarn.ac.uk/content/images/53/overview%2006.pdf3. Our <strong>Health</strong>ier Nation – A contract for <strong>Health</strong>. Departmentof <strong>Health</strong>, 19984. The Royal College of Surgeons of England and the BritishOrthopaedic Society. Better Care for the Severely Injured.20005. Department for Transport, Table 33, Casualties: by age,road user type and severity: 2001, 2002 and 20036. Gorman DF, Teanby DN, Sinha MP, Wotherspoon J, BootDA, Molokhia A. The epidemiology of major injuries inMersey and North Wales. Injury 1995; 26(1):51-47. Offi ce for National Statistics http://www.statistics.gov.uk/8. Report of the working party on the management ofpatients with major injury. Royal College of Surgeons ofEngland, <strong>London</strong>. 19889. Lecky FE, Woodford M, Bouamra O, Yates DW, on behalfof the <strong>Trauma</strong> Audit and Research Network. Lack ofchange in trauma care in England and Wales since 1994.Emerg Med J 2002; 19:520-310. Crystal R, Bleetman A, Steyn R. Ambulance crewassessment of trauma severity and alertingpractice for trauma patients brought to ageneral hospital. Resuscitation 2004; 60:279-8211. Oakley PA, MacKenzie G, Templeton J, Cook AL, KirbyRM. Longitudinal trends in trauma mortality andsurvival in Stoke-on-Trent 1992-1998. Injury 2004;35:379-8512. McGinn GH, MacKenzie RE, Donnelly JA, Smith EA,Runcie CJ. Interhospital transfer of the criticallyill trauma patient: the potential role of a specialisttransport system. J Accid Emerg Med 1996; 13:90-213. Cooke RS, McNicholl BP, Byrnes DP. Earlymanagement of severe head injury in Northern Ireland.Injury 1995; 26(6):395-714. Lloyd DA, Patterson M, Robson J, Phillips B.A stratifi ed response system for the emergencymanagement of the severely injured. Ann R Coll SurgEngl 2001; 83:15-2015. Clayton TJ, Nelson RJ, Manara AR. Reduction inmortality from severe head injury following introductionof a protocol for intensive care management.British Journal of Anaesthesia 2004; 93(6):761-716. McKeating EG, Andrews PJD, Tocher JI, Menon DK.The intensive care of severe head injury: a survey of nonneurosurgicalcentres in the United Kingdom.British Journal of Neurosurgery 1998; 12(1):7-1417. Lecky F, Woodford M, Yates DW. Trends in traumacare in England and Wales 1989-1997. Lancet 2000;355:1771-518. The First Decade 1990-2000. <strong>Trauma</strong> Audit andResearch Network, 200019. Report of the Working Party on the Managementof Patients with Head Injuries. Royal College of Surgeonsof England, <strong>London</strong>. 199920. Triage, assessment, investigation and earlymanagement of head injury in infants, childrenand adults: NICE guidelines, 200321. Darzi A. Framework for Action. 2007.http://www.healthcareforlondon.nhs.uk/framework_for_ action.asp16
MethodMethodStudy aimThe aim of this study was to examine the process of care forseverely injured patients and identify variations that affect theachievement of agreed endpoints.The expert group identifi ed six main thematic areasthat would address the overall aim of the study:1. Timeliness of events making up the clinicalmanagement process.2. Issues associated with prehospital care at the siteof injury and transfer to hospital.3. Issues associated with the care team that performsthe initial resuscitation.4. Processes and procedures associated withsecondary transfers.5. Issues associated with pathways, handoversand communication.6. Membership of the <strong>Trauma</strong> Audit Research Network(TARN).Expert groupA multidisciplinary group of experts comprising cliniciansfrom emergency medicine, general surgery, neurosurgery,radiology, anaesthetics, and lay representatives contributedto the design of the study and reviewed the combinedanalysis of the data; both from the questionnaires and theextra information from the advisory groups.Case identificationPatients were identifi ed prospectively. A nominated contactin the emergency department identifi ed patients as severelyinjured based primarily on their, and their colleagues’, clinicaljudgement. A list of patients (which included a patientidentifi er and the date and time of admission) was thenforwarded to the <strong>NCEPOD</strong> local reporter who completed amonthly spreadsheet which contained additional information(for example, the name of the admitting clinician). Datacollection ran for three months from February 1st 2006to April 30th 2006. Patients of all ages were eligible forinclusion. After each month of sampling, a spreadsheetwas returned, password-protected, to <strong>NCEPOD</strong> along withphotocopies of all of the casenotes for the fi rst 72 hoursin hospital. The casenotes were used by <strong>NCEPOD</strong> staffto calculate an injury severity score (ISS) for each patient(see Appendix B). Patients with an ISS of 16 or more wereincluded in the study. The casenotes of included patientswere subsequently used for the peer review process.ExclusionsThe following patient groups were excluded:• Death by hanging or drowning (the pathology isasphyxia rather than trauma); and• Patients brought in for confirmation of death.17
MethodQuestionnaires and casenotesThere were three questionnaires used to collect data forthis study, two clinical questionnaires per patient and oneorganisational questionnaire per site.1. A&E clinician questionnaireThis questionnaire was sent to the A&E clinician in charge ofthe patient’s initial resuscitation. Information was requestedconcerning the mode and time of arrival, initial traumaresponse, timeliness of investigations and hospital transfers.2. Admitting consultant questionnaireThis questionnaire concerned information on the locationand consultant specialty to which the patient was admitted.It also contained information on surgical procedures, patientoutcome and secondary transfers.3. Organisational questionnaireThis questionnaire concerned data on the staff, departments,facilities and protocols for each participating hospital.Information was collected at the hospital level as it gave abetter indication of the facilities available for a patient at thelocation where they were receiving care, rather than all thefacilities available within the trust as a whole.The organisational questionnaire was sent to the medicaldirector for completion. If, after a reminder, it was notreturned to <strong>NCEPOD</strong> a copy was sent to the <strong>NCEPOD</strong> localreporter of that hospital. Clinical questionnaires were eithersent to the <strong>NCEPOD</strong> local reporter for dissemination ordirectly to the clinician involved, depending on the choice ofthe hospital local reporter. However, whichever method wasused, it was requested that the completed questionnaireswere returned directly to <strong>NCEPOD</strong>.It had been hoped at the outset of the study that, in additionto these questionnaires, some information not otherwiseavailable regarding the prehospital management of patientscould be obtained from a questionnaire completed byambulance crews. However, it proved diffi cult to agree thiswith ambulance services, partly due to employment contractissues and partly due to reorganisation of ambulance trusts.Therefore, assessment of prehospital care has been acquiredfrom:a) The patient report form (PRF); completed by ambulancecrews at the scene and en route, a copy of which shouldbe available in the medical records.b) Advisors’ assessments of the prehospital care followingreview of both the PRF and clinical records andquestionnaires completed by the clinicians relatingto hospital management.To complement the data available from the abovequestionnaires, copies of all the casenotes for patients’fi rst 72 hours in hospital were requested. If the patient wastransferred within 72 hours, the casenotes from the receivinghospital were also requested.Advisor groupA multidisciplinary group of advisors was recruited to reviewthe casenotes and associated questionnaires. The group ofadvisors comprised clinicians from the following specialties:emergency medicine, anaesthetics, general surgery, intensivecare medicine, maxillofacial surgery, neurosurgery, nursing,paediatrics, plastics, orthopaedics and vascular surgery.For each case reviewed, the advisor completed anassessment form. This allowed both quantitative andqualitative analysis of the advisor’s opinion.18
MethodSpecifi c sections of the assessment form were completedby <strong>NCEPOD</strong> researchers using information extracted fromthe casenotes such as the times of investigations, Airway,Breathing, Circulation (ABC) measurements and the gradesof doctors involved in the patients’ care. The remainder ofthe assessment form was completed by the advisors whowere asked to provide expert opinion on the prehospitalcare, trauma response, timeliness of investigations and theoverall care of the patient.Peer review processAll questionnaires and casenotes were anonymised bythe non-clinical staff at <strong>NCEPOD</strong>. All patient, clinician andhospital identifi ers were removed. Neither clinical staff at<strong>NCEPOD</strong>, nor the advisors had access to any identifi ableinformation.After being anonymised each case was reviewed by oneadvisor within a multidisciplinary group. At regular intervalsthroughout the meeting, the chair allowed a period ofdiscussion for each advisor to summarise their cases andask for opinions from other specialties or raise aspects of acase for discussion.Good practice:A standard that you would accept from yourself, yourtrainees and your institution.Room for improvement:Aspects of clinical care that could have been better.Room for improvement:Aspects of organisational care that could have beenbetter.Room for improvement:Aspects of both clinical and organisational care thatcould have been better.Less than satisfactory:Several aspects of clinical and/or organisationalcare that were well below that you would accept fromyourself, your trainees and your institution.Insuffi cient information submitted to assess thequality of care.The grading system below was used by the advisors tograde the overall care each patient received.19
MethodQuality and confidentialityA number of predetermined, mandatory key fi elds on eachquestionnaire had been set to ensure that data analysiscould be performed effectively. If these key fi elds were notcompleted on receipt of the questionnaire by <strong>NCEPOD</strong>, the<strong>NCEPOD</strong> local reporter or clinician was contacted to see ifthe data could be obtained.Each case was given a unique <strong>NCEPOD</strong> number so thatcases could not easily be linked to a hospital.The data from all questionnaires received were electronicallyscanned into a preset database. Prior to any analysis takingplace, the data were cleaned to ensure that there were noduplicate records and that erroneous data had not beenentered during scanning. Any fi elds that contained spuriousdata that could not be validated were removed.Data analysisFollowing cleaning of the quantitative data, descriptivestatistics were produced.The qualitative data collected from the assessment form andfree text answers in the clinical questionnaires were codedaccording to content and context. The data were reviewedby <strong>NCEPOD</strong> clinical staff to identify the nature and frequencyof recurring themes.Case studies have been used throughout this report toillustrate particular themes.All data were analysed using Microsoft Access and Excel bythe staff at <strong>NCEPOD</strong>.The fi ndings of the report were reviewed by the expertgroup, advisors and the <strong>NCEPOD</strong> steering group prior topublication.20
1Data overviewCHAPTER 1 - Data overviewHospital participationAn organisational questionnaire was completed for 183/218(83.9%) hospitals, that were expected to participate.Patient identifier spreadsheetsA patient identifi er spreadsheet was returned for 180/218(82.6%) hospitals that were expected to participate. In totalthis equated to 2203 patients, for which <strong>NCEPOD</strong> received1735 (78.8%) sets of casenotes to calculate an injury severityscore (ISS). Of these 909 cases had an ISS less than 16 and826 patients had an ISS ≥ 16, 31 of which were excludedas they were either dead on arrival, had complications of aprevious injury or there was insuffi cient information for theadvisors to assess any aspect of the patient’s care. Theremaining 795 patients were included in the study sample.Clinician questionnairesThe study was designed such that the overwhelming majorityof the quantitative and qualitative data could be obtaineddirectly from the casenotes and the focussed opinionsof the advisors’ (i.e. from the advisor assessment form).To supplement this, the clinician responsible for the initialresuscitation of the patient and the admitting consultant(if applicable) were asked to complete a patient carequestionnaire. In total 513 A&E clinician questionnaires and432 admitting consultant questionnaires were returned.Age and genderSeventy fi ve percent (594/795) of the patients were males,and the mean age of the whole sample was 39.6 years. Themode age of the study sample was 18; one in six (128/795)patients being 16 – 20 years old (Figure 1).Figure 1. Age range of patient sample140120Number of patients1008060402000 -56 -1011 -1516 -2021 -2526 -3031 -3536 -4041 -4546 -5051 -55Age (years)56 -6061 -6566 -7071 -7576 -8081 -8586 -9091 -9521
CHAPTER 1 - Data overviewFigure 2. Age range of patient sample by gender100Number of patients908070605040302010MaleFemale00 -56 -1011 -1516 -2021 -2526 -3031 -3536 -4041 -4546 -5051 -55Age (years)56 -6061 -6566 -7071 -7576 -8081 -8586 -9091 -95Figure 2 shows the age range analysed by gender. The meanage for males was 38 and mean age for females 44. Therewas a peak in frequency for males aged 16-25.Of the patients in the study 56.3% (442/785) were involved ina road traffi c collision (RTC) (Table 1).Table 1. Mechanism of injuryNumber of patients %RTC (driver/passenger) 319 40.6RTC (pedestrian) 123 15.7Fall from height 136 17.3Assault 72 9.2Industrial/agricultural 21 2.7Sport/leisure 18 2.3Self harm 15 1.9Other 81 10.3Subtotal 785Not recorded 10Total 795Day and time of arrivalThe number of severely injured patients presenting to theemergency department peaked on Friday and Saturday(Figure 3).The rise in number of patients on Friday and Saturday waslargely due to an increase in patients arriving at night (‘outof hours’) at the weekend (see Table 2). Daytime admissionswere largely constant and were actually lower than theweekly average on Friday and Saturday. The mean age of thepatients who presented out of hours on Friday, Saturday andSunday was considerably lower than the remainder of thepopulation: 33.5 years compared to 42.3 years.22
1Data overviewFigure 3. Patient arrivals by day of weekNumber of patients160140120100806040200MON TUE WED THU FRI SAT SUN NotrecordedDayTable 2. Patient arrivals by time of day and day of weekDay 08.00-17.59 Night 18.00-07.59% %SubtotalTime of daynot recordedMon 41 47.1 46 52.9 87 2 89Tue 56 63.6 32 36.4 88 3 91Wed 59 53.6 51 46.4 110 1 111Thu 54 49.1 56 50.9 110 0 110Fri 50 44.6 72 59.0 122 4 126Sat 46 32.2 97 67.8 143 4 147Sun 38 36.9 65 63.1 103 13 116Subtotal 344 419 763 27 790Day not recorded 0 0 0 5 5Total 344 419 763 32 795Total23
CHAPTER 1 - Data overviewMode of arrivalTable 3. Mode of arrival to hospitalNumber of patients %Ambulance 652 83.3Helicopter 92 11.7Other emergency service 5
2Organisational dataCHAPTER 2 - Organisational dataThis chapter summarises the collated data from the183 hospitals that returned a completed organisationalquestionnaire. It provides the reader with an overview of thedepartments, facilities, staff and protocols that were availablefor the care of severely injured patients during the studyperiod.Departments and proceduresTable 7 summarises the departments and/or proceduresthat were available at the participating hospitals. It shouldbe noted that some hospitals without a specifi c departmente.g. vascular surgery, did have staff that were able to performsurgical procedures related to that specialty.The most striking, albeit well known fact, was the smallnumber of hospitals that had a neurosurgery department(31) or performed neurosurgical procedures (a furtherseven hospitals). This is of particular concern given thelarge number of severely injured patients who sufferedneurotrauma as part of their constellation of injuries (over60% of patients in this study). The availability in patientservices is also refl ected in the Transfer chapter later in thisreport. By far the most common reason for a secondarytransfer was the requirement for neurosurgery and/orneurological monitoring. Time to defi nitive neurosurgicalintervention can be a major determinant of outcome forpatients with traumatic brain injury and the requirementfor a secondary transfer to access neurosurgical serviceslengthens this time (see Time to surgery page 106).More than half of the patients in the current study presentedto the emergency department out of hours. Furthermore,many required immediate treatment. While in the largemajority of hospitals procedures were available fororthopaedic trauma (168/173) and general surgery (166/173)out of hours, immediate intervention for more specialisedinjuries was often not available.Table 7. Overview of departments and proceduresDepartmenton siteDepartment not on site butspecialty procedures availableSubtotalNotansweredTotalYes Yes NoOrthopaedic trauma 166 7 9 182 1 183Neurosurgery 31 7 132 170 13 183General surgery 173 2 7 182 1 183Vascular surgery 131 15 33 179 4 183Plastic surgery 44 30 98 172 11 183Cardiac surgery 28 7 136 171 12 183Thoracic surgery 31 24 115 170 13 183Maxillofacial surgery 111 13 53 177 6 183ENT 137 14 28 179 4 183Urology 153 13 15 181 2 183Vascular interventional radiology 108 19 47 174 9 18325
CHAPTER 2 - Organisational dataTable 8. Availability of multiple 24 hour treatmentEmergencydepartmentEmergencydepartmentGeneralsurgeryEmergencydepartmentGeneralsurgeryOrthopaedictraumaEmergencydepartmentGeneralsurgeryOrthopaedictraumaVascularsurgeryEmergencydepartmentGeneralsurgeryOrthopaedictraumaVascularsurgeryNeurosurgeryEmergencydepartmentGeneralsurgeryOrthopaedictraumaVascularsurgeryCardiac orThoracicsurgery183 166 159 90 23 33 17EmergencydepartmentGeneralsurgeryOrthopaedictraumaVascularsurgeryNeurosurgeryCardiac orThoracicsurgeryTable 9. X-ray with immediate reporting by proximity to emergency department and 24 hour accessibility24 hour accessibilityProximity Yes No Subtotal Not answered TotalAdjacent 112 25 137 9 146Onsite not adjacent 15 7 22 1 23Offsite 0 2 2 0 2Subtotal 127 34 161 10 171Not answered 2 4 6 6 12Total 129 38 167 16 183The availability of multiple specialty treatment was furtheranalysed. It is clear from Table 8 that regional planning oftrauma services should consider the availability of servicesat each hospital and consider whether it is appropriate totake some severely injured patients to hospitals without afull range of services, available at all times. Only 17 hospitalsthat participated in this study could have been considered forLevel 1 verifi cation as a <strong>Trauma</strong> Centre (see Appendix E).Twenty four hour accessibility was defi ned as a facility whichcan be fully staffed and functional when required anytime ofday or night. Thirty four hospitals reported that they did nothave x-ray with immediate reporting meeting this defi nition(Table 9). Such a fundamental facility should be available atall times at every hospital that has the potential to receive aseverely injured patient.Whilst 161/169 (95.3%) hospitals had CT scanning thatmet the 24 hour defi nition, only 97/169 (57.4%) had thescanners located adjacent to the emergency department26
2Organisational dataTable 10. CT scanner and access to immediate reporting; proximity to emergency departmentand 24 hour accessibility24 hour accessibilityProximity Yes No Subtotal Not answered TotalAdjacent 93 4 97 6 103Onsite not adjacent 68 4 72 4 76Subtotal 161 8 169 10 179Not answered 2 0 2 2 4Total 163 8 171 12 183(Table 10). Since the risk to a patient’s stability is increasedduring movement, close proximity of the CT scanner to thepatient in the emergency department is of huge importance.It should be noted that advisors and clinicians completingquestionnaires frequently indicated that a patient could notbe scanned because of their instability. It is likely that thisscenario could be improved by the relocation of CT scannersinto the resuscitation room.In accordance with The Royal College of Radiologists’technical standards for CT 1 there appears to have been afairly good investment in CT scanner technology, as 117/145(80.7%) hospitals that answered the question reportedhaving a scanner less than six years old (Table 11). Theremaining 28 hospitals should consider updating their CTscanner in line with newer technology.Table 12 demonstrates excellent access to a blood bankfrom emergency departments.Table 11. Age of CT scanners (years)Number of hospitals %0 11 7.61 28 19.32 21 14.53 13 9.04 21 14.55 23 15.96 10 6.97 8 5.58 3 2.19 5 4.910 2 1.4Subtotal 145Not answered 38Total 183Table 12. Blood bank location and 24 hour accessibility24 hour accessibilityProximity Yes No Subtotal Not answered TotalAdjacent 19 0 19 3 22Onsite not adjacent 145 0 145 10 155Offsite 2 0 2 1 3Subtotal 166 0 166 14 180Not answered 0 0 0 3 3Total 166 0 166 17 18327
CHAPTER 2 - Organisational dataTable 13. 24 hour access to haematology andbiochemistry investigationsHaematologyBiochemistryYes 165 165No 1 0Subtotal 166 165Notanswered17 18Total 183 183Table 14. Number of resuscitation baysNumber of hospitals %1 5 2.72 19 10.43 46 25.34 60 33.05 29 15.96 18 9.9> 6 5 2.7Subtotal 182Not answered 1Total 183Only one hospital was reported not to have access to 24hour haematology investigations, however a further 17 sitesfailed to answer the question (Table 13). This fi nding wassimilar for the 24 hour accessibility to biochemistry.The resuscitation bay provides an area and an array ofequipment that are essential for the immediate treatment ofpatients. Since there are often two or more victims from oneroad traffi c collision (RTC), and other seriously ill patients alsoneed to be treated in this location, it is important to note that70 hospitals had less than four resuscitation bays(Table 14).Table 15. Equipment available to eachresuscitation bayNumber of hospitalsAnaesthetic machine/head 136Diffi cult intubation trolley 149Positive pressure ventilator 166SpO 2monitoring 182FeCO 2monitoring 158Central venous171pressure monitoringArterial pressure monitoring 170Surgical set 146Cricothyroidotomy set 178Intercostal drain set 180Tracheosotomy set 165Diagnostic peritoneal lavage 144Cut down set 177External pelvic fi xation set 48Foley catheter 182Nasogastric tube 183Obstetric wedge 87Rapid infusion equipment 147Fluid warming equipment 171Rhesus negative blood 112Defi brillator 181Focused Assessment withSonography for <strong>Trauma</strong>Portable x-ray 165Fixed gantry x-ray 56Portable or fi xed gantry x-ray 1836128
2Organisational dataThere are some notable fi ndings in Table 15. Manyseverely injured patients require anaesthesia and trachealintubation. If already intubated in the prehospital phase,maintenance of anaesthesia will often be required. Despitethis, one in four hospitals reported that they did not haveanaesthetic machines in each bay and one in ten reportedthat they did not have ventilators. Rapid investigation ofpossible intraperitoneal haemorrhage is another essentialcomponent in the care of these patients. However, FocussedAssessment with Sonography for <strong>Trauma</strong> (FAST) was onlyavailable in 33.3% (61/183) of emergency departments anddiagnostic peritoneal lavage in 78.7% (144/183).In the 1993/1994 <strong>NCEPOD</strong> report, it was recommendedthat all acute hospitals should have a theatre that is kept freefrom elective surgery in the event that a patient requires anemergency procedure. Such emergency daytime theatresare often referred to as ‘<strong>NCEPOD</strong> theatres’. Table 16 showsthat 151/177 (85.3%) hospitals had a <strong>NCEPOD</strong> theatre, asignifi cant improvement on 1993/1994.Table 16. Number of hospitals with dedicated emergency and trauma theatresDedicated trauma theatre<strong>NCEPOD</strong> theatre Yes No Subtotal Not answered TotalYes 129 22 151 3 154No 10 16 26 1 27Subtotal 139 38 177 4 181Not answered 0 1 1 1 2Total 139 39 178 5 183Table 17. Number of consultants (whole time equivalents) by specialtyEmergencymedicineOrthopaedicsurgeonsGeneralsurgeonsVascularsurgeonsInterventionalradiologists0 3 6 2 43 51> 0 < 1 1 1 0 25 14≥ 1 < 2 16 2 3 43 32≥ 2 < 3 29 5 11 29 36≥ 3 < 4 47 7 16 24 21≥ 4 < 5 40 21 17 8 6≥ 5 < 6 21 30 31 1 8≥ 6 25 101 93 2 6Subtotal 182 173 173 175 174Not answered 1 10 10 8 9Total 183 183 183 183 18329
CHAPTER 2 - Organisational dataTable 18. Number of consultants (whole time equivalents) that took part in the emergency rotaOrthopaedicsurgeons General surgeons Vascular surgeonsInterventionalradiologists0 9 12 51 84> 0 < 1 2 0 18 2≥ 1 < 2 0 2 35 17≥ 2 < 3 5 12 23 22≥ 3 < 4 6 17 19 14≥ 4 < 5 25 18 6 7≥ 5 < 6 32 32 2 7≥ 6 89 78 1 4Subtotal 168 171 155 157Not answered 15 12 28 26Total 183 183 183 183Table 19. Number of consultants who had taught on an Advanced <strong>Trauma</strong> Life Support (ATLS) course in thelast two yearsEmergencymedicineOrthopaedicsurgeonsGeneralsurgeonsVascularsurgeons0 33 88 119 1271 43 32 22 132 37 21 14 23 31 8 3 24 11 1 1 15 8 3 1 0≥ 6 11 1 0 0Subtotal 174 154 160 145Not answered 9 29 23 38Total 183 183 183 183Table 19 demonstrates that ATLS, at the instructor level, was very much more supported by emergency medicine than surgery –this is in contrast to the USA where surgeons are in charge of the trauma system and trauma education.30
2Organisational dataTable 20. Number of consultants who had a specialist interest in traumaOrthopaedicsurgeonsGeneralsurgeonsVascularsurgeonsInterventionalvascular radiologists0 66 137 128 1231 25 10 13 122 9 5 6 103 9 5 2 44 9 1 3 25 7 3 0 0≥ 6 39 6 0 0Subtotal 164 167 152 151Not answered 19 16 31 32Total 183 183 183 183The management of trauma patients requires amultidisciplinary approach. However, at the time of this studythere was a lack of specialist interest in trauma across thespecialties (Table 20). This may well be a refl ection of thelow trauma workload which makes it diffi cult to developand maintain a special interest in this area, given the currentconfi guration of trauma services.To explore the apparent lack of specifi c consultant interest intrauma further, we looked at the 33 hospitals that performedneurosurgical procedures at all times. Table 21 demonstratesthat even in those hospitals with neurosurgery, other thaninterest from orthopaedic surgeons there was little specialistinterest in trauma. This is important as it has been proposedthat hospitals with neurosurgery could form the basis ofregional trauma centres 2 .Table 22 illustrates the number of hospitals which had aformal trauma team and whether or not ATLS courses wererun onsite. One hundred and forty three hospitals (78.1%)had a formal trauma team, and 82 (44.8%) indicated thatthey ran ATLS courses onsite. It is diffi cult to comprehendthe fi nding that 16 hospitals that ran ATLS courses did nothave a formal trauma team; a key component of ATLS.Table 21. Hospitals that perform neurosurgicalprocedures at all times and consultants with aspecialist interest in traumaNumber ofhospitalsOrthopaedic surgeons 24General surgeons 5Vascular surgeons 6Vascular interventional radiologists 5Table 22. Formal trauma team/responseassociated with an ATLS course run onsiteFormal trauma teamATLS courses Yes No TotalYes 66 16 82No 77 24 101Total 143 40 18331
CHAPTER 2 - Organisational dataTable 23. Specialty of trauma team by residencyConsultantEmergency MedicineSpR or aboveAnaesthetic SpRor aboveSurgical SpR orabove% % % %Resident 6 3.3 109 59.6 111 60.7 86 47.0Non resident 59 32.2 36 19.7 13 7.1 34 18.6Not present 118 64.5 38 20.8 59 32.2 63 34.4Total 183 183 183 183The majority (134/143) of hospitals with a formal traumateam had a written protocol for activating a trauma response.To determine who would respond to a severely injured patientout of hours, we asked for a list of the grades, specialties,ATLS and residency status, for each of the clinicians whowere on call on Sunday February 5th 2006 at 2am.Despite the recommendation that the trauma team leadershould be a consultant 3 , the majority of hospitals (118/183) didnot have consultant presence for the management of majortrauma during the early hours of Sunday morning on February5th 2006. Furthermore, in only six cases was the consultanta resident and thus immediately available (Table 23).Immediate airway control is vital. Only 111/183 hospitals(60.7%) had an anaesthetic SpR or above immediatelyavailable. <strong>Trauma</strong> airways are likely to be diffi cult and ananaesthetic SpR or above should be present immediately inthe emergency department.The management of the severely injured patient can beextremely challenging and rapid, accurate communication ofall aspects of care is essential. This is particularly importantgiven that many different specialties may be involved. It canbe seen from Table 24 that only 51/175 hospitals had writtenprotocols covering this important area.Table 24. Communication and handoversWritten protocol forhanding over careClinical teamsClinical specialties% %Yes 59 33.1 51 29.1No 119 66.9 124 70.9Subtotal 178 175Notanswered5 8Total 183 183Over a third (65/183) of hospitals indicated that they did notallocate a named person for communicating with the patient/relatives. This insuffi ciency was refl ected by the individualcases. Where the advisors felt they were able to assess thelevel of communication with the patient/relatives, 31.4%(141/449) of cases were found to be less than satisfactoryfor quantity and quality of communication. This clearlyindicates that a named person of appropriate senioritymust be nominated to the patient/relatives as a point ofcontact. Communication with the patient/relatives must bedocumented to allow all involved with the care of the patientto be aware of the occurrence and content ofthis communication.32
2Organisational dataKey findingsRecommendationsMany severely injured patients are taken to hospitals thatdo not have the staff or facilities to provide defi nitive care.In this study only 17 hospitals had the range ofspecialities available to be considered for a Level 1<strong>Trauma</strong> Centre (under the verifi cation system of theAmerican College of Surgeons).39.3% (72/183) of hospitals did not have a residentanaesthetist at SpR level or above.65% (118/183) of hospitals stated that a consultant wasnot involved in the initial care of a severely injured patientwho presented at 0200 on Sunday 5th February 2006.There is a need for designated Level 1 trauma centresand a verifi cation process needs to be developedto quality assure the delivery of trauma care (as hasbeen developed in USA by the American College ofSurgeons). (Royal College of Surgeons of England,College of Emergency Medicine)All hospitals receiving trauma cases should have at leastfour resuscitation bays. (Hospital trusts)All hospitals receiving trauma patients should have aresident SpR or above with the skills to immediatelysecure the airway in trauma patients. (Hospital trusts)There should be a CT scanner within or adjacent to theresuscitation room. (Hospital trusts)Each trust involved in trauma care should develop acore group of clinicians with a special interest in traumamanagement. This trauma care delivery group shouldinclude a member of the trust executive staff. (Hospital trusts)References1. http://www.rcr.ac.uk/docs/radiology/worddocs/RCRStandardsforCT11thNov2003webed.doc2. A Darzi. Framework for Action. 2007.http://www.healthcareforlondon.nhs.uk/framework_for_ action.asp3. The Royal College of Surgeons of England and the BritishOrthopaedic Society. Better Care for the Severely Injured.200033
CHAPTER 3 - Overall assessmentAll casesFigure 4 shows the advisors’ assessment of overallquality of care for the whole study population. More thanhalf the patients (415/795) were subjected to less thangood practice. There was greater room for improvementin organisational (180/795) rather than clinical (129/795)aspects of care.Overall assessment by volume of casesFigure 5 shows the overall assessment of care analysed bythe volume of cases each hospital reported to <strong>NCEPOD</strong>during the study period. Hospitals that reported greater than20 patients during the study period had a higher percentageof cases classed as good practice than centres that reportedfewer cases (57% v 39%).Figure 4. Overall assessment of care (advisors’ view)400Number of patients3002001000Good practiceRoom forimprovement -clinicalRoom forimprovement -organisationalRoom forimprovement -clinical andorganisationalLess thansatisfactoryInsuff icientdataFigure 5. Number of patients per hospital vs. advisors’ overall assessment70Percentage of group60504030201-56-1011-20>20100Good practiceRoom forimprovement -clinicalRoom forimprovement -organisationalRoom forimprovement -clinical andorganisationalLess thansatisfactoryInsufficient data34
3Overall assessmentTable 25. Appropriate initial responseNumber of patients %Yes 605 86.6No 94 13.4Subtotal 699Insuffi cient data 96Total 795Table 26. Appropriateness of the response bygrade of reviewerGrade offirst reviewerAppropriate responseYes No Total% %Consultant 154 96.9 5 3.1 159NCCG 16 84.2 3 15.8 19SpR 204 88.3 27 11.7 231SHO 52 76.5 16 23.5 68Total 426 51 477Table 27. Overall assessment in patients withinappropriate initial responseNumber ofpatients %Good practice 8 8.5Room for improvement –clinicalRoom for improvement –organisationalRoom for improvement –clinical and organisational28 29.817 18.121 22.3Less than satisfactory 17 18.1Insuffi cient data 3 3.2Total 94Appropriateness of initial hospital responseThe advisors were asked to assess the initial response to thetrauma patient. Table 25 shows that 94/699 (13.4%) cases,where the advisors could make an assessment, were gradedas having an inappropriate initial response. In a further96/795 cases there was insuffi cient data to comment.Appropriateness of initial response by gradeof staffTable 26 shows the appropriateness of initial response incases where the grade of staff involved could be determined.When these data were considered by grade of the fi rstclinical reviewer at the hospital a clearer picture emerged andthe percentage of inappropriate responses rose from 3.1%when consultants were the fi rst reviewer to 23.5% whenSHOs were the fi rst reviewer.Appropriateness of initial hospital responseand overall careTable 27 shows only those patients who were classifi ed ashaving an inappropriate initial response (94/699 from Table25). Only a handful of the cases (8/94) were graded ashaving good overall care. In addition 17/94 received lessthan satisfactory care in the view of the advisors.Table 27 refl ects the importance of the initial response inthe view of the advisors; both in terms of clinical decisionmaking, and overall care for the severely injured patient.If the initial in-hospital phase of trauma care is not goodthen the remainder of the patient journey is more likely tobe sub-standard.35
CHAPTER 3 - Overall assessmentKey findingsLess than half (47.7%) of the patients in this studyreceived good care.Patients were more likely to receive good care in centresthat reported a high volume of cases (>20) compared toa low volume of cases (
4Prehospital careCHAPTER 4 - Prehospital careIntroductionThe administration of high quality prehospital care is vital inany system of trauma care. Prioritisation and managementof life threatening injuries, coupled with rapid transfer todefi nitive care in an appropriately equipped trauma unitare the mainstay of this phase of the trauma system. Theemphasis on prehospital care versus rapid transfer variesbetween countries, with little evidence of one systemhaving advantages over the other 1 . However, it must beemphasised that there is no dichotomy between prehospitalcare and rapid transfer as all care should be tailored to dealwith the patient’s injuries and any consequent physiologicalderangements. Patients undergoing rapid transfer must stillreceive appropriate prehospital care.<strong>Trauma</strong> systems are primarily geared towards themanagement of small and manageable numbers ofcasualties, which do not overwhelm the local resourcesavailable. Special measures are required when the numberof casualties exceeds the capacity of the local resources. Inthis event, a major incident will be declared, and a multiagencypredetermined major incident plan will be initiated.Such a plan is necessary to ensure a high standard of careis delivered to all patients presenting as part of a majorincident. In this study there were 12 cases reported whereit was indicated on the questionnaire that a “major incident”had occurred 2 . However, on more detailed examination ofthe casenotes, none of these cases arose in situations whichfulfi lled the requirements of the defi nition of a major incidentand in no case was a major incident formally declared. Sincenone of the patients in this study were involved in a majorincident, it would be expected that resources should havebeen suffi cient to provide the usual standard of care.As mentioned in the methods section, it had been hopedthat some additional information regarding the prehospitalmanagement of patients could be obtained from aquestionnaire completed by ambulance crews. However, itproved diffi cult to agree this with ambulance services, partlydue to employment contract issues and partly due to there-organisation of ambulance trusts.Organisational aspects of carePrehospital documentationIn a third of cases (245/749), the ambulance patient reportform (PRF) was not available. Data in this chapter thereforerefers to the 504 cases where a PRF was returned. This is animportant healthcare record which provides treating clinicianswith vital prehospital information regarding the incident andprehospital management. This form could also provide astructure to ensure that protocols of prehospital managementare followed, and that data relevant to subsequent serviceaudit are accurately recorded. Unfortunately, there was nouniformity between ambulance trusts; with wide variation inthe content of PRFs. Appendix D demonstrates an exampleof an excellent PRF. It should be noted that the PRF is oftena non-standard size which does not fi t into the hospitalcasenotes and, therefore, it may become misplaced.37
CHAPTER 4 - Prehospital careResponse timesResponse times from the time of the emergency call to arrivalat the scene of accident varied. This information, analysed bytime of day, is shown in Figure 6. The mean response timefor day, evening and night was 12.5, 11.6 and 10.1 minutesrespectively.Overall there were better response times at night, although itis doubtful if this is of clinical relevance.Response time and outcomeIt is often said that rapid response times are essential andassociated with better outcomes although it is diffi cult to fi nddata to support this statement. Table 28 shows mortality rateat 72 hours post injury against response time.In this study there was no clear evidence to support theassociation of response time with better outcome. Indeed thegroup with the fastest response time (0-5min) did not have alower mortality than the rest of the population (Table 28).Figure 6. Time from emergency call to scene of accident (daytime is defined as 08.00–17.59,evening from 18.00-23.59 and night time from 00.00-07.59)1412Time (minutes)1086420Day Evening NightTable 28. Prehospital response times (minutes) and patient outcome at 72 hoursAlive Deceased Total % mortality0-5 72 20 92 21.76-10 111 18 129 14.011-15 66 12 78 15.416-20 40 6 46 13.021-25 24 6 30 20.026-30 7 2 9 22.2> 30 11 2 13 15.438
4Prehospital careMode of arrivalThe mode of arrival is shown in Table 29.Table 29. Mode of arrivalNumber ofpatients %Effect of time on mode of arrivalFigure 7 shows that helicopters were much less likely tobe employed at night. Approximately 75% of helicoptertransfers occurred during daytime hours.Ambulance 652 83.3Helicopter 92 11.7Other emergency service 5
CHAPTER 4 - Prehospital careFigure 8. Length of time at scene of injury140120Number of patients100806040200≤ 10 > 10 ≤ 20 > 20 ≤ 30 > 30 ≤ 40 > 40 ≤ 50 > 50 ≤ 60 > 60Time (minutes)Time at sceneIn those cases (386/504) where the timings could bedetermined, the vast majority (349), exceeded therecommended length of time on scene of 10 minutes 3 (Figure8). In 71 cases delay was due to entrapment. Even if theentrapped were excluded, 278 cases exceeded 10 minutesat the scene. In a further 105 cases either intubation and/or cannulation were undertaken at the scene, and thesemanoeuvres may have contributed to the extended time atthe scene. The 10 minute on scene recommendation refersto paramedic care and in the presence of a prehospitalphysician system (where more interventions are likely, e.g.tracheal intubation) a longer time is probably justifi able.Transport system and prehospital timingsThe role of helicopters in the management of trauma patientsremains controversial 4 . Some trauma victims may benefi t butothers may not. Previous studies in the USA have suggestedthat total times from alert to arrival at hospital are signifi cantlylonger in all types of location by helicopter as opposed toroad ambulance 5 .There was a greater time to reach hospital from the timeof the emergency call, and an increased time spent at thescene of the incident, for those patients transported byhelicopter (Figure 9).The longer time spent at the scene for patients transportedby helicopter could, in part, be attributed to the greaterlikelihood of there being a doctor on the scene, and of thepatient being intubated before transfer. We were unableto identify which cases were attended by doctors orparamedics.40
4Prehospital careFigure 9. Average response times and time at scene: ambulance vs. helicopter90Time (minutes)807060504030ambulancehelicopter20100Time to hospital from emergency callLength of time at sceneTransport system and prehospital airwaymanagementFrom the cases where it could be determined, 23/56 (41.1%)patients transported by helicopter were intubated at thescene versus 32/440 (7.3%) of those patients transportedby ambulance. Additionally it was found that a greaterpercentage of patients transported by ambulance arrived athospital with a noisy or blocked airway compared with thosetransported by helicopter (52/380; 13.7% v 3/54; 5.6%).Patients treated and transferred by a helicopter system had agreater chance of defi nitive airway control than those treatedand transferred by a road ambulance system.Transport system and severity of injuriesThe severity of injuries in both groups was comparable(Table 30).Table 30. Transport system by injury severity scoreISSRoad ambulanceNumber ofpatientsHelicopterNumber ofpatients% %16 - 24 240 54.5 31 52.525 - 35 156 35.5 20 33.936 - 75 44 10.0 8 13.6Total 440 5941
CHAPTER 4 - Prehospital careTransport system and secondary transfer rateThe likelihood of requiring a secondary transfer was lower if thepatient’s mode of arrival was by helicopter than for those patientswho arrived by road ambulance. Only 7/59 (11.9%) patientsrequired a secondary transfer in the helicopter group comparedwith 112/440 (25.5%) transported initially by road ambulance.55.2mins). However, the patient was more likely to be intubated(41.1% v 7.3%), less likely to arrive at hospital with a completelyor partially blocked airway, more likely to be triaged to anappropriate hospital (100% v 93%) and less likely to require asecondary transfer (11.9% v 25.5%).Clinical aspects of careTransport system and appropriatenessof initial hospitalIt was judged that all of the patients transported by helicopterwere taken to an appropriate hospital. However, it wasdeemed that 31/440 (7%) patients transported by roadambulance were taken to an inappropriate fi rst hospital.Transport systems – summaryOverall, the picture regarding mode of transport is complex.There is a potential danger in making assumptions regarding theappropriateness of the mode of transport in any individual caseif conclusions are drawn from aggregated data derived froma heterogeneous population. Helicopters should not only beconsidered as a mode of transport, but also as a system of carewith the potential to deliver rapidly to the scene of the incidenta doctor with suffi cient expertise to manage these challengingpatients. However, given the signifi cant expense involved inoperating helicopters, it is important that a careful and detailedaudit of the value of helicopter transport is undertaken.In summary, helicopter transport was used for 11.7% of theseverely injured patients in this study, with most episodes takingplace in daylight hours. Treatment and transport by a helicopterbasedteam compared to a ground ambulance-based teamwas associated with a longer on scene time (36.9 minutes v25.3 minutes) and a longer total prehospital time (77.4mins vPrimary and secondary surveyIn the majority of patients, a primary survey was conductedat the site of the incident, en route or at some unspecifi edstage prior to arrival at hospital.Table 31. Primary and secondary survey performedPrimary Secondary% %Yes at scene 248 52.4 169 60.6Yes en route 5 1.1 30 10.8Yes unknown 220 46.5 80 28.7Subtotal 473 279Not recorded 31 225Total 504 504However, in 31/504 (6.2%) cases, there was no record of aprimary survey having been completed (Table 31).In 199/504 cases a secondary survey was known to havebeen performed in the prehospital phase. In nearly half ofcases the secondary survey was not recorded.It is not clear why so many patients had a secondary surveyperformed, as the priority in the prehospital phase shouldbe a good primary survey and attention to any immediate42
4Prehospital careproblems with the airway, cervical spine, breathing andcirculation as the prime focus. Repeated evaluation of theseaspects of care is required en route to hospital and while asecondary survey may provide valuable information regardingthe patient’s overall condition, it must not distract from this.Airway and ventilationPrehospital intubationTwenty two of the patients with airway obstruction wereintubated at the scene. Attempted intubation failed in sixpatients at the scene but all were successfully intubated inthe emergency department. A further 34 patients, for whomthe airway status was clear or not recorded, were intubatedat the scene (56 in total). However, three more failedattempts were documented in this group.Airway status at sceneIn 85/504 cases it was recorded that the airway was eitherpartially (noisy) or completely obstructed (blocked) (Table 32).Table 32. Airway statusNumber of patients %Clear 343 80.1Noisy 46 10.7Blocked 39 9.1Subtotal 428Not recorded 76Total 504Monitoring and oxygen therapyThe respiratory rate is an important indicator of respiratoryfunction and of shock. Respiratory rate was not recorded in65/504 (13%) patients (Figure 10).Oxygen therapy was administered to 372/504 (73.8%)patients, but was not documented as being administered inthe remaining 132 cases. The use of assisted ventilation waspoorly documented.Figure 10. Documentation of prehospital airway and ventilatory managementNumber of patients500400300200YesNot documented1000Respiratory rate SpO 2 O 2 therapy43
CHAPTER 4 - Prehospital careAdequacy of prehospital airway and ventilationTables 33 and 34 show the advisors’ opinion on prehospitalairway and ventilation management.Table 33. Adequate airway securedNumber of patients %Yes 396 90.4No 42 9.6Subtotal 438Insuffi cient data 66Total 504Table 34. Adequate ventilation securedNumber of patients %Yes 401 92.0No 35 8.0Subtotal 436Insuffi cient data 68Total 504The advisors were of the opinion that airway management inthe prehospital phase was inadequate in 42 out of the 438cases that could be assessed. In a number of these cases(12/42), it was felt that prehospital intubation should havebeen attempted. In 35/436 (8%) cases, advisors felt thatventilation was inadequate. <strong>NCEPOD</strong> did not request anydata on the use of capnography in the prehospital phase.The management of the airway and breathing in theprehospital setting is currently the responsibility ofparamedics because very few areas in the UK have a systemof care that ensures a doctor is part of the response team.Whilst it is not current practice for paramedics to routinelyperform tracheal intubation on trauma patients, they mayundertake this task when the airway is compromised andbasic airway manoeuvres have failed. Paramedics in Britaindo not use anaesthetic drugs or muscle relaxants to achieveintubation and, therefore, can only attempt this in the mostobtunded patients.The literature points to a high mortality in the prehospital phasewhen trauma patients are intubated without the need foranaesthesia 6, 7 . This probably refl ects the severity of their injuries,in that they can tolerate laryngoscopy and intubation withoutanaesthesia, rather than the effect of the procedure itself.The literature is confusing with regards to the effects ofprehospital intubation of trauma patients. Some studies haveshown increased mortality whilst others have shown benefi t 8-11. It is diffi cult to separate the effects of underlying injuries,anaesthesia, skill and experience of the intubator from thepossible benefi ts or side effects of the procedure.A recent expert panel concluded that suboptimal anaesthetictechnique as well as subsequent hyperventilation may accountfor some of the mortality reported with prehospital airwaymanagement in systems where anaesthesia is available 12 .Invasive airway management at the scene is successfullyperformed in systems that supply physician staffed ambulances,and is considered a vital part of their advanced trauma lifesupport 10, 13, 14 .As can be seen, there is little high quality evidence to supporteither opinion. Most of the studies favouring prehospitalendotracheal intubation of severely traumatised patients wereconducted in out-of-hospital systems that rely on highly skilledpersonnel such as anaesthetists, emergency physicians,or specially trained nurses, mostly in continental Europe orAustralia. In contrast, studies that do not support this approachrely on data from paramedic or emergency technician staffedservices, mostly in the USA or the UK. The conclusion must bethat if prehospital intubation is to be part of prehospital traumamanagement then it needs to be in the context of a physicianbasedprehospital care system.44
4Prehospital careFigure 11. Documentation of prehospital cardiovascular measurements500Number of patients400300200100YesNo0Pulse BP Capillary refill BP orCapillary refillCardiovascular managementThere are two sets of recommendations and guidelinesin relation to this that are closely interlinked: The NationalInstitute for <strong>Health</strong> and Clinical Excellence (NICE) andJoint Royal Colleges Ambulance Liaison Committee(JRCALC). Prehospital staff are more likely to be familiar withJRCALC guidelines, and hospital staff more familiar withNICE recommendations, which are in fact published as atechnology appraisal 16 , not as clinical guidelines.The recommendations arising from the NICE technologyappraisal, and included within the JRCALC guidelines 15 , areas follows:“It is recommended that in the prehospital managementof adults and older children, IV fl uid should not beadministered if a radial pulse can be felt (or, forpenetrating torso injuries, if a central pulse can be felt).In the absence of a radial pulse (or a central pulse forpenetrating torso injuries) in adults and older children, itis recommended that IV fl uid should be administered inboluses of no more than 250 ml. The patient should thenbe reassessed, and the process repeated until a radialpulse (or central pulse for penetrating torso injuries)is palpable.The administration of IV fl uid should not delaytransportation to hospital, but when given in accordancewith the recommendation above, consideration shouldbe given to administration en route to hospital.It is recommended that when IV fl uid is indicated in theprehospital setting, crystalloid solutions should be theroutine choice.There is inadequate evidence on which the Institute canbase recommendations on when prehospital use of IVfl uid in young children and infants following trauma isappropriate, or on the volumes of fl uid to use. However,there is a broad consensus that transfer to hospitalshould not be delayed by attempts to administer IV fl uid.It is recommended that only healthcare professionals whohave been appropriately trained in advanced life-supporttechniques and prehospital care should administer IV fl uidtherapy to trauma patients in the prehospital setting.Training programmes for healthcare professionals shouldincorporate the above recommendations.”45
CHAPTER 4 - Prehospital careIn 40/504 (7.9%) cases the pulse was not recorded. Bloodpressure was recorded in 398/504 (78.9%) cases. 21/504(4.2%) patients did not have any measurements of theircardiovascular status recorded prior to arrival at hospital.Measurement of blood pressure at the site of incident or enroute, is not recommended particularly in children, as it maylead to unnecessary delay.Fluid therapy was recorded as being administered either atthe scene or en route in 188/504 cases.Table 35. Appropriate haemorrhage control(advisors’ opinion)Number of patients %Yes 356 96.7No 12 3.3Subtotal 368Insuffi cient data 136Total 504Table 36. Appropriate fluid therapy(advisors’ opinion)Number of patients %Yes 279 87.2No 41 12.8Subtotal 320Insuffi cient data 184Total 504The advisors assessed that in 12 cases, insuffi cient stepshad been taken to control haemorrhage (Table 35), and in41 cases fl uids were not administered appropriately (Table36). In most cases this was because inadequate volumes,or in some cases no fl uid, was administered, despite clinicalfeatures of shock. However, there were no cases in whichthe advisors believed that children under the age of 16 yearshad received inappropriate fl uid resuscitation prehospital.Head injuryIn 25 cases the Glasgow Coma Score (GCS) or AVPU (Alert,Verbal, Pain, Unresponsive) score was not recordedFigure 12. Prehospital Glasgow Coma Score (GCS)140120Number of patients10080604020015 14 13 12 11 10 09 08 07 06 05 04 03Glasgow Coma Score46
4Prehospital careFigure 13. Prehospital Glasgow Coma Score and intubation140Number of patients120100806040200Not intubatedIntubatedFailed attempt15 14 13 12 11 10 09 08 07 06 05 04 03GCS(Table 37). This could be taken to mean that the score wasnormal. However, it is important that the GCS or AVPU isrecorded, so that any deterioration later in the patient journeycan be clearly and unequivocally identifi ed.Where the airway was at risk because of a GCS lessthan 9, intubation was performed in only 46/170 patients.Documentation of other forms of assisted ventilation was notedto be poor. Advisors considered that the airway/ventilatorymanagement could have been better in a substantial numberof patients, a number of whom had a lowered GCS (Figure 13and Table 38). Many patients who may have benefi ted fromintubation did not have this procedure performed because theappropriate skills were not available.Table 37. Prehospital AVPU scoreAlert 68Verbal 21Pain 17Unresponsive 21Subtotal 127GCS or AVPU not recorded 25Total 152Table 38. Prehospital AVPU score and intubationNotintubatedIntubatedFailedattemptAlert 68 0 0AnalgesiaThe administration of analgesia prehospital was documentedin 110/504 cases. The advisors considered that theanalgesia was inappropriate for 7/110 of these cases.In one such case it was felt that an overdose had beenadministered. In another case the administration of analgesiaVerbal 21 0 0Pain 11 5 1Unresponsive 13 8 0Total 113 13 147
CHAPTER 4 - Prehospital carecaused respiratory depression which was not adequatelymanaged by suitable respiratory support. In three cases withsignifi cant thoracic injuries Entonox was the analgesic usedand this was considered by the advisors to be inappropriatebecause of the risk of tension pneumothorax.One must question why the provision of analgesia in a groupof severely injured patients was so low (110/504 – 21.8%)?Patients with severe injuries are likely to experience pain and theprovision of analgesia to reduce this is a basic humanitarian aim.It is rare that contraindications exist to the provision of pain relief.Key findingsIn a third of cases (245/749), the ambulance patient reportform was not available.652/783 patients (83.3%) were transported to hospital byroad ambulance and 92/783 patients (11.7%) by helicopter.23/56 (41.1%) patients treated by a helicopter-basedsystem were intubated on scene compared to 32/440(7.3%) patients treated by a road ambulance system.None of the patients treated by a helicopter based systemwere taken to an inappropriate hospital compared to31/440 (7%) patients treated by a road ambulance systemwho were initially taken to an inappropriate hospital.Blood pressure was recorded in 398/504 (80%) casesdespite recommendations that this should not bemeasured in the prehospital phase.Only 46/170 (27.1%) patients who suffered a severe headinjury (GCS less than 9) were intubated prehospital.Only 110/504 (21.8%) patients were given analgesia in theprehospital phase.RecommendationsAll agencies involved in trauma management, includingemergency medical services, should be integrated intothe clinical governance programmes of a regional traumaservice. (All healthcare providers)Ambulance trusts should work together to standardisethe content and layout of the Patient Report Form(PRF), and ensure that it is fi t for purpose and facilitatescomparative audit. Clinicians must ensure that a PRFis received for every patient and secured in the medicalrecord. (Emergency medicine physicians and ambulancecrews)It is important that where guidelines exist, they are widelydisseminated to appropriate groups, and there is arobust system in place to monitor compliance with thoseguidelines. (Ambulance and hospital trusts)It is vital that all patients who have sustained serioustrauma should have a primary survey conducted atthe earliest opportunity, and that critical resuscitationinvolving airway, breathing and circulation (with cervicalspine control) should be undertaken and reviewedthroughout the prehospital phase of care. This must bedocumented. (Emergency medicine physicians)Airway management in trauma patients is oftenchallenging. The prehospital response for these patientsshould include someone with the skill to secure theairway, (including the use of rapid sequence intubation),and maintain adequate ventilation. (Ambulance andhospital trusts)Severely injured patients are likely to be in pain and theprovision of adequate analgesia is required. If analgesiais not given there should be a clear record in the PatientReport Form of the reasons for this. (Ambulance trusts)48
4Prehospital careReferences1. Nathens AB, Brunet FP, Maier RV. Development oftrauma systems and effect on outcomes after injury.Lancet 2004; 363(9423):1794-8012. The form sent to lead A&E Clinicians contained thefollowing defi nition of a major incident protocol:“Pre-planned and exercised procedures which areactivated once a major incident has been declared.A major incident is any emergency that requires theimplementation of special arrangements by one or moreemergency services, the NHS or the local authority”.3. The Royal College of Surgeons of England and the BritishOrthopaedic Society. Better Care for the Severely Injured.20004. Thomas SH, Biddinger PD, Helicopter trauma transport:an overview of recent outcomes and triage literature.Current Opinion in Anaesthesiology 2003; 16(2):153-85. Carr BG, Caplan JM, Pryor JP, Branas CC. A metaanalysisof prehospital care times for trauma.Prehospital Emergency Care 2006; 10(2):198-2066. Lockey D, Davies G, Coats T. Survival of trauma patientswho have prehospital tracheal intubation withoutanaesthesia or muscle relaxants: observational study.BMJ 2001; 323:1417. Christensen EF, Hoyer CC. Prehospital tracheal intubationin severely injured patients: a Danish observational study.BMJ 2003; 327:533-48. Winchell RJ, Hoyt DB: Endotracheal intubation in thefi eld improves survival in patients with severe head injury.<strong>Trauma</strong> Research and Education Foundation of SanDiego. Arch Surg 1997; 132:592-79. Garner A, Rashford S, Lee A, Bartolacci R. Addition ofphysicians to paramedic helicopter services decreasesblunt trauma mortality. Aust N Z J Surg 1999; 69:697-70110. Adnet F, Jouriles NJ, Le Toumelin P, Hennequin B,Taillandier C, Rayeh F, Couvreur J, Nougiere B, Nadiras P,Ladka A, Fleury M: Survey of out-of-hospital emergencyintubations in the French prehospital medical system: amulticenter study. Ann Emerg Med 1998; 32:454-6011. Bochicchio GV, Ilahi O, Joshi M, Bochicchio K, ScaleaTM. Endotracheal intubation in the fi eld does not improveoutcome in trauma patients who present without anacutely lethal traumatic brain injury. J <strong>Trauma</strong> 2003;54:307-1112. Davis DP, Fakhry SM, Wang HE, Bulger EM, DomeierRM, Trask AL, Bochiocchio GV, Hauda WE, RobinsionL. Paramedic rapid sequence intubation for severetraumatic brain injury: perspectives from an expert panel.Prehosp Emerg Care 2007; 11:1-813. Gerich TG, Schmidt U, Hubrich V, Lobenhoffer HP,Tscherne H: Prehospital airway management in theacutely injured patient: the role of surgical cricothyrotomyrevisited. J <strong>Trauma</strong> 1998; 45:312-414. Schmidt U, Frame SB, Nerlich ML, Rowe DW,Enderson BL, Maull KI, Tscherne H: On-scene helicoptertransport of patients with multiple injuries: comparisonof a German and an American system. J <strong>Trauma</strong> 1992;33:548-5315. UK Ambulance Service Clinical Practice Guidelines 2006.Joint Royal Colleges Ambulance Liaison Committee(JRCALC)16. NICE Technology Appraisal. Prehospital initiation of fl uidreplacement therapy in trauma. 200449
CHAPTER 5 - Hospital receptionIntroductionDeaths after major trauma can be grouped into immediate,early, and late deaths.Immediate deaths are caused by a fatal disruption of thegreat vessels, heart, lungs or a major disruption of bodycavities. Immediate death occurs at the scene of injury. Thisgroup of deaths is least likely to be infl uenced by measurestaken post injury. Injury prevention strategies and publichealth measures must remain the major strategy for reducingthis major source of mortality.Early deaths occur in the hours just after the injury. Thesepatients frequently arrive at a hospital prior to death whichusually occurs because of cardiovascular and/or pulmonarycollapse. Early trauma deaths result from failed oxygenationof the vital organs, massive central nervous system injury, orboth. The mechanisms of failed tissue oxygenation includeinadequate ventilation, impaired oxygenation, circulatorycollapse, and insuffi cient end-organ perfusion. Injuries thatcause early trauma mortality occur in predictable patternsbased on the mechanism of injury; the patient’s age, gender,and body habitus; or environmental conditions. Rapidresuscitation coupled with rapid defi nitive management ofinjuries and complications has the potential to reduce thesedeaths.Late deaths peak from days to weeks after the injury and aredue primarily to sepsis and multiple organ failure.Organised systems for trauma care are often thoughtto be focused on the salvage of a patient from earlytrauma mortality, while critical care is designed to managecomplications and avert late trauma mortality. However, itmust be noted that a good trauma process (early defi nitivecare and optimal resuscitation) will not only reduce earlymortality but also reduce the number of late deaths byminimising the number of patients who go on to developmultiple organ failure and require critical care. Importantlyfrom the perspective of survivors, a good trauma processmay also reduce morbidity.The recognition of these patterns led to the developmentof the advanced trauma life support (ATLS) approach bythe American College of Surgeons. ATLS is the basis oftrauma care and it is built around a standardised protocolfor patient evaluation. This protocol ensures that the mostimmediate life-threatening conditions are actively identifi edand addressed in the order of their risk potential.The objectives of the initial evaluation of the trauma patientare:1. to identify life-threatening injuries and to initiate adequatesupportive therapy;2. to effi ciently and rapidly organise either defi nitive therapyor transfer to a facility that provides defi nitive therapy.This chapter describes the initial reception of the severelyinjured patient and organisation of the trauma response.ResultsPre-alertsFrom the introduction above it can be appreciated thatone of the key steps in maximising outcome for theseverely injured patient is to ensure a rapid and appropriateemergency department response. One mechanism forensuring that this occurs is communication from theprehospital clinicians to the receiving emergency department,passing on details of the extent of the injuries and theresponse required in hospital. This communication is referredto as a pre-alert.50
5Hospital receptionFigure 14. Documentation of a pre-alert (daytime was defined as 08.00–17.59,evening from 18.00-23.59 and night time from 00.00-07.59)Number of patients160140120100806040200YesNoWeekday Weekend Weekday Weekend Weekday WeekendDay Evening NightDocumentation of ambulance pre-alertAs can be seen from Figure 14 the use of pre-alerts wasquite low with only 50.1% (375/749) of the patients arrivingat hospital with a pre-alert. It does not appear that the timeof day, nor day of week, affected the use of pre-alerts to anygreat extent.It has previously been recommended that all hospitals thatreceive patients following major injury should establish asystem of advance notifi cation with the ambulance service 1 .This arrangement should allow the ambulance paramedicat the scene to notify the emergency department directlyof the details of the injured patient(s). The aim of pre-alertsis to anticipate and be prepared for problems so thatresuscitation, investigation and defi nitive management canproceed with minimum delay.Worthy of note was the fact that the use of pre-alerts wasso infrequent in this dataset; particularly in view of the factthat only patients with a verifi ed injury severity score (ISS)score of 16 or greater were included in this study. It is likelythat the low use of pre-alerts may slow down an appropriateinitial response to these severely injured patients and delaydefi nitive care, especially as we have seen that senior traumateam leaders were often not immediately available.<strong>Trauma</strong> team responseIt is essential for each hospital that admits major traumacases to have a trauma response team 1 . The initialmanagement of the trauma patient can be extremelychallenging and requires a co-ordinated team approach todeliver timely and correct treatment to these patients. Eachhospital and the ambulance service should also agree criteriafor activation of the trauma team. Ideally this should occurprior to the patient’s arrival in the resuscitation room.<strong>Trauma</strong> team response – organisational aspectsOf the 183 sites that submitted an organisationalquestionnaire 143 (78.1%) had a formal trauma team. Allbut nine of these had a written protocol for activation of thetrauma team.51
CHAPTER 5 - Hospital receptionTable 39. <strong>Trauma</strong> respondents by grade of specialtyConsultantEmergency MedicineSpR or above Anaesthetic SpR or above Surgical SpR or above% % % %Resident 6 3.3 109 59.6 111 60.7 86 47.0Non-resident 59 32.2 36 19.7 13 7.1 34 18.6Not present 118 64.5 38 20.8 59 32.2 63 34.4Total 183 183 183 183It has previously been shown that only half of the emergencydepartments attending more than 30 000 patients per yearoperated a trauma team system 2 . A more recent study hasshown some improvement in availability of trauma teams with61% of departments surveyed operating such a system 3 . Theavailability of trauma teams has continued to increase andthat the fi gure now approaches 80%. However, one in fi vedepartments in this study, despite accepting severely injuredpatients, did not have a formal trauma team. This is presumablyan issue of organisation as these departments should have thenecessary personnel but for some reason had not arrangedtheir activity into a structured trauma response.As part of the organisational questionnaire <strong>NCEPOD</strong>requested information about who would respond to arequest for a trauma response in the early hours of a Sundaymorning (0200). Table 39 shows the response analysed bygrade and availability.One hundred and eighteen of the 183 (65%) hospitalsfrom which an organisational questionnaire was receivedresponded that a consultant would not be present during thetrauma call. There were also a number of hospitals where itwas stated that they would not have the presence of a SpRor above from the emergency department (38/183; 20.8%),anaesthesia (59/183; 32.2%) or surgery (63/183; 34.4%).There are clear recommendations regarding the compositionof a trauma team: consultant leadership plus the presence ofSpRs or above from the emergency department, anaesthesiaand surgery are probably the key elements 1 . Table 39 showsthat the current provision of staff falls well short of theserecommendations.In the hospitals where SpRs or above were either not presentor non-resident, the initial care was presumably providedby more junior members of staff. This is a concern, as initialmanagement may have a substantial impact on eventualoutcome.Immediate airway control is vital. Only 111/183 (60.7%)hospitals had an anaesthetic SpR or above immediatelyavailable. <strong>Trauma</strong> airways are likely to be diffi cult and a SpRor above should be present immediately.<strong>Trauma</strong> team response- individual casesDocumentation of trauma team responseFigure 15 shows the trauma response analysed bytime of day and weekday/weekend. Overall there wasdocumentation of a trauma team response in 59.7%(460/770) of cases. In 25 cases there was insuffi cient data52
5Hospital receptionFigure 15. Documentation of trauma response (daytime was defined as 08.00–17.59,evening from 18.00-23.59 and night time from 00.00-07.59)Number of patients180160140120100806040200YesNoWeekday Weekend Weekday Weekend Weekday WeekendDay Evening Nightto determine if there was a trauma response. There wassome variation in the activation of the trauma team by time ofday and day of week. The trauma team was less likely to bepresent on a weekday during the day (137/259; 52.9%) thanat nights (100/163; 61.3%) and weekends (168/256; 65.6%).Possible explanations for the variation in trauma teamresponse are:1. Less need for a trauma team during the normal workingday as there was an appropriate consultant response,and supporting team, immediately available within thereceiving emergency department.2. The trauma team had other responsibilities during theworking day and so was less likely to be available to attendthe emergency department for daytime trauma calls.Influence of the severity of injury on the use oftrauma teamsTable 40 describes the infl uence of the severity of injury andthe initiation of a trauma team response. There was a trendtowards greater involvement of trauma teams for patientswith more severe injuries.Table 40. <strong>Trauma</strong> call documented by ISS<strong>Trauma</strong> call documentedISS Yes No Total16 - 24 231 218 44925 - 35 185 94 27936 - 75 55 12 67Total 471 324 795While this may appear reassuring it must be rememberedthat this score was calculated retrospectively and cannotdrive real time management decisions. Also many patientswith an ISS in the range 16-24 can pose great challengesand do require the input of a well-organised trauma service.53
CHAPTER 5 - Hospital reception<strong>Trauma</strong> team response to pre-alertsThe use of pre-alerts and activation of the trauma team arekey initial components of an organised trauma system. Figure16 shows the relationship between these two elements (datafrom A&E clinician questionnaire). It can be seen that evenin the presence of a pre-alert there was no trauma teamresponse in 99/383 (25.8%) cases.The reasons for the lack of trauma team response to apre-alert were not clear but in a substantial number of cases(99/383), where the prehospital clinicians had suffi cientconcerns to issue a pre-alert, no trauma team was activated.Figure 16. <strong>Trauma</strong> team activation in response to pre-alert300Number of patients250200150100500Yes No Not answeredPre-alertYesNoNot answeredFigure 17. Grade of first reviewer/team leader in response to trauma call40Percentage of patients in dataset3530252015105<strong>Trauma</strong> callNo trauma call0Consultant NCCG SpR 3+ SpR 1/2 SpR SHO Nurse Other NotansweredGrade of clinician54
5Hospital reception<strong>Trauma</strong> team leadershipThe recommendations for an organised trauma responsestates that the trauma team leader must be a consultantfrom a relevant specialty 1 , recognising that the managementof the severely injured patient is potentially very challengingand requires considerable skill and experience.Figure 17 shows the grade of fi rst reviewer/team leaderanalysed by whether or not a trauma call had been made.A consultant was the team leader/fi rst reviewer in 136 out of502 cases (27%). An SHO was the team leader/fi rst reviewerin 54 out of 502 cases (10.8%). In 11 cases the grade ofreviewer was not answered.Two other main fi ndings emerge from these data.1. If a trauma call had been made it was much more likelythat a consultant was the fi rst reviewer/team leader.Consultants were team leaders in 36.2% (111/307) ofcases where a trauma call was made compared to only12.8% (25/195) of cases where no trauma call wasmade.2. If a trauma call had not been made it was much morelikely that an SHO was the fi rst reviewer/team leader.SHOs were team leaders in 20.5% (40/195) of caseswhere no trauma call was made compared to only 4.6%(14/307) of cases where a trauma call was made.It was also noted from the A&E clinician questionnaire that176/513 (34.3%) patients were not seen by a consultantfrom any specialty while in the emergency department. Fora further 53/513 (10%) patients, the clinician completing thisquestionnaire was unable to determine what time the patientwas fi rst seen by a consultant in the emergency department.during the day because the emergency department wasappropriately staffed by consultants, then the proportion ofconsultants seeing patients where a trauma team was notcalled would be much higher and the involvement of SHOslower. This was not the case. The above data supports theview that the response rate of the trauma team during normalworking hours was lower than out of hours as the team hadcompeting commitments during the normal working day andwas not always available to attend trauma calls.Junior medical staff were still the fi rst reviewer/team leaderin a substantial number of cases. Indeed, an SHO was thefi rst reviewer/team leader in 54/502 (10.8%) cases. However,it appears that progress has been made in this aspectsince 1992 when an SHO was in charge of initial hospitalresuscitation in 826 out of 1445 patients with an ISS of 16or greater (57.2%) 4 . While this progress is encouraging, it isimportant to recognise the challenge that the severely injuredpatient poses and that it is inappropriate for very juniormedical staff to lead their care.Time to consultant reviewGiven the current staffi ng of emergency departments itis clear that not all patients can be seen and assessedimmediately by a consultant. In the absence of immediateconsultant involvement timely review is required. Table41 shows time to consultant involvement. Fifty percent ofpatients (210/419) were either seen immediately or within30 minutes. However, 42% (176/419) were not seen by aconsultant (of any specialty) in the emergency departmentand in a further 94 cases the time interval was not knownor not answered.The above data highlights the data shown earlier regardingthe variability of trauma team response by time and day(Figure 15). If the trauma team was called less frequently55
CHAPTER 5 - Hospital receptionTable 41. Consultant involvementNumber ofpatients %On arrival 169 40.3> 0 ≤ 30 minutes 41 9.8> 30 minutes 33 7.9Not seen by consultant 176 42.0Subtotal 419Time unknown 59Not answered 35Total 513These data are taken directly from the A&E clinicianquestionnaire (self reported) and as such should not sufferfrom the diffi culty of obtaining information from the casenotes(where poor documentation often hinders assessment ofstaff involvement).The time to consultant involvement was analysed by ISS,to see if consultants were more likely to be involved early inmore severely injured patients. There was no infl uence of ISSon time to consultant involvement.Impact of time of day on grade of reviewerAnother way to analyse the data on grade of the fi rstreviewer/team leader was to consider the impact of time ofday of presentation to the emergency department. Thesedata are summarised in Table 42.From Table 42 it can be seen that consultant involvementwas highest during the day (39.6% of cases presentingduring the day) and fell over the evening and into the night(11.5% of cases presenting during night). The trend for staffin training involvement was in the opposite direction. NotablySHOs were the fi rst reviewer/team leader in 20.4% (23/113)of cases at night.While this pattern of reduced consultant involvement andincreased junior staff involvement during the eveningsand night is not new data, it is concerning since traumaoften presents out of hours when the hospital is least wellstaffed to deal with these challenges. It is clear that patientspresenting in the evenings and nights were, in the view of theadvisors, being subjected to a lesser standard of care thanduring the daytime.Table 42. Time of day by grade of reviewerDay (08.00-17.59) Evening (18.00-23.59) Night (00.00-07.59)Grade Number of patients Number of patients Number of patients% % %Consultant 82 39.6 40 27.8 13 11.5NCCG 56 27.1 45 31.3 24 21.2SpR 3+ 28 13.5 31 21.5 34 30.1SpR 1/2 17 8.2 17 11.8 15 13.3SHO 22 10.6 9 6.3 23 20.4Nurse 1
5Hospital receptionRelationship between grade of reviewer andquality of careAs stated previously, the experience of the staff makingthe initial assessment and leading the trauma team is oneof the factors that may impact on patient outcome. Onequestion that was asked of the advisors during the peerreview process was ‘was the initial response in hospitalappropriate?’.It was possible to look at the relationship between theadvisors’ opinion on appropriateness of initial responseand the grade of initial reviewer/team leader in 477/795cases. In 318 cases, poor documentation of clinicians’grades prevented this analysis. Overall 51 of the 477(10.7%) cases that could be assessed were consideredto have an inappropriate response. When these data weredisaggregated by grade of fi rst reviewer a clearer pictureemerged and the percentage of inappropriate responsesrose from 3.1% (5/159) when consultants were the fi rstreviewer to 23.5% (16/68) when SHOs were the fi rst reviewer(Table 43).Table 43. Appropriate response by grade ofreviewer (advisors’ view)Grade of firstreviewerAppropriate responseYes No Total% %Consultant 154 96.9 5 3.1 159NCCG 16 84.2 3 15.8 19SpR 204 88.3 27 11.7 231SHO 52 76.5 16 23.5 68Total 426 51 477Figure 18. Time to first consultant review400300Number of patients20010000 6 12 18 24 30 36 42 48 54 60 66Time (hours)57
CHAPTER 5 - Hospital receptionThese data provide a clear association between grade of fi rstreviewer and the advisors’ assessments of appropriatenessof response.Table 44. Time to first consultant reviewNumber of patients %On arrival 108 29.0> 0 ≤ 30 minutes 34 9.1> 30 minutes ≤ 1 hour 12 3.2> 1 hour ≤ 6 hours 96 25.7> 6 hours ≤ 12 hours 53 14.2> 12 hours 70 18.8Subtotal 373Insuffi cient data 422Total 795care process. It was recently shown in a study of severelyinjured patients 5 that consultant presence in the emergencydepartment reduced the mean time to operating theatre inthese patients: (43.8 minutes (+/-20.1) when a consultantwas present and 109.4 minutes (+/-10.7) when a consultantwas not present, p
5Hospital receptionPrimary survey and overallassessmentPrimary surveyIn 88.8% (706/795) of cases a primary survey wasdocumented on arrival in the emergency department(Table 45). In the opinion of the advisors this primary surveywas performed suffi ciently early enough in 680/706 (96.3%)cases, not suffi ciently early enough in 26 cases (3.7%)and there was insuffi cient data to comment in 89 cases(Table 46).Table 45. Documentation of a primary surveyNumber of patients %Yes 706 88.8No 89 11.2Total 795Appropriateness of initial responseThe advisors were asked to assess the initial response tothe trauma patient. Table 47 shows that of the 699 casesthat could be assessed, 94 (13.4%) were graded as havingan inappropriate initial response. In a further 96/795 cases,there was insuffi cient data to comment.Table 47. Appropriateness of initial responseNumber of patients %Yes 605 86.6No 94 13.4Subtotal 699Insuffi cient data 96Total 795Table 46. Timeliness of a primary surveyNumber of patients %Yes 680 96.3No 26 3.7Subtotal 706Insuffi cient data 89Total 795Despite the widespread adoption of the ATLS system noprimary survey was documented in 11.2% (89/795) of cases.Immediate management of life-threatening emergencies andidentifi cation of major injuries is a key to good outcomes forseverely injured patients and it is diffi cult to see how this canreliably happen in the absence of a primary survey.59
CHAPTER 5 - Hospital receptionOverall assessment and appropriateness ofinitial responsePart of the advisors’ role was to come to an overallassessment of each case using the grading systemdescribed in the method section. Table 48 shows how thepatients classifi ed as having an inappropriate initial responsewere graded (94/699 from Table 47).Table 48. Overall assessment in patients withinappropriate initial responseNumber of patients %Good practice 8 8.5Room for improvement28 29.8clinicalRoom for improvementorganisationalRoom for improvementclinical andorganisational17 18.121 22.3Less than satisfactory 17 18.1Insuffi cient data 3 3.2Total 94Only a small number of the cases (8/94) were graded asgood practice. Additionally, in the view of the advisors, 17patients received less than satisfactory care. The aboverefl ects the importance of the initial response, in terms ofclinical decision-making and overall care for the severelyinjured patient.Key findingsA pre-alert from the ambulance crew to the receivingemergency department was documented for only 50.1%of patients in this study.One in fi ve hospitals admitting severely injured patientsdid not have a formal trauma team.When a pre-alert was made to the receiving emergencydepartment, there was no trauma response in one infour cases.A trauma team response was documented for only59.7% of patients in this study.A consultant was the team leader/ fi rst reviewer in only169/419 (40.3%) of cases.Advisors felt that the patient’s initial management wasinappropriate in 23.5% of cases where an SHO was theteam leader/ fi rst reviewer compared to 3.1% of caseswhere a consultant was the team leader/ fi rst reviewer.If no trauma response was activated, then it was morelikely that an SHO was the fi rst reviewer or team leaderfor the severely injured patient.176/419 (42%) patients were not seen by a consultant inthe emergency department.89/795 (11.2%) patients did not have a primary surveydocumented in their casenotes.The initial management of the patient was thought to beinappropriate in 94/699 cases (13.4%).60
5Hospital receptionRecommendationsAmbulance trusts and emergency departments shouldhave clear guidelines for the use of pre-alerts in theseverely injured patient population. The ambulancecrew should be able to speak directly to clinical staffin the receiving emergency department to ensure anappropriate clinical response is available immediately.(Ambulance trusts and emergency departments)Trusts should ensure that a trauma team is available 24hours a day, seven days a week. This is an essential partof an organised trauma response system. (Hospital trusts)Hospital and ambulance trusts should ensure there areagreed explicit criteria for issuing a pre-alert activation ofthe trauma team. (Hospital and ambulance trusts)A consultant must be the team leader for the managementof the severely injured patient. There should be no reasonfor this not to happen during the normal working week.Trusts and consultants should work together to providejob plans that will lead to better consultant presence in theemergency department at all times to provide more uniformconsultant leadership for all severely injured patients.(Hospital trusts and clinical directors)All patients should have a primary survey performed andclearly documented on admission to the emergencydepartment. (Emergency medicine physicians)Standardised documentation for the trauma patientshould be developed. This will improve patient careand multidisciplinary communication. In addition,comparative audit will be facilitated. (RCS and College ofEmergency Medicine)As previously recommended, a consultant must be theteam leader for the management of the severely injuredpatient. However, it is appreciated that this will not beachievable immediately. In the absence of this standardall severely injured patients should be reviewed by aconsultant as soon as possible; ideally this should bewithin four hours of arrival at hospital, but must be within12 hours of arrival. (Hospital trusts)References1. The Royal College of Surgeons of England and theBritish Orthopaedic Society. Better Care for the SeverelyInjured. 20002. Kazemi AR, Nayeem N. The existence and compositionof trauma teams in the UK. Injury 1997; 28:119-213. Brooks A, Williams J, Butcher W, Ryan J. GeneralSurgeons and <strong>Trauma</strong>. A questionnaire survey of GeneralSurgeons training in ATLS and involvement in the traumateam. Injury 2003; 34(7):484-64. Yates DW, Woodford M, Hollis S. Preliminary analysis ofthe care of injured patients in 33 British hospitals: fi rstreport of the United Kingdom major trauma outcomestudy. BMJ 1992; 305(6856):737-405. Porter JM, Ursic C. <strong>Trauma</strong> attending in the resuscitationroom: does it affect outcome? Am Surg 2001;67(7):611-461
CHAPTER 6 - Airway and breathingIntroductionAdequate oxygenation of the tissues is critical to survivalafter trauma, and the maintenance of adequate levels ofoxygen in the blood stream is a paramount objective in themanagement of severe trauma. Tissue hypoxia may occuras a result of multiple injuries, haemorrhage or depressedrespiration and it may occur acutely or insidiously. A leading,but rapidly reversible, life-threatening cause of insuffi cientoxygenation is obstruction of the airway. Therefore, thereversal of an obstructed airway is regarded as fundamentalin any approach to managing the severely injured patient.Airway management is therefore one of the key componentsof emergency care. The primary objective is to recognisean obstructed or potentially obstructed airway, to clearthe obstruction and keep the airway patent. No medicalemergency, short of complete cardiopulmonary arrest,is more immediately life-threatening than the loss of anadequate airway. Failure to manage airway patency andventilation adequately has been identifi ed as a major causeof preventable death in trauma 1-4 .Many studies highlight the preventable mortality andmorbidity that occur following major trauma 5, 6 . Airwayproblems and hypovolaemia are very often the causes.The advanced trauma life support (ATLS) system of traumacare stresses the importance of recognition of airway andventilation problems. The value of early senior experiencedanaesthetic involvement cannot be over-stated. Theanaesthetist should be a key member of the resuscitationtrauma team, and not simply called when serious problemshave already developed.ResultsAirway and ventilation in hospitalTable 49 shows the airway status on arrival at the emergencydepartment and the 72 hour mortality for each group ofpatients. As can be seen, 85/676 (12.6%) of patients arriveat hospital with either a partially or completely obstructedairway and these groups had a much higher mortality ratealthough from this dataset, causality cannot be assumed.Table 49. Airway status on arrival at hospitalAlive Deceased Total % MortalityClear 526 65 591 11.0Noisy 27 13 40 32.5Blocked 28 17 45 37.8Subtotal 581 95 676Not97 22 119 18.5recordedTotal 678 117 795The provision of an adequate airway by intubation of thetrachea is often required to facilitate the management of theseverely injured patient. Table 50 shows that 74 patientswere intubated before arrival at hospital, 11 patients hadattempted but failed intubation and 362 patients wereintubated after arrival at hospital. Table 50 also showsmortality rates at 72 hours after injury. It can be seen that thegroup that was intubated prehospital had a higher mortalitythan the group intubated in hospital. This is in line withprevious literature 7 although a causal relationship cannot bedetermined from this dataset.62
6Airway and breathingThere are issues with prehospital and hospital airwaymanagement. In the prehospital chapter concerns wereraised about the delays on scene whilst attempting to securean airway. Despite the prehospital care, 12.6% of patientsarrived at hospital with a partially or completely obstructedTable 50. Intubation status and mortalityAlive Deceased Total % MortalityPrehospital 45 29 74 39.2Failedattempt(prehospital)3 8 11 72.7Hospital 290 72 362 19.9Subtotal 338 109 447No evidence 340 8 348 2.3Total 678 117 795Table 51. Grade of clinician involved with intubationNumber of patients %Consultant 22 15.8SpR 95 68.3SHO 22 15.8Subtotal 139Not recorded 223Total 362Table 52. Specialty of clinician involved with intubationNumber of patients %Anaesthetics 203 88.3Critical care medicine 20 8.7Emergency medicine 7 3.0Subtotal 230Not recorded 132Total 362airway. This raises questions about what forms of airwayprovision should be used in the prehospital phase, what skillsthe prehospital staff need to possess and what backgroundthese practitioners should come from (paramedical, medical).Tables 51 and 52 show data relevant to the personnelinvolved in, and the timing of, tracheal intubation. Data ongrade of medical staff involved was poorly documentedand not available in 223/362 cases. Anaesthetists wereresponsible for the majority of this activity (203/230 cases– 88.3%). There was evidence for use of rapid sequenceinduction in 237/362 (65.5%) patients intubated in hospital.In a substantial number of cases the grade and/or specialtywere not recorded. Where data were available it is clear thatmany patients were intubated on arrival at hospital or veryshortly after. This, combined with the 12.6% of patients whoarrived at hospital with an obstructed or partially obstructedairway, raises concerns over the adequacy of prehospitalairway management under the current system of prehospitalcare, which is largely provided by paramedic staff who arenot trained to use drugs to facilitate tracheal intubation.Table 53. Time of intubation (minutes)Number of patients %On arrival 54 22.20 ≥ 10 31 12.8> 10 ≤ 20 21 8.6> 20 ≤ 30 25 10.3> 30 ≤ 40 10 4.1> 40 ≤ 50 10 4.1> 50 ≤ 60 7 2.9> 60 85 35.0Subtotal 243Not recorded 119Total 36263
CHAPTER 6 - Airway and breathingFigure 19. First hospital respiration rate350Number of patients300250200150100500≤ 5 > 5 ≤ 10 > 10 ≤ 15 > 15 ≤ 20 > 20 ≤ 25 > 25 ≤ 30 > 30 ≤ 35 > 35 ≤ 40 > 40 Not recordedBreaths/minFigure 20. First hospital SpO 2350Number of patients300250200150100500< 80 ≥ 80 < 85 ≥ 85
6Airway and breathingFigure 21. First ABG pH measurements350300Number of patients250200150100500≤ 7.15 > 7.15≤ 7.25> 7.25≤ 7.35> 7.35≤ 7.45pH> 7.45≤ 7.55> 7.55 NotrecordedFigure 22. First ABG PaO 2measurements350300Number of patients250200150100500≤5 >5≤10 >10≤15 >15 Not recordedPaO 2 (kPa)65
CHAPTER 6 - Airway and breathingFigure 23. First ABG PaCO 2measurements350300Number of patients250200150100500≤ 3 > 3 ≤ 4 > 4 ≤ 5 > 5 ≤ 6 > 6 ≤ 7 > 7 ≤ 8 > 8 ≤ 9 > 9 NotrecordedPaCO 2 (kPa)One of the challenges in the trauma patient can be provisionof an adequate airway 9 and tracheal intubation is frequentlya much more diffi cult procedure in the trauma patient 10 .Table 54 shows that in 56/753 (7.4%) cases, the advisorssaw evidence of diffi culty in obtaining an adequate airway.In 42 cases it was not possible to assess this. Of interest waswhether this was associated with the grade or experienceof personnel involved. Unfortunately, the information on thepersonnel involved was so poorly documented, thatno comment can be made on this relationship.Table 54. Evidence of difficulty in obtaining an airwayNumber of patients %Yes 56 7.4No 697 92.6Subtotal 753Insuffi cient data 42Total 795The group of patients who are diffi cult to intubate may havedifferent injuries, or a greater severity of injury, compared tothe group in whom there was no diffi culty with intubation.The mortality rate at 72 hours in the group of patients withairway diffi culty was 25% (14/56) compared with 13.6%(95/697) in the non-diffi cult group. However, it is not clear ifthere was any direct causal relationship between the diffi cultywith airway provision and mortality.Advisors were asked to make an overall assessment of themanagement of the airway and breathing. From Table 55it can be seen that this was considered unsatisfactory in52/741 cases (7%) where the data could be assessed.Table 55. Satisfactory airway managementNumber of patients %Yes 689 93.0No 52 7.0Subtotal 741Insuffi cient data 54Total 79566
6Airway and breathingCervical spine managementThe National Institute for <strong>Health</strong> and Clinical Excellence(NICE) guidance on management of head injuries 11recognises the problems of cervical spine imaging in somecircumstances and states that:“The current initial investigation of choice for thedetection of injuries to the cervical spine is the plainradiograph. Three views should be obtained and be ofsuffi cient quality for reliable interpretation. However, incertain circumstances CT is preferred.• GCS below 13 on initial assessment,• has been intubated,• plain film series is technically inadequate (forexample, desired view unavailable), suspiciousor definitely abnormal,• continued clinical suspicion of injury despitea normal x-ray,• the patient is being scanned formulti-region trauma”.All severely injured patients who undergo CT imaging of thehead, or other body parts, should have CT imaging of thecervical spine performed at the same time.Table 56. Prehospital spine immobilisationNumber ofpatients %Cervical spine 32 9.6<strong>Who</strong>le spine 45 13.6Cervical spine & whole spine 255 76.8Subtotal 332Neither documented 172Total 504Table 56 shows data on what protection was given to thecervical spine, and whole spine, in the prehospital phase(data from PRF).Of the 172 patients with no cervical spine immobilisationdocumented in the prehospital phase 69 had cervical spineimmobilisation on admission to the emergency department(40.1%).Table 57 shows the advisors’ assessment of measures tocontrol the cervical spine. Overall there was concern that in55/660 (8.3%) cases where it could be assessed the cervicalspine was not adequately managed. In 135 cases there wasinsuffi cient data for the advisors to make an assessment.Table 57. Appropriate control of cervical spine (advisors’ opinion)Yes No Subtotal Insufficient data TotalPrehospital 332 6 338 35 373In hospital 166 15 181 29 210Subtotal 498 21 519 64 583Not recorded 107 34 141 71 212Total 605 55 660 135 79567
CHAPTER 6 - Airway and breathingTable 58 shows reasons for advisors’ concerns.Table 58. Reasons for advisors’ concerns withregard to inappropriate control of cervical spineNo evidence of protection 22Delay in protection 5Not appropriately cleared 11Needed imaging 3Unable to fi t collar 4Other 10Total 55Imaging and clearance of the cervical spine was oftencommented on during the peer review process. There werefrequent problems with adequate imaging of the cervical spinein unconscious patients. There were often multiple attemptsat plain x-rays of the cervical spine, even in those patientswho were undergoing CT scanning of another body part.Reluctance to provide CT imaging of the cervical spine at thesame time as head CT scan was commonly encountered.Case study 1A young patient was admitted following a motorvehicle crash. Initial Glasgow Coma Score was 5 andthe right pupil was fi xed and dilated. The patient wastransferred for a CT head scan which showed somecerebral contusions and swelling but no lesion requiringneurosurgical intervention. Given the mechanism ofinjury there was concern that the cervical spine may alsohave been damaged. No CT of the cervical spine wasperformed; instead the patient was transferred back tothe emergency department to have plain x-rays of thecervical spine. Despite several attempts, plain x-raysprovided inadequate views of the whole cervical spineand the patient was then transferred back to the CTscanner for CT imaging of the cervical spine.The clinical scenario in Case study 1 was not uncommon.Key findingsOne in eight patients arrived at hospital with eithera partially or completely obstructed airway.Prehospital intubation failed on 11/85 attempts (12.9%).131 patients were intubated either on admission orwithin the fi rst 30 minutes after admission to hospital.Data on grade of medical staff performing trachealintubation was poorly documented and not available in223/362 cases (61.6%).Management of the airway was consideredunsatisfactory in 52/741 cases (7%).The management of the potentially unstable spine wasconsidered unsatisfactory in 55/660 cases (8.3%).RecommendationsThe current structure of prehospital management isinsuffi cient to meet the needs of the severely injuredpatient. There is a high incidence of failed intubationand a high incidence of patients arriving at hospital witha partially or completely obstructed airway. Changeis urgently required to provide a system that reliablyprovides a clear airway with good oxygenation andcontrol of ventilation. This may be through the provisionof personnel with the ability to provide anaesthesiaand intubation in the prehospital phase or the use ofalternative airway devices. (Ambulance trusts)CT scanning of the cervical spine should be performedin adult patients who have any of the following features:• GCS below 13 on initial assessment• has been intubated• is being scanned for multi-region trauma(Radiology heads)68
6Airway and breathingReferences1. Gorman DF, Teanby DN, Sinha MP, Wotherspoon J, BootDA, Molokhia A. Preventable deaths among major traumapatients in Mersey Region, North Wales and the Isle ofMan. Injury 1996; 27:189–922. Esposito TJ, Sanddal ND, Dean JM, Hansen JD,Reynolds SA, Battan K. Analysis of preventable pediatrictrauma deaths and inappropriate trauma care inMontana. The Journal of <strong>Trauma</strong> 1999; 47:243–5110. Dunham CM, Barraco RD, Clark DE, Daley BJ, Davis FE3rd, Gibbs MA, Knuth T, Letarte PB, Luchette FA, OmertL, Weireter LJ, Wiles CE 3rd; EAST Practice ManagementGuidelines Work Group. Guidelines for emergencytracheal intubation immediately after traumatic injury.J <strong>Trauma</strong> 2003; 55:162-19711. National Institute for <strong>Health</strong> and Clinical Excellence. DraftNICE head injury guidance 2007 – http://guidance.nice.org.uk/page.aspx?o=267085&c=915223. Papadopoulos IN, Bukis D, Karalas E, Katsaragakis S,Stergiopoulos S, Peros G, Androulakis G. Preventableprehospital trauma deaths in a Hellenic urban healthregion: an audit of prehospital trauma care. The Journalof <strong>Trauma</strong> 1996; 41:864–94. Hussain LM, Redmond AD. Are prehospital deaths fromaccidental injury preventable? BMJ 1994; 23:1077–805. Cales RH, Trunkey DD. Preventable trauma deaths.JAMA 1985; 254: 1059-636. Anderson ID, Woodford M, Donbal FT, Irving M.Retrospective Study of 1000 Deaths from Injury inEngland and Wales. BMJ 1989; 296:1305-87. Lockey D, Davies G, Coats T. Survival of trauma patientswho have prehospital tracheal intubation withoutanaesthesia or muscle relaxants: observational study.BMJ 2001;323:1418. An Acute Problem? National Confi dential Enquiry intoPatient Outcome and Death. 2005.http://www.ncepod.org.uk9. Boegtz MS, Katz JA. Airway management of the traumapatient. Semin Anaes 1985; 4:114-2369
CHAPTER 7 - Management of circulationIntroductionThe importance of haemorrhage control after injury is crucial.Best published evidence suggests that 30-40% of earlytrauma deaths are directly attributable to haemorrhage 1,2 .The American College of Surgeons Committee on <strong>Trauma</strong>Multiple Outcome Study has estimated that 62% of allin-hospital trauma deaths occur within the fi rst four hours,of which haemorrhage is either the primary cause or amajor contributing factor 3 . Not only does haemorrhagecontribute directly to early mortality, but blood loss leadingto hypotension is a major factor in the development ofsecondary brain injury 4,5 as well as contributing signifi cantlyto late trauma deaths from multi-organ failure 6,7 .Shock is a condition of inadequate end-organ perfusion.In the severely injured patient, shock may be multifactorial,but haemorrhage is the leading aetiology. In the shockedpolytrauma patient, the physiologic and metabolic reservecan quickly become exhausted, leading to decompensationand a deadly triad of hypothermia, coagulopathy andacidosis, all of which are independent prognostic indicatorsof outcome 8-13 . Treatment of these patients is aimed atpreventing or reversing this metabolic derangement byrecognising fi rstly that haemorrhage exists (preferentiallybefore decompensation), followed by timely intervention toarrest the bleeding and restore circulating volume, and henceoxygenation, to the tissues. Such timely management isassociated with improved patient outcomes 14,15 .The management of haemorrhage should begin in theprehospital fi eld and continue right through the hospitalsystem in a continuous process of assessment, treatmentand reassessment in a timely, co-ordinated fashion. Modern,dedicated trauma systems and major trauma centreshave developed out of a need for rapid transportation,assessment and treatment of the bleeding patient. Suchdedicated shock-trauma systems are associated with shorterprehospital times 16-18 , shorter throughput times to defi nitivecare at an appropriate facility 19,20 and better outcomes forthe severely injured patient 16, 21-24 . Nevertheless, the majorityof preventable deaths after injury occur from unrecognisedand hence untreated haemorrhage, particularly within theabdominal cavity 25-28 making it perhaps the single mostimportant reversible cause of death in the trauma population.Defi ning the point at which a patient becomes ‘shocked’ isdiffi cult as bleeding patients are often in a state of dynamicphysiologic fl ux. However, recognition of ongoing bleedingis the fi rst step in management. The Advanced <strong>Trauma</strong>Life Support (ATLS) course has become a well-recognisedand accepted paradigm in the initial management of thebleeding patient. Although the optimum end points foreffective resuscitation are less clear clinically 29,30 , currentpractice in the acute assessment of the injured patient isbased on a dictum of readily available and measurableparameters such as blood pressure, pulse rate, respiratoryrate, capillary refi ll, oxygen saturations and GlasgowComa Score. This has formed the basis for the format ofquestions in the management of circulation after injury forthis <strong>NCEPOD</strong> study. These are simple bedside assessmentswhich may be repeated, and aim to recognise the bleedingpatient early. In the physiologically normal, stable patientwho has not decompensated, time allows for more detaileddiagnostic workup for occult bleeding and organ injury.Simple, rapidly performed tests should also be performedearly in management that may refl ect both regional andglobal hypoperfusion including; pH, lactate, base defi cit andbicarbonate levels 31-36 .The modern approach to the management of haemorrhageafter injury has evolved greatly in the two decades with theadvent of better evidence based practice. Older diagnostictests, such as diagnostic peritoneal lavage (DPL) have nowbeen largely superseded by other imaging techniques suchas bedside ultrasound (focussed abdominal sonography fortrauma (FAST)) 37-39 and more judicious use of CT scanningfor the physiological normal and stable patient. In many70
7Management of circulationways, CT scanning is the ideal non-invasive test as long asthe patient’s condition allows. As a result many injuries cannow be safely managed conservatively or non-operatively 40,41 .Advances in radiology have allowed a greater proportion ofbleeding patients to undergo successful angioembolisationof bleeding arterial vessels, especially for injuries that aretraditionally diffi cult to manage operatively or are associatedwith a high mortality 42,43 .Other important standards of care have now becomecommonplace for the exsanguinating trauma patientsubgroup. These approaches, which are almostcounterintuitive to classical surgical dogma, includehypotensive resuscitation and damage control surgery.These concepts place a much greater emphasis onpermissive blood pressure control at a subnormal butsurvivable level, followed by rapid, intraoperative control ofhaemorrhage in a staged fashion and less on diagnosticworkup and defi nitive treatment of injuries during the earlystages of treatment. Both concepts have been associatedwith higher survival rates for the exsanguinating subgroup ofinjured patients 44-46 .Despite the modern approach to the bleeding patient, thereis still one concept that has remained unchanged. Bloodis a precious commodity and early haemorrhage control,whether it occurs naturally or after iatrogenic interventionsuch as angioembolisation or intraoperatively by a surgeon,is still paramount in achieving good patient outcomes. Thus,effective and timely haemorrhage recognition and controlmay be the single most important step in the emergencymanagement of the severely injured patient.ResultsInitial haemodynamic assessmentThe casenotes available identifi ed that assessment ofpulse, blood pressure, capillary refi ll and temperature weremeasured on arrival at hospital in 95.4%, 95.7%, 31.6% and53.2% of cases respectively (Figure 24).Figure 24. Measurements in hospital800Number of patients7006005004003002001000Blood pressure Pulse Capillary refill Temperature FluidYesNot recorded71
CHAPTER 7 - Management of circulationFigure 25. Appropriate fluid resuscitation to the degree of shockNumber of patients7006005004003002001000Yes No Insufficient dataFluid therapyFluids were administered to 638/795 (80.3%) patients.Appropriateness of fluid therapyIt was assessed by the advisors that fl uid resuscitation wasappropriate in 93.2% (602/646) of patients and inappropriatein 44/646 cases (6.8%).In 16 cases it was considered that there was very aggressivefl uid therapy and that too much crystalloid was given. In fi vecases it was considered that blood, rather than continuedcrystalloid, should have been transfused, as there was verysignifi cant haemorrhage. In 21 cases it was considered thatinsuffi cient fl uid was given.Case study 2A young back seat passenger was involved in a highspeedroad traffi c collision. Glasgow Coma Score was14 on admission. A CT head scan excluded signifi canthead injury. Haemoglobin level fell from 12 to 6 overthree hours. The eventual injuries identifi ed were: pelvicfracture; splenic and renal lacerations; and mediastinalhaematoma. There was only one measurement of bloodpressure in the fi rst hour of admission and no IV access.When the blood loss was recognised, the patient wasover transfused with six litres of crystalloid and threeunits of blood.72
Management of circulationFigure 26. CT scan of the chest, abdomen or pelvis performed300250Number of patients200150100500Yes No Not answeredInvestigation of haemorrhageIt is often the case that an experienced trauma surgeon willidentify patients who need an immediate trauma laparotomysimply by the nature of the trauma and their failure torespond to fl uid therapy. In these cases further investigationmay be unnecessary and delay the time to defi nitive care,which is associated with poorer outcomes.Some patients will require further investigation and optionsinclude DPL, FAST or CT scanning. The availability of theseoptions is described in the organisational chapter. Whilst theuse of DPL is falling as a consequence of better access tomore sophisticated imaging, only one in three emergencydepartments had access to FAST.Use of investigationsClinicians completing the A&E questionnaire indicated that254/495 (51.3%) patients had a CT scan of the chest and/or abdomen and/or pelvis for the assessment of injuries andpotential haemorrhage. For 18 patients this question was notanswered (Figure 26).For the large majority of patients (185/241; 76.8%) thereason given for not scanning the chest, abdomen or pelviswas because it was not clinically indicated. However, 22patients did not have a CT scan as they were considered toounstable to be transferred to the CT scanner. For a furtherthree patients it was indicated that they were taken straightto theatre. There was one case where a scan could not beperformed as the CT scanner was broken.The percentage of patients requiring CT for investigationfor haemorrhage was found to be higher on assessmentof the casenotes (483/795; 60.8%) compared to thatreported in the A&E questionnaire. This was simply becauseof the difference in the returned documentation (513 A&Equestionnaires v 795 sets of casenotes), there were no cases73
CHAPTER 7 - Management of circulationfor which a discrepancy was found between the casenotesand A&E questionnaire. Three hundred and ninety threepatients had a CT alone and 90 patients had a CT plusanother investigation. Other investigations for haemorrhage,such as FAST, were performed alone on 66 patients.With advances in CT scanning it is possible to obtainrapid and detailed information on injuries and site ofhaemorrhage. If CT scanning is appropriately co-located withthe emergency department and suitably staffed, then thisimaging modality has the potential to provide information onall but the most unstable patients. There is now emergingliterature showing the use of whole body CT scanning inthe multiple injured patient can reveal unsuspected injuries,locate the source of haemorrhage, speed up defi nitive careand reduce additional unnecessary investigations. <strong>Who</strong>lebody multi-sliced CT scanning with contrast should becomeroutine in the patient with multiple injuries. There is probablyno role for chest x-ray, pelvic x-ray and other plain fi lms if thepatient is to undergo whole body CT scanning as these plainfi lms will delay defi nitive investigation.The advisors assessed the necessity of a CT scan forhaemorrhage, for each patient. Table 59 shows thesedata and demonstrates that there was general agreementbetween the clinical decisions and the advisors’ opinions.However, in 21/457 (4.6%) cases advisors judged that a CTscan was performed unnecessarily. In addition it was judgedthat in 30/309 (9.7%) cases a CT scan was indicated, butwas not performed.Table 59. Advisors’ opinion on the necessity of aCT scan for haemorrhageCTscanCT necessaryYes No Subtotal InsufficientdataTotalYes 436 21 457 26 483No 30 279 309 3 312Total 466 300 766 29 795Time to CT scanningIn those cases where the time to CT scan could bedetermined from the casenotes, the average time taken for aCT scan after arrival in hospital was 138 minutes (2.3 hours)in those patients who only had a CT scan to investigatehaemorrhage and 181 minutes (3.0 hours) in patients whohad a CT scan and another investigation.Long time delays to the CT scanner frequently occurred(Figure 27). This is likely to have major clinical implicationsand ultimately be detrimental to patient outcome. Therefore,hospitals admitting severely injured patients must providemore timely access to this important imaging modality.Timeliness of CT scanningIn 55/254 cases, the clinician completing the A&Equestionnaire indicated that there was a delay to CTscanning. Twenty out of these 55 delays were due theinstability of the patient. The remaining 35 cases weredelayed due to organisational factors.Awaiting radiology staff was a major source of delay (Figure28). This occurs as it is unusual for any hospital in the UKto have resident CT radiographers, unlike North America,Australasia, the Far East or mainland Europe where thiswould be considered normal. The lack of the timely presenceof CT radiography staff is a major issue and an apparentweakness of the multidisciplinary team required to providerapid defi nitive care to the severely injured patient.Even the cases where the reason for delay was cited as‘patient instability’ may be contributed to organisationalfactors: consultant involvement was variable (especially out ofhours) and junior medical staff may have been more reticentthan consultants to move potentially unstable patients to theCT scanner. Furthermore, the location of the CT scanner may74
7Management of circulationFigure 27. Time to CT scan from arrival at hospital120100Number of patients806040200≤ 1 > 1 ≤ 2 > 2 ≤ 3 > 3 ≤ 4 > 4Time (hours)Figure 28. Reason for delay in CT scan (data from the A&E questionnaire)25Number of patients20151050Patient notstable enoughAwaitingradiology staffPatient notstable enoughand awaitingradiology staffAwaitingaccess to CTReasonAwaitingsuitablemedical staff toaccompanypatientOtherNot answeredchange the threshold for making the clinical decision thatthe patient is stable enough to scan: it is clearly easier andsafer if the CT scanner is close to the emergency departmentrather than in a remote area. In Europe, CT scanners are nowbeing installed into resuscitation rooms within the emergencydepartment to provide a comprehensive combinedresuscitation/investigation area.The philosophy of care that ‘unstable’ patients should notbe taken to the CT scanner is widely accepted but notbased on any evidence. It is common sense that an unstablepatient (i.e. a bleeding patient) will only be stabilised bystopping the bleeding. Delaying surgery or scanning ‘towait for stabilisation’ does not make sense. If the patient isconsidered too unstable for CT scan then transfer to theatreis required instead.75
CHAPTER 7 - Management of circulationCase study 3An elderly patient was involved in a road traffi c collision.The patient arrived at hospital speaking, pulse 120 butblood pressure was unrecordable. The patient becameagitated and was intubated. A chest x-ray, pelvicx-ray and abdominal ultrasound were performed. Theultrasound of the abdomen revealed a splenic injuryand free fl uid in the peritoneal space. The patient wasthen transferred to CT for chest, abdomen, head andspine. During this time the patient was unstable andreceived seven litres of fl uid and fi ve units of blood.Following CT scanning, the patient was transferred tocritical care to be stabilised prior to laparotomy andthoracotomy. At surgery splenic and liver injuries werepacked and a diaphragmatic tear repaired. The patientreturned from theatre unstable despite inotropic supportand subsequently arrested and died. The casenotesdid not document any consultant involvement in themanagement of this patient and the advisors believedthat this was an avoidable death.Appropriateness of CT scanningIt was judged by the clinical advisors that a CT scan wasnecessary in 466 of the cases. Seventeen patients did nothave a CT when the advisors thought that it was required. Afurther 21 cases had a CT scan but it was assessed as beingunnecessary.Reasons for assessment that the CT scan was unnecessary(21cases) were:• The patient was shocked with obviousintraperitoneal haemorrhage and it was felt thatimmediate surgery, rather than imaging, wasrequired (five cases)• FAST had revealed free fluid and it was felt that nofurther imaging should have been required prior tosurgery (five cases)• No indication for imaging (six cases)• No reason was supplied for this assessment(five cases).Appropriateness of assessment ofhaemorrhageIn general it was assessed that the possibility ofhaemorrhage was investigated satisfactorily in 90.9%(610/671) of cases. However, in 61/671 cases (9.1%) itwas considered that the possibility of haemorrhage was notinvestigated satisfactorily. In 124 cases there was insuffi cientinformation to assess this.76
7Management of circulationInterventionsOne hundred and ten patients underwent surgery or furtherprocedures for the control of haemorrhage.Procedures performed to manage haemorrhageThe procedures performed to manage haemorrhage areshown in Figure 29. The majority of patients who wereoperated on to manage abdominal trauma – 67/110 (60.9%)required a laparotomy.Interventional radiology has an increasing role to play in themanagement of the multiple trauma patient 44 and it wasnoted that this was undertaken in only one case.Grade of surgeonFifty seven out of 73 (78%) operations, where the gradecould be determined, were performed by consultants(Table 60).Table 60. Grade of operating surgeonNumber of patients %Consultant 57 78.1SpR 16 21.9Subtotal 73Insuffi cient data 37Total 110The infrequent use of interventional radiology is likelyto refl ect the lack of 24 hour availability of interrentionalradiology consultants who possess the necessary expertiseto perform these procedures. Such factors should beconsidered and taken into account when planning regionaltrauma services.Figure 29. Procedure performed for haemorrhage control8070Number of cases6050403020100LaparotomyThoracotomyOrthopaedicCraniotomy/evacuationVascular repairInterventional radiologyOtherNot answered77
CHAPTER 7 - Management of circulationAppropriateness of surgeonThe advisors agreed that the experience of the surgeonwas appropriate in 63/73 of the cases for which the gradecould be determined. However, for 37/110 cases, poordocumentation, particularly of the grade of the surgeonprevented judgement on the appropriateness of thesurgeon’s experience.Time to surgeryIt is important that defi nitive surgery is performed as soon aspossible after admission for the trauma patient with ongoinghaemorrhage.It was possible to calculate the time to laparotomy in 51/67cases.The mean time to laparotomy in the whole group was 384minutes (median 200 minutes).The mean time to laparotomy in the group of patientswho had a CT scan was 499 minutes. The mean time tolaparotomy in the group of patients who did not have a CTscan was 110 minutes.Table 61 and Figure 30 show the relationship between CTscanning and time to laparotomy.Table 61. Time to laparotomy (hours) relatedto CT useCT scanYes % No %≤ 1 2 5.6 5 33.3> 1 ≤ 2 4 11.1 6 40> 2 ≤ 3 4 11.1 3 20> 3 ≤ 4 8 22.2 0> 4 18 50 1 6.7Total 36 15Figure 30. CT scan for haemorrhage and time to laparotomy60Percentage of cases5040302010CT scanNo CT scan0≤ 1 > 1 ≤ 2 > 2 ≤ 3 > 3 ≤ 4 > 4Time to laparotomy (hours)78
7Management of circulationThe time to trauma laparotomy in the whole group didnot compare favourably to published data from a traumacentre 47 . In that study 47 median time to laparotomy was 127minutes compared to 200 minutes in this study. It can beseen that the use of CT scanning was associated with muchlonger times to trauma laparotomy but the reasons behindthis were not clear from the data collected.laparotomy was required. In 12 cases it was believed that theseverity of haemorrhage and urgency of the situation werenot appreciated. In two cases there was a delay in provisionof a staffed operating theatre.Lack of senior involvement and lack of appreciation of clinicalurgency have been found in many areas of medicine involvedwith acute care and the same problems have been found intrauma management.Timeliness of surgeryThe advisors were able to assess the timeliness of 87 ofthe 110 procedures for haemorrhage. The interventionsperformed were judged to be timely in 63/87 (72.4%) casesand delayed in 24/87 (27.6%) (Figure 31).Reasons given for delays in the initiation of the procedurewere multiple and often associated with the medical staffnot appreciating the urgency of the requirement to controlhaemorrhage. Five patients were believed to have hadunnecessary imaging (CT scan) as it was clear that a traumaImaging and delays to definitive careTable 62 shows more data for the patients who requiredsurgery and the relationship between imaging and timelinessof operation. As can be seen from the data, it was morelikely that delays were reported if imaging was performed asopposed to a clinical decision that the patient required animmediate operation. In the latter group, 19/20 patients wereconsidered to have received timely surgery.Figure 31. Procedure performed was timely (advisors’ view)7060Number of patients50403020100Yes No Insufficient data79
CHAPTER 7 - Management of circulationTable 62. Timely procedure and imaging for haemorrhageImaging for haemorrhageProcedure timely CT CT & Other Other None TotalYes 24 9 11 19 63No 12 5 6 1 24Subtotal 36 14 17 20 87Insuffi cient data 15 3 2 3 23Total 51 17 19 23 110Imaging has a major role to play in the management of theseverely injured patient. However, as assessment must berapid and accurate, imaging should be appropriate and thechoice of modality should refl ect which is more likely to givea rapid diagnosis. Inappropriate application of imaging ordelays in accessing imaging may delay defi nitive care.Operative management – summaryIt is clear from the above that there are concerns aboutthe operative management of the trauma patient. Whilst78.1% of patients for whom the grade of surgeon could bedetermined were operated on by a consultant, in 37 casesrequiring an intervention for haemorrhage there was nodocumentation of the surgeon’s grade. In 27.6% of casesit was felt that the operation was not performed in a timelyfashion.Outcome for patients requiring surgeryIn this sample 72 hour mortality for patients who had surgerywas 22.7% (25/110) whereas for those who did not havesurgery for haemorrhage it was 13.7% (92/670).It was observed that for those patients who had timelyintervention to control bleeding the 72 hour mortality was23.8% (15/63) compared with 33.3% (8/24) where theintervention was considered delayed.Overall managementThe overall management of the patients’ haemorrhage wasconsidered satisfactory by the advisors in 412/462 (89.2%).More importantly, 50/462 (10.8%) cases were identifi ed asnot having satisfactory management of haemorrhage. Noassessment was made by the advisors on the remaining333 cases, presumably as there was no clinical indication forhaemorrhage in these patients.80
7Management of circulationOverall management – operated casesTable 63 shows that 19/98 patients who required anoperation were considered to have unsatisfactorymanagement.Table 63. Overall management of haemorrhagewas satisfactoryNumber of patients %Yes 79 80.6No 19 19.4Subtotal 98Insuffi cient data 12Total 110In summary, there appeared to be problems with theinvestigation and control of haemorrhage. The areasof concern were principally the rapid recognition ofhaemorrhage and the institution of defi nitive management.There appeared to be delays to laparotomy and lack of initialconsultant input.The inability to rapidly CT scan trauma patients may relateto the proximity of the CT scanner to the emergencydepartment. Locating the scanner adjacent to, or as part of,the resuscitation suite may rectify this problem. We also notethe limited use of interventional radiology in the managementof bleeding patients. There is evidence that increased useof interventional radiology plays an important role in themanagement of blood loss in the severely injured patientand that integration of radiology staff and resources into thetrauma system may improve patient outcomes 44 .Key findings51.3% (254/495) of the patients had a CT scan of thechest, abdomen and pelvis for assessment of blood loss.In 55/254 (21.7%) cases there was a delay toCT scanning.In 61/671 cases (9.1%) it was felt that the possibility ofhaemorrhage was not investigated satisfactorily.110/795 patients (13.8%) underwent surgery or furtherprocedures for the control of haemorrhage.57/73 (78.1%) operations were performed byconsultants.In 37/110 (33.6%) poor documentation prevented thegrade of the surgeon being determined.The interventions performed were considered untimely in27.6% (24/87) of patients.Where operative intervention for haemorrhage wasconsidered timely the 72 hour mortality was 23.8%(15/63) compared to 33.3% (8/24) where the interventionwas considered delayed.19/98 (19.4%) patients from whom data wereavailable and who required surgery for management ofhaemorrhage had unsatisfactory overall management.81
CHAPTER 7 - Management of circulationRecommendationsRapid identifi cation of patients who require immediatesurgery for control of haemorrhage is essential. Ongoingfl uid requirements and instability identify a group ofpatients who require immediate intervention ratherthan further investigation. Local protocols shouldclearly identify the patient population for whom it isinappropriate to delay the surgery/intervention forreasons of ‘stabilisation’ or further investigation. (Hospitaltrusts, clinical directors and emergency physicians)<strong>Trauma</strong> laparotomy is potentially extremely challengingand requires consultant presence within the operatingtheatre. (Clinical directors)CT scanning will have an increasing role in theinvestigation and management of trauma patients. Inmajor centres, CT facilities should be co-located withthe emergency department to provide a combinedinvestigation/resuscitation area. (Hospital trusts)If CT scanning is to be performed, all necessary imagesshould be obtained at the same time. Routine use of‘top to toe’ scanning is recommended in the adulttrauma patient if no indication for immediate interventionexists. (Royal College of Radiology and radiologydepartment heads)Timely access to CT scanning is essential. CTradiographers should be available within 30 minutes ofthe patient arriving in hospital. In larger trauma centres,with a higher workload, CT radiographers should beimmediately available at all times.In the setting of remote radiology facilities and/or lack oftimely access to CT scanning, unstable patients shouldnot be taken to the CT scanner. These unstable patientsshould have immediate surgery. (<strong>Trauma</strong> team leader)References1. Shackford SR, Mackersie RC, Holbrook TL, et al. Theepidemiology of traumatic death: A population-basedanalysis. Arch Surg 1993;128:5712. Sauaia A, Moore FA, Moore EE, et al. Epidemiology oftrauma deaths: A reassessment. J <strong>Trauma</strong> 1995;38:185-1933. Champion HR, Copes WS, Sacco WJ, Lawnick MM,Keast SL, Bain LW, Flanagan ME, Frey CF. The Major<strong>Trauma</strong> Outcome Study: Establishing National Norms for<strong>Trauma</strong> Care. J <strong>Trauma</strong> 1990; 30: 1356-13654. Marmarou A, Anderson RL, Ward JD, et al. Impacton ICP instability and hypotension on outcome inpatients with severe head trauma. J Neurosurg1991;75(suppl):S59-S665. Chestnut RM, Marshall LF, Klauber MR, et al. The roleof secondary brain injury in determining outcome fromsevere head injury. J <strong>Trauma</strong> 1993;34:216-2226. Goins WA, Reynolds HN, Nyanjom D, et al. Outcomefollowing prolonged intensive care unit stay in multipletrauma patients. Crit Care Med 1991;19:3397. Moore FA, Moore EE. Evolving concepts in thepathogenesis of postinjury multiple organ failure. SurgClin North Am 1995;75:2578. Jurkovich GJ, Greiser WB, Lyterman A, et al.Hypothermia in trauma victims: an ominous predictorof survival. J <strong>Trauma</strong> 1987;27:1019-10249. Luna GK, Maier RV, Pavlin EG, et al. Incidence and effectof hypothermia in seriously injured patients. J <strong>Trauma</strong>1987;27:1014-101782
7Management of circulation10. Reed RL, Bracey AW, Hudson JD, et al. Hypothermiaand blood coagulation: dissociation betweenenzyme activity and clotting factor levels. Circ Shock1990;32:141-15211. Schreiber MA. Damage control surgery. Crit Care Clin2004;20:101-11812. MacLeod JB, Lynn M, McKenny MG, et al. Earlycoagulopathy predicts mortality in trauma. J <strong>Trauma</strong>2003;55:39-4413. Cosgriff N, Moore EE, Sauaia A, et al. Predicting lifethreateningcoagulopathy in the massively transfusedpatient: hypothermia and acidosis revisited. J <strong>Trauma</strong>1997;42:857-6214. Hill DA, West RH, Roncal S. Outcome of patients withhaemorrhagic shock: an indicator of performance in atrauma centre. J R Coll Surg Edinb 1995;40:221-415. Spahn DR, Cerny V, Coats TJ, et al. Management ofbleeding patients following major trauma: A Europeanguideline. Criti Care 2007;11:R1716. Demetriades D, Chan L, Cornwell E, et al. Paramedicvs. private transportation of trauma patients. Effect onoutcome. Arch Surg. 1996;131:133-817. Gervin AS, Fischer RP. The importance of prompttransport of salvage patients with penetrating heartwounds. J <strong>Trauma</strong> 1982;22:443-818. Gold CR. Prehospital advanced life support vs. ‘scoopand run’ in trauma management. Ann Emerg Med.1987;16:797-80119. Feero S, Hedges JR, Simmons E, Irwin L. Does out-ofhospitalEMS time affect survival? Am J Emerg Med.1995;13:133-520. Regel G, Stalp M, Lehmann U, Seekamp A. Prehospitalcare, importance of early intervention on outcome. ActaAnaesthesiol Scand. 1997;110(Suppl.):71-621. Ruteledge R, Fakhry SM, Meyer A, Sheldon GF, BakerCC. An analysis of the association of trauma centres withper capita hospitalisations and death rates from injury.Ann Surg 1993;218:512-2422. Eastman AB, Schwab CW, Annest JL, et al. Positionpaper on trauma care systems. J <strong>Trauma</strong> 1992;32:127-923. Shackford SR, Mackersie RC, Hoyt DB, et al. Impact ofa trauma system on outcome of severely injured patients.Arch Surg 1987; 122:523-724. MacKenzie EJ, Rivara FP, Jurkovich GJ, et al.A national evaluation of the effect of trauma-center careon mortality. N Engl J Med. 2006;354:366-7825. West JG, Trunkey DD, Lim RC. Systems of trauma care:A study of two counties. Arch Surg 1979;114:45526. Lowe DK, Gately HL, Goss JR, et al. Patterns of death,complication and error in the management of motoraccident victims: Implications for a regional systemof trauma care. J <strong>Trauma</strong> 1983;23:50327. Van Wagoner FH. A three year study of deaths followingtrauma. J <strong>Trauma</strong> 1961;1:40128. Tien HC, Spencer F, Tremblay LN, Rizoli SB, BrennemanFD. Preventable deaths from hemorrhage at a level 1Canadian trauma center. J <strong>Trauma</strong>. 2007; 62: 142-629. Porter JM, Ivatury RR. In search of the optimal endpoints of resuscitation in trauma: a review. J <strong>Trauma</strong>1998;44:908-1430. Revell M, Greaves I, Porter K. Endpoints for fl uidresuscitation in hemorrhagic shock. J <strong>Trauma</strong>2003;54:S63-S6783
CHAPTER 7 - Management of circulation31. Vincent JL, Dufaye P, Berre J, et al. Serial lactatedeterminations during circulatory shock. Crit Care Med1983;11:449-45132. Abramson D, Scalea TM, Hitchcock R, et al. Lactateclearance and survival following injury. J <strong>Trauma</strong>1993;35:584-58933. Davis JW, Kaups KL, Parks SN. Base defi cit is superiorto pH in evaluating clearance of acidosis after traumaticshock. J <strong>Trauma</strong> 1998;44:114-11834. Davis JW, Shackford SR, MacKersie RC, Hoyt DB. Basedefi cit as a guide to volume resuscitation. J <strong>Trauma</strong>1988;28:1464-146735. Davis JW, Kaups KL. Base defi cit in the elderly: a markerof severe injury and death. J <strong>Trauma</strong> 1998;45:873-87736. Fitzsullivan E, Salim A, Demetriades D, et al. Serumbicarbonate may replace the arterial base defi cit in thetrauma intensive care unit. Am J Surg 2005;190:961-96737. Porter RS, Nester BA, Dalsey WC. Use of ultrasound todetermine need for laparotomy in trauma patients. AnnEmerg Med 1997;29:323-33038. Rozycki GS, Ochsner MG, Schmidt JA, et al. Aprospective study of surgeon-performed ultrasoundas the primary adjuvant modality for injured patientassessment. J <strong>Trauma</strong> 1995;39:492-49839. Stengel D, Bauwens K, Sehouli J, et al. Systematicreview and meta-analysis of emergency ultrasounographyfor blunt abdominal trauma. Br J Surg 2001;88:901-91240. Velmahos GC, Toutouzas KG, Radin R, Chan L,Demetriades D. Nonoperative treatment of bluntinjury to solid organs. A prospective study. Arch Surg2003;138:844-85141. Velmahos GC, Toutouzas KG, Radin R, Chan L, Rhee P,Tillou A, Demetriades D. High success with nonoperativemanagement of blunt hepatic trauma. The liver is a sturdyorgan. Arch Surg 2003;138:475-48142. Cook RE, Keating JF, Gillespie I: The role of angiographyin the management of haemorrhage from major fracturesof the pelvis. J Bone Joint Surg Br 2002;84:178-18243. Hamill J, Holden A, Paice R, et al. Pelvic fracture patternpredicts pelvic arterial haemorrhage. Aust N Z J Surg2000;70:338-34344. Pryor JP, Braslow B, Reilly PM, Gullamondegi O,Hendrick JH, Schwab CW. The evolving role ofinterventional radiology in trauma care. J <strong>Trauma</strong>2005;59:102-445. Rotondo M, Schwab CW, McGonigal M, et al.Damage control: an approach for improved survival inexsanguinating penetrating abdominal injury. J <strong>Trauma</strong>1993;35:375-38346. Shapiro MB, Jenkins DH, Schwab CW, et al. DamageControl: collective review. J <strong>Trauma</strong> 2000;49:969-97847. Henderson KI, Coats TJ, Hassan TB, Brohi K. Audit oftime to trauma laparotomy. Br J Surg 2000; 87:472-47684
8CHAPTER 8 - Head injury managementHead injury managementIntroductionIn the UK, traumatic brain injury accounts for 15-20%of deaths between the ages of 5 and 35 years, with anincidence of 9 per 100 000 per year 1 . Outcome after headinjury depends upon the initial severity of injury and also theextent of any subsequent complications and how these aremanaged. Most of the patients who attend hospital aftera head injury do not develop life threatening or disablingcomplications in the acute stage. However, in a small butimportant group of patients, outcome is made worse bya failure to detect promptly or to deal adequately withcomplications 2-7 .There is a growing body of evidence that secondaryinsults occur frequently and exert a profound, adverseeffect on outcome from severe head injury. It is thereforerecommended that hypotension (Systolic BP
CHAPTER 8 - Head injury managementIn addition to a higher 72 hour mortality, head injured patientsrequired more critical care resources than non-head injuredpatients.Prehospital dataAssessment of neurological functionFigure 32 and Table 65 show the prehospital assessmentof conscious level in the patients who had suffered a headinjury. It should be noted that a patient report form (PRF) wasavailable for 320 of the 493 head injury group.Most patients had a Glasgow Coma Score (GCS) calculated,although some prehospital assessment was performed usingthe AVPU (Alert, Verbal, Pain, Unresponsive) scale. Eighteenpatients had no assessment of neurological dysfunction.Table 65. AVPU score in head injury groupNumber of patients %Alert 27 34.6Verbal 18 23.1Pain 13 16.7Unresponsive 20 25.6Subtotal 78GCS and/or AVPUnot recorded18Total 96It is important to document neurological status so that anychanges can be recognised and acted upon. Pupil sizeand reactivity should also be recorded when assessment ofconscious level is being made. NICE guidance recommendsthat the GCS should be used in all communications abouthead injured patients and that ambulance crews shouldbe fully trained in the adult and paediatric versions of theGlasgow Coma Scale 17 .Figure 32. Prehospital Glasgow Coma Score measurement in head injury group50Number of patients40302010015 14 13 12 11 10 09 08 07 06 05 04 03Glasgow Coma Score86
8Head injury managementTable 66. Prehospital SpO 2 (%) measurementsAlive Deceased Total % MortalityUnrecordable 1 4 5 80< 80 6 4 10 40≥ 80 < 85 9 5 14 35.7≥ 85 < 90 9 4 13 30.7≥ 90 < 95 24 5 29 17.2≥ 95 < 100 95 19 114 16.7100 47 8 55 14.5Subtotal 191 49 240 20.4Not recorded 65 15 80 18.8Total 256 64 320 20Oxygen therapy and oxygenationOxygen therapy is considered basic care in the severelyinjured patient. This is particularly relevant to the head injuredpatient where hypoxia signifi cantly increases the risk ofmortality 18-20 .Oxygen therapy was administered to only 78.1% (250/320)of patients with neurotrauma.Table 66 shows the prehospital SpO 2measurements.There were substantial numbers of patients who wereprofoundly hypoxaemic in the prehospital phase. In thisstudy 37/240 (15.4%) patients had SpO 2
CHAPTER 8 - Head injury managementThe patients who required prehospital intubation mightwell have been more severely injured (hence the need foradvanced airway intervention). Table 68 shows outcome dataat 72 hours post injury in the head injured patients.Table 68. Outcome at 72 hours by intubation in theprehospital phaseNotintubatedIntubatedFailedattempt% % %Alive 225 84.9 30 62.5 1 14.3Deceased 40 15.1 18 37.5 6 85.7Total 265 48 7The intubated group had a higher mortality than the nonintubatedgroup (37.5% v 15.1%). The failed intubation grouphad a mortality rate of 85.7%. Although these are very smallnumbers this group had a much worse outcome.Airway intervention and Glasgow Coma ScoreFigure 33 and table 69 relate airway intervention toprehospital assessment of conscious level. The greater thedegree of neurological injury, the greater the likelihood of theneed for intubation. All but two of the patients who had afailed intubation attempt had a GCS of 3.Table 69. AVPU score by intubationNotintubatedIntubatedFailedattemptAlert 0 0 0Verbal 0 0 0Pain 8 4 1Unresponsive 13 7 0Total 21 11 1Tables 70 and 71 show advisors’ assessment of prehospitalairway and ventilation management. In the opinion of theadvisors, all measures were taken to secure an adequateairway in 234/273 cases and all measures to ensureFigure 33. Prehospital Glasgow Coma Score and intubation for the head injury group50454035Not intubatedIntubatedfailed attemptNumber of patients30252015105015 14 13 12 11 10 09 08 07 06 05 04 03GCS/AVPU88
8Head injury managementadequate ventilation in 245/274 cases where suffi cient datawere available to make these assessments. This means thatthere were concerns with airway management in 39 (14.3%)cases and ventilatory management in 29 (10.6%) cases.Table 70. Adequate airwayNumber of patients %Yes 234 85.7No 39 14.3Subtotal 273Insuffi cient data 47Total 320Table 71. Adequate ventilationNumber of patients %Yes 245 89.4No 29 10.6Subtotal 274Insuffi cient data 46Total 320This incidence of inadequate airway management doesnot fi t with the current guidelines for the management ofsevere head injury which state that patients who havesuffered severe head injury should be intubated andreceive ventilatory support. From Figure 33, 103 patientswith GCS less than 9 were not intubated prior to arrival athospital. It may be that the advisors did not include all theunintubated patients in the inadequate airway managementgroup as they were aware of the constraints of the currentprehospital paramedic based system (with respect to abilityto anaesthetise and intubate patients).Despite the above comments on the advisors’ opinion ofthe incidence of airway problems, and the possible underreporting of this issue, Table 72 shows that the 72 hourmortality rate more than doubled for the group of patientsthat advisors judged had received inadequate airway orventilatory management prehospital.These data serve to underline the importance of adequateairway control and avoidance of hypoxia and hypercapnia.Table 72. Adequate airway/ventilation by outcome at 72 hoursAdequate airwayAdequate ventilationYes % No % Yes % No %Alive 192 82.1 23 59.0 199 81.2 16 55.2Deceased 42 17.9 16 41.0 46 18.8 13 44.8Total 234 39 245 2989
CHAPTER 8 - Head injury managementThere is a consistent message throughout this report thatsignifi cant problems are encountered in prehospital airwaymanagement:• Many patients arrived at hospital with anobstructed or partially obstructed airway,• There was a high rate of failed intubation in theprehospital phase,• Most patients with acute severe head injury weretransported to hospital unintubated,• There was a high incidence of hypoxia andhypercapnia on admission to hospital,• Many patients were intubated in the immediateperiod after admission to hospital.It is known from the literature and has been shown in thisstudy that these problems are associated with a highermortality rate. This implies that there is the need to routinelymake available individuals with the skills and ability to provideanaesthesia and intubation to severely injured patients in theprehospital phase. This is likely to require the inclusion ofphysicians in the prehospital response team.Blood pressure and cerebral perfusionWhile the desirable level of blood pressure in the bleedingmultiple trauma patient is subject to some debate, it is clearthat hypotension worsens neurological outcome. Cerebralperfusion in patients with traumatic brain injury is criticallydependent on systemic blood pressure. The minimumacceptable level of systolic blood pressure recommendedby the Brain <strong>Trauma</strong> Foundation 20 is 90mmHg but even thisis insuffi cient to maintain an adequate cerebral perfusionpressure in the case of cerebral injury. The existence of bothhypoxia and hypotension in patients with traumatic braininjury is associated with a mortality rate of 75% 20 .Table 73 shows the prehospital systolic blood pressure in thehead injured patients. In 21/241 (8.7%) patients a systolicblood pressure less than the minimum level suggested by theBrain <strong>Trauma</strong> Foundation was recorded.Table 73. Systolic blood pressure (mmHg)Number of patients %< 90 21 8.7> 90 ≤ 120 72 29.9>120 148 61.4Subtotal 241Not Recorded 79Total 32090
8Head injury managementHospital dataPre-alertsPre-alerts allow the emergency department to provide arapid and appropriate response. In the head injured patient,where there is very strong linkage between avoidanceof secondary injury and good outcome, this rapid andappropriate response is particularly important. Figure 34shows the use of pre-alerts analysed by prehospital GCS.The use of pre-alerts was variable. Even in the patient groupwith a GCS of 8 or less (severe head injury) there were asubstantial number of patients arriving at hospital withouta pre-alert. Indeed, in the group with a GCS of 3, 22.4%(17/76) of patients arrived at hospital without a pre-alert.NICE guidance on this aspect of care states 17 :“Standby calls to the destination A&E Department should bemade for all patients with a GCS less than or equal to 8, toensure appropriately experienced professionals are availablefor their treatment and to prepare for imaging”.Data from this study showed that practice was falling wellshort of this guideline. Fifty nine out of 160 (36.9%) patients,in which it was recorded, with severe head injury did nothave a pre-alert. Delays to the amelioration of secondaryinsults, imaging and defi nitive surgery (if required) couldadversely affect outcome.Figure 34. Prehospital Glasgow Coma Score and documentation of an ambulance pre-alert120Number of patients10080604020015 13-14 9-12 4-8 3 NotrecordedGlasgow Coma ScoreYesNo91
CHAPTER 8 - Head injury managementAssessment of neurological functionon admissionFigure 35 shows the fi rst documented hospital GCS in thegroup of patients who had suffered a head injury.From Figure 35 it can be seen that 91 patients had minorhead injury (GCS 15), 99 had mild head injury (GCS 13-14), 63 had moderate head injury (GCS 9-12) and 215had severe head injury (GCS 3-8). Of these, 100 were fi rstassessed to be completely unresponsive (GCS 3). For theremaining 25 patients a GCS was not documented.The 72 hour mortality rate for each group is shown in Table74. The group of patients with GCS 3 had a much worseoutcome. It is well known that initial GCS is an independentpredictor of outcome.Table 74. Mortality rate by Glasgow Coma ScoreGlasgowComa Score Alive Deceased Total%Mortality03 51 49 100 49.004-08 98 17 115 14.809-12 56 7 63 11.113-14 97 2 99 2.015 87 4 91 4.4Subtotal 389 79 468 16.9Not recorded 17 8 25 32.0Total 406 87 493 17.6Figure 35. First hospital Glasgow Coma Score measurement in the head injury group120Number of patients10080604020015141312111009Glasgow Coma Score080706050403Not recorded92
8Head injury managementFrequency of neurological assessmentNICE guidance on this aspect of head injury managementstates 17 :“For patients admitted for head injury observationthe minimum acceptable documented neurologicalobservations are: GCS; pupil size and reactivity; limbmovements; respiratory rate; heart rate; blood pressure;temperature; blood oxygen saturation. Observationsshould be performed and recorded on a half-hourlybasis until GCS equal to 15 has been achieved.”Frequent assessment of neurological function is a key part ofthe management of the head injured patient. Rapid detectionof deterioration is important to allow timely investigation andintervention, if required. Table 75 shows how often a GCS wasdocumented in the fi rst four hours after admission to hospital.Table 75. Frequency of Glasgow Coma Scoremeasurements during the first four hoursafter admissionNumber of patients %0 41 8.31 92 18.72 98 19.93 73 14.84 44 8.95 29 5.96 27 5.57 18 3.78 13 2.6> 8 58 11.8Total 493While data was not collected about time to normalisationof GCS in this study, it appears from Table 75 that thefrequency of observations may have been falling far shortof this NICE recommendation, as there is the opportunity toperform eight sets of observations in the fi rst four hours.Airway status on admissionTable 76 shows airway status on admission to hospital forthe head injured group. Sixty six patients arrived at hospitalwith either a partially or completely obstructed airway. Thisrepresented 18.3% of the non-intubated patients (66/361).Table 76. Airway status on arrival for thehead injury groupNumber of patients %Clear 295 69.7Noisy 31 7.3Blocked 35 8.3Intubated 62 14.7Subtotal 423Not recorded 70Total 493Airway management in hospitalMany of these problems were addressed after arrival tohospital but there were 37 patients for whom the advisorsfelt that management of the airway and/or ventilation wasunsatisfactory in hospital (Table 77). These were primarilyconcerns over lack of timely intubation and controlof ventilation.93
CHAPTER 8 - Head injury managementTable 77. Overall airway management satisfactoryNumber of patients %Yes 417 91.9No 37 8.1Subtotal 454Insuffi cient data 39Total 493After admission, mortality at 72 hours in the groups withsatisfactory and unsatisfactory airway management was73/417 (17.5%) and 10/37 (27.0%) respectively.There were a substantial number of patients who had lessthan satisfactory management of airway and ventilation inboth the prehospital and hospital phase. These fi ndingsindicate the potential for secondary insults to occur. Themortality rate in the unsatisfactory group supported this.Admission pulse oximetry and blood gas analysisTable 78. SpO 2 (%) measurements in hospitalNumber of patients %< 80 8 1.8≥ 80 < 85 10 2.3≥ 85 < 90 7 1.6≥ 90 < 95 32 7.4≥ 95 < 100 184 42.4100 193 44.5Subtotal 434Not recorded 59Total 493Figures 36, 37 and 38 show the results of the fi rst arterialblood gas (ABG) analysis after hospital admission. As can beseen there were small, but appreciable, numbers of patientswho have signifi cant hypoxia (PaO 26kPa), hypocapnia (PaCO 215 Not recordedPaO 2 (kPa)94
8Head injury managementFigure 37. First documented ABG PaCO 2measurement250200Number of patients150100500≤ 3 > 3 ≤ 4 > 4 ≤ 5 > 5 ≤ 6 > 6 ≤ 7 > 7 ≤ 8 > 8 ≤ 9 > 9 NotrecordedPaCO 2 (KPa)Figure 38. First documented ABG pH measurement250Number of patients200150100500≤ 7.15 > 7.15≤ 7.25> 7.25≤ 7.35> 7.35≤ 7.45pH> 7.45≤ 7.55> 7.55 Notrecorded95
CHAPTER 8 - Head injury managementHypoxia, hypercapnia, hypocapnia and acidosis are knownto be secondary insults that can worsen outcome in the headinjured patient. Hypocapnia is also detrimental to the headinjured patient as it causes cerebral vasospasm and canexacerbate cerebral ischaemia. Clearly these physiologicalderangements are likely to occur in severely injured patients,therefore the aim of prehospital care and a well-organisedemergency department response should be to minimise andrapidly correct these changes.Given the importance of normoventilation and avoidance ofboth hyper and hypocapnia in the setting of traumatic braininjury the high number of patients without blood gas analysisis unacceptable.Figure 39. Glasgow Coma Score and intubation120Number of patients100806040PrehospitalHospitalNo evidence20015 13-14 09-12 04-08 03 NotrecordedGlasgow Coma Score96
8Head injury managementCarbon dioxide and outcomeTable 79 shows data on admission PaCO 2and 72 hourmortality and illustrates the relationship between hypercapniaand poor outcome.Table 79. PaCO 2 and 72 hour mortalityPaCO 2 Alive Deceased TotalMortality(%)≤ 3 3 0 3 0> 3 ≤ 4 21 3 24 12.5> 4 ≤ 5 76 15 91 16.5> 5 ≤ 6 72 10 82 12.2> 6 ≤ 7 37 9 46 19.6> 7 ≤ 8 14 5 19 26.3> 8 ≤ 9 6 3 9 33.3> 9 8 9 17 52.9Subtotal 237 54 291 18.6Not recorded 169 33 202 16.3Total 406 87 493 17.7Glasgow Coma Score and intubationHypoxia and hypercapnia may be precipitated by problemswith airway patency and/or ventilatory inadequacy. This ismore likely in the group of severe head injuries (GCS
CHAPTER 8 - Head injury managementCerebral swelling and corticosteroidsCerebral swelling and intracranial hypertension are otherimportant factors in secondary brain injury. There hasbeen a long-standing interest in the use of steroids tominimise cerebral oedema and reduce intracranial pressure.However, there are concerns over detrimental side effectscaused by steroid therapy and whether, in fact, steroidsconfer any outcome benefi t. A recent study has addressedthis question 22 showing that the use of corticosteroids intraumatic brain injury caused harm. A signifi cant increase indeath and disability was found in the corticosteroid group.There was no evidence that the effect of corticosteroidsdiffered by injury severity or time since injury. The conclusionwas that corticosteroids should not be used routinely in thetreatment of head injury.There were a small number of cases (six) within this current<strong>NCEPOD</strong> study where steroids were prescribed and given topatients with head injuries as part of a management strategyto prevent brain swelling and secondary injury. Clearly thisis not in line with current best evidence and cannot besupported or recommended by <strong>NCEPOD</strong>.Investigation of head injuryThe NICE guidance on management of head injuries 17 givesa list of indicators for head CT scan. The list below is takenfrom that guidance. Any patient who has suffered a headinjury with any of these factors should have a CT scan of thehead requested immediately.Indicators for CT scanning in head injury:• GCS less than 13 on initial assessment in theemergency department,• GCS less than 15 at two hours after the injury onassessment in the emergency department,• Suspected open or depressed skull fracture,• Any sign of basal skull fracture (haemotympanum,‘panda’ eyes, cerebrospinal fluid leakage from theear or nose, Battle’s sign),• Post traumatic seizure,• Focal neurological deficit,• More than one episode of vomiting,• Amnesia for events more than 30 minutesbefore impact.Figure 40. Head CT scan and Glasgow Coma Score200Number of patients15010050YesNot documented015 13-14 09-12 04-08 03Glasgow Coma Score98
8Head injury managementFigure 41. Time to head CT scan by Glasgow Coma Score40Number of patients353025201510501513-1409-1204-0803≤ 1 > 1 ≤ 2 > 2 ≤ 3 > 3 ≤ 4 > 4Time to CT scan (hours)It would appear that despite this guidance some patientswere not investigated appropriately. Forty-four patients witha GCS less than 13 had no evidence of head CT scanning.Without this essential investigation the scope of the injurycannot be delineated and any subsequent management planmay be sub-optimal.Most patients who had suffered a signifi cant head injuryhad a CT scan of the head (Figure 40). A small numberof patients with a depressed level of consciousness didnot have a CT head scan although the reasons for thisdecision were not clear. It may be that within the group ofpatients with a GCS of 3 there was no requirement for a CThead scan as the severity of the injuries led to the clinicalconclusion that death was inevitable or that death occurredbefore CT scanning could be undertaken.Table 80 shows the reasons, stated in the A&E clinicianquestionnaire, for not carrying out a CT head scan. In themajority it was felt that scanning was not clinically indicated.Table 80. Reasons why a CT was not performedNumber ofpatients %Not clinically indicated 128 88.9Patient not stable enough 14 9.7Unable to access CT 2 1.4Subtotal 144Not answered 11Total 155Timing of investigation of head injuryIn the event that a CT scan of the head is required, it shouldbe performed as rapidly as possible. This does not onlymean that a scan is performed in a timely fashion, but alsothat the images should be assessed and a report available.Figure 41 shows the time from admission to CT scananalysed by GCS. Few scans were performed within the99
CHAPTER 8 - Head injury managementfi rst hour after admission and some patients were not scanneduntil several hours after admission. While this may be lessof a concern for patients with mild head injuries it may wellbe that those with moderate to severe head injuries havedelays to recognition and management of remediable lesions.Unfortunately, as can be seen from Figure 41, delays to CTscanning were present across all categories of head injuryseverity. Thirty-two patients with severe head injuries had to waitmore than two hours for this investigation to be performed.The emergency medicine clinicians’ reasons for any delays toCT head scanning are shown in Table 81.Table 81. Reasons why there was a delay toa CT head scanNumber ofpatients %Patient not stable 22 29.3Awaiting radiology staff 28 37.3Awaiting access to CT 17 22.7Awaiting suitable medical staff 3 4.4Other 5 6.7The majority of cases were delayed because oforganisational factors (awaiting access to CT or awaitingsuitable medical staff). In only 22/75 cases was the delayconsidered to be due to patient instability. Again, theavailability of CT radiography and radiology staff needs to beconsidered.Even patient instability may be considered an organisationalfactor if one considers the grade of medical staff involved inthe early management of these patients. As shown earlier,consultant involvement was variable (especially out ofhours) and junior medical staff may be more reticent thanconsultants to move potentially unstable patients to the CTscanner. Furthermore, the location of the CT scanner maychange the threshold for making the clinical decision thatthe patient is stable enough to scan; it is clearly easier andsafer if the CT scanner is close to the emergency departmentrather than in a remote area.NICE gives guidance on the timing of CT scan after headinjury 17 . The guidance states that in those circumstancesdescribed earlier:Total 75Figure 42. Timeliness of CT scan by Glasgow Coma Score (advisors’ opinion)80Number of patients706050403020100YesNoInsufficient data15 13-14 09-12 04-08 03 Not recordedGlasgow Coma Score100
8Head injury management“CT imaging of the head should be performed (i.e. imagingcarried out and results analysed) within one hour of therequest having been received by the radiology department.”The practice demonstrated in this dataset fell well short of thatguidance. As a result there is the potential for delays in bothdiagnosis and subsequent management of reversible pathology.timely fashion. Patients with severe head injuries, whosemanagement is most time critical, did not appear to havemore timely investigations. Again it should be noted thatthe main reasons for delay were organisational, rather thanpatient related, factors.Interpretation of CT scansAdvisor assessment of investigationof head injuryThe advisors assessed whether a head CT scan was anecessary part of each patient’s management. Table 82shows these data and makes the point that there wasgeneral agreement between the clinical decisions and theadvisors’ opinions. However, in 23/539 cases it was thoughtthat a CT scan was performed unnecessarily. Also in 24/220cases a CT scan was indicated although this was notperformed: and it was felt that the lack of CT scanning mayhave missed potentially treatable pathology.Accurate interpretation of the CT scan is essential. Tables83 and 84 show the grade and specialty of cliniciansinvolved. The majority of images were reported byconsultant radiologists. These data were taken from the A&Equestionnaire and most likely refl ect the fi nal report of theCT scan. Most investigations performed, particularly out ofhours, had a provisional report written in the notes by a morejunior doctor.Table 83. Grade of clinician interpreting the CT scanNumber of patients %Consultant 196 59.9Table 82. Advisors’ opinion on the necessity ofa head CT scanCTscanCT necessaryYes No Subtotal InsufficientdataTotalYes 516 23 539 10 549No 24 196 220 26 246Total 540 219 759 36 795NCCG 1
CHAPTER 8 - Head injury managementTable 84. The specialty of the clinician interpretingthe CT scanNumber of patients %Radiology 312 94.8Emergencymedicine10 3.0Neurology 6 1.8Anaesthetics 1
8Head injury managementFigure 44. Location of consulted neurosurgeon60Number of patients5040302010OnsiteOffsiteNot documented015 13-14 09-12 04-08 03 Not recordedGlasgow Coma ScoreFigure 43 shows data on whether there was discussion withthe neurosurgical service. In the majority of cases where apatient suffered a head injury, a neurosurgical consultationwas performed. However, it was noted that 44/271 (16.2%)patients with moderate or severe head injuries had noevidence of neurosurgical involvement. Within this groupof 44 patients it is possible that consultation was notundertaken due to the extent of head and/or other injuriesleading to the conclusion that death was inevitable.As part of the peer review process, advisors were askedwhether a neurosurgical consultation was a necessary part ofeach individual case. Of the 155 cases where there was noevidence of neurosurgical involvement the advisors felt thatthis should have occurred in 28 cases (18.1%).Location of neurosurgical supportFigure 44 shows the location of the neurosurgical service inrelation to the admission location. More patients receivedoffsite neurosurgical support than onsite.These data suggest that 197/365 (54.0%) patients whorequired neurosurgical involvement were taken to hospitalsthat may not have had the necessary infrastructure (on siteneurosurgical expertise) to meet their needs. Given thetime critical nature of neurosurgical intervention in traumaticbrain injury this had the potential to introduce delaysinto defi nitive management, which may affect outcome.Although we accept that in many circumstances takingthe patient directly to a neurosurgical centre may be moreappropriate, consideration of the pattern and severity ofinjuries and the likely services required should be taken intoaccount when the prehospital clinicians are transportingthe severely injured patient to hospital. However, it doesappear that direct admission to a trauma centre compared tosecondary transfer is associated with a better outcome 25 andneurosurgeons and ambulance trusts should agree protocolson this aspect of care.103
CHAPTER 8 - Head injury managementTime to neurosurgical consultationThe availability of onsite neurosurgical support may affecttime to consultation and intervention. In 14 cases it was notknown if the consultation was on or offsite. These data areshown in Table 85.Table 85. Time (hours) to neurosurgical consultationAll (%) Onsite (%) Offsite (%)≤ 1 26 10.2 15 13.6 8 6.2>1≤2 56 22.1 24 21.8 30 23.1>2≤3 54 21.3 20 18.2 30 23.1>3≤4 32 12.6 7 6.4 24 18.5>4≤5 21 8.3 5 4.6 7 5.4>5≤6 14 5.5 13 11.8 8 6.2>6≤12 28 11.0 10 9.1 17 13.1>12 23 9.1 16 14.6 6 4.6Total 254 110 130Neurocritical care capacityThe supply of emergency neurosurgical beds in the UK islimited. A recent survey revealed that only 43 neurosurgicalintensive care beds are available for an overall estimatedpopulation of 63.6 million 26 . This shortfall can lead to delaysin patient transfer, and is symptomatic of larger resource andworkload issues for neurosurgery in the UK 27 . These largerresource problems have many implications for head injurycare, including delays obtaining a neurosurgical opinion atnight, or at the weekend.One consequence of this lack of capacity in neurosurgicalcritical care beds is that some patients may stay in their‘local’ critical care unit rather than be transferred to theneurosurgical centre. This may have an adverse effect onpatient outcome. In a recent study it was shown that patientswith severe head injury who were treated only in nonneurosurgicalcentres had a 26% increase in mortality and a2.15-fold increase (95% CI 1.77-2.60) in the odds of deathadjusted for case mix compared with patients treated at aneurosurgical centre 28 . This suggests that transfer to, andtreatment in, a neurosurgical centre is an important part ofthe management plan for patients with severe head injury.Case study 5A young patient was admitted to hospital after sustaininga head injury. Admission GCS was 5. CT headscanning revealed a large intracerebral haemorrhage,cerebral oedema and midline shift. Referral was madeto the regional neurosurgical centre at 01:15. Theneurosurgical SpR stated that there were no beds in theICU and advised that the patient be referred to anotherneurosurgical centre. After some diffi culty in contactingthe on call neurosurgeon, the patient was discussedwith the neurosurgical SpR at a second centre. Thisoccurred at 02:15. The neurosurgical SpR stated thatthey had beds available and would be prepared to takethe patient but that the opinion of whether transfershould occur should be made by the local neurosurgicalcentre that had no capacity to take the patient. A furthertelephone call was made to the local neurosurgicalcentre at 02:30 who felt that as they had no capacitythey could not comment on the patient care. At 03:00a second telephone call was made to the secondneurosurgical centre and at that point the neurosurgicalSpR requested that hard copies of the CT be sent tohim. Six more telephone calls occurred over the nextfew hours between the initial hospital and three differentneurosurgical centres. By 06:30 the patient, who wasstill in the emergency department, had fi xed and dilatedpupils and it was believed that death was the inevitableoutcome. The patient was admitted to ICU and aftera period of family discussion ventilatory support waswithdrawn. At no time was brain stem death confi rmedor considered. Organ donation, either heart beating ornon-heart beating, was never discussed.104
8Head injury managementWithin this current study there were many, albeit lessextreme, instances of diffi culties in contacting theneurosurgeon on call, lack of willingness to accept patientswith severe head injuries, lack of capacity in neurosurgicalcentres and clear lack of protocols to smooth the process ofcare between the local centres and the neurosurgical centre.Table 86 shows that 114 patients had a surgical procedureas a consequence of head trauma (23% of the head injuredpatients). The majority of this activity (48 cases) involved theinsertion of an intracranial pressure (ICP) monitoring device,with no further surgery in the fi rst 72 hours. A further 54operations were related to the evacuation of traumatic spaceoccupying lesions or decompressive craniectomy.Neurosurgical proceduresThe number of patients who undergo major neurosurgicalprocedures each year following a head injury is also unclear. Afi gure of around 4,000 patients per year for the UK as a wholehas been quoted 29 , but this may an overestimate. HospitalEpisode Statistics data for the 2000/2001 annual dataset indicatethat 398 patients in England underwent an operation to drainthe extradural space (OPCS code A40) and 2,048 patientsunderwent an operation to drain the subdural space (OPCScode A41) 30 . These fi gures do not include a number of otherneurosurgical procedures possible after head injury (including burrhole for chronic subdural haematoma or insertion of intracranialpressure monitors), and include some patients with a non-headinjury diagnosis. Thus, the routine data available does not allowfor a precise fi gure of neurosurgical volume after head injury forEngland and Wales, but points to a fi gure in the low thousands.Table 86. Type of surgery performedNumber ofpatients %Evacuation of subdural haematoma 20 17.5Evacuation of extraduralhaematomaEvacuation of intracerebralhaematoma / contusionInsertion of intracranialpressure bolt only22 19.37 6.148 42.1Elevation of fracture 7 6.1Decompressive craniectomy 5 4.4Other 5 4.4Total 114Grade of operating surgeonTable 87 shows the grade of clinician performing the surgery.Only 15.8% of interventions were documented as beingperformed by consultants.Table 87. Grade of surgeon performing the surgeryNumber of patients %Consultant 12 15.8SpR 56 73.7SHO 8 10.5Subtotal 76Not documented 38Total 114This was a lower level of consultant involvement than hasbeen seen in past <strong>NCEPOD</strong> studies 31,32 . Given the volumeof surgery performed annually as a result of head trauma 29this potentially represents a substantial amount of surgeryperformed by doctors in training. However, the insertion ofan intracranial pressure monitor is generally performed at thebedside and is likely to be an appropriate procedure to bedelegated to junior neurosurgical staff with suffi cient training.105
CHAPTER 8 - Head injury managementFor this reason Table 88 shows the grade of surgeon for thecases excluding insertion of an ICP monitor.Table 88. Grade of surgeon excluding insertionof an ICP monitorNumber of patients %Consultant 9 18.8SpR 38 79.2SHO 1 2.1Subtotal 48Not recorded 18Total 66Even when these more minor procedures have beenexcluded only 18.8% (9/48) of operations were documentedas being performed by a consultant.During expert and advisor group meetings to discuss thefi ndings in this study the issue of consultant neurosurgicalinvolvement generated signifi cant discussion. Whilst theinsertion of an intracranial pressure monitor may well bewithin the remit of appropriately trained junior staff, mostmajor neurosurgical procedures were being performed bythese same staff in training.The system of junior staff care is also changing: EuropeanWorking Time Directive, Modernising Medical Careers andthe Hospital at Night project have signifi cantly changed thelevel of junior staff experience and support from that availablein previous years.Given this discussion, it is felt that the low level of directconsultant involvement in the management of patients whorequire major neurosurgical procedures is undesirable andthat a much higher input is required.Time to neurosurgical interventionTable 89 shows time to surgery analysed by whether thepatient required a secondary transfer to another site to havethis surgery performed.Table 89. Time to surgery (hours)Onsite Transferred% %≤ 4 22 66.7 6 14.0>4 ≤ 8 9 27.3 23 53.5>8 ≤ 12 2 6.0 4 9.3>12 0 0 10 23.3Subtotal 33 43Not recorded 23 15Total 56 58The requirement for a secondary transfer signifi cantlyincreased the time to surgical intervention. Indeed, only6/43 patients requiring transfer had neurosurgery withinthe fi rst four hours after injury. Intensive head injury carebegins at the scene of the accident. It includes protectingthe airway and cerebral circulation which may involve theurgent removal of clots, but may also (or only) require theinsertion of pressure monitors to guide longer-term therapy.Rapid surgery is crucial for patients with intracerebralhaematomas requiring evacuation, where every moment’sdelay jeopardises eventual outcome, but is less vital forpatients requiring intracerebral pressure monitoring as partof the overall intensive care management of diffuse braininjury. For this reason, despite surgery occurring after fourhours in 11/33 (33.3%) of onsite patients and 37/43 (86.0%)of transferred patients, these operations were considered106
8Head injury managementtimely in 68/81 (84.0%). Of the 16% of cases where it wasfelt that surgery was not performed in a timely manner, 10/13required evacuation of clots or craniectomies where delaysare undesirable and have a negative impact on outcome(Table 90).This delay is in keeping with a recent study which showedthat the mean transfer time to a neurosurgical centre forpatients with an extradural haematoma and subduralhaematoma was 5.25 and 6 hours respectively 33 .Clearly these delays may affect outcome and this againraises the issue of transfer to an appropriate hospital inthe fi rst instance and reconfi guration of trauma servicesfor regions.Table 90. Timeliness of neurosurgeryNumber of patients %Yes 68 84.0No 13 16.0Subtotal 81Insuffi cient data 33Total 114Overall assessment of management of headinjured patientsThe advisors were asked to assess the overall managementof the patient using the grading system detailed in themethods section (Table 91).Table 91. Overall assessment ofhead injury managementNumber ofpatientsGood practice 205 41.6Room for improvement clinical 80 16.2Room for improvement organisational 114 23.1Room for improvement clinical and 46 9.3organisationalLess than satisfactory 25 5.1Insuffi cient data 23 4.7Total 493Less than half the patients (205/493) were thought to havereceived a standard of care that could be described as goodpractice. In 240/493 (48.7%) cases it was thought that therewas room for improvement in organisational and /or clinicalaspects of care. Of concern were the 25/493 (5.1%) caseswhere it was thought that patient management was lessthan satisfactory, signifying a signifi cant problem in thecare process.%107
CHAPTER 8 - Head injury managementKey findingsHead trauma is very common in the severely injuredpatient and has a negative impact on outcome.Secondary insults (hypoxia, hypercapnia andhypotension) are common and these are known toworsen eventual outcome (higher mortality and moresevere disability).Only 9/48 (18.8%) patients who had major neurosurgicalprocedures as a result of trauma were operated on byconsultant surgeons.Less than half of the severely injured patients whosuffered head trauma received a standard of care thatwas judged to be good practice.The prehospital management of the airway andventilation was inadequate in 14.3% and 10.6% of casesrespectively.In a small number of cases steroids are being used inthe routine management of the head injured patient,despite evidence that this therapy may cause harm.One in fi ve patients who required a head CT scan didnot have this performed in a timely fashion.Delays in CT scanning were primarily due toorganisational factors rather than patient factors.More than half of the patients who required neurosurgicaladvice or input were taken to hospitals where there wasno onsite neurosurgical service.Only 6/43 (14.0%) patients who required a secondarytransfer to access neurosurgical services had anoperation within four hours of injury.There were delays to neurosurgery in 13/81 (16.0%)cases. Most of these cases were evacuation of traumaticspace occupying lesions.108
8Head injury managementRecommendationsPrehospital assessment of neurological status should beperformed in all cases where head injury is apparent orsuspected. This should be performed using the GlasgowComa Scale. Pupil size and reactivity should also berecorded. (Ambulance trusts)A pre-alert should be made for all trauma patients witha GCS less than or equal to 8, to ensure appropriatelyexperienced professionals are available for theirtreatment and to prepare for imaging. (Ambulance trusts)Patients with severe head injury require early defi nitiveairway control and rapid delivery to a centre with onsiteneurosurgical service. This implies regional planningof trauma services, including prehospital physicianinvolvement, and reconfi guration of services. (Ambulanceand hospital trusts)Patients with severe head injury should have a CT headscan performed as soon as possible after admissionand within one hour of arrival at hospital. (<strong>Trauma</strong> teamleader and radiology heads)All patients with moderate or severe head injuryshould have case and CT fi ndings discussed with aneurosurgical service. (<strong>Trauma</strong> team lead)All patients with severe head injury should be transferredto a neurosurgical/critical care centre irrespective of therequirement for surgical intervention. (Strategic healthauthorities, hospital trusts, trauma team leaders)Consultant presence should be increased at operationsrequiring major neurosurgery. (Hospital trusts)References1. Teasdale GH. J Neurol Neurosurg Psychiatry 1995; 58:855-8872. Rose J, Valtonen S, Jennett B. Avoidable factorscontributing to death after head injury. BMJ 1977; 2:615-83. Jennett B, Carlin J. Preventable mortality and morbidityafter head injury. Injury 1978; 10: 31-94. Rockswold GL, Leonard PR, Nagib MG. Analysis ofmanagement in thirty-three closed head injury patientswho ‘talked and deteriorated’. Neurosurgery 1987; 21:51-55. Mendelow AD, Karma MZ, Paul KS, Fuller GA, GillinghamFJ. Extradural haematoma: effect of delayed treatment.BMJ 1979; I: 1240-26. Klauber MR, Marshall LF, Luerssen TG, FrankowskiR, Tabaddor K, Eisenberg HM. Determinants of headinjury mortality: importance of the low risk patient.Neurosurgery 1989; 24: 31-67. O’Sullivan MG, Gray WP, Buckley TF. Extraduralhaematoma in the Irish Republic: an analysis of 82 caseswith emphasis on delay. Br J Surg 1990; 77: 1391-48. Brain <strong>Trauma</strong> Foundation, American Association ofNeurological Surgeons, Joint Section on Neurotraumaand Critical Care. Guidelines for the management ofsevere head injury. J. Neurotrauma 1996; 13: 641-7349. The management of acute head injury: seminar papers.<strong>London</strong>: DHSS 1983109
CHAPTER 8 - Head injury management10. Guidelines for initial management after head injury inadults. Suggestions from a group of neurosurgeons. BMJ1984 288: 983-511. Report of the Working Party on Head Injuries. <strong>London</strong>:Royal College of Surgeons of England Commission onthe Provision of Surgical Services; 198612. Bartlett J, Kett-White R, Mendelow AD, Miller JD, PickardJ, Teasdale G. Recommendations from the Society ofBritish Neurological Surgeons. Br J Neurosurg 1998;12(4): 349-5213. The Royal College of Radiologists. Making the bestuse of a department of clinical radiology: guidelines forDoctors. 4th Ed. <strong>London</strong>; The College; 199814. Royal College of Surgeons of England. Report of theWorking Party on the Management of Patients with HeadInjuries. <strong>London</strong>: The College; 199915. Working Party of the British Paediatric Association andBritish Association of Paediatric Surgeons, Joint StandingCommittee in Childhood Accidents. Guidelines on theManagement of Head Injuries in Childhood. <strong>London</strong>:British Paediatric Association; 199116. Scottish Intercollegiate Guidelines Network: EarlyManagement of Patients with a head injury. 2007.– http://www.sign.ac.uk/guidelines/fulltext/46/index.html17. National Institute for <strong>Health</strong> and Clinical Excellence.Managing head injury: updated NICE guidelines.2007.– http://www.nice.org.uk/page.aspx?o=45535018. Chi JH, Knudson MM, Vassar MJ, et al. Prehospitalhypoxia affects outcome in patients with traumatic braininjury: a prospective multicenter study. J <strong>Trauma</strong>. 2006Nov; 61(5):1134-4119. Brain <strong>Trauma</strong> Foundation, American Association ofNeurological Surgeons, Joint Section on Neurotraumaand Critical Care. Guidelines for the management ofsevere head injury. J. Neurotrauma 1996; 13: 641-73420. Chestnut RM, Marshall LF, Klauber MR et al. The roleof secondary brain injury in determining outcome fromsevere head injury. J <strong>Trauma</strong>. 1993; 34(2):216-2221. Dunham CM, Barraco RD, Clark DE, et al.; EASTPractice Management Guidelines Work Group. Guidelinesfor emergency tracheal intubation immediately aftertraumatic injury. J <strong>Trauma</strong> 2003; 55:162-19722. Edwards P, Arango M, Balica L, et al. CRASHtrial collaborators. Final results of MRC CRASH, arandomised placebo-controlled trial of intravenouscorticosteroid in adults with head injury-outcomes at 6months. Lancet. 2005; 365(9475):1957-923. The Royal College of Surgeons of England. Report ofthe working party on the management of head injuries.<strong>London</strong>: RCS, 199924. Working party of the Neuroanaesthesia Society andAssociation of Anaesthetists. Recommendations forthe transfer of patients with acute head injuries toneurosurgical units. Neuroanaesthesia Society of GreatBritain and Ireland and the Association of Anaesthetistsof Great Britain and Ireland, 199625. Sampalis JS, Denis R, Fréchette P, Brown R, FleiszerD, Mulder D. Direct transport to tertiary trauma centersversus transfer from lower level facilities: impact onmortality and morbidity among patients with majortrauma. 1997 Aug;43(2):288-29526. Crimmins DW, Palmer JD. Snapshot view of emergencyneurosurgical head injury care in Great Britain andIreland. J Neurol Neurosurg Psychiatry 2000; 68: 8-13110
8Head injury management27. Ashkan K, Edwards RJ, Bell BA. Crisis in resources: aneurosurgical perspective. Br J Neurosurg 2001; 15:342-628. Patel HC, Bouamra O, Woodford M, King AT, YatesDW, Lecky FE. Trends in head injury outcome from1989 to 2003 and the effect of neurosurgical care:an observational study. Lancet. 2005; 29-Nov4;366(9496):1538-4429. Safe Neurosurgery 2000. A Report from the Society ofBritish Neurological Surgeons. Nelson MJ, SBNS, 35-43Lincoln’s Inn Fields, <strong>London</strong>30. Hospital Episode Statistics. 2000/2001. Departmentof <strong>Health</strong>31. Abdominal Aortic Aneurysm: A service in need ofsurgery? National Confi dential Enquiry into PatientOutcome and Death. 2005. http://www.ncepod.org.uk32. <strong>Who</strong> Operates When II? National Confi dential Enquiryinto Patient Outcome and Death. 2005.http://www.ncepod.org.uk33. Leach P, Childs C, Evans J, Johnston N, ProtheroeR, King A.Transfer times for patients with extraduraland subdural haematomas to neurosurgery in GreaterManchester. Br J Neurosurg. 2007 Feb; 21(1):11-5111
CHAPTER 9 - Paediatric careOrganisational dataInjury remains a leading cause of death in childhood. In theUK three million children present to emergency departmentseach year following injury. The majority of attendances atemergency departments are due to moderate or minorinjuries. The absolute numbers of severe injuries are low andthese patients present to a number of different hospitals.Therefore it is more diffi cult to maintain specifi c clinical skillsin the management of severe trauma in children.The injuries sustained by children differ from those of adultsand consequently there are signifi cant differences in theirpost-trauma management. In particular, the incidence ofhead trauma is more common in the paediatric population.The defi nitions of neonates, infants and children differedbetween hospitals. The maximum age of a neonate asdefi ned by the departments surveyed varied between 1 and24 months. The maximum age of infants varied from 12 to60 months. Two thirds of departments (110/183; 60.1%)Figure 45. Availability of an advanced paediatric life support provider resident or 24 hours a day100Number of sites9080706050403020HospitalA&E department100Yes, resident Yes, available Neither Not answeredFigure 46. Availability of paediatric specialties at hospitals that accept paediatric patients180Number of hospitals160140120100806040Yes No Not answered200Paediatric Anaesthetist Paediatrician Paediatric Surgeon112
9Paediatric caredefi ned children as being up to 16 years of age, but 9.8%(18/183) had a higher maximum age; the oldest being 19years of age.An Advanced Paediatric Life Support (APLS) provider wasresident or available 24 hours a day in 79.8% of hospitals(Figure 45).ProtocolsIt is recommended that protocols for the management ofpaediatric cases should be in place 1 . One hundred and fi ftyfi ve (84.7%) of the 183 sites for which an organisationalquestionnaire was returned to <strong>NCEPOD</strong> had up to dateguidelines for the management of paediatric trauma. Of the160 hospitals (87.4%) which accepted children for defi nitivecare, 23 (14.4%) did not have up to date guidelines for themanagement of children.Thirteen out of 22 (59.1%) sites that did not admit childrenfor defi nitive care had a bypass protocol in place in order toreduce the likelihood of a severely injured child being broughtto the hospital.If non-accidental injury is suspected in children, up todate guidelines on the management and referral of thesepatients should be in place. One hundred and seventy six(96.2%) hospitals had up to date guidelines on referral andmanagement of suspected non-accidental injury in children.Facilities and staffing in hospitals acceptingchildren for definitive careAs Figure 46 illustrates, the majority of hospitals acceptingpaediatric patients had a specialist in paediatric anaesthesiaand a consultant paediatrician; 70.6% (113/160) and 98.8%(158/160) respectively. Guidelines do not specify the needfor a paediatric surgical consultant at all hospitals acceptingchildren. Only 23.8% (38/160) of hospitals accepting childrenfor defi nitive care have a paediatric surgical consultant,suggesting that the transfer of patients to these sites forsurgery is often necessary.The Royal College of Surgeons of England guidelinesalso recommend that hospitals admitting children have afull range of appropriate resuscitation equipment 2 . Of theemergency departments at these hospitals 149/160 (93.2%)had a listed and checked mobile equipment kit to assist inthe resuscitation of children.It is recommended that emergency departments receivingchildren should have a children’s nurse available at all times.A Registered Sick Children’s Nurse (RSCN) was available at146/160 (91.3%) of hospitals accepting children. However,only 22 of these 146 hospitals (15.1%) had cover 24 hours aday, 7 days a week.Clearly there are diffi culties in providing all necessary staff forthe comprehensive management of the paediatric traumapatient. The data above shows problems with paediatricanaesthetic support and paediatric surgical support insome centres. This is in the context of the centralisationof many specialised paediatric services including surgery,neurosurgery and paediatric intensive care medicine.Some hospitals have acknowledged this fact by the use ofprotocols to avoid admitting severely injured children. Theuse of such protocols and close working within a network toprovide trauma care to children is required.It was recommended in the Better Care for the SeverelyInjured Patient Report 2 that “any hospital receiving and caringfor the severely injured child must have on-site support frompaediatrics’ and paediatric anaesthetists”.113
CHAPTER 9 - Paediatric careClinical dataAge rangeThere were 68 patients included in the study who were aged16 years of age or less.Most of the data analyses in the previous chapters wererepeated for this small subset of patients. Only in a very fewcases did the analysis show any different patterns from thewhole sample. The bulk of this report is therefore applicableto both adults and children and the analysis will not bepresented again for this group.Figure 47. Age range of patient sample140120Number of patients1008060402000-5 6-10 11-15 16-20 21-25 26-30 31-35 36-40 41-45 46-50 51-55 56-60 61-65 66-70 71-75 76-80 81-85 86-90 91-95Age (years)Figure 48. Overall assessment of care (advisors’ view)Percentage of patients in data set50403020100Good practiceimprovement -clinicalRoom forimprovement -clinicalRoom forimprovement -organisationalRoom forimprovement -clinical andorganisationalLess thansatisfactory>16 years≤16 yearsInsufficient data114
9Paediatric careFigure 49. Grade of first reviewer/team leaderPercentage of patients in dataset6050403020100ConsultantNCCGSpR 3SpR 1/2SpRGrade of clinicianSHONurse>16 years≤16 yearsOtherOverall assessment of careFigure 48 shows overall assessment of care for the paediatricsample compared with the adult sample. There was littledifference between the two groups.Appropriateness of initial responseTable 92 shows advisor assessment of appropriateness ofinitial hospital response.Grade of first reviewer/team leaderFigure 49 shows grade of fi rst reviewer/team leader analysedby age of patient. In comparison with the adult data, it wasencouraging that there was more consultant involvementin the initial management, but still worth noting that aconsultant was the fi rst reviewer in only 54% of cases.<strong>Trauma</strong> team responseA trauma response was documented in the notes in 69% of≤16 year olds, slightly higher than the overall data (58%).Table 92. Appropriateness of initial responsedepending on patient age>16 years ≤16 yearsNumber ofpatientsNumber ofpatients% %Yes 548 86.4 53 88.3No 86 13.6 7 11.7Subtotal 634 60Insuffi cient data 89 8Total 723 68Outcome at 72 hoursSix out of 68 paediatric cases (8.8%) were deceased at 72hours post injury.115
CHAPTER 9 - Paediatric careKey findingsRecommendations68/795 (8.6%) cases were aged 16 or less.Only 54% of cases had consultant staff involved in theimmediate management.The pattern of assessment of overall care was similar toadults with less than half the cases judged as receivingcare classifi ed as good practice.Advanced Paediatric Life Support (APLS) trained staffwere not resident or available 24 hours in 20.2% ofhospitals.Only 22 out of 146 hospitals had Registered SickChildren’s Nurse cover 24 hours a day, 7 days a week.All recommendations in this report apply equally toseverely injured children.All sites accepting children for defi nitive traumamanagement should have protocols for theirmanagement in place. These protocols should beregularly reviewed and updated. (Hospital trusts)All hospitals should have up to date guidelines on themanagement and referral of suspected non-accidentalinjury in children. (Hospital trusts)Hospitals should use standard, universal defi nitionsfor neonates, infants and children. (Royal College ofPaediatrics and Child <strong>Health</strong>)Each receiving unit should have up to date guidelines forchildren which recognise the paediatric skills available onsite and their limitations and include agreed guidelinesfor communication and transfer with specialisedpaediatric services within the local clinical network.(Strategic health authorities and hospital trusts)An Advanced Paediatric Life Support (APLS) (orequivalent) trained consultant and a Registered SickChildren’s Nurse (RSCN) or an APLS trained nurseshould be involved in the immediate management of allseverely injured children. (Hospital trusts)If a hospital does not admit children for defi nitive carethen a bypass protocol should be in place. (Hospital andambulance trusts)116
9Paediatric careReferences1. Services for Children in Emergency departments. RoyalCollege of Paediatrics and Child <strong>Health</strong>. 2007www.rcpch.ac.uk/health-services/emergen-care2. The Royal College of Surgeons of England and the BritishOrthopaedic Society. Better Care for the Severely Injured.2000117
CHAPTER 10 - TransfersIntroductionMost patients with severe injuries are admitted to hospitalsthat are geographically closest to the location of the incidentwhere the injuries were sustained. Consequently, earlymanagement of the patient occurs at centres that may nothave the facilities or resources suitable for the appropriatecare of the severely injured.The lack of available appropriate care may result in thetransfer to a site with more appropriate facilities. Someambulance trusts have a policy of bypassing local hospitalsto larger trauma centres to obviate the need for later transfer.However, little data supports the fact that such a ‘bypass’policy is used with any frequency. In 1997, it was estimatedthat more than 11,000 patients in the UK with criticalillnesses required transfer annually 1 .An example of such a situation is the head injury patient.Approximately 2,200 patients are admitted annually tohospital with head injuries 2 . Of these, 3 – 5% are transferredto regional neurosurgical units for further management.It has been well recognised that the outcome of patientswho require a transfer because of a mismatch betweenthe patient’s needs and the available resources at the initialplace of admission have a better eventual outcome if thattransfer is performed by dedicated transport teams 3-6 .However, despite extensive literature highlighting this, in2002 the Intensive Care Society commented that ‘manycritically ill patients are transferred between hospitals in anad hoc manner by inexperienced trainees with little formalsupervision and potentially serious complications canoccur’ 7 .Many studies that have reported on the quality of transferof patients with head injuries have identifi ed major problemswith resuscitation and transfer, including: delays; missedinjuries; poor airway management; hypotension; hypoxia;and, the quality of medical escort 8-12 .As a result of these concerns, in 1996, the Associationof Anaesthetists of Great Britain and Ireland producedguidelines surrounding the transfer of head injured patients 13 .The main recommendations were:• There should be a designated consultant at boththe referring and receiving hospitals who haveoverall responsibility for the transfer of patients.• Local guidelines should be in existence and shouldbe consistent with national guidelines.• Resuscitation and stabilisation of the patient mustbe achieved before transfer.• Only in exceptional circumstances should apatient with altered conscious level be transferredunintubated.• The doctor accompanying the patient must be ofsufficient experience and have received supervisedtraining in the transfer of patients with headinjuries.• There must be a means of communication to boththe dispatching hospital and the receiving hospital.118
10TransfersThe Intensive Care Society produced guidelines for thetransport of the Critically Ill Patient in 1997 14 and thenfurther refi ned these recommendations in 2002 15 . Therecommendations include the following; there should be‘regular meetings of relevant consultants, senior nurses,ambulance providers, bed bureaux managers andcommissioners to develop admission and discharge andreferral policies and transport protocols, to ensure availableresources to enable timely and safe transfers and to developassurance programmes’.It was hoped that compliance and subsequent audit of theseguidelines, combined with the wider acceptance of theprinciples and uptake of the Advanced <strong>Trauma</strong> Life Support(ATLS) approach in the management of patients, wouldresult in an improvement in the quality of transfer. Despitethese recommendations, later audits of transfers still revealedinadequacies 11-15 .ResultsNumber of secondary transfersOf the 795 patients admitted to hospitals with severe injuries,194 patients underwent a secondary transfer (24.4%).Eight of these were retrievals with the remaining 186 beingtransfers conducted by the original admitting hospital.Effect of mode of initial transport system onsecondary transfersPatients brought to the initial hospital by helicopter wereless likely to undergo secondary transfer. Seven out of59 (11.9%) patients who arrived at the fi rst hospital byhelicopter required a secondary transfer within 72 hours ofarrival compared with 112/440 (25.5%) patients brought tohospital by road ambulance. The use of helicopters facilitatesadmission of the severely injured patient to the correct facilityinitially, thereby reducing subsequent transfers and speedingup defi nitive care.Only transfers within 72 hours of arrival at hospital wereincluded in the study.Protocols for secondary transferOnly 126 of the 183 (68.9%) hospitals involved in themanagement of patients with severe injuries had protocolsfor the secondary transfer of patients despite numerousrecommendations mandating such protocols.119
CHAPTER 10 - TransfersArrangement of transfersA consultant arranged the transfer in only 49 of 137 (35.8%)cases reported by clinicians on the A&E questionnaire.From the casenotes provided to <strong>NCEPOD</strong>, the grade ofthe clinician arranging the transfer could only be identifi edin 87/194 (44.8%) cases. A consultant was responsible forarranging 39/87 (44.8%) of these transfers (Figure 50).Figure 50. Grade of clinician organising transfer60Number of patients50403020100CON NCCG SpR3 SpR 1/2 SpR unknown SHO Other NotrecordedTable 93. Grade of clinician receiving the transferNumber of patients %Consultant 14 18.4NCCG 2 2.6SpR 3 2 2.6SpR 1/2 1 1.3SpR undefi ned 46 60.5SHO 10 13.2Other 1 1.3Subtotal 76Not documented 118Total 194The documentation of the grade of clinician receiving thepatient was equally poorly documented. In 118/194 cases(60.8%) it could not be determined who received the patient.Only 14 cases were documented as being received byconsultants (Table 93).The standards and guidelines for the Transport of theCritically Ill Patient 9 recommends that “each hospital shouldhave a designated consultant available 24 hours a day toorganise, supervise and where necessary undertake allinter-hospital transfers” and that the decision to transfera patient “must be made by a consultant in intensivecare in discussion with consultant colleagues”. This is not120
10Transfershappening. The lack of documented consultant input is aconcern. Either local guidelines exist which obviate the needfor consultant involvement or the process of care, includingtransfers, is being managed and delivered by staff in training.Accompanying staffRecommendations state that a minimum of two attendantsshould be present for the transfer 9 .Of the 194 transfers only 35 (18.0%) had a documentedsecond attendant and 3 (1.5%) a third attendant.In 155/194 cases notifi ed to <strong>NCEPOD</strong>, the grade of theaccompanying person was not documented. In the 39/194cases where specialty was documented, an anaesthetistor critical care specialist accompanied 36 of the cases.The published recommendations mandate that one of theattendants should be competent in intensive care medicine,anaesthesia or another acute specialty in order to be able tomanage any signifi cant airway complication.Reason for transferThe reasons for transfer were mainly for specialistmanagement of injuries (172/194; 88.7%). Six patients weretransferred due to lack of critical care facilities at the initialhospital. Other reasons cited for transfers were because oflack of local facilities (primarily lack of imaging facilities).The transfers for specialist care are detailed in Figure 51.Of the 172 cases transferred for specialist treatment, themajority were transferred for neurosurgical care – 106/172(61.6%). Six (3.5%) patients were transferred to paediatricunits. Eighteen (10.5%) patients were transferred for burns/plastic surgery input and 7 (4.1%) for the management ofcardiothoracic injuries.While it is essential to transfer patients if the appropriatecare is not available at the initial receiving hospital, it mustbe remembered that this will inevitably incur delays in thetime to defi nitive management. In cases where there is atime critical injury e.g. neurosurgical operation for expandingintracranial haematoma, this type of care may not allowFigure 51. Specialty to which the patients were transferred120Number of patients100806040200NeurosurgeryBurns/plasticsPaediatricsSpinal/neurologyCardiothoracics/thoracicsurgerySpecialtyOrthopaedicsLiverOtherNot recorded121
CHAPTER 10 - TransfersFigure 52. Delay in transfer/retrievalNumber of patients1009080706050403020100TransferRetrievalYesNothe optimal outcome. Given these clinical considerationsand the constraints of staffi ng in a time of changing trainingand working hours, it is probably time to consider carefullywhich hospitals receive severely injured patients and to plana proper regional trauma service. Patient transport servicesand the role of doctors in prehospital care must be anintegral part of any plans to change trauma services. Both ofthese plans must occur in parallel as part of a wider traumacare network 12 .Appropriateness of transferNinety one out of the 194 (46.9%) transfers were consideredappropriate by the advisors and 17 (8.8%) transferswere considered inappropriate. There were insuffi cient orincomplete data to comment and classify the remainder ofthe transfers.The reasons identifi ed for the inappropriateness of thetransfers included:Timeliness of transferFigure 52 shows information on timeliness of transfer. Whereit could be assessed there were delays in 26.4% (34/129) ofall transfers and 50% (4/8) of retrievals.• transfers with unsurvivable injuries (burns case),• failure of closer centre to accept the patient and,therefore, a longer and delayed transfer wasneeded,• failures in effective communication betweenhospitals, and• missed injuries.122
10TransfersCase study 6A young patient had a severe brain injury following afall. The patient had a GCS of 3 at presentation withunresponsive pupils and a compound skull fracturewith brain matter exuding from the ear. The patient wastransferred to a neurosurgical unit but certifi ed braindead shortly after arrival.In addition, there were some concerns over the transfer of anumber of patients who had sustained a head injury. Fromthe records available six patients with a Glasgow ComaScore of less than 10 were transferred without intubation.Case study 7An elderly patient tripped while intoxicated. A GlasgowComa Score of 3 was recorded in the ambulance. At thereceiving hospital it was recoded as 8. The hospital wasunable to perform a CT head scan therefore the patientwas transferred to the local neurosurgical hospital. Thetransfer was performed without securing the airway. Atthe neurosurgical hospital the patient was transferredto CT still with an unprotected airway. Intubation wassubsequently performed after CT scanning.The recommendations on the transfer of patients with headinjuries 7 state that only in exceptional circumstances shoulda patient with a signifi cantly altered conscious level requiringtransfer not be sedated, intubated and ventilated.This review gives a picture of a haphazard arrangement forthe secondary transfer of severely injured patients. It is ofgreat concern that one in four patients required secondarytransfer to receive defi nitive care and this must be a majorcriticism of the current arrangements for the managementof severely injured patients. There were defi ciencies in localprotocols, use of national guidelines, consultant oversightand documentation.Furthermore, avoidance of transfers by the initial directtransport of the severely injured patient to a centre withthe appropriate facilities should be considered. This wouldneed regional planning of all aspects of the trauma serviceincluding the prehospital emergency services.123
CHAPTER 10 - TransfersKey findingsRecommendationsThere was a lack of adherence to the numerousrecommendations and guidelines that exist regarding thetransfer of critically ill and severely injured patients.The arrangements for the secondary transfer of severelyinjured patients were haphazard.One in four severely injured patients required asecondary transfer to receive defi nitive care.The use of a helicopter system reduced the need forsecondary transfers compared to a road ambulancesystem.The documentation of transfers was almost uniformlypoor.Despite the limited information available from thepoor documentation, there was an apparent lack ofconsultant input into the arrangement and conduct ofsecondary transfers.This study of a three month period suggests that thereare approximately 800 transfers annually for severetrauma and that the situation of ‘many critically illpatients are transferred between hospitals in an adhoc manner by inexperienced trainees with little formalsupervision and potentially serious complications canoccur’ is correct. There does not appear to have beenany signifi cant change in the last fi ve years.A clear record of the grade and specialty of allaccompanying staff involved in the transfer or retrievalof severely injured patients should be made and thisdocumentation should accompany the patient ontransfer. (<strong>Trauma</strong> team leader)There should be standardised transfer documentation ofthe patients’ details, injuries, results of investigations andmanagement with records kept at the dispatching andreceiving hospitals. (<strong>Trauma</strong> team leader, Department of<strong>Health</strong>)Published guidelines must be adhered to and auditsperformed of the transfers and protocols. (Hospitaltrusts)Local networks should develop protocols for thetransfer of severely injured patients suitable for regionalrequirements. (Hospital trusts)The number of transfers may be decreased ifappropriate arrangements are made for cross cover inspecialties, e.g. interventional radiology, between trusts.(Hospital trusts)124
10TransfersReferences1. Mackenzie PA, Smith EA, Wallace PG. Transfer of adultsbetween intensive care units in the United Kingdom:postal survey. BMJ. 1997 May 17; 314(7092):1455-62 Mendelow et al. Risks of intracranial haematoma in headInjured Adults. BMJ 1983; 287:11733. McMonagle MP et al. Anz J Surg 2007; 77: 241 – 24613. AAGBI Recommendations for the transfer of patientswith head injuries to neurosurgical injuries. 199614. Intensive Care Society. Guidelines for transport of thecritically ill adult. <strong>London</strong>: Intensive care Society 199715. Stevenson A et al. Emergency department organisationof critical care transfers in the UK. Emerg Med J. 2005Nov; 22(11):795-84. Deane SA et al. Anz J Surg 1990; 60: 441-4465. Strobos J. Ann Emerg Med 1991; 20: 302-3106. Clemmer TP Crit Care Med 2000; 28: 265-266)7. Intensive Care Society. Guidelines for transport of thecritically ill adult. <strong>London</strong>: Intensive Care Society 20028. Dunn LT. Secondary insults during the intra hospitaltransfer of head injured patients: an audit of transfers inthe Mersey Region. Injury 1997; 28:427-319. Gentleman D. Causes and effects of systemiccomplications among severely head-injured patientstransferred to a neurosurgery unit. Int Surg 1992;77:297-30210. Gentleman D et al. Audit of transfer of unconscious headinjured patients to a neurosurgical unit. Lancet 1990;335:330-411. Have ATLS and national transfer guidelines improvedthe quality of resuscitation and transfer of head-injuredpatients? Injury 2003 34:834-83812. Knowles PR et al. Meeting the standards for interhospitaltransfer of adults with severe head injury in the UnitedKingdom. Anaesthesia. 1999 Mar; 54(3):283-8125
CHAPTER 11 -Incidence of trauma and organisation of trauma servicesIntroductionAlmost all of the evidence of the effectiveness ofimprovements in the organisation of trauma care servicescomes from developed countries. In most cases, the betterorganisation comes in the form of two related activities:(1) planning of integrated systems for traumamanagement; and(2) verifi cation of trauma services throughhospital inspections.Verifi cation applies to a review of individual facilities asregards their provision of a variety of items, includinghuman resources (e.g. availability of personnel with certainqualifi cations), physical resources (equipment and supplies)and administrative and organisational functions, such asquality improvement, audit (including outcome comparisons)and implementation of protocols (e.g. Advanced <strong>Trauma</strong>Life Support (ATLS). The American College of Surgeons hasmade signifi cant progress in this area 1 .The planning of systems for trauma management impliesseveral integrated functions. This includes regionaldesignation of those hospitals able to fulfi l the roles of traumacentres at varying levels of complexity; ranging from largeurban trauma centres to small rural hospitals and clinics.It also implies the planning of mobile emergency medicalservices, prehospital triage (to determine which patientsshould go to which types of designated facilities), transfercriteria and transfer arrangements between hospitals.patients. This relationship between volume, quality of careand outcome in trauma has been in the literature for someyears 2,3 . This suggests that there is a need to integrate andconcentrate major trauma in fewer centres, thus giving abetter quality of care.The incidence of severe trauma defi ned by an injury severityscore of 16 or more is estimated to be four per millionper week in the UK 4 ; a lower prevalence than in the USA.Burdett-Smith et al estimated that there are between 10,000and 10,600 patients suffering multiple injuries in the UKeach year 5 . Given the above estimates, the average acutehospital in the UK is not likely to be called upon to treatmore than one severely injured patient each week. Such lownumbers suggest that some acute hospitals may have toolittle experience to give these patients their best chance ofoptimum outcome. Adequate experience in the defi nitivemanagement of such diffi cult problems is hard to acquirewithout reorganisation of trauma services. Furthermore, it isalmost certainly unrealistic to expect every hospital to havethe necessary staff and services to be able to provide thestandard of care required 24 hours per day, 7 days per week.ResultsIn this study, 795 patients with a verifi ed injury severity scoreof 16 or more were identifi ed over a 12 week period. Table94 shows data concerning the number of severely injuredpatients seen by each emergency department in the 12week study period.Much of the data collected in this study pertains to the fi rstcategory above (verifi cation). However, the incidence of majortrauma in the UK is actually quite low and this has a directbearing on the ability to provide high quality care to trauma126
11Incidence of trauma andorganisation of trauma servicesTable 94. Number of patients seen per hospitalNumber of hospitals1-2 483-4 295-6 297-8 149-10 311-12 613-14 315-16 217-18 219-20 1> 20 4Total 141Only 12 emergency departments treated more than oneseverely injured patient per week during the study period andmany departments only treated one to two patients in thewhole 12 week study period.During the study, 243 patients were admitted initially tohospitals that reported 1-5 patients in the study, 226 patientsto hospitals that admitted 6-10 patients, 197 patients tohospitals that admitted 11-20 patients to the study and 129patients to hospitals that admitted more than 20 patients tothe study. Figure 53 illustrates the advisors’ assessment ofoverall care analysed by number of patients includedin the study.It can be seen that the high volume hospitals (>20 patients inthe study) were assessed as providing a higher percentageof good practice and a lower percentage of all othercategories, including insuffi cient data (Figure 53).Figure 53. Number of patients per hospital vs. advisors’ overall assessment70Percentage of group6050403020101-56-1011-20>200Good practiceRoom forimprovement -clinicalRoom forimprovement -organisationalRoom forimprovement -clinical andorganisationalLess thansatisfactoryInsufficient data127
CHAPTER 11 - Incidence of trauma and organisation of trauma servicesDiscussionThe low number of severely injured patients in this study is inkeeping with the literature previously referenced. However,these present fi gures are somewhat lower and this mayrefl ect several factors:1. Although the study was well publicised and <strong>NCEPOD</strong>local reporters attempted to collect all cases, it may wellbe that not all severely injured patients were included inthe study.2. All patients in this study were scored by <strong>NCEPOD</strong> staff,and patients who were identifi ed as severely injured bythe participating centre but who subsequently had aninjury severity score (ISS)
11Incidence of trauma andorganisation of trauma servicesNeurosurgery (page 102-107)One hundred and fourteen patients required neurosurgery asa result of head trauma. Fifty eight of these patients (50.9%)were initially taken to a non-neurosurgical centre. Only oneout of seven of these patients had surgery within four hours.Two out of three patients taken initially to a neurosurgicalcentre had surgery within four hours of injury.Availability of interventional radiology (page 25-33 and page 98-102)The use of interventional radiology has an increasing rolein the management of haemorrhage in the trauma patient.Only one patient in this study underwent an interventionalradiology technique. Only six out of 10 hospitals statedthat they had 24 hour access to this therapy and in manyof those this is ad hoc due to the small number of trainedindividuals.Secondary transfers (page 118-124)One in four severely injured patients required a secondarytransfer to receive defi nitive care. This underlines the inabilityof the original admitting facility to provide defi nitive care.Furthermore, these transfers were conducted in a haphazardfashion with little consultant oversight.Prehospital airway management (page 37-48)One in 10 patients arrived at hospital with an obstructed orpartially obstructed airway.Eleven out of 85 attempted prehospital intubations failed(12.9%). Eight of these patients were dead at 72 hours postinjury (72.7% mortality rate).These six issues have been used for illustrative purposesonly. It can be appreciated that not every hospital can havethe manpower, facilities, equipment and expertise to providedefi nitive care for all severely injured patients. Furthermore,many of the problems that exist in trauma management,including the prehospital phase, are organisational and donot refl ect on the abilities or enthusiasm of clinical teams.The infrequent incidence of major trauma compounds theseissues.As previously referenced, and shown in this study (Figure53), there is an association between the volume of casesand good outcomes 2,3 . It is also known that patients who areadmitted directly to a trauma centre have less morbidity anda lower mortality than patients who are initially admitted to amore local hospital and subsequently transferred to a traumacentre 12 .Regional reconfi guration of trauma services will allow theconcentration of relatively few patients in limited numberof centres that could develop their expertise. This willensure that all the staff, facilities, equipment and expertiseto manage these challenging patients will be immediatelyavailable. Sustainable rotas will be deliverable and will ensurebetter availability of consultants and other staff at all times.There will be more effi cient use of limited resources and itappears that the societal cost of such a system is favourable13. Concentration of major trauma will give opportunities toincrease the robustness of audit and quality control and willalso facilitate much needed research in this area. The currentdraft of National Institute for <strong>Health</strong> and Clinical Excellence(NICE) guidance on head injury management included aresearch question about the benefi t of direct transfer of headinjured patients to neurosurgical centres.However, the current system is likely to change slowly. Evenin a system of more regionalised trauma care there will bemany patients presenting to and managed at a number of129
CHAPTER 11 - Incidence of trauma and organisation of trauma servicesdifferent hospitals within a region. All hospitals within aregion have a major part to play in the management of theinjured patient.Under the current system where there is little regionalisation,the role of the district general hospital is crucial. All hospitalshave a major role in the initial management, stabilisation, andidentifi cation of injuries and provision of defi nitive care wherepossible. Too often the district general hospitals perceivetheir role to be solely the organisation of secondary transferto an ‘ivory tower’. This can result in the focus of care beingthe transfer rather than the immediate management of theunstable patient.<strong>Trauma</strong> auditThe care of the severely injured patient requires amultidisciplinary team, often working across more thanone hospital. This is different from most other types ofmedical care (where usually only one specialist is involved)and means that special arrangements have to be made todevelop a system that coordinates the complex interactionsbetween the different individuals involved in trauma care. Toshow whether or not these arrangements are working well,a robust audit system is required – ideally evaluating bothprocesses and outcomes. A key part of a trauma system isthe multidisciplinary trauma audit meeting, where all thoseinvolved in trauma care can meet to discuss both individualpatient management and the overall performance of thetrauma system. This type of audit is more effective if thedata presented for discussion allows comparisons with otherhospitals (benchmarking) to occur.<strong>Trauma</strong> audit follows this benchmarking pattern in America,Germany, Scandinavia and Australia. In the USA, traumaoutcome audit has become a mandatory requirement fortrauma centre status. In the UK, the <strong>Trauma</strong> Audit andResearch Network (TARN) is a well-established process andoutcome audit in trauma care, which was originally derivedfrom the methods used in the American Major <strong>Trauma</strong>Outcome Study (MTOS). TARN data is used in three ways toclose the cycle of trauma audit:1) To highlight individual cases where unexpected outcomesoccur (either good or bad). This allows multidisciplinarytrauma audit meetings to focus on the particularcases that are most likely to contain the lessons forimprovement.2) Four times a year the Quarterly Report focuses ona particular specialist area of trauma management– comparing performance with standards set by theRoyal College of Surgeons <strong>Trauma</strong> Committee and alsobenchmarking performance of one hospital against therest of the UK. This information usually forms the basisfor a departmental or multidisciplinary trauma auditmeeting.3) Comparisons of outcome between hospitals can bemade, and are publicly available to purchasers andservice users through the <strong>Health</strong>care Commissionwebsite, along with case mix data by hospital. This allowsthe identifi cation of ‘outliers’ with either very good or verypoor trauma outcomes, allowing potential causes to beidentifi ed.TARN is a voluntary system, funded by subscription fromparticipating hospitals. It has data from about 50% of UKhospitals; with about one third participating at any one time.The database collected by TARN now contains about200,000 patient records, so it can also be used for varioustypes of research and to look at long-term trends in traumaoutcomes 14-17 .130
11Incidence of trauma andorganisation of trauma servicesIn this study, 183 hospitals returned an organisationalquestionnaire. Of these 183 hospitals, only 77 (42.1%)participated in, and provided data to, TARN.Key findings129/141 (91.5%) hospitals in this study dealt with aseverely injured patient less often than once per week.High volume hospitals (>20 severely injured patients inthis study) deliver a higher percentage of care assessedas good practice.Only 77/183 (42.1%) hospitals participate in TARN.RecommendationsA system should be initiated for identifying thesepatients so that the demand on the health service canbe properly quantifi ed and resources appropriate to thatdemand be made available. (Department of <strong>Health</strong>)Given the relatively low incidence of severe traumain the UK, it is unlikely that each individual hospitalcan deliver optimum care to this challenging group ofpatients. Regional planning for the effective delivery oftrauma services is therefore essential. (Strategic healthauthorities, hospital trusts)Given the importance of evaluation of processes andoutcomes in the trauma patient, all units providingtreatment for severely injured patients should contributeto the <strong>Trauma</strong> Audit Research Network. (Hospital trusts)There should be a system of designation and verifi cationof each hospital with regards to their function asa trauma centre, in a similar fashion to the systeminstituted by the American College of Surgeons.(Strategic health authorities, Royal College of Surgeons)131
CHAPTER 11 - Incidence of trauma and organisation of trauma servicesReferences1. www.facs.org/trauma/verifi cationhosp.html2. Nathens AB, Jurkovich GJ, Maler RV et al. Relationshipbetween trauma centre volume and outcomes. JAMA2001; 285: 1164-713. MacKenzie EJ et al. A national evaluation of the effect oftrauma centre care on mortality NEJM 2006; 354: 366-3784. Gorman et al. The epidemiology of major injuries inMersey and North Wales. Injury. 1995 26; 1 51-545. Burdett-Smith P, Airey GM, and Franks AJ. Improvementin trauma survival in Leeds. Injury. 1995 26; 7.455-458.6. Lecky FE, Woodford M, Bouamra O, Yates DW. Lack ofchange in trauma care in England and Wales since 1994.Emerg Med J. 2002 Nov; 19(6):520-37. Commission on the Provision of Surgical Services. TheManagement of Patients with Major Injuries. The RoyalCollege of Surgeons of England; 19888. The Management of Skeletal <strong>Trauma</strong> in the UnitedKingdom. British Orthopaedic Association. <strong>London</strong>; 199212. Sampalis JS, Denis R, Fréchette P, Brown R, FleiszerD, Mulder D. Direct transport to tertiary trauma centersversus transfer from lower level facilities: impact onmortality and morbidity among patients with majortrauma. J <strong>Trauma</strong>. 1997 Aug; 43(2):288-9513. Durham R, Pracht E, Orban B, Lottenburg L, Tepas J,Flint L. Evaluation of a mature trauma system. Ann Surg.2006; 243(6):775-8314. Lecky FE, Woodford M, Bouamra O, Yates DW. Lack ofchange in trauma care in England and Wales since 1994.Emergency Medical Journal 2002; 19:0-315. Patel HC, Woodford M, King AT, Yates DW, Lecky FE.Trends in head injury outcome from 1989 to 2003 andthe effect of neurosurgical care: an observational studyon behalf of the <strong>Trauma</strong> Audit & Research Network. TheLancet 2005; 366: 1538-4416. Dark P, Woodford M, Vail A, Mackway-Jones K, Yates D,Lecky F. Systolic hypertension and the response to blunttrauma in infants and children. Resuscitation 2002; 54:245-25317. Henderson K, Coats TJ, Hassan TB, Brohi K. Audit oftime to emergency trauma laparotomy. Br J Surg 2000;87: 472-4769. The Care of Severely Injured Patients in the UnitedKingdom. British Orthopaedic Association. <strong>London</strong>; 199710. The Royal College of Surgeons of England and the BritishOrthopaedic Society. Better Care for the Severely Injured.200011. http://www.healthcareforlondon.nhs.uk/framework_for_action.asp132
AGlossaryAPPENDIX A - GlossaryA&EAccident and EmergencyMTOSMajor <strong>Trauma</strong> Outcome StudyABCAirway, breathing, circulationNCCGNon consultant career gradeABGArterial blood gasNHSNational <strong>Health</strong> ServiceAPLSATLSAVPUCTDPLFASTAdvanced paediatric life supportAdvanced trauma life supportAlert, verbal, pain, unresponsiveComputed tomographyDiagnostic peritoneal lavageFocussed Assessment with Sonographyfor <strong>Trauma</strong>NICEOPCSPaCO 2PaO 2PRFRCSNational Institute for <strong>Health</strong>and Clinical ExcellenceOffi ce of Population, Censuses and SurveysPartial pressure of Carbon DioxidePartial pressure of OxygenPatient report formRoyal College of Surgeons of EnglandGCSGlasgow coma score / scaleRSCNRegistered sick children’s nurseICPIntracranial pressureRTCRoad traffi c collisionICUIntensive care unitSHOSenior house offi cerISSInjury severity scoreSIGNScottish Intercollegiate Guidelines NetworkIVIntra venousSpCO 2Saturation of peripheral Carbon DioxideJRCALC Joint Royal Colleges AmbulanceLiaison CommitteekPa Kilo PascalsmmHg Millimetres of MercurySpO 2SpRTARNSaturation of peripheral OxygenSpecialist registrar<strong>Trauma</strong> Audit Research Network133
APPENDIX B - Injury severity scoreAbbreviated Injury ScaleThe Abbreviated Injury Scale (AIS) is an anatomical scoringsystem fi rst introduced in 1969. Injuries are ranked on a scaleof 1 to 6, with 1 being minor, 4 severe and 6 an unsurvivableinjury. This represents the ‘threat to life’ associated withan injury and is not meant to represent a comprehensivemeasure of severity. The AIS is not an injury scale, in that thedifference between AIS1 and AIS2 is not the same as thatbetween AIS4 and AIS5.Injury Severity ScoreThe Injury Severity Score (ISS) is an anatomical scoringsystem that provides an overall score for patients withmultiple injuries. Each injury is assigned an AbbreviatedInjury Scale (AIS) score and is allocated to one of six bodyregions (Head, Face, Chest, Abdomen, Extremities (includingPelvis), External). Only the highest AIS score in each bodyregion is used. The three most severely injured body regionshave their score squared and added together to produce theISS score.AIS ScoreInjuryAn example of the ISS calculation is shown below:1 Minor2 Moderate3 Serious4 Severe5 Critical6 UnsurvivableRegionInjuryDescriptionAISSquareTopThreeHead & Neck Cerebral Contusion 3 9Face No Injury 0Chest Flail Chest 4 16AbdomenMinor Contusion of2Liver Complex5 25Rupture SpleenExtremity Fractured femur 3External No Injury 0Injury Severity Score: 50The ISS score takes values from 0 to 75. If an injury isassigned an AIS of 6 (unsurvivable injury), the ISS scoreis automatically assigned to 75. The ISS score correlateslinearly with mortality, morbidity, hospital stay and othermeasures of severity.Tables and information taken from http://www.trauma.org/scores/ais.html and http://www.trauma.org/scores/iss.html134
CAPPENDIX C -Adult and paediatric Glasgow Coma ScaleAdult and paediatricGlasgow Coma ScaleThe Glasgow Coma Scale and Coma Score (GCS)Table Glasgow Coma Scale and Score (Adults)For clarity the Glasgow Coma Scale and Glasgow ComaScore are described below.The Glasgow Coma Scale provides a framework fordescribing the state of a patient in terms of three aspectsof responsiveness: eye opening, verbal response, and bestmotor response, each stratifi ed according to increasingimpairment. In the fi rst description of the Scale for generaluse, the motor response had only fi ve options, with nodemarcation between ‘normal’ and ‘abnormal’ fl exion.The distinction between these movements can be diffi cultto make consistently and is rarely useful in monitoringan individual patient but is relevant to prognosis and is,therefore, part of an extended six option scale used toclassify severity in groups of patients.The Glasgow Coma Score is an artifi cial index; obtained byadding scores for the three responses. The notation for thescore was derived from the extended scale, incorporatingthe distinction between normal and abnormal fl exionmovements, producing a total score of 15. This score canprovide a useful single fi gure summary and a basis forsystems of classifi cation, but contains less information thana description separately of the three responses.FeatureEyeopeningVerbalresponseBest motorresponseScale responsesSpontaneousTo speechTo painNoneOrientatedConfused conversationWords (inappropriate)Sounds (incomprehensible)NoneObey commandsLocalise painFlexion - Normal- AbnormalExtendNoneScorenotation432154321654321Total coma score 3/15 - 15/15The three responses of the coma scale, not the total score,should therefore be of use in describing, monitoring andexchanging information about individual patients.135
APPENDIX C - Adult and paediatric Glasgow Coma ScalePaediatric Glasgow Coma ScaleThe paediatric version of the Glasgow Coma Scale ismodifi ed from the Adult Glasgow Coma Scale to take intoaccount of problems assessing the Best Verbal Response inpre-verbal patients.It is composed of three parameters: Best Eye Response,Best Verbal Response and Best Motor Response. Thedefi nition of these parameters is given below.Best Eye Response (4)4. Eyes open spontaneously3. Eye opening to verbal commandCommunication with the infant or child’s caregivers isrequired to establish the best usual verbal response. A‘grimace’ alternative to verbal responses should be usedin pre-verbal or intubated patients.Best Grimace Response (5)5. Spontaneous normal facial/oro-motor activity4. Less than usual spontaneous ability or only responseto touch stimuli3. Vigorous grimace to pain2. Mild grimace to pain1. No response to pain2. Eye opening to pain1. No eye openingBest Verbal Response (5)5. Alert, babbles, coos, words or sentences to usual ability4. Less than usual ability and/or spontaneous irritable cry3. Cries inappropriately2. Occasionally whimpers and/or moans1. No vocal responseBest Motor Response (6)6. Obeys commands or performs normalspontaneous movements5. Localises to painful stimuli or withdraws to touch4. Withdrawal to painful stimuli3. Abnormal fl exion to pain2. Abnormal extension to pain1. No motor response to pain136
CAdult and paediatricGlasgow Coma ScaleClassifi cation of severity of headinjury using GCSWhilst the individual components of the Glasgow ComaScale should be used in communication about individualpatients the use of the aggregate Glasgow Coma Score canbe useful for describing patient populations.The use of the aggregate score does allow the severity ofhead injury to be classifi ed into the following categories:Minor GCS 15Mild GCS 13-14Moderate GCS 9-12Severe GCS 3-8These classifi cations allow easy description of a head injuredpopulation and are used within this text.For some data presentation patients with GCS equal to3 have been separated out from the rest of the severehead injury group (GCS 4-8). This has been done to helpunderstand that data more easily as it is know that patientswith GCS equal to 3 have a much poorer prognosis than therest of the severe head injured group.137
APPENDIX D - An example of an excellentPatient Report Form (PRF)138
DAn example of an excellentPatient Report Form (PRF)139
APPENDIX E - Level 1 trauma careAs defi ned in Better Care for the Severely Injured. A Reportfrom the Royal College of Surgeons of England and theBritish Orthopaedic Society. 2000• There must be on-site departments of:• Orthopaedic trauma• NeurosurgeryThe Required Facilities at the Major AcuteHospitals (Level 1)• A 24-hour resuscitative trauma team, led by aconsultant with current ATLS ® certification orequivalent, must be in place.• A 24-hour, fully staffed A&E department,supported by on-call A&E consultants,supported by specialist registrars.• ICU beds and trauma beds on the same siteas the A&E department.• On-site 24-hour X-ray and CT scanningwith appropriate staffing and immediatereporting facilities.• The equivalent of four to eight whole-timeconsultants exclusively dealing withorthopaedic trauma.• General and vascular surgery• Plastic surgery• Cardiothoracic or thoracic surgery• Head & neck surgery• Urology• Anaesthesia with intensive care• Interventional radiology• Paediatric surgery• Intensive care beds for children• A named consultant director of trauma.• A dedicated trauma theatre and dailyconsultant orthopaedic trauma lists.• A helicopter pad close to the A&E departmentis mandatory. There should be no additionalsecondary journey by road. The helicopter landingsite should allow landing throughout the 24 hours.140
FParticipationAPPENDIX F - ParticipationTrustCasesidentifiedOrganisationalquestionnairereturnedAintree Hospitals NHS Trust Yes YesAiredale NHS Trust Yes YesAshford & St Peter’s Hospital NHS Trust Yes YesBarking, Havering and Redbridge Hospitals NHS Trust Yes YesBarnet and Chase Farm Hospitals NHS Trust No YesBarnsley Hospital NHS Foundation Trust Yes YesBarts and The <strong>London</strong> NHS Trust Yes YesBasildon & Thurrock University Hospitals NHS FoundationTrust Yes YesBasingstoke & North Hampshire Hospitals NHS Foundation Trust Yes YesBedford Hospital NHS Trust Yes YesBirmingham Childrens Hospital NHS Trust Yes YesBlackpool, Fylde and Wyre Hospitals NHS Trust Yes YesBolton Hospitals NHS Trust Yes YesBradford Teaching Hospitals NHS Foundation Trust Yes YesBrighton and Sussex University Hospitals NHS Trust Yes YesBro Morgannwg NHS Trust Yes YesBromley Hospitals NHS Trust Yes YesBuckinghamshire Hospitals NHS Trust No YesBurton Hospitals NHS Trust Yes YesCalderdale & Huddersfi eld NHS Trust Yes NoCambridge University Hospitals NHS Foundation Trust Yes YesCardiff and Vale NHS Trust Yes YesCarmarthenshire NHS Trust Yes YesCentral Manchester/Manchester Childrens Univ Hosps NHST Yes YesCeredigion & Mid Wales NHS Trust Yes YesChelsea & Westminster <strong>Health</strong>care NHS Trust Yes No141
APPENDIX F - ParticipationTrustCasesidentifiedOrganisationalquestionnairereturnedChesterfi eld Royal Hospital NHS Foundation Trust Yes YesCity Hospitals Sunderland NHS Foundation Trust Yes YesConwy & Denbighshire NHS Trust Yes YesCountess of Chester Hospital NHS Foundation Trust Yes YesCounty Durham and Darlington Acute Hospitals NHS Trust Yes YesCraigavon Area Hospital Group Trust Yes YesDartford & Gravesham NHS Trust Yes YesDerby Hospitals NHS Foundation Trust Yes YesDoncaster and Bassetlaw Hospitals NHS Foundation Trust Yes YesDorset County Hospital NHS Foundation Trust Yes YesDown Lisburn <strong>Health</strong> & Social Services Trust No YesDudley Group of Hospitals NHS Trust Yes YesEaling Hospital NHS Trust Yes YesEast & North Hertfordshire NHS Trust Yes YesEast Cheshire NHS Trust Yes YesEast Kent Hospitals NHS Trust Yes YesEast Lancashire Hospitals NHS Trust No NoEast Sussex Hospitals NHS Trust Yes YesEpsom and St Helier University Hospitals NHS Trust Yes YesEssex Rivers <strong>Health</strong>care NHS Trust Yes YesFrimley Park Hospitals NHS Trust Yes YesGateshead <strong>Health</strong> NHS Trust No YesGeorge Eliot Hospital NHS Trust Yes YesGloucestershire Hospitals NHS Foundation Trust Yes YesGood Hope Hospital NHS Trust Yes NoGuy’s & St Thomas’ NHS Foundation Trust Yes Yes142
FParticipationTrustCasesidentifiedOrganisationalquestionnairereturnedGwent <strong>Health</strong>care NHS Trust Yes YesHammersmith Hospitals NHS Trust Yes YesHarrogate and District NHS Foundation Trust Yes Yes<strong>Health</strong> & Social Services, States of Guernsey Yes YesHeart of England NHS Foundation Trust Yes YesHeatherwood and Wexham Park Hospitals NHS Trust Yes YesHereford Hospitals NHS Trust Yes YesHillingdon Hospital NHS Trust No YesHinchingbrooke <strong>Health</strong> Care NHS Trust No YesHomerton University Hospital NHS Foundation Trust Yes YesHull and East Yorkshire Hospitals NHS Trust Yes YesIpswich Hospital NHS Trust No YesIsle of Man Department of <strong>Health</strong> & Social Security Yes YesIsle of Wight <strong>Health</strong>care NHS Trust Yes YesJames Paget <strong>Health</strong>care NHS Trust Yes YesKettering General Hospital NHS Trust Yes YesKing’s College Hospital NHS Trust Yes YesKingston Hospital NHS Trust Yes YesLancashire Teaching Hospitals NHS Foundation Trust No NoLeeds Teaching Hospitals NHS Trust (The) Yes YesLewisham Hospital NHS Trust Yes YesLuton and Dunstable Hospital NHS Trust No YesMaidstone and Tunbridge Wells NHS Trust Yes YesMater Hospital Belfast <strong>Health</strong> & Social Services Trust Yes YesMayday <strong>Health</strong> Care NHS Trust Yes YesMedway NHS Trust No Yes143
APPENDIX F - ParticipationTrustCasesidentifiedOrganisationalquestionnairereturnedMid Cheshire Hospitals NHS Trust Yes YesMid Staffordshire General Hospitals NHS Trust Yes YesMid Yorkshire Hospitals NHS Trust Yes YesMid-Essex Hospital Services NHS Trust No YesMilton Keynes General NHS Trust Yes YesNewcastle upon Tyne Hospitals NHS Foundation Trust Yes YesNewham <strong>Health</strong>care NHS Trust Yes NoNorfolk & Norwich University Hospital NHS Trust Yes YesNorth Bristol NHS Trust Yes YesNorth Cheshire Hospitals NHS Trust Yes YesNorth Cumbria Acute Hospitals NHS Trust Yes NoNorth East Wales NHS Trust No YesNorth Glamorgan NHS Trust No NoNorth Middlesex University Hospital NHS Trust Yes YesNorth Tees and Hartlepool NHS Trust Yes YesNorth West <strong>London</strong> Hospitals NHS Trust Yes YesNorth West Wales NHS Trust No YesNorthampton General Hospital NHS Trust Yes YesNorthern Devon <strong>Health</strong>care NHS Trust Yes YesNorthern Lincolnshire & Goole Hospitals Trust Yes YesNorthumbria <strong>Health</strong>care NHS Trust Yes YesNottingham University Hospitals NHS Trust Yes YesOxford Radcliffe Hospital NHS Trust Yes YesPembrokeshire & Derwen NHS Trust Yes YesPennine Acute Hospitals NHS Trust (The) Yes YesPeterborough & Stamford Hospitals NHS Foundation Trust Yes Yes144
FParticipationTrustCasesidentifiedOrganisationalquestionnairereturnedPlymouth Hospitals NHS Trust Yes YesPontypridd & Rhondda NHS Trust No YesPoole Hospital NHS Trust No NoPortsmouth Hospitals NHS Trust Yes YesPrincess Alexandra Hospital NHS Trust No NoQueen Elizabeth Hospital NHS Trust Yes YesQueen Mary’s Sidcup NHS Trust Yes YesRoyal Berkshire NHS Foundation Trust Yes YesRoyal Bournemouth and Christchurch Hospitals NHS Trust Yes YesRoyal Cornwall Hospitals NHS Trust Yes YesRoyal Devon and Exeter NHS Foundation Trust Yes YesRoyal Free Hampstead NHS Trust Yes YesRoyal Group of Hospitals & Dental Hospitals & Maternity Hosp Yes YesRoyal Liverpool & Broadgreen University Hospitals NHS Trust Yes YesRoyal Liverpool Children’s NHS Trust Yes YesRoyal Surrey County Hospital NHS Trust Yes YesRoyal United Hospital Bath NHS Trust Yes YesRoyal West Sussex NHS Trust Yes NoRoyal Wolverhampton Hospitals NHS Trust (The) Yes YesSalford Royal Hospitals NHS Trust Yes YesSalisbury Foundation NHS Trust Yes YesSandwell and West Birmingham Hospitals NHS Trust Yes YesScarborough and North East Yorkshire <strong>Health</strong> Care NHS Trust Yes YesSheffi eld Children’s NHS Foundation Trust Yes NoSheffi eld Teaching Hospitals NHS Foundation Trust Yes YesSherwood Forest Hospitals NHS Trust Yes No145
APPENDIX F - ParticipationTrustCasesidentifiedOrganisationalquestionnairereturnedShrewsbury and Telford Hospitals NHS Trust Yes YesSouth Devon <strong>Health</strong>care NHS Trust Yes YesSouth Tees Hospitals NHS Trust Yes YesSouth Tyneside NHS Foundation Trust Yes YesSouth Warwickshire General Hospitals NHS Trust No NoSouthampton University Hospitals NHS Trust Yes YesSouthend Hospital NHS Trust Yes YesSouthport and Ormskirk Hospitals NHS Trust Yes YesSperrin Lakeland <strong>Health</strong> & Social Care NHS Trust No YesSt George’s <strong>Health</strong>care NHS Trust Yes YesSt Helens and Knowsley Hospitals NHS Trust Yes YesSt Mary’s NHS Trust Yes YesStates of Jersey <strong>Health</strong> & Social Services Yes YesStockport NHS Foundation Trust Yes YesSurrey & Sussex <strong>Health</strong>care NHS Trust Yes YesSwansea NHS Trust Yes YesSwindon & Marlborough NHS Trust Yes YesTameside and Glossop Acute Services NHS Trust Yes YesTaunton & Somerset NHS Trust Yes YesThe Queen Elizabeth Hospital King’s Lynn NHS Trust Yes YesThe Rotherham NHS Foundation Trust Yes YesTrafford <strong>Health</strong>care NHS Trust Yes YesUlster Community & Hospitals NHS Trust No YesUnited Bristol <strong>Health</strong>care NHS Trust Yes YesUnited Hospitals <strong>Health</strong> & Social Services Trust Yes YesUnited Lincolnshire Hospitals NHS Trust Yes Yes146
FParticipationTrustCasesidentifiedOrganisationalquestionnairereturnedUniv. Hospital of South Manchester NHS Foundation Trust Yes YesUniversity College <strong>London</strong> Hospitals NHS Foundation Trust No YesUniversity Hospital Birmingham NHS Foundation Trust Yes YesUniversity Hospital of North Staffordshire NHS Trust No NoUniversity Hospitals Coventry and Warwickshire NHS Trust Yes YesUniversity Hospitals of Leicester NHS Trust Yes YesUniversity Hospitals of Morecambe Bay NHS Trust Yes YesWalsall Hospitals NHS Trust Yes NoWest Hertfordshire Hospitals NHS Trust No NoWest Middlesex University Hospital NHS Trust No NoWest Suffolk Hospitals NHS Trust Yes YesWhipps Cross University Hospital NHS Trust Yes YesWhittington Hospital NHS Trust Yes YesWinchester & Eastleigh <strong>Health</strong>care NHS Trust Yes YesWirral Hospital NHS Trust Yes YesWorcestershire Acute Hospitals Yes YesWorthing and Southlands Hospitals NHS Trust Yes YesWrightington, Wigan & Leigh NHS Trust Yes YesYeovil District Hospital NHS Foundation Trust Yes YesYork Hospitals NHS Trust Yes YesTrusts are listed that were expected to participate.147
APPENDIX G - Corporate structureThe National Confi dential Enquiry into Patient Outcomeand Death (<strong>NCEPOD</strong>) is an independent body to which acorporate commitment has been made by the Medical andSurgical Colleges, Associations and Faculties related to itsarea of activity. Each of these bodies nominates members onto <strong>NCEPOD</strong>’s Steering Group.Dr M ClementsDr A NicholsonMr B ReesMr M ParkerRoyal College of PhysiciansRoyal College of RadiologistsRoyal College of Surgeons of EnglandRoyal College of Surgeons of EnglandSteering Group as at 21st November 2007Mr D MitchellFaculty of Dental Surgery, RoyalCollege of Surgeons of EnglandDr D WhitakerAssociation of Anaesthetistsof Great Britain and IrelandDr S LishmanMs S PanizzoRoyal College of PathologistsPatient RepresentativeMr T BatesAssociation of Surgeonsof Great Britain & IrelandMrs M WangPatient RepresentativeDr S BridgmanFaculty of Public <strong>Health</strong> MedicineDr P CartwrightRoyal College of AnaesthetistsObserversDr P NightingaleRoyal College of AnaesthetistsMrs C MilesInstitute of <strong>Health</strong>care ManagementDr B EllisRoyal College of General PractitionersDr R PalmerCoroners’ Society of Englandand WalesMs M McElligottRoyal College of NursingMrs H BurtonScottish Audit of Surgical MortalityProf D LuesleyRoyal College of Obstetriciansand GynaecologistsMrs E StevensonNational Patient Safety AgencyMrs M WishartRoyal College of OphthalmologistsDr I DoughtyRoyal College of Paediatricsand Child <strong>Health</strong>Dr R DowdleRoyal College of PhysiciansProfessor T Hendra Royal College of PhysiciansDr M ArmitageRoyal College of Physicians148
GCorporate structureDr K ClearyNational Patient Safety Agency<strong>NCEPOD</strong> is a company, limited by guarantee and aregistered charity, managed by Trutees.TrusteesChairmanProfessor T TreasureTreasurerMr G T LayerProfessor M BrittonProfessor J H ShepherdMr M A M S LeighDr D JustinsCompany Secretary Dr M MasonClinical Co-ordinatorsThe Steering Group appoint a Lead Clinical Co-ordinator fora defi ned tenure. In addition there are seven Clinical Coordinatorswho work on each study. All Co-ordinators areengaged in active academic/clinical practice (in the NHS)during their term of offi ce.Lead Clinical Co-ordinator Mr I C Martin (Surgery)Clinical Co-ordinators Dr D G Mason (Anaesthesia)Dr J Stewart (Medicine)Professor S B Lucas (Pathology)Dr G Findlay (Intensive Care)Dr D Mort (Medicine)Mr S Carter (Surgery)Mr M Lansdown (Surgery)149
Published November 2007 by the National Confidential Enquiryinto Patient Outcome and Death (2007)4-8 Maple Street, <strong>London</strong> W1T 5HDT 020 7631 3444F 020 7631 4443E info@ncepod.org.ukW www.ncepod.org.ukISBN 0-9539240-8-4A company limited by guarantee Company no. 3019382Registered Charity no. 1075588This report can be found on the <strong>NCEPOD</strong> web site www.ncepod.org.ukDesigned and produced by Interface, Bristol. Telephone 0117 923 2235