North Shore Hospital report - New Zealand Doctor
North Shore Hospital report - New Zealand Doctor
North Shore Hospital report - New Zealand Doctor
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
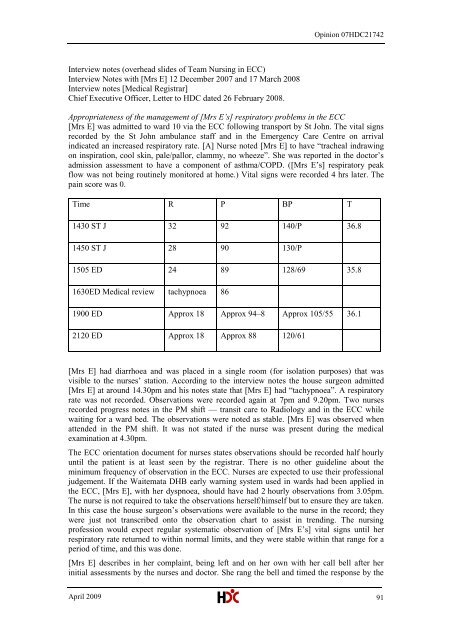
Opinion 07HDC21742Interview notes (overhead slides of Team Nursing in ECC)Interview Notes with [Mrs E] 12 December 2007 and 17 March 2008Interview notes [Medical Registrar]Chief Executive Officer, Letter to HDC dated 26 February 2008.Appropriateness of the management of [Mrs E‘s] respiratory problems in the ECC[Mrs E] was admitted to ward 10 via the ECC following transport by St John. The vital signsrecorded by the St John ambulance staff and in the Emergency Care Centre on arrivalindicated an increased respiratory rate. [A] Nurse noted [Mrs E] to have ―tracheal indrawingon inspiration, cool skin, pale/pallor, clammy, no wheeze‖. She was <strong>report</strong>ed in the doctor‘sadmission assessment to have a component of asthma/COPD. ([Mrs E‘s] respiratory peakflow was not being routinely monitored at home.) Vital signs were recorded 4 hrs later. Thepain score was 0.Time R P BP T1430 ST J 32 92 140/P 36.81450 ST J 28 90 130/P1505 ED 24 89 128/69 35.81630ED Medical review tachypnoea 861900 ED Approx 18 Approx 94–8 Approx 105/55 36.12120 ED Approx 18 Approx 88 120/61[Mrs E] had diarrhoea and was placed in a single room (for isolation purposes) that wasvisible to the nurses‘ station. According to the interview notes the house surgeon admitted[Mrs E] at around 14.30pm and his notes state that [Mrs E] had ―tachypnoea‖. A respiratoryrate was not recorded. Observations were recorded again at 7pm and 9.20pm. Two nursesrecorded progress notes in the PM shift — transit care to Radiology and in the ECC whilewaiting for a ward bed. The observations were noted as stable. [Mrs E] was observed whenattended in the PM shift. It was not stated if the nurse was present during the medicalexamination at 4.30pm.The ECC orientation document for nurses states observations should be recorded half hourlyuntil the patient is at least seen by the registrar. There is no other guideline about theminimum frequency of observation in the ECC. Nurses are expected to use their professionaljudgement. If the Waitemata DHB early warning system used in wards had been applied inthe ECC, [Mrs E], with her dyspnoea, should have had 2 hourly observations from 3.05pm.The nurse is not required to take the observations herself/himself but to ensure they are taken.In this case the house surgeon‘s observations were available to the nurse in the record; theywere just not transcribed onto the observation chart to assist in trending. The nursingprofession would expect regular systematic observation of [Mrs E‘s] vital signs until herrespiratory rate returned to within normal limits, and they were stable within that range for aperiod of time, and this was done.[Mrs E] describes in her complaint, being left and on her own with her call bell after herinitial assessments by the nurses and doctor. She rang the bell and timed the response by theApril 2009 91