Hyperbaric Oxygen Therapy :Current Trends And ... - Hyperbaric India
Hyperbaric Oxygen Therapy :Current Trends And ... - Hyperbaric India
Hyperbaric Oxygen Therapy :Current Trends And ... - Hyperbaric India
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
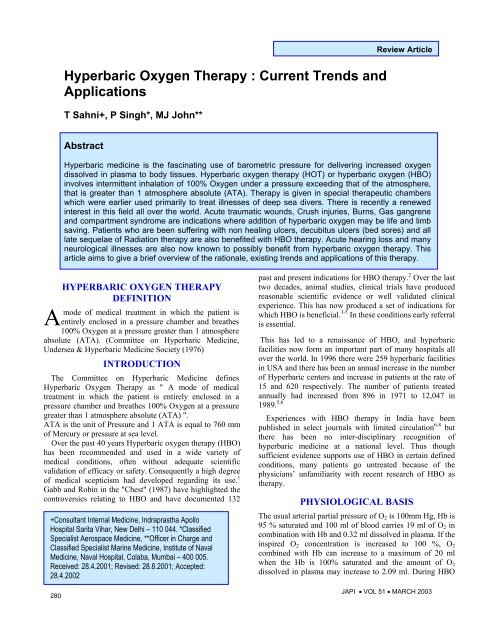
<strong>Hyperbaric</strong> <strong>Oxygen</strong> <strong>Therapy</strong> : <strong>Current</strong> <strong>Trends</strong> andApplicationsT Sahni+, P Singh*, MJ John**Review ArticleAbstract<strong>Hyperbaric</strong> medicine is the fascinating use of barometric pressure for delivering increased oxygendissolved in plasma to body tissues. <strong>Hyperbaric</strong> oxygen therapy (HOT) or hyperbaric oxygen (HBO)involves intermittent inhalation of 100% <strong>Oxygen</strong> under a pressure exceeding that of the atmosphere,that is greater than 1 atmosphere absolute (ATA). <strong>Therapy</strong> is given in special therapeutic chamberswhich were earlier used primarily to treat illnesses of deep sea divers. There is recently a renewedinterest in this field all over the world. Acute traumatic wounds, Crush injuries, Burns, Gas gangreneand compartment syndrome are indications where addition of hyperbaric oxygen may be life and limbsaving. Patients who are been suffering with non healing ulcers, decubitus ulcers (bed sores) and alllate sequelae of Radiation therapy are also benefited with HBO therapy. Acute hearing loss and manyneurological illnesses are also now known to possibly benefit from hyperbaric oxygen therapy. Thisarticle aims to give a brief overview of the rationale, existing trends and applications of this therapy.HYPERBARIC OXYGEN THERAPYDEFINITIONAmode of medical treatment in which the patient isentirely enclosed in a pressure chamber and breathes100% <strong>Oxygen</strong> at a pressure greater than 1 atmosphereabsolute (ATA). (Committee on <strong>Hyperbaric</strong> Medicine,Undersea & <strong>Hyperbaric</strong> Medicine Society (1976)INTRODUCTIONThe Committee on <strong>Hyperbaric</strong> Medicine defines<strong>Hyperbaric</strong> <strong>Oxygen</strong> <strong>Therapy</strong> as " A mode of medicaltreatment in which the patient is entirely enclosed in apressure chamber and breathes 100% <strong>Oxygen</strong> at a pressuregreater than 1 atmosphere absolute (ATA) ".ATA is the unit of Pressure and 1 ATA is equal to 760 mmof Mercury or pressure at sea level.Over the past 40 years <strong>Hyperbaric</strong> oxygen therapy (HBO)has been recommended and used in a wide variety ofmedical conditions, often without adequate scientificvalidation of efficacy or safety. Consequently a high degreeof medical scepticism had developed regarding its use. 1Gabb and Robin in the "Chest" (1987) have highlighted thecontroversies relating to HBO and have documented 132+Consultant Internal Medicine, Indraprastha ApolloHospital Sarita Vihar, New Delhi – 110 044. *ClassifiedSpecialist Aerospace Medicine, **Officer in Charge andClassified Specialist Marine Medicine, Institute of NavalMedicine, Naval Hospital, Colaba, Mumbai – 400 005.Received: 28.4.2001; Revised: 28.8.2001; Accepted:28.4.2002280past and present indications for HBO therapy. 2 Over the lasttwo decades, animal studies, clinical trials have producedreasonable scientific evidence or well validated clinicalexperience. This has now produced a set of indications forwhich HBO is beneficial. 3-5 In these conditions early referralis essential.This has led to a renaissance of HBO, and hyperbaricfacilities now form an important part of many hospitals allover the world. In 1996 there were 259 hyperbaric facilitiesin USA and there has been an annual increase in the numberof <strong>Hyperbaric</strong> centers and increase in patients at the rate of15 and 620 respectively. The number of patients treatedannually had increased from 896 in 1971 to 12,047 in1989. 5,6Experiences with HBO therapy in <strong>India</strong> have beenpublished in select journals with limited circulation 6-8 butthere has been no inter-disciplinary recognition ofhyperbaric medicine at a national level. Thus thoughsufficient evidence supports use of HBO in certain definedconditions, many patients go untreated because of thephysicians’ unfamiliarity with recent research of HBO astherapy.PHYSIOLOGICAL BASISThe usual arterial partial pressure of O 2 is 100mm Hg, Hb is95 % saturated and 100 ml of blood carries 19 ml of O 2 incombination with Hb and 0.32 ml dissolved in plasma. If theinspired O 2 concentration is increased to 100 %, O 2combined with Hb can increase to a maximum of 20 mlwhen the Hb is 100% saturated and the amount of O 2dissolved in plasma may increase to 2.09 ml. During HBOJAPI • VOL 51 • MARCH 2003
in addition to the Hb which is 100% saturated the amount ofO 2 carried in solution will increase to 4.4 ml % at a pressureof 2 ATA to 6.8 ml % at 3 ATA which is almost sufficientto supply the resting total oxygen requirement of manytissues without a contribution from oxygen bound tohemoglobin 9 Table 1. It is this increased oxygen in plasmawhich is responsible for most of the beneficial effects ofhyperbaric oxygen. 1,5TotalpressureATATable 1 : Effect of pressure on arterial O 2Content of oxygen dissolved in plasma(vol %)MmHgBreathingAir100%<strong>Oxygen</strong>1 760 0.32 2.091.5 1140 0.61 3.262 1520 0.81 4,442.5 1900 1.06 5.623 2280 1.31 6.804 3040 1.805 3800 2.806 4560 2.80O 2 is notadministeredat pressureabove 3ATAAll values assume arterial pO2 = alveolar O2 and that Hb oxygen capacity ofblood is 20 vol %; From Bassett and Bennett (1977)THERAPEUTIC EFFECTS OF HBOTHERAPYIncreased pressure by its direct mechanical effect reducesbubble size in conditions such as air embolism anddecompression sickness. Hyperoxygenation causes Immunestimulation by restoring WBC function, enhancedphagocytic capabilities and neutrophil mediated killing ofbacteria. HBO 2 accelerates neo-vascularization in hypoxicareas by augmentation of fibroblastic activity, which furtherpromotes capillary growth. HBO causes vasoconstriction innormal tissues but with an over all increased delivery ofoxygen due to the hyperoxygenation. This is the basis ofuse in reducing edema and tissue swelling. In cerebraledema this helps to reduce edema while maintainingHyperoxia. It also reduces the adherence of white cells tocapillary walls and is useful in acute brain and spinal cordinjury. HBO therapy is bactericidal for anaerobic organismssuch as Clostridia Welchii, and also inhibits the growth ofaerobic bacteria at pressures greater than 1.3 ATA. HBO at2.5 ATA reduces the half-life of carboxy-haemoglobin from4 to 5 hours in subjects breathing room air to 20 minutes orless and is the treatment of choice in carbonmonoxide (CO),smoke inhalations and acute cyanide poisoning. 1,3-5METHOD OF ADMINISTRATIONHBO therapy can be given in a "Monoplace chamber" inwhich a single patient is placed in a chamber which is thenpressurised with 100% oxygen. Monoplace chambers areused to treat stable patients with chronic medical conditions.JAPI • VOL 51 • MARCH 2003Or it can be given in a "Multiplace chamber" where manypatients can be treated at the same time. These chambers areused for acute problems and also for critically ill patientswho require a medical attendant within the chamber. Thesechambers are pressurised with compressed air and thepatient breathes 100% oxygen at that pressure throughspecial masks or oxygen hoods. The treatment control panelcontrols the therapy and monitors the patient during thetreatment. Most therapy is given at 2 or 3 ATA and theaverage duration of therapy is 60 to 90 minutes. Number oftherapies may vary from 3-5 for acute conditions to 50-60for radiation illnesses. 1,3,5TOXIC EFFECTS/COMPLICATIONSWhen used in standard protocols of pressures that do notexceed 3 ATA (300 kPa) and the length of treatment is lessthan 120 minutes, hyperbaric oxygen therapy is safe.Commonest side effect is pain in the ears (aural barotrauma)as a result of inability to equalize pressure on both sides ofthe tympanic membrane due to a blocked eustachian tube.Pneumo-thorax and air embolism are more dangerouscomplications due to tear in pulmonary vasculature duepressure changes but are rare. Other rare side effects arepulmonary and neurological oxygen toxicity (Paul Berteffect), retrolental fibroplasia and cataracts. 10 Transientreversible myopia can also rarely occur after prolongedHBO therapy. Fire is a realistic hazard but preventable bystrict safety procedures and the patient may beclaustrophobic. 1 Rare instances of hypersenstivity to O 2 arealso documented. 11 <strong>Oxygen</strong> toxicity can be prevented inmost tissues by using 5 minutes air in the chamber for every30 minutes of <strong>Oxygen</strong>. This allows antioxidants to deal withfree oxygen radicals formed during the hyperoxic period. 1,5A suggested carcinogenic effect of hyperbaric oxygen hasnot been substantiated in extensive studies. 12INDICATIONS FOR HBO THERAPYUniversally accepted indicationsThese indications are supported with peer reviewed proofof efficacy and early referral is essential. 1,3 ( Table 2)Non-healing ulcers, problem wounds, compromised skingrafts and flaps : These wounds have the underlyingproblem of tissue hypoxia, with oxygen tension usuallybelow 20 mmHg, and therefore more prone to infection. Theelevation of oxygen tension by hyperbaric oxygen therapyhas powerful effects on wound dynamics, by both enhancingleukocyte bactericidal activity and promoting the fibroblastcollagensupport needed for neovascularization. In theUnited States problem wounds are the commonestindication for adjunctive hyperbaric oxygen therapy andinclude diabetic and other small vessel ischaemic footulcers, dehiscent amputation sites, nonhealing traumaticwounds and vascular insufficiency ulcers and post radiationulcers. Several studies have shown improved healing and alower incidence of amputation with 4-30281
Table 2 : Universally accepted indications for hyperbaric oxygentherapyAcute conditions (where HBO therapy should be given earliest when combinedto conventional treatment.)1. Non-healing ulcers, problem wounds, compromised skin grafts and flaps2. Crush injury, compartment syndrome, & acute traumatic ischemias3. Gas gangrene / clostridial infections4. Necrotizing soft tissue infections (subcutaneous tissue, muscle, fascia)5. Thermal burns6. Exceptional blood loss (anemia)7. Intracranial abscess8. Burns9. Sudden deafness10. Ocular ischemic pathology11. Air or gas embolism *12. Decompression sickness*13. Carbon monoxide poisoning & smoke inhalation**Curative / Primary Line of TreatmentChronic conditions1. Non-healing wounds / problem wounds (diabetic / venous etc.)2. Radiation tissue damage3. Skin grafts and flaps (compromised)4. Chronic osteomyelitis (refractory)sessions. 1,13,14 HBO improves both graft and flap survivalcompared with routine postoperative surgical care alone.The beneficial role of HBO therapy in plastic surgery andthe role in occlusive arterial diseases in the extremities iswell known. 15,16Acute traumatic ischaemias ATI (Crush injury,compartment syndromes and others) : ATI occurs when aninjury compromises circulation. This may place portions ofthe extremity or the entire extremity at risk of necrosis oramputation. Secondary complications such as infections,non-healing wounds and ununited fractures frequentlydevelop. The immediate effect of HBO in ATI is enhanced<strong>Oxygen</strong> at the tissue level, Increased <strong>Oxygen</strong> delivery perunit of blood flow and reduction of edema. Finally HBOmay mediate the effects of the reperfusion injury in ATI’sespecially in those where tissue ischaemia is severe and orprolonged (revascularisation, reimplantations, etc.). Surgery& antibiotics remains the corner stone of therapy. Additionof adjunctive HBO has shown to significantly reduce themorbidity and mortality associated with these injuries.Overall cost of management of these injuries is also reducedsubstantially. 1,17Clostridial myonecrosis (Gas Gangrene) : Clostridiumwelchii cannot produce alpha-toxin when the patientundergoes HBO therapy. The organism is not killed byhyperbaric oxygen and alpha-toxin is not detoxified byHBO, however, with production shut-off, alpha-toxin isfixed in the tissues within 30 minutes. It also has antibioticsynergism with aminoglycosides, quinolone drugs, sulphaand amphotericin B. A three-pronged approach consisting ofHBO, surgery, and antibiotics is essential in treating gasgangrene. 1,3,6,18Necrotizing soft tissue infections : <strong>Hyperbaric</strong> oxygentherapy may be used as an adjunct treatment of soft tissueinfections with tissue necrosis, due to mixed aerobic and282anaerobic organisms. Increasing tissue oxygen tensionenhances white cell killing of bacteria, promotes inhibitionof anaerobic organism growth, and increases the oxidationreductionpotential These conditions include necrotizingcellulitis, progressive dermal gangrene, anaerobicstreptococcal myositis, crepitant anaerobic cellulitis, andnecrotizing fascitis. Primary management remains adequatesurgical debridement and antibiotic coverage. The highmortality and morbidity with these conditions warrant theaddition of adjunctive hyperbaric oxygen therapy. 1,2,5,19Treatment of late radiation tissue damage(osteoradionecrosis, radiation cystitis, enteritis,etc.) : In apatient who has had between 2,000 and 5,000 rads, there is apossibility that there may be difficulties with subsequenthealing. Above 5,000 rads healing of any subsequentsurgical wound will be a definite problem. HBO therapyremains the keystone of treatment of radiation-inducedillnesses. Recently a clearer understanding of itspathophysiology has evolved. The basic physiology of thisprocess is a progressive obliterative endarteritis withresultant hypoxic and tissues ischemia. <strong>Hyperbaric</strong> oxygeninduces neovascularization of tissue and the tissue PO 2 risesto 81% of normal plus or minus 5% between 18 and 30hyperbaric treatments. Successful surgery and grafting ispossible with a PO 2 of 75% of normal. Controlled clinicalexperience has demonstrated a perioperative staging ofhyperbaric oxygenation, termed the "Marx Protocol", hassignificantly reduced the incidence of post-operativeinfection, dehiscence, and healing delays. Two reports havespecifically addressed the issue of hyperbaric oxygen's costeffectiveness in this disorder: Marx and colleagues andDempsey et al. 20,21 The authors concluded that in carefullyselected patients, managed along algorithmic lines, theaddition of hyperbaric oxygen therapy resulted in improvedclinical outcomes while greatly reducing the overall cost.The effect of <strong>Hyperbaric</strong> <strong>Oxygen</strong> in radiation induced bonenecrosis, severe laryngeal necrosis, hemorrhagic RadiationCystitis, colitis,scleral necrosis is also now wellrecognised.The cure rate for radionecrosis of the mandiblenow approaches 94% in those patients treated with<strong>Hyperbaric</strong> oxygen.Thermal Burns : The burn wound is a complex anddynamic pathophysiologic process characterized by a zoneof coagulation, surrounded by a region of stasis, bounded byan area of hyperemia. A significant body of data clearlysupports the efficacy of hyperbaric oxygen in the treatmentof thermal injury. Reduction in fluids, less conversion to fullthickness injury, preservation of marginally viable tissue,improved microcirculation, reduction in edema, fasterepithelialization, less inflammatory response,enhancement of PMN killing, preservation of tissue creatinephosphate, adenosine triphosphate and decreased woundlactate have all been reported with HBO. A significantreduction in hospital stay and cost of treatmentis noted withadjunctive hyperbaric oxygen therapy has been reported. 22JAPI • VOL 51 • MARCH 2003
Carbon monoxide (CO) poisoning & smoke inhalation : Itis recommended that patients with severe CO poisoning,those with neuropsychological changes and those in highrisk group be treated with HBO irrespective of their COHblevels. HBO at 2.5 ATA reduces the half-life ofcarboxyhaemoglobin from 4 to 5 hours in subjects breathingroom air to 20 minutes or less. Timely administration ofHBO prevents neuronal injury, prevents delayedneurolopsychological sequel and terminates the biochemicaldeterioration. 1,3,5Osteomyelitis (Refractory) : <strong>Hyperbaric</strong> oxygen providesperiodic elevation of bone and tissue oxygen tensions fromhypoxic to normal or hyperoxic levels. This promotesangiogenesis, increased leukocyte killing, aminoglycosidetransport across bacterial cell walls and osteoclast activity inremoving necrotic bone. 23,24Air or gas embolism (AGE) / Decompression sickness(DCS) : Air embolism can occur as a result of surgicalprocedures in a hospital setting. It can also occur in nonsurgicalpatients due to over expansion in a patient onrespirator. Traumatic injuries such as penetrating injuries ofthe chest, blast injuries etc. can all lead to AGE. HBO is theprimary treatment for AGE from any cause. DCS is causedby nitrogen bubble formation in the vascular system and intissues sufficient to interfere with the function of an organ.The cause is rapid decompression during ascent fromdiving, flying or a hyperbaric / hypobaric chamber. HBOtherapy should be begun during the acute episode andcontinued till symptoms clear. 25,26Exceptional blood loss (Anemia) : The patient has lostsufficient red cell mass to compromise respiratoryrequirements and will not receive transfusions because ofmedical or religious reasons. The intermittent use ofhyperbaric oxygen therapy will supply enough oxygen tosupport the basic metabolic needs of the respective tissuesof the body until red blood cells are restored. 27Intracranial abscesses : HBO is recommended as anadjunctive therapy in abscesses in deep locations or multipleabscesses, in compromised hosts, in situations wheresurgery is contraindicated and in patients showing noresponse to conventional treatment. HBO therapy will bebeneficial because of the anaerobic bacterial flora, reductionof edema, enhancement of host defence mechanism and thewell known beneficial effect of HBO in concomitant skullosteomyelitis. 3Sudden deafness : It is well known that cochlear activityis very sensitive to constant supply of <strong>Oxygen</strong>. Manystudies have shown that the performance of the auditorysystem can be improved by an intense application of<strong>Oxygen</strong> during HBO therapy along with haemodilution andvasoactive drugs. Literature survey of 50 studies: 4109patients treated within three months when conventionaltreatment failed concluded that HBO therapy is warrantedJAPI • VOL 51 • MARCH 2003within three months of above indications. 28Post-anoxic encephalopathy : HBO increases oxygensupply to the ischemic neurons, reduces edemas andreverses the reduced flexibility of erythrocytes. HBO 2should be administered as soon as possible and must be partof an intensive reanimation program. 29Visual vascular pathology : HBO has been used in retinalarterial thrombosis (along with other measures) and hasbeen shown to be effective if performed at the earliest inpatients who can still tell the difference between light anddark. In retinal venous thrombosis it is beneficial inreducing vasogenic edema. It must be given as soon aspossible and combined with other pharmacologicalmeasures. 30INDICATIONS WITH PROMISE WHICHARE PROMOTING RECENT INTERESTNeurological indications : The rationale of use of<strong>Hyperbaric</strong> <strong>Oxygen</strong> in neurological indications is based onthe finding in SPECT studies that around the central area ofneuronal death is the penumbra: peri-infarct zone. This zonehas hibernating/idling or sleeping neurons. Also whatappears as gliosis (dead neurons) on CT scans may actuallybe viable tissue for years following the insult (confirmedwith SPECT). 32 HBO delivers high <strong>Oxygen</strong> to these“sleeping cells” and reactivates them. HBO Increasesoxygen supply to the ischemic neurons, reducesedemas and reverses the reduced flexibility of erythrocytes.This is the basis of its use by some centres in acute stroke,post-traumatic brain injuries and cerebral palsy. Thesestudies have shown improvement in these indications. 35Clinical trials & research areas : A number of areas arebeing explored to determine if hyperbaric oxygen might beof clinical benefit. Senility, stroke, and multiple sclerosis areall being investigated. Sports Injuries, high altitude sickness,acute myocardial infarction, brain injury, malignancies,cognitive functions, migraine, glaucoma, fulminant hepaticfailure, are also being actively researched. Sickle cell crisis,spinal cord injury, closed head injury. purpura fulminans,actinomycosis, mesenteric thrombosis, central retinal arteryocclusion , cystoid macular edema, Bell's palsy and leprosyare other areas being explored by workers in multicentrictrials the world over. Other areas being addressed aredesigns of randomised clinical trials, placebo effect,Hawthorne effect, pharmokinetics etc. 3,32CONCLUSION<strong>Hyperbaric</strong> medicine is poised at an exciting era ofrevival. The role of hyperbaric oxygen therapy isscientifically established in certain well defined conditionsand the hyperbaric chamber is now an integral part ofhospital services. Doctors in all fields must familiarisethemselves with recent evidence on this mode of therapy, so283
that their patients are not denied the gains of this moderntreatment. Cost analyses have shown that the addition ofhyperbaric oxygen to conventional treatment results insignificant cost savings due to lesser stay in hospital andshorter course of illness.REFERENCES1. Leach RM, Rees PJ, Wilmshurst P. <strong>Hyperbaric</strong> oxygentherapy. BMJ 1998; 317:1140-3.2. Gabb G, Robin ED. <strong>Hyperbaric</strong> oxygen: a therapy in search ofdisease. Chest 1987;92 :1074 -82.3. Hampson NB. Chairman & Editor. <strong>Hyperbaric</strong> oxygentherapy: 1999 committee report. Kensington MD: Undersea &<strong>Hyperbaric</strong> Medical Society, 1999.4. Grim PS, Gottlieb LJ, et al. <strong>Hyperbaric</strong> oxygen therapy(review). JAMA 1990; 263: 2216-20.5. Tibbles PM, Edelsberg JS. <strong>Hyperbaric</strong> oxygen therapy(Review article). NEJM 1996;1642-1648.6. Sahni TK, John MJ, Madhwal AM et al. <strong>Hyperbaric</strong> oxygentherapy in hospital practice. Bombay Hospital J. 1993;35(4):59 - 64.7. Soodan KS; Roy AK, Singh PK et al. <strong>Hyperbaric</strong> oxygentherapy in stroke cases. Ind J Aerospace Med 1992; 36 (1) :28 - 31.8. Malik D, Gomez G. <strong>Hyperbaric</strong> oxygen therapy: Ourexperiences at 1 AMTC. Ind J Aerospace Med 1999;43 (1):18 –23.9. Bassett BE, Bennett PB. Introduction to the physical andphysiological basis of hyperbaric therapy. In: Davis JC, HuntTK Ed., <strong>Hyperbaric</strong> <strong>Oxygen</strong> <strong>Therapy</strong>, Kensington MD:Undersea & <strong>Hyperbaric</strong> Medical Society. 1986; 11-24.10. Edmonds C, Lowry C, Pennefather J. <strong>Oxygen</strong> toxicity. In:Diving and Subaquatic Medicine 3 rd ed. Oxford: Butterworth -Heineman Ltd. 1994; 241-256.11. Van Den Brenk. The hazards of oxygen toxicity in ahyperbaric environment. In: GS Innes Ed., The productionand hazards of a hyperbaric oxygen environment. London:Pergamon Press, 1970;49-54.12. Feldmeirer JJ, Heimbach RD, Davolt DA, et al. <strong>Hyperbaric</strong>oxygen and the cancer patient, a survey of practice patterns.Undersea and <strong>Hyperbaric</strong> Med 1993;20:337-345.13. Boykin VJ. <strong>Hyperbaric</strong> oxygen therapy: A physiologicalApproach to selected problem wound healing. Wounds1996;8:83-198.14. Cohn GH. <strong>Hyperbaric</strong> oxygen therapy - promoting healing indifficult cases. Postgraduate Medicine 1986;79:89 -92.15. Kindwall EP, Gottlieb FJ, Larson DL. <strong>Hyperbaric</strong> oxygentherapy in plastic surgery. Plastic and Reconstructive <strong>Therapy</strong>1991;888:898-908.16. Urayama H, Takemura H, Kasajima F, et al. <strong>Hyperbaric</strong>oxygen therapy for chronic occlusive arterial diseases of theextremeties. J Japanese Surg Soc 1992; 93:429-33.17. Cramer FS. Care of the injured soldier: A medical readinessrole for clinical hyperbaric oxygen therapy. Medical CorpsInternational 1990;5:36-40.18. Bakker DJ. The use of hyperbaric oxygen in the treatment ofcertain infectious diseases especially gas gangrene and284acute dermal gangrenes. Wageninger: Drukkerij Veenam,1984.19. Riseman JA, Zambons WA, Curtis A, et al. <strong>Hyperbaric</strong>oxygen for necrotising fascitis reduces mortality and need fordebridements. Surgery 1990;108:847-50.20. Marx RE, et al. Radiation injury to tissue. In: EP Kindwall. Ed.,<strong>Hyperbaric</strong> medicine practice. Flag Staff AZ : Best PublishingCo. 1994;447-504.21. Dempsey J, et al. Cost effectiveness analysis of hyperbarictherapy in osteoradionecrosis. Can J Plast Surg 1997;5:221-229.22. Cianci P, Sato R. Adjunctive hyperbaric oxygen therapy in thetreatment of thermal burns: a review. Burns 1994;20:5-14.23. Calhoun JH, Cobos JA, Mader JT. Does hyperbaric oxygenhave a place in the treatment of osteomyelitis? Ortho ClinNorth Am 1991;22:467-71.24. TenheyJE, DavisJC, WorkmanWT. <strong>Hyperbaric</strong> oxygentherapy. Ortho Rev 1987;XIV:829-833.25. Catron PW, Dutka AJ, Biondi DM et al. Cerebral air embolismtreated by pressure and hyperbaric oxygen. Neurology1991;41:314-5.26. Davis JC, Elliot DH. Treatment of the decompressiondisorders. In: Bennett PB, Elliot DH. Ed., The physiology andmedicine of Diving .3 rd Ed. SanPedro: Best Publishers.1982;473-486.27. Hart GB. Exceptional blood loss anemia, treatment withhyperbaric oxygen. JAMA 1974;228:1028-1029.28. Lamm K, Lamm H, Arnold W. Effect of hyperbaric oxygentherapy in comparison to conventional or placebo therapy orno treatment in idiopathic sudden hearing loss, acoustictrauma, noise-induced hearing loss and tinnitus. A literaturesurvey. Adv Otorhinolaryngology 1998;54:86-9929. Astrup J, Sazio BC, Simon L. Threshold of ischemia: Theischemic penumbra. Stroke 1981;12:723-5.30. Oriani G, Magni R et al. A new electrophysiological test toassess opthalmological benefits of hyperbaric oxygentherapy. J <strong>Hyperbaric</strong> Medicine 1990;5:231-7.31. Rockswold GL, Ford SE et al. Results of a prospectiverandomised trial for treatment of severely brain injuredpatients with hyperbaric oxygen. J Neurosurgery1992;76:929-34.32. Jain KK. Ed., Textbook of <strong>Hyperbaric</strong> Medicine. 2 nd Ed.Toronto: Hogrefe & Huber Publishers, 1996.JAPI • VOL 51 • MARCH 2003