Fluent Newsletter Summer 2005
Fluent Newsletter Summer 2005
Fluent Newsletter Summer 2005
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
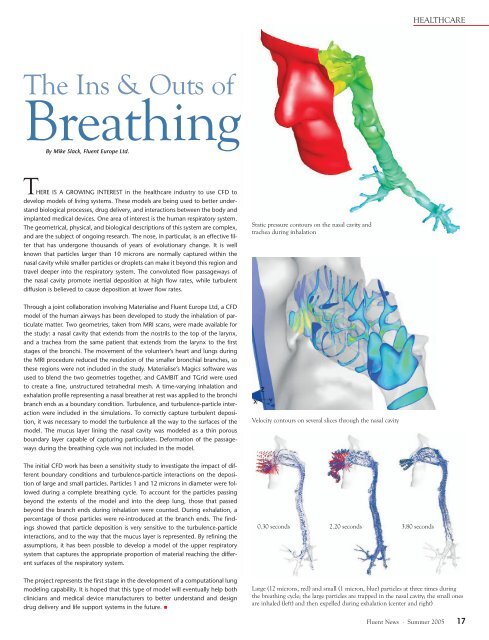
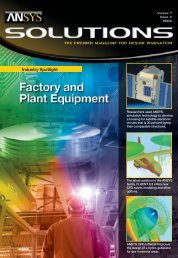
HEALTHCAREThe Ins & Outs ofBreathingBy Mike Slack, <strong>Fluent</strong> Europe Ltd.THERE IS A GROWING INTEREST in the healthcare industry to use CFD todevelop models of living systems. These models are being used to better understandbiological processes, drug delivery, and interactions between the body andimplanted medical devices. One area of interest is the human respiratory system.The geometrical, physical, and biological descriptions of this system are complex,and are the subject of ongoing research. The nose, in particular, is an effective filterthat has undergone thousands of years of evolutionary change. It is wellknown that particles larger than 10 microns are normally captured within thenasal cavity while smaller particles or droplets can make it beyond this region andtravel deeper into the respiratory system. The convoluted flow passageways ofthe nasal cavity promote inertial deposition at high flow rates, while turbulentdiffusion is believed to cause deposition at lower flow rates.Static pressure contours on the nasal cavity andtrachea during inhalationThrough a joint collaboration involving Materialise and <strong>Fluent</strong> Europe Ltd, a CFDmodel of the human airways has been developed to study the inhalation of particulatematter. Two geometries, taken from MRI scans, were made available forthe study: a nasal cavity that extends from the nostrils to the top of the larynx,and a trachea from the same patient that extends from the larynx to the firststages of the bronchi. The movement of the volunteer’s heart and lungs duringthe MRI procedure reduced the resolution of the smaller bronchial branches, sothese regions were not included in the study. Materialise’s Magics software wasused to blend the two geometries together, and GAMBIT and TGrid were usedto create a fine, unstructured tetrahedral mesh. A time-varying inhalation andexhalation profile representing a nasal breather at rest was applied to the bronchibranch ends as a boundary condition. Turbulence, and turbulence-particle interactionwere included in the simulations. To correctly capture turbulent deposition,it was necessary to model the turbulence all the way to the surfaces of themodel. The mucus layer lining the nasal cavity was modeled as a thin porousboundary layer capable of capturing particulates. Deformation of the passagewaysduring the breathing cycle was not included in the model.Velocity contours on several slices through the nasal cavityThe initial CFD work has been a sensitivity study to investigate the impact of differentboundary conditions and turbulence-particle interactions on the depositionof large and small particles. Particles 1 and 12 microns in diameter were followedduring a complete breathing cycle. To account for the particles passingbeyond the extents of the model and into the deep lung, those that passedbeyond the branch ends during inhalation were counted. During exhalation, apercentage of those particles were re-introduced at the branch ends. The findingsshowed that particle deposition is very sensitive to the turbulence-particleinteractions, and to the way that the mucus layer is represented. By refining theassumptions, it has been possible to develop a model of the upper respiratorysystem that captures the appropriate proportion of material reaching the differentsurfaces of the respiratory system.0.30 seconds 2.20 seconds 3.80 secondsThe project represents the first stage in the development of a computational lungmodeling capability. It is hoped that this type of model will eventually help bothclinicians and medical device manufacturers to better understand and designdrug delivery and life support systems in the future. Large (12 microns, red) and small (1 micron, blue) particles at three times duringthe breathing cycle; the large particles are trapped in the nasal cavity; the small onesare inhaled (left) and then expelled during exhalation (center and right)<strong>Fluent</strong> News · <strong>Summer</strong> <strong>2005</strong> 17