Vital Signs: Assessment and Interpretation Importance ... - TMedWeb
Vital Signs: Assessment and Interpretation Importance ... - TMedWeb
Vital Signs: Assessment and Interpretation Importance ... - TMedWeb
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
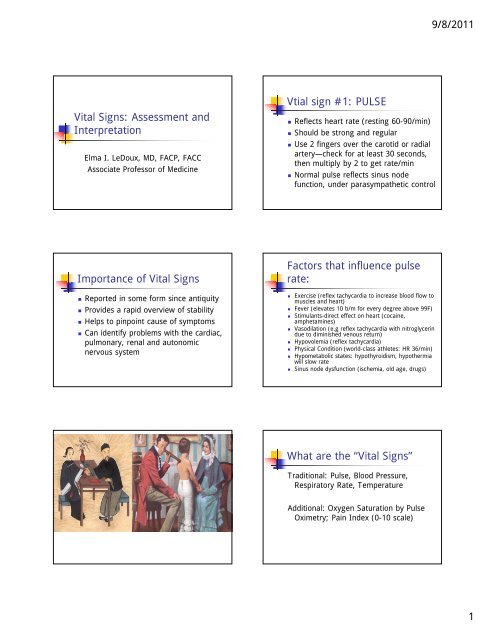
9/8/2011<strong>Vital</strong> <strong>Signs</strong>: <strong>Assessment</strong> <strong>and</strong><strong>Interpretation</strong>Elma I. LeDoux, MD, FACP, FACCAssociate Professor of MedicineVtial sign #1: PULSE• Reflects heart rate (resting 60-90/min)• Should be strong <strong>and</strong> regular• Use 2 fingers over the carotid or radialartery—check for at least 30 seconds,then multiply by 2 to get rate/min• Normal pulse reflects sinus nodefunction, under parasympathetic control<strong>Importance</strong> of <strong>Vital</strong> <strong>Signs</strong>• Reported in some form since antiquity• Provides a rapid overview of stability• Helps to pinpoint cause of symptoms• Can identify problems with the cardiac,pulmonary, renal <strong>and</strong> autonomicnervous systemFactors that influence pulserate:• Exercise (reflex tachycardia to increase blood flow tomuscles <strong>and</strong> heart)• Fever (elevates 10 b/m for every degree above 99F)• Stimulants-direct effect on heart (cocaine,amphetamines)• Vasodilation (e.g reflex tachycardia with nitroglycerindue to diminished venous return)• Hypovolemia (reflex tachycardia)• Physical Condition (world-class athletes: HR 36/min)• Hypometabolic states: hypothyroidism, hypothermiawill slow rate• Sinus node dysfunction (ischemia, old age, drugs)What are the “<strong>Vital</strong> <strong>Signs</strong>”Traditional: Pulse, Blood Pressure,Respiratory Rate, TemperatureAdditional: Oxygen Saturation by PulseOximetry; Pain Index (0-10 scale)1
9/8/2011Pulse can be palpated, but actualrhythm is determined byrecording an electrocardiogram<strong>Vital</strong> sign #3: Respirations• Normal rate is 14-18/min for adults• Rate is driven by metabolic dem<strong>and</strong>s<strong>and</strong> pCo2• Depth of respirations also important• Usually increases along with heart rate• Altered breathing seen in disease:Kussmaul’s, Cheyne-Stokes, SleepApneaRhythms that would causeIrregular <strong>and</strong> Regular Pulses:<strong>Vital</strong> sign 4: Blood Pressure• BP=Cardiac Output X Systemic VascularResistance (i.e. tone in wall of vessels)• Cardiac Output=HR X Stroke Volume (afunction of heart’s contractility <strong>and</strong>amount of blood in Left Ventricle), so• BP= HRXSVxSVR, so a change in any ofthese 3 factors will affect bloodpressure<strong>Vital</strong> Sign #2 Temperature• Reflects normal homeostasis (98.6 d F)• Will increase with hypermetabolic <strong>and</strong>inflammatory states: cocaine, infection, tissuedamage, etc.• Every degree of temp above normal willincrease pulse by 10/min. Why?• Hypothermia -core below 92 degrees F willslow heart rate• Beware of mouth temperature/thermometerBlood pressure:normal 110/70• Expressed as systolic (upper number) <strong>and</strong> diastolic(lower number) pressure in mm of mercury (mmHg)• Determined by inflating BP cuff attached tomanometer <strong>and</strong> measuring gpressure in brachial artery• Flow must be occluded <strong>and</strong> then gradually releasedto obtain the (systolic pressure) sound• Loss of sound as cuff is further deflated is diastolicBP• Referred to as Korotkoff sounds• BP of 140/90 is consistent with hypertension ifrecorded at two or more sittings2
9/8/2011Pitfalls• Cuff too big: artificially low BP• Cuff too small: artificially high BP• Old age <strong>and</strong> stiff blood vessels: requireshigher pressure to occlude flow, givingartifically high BP• Auscultatory Gap- transient loss of sound ascuff is deflated. Be sure to deflate cuff all theway to zero. Always palpate BP first.Putting it all together• The vital signs should be viewed as agroup, because this method gives usthe most information to form adifferential diagnosis.Let’s see if you can determine the causesof the following patients’ vital signmeasurements:Pulse Oximetry• Measures oxygen saturation throughthe use of a transcutaneous deviceattached to the finger or earlobe• Uses photodiode to measure absorptionof light/infrared by blood• Normal pulse oximetry measurementsat room air: 98-100%T 99 P 126 R 24 BP 100/60Pulse Ox 90% RA ; Pain 0/10This 49 year old patient is complaining ofshortness of breath after a surgicalprocedure. She is a not smoker <strong>and</strong> hasnot been able to get out of bed forthree days due to the surgery. She hasnever had any lung problems.Pain Index (on a 0-10 scale)• Makes sure that physicians address painissues• Allows us to quantify pain over time <strong>and</strong>in response to treatment• Often will use face scale3
9/8/2011T98 P 116 R 22 BP 80/60Pulse Ox 93% RA Pain 10/10This 66 year old woman presents withone hour of severe, substernal chestpainT 103 P120 BP150/90 R 30Pulse Ox 90% RA Pain 7/10This 72 year old smoker presentscoughing up green sputum for the pastthree days. He has inspiratory pain overthe right middle lobe of the lung.T98 P110 BP 130/70 R 24Pulse Ox 99% RA Pain 0/10This 49 year old medical school professorrecords these vital signs after runningup six flights of stairs4
9/8/2011T95 P 52 R 14 BP110/70Pulse Ox 94% Pain 0/10This 72 year old woman has becomeprogressively more limited in heractivity, according to her family. Hervoice has become deep <strong>and</strong> shecomplains of feeling cold all of the time.Her face has become puffy <strong>and</strong> shesleeps most of the day.T 98 R36 BP 126/76 P 110Pulse Ox 99% RA Pain 10/10This 16 year old girl just exited a HauntedHouse. She complains of feeling numb<strong>and</strong> tingly all over after being chased bya chain saw masker.T 98 P 54 R 28 BP100/74Pulse Ox 99% pain 0/10This 58 year old man is taking medicationfor high blood pressure. He complainsof tiring easily when he exercises. Youhave taken his vital signs right after hehas walked a brisk 100 yards.5













![Research Opportunities for Medical Students 10-13[1] - TMedWeb](https://img.yumpu.com/35158682/1/190x245/research-opportunities-for-medical-students-10-131-tmedweb.jpg?quality=85)