Path Cardio Outline - TMedWeb
Path Cardio Outline - TMedWeb
Path Cardio Outline - TMedWeb
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
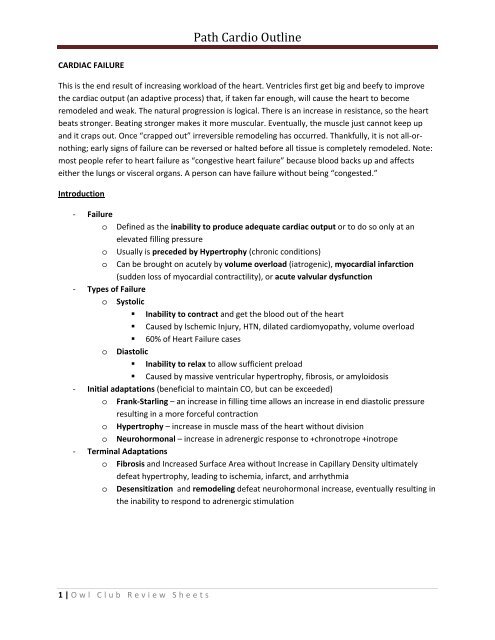
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>CARDIAC FAILUREThis is the end result of increasing workload of the heart. Ventricles first get big and beefy to improvethe cardiac output (an adaptive process) that, if taken far enough, will cause the heart to becomeremodeled and weak. The natural progression is logical. There is an increase in resistance, so the heartbeats stronger. Beating stronger makes it more muscular. Eventually, the muscle just cannot keep upand it craps out. Once “crapped out” irreversible remodeling has occurred. Thankfully, it is not all‐ornothing;early signs of failure can be reversed or halted before all tissue is completely remodeled. Note:most people refer to heart failure as “congestive heart failure” because blood backs up and affectseither the lungs or visceral organs. A person can have failure without being “congested.”Introduction‐ FailureoooDefined as the inability to produce adequate cardiac output or to do so only at anelevated filling pressureUsually is preceded by Hypertrophy (chronic conditions)Can be brought on acutely by volume overload (iatrogenic), myocardial infarction(sudden loss of myocardial contractility), or acute valvular dysfunction‐ Types of Failureo Systolic• Inability to contract and get the blood out of the heart• Caused by Ischemic Injury, HTN, dilated cardiomyopathy, volume overload• 60% of Heart Failure caseso Diastolic• Inability to relax to allow sufficient preload• Caused by massive ventricular hypertrophy, fibrosis, or amyloidosis‐ Initial adaptations (beneficial to maintain CO, but can be exceeded)o Frank‐Starling – an increase in filling time allows an increase in end diastolic pressureresulting in a more forceful contractiono Hypertrophy – increase in muscle mass of the heart without divisiono Neurohormonal – increase in adrenergic response to +chronotrope +inotrope‐ Terminal Adaptationso Fibrosis and Increased Surface Area without Increase in Capillary Density ultimatelydefeat hypertrophy, leading to ischemia, infarct, and arrhythmiao Desensitization and remodeling defeat neurohormonal increase, eventually resulting inthe inability to respond to adrenergic stimulation1 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>Normal: ClearWhite AlveoliEdema = no whiteair spaces, all pinkfrom fluidLeft‐Sided Failure‐ CausesoooIschemic Heart Disease = infarction and loss of myocardium (acute)HTN, Aortic Stenosis = increased afterload, hypertrophy, subsequent failure (chronic)Some Diastolic Dysfunction can result from nonischemic myocardial disease• Restrictive or Hypertrophic <strong>Cardio</strong>myopathy•‐ Morphologyo Chamber is usually hypertrophied and dilated (according to Robbins its also dilated)o Fibrosis within myocardiumo Secondary Atrial Enlargement with resultant Atrial Fibrillation• Fluid is not ejected, so backs up into atrium, which cannot hypertrophy, onlydilate• Atrial enlargement = atrial failure = inability to contract• Compromise of cardiac output (loss of atrial kick)• Increased risk of thrombus from stagnant fluid‐ Effect on Lungso ↑Pressure in pulmonary veins is translated to arterioles and capillaries• Leads to pulmonary edema (the congestive part of congestive heart failure)o Hemosiderin• Iron or Heme containing compounds are phagocytized by macrophages,converting them to hemosiderin.• Presence of these siderophages in pulmonary tissue denotes previous edemao• Nick‐named “heart failure cells” or hemosiderin‐laden macrophages• <strong>Path</strong>ognomonic for Pulmonary Edema (current or past)Symptoms• Dyspnea = difficulty breathing, especially during activity• Orthopnea = difficulty breathing upon laying down, patients sleep with pillows• Paroxysmal Nocturnal Dyspnea = severe Dyspnea at night‐ Effect on Kidneyso Decreased CO = Decrease RBF = Increase in Renin/ANGII in response. ANG II causes:• Constriction of efferent arteriole = increased filtration = good• Vasoconstriction = increased TPR = increased afterload = bad• Salt Retention = Fluid Retention = increased preload (venous return) = bad• “Bad” is bad because it ↑cardiac demand in an already failed hearto Decreased filtration = decreased nitrogen excretion = azotemia‐ Effect on Braino Cerebral Hypoxia = Hypoxic Encephalopathy, only in severe cases• If you can’t breathe because there is fluid in your lungs where oxygen should be,you obviously won’t get enough oxygen to your brain3 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>InflammationNormalHepatic HistologyRight Sided Failure‐ CauseooLeft failure pulmonary HTN increased afterload for Right RightHypertrophy/Failure• The most common cause of Right Failure is Left Failure, but often they are testedas separate elementsCor Pulmonale = Primary Pulmonary Hypertension• Chronic hypoxia (COPD, Bronchitis, Asthma) leads to pulmonary vasoconstriction• Pulmonary Vasculitis decreases luminal size, again increasing resistance• Vasoconstriction, Increased Resistance, HTN, all the same as saying “more towork against” making the right ventricle hypertrophy, then fail.‐ Portal Hypertensiono Congestive Hepatomegaly• Increased size and weight from engorgement of blood• Central Hypoxia with centrilobar necrosis• Prolonged ischemia = cardiac sclerosis/cirrhosis from increased fibrous tissue• Nicknamed a nutmeg livero Congestive Splenomegaly• Engorged spleen with sinusoidal enlargement, stasiso Ascites• Edema into the peritoneum from GI/Portal Overloado Distended Jugular Veins and pitting edema• Backup of the vena cava superiorly (JVD)• Backup of the vena cava inferiorly (edema of the ankles)‐ Kidneyso Backup of blood = increase pressure in portal vein = decreased blood flow throughkidneys = decreased filtration = worsening azotemia‐ Lungs and Hearto Pulmonary Effusions = accumulation of fluid in pleural space (not the alveoli)o Pericardial Effusions = accumulation of fluid in pericardial spaceSide Causes Heart Changes Lungs Organs EffectedLeft Systemic HypertensionAortic StenosisIschemic InjuryNonischemic Injury (genetics)ConcentricHypertrophy, dilatedor notPulmonary Edema,fluid in alveolarspacesKidneys, Lungs,BrainRightCor PulmonaleLeft Ventricular FailureConcentricHypertrophy, dilatedor notPericardial effusions(fluid in pleuralspace)Liver, Kidneys,Lungs, heart, brain4 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>Left Atrium to Right AtriumLeft Ventricle to Right VentricleCONGENTIAL ABNORMALITIESLEFT TO RIGHT SHUNTLeft to right shunts are characterized by insufficient cardiac output (since some of the left ventricle goesto the right side of the heart) that causes cyanosis months after birth. The blood is oxygenated, just notall of it gets out into the systemic vasculature. This high pressure entering the pulmonary vasculaturemurders the lungs, causing eventual pulmonary Vasculitis and eventual reversal of the shunt leading tocyanosis and death. All LR Shunts have a D in their acronym.Atrial Septal Defect (ASD)‐ Definitiono Abnormal opening permitting flow between the left and right atria that is not a patentforameno If on its own, it is asymptomatic until adulthood‐ Morphologyo Usually isolated = occurring on their owno When with other abnormalities, the other malformation is more hemodynamicallysignificanto Types are dependent on where they occur• Secundum = 90% of cases, defect or fenestration of the oval fossa• Primum = 5%, occurring at the AV valves, occur with cleft anterior mitral valve• Sinus Venosus = 5% occurring at entrance of vena cava.‐ Clinical Presentationo L R shunt because the left ventricle has a higher pressure and the right ventricle ismore distensible (the push comes from the atria, remember)o Profound Pulmonary edema if the opening is severeo Murmur is present from excessive fluid, present in all caseso Right Ventricle Hypertrophy or Dilated Right Atrium is almost a certainty, regardless oflevel of symptomsVentricular Septal Defect (VSD)‐ Definitiono Incomplete closure of the ventricular septum allowing a ventricular L R shunto It is the most common congenital cardiac abnormality (Robbins says both VSD and ASDare, review books say VSD is)o Only 30% are isolated, many occurring with tetroloagy of fallot.‐ Morphologyo There is a hole about the size of the aortic valve in the septum• Membranous VSD = 90%, involving the septum• Infundibular VSD = 10%, involving the are below the pulmonary artery5 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>Out the aorta, back into thepulmonary vasculature,‐ Clinical Presentationo Small defects = close spontaneously (which is why surgery is delayed until 1 year of age)o Large Defects = permission of LR flow• Right Ventricular Hypertrophy and Pulmonary Hypertension as expected• Pulmonary Vascular Disease will lead to narrowing of pulmonary vessels leadingto an essential stenosis, reversing the shunt to make a “blue baby syndrome” asin RL shunts, in the adult, which is fatal.o Cardiac Failure and Murmur are present at birthPatent Ductus Arteriosis (PDA)‐ Definitiono Persistent ductus arteriosis, maintaining shunt between pulmonary artery and aortadistal to the major branches (carotid and subclavian).o Used to bypass pulmonary circulation in the fetus (RL shunt), now that there is a largeleft ventricle, it creates a patent LR shunt‐ Clinicalo Usually no difficulties at birth or with developmento Detected as a continuous harsh murmur, “machine‐like”o LR = no cyanosis, right ventricular hypertrophy, pulmonary hypertension andVasculitis (as expected with all LR)• Pulmonary Vasculitis will cause a reversal of shunt = blue baby syndrome inadults, which is fatal• Closure of patent ductus is necessary as soon as possible when isolated• Patency is the only thing keeping the infant alive if there is pulmonary orsystemic obstruction. Indomethicin to close, Misoprostol (PGE) to open.Atrioventricular Septal Defect (AVSD)Two giant chambers,separated by one valve‐ When Complete. Basically, you have one giant heart with two chambers, and two outflows. Theone ventricle communicates with the pulmonary vasculature and the systemic vasculature,causing a mixture of oxygenated and deoxygenated blood to circulate. Causes volume overloadhypertrophy and failure. Surgical repair is possible. This one is almost never asked in anyreview book.RIGHT TO LEFT SHUNTSRight to left shunts mix deoxygenated blood with the systemic vasculature. This causes “blue babysyndrome” caused by cyanosis. In these cases deoxygenated blood from the right side of the heartenters systemic circulation without passing through the lungs. In order for this to occur, there musteither be extreme resistance in the pulmonary vasculature with a passage between left and right sides(otherwise the left ventricle would force a LR shunt), or there is a problem with the outflow pipes(switching of position, failure to separate, etc). All acronyms have a “T” in them.6 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>Pulmonary valve is“closed” or heavilystenosed and there isa communicationbetween RV and LVTransposition of greatvesselsTransposition of aorta to RV andpulmonary trunk to LV with VSDto convey survivalTetralogy of Fallot – TOF‐ Definitiono Tetralogy is:• Ventral Septal Defect that give communication between left and right ventricles• Obstruction of Right Ventricular Outflow (subpulmonary stenosis) preventing theLR shunt that would occur with a VSD• Aorta positioned on top of the VSD, allowing right ventricle to pump into aorta• Right Ventricular Hypertrophy as a result of increased pulmonary resistance andthe right heart’s ability to pump to the left/systemic vasculatureo Caused by an anterior superior displacement of infundibulum‐ Clinical Courseo Dependent on the severity of pulmonary stenosis• Mild = symptoms of an isolated VSD with a LR shunt, so called “pink fallot”• Severe = classic RL shunt, called “blue baby fallot”o Classic Case progression• Right Ventricle pushes blood through VSD and into systemic circulation becauseAortaPARV (hypertrophic)LV (hypoplastic)Without Shunt, there are effectivelytwo independent circulationsthe stenosed pulmonary outflow causes increased resistance, resulting in RVH• Pulmonary Vasculature gets smaller and thin walled = hypoplastic• Aorta gets larger in diameter, while the pulmonary gets smaller• Makes the stenosis worse• Even pink fallot babies progress to blue babieso Fixable with surgery‐ Transposition of Great Arteries – TGAo Definition• Normal vasculature is VCRARVPAPVLALVAorta• TGA vasculature is VCRARVAorta and a separate PVLALVPA• The left ventricle and lungs form their own circuitoo• Blood circulating to system is purely deoxygenated• Aorta is normally posterior and to the left of the pulmonary artery, and now itanterior and to the right of the pulmonary artery.Morphology• Without other defect this is incompatible with life• Right Ventricular Hypertrophy because the right ventricle is now systemic• Left Ventricular Atrophy because the left ventricle is now pulmonary• Some shunt must exist for survivalClinical Course• There is an increased survival with increased mixing of blood(LR)• A large ventral septal defect conveys survival• A patent foramen ovale is tenuous, as it is likely to close• Surgery is made to maintain VSD or Patent Foramen Ovale, while areswitching of great vessels is made later in life7 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>RA and RV communicatethrough a RL atrialconnection, and againthrough a LR ventricularconnectionTruncus Arteriosis ‐ TA‐ Causeo‐ ClinicaloooTricuspid Atresia – TA‐2‐ CauseooA failure of the Aorta and the Pulmonary artery to separate from the truncus arteriosis.• Both come from the same embryonic tube, and they must separate to form twovessels.• Results in one giant great vessel connected to both ventriclesSingle great artery connecting everything resulting in normal and abnormal connectionsAbnormal• The Left ventricle to the lungs causing pulmonary hypertension and Vasculitis• The right ventricle to the systemic vasculature causing cyanosis and rightventricular hypertrophyNormal• Left ventricle to the systemic vasculature• Right ventricle to the pulmonary vasculatureUnequal division of the AV canal results in a larger‐than‐normal mitral valve and atricuspid vale that doesn’t open.The Right Atrium and the right ventricle cannot communicate because there is just awall, where there should be a valve‐ Morphologyo Atrophy/Hypoplastic Right ventricleo If survival is to be achieved, there must be a means around the atresic valve• Patent Foramen Ovale or ASD allows RL shunt atria to atria• VSD allows the left ventricle to push deoxygenated blood from RA intopulmonary vasculature‐ Clinicalo Cyanosis from birth with a high mortality rateTotal Anomalous Pulmonary Venous Connection (TAPVC)‐ CauseoCommon pulmonary vein does not form, and therefore there is no great vessel comingfrom the lungs to the right atrium. Longevity dependent on severity‐ Morphology and Clinicalo TAPVC are the veins that make the difference, coming from the lungs back to the rightatrium, requiring an ASD or a patent foramen ovale to get oxygenated blood to the LVo RA is dilated, RV is dilated and hypertrophic, LA is hypoplastic, LV is normal, pulmonaryvasculature is dilated8 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>StenosisInfantile. Notice where bloodis blue and where it is redAdult. Notice there isonly oxygenated blood.OBSTRUCTIVE CONGENITAL DEFECTSThese are defects whereby there is an inappropriate closure or failure to open of one of the largervessels or valves. It creates an obstruction (a stenosis or other increase in resistance) that causesabnormal flow.Coarctation of the Aorta‐ Definitiono Narrowing or encroachment on the lumen of the aorta, either descending or ascending(meaning proximal or distal) to the major brancheso Increased resistance to left ventricular outflow and decreased perfusion to organssupplied distal to occlusion/stenosiso Coarctation with Patent Ductus = “Infantile”• Symptom onset is early in life, and is usually fatal• Coarctation is proximal to major branches, with patent ductus arteriosis• Oxygenated blood cannot get through the stenosisoStenosis• Deoxygenated blood gets around the stenosis through PDA, supplyingbrain and body with deoxygenated bloodCoarctation without Patent Ductus = “Adult”• Symptom onset is dependent on severity of stenosis, in childhood or evenadulthood, with coarctation distal to major branches• Significant hypertension in upper extremities because left ventricle suppliesthem well with oxygenated blood, but the lower half is “cut off”• Weak Pulses and hypotension in the lower extremities, revealed as intermittentpain (claudication) on excess movement of the legs• Collateral circulation through enlarged intercostals supplying organs distal tocoarctation, revealed as “rib‐notching” on chest X‐ray.‐ Commonalitieso Systolic murmur that may be a thrill (more likely in infantile)o Left Ventricular Hypertrophy from increased resistanceo Grafting, Ballooning, and surgery have good outcomes (remember Anatomy PBL)Pulmonary Stenosis and Atresia‐ Causeo Mild to severe obstruction of pulmonary valveo Can be isolated or occur with other abnormalities (Tetralogy of Fallot or TGA)‐ Morphologyo Right Ventricular Hypertrophy from increased resistanceo Pulmonary Artery Dilation from forceful stream through stenosed valveo If entirely atretic = must be ASD with PDA to maintain blood blow, RV is hypoplastico If with another disease, RV pressure is not translated to the valve, meaning rightventricular hypoplasia9 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>Aortic Stenosis and Atresia‐ Cause (3 kinds, all result in obstruction to left ventricular outflow)o Valvular – effects the cusps = dysplastic (thick) or abnormal number (fusion)o Subaortic – thickening of fibrous subendocardium prior to the cuspso Supravalvular – ascending wall is abnormally thick with luminal intrusion‐ Clinical and Morphologyo Severe Atresia = Hypoplastic Left Heart Syndrome• LV hypoplasia with Aortic Hypoplasia from decrease outflow tract• Requires a patent ductus arteriosis to get any blood through.• Fatal after the first week of life as the ductus closeso Moderate to mild• LVH from afterload increase• Requires prophylactic antibiotics• Strenuous activity can cause deatho In all cases there is a prominent systolic murmur that is nondiagnostic for locationDISEASES OF THE BLOOD VESSELSDisease Type Cause SymptomsAtrial SeptalDefectL R ShuntVentralSeptal DefectPatentDuctusArteriosisTetralogy ofFallotTranspositionGreatArteriesTruncusArteriosisTricuspidAtresiaCoarctationof AortaL R ShuntL R ShuntRL ShuntRL ShuntRL ShuntRL ShuntObstructionHole between the atria allowing oxygenated blood intoright ventricle. Most common defect to occur alone, notthe most common in general. More commonly occurs inthe Primum (90%) and sometimes in Secundum (10%)Hole between the ventricles allowing oxygenated bloodinto right ventricle. Most common defect in the heart.Associated with Down’s Syndrome.Hole between the aorta and pulmonary artery allowing oxblood into lungs. Kept open with prostaglandin, closedwith indomethacinRVH, Subpulmonary Stenosis, VSD, Aorta on top of VSD.Caused by a anterosuperior movement of infundibulum.Must be surgically corrected. Look for “boot‐shapedheart” in the vignette.Swapping of aorta to RV and pulmonary artery to LV,requiring communication (PDA) for life. Requires surgicalcorrection. If no surgery, is fatal in 1 st month of lifePulmonary artery and aorta do not separate, so are one bigoutflow vessel allowing mixing of blood in both directions.RA and RV do not communicate, requires ASD and VSD forlife. The tricuspid valve never forms a holeInfantile = Coarctation proximal major branches (fatal)Adult = Coarctation distal major branches (found as a kid)Occurs in Turner SyndromeAortic Atresia Obstruction Stenosis or Atresia from something being in the way of leftventricular outflowPulmonary Obstruction Stenosis or Atresia from something being in the way ofAtresiaright ventricular outflowPulmonary hypertension,Pulmonary Vasculitis, Latestage reversal of shunt =cyanosis and fatality, calledEisenminger’s Syndrome. TheRV will hypertrophy and/orpulmonary artery will stenose,reversing the flow to RLBlue baby syndrome, occursearly in life, deoxygenatedblood gets into systemicvasculature causing cyanosis.High mortality rate, requiringsurgical intervention. Right toleft shunts will not reverse.Variable on PDA and extent ofcoarctation, usually distalcyanosis or weak pulseAtresia = Hypoplastic LVStenosis = LVHRight ventricular hypertrophyand Pulmonary Dilation10 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>ISCHEMIC HEART DISEASEIschemia is defined as a mismatch between myocardial oxygen supply and demand. Whether ithappens over years or happens right now, if there is not enough supply, the myocardium will suffer.Types of IschemiaLumenConcentric Plaque‐ Chronico Caused by atherosclerosis, with the formation of plaques and a concentric stenosis ofthe coronary vessels leading to decreased blood flow. May be associated withvasospasm, thrombosis, or embolus.• At 75% occlusion, 25% flow, patients will experience exercise induced ischemia• At 90% occlusion, 10% flow, patients will experience ischemia at rest.o This represents the little old lady with years of smoking and fried chicken, with sufficientstenosing of her vessels• Multiple angina events will indicate ischemic disease, and can be managed‐ Acuteo Caused by vasospasm, embolus, or thrombosis without previous indication of ischemicdisease. The first event is the Myocardial Infarction that kills them.• There is no significant stenosis, there is no induced angina/ischemia• May be histological indications, eccentric non stenosing plaques.o This is the 16 year old kid who does cocaine, suffering from an increased heart rate(increase myocardial demand) with vasospasm, reporting the ER with chest painCauses of Ischemia‐ Acute Plaque Changeo Changes in the condition of a stable plaque (either concentric/nonconcentric) lead tothrombosis and complete occlusion of a vessel• Rupture/Fissure = exposes highly thrombogenic plaque interna• Ulceration/Erosion = exposes highly thrombogenic basement membrane• Fragmentation/Embolus = plaque breaks off and occludes smaller vessel (rare)o Intrinsic plaque Influences• Increase in Foam Cells, Lipids, thin fibrous cap, Increase Inflammatory cells allincrease the risk of plaque changeo Extrinsic Plaque Influences• An increase in mechanical stress on a weak fibrous cap leads to damage• Adrenergic Stimulation, Emotional Stress, even the awakening from sleep allincrease cardiac output and predispose for increased mechanical stress11 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>Angina‐ Inflammationo The stability of a plaque is dependent on collagen and the fibrous content.o Activation of macrophages (active inflammation) results in metalloproteinases thatdegrade the collagen, weakening the fibrous cap.o C Reactive Protein is an acute phase molecule of inflammation, used as a prognosticindicator for ischemic events‐ Vasoconstrictiono Vasospasm, for whatever reason, occludes blood vessel. In a healthy vessel, this doesnothing. In an already stenosed vessel, this causes occlusion.o Responds well to nitratesThere is a spectrum of conditions that represent minor occlusion to complete occlusion. Thus, there aredifferent types of angina. While categorized in the coming section, it must be noted that there is in facta continuum of states and conditions that makes its way from stable to unstable to full blownMyocardial Infarction. Pritzmental is a special kind of angina. Angina itself is ischemic chest pain.‐ Stable Anginao Significant stenosis = 75% occlusion = decreased perfusiono Perfusion maintained while at resto Exercise or emotional stress = increase in demand = ischemic chest paino Alleviated with rest or nitrates‐ Unstable Anginao Worsening stenosis = 90% occlusion = critically decreased perfusiono Perfusion compromised while at rest or with little exertion.o Severe stenosis, thrombus, or vasospasm not alleviated by nitrates‐ Pritzmental Anginao Uncommon, irregular attacks caused by vasospasmo Responds well to nitrateso Is unrelated to physical activity, BP, stress, etcMyocardial InfarctionAn infarct occurs in an area supplied by an occluded coronary vessel. For all intents and purposes, thereis no collateral circulation in the heart, except in the case of long term, severely stenotic disease. Thewall is thick, the arteries are on the epicardial surface. Therefore, the myocytes of the endocardialsurface (called the subendocardium) are at particular risk, being farthest from the blood supply whilethe myocytes of the epicardial surface (called the subepicardium) are at least risk. Infarction results innecrosis and loss of function, unless reperfusion can be achieved in a relatively short amount of time.12 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>‐ Typeso Transmural• Complete thickness, literally “across the wall” from subendocardium tosubepicardium representing a long standing, severe ischemia• Caused by an unalleviated completely occluding thrombosis or stenosis.• Occurs in a single geographical region supplied by the occluded vesselo Subendocardial• Involves less than the full thickness (1/3 – 1/2)• Subendocardium is the least well perfused and is most vulnerable• Coronary occlusion causes single area of riskPink area representsSubendocardial infarct• Systemic hypotension may result in global ischemia of vulnerablesubendocardium throughout heartPink arearepresentstransmural infarctInverted TST ElevationQ Wave‐ Clinical Features of MIo Patient ‐ Presentation Suspects an MI• Cold, Clammy, Diaphoretic, Dyspnea, Substernal Chest Pain (visceral painexplained as a crushing) that radiates to the Jaw or down the arm• Feeling of Impending Doom – “I’m going to die!”• Diabetics, Elderly and Women may be asymptomatic (silent MI).o Electrocardiogram ‐ Screen Suspected patients for MI• Hallmark of ischemia is the T wave inversion• Hall mark of Infarct = ST Segment Elevation (Transmural) ST SegmentDepression (Subendocardial)• Hallmark of Old Infarct is Q wave ElongationoCK‐MB Troponin82,000 24,000Mol.WeightIncrease 3‐6hrs 4‐8hrsPeak 12‐24hrs 12‐16hrsReturn 24‐72hrs 5‐9daysLabs – Troponins and Ck‐MB Confirm the Diagnosis• Cardiac Troponins are the new golden standard. Unique to myocytes,detectable throughout evolution of MI. Get Troponin I• CK‐MB is former golden standard. Creatine Kinase is in brain (CK‐BB), muscle(MM) and in heart (MB). When damaged, the heart should release CK‐MB.Difficult to track, could be associated with another condition, and is onlydetectable later in evolution• Myoglobin, lactate Dehydrogenase (LDH), C reactive Protein, are usefulmarkers when the clinical picture of infarct is present. These are nonspecific formyocardium and may be elevated if the patient worked out that day13 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>‐ Coronary Artery Occlusiono Atherosclerosis causes occlusion of the coronary vesselo Rupture of the atherosclerotic plaque causes thrombosis ischemiao Vasospasm of the vessel around it causes vasoocclusion ischemia‐ Reperfusiono Methods• Thrombolytics = “clot busters” eliminate thrombus, not plaque• Percutaneous Coronary Intervention (Angioplasty/Stent) gets rid of theocclusion, the thrombus, and the plaque• Coronary Artery Bypass Graft (CABG) provides flow around obstructiono Effects• Early Reperfusion (6hrs) no help = and may actually be hazardous, will notimprove infarct size.o Reperfusion Injury• Caused by leukocyte produced O 2 Free Radicals distributed to healthy tissueupon reperfusion• Probably apoptosis mediated (future of anti‐apoptotic meds)o Terminology• Stunning = post infarct dysfunction that may result in permanent remodeling orfailure. Ischemic tissue becomes more damaged because of reperfusion.• Preconditioning = frequent angina attacks prior to major ischemic event trainsthe tissue to be hypoxic and the ischemic event is not as severe.Ventricular Aneurysm (not rupture)Transmural (grey) MI on the upper right ofimageFibrinous Pericarditis, DresslerSyndrome, post MIHere are some gross images of an MI and complications. Check out the next page for histology.On the following page you will see the evolution of an MI in chart form. You must know what it looks likein gross, what it looks like in micro, and what the risks are for any given period. The paragraph formathas a simplistic view that is similar to First Aid.The questions you will have to answer is usually “if a patient dies at time X… what did he die of or whatdoes his hear look like?”14 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>GROSS CHANGES FOLLOWING MISurvival Time Predominant Finding0‐18 hrs No Change18‐24hrsVague pallor change, visible with special stain1‐3 Days Yellow Pallor in the center3 Days – 4 weeks Yellow Pallor with surrounding Hyperemia6 Weeks + White/Grey Firm ScarSee page First Aid Page 262, Edition 2009 for a simplistic version of all this informationHISTOLOGIC CHANGES FOLLOWING MISurvival Time Predominant Finding1‐4 hrs Wavy Myocytes and contraction bands4‐24hrsCoagulative Necrosis with few Neutrophils1‐3 Days Coagulative Necrosis with many Neutrophils3‐7 Days Coagulative Necrosis with Macrophages10+ Days Collagen Deposition, Fibroblasts, MacrophagesRISK FOLLOWING MISurvival Time Predominant Finding0‐1 hrs Fatal Arrhythmia1‐7daysVentricular Rupture (Septal Wall or Ventricular Wall)7+ Days Ventricular Aneurysm (no rupture, just outpouching, leading to mural thrombus)Any pointChordae Rupture, Valve Prolapse, HypotensionCoagulative Necrosis (pink myocytes have no dark blue nuclei) withinfiltrates in between. You can’t tell if they are neutrophils ormacrophages, so you don’t know if you are at 1‐3 or 3‐7daysGranulation Tissue. Good Myocytes are to the bottom right. The rest isamorphous, mostly white fibrous tissue. The repair process if nearlycomplete. Note that myocytes do not regenerate, as they arepermanent cells, permanently in G oTrichrome stain showing the blue collagen laid down after everythingis said and done. This is an old MI with scar tissue already formed.Normal myocytes are to the left, blue collagen all over, new arteries(granulation tissue) to the right)15 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>HYPERTENSIVE HEART DISEASEThe topic here goes very closely with the section at the beginning of the discussion on heart. Why it isseparated, I am uncertain. However, it is kept separate so as to go along with Robbins. This is whathappens BEFORE the heart fails.Left Ventricular Hypertensive Heart DiseaseLeft Ventricle is largerthan normal‐ Diagnosiso Left ventricular hypertrophy with a history of pathologic hypertension (140/90 orgreater on either systolic or diastolic) without any other pathology to explain it‐ Signs and Symptomso May be asymptomatic and the hypertrophic heart is found on routine echo or ECG. Thistype of heart disease would be considered compensatedo May present with atrial fibrillation (atrial dilation), Congestive Heart Failure (pulmonaryedema), or both. This is an example of uncompensated‐ Morphologyo Concentric Left Ventricular Hypertrophy without Dilation on grosso Myocytes show an increased transverse diameter, irregular or large nuclei and cells,with evidence of interstitial fibrosis on histologic prep.‐ Outcomeso Spectrum depending on how well hypertension is managed. There may be a completereversion of remodeling back to a normal heart, or the patient may progress to full onfailure and die of CHF. Anything in between is possible as well.Right ventricle is dilatedHypertrophy is tough tosee.Right ventricular Hypertensive Heart Disease‐ Definitiono Rare form of hypertensive heart disease, occurring only in cases of diseases of thepulmonary system or of the pulmonary vasculature that result in an increase inresistance of the right ventricle• COPD, Cystic Fibrosis, Sarcoidosis• Recurrent Embolism, Primary Pulmonary Hypertension, Drugs (Digoxin,Bleomycin, Isoiazid)• Obstruction of airway, metabolic acidosiso Left ventricular failure resulting in fluid backup and subsequent right ventricular failuredoes not count as RV Hypertensive Heart Disease, but is the most common cause ofRight Ventricular Hypertrophy and Failure.Morphologyo Acute cor pulmonale = Dilation of the right ventricleo Chronic cor pulmonale = Hypertrophy of right ventricle (to the width of a normal LV)o Cor Pulmonale = primary pulmonary hypertension16 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>VALVULAR HEART DISEASEValves control the flow of blood. Problems arise when the valves cannot close properly allowingbackflow (regurgitation / insufficiency), when they cannot open correctly causing an increase inresistance to flow (stenosis), or a combination of both. Regurgitation can occur either as a pathologicalfinding of the valve, or of a functional regurgitation whereby the dilation of the ventricle pulls thechordate tendinae apart, preventing the normal healthy valve from functioning correctly. The severity ofthe disease is variable, ranging from chronic long‐onset (chronic rheumatic fever) with adaptation torapid, fatal onset (bacterial endocarditis). The morphological changes to the heart will representwhatever is wrong (outflow blocked = hypertrophy, regurgitent jet = fibrosis) as will be shown. The fourmost relevant dysfunctions are mitral valve regurgitation and stenosis, and aortic valve regurgitationand stenosis.Calcific Aortic Stenosis (can also happen to the Mitral Valve, called “Mitral Annular Calcification”)NormalCalcifications‐ Causeo Induced by the normal “wear‐and‐tear” of valve leaflets, experiencing 40 millioncontractions per dayo Calcifications develop slowly over many decades‐ Morphologyo Heaped‐up calcified masses within the aortic cusps that protrude through the outflowsurfaces preventing opening of the valves. Basically, calcifications act as door stops,preventing the valve from opening all the wayo Calcification begins at the valvular fibrosa, the points of maximal tensiono There are no commissural fissures‐ Clinical Featureso Increased stenosis = increase resistance = effective systemic hypertension = LeftVentricular Hypertrophy which leads to left ventricular failure.o Crescendo‐Decrescendo Systolic MurmurBalloonMyxomatous Degeneration of the Mitral Valve (aka Mitral Valve Prolapse)‐ Causeo Unknowno Prospect says there is a defect in connective tissue that causes prolapsed after stressfrom ventricular pressure‐ Morphologyo Gross• Enlarged Ballooning of mitral leaflets• Tendinous Cords are long, thin, stretched, or even snapped off• Annular Dilation is common in mitral valve prolapsed, rare in other conditionso Histology• Attenuation of the fibrous layer• Focally marked thickening of the spongiosa17 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>Cardiac Muscle‐ Clinical featureso Generally asymptomatic, with approximately 1% of population having the condition,diagnoses on routine echo or physical examo Holosystolic Systolic Murmur can be audible if sufficiently bado While asymptomatic, there is an increased risk of developing• Infective Endocarditis – Bugs hide in the pocket formed by the bulging• Thrombi – Stagnation and clots can hide in that same pocket• Mitral Insufficiency – if the prolapsed gets really bad, ejection fraction (to theperiphery) is so low as to require surgeryRheumatic Fever and Rheumatic Heart DiseaseBoth of these diseases affect the heart. Rheumatic Fever is technically the acute condition, upon which,with subsequent repeated episodes, results in Rheumatic Heart Disease, the chronic condition.Giant CellsInflammatory InfiltrateRemoved Mitral Valve showingthickening and commissuralfusion‐ Causeo Sequella of an untreated Strep A pharyngitis (S. Pyogenes)• Antibodies to Strep A M protein cross react with heart and joint tissue in host• Reinfection causes reactivation of antibodies and subsequent autoimmuneo Chronic damage from repeated exposure causes long term destruction and fibrosis ofthe cardiac tissue (which cannot regenerate)‐ Morphologyo Acute• Aschoff Bodies = inflammatory lesions• Swollen Eosinophilic Collagen + Tc cells + Plump Macrophages calledAntishkow Cells• Cause a Pancarditis infecting any layer of heart (epi, endo, myocardium)oChronic• Organization of acute inflammation that leads to fibrosis• Gross• Leaflet Thickening, Commissural Fusion and Shortening, Thickeningand Fusion of Chordae Tendinae• Is the leading and definitive cause of mitral stenosis (99% of cases)‐ Clinical Featureso Acute• 10days‐6weeks after Strep A infection pharyngitis (must be pharyngitis)• Arthritis of large joints (adults>kids, resolve spontaneously)• Carditis (pleural friction rub, weak pulse, tachycardia)• Rash, Fever, Spastic Movementso Chronic• No symptoms for decades, results in a fibrotic stenosis eventually• Symptoms depend on severity and valvular involvement• 75% cases Mitral Stenosis Alone, 25% cases Mitral and Aortic18 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>Red bumps should notbe thereInfectious EndocarditisNormal ChordeaInfective Endocarditis has large,friable vegetative lesions usuallyon one side of the valveFibrosisInflammatory cells‐ Causeo Predisposing factors• Rheumatic heart disease, mitral valve prolapsed, calcified aortic stenosis,prosthetic heart valves, or any condition that causes abnormal flow or creates apocket for the organism to hide inooLots of inflammatory cells and fibrousspots on the valveOrganisms• S. Pyogenes = RHD, noninfective fibrosis is more of a predisposition than aninfection• S. Viridans = 50‐60% of all cases of normal heart valves, the dental organisms• S. Aureus = Highly virulent, seen commonly in IV drug users• S. Epidermis = commonly infect prosthetic valves• Other = Fungi or Gram negative BacilliRoutes• The foremost predisposing factor is bacterial seeding (you have to let them in)• Obvious infection, dental work, IV drug use, penetrating trauma, occult gut‐ Morphologyo Vegetations• Effect mitral or aortic valves usually, though right sided is possible• Vegetations are friable (they break), bulky, potentially destructive containingfibrin, inflammatory cells, and the bacteria• They may erode into the myocardium forming a ring abscesso Changes• Systemic Emboli may break off and cause infarcts with abscesses because of thebacteria (called septic infarcts)• Subacute Endocarditis = less destruction of the valve, presence of granulationtissue, and, with time, calcification or fibrosis• Acute Endocarditis = giant holes and abscesses in valves without inflammation‐ Clinicalo Fever = Most consistent sign of Infectious Endocarditis, though may be falsely low insubacute (nonsevere) cases or in the elderlyo Murmurs = occur in 90% of cases but may represent a predisposing condition, not a signo Autoimmune = glomerular nephritis (Ag‐Ab deposition) with hematuria and proteinuriao Duke Criteria• System of labs, clinical, echo, cultures that identify IE• Used to use outdated clinical appearance• Roth Spots = retinal hemorrhage• Osler Nodes = Subcutaneous Nodules in the Digits• Janeway Lesions = Erythmatous Nontender Nodules on Palms/Soles• Petechial Rashes‐ Treatment/Preventiono Find the bug, find what it is vulnerable to, and give that antibiotico Prophylaxis broad spectrum antibiotics or targeted therapy for area of surgery (dental,gut, etc)19 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>Red Bumps all lined up in a row onthe edge of the valve, nopenetration into myocardium orchordaeNoninfectious Endocarditis‐ Nonbacterial Thrombotic Endocarditis (NBTE)o Causes• Hypercoagulable State• Frequently occurs with venous thrombosis or pulmonary embolismindicative of hypercoagulabilityo• Causes by underlying condition (Cancer, Sepsis, Burns, elevate estrogen)• Endocardial trauma, such as with a Swan‐Ganz Pulmonary CatheterMorphology• Characterized by small deposits of fibrin, platelets and blood components onthe leaflets of the valves which are sterile and contain no organisms• Nondestructive lesions occurring in bands or single, which are small• Histologically thy are bland thrombi without an immune reactionNormal valve with a fibrinous thrombus(no immune reaction)On BottomDifficult to see the yellowlesions on both sides ofvalve‐ Libman Sacks Endocarditiso Cause• Antiphospholipid Syndrome associated with LupusOn Top• Thrombotic, Hypercoagulable lesions associated with venous and arterialthrombosisoMorphology• Single or multiple granular, pink, small lesions on either or both side of thevalve• Histology reveals NBTE with hematoxilin bodies (review Inflammation)• Fibrinoid Necrosis of the valve material occurs contiguous with the lesion• Repeated damage and fibrosis may require surgeryRHD is marked by a row of small, warty vegetations along the lines of closure of the valve leaflets.IE is characterized by large, irregular masses on the valve cusps that can extend onto the chordaeNBTE exhibits one or more small, bland vegetations, usually attached at the line of closure.LSE has small or medium‐sized vegetations on either or both sides of the valve leaflets.20 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>PERICARDIAL DISEASESPericardial Effusion‐ Normal pericardial fluid = 30‐50mL of straw‐colored, thin, serous fluid‐ Extra fluid can accumulate of variable compositiono Pericardial Effusion = Variable, usually serouso Blood = hemopericardium from traumao Pus = purulent Pericarditis‐ Response is dependent on quantity and rate of pericardial fillingo Depends on how much the heart can stretcho Rapid filling, even with low fluid levels (200‐300mL) = cardiac tamponadeo Slow filling can accommodate more fluid (up to 500mL) and still be okPERICARDITISThis is an inflammation of the pericardium. It is often caused secondary to something else (metastasis,surgery, thoracic/systemic disease, or infectious agents). Most causes result in an acute pericarditis withan acute inflammation reaction. Some cause chronic Pericarditis.Acute Pericarditis‐ Serous Pericarditiso Serous inflammatory exudate that is produced by noninfectious inflammation (RF, SLE,scleroderma) or an infection near the serosal layer (pleuritis)o The increased vascular permeability of inflammation results in an exudative fluid thatnormal has scant inflammatory cells in a fluid that accumulates slowly‐ Fibrinous and Serofibrinous Pericarditiso Most Common type of Pericarditiso Composed of a serous fluid mixed with fibrinous exudateo Causes include MI, post infarction syndrome (Dressler’s Autoimmune), RF, SLE, traumao Development of a loud pericardial friction rub is seen often with pain and systemicfebrile reactions.o The fluid is either dry (fibrinous) or there can be thick yellow fluid owing to erythrocytesand inflammatory cells‐ Purulent or Supparative Pericarditiso Caused by the invasion of foreign organisms.• Direct extension of neighboring inflammation (pleuritis, infectious endocarditis)• Seeding from the blood or lymphatic extension• Direct introduction during cardiotomyo Clinical findings = those of fibrinous Pericarditis with increased systemic reactions (fever,chills, etc)o There is a large amount of fluid (500mL) with a variable consistency dependent on theconcentration of organisms and strength of the immune response)21 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>oooHistologically you see an acute inflammatory reactionThis can spread to involve the mediastinum = mediastinopericarditisOrganization is the usual outcome, resulting in a constrictive pericarditis, resolution israre‐ Hemorrhagico Fibrinous + Blood in the pericardium caused by metastasis, infection or traumao Basically the same as everything above, just with a lot of blood‐ Caseouso Almost certainly caused by TB, though can be fungalo Caused by a direct spread from the tracheobronchial tree, resulting in caseous necrosisChronic or Healed Pericarditis‐ Normalo Most of the pericarditis listed results in organization of fibrino “Organization” usually means 1 of 3 things, all that do not hamper cardiac function• Fibrous plaques (“soldiers plaques”) on the serosal membrane• Thin, delicate adhesions of obscure origin• Adhesive Pericarditis = stringy fibrous connection between layers ofpericardium, essentially obliterating the sac‐ Adhesive Mediastinopericarditiso Follows caseous or supparative pericarditis, sometimes irradiationo The pericardial sac is obliterated, forming adhesions between the external parietal layerand the rest of the mediastinumo With each contraction, the heart must pull against all organs in the mediastinum inorder to squeeze blood, significantly compromising cardiac functiono Increased workload results in hypertrophy and dilation mimicking DCMo Pulsus paradoxus, systolic retraction of rib cage, and other clinical findings‐ Constrictive Pericarditiso If present, was usually a Sequella of supparative pericarditiso The pericardial sac is obliterated, replaced with a fibrous shell which can be calcified ornot.o Limits Diastolic Relaxation and therefore results in compromised cardiac functiono Hypertrophy and Dilation cannot occur, because the heart has no room in which toexpand intoo Surgery to remove the shell is the only therapy available.22 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>Enlarged Atria, andBulging VentriclesCARDIOMYOPATHYMuscular Hypertrophy withinterstitial fibrosis (stained blue)Dilated atrium, stiff nonfilling,hypertrophic ventricleDilated <strong>Cardio</strong>myopathy‐ Definitiono Progressive Cardiac Dilation and Contractile (systolic) dysfunction without hypertrophyo 25‐30% genetic, 10% EtOH, low % Myocarditis, low% pregnancy, the rest is idiopathic• First Aid, Kaplan, and Goljan say “alcohol is the most common cause”‐ Morphologyo Large, Heavy, Flabby Heart with dilation of all 4 chamberso With dilation comes stretching of the myocardium so there is no visible thickening of theventricular walls = “no hypertrophy”o With dilation comes stretching of the myocardium and with it the valves, so there maybe a functional regurgitation of valves‐ Causeso Myocarditis (see later)o Alcohol = caused by aldehydes or direct toxicity, is indistinguishable from other kindso Pregnancy = poorly understood. There is probably a multi‐factorial combination of HTN,volume expansion, and nutritional deficiency. Called peripartum cardiomyopathyo Genetic = Gene mutation of the cytoskeleton X‐Linked, usually with Dystrophin.ClinicalAges 20‐50 causing slow onset CHF that may precipitously lead to failure (EF
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>Atrium is dilated, LV isnormal, but stiff withfibrosisSomething gets in theway of relaxation.Whether that isFibroelastosis,Eosinophils, or evenAmyloid, the heartcannot relax andtherefore cannot fill.InfiltratesMyocytesGiant CellsRestrictive <strong>Cardio</strong>myopathyMyocarditis‐ Definitiono Primary Decrease in Ventricular Compliance (Systolic Dysfunction)o Associated with restrictive disease = amyloidosis, sarcoidosis, fibrosis‐ Morphologyo Normal sized ventricles, no dilation, but with firm chambers and enlarged atriao Patchy diffuse interstitial fibrosis‐ Other Causeso Endomyocardial Fibrosis• Disease of children/young adults in Africa• Fibrosis begins at Apex and travels to the valves with regular mural thrombi• Unknown EtiologyooLoeffler Endomyocarditis• Endomyocardial fibrosis caused by increased abnormal eosinophils releasingtoxic granules that injures the ventricles. Repair leads to fibrosis.• Removal of fibrotic layer (endomyocardial stripping), surgically, will fix it.Endocardial Fibroelastosis• Infantile/Childhood illness of unknown etiology• Causes fibrosis of mural left ventricular myocardium associated with some otherstenotic valve disease responsible for the increased mortality.‐ Causeo Inflammation is the cause of, NOT a reaction to myocardial insufficiencyo Infection• T. Cruzi = Chagas Disease = 80% of cases have Myocarditis• Trichinosis (helminthes), Lyme disease (B. Burgdorfi), parasite, etco Noninfectious• Hypersensitivity Myocarditis = allergic reaction to drugs, diuretic, anti‐HTN• Autoimmune Inflammation = RF, SLE, Polymyositis or transplant sensitivity‐ Morphologyo Patchy and diffuse inflammation• Interstitial Fibrosis with areas of necrosis adjacent to inflammatory cells• While mononuclear lymphocytes are most common, endocardial biopsy mayshow nothing because of the patchy nature of infiltrateso In gross, it can appear normal, hypertrophic, or dilated with patch lesionso Giant Cell Myocarditis has multinucleated giant cells and a poor prognosiso Chagas Disease = trypanosomes inside the myocytes‐ Clinicalo Acute illness can mimic MI (Dyspnea, chest pain, fatigue, fever)o Spectrum = asymptomatic/spontaneous resolution death. Moderate cases progressto look like DCM24 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>ANNUERYSMSSelf Study content from here on outAortic Aneurysm = Abdominal AortaNormal AortaWhoa Bulge!‐ Definitiono Out pouching of the aorta, most commonly in abdominal aorta, followingatherosclerotic destruction of the aortic media, leading to vessel wall weakness‐ Morphologyo Big ass bulge out the side of the abdominal aorta of varying width and lengtho Often contains atheromatous ulcers with thrombi (source of atherothrombotic origin)o May be so large that it compresses nearby vessels or the thrombus causes occlusionsyndromeso Special Variants• Inflammatory AAA = Macrophages, Giant Cells, Lymphocytes, Plasma cells, AAA• Mycotic AAA = Supuritic lesions with organisms hiding inside (salmonella)‐ <strong>Path</strong>ogenesiso Atherosclerosis is number 1 causeo Cystic Medial Degeneration = Collagen. Aneurysms come from abnormal collagen(Marfan’s) or an abnormality of collagen remodeling (increased degradation decreasedsynthesis caused by an immune reaction) resulting in an inherently weakened aortic wall‐ Clinical Courseo Rupture is often fatal. Hemorrhage occurs into the peritoneum. ↑size = ↑risko Obstruction of a vessel (mesenteric, renal, vertebral) leading to ischemic injuryo Direct Compression of the ureter or of the vertebrae (casing vertebral erosion)o Embolism from the thrombus that’s sitting insideo Tumor = AAA is a palpable mass that may be mistaken as a tumorTertiarty Syphilis,Ascending Aorta, Deathfrom Rupture, AorticRegurgiation, Tree‐Barking WallSyphilitic (Leutic) Aneurysms = Ascending Aorta‐ Causeo Syphilis (stage 3) has a vascular predilection for small vessels, especially of the aortao Infection with subsequent Inflammation of the vasa vasorum leads to obstruction,inducing ischemia and obliterative endarteritis of the aorta, causing death of muscle andelastic tissue, called syphilitic aortitis‐ Morphologyo Starts in the adventitia with vessels with inflammation reactions in adventitia (above)o Muscle that dies is replaced with fibrous scar tissue in the media, contraction of whichcauses the “tree‐barking” appearanceo Effects thoracic aorta with possible dilation of aortic valve leading to insufficiency‐ Presentationo All causes by the encroachment on mediastinal tissueso Crush the lungs = Dyspnea Crush the esophagus = DysphagiaPain from rib and vertebral erosions Cardiac Disease from valve involvementDeath from ruptureAortic Regurgitation25 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>Medial degeneration of elastictissue (top) versus normal (bottom)Lumen IntimaDissecting Hematoma = Thoracic Aorta (Ascending common, Descending less common)Media‐ Definitiono Catastrophic illness characterized by dissection of blood between and along thelaminar planes of the media with formation of a blood‐filled channel within the aorticwall which can rupture outward‐ Morphologyo A single intimal tear cuts into but not through the media of the ascending aortacreating a blood filled pocket within the aorta, between layerso Dissection can continue in both direction (towards the heart and towards the femoral)o Usually rupture outwards, but can rupture back inwards• Outward = hemorrhage = fatal• Inward = second intimal tear back into the normal lumen, forming a newvascular channel (“double‐barrel Aorta”) which can, over time, endothelize andbecome a permanent vesselo No distinguishing histology except for warning signs = elastic tissue fragmentation andmedial degeneration‐ <strong>Path</strong>ogenesiso HTN is primary causative agent, if you see HTN pick Dissecting Hematomao Medial weakening is not required for dissection, but cystic medial necrosis fromMarfan’s or Ehler’s Danlos (weak elastic layer) predisposes dissection• If you have a dissection, pick HTN. If HTN isn’t there, pick Marfanso Once dissection has happened, arterial blood pressure favors hematomaClinical Courseo If the dissection is Proximal subclavian/carotid (type A = bad), if distal (type B = better)o Pain in the chest radiating to the back is a tell tale signo Death usually results from ruptureo If dissection involves aortic root, you can get valve problems (regurgitation, murmur)Adventitia Media BloodVASCULITIDESThis is more a rapid rundown of critical buzzwords, presentations, and treatments associated with thevarious diseases. We did not get a lecture on this content and should be part of your “tutorial.” BabyRobbins is sufficient for this section, and this is an outline of the content in that book. We begin witharterial vasculitidies.Multinucleated giant cells ingranulomas in the internalelastic lamina, narrowingthe lumenGiant Cell Arteritis (Temporal Arteritis) = Board Favorite‐ ‐ Effects medium and small sized arteries‐ ‐ Most common form of Vasculitis, especially in Elderly Women‐ ‐ Characterized by giant cell granulomatous inflammation‐ ‐ Head pain, vision disturbances (can lead to blindness), arthralgias‐ ‐ Responds well to steroids26 | O wl Club Review SheetsClassic presentation is an elderly femalewith unilateral temporal pain with firmnodules on palpation. She may or may notcomplain of blindness. When you take abiopsy you will see a giant cell granuloma.Don’t be surprised if her joints her too;don’t be fooled into an arthritis!
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>Fibrinoid Necrosis (pink)with a severely stenosedlumen. Look at all theinflammatory cells in thewall of the artery.Takayasu Arteritis‐ Effects Japanese women more than anyone else‐ Effects medium + large sized arteries = the carotid and subclavian as they branch from aorta‐ Granulomatous inflammation limits blood flow to the upper extremities‐ Called pulseless disease since pulses are weak or absent in upper extremity periphery‐ The vignette may sound like Giant Cell Arteritis, but these will be young asian womenPolyarteritis Nodosum (PAN)‐ Effects medium and small sized arteries, disseminated randomly through periphery‐ Causes a necrotizing Vasculitis which is diffuse and difficult to pinpoint‐ Symptoms reflect organ supplied by necrotized artery, but the general fatigue, fever, andweight loss is generally always present.‐ Critical Associations are with Hep B Seropositivity and with p‐ANCA (pANca for PAN)‐ Morphology dependent on stage, multiple stages present at one timeo Acute = sharply inscribed fibrinoid necrosiso Healing = fibrinoid necrosis + fibroblastso Healed = fibrous lesion into lumen with destruction of elastic lamina, possible aneurysm‐ Responds well to steroidsKawasaki’s Disease‐ Effects medium and small sized arteries effects the Coronary Arteries‐ Manifests as fever, lymphadenopathy, with oral or conjunctival erythema, and amaculopapular rash on the skin‐ Usually self‐limiting but involvement of carotid can lead to fatal aneurysm or thrombosiso Aneurysm leads to tamponade, Thrombosis leads to infarctionWegner’s Granulomatosis‐ Effects small but can effect medium sized arteries with a necrotizing granulomatousinflammation which can lead to Rapidly Progressive Cresentic Glomerulonephritis (Renal)‐ Effects middle‐aged women (40‐50)‐ Targets focal lesions of the lungs, kidneys, and upper respiratory system (Nose, Sinus)‐ No causative agent or pathology known, responds well to treatment with immunosuppresion(cyclophosphamide) works well. Do well with treatment, poorly without‐ C‐ANCA is usually elevated (90%), p‐ANCA is PAN, c‐ANCA is the “other one”Buerger’s Syndrome (Thromboangiitis Obliterans)STOP SMOKING!It’s the onlytreatment‐ Effects medium and small sized arteries of the extremities in young (
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>VEINS AND LYMPHATICSVaricose Veins‐ Superficial veins (usually of the legs) become distended, more cosmetic than anything else‐ Obesity, jobs with legs dependent (barber, surgeon), and pregnancy are disposing factors‐ Stasis of blood, rupture of valves, or thinning of walls allows distention‐ May cause ulceration, but are generally asymptomatic (do not cause emboli)‐ Can also be in the esophagus (esopheal varices) and in the anus (hemorrhoids).Thrombophlebitis and Phlebothrombosis (aka Deep Vein Thrombosis, DVT)‐ The distinction between thrombosis of the vein (phlebothrombosis) and inflammation of thevein with thrombosis (thrombophlebitis) is not relevant, they are all DVTs‐ Presents with pain in the calf with red, tender lesions, with a positive Homan’s Sign(dorsiflexion induces pain)‐ Risk increases with Estrogen, Birth Control, Smoking, Age, Hypercoagulability‐ Can result in pulmonary embolism or edemaSuperior and Inferior Vena Cava Syndromes‐ Something blocks these large veins (invasive neoplasm, mural thrombosis) that causes a backup distally, without a failure of the heart‐ Massive edema inferiorly for IVC (ankle, ascites, pelvis) or superiorly for SVC (face, neck,arms)Lymphangitis and Lymphedema‐ Infection gets into the lymph nodes‐ Red streaks from site of penetration, follows along lymph tract, finished at lymph node‐ Lymphadenopathy is present with PMNs and Lymphocytes infiltrating site of infection‐ Caused by Cancer or Virulent Bacteria (Staph)THE REST OF THE CONTENT OF THIS CHAPTER, “CANCERS”, WAS COVERED IN NEOPLASIA. Know thatkids get rhadomyosarcomas and adults get atrial myxomas. That was Kaplan’s entire review of thatmaterial.28 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>DiseaseAtherosclerosisMonckenberg’sArteriosclerosisEssentialHypertensionMalignantHypertensionStable AnginaUnstable AnginaPrinzmental AnginaMyocardial InfarctionRight Sided FailureLeft Sided FailureISCHEMIC HEART DISEASENotesDevelopment of atheromatous plaques from fibrous streaksFormed of lipid‐laden macrophages surrounded by a fibrous capAtheromas may rupture leading to bleed, thrombus or embolusAccelerated in Diabetes, causes Abdominal Aortic AneurysmAlso termed Medial Calcific Arteriosclerosis; Benign condition of aging,Vessels become more rigid and the pulse pressure widensInduced by atheromatous plaques and aging, i.e. the normal process of agingHypertension induces hyaline formation of the vasculatureIncreases risk of myocardial infarction, kidney failure, stroke, and Dissecting Aneurysm/HematomaHyperplastic Arteriosclerosis = are the typical onion skinning vasculature and flea‐bitten kidneysLook for a BP of >200/>120 in the vignette, pick hyperplastic or malignant HTNChest pain induced by stress or exercise that subsides with rest or nitratesProduces no myocardial damage, beginning stages of heart disease, ST Segment DepressionAtherosclerosis causes 75% occlusionChest pain induced by stress or exercise that does not subside with rest or nitrates = 90% occlusionNo permanent damage, but serious intervention is required (Stent, CABG)Seen as ST Segment Depression with chest pain, mimicking Subendocardial InfarctChest pain that has nothing to do with stress or exercise (vasospasm induced)Chest Pain radiating to the jaw/arm with sweating and hypotensionIndicated by ST Segment Depression (for Subendocardial infarct, usually hypotension) andST Segment Elevation (for Transmural Infarct, usually thrombus)Death in the first few hours occurs from arrhythmia, death in a few days HempericardiumYou must know what it looks like in gross and histo, and what are complications (see last page)Risk factors include Hypertension, Diabetes, Increased Age, ↑TG, ↑Chol; Estrogen is PROTECTIVEElevations in Troponin I (best choice), CK‐MB (sort of specific), LDH (not specific)Back up of blood before the lungs.Causes cardiac cirrhosis, pitting edema of lower extremities, and ↑JVPIs generally the result of Left Failure, or may be Cor Pulmonale from COPDBack up of blood after the lungsCauses pulmonary edema, paroxysmal nocturnal dyspnea (sleep with pillows)Is generally the result of systemic hypertension or myocardial infarctionCalled “Congestive Heart Failure” even though it does not require congestion to be failureDiseaseSyphilitic AneurysmDissecting AneurysmAbdominal AorticAneurysmAORTIC ANEURYSMSNotesCaused by Tertiary Syphilis Infection, causes obliterative endarteritis (death of vaso vasorum)Characterized as a tree‐bark or tissue paper wrinkling of the aorta on grossMay involve aortic root, producing aortic regurgitation, affecting the ascending aortaRare because all antibiotics treat syphilis; look for a homeless sexually active male in vignetteCaused by Hypertension (first choice), or Cystic Medial Necrosis from Marfan’s (2 nd choice)Presents as a tearing pain radiating to the back, affecting the descending aortaDeath results from rupture, look for double‐lumen or mediastinal widening on X‐ray or CTCaused by atherosclerosis generally occurring below the renal arteryPresents with intense flank pain, palpable abdominal mass, abdominal bruitCan be fixed with a large stent but rupture = death29 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>DiseaseInfectiousEndocarditis(IV Drug Abuser)NoninfectiousEndocarditis(Old Man or Woman)Libmann‐SacksEndocarditis(Young Woman 20‐40)Rhuematic HeartDisease(Kids Post‐Strep)Aortic StenosisMitral StenosisMitral Prolapse akaInsufficiencyVALVULAR DISEASESNotesAcute = Staph Aureus, 50% fatal even WITH treatment; Subacute = Strep Viridans/ Rheumatic heartFriable vegetations on the atrial side of the valve, can embolize and cause septic infarctMay effect the right side (Intravenous Drug Abuser), Mitral most common, can effect Aortic ValveProduces Splinter Hemorrhages on the fingernails, Osler Nodes which are Painful, JanewayLesions which are painless, and Roth Spots on the eyes (red with white in the center).Marantic Endocarditis occurs in the elderly and is usually associated with metastasis/cancerIt is NOT a metasisis, but Marantic Endocarditis occurs only in old dying, very sick patientsMay break off and cause sterile emboliAssociated with Lupus (usually a women with positive ANA, positive dsDNA‐Ab); SLE LSESterile Vegetations on both sides of the valve, which may embolize causing sterile emboliUsually a picture of a valve with vegetations on both sides, putting it in words is too easyFollows a Streptococcal Infection of pharynx, develops an increased ASO Titer (Anti‐M protein)There is a cross‐reactivity to the mitral valve, causing Aschoff bodies with Anitschkow CellsIs not an infection but it predisposes the mitral valve to infection (Viridans Prophylaxis at dentist)Jones criteria: chorea, arthralgia, subcutaneous nodules, fever, and others (10+ criteria)Caused by aging (benign calcification) or by rheumatic fever (fish‐mouth fusion of leaflets)Characterized by a crescendo‐decrescendo systolic murmur located at the 2 nd intercostal spaceCauses left ventricle hypertrophy (from ↑afterload), heard at the Right sterna BorderMost common valve affected by Rhuematic Fever, heard at the apex, 5 th intercostal spaceCauses a diastolic murmur as blood fills the ventricles through a stenosed valveHolosystolic Harsh Murmur occurring at S2, ending at S1Causes a “backward failure” with blood rushing back into the atria, a result of Papillary MuscleRupture (Ballooning), myocardial infarction, or Myxomatous degeneration (Dermatan Sulfate)DiseaseDilated<strong>Cardio</strong>myopathyHypertrophic<strong>Cardio</strong>myopathyRestrictive<strong>Cardio</strong>myopathyMyocarditisCARDIOMYOPATHIESNotesMost commonly caused by Alcohol, but can also be Chagas, Doxorubicin, or Coxsackie VirusAll four chambers are dilated and there is a left and right heart failure (systolic dysfunction)Autosomal Dominant mutation of the β‐MHC gene resulting in a fatty heart, Myocyte disarrayFirst presentation is usually an athlete who drops dead on the court (no warning signs)Shows a banana‐lumen producing obstruction to outflow; septum is hypertrophied > free wallIron overload from hemochromotosis (GI block), Amyloid, or Fibro‐Elastosis are causesThere is a diastolic dysfunction as the muscle cannot relaxChronic or Acute Inflammation WITHIN the heart muscleMost commonly caused by Chagas DiseaseDiseaseRhabdomyosarcomaAtrial MyxomaCARDIAC TUMORSNotesYou find them in kids (if child in vignette and has a heart cancer, pick Rhabdo)Associated with autosomal dominant Tuberus Sclerosis (not mentioned in this block)Contains a “muscle background;” i.e. the tumor is of the muscleYou find them in adults (if adult in vignette and has a heart cancer, pick Atrial Myxoma)Has a Myxomatous background within the Left AtriumCan cause sudden cardiac death from ball‐valve dropping into the mitral valve = 0 Cardiac Output30 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>DiseaseFibrinousSerousPurulentHemorrhagicAdhesiveConstrictivePericardialEffusionsPERICARDITISNotesOccurs two weeks after MI looking like “bread‐and‐butter,” called Dressler’s SyndromeRepresents an exudate on the pericardial surfaceCaused by Lupus or other autoimmune disorderCaused by infection, it is, obviously, purulent. Commonly a thick white or yellow fluidInflammation and blood enters the pericardium, but is NOT from a ventricular rupture (hemopericardium)Associated with post‐surgrical conditionsSequellae of infectious pericarditis where the pericardium is obliterated and the muscle adheres to all tissuesHeart must contract against lungs and diaphragm (which is not easy) resulting in hypertrophySquella of infectious pericarditis where the pericardium gets stiff, resulting in failure‐to‐relax (diastolic)Beck’s Triad = Kussumal Sign, Pulsus Paradoxus, Neck Vein DistentionLook for muffled heart sounds, from fluid around the heart, preventing diastolic relaxationDiseaseGiant CellArteritisKawasaki’sTakayasuWegner’sGranulomatosisPolyarteritisNodosa (PAN)Henoch‐SchloneinPurpuraBuerger’sSyndromeVaricose VeinsVeinsDVTsVeinsSuperior VenaCava SyndromeVeinsDISEASES OF THE BLOOD VESSELSNotesGranulomatous inflammation effecting the temporal artery of the elderlyPresents with head pain (especially with palpation) and maybe blurry visionMay lead to blindness. Do a ESR (↑in disease) to differentiate from strokeNecrotizing Granulomatous inflammation in a baby (in this block, baby will do it)Look for mucocutaneous involvement, lymphadenopathy, or a desquaminating rash in a kid in the stemMay involve the coronary artery leading to a fatal aneurysm (tamponade) or thrombosis (infarction)Pulseless Disease effecting middle aged Japanese womenLook for absent pulses in the upper torso, caused by inflammation of aorta or carotid as it branchesMay produce neurologic or visual symptoms that may lead you to think its Giant CellNecrotizing Granulomatous inflammation of the lungs, kidney, and nose/sinus (all 3 = pathognomonic)Associated with C‐ANCA and treated with Cyclophosphamide and CorticosteroidsSymptoms that affect multiple organs but do not fit together causing a Fibrinoid Necrosis in each oneAssociated with P‐ANCA (P‐ANCA for PAN). Treat with steroids or cyclophosphamide (90% remission)Strong association with Hepatitis B infection (far more sensitive than p‐ANCA)Common childhood systemic Vasculitis characterized by palpable Purpura on the legs and buttocksCommonly follows an Upper Respiratory infection, it is an IgA Immune DiseaseLook for other IgA diseases such as Pernicious Anemia or Dermatitis HerpatiformisDisease of young males who chain smoke and are usually middle easternCauses Raynaud’s Phenomenon in the distal extremities which may lead to amputationSmoking Cessation is the only treatmentBenign lesions that may thrombose but cannot embolizePresent problems of cosmetics though they may ulcerate and can be painful if neglectedDeep Vein Thrombosis develops in the popliteal and femoral veins = swollen, tender, red calvesMay embolize causing a pulmonary embolism. Look for postsurgical or post flight dyspnea↑Risk with Oral Contraceptives, Smoking, Factor V Leiden, and Stasis (immobility)Pulmonary tumor compresses the superior vena cava, causing a backup above itMay produce blurry vision or may induce sufficient stasis for cerebral infarctionLook for vein engorgement superior to the neck, especially if the engorgement is unilateral face31 | O wl Club Review Sheets
<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>CONGENITAL DEFECTSDisease Type Cause/Character SymptomsAtrial SeptalDefectL RShuntVentralSeptal DefectPatentDuctusArteriosisTetralogy ofFallotTranspositionGreatArteriesTruncusArteriosisTricuspidAtresiaCoarctationof AortaL RShuntL RShuntRLShuntRLShuntRLShuntRLShuntObstructHole between the atria allowing oxygenated blood into rightventricle. Most common defect to occur alone, not the mostcommon in general. More commonly occurs in the SeptumSecundum (90%) and sometimes in Septum Primum (10%)Hole between the ventricles allowing oxygenated blood intoright ventricle. Most common defect in the heart. Associatedwith Down’s Syndrome. Presents with a systolic murmurHole between the aorta and pulmonary artery allowing ↑O 2blood into lungs. Kept open with prostaglandin, closed withindomethacin. Causes a continuous machine‐like murmurRVH, Subpulmonary Stenosis, VSD, Aorta on top of VSD.Caused by an anterosuperior movement of infundibulum.Must be surgically corrected. Look for “boot‐shaped heart” inthe vignette, or cyanosis relieved by squatting (↑TPR)Swapping of aorta to RV and pulmonary artery to LV, requiringcommunication (PDA) for life. Requires surgical correction. Ifno surgery, is fatal in 1 st month of life. Occurs in diabeticmothers (but NOT in diabetes of pregnancy)Pulmonary artery and aorta do not separate, so are one bigoutflow vessel allowing mixing of blood in both directions.RA and RV do not communicate, requires ASD and VSD for life.The tricuspid valve never forms a holeInfantile = Coarctation proximal major branches (fatal)Adult = Coarctation distal major branches (found as a kid)Occurs in Turner Syndrome. Look for rib notching.Aortic Atresia Obstruct Stenosis or Atresia from something being in the way of leftventricular outflowPulmonary Obstruct Stenosis or Atresia from something being in the way of rightAtresiaventricular outflowPulmonary hypertension,Pulmonary Vasculitis, Latestage reversal of shunt =cyanosis and fatality, calledEisenminger’s Syndrome. TheRV will hypertrophy and/orpulmonary artery will stenose,reversing the flow to RLBaby is initially pinkBlue baby syndrome, occursearly in life, deoxygenatedblood gets into systemicvasculature causing cyanosis.High mortality rate, requiringsurgical intervention. Right toleft shunts will not reverse.Baby is initially blueVariable on PDA and extent ofcoarctation, usually distalcyanosis or weak pulse (feet)Atresia = Hypoplastic LVStenosis = LVHRight ventricular hypertrophyand Pulmonary DilationGROSS CHANGES FOLLOWING MISurvival Time Predominant Finding0‐24 hrs No Change1‐3 Days Yellow Pallor in the center3 Days – 4 weeks Yellow Pallor with surrounding Hyperemia6 Weeks + White/Grey Firm ScarHISTOLOGIC CHANGES FOLLOWING MISurvival Time Predominant Finding1‐4 hrs Wavy Myocytes and contraction bands4‐24hrsCoagulative Necrosis with few Neutrophils, No Myocyte Nuclei, All Pink1‐3 Days Coagulative Necrosis with many Neutrophils increasing in number3‐7 Days Coagulative Necrosis with Macrophages10+ Days Collagen Deposition, Fibroblasts, Macrophages, Granulation TissueRISK FOLLOWING MISurvival Time Predominant Finding0‐1 hrs Fatal Arrhythmia, usually Ventricular Fibrillation or Ventricular Tachycardia1‐7daysVentricular Rupture (Septal Wall or Ventricular Wall) Hemopericardium Death7+ Days Ventricular Aneurysm (no rupture, just outpouching, leading to mural thrombus)32 | O wl Club Review Sheets
33 | O wl Club Review Sheets<strong>Path</strong> <strong>Cardio</strong> <strong>Outline</strong>













![Research Opportunities for Medical Students 10-13[1] - TMedWeb](https://img.yumpu.com/35158682/1/190x245/research-opportunities-for-medical-students-10-131-tmedweb.jpg?quality=85)