Ethical Theory to Ethical Practice - TMedWeb - Tulane University
Ethical Theory to Ethical Practice - TMedWeb - Tulane University
Ethical Theory to Ethical Practice - TMedWeb - Tulane University
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
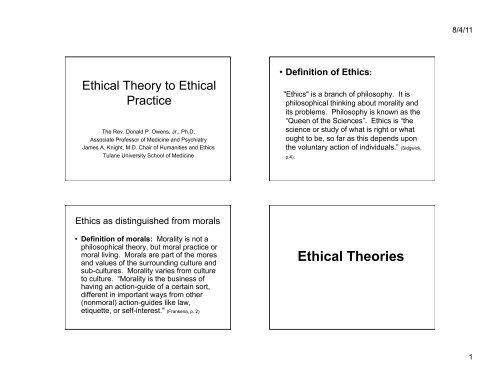
8/4/11<strong>Ethical</strong> <strong>Theory</strong> <strong>to</strong> <strong>Ethical</strong><strong>Practice</strong>The Rev. Donald P. Owens, Jr., Ph.D.Associate Professor of Medicine and PsychiatryJames A. Knight, M.D. Chair of Humanities and Ethics<strong>Tulane</strong> <strong>University</strong> School of Medicine• Definition of Ethics:"Ethics" is a branch of philosophy. It isphilosophical thinking about morality andits problems. Philosophy is known as the“Queen of the Sciences”. Ethics is “thescience or study of what is right or wha<strong>to</strong>ught <strong>to</strong> be, so far as this depends uponthe voluntary action of individuals.” (Sidgwick,p.4).Ethics as distinguished from morals• Definition of morals: Morality is not aphilosophical theory, but moral practice ormoral living. Morals are part of the moresand values of the surrounding culture andsub-cultures. Morality varies from culture<strong>to</strong> culture. “Morality is the business ofhaving an action-guide of a certain sort,different in important ways from other(nonmoral) action-guides like law,etiquette, or self-interest." (Frankena, p. 2)<strong>Ethical</strong> Theories1
8/4/11Hedonism: equates happiness with pleasure andpleasure with the good.Non-hedonism: may or may not equate happinesswith pleasure, but never equates the good withpleasureTeleological . theory: We ought <strong>to</strong> do the action oradopt the rule that will produce the greatest possiblebalance of good over evil.Deon<strong>to</strong>logical theory:One decides <strong>to</strong> act in acertain way in a given situation based solely uponduty (Kant), i.e., what the rules say.Utilitarianism: the determination of what is righ<strong>to</strong>r wrong by determining what position will producethe greatest balance between good over evil in theworld as a whole.Theological voluntarism or the divine commandtheory. The operative in this type is that something“is right or wrong if and only if and because it iscommanded or forbidden by God.”• Seldom are ethical decisions made <strong>to</strong>day using only oneethical theory. Theories are combined and inform eachother.This book will changed the way you practice medicine. It is only126 pages long, but few are able <strong>to</strong> make their way through it!2
8/4/11Ethics and Law• What is <strong>Ethical</strong> may not be lawfulEthics and Morals• What is <strong>Ethical</strong> may not be Moral• And What is legal may not be ethical!• What is Moral may not be <strong>Ethical</strong>Medical Ethics• From Paternalism <strong>to</strong> Informed Consent– Until the 1960’s the physician “knew whatwas best for the patient” and the patient was<strong>to</strong>ld only what the physician wished.• The AMA rejects “therapeutic privilege” 2006AMA code of EthicsThe Two Pivotal Oaths in theWest• Oath of Hippocrates:– Hippocrates (460-377 B.C.) is traditionallyregarded as the father of medicine• Prayer and Oath of Moses Maimonides– The great Jewish Physician, Philosopher,Torah Scholar. (1135/38-1204)– Most influential Physician of the Middle Ages3
8/4/11• These two Oaths have shaped thepractice of Western medicine over thecenturies. They remain foundational <strong>to</strong> allother oaths and codes of ethics that are inuse <strong>to</strong>day.Major Concepts inMedical EthicsAu<strong>to</strong>nomyThe right <strong>to</strong> decide; the liberty <strong>to</strong> followone’s will; self-determinationBeginning in the 1970’s thisprinciple came <strong>to</strong> the forefront ofmedical ethics as a primaryprinciple in the treatment ofpatients.Dignity is the quality of being worthy orhonorable; being of worth. All humanshave dignity and this ought <strong>to</strong> bemaintained and respected for all people.• Beneficence– One ought <strong>to</strong> prevent evil or harm– One ought <strong>to</strong> remove evil or harm– One ought <strong>to</strong> do or promote good4
8/4/11• Do no harm---nonmaleficence– The principle of nonmaleficence asserts anobligation not <strong>to</strong> inflict harm on others.This principle has been part of the medicalprofession from the earliest times.• Justice: Treatment of others in a fair,appropriate, and equitable manner– Distributive Justice refers <strong>to</strong> all of the rights andresponsibilities in society.• Problems arise in Distributive Justice whenthere is scarcity of products or goods.– Principles of distributive justice» To each person an equal share» According <strong>to</strong> need» According <strong>to</strong> effort» According <strong>to</strong> contribution» According <strong>to</strong> merit» According <strong>to</strong> free-market exchanges– Pro<strong>to</strong>col of Authority• Patient• designee (power of at<strong>to</strong>rney)• guardian or tu<strong>to</strong>r or cura<strong>to</strong>r (appointed by court)• spouse• adult children• parents• siblings• other ascendants or descendants (aunts anduncles, cousins etc)• court– Living Will or Advanced Directives• a legal document that describes the person’swishes as <strong>to</strong> medical treatments not <strong>to</strong> be usedsuch as intubation, artificial nutrition andhydration, CPR, etc.– The patient can rescind the Advance Directive– in writing» verbally• When not followed—is this an interpretation bythe medical personnel?– Is it a deliberate refusal <strong>to</strong> follow a clear directive?• It is a legal issue <strong>to</strong> ignore a validly executedAdvance Directive– The problem is that if the outcome is life then it isdifficult <strong>to</strong> get a court <strong>to</strong> hear the case! The out comewas deemed positive.5
8/4/11– Medical Power of At<strong>to</strong>rney• a legal document giving another person the decisionmaking power on behalf of the person making thedocument when the person is incapacitated and unable <strong>to</strong>make decisions for him/her self. This may be included asa separate part of a general power of at<strong>to</strong>rney, but mostgenerally in our case it is a separate document specificallyfor medical care.– The patient can rescind the Medical Power of At<strong>to</strong>rney» in writing» verbally• Conflict between Person with Power of At<strong>to</strong>rney and theAdvance Directive– The Power of At<strong>to</strong>rney takes precedence over theAdvance Directive» This is because the person with Power of At<strong>to</strong>rney isby definition the individual. Because the individualcan rescind the Advance Directive at anytime, sodoes the Power of At<strong>to</strong>rney take precedence over it.FutilityFutility—agreed upon by a minimum oftwo physicians—removal of treatmentin order not <strong>to</strong> prolong dying.A determination of futile is reached whentreatment does not offer any benefit <strong>to</strong>the patient because it is pointless orfutile. It typically refers <strong>to</strong> a situation inwhich the patient is irreversibly dying,and any further treatment provides nophysiological benefit, is hopeless, andbecomes optional.This spans Neonate through Old Age.» When futility is determined thenwithdrawal of treatment is the ethicalprocedure.» It is important <strong>to</strong> include the patient,surrogate, and physicians in makingdetermination. It is recommendedthat the Hospital Ethics Committee beinvolved in the process, particularly ifthere is not agreement on the issue.» It is scarcity of products, goods,resources of all types.When treatment is determined <strong>to</strong>be futile then any furtherexpenditure of resources otherthan making the patientcomfortable and pain free asmuch as possible is unjust.This determination by themedical staff takes precedenceover the Living Will and Power ofAt<strong>to</strong>rney and the patient.6
8/4/11Profession• A Profession’s primary endeavor is <strong>to</strong>render services and not the sale ofproducts or things.– The three traditional professions are:• Theology• Law• Medicine– There are other professions that have developed, but allrender services not sell products: such as Architecture,Engineering, Education, etc.The Profession Informs us• The Profession of Medicine or Theology ispeculiar in that a member of either ofthese does not have the privilege <strong>to</strong> stepout of the profession at will.• That means that we loose our privacy. This isexhibited in who we date, comments we make,opinions we have, and who we treat. The law insome states also require physicians <strong>to</strong> s<strong>to</strong>p inemergencies.• Example: girl next doorA Profession Governs itself• A profession governs its members– Educational requirements– Through licensing– Conduct reviews– Peer reviews– A Code of Ethics• Professional—Patient Relationships– Veracity: dealing honestly with patients andcolleagues.» Refers <strong>to</strong> comprehensive, accurate, andobjective transmission of information.– Privacy» Informational privacy: personal information» Decisional privacy: personal choices» Physical privacy: personal spaces» Proprietary privacy: property interest– Confidentiality» Pledging not <strong>to</strong> divulge information obtainedfrom another» This has been diluted over time, once absolutenow under certain circumstances requiredreporting.– Fidelity» Acting in good faith, fulfill agreements,maintain relationships, and discharge fiduciaryresponsibilities.7
8/4/11• Remember that we deal with Gray <strong>to</strong>nes inmedical ethics—there will be those whoquestion our decisions regardless.• We make the best decisions possible withthe information we have at hand!8













![Research Opportunities for Medical Students 10-13[1] - TMedWeb](https://img.yumpu.com/35158682/1/190x245/research-opportunities-for-medical-students-10-131-tmedweb.jpg?quality=85)