An Example of Using Present on Admission Data - HCUP
An Example of Using Present on Admission Data - HCUP
An Example of Using Present on Admission Data - HCUP
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<str<strong>on</strong>g>An</str<strong>on</strong>g> <str<strong>on</strong>g>Example</str<strong>on</strong>g> <str<strong>on</strong>g>of</str<strong>on</strong>g> <str<strong>on</strong>g>Using</str<strong>on</strong>g> <str<strong>on</strong>g>Present</str<strong>on</strong>g> <strong>on</strong> Admissi<strong>on</strong> <strong>Data</strong>:CMS-Defined Hospital-Acquired C<strong>on</strong>diti<strong>on</strong>s in All-Payer <strong>Data</strong>Introducti<strong>on</strong>Many statewide data organizati<strong>on</strong>s have begun to collect present <strong>on</strong> admissi<strong>on</strong> (POA) data intheir all-payer hospital discharge data since the data element was added to the nati<strong>on</strong>al hospitalbilling standard (Uniform Bill-04) effective October 2007. This document provides an example<str<strong>on</strong>g>of</str<strong>on</strong>g> how statewide data organizati<strong>on</strong>s might apply their POA data to their all-payer populati<strong>on</strong>.The example uses the Centers for Medicare and Medicaid defined healthcare acquired-c<strong>on</strong>diti<strong>on</strong>s(HACs).In resp<strong>on</strong>se to the Deficit Reducti<strong>on</strong> Act, the Centers for Medicare and Medicaid Services(CMS) requires the POA informati<strong>on</strong> <strong>on</strong> Medicare fee-for-service claims. CMS uses thisinformati<strong>on</strong> to no l<strong>on</strong>ger reimburse hospitals for the additi<strong>on</strong>al cost <str<strong>on</strong>g>of</str<strong>on</strong>g> certain c<strong>on</strong>diti<strong>on</strong>s thatthey have identified as hospital-acquired (HAC). 1 A similar payment policy will also beimplemented in the Medicaid program. 2 CMS included 10 categories <str<strong>on</strong>g>of</str<strong>on</strong>g> c<strong>on</strong>diti<strong>on</strong>s that wereselected for their HAC payment provisi<strong>on</strong>. 3 The 10 categories utilize an ICD-9-CM basedalgorithm that relies <strong>on</strong> inclusi<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> the POA variable (See Appendix A). Although researchershave identified weaknesses in some measures in the CMS HACs 4 , the algorithm provides acurrent illustrative example for the use <str<strong>on</strong>g>of</str<strong>on</strong>g> POA. This document applies the CMS HAC algorithmto statewide discharge all-payer data that c<strong>on</strong>sistently collect the POA data element. Thedocument illustrates a use <str<strong>on</strong>g>of</str<strong>on</strong>g> POA and presents statistics <strong>on</strong> the distributi<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> CMS HACsacross different payers and across adult age groups.MethodThe analysis focuses <strong>on</strong> n<strong>on</strong>-maternity hospital stays for adults (18 years and older. The analysisused data from the <strong>HCUP</strong> 2008 State Inpatient <strong>Data</strong>bases (SID) for 15 states: Arkansas,Ariz<strong>on</strong>a, California, Florida, Hawaii, Kentucky, Massachusetts, Maryland, Maine, Michigan,New Jersey, Nevada, New York, Oreg<strong>on</strong>, and Tennessee. The SID c<strong>on</strong>tains the universe <str<strong>on</strong>g>of</str<strong>on</strong>g> theinpatient discharge abstracts in the states, translated into a uniform format to facilitate multistatecomparis<strong>on</strong>s and analyses. These 15 states were selected because (a) their 2008 SID included thepresent-<strong>on</strong>-admissi<strong>on</strong> (POA) indicator, (b) they had a large percentage <str<strong>on</strong>g>of</str<strong>on</strong>g> hospitals that reportedPOA for each sec<strong>on</strong>dary diagnosis, and (c) they had POA informati<strong>on</strong> reported for at least 55percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the sec<strong>on</strong>dary diagnoses.Within these 15 states, the analysis included community, n<strong>on</strong>-rehabilitati<strong>on</strong> hospitals, excludingthe following: (a) hospitals that had 10 percent or more sec<strong>on</strong>dary diagnoses with missing POAinformati<strong>on</strong>, (b) hospitals that <strong>on</strong>ly reported the POA informati<strong>on</strong> for Medicare patients, and (c)hospitals that reported all sec<strong>on</strong>dary diagnosis POA informati<strong>on</strong> as “Yes” or all as “No.” A total<str<strong>on</strong>g>of</str<strong>on</strong>g> 386 hospitals out <str<strong>on</strong>g>of</str<strong>on</strong>g> 1,725 (22 percent) community, n<strong>on</strong>-rehabilitati<strong>on</strong> hospitals in the 15states were excluded. Thus, the analysis included 1,339 hospitals. These hospitals cared for12,034,280 discharges in 2008, which is 30.2 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the 39.9 milli<strong>on</strong> discharges fromcommunity, n<strong>on</strong>-rehabilitati<strong>on</strong> hospitals in 2008.The <str<strong>on</strong>g>Present</str<strong>on</strong>g>-<strong>on</strong>-Admissi<strong>on</strong> (POA) indicator indicates whether a diagnosis was present at the time<str<strong>on</strong>g>of</str<strong>on</strong>g> admissi<strong>on</strong>. There are five opti<strong>on</strong>s for reporting POA diagnosis: present <strong>on</strong> admissi<strong>on</strong>, not1
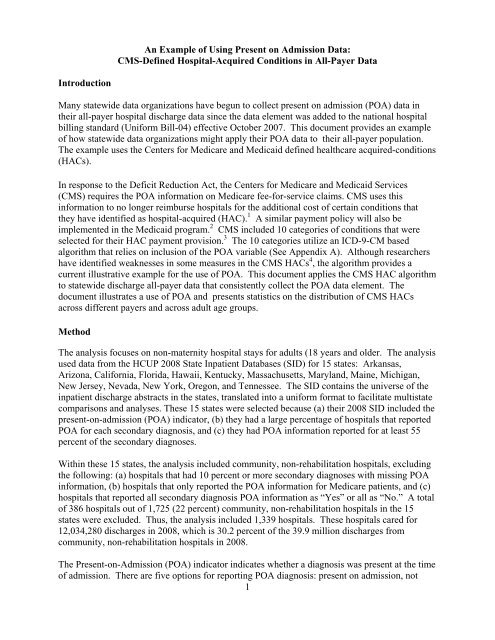
present <strong>on</strong> admissi<strong>on</strong>, insufficient informati<strong>on</strong>, clinically undetermined, and exempt from POAreporting. CMS HACs were identified using the criteria set forth in the Inpatient ProspectivePayment System (IPPS) Fiscal Year 2009 Final Rule by the Centers for Medicare and MedicaidServices. 5 The criteria includes using the POA indicator to determine whether the CMS HACwas not present <strong>on</strong> admissi<strong>on</strong> (i.e., acquired or detected during the hospital stay). For thisanalysis, if a discharge record c<strong>on</strong>tained <strong>on</strong>e or diagnosis codes for a specific CMS HACcategory, the specific CMS HAC was c<strong>on</strong>sidered not present <strong>on</strong> admissi<strong>on</strong> (hospital acquired) ifany <str<strong>on</strong>g>of</str<strong>on</strong>g> the POA indicators associated with these diagnoses were coded as not present <strong>on</strong>admissi<strong>on</strong>.The CMS HAC rate was calculated by dividing the number <str<strong>on</strong>g>of</str<strong>on</strong>g> hospitals stays with the CMSHAC by the populati<strong>on</strong> at risk <str<strong>on</strong>g>of</str<strong>on</strong>g> the CMS HAC and multiplied by 100,000. The relative ratesare calculated by dividing the CMS HAC rate for the group <str<strong>on</strong>g>of</str<strong>on</strong>g> interest (Medicaid, private pay orolder age group) by the reference group rate (Medicare or 18-44 years old age group rate). Whenthe groups <str<strong>on</strong>g>of</str<strong>on</strong>g> interest have higher CMS HAC rates compared to the reference group they have avalue greater than 1.0, while those with lower rates than the reference group have a value lessthan 1.0. A value equal to 1.0 describes similar rates for the group <str<strong>on</strong>g>of</str<strong>on</strong>g> interest and the referencegroup.Payer is the expected payer for the hospital stay. To make coding uniform across all <strong>HCUP</strong> datasources, payer combines detailed categories into more general groups:– Medicare includes fee-for-service and managed care Medicare patients.– Medicaid includes fee-for-service and managed care Medicaid patients. Patients covered by theState Children's Health Insurance Program (SCHIP) may be included here. Because most statedata do not identify SCHIP patients specifically, it is not possible to present this informati<strong>on</strong>separately.– Private insurance includes Blue Cross, commercial carriers, and private HMOs and PPOs.Up to two payers can be coded for a hospital stay in <strong>HCUP</strong> data. For the purpose <str<strong>on</strong>g>of</str<strong>on</strong>g> thisanalysis, when more than <strong>on</strong>e payer is listed for a hospital discharge, the following hierarchy isused:• If either payer is listed as Medicare, the payer is "Medicare."• For n<strong>on</strong>-Medicare stays, if either payer is listed as Medicaid, the payer is "Medicaid."• For stays that are neither Medicare nor Medicaid, if either payer is listed as privateinsurance, the payer is "private insurance."ResultsOverall, the CMS HAC <str<strong>on</strong>g>of</str<strong>on</strong>g> vascular catheter-associated infecti<strong>on</strong>s (blood stream infecti<strong>on</strong>srelated to a catheter in a large, central vein) were the most comm<strong>on</strong> am<strong>on</strong>g the ten reported CMSHACs in 2008 (table 1). The CMS-defined vascular catheter-associated infecti<strong>on</strong>s comprised 49percent <str<strong>on</strong>g>of</str<strong>on</strong>g> stays involving the ten CMS-defined HACs for a rate <str<strong>on</strong>g>of</str<strong>on</strong>g> 128 per 100,000 medicalsurgicalstays. The sec<strong>on</strong>d most comm<strong>on</strong> CMS HAC examined was falls or trauma, whichaccounted for another 20 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> stays involving CMS HACs—a rate <str<strong>on</strong>g>of</str<strong>on</strong>g> 52 per 100,000medical-surgical stays. Although deep vein thrombosis (DVT)/pulm<strong>on</strong>ary embolism (PE)following total knee or hip replacement comprised <strong>on</strong>ly 8 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the ten CMS HACsexamined, it occurred at a rate <str<strong>on</strong>g>of</str<strong>on</strong>g> 649 per 100,000 total knee or hip replacement surgical stays.2
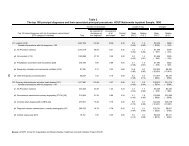
Table 1. Adult discharges with a reported CMS hospital-acquired c<strong>on</strong>diti<strong>on</strong> (HAC) in selectedcommunity hospitals in 15 states, 2008Discharges with reported HACPercent Rate per(%) <str<strong>on</strong>g>of</str<strong>on</strong>g> 100,000Hospital-acquired c<strong>on</strong>diti<strong>on</strong>s defined by Centersfor Medicare and Medicaid ServicesDischargesat risk a NumberallHACsdischargesat riskAll HACs -- 23,219 100.0 --Medical-surgical patients (n<strong>on</strong>-maternal)Vascular catheter-associated infecti<strong>on</strong> 8,959,419 11,435 48.7 127.6Falls and trauma 8,959,419 4,676 19.9 52.2Catheter-associated urinary tract infecti<strong>on</strong> (UTI) 8,959,419 3,128 13.3 34.9Manifestati<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> poor glycemic c<strong>on</strong>trol 8,959,419 673 2.9 7.5Stage III and IV pressure ulcers 8,959,419 615 2.6 6.9Air embolism 8,959,419 45 0.2 0.5Blood incompatibility 8,959,419 36 0.2 0.4Selected surgical patients (n<strong>on</strong>-maternal)Deep vein thrombosis (DVT)/pulm<strong>on</strong>aryembolism (PE) b 274,207 1,780 7.6 649.1Surgical site infecti<strong>on</strong>s (selected surgeries) c 240,701 656 2.8 272.5Foreign object retained after surgery 3,041,774 442 1.9 14.5Source: AHRQ, Center for Delivery, Organizati<strong>on</strong>, and Markets, Healthcare Cost and Utilizati<strong>on</strong> Project, StateInpatient <strong>Data</strong>bases, 2008 from the following states with POA data: AR, AZ, CA, FL, HI, KY, MA, MD, ME, MI, NJ,NV, NY, OR, and TN.aPopulati<strong>on</strong> at risk are selected n<strong>on</strong>-maternal adult discharges: medical-surgical stays (8,959,419); surgical stays(3,041,774); surgical stays with knee and hip replacement procedures (274,207); and surgical stays with CABG;spine, neck, shoulder, or elbow orthopedic procedures; and laparoscopic gastric bypass, gastroenterostomy, orlaparascopic gastric restrictive surgery (240,701).b Deep vein thrombosis (DVT)/pulm<strong>on</strong>ary embolism (PE) following total knee replacement or hip replacement.cIncludes CABG mediastinitis; surgical site infecti<strong>on</strong> following spine, neck, shoulder, or elbow orthopedicprocedures; and surgical site infecti<strong>on</strong> following laparoscopic gastric bypass, gastroenterostomy, or laparoscopicgastric restrictive surgery.CMS Hospital-acquired c<strong>on</strong>diti<strong>on</strong>s by payerAcross all <str<strong>on</strong>g>of</str<strong>on</strong>g> the ten CMS HACs combined, 62 percent occurred in Medicare patients, 12 percentin Medicaid patients, and 21 percent in privately insured patients (data not shown). Table 2highlights a subset <str<strong>on</strong>g>of</str<strong>on</strong>g> the CMS-defined HACs—the five most comm<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> the medical-surgicalHACs—and presents the percent distributi<strong>on</strong> and populati<strong>on</strong> at risk by payer for each. Medicaredischarges represented 53 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the populati<strong>on</strong> at risk (n<strong>on</strong>-maternal, medical-surgical stays)in 2008, but a higher share <str<strong>on</strong>g>of</str<strong>on</strong>g> three CMS HACs: falls and trauma (75 percent), catheterassociatedurinary tract infecti<strong>on</strong>s (72 percent), and stage III and IV pressure ulcers (66 percent).Medicaid represented 12 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the populati<strong>on</strong> at risk, but 18 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the stage III and IVpressure ulcer and 18 percent had manifestati<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> poor glycemic c<strong>on</strong>trol CMS HACs. Inc<strong>on</strong>trast, private insurance represented 26 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the populati<strong>on</strong> at risk, but <strong>on</strong>ly 10 percent <str<strong>on</strong>g>of</str<strong>on</strong>g>the stage III and IV pressure ulcer, 13 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> falls and trauma, and 16 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the catheterassociatedurinary tract infecti<strong>on</strong> HACs.3
Table 2. Percentage <str<strong>on</strong>g>of</str<strong>on</strong>g> adult discharges with a selected reported CMS hospital-acquired c<strong>on</strong>diti<strong>on</strong>by payer in selected community hospitals in 15 states, 2008Discharges and populati<strong>on</strong> at risk by CMSdefined hospital-acquired c<strong>on</strong>diti<strong>on</strong>Percent (%) distributi<strong>on</strong> by payerAllpayers Medicare MedicaidPrivateInsurancePopulati<strong>on</strong> at risk a 100.0% 53.2% 11.8% 25.7%CMS defined hospital acquired c<strong>on</strong>diti<strong>on</strong>sVascular catheter-associated infecti<strong>on</strong> 100.0% 54.0% 15.7% 23.6%Falls and trauma 100.0% 74.7% 6.9% 13.4%Catheter-associated urinary tract infecti<strong>on</strong> (UTI) 100.0% 71.7% 8.0% 16.0%Manifestati<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> poor glycemic c<strong>on</strong>trol 100.0% 51.6% 17.5% 23.3%Stage III and IV pressure ulcers 100.0% 65.5% 18.2% 10.2%Source: AHRQ, Center for Delivery, Organizati<strong>on</strong>, and Markets, Healthcare Cost and Utilizati<strong>on</strong> Project,State Inpatient <strong>Data</strong>bases, 2008 in the following states with POA data: AR, AZ, CA, FL, HI, KY, MA, MD,ME, MI, NJ, NV, NY, OR, and TN.aPopulati<strong>on</strong> at risk is n<strong>on</strong>-maternal, adult medical-surgical stays (8,959,419).Table 3 shows the distributi<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> CMS HACs and discharges at risk by payer for DVT/PEfollowing knee or hip replacement and surgical site infecti<strong>on</strong> (selected surgeries) CMS HACs.Medicare represented 62 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the populati<strong>on</strong> at risk, but 69 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the stays with aDVT/PE CMS HAC. Private insurance represented 31 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the populati<strong>on</strong> at risk, but <strong>on</strong>ly24 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the stays with a DVT/PE CMS HAC.Medicaid represented 6 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the populati<strong>on</strong> at risk, but 13 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the Medicaid stayshad a CMS HAC <str<strong>on</strong>g>of</str<strong>on</strong>g> surgical site infecti<strong>on</strong> following selected surgeries. Private insurancerepresented 44 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the populati<strong>on</strong> at risk but <strong>on</strong>ly 32 percent <str<strong>on</strong>g>of</str<strong>on</strong>g> the stays with a CMSHAC <str<strong>on</strong>g>of</str<strong>on</strong>g> surgical site infecti<strong>on</strong> following selected surgeries.4
Table 3. Percentage <str<strong>on</strong>g>of</str<strong>on</strong>g> adult discharges with a selected reported surgery-related CMS hospitalacquiredc<strong>on</strong>diti<strong>on</strong> and populati<strong>on</strong> at risk by payer in selected community hospitals in 15 states,2008Discharges and populati<strong>on</strong> at risk by CMS-definedhospital-acquired c<strong>on</strong>diti<strong>on</strong>Percent (%) distributi<strong>on</strong> by payerAllpayers Medicare MedicaidPrivateInsurancePopulati<strong>on</strong> at risk a 100.0% 62.4% 3.0% 30.9%Deep vein thrombosis (DVT)/pulm<strong>on</strong>aryembolism (PE) a 100.0% 68.8% 3.0% 24.3%Populati<strong>on</strong> at risk b 100.0% 40.4% 5.6% 44.3%Surgical site infecti<strong>on</strong> (selected surgeries) b 100.0% 40.4% 13.1% 32.0%Source: AHRQ, Center for Delivery, Organizati<strong>on</strong>, and Markets, Healthcare Cost and Utilizati<strong>on</strong> Project,Selected State Inpatient <strong>Data</strong>bases, 2008 in the following states with POA data: AR, AZ, CA, FL, HI, KY,MA, MD, ME, MI, NJ, NV, NY, OR, and TN.aSurgical patients with total knee or hip replacement.bSelected surgical patients with CABG, orthopedic procedures <str<strong>on</strong>g>of</str<strong>on</strong>g> the spine, neck, shoulder, or elbow, orbariatric surgery for obesity including laparoscopic gastric bypass, gastroenterostomy, or laparoscopicgastric restrictive surgery.Figure 1 highlights the rate <str<strong>on</strong>g>of</str<strong>on</strong>g> selected CMS-defined HACs for Medicare patients relative topatients insured by private insurance and Medicaid. Medicaid patients had about half the rate <str<strong>on</strong>g>of</str<strong>on</strong>g>CMS HACs for falls and trauma and catheter-associated urinary tract infecti<strong>on</strong>s as compared toMedicare patients. However, Medicaid had <strong>on</strong>e and a half times the rate <str<strong>on</strong>g>of</str<strong>on</strong>g> CMS HACs formanifestati<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> poor glycemic c<strong>on</strong>trol and more than twice the rate <str<strong>on</strong>g>of</str<strong>on</strong>g> CMS HACs for surgicalsite infecti<strong>on</strong> as Medicare. Overall, the privately insured had lower rates <str<strong>on</strong>g>of</str<strong>on</strong>g> most CMS HACscompared to Medicare.5
Figure 1. Rate <str<strong>on</strong>g>of</str<strong>on</strong>g> CMS-defined Hospital-Acquired C<strong>on</strong>diti<strong>on</strong>s for Medicaidand Private Payers Relative to Medicare, in Selected Community Hospitalsin 15 States, 2008 ±Vascular catheter-associated infecti<strong>on</strong>Falls and traumaCatheter-associated urinary tract infecti<strong>on</strong> (UTI)1.0 = Medicare(reference group)Manifestati<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> poor glycemic c<strong>on</strong>trolPrivate InsuranceMedicaidStage III and IV pressure ulcersDeep vein thrombosis (DVT)/pulm<strong>on</strong>aryembolism (PE)‡Surgical site infecti<strong>on</strong> (selected surgeries)§0.00 0.50 1.00 1.50 2.00 2.50± Adults 18 years and older.Payer-specific discharge rate relative to Medicare‡ Deep vein thrombosis (DVT)/pulm<strong>on</strong>ary embolism (PE) following total knee replacement or hip replacement.§ Surgical site infecti<strong>on</strong> includes CABG mediastinitis; surgical site infecti<strong>on</strong> following spine, neck, shoulder, or elbow orthopedic procedures; and surgical siteinfecti<strong>on</strong> following laparoscopic gastric bypass, gastroenterostomy, or laparoscopic gastric restrictive surgery.Source: AHRQ, Center for Delivery, Organizati<strong>on</strong>, and Markets, Healthcare Cost and Utilizati<strong>on</strong> Project, State Inpatient <strong>Data</strong>bases, 2008 from the followingstates with POA data: AR, AZ, CA, FL, HI, KY, MA, MD, ME, MI, NJ, NV, NY, OR, and TN.CMS Hospital-acquired c<strong>on</strong>diti<strong>on</strong>s by age groupAcross all <str<strong>on</strong>g>of</str<strong>on</strong>g> the ten CMS-defined HACs combined, 13 percent occurred in 18-44 year olds, 32percent occurred in 45-64 year olds, 44 percent occurred in 65-84 year olds, and 12 percentoccurred in those 85 years and older (data not shown). Figure 2 denotes the rate <str<strong>on</strong>g>of</str<strong>on</strong>g> selectedCMS-defined HACs for three age groups relative to the rate for young adults (18-44 year olds).Relative to young adults, older adults had higher rates for the CMS HACs for stage III and IVpressure ulcers, falls and trauma, catheter-associated urinary tract infecti<strong>on</strong>, and deep veinthrombosis/pulm<strong>on</strong>ary embolism following total knee or hip replacement. The discrepancy withyoung adults generally widened as the age group increased in age. For example, those 85 yearsand older had nearly six times the rate <str<strong>on</strong>g>of</str<strong>on</strong>g> CMS HACs for falls and trauma and about four and ahalf times the rate <str<strong>on</strong>g>of</str<strong>on</strong>g> CMS HACs for catheter-associated urinary tract infecti<strong>on</strong>s relative to 18-44year olds. However, for the CMS HACs for c<strong>on</strong>diti<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> manifestati<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> poor glycemicc<strong>on</strong>trol and vascular catheter-associated infecti<strong>on</strong>s, the older age groups had lower CMS HACrates than the young adults.6
Figure 2. Rate <str<strong>on</strong>g>of</str<strong>on</strong>g> CMS-defined Hospital-Acquired C<strong>on</strong>diti<strong>on</strong>s for Older AgeGroups Relative to Young Adults, in Selected Community Hospitals in 15States, 2008 ±Vascular catheter-associated infecti<strong>on</strong>Falls and traumaCatheter-associated urinary tract infecti<strong>on</strong>(UTI)Manifestati<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> poor glycemic c<strong>on</strong>trolStage III and IV pressure ulcersDeep vein thrombosis (DVT)/pulm<strong>on</strong>ary embolism(PE)‡1.0 = 18-44 year olds(reference group)85 years and older65-84 year olds45-64 year oldsSurgical site infecti<strong>on</strong> (selected surgeries)§0.00 1.00 2.00 3.00 4.00 5.00 6.00 7.00Age-specific discharge rate relative to 18-44 year olds± Adults 18 years and older.‡ Deep vein thrombosis (DVT)/pulm<strong>on</strong>ary embolism (PE) following total knee replacement or hip replacement.§ Surgical site infecti<strong>on</strong> includes CABG mediastinitis; surgical site infecti<strong>on</strong> following spine, neck, shoulder, or elbow orthopedic procedures; and surgical siteinfecti<strong>on</strong> following laparoscopic gastric bypass, gastroenterostomy, or laparoscopic gastric restrictive surgery.Source: AHRQ, Center for Delivery, Organizati<strong>on</strong>, and Markets, Healthcare Cost and Utilizati<strong>on</strong> Project, State Inpatient <strong>Data</strong>bases, 2008 from the followingstates with POA data: AR, AZ, CA, FL, HI, KY, MA, MD, ME, MI, NJ, NV, NY, OR, and TN.7
Endnotes1. Effective October 1, 2008.2. Effective July 1, 2011; Medicaid Program; Payment Adjustments for Provider-PreventableC<strong>on</strong>diti<strong>on</strong>s Including Healthcare-Acquired C<strong>on</strong>diti<strong>on</strong>s, Final Rule, 2011.http://www.<str<strong>on</strong>g>of</str<strong>on</strong>g>r.gov/OFRUpload/OFR<strong>Data</strong>/2011-13819_PI.pdf3. U.S. Centers for Medicare and Medicaid Services. Hospital-Acquired C<strong>on</strong>diti<strong>on</strong>s.https://www.cms.gov/HospitalAcqC<strong>on</strong>d/06_Hospital-Acquired_C<strong>on</strong>diti<strong>on</strong>s.asp4. For example:Meddings J, Saint S, McMah<strong>on</strong> LF Jr. Hospital-acquired catheter-associated urinary tractinfecti<strong>on</strong>: documentati<strong>on</strong> and coding issues may reduce financial impact <str<strong>on</strong>g>of</str<strong>on</strong>g> Medicare's newpayment policy. Infect C<strong>on</strong>trol Hosp Epidemiol. 2010 Jun;31(6):627-33.McNutt R, Johns<strong>on</strong> TJ, Odwazny R, Remmich Z, Skarupski K, Meurer S, Hohmann S,Harting B. Change in MS-DRG assignment and hospital reimbursement as a result <str<strong>on</strong>g>of</str<strong>on</strong>g>Centers for Medicare & Medicaid changes in payment for hospital-acquiredc<strong>on</strong>diti<strong>on</strong>s: is it coding or quality? Qual Manag Health Care. 2010Jan-Mar;19(1):17-24.5 U.S. Centers for Medicare and Medicaid Services, Inpatient Prospective Payment System(IPPS) Fiscal Year 2009 Final Rule. http://edocket.access.gpo.gov/2008/pdf/E8-17914.pdfAcknowledgementsThis document was prepared by :Jared Lane Maeda, Ph.D., M.P.H., Judy Parlato, M.B.A., B.S.N., R.N., Katharine Levit, <str<strong>on</strong>g>of</str<strong>on</strong>g>Thoms<strong>on</strong> Reuters; and Roxanne M. <str<strong>on</strong>g>An</str<strong>on</strong>g>drews, Ph.D., and H. Joanna Jiang, Ph.D. <str<strong>on</strong>g>of</str<strong>on</strong>g> AHRQ.Y. Clare Sun (Thoms<strong>on</strong> Reuters) provided programming assistance.This analysis would not be possible without the data provided by the following <strong>HCUP</strong> Partnerdata organizati<strong>on</strong>s:Ariz<strong>on</strong>a Department <str<strong>on</strong>g>of</str<strong>on</strong>g> Health ServicesArkansas Department <str<strong>on</strong>g>of</str<strong>on</strong>g> HealthCalifornia Office <str<strong>on</strong>g>of</str<strong>on</strong>g> Statewide Health Planning and DevelopmentFlorida Agency for Health Care Administrati<strong>on</strong>Hawaii Health Informati<strong>on</strong> Corporati<strong>on</strong>Kentucky Cabinet for Health and Family ServicesMaine Health <strong>Data</strong> Organizati<strong>on</strong>Maryland Health Services Cost Review Commissi<strong>on</strong>Massachusetts Divisi<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> Health Care Finance and PolicyMichigan Health & Hospital Associati<strong>on</strong>Nevada Department <str<strong>on</strong>g>of</str<strong>on</strong>g> Health and Human ServicesNew Jersey Department <str<strong>on</strong>g>of</str<strong>on</strong>g> Health and Senior ServicesNew York State Department <str<strong>on</strong>g>of</str<strong>on</strong>g> Health8
Oreg<strong>on</strong> Associati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> Hospitals and Health SystemsTennessee Hospital Associati<strong>on</strong>Texas Department <str<strong>on</strong>g>of</str<strong>on</strong>g> State Health ServicesUtah Department <str<strong>on</strong>g>of</str<strong>on</strong>g> HealthVerm<strong>on</strong>t Associati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> Hospitals and Health SystemsVirginia Health Informati<strong>on</strong>Washingt<strong>on</strong> State Department <str<strong>on</strong>g>of</str<strong>on</strong>g> HealthWest Virginia Health Care AuthorityWisc<strong>on</strong>sin Department <str<strong>on</strong>g>of</str<strong>on</strong>g> Health ServicesWyoming Hospital Associati<strong>on</strong>∗9
Appendix A: Definiti<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> CMS Hospital-Acquired C<strong>on</strong>diti<strong>on</strong>sThe ICD-9-CM diagnosis codes for the CMS hospital-acquired c<strong>on</strong>diti<strong>on</strong>s are as follows:The ICD-9-CM codes defining Foreign Object retained after surgery are:• 998.4, foreign body left during a procedure not elsewhere classified.• 998.7, acute reacti<strong>on</strong> to foreign body left during a procedure not elsewhere classifiedThe ICD-9-CM code defining Air Embolism is:• 999.1, air embolism as complicati<strong>on</strong> <str<strong>on</strong>g>of</str<strong>on</strong>g> medical care not elsewhere classifiedThe ICD-9-CM code defining Blood Incompatibility is:• 999.6, ABO incompatibility reacti<strong>on</strong> not elsewhere classified, incompatible bloodtransfusi<strong>on</strong>The ICD-9-CM codes defining Stage III and IV Pressure Ulcers are:• 707.23, pressure ulcer, stage III• 707.24, pressure ulcer, stage IVThe ICD-9-CM codes defining Falls and Trauma include diagnosis codes in the following range:• 800-829.99, fractures• 830-839.99, dislocati<strong>on</strong>• 850-854.99, intracranial injury• 925-929.99, crushing injury• 940-949.99, burn• 991-994.99, electric shockThe ICD-9-CM codes defining Manifestati<strong>on</strong>s <str<strong>on</strong>g>of</str<strong>on</strong>g> Poor Glycemic C<strong>on</strong>trol are:• 250.10, diabetes mellitus with ketoacidosis type II or unspecified type• 250.11, diabetes mellitus with ketoacidosis type I not stated as unc<strong>on</strong>trolled• 250.12, diabetes mellitus with ketoacidosis type II or unspecified type unc<strong>on</strong>trolled• 250.13, diabetes mellitus with ketoacidosis type I or unc<strong>on</strong>trolled• 250.20, diabetes mellitus with hyperosmolarity type II not stated as unc<strong>on</strong>trolled• 250.21, diabetes mellitus with hyperosmolarity type I not stated as unc<strong>on</strong>trolled• 250.22, diabetes mellitus with hyperosmolarity type II or unspecified type unc<strong>on</strong>trolled10
• 250.23, diabetes mellitus with hyperosmolarity type I unc<strong>on</strong>trolled• 251.0, hypoglycemic coma• 249.10, sec<strong>on</strong>dary DM with ketoacidosis, not stated as unc<strong>on</strong>trolled or unspecified• 249.11, sec<strong>on</strong>dary DM with ketoacidosis, unc<strong>on</strong>trolled• 249.20, sec<strong>on</strong>dary DM with hyperosmolarity, not stated as unc<strong>on</strong>trolled, unspecified• 249.21, sec<strong>on</strong>dary DM with hyperosmolarity, unc<strong>on</strong>trolledThe ICD-9-CM code defining Catheter-Associated Urinary Tract Infecti<strong>on</strong> (CA-UTI) is:• 996.64, infecti<strong>on</strong> and inflammatory reacti<strong>on</strong> due to indwelling urinary catheterThe ICD-9-CM code defining Vascular Catheter-Associated Infecti<strong>on</strong> is:• 999.31, infecti<strong>on</strong> due to central venous catheterThe ICD-9-CM code defining Surgical Site Infecti<strong>on</strong>: Mediastinitis following Cor<strong>on</strong>ary ArteryBypass Graft (CABG) is:• 519.2, mediastinitisThe ICD-9-CM code defining Surgical Site Infecti<strong>on</strong> Following Orthopedic Procedures is:• 998.59, post-procedural fever• 996.67, infecti<strong>on</strong> and inflammatory reacti<strong>on</strong> due to other internal orthopedic deviceimplant and graftThe ICD-9-CM codes defining Surgical Site Infecti<strong>on</strong> Following Bariatric Surgery for Obesityare:• 278.01, morbid obesity (Principal Diagnosis)• 998.59, post-procedural feverThe ICD-9-CM codes defining Deep Vein Thrombosis/Pulm<strong>on</strong>ary Embolism are:• 415.11, iatrogenic pulm<strong>on</strong>ary embolism and infarcti<strong>on</strong>• 415.19, other pulm<strong>on</strong>ary embolism and infarcti<strong>on</strong>• 453.40, acute venous embolism and thrombosis <str<strong>on</strong>g>of</str<strong>on</strong>g> unspecified deep vessels <str<strong>on</strong>g>of</str<strong>on</strong>g> lowerextremity• 453.41, acute venous embolism and thrombosis <str<strong>on</strong>g>of</str<strong>on</strong>g> deep vessels <str<strong>on</strong>g>of</str<strong>on</strong>g> proximal lowerextremity• 453.42, acute venous embolism and thrombosis <str<strong>on</strong>g>of</str<strong>on</strong>g> deep vessels <str<strong>on</strong>g>of</str<strong>on</strong>g> distal lower extremity11