ventilation_JEMS_feb.. - Swissrescue
ventilation_JEMS_feb.. - Swissrescue
ventilation_JEMS_feb.. - Swissrescue
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
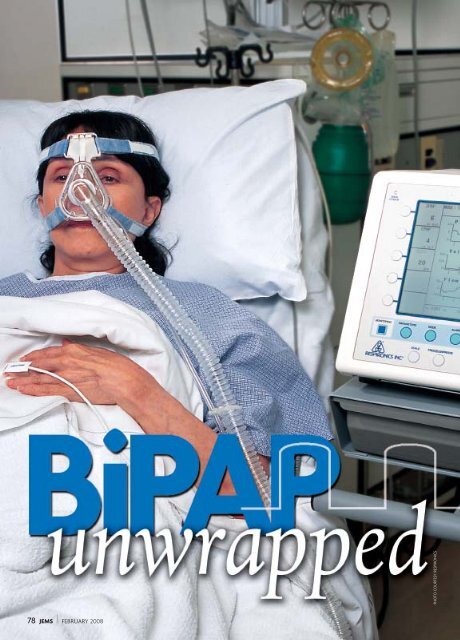
78 <strong>JEMS</strong> FEBRUARY 2008PHOTO COURTESY RESPIRONICS
HOW NON-INVASIVE VENTILATIONHELPS PATIENTS IN RESPIRATORY FAILURE>> BY JAMES F. GOSS, MHA, MICPCASE PRESENTATIONYou respond to the home of a 62-yearoldfemale presenting with shortness ofbreath, which increases on exertion. Thepatient’s daughter informs you that hermother has a history of coronary arterydisease, congestive heart failure (CHF) andchronic bronchitis. She also reports a longhistory of orthopnea, which requires herto sleep propped up on four pillows.The patient is unable to speak morethan a few words at a time and appears tobe weakening. Vitals: HR 118, RR 26 andshallow, BP 160/104, with a room airoxygen saturation of 88%. You observejugular venous distention and obviousaccessory muscle use. Auscultation ofthe lungs reveals diminished tidal volumeand crackles in the bases of thelungs bilaterally.You quickly place her on supplementaloxygen, while your partner readiesequipment to deliver continuous positiveairway pressure (CPAP). Shortlyafter CPAP is initiated, the patientreports improvement and appears to bebreathing more comfortably, althoughshe remains in severe distress.During transport, her blood pressureremains elevated, so you administerrepeated doses of nitroglycerine at 0.4 mgsublingual and 4 mg of morphine sulfateintravenously. On arrival at the localhospital, the emergency department(ED) staff removes the patient fromCPAP and places her on a device thatdelivers biphasic positive airway pressure(BiPAP) and continues with nitroglycerineand morphine sulfate. Theyalso administer diuretics and nebulizedalbuterol. As you leave the ED, you wonderwhy the hospital switched yourpatient from CPAP—which worked wellduring transport—to BiPAP.INTRODUCTIONUtilization of CPAP is increasing in theprehospital setting, but it isn’t always thebest choice of non-invasive positive pressure<strong>ventilation</strong> (NPPV). To understandwhy, we must first understand the relatedanatomy and physiology, mechanisms ofaction and indications for treatment.NPPV can be effectively used in theprehospital environment and improvesemergency management of patientswith acute respiratory failure due tochronic obstructive pulmonary disease(COPD) and cardiogenic pulmonaryedema. 1,2 It has been shown to improvealveolar <strong>ventilation</strong> and gas exchangewhile decreasing preload and afterload,improving lung compliance, increasingfunctional residual capacity anddecreasing breathing work. 3 When usedwith other therapies, it’s effective in thetreatment of acute respiratory failure inthe emergency setting.Because as many as 19% of intubatedpatients must be re-intubated, which isan independent predictor of death,avoiding intubation whenever possiblebenefits our patients. 4 Further, with theincreased incidence of pneumonia andother complications, associated endotrachealintubation can be avoided throughuse of NPPV. With increased utilizationand development of NPPV techniques,intubation of these patients may becomeobsolete and outcomes for these patientscan improve.THE BASICS OF BREATHINGCardiogenic pulmonary edema and COPDare the two disease states leading to acuterespiratory failure that necessitate the useof NPPV in the prehospital environment.Thus, it’s important for emergency caregiversto understand the basic conceptssurrounding the anatomic and physiologicaspects of breathing in both the healthyand diseased lung.The primary purpose of the lungs is tofacilitate gas exchange via the 300 millionalveoli in the normal adult lung. This numberof alveoli provides 70–80 squaremeters of surface area in close contactwith a meshwork of tiny capillaries thatcarry carbon dioxide and exchange it foroxygen. The lungs receive essentiallyWWW.<strong>JEMS</strong>.COM FEBRUARY 2008 <strong>JEMS</strong> 79
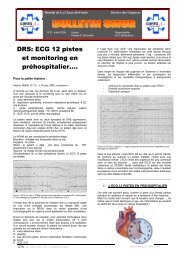
BIPAP UNWRAPPED>> CONTINUED FROM PAGE 79100% of the cardiac outputand contain up to 12% of thebody’s total blood volume atone time. 5The lungs are ventilatedthrough a bellows-like systemor ventilatory pump. Anyonewho has observed a dissectionor autopsy has seen howthe chest expands and thelungs contract when the thoraxis dissected. This actiondemonstrates the natural tendencyof the chest wall tomove outward and the lungsto recoil inward.As compared to the chest,the lungs are the more compliant;that is, they yield toforce. In this case, the forceis provided by the ventilatorypump, which consists ofthe chest wall, diaphragmand pleura.Normal lungs are flexiblebecause they’re made up oflarge amounts of elastinand collagen. Surface tensionwithin the 300 millionalveoli also contributes tothe lungs elastic recoil. 5COPD, pulmonary edemaand asthma damage thelung’s elastic airways andthe alveoli themselves, causinga loss of surface tension.The combined effect is thatthe lungs become much stiffer, as occurswith pulmonary edema, making it more difficultfor the ventilatory pump to expandthe lungs, especially during exacerbationsof the illness.The diaphragm and other respiratorymuscles within the chest wall are consideredthe only skeletal muscles essential to life. 6Fatigue of the respiratory muscles is a commoncause of respiratory failure. 5Respiratory muscles become fatiguedwhen there’s an increased ventilatorydemand, increased work of breathing or inadequateenergy production by the musclesthemselves. These conditions often resultfrom disease states, such as COPD, asthmaand CHF.Inspiration is an active process. Musclesneed to work and expand the pump so airFigure 1: Primary Airway DefensesAirway lumenPressureBiPAPCPAPAmbientpressureMucus-secretinggoblet cellTimeForeign particlesGel layerCiliaSol layerCiliatedepitheliumBasementmembraneThe thin sol layer allows cilia to move rhythmically, propelling the upper gel layerand any trapped particles toward the larynx to be coughed up or swallowed.Figure 2: BiPAP & CPAP in the Respiratory CycleBiPAP performs the same function as CPAP but, in addition, detects the patient’sinspiratory effort and delivers greater pressure when necessary.ILLUSTRATIONS BROOK WAINWRIGHTmoves into the lungs. Exhalation is a passiveprocess in the normal healthy lung. Itbecomes an active process when air becomestrapped by mucus or collapsed airways inthe presence of certain diseases, such asCOPD. This effect increases the likelihood ofmuscular fatigue.The diaphragm is the primary muscle of<strong>ventilation</strong> and moves downward to draw airinto the lungs. When the lungs are alreadyhyperinflated due to emphysema, thediaphragm is limited because it’s already lowand flat. 5 With severe hyperinflation, thecontraction of the diaphragm causes anexpiratory effect during inhalation becausethe lower portion of the ribs are pulled inrather than pushed out.Mucociliary clearance provides one of theprimary defenses of the lungs. Ciliated epithelia(little hairs) within the airwaystransport depositedmaterials from the level ofthe terminal bronchioles tothe larynx where they’recoughed out or swallowed.The cilia are capable ofmoving particles at a rate of3 mm per minute, allowingfor 90% of deposited particlesto be cleared every twohours. 5Many diseases, includingasthma and COPD cause aloss of cilia, impairing thisdefense mechanism. Particlesbecome trapped in mucussecreted by goblet cells. Twolayers of mucus and a thicktop layer of gel trap material,while the cilia are housedin the thin sol layer (seeFigure 1).Chronic bronchitis resultsin a thickening of mucus dueto the proliferation of mucussecretinggoblet cells. Thisimpairs the ability of the ciliato function normally.Another defense mechanismpresent in the lungs isthe lymphatic drainage system.The lymphatic systemcan remove an estimated10–20 mL of fluid per hour inthe healthy lung. Under severestress, this capability isexceeded, resulting in fluid accumulation andinterstitial edema. The interstitium of eachlung can hold more than 500 mL of fluid.When this volume is exceeded, tight junctionsof the alveolar epithelium becomedamaged and the fluid floods into the alveolarair spaces, interfering with surface tensionand gas exchange. 5PATIENTS IN RESPIRATORY FAILUREAlthough cardiogenic pulmonary edema andCOPD are two completely different conditions,they can both result in respiratory failure.It may develop over time, or it may appearsuddenly with little or no warning.Chronic obstructive lung disease (COLD)includes a group of disorders that causechronic airflow obstruction. These disordersinclude emphysema and chronic bronchitis.80 <strong>JEMS</strong> FEBRUARY 2008
BIPAP UNWRAPPED>> CONTINUED FROM PAGE 80PHOTO KEVIN LINKCOLD affects 5% of the adult population inthe U.S. 5The incidence and mortality of COLD isrising worldwide due to the increasedprevalence of smoking in women and children.5 COLD is characterized by progressive,permanent destruction of the lung’sparenchyma. Although bronchodilators andanti-inflammatory agents do help, theycan’t reverse the damage.Chronic bronchitis is accompanied bynarrowing of the airways due to inflammationand hypertrophy of mucus glands,along with excessive mucus secretion. Thetissue of terminal airways and alveolibecome fibrotic and stiff. Remodeling of thepulmonary vasculature results in a backpressure that causes the patient’s liver toenlarge, ankles to swell and neck veins todistend. 5 These patients tend to be overweight,edematous and cyanotic.Emphysema is characterized by permanentalveolar enlargement and alveolar walldestruction without fibrosis. Emphysemapatients are frequently thin and barrelchesteddue to the enlarged alveoli. They’reoften pink due to excessive production ofred blood cells, called polycythemia.An increased work of breathing can lead to fatigue of therespiratory muscles, which often results in respiratory failure.The Elisée 250 bilevel device by ResMed (left) has three <strong>ventilation</strong> modes and can be used on pediatricpatients. The S/T-D 30 by Respironics (right) has the controls under a cover to keep the settings intact.THE DIFFERENCEBETWEEN CPAP & BIPAPIt should be noted that there’s disagreementamong the literature as to whether CPAP is aform of NPPV. CPAP provides oxygenationbut not <strong>ventilation</strong>, which is the actual movementof air into the lungs. CPAP augments<strong>ventilation</strong>, which should qualify it as a formof NPPV. For the purpose of this discussion,CPAP and BiPAP will both be considered asforms of NPPV.CPAP is a continuous pressure providedabove ambient pressure, which helps preventalveoli from collapsing and augments<strong>ventilation</strong>. This pressure remains relativelyconstant through each phaseof the respiratory cycle, varyingonly slightly as the patientbreathes (see Figure 2, p. 80).Because the pressure is thesame throughout all phases ofthe respiratory cycle, the patientmust overcome the pressureduring expiration. CPAP is limitedby the patient’s ability tobreathe and would be ineffectivein those who can’t generatea strong enough tidal breath ontheir own.BiPAP also provides CPAP,but it also detects the patient’sinspiratory effort and deliversgreater pressure during inspiration(see Figure 2). This is similarto squeezing the bag whileassisting a patient with breathing.At the end of the inspiratoryphase, the pressure drops backto the preset level of CPAP.The term “BiPAP” is actuallythe trade name for the biphasicpositive airway pressuredevice developed and sold byRespironics. Today, however, it’s commonlyused to describe biphasic positive airway pressure.Other names include bilevel (or biphasic)airway pressure, bilevel (or biphasic) positivepressure, bilevel (or biphasic) CPAP, bilevel (orbiphasic) pressure support, among others. 7CPAP machines are generally capable ofdelivering only CPAP, whereas BiPAP machinescan deliver either CPAP or BiPAP. Respiratorycare practitioners and emergency physiciansreport that BiPAP provides a greater level ofcontrol than CPAP. So it’s not uncommon fora patient to be removed from the prehospitalCPAP device and placed on a device capableof BiPAP. Usually the patient is kept on CPAPuntil blood gases are obtained. Once bloodgas measurements are evaluated, BiPAP isinitiated at settings that will provide the bestgas exchange and optimum cardiopulmonaryperformance.A 1997 study suggests that BiPAPimproves <strong>ventilation</strong> and vital signs morequickly than CPAP. 8 So in systems wheretransport times are long (e.g., rural areas), itmay be beneficial for patients to be placed onBiPAP rather than CPAP. Improvements in<strong>ventilation</strong> and vital signs would occur soonerand can be maintained for the duration ofthe transport. However, the study alsorevealed an increase in the incidence ofmyocardial infarction in those patientsplaced on BiPAP. Thus, it’s necessary for theprovider to reassess the patient frequently.BENEFITS & DRAWBACKSBiPAP and CPAP are beneficial because theydecrease the need for endotracheal intubation,thereby lessening the complicationsassociated with intubation. These includepneumonia, upper-airway injury and prolongedICU and hospital stays. Additionally,although the use of NPPV is recommendedfor relaxed, non-combative patients, the usePHOTOS COURTESY RESMED & JAMES GOSS82 <strong>JEMS</strong> FEBRUARY 2008
of these forms of NPPV doesn’t generallyrequire sedation.Complications of BiPAP and CPAP are typicallyminor and include injury to tissues wherethe mask makes contact with the face. Thisrisk is especially true for older patients whotypically have thinner skin.Other complications include gastric distention,aspiration pneumonia, hypotension andpneumothorax. For these reasons, NPPVshouldn’t be used on patients who have undergonerecent facial surgery, have excessivesecretions, are experiencing gastrointestinalbleeding or don’t have the ability to protecttheir own airways.CONCLUSIONThere’s significant support for NPPV in theemergency management of patients sufferingfrom acute respiratory failure due tocardiogenic pulmonary edema and COPD.Although CPAP and BiPAP are both gainingpopularity, BiPAP is sometimes preferableconsidering transport times and environment.Unfortunately, BiPAP machines aresignificantly more expensive, making CPAPthe more common form of NPPV used inthe field.In the case presentation, the patient wasremoved from the CPAP device and placedon a BiPAP device. This therapy providedthe hospital staff greater control once arterialblood gases were determined. Thepatient was kept on a CPAP mode untilthese values were determined, at whichpoint inspiratory pressure support was initiatedusing BiPAP modes.NPPV will likely be increasingly used by prehospitalproviders in the treatment of respiratoryfailure, and it’s critical for us to understandwhen and how to apply this therapy for thebest possible outcome for our patients. <strong>JEMS</strong>James F. Goss, MHA, MICP, is program director andlead paramedic instructor for NCTI in Riverside, Calif.He’s also assistant professor of emergency medicalcare at Loma Linda University in Loma Linda, Calif.,and a frequent contributor to <strong>JEMS</strong>. Contact him atJames_Goss@amr-ems.com.The author thanks the respiratory care faculty atLoma Linda University for their assistance in the preparationof this article.REFERENCES1. Weitz G, Struck J, Zonak A, et al: “Prehospital noninvasivepressure support <strong>ventilation</strong> for acute cardiogenicpulmonary edema.” European Journal of EmergencyMedicine. 14(5):276–279, 2007.2. Hess DR: “The evidence for noninvasive positive pressure<strong>ventilation</strong> in the care of patients in acute respiratoryfailure: A systematic review of the literature.”Respiratory Care. 49(7):810–829, 2004.3. Goss JF, Zygowiec J: “Positive pressure: CPAP in the treatmentof pulmonary edema and COPD.” <strong>JEMS</strong>. 31(11):48-58, 2006.4. Agarwal R, Aggarwal AN, Gupta D, et al: “Role of noninvasivepositive-pressure <strong>ventilation</strong> in postextubationrespiratory failure: A meta-analysis.” Respiratory Care.52(11):1472–1479, 2007.5. George RB, Light RW, Matthay MA, et al (Eds.): ChestMedicine: Essentials of Pulmonary and Critical CareMedicine. Lippincott Williams & Wilkins: NewYork, 2005.6. Macklem PT: “Respiratory muscles: The vital pump.”Chest. 78(5):753–758, 1980.7. Pilbeam SP, Cairo JM (Eds.): Mechanical Ventilation:Physiological and Clinical Applications. Mosby: St. Louis, 2006.8. Mehta S, Jay GD, Woolard RH, et al: “Randomized,prospective trial of bilevel versus continuous positiveairway pressure in acute pulmonary edema.” CriticalCare Medicine. 25(4):620–628, 1997.WWW.<strong>JEMS</strong>.COM FEBRUARY 2008 <strong>JEMS</strong> 83