Normal-Pressure Hydrocephalus - International Hydrocephalus ...
Normal-Pressure Hydrocephalus - International Hydrocephalus ...
Normal-Pressure Hydrocephalus - International Hydrocephalus ...
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
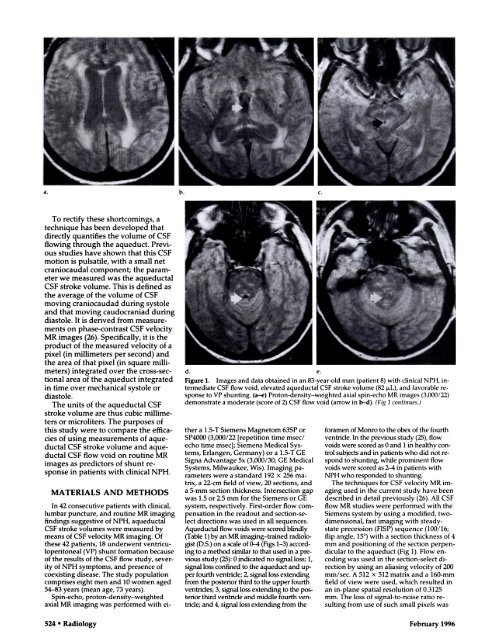
a. b. c.To rectify these shortcomings, atechnique has been developed thatdirectly quantifies the volume of CSFflowing through the aqueduct. Previousstudies have shown that this CSFmotion is pulsatile, with a small netcraniocaudal component; the parameterwe measured was the aqueductalCSF stroke volume. This is defined asthe average of the volume of CSFmoving craniocaudad during systoleand that moving caudocraniad duringdiastole. It is derived from measurementson phase-contrast CSF velocityMR images (26). Specifically, it is theproduct of the measured velocity of apixel (in millimeters per second) andthe area of that pixel (in square millimeters)integrated over the cross-sectionalarea of the aqueduct integratedin time over mechanical systole ordiastole.The units of the aqueductal CSFstroke volume are thus cubic millimeterson microliters. The purposes ofthis study were to compare the efficaciesof using measurements of aqueductalCSF stroke volume and aqueductalCSF flow void on routine MRimages as predictors of shunt responsein patients with clinical NPH.MATERIALS AND METHODSd. e.Figure 1. Images and data obtained in an 83-year-old man (patient 8) with clinical NPH, intermediateCSF flow void, elevated aqueductal CSF stroke volume (82 p.L), and favorable responseto VP shunting. (a-e) Proton-density-weighted axial spin-echo MR images (3,000/22)demonstrate a moderate (score of 2) CSF flow void (arrow in b-cl). (Fig 1 continues.)In 42 consecutive patients with clinical,lumbar puncture, and routine MR imagingfindings suggestive of NPH, aqueductalCSF stroke volumes were measured bymeans of CSF velocity MR imaging. Ofthese 42 patients, 18 underwent ventriculoperitoneal(VP) shunt formation becauseof the results of the CSF flow study, severityof NPH symptoms, and presence ofcoexisting disease. The study populationcomprises eight men and 10 women aged54-83 years (mean age, 73 years).Spin-echo, proton-density-weightedaxial MR imaging was performed with eithera 1.5-T Siemens Magnetom 63SP orSP4000 (3,000/22 [repetition time msec/echo time msec]; Siemens Medical Systems,Erlangen, Germany) or a 1.5-T GESigna Advantage 5x (3,000/30; GE MedicalSystems, Milwaukee, Wis). Imaging parameterswere a standard 192 x 256 matrix,a 22-cm field of view, 20 sections, anda 5-mm section thickness. Intersection gapwas 1.5 or 2.5 mm for the Siemens or GEsystem, respectively. First-order flow compensationin the readout and section-selectdirections was used in all sequences.Aqueductal flow voids were scored blindly(Table 1) by an MR imaging-trained radiologist(D.S.) on a scale of 0-4 (Figs 1-3) accordmgto a method similar to that used in a previousstudy (25): 0 indicated no signal loss; 1,signal loss confined to the aqueduct and upperfourth ventride; 2, signal loss extendingfrom the posterior third to the upper fourthventrides; 3, signalloss extending to the postetiorthird ventricle and middle fourth yentmicle;and 4, signal loss extending from theforamen of Monro to the obex of the fourthventricle. In the previous study (25), flowvoids were scored as 0 and 1 in healthy controlsubjects and in patients who did not respondto shunting, while prominent flowvoids were scored as 2-4 in patients withNPH who responded to shunting.The techniques for CSF velocity MR imagingused in the current study have beendescribed in detail previously (26). All CSFflow MR studies were performed with theSiemens system by using a modified, twodimensional,fast imaging with steadystateprecession (FISP) sequence (100/16;flip angle, 15#{176}) with a section thickness of 4mm and positioning of the section perpendicularto the aqueduct (Fig 1). Flow encodingwas used in the section-select directionby using an aliasing velocity of 200mm/sec. A 512 x 512 matrix and a 160-mmfield of view were used, which resulted inan in-plane spatial resolution of 0.3125mm. The loss of signal-to-noise ratio resultingfrom use of such small pixels was524 #{149} Radiology February 1996