Normal-Pressure Hydrocephalus - International Hydrocephalus ...
Normal-Pressure Hydrocephalus - International Hydrocephalus ...
Normal-Pressure Hydrocephalus - International Hydrocephalus ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
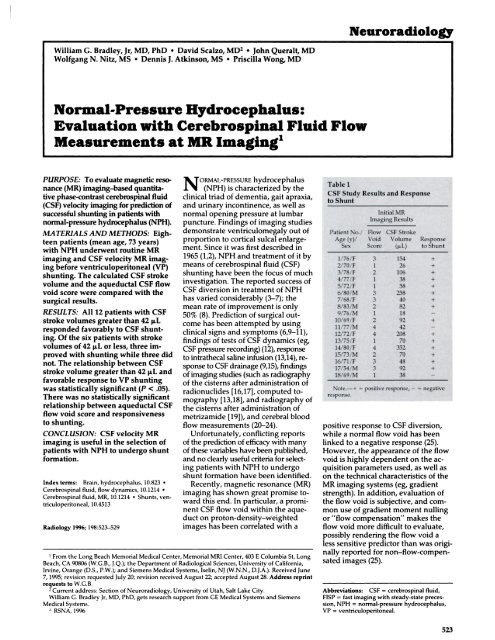
NeuroradlologyWilliam C. Bradley, Jr. MD, PhD #{149}David Scalzo, MD2 #{149}John Queralt, MDWolfgang N. Nitz, MS #{149}Dennis J. Atkinson, MS #{149}Priscilla Wong, MD<strong>Normal</strong>-<strong>Pressure</strong><strong>Hydrocephalus</strong>:Evaluation with Cerebrospinal Fluid FlowMeasurements at MR Imaging’PURPOSE: To evaluate magnetic resonance(MR) imaging-based quantitativephase-contrast cerebrospmal fluid(CSF) velocity imaging for prediction ofsuccessful shunting in patients withnormal-pressure hydrocephalus (NPH).MATERIALS AND METHODS: Eighteenpatients (mean age, 73 years)with NPH underwent routine MRimaging and CSF velocity MR imagingbefore ventriculoperitoneal (VP)shunting. The calculated CSF strokevolume and the aqueductal CSF flowvoid score were compared with thesurgical results.RESULTS: All 12 patients with CSFstroke volumes greater than 42 tLresponded favorably to CSF shunting.Of the six patients with strokevolumes of 42 L or less, three improvedwith shunting while three didnot. The relationship between CSFstroke volume greater than 42 tL andfavorable response to VP shuntingwas statistically significant (P < .05).There was no statistically significantrelationship between aqueductal CSFflow void score and responsivenessto shunting.CONCLUSION: CSF velocity MRimaging is useful in the selection ofpatients with NPH to undergo shuntformation.yen-Index terms: Brain, hydrocephalus, 10.823Cerebrospinal fluid, flow dynamics, 10.1214Cerebrospinal fluid, MR, 10.1214 #{149} Shunts,triculoperitoneal, 10.4513Radiology 1996; 198:523-5291 From the Long Beach Memorial Medical Center, Memorial MRI Center, 403 E Columbia St. LongBeach, CA 90806 (W.G.B., J.Q.); the Department of Radiological Sciences, University of California,Irvine, Orange (D.S., P.W.); and Siemens Medical Systems, Iselin, NJ (W.N.N., D.J.A.). Received June7, 1995; revision requested July 20; revision received August 22; accepted August 28. Address reprintrequeststo W.G.B.N ORMAL-PRESSURE hydrocephalus(NPH) is characterized by theclinical triad of dementia, gait apraxia,and urinary incontinence, as well asnormal opening pressure at lumbarpuncture. Findings of imaging studiesdemonstrate ventriculomegaly out ofproportion to cortical sulcal enlargement.Since it was first described in1965 (1,2), NPH and treatment of it bymeans of cenebrospinal fluid (CSF)shunting have been the focus of muchinvestigation. The reported success ofCSF diversion in treatment of NPHhas varied considerably (3-7); themean mate of improvement is only50% (8). Prediction of surgical outcomehas been attempted by usingclinical signs and symptoms (6,9-1 1),findings of tests of CSF dynamics (eg,CSF pressure necording)(12), responseto intrathecal saline infusion (13,14), responseto CSF drainage (9,15), findingsof imaging studies (such as radiographyof the cisterns after administration ofnadionuclides [16,17], computed tomography[13,18], and radiography ofthe cisterns after administration ofmetrizamide [191), and cerebral bloodflow measurements (20-24).Unfortunately, conflicting reportsof the prediction of efficacy with manyof these variables have been published,and no clearly useful criteria for selectingpatients with NPH to undergoshunt formation have been identified.Recently, magnetic resonance (MR)imaging has shown great promise towardthis end. In particular, a prominentCSF flow void within the aqueducton proton-density-weightedimages has been correlated with a2 Current address: Section of Neuroradiology, University of Utah, Salt Lake City.William G. Bradley Jr. MD, PhD, gets research support from GE Medical Systems and SiemensMedical Systems.‘. RSNA, 1996positive response to CSF diversion,while a normal flow void has beenlinked to a negative response (25).However, the appearance of the flowvoid is highly dependent on the acquisitionparameters used, as well ason the technical characteristics of theMR imaging systems (eg, gradientstrength). In addition, evaluation ofthe flow void is subjective, and commonuse of gradient moment nullingor “flow compensation” makes theflow void more difficult to evaluate,possibly rendering the flow void aless sensitive predictor than was originallyreported for non-flow-compensatedimages (25).Abbreviations: CSF = cerebrospinal fluid,FISP = fast imaging with steady-state precession,NPH = normal-pressure hydrocephalus,VP = ventriculoperitoneal.523
a. b. c.To rectify these shortcomings, atechnique has been developed thatdirectly quantifies the volume of CSFflowing through the aqueduct. Previousstudies have shown that this CSFmotion is pulsatile, with a small netcraniocaudal component; the parameterwe measured was the aqueductalCSF stroke volume. This is defined asthe average of the volume of CSFmoving craniocaudad during systoleand that moving caudocraniad duringdiastole. It is derived from measurementson phase-contrast CSF velocityMR images (26). Specifically, it is theproduct of the measured velocity of apixel (in millimeters per second) andthe area of that pixel (in square millimeters)integrated over the cross-sectionalarea of the aqueduct integratedin time over mechanical systole ordiastole.The units of the aqueductal CSFstroke volume are thus cubic millimeterson microliters. The purposes ofthis study were to compare the efficaciesof using measurements of aqueductalCSF stroke volume and aqueductalCSF flow void on routine MRimages as predictors of shunt responsein patients with clinical NPH.MATERIALS AND METHODSd. e.Figure 1. Images and data obtained in an 83-year-old man (patient 8) with clinical NPH, intermediateCSF flow void, elevated aqueductal CSF stroke volume (82 p.L), and favorable responseto VP shunting. (a-e) Proton-density-weighted axial spin-echo MR images (3,000/22)demonstrate a moderate (score of 2) CSF flow void (arrow in b-cl). (Fig 1 continues.)In 42 consecutive patients with clinical,lumbar puncture, and routine MR imagingfindings suggestive of NPH, aqueductalCSF stroke volumes were measured bymeans of CSF velocity MR imaging. Ofthese 42 patients, 18 underwent ventriculoperitoneal(VP) shunt formation becauseof the results of the CSF flow study, severityof NPH symptoms, and presence ofcoexisting disease. The study populationcomprises eight men and 10 women aged54-83 years (mean age, 73 years).Spin-echo, proton-density-weightedaxial MR imaging was performed with eithera 1.5-T Siemens Magnetom 63SP orSP4000 (3,000/22 [repetition time msec/echo time msec]; Siemens Medical Systems,Erlangen, Germany) or a 1.5-T GESigna Advantage 5x (3,000/30; GE MedicalSystems, Milwaukee, Wis). Imaging parameterswere a standard 192 x 256 matrix,a 22-cm field of view, 20 sections, anda 5-mm section thickness. Intersection gapwas 1.5 or 2.5 mm for the Siemens or GEsystem, respectively. First-order flow compensationin the readout and section-selectdirections was used in all sequences.Aqueductal flow voids were scored blindly(Table 1) by an MR imaging-trained radiologist(D.S.) on a scale of 0-4 (Figs 1-3) accordmgto a method similar to that used in a previousstudy (25): 0 indicated no signal loss; 1,signal loss confined to the aqueduct and upperfourth ventride; 2, signal loss extendingfrom the posterior third to the upper fourthventrides; 3, signalloss extending to the postetiorthird ventricle and middle fourth yentmicle;and 4, signal loss extending from theforamen of Monro to the obex of the fourthventricle. In the previous study (25), flowvoids were scored as 0 and 1 in healthy controlsubjects and in patients who did not respondto shunting, while prominent flowvoids were scored as 2-4 in patients withNPH who responded to shunting.The techniques for CSF velocity MR imagingused in the current study have beendescribed in detail previously (26). All CSFflow MR studies were performed with theSiemens system by using a modified, twodimensional,fast imaging with steadystateprecession (FISP) sequence (100/16;flip angle, 15#{176}) with a section thickness of 4mm and positioning of the section perpendicularto the aqueduct (Fig 1). Flow encodingwas used in the section-select directionby using an aliasing velocity of 200mm/sec. A 512 x 512 matrix and a 160-mmfield of view were used, which resulted inan in-plane spatial resolution of 0.3125mm. The loss of signal-to-noise ratio resultingfrom use of such small pixels was524 #{149} Radiology February 1996
f. g. h.1. j.Figure 1 (continued). (f) Sagittal, scout, TI-weighted, spin-echo MR image (500/15) demonstratesposition of section for assessing CSF flow through the aqueduct. (g) Magnitude FISPMR image (100/16; 15#{176} flip angle) obtained during CSF flow study demonstrates aqueduct(arrow). (h) Phase-contrast FISP MR image (100/16; 15#{176} flip angle) obtained during systoledemonstrates craniocaudal flow (arrow; whitest areas = 200 mm/sec craniocaudal). (1) PhasecontrastFISP MR image (100/16; 15#{176} flip angle) obtained during diastole demonstrates caudocranialflow (arrow; blackest areas = 200 mm/sec caudocranial). (j) Plots of mean velocity (millimetersper second; upper left), peak velocity (millimeters per second; upper right), andvolumetric flow rate (cubic millimeters per second; lower left) as functions of the cardiac cycle(milliseconds). Peak velocity plot demonstrates aliasing.Findings of previous studies (27) in whicha pulsatile flow phantom has been usedhave verified the accuracy of the aqueductalCSF stroke volume measurement whileshowing that the peak velocity measurementsare particularly sensitive to noise(Figlj).Clinical data were collected from chartreview and discussion with clinicians. Apositive response to shunting was definedas any substantial clinical functional improvement,even if not all symptoms werealleviated. For example, patient 6 (Table1), who was nonambulatory before shunting,became ambulatory and had decreasedurinary incontinence after surgery. Althoughthis patient had no improvement in his substantialdementia, these other improvementsallowed his family to provide care at homeand alleviated the need for skilled nursing.Thus, this was considered a positive outcome.This mixed response, however, wasatypicaL In most patients, there was eitherobvious improvement or clearly no substantialchange; thus, differentiation betweenpositive and negative responses to shuntingwas, in most cases, not difficult.partially compensated for by reducing thebandwidth from 130 Hertz per pixel to 78Hertz per pixel. Use of a half-Fourier algorithm(with 16 lines of oversampling)helped to keep the measurement timewithin reason (14 minutes). The CSF yelocitydata ultimately used to calculate theaqueductal CSF stroke volume were obtamedfrom these images.Continuous data acquisition and retrospectivecardiac gating with electrocardiographicleads were used to allow evaluationof CSF velocity during the entirecardiac cycle (26). Thirty-two flow-encodedacquisitions were obtained in 3.2seconds (usually three or four cardiaccycles) before advance of the phase-encodinggradient. Data were then retmospectivelysorted into 18 cine frames spanningthe complete cardiac cycle. A “zerovelocity”reference image was calculatedby averaging all the phase measurementson each of the phase images with the assumptionof zero net flow through theaqueduct of Sylvius during one cardiaccycle. The phase measurements on thiszero-velocity reference image were thensubtracted from the phase measurementson each of the phase images to produce 18phase-contrast, CSF velocity MR images.While this assumption of zero net flowclearly introduces some error, the magnitudeof the error has been shown to beless than 5% in healthy control subjectsand considerably less than 5% in patientswith hydrocephalus, because more than95% of the volumetric flow during onecardiac cycle is to-and-fro (26).Software was developed to determinethe mean and peak velocities and the volumetricflow rate through the aqueduct asa percentage of the cardiac cycle (Figs Ij,2f, 3f). Stroke volumes for both diastoleand systole were then calculated by integratingthe area under the volumetric flowrate curve versus time. The mean of theabsolute value of these two measurementswas the aqueductal CSF stroke volume.RESULTSThe routine MR images obtained inall patients displayed ventriculomegaly,usually out of proportion tosulcal enlargement (although varyingdegrees of atrophy were also present).Age, sex, aqueductal CSF flow voidscore, aqueductal CSF stroke volume,and response to shunting are summarizedin Table 1.All 12 patients in this series withstroke volumes greater than 42 p.Lresponded to shunting (Fig 1), whilehalf of the six patients with an aqueductalCSF stroke volume of 42 iL orless did not respond (Figs 2, 3). Patientswith an aqueductal CSF strokevolume greater than 42 p1 were,therefore, considered to have hyperdynamicCSF flow and positive CSFflow study findings, while those withVolume 198 #{149} Number 2 Radiology #{149} 525
a. b. c.d. e. f.Figure 2. Images and data obtained in a 77-year-old man (patient 11) with increased CSF flow void; borderline, decreased aqueductal CSFstroke volume (42 p1); and negative response to VP shunting. (a-e) Proton-density-weighted axial spin-echo MR images (3,000/22) demonstratemarked CSF flow (score of 4) through aqueduct and third and fourth ventricles (arrow). (f) Plot of mean velocity (millimeters per second)and volumetric flow rate (cubic millimeters per second) as a function of the cardiac cycle (milliseconds). Velocity is substantially reduced comparedwith that in the patient in Figure 1, who had hyperdynamic flow.an aqueductal CSF stroke volume lessthan 42 .L were considered to havenormal CSF flow and negative CSFflow study findings. Of the 12 patientswith positive study findings, allimproved after CSF diversion; thus,positive predictive value was 100%.Three of the patients with negativeCSF flow study findings respondedpositively to shunting, while threedid not respond; thus, negative predictivevalue was 50%.The sensitivity of the aqueductalstroke volume criteria was 80%, and thespecificity was 100%. Overall accuracywas 83%. These results are summarizedin Tables 2 and 3. Results of a Fisher exacttest performed with the data in Table2 indicate a significant assodation betweenhigh CSF stroke volume and favorablesurgical response (P < .05).As in a previous study (25), all patientswith CSF flow void scores of 2or higher were considered to havehyperdynamic CSF flow and positivestudy findings, while those with ascone of 0 on 1 were considered tohave normal CSF flow and negativestudy findings. Of the 12 patientswith positive findings according tothese criteria, 11 had improvementwith CSF shunting (Fig 1) while onedid not (Fig 2). In contrast, four of thepatients with negative findings hadimprovement while two did not (Fig3). These data are listed in Table 4;there was no statistically significantrelationship between the CSF flowvoid score and response to CSFshunting according to Fisher exacttest results. The sensitivity of usingthese CSF flow void score criteria was73%; specificity, 67%; positive predictivevalue, 92%; and negative predictivevalue, 33%. Overall accuracy was72%. These results are summarized inTable 3.DISCUSSIONThe following conclusions can bedrawn from this study. Positive CSFflow study findings (ie, stroke volumegreater than 42 1iL) are associatedwith an increased likelihood of improvementwith CSF shunting. Positivepredictive value in the patients inthis study was 100%. Negative predictivevalue of the quantitative CSFflow study findings was 50% . Positivepredictive value for the CSF flow voidscore was 92%; thus, when findingsare positive, theme is a reasonable526 #{149} Radiology February 1996
a. b. c.d. e. f.Figure 3. Images and data obtained in a 69-year-old man (patient 18) with minimal CSF flow void (score of 1) and decreased aqueductal CSFstroke volume (38 p1) consistent with atrophy who nonetheless underwent shunt formation without response. (a-e) Proton-density-weightedaxial spin-echo MR images (3,000/22) demonstrate minimal CSF flow void. (f) Plot of volumetric flow rate versus phase of the cardiac cycleshows decreased flow compared with that in Figure 1. X axis indicates milliseconds, and y axis indicates cubic millimeters or microliters persecond.chance of a favorable surgical mesponse.Negative predictive value forthe CSF flow void score was only33%. Thus, when a marked flow voidis not seen, the patient may still havea favorable response to surgery. Thisprobably represents CSF motion averagingduring the cardiac cycle in apatient with an elevated aqueductalCSF stroke volume. Overall, the quantitativeaqueductal CSF stroke volumeis a better predictor than the qualitativeCSF flow void score.That the aqueductal CSF stroke volumewas more sensitive to hyperdynamicflow than the CSF flow voidscone was predictable. The aqueductalCSF flow void represents an averageof CSF motion during the entire cardiaccycle. The aqueductal CSF strokevolume, on the other hand, is derivedfrom cardiac-gated data without averagingover systole and diastole. Beforethe use of flow compensation,aqueductal CSF flow resulted in relativelygreater signal loss. With theroutine use of flow-compensationtechniques, the aqueductal flow voidis less prominent, and the CSF flowvoid sign previously reported (25) hasbecome a less sensitive predictor ofNPH response to ventricular shunting.Understanding the association betweenelevated CSF stroke volumeand favorable shunt response requiresknowledge of the underlying cause ofNPH. Unfortunately, this pathophysiologyhas eluded investigators sincethe initial description of the disease.Indeed, multiple explanations havebeen put forth, none of which is entimelyadequate. However, one modelpreviously described (25) explainsmuch of what is seen in the currentstudy and is compatible with many ofthe theories and phenomena describedin the literature.As originally conceived (25), theprimary purpose of CSF flow analysiswas to differentiate shunt-responsiveNPH from cerebral atrophy (“burnedout” NPH). Both conditions are characterizedby ventriculomegaly; however,the latter does not respond toCSF diversion.In the setting of NPH, the brain ispushed close to the cranium becauseof ventricular enlargement. Duringsystole, blood fills the cerebral hemi-Volume 198 #{149} Number 2 Radiology #{149} 527
spheres. Because the brain cannot expandoutward, it expands inward.This compresses the lateral and thirdventricles, expressing a relativelylarge volume of CSF through the aqueduct.This results in a prominentCSF flow void and a large CSF strokevolume. Roughly the same volume ofCSF returns to the lateral ventriclesduring diastole with egress of bloodfrom the cranial vault through thevenous system. In atrophy, by comparison,blood flow to the brain isdecreased; thus, stroke volume issmaller and there is a reduced CSFflowvoid.It is generally accepted that NPHlikesymptoms are produced whenthe expanded lateral ventricles placeexcessive tangential shearing forceson periventriculam white matter fibersassociated with gait; problem withgait is often the primary symptom inNPH. With continued ventricular expansion,the cortex is exposed to increasedradial shearing forces, leadingto dementia. Recent preliminary MRimaging studies depicting brain motion(28) hold promise for the evaluationof such shearing motions. Indeed,abnormal findings have beendocumented at histopathologic analysisand MR imaging in the periventricularregion in patients with NPH(29-31). Some authors have implicatedcompromised cerebral blood flow as themain contributing factor to these histopathologicchanges (31-35).Pettonossi et al (36) placed latex balloonsin the lateral ventricles of lambsposterior to the fomamen of Monmo.They inflated and deflated them synchronouslywith normal CSF pulsationssuch that the CSF pulse pressurewas increased without a concomitantincrease in the mean CSF pressure-asituation analogous to that seen inNPH (36,37). A second group of animalsunderwent similar inflation anddeflation of a balloon within the brainparenchyma, while a third group underwentpermanent inflation of balloons(without pulsation) in both latemalventricles. In only the first group,in which the elevated CSF pulse pressureoriginated from within the latemalventricles, did periventricularhistopathologic changes such as thosereported in patients with NPH manifest.Thus, it was concluded that thecritical factor responsible for symptomsin NPH was the “waterhammem” forceexerted by the reexpanding lateral yentricleson the penventricular tissues. Thepurpose of shunting in such patientswas, therefore, not to decrease the meanpressure (which was already normal),but rather to provide additional capacitance.Thus, when the brain expandsduring systole, some of the CSF can goout the shunt, limiting the maximumpressure rise and the shearing forces onthe periventriculam fibers.One must explain why some patientswith imaging findings suggestiveof atrophy have improvementafter CSF shunting (7). To do this, onemust consider that both the CSFstroke volume and CSF pulse pressureare influenced not only by thedegree of atrophy present, but also bythe ventricular size, aqueductal diameter,brain compliance, and cerebralblood flow. For example, compromisedmicrovasculatume in the penventricularregion might allow thesetissues to become injured at a lowerpulse pressure than would tissueswith a normal microvascular supply(31). Alternatively, decreased tensilestrength of the ventricular wall or adjacentparenchyma might allowgreater diastolic reexpansion of theventricles (32-42), leading to increasedmechanical trauma to theperiventriculan white matter tractsand/or increased transependymalCSF flow. This would cause decreasedtissue pressure and microvasculancompromise (35).Several limitations of this studyshould be noted. First, the number ofpatients, especially those with negativeCSF flow study findings who underwentshunt formation, is small.Second, the study is retrospective. (Aprospective trial in which all patientsundergoing a quantitative CSF flowstudy, including those thought not tohave NPH, also would undergo shuntformation would be difficult to justifyethically.) Third, although attemptswere made at blinding chant reviews,this was not always possible becauseof information about the CSF flowstudy written in the physician’s notes.Fourth, although this phase-contrasttechnique is excellent for quantitatinglaminar flow (27), it may result in substantialunderestimation of turbulentflow in patients with especially hyperdynamicCSF flow. Fortunately, insuch cases, the CSF flow void shouldbe particularly prominent.Despite these shortcomings, it isthought that the quantitative CSFflow study is a useful method of predictingresponse to shunting in patientswith NPH and should be consideredthe test of choice after clinicalevaluation and routine imaging (ie,computed tomography or MR imaging)in the work-up in such patients.UReferences1. Hakim 5, Adams RD. The special clinicalproblem of symptomatic hydrocephaluswith normal cerebrospinal fluid pressure:observations on cerebrospinal fluid hydrodynamics.J Neurol Sci 1965; 2:307-327.2. Adams RD. Fisher CM, Hakim 5, et al.Symptomatic occult hydrocephalus with“normal” cerebrospinal fluid pressure. NEnglJ Med 1965; 273:117-126.3. Black PN. Idiopathic normal-pressurehydrocephalus: results of shunting in 62patients. I Neurosurg 1980; 53:371-377.4. Black PN, Ojemann G, Tsouras A. Cerebrospinalfluid shunts for dementia, gaitdisturbance, and incontinence. Clin Neurosurg1985; 32:632-656.5. Greenberg JO, Shenkin HA, Adam R. Idiopathicnormal pressure hydrocephalus: areport of 73 patients. J Neurol NeurosurgPsychiatry 1977; 40:336-341.528 #{149} Radiology February 1996
6. Laws ER, Mokri B. Occult hydrocephalus:results of shunting correlated with diagnostictests. Clin Neurosurg 1977; 24:316-333.7. Black PN, Ojemann RG. <strong>Hydrocephalus</strong>in adults. In: Youmans JT, ed. Neurologicalsurgery. New York, NY: Saunders, 1990;1284-1298.8. Vanneste J, Augustijn P, Dirven C, Tan WF,Goedhart ZD. Shunting normal-pressurehydrocephalus: do the benefits outweighthe risks? A multicenter study and literaturereview. Biology 1992; 42:54-59.9. Fisher CM. The clinical picture in occulthydrocephalus. Clin Neurosurg 1977; 24:270-284.10. Jacobs L, Conti D, Kinkel WR. <strong>Normal</strong>pressurehydrocephalus. Relationships ofclinical and radiologic findings to improvementfollowing shunt surgery. JAMA 1976;235:510-512.11. Vassiloughis J. The syndrome of normalpressurehydrocephalus. J Neurosurg 1984;61 :501-509.12. Borgsen SE, Gjerris F, Sorensen SC. Cerebrospinalfluid conductance and complianceof the cranial spinal space in normalpressure hydrocephalus. J Neurosurg 1979;51:521-525.13. Borgsen SE, Gjerns F. The predictivevalue of conductance to outflow of cerebrospinalfluid in normal pressure hydrocephalus.Brain 1982; 105:65-86.14. Nelson JR. Goodman SJ. An evaluation ofthe cerebrospinal fluid infusion test for hydrocephalus.Neurology 1971;21:1037-1053.15. Wikkelso C, Andersson H, Blomstrand C.The clinical effect of lumbar puncture innormal pressure hydrocephalus. J NeurolNeurosurg Psychiatry 1982; 45:64-69.16. Heinz ER, Davis DO, Carp HR. Abnormalisotope cisternography and symptomaticoccult hydrocephalus: a cooperative isotopic-neuroradiologicstudy in 130 patients.Radiology 1970; 95:109-120.17. Tator CH, Murray SA. A clinical, pneumoencephalographicand radio-isotopestudy of normal-pressure communicatinghydrocephalus. Can Med Assoc J 1971; 105:573-579.18. Jacobs L, Kinkel WR. Computerized axialtransverse tomography and normal pressurehydrocephalus. Neurology 1976; 26:501-507.19. Drayer BP, Rosenbaum AE. Dynamics ofcerebrospinal fluid system as defined bycranial computed tomography. In: WoodJH, ed. Neurobiology of cerebrospinalfluid. Vol 1. New York, NY: Plenum, 1980.20. Greitz TVB, Grepe OAL, Kalmer MSF,Lopez, J. Pre- and postoperative evaluationof cerebral blood flow in low-pressurehydrocephalus. J Neurosurg 1969; 31:644-651.21. Grubb RL, Raichle ME, Gado MH, EichlingJO, Hughes CP. Cerebral blood flow, oxygenutilization and blood volume in dementia.Neurology 1977; 27:905-910.22. Mathew NT, MeyerJS, Hartmann A, OttEO. Abnormal cerebrospinal fluid-bloodflow dynamics: implications in diagnosis,treatment, and prognosis in normal pressurehydrocephalus. Arch Neurol 1975;32:657-664.23. MeyerJS, Kitagaura Y, Tanabashi N, et al.Evaluation of treatment of normal pressurehydrocephalus. J Neurosurg 1985; 62:513-521.24. MeyerJS, Kitagaura Y, Tanabashi N, et al.Pathogenesis of normal pressure hydrocephalus:preliminary observations. SurgNeurol 1985; 23:121-133.25. Bradley WG, Whittemore AR, Kortman KE,et al. Marked cerebrospinal fluid void:indicator of successful shunt in patientswith suspected normal-pressure hydrocephalus.Radiology 1991; 178:459-466.26. Nitz WR, Bradley WG, Watanabe AS, et al.Flow dynamics of cerebrospinal fluid: assessmentwith phase-contrast velocity MRimaging performed with retrospective cardiacgating. Radiology 1992; 183:395-405.27. Mullin WJ, Atkinson D, Hashemi RH, Yu J,Bradley WG. High resolution quantitativeassessment of aqueductal CSF motion byphase contrast MRI technique: correlationwith pulsatile flow phantom. JMRI 1993;3:55.28. Enzmann DR. Pelc NJ. Brain motion:measurement with phase contrast MR imaging.Radiology 1992; 185:653-658.29. DeLand FH, James AEJr, Ladd DJ, et al.<strong>Normal</strong> pressure hydrocephalus: a histologicstudy. Am J Clin Pathol 1972; 58:58-63.30. Di Rocco C, Di TrapaniJ, Maira G, et al.Anatomic-clinical correlations in normaltensive hydrocephalus: reports on 3 cases.Neurol Sci 1977; 33:436-452.31. Bradley WG, Whittemore AR, WatanabeAS, Davis SJ, Teresi LM, Homyak M. Associationof deep white infarction withchronic communicating hydrocephalus:implications regarding the possible originof normal-pressure hydrocephalus. AJNR1991; 12:31-39.32. Greitz T. Effect of brain distention on cerebralcirculation. Lancet 1969; 1:863-865.33. Greitz TVB, Grepe AOL, Kalmer MSF,Lopez J. Pre- and postoperative evaluahonof cerebral blood flow and low pressurehydrocephalus. J Neurosurg 1969; 31:644-651.34. Mathew NT, MeyerJS, Hartmann A, OttEO. Abnormal cerebrospinal fluid-bloodflow dynamics: implications in diagnosis,treatment, and prognosis in normal pressurehydrocephalus. Arch Neurol 1975;32:657-664.35. MeyerJS, Kitagawa Y, Tanahashi N, et al.Pathogenesis of normal pressure hydrocephalus:preliminary observations. SurgNeurol 1985; 23:121-133.36. Pettorossi yE, Di Rocco C, Mancinelli R,Caldareli M, Velardi F. Communicatinghydrocephalus induced by mechanicallyincreased amplitude of the intraventricularcerebrospinal fluid pulse pressure: rationaleand method. Exp Neurol 1978; 59:30-39.37. Sato K, Fuchinoue T, Yahagi Y. CSF pulsewave changes in cases with normal pressurehydrocephalus. In: Lundberg N,Ponten U, Brock M, eds. Intracranial pressure.Vol 2. New York, NY: Springer-VerlagNew York, 1975; 133-136.38. Di Rocco C. <strong>Hydrocephalus</strong> and cerebrospinalfluid pulses. In: Shapiro K, MarmarouA, Portnoy H, eds. <strong>Hydrocephalus</strong>.New York, NY: Raven, 1984; 231-249.39. Foltz EL, Aine C. Diagnosis of hydrocephalusby CSF pulse-wave analysis: aclinical study. Surg Neurol 1981; 15:283-293.40. Sklar FH, Diehl JT, Beyer CWJr, Clark WK.Brain elasticity changes with ventriculomegly.Gen Neurosurg 1980; 53:173-179.41. Tamaki N, Kusunoki T, Wakabayashi T,Matsumoto S. Cerebral hemodynamics innormal-pressure hydrocephalus. Gen Neurosurg1984; 61:510-514.42. Ingvar DH, Schwartz MS. The cerebralblood flow in low pressure hydrocephalus.In: Lundberg N, Ponten U, Brock M, eds.Intracranial pressure. Vol 2. New York, NY:Springer-Verlag New York, 1975; 153-156.Volume 198 #{149} Number 2 Radiology #{149} 529