Normal-Pressure Hydrocephalus - International Hydrocephalus ...
Normal-Pressure Hydrocephalus - International Hydrocephalus ...
Normal-Pressure Hydrocephalus - International Hydrocephalus ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
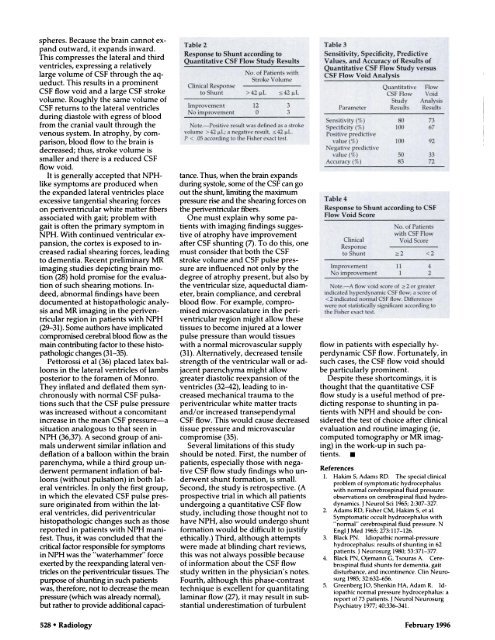
spheres. Because the brain cannot expandoutward, it expands inward.This compresses the lateral and thirdventricles, expressing a relativelylarge volume of CSF through the aqueduct.This results in a prominentCSF flow void and a large CSF strokevolume. Roughly the same volume ofCSF returns to the lateral ventriclesduring diastole with egress of bloodfrom the cranial vault through thevenous system. In atrophy, by comparison,blood flow to the brain isdecreased; thus, stroke volume issmaller and there is a reduced CSFflowvoid.It is generally accepted that NPHlikesymptoms are produced whenthe expanded lateral ventricles placeexcessive tangential shearing forceson periventriculam white matter fibersassociated with gait; problem withgait is often the primary symptom inNPH. With continued ventricular expansion,the cortex is exposed to increasedradial shearing forces, leadingto dementia. Recent preliminary MRimaging studies depicting brain motion(28) hold promise for the evaluationof such shearing motions. Indeed,abnormal findings have beendocumented at histopathologic analysisand MR imaging in the periventricularregion in patients with NPH(29-31). Some authors have implicatedcompromised cerebral blood flow as themain contributing factor to these histopathologicchanges (31-35).Pettonossi et al (36) placed latex balloonsin the lateral ventricles of lambsposterior to the fomamen of Monmo.They inflated and deflated them synchronouslywith normal CSF pulsationssuch that the CSF pulse pressurewas increased without a concomitantincrease in the mean CSF pressure-asituation analogous to that seen inNPH (36,37). A second group of animalsunderwent similar inflation anddeflation of a balloon within the brainparenchyma, while a third group underwentpermanent inflation of balloons(without pulsation) in both latemalventricles. In only the first group,in which the elevated CSF pulse pressureoriginated from within the latemalventricles, did periventricularhistopathologic changes such as thosereported in patients with NPH manifest.Thus, it was concluded that thecritical factor responsible for symptomsin NPH was the “waterhammem” forceexerted by the reexpanding lateral yentricleson the penventricular tissues. Thepurpose of shunting in such patientswas, therefore, not to decrease the meanpressure (which was already normal),but rather to provide additional capacitance.Thus, when the brain expandsduring systole, some of the CSF can goout the shunt, limiting the maximumpressure rise and the shearing forces onthe periventriculam fibers.One must explain why some patientswith imaging findings suggestiveof atrophy have improvementafter CSF shunting (7). To do this, onemust consider that both the CSFstroke volume and CSF pulse pressureare influenced not only by thedegree of atrophy present, but also bythe ventricular size, aqueductal diameter,brain compliance, and cerebralblood flow. For example, compromisedmicrovasculatume in the penventricularregion might allow thesetissues to become injured at a lowerpulse pressure than would tissueswith a normal microvascular supply(31). Alternatively, decreased tensilestrength of the ventricular wall or adjacentparenchyma might allowgreater diastolic reexpansion of theventricles (32-42), leading to increasedmechanical trauma to theperiventriculan white matter tractsand/or increased transependymalCSF flow. This would cause decreasedtissue pressure and microvasculancompromise (35).Several limitations of this studyshould be noted. First, the number ofpatients, especially those with negativeCSF flow study findings who underwentshunt formation, is small.Second, the study is retrospective. (Aprospective trial in which all patientsundergoing a quantitative CSF flowstudy, including those thought not tohave NPH, also would undergo shuntformation would be difficult to justifyethically.) Third, although attemptswere made at blinding chant reviews,this was not always possible becauseof information about the CSF flowstudy written in the physician’s notes.Fourth, although this phase-contrasttechnique is excellent for quantitatinglaminar flow (27), it may result in substantialunderestimation of turbulentflow in patients with especially hyperdynamicCSF flow. Fortunately, insuch cases, the CSF flow void shouldbe particularly prominent.Despite these shortcomings, it isthought that the quantitative CSFflow study is a useful method of predictingresponse to shunting in patientswith NPH and should be consideredthe test of choice after clinicalevaluation and routine imaging (ie,computed tomography or MR imaging)in the work-up in such patients.UReferences1. Hakim 5, Adams RD. The special clinicalproblem of symptomatic hydrocephaluswith normal cerebrospinal fluid pressure:observations on cerebrospinal fluid hydrodynamics.J Neurol Sci 1965; 2:307-327.2. Adams RD. Fisher CM, Hakim 5, et al.Symptomatic occult hydrocephalus with“normal” cerebrospinal fluid pressure. NEnglJ Med 1965; 273:117-126.3. Black PN. Idiopathic normal-pressurehydrocephalus: results of shunting in 62patients. I Neurosurg 1980; 53:371-377.4. Black PN, Ojemann G, Tsouras A. Cerebrospinalfluid shunts for dementia, gaitdisturbance, and incontinence. Clin Neurosurg1985; 32:632-656.5. Greenberg JO, Shenkin HA, Adam R. Idiopathicnormal pressure hydrocephalus: areport of 73 patients. J Neurol NeurosurgPsychiatry 1977; 40:336-341.528 #{149} Radiology February 1996