Lessons Learned from a Decade of Conflict - Boekje Pienter
Lessons Learned from a Decade of Conflict - Boekje Pienter
Lessons Learned from a Decade of Conflict - Boekje Pienter
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Lessons</strong> <strong>Learned</strong> <strong>from</strong> a <strong>Decade</strong> <strong>of</strong> <strong>Conflict</strong>A Supplement toOctober 2008 JEMS sponsored byNorth American Rescue Inc.
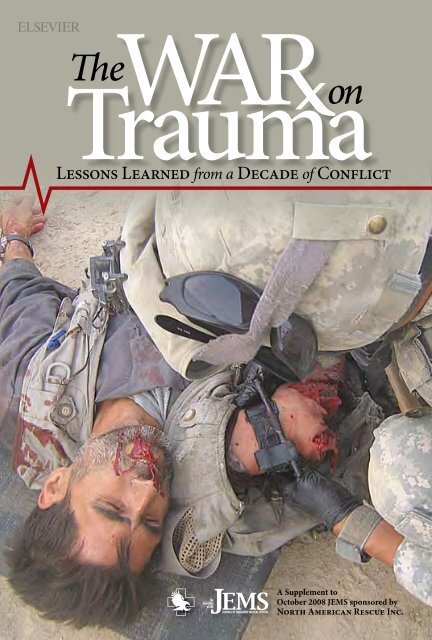
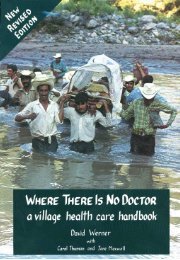
Photos courtesy SSG Fredrick GoldackerAbout the Cover:A U.S. Armymedic appliesa C-A-Ttourniquetto an Afghansoldier afteran improvisedexplosive device(IED) detonated while he was onpatrol. Tourniquet use is having asignificant impact on the number <strong>of</strong>lives being saved on the battlefieldand they are now being placed inservice in civilian EMS systems.A Supplement to October 2008 JEMS, sponsored by North American Rescue Inc.3IntroductionForward Thinking RequiredBy A.J. Heightman, MPA, EMT-P411162428<strong>Lessons</strong> <strong>from</strong> the Home FrontTerror in America’s SchoolsThe need to prepare first responders to defend our nation’s childrenBy John Giduck<strong>Lessons</strong> <strong>from</strong> HistoryThe Origins <strong>of</strong> EMS in Military MedicineHow combat medicine influenced the advent <strong>of</strong> today’s EMS modelBy Daved van Stralen, MD<strong>Lessons</strong> <strong>from</strong> the FrontlineFrom the Battlefield to Our StreetsHow combat medicine is revolutionizing civilian prehospital careBy Jeffrey S. Cain, MD<strong>Lessons</strong> in Evidence-Based ProtocolsTourniquet First!Safe & rational protocols for prehospital tourniquet useBy Peter P. Taillac, MD, FACEP, &Gerard S. Doyle, MD, MPH<strong>Lessons</strong> in Human Performance FactorsThe Stress ParadoxUnderstanding how the body’s programming can inhibitthe performance <strong>of</strong> first respondersBy Bruce K. Siddle<strong>Lessons</strong> <strong>Learned</strong> <strong>from</strong> a <strong>Decade</strong> <strong>of</strong> <strong>Conflict</strong>Vice President/PublisherJeff Berend j.berend@elsevier.comEditorial DirectorA.J. Heightman a.j.heightman@elsevier.comAdvertising DirectorJudi Leidiger jleidiger@adreturn.comSupplement EditorCindy Devone c.devone@elsevier.comDisclosure <strong>of</strong> Author Relationships: Authors have been asked todisclose any relationships they may have with commercial supporters<strong>of</strong> this supplement or with companies that may have relevance to thecontent <strong>of</strong> the supplement. Such disclosure at the end <strong>of</strong> each articleis intended to provide readers with sufficient information to evaluatewhether any material in the supplement has been influenced by thewriter’s relationship(s) or financial interests with said companies.The War on Trauma is a supplement sponsored by North AmericanRescue Inc. and published by Elsevier Public Safety, 525 B Street,Ste. 1900, San Diego, CA 92101-4495; 800/266-5367 (Fed. ID#13-935377). Copyright 2008 Elsevier Inc. No material may bereproduced or uploaded on computer network services without theexpressed permission <strong>of</strong> the publisher. Subscription information: Tosubscribe to an Elsevier publication, visit www.jems.com. Advertisinginformation: Rates are available on request. Contact Elsevier PublicSafety, Advertising Department, 525 B Street, Ste. 1900, San Diego,CA 92101-4495; 800/266-5367.2 War on TraumaJournal <strong>of</strong> Emergency Medical Services
You check your rig and preparefor another shift full<strong>of</strong> chest pain and dyspneacalls. But what you don’t know isthat terrorists have walked unabatedinto a middle school nearyour station, forced 1,800 studentsand teachers into the auditoriumand killed several hostages whoresisted their takeover.Minutes later, you get dispatchedto assist police at the scene. Onarrival, you see five dead childrenbeing thrown out school windowsand at least 48 others with gunshotwounds laying on or runningacross the school property.Then you watch in horror as sixpolice <strong>of</strong>ficers approach the schoolin a rescue attempt and terroristsopen fire with a hail <strong>of</strong> bullets <strong>from</strong> automaticassault rifles. As the <strong>of</strong>ficers return fire, the terroristsdetonate improvised explosive devices(IEDs) strategically placed at the front entrance<strong>of</strong> the school, severely injuring the approaching<strong>of</strong>ficers and now causing them to have torescue their own.Suddenly, you’re tasked with performing initialtriage and managing the injuries <strong>of</strong> dozens<strong>of</strong> children and police <strong>of</strong>ficers struggling tostay alive. You’re not currently allowed to carryand use tourniquets for amputations, let aloneuse them to temporarily stem massive bleeding.You’re also not allowed to carry hemostaticdressings because your medical directorsees no need for them. And your protocols onlyallow you to perform pleural decompressionswhen there’s a confirmed tension pneumothoraxpresent.Many <strong>of</strong> these patients and the circumstancesconfronting you fall outside your normalthought and action processes, and way outsideyour EMS system’s protocols and procedures.So, what do you do?If you think this scenario can’t happen inyour community, put this special supplementto JEMS aside, go to a local elementary school,bury your head in playground sand and pretendthat no one hates you, your governmentand your way <strong>of</strong> life. Because such threats toyour community are real, the subsequentchallenges they present to your organizationmust be dealt with. It requires a lot <strong>of</strong> forwardthinking to prepare for what experts predictwill strike many EMS systems in the future.This supplement brings together experts inthe field <strong>of</strong> military and civilian medicine whopresent new concepts, techniques and productsthat have proven essential to military and tacticalenvironments. Their articles are wovenForward ThinkingRequiredAn Introduction by A.J. Heightman,MPA, EMT-P, Editor-in-Chief, JEMStogether to show why and how military and tacticalmedical advances should be applied to civilian EMS.In Terror in America’s Schools, John Giduck, author<strong>of</strong> Terror at Beslan, focuses on al Qaeda’s promiseto attack America’s schools. He uses his extensiveknowledge <strong>of</strong> the Sept. 1, 2004, Beslan, Russia schoolmassacre to illustrate how easily a similar event couldoccur in the United States.Pointing out how soldiers, police <strong>of</strong>ficers and EMS/fire personnelwere fired on and killed while attempting to rescue the morethan 300 hostages in the school, Giduck stresses the need for EMS/fire responders to go into these battles with a tactical mindset andbe trained to use available weapons if/when they’re trapped andunable to escape terrorist gunfire.In The Origins <strong>of</strong> EMS in Military Medicine, Daved van Stralen,MD, discusses how advances in combat medicine have influencedcivilian EMS. Through this historical overview, van Stralenunderscores why and how EMS providers should look to militarymedicine for developments in trauma care, especially while thiscountry is at war.In From the Battlefield to Our Streets, Jeffrey Cain, MD, a WestPoint graduate who served with the 75th Ranger Regiment andas a battalion physician in Iraq, details how combat medicine isrevolutionizing civilian trauma care. He highlights the military’sTactical Combat Casualty Care guidelines and points out militarylessons learned in hemorrhage control, airway care, penetratingchest injury management, hypothermia prevention, pain managementand rapid patient evacuation.Peter Taillac, MD and Gerald Doyle, MD, present protocols forthe safe and effective use <strong>of</strong> tourniquets by civilian EMS personnelin Tourniquet First! They also venture into uncharted EMSwaters and illustrate how tourniquets can, and should, be used astemporary hemorrhage control devices when you’re overtaxed by aseriously injured patient or a host <strong>of</strong> patients at an MCI.Finally, in The Stress Paradox, Bruce Siddle explores how thehuman body responds (positively and negatively) to stress anddanger, specifically the sympathetic nervous system’s reactionto stress, and how this impacts precision skills, <strong>from</strong> complexmedical procedures to such basic tasks as opening our kits andfinding and deploying supplies.The military, by virtue <strong>of</strong> their experience treating large numbers<strong>of</strong> casualties in a relatively short time period, and under theworst circumstances, once again is leading the way in trauma careinnovations and saving lives we previously thought couldn’t besaved. Progressive EMS systems will not let such developments goignored. Only by studying the lessons being learned daily on thebattlefields <strong>of</strong> the war on terror can we ensure that our trauma careis state-<strong>of</strong>-the-art back home.Elsevier Public Safety War on Trauma 3
Above: A Columbine HighSchool student is rescuedby Lakewood PoliceDepartment SWAT teamleader, Donn Kraemer,during the shooting spreein Littleton, Colo. Manyschool administratorsdidn’t realize thatKleibold and Harrisbrought more than 90explosive devices to theschool; had they beensuccessful in detonatingthem, the incident wouldhave been much worse.Photos AP/KCNC-TV Denver/ STOCK Photo Jim JuricaBy John GiduckAmerica is a nation at war. That’s a reality, not politicalrhetoric. And some <strong>of</strong> the battles in that war are goingto be fought on American soil—in our communities,among our homes and loved ones. Our enemy has promised usthat some <strong>of</strong> those battles will be fought in our schools as ourchildren are captured, tortured and even killed.Yet for all the courage and desire <strong>of</strong> our brave men and womenin military uniform to be at the forefront <strong>of</strong> every battle, they won’tfight such battles exclusively. As I explained inmy book, Terror at Beslan, most, if not all, <strong>of</strong>these battles on American soil will be fought byour law enforcement <strong>of</strong>ficers in conjunctionwith fire/rescue and EMS personnel. 1There are countless terror targets inAmerica. For this reason, we must understandthe targets terrorists are most likely to strikeand develop plans to respond to those attacks.Terror targets can be categorized in a number<strong>of</strong> ways. There are high-, medium- andlow-value strategic targets; high-, mediumandlow-value tactical targets; critical infrastructuretargets; government, law enforcementand military targets; psychological andemotional targets; financial and economictargets; and even symbolic targets. Example:Although they had tremendous psychologicaland economic side effects, the Twin Towerswere primarily symbolic targets to the enemy,representing American economic hegemonythroughout the Muslim world.4 War on TraumaJournal <strong>of</strong> Emergency Medical Services
The Department <strong>of</strong> Homeland Security(DHS), after a lengthy study, recently compileda list <strong>of</strong> 7,000 <strong>of</strong> the most “at risk” sitesfor terror attack. 2 But even that does not beginto acknowledge the many thousands morethat are not only predictably attractive to terrorists,but are the very types <strong>of</strong> targets thathave been attacked by this same enemy countlesstimes around the world.Indeed, in developing its 7,000-site terrortarget list, the DHS included merely 100 <strong>of</strong> thenation’s 3,400 drinking-water facilities thatstore large amounts <strong>of</strong> chlorine gas; if any <strong>of</strong>these facilities were attacked, the gas storedcould result in harm to, or the deaths <strong>of</strong>, 1,000or more people. 2Worse still: There isn’t a single elementary,middle or high school on the list.Why Schools?When anyone with a terrorist mindset isdeciding what type <strong>of</strong> attack to launch, theyhave two essential options: decimation assaultor mass-hostage siege. Decimation assaultsare much more frequent, easier to planand execute, and can usually yield all theresults the terrorists seek with the majority<strong>of</strong> targets. That is, they need only send suicidebombers into a site, or plant explosivesin advance <strong>of</strong> actual detonation. By simplybombing most physical targets,they accomplish this objective;however, because the attacks areusually cleaned up quickly and thebody count is generally low, theseattacks rarely have long-lastingimpact.However, when seeking to causethe greatest psychological, emotionaland lifestyle impact on anentire nation, through the deaths<strong>of</strong> large numbers <strong>of</strong> the most innocent,no target <strong>of</strong>fers terrorists asmuch impact as the killing <strong>of</strong> children.Terrorists have learned that when you takeand hold large numbers <strong>of</strong> children hostage,you, in fact, hold an entire nation hostage.Should terrorists come to America and takemore than 1,000 <strong>of</strong> our children and womenhostage as they did in September 2004 atBeslan Middle School No.1 in southern Russia,all <strong>of</strong> America would hold its collective breaththrough the days <strong>of</strong> that siege, terrified <strong>of</strong> theend result. Holding innocents hostage overlong periods <strong>of</strong> time exponentially increasesthe terror impact on not only the target governmentand the citizens <strong>of</strong> that country, but<strong>of</strong> that nation’s allies.Prolific Terror TargetsWhether decimation assaults or mass-hostage sieges, childrenand schools rate high among the most prolific terror targetsin the world. Israel experienced its own Beslan on May 4,1974, when terrorists took and held 105 children in a school inthe town <strong>of</strong> Ma’a lot, near the Syrian border. When the battle toretake the school was over, 22 children were dead and 56 otherswounded. Another school was taken in Bovennsmilde, Holland,in May 1977. Between 1984 and 1993, more than 300 schoolswere attacked in Turkey, ultimately resulting in the closing down<strong>of</strong> more than 3,000 schools in that country.In the first six months <strong>of</strong> 2006 alone, 204 schools were attackedin Afghanistan, at a time when U.S. and NATO troops held theirpeak control <strong>of</strong> that country. Many more have been attacked sincethen. The number <strong>of</strong> schools being attacked in Pakistan is rising,as well as in Indonesia and Iraq. All <strong>of</strong> the schools in the southernzone <strong>of</strong> Thailand have been closed due to Syrian planned andexecuted attacks on them in recent years. The list goes on.Famed military and law enforcement trainer Lt. Col. DaveGrossman stresses repeatedly that the best predictor <strong>of</strong> futurebehavior is past behavior. From its own past behavior, our enemyhas not only learned the great value <strong>of</strong> children in schools as anoptimal terror target, but has told us what they may yet do to anAmerica that has gone back to sleep since 9/11.Usama bin Laden has stated on prior occasions that before thisjihad is over he will see to the deaths <strong>of</strong> millions <strong>of</strong> Americancitizens, and that children are viable targets. Having been assuredthat the Koran and the Hadith give him the right to exact sucha toll, his statement has been repeated by al Qaeda spokesmenTerrorists have learned that whenyou take & hold large numbers <strong>of</strong>children hostage, you, in fact, holdan entire nation hostage.and exists on Web sites to this day, including the following bybin Laden spokesman Suleiman Abu Ghaith in May 2002: “Wehave the right to kill 4 million Americans—2 million <strong>of</strong> themchildren—and to exile twice as many, and wound and cripplehundreds <strong>of</strong> thousands.”For this reason, there’s much to be derived <strong>from</strong> studying previousattacks. Whether dealing with a strategic-level attack byal Qaeda or similar international terrorist groups, or our ownterror-minded citizens who crave revenge on an uncaring societyfor all the wrongs done to them in their lives—real or imagined—they all come to recognize the value <strong>of</strong> attacking children.When terrorists desire to hold and control an exponentiallygreater number <strong>of</strong> hostages, no population is easier to controlthan children. And when terrorists ultimately seek to kill a largenumber <strong>of</strong> hostages, no one is easier to kill than children.Elsevier Public Safety War on Trauma 5
And schools are the only place in America where large numbers<strong>of</strong> children can be found, relatively unprotected, throughlong periods <strong>of</strong> the year and where schedules are easy to obtainthrough even rudimentary intelligence-gathering efforts (mostare on school Web sites).Learning <strong>from</strong> the PastIn examining even the most recent significant school attacks inAmerica, we can glean valuable lessons. Although the attack onthe elementary school in Beslan may well be the worst situationimaginable, right now our enemy is imagining an attack quite abit worse than even that.Attacks on schools can and will take place on a variety <strong>of</strong> levelsfor both our tactical operators and medic/rescuers. For instance,lower-level school attacks by U.S. children and adults in recentyears may well approximate the homegrown, individually motivatedterrorist attacks al Qaeda is seeking to inspire in every oneColumbine: <strong>Lessons</strong> <strong>Learned</strong>Visit www.JEMS.com for a look back on lessons learned<strong>from</strong> the Columbine school shooting as we near the 10thanniversary <strong>of</strong> the incident. Wayne Zygowicz, EMS chieffor Littleton (Colo.) Fire Rescue, shares his thoughts onhow the incident has changed his agency’s response toactive shooter incidents.<strong>of</strong> the 2 million Muslims in America. Therefore, it’s importantto look at some <strong>of</strong> the more significant recent attacks that ourenemy is even now studying, and looking to outdo.I’ve encountered many school administrators who say theydon’t have to worry about Beslan happening at their schools.They point out that there were more than 100 bombs in that attackand that was possible only because Beslan sat on the edge <strong>of</strong>a war zone. In reaching such a conclusion, however, they’re ignoringthe intel on one <strong>of</strong> the more devastating attacks Americahas already experienced.Most people in our country are familiar with some aspects <strong>of</strong>the attack on Columbine High School in Colorado, committed byDylan Kleibold and Eric Harris on April 20, 1999. What many donot know: In that attack, two untrained teenage assaulters manufacturedand transported more than 90 explosive devices to the school.The majority <strong>of</strong> the bombs did not explode, due to an error theymade in the use <strong>of</strong> a certain type <strong>of</strong> clock as a timed detonator.And while most school administrators and teachers don’tknow what that mistake was, they must recognize that studentswho contemplate launching a Columbine-style attack—and terroristsconsidering the same thing—do know what Kleibold andHarris did wrong. Each <strong>of</strong> them will ensure the same mistake isnot repeated.The body count at Columbine resulted in modificationsin law enforcement response tactics throughout the country.“Active Shooter” responses by police since that time (immediatelyattacking the threat) have resultedin many school attacks being quicklystopped before the shooters could amass aColumbine-level toll in human life. Butnothing about the Active Shooter responseaddresses the holding <strong>of</strong> children hostage.In two <strong>of</strong> the more recent attacks inAmerica, we’ve seen adults entering schools,intent on holding hostages, sexually assaultingyoung girls and ultimately killing studentsin buildings that should be sanctuaries <strong>from</strong>harm. On Sept. 27, 2006, Duane Morrison enteredRoom 206 in Platte Canyon High Schoolin bucolic Bailey, Colo. He held hostage sevenyoung ladies, brutally sexually assaulting all <strong>of</strong>them over a four-hour period, before his threatsto blow up the building forced a law enforcemententry that resulted in the death <strong>of</strong>16-year-old Emily Keyes and himself.One week later, on Oct. 2, 2006, CharlesCarl Roberts walked into a one-roomAmish school building in tiny NickelMines, Pa. He drove everyone out <strong>of</strong> thebuilding but 10 young girls, all <strong>of</strong> whomwere bound by their feet and made to lieshoulder to shoulder beneath the blackboard.He, too, sexually abused childrenbefore killing them.Shortly after the arrival <strong>of</strong> the PennsylvaniaState Police (PSP), he began shooting.At the sound <strong>of</strong> the first shot, PSPtroopers raced to the building and attemptedimmediate entry, where they encounteredlumber barricades Roberts had nailed over thedoors and windows. The police fought desperatelyto gain entry; one state trooper tore outall his fingernails trying to rip wood away.Breaching the building took a little more thantwo minutes—rapid entry in light <strong>of</strong> the fortificationsencountered. But Roberts neededmerely eight seconds to discharge 13 roundsinto the 10 girls, killing five and leaving one in avegetative state.Seung-Hui Cho had the advantage <strong>of</strong> seeingall <strong>of</strong> this in the half-year prior to his attackon the Virginia Tech campus. And in each attack,the tactics and fortifications <strong>of</strong> the assailantwere better than the ones that had comebefore. At the Bailey, Colo., school attack,Morrison had packed the space between thedoor and himself—30 feet across the room—with all <strong>of</strong> the desks and chairs. He held EmilyKeyes in front <strong>of</strong> him as a human shield whilepolice fought their way through the jumbledfurniture, not daring to take a thin-marginshot <strong>from</strong> such a distance. One week later,Roberts’ fortifications in the small schoolhousewere even better.6War on TraumaJournal <strong>of</strong> Emergency Medical Services
Cho improved on them both during his attackat Virginia Tech. He selected Norris Hallin part because it was one <strong>of</strong> the few remainingbuildings whose doors had the old-stylehinged swing bars, rather than the solid pushbars found in buildings today. This enabledhim to simply loop chain through the bars andsecure them with inexpensive locks, therebyeasily trapping his prey in the building, as wellas fortifying it against law enforcement entry.As with the two prior school incidents, lawenforcement fought to gain entry, ultimatelyblowing the deadbolt lock out <strong>of</strong> another doorwith a shotgun slug. Contrary to news reports,<strong>from</strong> the moment <strong>of</strong> the breaching round, ittook the entry teams merely 38 seconds to maneuverthrough a large and complex machineshop, race around a corner, down a short halland into a recessed staircase (while a secondteam raced all the way down a 40-yard corridorto the next set <strong>of</strong> stairs) and reach thesecond floor, forcing Cho to take his own life.Even then, the carnage was so great the policewould not initially accept there had beenonly one shooter. While attempting to securethe students against further attack, police andtwo tactical medics began providing medicalcare to the dozens <strong>of</strong> affected students andteachers. In all, 30 innocent people perished,with another 25 suffering wounds and injuries;this, in addition to the two lives Cho tookearlier that morning in a distant dormitory.Beslan Stands AloneMy own experience with school attacks isgreater than I would like it to be. Two <strong>of</strong> ourorganization’s founding directors led the investigationinto Columbine; I know dozens <strong>of</strong> thepolice and SWAT team members and leaderswho responded to that attack.I was asked to conduct an assessment <strong>of</strong> thelaw enforcement response immediatelyafter the siege ended at the Bailey,Colo., school. I know two <strong>of</strong>the Pennsylvania StatePolice SRT team members and leaders at Nickel Mines, and hadcoincidentally been nearby training the York City SWAT Teamwhen the shooting took place, enabling me to contact the operatorsto understand what they had confronted. And when VirginiaTech happened, I was asked to travel there immediately with asmall team <strong>of</strong> top law enforcement pr<strong>of</strong>essionals to begin an indepthassessment.But as bad as Norris Hall was, it was not the worst either I, orthe world, had ever seen, for the tragic title <strong>of</strong> “the worst school attack”belongs to Beslan, Russia. The time I had spent working andstudying in Russia every year for almost two decades—includingannual time spent over 13 years with Russian Airborne and SpecialForces units—proved invaluable to helping me gain entry intothe school immediately after the battle ended. I debriefed dozens<strong>of</strong> soldiers, government <strong>of</strong>ficials and townspeople.Beslan FactsAt Beslan, 49 terrorists took more than 1,200 people, mostlywomen and children, hostage at approximately 9 a.m. on Sept. 1,2004 (the first day <strong>of</strong> school in Russia, when families typically accompanyschoolchildren to school). Hostages were brutalized inways almost unspeakable. Children were beaten savagely; olderteenage girls were raped, some repeatedly, through the days <strong>of</strong>the siege. Two fathers were murdered immediately in the gymwhere the hostages were originally massed, and another 21 <strong>of</strong> thelargest adult males and older teenage boys were shot to death.The Beslan terrorists brought upward <strong>of</strong> 200 explosives intothe school. Many were placed in the gym where the majority <strong>of</strong>hostages were held throughout the siege. Others were spreadthroughout the school, with numerous booby traps set in thehallways. Other groups <strong>of</strong> children were held in separate roomsamidst bombs designed to kill them when a rescueattempt ultimately came.Photo AP / ivan SekretaravDuring the Beslan siege, soldiers,medics and even townspeople joinedin the rescue effort, which quicklyoverwhelmed available forces.Elsevier Public Safety War on Trauma 7
Aida Sidikova, a girl held hostage during theBeslan school siege escapes momentarily, onlyto return to the school in confusion. Terroristsultimately killed more than 300 hostages.Photo courtesy John GiduckThree PKM belt-fed machine guns were set up in the 80-yardlongmain corridors on the first and second floors. These corridorswere barely 8 feet wide, similar to the tight confines <strong>of</strong> thehallway in Norris Hall at Virginia Tech.When exploding bombs in the gym forced a rescue attempttwo-and-a-half days later, terrorists stood children up in windowsas human shields while they fired indiscriminately at bothfleeing hostages and rescuers racing toward the school. The RussianSpecial Forces couldn’t return fire at the terrorists for fear<strong>of</strong> hitting the children. This was repeated inside the buildingthroughout the 10-plus-hour gun battle to retake the school.In the northern courtyard, the military moved up two BTR80s (wheeled armored personnel carriers) to provide cover foradvancing teams, and to protect wounded and rescued hostageswhile being evacuated. Avenues into the southern courtyardwere too narrow to permit vehicles that would have provided anybenefit at all, leaving hostages and soldiers alike to fend for themselvesout in the open.Inside the building, the Special Forces had to contend withseveral series <strong>of</strong> fighting positions staggered throughout the longcorridors, tripwires and booby traps, and the three belt-fed machineguns in hard fighting positions with children stood up beforethem to slow down the attack <strong>of</strong> the soldiers.Even as the battle raged in different parts <strong>of</strong> the school, many<strong>of</strong> the more than 700 wounded hostages were evacuated underfire. With more than 300 additional hostages ultimately dying,the stress and demands were overwhelming on the soldiers,medics and even townspeople to provide critical lifesaving careto all <strong>of</strong> those affected by bullets, bombs, ceiling collapses in severalplaces (including the entire gym ro<strong>of</strong> caving in) and fire. Inaddition, 21 elite Special Forces soldiers were killed and morethan 60 wounded.Preparing for the WorstThe recent attacks on U.S. schools provideimportant realizations about the need to preparefor such attacks. The mass chaos and tacticalneeds presented by these major incidentsyields a valuable model for our preparednessand training. If studied and applied, the lessonslearned should ultimately ensure those liveswere not lost in vain.The one consistency with all people possessed<strong>of</strong> a terror mindset is the desire for attention, theneed to be made famous as a result <strong>of</strong> the horrorthey perpetrate. To garner that level <strong>of</strong> devotionby the news media, they need accomplish onlyone thing: outdo the last, biggest body count <strong>of</strong>innocent victims.That means that the next Kleibold and Harrisare putting together a plan to kill more peoplethan died at Columbine. To achieve that, theyneed better fortifications to slow the police responseand entry into the building. They’restudying the attacks that have come before anddevising tactics they believe will be impossiblefor law enforcement to overcome.For that reason, it’s important U.S. emergencyresponders recognize the value in preparing forthe worst thing that could happen, making theBeslan model <strong>of</strong> tremendous value. In lookingat both Beslan and the recent attacks onAmerican schools by our own societally manufacturedpredators, the conclusion is inescapablethat there are only two things that will stopthe next attack and save the lives <strong>of</strong> the targetedvictims: brave men and women with guns, andbrave men and women with the medical skillsto save the wounded under combat conditions.Thus, the single most crucial aspect <strong>of</strong> preparednessfor all <strong>of</strong> America’s tactical operators,firefighters and paramedics is the need to trainto rescue and to kill (if necessary) to save lives.This will be a tough concept for many agenciesto accept, but it must be considered, especiallysince fire and EMS personnel may be the first toarrive at these incidents and the first to encounterterrorists intent on killing them and anyoneelse who gets in their way.At Beslan, rescuers spent all day racingtoward the school, across open ground, tobring stretchers full <strong>of</strong> much-needed bullets,weapons, water and medical kits to the beleagueredtroops inside, only to turn around andrace back out across those same killing fieldscarrying the wounded on stretchers. Many justcarried children in their arms, or dragged adultsby limbs across the yards to safety. Exhausted,these teams needed others to step into their rolewhile they sought brief respite. Others weresimply shot down trying to shield children withtheir bodies.8 War on TraumaJournal <strong>of</strong> Emergency Medical Services
In this era <strong>of</strong> terrorism, all personnel must notonly hone their abilities to take life to save the innocent,but also save life and rescue the woundedunder fire. Just as importantly, our fire/rescue andEMS personnel must go into these battles witha tactical mindset and knowledge to ensure notonly the safety <strong>of</strong> the wounded, but <strong>of</strong> themselvesand those around them.New Skills NeededTo deal with both the tactical (combat) andcombat casualty care (first aid under fire) aspects<strong>of</strong> the battles yet to come to America,law enforcement operators and tactical medicsalike must possess the same capabilities. If theydon’t, people will die. Medical pr<strong>of</strong>essionalsmust realize the differences between first aidand tactical combat casualty care (TCCC).In a combat environment, priorities change.Stopping hemorrhage through the use <strong>of</strong> clottingagents and tourniquets is critical; other articlesin this supplement address this in detail.The first personnel on scene to assist victims<strong>of</strong> gunshots and bombs must be able to stophemorrhage, invasively open breathing passages,treat collapsed lungs and evacuate thewounded, <strong>of</strong>ten through walls and out windows.The same “tactics” can benefit law enforcementoperators who may have to advancedown hallways, straight into the face <strong>of</strong> automaticweapons fire.Police must be able to use these same skillsto treat the hostages, their teammates andthemselves, because TCCC is all about stayingin the fight. Though the combat capabilityand synergy <strong>of</strong> actual tactical medics must besubstantial, both fire/rescue and EMS personnelmust also be able to pick up any weaponand either load or unload it, relieve a jam andreturn it to combat effectiveness. In a gun battlewith a committed enemy and innocent victimsin between, no one can afford the luxury<strong>of</strong> job specialization. All personnel must beable to deal with re-supply and evacuation <strong>of</strong>wounded, and all personnel must be able toIn the new era <strong>of</strong> terrorism, EMS personnel must be trained in combat tactics, andpolice must be trained in superior first aid. Such situations can produce high numbers<strong>of</strong> casualties among citizens and police, quickly overwhelming tactical medics. AtVirginia Tech’s Norris Hall, two tactical medics would have had to treat 55 people ifthe police had not been sufficiently trained to assist in providing trauma care.Photo AP / The Roanoke times, Alan Kimuse the same devices and tactics to do both while keeping theirhands free to provide their own suppression fire.In short, tactical medics and law enforcement personnel alikemust be able to shoot their way into and out <strong>of</strong> a building, andacross open ground. And police <strong>of</strong>ficers must not be afraid tobreak traditional rules <strong>of</strong> emergency care. Lt. Anthony Wilson,commander <strong>of</strong> the Blacksburg, Va., SWAT team that led the assaulton Norris Hall, says:“When it comes to kids,Our fire/rescue & EMS personnel mustgo into these battles with a tacticalmindset & knowledge to ensure notonly the safety <strong>of</strong> the wounded, but <strong>of</strong>themselves & those around them.the rules all change.No matter what you’vebeen told as a cop, ifit’s a child and you haveto stick your glovelesshands into that littlebody to stop bleeding,you’re going to do it. Ifyou have to put yourmouth on that littlekid’s mouth to breathelife into him, you’ll do itwithout hesitation.”The wheel need not be reinvented; America’s conventionalcombat arms units and our Special Operations Forces provide amodel for preparing fire/EMS/law enforcement personnel to respondto the next Columbine, Norris Hall or Beslan.Specifically, there must be three essential evolutions in the training:1At the top are the medics assigned to SWAT. Just as our mostelite counter-terror hostage-rescue units have highly trainedmedics who deploy with every entry team, specialized tacticalmedics must also undergo substantial training with the SWATteams to which they’re assigned. This will cost very little. Medicsmust be willing to undergo SWAT training with their assignedunits, and hold themselves to the same physical standards. Theywill need equipment similar to their police teammates in the wayElsevier Public Safety War on Trauma 9
<strong>of</strong> body armor, uniform and clothing, but little else. They mayeven be considered an added resource for extra ammunition, asthey can carry heavier loads than the operators who must moveat lightning speed in tight confines. Whether these medics shouldbe armed is a matter for the individual departments, and may bedetermined by pre-existing policies, and, in some cases, state law.Having at least one sidearm for each medic, however, would likelyresult in the lives <strong>of</strong> police, medics and innocent victims beingsaved at some point.2The next level <strong>of</strong> advancement in training and ability is increasedtactical awareness and understanding for all fire/rescue and EMS personnel. Although these individualsdon’t need the expertise <strong>of</strong> the tactical medics, they must be aware<strong>of</strong> what tactics patrol <strong>of</strong>ficers employ when entering a building,clearing and securing areas, handling hostages and woundedsuspects, withdrawing under fire, and working in small teams.This will greatly enhance the ability <strong>of</strong> the two groups to operatetogether in active shooter situations, particularly in those jurisdictionswhere it’s likely patrol will arrive ahead <strong>of</strong> SWAT. Thesemedical pr<strong>of</strong>essionals will not require extreme tactical knowledge,but they will need sufficient knowledge to ensure they canget their medical expertise to where it’s needed, while under fire,and without interfering with those engaged in combat. These pr<strong>of</strong>essionalscan also receive all <strong>of</strong> the training they need <strong>from</strong> thevery departments they will be assisting.3And finally, just as the medics must be trained in combattactics by the police, the police must also be trained in superiorfirst aid by the medics. Police must be better at renderingaid to their law enforcement comrades, themselves and thevictims. In a battle environment where police can expect to suffercasualties at the rate <strong>of</strong> one cop for every five terrorists shot (as theRussian special forces do), in addition to dozens (and even hundreds)<strong>of</strong> dead and dying victims, medics assigned to police willbe overwhelmed. At Norris Hall, there were two tactical medicswho would have had to treat 55 people if the police had not beensufficiently trained.To develop this evolution in training does not require largebudgets for equipment or six-figure DHS grants. What it doesrequire, however, is the willingness to train, and a desire to bebetter than we are now. In advancing the skill level in the twocritical areas <strong>of</strong> tactics and medicine-under-fire, we can, onceagain, turn to the model <strong>of</strong> the Army Special Forces, in which thefirst duty <strong>of</strong> each specialist is to teach his expert skill set to all <strong>of</strong>the other members <strong>of</strong> the team, so that any one team member canstep in and do another’s job if that person is wounded or killed.Police <strong>of</strong>ficers, paramedics, EMS personnel and firefighterscan ill afford a different attitude in the battles America is yet t<strong>of</strong>ight on her own soil. While some advances in equipment will behelpful, the real requirements are dedication, discipline and awillingness to commit time and effort.For these reasons, both North American Rescue Inc. (NAR)and the Archangel Group Ltd. have been working to prepareAmerica’s warriors to be able to do just that: kill and rescue. Since9/11, Archangel has trained thousands <strong>of</strong> police, soldiers, andstate and federal agents in unprecedented and innovative waysto conduct these battles against a committed, well-prepared anddeadly enemy.At the same time, NAR has been workingwith the most elite Special Operations soldiersand sailors who are conducting operations inour overseas combat zones to provide the mostadvanced, efficacious casualty care and extractiontechniques for combat at home—techniquesthat represent an enormous evolutionin casualty care <strong>from</strong> early conventional firstaid and CPR.Together, these organizations have forged aset <strong>of</strong> common skills that have joint tactical andmedical applications. No police <strong>of</strong>ficer, SWAToperator, firefighter or paramedic can be withoutthis skill set. New, and inexpensive, evacuationand medical equipment is now availablethat every police <strong>of</strong>ficer, soldier, medic, EMSpr<strong>of</strong>essional and firefighter can benefit <strong>from</strong>.Cutting-edge training in TCCC is nowavailable to everyone. No longer is this equipmentand training limited only to our elitemilitary Special Operations Forces. Nor canwe afford for it to be, because police <strong>of</strong>ficers,paramedics and firefighters are the ones wewill be turning to when this enemy returns.The enemy has promised us the deaths <strong>of</strong>millions <strong>of</strong> American citizens—including ourown children—before this war is over. Theonly way to prevent them <strong>from</strong> reaching thatgoal is our ability to kill them and rescue andresuscitate our own; for our enemy will allowus no other solution.John Giduck is a senior consultant with the ArchangelGroup (www.antiterrorconsultants.org), an agencythat provides training to U.S. law enforcement,government agencies and military. He has a lawdegree and a master’s degree in Russian studies, andhas worked with several Russian special forces units.He authored Terror at Beslan and co-authoredthe newly released The Green Beret in You:Living with Total Commitment to Family,Career, Sports and Life. Currently he’s finishinga doctoral dissertation on the global expansion <strong>of</strong>radical Islam. Giduck has reported no conflicts <strong>of</strong>interest related to the sponsor <strong>of</strong> this supplement,North American Rescue.Editor’s Note: The author’s book, Terror atBeslan: A Russian Tragedy with <strong>Lessons</strong>for America’s Schools, provides a detailedaccount <strong>of</strong> the events at the Beslan school siege.Learn more at:www.antiterrorconsultants.org/terror_beslan.htm.References:1. Giduck J: Terror At Beslan: A Russian Tragedywith <strong>Lessons</strong> for America’s Schools. ArchangelPublishing Group Inc.: Golden, Colorado, 2005.2. Ahlers MM: “Agency says 7,000 sites at ‘high risk’<strong>of</strong> terrorist attack.” CNN.com News Report, June21, 2008.10 War on TraumaJournal <strong>of</strong> Emergency Medical Services
Photo <strong>of</strong>fice <strong>of</strong> medical history/Surgeon GeneralWWIIWWIPhoto <strong>of</strong>fice <strong>of</strong> medical history/Surgeon General“It is appropriate that experienceduring unavoidable ‘epidemics <strong>of</strong>trauma’ be exploited in improvingour national capability to providebetter surgical and medical care forour citizens. ”Spurgeon Neel,Colonel, Medical Corps, U.S. Army 1Though EMS as medical treatment <strong>of</strong> apatient prior to and during transportationto the hospital may have roots datingback centuries, it is only since Napoleon’sEuropean campaigns that we can draw a directline <strong>from</strong> his system for moving combat casualtiesto today’s EMS. Napoleon’s physician,Dominique-Jean Larrey, developed a systemspecifically for transportation <strong>of</strong> battle casualties(the “flying” ambulance), which was introducedinto the U.S. Army during the Civil War.Photo APVietnamIraq &AfghanistanPhoto courtesy SSG Fredrick GoldackerBy Daved van Stralen, MDIn the trench warfare <strong>of</strong> WWI, the U.S. Armyassigned nonphysicians to the trenches for treatment<strong>of</strong> casualties. In WWII, these first aid menentered combat, becoming the corpsmen andcombat medics in service today.During WWII, the Army also introducedair transport <strong>of</strong> the injured; this developmentwas followed by helicopter transport directly<strong>from</strong> the scene <strong>of</strong> injury to the hospital in theKorean <strong>Conflict</strong> and the Vietnam War. Asalluded to in Col. Neel’s 1968 statement, each<strong>of</strong> these advances in prehospital care came<strong>from</strong> the epidemic <strong>of</strong> trauma that occursduring military combat.Elsevier Public Safety War on Trauma 11
From the current epidemic <strong>of</strong> trauma, the Global War on Terrorin Iraq and Afghanistan, military combat medicine has furtherdefined and validated Tactical Combat Casualty Care (TCCC) 2 withtreatment guidelines for the use <strong>of</strong> tourniquets, hemostatic agents,needle chest decompression, and hypotensive resuscitation. Thissupplement presents some <strong>of</strong> what we’ve learned, which, in Col.Neel’s words, will improve “our national capability to provide bettersurgical and medical care for our citizens.”The U.S. military constantly strives to improve the medical careprovided to combat casualties with the indirect result <strong>of</strong> improvementsto civilian emergency medical care over the past two centuries.In this article, I’ll explore the development <strong>of</strong> emergency care<strong>from</strong> the military experience, including casualty movement, providingemergency care to the injured soldier at the point <strong>of</strong> wounding,use <strong>of</strong> aeromedical evacuation, clinical advancements in treatmentand medical equipment, as well as critical decision-making skills.The Origins <strong>of</strong> EMSNapoleon used ambulances, or what’s known today as ourmilitary field hospital, during his military campaigns, but armyregulations kept them one league (about 3 miles) away <strong>from</strong> thearmy and several hours <strong>from</strong> wherethe battle occurred.Combat veterans working withveterans <strong>of</strong> major emergenciesbegan to influence the systematicapproach public safety agencies(police, fire, EMS) used whenworking in hazardous or hostileenvironments.Larrey began to recognize thatthis distance, along with the difficulty<strong>of</strong> moving the wounded,delayed treatment and increasedthe mortality rate. During a retreatat one battle, Larrey marveled athow fast the “flying” horse-drawnartillery could move and thought<strong>of</strong> developing a “flying ambulance”(ambulance volante) to move thewounded <strong>from</strong> the battlegroundto the ambulance field hospital. Helater designed a specialized horsedrawncart to transport the sick and injured, which graduallyevolved into our modern ambulance. 3Flying ambulances reached America in 1862, when Dr. JonathanLetterman, a medical director in the Union Army, introduced themas a means to transport wounded soldiers. Prior to then, the QuartermasterCorps provided wounded transport as part <strong>of</strong> its duties totransport supplies.After the Seven Days Battle in July 1862, Dr. Letterman transferredthe Quartermaster Corps to the medical staff <strong>of</strong> the UnionArmy and introduced forward first-aid stations at the regimentlevel to administer medical care closer to the battle. Both <strong>of</strong> thesedecisions significantly reduced mortality rates at the Battle <strong>of</strong>Antietam and led the U.S. Congress to establish these procedures asthe model medical procedure for the entire U.S. Army in 1864. 4During World War I, the U.S. Army’s Medical Department assignedtwo enlisted men with first-aid training to each companystationed along the French front lines. These men treated the injuredwhere they lay if they had only a few casualties to treat; otherwise,company litter bearers carried the injured to the company aidstation and then to the battalion aid post. In the trenches, treatmentalso occurred where the man fell, at the point <strong>of</strong> wounding, andincluded control <strong>of</strong> hemorrhage and the splinting <strong>of</strong> fractures.At the company aid station, medical personnelfurther controlled hemorrhage, adjustedbandages and splints, and administered antitetanicserum before moving the injured to thebattalion aid post. From there, the soldier wasevacuated to the ambulance dressing station, thefarthest point forward that ambulances couldreach safely and where battlefield placement <strong>of</strong>dressings and splints could be corrected and thewounded sorted for transport. 5Procedures that began in WWI carried overto WWII. Each company was again assignedtwo first-aid men, called company aid men andlater known as combat medics or corpsmen(Navy medics assigned to a ship or company <strong>of</strong>Marines), but these medics brought emergencycare to the injured soldier at the point <strong>of</strong> wounding—onthe battlefield under exposure to enemyfire. To administer care that was safe for boththe casualty and medic in this hazardous environment,the medic began to synthesize combatdecision making with the principles<strong>of</strong> first aid. Medical aid measuresduring WWII included controllinghemorrhage (including tourniquetuse), applying splints and dressings,administering booster dose <strong>of</strong>tetanus toxoid and initiating chemotherapy(in the form <strong>of</strong> antibiotics,such as sulfa powder sprinkled onwounds and given orally). 6Air Transport <strong>of</strong>Combat CasualtiesCasualty evacuation <strong>of</strong> combatwounded by air has also continuedto improve due to the experience <strong>of</strong> themilitary. In WWII, a Medical Air AmbulanceSquadron was activated at Fort Benning, Ga., inMay, 1942, and began training Army air forceflight surgeons, flight nurses, and enlisted personnelfor duty. 7 In August 1942, because <strong>of</strong> amountain range, the Fifth Air Force used troopcarrier and air transport units to fly 13,000 sickand injured patients to New Guinea to receivefurther medical care.In Korea, as in WWII, the military usedhelicopters to rescue downed aviators, but soonbegan to use them for evacuating combat casualtiesin areas inaccessible to ground vehicles. Thisestablished the effectiveness <strong>of</strong> forward aerialevacuation by means <strong>of</strong> a helicopter and was thebasis for helicopter evacuation in Vietnam.In April 1962, the U.S. Army initiated helicopterevacuation <strong>of</strong> combat wounded on thebattleground with the 57th Medical Detachment(HelAmb). Because <strong>of</strong> the dust kicked up duringoperations in the dry country, they adopted thecall sign DUSTOFF. In a DUSTOFF operation,12 War on TraumaJournal <strong>of</strong> Emergency Medical Services
the patient is flown directly to the medical treatmentfacility best situated for the care required.More similar to civilian EMS was the Army’sFLATIRON Operation <strong>of</strong> the late 1950s. InFLATIRON rescues, the objective <strong>of</strong> the aerialcrash rescue service is to save human life. Itcombines fire suppression, extrication, recovery<strong>of</strong> injured personnel, initial emergency medicaltreatment, and evacuation to an appropriatemedical treatment facility. Neely described theuse <strong>of</strong> FLATIRON rescues by Army teams forcivilian highway accident victims and developedthe concept <strong>of</strong> using helicopters for this missionin routine civilian operations for rural America.Civilian ApplicationsIn the mid-1950s, physicians began to ask whylessons learned for emergency medical treatmentand transportation during WWII and theKorean <strong>Conflict</strong> could not be applied for civilianuse. Drs. J.D. “Deke” Farrington and Sam Banksused these combat lessons to developa trauma training program forthe Chicago Fire Department. Thisprogram later developed into theEMT-Ambulance (EMT-A) course.The American Academy <strong>of</strong>Orthopaedic Surgeons had a previouslyestablished Committee onTrauma (COT), with an interestin prehospital care <strong>of</strong> the injured.In 1967, the COT, chaired by Dr.Walter A. Hoyt and including Dr.Farrington, developed the firstEMT program for ambulance personnelthat trained them to fullyevaluate an injured patient before transportation.This resulted in the 1967 publication <strong>of</strong>“Emergency Care and Transportation <strong>of</strong> theSick and Injured,” which became the standardfor EMT training in the 1970s.During this period, cardiologists identifiedan epidemic plaguing modern society: death<strong>from</strong> myocardial infarction. Before reachingmedical care in the hospital, 40–60% <strong>of</strong> heartattack victims would die. In 1967, Pantridgeand Geddes in Belfast, Ireland, published theirexperience using morphine and lignocaine(lidocaine in the United States) to treat myocardialinfarction in the field, bringing medicalcare to the patient rather than waiting forthe patient to seek medical care. When theydid this, no patient died, which represented areduction <strong>of</strong> the mortality rate <strong>from</strong> about 50%to 0% because <strong>of</strong> one intervention. 8 The ideathat intensive (cardiac) care units could becomemobile led to the creation <strong>of</strong> the mobileintensive care unit (MICU), staffed by mobileintensive care paramedics.In the 1950s and up through the 1970s, combat veterans workingwith veterans <strong>of</strong> major emergencies began to influence the systematicapproach public safety agencies (police, fire, EMS) used whenworking in hazardous or hostile environments. During this period,physicians became more involved in prehospital medical care,which resulted in a synergistic relationship between medicine, publicsafety problem solving and leadership functions.By the 1970s, the term “ambulance” no longer referred to a vehiclefor transporting the sick and injured patient or non-ambulatorypatient. The TV series Emergency! catapulted advances in life supportand prehospital care into American living rooms and inspiredan advanced prehospital care movement that spread across thecountry. Ambulances became specialized patient carriers, and otheremergency workers, such as firefighters and police <strong>of</strong>ficers, startedenrolling in first-aid programs to further their medical training.As the field <strong>of</strong> emergencymedicine began to emerge, thefocus shifted to medical carebefore the diagnosis. “First do noharm” began to give way to thepublic safety creed, “Duty to act;doing nothing is harmful.”Through the 1980s, EMT education merged with paramedic trainingto produce EMS pr<strong>of</strong>essionals who treated trauma and medicalillnesses before and during transportation. Building upon heavyexperience and influence <strong>from</strong> military combat and major civilianemergencies, public safety veterans had developed a means to performunder time constraints, in austere conditions and in a hostileenvironment using what’s describedas “interactive, real-time risk assessment.”9 With these pr<strong>of</strong>essionals, themedical community could now bringadvanced medical care into the publicsafety environment.A Different ApproachThrough the 1970s, medicine focusedon diagnosis first, then treatment,but as the field <strong>of</strong> emergencymedicine began to emerge, the focusshifted to medical care before the diagnosis.“First do no harm” began togive way to the public safety creed,“Duty to act; doing nothing is harmful.”This commonality—the need to intervene before knowing thesituation—linked physicians and nurses to ambulance and rescuesquads with a camaraderie based on response to a shared threat:knowing what to do in the uncertain situation. The collaborationhad a measurable effect. For example, spinal cord injuries changed<strong>from</strong> predominantly complete lesions to predominantly incompletelesions, meaning victims <strong>of</strong> trauma retained some function in theirlower body, solely because <strong>of</strong> prehospital care. Heart attacks alsochanged <strong>from</strong> the dreaded sick call, which was a patient dying <strong>from</strong>myocardial infarction, to a routine, near-boring response.Although medical decision-making skills have advanced slowly,in the past 20 years the military has made great advances in TacticalCombat Casualty Care (TCCC); the use <strong>of</strong> cognitive function in theface <strong>of</strong> uncertainty and the unexpected; and the use <strong>of</strong> decisionmakingprocesses, such as John Boyd’s OODA Loop (Observe-Orient-Decide-Act), which provides a way to rapidly make sense <strong>of</strong>a changing and uncertain environment. 10Such advances are centered on the decisions combat medics mustmake to stop bleeding, support the respiratory system, prevent infectionand transport the wounded as quickly as possible—decisionsthat our EMS providers routinely face as well.Elsevier Public Safety War on Trauma 13
It makes sense for us to ask ourselves, “What approaches can wetake <strong>from</strong> medics in Iraq and Afghanistan?”Physical TacticsOther articles within this supplement detail some <strong>of</strong> the combatmedical treatments that are applicable to civilian EMS. Briefly, theseinclude:1Use<strong>of</strong> Tourniquets:The most common cause<strong>of</strong> preventable death onthe battlefield is exsanguination<strong>from</strong> extremity wounds, which issignificantly diminished by the use<strong>of</strong> a tourniquet. The U.S. Army’sInstitute <strong>of</strong> Surgical Research (USAISR)notes that the ideal tourniquet should be light, durable, easilyapplied, and capable <strong>of</strong> occlusion <strong>of</strong> arterial blood flow (cost is alsoa factor). With numerous tourniquets on the market, the CombatApplication Tourniquet (C-A-T) (shown above) was selectedas the tourniquet <strong>of</strong> choice by the Army for use by deployedindividuals. The American College <strong>of</strong> Surgeons Committee onTrauma (PHTLS 6th Edition) no longer recommends elevation<strong>of</strong> the limb or use <strong>of</strong> pressure points because <strong>of</strong> insufficient datasupporting these techniques. They recommend use <strong>of</strong> a tourniquetif external bleeding <strong>from</strong> an extremity cannot be controlledby pressure. Direct pressure by hand is problematic in the prehospitalsetting because <strong>of</strong> the difficulty maintaining pressure duringextrication and patient movement.2UseC-A-T®CombatApplication Tourniquet®<strong>of</strong> Hemostatic Agents:USAISR also reports several livessaved in combat using hemostaticagents for bleeding not amenableto tourniquet placement. In May 2008,Combat Gauze and WoundStat wereidentified as the first- and second-linehemostatic agents, respectfully, because<strong>of</strong> successes in animal studies. A gauzeagent, <strong>from</strong> experience, works betterwhere the bleeding vessel is at thebottom <strong>of</strong> a narrow wound tract and is more easily removable atthe time <strong>of</strong> surgery.3ChestDecompression:During the Vietnam War,tension pneumothorax followedexsanguinations as the secondleading cause <strong>of</strong> preventabledeath, accounting for 3–4% <strong>of</strong> fatallywounded combat casualties. 11,12Because <strong>of</strong> the success in treatingtension pneumothorax in TCCCand the rarity <strong>of</strong> complications,USAISR recommended the diagnosis<strong>of</strong> tension pneumothorax and decompression with a 14-gaugex 3.25-inch needle if the casualty has unilateral penetrating chesttrauma or blunt torso trauma and progressive respiratory distress.Today, all combatants should possess this skill, and nonmedicsshould now be able to decompress the chest.Cognitive TacticsToday in EMS and public safety, not enoughemphasis is placed on how to teach and developproblem-solving skills when a rule for a particularscenario doesn’t exist or apply, or when rulescompete or conflict with each other.For example, most protocols treat hypovolemiaand severe dehydration viareplenishment <strong>of</strong> blood volume with afluid bolus <strong>of</strong> a balanced salt solution,such as normal saline. For symptomaticheart failure, most protocols wouldrestrict fluids and salt by using a dextrosesolution and may also use a diuretic. In hotregions, it’s quite common to find a patient insymptomatic heart failure and with symptomatichypovolemia and dehydration. Does your systemhave a protocol for administration <strong>of</strong> fluids to afluid-restricted patient?The military and public safety pr<strong>of</strong>essionalsadapt their teams to threat and uncertainty byshifting team structure <strong>from</strong> a rigid, verticalhierarchy in stable situations to a more horizontalhierarchy in unstable situations. This allowsinformation to flow more readily to those whoneed it and makes for shorter chains <strong>of</strong> commandfor decisions and actions, with increasedsafety and effectiveness. Their approach can helpEMS providers increase safety in patient care.In my experience, veterans <strong>of</strong> combat andthose involved in early public safety followedthe rules, but they also identified when a ruledidn’t apply, particularly in an environmentwith uncertainty, time pressure and grave threat.Combat and public safety veterans approachedknowledge-based error situations differently,because evidence-based approaches would not,nor could not, work. When uncertainty existedin a situation, these veterans would focus ona shared objective and problem solve with theresources at hand, requesting additional aidbut accepting the fact that one could not delayproblem solving.Today, with protocols and evidence-basedmedicine, EMS personnel must identify theproper rule when faced with the uncertaintythat occurs between the rules. Teaching and theuse <strong>of</strong> discipline for error, even with due process,influence individuals to find a rule that could fitand, subsequently, <strong>of</strong>fer protection <strong>from</strong> supervisorsand regulators.Emergency personnel must continuallysearch for answers even when the initial solutionappears to work. Learning what works throughaction or an interactive, real-time risk assessmentinvolves a different type <strong>of</strong> decision-makingprocess than algorithms or decision trees.14 War on TraumaJournal <strong>of</strong> Emergency Medical Services
At times, EMS providers may not know withsufficient clarity the situation or the interventionthat will likely work. When this occurs, theymust move toward the objective, identifyingwhat works through action, then reconstructingthe initial problem by reviewing the course <strong>of</strong>events that led to the problem.Photo AP / Jacob SilberbergBoyd’s OODA Loop, developed for air combatduring the Vietnam War, provides a frameworkto problem solve during moments <strong>of</strong> uncertaintyand under grave threat. When the loopis used by a paramedic, one rapidly observes thescene or patient; becomes oriented through theculture <strong>of</strong> the organization, training, education,experience and awareness <strong>of</strong> one’s immediatephysiological limitations; decides what to do bycreating a hypothesis <strong>of</strong> what might work; actson that hypothesis by testing it; then closes theloop by observing the results <strong>of</strong> the test.Learn more by reading Boyd: The Fighter PilotWho Changed the Art <strong>of</strong> War, 10 or visit http://en.wikipedia.org/wiki/OODA_Loop.A Final WordPut simply: Just as the military anticipates combat,public safety personnel continue to anticipatethe possibility <strong>of</strong> an event, or ease with which anevent can occur, while civilians plan for the probability<strong>of</strong> an event, or the likelihood an event willoccur. This contributes to the development <strong>of</strong>individuals who believe in themselves enough tomove forward into a hazardous or hostile environmentto help a fellow human being.Military conflict has provided many <strong>of</strong>today’s EMS tools. Safe transportation <strong>of</strong> thecasualty to the hospital came <strong>from</strong> Larrey’slying ambulance. Treatment <strong>of</strong> a wounded soldierby enlisted men at the point <strong>of</strong> woundingderives <strong>from</strong> trench warfare in WWI throughthe combat medics <strong>of</strong> WWII. Use <strong>of</strong> aircraftto expedite transport <strong>of</strong> the casualty to a hospital came <strong>from</strong>air evacuation procedures developed in WWII, culminating inDUSTOFF and FLATIRON operations by the military in Vietnam.Decision making in the face <strong>of</strong> uncertainty, under threat and in timedependentsituations derives <strong>from</strong> combat and public safetysituations through the 1970s. And today, the War on Terror isproducing better methods and equipment for treating victims <strong>of</strong>severe trauma utilizing TCCC guidelines, which call for the use <strong>of</strong>tourniquets, hemostatic agents, needle chest decompression andhypotensive resuscitation.The U.S. military continues to identify better means <strong>of</strong>providing care to combat casualties. EMS can now learn <strong>from</strong> theseexperiences to improve the capability <strong>of</strong> the EMT and paramedic sothey can provide better EMS care to our citizens. Civilian EMS willbenefit <strong>from</strong> the military’s experiences in treating the severe traumaseen in the War on Terror through advances in medical proceduresand new, innovative equipment that is not only life saving to oursoldiers, but also for treating the “epidemic <strong>of</strong> trauma” seen by ourcitizens.Daved van Stralen, MD, entered the field as an “ambulance man” in 1972and is a former paramedic for the Los Angeles City Fire Department. Hebecame a pediatric intensive care physician and now serves as medicaldirector for American Medical Response, San Bernardino County, Calif.He’s also an assistant pr<strong>of</strong>essor in the Department <strong>of</strong> Pediatrics at LomaLinda University School <strong>of</strong> Medicine and adjunct pr<strong>of</strong>essor <strong>of</strong> EmergencyMedical Care, Crafton Hills College, Yucaipa, Calif. Van Stralen has usedEMS human factors principles in medical care for more than 20 yearsand has worked with Karlene Roberts and Karl Weick. Van Stralen hasreported no conflicts <strong>of</strong> interest related to the sponsor <strong>of</strong> this supplement,North American Rescue.References1. Neel S. “Army aeromedical evacuation procedures in Vietnam:Implications for rural America.” JAMA. 204(4):99–103, 1968.2. Butler FK, Holcomb JB, Giebner SD, et al: “Tactical combat casualty care2007: Evolving concepts and battlefield experience.” Military Medicine.172(11 Suppl):1–19, 2007.3. Ortiz JM: “The revolutionary flying ambulance <strong>of</strong> Napoleon’s surgeon.”U.S. Army Medical Department Journal. October–December:17–25, 1998.4. Tooker J: “Antietam: Aspects <strong>of</strong> medicine, nursing and the Civil War.”Transactions <strong>of</strong> the American Clinical and Climatological Association.118:214–223, 2007.5. Ireland MW. Volume VIII Field Operations. U.S. Government PrintingOffice: Washington, D.C., 1925. http://history.amedd.army.mil/booksdocs/wwi/fieldoperations/frameindex.html.6. Ulio JA, Marshall GC: “1945 Notes on Care <strong>of</strong> Battle Casualties. WarDepartment Technical Bulletin.” Department <strong>of</strong> the Army TechnicalBulletin. 147:234–248.7. Grant DNW. A review <strong>of</strong> air evacuation operations in 1943. The AirSurgeon’s Bulletin. 1(4):1–4, 1944.8. Pantridge JF, Geddes JS: “A mobile intensive-care unit in the management<strong>of</strong> myocardial infarction.” Lancet. 2(7510):271–273. 1967.9. Bea R: “Managing the unpredictable.” Mechanical Engineering. March,2008.10. Coram R: Boyd: The Fighter Pilot Who Changed the Art <strong>of</strong> War. Little,Brown and Company: London, England, 2002.11. Mabry R, McManus. JG: “Prehospital advances in the management <strong>of</strong>severe penetrating trauma.” Critical Care Medicine. 36(7)[Suppl]:S258–S266, 2008.12. McPherson JJ, Feigin DS, Bellamy RF: “Prevalence <strong>of</strong> tensionpneumothorax in fatally wounded combat casualties.” Journal <strong>of</strong> Trauma.60(3):573–578, 2006.Elsevier Public Safety War on Trauma 15
Rapid evacuation and transport <strong>of</strong> non-ambulatorycasualties is just one <strong>of</strong> the areas where civilian EMSagencies can learn more <strong>from</strong> the U.S. military.Photo AP / John MooreBy Jeffery S. Cain, MDIn 1996, a revolutionary concept occurred in military medicine.Until then, battlefield prehospital trauma care followedthe same guidelines developed for the urban U.S. civilianenvironment. But following the October 3, 1993, Battle <strong>of</strong>Mogadishu 1 , the U.S. Special Operations Command sponsoreda study to review how casualty care was conducted. The panel’sconsensus: Conventional civilian medicine was not appropriatefor optimizing casualty care within the tactical environment.To that end, two military physicians with extensive tacticalexperience authored a set <strong>of</strong> guidelines intended to improvecasualty care during tactical operations. 1,2 These TacticalCombat Casualty Care (TCCC) guidelines have been consistentlyreviewed and updated, and are approved by the AmericanCollege <strong>of</strong> Surgeons Committee on Trauma for inclusion in theirPre-hospital Trauma Life Support guidelines. 3A decade ago, we were attempting to applycivilian techniques to the combat environment;today, we’re examining the opposite: Are therelessons learned <strong>from</strong> tactical medicine thatmay improve or facilitate civilian prehospitaltrauma care? Although tactical medicine generallybreaks down care by tactical situation (e.g.,care under fire, tactical field care and tacticalevacuation), this article will examine the issue bycategories <strong>of</strong> trauma interventions.Hemorrhage ControlIsolated extremity hemorrhage remains theprimary cause <strong>of</strong> potentially preventable deathduring combat operations. Casualty care improvements,including better medical devices,guidelines and training down to the individualsoldier level, have focused on decreasing thiscause <strong>of</strong> mortality.Another article within this supplement(“Tourniquet First!” p.24) explores temporaryemergency tactical tourniquets in depth. Forthe purposes <strong>of</strong> this article, it’s simplest to pointout that new tourniquets, and new guidelinesfor early tourniquet use in far-forward casualtycare, are saving lives. 4 The primary tactical tourniquetrecommended by the U.S. Army Institute<strong>of</strong> Surgical Research (USAISR) is the CombatApplication Tourniquet (C-A-T), followed by theSpecial Operations Forces Tactical Tourniquet16 War on TraumaJournal <strong>of</strong> Emergency Medical Services
Delphi®EMTEmergency& MedicalPneumaticTourniquetC-A-T® CombatApplication Tourniquet®(SOF-TT). The Delphi Emergency & MedicalTourniquet (EMT) is the primary pneumatictourniquet used with fixed surgical facilitiesand unit aid stations. 5,6,7Compression bandages are widely usedthroughout the military. Several new commercialproducts represent a significant improvementover older, non-compression style bandages.These newer devices all incorporate a non-adherentbandage in the form <strong>of</strong> an elastic wrap tail.Sequential wrapping <strong>of</strong> the elastic tail generatesa compressive force that, when combined withgauze packing, creates an extremely efficient andeffective pressure bandage. TheEmergency Bandage by First CareProducts was the first <strong>of</strong> thesemodern compression bandages togain widespread acceptance.The Emergency Trauma Dressingby North American Rescue(NAR) represents a significantdesign improvement over olderdevices. 8 This elastic compressionwrap is a tighter weave and generatesgreater compressive force.The wrap’s “Quick Grip” feature(Velcro® enclosures equally spacedalong the wrap) prevents the entirewrap <strong>from</strong> unrolling prematurelyif the wrap is accidentally droppedduring application.Certain wound locations—such as the proximalextremities,axilla, groin, torsoand neck—makeit difficult to controlhemorrhage with directpressure and compressiondressings; tourniquets are alsoineffective in many <strong>of</strong> these areas.Researchers have developed severalnew tools and clinical guidelines to address thiscritical issue. Over the past few years, a number <strong>of</strong>hemostatic agents, in both bandage and powderform, have been developed that actually arrest lifethreateningarterial hemorrhage. 9,10,11The most recent research conducted by both the Army and Navyresearch centers compared more than 10 types <strong>of</strong> hemostatic agentsfor controlling arterial hemorrhage in animal models. One granularproduct (WoundStat, manufactured by Trauma Cure) was found to havea 100% survival rate for subjects with wounds that would otherwisebe fatal. Another product, an improved gauze impregnated with akaolin substance (Combat Gauze, manufactured by Z-Medica), demonstratedgreater than 80% efficacy in independent lab presentationsto the research committee. This product is actually a pro-coagulant thatpromotes blood clotting.These newer hemostatic agents are proving to be both more effectiveand less expensive than those previously approved by the TCCCcommittee. In clinical trials, WoundStat showed the highestclinical efficacy, yet it is a granular-based product,which is problematic to adequatelyapply during tactical operations.Combat Gauze showed the nexthighest efficacy. Both were superiorto the benchmark HemCon andQuikClot. Celox, a granular chitosan-basedagent, also outperformedboth HemCon and QuikClot inboth USAIR and Naval Research LabStudies. Note: This data was taken <strong>from</strong>the “Comparative Testing and Analysis<strong>of</strong> New Hemostatic Agents in LethalInjury Models” presentation, which providespre-published data <strong>from</strong> the NavyResearch Lab and the Army Institute<strong>of</strong> Surgical Research to the TCCCcommittee.ETDCompressionBandageHowever, Celox didn’t performas well as WoundStat or CombatGauze. It’s a lighter weight powderthan WoundStat, which makes applicationto arterial hemorrhage injurydifficult.Based upon the results <strong>of</strong> thesestudies and input <strong>from</strong> combat medicsregarding device preferences, the TCCCcommittee revised its recommendations. Thenewest guideline change is to utilize CombatGauze as the primary hemostatic agent, withWoundStat as the backup or when thewound characteristics are moreamenable to a granular agent.Hemostatic Agents:Combat GauzeWoundStatElsevier Public Safety War on Trauma 17
Although mortality <strong>from</strong> isolatedhemorrhage is not as high inthe civilian community as it is inthe combat environment, it doesexist. Additionally, reducing thepotential morbidity and cost <strong>of</strong>blood transfusion requirements byarresting hemorrhage early, at littleto no risk to the patient or rescuer,is a huge potential benefit.Many EMS agencies have been usinghemostatic agents for some time with excellentresults. The newer agents are far superior to theearlier ones and have come down in price. Whywouldn’t we want to place an additional tool inthe EMT, paramedic and first responder’s toolkitthat requires little training, is cost effectiveand has few side effects?Airway & BreathingHistorically, tension pneumothorax and simpleairway obstruction comprise the second and thirdmost common causes <strong>of</strong> potentially preventablecombat deaths. Penetrating trauma still remainsthe leading mechanism <strong>of</strong> injury during combat.Because the incidence <strong>of</strong> cervical spine injurieswith isolated penetrating trauma is extremely low,obtaining and maintaining C-spine immobilizationis neither practical nor advisable during themajority <strong>of</strong> tactical operations. Instead, soldiersare taught to place unconscious casualties in thelateral recovery position, thus minimizing therisk <strong>of</strong> airway occlusion <strong>from</strong> blood, vomitus ora flaccid tongue. When a casualty is placed in theprone position, the nasal pharyngeal airway representsthe best choice for a simple airway adjunct.Appropriate PrehospitalTourniquetUseBy Jeffery S. Cain, MDFCricKit®Surgical CricothyroidotomyKitFew medical topicsinvoke as much passionatedebate as the use <strong>of</strong>tourniquets to control traumatichemorrhage. Discussionsregarding the role that thispotentially life-saving deviceshould play in the prehospitalenvironment appear to havepolarized the medical communityinto two distinct camps:staunch advocates and absoluteopponents. The truly unfortunateaspect <strong>of</strong> this division: It’sbased largely on unsubstantiatedconjecture regarding theperils <strong>of</strong> tourniquet use.Looking to the literature,we can begin to sort conjecture<strong>from</strong> fact. It’s true that inappropriatelyapplied tourniquetscan cause unnecessary morbidity.It’s also true that associatedmorbidity with properly appliedtourniquets is proportional tothe length <strong>of</strong> time they remainin place.Put simply: A poor understanding<strong>of</strong> indications fortourniquet use, anatomicalconsiderations for placement,employment strategies andmaterials required for sounddevices—as well as prolongeddelays in transporting patientsto definitive care—will mostlikely result in a suboptimaloutcome.However, if we examinetourniquet use in terms <strong>of</strong>risk-benefit in the hands <strong>of</strong>trained rescuers, we should seethe tourniquet as an invaluableasset for facilitating rapidand appropriate management<strong>of</strong> hemorrhagic trauma andattenuating associated shockwithin the prehospitalenvironment.Why They’re NeededCertain segments <strong>of</strong> societyare at higher risk than othersfor hemorrhage caused bypenetrating trauma. Militaryforces engaged in combat, lawenforcement <strong>of</strong>ficers engagedin tactical operations, civiliansaccidentally or purposelyinjured by penetrating objectsand emergency services personnelexposed to explosionsor penetrating objects typifythose at highest risk.Hemorrhage due to penetratingtrauma is the leadingcause <strong>of</strong> preventable death duringmilitary operations. 1,2 Thetactical environment requiresan approach to appropriatecasualty care that accounts forlow visibility, active hostilities,austere locations, limited medicalresources and unknownevacuation times. 3,4 The use <strong>of</strong>temporary emergency tacticaltourniquets is the cornerstone<strong>of</strong> TCCC hemorrhage control.Every individual operatingwithin the tactical environmentmust be trained to applya tourniquet, and should carryat least one tactical tourniquetat all times (see Table 1,p. 20, for desirable tourniquetcharacteristics). Following arigorous evaluation process,the Department <strong>of</strong> Defenseselected the Combat ApplicationTourniquet (C-A-T) as theprimary tourniquet issued toevery service member in thecurrent theater <strong>of</strong> operation.Results <strong>from</strong> combat evaluationsindicate that the C-A-T ishighly effective and when usedappropriately, does not causesignificant morbidity. 5,6,718 War on TraumaJournal <strong>of</strong> Emergency Medical Services
These results can be appliedto the civilian prehospitalenvironment. As long as weconduct due diligence for trainingand education, and matchthe best available options to theappropriate environment andindications, tourniquets will bean important tool for prehospitalproviders.When They’re NeededThe law enforcement environmentis most similar to themilitary tactical environment.An increasingly dangeroussociety puts our law enforcement<strong>of</strong>ficers at higher risk forpenetrating trauma. All lawenforcement <strong>of</strong>ficials should betrained in basic TCCC tenetsand adequately equipped toaddress those same life-threateninginjuries identified for thearmed forces.Other situations may arisewithin the civilian communitythat make the routine use <strong>of</strong>temporary emergency tourniquetsa very wise option. Masscasualtysituations with multipletraumatic bleeding injuries willoverwhelm medical capabilitiesif rapid treat-as-you-triage methodsare not employed. A trainedrescuer can effectively employ amodern tourniquet in seconds,allowing them to rapidly addressa large number <strong>of</strong> casualtiesquickly. Rescuers can then reassessthose treated and converttourniquets to less restrictivehemorrhage control measures.Even in single-trauma cases,an injury with significantbleeding requires significanteffort to maintain direct pressureor apply adequate woundpacking and pressure dressings.This reduces the amount<strong>of</strong> time the rescuer can spendon other necessary and <strong>of</strong>tencomplex tasks, such as airwayor respiratory management, orinitiating treatment for shock.By controlling hemorrhageimmediately, the rescuer’shands are free to attend toother tasks. Transport is notdelayed, and hemorrhagecontrol can be attended tounder adequate lighting andconditions either inside theambulance or on arrival in theemergency department. 8A Final WordProtocols for safe andeffective prehospital tourniquetuse can and should be implemented(see “Tourniquet First!”p. 24). Although tourniquet useis not without risk, an informedapproach that providesadequate education, training,assessment, validation andappropriate device selectionwill significantly reduce therisk to acceptable levels.Editor’s note: For more onthe subject <strong>of</strong> civilian prehospitaltourniquet use, read “The Return<strong>of</strong> Tourniquets: Original researchevaluates the effectiveness <strong>of</strong>prehospital tourniquets for civilianpenetrating extremity injuries,” inAugust 2008 JEMS, p. 44–54.References1. Bellamy RF: “The causes <strong>of</strong> death inconventional land warfare: Implicationsfor combat casualty care research.” MilitaryMedicine. 149(2):55–62, 1984.2. Holcomb JB, McMullin NR, Pearse L,et al: “Causes <strong>of</strong> death in U.S. SpecialOperations Forces in the global war onterrorism: 2001–2004.” Annals <strong>of</strong> Surgery.245(6):986–991, 2007.3. Butler FK Jr, Hagmann J, Butler EG:“Tactical combat casualty care inspecial operations.” Military Medicine.161(Suppl):3–16, 1996.4. National Association <strong>of</strong> EmergencyMedical Technicians: Prehospital traumalife support: Military version. 6th ed.Mosby: St. Louis, Mo., 2006.5. Beekley AC, Sebesta JA, BlackborneLH, et al: “Prehospital tourniquet usein Operation Iraqi Freedom: Effect onhemorrhage control and outcomes.”Journal <strong>of</strong> Trauma. 64(2 Suppl):S28–37,2008.6. Kragh JF Jr, Walters TJ, Baer DG, et al:“Practical use <strong>of</strong> emergency tourniquetsto stop bleeding in major limb trauma.”Journal <strong>of</strong> Trauma. 64(2 Suppl):S38–S50,2008.7. Kragh JF Jr, Baer DG, Walters TJ:“Extended (16-hour) tourniquetapplication after combat wounds: A casereport and review <strong>of</strong> the current literature.”Journal <strong>of</strong> Orthopaedic Trauma. 21(4):274–278, 2007.8. Doyle GS, Taillac PP: “Tourniquets: Areview <strong>of</strong> current use with proposals forexpanded prehospital use.” PrehospitalEmergency Care. 12(2):241–256, 2008.When a more definitive method <strong>of</strong> airway controlis required within the tactical environment,especially in the setting <strong>of</strong> facial trauma, mostexperts recommend the surgical cricothyrotomyas the procedure <strong>of</strong> choice. This complex, invasiveprocedure requires appropriate training underrealistic conditions to maximize a rescuer’s chancefor successful task completion.Adequate tools are required to facilitate thisprocedure, one <strong>of</strong> the most important being alaryngeal hook. Although few surgical instrumentsare designed specifically for the tactical environment,NAR’s Tracheal Hook is one exception.The Tracheal Hook is designed specifically t<strong>of</strong>acilitate this surgical procedure under less-thanoptimalconditions. Once an incision is made, thethe small end <strong>of</strong> the Tracheal Hook is insertedinto the cricoid cartilage and lifted up for stabilizationand anterior displacement. This betterexposes the hole opening for insertion <strong>of</strong> the trachealtube.Finger Grip End(Lift Up)NAR Tracheal HookInsert into TrachealOpening and HookN A RCricoid Cartilageincludes thisTracheal Hook ina complete, compactsurgical cricothyroidotomykit that facilitates rapid completion<strong>of</strong> this procedure under highstresscircumstances.Other airway devices for the tactical environmentremain controversial. Although retrospectivecasualty analysis is still being conducted,there has been no data supporting a clear survivalbenefit for supraglottic devices. Multiple prehospitalstudies have been conducted on these devices,but those studies did not account for the extentto which casualties are moved within the tacticalenvironment.Although the Laryngeal Mask Airway (LMA)has received many favorable reports <strong>from</strong> boththe anesthesia and prehospital literature, militarytrauma providers are concerned that thedevices are too easily dislodged during rigorousextractions and evacuations. The Army evaluatedseveral devices and chose two: the dual-lumenCombiTube and the single-lumen King LT-D. Ofthese two devices, the King LT-D demonstrated adistinct advantage in terms <strong>of</strong> rapid, correct insertionover the CombiTube. 12 Training novice usersto correctly employ the King LT-D was easier, andthe skill was retained for a longer period <strong>of</strong> timethan with the CombiTube. 13Elsevier Public Safety War on Trauma 19
Adjustable StrapTable 1Securing Device2"Width1Must StopArterialBleedingin LowerExtremities• Must be 100% effectivein clinical environment• Must account for largegirth lower extremities(95% male soldier =26.7")Optimal Design:Pneumatic CuffNote: USAISR and historicalstudies show pneumaticdevice superiority because<strong>of</strong> the manner in which theydistribute force evenly overa wider area, making themsuitable for surgical procedures.Only the Delphi EMT receivedrecommendations by theUSAISR due to its ability to besecured by a clamp; surgicaltourniquets were consideredtoo expensive.Advantages:• Creates even pressuredistribution overwider area• Pressure can be easilymeasured• Lower incidence <strong>of</strong>comorbidity; lower shearstress forces along edgesDisadvantages:• Difficult to ruggedize foraustere environment(shelf life, puncture, leaks)• Larger/heavier• ExpensiveWindlassOptimalTourniquetEngineeringFeatures2 3Temporary TacticalTourniquets• Width > 1"• Integrated mechanicalaugmentation (windlass,ratchet, cam)• Easily applied to upper orlower extremity (in lessthan one minute)• No external powerrequirement (batteries)• Light weight (< 230 g)and minimal cube space(facilitates individual carry)• Easy to train• Must not slip duringapplication• Must have easy release andreapplication capability• Must prevent accidentalreleaseLong shelf/storage life4•OtherConsiderations• Can be applied toentrapped limbs• Can be self-applied withone hand• Protection <strong>from</strong> overtightening• ExpenseHyFin®Chest SealPenetrating chest injuries represent a complexproblem in the tactical environment. Traditionalmethods <strong>of</strong> patient assessment, such as visualinspection and auscultation with a stethoscope,are not always possible in a low-light, highnoisecombat environment. Although medicsare trained to locate and seal open chestwounds, securing an occlusive dressing toa sweaty, bloody, hairy chest to preventair entry is not an easy task. Surgical tapedoesn’t always stick, and fashioning bandagesunder duress is difficult.As a result, a single adhesive dressingthat effectively occludes a chest wall defectis a required item in the medic’s kit. Thecommercially available Asherman ChestSeal has been used by the military, but newerproducts, such as the Hyfin chest seal, <strong>of</strong>fermore aggressive adhesive that keeps the pliabledressing in place throughout a rigorousevacuation process. Although the Hyfin chestseal does not feature a relief valve, tactical andcivilian medics are well trained in recognizingand treating a tension pneumothorax.Penetrating chest trauma is responsiblefor the second leading historical cause <strong>of</strong>potentially preventable combat death: tensionpneumothorax. 14,15 Combat medics aretaught to have a very high suspicion for thisproblem when managing penetrating trauma,and to treat it with a needle thoracostomy. Althoughcontroversy exists regarding the efficacy<strong>of</strong> this procedure in civilian prehospital literature,combat experience shows it to be a life-savingprocedure within the tactical environment.Realizing that a needle thoracostomy is not adefinitive treatment, combat medics are taught touse a 14-gauge by 8-cm (3.25") angiocath device toperform an invasive procedure that converts a lifethreateningtension pneumothorax to a survivablesimple pneumothorax.20 War on TraumaJournal <strong>of</strong> Emergency Medical Services
Military rescuers are trained to utilize the 2ndor 3rd intercostal spaces, mid-clavicular lineapproach as their primary procedure, with adjustmentto the anterior axillaryline if the primarysite is compromisedor unsuccessful.Insert the needleinto the skin over thesuperior border<strong>of</strong> the third or fourthrib, mid-clavicularline and direct itinto the intercostalspace at a 90° angle.Select site on theaffected side, 2nd or3rd intercostal space,mid-clavicular lineNote: Numbers denoteintercostal spacesThe NAR Air Release System features a3.25" decompression needle without a flashport, packaged in a compact, sealed brightred tube.Needle thoracostomy will be successful only ifthe needle tip penetrates into the air pocket. Note:The 3.25" catheter is recommended because severalstudies confirm that the average adult chestwall is greater than 5 cm, and if the insertion angleis not perpendicular, that distance may increase byalmost a full centimeter. 16–18NAR’s Air Release System (ARS) represents asignificant advance in human-factors engineeringfor this simple device. Many systems use thetypical angiocaths for this procedure, which havea flash chamber cap attached to the catheterassembly. Although this chamber cap prevents unnecessaryblood loss when used to start an IV, itprecludes the release <strong>of</strong> air when used in needle thoracostomy. Therefore,providers <strong>of</strong>ten fail to remove the cap on the standard angiocathwhen performing this procedure under duress.When they insert an ordinary angiocatheter through the chest walland fail to appreciate an improvement in the casualty’s status, providersassume the procedure wasn’t effective and remove the entire catheterassembly without having treated the underlying problem.The ARS does not incorporate a flash chamber cap; thus, when arescuer penetrates the chest wall into the pneumothorax pocket, there’sno additional step required to relieve the pressure. Air immediatelyescapes through the device, confirming successful placement.CirculationTCCC guidelines emphasize a hypovolemic resuscitationalgorithm. Combat medics are trained to evaluatecombat casualties for hypovolemic shock, and initiateIV fluid resuscitation only after obtaining hemorrhagecontrol. They assess the radial pulse character and mentalstatus as clinical markers for IV fluid requirements.ILLUSTRATIONS COURTESY NARARS 3.25" NeedleDecompression DeviceMedical supply resources are extremely limited inthe tactical environment, <strong>of</strong>ten constrained by whatthe medics can carry in their aid bags. IV fluids representthe heaviest component <strong>of</strong> all medical supplies,necessitating a fluid that provides appropriatevolume expansion for the longest possible time. Themilitary selected Hextend as the fluid <strong>of</strong> choice forhypovolemic resuscitation due to hemorrhage.Medics are trained to secure IV accessfor combat casualties through the use <strong>of</strong>a saline lock device. The saline lock procedureis slightly modified <strong>from</strong> typicalclinical applications in that, once secured,it’s accessed by a second IV catheter. Thisprovides a measure <strong>of</strong> security to preventaccidental dislodgement and allows medicsto administer IV medications when IVfluid resuscitation is not required.Securing IV access via a saline lock is atechnique used by many civilian prehospital services so they have IVaccess and don’t have to expend medical supplies to run IV fluids at a“TKO” rate.When IV access is difficult to obtain in the VidaCare® EZ-IOIntraosseous Devicehypovolemic combat casualty, medics useintraosseous (IO) devices tosecure parenteral access.Military medics accessmultiple sites for rapid fluidadministration, including the manubrium,tibia, humeral head and clavicle.The devices that have demonstrated superiorefficacy in battlefield medicine includethe Pyng FAST1 sternal intraosseous deviceand the VidaCare EZ-IO. 19-22 Many civilian EMSagencies and hospital emergency departmentshave successfully incorporated these devices into theirprotocols. Note: A pressure infusion device must be usedwhen administering fluids through an IO needle.Elsevier Public Safety War on Trauma 21
Evacuation & TransportationTraditional manual carries and drags <strong>of</strong> non-ambulatory casualtiesdepicted in numerous texts simply aren’t effective when rescuer andcasualty alike are outfitted in full combat gear. Additionally, a tacticalunit carrying evacuation platforms/stretchers into live combat cannegatively impact maneuverability if the selected platform is too bulkyor heavy for a single person to carry effectively.Talon II® 90CCollapsibleHandle LitterThe Talon II by NARprovides the material solutionfor this issue. Unlike non-rigid litters,the Talon provides a measure <strong>of</strong> patient safetyby preventing excessive body movement, securingthe casualty to the device via the integrated safetystraps. In addition, over most terrain, moving a rigid litter requiresmuch less effort than other types <strong>of</strong> platforms. The litter can then besecured directly to a vehicle or to a traditional movement gurney. Collapsiblerigid litters are also easily stored in vehicles and occupy relativelylittle space.Until fairly recently, hypothermia was a major source <strong>of</strong> morbidityamong combat casualties. Even though ambient temperatures in combatareas <strong>of</strong>ten exceeded 100º F during daytime hours, casualties whohad been previously exposed during evaluation and treatment werearriving at Combat Support Hospitals and Forward Surgical Teamspr<strong>of</strong>oundly hypothermic.One retrospective review revealed that 18% <strong>of</strong>casualties evacuated to one hospital arrived with coretemperatures <strong>of</strong> less than 36ºC. 23 This study showedthat the presence <strong>of</strong> hypothermia was an independentpredictor <strong>of</strong> operative management,surgical procedures, Factor VIIa use and mortality,with temperatures <strong>of</strong> less than 34ºC associatedwith a near 100% mortality rate.Acknowledging that active re-warming capabilityat the point <strong>of</strong> injury during tactical operationsis not logistically feasible, military medical researchersturned their efforts toward hypothermia prevention.Traditional “space blankets” were found not to be effective enough;soldiers needed a small, lightweight product that could be easily carriedin a medic’s aid bag, preferably without an external power source.The result was a system that incorporates a heat source with an improvedinsulator. 24NAR’s Hypothermia Prevention Management Kit (HPMK) is avacuum-sealed compact kit that has proven very effective in preventinghypothermia. It was selected as one <strong>of</strong> the hot products at the 2008EMS Today Conference.Educating military rescuers on the importance<strong>of</strong> hypothermia and employing an effective kitvirtually eliminated the incidence <strong>of</strong> hypothermiarelatedcomplications and mortality. The HPMK’scompact size and proven performance makes it anideal candidate for consideration as a contingencyitem in civilian emergency vehicles and an importantasset to have on hand in large quantities foruse at MCIs.MedicinesAnother challenge encountered during tacticaloperations: adequately medicating casualtiesin a timely manner. When casualty evacuationdelays occur, the timely administration <strong>of</strong> antibioticsis crucial for the prevention <strong>of</strong> subsequentwound infections.One product that addresses both moderatepain control and antibiotic prophylaxis is theCombat Wound Pill Pack, a “homemade” packetthat Special Operations Forces use consisting<strong>of</strong> acetaminophen, meloxicam and a flouroquinolone.The combination <strong>of</strong> acetaminophen andmeloxicam provides analgesia for mild to moderatepain without altering the sensorium, thusallowing the operator to continue participating inthe tactical mission.Military medical providers have also successfullyused oral trans-mucosal fentanyl devicesfor pain management during combat operations.These devices have the advantage <strong>of</strong> rapidonset <strong>of</strong> action, significant pain-control properties,not requiring IV/IO access and the ability tobe self-administered and titrated. 25 Although notrequired for every trauma patient, such devicescertainly bear consideration for use as a viableoption in civilian prehospital and emergencydepartment pain-control protocols.VacuumSealedPackageSelf-HeatingShell LinerHPMKHypothermia Prevention& Management Kit22 War on TraumaJournal <strong>of</strong> Emergency Medical Services
ConclusionMilitary medicine has contributed to manyadvances in prehospital trauma care by applyingsound medical principles to account for thechallenging tactical environment. These advanceswere achieved due to the requirement to optimizecasualty care while simultaneously minimizing theimpact on ongoing combat operations. Althoughall these applications may not be appropriatefor the contemporary civilian environment, weshould examine current military tactical medicaltechniques and procedures for possible crossoverbenefit to our civilian trauma patients, or as areasthat may require further study.Dr. Jeffrey Cain is an emergency medicine physicianpracticing in McKinney, Texas. He is a graduate <strong>of</strong>West Point and the Uniformed Services University<strong>of</strong> the Health Sciences, with service in the 75thRanger Regiment as an infantry <strong>of</strong>ficer and lateras a battalion physician. Other active-duty Armyassignments included academic director for theArmy Combat Medic Course and research physicianwith the U.S. Army Institute <strong>of</strong> Surgical Research.He has conducted extensive TCCC training forthe Department <strong>of</strong> Defense and other governmentorganizations, and is currently serving as the vicechairman for the Committee on TCCC. Cainhas reported receiving honoraria and/or researchsupport, either directly or indirectly, <strong>from</strong> the sponsor<strong>of</strong> this supplement, North American Rescue.Dr. Jeff Cain will be a featured speakerat the EMS Today Conference inBaltimore, Maryland, March 26–29, 2009.References1. Butler FK, Hagmann JH, Richards DT: “Tacticalmanagement <strong>of</strong> urban warfare casualties in specialoperations.” Military Medicine. 165(4 Suppl):1–48,2000.2. Butler FK Jr, Hagmann J, Butler EG: “Tacticalcombat casualty care in special operations.” MilitaryMedicine. 161(Suppl):3–16, 1996.3. McSwain NE, Salomone JP (eds): PreHospitalTrauma Life Support Manual, 6th edition. Mosby:Akron, Ohio, 2006.4. Butler FK Jr, Holcomb JB, Giebner SD: “Tacticalcombat casualty care 2007: Evolving concepts andbattlefield experience.” Military Medicine. 172(11Suppl):1–19, 2007.5. Beekley AC, Sebesta JA, Blackborne LH, etal: “Prehospital tourniquet use in Operation IraqiFreedom: Effect on hemorrhage control andoutcomes.” Journal <strong>of</strong> Trauma. 64(2Suppl):S28–S37, 2008.6. Kragh JF Jr, Walters TJ, Baer D, et al: “Practical use <strong>of</strong> emergencytourniquets to stop bleeding in major limb trauma.” Journal <strong>of</strong> Trauma.64(2 Suppl):S38–S50, 2008.7. Walters TJ, Wenke JC, Kauvar DS, et al: “Effectiveness <strong>of</strong> self-appliedtourniquets in human volunteers.” Prehospital Emergency Care. 9(4):416–422, 2005.8. Grimes M, Rocheleau DN: Analysis <strong>of</strong> pressure distribution <strong>of</strong> armybandages. University <strong>of</strong> South Carolina Department <strong>of</strong> MechanicalEngineering Technical Report; September 21, 2007.9. Wedmore I, McManus JG, Pusateri AE: “A special report on the chitosanbasedhemostatic dressing: Experience in current combat operations.”Journal <strong>of</strong> Trauma. 60(3):655–658, 2006.10. Ward KR, Tiba MH, Holbert WH: “Comparison <strong>of</strong> a new hemostatic agentto current combat hemostatic agents in a Swine model <strong>of</strong> lethal extremityarterial hemorrhage.” Journal <strong>of</strong> Trauma. 63(2):276–284, 2007.11. Rhee P, Brown C, Martin M: “QuikClot use in trauma for hemorrhagecontrol: Case series <strong>of</strong> 103 documented uses.” Journal <strong>of</strong> Trauma.64(4):1093–1099, 2008.12. Schwartz R, McManus J, Hill G: “Supraglottic devices in tactical airwaymanagement: A comparison <strong>of</strong> the King Laryngeal Tracheal device and theCombitube in Army combat medic students.” Paper presentation, AnnualMeeting <strong>of</strong> the National Association <strong>of</strong> EMS Physicians, 2008.13. Russi CS, Miller L, Hartley MJ: “A comparison <strong>of</strong> the King-LT toendotracheal intubation and CombiTube in a simulated difficult airway.”Prehospital Emergency Care. 12(1):35–41, 2008.14. Bellamy RF: “The causes <strong>of</strong> death in conventional land warfare:Implications for combat casualty care research.” Military Medicine.149(2):55–62, 1984.15. Holcomb JB, McMullin NR, Pearse L: “Causes <strong>of</strong> death in U.S. SpecialOperations Forces in the global war on terrorism 2001–2004.” Annals <strong>of</strong>Surgery. 245(6):986–991, 2007.16. Zengerink I, Brink PR, Laupland KB: “Needle thoracostomy in thetreatment <strong>of</strong> pneumothorax in trauma patients: What size needle?” Journal<strong>of</strong> Trauma. 64(1):111–114, 2008.17. Harcke HT, Pearse LA, Levy AD: “Chest wall thickness in militarypersonnel: Implications for needle thoracentesis in tensionpneumothorax.” Military Medicine. 172(12):1260–1263, 2007.18. Givens ML, Ayotte K, Manifold C: “Needle thoracostomy: Implications<strong>of</strong> computed tomography chest wall thickness.” Academic EmergencyMedicine. 11(2):211–213, 2004.19. Beekley AC, Starnes BW, Sebesta JA: “<strong>Lessons</strong> learned <strong>from</strong> modernmilitary surgery.” Surgical Clinics <strong>of</strong> North America. 87(1):157–184, 2007.20. Dubick MA, Holcomb JB: “A review <strong>of</strong> intraosseous vascular access:Current status and military application.” Military Medicine. 165(7):552–559, 2000.21. Calkins MD, Fitzgerald G, Bentley TB, et al: “Intraosseous infusiondevices: A comparison for potential use in special operations.” Journal <strong>of</strong>Trauma. 48(6):1068–1074, 2000.22. Frascone RJ, Jensen JP, Kaye K: “Consecutive field trials using two differentintraosseous devices.” Prehospital Emergency Care. 11(2):164-171, 2007.23. Arthurs Z, Cuadrado D, Beekley A, et al: “The impact <strong>of</strong> hypothermiaon trauma care at the 31st combat support hospital” American Journal <strong>of</strong>Surgery. 191(5):610–614, 2006.24. Winkenwerder W: “ASDHA Policy Letter on Hypothermia Prevention andTreatment.” Feb. 16, 2006.25. Kotwal RS, O’Connor KC, Johnson TR, et al: “A novel pain managementstrategy for combat casualty care.” Annals <strong>of</strong> Emergency Medicine.44(2):121–127, 2004.Elsevier Public Safety War on Trauma 23
By Peter P. Taillac, MD, FACEP &Gerard S. Doyle, MD, MPHFew issues in the long and colorful history <strong>of</strong> medicinehave generated as much controversy and confusion as theuse <strong>of</strong> tourniquets to arrest severe extremity hemorrhage.As with many strongly held, traditional beliefs, the tradition isstrong, but the evidence weak.Conventional teaching has upheld the belief that a tourniquetis a tool only to be applied as a last resort.1 However, evidence is now available,both <strong>from</strong> the recent military use <strong>of</strong>tourniquets 2 and their long, safe history<strong>of</strong> operative use for bloodless extremitysurgery, 3,4 which compels a reevaluation<strong>of</strong> this potentially lifesaving device incivilian prehospital care. This article presentssuggested protocols for the safe andrational use <strong>of</strong> extremity tourniquets bycivilian EMS.It is our opinion that any blood loss isdetrimental to the patient’s wellbeing andshould be avoided. Modern tourniquetshave been demonstrated to rapidly and effectively stop extremityhemorrhage, thus minimizing blood loss. Pressure dressings are, <strong>of</strong>course, also effective tools to stop bleeding, and are the preferredmethod <strong>of</strong> hemorrhage control because they do not risk limb ischemiaor other complications. However, effective pressure dressingapplication requires more time, hands and supplies to apply, andmay require a rescuer to stay with the patient to continue to applypressure sufficient to arrest severe hemorrhage.A tourniquet, on the other hand, can be applied quickly, withminimal personnel and no other equipment. In fact, most moderntourniquets are designed to be self-applied, if necessary.In the past, the rule was“tourniquet last”; however,it’s time we begin teaching theprinciple <strong>of</strong> “TourniquetFirst!” in severe extremityhemorrhage.This immediate hemorrhagecontrol allows the rescuer toturn their attention to the airway,breathing, and circulationand assessment <strong>of</strong> otherinjuries. After completingthis evaluation andstabilization, and whentime and resources betterallow—and if the woundallows—the well-trained EMSprovider can remove the tourniquetand replace it with a standardpressure dressing.Although this protocol contradicts the traditionaldogma that a tourniquet, once placed,can be removed only by a physician when thepatient arrives at definitive care, it’s simplycommon sense to train EMS personnel to reassessthe wound and replace the tourniquet witha pressure dressing if the situation allows.Considerations for UseIschemic complications <strong>from</strong> tourniquet usehave been found to be related to the amount <strong>of</strong>time the tourniquet is left in place. 4,5 Extensiveexperience with operative tourniquet use hasdemonstrated that the incidence <strong>of</strong> injury is verylow with tourniquet times <strong>of</strong> two hours or less;military experience has confirmed the safety <strong>of</strong>this two-hour limit in the field. 4–8Urban EMS agencies, withgenerally short transporttimes, would rarely be confrontedwith this limitation.However, rural agencies inisolated areas will frequentlyencounter longer transporttimes that may exceed thissafe interval. In these cases,attempts to replace the tourniquetwith a less aggressivemethod <strong>of</strong> hemostaticdressing must be made toavoid the possibility <strong>of</strong> limbischemia.In the rare event that severe hemorrhage persistsbeyond two hours during a long transport,the medical rule “life over limb” is invoked. Inthese cases, it must be kept in mind that a patientwith extremity hemorrhage severe enoughto require a tourniquet for more than two hourswould certainly have died without it.Another consideration for the use <strong>of</strong> tourniquets:pain. The effective application <strong>of</strong> atourniquet above arterial pressure will cause24 War on TraumaJournal <strong>of</strong> Emergency Medical Services
pain to the distal extremity, sometimes severe.Patients will generally require opiate pain medication,such as morphine or fentanyl, titrated tocontrol such pain, particularly if the tourniquetis to be left in place for more than a shortperiod <strong>of</strong> time.Tourniquet ProtocolsThe following protocols provide a safe andrational technique for civilian EMS agenciesto use tourniquets to minimize blood loss andmorbidity in extremity trauma while reducingthe risk <strong>of</strong> ischemic complications. These protocolsare based on military battlefield and civilianoperative experience.1Design: To minimize complications,particularly those related to direct injuryto skin, muscle and neurovascular structures,emergency personnel must use a commercialtourniquet specifically designed for thepurpose. Such tourniquets feature wide strapswithout sharp edges, uniform application <strong>of</strong>pressure and ease <strong>of</strong> application and removal.Field-expedient and hastily devised tourniquets(such as the cravat andstick, belt, cord or twine) aremuch less likely to be effectivebecause it’s difficult to get themtight enough. Because <strong>of</strong> narrowgirth, sharp edges and difficultyin accurately controlling tightness,such makeshift tourniquetsare also much more proneto compressive neuropathy andother injuries resulting <strong>from</strong>direct trauma to the under lyingtissues.2Models: A number <strong>of</strong>commercial tourniquets areavailable and have proveneffective in testing and combatuse. It’s worth mentioning thata standard BP cuff can <strong>of</strong>tenbe utilized as a safe and effectivetourniquet. However, BPcuffs are not designed to holdpressures above arterial systolicpressure for prolonged periods <strong>of</strong>time. A cuff that gradually losespressure could result in recurrence<strong>of</strong> hemorrhage, which initiallymay go unnoticed by thebusy EMS provider.In addition, the BP cuff ’swide girth, while minimizing therisk <strong>of</strong> underlying neurovascularor skin compressive injuries, may be difficult to apply to the shortstump <strong>of</strong> an amputated extremity. So, while a BP cuff is probablythe safest and most easily accessible improvised tourniquet availableto you, wide-band commercial tourniquets are more versatileand reliable for severe extremity hemorrhage.3Tightening the Tourniquet: How tight youmake the tourniquet depends on how severe or pr<strong>of</strong>use thebleeding is, and whether it’s arterial or venous bleeding (orboth). Simply stated: The tourniquet should be gradually tighteneduntil all hemorrhage ceases. With arterial bleeding, this willrequire a tourniquet pressure above the arterial pressure. With venoushemorrhage, lower pressures may be sufficient. Tourniquetpressure will require frequent reassessment as the resuscitation <strong>of</strong>the patient proceeds, and further tightening may be required asperfusion improves.4Initial Application: Figure 1 illustrates our suggestedprotocol for evaluation and application <strong>of</strong> a tourniquetto a bleeding extremity. The patient is initially assessedand determined to have severe extremity bleeding controllable withthe equipment or resources immediately at hand.This may simply mean that EMS personnel must open their kitand assemble the gauze, tape or elastic bandage necessary to applya pressure dressing, and may need to apply a tourniquet to the patientfor just the one or twominutes required to completethis task. Or this maymean the patient has severeextremity bleeding with othersevere injuries, such as anunstable airway or an openchest injury. In this case, thetourniquet may be appliedinitially to stop the extremityhemorrhage, leaving theEMS provider free to focustheir attention on stabilizingthese other life-threateningproblems.If a short transport time(less than 30 minutes) is anticipated,then the tourniquetmay be safely left in place,or replaced with a pressuredressing whenever the providerfeels they have the timeand resources to devote tothis task. If transport is anticipatedto be longer than30 minutes, an effort to replacethe tourniquet shouldbe undertaken to minimizeany possibility <strong>of</strong> limb ischemiaand decrease the painthe patient may experience<strong>from</strong> prolonged effectivetourniquet application.Elsevier Public Safety War on Trauma 25
Note: We strongly suggest 30 minutes as thetime limit for replacing a tourniquet with apressure dressing. Although the studies citedin the discussion above indicate two hours tobe a safe limit, we use 30 minutes as a protocolguideline to ensure a wide margin <strong>of</strong> safety.5Reassessment: When the EMSprovider has sufficient time, equipmentand resources, they may decide to attemptto replace the tourniquet with a pressuredressing. Figure 2 outlines the TourniquetReassessment Algorithm to assist the medic indetermining if tourniquet replacement is advisableand safe and to suggest that the tourniquetbe left in place if the patient or the overallsituation is unstable.6Removal: If the EMS provider determinesthat the patient and clinical situationare stable, they should proceed tothe Tourniquet Removal Algorithm, as shownin Figure 3. Note: In cases <strong>of</strong> amputation ornear-amputation, the tourniquet should be leftin place because <strong>of</strong> the difficulty <strong>of</strong> applying apressure dressing to such wounds.A pressure dressing is applied to the woundsite and the tourniquet is then carefully loosened.If there’s no further bleeding, the tourniquetshould be left loosely in place in caseit’s needed again. For example, bleeding couldresume as the patient is resuscitated and perfusionand flow to the injury are improved.If further bleeding isn’t controllable with thepressure dressing, the tourniquet can be easilyretightened until the bleeding is once againcontrolled.7Mass-Casualty Use: TheMass Casualty Algorithm (Figure 4) isdesigned to incorporate the tourniquetinto the initial triage <strong>of</strong> patients at the scene<strong>of</strong> a large, resource-taxing MCI. As triage isperformed, EMS providers can use tourniquetsto control any visible extremity hemorrhage.They then assign a triage label to thepatient and move to triage the next victim.Note: We recommend that any patient whoreceives a tourniquet be initially triaged atleast “yellow-urgent” to ensure the victim is attendedto (and the tourniquet reassessed) in atimely fashion.It’s possible that subsequent providerscould overlook a tourniquet on a severelyinjured patient, as they attend to more obviousor urgent injuries. To minimize thisrisk, we recommend that any patient treatedwith a tourniquet should be clearly marked26 War on TraumaJournal <strong>of</strong> Emergency Medical Services
with the letters “TK” on their forehead andon the triage tag; the time the tourniquet wasapplied should also be noted prominently.If possible, the tourniquet itself should bemarked with brightly colored tape to make itstand out to all subsequent caregivers. If the patientis conscious, they should be instructed totell every subsequent provider that a tourniquetis in place.ConclusionThe tourniquet has traditionally been thoughtto be a dangerous tool <strong>of</strong> last resort. However, itis clear <strong>from</strong> recent experience with tourniquetson the battlefield and in the operating room thatmodern tourniquets are not only safe and useful,but lifesaving. It is our intent to encouragethe safe and rational use <strong>of</strong> tourniquets in civilianEMS, using simple protocols and training toensure they’re used properly and safely.In the past, the rule was “tourniquet last”;however, it’s time we begin teaching the principle<strong>of</strong> “Tourniquet First!” in severe extremityhemorrhage.Editor’s Note: These protocols were originally published by theauthors in “Tourniquets: A review <strong>of</strong> current use withproposals for expanded prehospital use,” April–June 2008,Prehospital Emergency Care.Peter P. Taillac, MD, FACEP, is an associate clinical pr<strong>of</strong>essor inthe University <strong>of</strong> Utah Division <strong>of</strong> Emergency Medicine. He servesas the state medical director for the Utah Bureau <strong>of</strong> EmergencyMedical Services, Utah Department <strong>of</strong> Health, and is the medicaldirector for West Valley City (Utah) Fire and Emergency MedicalServices. Dr. Taillac has reported no conflicts <strong>of</strong> interest related tothe sponsor <strong>of</strong> this supplement, North American Rescue.Gerard S. Doyle, MD, MPH, is assistant pr<strong>of</strong>essor in the EmergencyMedicine Section and medical director for the Emergency EducationCenter at the University <strong>of</strong> Wisconsin School <strong>of</strong> Medicineand Public Health in Madison. Dr. Doyle has reported no conflicts<strong>of</strong> interest related to the sponsor <strong>of</strong> this supplement, NorthAmerican Rescue.References1. Coupland RM, Molde A, Navein J: Care in the field for victims <strong>of</strong>weapons <strong>of</strong> war: a report <strong>from</strong> the workshop organized by the ICRCon prehospital care for war and mine-injured. Geneva: InternationalCommittee <strong>of</strong> the Red Cross 2001.2. Beekley AC, Sebesta JA, Blackbourne LH, et al:“Prehospital tourniquet use in Operation IraqiFreedom: Effect on hemorrhage control andoutcomes.” Journal <strong>of</strong> Trauma. 64(2):S28–37, 2008.3. Klenerman L: “The tourniquet in surgery.” J BoneJoint Surg Br. 44B:937–943, 1962.4. Wakai A, Winter DC, Street JT, et al: “Pneumatictourniquets in extremity surgery.” Journal <strong>of</strong> theAmerican Academy <strong>of</strong> Orthopaedic Surgeons.9(5):345–351, 2001.5. Kam PC, Kavanagh R, Yoong FF: “The arterialtourniquet: Pathophysiological consequences andanaesthetic implications.” Anaesthesia. 56(6):534–545, 2001.6. Walters TJ, Mabry RL: “Issues related to the use <strong>of</strong>tourniquets on the battlefield.” Military Medicine.170(9):770–775, 2005.7. Lakstein D, Blumenfeld A, Sokolov T, et al:“Tourniquets for hemorrhage control on thebattlefield: A 4-year accumulated experience.Journal <strong>of</strong> Trauma. 54(5):S221–225, 2003.8. Kragh JF Jr, Walters TJ, Baer DG, et al: “Practical use<strong>of</strong> emergency tourniquets to stop bleeding in majorlimb trauma.” Journal <strong>of</strong> Trauma. 64(2):S38–50, 2008.Elsevier Public Safety War on Trauma 27
School shootings like the oneat Columbine High Schoolunderscore the need for EMSpr<strong>of</strong>essionals to be aware <strong>of</strong>how the body’s response willundermine their best efforts inan active shooter situation.By Bruce K. SiddleAtrauma surgeon was recently involved in a case wherestress affected his ability to perform a tracheotomy. Thecase involved a tactical team <strong>of</strong>ficer, who was broughtto the ED with a gunshot wound that required an emergencytracheotomy. The surgeon knew the <strong>of</strong>ficer well, knew the members<strong>of</strong> his tactical team and had actually trained with the teamon many occasions as their emergency team doctor. Therefore, aspecial bond existed between them.The <strong>of</strong>ficer’s wounds were serious, and his fellow <strong>of</strong>ficers refusedto leave his side. As the surgeon began what should have beena simple procedure, his vision became distorted and his handsbecame sweaty and shook, resulting in his inability to firmly graspthe surgical tool. A simple straight-line incision took severalattempts, leading to what he described as a “road map” <strong>of</strong> scars.In the end, the surgeon saved the <strong>of</strong>ficer’s life. The <strong>of</strong>ficer recoveredand is again active on the tactical team. But the surgeonconfessed to me that the stress associated with the seriousness <strong>of</strong>the injury, his personal association with the <strong>of</strong>ficer, and the peerpressure <strong>from</strong> the patient’s team members impacted his visualclarity, his ability to concentrate and his precision motor skills.Photo george Kochaniec / SygmaPrior to this event, the surgeon hadperformed dozens <strong>of</strong> the same procedures in avariety <strong>of</strong> conditions with absolute precision.So what went wrong?Operational CharacteristicsThere’s a saying, “To err is human.” I proposethat “error is subsequent to the human factor.”In EMS, human factors collide with the needto decide quickly and act precisely, underconditions that are dynamic, stress-inducingand occasionally hostile. The key to ensuringeffective performance under those conditionslies in understanding the body’s response tostress and danger.Consider for a moment the basic operationalparameters <strong>of</strong> the emergency medicalpr<strong>of</strong>essional:• The mission <strong>of</strong> EMS pr<strong>of</strong>essionals is toprovide care and save lives.• They operate in environments that aredynamic, unstable, time-sensitive and attimes hostile to their safety.• They work under the stress that is multidimensional—ranging<strong>from</strong> self-inducedstress, peer-based stress, patient stress andbystander stress—and magnified by theneed to treat/save the patient.• They are required to exhibit absolute precision—inperception, diagnosis, treatment(precise motor skills), communications(to fellow operators and the patient) andpatient protection.• They are constantly exposed to spontaneousand unexpected threats that can triggertheir startle response.Very few pr<strong>of</strong>essions operate in extremeenvironments that also require precise skills;even fewer have the added stress <strong>of</strong> saving livesas their core mission. In fact, <strong>from</strong> the perspective<strong>of</strong> basic human physiology, the EMSpr<strong>of</strong>essional’s mission is a scientific paradox: theoperational environment is extremely dynamicand <strong>of</strong>ten life-threatening to the operator; butthe operational requirement is extreme precision—theprecision required when threading aneedle, only there’s a life on the line.The focus <strong>of</strong> this article is the role <strong>of</strong> thesympathetic nervous system (SNS) as it relatesto the mission, operational environment andoperational requirements <strong>of</strong> the emergencymedical pr<strong>of</strong>essional. My goal is to educateemergency personnel on the hard-wiredmechanics <strong>of</strong> the body’s stress physiologycircuitry and how it impacts precision skills,<strong>from</strong> complex medical procedures to suchbasic acts as opening medical kits and supplies.28 War on TraumaJournal <strong>of</strong> Emergency Medical Services
Identification <strong>of</strong> Stress SymptomsEmergency medical pr<strong>of</strong>essionals canexperience various predictable EMS stressors,such as:• Self-induced stress to save a life• Time constraints• Colleagues’ presence• Dynamic and unstable environment(terrain, weather, crowds, etc.)• Patient’s psychological state (scared,irritated, angry or combative)• Third parties (family, friends or bystanders)• Poorly designed equipment• Failure to perform a skill correctly the firsttime• Threat to the operator <strong>from</strong> a third partyor environmental conditionsEach form <strong>of</strong> stress can be equally debilitatingto precision-based skills. A combination <strong>of</strong>any two stressors can magnify the deterioration<strong>of</strong> precision skills. Combinations <strong>of</strong> threeor more stressors can trigger an immediatecascade <strong>of</strong> all precision skills. Further, survivalstress trumps all combinations <strong>of</strong> stressors.To combat these stressors during emergencysituations, many medics employ“tactical breathing,” which, when done properly,turns <strong>of</strong>f the SNS for short periods <strong>of</strong> time.Multiple Precision NeedsThe EMS pr<strong>of</strong>essional’s operational requirementis precision, but not in one single area <strong>of</strong>performance. Rather, they require:• “Precision in Perception” —not a singlesensory experience, but all <strong>of</strong> the processessimultaneously.• “Precision (Analytical) Processing” —theoutcome <strong>of</strong> interpreting all <strong>of</strong> the perceptualsensory information into a singleworking hypothesis <strong>of</strong>patient symptoms andtreatment.• “Precision-Based Pretreatment”—anoutcome<strong>of</strong> preparing yourmedical kit with productsthat are stresscompatible.A well-laidout and stocked kitreduces the time neededto treat a trauma patient.The kit should be alsodesigned and stockedaccording to levels <strong>of</strong>The Braintrauma/care, in a way that compensates for stress-inducedvisual distortions. In addition, products within the kit must bedesigned to be gripped easily and firmly.• “Precision in Treatment” —the hallmark <strong>of</strong> an emergencymedical pr<strong>of</strong>essional. Virtually every skill an emergencymedical pr<strong>of</strong>essional provides requires hand-eye coordinationwithin finite spaces.• “Precision in Demeanor” —the emergency medical pr<strong>of</strong>essionalmust exude an aura <strong>of</strong> confidence, competenceand calmness. All <strong>of</strong> these attributes are absorbed by thepatient and directly affect the patient’s respiratory rates, bloodpressure and the level <strong>of</strong> hemorrhaging.Our Body’s ResponseThe prefrontal cortex is the centerfor precision perceptual processing,precision analytical skills and theformation (and execution) <strong>of</strong>precision motor skills. But as stressincreases, the efficiency <strong>of</strong> theprefrontal cortex breaks down,resulting in a loss <strong>of</strong> perception,analysis, evaluation, precision motorskills, processing <strong>of</strong> time and memory<strong>of</strong> past experiences.Extreme stress and absolute precision create a conflict withinour body’s performance network, the autonomic nervous system(ANS). The ANS controls all <strong>of</strong> the voluntary and involuntaryfunctions <strong>of</strong> the body, and is divided into the parasympatheticnervous system (PNS) and the sympathetic nervous system (SNS).During waking hours and times <strong>of</strong> non-stress, the two brancheswork together to create a state <strong>of</strong> balance, or homeostasis, inwhich our high-level cerebral functions (perception, analysis, theexecution <strong>of</strong> precision motor skills) are performed optimally. TheSNS performs the opposite function <strong>of</strong> the PNS and is referred toas the “fight or flight response,” the “fear system,” the “predatordefense system” and the “survival system.”SNS activation stimulates the immediate release <strong>of</strong> stress hormonesin proportion to the threat. It also increases arterial pressureand blood flow to large muscle mass (resulting in enhancedgross motor skill and strength), stimulates vasoconstriction <strong>of</strong>minor blood vessels at the end <strong>of</strong> the appendages, increases pupildilation and causes cessation <strong>of</strong> the digestive process.The SNS is always on a hair-trigger and is activated by perceivingconscious and unconscious threats. The result is asurvival system that makes us explosively strong throughincreased adrenaline levels, whereby reactions to threats areautomatic and without hesitation.But our system gains speed by bypassing the high analyticalcapabilities <strong>of</strong> the prefrontal cortex. Thus, we become fast, quickand strong—but dumb—because we don’t need precision <strong>of</strong>perception, analysis and execution when running for thenearest tree.ILLUSTRATIONCOURTESYBRUCE SIDDLEElsevier Public Safety War on Trauma 29
Here lies the paradox: Our hardwiredsurvival system (SNS) isnot conducive to the environmentalstress <strong>of</strong> EMS.Role & Outcome <strong>of</strong>SNS ActivationOur survival throughouthistory has been a byproduct<strong>of</strong> both our intellect andthe hair-trigger wiring <strong>of</strong> theSNS. Our intellect works bestwhen we have time, distanceand cover, and are calm andin a quiet place where we canconcentrate.The SNS, on the other hand,is wired for spontaneous attacks,giving us an automaticand explosively quick system tosurvive charging predators orpoisonous critters (stepping ona snake or touching a spider).SNS wiring is so sensitive itshaves one-half to two seconds<strong>from</strong> a consciously directed motorskill. Put into perspective:A grizzly bear can out-sprinta racehorse in a ¼-mile race.Thus, even a ½-second delaycould be fatal when racing for atree with a grizzly on your heels.ILLUSTRATION COURTESY NARBut reacting without accessing our intellect is just one <strong>of</strong> dozens<strong>of</strong> survival responses the SNS induces. Let’s take a closer look athow SNS activation affects other areas.Perception: From the moment <strong>of</strong> arrival at an incident to thehand-<strong>of</strong>f <strong>of</strong> a patient at the hospital, the emergency medical pr<strong>of</strong>essionalshould be scanning the environment. Scanning perceptionmust be continuous, adapting <strong>from</strong> wide to narrow and distant tonear, and closer yet when applying medical care. When scanning,your head rotates, your pupils dilate and constrict, you orient yourhead to noise, and you recoil <strong>from</strong> putrid smells.SNS activation, however, doesn’t allow for scanning, becauseit’s counter-productive to capturing as much information possibleabout a charging predator. During SNS activation, you’ll involuntarilylock all <strong>of</strong> your perceptual systems onto the pending threatthrough a process called perceptual narrowing, which provides themost information to the brain as possible. Perceptual narrowingwill manifest itself as tunnel vision, auditory exclusion and the loss<strong>of</strong> touch sensations (as in not feeling pain).Once the SNS is triggered, humans become binocular and losethe ability to focus on near objects. Depth perception is impacted,and detailed color vision is <strong>of</strong>ten lost, but in an interesting twist,our primal visual system locks onto certain colors—those that areassociated with poisonous critters. Auditory perception is alsolikely to be impacted by the SNS.Analytical Processing: Although theneural networks <strong>of</strong> analytical processing aren’tcompletely understood, the basic processesoccur in the prefrontal cortex, which acts asthe initiator, the time estimator and the selfmonitor.It’s responsible for directing attention,focusing attention, ending focused attention,identifying the details <strong>of</strong> stimuli, etc.More importantly, the prefrontal cortex isthe center for precision perceptual processing,precision analytical skills and the formation(and execution) <strong>of</strong> precision motor skills (grossmotor skills are formatted and launched <strong>from</strong>the older brain structures).However, high-level prefrontal cortexprocessing can only occur during states <strong>of</strong>homeostasis. Functional magnetic resonanceimaging (fMRI) scans have demonstratedthat as stress increases, the efficiency <strong>of</strong> theprefrontal cortex breaks down and we becomemore instinctive or primal in action.30 War on TraumaJournal <strong>of</strong> Emergency Medical Services
A breakdown <strong>of</strong> analytical processes results ina cascade <strong>of</strong> deteriorating performance. Perception,analysis, evaluation, precision motor skills,the processing <strong>of</strong> time that’s so critical in emergencycare, memory <strong>of</strong> past experiences (successfuland unsuccessful) are all lost.Indecision, hesitation, failure to sense (hear,see, feel), failure to act, over-reaction or underreactionshould be expected when the SNSis triggered. Even the simple act <strong>of</strong> opening abandage can be overwhelming. The prefrontalcortex is the center for precision, and without itthe emergency medical pr<strong>of</strong>essional functionsat the same precision level as an ape.SNS-Induced Motor Skills: Grossmotor skills—those used when the SNS is activated,such as gripping, squeezing, pushing,pulling, sprinting or lunging—are enhancedby adrenaline. But when adrenaline isn’t usedup in explosive movements, it continues t<strong>of</strong>ire away within the muscles. The after-effectis not a fun experience; muscle tremors, uncontrolledshaking and the loss <strong>of</strong> most fine/complex motor skills occur.SNS-induced motor skills are also affectedby the brain’s survival circuit (thalamusamygdalacircuit). As explained previously, theprefrontal cortex is critical to higherfunctions, but is also thelocation for the formationand activation<strong>of</strong> fine and complexmotor skills. Thecombination <strong>of</strong> thesurvival circuit andthe effects <strong>of</strong> adrenalinelead to the loss<strong>of</strong> precision motorskills (either fine orcomplex skills).ImplicationsFor the emergencymedical pr<strong>of</strong>essional, thereare several implications <strong>of</strong> SNSresearch. The most obvious:The EMS operational environmentisn’t compatible with theoperational requirement <strong>of</strong> pre cisionmotor skills. Precision—<strong>from</strong> perception, to analyticalprocessing, to motorskills—will be inhibitedif not totally lost when theSNS is triggered, and this factmust be incorporated into training.EMS crews must be trainedto control the SNS, and teammembers must be taught to scan for signs <strong>of</strong> SNS activation amongcrewmembers, so they can step in when necessary.The next implication centers on the design and development <strong>of</strong> amedical kit. The SNS narrows visual perception, so personnel willoverlook products if the kit isn’t laid out in a system conducive totrauma priorities. The loss <strong>of</strong> fine and complex motor skills mustalso be made a priority, as the SNS inhibits the ability to manipulatesmall, smooth objects that become slippery.Finally, SNS research reveals the liability related to humanerror. This research has been used dozens <strong>of</strong> times to defend police<strong>of</strong>ficers, pilots and soldiers who were victim to their SNS. The bottomline: There will be times when a good operator makes a mistake,but the mistake is due to uncontrollable factors that triggered theSNS. The ramifications <strong>of</strong> this research not only impact the agency’sfinances, but also the guilt an emergency medical pr<strong>of</strong>essional maycarry for life. On more than one occasion, I’ve given a lecture onextreme performance human factors and have been posed the followingquestion <strong>from</strong> an audience member: “Then there’s nothingwrong with me?”In each case the question came <strong>from</strong> someone who had been carryingunnecessary guilt that was as heavy as any cross you couldcarry. This research should be considered preventative medicine.Bruce Siddle is a 20-year (plus) law enforcement veteran specializingin training and survival human factors. He is the founder <strong>of</strong> PPCTManagement Systems and the managing partner <strong>of</strong> Warrior ScienceGroup. Siddle has been a consultant for hundreds <strong>of</strong> criminal justice andpublic safety agencies, including the U. S. Department <strong>of</strong> State’s DiplomaticSecurity Service, FBI’s Hostage Rescue Unit, U. S. Secret Service CounterAssault Team, the Transportation Security Agency, U.S. Armed Forcesand the Queen <strong>of</strong> England’s personal protection unit. He is the author<strong>of</strong> Sharpening the Warrior’s Edge and is working on a secondtext, Warrior Science, The Study <strong>of</strong> Combat Human Factors.Siddle has reported receiving honoraria and/or research support,either directly or indirectly, <strong>from</strong> the sponsor <strong>of</strong> this supplement,North American Rescue.The author would like to thank Sean McKay, Dave Grossman andDr. Steve Stahle for their assistance in preparing this article.EMS Rapid Deployment KitTrauma Kit Designed for OptimalUse under Operational StressElsevier Public Safety War on Trauma 31