Hereditary Angioedema - BMC HealthNet Plan
Hereditary Angioedema - BMC HealthNet Plan
Hereditary Angioedema - BMC HealthNet Plan
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
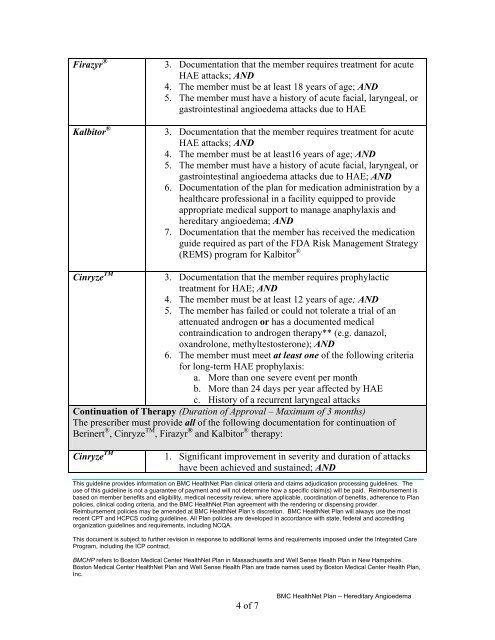
Firazyr ®Kalbitor ®3. Documentation that the member requires treatment for acuteHAE attacks; AND4. The member must be at least 18 years of age; AND5. The member must have a history of acute facial, laryngeal, orgastrointestinal angioedema attacks due to HAE3. Documentation that the member requires treatment for acuteHAE attacks; AND4. The member must be at least16 years of age; AND5. The member must have a history of acute facial, laryngeal, orgastrointestinal angioedema attacks due to HAE; AND6. Documentation of the plan for medication administration by ahealthcare professional in a facility equipped to provideappropriate medical support to manage anaphylaxis andhereditary angioedema; AND7. Documentation that the member has received the medicationguide required as part of the FDA Risk Management Strategy(REMS) program for Kalbitor ®Cinryze TM3. Documentation that the member requires prophylactictreatment for HAE; AND4. The member must be at least 12 years of age; AND5. The member has failed or could not tolerate a trial of anattenuated androgen or has a documented medicalcontraindication to androgen therapy** (e.g. danazol,oxandrolone, methyltestosterone); AND6. The member must meet at least one of the following criteriafor long-term HAE prophylaxis:a. More than one severe event per monthb. More than 24 days per year affected by HAEc. History of a recurrent laryngeal attacksContinuation of Therapy (Duration of Approval – Maximum of 3 months)The prescriber must provide all of the following documentation for continuation ofBerinert ® , Cinryze TM , Firazyr ® and Kalbitor ® therapy:Cinryze TM1. Significant improvement in severity and duration of attackshave been achieved and sustained; ANDThis guideline provides information on <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> clinical criteria and claims adjudication processing guidelines. Theuse of this guideline is not a guarantee of payment and will not determine how a specific claim(s) will be paid. Reimbursement isbased on member benefits and eligibility, medical necessity review, where applicable, coordination of benefits, adherence to <strong>Plan</strong>policies, clinical coding criteria, and the <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> agreement with the rendering or dispensing provider.Reimbursement policies may be amended at <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong>’s discretion. <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> will always use the mostrecent CPT and HCPCS coding guidelines. All <strong>Plan</strong> policies are developed in accordance with state, federal and accreditingorganization guidelines and requirements, including NCQA.This document is subject to further revision in response to additional terms and requirements imposed under the Integrated CareProgram, including the ICP contract.<strong>BMC</strong>HP refers to Boston Medical Center <strong>HealthNet</strong> <strong>Plan</strong> in Massachusetts and Well Sense Health <strong>Plan</strong> in New Hampshire.Boston Medical Center <strong>HealthNet</strong> <strong>Plan</strong> and Well Sense Health <strong>Plan</strong> are trade names used by Boston Medical Center Health <strong>Plan</strong>,Inc.4 of 7<strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> – <strong>Hereditary</strong> <strong>Angioedema</strong>