Hereditary Angioedema - BMC HealthNet Plan
Hereditary Angioedema - BMC HealthNet Plan
Hereditary Angioedema - BMC HealthNet Plan
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
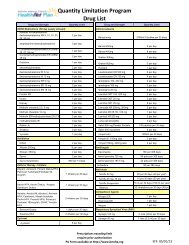
Berinert ® ,Firazyr ® , andKalbitor ®2. Clinical documentation of functional improvement have beenachieved and sustained.1. Significant improvement in severity and duration of attackshave been achieved and sustained; AND2. The member is receiving prophylactic therapy with attenuatedandrogens or C1 INH if the member has filled Berinert ® ,Firazyr ® or Kalbitor ® more than once per month for 3 of thelast 6 months (as evidenced by pharmacy claims)3. Documentation of member adherence to prophylactic therapyfor HAE if applicable.*<strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> will NOT approve coverage of Berinert ® , Cinryze TM , andKalbitor ® for the treatment or prevention of angioedema due to causes other thanHAE.**Adherence to prescribed androgen therapy must be confirmed by prescriptionclaims. If the member is new to <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> and does not have a prescriptionclaims history, the prescriber must certify that the member has been adherent to theprescribed androgen therapy.Quantity Limitations Apply – see Appendix AApplicable Coding:J-CodeMedicationJ0597 C1 esterase inhibitor (human), 10 units (Berinert ® )J0598 C1 esterase inhibitor (human) 10 units (Cinryze TM )J1290 Ecallantide 1mg (Kalbitor ® )--- Icantibant (Firazyr ® )Limitations:<strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> will not approve coverage of Berinert ® , Cinryze TM , Firazyr ® andKalbitor ® in the following instances:1. When the above criteria are not met.This guideline provides information on <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> clinical criteria and claims adjudication processing guidelines. Theuse of this guideline is not a guarantee of payment and will not determine how a specific claim(s) will be paid. Reimbursement isbased on member benefits and eligibility, medical necessity review, where applicable, coordination of benefits, adherence to <strong>Plan</strong>policies, clinical coding criteria, and the <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> agreement with the rendering or dispensing provider.Reimbursement policies may be amended at <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong>’s discretion. <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> will always use the mostrecent CPT and HCPCS coding guidelines. All <strong>Plan</strong> policies are developed in accordance with state, federal and accreditingorganization guidelines and requirements, including NCQA.This document is subject to further revision in response to additional terms and requirements imposed under the Integrated CareProgram, including the ICP contract.<strong>BMC</strong>HP refers to Boston Medical Center <strong>HealthNet</strong> <strong>Plan</strong> in Massachusetts and Well Sense Health <strong>Plan</strong> in New Hampshire.Boston Medical Center <strong>HealthNet</strong> <strong>Plan</strong> and Well Sense Health <strong>Plan</strong> are trade names used by Boston Medical Center Health <strong>Plan</strong>,Inc.5 of 7<strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> – <strong>Hereditary</strong> <strong>Angioedema</strong>