Instructions on how to fill out the CMS 1500 Form - LA Care Health ...
Instructions on how to fill out the CMS 1500 Form - LA Care Health ...
Instructions on how to fill out the CMS 1500 Form - LA Care Health ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
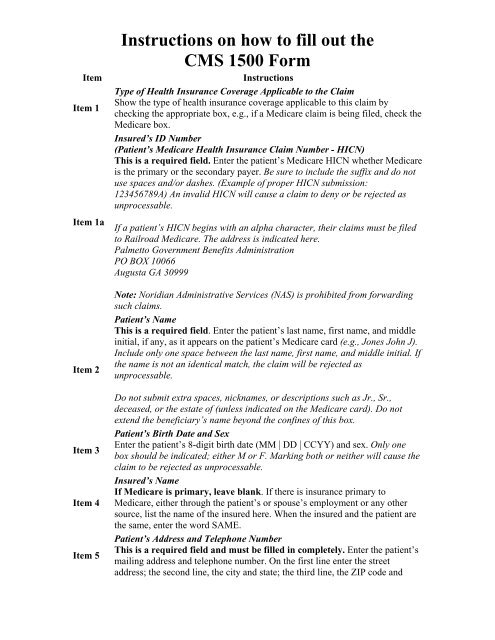
ItemItem 1Item 1aItem 2Item 3Item 4Item 5<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong><str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g>Type of <strong>Health</strong> Insurance Coverage Applicable <strong>to</strong> <strong>the</strong> ClaimS<strong>how</strong> <strong>the</strong> type of health insurance coverage applicable <strong>to</strong> this claim bychecking <strong>the</strong> appropriate box, e.g., if a Medicare claim is being filed, check <strong>the</strong>Medicare box.Insured’s ID Number(Patient’s Medicare <strong>Health</strong> Insurance Claim Number - HICN)This is a required field. Enter <strong>the</strong> patient’s Medicare HICN whe<strong>the</strong>r Medicareis <strong>the</strong> primary or <strong>the</strong> sec<strong>on</strong>dary payer. Be sure <strong>to</strong> include <strong>the</strong> suffix and do notuse spaces and/or dashes. (Example of proper HICN submissi<strong>on</strong>:123456789A) An invalid HICN will cause a claim <strong>to</strong> deny or be rejected asunprocessable.If a patient’s HICN begins with an alpha character, <strong>the</strong>ir claims must be filed<strong>to</strong> Railroad Medicare. The address is indicated here.Palmet<strong>to</strong> Government Benefits Administrati<strong>on</strong>PO BOX 10066Augusta GA 30999Note: Noridian Administrative Services (NAS) is prohibited from forwardingsuch claims.Patient’s NameThis is a required field. Enter <strong>the</strong> patient’s last name, first name, and middleinitial, if any, as it appears <strong>on</strong> <strong>the</strong> patient’s Medicare card (e.g., J<strong>on</strong>es John J).Include <strong>on</strong>ly <strong>on</strong>e space between <strong>the</strong> last name, first name, and middle initial. If<strong>the</strong> name is not an identical match, <strong>the</strong> claim will be rejected asunprocessable.Do not submit extra spaces, nicknames, or descripti<strong>on</strong>s such as Jr., Sr.,deceased, or <strong>the</strong> estate of (unless indicated <strong>on</strong> <strong>the</strong> Medicare card). Do notextend <strong>the</strong> beneficiary’s name bey<strong>on</strong>d <strong>the</strong> c<strong>on</strong>fines of this box.Patient’s Birth Date and SexEnter <strong>the</strong> patient’s 8-digit birth date (MM | DD | CCYY) and sex. Only <strong>on</strong>ebox should be indicated; ei<strong>the</strong>r M or F. Marking both or nei<strong>the</strong>r will cause <strong>the</strong>claim <strong>to</strong> be rejected as unprocessable.Insured’s NameIf Medicare is primary, leave blank. If <strong>the</strong>re is insurance primary <strong>to</strong>Medicare, ei<strong>the</strong>r through <strong>the</strong> patient’s or spouse’s employment or any o<strong>the</strong>rsource, list <strong>the</strong> name of <strong>the</strong> insured here. When <strong>the</strong> insured and <strong>the</strong> patient are<strong>the</strong> same, enter <strong>the</strong> word SAME.Patient’s Address and Teleph<strong>on</strong>e NumberThis is a required field and must be <strong>fill</strong>ed in completely. Enter <strong>the</strong> patient’smailing address and teleph<strong>on</strong>e number. On <strong>the</strong> first line enter <strong>the</strong> streetaddress; <strong>the</strong> sec<strong>on</strong>d line, <strong>the</strong> city and state; <strong>the</strong> third line, <strong>the</strong> ZIP code and
Item 6Item 7Item 8<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>teleph<strong>on</strong>e number.Patient’s Relati<strong>on</strong>ship <strong>to</strong> InsuredIf Medicare is primary, leave blank. Check <strong>the</strong> appropriate box for <strong>the</strong>patient’s relati<strong>on</strong>ship <strong>to</strong> <strong>the</strong> insured when item 4 is completed.Insurance Primary <strong>to</strong> Medicare, Insured’s Address and Teleph<strong>on</strong>e NumberComplete this item <strong>on</strong>ly when items 4, 6, and 11 are completed. Enter <strong>the</strong>insured’s address and teleph<strong>on</strong>e number. When <strong>the</strong> address is <strong>the</strong> same as <strong>the</strong>patient’s, enter <strong>the</strong> word SAME.Patient’s Marital Status and Whe<strong>the</strong>r Employed or a StudentCheck <strong>the</strong> appropriate box for <strong>the</strong> patient’s marital status and whe<strong>the</strong>remployed or a student.Medigap Benefits, O<strong>the</strong>r Insured’s NameIf no Medigap benefits are assigned, leave blank. Enter <strong>the</strong> last name, firstname, and middle initial of <strong>the</strong> enrollee in a Medigap policy if it is differentfrom that s<strong>how</strong>n in item 2. O<strong>the</strong>rwise, enter <strong>the</strong> word SAME. This field maybe used in <strong>the</strong> future for supplemental insurance plans.NOTE: Only Participating Physicians and Suppliers are <strong>to</strong> complete item 9and its subdivisi<strong>on</strong>s and <strong>on</strong>ly when <strong>the</strong> Beneficiary wishes <strong>to</strong> assign his/herbenefits under a MEDIGAP policy <strong>to</strong> <strong>the</strong> Participating Physician or Supplier.Item 9Participating physicians and suppliers must enter informati<strong>on</strong> required in item9 and its subdivisi<strong>on</strong>s if requested by <strong>the</strong> beneficiary. Participatingphysicians/suppliers sign an agreement with Medicare <strong>to</strong> accept assignment ofMedicare benefits for all Medicare patients. A claim for which a beneficiaryelects <strong>to</strong> assign his/her benefits under a Medigap policy <strong>to</strong> a participatingphysician/supplier is called a mandated Medigap transfer. (See chapter 28 of<strong>the</strong> Medicare Claims Processing Manual.)Medigap - Medigap policy meets <strong>the</strong> statu<strong>to</strong>ry definiti<strong>on</strong> of a “Medicaresupplemental policy” c<strong>on</strong>tained in §1882(g)(1) of title XVIII of <strong>the</strong> SocialSecurity Act (<strong>the</strong> Act) and <strong>the</strong> definiti<strong>on</strong> c<strong>on</strong>tained in <strong>the</strong> NAIC ModelRegulati<strong>on</strong> that is incorporated by reference <strong>to</strong> <strong>the</strong> statute. It is a healthinsurance policy or o<strong>the</strong>r health benefit plan offered by a private entity <strong>to</strong> thosepers<strong>on</strong>s entitled <strong>to</strong> Medicare benefits and is specifically designed <strong>to</strong>supplement Medicare benefits. It <strong>fill</strong>s in some of <strong>the</strong> “gaps” in Medicarecoverage by providing payment for some of <strong>the</strong> charges for which Medicaredoes not have resp<strong>on</strong>sibility due <strong>to</strong> <strong>the</strong> applicability of deductibles,coinsurance amounts, or o<strong>the</strong>r limitati<strong>on</strong>s imposed by Medicare. It does notinclude limited benefit coverage available <strong>to</strong> Medicare beneficiaries such as“specified disease” or “hospital indemnity” coverage. Also, it explicitlyexcludes a policy or plan offered by an employer <strong>to</strong> employees or formeremployees, as well as that offered by a labor organizati<strong>on</strong> <strong>to</strong> members or
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>former members.Item 9aItem 9bItem 9cItem 9dItems10a–10cDo not list o<strong>the</strong>r supplemental coverage in item 9 and its subdivisi<strong>on</strong>s at <strong>the</strong>time a Medicare claim is filed. O<strong>the</strong>r supplemental claims are forwardedau<strong>to</strong>matically <strong>to</strong> <strong>the</strong> private insurer if <strong>the</strong> private insurer c<strong>on</strong>tracts with <strong>the</strong>carrier <strong>to</strong> send Medicare claim informati<strong>on</strong> electr<strong>on</strong>ically. If <strong>the</strong>re is no suchc<strong>on</strong>tract, <strong>the</strong> beneficiary must file his/her own supplemental claim.Medigap Benefits, O<strong>the</strong>r Insured’s Policy or Group NumberIf no Medigap benefits are assigned, leave blank. Enter <strong>the</strong> policy and/orgroup number of <strong>the</strong> Medigap insured preceded by MEDIGAP, MG, orMGAP. Do not enter o<strong>the</strong>r types of insurance (e.g., supplemental).NOTE: Item 9d must be completed if <strong>the</strong> provider enters a policy and/orgroup number in item 9a.Medigap Benefits, O<strong>the</strong>r Insured’s Date of BirthEnter <strong>the</strong> Medigap insured’s 8-digit birth date (MM | DD | CCYY) and sex.Medigap Benefits, Employer’s/School NameIf a Medigap PayerID is entered in item 9d, leave blank. O<strong>the</strong>rwise, enter<strong>the</strong> claims processing address of <strong>the</strong> Medigap insurer. Use an abbreviatedstreet address, two-letter postal code and ZIP code copied from <strong>the</strong> Medigapinsured’s Medigap identificati<strong>on</strong> card. For example:1257 Anywhere StreetBaltimore MD 21204is s<strong>how</strong>n as: 1257 Anywhere St. MD 21204Medigap Benefits, Insurance Plan/Program Name, PAYERID NumberEnter <strong>the</strong> nine-digit PAYERID number of <strong>the</strong> Medigap insurer. If noPAYERID number exists, <strong>the</strong>n enter <strong>the</strong> Medigap insurance program or planname.If <strong>the</strong> beneficiary wants Medicare payment data forwarded <strong>to</strong> a Medigapinsurer under a mandated Medigap transfer, <strong>the</strong> participating provider orsupplier must accurately complete all of <strong>the</strong> informati<strong>on</strong> in items 9, 9a, 9b, and9d. O<strong>the</strong>rwise, <strong>the</strong> Medicare carrier cannot forward <strong>the</strong> claim informati<strong>on</strong> <strong>to</strong><strong>the</strong> Medigap insurer.NOTE: The c<strong>on</strong>figurati<strong>on</strong> of <strong>the</strong> PAYERID is alpha numeric and up <strong>to</strong> 9digits. NAS assigns five digit alpha numeric or numeric PAYERID numbersra<strong>the</strong>r than nine digit numbers.C<strong>on</strong>diti<strong>on</strong> Relati<strong>on</strong>ship? Employment, Au<strong>to</strong> Liability, or O<strong>the</strong>r AccidentCheck “YES” or “NO” by placing an (X) in <strong>the</strong> center of <strong>the</strong> box <strong>to</strong> indicatewhe<strong>the</strong>r employment, au<strong>to</strong> liability, or o<strong>the</strong>r accident involvement applies <strong>to</strong><strong>on</strong>e or more of <strong>the</strong> services described in item 24. Enter <strong>the</strong> State postal code.Any item checked “YES,” indicates <strong>the</strong>re may be o<strong>the</strong>r insurance primary <strong>to</strong>Medicare. Identify primary insurance informati<strong>on</strong> in item 11.
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>Item 10d Leave blank. Not required by NAS.Insured’s Policy Group or FECA NumberNote: All claims can be submitted electr<strong>on</strong>ically. For more informati<strong>on</strong>pleaser refer <strong>to</strong> <strong>the</strong> EDISS web site.THIS ITEM MUST BE COMPLETED, IT IS A REQUIRED FIELD. BYCOMPLETING THIS ITEM, THE PHYSICIAN/SUPPLIERACKNOWLEDGES HAVING MADE A GOOD FAITH EFFORT TODETERMINE WHETHER MEDICARE IS THE PRIMARY ORSECONDARY PAYER.If <strong>the</strong>re is insurance primary <strong>to</strong> Medicare for <strong>the</strong> service date(s), enter <strong>the</strong>insured’s policy or group number within <strong>the</strong> c<strong>on</strong>fines of <strong>the</strong> box and proceed <strong>to</strong>items 11a–11c. Items 4, 6, and 7 must also be completed. If item 11 is leftblank, <strong>the</strong> claim will be denied as unprocessable.NOTE: Enter <strong>the</strong> appropriate informati<strong>on</strong> in item 11c if insurance primary <strong>to</strong>Medicare is indicated in item 11.If <strong>the</strong>re is no insurance primary <strong>to</strong> Medicare, do not enter “n/a,” “not,” etc.,enter <strong>the</strong> word NONE within <strong>the</strong> c<strong>on</strong>fines of <strong>the</strong> box and proceed <strong>to</strong> item 12.Item 11If <strong>the</strong> insured reports a terminating event with regard <strong>to</strong> insurance which hadbeen primary <strong>to</strong> Medicare (e.g., insured retired), enter <strong>the</strong> word NONE andproceed <strong>to</strong> item 11b.If a lab has collected previously and retained MSP informati<strong>on</strong> for abeneficiary, <strong>the</strong> lab may use that informati<strong>on</strong> for billing purposes of <strong>the</strong> n<strong>on</strong>face-<strong>to</strong>-facelab service. If <strong>the</strong> lab has no MSP informati<strong>on</strong> for <strong>the</strong> beneficiary,<strong>the</strong> lab will enter <strong>the</strong> word NONE in item 11 of <strong>the</strong> <strong>CMS</strong>-<strong>1500</strong> <strong>Form</strong>, whensubmitting a claim for payment of a reference lab service. Where <strong>the</strong>re hasbeen no face-<strong>to</strong>-face encounter with <strong>the</strong> beneficiary <strong>the</strong> claim will <strong>the</strong>n follow<strong>the</strong> normal claims process. When a lab has a face-<strong>to</strong>-face encounter with abeneficiary, <strong>the</strong> lab is expected <strong>to</strong> collect <strong>the</strong> MSP informati<strong>on</strong> and billaccordingly.Insurance Primary <strong>to</strong> Medicare - Circumstances under which Medicarepayment may be sec<strong>on</strong>dary <strong>to</strong> o<strong>the</strong>r insurance include:• Group <strong>Health</strong> Plan Coverageo Working Aged (Type 12);o Disability (Large Group <strong>Health</strong> Plan – Type 43); ando End Stage Renal Disease (ESRD – Type 13);• No Fault (Type 14) and/or O<strong>the</strong>r Liability (Type 47); and• Work-Related Illness/Injury:
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>NOTE: This can be Signature <strong>on</strong> File and/or a computer generated signature.The patient’s signature authorizes release of medical informati<strong>on</strong> necessary <strong>to</strong>process <strong>the</strong> claim. It also authorizes payment of benefits <strong>to</strong> <strong>the</strong> provider ofservice or supplier when <strong>the</strong> provider of service or supplier accepts assignment<strong>on</strong> <strong>the</strong> claim.Item 13Signature by Mark (X) - When an illiterate or physically handicappedenrollee signs by mark, a witness must enter his/her name and address next <strong>to</strong><strong>the</strong> mark.Medigap Benefits, Insured’s/Authorized Pers<strong>on</strong>’s SignatureThe signature in this item authorizes payment of mandated Medigap benefits<strong>to</strong> <strong>the</strong> participating physician or supplier if required Medigap informati<strong>on</strong> isincluded in item 9 and its subdivisi<strong>on</strong>s. The patient or his/her authorizedrepresentative signs this item or <strong>the</strong> signature must be <strong>on</strong> file as a separateMedigap authorizati<strong>on</strong>. The Medigap assignment <strong>on</strong> file in <strong>the</strong> participatingprovider of service/supplier’s office must be insurer specific. It may state that<strong>the</strong> authorizati<strong>on</strong> applies <strong>to</strong> all occasi<strong>on</strong>s of service until it is revoked.NOTE: This can be Signature <strong>on</strong> File and/or a computer generated signature.Date of Current Illness/Injury/PregnancyItem 14• For current illness, injury, or pregnancy, enter ei<strong>the</strong>r an 8-digit(MM | DD | CCYY) or 6-digit (MM | DD | YY) date.• For chiropractic services, enter an 8-digit (MM | DD | CCYY) or 6-digit (MM | DD | YY) date of <strong>the</strong> initiati<strong>on</strong> of <strong>the</strong> course of treatmentand enter an 8-digit (MM | DD | CCYY) or 6-digit (MM | DD | YY)date of x-ray (if used <strong>to</strong> dem<strong>on</strong>strate subluxati<strong>on</strong>) in item 19.Item 15Item 16Item 17Leave blank. Not required by Medicare.Dates Patient Unable <strong>to</strong> Work in Current Occupati<strong>on</strong>If <strong>the</strong> patient is employed and is unable <strong>to</strong> work in his/her current occupati<strong>on</strong>,enter an 8-digit (MM | DD | CCYY) or 6-digit (MM | DD | YY) date when <strong>the</strong>patient is unable <strong>to</strong> work.An entry in this field may indicate employment related insurance coverage.Name of <strong>the</strong> Referring or Ordering PhysicianEnter <strong>the</strong> name of <strong>the</strong> referring or ordering physician if <strong>the</strong> service or item wasordered or referred by a physician. Use <strong>the</strong> physician’s last name and as muchof <strong>the</strong> first name as will fit in item 17. Do not use “self,” “friend,” etc.The term “physician” when used within <strong>the</strong> meaning of §1861(r) of <strong>the</strong> Actand used in c<strong>on</strong>necti<strong>on</strong> with performing any functi<strong>on</strong> or acti<strong>on</strong> refers <strong>to</strong>:
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>1. A doc<strong>to</strong>r of medicine or osteopathy legally authorized <strong>to</strong> practicemedicine and surgery by <strong>the</strong> State in which he/she performs suchfuncti<strong>on</strong> or acti<strong>on</strong>;2. A doc<strong>to</strong>r of dental surgery or dental medicine who is legally authorized<strong>to</strong> practice dentistry by <strong>the</strong> State in which he/she performs suchfuncti<strong>on</strong>s and who is acting within <strong>the</strong> scope of his/her license whenperforming such functi<strong>on</strong>s;3. A doc<strong>to</strong>r of podiatric medicine for purposes of §§(k), (m), (p)(1), and(s) and §§1814(a), 1832(a)(2)(F)(ii), and 1835 of <strong>the</strong> Act, but <strong>on</strong>ly withrespect <strong>to</strong> functi<strong>on</strong>s which he/she is legally authorized <strong>to</strong> perform assuch by <strong>the</strong> State in which he/she performs <strong>the</strong>m;4. A doc<strong>to</strong>r of op<strong>to</strong>metry, but <strong>on</strong>ly with respect <strong>to</strong> <strong>the</strong> provisi<strong>on</strong> of itemsor services described in §1861(s) of <strong>the</strong> Act which he/she is legallyauthorized <strong>to</strong> perform as a doc<strong>to</strong>r of op<strong>to</strong>metry by <strong>the</strong> State in whichhe/she performs <strong>the</strong>m; or5. A chiroprac<strong>to</strong>r who is licensed as such by a State (or in a State whichdoes not license chiroprac<strong>to</strong>rs as such), and is legally authorized <strong>to</strong>perform <strong>the</strong> services of a chiroprac<strong>to</strong>r in <strong>the</strong> jurisdicti<strong>on</strong> in whichhe/she performs such services, and who meets uniform minimumstandards specified by <strong>the</strong> Secretary, but <strong>on</strong>ly for purposes of§§1861(s)(1) and 1861(s)(2)(A) of <strong>the</strong> Act, and <strong>on</strong>ly with respect <strong>to</strong>treatment by means of manual manipulati<strong>on</strong> of <strong>the</strong> spine (<strong>to</strong> correct asubluxati<strong>on</strong>). For <strong>the</strong> purposes of §1862(a)(4) of <strong>the</strong> Act and subject <strong>to</strong><strong>the</strong> limitati<strong>on</strong>s and c<strong>on</strong>diti<strong>on</strong>s provided above, chiroprac<strong>to</strong>r includes adoc<strong>to</strong>r of <strong>on</strong>e of <strong>the</strong> arts specified in <strong>the</strong> statute and legally authorized<strong>to</strong> practice such art in <strong>the</strong> country in which <strong>the</strong> inpatient hospitalservices (referred <strong>to</strong> in §1862(a)(4) of <strong>the</strong> Act) are furnished.Referring physician - is a physician who requests an item or service for <strong>the</strong>beneficiary for which payment may be made under <strong>the</strong> Medicare program.Ordering physician - is a physician or, when appropriate, a n<strong>on</strong>-physicianpractiti<strong>on</strong>er who orders n<strong>on</strong>-physician services for <strong>the</strong> patient. See Pub. 100-02, Medicare Benefit Policy Manual, Chapter 15, for n<strong>on</strong>-physicianpractiti<strong>on</strong>er rules. Examples of services that might be ordered includediagnostic labora<strong>to</strong>ry tests, clinical labora<strong>to</strong>ry tests, pharmaceutical services,durable medical equipment, and services incident <strong>to</strong> that physician’s or n<strong>on</strong>physicianpractiti<strong>on</strong>er’s service.The ordering/referring requirement became effective January 1, 1992, and isrequired by Secti<strong>on</strong> 1833(q) of <strong>the</strong> Social Security Act. All claims forMedicare covered services and items that are <strong>the</strong> result of a physician’s orderor referral shall include <strong>the</strong> ordering/referring physician’s name. See items 17aand 17b below for fur<strong>the</strong>r guidance <strong>on</strong> reporting <strong>the</strong> referring/orderingprovider’s UPIN and/or NPI. The following services/situati<strong>on</strong>s require <strong>the</strong>
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>submissi<strong>on</strong> of <strong>the</strong> referring/ordering provider informati<strong>on</strong>:• Medicare covered services and items that result from a physician’sorder or referral;• Parenteral and enteral nutriti<strong>on</strong>;• Immunosuppressive drug claims;• Hepatitis B claims;• Diagnostic labora<strong>to</strong>ry services;• Diagnostic radiology services;• Portable x-ray services;• C<strong>on</strong>sultative services;• Durable medical equipment;• When <strong>the</strong> ordering physician is also <strong>the</strong> performing physician (as oftenis <strong>the</strong> case with in-office clinical labora<strong>to</strong>ry tests);• When a service is incident <strong>to</strong> <strong>the</strong> service of a physician or n<strong>on</strong>physicianpractiti<strong>on</strong>er, <strong>the</strong> name of <strong>the</strong> physician or n<strong>on</strong>-physicianpractiti<strong>on</strong>er who performs <strong>the</strong> initial service and orders <strong>the</strong> n<strong>on</strong>physicianservice must appear in item 17;• When a physician extender or o<strong>the</strong>r limited licensed practiti<strong>on</strong>er refersa patient for c<strong>on</strong>sultative service, submit <strong>the</strong> name of <strong>the</strong> physician whois supervising <strong>the</strong> limited licensed practiti<strong>on</strong>er.Do not extend <strong>the</strong> name bey<strong>on</strong>d <strong>the</strong> c<strong>on</strong>fines of this box. Only enter what willfit in<strong>to</strong> item 17. Do not run <strong>the</strong> name in<strong>to</strong> item 17a or 17b.UPIN of <strong>the</strong> Referring/Ordering PhysicianEnter <strong>the</strong> ID Qualifier 1G in <strong>the</strong> smaller box and <strong>the</strong> <strong>CMS</strong> assigned UPIN of<strong>the</strong> referring/ordering physician listed in item 17 in <strong>the</strong> larger box. The 1G andUPIN must be submitted within <strong>the</strong> c<strong>on</strong>fines of <strong>the</strong> appropriate boxes. TheUPIN may be reported <strong>on</strong> <strong>the</strong> <strong>CMS</strong>-<strong>1500</strong> <strong>Form</strong> until May 22, 2007, andMUST be reported if an NPI is not available. An invalid UPIN format willcause <strong>the</strong> claim <strong>to</strong> be rejected as unprocessable.Item 17aAttenti<strong>on</strong> Providers: Effective immediately providers should include both <strong>the</strong>UPIN and <strong>the</strong> NPI of <strong>the</strong> referring physician. For claims received after July2, 2007, providers may enter <strong>on</strong>ly <strong>the</strong> NPI number of <strong>the</strong> referring physician.NOTE: <strong>CMS</strong> has announced that it is implementing a c<strong>on</strong>tingency plan forall covered entities that will not meet <strong>the</strong> May 23, 2007 deadline for NPI. Fora complete overview of <strong>the</strong> <strong>CMS</strong> C<strong>on</strong>tingency plan and related informati<strong>on</strong>,visit: http://www.cms.hhs.gov/nati<strong>on</strong>alprovidentstand/NOTE: Field 17a and/or 17b is required when a service was ordered orreferred by a physician. Effective May 23, 2007, and later, 17a is not <strong>to</strong> bereported but 17b MUST be reported when a service was ordered or referred bya physician.
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>When “yes” is annotated, item 32 must be completed. When billing formultiple purchased diagnostic tests, each test must be submitted <strong>on</strong> aseparate <strong>CMS</strong>-<strong>1500</strong> <strong>Form</strong>.Patient’s Diagnosis/C<strong>on</strong>diti<strong>on</strong>Enter <strong>the</strong> patient’s diagnosis/c<strong>on</strong>diti<strong>on</strong>. With <strong>the</strong> excepti<strong>on</strong> of claims submittedby ambulance suppliers (specialty type 59), all physician and n<strong>on</strong>-physicianspecialties (i.e., PA, NP, CNS, CRNA) must use an ICD-9-CM code numberand code <strong>to</strong> <strong>the</strong> highest level of specificity for <strong>the</strong> date of service. Enter up <strong>to</strong>four diagnoses in priority order. All narrative diagnoses for n<strong>on</strong>-physicianspecialties shall be submitted <strong>on</strong> an attachment.NOTE: Although ambulance suppliers are not required <strong>to</strong> submit ICD-9 codes<strong>on</strong> <strong>the</strong> claim, NAS highly encourages <strong>the</strong>m <strong>to</strong> do so with <strong>the</strong> code that bestdescribes <strong>the</strong> sign, symp<strong>to</strong>m, and/or c<strong>on</strong>diti<strong>on</strong> of <strong>the</strong> beneficiary at <strong>the</strong> time oftransport.Item 21Item 22Item 23Enter <strong>the</strong> diagnosis code <strong>on</strong>ly, not <strong>the</strong> descripti<strong>on</strong>. Any extraneous data inthis field will cause an up fr<strong>on</strong>t rejecti<strong>on</strong> of your claim. Do not use decimalpoints.NOTE: You may place up <strong>to</strong> eight diagnosis codes <strong>on</strong> <strong>the</strong> claim form. Thediagnosis that is pointed <strong>to</strong> in Item 24E must be placed in <strong>on</strong>e of <strong>the</strong> first fourdiagnoses entry spaces in Item 21. Any indica<strong>to</strong>r o<strong>the</strong>r than a 1, 2, 3, or 4 inItem 24E will cause <strong>the</strong> claim <strong>to</strong> deny as unprocessable. Place additi<strong>on</strong>aldiagnosis codes 5-8 (if necessary) in Item 19. Enter <strong>on</strong>ly <strong>the</strong> number (withdecimal if needed) and separate each diagnosis in Item 19 with a comma. [Forexample: 719.41, 719.42, 816.00]The diagnosis codes listed in Item 19 should not be for codes that arerequired for payment, submit a sec<strong>on</strong>d claim form with <strong>the</strong> additi<strong>on</strong>alrequired codes in Item 21. [For example: if CPT code “A” requires threediagnosis codes for payment and CPT “B” requires three different codes forpayment, <strong>the</strong>se two procedures would need <strong>to</strong> be billed <strong>on</strong> two separate claimforms so <strong>the</strong> processing system could pick up all six of <strong>the</strong> diagnosis codes aspayable.]Leave blank. Not required by MedicarePrior Authorizati<strong>on</strong> NumberThis is a required field for <strong>the</strong> purposes <strong>out</strong>lined below.• Enter <strong>the</strong> Quality Improvement Organizati<strong>on</strong> (QIO) prior authorizati<strong>on</strong>number for those procedures requiring QIO prior approval.• Enter <strong>the</strong> Investigati<strong>on</strong>al Device Exempti<strong>on</strong> (IDE) number when aninvestigati<strong>on</strong>al device is used in an FDA-approved clinical trial. PostMarket Approval number should also be placed here when applicable.
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>• Enter <strong>the</strong> 10-digit Clinical Labora<strong>to</strong>ry Improvement Act (CLIA)certificati<strong>on</strong> number for labora<strong>to</strong>ry services billed by an entityperforming CLIA covered procedures.• Enter <strong>the</strong> ZIP code for <strong>the</strong> point of pickup for ambulance claims.Because <strong>the</strong> ZIP code is used for pricing, more than <strong>on</strong>e ambulanceservice may be reported <strong>on</strong> <strong>the</strong> same claim for a beneficiary if allpoints of pickup are located in <strong>the</strong> same ZIP code. However, suppliersmust prepare a separate claim form for each trip if <strong>the</strong> points of pickupare located in different ZIP codes. A claim with<strong>out</strong> a ZIP code or withmultiple ZIP codes will be denied as unprocessable.NOTE: Item 23 can c<strong>on</strong>tain <strong>on</strong>ly <strong>on</strong>e c<strong>on</strong>diti<strong>on</strong>. Any additi<strong>on</strong>al c<strong>on</strong>diti<strong>on</strong>sshould be reported <strong>on</strong> a separate <strong>CMS</strong>-<strong>1500</strong> <strong>Form</strong>.Service LineThe six service lines in secti<strong>on</strong> 24 have been divided horiz<strong>on</strong>tally <strong>to</strong>accommodate submissi<strong>on</strong> of both <strong>the</strong> NPI and legacy identifier during <strong>the</strong> NPItransiti<strong>on</strong> and <strong>to</strong> accommodate <strong>the</strong> submissi<strong>on</strong> of supplemental informati<strong>on</strong> <strong>to</strong>support <strong>the</strong> billed service. The <strong>to</strong>p porti<strong>on</strong> in each of <strong>the</strong> six service lines isItem 24shaded and is <strong>the</strong> locati<strong>on</strong> for reporting supplemental informati<strong>on</strong>. It is notintended <strong>to</strong> allow <strong>the</strong> billing of 12 service lines. At this time, <strong>the</strong> shaded areain 24A through 24H is not used by Medicare. Future guidance will beprovided <strong>on</strong> when and <strong>how</strong> <strong>to</strong> use this shaded area for <strong>the</strong> submissi<strong>on</strong> ofMedicare claims.Date of ServiceThis is a required field. Enter a 6-digit (MMDDYY) or 8-digit(MMDDCCYY) date for each procedure, service, or supply within <strong>the</strong> c<strong>on</strong>finesof this box. When “from” and “<strong>to</strong>” dates are s<strong>how</strong>n for a series of identicalservices, enter <strong>the</strong> number of days or units in column G. Return asunprocessable if a date of service extends more than 1 day and a valid “<strong>to</strong>”Item 24A date is not present.Item 24BWhen billing a date span, it must be for c<strong>on</strong>secutive days. If it is not, <strong>the</strong>n billeach service separately. Days billed should corresp<strong>on</strong>d with <strong>the</strong> number ofunits in column G. If days span over a m<strong>on</strong>th, bill <strong>the</strong> services for each m<strong>on</strong>th<strong>on</strong> separate lines. Do not use quotati<strong>on</strong> marks <strong>to</strong> indicate <strong>the</strong> date of service is<strong>the</strong> same as <strong>the</strong> line above. A date must be reported in this item.Place of ServiceThis is a required field. Enter <strong>the</strong> appropriate 2-digit place of service code(s)from <strong>the</strong> list provided in Secti<strong>on</strong> 10.5 of <strong>the</strong> Medicare Claims ProcessingManual, Chapter 26. Identify <strong>the</strong> locati<strong>on</strong>, using a place of service code, foreach item used or service performed.NOTE: When a service is rendered <strong>to</strong> a hospital inpatient, use <strong>the</strong> “inpatient
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>hospital” code.Enter <strong>on</strong>ly <strong>on</strong>e place of service code per <strong>CMS</strong>-<strong>1500</strong> <strong>Form</strong>, unless <strong>the</strong> sec<strong>on</strong>dplace of service code is 12 (patient’s home).Item 24C Leave blank. Not required by Medicare.Procedures, Services, or Supplies CodeThis is a required field. Enter <strong>the</strong> procedures, services, or supplies using <strong>the</strong><strong>CMS</strong> <strong>Health</strong>care Comm<strong>on</strong> Procedure Coding System (HCPCS) code. Whenapplicable, s<strong>how</strong> HCPCS code modifiers with <strong>the</strong> HCPCS code. The <strong>CMS</strong>-<strong>1500</strong> <strong>Form</strong> has <strong>the</strong> ability <strong>to</strong> capture up <strong>to</strong> four modifiers.Item 24DItem 24EEnter <strong>the</strong> specific procedure code with<strong>out</strong> a narrative descripti<strong>on</strong>. However,when reporting an “unlisted procedure code” or a “not o<strong>the</strong>rwise classified”(NOC) code, include a narrative descripti<strong>on</strong> in item 19 if a coherentdescripti<strong>on</strong> can be given within <strong>the</strong> c<strong>on</strong>fines of that box. O<strong>the</strong>rwise, anattachment must be submitted with <strong>the</strong> claim.Return as unprocessable if an “unlisted procedure code” or a “not o<strong>the</strong>rwiseclassified” (NOC) code is indicated in item 24D, but an accompanyingnarrative is not present in item 19 or <strong>on</strong> an attachment.Modifiers must be two alpha/numeric characters. Do not place extra narrativeafter, under, or above <strong>the</strong> procedure code. Pricing modifiers should be placedin <strong>the</strong> first modifier positi<strong>on</strong>. Procedure codes should not be placed in <strong>the</strong> firstmodifier positi<strong>on</strong>. Be sure <strong>to</strong> distinguish between zeros and <strong>the</strong> letter “O”.Hyphens or any o<strong>the</strong>r separa<strong>to</strong>rs should not be used between procedure codesand modifiers. Only uppercase characters should be used for procedurecodes and modifiers.Diagnosis Code Reference NumberThis is a required field. Enter <strong>the</strong> diagnosis code reference number as s<strong>how</strong>nin item 21 <strong>to</strong> relate <strong>the</strong> date of service and <strong>the</strong> procedures performed <strong>to</strong> <strong>the</strong>primary diagnosis. Enter <strong>on</strong>ly <strong>on</strong>e reference number per line item. Whenmultiple services are performed, enter <strong>the</strong> primary reference number for eachservice, ei<strong>the</strong>r a 1, or a 2, or a 3, or a 4. Entering anything o<strong>the</strong>r than a 1, ora 2, or a 3, or a 4 will cause <strong>the</strong> claim <strong>to</strong> be rejected as unprocessable,If a situati<strong>on</strong> arises where two or more diagnoses are required for a procedurecode (e.g., pap smears), <strong>the</strong> provider shall reference <strong>on</strong>ly <strong>on</strong>e of <strong>the</strong>diagnoses in item 21.Place <strong>on</strong>ly a single diagnosis pointer <strong>on</strong> each line. Do not enter <strong>the</strong> ICD-9code(s) and/or diagnosis narratives in this item. The NAS processing systemis capable of referencing all diagnosis codes in item 21 as needed.Item 24F Enter <strong>the</strong> charge for each listed service
Item 24G<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>Enter <strong>the</strong> charge for each listed service. Include <strong>the</strong> cents with dollar amounts.For example, $24.00 must be entered as 2400 ra<strong>the</strong>r than 24 or 24-. Do notuse dollar signs, decimals, dashes, commas, or lines. Negative dollar amountsare not allowed.Note: Competitive Acquisiti<strong>on</strong> Program (CAP) physicians should enter abilled amount for each CAP drug. Do not enter a zero dollar amount.Days or UnitsEnter <strong>the</strong> number of days or units. This field is most comm<strong>on</strong>ly used formultiple visits, units of supplies, anes<strong>the</strong>sia minutes, or oxygen volume. If<strong>on</strong>ly <strong>on</strong>e service is performed, <strong>the</strong> numeral 1 must be entered.Some services require that <strong>the</strong> actual number or quantity billed be clearlyindicated <strong>on</strong> <strong>the</strong> claim form (e.g., multiple os<strong>to</strong>my or urinary supplies,medicati<strong>on</strong> dosages, or allergy testing procedures). When multiple services areprovided, enter <strong>the</strong> actual number provided.For anes<strong>the</strong>sia, s<strong>how</strong> <strong>the</strong> elapsed time (minutes) in item 24G. C<strong>on</strong>vert hoursin<strong>to</strong> minutes and enter <strong>the</strong> <strong>to</strong>tal minutes required for this procedure (e.g., 2hours and 10 minutes would be reported as 130. One hour and 10 minuteswould be reported as 70).For instructi<strong>on</strong>s <strong>on</strong> submitting units for oxygen claims, see chapter 20, secti<strong>on</strong>130.6 of <strong>the</strong> Medicate Claims Processing Manual.Do not place zeros before or after <strong>the</strong> number of units (e.g., a service of 1should not be billed as 010; it should be billed as 1. Indicate <strong>on</strong>ly wholenumbers, e.g., do not bill 1.5).NOTE: This field should c<strong>on</strong>tain at least 1 day or unit. The carrier shouldprogram <strong>the</strong>ir system <strong>to</strong> au<strong>to</strong>matically default “1” unit when <strong>the</strong> informati<strong>on</strong> inthis field is missing <strong>to</strong> avoid returning as unprocessable.Leave blank. Not required by Medicare. Entering informati<strong>on</strong> in this itemItem 24Hmay cause delays in claims processing.ID QualifierItem 24I Enter <strong>the</strong> ID qualifier 1C in <strong>the</strong> shaded porti<strong>on</strong> when submitting <strong>the</strong> renderingphysician’s PIN in 24J.PIN/NPI of <strong>the</strong> Rendering ProviderPrior <strong>to</strong> May 23, 2007, enter <strong>the</strong> rendering provider’s PIN in <strong>the</strong> shadedporti<strong>on</strong>. In <strong>the</strong> case of a service provided incident <strong>to</strong> <strong>the</strong> service of a physicianItem 24J or n<strong>on</strong>-physician practiti<strong>on</strong>er, when <strong>the</strong> pers<strong>on</strong> who ordered <strong>the</strong> service is notsupervising, enter <strong>the</strong> PIN of <strong>the</strong> supervisor in <strong>the</strong> shaded porti<strong>on</strong>. Do not enterPIN numbers with <strong>the</strong> alpha state code indica<strong>to</strong>r, before <strong>the</strong> PIN number. Theadditi<strong>on</strong> of this indica<strong>to</strong>r will cause <strong>the</strong> claim <strong>to</strong> be rejected as unprocessable.
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>For example, a North Dakota PIN would be entered as 000, not N000.Effective May 23, 2007 and later, do not use <strong>the</strong> shaded porti<strong>on</strong>. Beginning noearlier than January 1, 2007, enter <strong>the</strong> rendering provider’s NPI number in <strong>the</strong>lower n<strong>on</strong>-shaded porti<strong>on</strong>. In <strong>the</strong> case of a service provided incident <strong>to</strong> <strong>the</strong>service of a physician or n<strong>on</strong>-physician practiti<strong>on</strong>er, when <strong>the</strong> pers<strong>on</strong> whoordered <strong>the</strong> service is not supervising, enter <strong>the</strong> NPI of <strong>the</strong> supervisor in <strong>the</strong>lower n<strong>on</strong>-shaded porti<strong>on</strong>. An invalid NPI will cause <strong>the</strong> claim <strong>to</strong> be rejectedas unprocessable.Attenti<strong>on</strong> Providers:Billing and Placement of <strong>the</strong> NPI and Legacy Numbers <strong>on</strong> <strong>the</strong> Revised<strong>CMS</strong>-<strong>1500</strong> (08-05) Claim <strong>Form</strong>1. An incorporated Solo Provider with <strong>on</strong>e Legacy ProviderIdentificati<strong>on</strong> Number (PIN) and both an Individual Nati<strong>on</strong>al Provideridentifier (NPI) number and a Group NPI number, must bill as follows:o Individual NPI number in 33ao Leave Item 24J blank (Rendering Physician NPI number)Note: Claims will reject if <strong>the</strong> Group/Organizati<strong>on</strong> NPI number is usedin Item 33a. The claims processing system has no Group/Organizati<strong>on</strong>Legacy PIN number <strong>to</strong> which <strong>to</strong> cross-reference <strong>the</strong> NPI number at thistime.At some point, an incorporated solo provider with <strong>on</strong>ly an IndividualLegacy PIN and NPI number may receive both a Group Legacy PINand a Group NPI number. This will happen if any provider file changesare made through <strong>the</strong> NAS Enrollment Department (e.g. Tax ID,address, etc.). If and when this occurs, <strong>the</strong> provider will <strong>the</strong>n bill as agroup.2. An Incorporated Solo Provider with an Individual Legacy PIN and aGroup Legacy PIN, as well as an Individual NPI and a Group NPI,must bill as following:o Group/Organizati<strong>on</strong> NPI number in Item 33a ando Individual/Rendering provider NPI in Item 24J3. Clinics and multiple group offices, must bill as following:o Group/Organizati<strong>on</strong> NPI number in Item 33a ando Individual/Rendering provider NPI in Item 24J4. Solo/Individual provider NOT incorporated, must bill as following:o NPI in 33a ando Leave 24J blank
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>NOTE: <strong>CMS</strong> has announced that it is implementing a c<strong>on</strong>tingency plan forall covered entities that will not meet <strong>the</strong> May 23, 2007 deadline for NPI. Fora complete overview of <strong>the</strong> <strong>CMS</strong> C<strong>on</strong>tingency plan and related informati<strong>on</strong>,visit: http://www.cms.hhs.gov/nati<strong>on</strong>alprovidentstand/Informati<strong>on</strong> must be submitted within <strong>the</strong> c<strong>on</strong>fines of this box. Be sure <strong>to</strong>distinguish between zeros and <strong>the</strong> letter “O”. Do not enter provider names,UPIN numbers, or state postal codes in this item.Item 24K There is no item 24K <strong>on</strong> this versi<strong>on</strong>.Provider or Supplier Federal Tax ID (Employer Identificati<strong>on</strong> Number)Enter <strong>the</strong> provider of service or supplier Federal Tax ID (EmployerIdentificati<strong>on</strong> Number) or Social Security Number. Enter an (X) in <strong>the</strong>appropriate box <strong>to</strong> indicate which number is being reported. Only <strong>on</strong>e box canbe marked. Do not enter hyphens or spaces. Medicare providers are notItem 25 required <strong>to</strong> complete this item for crossover purposes since <strong>the</strong> Medicarec<strong>on</strong>trac<strong>to</strong>r will retrieve <strong>the</strong> tax identificati<strong>on</strong> informati<strong>on</strong> from <strong>the</strong>ir internalprovider file for inclusi<strong>on</strong> <strong>on</strong> <strong>the</strong> COB <strong>out</strong>bound claim. However, taxidentificati<strong>on</strong> informati<strong>on</strong> is used in <strong>the</strong> determinati<strong>on</strong> of accurate Nati<strong>on</strong>alProvider Identifier reimbursement. Reimbursement of claims submittedwith<strong>out</strong> tax identificati<strong>on</strong> informati<strong>on</strong> will/may be delayed.Patient’s Account NumberThis field is opti<strong>on</strong>al <strong>to</strong> assist <strong>the</strong> provider in patient identificati<strong>on</strong>. Enter <strong>the</strong>patient’s account number assigned by <strong>the</strong> provider’s of service or supplier’sItem 26accounting system. As a service, any account numbers entered here will bereturned <strong>to</strong> <strong>the</strong> provider. If an account number is entered in this item, it willappear <strong>on</strong> <strong>the</strong> provider remittance notice/advice.Accept Assignment?This is a required field, even if you are a participating provider. Check <strong>the</strong>appropriate box with an (X) <strong>to</strong> indicate whe<strong>the</strong>r <strong>the</strong> provider of service orsupplier accepts assignment of Medicare benefits or not. If Medigap isindicated in item 9 and Medigap payment authorizati<strong>on</strong> is given in item 13, <strong>the</strong>provider of service or supplier shall also be a Medicare participating providerof service or supplier and accept assignment of Medicare benefits for allcovered charges for all patients.Item 27The following providers of service/suppliers and claims can <strong>on</strong>ly be paid <strong>on</strong> anassignment basis:• Clinical diagnostic labora<strong>to</strong>ry services;• Physician services <strong>to</strong> individuals dually entitled <strong>to</strong> Medicare andMedicaid;• Participating physician/supplier services;• Services of physician assistants, nurse practiti<strong>on</strong>ers, clinical nursespecialists, nurse midwives, certified registered nurse anes<strong>the</strong>tists,
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>clinical psychologists, and clinical social workers;• Ambula<strong>to</strong>ry surgical center services for covered ASC procedures;• Home dialysis supplies and equipment paid under Method II;• Ambulance services;• Drugs and biologicals; and• Simplified Billing Roster for influenza virus vaccine andpneumococcal vaccine.Item 28Item 29Total charges for services <strong>on</strong> claimEnter <strong>the</strong> <strong>to</strong>tal charges for <strong>the</strong> services (i.e., <strong>to</strong>tal of all charges in 24F). Include<strong>the</strong> cents with dollar amounts. For example, $24.00 must be entered as 2400ra<strong>the</strong>r than 24 or 24-. Do not use dollar signs, decimals, dashes, commas, orlines. Negative dollar amounts are not allowed. Do not mark as c<strong>on</strong>tinued or<strong>the</strong> claim will be rejected as unprocessable; each <strong>CMS</strong>-<strong>1500</strong> <strong>Form</strong> shouldhave its own <strong>to</strong>tal.Total amount <strong>the</strong> patient paid <strong>on</strong> <strong>the</strong> covered services <strong>on</strong>lyEnter <strong>the</strong> <strong>to</strong>tal amount <strong>the</strong> patient paid <strong>on</strong> <strong>the</strong> covered services <strong>on</strong>ly. Include<strong>the</strong> cents with dollar amounts. For example, $24.00 must be entered as 2400ra<strong>the</strong>r than 24 or 24-. Do not use dollar signs, decimals, dashes, commas, orlines. Negative dollar amounts are not allowed. Do not mark as c<strong>on</strong>tinued or<strong>the</strong> claim will be rejected as unprocessable; each <strong>CMS</strong>-<strong>1500</strong> <strong>Form</strong> shouldhave its own <strong>to</strong>tal.Do not include <strong>the</strong> amount paid by <strong>the</strong> primary insurance, co-insurance,deductibles, account balance, or payments <strong>on</strong> previous claims in this item.Item 30Item 31Note: If any dollar amount is entered here, part or all of <strong>the</strong> payment will godirectly <strong>to</strong> <strong>the</strong> patient, even if you are a participating provider.Leave blank. Not required by Medicare.Signature of Provider of Service or SupplierThis is a required field. Enter <strong>the</strong> signature of <strong>the</strong> provider of service orsupplier, or his/her representative, and ei<strong>the</strong>r <strong>the</strong> 6-digit date (MM | DD | YY),8-digit date (MM | DD | CCYY), or alpha-numeric date (e.g., January 1, 2006)<strong>the</strong> form was signed.In <strong>the</strong> case of a service that is provided incident <strong>to</strong> <strong>the</strong> service of a physician orn<strong>on</strong>-physician practiti<strong>on</strong>er, when <strong>the</strong> ordering physician or n<strong>on</strong>-physicianpractiti<strong>on</strong>er is directly supervising <strong>the</strong> service as in 42 CFR 410.32, <strong>the</strong>signature of <strong>the</strong> ordering physician or n<strong>on</strong>-physician practiti<strong>on</strong>er shall beentered in item 31. When <strong>the</strong> ordering physician or n<strong>on</strong>-physician practiti<strong>on</strong>eris not supervising <strong>the</strong> service, <strong>the</strong>n enter <strong>the</strong> signature of <strong>the</strong> physician or n<strong>on</strong>physicianpractiti<strong>on</strong>er providing <strong>the</strong> direct supervisi<strong>on</strong> in item 31.NOTE: This is a required field, <strong>how</strong>ever <strong>the</strong> claim can be processed if <strong>the</strong>
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>following is true. If a physician, supplier, or authorized pers<strong>on</strong>’s signature ismissing, but <strong>the</strong> signature is <strong>on</strong> file; or if any authorizati<strong>on</strong> is attached <strong>to</strong> <strong>the</strong>claim or if <strong>the</strong> signature field has “Signature <strong>on</strong> File” and/or a computergenerated signature. NAS is unable <strong>to</strong> process claims with<strong>out</strong> <strong>the</strong> requiredsignature and date listed in item 31. If left blank, <strong>the</strong> claim will be rejected asunprocessable.The signature and date must be completely within <strong>the</strong> c<strong>on</strong>fines of this box.Additi<strong>on</strong>al acceptable signatures include: Signature stamp and computergenerated signature.Name and Address of Facility Where Services Were RenderedEnter <strong>the</strong> name, address, and ZIP code of <strong>the</strong> facility if <strong>the</strong> services werefurnished in a physician’s office, hospital, clinic, labora<strong>to</strong>ry, or facility o<strong>the</strong>rthan <strong>the</strong> patient’s home. Only <strong>on</strong>e name, address, and ZIP code may be enteredin <strong>the</strong> box. If additi<strong>on</strong>al entries are needed, separate claim forms shall besubmitted.Enter <strong>the</strong> name and address informati<strong>on</strong> in <strong>the</strong> following format:st1 Line – Namend2 Line – Addressrd3 Line – City, State Postal Code, and ZIP CodeItem 32Note: Enter a complete address for <strong>the</strong> locati<strong>on</strong> where <strong>the</strong> services wereperformed. A PO Box is not acceptable. Do not include teleph<strong>on</strong>e numbers,commas, periods, or o<strong>the</strong>r punctuati<strong>on</strong> in <strong>the</strong> address (e.g., 123 N Main Street101 instead of 123 N. Main Street, #101). Enter a space between <strong>the</strong> city and<strong>the</strong> state postal code. When entering a 9-digit ZIP code, include <strong>the</strong> hyphen.Providers of service (namely physicians) shall identify <strong>the</strong> supplier’s name,address, and ZIP code when billing for purchased diagnostic tests. When morethan <strong>on</strong>e supplier is used, a separate <strong>CMS</strong>-<strong>1500</strong> <strong>Form</strong> shall be used <strong>to</strong> bill foreach supplier.For foreign claims, <strong>on</strong>ly <strong>the</strong> enrollee can file for Part B benefits rendered<strong>out</strong>side of <strong>the</strong> United States. These claims will not include a valid ZIP code.When a claim is received for <strong>the</strong>se services <strong>on</strong> a beneficiary submitted <strong>Form</strong><strong>CMS</strong>-1490S, before <strong>the</strong> claim is entered in <strong>the</strong> system, it should be determinedif it is a foreign claim. If it is a foreign claim, follow instructi<strong>on</strong>s in chapter 1for dispositi<strong>on</strong> of <strong>the</strong> claim. The carrier processing <strong>the</strong> foreign claim will have<strong>to</strong> make necessary accommodati<strong>on</strong>s <strong>to</strong> verify that <strong>the</strong> claim is not returned asunprocessable due <strong>to</strong> <strong>the</strong> lack of a ZIP code.For durable medical, orthotic, and pros<strong>the</strong>tic claims, <strong>the</strong> name and address of<strong>the</strong> locati<strong>on</strong> where <strong>the</strong> order was accepted must be entered (DMERC <strong>on</strong>ly).This field is required. When more than <strong>on</strong>e supplier is used, a separate <strong>CMS</strong>-
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong><strong>1500</strong> <strong>Form</strong> shall be used <strong>to</strong> bill for each supplier. This item is completedwhe<strong>the</strong>r <strong>the</strong> supplier’s pers<strong>on</strong>nel performs <strong>the</strong> work at <strong>the</strong> physician’s office orat ano<strong>the</strong>r locati<strong>on</strong>.If a modifier is billed, indicating <strong>the</strong> service was rendered in a <strong>Health</strong>Professi<strong>on</strong>al Shortage Area (HPSA) or Physician Scarcity Area (PSA), <strong>the</strong>physical locati<strong>on</strong> where <strong>the</strong> service was rendered shall be entered if o<strong>the</strong>r than<strong>the</strong> patient’s home.If <strong>the</strong> supplier is a certified mammography screening center, enter <strong>the</strong> 6-digitFDA approved certificati<strong>on</strong> number.Complete this item for all labora<strong>to</strong>ry work performed <strong>out</strong>side a physician’soffice. If an independent labora<strong>to</strong>ry is billing, enter <strong>the</strong> place where <strong>the</strong> testwas performed.Ambulance suppliers are required <strong>to</strong> submit both originati<strong>on</strong> and destinati<strong>on</strong>informati<strong>on</strong>. The originating site informati<strong>on</strong> must be entered in item 32. It isrecommended that providers list <strong>the</strong> name of <strong>the</strong> facility, city, state and ZIPcode. The street address is not required. If <strong>the</strong>re is not enough space fordestinati<strong>on</strong> informati<strong>on</strong> in item 32, providers must enter this informati<strong>on</strong> initem 19. The origin and destinati<strong>on</strong> modifiers will identify <strong>the</strong> type of facility<strong>the</strong> beneficiary was transported <strong>to</strong>. When transport is bey<strong>on</strong>d <strong>the</strong> “closestfacility”, providers are required <strong>to</strong> briefly identify why and that informati<strong>on</strong> isalso placed in item 19.Example:32. SERVICE FACILITY LOCATION INFORMATIONItem 32aTO: Hospitals IncAny<strong>to</strong>wn IL 60610-6789FROM: Physician Practice IncAny<strong>to</strong>wn IL 60610-1234a. b.NPI of Service FacilityEnter <strong>the</strong> NPI of <strong>the</strong> service facility as so<strong>on</strong> as it is available. The NPI may bereported <strong>on</strong> <strong>the</strong> <strong>CMS</strong>-<strong>1500</strong> <strong>Form</strong> (08-05) as early as January 1, 2007, and mustbe reported May 23, 2007, and later.NOTE: <strong>CMS</strong> has announced that it is implementing a c<strong>on</strong>tingency plan forall covered entities that will not meet <strong>the</strong> May 23, 2007 deadline for NPI. Fora complete overview of <strong>the</strong> <strong>CMS</strong> C<strong>on</strong>tingency plan and related informati<strong>on</strong>,
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>visit: http://www.cms.hhs.gov/nati<strong>on</strong>alprovidentstand/Providers of service (namely physicians) shall identify <strong>the</strong> supplier’s NPI whenbilling for purchased diagnostic tests.Example:32. SERVICE FACILITY LOCATION INFORMATIONPhysician Practice Inc1234 <strong>Health</strong>care StreetAny<strong>to</strong>wn IL 60610-1234Item 32ba. 9876543210 b.ID Qualifier and PINEnter <strong>the</strong> ID qualifier 1C followed by <strong>on</strong>e blank space and <strong>the</strong>n <strong>the</strong> PIN of <strong>the</strong>service facility. Effective May 23, 2007, and later, 32b is not <strong>to</strong> be reported.NOTE: <strong>CMS</strong> has announced that it is implementing a c<strong>on</strong>tingency plan forall covered entities that will not meet <strong>the</strong> May 23, 2007 deadline for NPI. Fora complete overview of <strong>the</strong> <strong>CMS</strong> C<strong>on</strong>tingency plan and related informati<strong>on</strong>,visit: http://www.cms.hhs.gov/nati<strong>on</strong>alprovidentstand/Providers of service (namely physicians) shall identify <strong>the</strong> supplier’s PINwhen billing for purchased diagnostic tests.Item 33Item 33aFor durable medical, orthotic, and pros<strong>the</strong>tic claims, enter <strong>the</strong> PIN (of <strong>the</strong>locati<strong>on</strong> where <strong>the</strong> order was accepted) if <strong>the</strong> name and address was notprovided in item 32 (DMERC <strong>on</strong>ly).Provider’s/ Supplier’s Teleph<strong>on</strong>e Number, Billing Name, Address, and ZIPCode.This is a required field. Enter <strong>the</strong> provider of service/supplier’s teleph<strong>on</strong>enumber, billing name, address, and ZIP code.Enter <strong>the</strong> name and address informati<strong>on</strong> in <strong>the</strong> following format:1 st Line – Name2 nd Line – Address3 rd Line – City, State Postal Code, and ZIP CodeNPI of Billing Provider or GroupThis is a required field. Effective May 23, 2007, and later, you MUST enter<strong>the</strong> NPI of <strong>the</strong> billing provider or group. The NPI may be reported <strong>on</strong> <strong>the</strong><strong>CMS</strong>-<strong>1500</strong> <strong>Form</strong> (08-05) as early as January 1, 2007.Attenti<strong>on</strong> Providers:
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>Billing and Placement of <strong>the</strong> NPI and Legacy Numbers <strong>on</strong> <strong>the</strong> Revised<strong>CMS</strong>-<strong>1500</strong> (08-05) Claim <strong>Form</strong>1. An incorporated Solo Provider with <strong>on</strong>e Legacy ProviderIdentificati<strong>on</strong> Number (PIN) and both an Individual Nati<strong>on</strong>al Provideridentifier (NPI) number and a Group NPI number, must bill as follows:o Individual NPI number in 33ao Leave Item 24J blank (Rendering Physician NPI number)Note: Claims will reject if <strong>the</strong> Group/Organizati<strong>on</strong> NPI number is usedin Item 33a. The claims processing system has no Group/Organizati<strong>on</strong>Legacy PIN number <strong>to</strong> which <strong>to</strong> cross-reference <strong>the</strong> NPI number at thistime.At some point, an incorporated solo provider with <strong>on</strong>ly an IndividualLegacy PIN and NPI number may receive both a Group Legacy PINand a Group NPI number. This will happen if any provider file changesare made through <strong>the</strong> NAS Enrollment Department (e.g. Tax ID,address, etc.). If and when this occurs, <strong>the</strong> provider will <strong>the</strong>n bill as agroup.2. An Incorporated Solo Provider with an Individual Legacy PIN and aGroup Legacy PIN, as well as an Individual NPI and a Group NPI,must bill as following:o Group/Organizati<strong>on</strong> NPI number in Item 33a ando Individual/Rendering provider NPI in Item 24J3. Clinics and multiple group offices, must bill as following:o Group/Organizati<strong>on</strong> NPI number in Item 33a ando Individual/Rendering provider NPI in Item 24J4. Solo/Individual provider NOT incorporated, must bill as following:o NPI in 33a ando Leave 24J blankNOTE: <strong>CMS</strong> has announced that it is implementing a c<strong>on</strong>tingency plan forall covered entities that will not meet <strong>the</strong> May 23, 2007 deadline for NPI. Fora complete overview of <strong>the</strong> <strong>CMS</strong> C<strong>on</strong>tingency plan and related informati<strong>on</strong>,visit: http://www.cms.hhs.gov/nati<strong>on</strong>alprovidentstand/Example:33. BILLING PROVIDER INFO & PH# (312) 555 2222Physician Practice Inc1234 <strong>Health</strong>care StreetAny<strong>to</strong>wn IL 60610-1234
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>a. 9876543210 b.Note: Submitting an invalid NPI in this item will cause <strong>the</strong> claim <strong>to</strong> be rejectedas unprocessable.ID Qualifier and PINEnter <strong>the</strong> ID qualifier 1C followed by <strong>on</strong>e blank space and <strong>the</strong>n <strong>the</strong> PIN of <strong>the</strong>billing provider or group. Effective May 23, 2007, and later, 33b is not <strong>to</strong> bereported. Suppliers billing <strong>the</strong> DMERC will use <strong>the</strong> Nati<strong>on</strong>al SupplierClearinghouse (NSC) number in this item.Attenti<strong>on</strong> Providers:Billing and Placement of <strong>the</strong> NPI and Legacy Numbers <strong>on</strong> <strong>the</strong> Revised<strong>CMS</strong>-<strong>1500</strong> (08-05) Claim <strong>Form</strong>1. An incorporated Solo Provider with <strong>on</strong>e Legacy ProviderIdentificati<strong>on</strong> Number (PIN) and both an Individual Nati<strong>on</strong>al Provideridentifier (NPI) number and a Group NPI number, must bill as follows:o Individual NPI number in 33ao Leave Item 24J blank (Rendering Physician NPI number)Item 33bNote: Claims will reject if <strong>the</strong> Group/Organizati<strong>on</strong> NPI number is usedin Item 33a. The claims processing system has no Group/Organizati<strong>on</strong>Legacy PIN number <strong>to</strong> which <strong>to</strong> cross-reference <strong>the</strong> NPI number at thistime.At some point, an incorporated solo provider with <strong>on</strong>ly an IndividualLegacy PIN and NPI number may receive both a Group Legacy PINand a Group NPI number. This will happen if any provider file changesare made through <strong>the</strong> NAS Enrollment Department (e.g. Tax ID,address, etc.). If and when this occurs, <strong>the</strong> provider will <strong>the</strong>n bill as agroup.2. An Incorporated Solo Provider with an Individual Legacy PIN and aGroup Legacy PIN, as well as an Individual NPI and a Group NPI,must bill as following:o Group/Organizati<strong>on</strong> NPI number in Item 33a ando Individual/Rendering provider NPI in Item 24J3. Clinics and multiple group offices, must bill as following:o Group/Organizati<strong>on</strong> NPI number in Item 33a ando Individual/Rendering provider NPI in Item 24J4. Solo/Individual provider NOT incorporated, must bill as following:o NPI in 33a and
<str<strong>on</strong>g>Instructi<strong>on</strong>s</str<strong>on</strong>g> <strong>on</strong> <strong>how</strong> <strong>to</strong> <strong>fill</strong> <strong>out</strong> <strong>the</strong><strong>CMS</strong> <strong>1500</strong> <strong>Form</strong>o Leave 24J blank