National Board Ex- 6 Book .pmd - National Board Of Examination
National Board Ex- 6 Book .pmd - National Board Of Examination
National Board Ex- 6 Book .pmd - National Board Of Examination
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
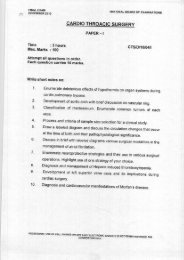
A fast of six to eight hours forsolid food and 2-4 hours for clearfluids is normally suggested in theuncomplicated patient. The mostimportant time interval is thatbetween the last meal and the timeof the injury. Alcohol also delaysgastric emptying. If surgery isnecessary in a patient with a fullstomach then a rapid sequenceinduction technique should beused.Choice of a local or generalanaesthetic techniqueThe choice of technique willdepend on patient factors as wellas local facilities and surgeonpreferences. <strong>Ex</strong>tra-ocular,anterior segment and vitreoretinaleye surgery is routinelyperformed using local anaesthetictechniques. But for emergencycases, general anaesthetic is oftenpreferable because the patientmust be able to lie flat, still andprotect his or her own airwaysafely for the duration of theprocedure, and spread of localanaesthetic agents is poor inpatients with eye and orbitalinfections. Local anaestheticinjection is associated with anincrease in intra-ocular pressurewhich may lead to vitreous lossand also oculocompression afterthe block can not be applied inopen eye injury.Thus, children, uncooperative orintoxicated patients and openglobe injury patients are usuallybetter candidates for a generalanaesthetic.SedationSedation should be usedcautiously and titrated in a patientwith a full stomach as it can causeairway problems and patientconfusion. Small doses of a shortacting agent such as midazolam,propofol, fentanyl or alfentanilcan be administered. The key togood sedation is to maintainverbal contact with the patient.Choice of drugs for generalanaesthesiaIf possible, early administrationof histamine H2 - receptorantagonist such as ranitidine(1-1.5mg/kg iv) with metoclopramide(0.15mg/kg iv) willdecrease gastric acidity andvolume, respectively, and providesome protection.Prior to rapid sequence inductionof anaesthesia, precautions mustbe taken to blunt thecardiovascular and IOP responsesto laryngoscopy and trachealintubation. Intravenous administrationof lidocaine (1.5mg/kg)and of sufentanil (0.05-0.15µg/kg), remifentanil (0.5-1.0 µg/kg) 3to 5 minutes before induction,may help in attenuating theincrease in IOP after trachealintubation. A beta adrenergicreceptor blocking drug such aslabetalol (0.03mg/kg IV) may alsohelp in blocking the cardiovascularresponse to trachealintubation, especially in patientswith angina or hypertension.Most intravenous inductionagents reduce intra-ocularpressure therefore preventingfurther damage to the injured eye.An adequate dose of thiopentoneor propofol will ensure adequatedepth of anaesthesia duringtracheal intubation. Ketamineshould be avoided in open eyeinjuries. All the non-depolarisingmuscle relaxants can be usedwithout adverse effects on theeye.Suxamethonium use in penetratingeye injury anaesthesia iscontroversial as it increases IOP.The extent of the rise in intraocularpressure will depend on theother drugs used and the responseto laryngoscopy and intubation.Adequate fasting prior to surgerywill allow suxamethonium to beavoided for the majority of urgentcases. For rapid sequenceinduction, the relative risks needto be weighed, i.e. prevention ofaspiration (potentially lifethreatening) verses ocular damage(potentially sight threatening).Suxamethonium avoiding techniquesinclude the use of largedoses of vecuronium (0.2mg/kg)or rocuronium (0.9-1.2mg/kg) tospeed up its onset of action aspart of a modified rapid sequenceinduction technique. A morerapid- acting rocuronium (60secs)with duration of 30 to 40 minutescan also be used for a rapidsequence induction technique.During general anaesthesia foropen eye surgery, depth ofanaesthesia must be adequate toensure lack of movement orcoughing. To ensure profoundneuromuscular blockade, train offour must be monitored toprevent any movement andcoughing during surgery.Airway management andmode of ventilationPatient should be intubated andventilated to ensure a secureairway and to facilitate mildhypocarbia to reduce IOP. Theproseal laryngeal mask airway isalso a good alternative withcontrolled ventilation as itsinsertion avoids the pressor30Journal of Postgraduate Medical Education, Training & ResearchVol. II, No. 5, September-October 2007