National Board Ex- 6 Book .pmd - National Board Of Examination
National Board Ex- 6 Book .pmd - National Board Of Examination
National Board Ex- 6 Book .pmd - National Board Of Examination
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
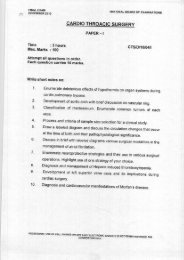
l Gentle induction ofanaesthesial Reduction of sympatheticstimulationl Avoidance of hypoxia,hypercarbial Coping with acute changes– HT, arrhythmias etcThe surgical procedure can beeither open or laparoscopic. Aftershifting the patient into theoperating room, at least two largebore venous cannulae sould be inplace. ECG, SpO2, EtCO2, temperatureand urine output shouldbe monitored. Invasive arterialblood pressure and centralvenous pressure should be monitored.Optional monitors includepulmonary capillary wedge pressureand neuromuscular blockademonitoring. A number of drugsshould be kept ready for use inacute hypertensive and hypotensivecrises, such as sodium nitroprusside,phentolamine, magnesiumsulphate, propranolol,esmolol, phenylephrine, dopamine,adrenaline and noradrenaline.Drugs that cause arrhythmias andtachycardia should be avoided,such as atropine, ketamine,succinyncholine, halothane,desflurane, pancuronium,atracurium etc. The anaesthetictechnique can be either controlledgeneral anaesthesia withmuscle relaxation or general anaesthesiacombined with epiduralanaesthesia 7 . Though it has alsobeen done with a regional anaesthetictechnique alone, it is notrecommended as control ofacute fluctuations of blood pressureis better with general anaesthesia.Any combination of drugscan be used for induction andmaintenance, avoiding the onesspecified before. Episodes of tachycardiashould be treated withesmolol or propranolol. Hypertensioncan occur, especially duringlaryngoscopy and tumor handling,and should be controlledwith sodium nitroprusside, nitroglycerineand labetolol. It hasbeen found that the peak totalcatecholamine level found duringsurgery correlated quite well withmore operative instability suggestingthat patients withphaeochromocytomas with highproduction of catecholaminesare more likely to show cardiovascularinstability 8 . Adequatevolume loading is necessary. Followingligation of the venousdrainage of the tumor, there isusually a sudden fall in bloodpressure due to sudden fall incatecholamine levels in the body,combination of residual alphaand beta blockade, receptordowngrading, and diminishedblood volume. This should betreated with i.v. fluids, and whichmay require noradrenaline oradrenaline infusions.Post-operatively, intensive carewith invasive monitoring is recommendedfor all patients. Inmost cases, cardiovascular stabilityreturns within a few hours ofcompletion of surgery and vasoactiveagents are withdrawn atthis stage. About 50% of patientsmight remain hypertensive for 1– 3 days. Adequate fluids shouldbe given post-operatively, titratedto CVP, and analgesia should bemaintained via epidural top-upsor intravenous narcotics. Thepatient should be extubated whenconsidered appropriate. Themortality as well as difficulty inmanagement of phaeochromocytomaincreases manifold whenit complicates other conditionssuch as pregnancy 9 , when magnesiumsulphate is one of thepreferred vasodilators 10 , or inpaediatric 11 patients. Other conditionsresembling phaeochromocytomainclude neuroblastomaand ganglione-uroma.It isessential to remember that not allcases of phaeochromocytomawill be well-controlled with medication,two other situations arepossible- when abdominal manipulationduring incidental surgeryleads to uncontrollable risesin blood pressure, leading to adiagnosis of phaeochromocytomain the operating room, andwhen a known case ofphaeochromocytoma, still notwell-controlled with drugs, presentsfor an emergency surgery.In both these cases, invasivemonitoring should be started,and the intra-operative fluctuationsof blood pressure controlledwith appropriateinotropes, dilators andfluids.Post-operative ICU carewith elective ventilation is a mustfor these patients till blood pressureis satisfactorily controlled.References1. St John Sutton MG,Sheps SG, Lie JT. Prevalenceof clinically unsuspectedphaeoch-romocytoma: Reviewof a 50-year autopsyseries.Mayo Clin Proc 56:354,1981.2. Geoghegan JG, Emberton M,Bloom SR, Lynn JA. Changingtrends in the managementof phaeochromocytoma. BrJ Surg. 1998 Jan;85(1):117-20.Journal of Postgraduate Medical Education, Training & Research67