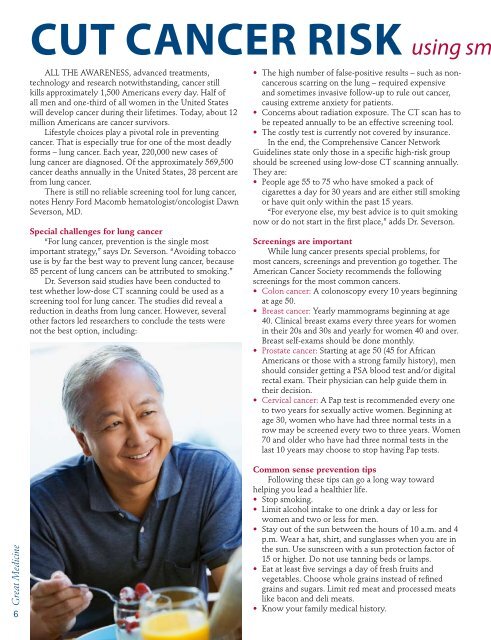
Cut cancer risk using smAll the awareness, advanced treatments,technology and research notwithstanding, cancer stillkills approximately 1,500 Americans every day. Half ofall men and one-third of all women in the United Stateswill develop cancer during their lifetimes. Today, about 12million Americans are cancer survivors.Lifestyle choices play a pivotal role in preventingcancer. That is especially true for one of the most deadlyforms – lung cancer. Each year, 220,000 new cases oflung cancer are diagnosed. Of the approximately 569,500cancer deaths annually in the United States, 28 percent arefrom lung cancer.There is still no reliable screening tool for lung cancer,notes <strong>Henry</strong> <strong>Ford</strong> Macomb hematologist/oncologist DawnSeverson, MD.Special challenges for lung cancer“For lung cancer, prevention is the single mostimportant strategy,” says Dr. Severson. “Avoiding tobaccouse is by far the best way to prevent lung cancer, because85 percent of lung cancers can be attributed to smoking.”Dr. Severson said studies have been conducted totest whether low-dose CT scanning could be used as ascreening tool for lung cancer. The studies did reveal areduction in deaths from lung cancer. However, severalother factors led researchers to conclude the tests werenot the best option, including:• The high number of false-positive results – such as noncancerousscarring on the lung – required expensiveand sometimes invasive follow-up to rule out cancer,causing extreme anxiety for patients.• Concerns about radiation exposure. The CT scan has tobe repeated annually to be an effective screening tool.• The costly test is currently not covered by insurance.In the end, the Comprehensive Cancer NetworkGuidelines state only those in a specific high-risk groupshould be screened using low-dose CT scanning annually.They are:• People age 55 to 75 who have smoked a pack ofcigarettes a day for 30 years and are either still smokingor have quit only within the past 15 years.“For everyone else, my best advice is to quit smokingnow or do not start in the first place,” adds Dr. Severson.Screenings are importantWhile lung cancer presents special problems, formost cancers, screenings and prevention go together. TheAmerican Cancer Society recommends the followingscreenings for the most common cancers.• Colon cancer: A colonoscopy every 10 years beginningat age 50.• Breast cancer: Yearly mammograms beginning at age40. Clinical breast exams every three years for womenin their 20s and 30s and yearly for women 40 and over.Breast self-exams should be done monthly.• Prostate cancer: Starting at age 50 (45 for AfricanAmericans or those with a strong family history), menshould consider getting a PSA blood test and/or digitalrectal exam. Their physician can help guide them intheir decision.• Cervical cancer: A Pap test is recommended every oneto two years for sexually active women. Beginning atage 30, women who have had three normal tests in arow may be screened every two to three years. Women70 and older who have had three normal tests in thelast 10 years may choose to stop having Pap tests.Great Medicine6Common sense prevention tipsFollowing these tips can go a long way towardhelping you lead a healthier life.• Stop smoking.• Limit alcohol intake to one drink a day or less forwomen and two or less for men.• Stay out of the sun between the hours of 10 a.m. and 4p.m. Wear a hat, shirt, and sunglasses when you are inthe sun. Use sunscreen with a sun protection factor of15 or higher. Do not use tanning beds or lamps.• Eat at least five servings a day of fresh fruits andvegetables. Choose whole grains instead of refinedgrains and sugars. Limit red meat and processed meatslike bacon and deli meats.• Know your family medical history.
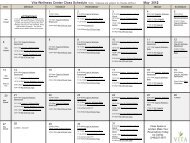
art, practical prevention strategiesNew program offers patients superior,collaborative care optionsLung cancer is the most prevalent cancer in Macomb County. To addressthis aggressive disease, <strong>Henry</strong> <strong>Ford</strong> Macomb Hospital has introduced its newMultidisciplinary Lung Cancer Program, the first of its kind in the region.This program combines a superior, collaborative consultation and care planningsession for patients with highly advanced treatment available through the Josephine<strong>Ford</strong> Cancer Center at <strong>Henry</strong> <strong>Ford</strong> Macomb Hospital.Immediately prior to their arrival, the patient’s case will be reviewed by amultidisciplinary team of specialists, including pulmonary medicine, thoracic surgery,medical oncology, radiation oncology, pathology, and radiology. Patients will then havethe unique experience of receiving a concise and collaborative consultation from fourspecialists in one visit. At the end of the visit, the patient will have a recommendedplan of care. All required follow-up care will be seamlessly coordinated by an oncologynurse navigator.For information or a referral into the program, talk with your physician or call theJosephine <strong>Ford</strong> Cancer Center at <strong>Henry</strong> <strong>Ford</strong> Macomb Hospitals at (586) 263-2230.*LIFETIMECancer Survivor’s Day:A Celebration of LifeAll cancer survivors and their specialsupport person are invited to a free,inspirational luncheon on June 22 from11:30 a.m. to 2:30 p.m. at the ItalianAmerican Cultural Center in ClintonTownship.RSVP by June 15 to (586) 263-2851.Leave your name and your guest’s name.Relay for Life<strong>Henry</strong> <strong>Ford</strong> Macomb Hospitals inviteseveryone to join our Relay for Life teamsin either Warren or Clinton Township.The Clinton Township Relay is May 19-20and the Warren Relay is June 9-10. Formore information, call the Josephine<strong>Ford</strong> Cancer Center at <strong>Henry</strong> <strong>Ford</strong>Macomb Hospitals at (586) 263-2230or go online to www.relayforlife.org.Skin Cancer ScreeningIf you have ever wondered about thatfreckle on your arm or the mole onyour ear, you’ll want to attend this skincancer check. This program is designedto address main areas of concern. It isnot a full body exam. An appointment isLEARNINGrequired by calling (800) 532-2411.May 23 • 9 to 11 a.m.Call for locationCancer Patient Support GroupThis weekly group, facilitated by aprofessional counselor, will give patientsan opportunity to express their feelingsand concerns and hear how others arecoping with cancer. Registration is notrequired. For more information, call(586) 263-2237.Mondays, 1:30 to 3 p.m., ongoingClinton Township CampusLook Good…Feel BetterThis class, sponsored by the AmericanCancer Society, is especially forwomen undergoing cancer treatment.A cosmetologist will be on handto demonstrate how to choose themake-up, wigs, scarves and hatsthat will best compliment yourappearance. Registration is extremelyimportant. For more information or toregister, please call (586) 263-2237.Second Wednesday of the month2:30 to 4:30 p.m.Clinton Township CampusHelp future generations<strong>Henry</strong> <strong>Ford</strong> <strong>Health</strong> <strong>System</strong>and other health care providers andbusinesses around the country areteaming up with the American CancerSociety (ACS) for a long-term CancerPrevention Study (CPS-3).The goal of CPS-3 is to betterunderstand factors such as lifestyle,environment and genetics that causeor prevent cancer. The ACS is hopingto enroll 300,000 people nationwidebetween the ages of 30 and 65 whohave never had cancer. Participants willbe followed for 20 years.Enrolling in the study takes about30 minutes and involves completing asurvey packet, and providing a waistcircumference and a small bloodsample. Participants will be mailed aquestionnaire every few years to updatelifestyle, environment and medicalinformation.Enrollment appointments areavailable throughout Metro Detroitduring the last week of April. Log onto www.cancer.org/cps3 for moreinformation. Enrollment opportunitiesat <strong>Henry</strong> <strong>Ford</strong> Macomb locationsinclude:• <strong>Henry</strong> <strong>Ford</strong> Macomb Hospital inClinton Township: April 26 from11:30 a.m. to 6 p.m. and April 28from 8:30 a.m. to 12:30 p.m.• <strong>Henry</strong> <strong>Ford</strong> Macomb <strong>Health</strong> Center– Chesterfield: April 26 from 3 to6:30 p.m.• <strong>Henry</strong> <strong>Ford</strong> Macomb <strong>Health</strong> Center– Washington: April 27 from 10 a.m.to 1:30 p.m.Great Medicine7