Emergency Airway Management Desaturation (Oxygen Sat below ...
Emergency Airway Management Desaturation (Oxygen Sat below ...
Emergency Airway Management Desaturation (Oxygen Sat below ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
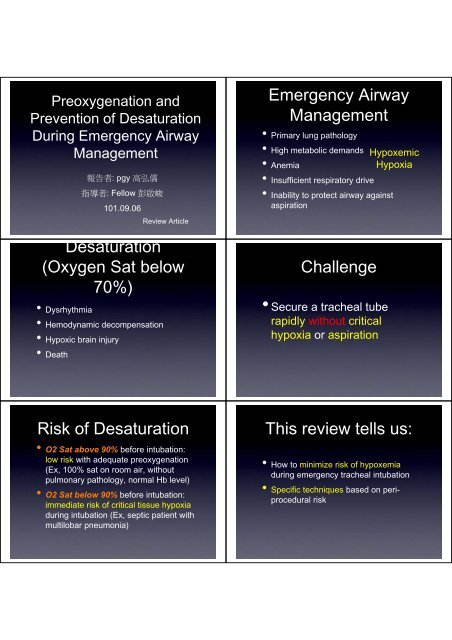
Preoxygenation andPrevention of <strong>Desaturation</strong>During <strong>Emergency</strong> <strong>Airway</strong><strong>Management</strong>報 告 者 : pgy 高 弘 儒指 導 者 : Fellow 彭 啟 峻101.09.06Review Article<strong>Desaturation</strong>(<strong>Oxygen</strong> <strong>Sat</strong> <strong>below</strong>70%)• Dysrhythmia• Hemodynamic decompensation• Hypoxic brain injury• Death<strong>Emergency</strong> <strong>Airway</strong><strong>Management</strong>• Primary lung pathology• High metabolic demands Hypoxemic• AnemiaHypoxia• Insufficient respiratory drive• Inability to protect airway againstaspirationChallenge• Secure a tracheal tuberapidly without criticalhypoxia or aspirationRisk of <strong>Desaturation</strong>• O2 <strong>Sat</strong> above 90% before intubation:low risk with adequate preoxygenation(Ex, 100% sat on room air, withoutpulmonary pathology, normal Hb level)• O2 <strong>Sat</strong> <strong>below</strong> 90% before intubation:immediate risk of critical tissue hypoxiaduring intubation (Ex, septic patient withmultilobar pneumonia)This review tells us:• How to minimize risk of hypoxemiaduring emergency tracheal intubation• Specific techniques based on periproceduralrisk
Rationale behindPreoxygenation• Enlarges safety buffer range duringperiods of hypoventilation and apnea• Extends duration of safe apnea (Def:the time until a patient reaches asaturation level of 88% to 90%) to allowplacement of definitive airwayStandard AnesthesiaInduction• Elective operative patients (stable pt’s)• Administer sedative• Provide manual ventilation• Administer muscle relaxant• Continue manual ventilation untilplacement of definitive airway• Preoxygenation is not mandatory3 Goals ofPreoxygenation• Bring patient’s saturation as close to100% as possible• Denitrogenate the residual capacity ofthe lungs (maximizing oxygen storagein the lungs)• Denitrogenate and maximallyoxygenate the bloodstream• When patients desaturate <strong>below</strong> 88%,their status is on the steep portion ofthe oxygen hemoglobin dissociationcurve, and can decrease to criticallevels of O2 sat (< 70%) withinmomentsRapid Sequence• Pt’s with highInductionaspiration risk (critically ill)• Simultaneous administration of thesedative and paralytic with no ventilation,while waiting for the paralytic to takeeffect, unless needed to preventhypoxemia.• In ED, all patients requiring airwaymanagement are assumed to be at riskof aspiration.• Default technique: rapid sequencetracheal intubationBest Source of FiO2• True nonrebreather mask: 90-100%FiO2• Self-inflating bag-valve-mask: ambientFiO2• Standardly nonrebreather mask,available in ED, set at flow rates of 15L/min: 60-70% FiO2• Standardly nonrebreather mask set at30-60 L/min: > 90% FiO2
Appropriate Duration ofPreoxygenation• Ideally, pt’s should continue to receivepreoxygenation until greater than 90%end-tidal oxygen level.• 3 minutes’ worth tidal-volume breathingwith high FiO2 source (> 90%)• Cooperative patients: take 8 vitalcapacitybreaths (maximally inhale andexhale)Can Increasing Mean <strong>Airway</strong>Pressure AugmentPreoxygenation?• If pt’s do not achieve 93-95% saturation levelafter 3 minutes of tidal-volume breathing witha high FiO2 source, it is likely that they areexhibiting shunt physiology.• Shunt physiology: perfused, but not ventilated(pulmonary edema, pneumonia)• Shunt physiology can be partially overcomeby augmenting mean airway pressureBaillard et al. (HypoxemicCritically-ill Pt’s in ICU)• Noninvasive positive-pressureventilation group had a 98% mean O2sat• Standard group: 93%• 6/26 were unable to improve O2 satwith high FiO2 until they receive NPPV• No negative cardiovascular effects orappreciable gastric distention wasobserved in noninvasive positivepressure preoxygenation studies.• Gastric distention and resultingaspiration is unlikely at pressures <strong>below</strong>25 cm H2O.• If tracheal intubation is attempted withsaturation <strong>below</strong> 90%, these patientscan critically desaturate in secondsDuring TrachealIntubation• Standard group’s levels decreased tosaturations of 81% compared with 93%in NPPV group• 12 of the control group and 2 of theNPPV group had saturation levels<strong>below</strong> 80%
Positive <strong>Airway</strong> Pressure• Standalone disposable continuouspositive airway pressure (CPAP) masks,leave it on until the moment ofintubation• Positive end-expiratory pressure (PEEP)valve on a standard bag mask• PEEP prevents absorption atelectasiscaused by breathing high FiO2 gaslevel• A disposable PEEP valve, inexpensive,strain gauge capable from 5-20 cmH2O• If combined with a nasal cannula set to15 L/min, it will provide CPAP evenwithout ventilations.Positioning• Supine positioning is not ideal toachieve optimal preoxygenation.• Head-up 20-25 degrees• Reverse Trendlenburg position (head ofstretcher 30 degrees higher than thefoot)When Laying Flat• More difficult to take full breaths• More of the posterior lung becomesprone to atelectatic collapse• Reduces the reservoir of O2 containedwithin the lungs• Reduces safe apnea timeStudies• Lane et al, RCT: 20-degree head-up vs.supine position = 386 : 283 sec (satdrop from 100% to 95% after 3 mins ofpreoxygenation)• Ramkumar et al: 20-degree head-upgroup takes 452 sec vs. 364 sec leftsupine group to desaturate• Altermatt et al (BMI > 35, intubated,SpO2 drop from 100-90%): Sitting vs.supine = 214 sec : 162 sec of safeapnea time.How Long Will It Take toDesaturate afterPreoxygenation• O2 consumption during apnea isapproximately 250 ml/min• In healthy pt’s, the duration of safeapnea on room air is about 1 minutecompares with approximately 8 minuteswhen breathing at a high FiO2 level.
In Sick Patients• Poor cardiac output may delay thereadings of actual central arterialcirculation by 30 to 60 sec when usingfinger-probe device.• The effect of shunting dramaticallyreduces oxygen storage in the lungsand shortens safe apnea in critically illpt’s.• <strong>Desaturation</strong> to 85% may be as shortas 23 seconds in critically ill pt’s versus502 seconds in a healthy adultApneic <strong>Oxygen</strong>ation• Aveoli will continue to take up oxygeneven without diaphragmatic movementsor lung expansion.• In an apneic patient, approximately 250ml/min of O2 will move from aveoli tothe blood stream.• Conversely, only 8-20 ml/min of CO2moves into the aveoli during apneaApneic <strong>Oxygen</strong>ation• The difference in O2 and CO2movement across the aveolarmembrane is due to the significantdifference in gas solubility in the blood,as well as the affinity of Hb for O2.• This causes the net pressure in theaveoli to become slightlysubatmospheric, thus generating amass flow of gas from pharynx to aveoli.• This phenomenon is called apneicoxygenation• It permits maintenance of oxygenationwithout spontaneous or administeredventilations.• Under uptimal circumstances, a PaO2can be maintained at greater than 100mmHg for up to 100 minutes without asingle breath.• 6 min (nasal catheter) vs 3.65 min(control) desaturate to 95% in a RCT ofanesthesia patients. Taha et al.• Apneic oxygenation will allow continuedoxygenation but will have no significanteffect on CO2.• To provide apeneic oxygenation duringED tracheal intubations, the nasalcannula is the device of choice.• The decreased O2 demands of theapneic state will allow nasal cannula tofill the pharynx with a high level of FiO2.• By increasing the flow rate to 15 L/min,near 100% FiO2 can be obtained.When and How Should WeProvide Manual Ventilations?• Ventilation provides 2 potential benefits:ventilation and increased oxygenationthrough aveolar distention andreduction in shunting.
Agressive Ventilation ShouldBe Executed When• Profound metabolic acidosis (ex, severesalicylate toxicity), because ofcardiovascular collapse with cessationof self-ventilation• Increased intracranial pressure, inwhich CO2 increase can lean tocerebral vasodilation• Risk: regurgitation and aspirationManeuvers and• Patients Positioningshoule be positioned tomaximize upper airway patency beforeand during apneic period, using ear-tosternalnotch positioning• Nasal airways may be needed• Jaw thrust to prevent posteriorpharyngeal structures to collapsebackwards• Cricoid pressure may negatively affectapneic oxygenation, but no stuidesexists to author’s knowledgeSecond Benefit: Increased<strong>Oxygen</strong>ation• Crucial, because pt’s O2 sat < 90% willnot tolerate apnea for 60 seconds• Ventilation during the onset phase ofmuscle relaxation can create aveolardistension and lengthen the duration ofsafe apnea.• Significant risk in critically ill pt’s:positive-pressure ventilation involvesdecrease venous return andhypotension.Choice of Paralytic Agent• In a study of operative pt’s, the time todesaturation to 95% was 242 secondsin succinylcholine group versus 378seconds in rocuronium group.• It is hypothesized that the fasiculationsinduced by succinylcholine may causeincreased oxygen use.Risk Stratification• Patients requiring emergency airwaymanagement can be risk stratified into 3groups, according to the pulse oximetryafter initial application of high-flowoxygen
We Should Know• Preoxygenation extends the duration ofsafe apnea, recommended for every EDtracheal intubation• Source: standard reservoir facemaskswith the flow rate of oxygen set tomaximum• How long: pt’s with an adequaterespiratory drive should receivepreoxygenation for 3 minutes or take 8breaths, with maximal inhalation andexhalation.• CPAP masks, NPPV, or PEEP valveson a bag-valve-mask device should beconsidered when high FiO2 cannotachieve 93-95% O2 sat• Positioning: head-elevated wheneverpossible. Reverse Trendlenburgposition for possible spinal injury andimmobolized pt’s.• Pt’s with high O2 sat on room air are atlow risk, and may maintain O2 sat aslong as 8 minutes. Critically ill pt’s areat high risk, and may desaturateimmediately.• Apneic oxygenation can extend theduration of safe apnea (after sedativeand muscle relaxant) with nasalcannula, set at 15 L/min of greater.• Manual ventilation: 1) low risk(95%), nonecessary 2) high risk(91-95%),evaluate risk/benefit 3) hypoxemicpatients: low-pressure, low-volume,low-rate ventilations will be required.• Ear-to-sternal notch positioning, jawthrust, and nasal airway may be neededto provide upper airway patency.• In patients at high risk of desaturation,rocuronium may provide a longerduration of safe apnea thansuccinylcholine.Conclusion• Low risk(96-100%): properly positionedand receive preoxygenation, activeventilation and passive apneicoxygenation may not be necessary• High risk(91-95%) after high FiO2:positioning, preoxygenation andpassive oxygenation should be used.Evaluate risk/benefit of using PEEP.
Conclusion• Initially hypoxemic(90% or less afterhigh FiO2): aggressive efforts should bemade, including PEEP duringpreoxygenation, ventilation during theonset of phase of muscle rexaxnts, andpassive oxygenation during trachealintubation.Thank you for theattention