NEWS BY USMAN I. LULA AND RICHARD AMOSRadiotherapy physics research <strong>in</strong> the UK:challenges <strong>and</strong> proposed solutionsTABLE 1StrengthsInfrastructure• Modern equipment• CR-UK cancer centre statusStaff• Motivated <strong>and</strong> highly skilled staffFund<strong>in</strong>g• Good grant fund<strong>in</strong>g track record• Industrial l<strong>in</strong>ksCulture• Track record <strong>in</strong> research• Track record <strong>in</strong> translational research• Trial <strong>in</strong>volvementL<strong>in</strong>ks• Academic l<strong>in</strong>ks• L<strong>in</strong>ks to academic oncologistsWeaknessesInfrastructure• Therapy equipment access <strong>and</strong>laboratory spaceStaff• Lack <strong>of</strong> protected time for physicsresearch• Lack <strong>of</strong> critical mass• Staff<strong>in</strong>g establishment less than IPEMst<strong>and</strong>ardsFund<strong>in</strong>g• Lack <strong>of</strong> grant <strong>in</strong>come or core fund<strong>in</strong>gCl<strong>in</strong>ical academics• Limited number <strong>of</strong> research-activecl<strong>in</strong>icians or no academic leadCulture• Large cl<strong>in</strong>ical service hamper<strong>in</strong>gresearch• Progress <strong>in</strong> advanced radiotherapyAcademic l<strong>in</strong>ks• No academic l<strong>in</strong>ksOpportunitiesInfrastructure• New technology opportunitiesL<strong>in</strong>ks• Academic l<strong>in</strong>ks• Increased l<strong>in</strong>ks withmanufacturers• Increased number <strong>of</strong> academiconcologistsThreatsFund<strong>in</strong>g• NHS fund<strong>in</strong>g cuts <strong>and</strong> costimprovement programmes• Current economic climate• Lack <strong>of</strong> (national) fund<strong>in</strong>g streamsfor radiotherapy-related researchCl<strong>in</strong>ical radiotherapy service• NHS service pressureTable 1: Summary <strong>of</strong> pre-meet<strong>in</strong>g strengths, weaknesses,opportunities <strong>and</strong> threats (SWOT) analyses from 23 radiotherapyphysics departments. Key factors (nom<strong>in</strong>ated by >5 centres) <strong>in</strong> bold,common factors (nom<strong>in</strong>ated by >2 centres) <strong>in</strong> pla<strong>in</strong> text. Table k<strong>in</strong>dlysupplied by Dr Ranald Mackay, Christie Medical <strong>Physics</strong> <strong>and</strong><strong>Eng<strong>in</strong>eer<strong>in</strong>g</strong>, The Christie NHS Foundation Trust, Manchester M204BX. © BIR, ‘Commentary – radiotherapy physics research <strong>in</strong> the UK:challenges <strong>and</strong> proposed solutions’, RI Mackay, NG Burnet, S Green,TM Illidge, JN Staffurth, Brit J Radiol 2012; 85: 1354–62RADIOTHERAPY PHYSICSRadiotherapy is a potent, costeffective,technology-ledtreatment modality. Scientificadvances such as IMRT, IGRT <strong>and</strong>SABR provide real improvement<strong>in</strong> patients’ outcomes. Innovation<strong>and</strong> implementation requiresignificant additional expertise, aswell as high levels <strong>of</strong> researchexpertise with<strong>in</strong> lead<strong>in</strong>g centres.The Cl<strong>in</strong>ical <strong>and</strong> TranslationRadiotherapy Research Work<strong>in</strong>gGroup (CTRad) is an NCRI work<strong>in</strong>ggroup formally launched <strong>in</strong> 2009to focus on cl<strong>in</strong>ical <strong>and</strong>translational issues relat<strong>in</strong>g toradiotherapy <strong>and</strong> radiobiology. In2011, CTRad organised a meet<strong>in</strong>g<strong>in</strong>volv<strong>in</strong>g 23 departments (withCR-UK status) to address theissues affect<strong>in</strong>g radiotherapyphysics research <strong>in</strong> the UK.Departments were asked tocomplete a pre-meet<strong>in</strong>gevaluation <strong>of</strong> their research<strong>in</strong>frastructure <strong>and</strong> the strengths,weaknesses, opportunities <strong>and</strong>threats (SWOT) with<strong>in</strong> their owncentre (table 1). There wereseveral meet<strong>in</strong>g discussionthemes <strong>in</strong>clud<strong>in</strong>g: R&D processfor radiotherapy physics; barriersto research; research time <strong>and</strong>staff<strong>in</strong>g models; academic careerstructure; fund<strong>in</strong>g dilemmas, <strong>and</strong>the impact <strong>of</strong> expansion <strong>of</strong>radiotherapy services.The meet<strong>in</strong>g discussions <strong>and</strong>evaluation forms highlightedseveral issues: lack <strong>of</strong> dedicatedaccess to a l<strong>in</strong>ac for research;research conducted ’out <strong>of</strong> hours’or fitted around a cl<strong>in</strong>ical servicerunn<strong>in</strong>g at full capacity <strong>and</strong> theneed for dedicated time toconduct research. In terms <strong>of</strong>priorities for research, the topthree areas were image guidance,verification <strong>of</strong> complex treatments<strong>and</strong> radiobiological modell<strong>in</strong>g.The expansion <strong>of</strong> radiotherapy hasstretched physics services <strong>and</strong>departments have been underpressure to exp<strong>and</strong> IGRT/IMRT. Asa result, R&D <strong>in</strong> radiotherapy hassuffered due to staff not keep<strong>in</strong>gpace with the expansion <strong>in</strong> cl<strong>in</strong>icalwork. This has further hamperedprogression towards the‘Roadmap to modern 4D-adaptiveRT’ for a world-class radiotherapyservice as envisioned byNRIG/NCAT. There is arequirement to re<strong>in</strong>force guidancefrom pr<strong>of</strong>essional bodies to<strong>in</strong>crease technologist numbers<strong>and</strong> thus liberate time forscientists to dedicate todevelopment <strong>and</strong> research.A symbiotic relationship isrequired between the medicalphysicist <strong>and</strong> the cl<strong>in</strong>ician foreffective multidiscipl<strong>in</strong>arywork<strong>in</strong>g. Several models werediscussed when maximis<strong>in</strong>g onthe effective use <strong>of</strong> staff forcl<strong>in</strong>ical research <strong>and</strong> also whenroll<strong>in</strong>g out a well-developedtechnique <strong>in</strong>to all centres.It is clear that there arechallenges <strong>in</strong> both fund<strong>in</strong>g <strong>and</strong>staff<strong>in</strong>g <strong>of</strong> radiotherapy physics.Recommendations forimprovements <strong>in</strong>cluded:n fund<strong>in</strong>g opportunities (e.g. fromEPSRC, the STF <strong>and</strong> CR-UK);n identification <strong>of</strong> academictra<strong>in</strong><strong>in</strong>g routes with<strong>in</strong>Modernis<strong>in</strong>g Scientific Careers;n <strong>in</strong>troduction <strong>of</strong> formal job plansto allow protected research time;n improved access to researchfacilities;n benchmark<strong>in</strong>g <strong>of</strong> research<strong>in</strong>frastructure aga<strong>in</strong>st othersuccessful centres;n develop<strong>in</strong>g strategies withpartner HEI’s <strong>and</strong> local <strong>in</strong>itiatives<strong>and</strong> collaboration betweenradiotherapy physicsdepartments.To realise the full potential <strong>of</strong>radiotherapy <strong>in</strong> improv<strong>in</strong>goutcomes for cancer patients, theNHS, HEIs <strong>and</strong> funders need toprovide a more secure physicsR&D environment.‘ MORE INFORMATIONThis work was published <strong>in</strong> Brit JRadiol 2012; 85: 1354–62.http://dx.doi.org/10.1259/bjr/6153068608 | MARCH <strong>2013</strong> | SCOPE
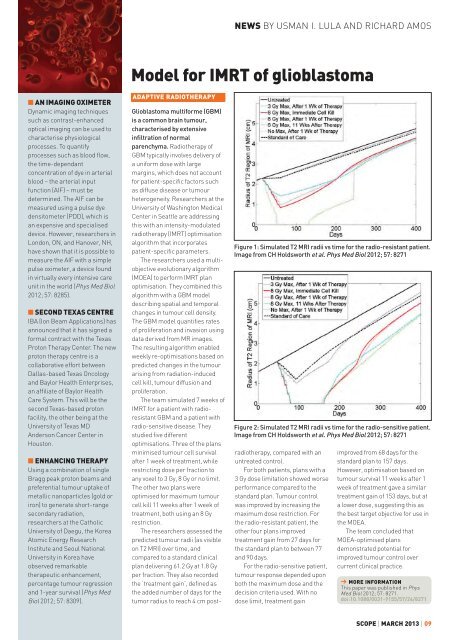
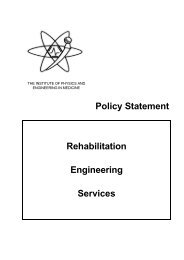
NEWS BY USMAN I. LULA AND RICHARD AMOSModel for IMRT <strong>of</strong> glioblastoman AN IMAGING OXIMETERDynamic imag<strong>in</strong>g techniquessuch as contrast-enhancedoptical imag<strong>in</strong>g can be used tocharacterise physiologicalprocesses. To quantifyprocesses such as blood flow,the time-dependantconcentration <strong>of</strong> dye <strong>in</strong> arterialblood – the arterial <strong>in</strong>putfunction (AIF) – must bedeterm<strong>in</strong>ed. The AIF can bemeasured us<strong>in</strong>g a pulse dyedensitometer (PDD), which isan expensive <strong>and</strong> specialiseddevice. However, researchers <strong>in</strong>London, ON, <strong>and</strong> Hanover, NH,have shown that it is possible tomeasure the AIF with a simplepulse oximeter, a device found<strong>in</strong> virtually every <strong>in</strong>tensive careunit <strong>in</strong> the world (Phys Med Biol2012; 57: 8285).n SECOND TEXAS CENTREIBA (Ion Beam Applications) hasannounced that it has signed aformal contract with the TexasProton Therapy Center. The newproton therapy centre is acollaborative effort betweenDallas-based Texas Oncology<strong>and</strong> Baylor Health Enterprises,an affiliate <strong>of</strong> Baylor HealthCare System. This will be thesecond Texas-based protonfacility, the other be<strong>in</strong>g at theUniversity <strong>of</strong> Texas MDAnderson Cancer Center <strong>in</strong>Houston.n ENHANCING THERAPYUs<strong>in</strong>g a comb<strong>in</strong>ation <strong>of</strong> s<strong>in</strong>gleBragg peak proton beams <strong>and</strong>preferential tumour uptake <strong>of</strong>metallic nanoparticles (gold oriron) to generate short-rangesecondary radiation,researchers at the CatholicUniversity <strong>of</strong> Daegu, the KoreaAtomic Energy Research<strong>Institute</strong> <strong>and</strong> Seoul NationalUniversity <strong>in</strong> Korea haveobserved remarkabletherapeutic enhancement,percentage tumour regression<strong>and</strong> 1-year survival (Phys MedBiol 2012; 57: 8309).ADAPTIVE RADIOTHERAPYFigure 1: Simulated T2 MRI radii vs time for the radio-resistant patient.Image from CH Holdsworth et al. Phys Med Biol 2012; 57: 8271Figure 2: Simulated T2 MRI radii vs time for the radio-sensitive patient.Image from CH Holdsworth et al. Phys Med Biol 2012; 57: 8271Glioblastoma multiforme (GBM)is a common bra<strong>in</strong> tumour,characterised by extensive<strong>in</strong>filtration <strong>of</strong> normalparenchyma. Radiotherapy <strong>of</strong>GBM typically <strong>in</strong>volves delivery <strong>of</strong>a uniform dose with largemarg<strong>in</strong>s, which does not accountfor patient-specific factors suchas diffuse disease or tumourheterogeneity. Researchers at theUniversity <strong>of</strong> Wash<strong>in</strong>gton MedicalCenter <strong>in</strong> Seattle are address<strong>in</strong>gthis with an <strong>in</strong>tensity-modulatedradiotherapy (IMRT) optimisationalgorithm that <strong>in</strong>corporatespatient-specific parameters.The researchers used a multiobjectiveevolutionary algorithm(MOEA) to perform IMRT planoptimisation. They comb<strong>in</strong>ed thisalgorithm with a GBM modeldescrib<strong>in</strong>g spatial <strong>and</strong> temporalchanges <strong>in</strong> tumour cell density.The GBM model quantifies rates<strong>of</strong> proliferation <strong>and</strong> <strong>in</strong>vasion us<strong>in</strong>gdata derived from MR images.The result<strong>in</strong>g algorithm enabledweekly re-optimisations based onpredicted changes <strong>in</strong> the tumouraris<strong>in</strong>g from radiation-<strong>in</strong>ducedcell kill, tumour diffusion <strong>and</strong>proliferation.The team simulated 7 weeks <strong>of</strong>IMRT for a patient with radioresistantGBM <strong>and</strong> a patient withradio-sensitive disease. Theystudied five differentoptimisations. Three <strong>of</strong> the plansm<strong>in</strong>imised tumour cell survivalafter 1 week <strong>of</strong> treatment, whilerestrict<strong>in</strong>g dose per fraction toany voxel to 3 Gy, 8 Gy or no limit.The other two plans wereoptimised for maximum tumourcell kill 11 weeks after 1 week <strong>of</strong>treatment, both us<strong>in</strong>g an 8 Gyrestriction.The researchers assessed thepredicted tumour radii (as visibleon T2 MRI) over time, <strong>and</strong>compared to a st<strong>and</strong>ard cl<strong>in</strong>icalplan deliver<strong>in</strong>g 61.2 Gy at 1.8 Gyper fraction. They also recordedthe ‘treatment ga<strong>in</strong>’, def<strong>in</strong>ed asthe added number <strong>of</strong> days for thetumor radius to reach 4 cm postradiotherapy,compared with anuntreated control.For both patients, plans with a3 Gy dose limitation showed worseperformance compared to thest<strong>and</strong>ard plan. Tumour controlwas improved by <strong>in</strong>creas<strong>in</strong>g themaximum dose restriction. Forthe radio-resistant patient, theother four plans improvedtreatment ga<strong>in</strong> from 27 days forthe st<strong>and</strong>ard plan to between 77<strong>and</strong> 90 days.For the radio-sensitive patient,tumour response depended uponboth the maximum dose <strong>and</strong> thedecision criteria used. With nodose limit, treatment ga<strong>in</strong>improved from 68 days for thest<strong>and</strong>ard plan to 157 days.However, optimisation based ontumour survival 11 weeks after 1week <strong>of</strong> treatment gave a similartreatment ga<strong>in</strong> <strong>of</strong> 153 days, but ata lower dose, suggest<strong>in</strong>g this asthe best target objective for use <strong>in</strong>the MOEA.The team concluded thatMOEA-optimised plansdemonstrated potential forimproved tumour control overcurrent cl<strong>in</strong>ical practice.‘ MORE INFORMATIONThis paper was published <strong>in</strong> PhysMed Biol 2012; 57: 8271.doi:10.1088/0031-9155/57/24/8271SCOPE | MARCH <strong>2013</strong> | 09