Clinical Practice Guidelines for Hypothyroidism in Adults ...
Clinical Practice Guidelines for Hypothyroidism in Adults ...
Clinical Practice Guidelines for Hypothyroidism in Adults ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
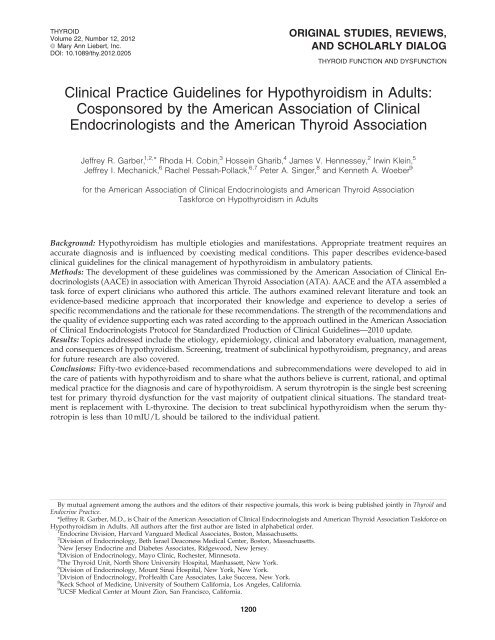
THYROIDVolume 22, Number 12, 2012ª Mary Ann Liebert, Inc.DOI: 10.1089/thy.2012.0205ORIGINAL STUDIES, REVIEWS,AND SCHOLARLY DIALOGTHYROID FUNCTION AND DYSFUNCTION<strong>Cl<strong>in</strong>ical</strong> <strong>Practice</strong> <strong>Guidel<strong>in</strong>es</strong> <strong>for</strong> <strong>Hypothyroidism</strong> <strong>in</strong> <strong>Adults</strong>:Cosponsored by the American Association of <strong>Cl<strong>in</strong>ical</strong>Endocr<strong>in</strong>ologists and the American Thyroid AssociationJeffrey R. Garber, 1,2, * Rhoda H. Cob<strong>in</strong>, 3 Hosse<strong>in</strong> Gharib, 4 James V. Hennessey, 2 Irw<strong>in</strong> Kle<strong>in</strong>, 5Jeffrey I. Mechanick, 6 Rachel Pessah-Pollack, 6,7 Peter A. S<strong>in</strong>ger, 8 and Kenneth A. Woeber 9<strong>for</strong> the American Association of <strong>Cl<strong>in</strong>ical</strong> Endocr<strong>in</strong>ologists and American Thyroid AssociationTask<strong>for</strong>ce on <strong>Hypothyroidism</strong> <strong>in</strong> <strong>Adults</strong>Background: <strong>Hypothyroidism</strong> has multiple etiologies and manifestations. Appropriate treatment requires anaccurate diagnosis and is <strong>in</strong>fluenced by coexist<strong>in</strong>g medical conditions. This paper describes evidence-basedcl<strong>in</strong>ical guidel<strong>in</strong>es <strong>for</strong> the cl<strong>in</strong>ical management of hypothyroidism <strong>in</strong> ambulatory patients.Methods: The development of these guidel<strong>in</strong>es was commissioned by the American Association of <strong>Cl<strong>in</strong>ical</strong> Endocr<strong>in</strong>ologists(AACE) <strong>in</strong> association with American Thyroid Association (ATA). AACE and the ATA assembled atask <strong>for</strong>ce of expert cl<strong>in</strong>icians who authored this article. The authors exam<strong>in</strong>ed relevant literature and took anevidence-based medic<strong>in</strong>e approach that <strong>in</strong>corporated their knowledge and experience to develop a series ofspecific recommendations and the rationale <strong>for</strong> these recommendations. The strength of the recommendations andthe quality of evidence support<strong>in</strong>g each was rated accord<strong>in</strong>g to the approach outl<strong>in</strong>ed <strong>in</strong> the American Associationof <strong>Cl<strong>in</strong>ical</strong> Endocr<strong>in</strong>ologists Protocol <strong>for</strong> Standardized Production of <strong>Cl<strong>in</strong>ical</strong> <strong>Guidel<strong>in</strong>es</strong>—2010 update.Results: Topics addressed <strong>in</strong>clude the etiology, epidemiology, cl<strong>in</strong>ical and laboratory evaluation, management,and consequences of hypothyroidism. Screen<strong>in</strong>g, treatment of subcl<strong>in</strong>ical hypothyroidism, pregnancy, and areas<strong>for</strong> future research are also covered.Conclusions: Fifty-two evidence-based recommendations and subrecommendations were developed to aid <strong>in</strong>the care of patients with hypothyroidism and to share what the authors believe is current, rational, and optimalmedical practice <strong>for</strong> the diagnosis and care of hypothyroidism. A serum thyrotrop<strong>in</strong> is the s<strong>in</strong>gle best screen<strong>in</strong>gtest <strong>for</strong> primary thyroid dysfunction <strong>for</strong> the vast majority of outpatient cl<strong>in</strong>ical situations. The standard treatmentis replacement with L-thyrox<strong>in</strong>e. The decision to treat subcl<strong>in</strong>ical hypothyroidism when the serum thyrotrop<strong>in</strong>is less than 10 mIU/L should be tailored to the <strong>in</strong>dividual patient.By mutual agreement among the authors and the editors of their respective journals, this work is be<strong>in</strong>g published jo<strong>in</strong>tly <strong>in</strong> Thyroid andEndocr<strong>in</strong>e <strong>Practice</strong>.*Jeffrey R. Garber, M.D., is Chair of the American Association of <strong>Cl<strong>in</strong>ical</strong> Endocr<strong>in</strong>ologists and American Thyroid Association Task<strong>for</strong>ce on<strong>Hypothyroidism</strong> <strong>in</strong> <strong>Adults</strong>. All authors after the first author are listed <strong>in</strong> alphabetical order.1 Endocr<strong>in</strong>e Division, Harvard Vanguard Medical Associates, Boston, Massachusetts.2 Division of Endocr<strong>in</strong>ology, Beth Israel Deaconess Medical Center, Boston, Massachusetts.3 New Jersey Endocr<strong>in</strong>e and Diabetes Associates, Ridgewood, New Jersey.4 Division of Endocr<strong>in</strong>ology, Mayo Cl<strong>in</strong>ic, Rochester, M<strong>in</strong>nesota.5 The Thyroid Unit, North Shore University Hospital, Manhassett, New York.6 Division of Endocr<strong>in</strong>ology, Mount S<strong>in</strong>ai Hospital, New York, New York.7 Division of Endocr<strong>in</strong>ology, ProHealth Care Associates, Lake Success, New York.8 Keck School of Medic<strong>in</strong>e, University of Southern Cali<strong>for</strong>nia, Los Angeles, Cali<strong>for</strong>nia.9 UCSF Medical Center at Mount Zion, San Francisco, Cali<strong>for</strong>nia.1200
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1201INTRODUCTIONThese updated cl<strong>in</strong>ical practice guidel<strong>in</strong>es (CPGs)(1–3) summarize the recommendations of the authors,act<strong>in</strong>g as a jo<strong>in</strong>t American Association of <strong>Cl<strong>in</strong>ical</strong> Endocr<strong>in</strong>ologists(AACE) and American Thyroid Association(ATA) task <strong>for</strong>ce <strong>for</strong> the diagnostic evaluation and treatmentstrategies <strong>for</strong> adults with hypothyroidism, as mandated by theBoard of Directors of AACE and the ATA.The ATA develops CPGs to provide guidance and recommendations<strong>for</strong> particular practice areas concern<strong>in</strong>g thyroiddisease, <strong>in</strong>clud<strong>in</strong>g thyroid cancer. The guidel<strong>in</strong>es are not <strong>in</strong>clusiveof all proper approaches or methods, or exclusive ofothers. the guidel<strong>in</strong>es do not establish a standard of care, andspecific outcomes are not guaranteed. Treatment decisionsmust be made based on the <strong>in</strong>dependent judgment of healthcare providers and each patient’s <strong>in</strong>dividual circumstances. Aguidel<strong>in</strong>e is not <strong>in</strong>tended to take the place of physician judgment<strong>in</strong> diagnos<strong>in</strong>g and treatment of particular patients (<strong>for</strong>detailed <strong>in</strong><strong>for</strong>mation regard<strong>in</strong>g ATA guidel<strong>in</strong>es, see the SupplementaryData, available onl<strong>in</strong>e at www.liebertpub.com/thy).The AACE Medical <strong>Guidel<strong>in</strong>es</strong> <strong>for</strong> <strong>Cl<strong>in</strong>ical</strong> <strong>Practice</strong> aresystematically developed statements to assist health careprofessionals <strong>in</strong> medical decision mak<strong>in</strong>g <strong>for</strong> specific cl<strong>in</strong>icalconditions. Most of their content is based on literature reviews.In areas of uncerta<strong>in</strong>ty, professional judgment is applied(<strong>for</strong> detailed <strong>in</strong><strong>for</strong>mation regard<strong>in</strong>g AACE guidel<strong>in</strong>es,see the Supplementary Data).These guidel<strong>in</strong>es are a document that reflects the currentstate of the field and are <strong>in</strong>tended to provide a work<strong>in</strong>g document<strong>for</strong> guidel<strong>in</strong>e updates s<strong>in</strong>ce rapid changes <strong>in</strong> this fieldare expected <strong>in</strong> the future. We encourage medical professionalsto use this <strong>in</strong><strong>for</strong>mation <strong>in</strong> conjunction with their bestcl<strong>in</strong>ical judgment. The presented recommendations may notbe appropriate <strong>in</strong> all situations. Any decision by practitionersto apply these guidel<strong>in</strong>es must be made <strong>in</strong> light of local resourcesand <strong>in</strong>dividual patient circumstances.The guidel<strong>in</strong>es presented here pr<strong>in</strong>cipally address themanagement of ambulatory patients with biochemicallyconfirmed primary hypothyroidism whose thyroid status hasbeen stable <strong>for</strong> at least several weeks. They do not deal withmyxedema coma. The <strong>in</strong>terested reader is directed to the othersources <strong>for</strong> this <strong>in</strong><strong>for</strong>mation (4). The organization of theguidel<strong>in</strong>es is presented <strong>in</strong> Table 1.Serum thyrotrop<strong>in</strong> (TSH) is the s<strong>in</strong>gle best screen<strong>in</strong>g test <strong>for</strong>primary thyroid dysfunction <strong>for</strong> the vast majority of outpatientcl<strong>in</strong>ical situations, but it is not sufficient <strong>for</strong> assess<strong>in</strong>g hospitalizedpatients or when central hypothyroidism is either presentor suspected. The standard treatment is replacement withL-thyrox<strong>in</strong>e which must be tailored to the <strong>in</strong>dividual patient.The therapy and diagnosis of subcl<strong>in</strong>ical hypothyroidism,which often rema<strong>in</strong>s undetected, is discussed. L-triiodothyron<strong>in</strong>e<strong>in</strong> comb<strong>in</strong>ation with L-thyrox<strong>in</strong>e <strong>for</strong> treat<strong>in</strong>g hypothyroidism,thyroid hormone <strong>for</strong> conditions other thanhypothyroidism, and nutraceuticals are considered.METHODSThis CPG adheres to the 2010 AACE Protocol <strong>for</strong> StandardizedProduction of <strong>Cl<strong>in</strong>ical</strong> <strong>Practice</strong> <strong>Guidel<strong>in</strong>es</strong> published<strong>in</strong> Endocr<strong>in</strong>e <strong>Practice</strong> (5). This updated protocol describes amore transparent methodology of rat<strong>in</strong>g the cl<strong>in</strong>ical evidenceand synthesiz<strong>in</strong>g recommendation grades. The protocol alsostipulates a rigorous multilevel review process.The process was begun by develop<strong>in</strong>g an outl<strong>in</strong>e <strong>for</strong> review<strong>in</strong>gthe pr<strong>in</strong>cipal cl<strong>in</strong>ical aspects of hypothyroidism.Computerized and manual searches of the medical literatureand various databases, primarily <strong>in</strong>clud<strong>in</strong>g Medl<strong>in</strong>e Ò , werebased on specific section titles, thereby avoid<strong>in</strong>g <strong>in</strong>clusion ofTable 1. Organization of <strong>Cl<strong>in</strong>ical</strong> <strong>Practice</strong> <strong>Guidel<strong>in</strong>es</strong> <strong>for</strong> <strong>Hypothyroidism</strong> <strong>in</strong> <strong>Adults</strong>Introduction 1201Methods 1201Objectives 1204<strong>Guidel<strong>in</strong>es</strong> <strong>for</strong> CPGs 1204Levels of scientific substantiation and recommendation grades (transparency) 1204Summary of recommendation grades 1205Topics Relat<strong>in</strong>g to <strong>Hypothyroidism</strong> 1205Epidemiology 1205Primary and secondary etiologies of hypothyroidism 1206Disorders associated with hypothyroidism 1207Signs and symptoms of hypothyroidism 1207Measurement of T 4 and T 3 1207Pitfalls encountered when <strong>in</strong>terpret<strong>in</strong>g serum TSH levels 1208Other diagnostic tests <strong>for</strong> hypothyroidism 1209Screen<strong>in</strong>g and aggressive case f<strong>in</strong>d<strong>in</strong>g <strong>for</strong> hypothyroidism 1209When to treat hypothyroidism 1210L-thyrox<strong>in</strong>e treatment of hypothyroidism 1210Therapeutic endpo<strong>in</strong>ts <strong>in</strong> the treatment of hypothyroidism 1213When to consult an endocr<strong>in</strong>ologist 1214Concurrent conditions of special significance <strong>in</strong> hypothyroid patients 1214<strong>Hypothyroidism</strong> dur<strong>in</strong>g pregnancy 1214Diabetes mellitus 1215Infertility 1215Page(cont<strong>in</strong>ued)
1202 GARBER ET AL.Table 1. (Cont<strong>in</strong>ued)PageObesity 1215Patients with normal thyroid tests 1215Depression 1215Nonthyroidal illness 1215Dietary supplements and nutraceuticals <strong>in</strong> the treatment of hypothyroidism 1216Overlap of symptoms <strong>in</strong> euthyroid and hypothyroid patients 1216Excess iod<strong>in</strong>e <strong>in</strong>take and hypothyroidism 1216Desiccated thyroid 12163,5,3¢-Triiodothyroacetic acid 1217Thyroid-enhanc<strong>in</strong>g preparations 1217Thyromimetic preparations 1217Selenium 1217Questions and Guidel<strong>in</strong>e Recommendations 1217Q1 When should anti-thyroid antibodies be measured? 1217R1 TPOAb measurements and subcl<strong>in</strong>ical hypothyroidism 1217R2 TPOAb measurements and nodular thyroid disease 1217R3 TPOAb measurements and recurrent miscarriage 1217R4 TSHRAb measurements <strong>in</strong> women with Graves’ disease who have1217had thyroidectomy or RAI treatment be<strong>for</strong>e pregnancyQ2 What is the role of cl<strong>in</strong>ical scor<strong>in</strong>g systems <strong>in</strong> the diagnosis of patients1218with hypothyroidism?R5 Do not use cl<strong>in</strong>ical scor<strong>in</strong>g systems to diagnose hypothyroidism 1218Q3 What is the role of diagnostic tests apart from serum thyroid hormone levels and TSH <strong>in</strong>1218the evaluation of patients with hypothyroidism?R6 Do not use <strong>in</strong>direct tests to diagnose hypothyroidism 1218Q4 What are the preferred thyroid hormone measurements <strong>in</strong> addition to TSH <strong>in</strong> the assessment of1218patients with hypothyroidism?R7 When to use free T 4 vs. total T 4 1218R8 Us<strong>in</strong>g free T 4 to monitor L-thyrox<strong>in</strong>e treatment 1218R9 Estimat<strong>in</strong>g serum free T 4 <strong>in</strong> pregnancy 1218R10 Prohibition aga<strong>in</strong>st us<strong>in</strong>g T 3 to diagnose hypothyroidism 1218R11 Measur<strong>in</strong>g TSH <strong>in</strong> hospitalized patients 1218R12 Serum T 4 vs. TSH <strong>for</strong> management of central hypothyroidism 1218Q5 When should TSH levels be measured <strong>in</strong> patients be<strong>in</strong>g treated <strong>for</strong> hypothyroidism? 1218R13 When to measure TSH <strong>in</strong> patients tak<strong>in</strong>g L-thyrox<strong>in</strong>e <strong>for</strong> hypothyroidism 1218Q6 What should be considered the upper limit of the normal range of TSH values? 1218R14.1 Reference ranges <strong>for</strong> TSH, age, and lab variability 1218R14.2 Reference ranges <strong>for</strong> TSH <strong>in</strong> pregnant women 1218Q7 Which patients with TSH levels above a given laboratory’s reference range should be considered <strong>for</strong> 1219treatment with L-thyrox<strong>in</strong>e?R15 Treat<strong>in</strong>g patients with TSH above 10 mIU/L 1219R16 Treat<strong>in</strong>g if TSH is elevated but below 10 mIU/L 1219Q8 In patients with hypothyroidism be<strong>in</strong>g treated with L-thyrox<strong>in</strong>e what should the target TSH1219ranges be?R17 Target TSH when treat<strong>in</strong>g hypothyroidism 1219Q9 In patients with hypothyroidism be<strong>in</strong>g treated with L-thyrox<strong>in</strong>e who are pregnant, what should the 1219target TSH ranges be?R18 Target TSH when treat<strong>in</strong>g hypothyroid pregnant women 1219Q10 Which patients with normal serum TSH levels should be considered <strong>for</strong> treatment with1219L-thyrox<strong>in</strong>e?R19.1 L-thyrox<strong>in</strong>e treatment <strong>in</strong> pregnant women with ‘‘normal’’ TSH 1219R19.2 L-thyrox<strong>in</strong>e treatment <strong>in</strong> women of child-bear<strong>in</strong>g age or pregnant with ‘‘normal’’ TSH1219and have positive TPOAb or history of miscarriage or hypothyroidismR19.3 L-thyrox<strong>in</strong>e treatment <strong>in</strong> pregnant women or those plann<strong>in</strong>g pregnancy with TPOAb1219and serum TSH is > 2.5 mIU/LR19.4 Monitor<strong>in</strong>g of pregnant women with TPOAb or a ‘‘normal’’ TSH but > 2.5 mIU/L1219who are not tak<strong>in</strong>g L-thyrox<strong>in</strong>eQ11 Who, among patients who are pregnant, or plann<strong>in</strong>g pregnancy, or with other characteristics,1220should be screened <strong>for</strong> hypothyroidism?R20.1.1 Universal screen<strong>in</strong>g of women plann<strong>in</strong>g pregnancy <strong>in</strong>cluded assisted reproduction 1220R20.1.2 Aggressive case f<strong>in</strong>d<strong>in</strong>g <strong>for</strong> hypothyroidism <strong>for</strong> women plann<strong>in</strong>g pregnancy 1220R20.2 Age and screen<strong>in</strong>g <strong>for</strong> hypothyroidism 1220(cont<strong>in</strong>ued)
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1203Table 1. (Cont<strong>in</strong>ued)PageR21 Aggressive case f<strong>in</strong>d<strong>in</strong>g <strong>for</strong> hypothyroidism—whom to target 1220Q12 How should patients with hypothyroidism be treated and monitored? 1220R22.1 Form of thyroid hormone <strong>for</strong> treatment of hypothyroidism 1220R22.2 L-thyrox<strong>in</strong>e and L-triiodothyron<strong>in</strong>e comb<strong>in</strong>ations to treat hypothyroidism 1220R22.3 Prohibition aga<strong>in</strong>st us<strong>in</strong>g L-thyrox<strong>in</strong>e and L-triiodothyron<strong>in</strong>e comb<strong>in</strong>ations1220to treat pregnant women or those plann<strong>in</strong>g pregnancyR22.4 Prohibition aga<strong>in</strong>st us<strong>in</strong>g desiccated thyroid hormone to treat hypothyroidism 1220R22.5 Prohibition aga<strong>in</strong>st us<strong>in</strong>g TRIAC (tiratricol) to treat hypothyroidism 1220R22.6 Resum<strong>in</strong>g L-thyrox<strong>in</strong>e treatment <strong>for</strong> hypothyroidism <strong>in</strong> patients without cardiac events 1220R22.7.1 L-thyrox<strong>in</strong>e treatment <strong>for</strong> overt hypothyroidism <strong>in</strong> young healthy adults 1220R22.7.2 L-thyrox<strong>in</strong>e treatment <strong>for</strong> overt hypothyroidism <strong>in</strong> patients older than 50 to 60 years 1220R22.8 L-thyrox<strong>in</strong>e treatment <strong>for</strong> subcl<strong>in</strong>ical hypothyroidism compared to overt1220hypothyroidismR22.9 Order of L-thyrox<strong>in</strong>e treatment and glucocorticoids <strong>in</strong> patients with adrenal1221<strong>in</strong>sufficiency and hypothyroidismR23 L-thyrox<strong>in</strong>e treatment <strong>for</strong> hypothyroidism—time to take, method of tak<strong>in</strong>g,1221and storageR24 Free T 4 as the target measurement when treat<strong>in</strong>g central hypothyroidism 1221R25.1 Test<strong>in</strong>g and treat<strong>in</strong>g women with hypothyroidism as soon as they become pregnant 1221R25.2 Goal TSH <strong>in</strong> pregnant women with hypothyroidism 1221R25.3 Monitor<strong>in</strong>g pregnant women with hypothyroidism 1221R26 Monitor<strong>in</strong>g hypothyroid patients who start drugs affect<strong>in</strong>g T 4 bioavailability1221or metabolismR27 Prohibition aga<strong>in</strong>st target<strong>in</strong>g specific TSH values <strong>in</strong> hypothyroid patients who are1221not pregnantQ13 When should endocr<strong>in</strong>ologists be <strong>in</strong>volved <strong>in</strong> the care of patients with hypothyroidism? 1221R28 Type of hypothyroid patient who should be seen <strong>in</strong> consultation with1221an endocr<strong>in</strong>ologistQ14 Which patients should not be treated with thyroid hormone? 1221R29 Need <strong>for</strong> biochemical confirmation of the diagnosis be<strong>for</strong>e chronic treatment1221of hypothyroidismR30 Prohibition aga<strong>in</strong>st us<strong>in</strong>g thyroid hormone to treat obesity 1221R31 Thyroid hormone treatment and depression 1222Q15 What is the role of iod<strong>in</strong>e supplementation, dietary supplements, and nutraceuticals1222<strong>in</strong> the treatment of hypothyroidism?R32.1 Prohibition aga<strong>in</strong>st us<strong>in</strong>g iod<strong>in</strong>e supplementation to treat hypothyroidism1222<strong>in</strong> iod<strong>in</strong>e-sufficient areasR32.2 Inappropriate method <strong>for</strong> iod<strong>in</strong>e supplementation <strong>in</strong> pregnant women 1222R33 Prohibition aga<strong>in</strong>st us<strong>in</strong>g selenium as treatment or preventive measure1222<strong>for</strong> hypothyroidismR34 Recommendation regard<strong>in</strong>g dietary supplements, nutraceuticals,1222and products marked as ‘‘thyroid support’’ <strong>for</strong> hypothyroidismAreas <strong>for</strong> Future Research 1222Cardiac benefit from treat<strong>in</strong>g subcl<strong>in</strong>ical hypothyroidism 1222Cognitive benefit from treat<strong>in</strong>g subcl<strong>in</strong>ical hypothyroidism 1223L-thyrox<strong>in</strong>e/L-triiodothyron<strong>in</strong>e comb<strong>in</strong>ation therapy 1223L-triiodothyron<strong>in</strong>e monotherapy 1223Thyroid hormone analogues 1223Screen<strong>in</strong>g <strong>for</strong> hypothyroidism <strong>in</strong> pregnancy 1223Agents and conditions hav<strong>in</strong>g an impact on L-thyrox<strong>in</strong>e therapy and <strong>in</strong>terpretation1223of thyroid testsAuthor Disclosure Statement 1224Acknowledgments 1224References <strong>in</strong>clud<strong>in</strong>g authors’ evidence level (EL) rank<strong>in</strong>gs 1224Supplementary DataOnl<strong>in</strong>e at www.liebertpub.com/thy1. Supplementary <strong>in</strong><strong>for</strong>mation regard<strong>in</strong>g ATA and AACE guidel<strong>in</strong>es2. Complete list of guidel<strong>in</strong>e recommendationsNote: When referr<strong>in</strong>g to therapy and therapeutic preparations <strong>in</strong> the recommendations and elsewhere, L-thyrox<strong>in</strong>e and L-triiodothyron<strong>in</strong>eare generally used <strong>in</strong>stead of their respective hormonal equivalents, T 4 and T 3 .AACE, American Association of <strong>Cl<strong>in</strong>ical</strong> Endocr<strong>in</strong>ologists; ATA, American Thyroid Association; CPG, <strong>Cl<strong>in</strong>ical</strong> <strong>Practice</strong> Guidel<strong>in</strong>e; RAI,radioactive iod<strong>in</strong>e; T 3 , triiodothyron<strong>in</strong>e; T 4 , thyrox<strong>in</strong>e; TPOAb, anti–thyroid peroxidase antibodies; TRIAC, 3,5,3¢-triiodothyroacetic acid;TSH, thyrotrop<strong>in</strong>; TSHRAb, TSH receptor antibodies.
1204 GARBER ET AL.unnecessary detail and exclusion of important studies. Compilationof the bibliography was a cont<strong>in</strong>ual and dynamicprocess. Once the pr<strong>in</strong>cipal cl<strong>in</strong>ical aspects of hypothyroidismwere def<strong>in</strong>ed, questions were <strong>for</strong>mulated with the <strong>in</strong>tent tothen develop recommendations that addressed these questions.The grad<strong>in</strong>g of recommendations was based on consensusamong the authors.The f<strong>in</strong>al document was approved by the American Associationof <strong>Cl<strong>in</strong>ical</strong> Endocr<strong>in</strong>ologists (AACE) and AmericanThyroid Association (ATA), and was officially endorsed bythe American Association of Diabetes Educators (AADE),American Academy of Otolaryngology—Head and NeckSurgery (AAO-HNS), American College of Endocr<strong>in</strong>ology(ACE), Italian Association of <strong>Cl<strong>in</strong>ical</strong> Endocr<strong>in</strong>ologists(AME), American Society <strong>for</strong> Metabolic & Bariatric Surgery(ASMBS), The Endocr<strong>in</strong>e Society of Australia (ESA), InternationalAssociation of Endocr<strong>in</strong>e Surgeons (IAES), Lat<strong>in</strong>American Thyroid Society (LATS), and Ukranian Associationof Endocr<strong>in</strong>e Surgeons (UAES).ObjectivesThe purpose of these guidel<strong>in</strong>es is to present an updatedevidence-based framework <strong>for</strong> the diagnosis, treatment, andfollow-up of patients with hypothyroidism.<strong>Guidel<strong>in</strong>es</strong> <strong>for</strong> CPGsCurrent guidel<strong>in</strong>es <strong>for</strong> CPGs <strong>in</strong> cl<strong>in</strong>ical medic<strong>in</strong>e emphasizean evidence-based approach rather than simply expert op<strong>in</strong>ion(6). Even though a purely evidence-based approach is notapplicable to all actual cl<strong>in</strong>ical scenarios, we have <strong>in</strong>corporatedthis <strong>in</strong>to these CPGs to provide objectivity.Levels of scientific substantiation andrecommendation grades (transparency)All cl<strong>in</strong>ical data that are <strong>in</strong>corporated <strong>in</strong> these CPGs havebeen evaluated <strong>in</strong> terms of levels of scientific substantiation.The detailed methodology <strong>for</strong> assign<strong>in</strong>g evidence levels(ELs) to the references used <strong>in</strong> these CPGs has been reportedby Mechanick et al. (7), from which Table 2 is taken. Theauthors’ EL rat<strong>in</strong>gs of the references are <strong>in</strong>cluded <strong>in</strong> theReferences section. The four-step approach that the authorsused to grade recommendations is summarized <strong>in</strong> Tables 3,4, 5, and 6 of the 2010 Standardized Production of <strong>Cl<strong>in</strong>ical</strong><strong>Practice</strong> <strong>Guidel<strong>in</strong>es</strong> (5), from which Table 3 is taken. Byexplicitly provid<strong>in</strong>g numerical and semantic descriptorsof the cl<strong>in</strong>ical evidence as well as relevant subjectivefactors and study flaws, the updated protocol has greatertransparency than the 2008 AACE protocol described byMechanick et al. (7).In these guidel<strong>in</strong>es, the grad<strong>in</strong>g system used <strong>for</strong> the recommendationsdoes not reflect the <strong>in</strong>struction of the recommendation,but the strength of the recommendation. Forexample <strong>in</strong> some grad<strong>in</strong>g systems ‘‘should not’’ implies thatthere is substantial evidence to support a recommendation.However the grad<strong>in</strong>g method employed <strong>in</strong> this guidel<strong>in</strong>eTable 2. Levels of Scientific Substantiation <strong>in</strong> Evidence-Based Medic<strong>in</strong>eLevel Description Comments1 Prospective, randomized, controlledtrials—large2 Prospective controlled trials with orwithout randomization—limitedbody of outcome data3 Other experimental outcomedata and nonexperimental dataData are derived from a substantial number of trials with adequatestatistical power <strong>in</strong>volv<strong>in</strong>g a substantial number of outcome datasubjects.Large meta-analyses us<strong>in</strong>g raw or pooled data or <strong>in</strong>corporat<strong>in</strong>gquality rat<strong>in</strong>gsWell-controlled trial at one or more centersConsistent pattern of f<strong>in</strong>d<strong>in</strong>gs <strong>in</strong> the population <strong>for</strong> which therecommendation is made (generalizable data).Compell<strong>in</strong>g nonexperimental, cl<strong>in</strong>ically obvious, evidence (e.g., thyroidhormone treatment <strong>for</strong> myxedema coma), ‘‘all-or-none’’ <strong>in</strong>dicationLimited number of trials, small population sites <strong>in</strong> trialsWell-conducted s<strong>in</strong>gle-arm prospective cohort studyLimited but well-conducted meta-analysesInconsistent f<strong>in</strong>d<strong>in</strong>gs or results not representative <strong>for</strong> the targetpopulationWell-conducted case-controlled studyNonrandomized, controlled trialsUncontrolled or poorly controlled trialsAny randomized cl<strong>in</strong>ical trial with one or more major or threeor more m<strong>in</strong>or methodological flawsRetrospective or observational dataCase reports or case seriesConflict<strong>in</strong>g data with weight of evidence unable to supporta f<strong>in</strong>al recommendation4 Expert op<strong>in</strong>ion Inadequate data <strong>for</strong> <strong>in</strong>clusion <strong>in</strong> level 1, 2, or 3; necessitatesan expert panel’s synthesis of the literature and a consensusExperience basedTheory drivenLevels 1, 2, and 3 represent a given level of scientific substantiation or proof. Level 4 or Grade D represents unproven claims. It is the ‘‘bestevidence’’ based on the <strong>in</strong>dividual rat<strong>in</strong>gs of cl<strong>in</strong>ical reports that contributes to a f<strong>in</strong>al grade recommendation.Source: Mechanick et al., 2008 (7).
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1205BestevidencelevelTable 3. Grade-Recommendation Protocol2010 AACE Protocol <strong>for</strong> Production of <strong>Cl<strong>in</strong>ical</strong> <strong>Practice</strong><strong>Guidel<strong>in</strong>es</strong>—Step III: Grad<strong>in</strong>g of recommendations;How different evidence levels can be mappedto the same recommendation gradeSubjectivefactorimpactTwothirdsRecommendationconsensus Mapp<strong>in</strong>g a grade1 None Yes Direct A2 Positive Yes Adjust up A2 None Yes Direct B1 Negative Yes Adjust down B3 Positive Yes Adjust up B3 None Yes Direct C2 Negative Yes Adjust down C4 Positive Yes Adjust up C4 None Yes Direct D3 Negative Yes Adjust down D1,2,3,4 N/A No Adjust down DAdopted by the AACE and the ATA <strong>for</strong> the <strong>Hypothyroidism</strong> CPG.a Start<strong>in</strong>g with the left column, best evidence levels (BELs),subjective factors, and consensus map to recommendation grades<strong>in</strong> the right column. When subjective factors have little or no impact(‘‘none’’), then the BEL is directly mapped to recommendationgrades. When subjective factors have a strong impact, then recommendationgrades may be adjusted up (‘‘positive’’ impact) or down(‘‘negative’’ impact). If a two-thirds consensus cannot be reached,then the recommendation grade is D.Source: Mechanick et al., 2010 (5).N/A, not applicable (regardless of the presence or absence ofstrong subjective factors, the absence of a two-thirds consensusmandates a recommendation grade D).enables authors to use this language even when the best evidencelevel available is ‘‘expert op<strong>in</strong>ion.’’ Although differentgrad<strong>in</strong>g systems were employed, an ef<strong>for</strong>t was made to makethese recommendations consistent with related portions of‘‘Hyperthyroidism and Other Causes of Thyrotoxicosis:Management <strong>Guidel<strong>in</strong>es</strong> of the American Thyroid Associationand American Association of <strong>Cl<strong>in</strong>ical</strong> Endocr<strong>in</strong>ologists’’(8,9), as well as the ‘‘<strong>Guidel<strong>in</strong>es</strong> of the American ThyroidAssociation <strong>for</strong> the Diagnosis and Management of ThyroidDisease Dur<strong>in</strong>g Pregnancy and Postpartum’’ (10).The shortcom<strong>in</strong>gs of this evidence-based methodology <strong>in</strong>these CPGs are that many recommendations are based onweak scientific data (Level 3) or consensus op<strong>in</strong>ion (Level 4),rather than strong scientific data (Levels 1 and 2). There arealso the problems of (i) subjectivity on the part of the authorswhen weigh<strong>in</strong>g positive and negative, or epidemiologicversus experimental, data <strong>in</strong> order to arrive at an evidencebasedrecommendation grade or consensus op<strong>in</strong>ion, (ii) subjectivityon the part of the authors when weigh<strong>in</strong>g subjectiveattributes, such as cost effectiveness and risk-to-benefit ratios,<strong>in</strong> order to arrive at an evidence-based recommendationgrade or consensus op<strong>in</strong>ion, (iii) potentially <strong>in</strong>complete reviewof the literature by the authors despite extensive diligence,and (iv) bias <strong>in</strong> the available publications, whichorig<strong>in</strong>ate predom<strong>in</strong>antly from experienced cl<strong>in</strong>icians andlarge academic medical centers and may, there<strong>for</strong>e, not reflectthe experience at large. The authors, through an a priorimethodology and multiple levels of review, have tried toaddress these shortcom<strong>in</strong>gs by discussions with three experts(see Acknowledgments).Summary of recommendation gradesThe recommendations are evidence-based (Grades A, B, andC) or based on expert op<strong>in</strong>ion because of a lack of conclusivecl<strong>in</strong>ical evidence (Grade D). The ‘‘best evidence’’ rat<strong>in</strong>g level(BEL), which corresponds to the best conclusive evidencefound, accompanies the recommendation grade. Details regard<strong>in</strong>gthe mapp<strong>in</strong>g of cl<strong>in</strong>ical evidence rat<strong>in</strong>gs to these recommendationgrades have already been provided [see Levels ofscientific substantiation and recommendation grades (transparency)].In this CPG, a substantial number of recommendations areupgraded or downgraded because the conclusions may notapply <strong>in</strong> other situations (non-generalizability). For example,what applies to an elderly population with established cardiacdisease may not apply to a younger population without cardiacrisk factors. Whenever expert op<strong>in</strong>ions resulted <strong>in</strong> upgrad<strong>in</strong>gor downgrad<strong>in</strong>g a recommendation, it is explicitly stated afterthe recommendation.TOPICS RELATING TO HYPOTHYROIDISMEpidemiology<strong>Hypothyroidism</strong> may be either subcl<strong>in</strong>ical or overt. Subcl<strong>in</strong>icalhypothyroidism is characterized by a serum TSHabove the upper reference limit <strong>in</strong> comb<strong>in</strong>ation with a normalfree thyrox<strong>in</strong>e (T 4 ). This designation is only applicable whenthyroid function has been stable <strong>for</strong> weeks or more, the hypothalamic–pituitary–thyroidaxis is normal, and there is norecent or ongo<strong>in</strong>g severe illness. An elevated TSH, usuallyabove 10 mIU/L, <strong>in</strong> comb<strong>in</strong>ation with a subnormal free T 4characterizes overt hypothyroidism.The results of four studies are summarized <strong>in</strong> Table 4.The National Health and Nutrition Exam<strong>in</strong>ation Survey(NHANES III) studied an unselected U.S. population over age12 between 1988 and 1994, us<strong>in</strong>g the upper limit of normal <strong>for</strong>Table 4. Prevalence of <strong>Hypothyroidism</strong>Study Subcl<strong>in</strong>ical Overt TSH CommentNHANES III 4.3% 0.3% 4.5Colorado Thyroid Disease Prevalence 8.5% 0.4% 5.0 Not on thyroid hormoneFram<strong>in</strong>gham 10.0 Over age 60 years: 5.9% women; 2.3% men; 39% ofwhom had subnormal T 4British Whickham 10.0 9.3% women; 1.2% menSources: Hollowell et al., 2002 (11); Canaris et al., 2000 (12); Saw<strong>in</strong> et al., 1985 (13); Vanderpump et al., 1995 (14); Vanderpump andTunbridge, 2002 (15).NHANES, National Health and Nutrition Exam<strong>in</strong>ation Survey.
1206 GARBER ET AL.TSH as 4.5 mIU/mL (11). The prevalence of subcl<strong>in</strong>ical diseasewas 4.3% and of overt disease was 0.3%. The Coloradothyroid disease prevalence survey, <strong>in</strong> which self-selected <strong>in</strong>dividualsattend<strong>in</strong>g a health fair were tested and an uppernormal TSH value of 5.0 mIU/L was used, reported a prevalenceof 8.5% and 0.4% <strong>for</strong> subcl<strong>in</strong>ical and overt disease,respectively, <strong>in</strong> people not tak<strong>in</strong>g thyroid hormone (12). In theFram<strong>in</strong>gham study, 5.9% of women and 2.3% of men over theage of 60 years had TSH values over 10 mIU/L, 39% of whomhad subnormal T 4 levels (13). In the British Whickham survey9.3% of women and 1.2% of men had serum TSH values over10 mIU/L (14,15). The <strong>in</strong>cidence of hypothyroidism <strong>in</strong> womenwas 3.5 per 1000 survivors per year and <strong>in</strong> men it was 0.6 per1000 survivors per year. The risk of develop<strong>in</strong>g hypothyroidism<strong>in</strong> women with positive antibodies and elevated TSHwas 4% per year versus 2%–3% per year <strong>in</strong> those with eitheralone (14,15). In men the relative risk rose even more <strong>in</strong> eachcategory, but the rates rema<strong>in</strong>ed well below those of women.Primary and secondary etiologiesof hypothyroidismEnvironmental iod<strong>in</strong>e deficiency is the most commoncause of hypothyroidism on a worldwide basis (16). In areasof iod<strong>in</strong>e sufficiency, such as the United States, the mostcommon cause of hypothyroidism is chronic autoimmunethyroiditis (Hashimoto’s thyroiditis). Autoimmune thyroiddiseases (AITDs) have been estimated to be 5–10 times morecommon <strong>in</strong> women than <strong>in</strong> men. The ratio varies from seriesto series and is dependent on the def<strong>in</strong>ition of disease,whether it is cl<strong>in</strong>ically evident or not. In the Whickhamsurvey (14), <strong>for</strong> example, 5% of women and 1% of men hadboth positive antibody tests and a serum TSH value > 6.This <strong>for</strong>m of AITD (i.e., Hashimoto’s thyroiditis, chronicautoimmune thyroiditis) <strong>in</strong>creases <strong>in</strong> frequency with age(11), and is more common <strong>in</strong> people with other autoimmunediseases and their families (17–25). Goiter may or may notbe present.AITDs are characterized pathologically by <strong>in</strong>filtration ofthe thyroid with sensitized T lymphocytes and serologicallyby circulat<strong>in</strong>g thyroid autoantibodies. Autoimmunity to thethyroid gland appears to be an <strong>in</strong>herited defect <strong>in</strong> immunesurveillance, lead<strong>in</strong>g to abnormal regulation of immune responsivenessor alteration of present<strong>in</strong>g antigen <strong>in</strong> the thyroid(26,27).One of the keys to diagnos<strong>in</strong>g AITDs is determ<strong>in</strong><strong>in</strong>gthe presence of elevated anti-thyroid antibody titerswhich <strong>in</strong>clude anti-thyroglobul<strong>in</strong> antibodies (TgAb), anti–microsomal/thyroid peroxidase antibodies (TPOAb), andTSH receptor antibodies (TSHRAb). Many patients withchronic autoimmune thyroiditis are biochemically euthyroid.However, approximately 75% have elevated anti-thyroidantibody titers. Once present, these antibodies generallypersist, with spontaneous disappearance occurr<strong>in</strong>g <strong>in</strong>frequently.Among the disease-free population <strong>in</strong> the NHANESsurvey, tests <strong>for</strong> TgAb were positive <strong>in</strong> 10.4% and TPOAb <strong>in</strong>11.3%. These antibodies were more common <strong>in</strong> women thanmen and <strong>in</strong>creased with age. Only positive TPOAb tests weresignificantly associated with hypothyroidism (11). The presenceof elevated TPOAb titers <strong>in</strong> patients with subcl<strong>in</strong>icalhypothyroidism helps to predict progression to overt hypothyroidism—4.3%per year with TPOAb vs. 2.6% per yearwithout elevated TPOAb titers (14,28). The higher risk ofdevelop<strong>in</strong>g overt hypothyroidism <strong>in</strong> TPOAb-positive patientsis the reason that several professional societies and manycl<strong>in</strong>ical endocr<strong>in</strong>ologists endorse measurement of TPOAbs <strong>in</strong>those with subcl<strong>in</strong>ical hypothyroidism.In patients with a diffuse, firm goiter, TPOAb should bemeasured to identify autoimmune thyroiditis. S<strong>in</strong>ce nonimmunologicallymediated mult<strong>in</strong>odular goiter is rarely associatedwith destruction of function<strong>in</strong>g tissue andprogression to hypothyroidism (29), it is important to identifythose patients with the nodular variant of autoimmune thyroiditis<strong>in</strong> whom these risks are significant. In some cases,particularly <strong>in</strong> those with thyroid nodules, f<strong>in</strong>e-needle aspiration(FNA) biopsy helps confirm the diagnosis and to excludemalignancy. Also, <strong>in</strong> patients with documentedhypothyroidism, measurement of TPOAb identifies the cause.In the presence of other autoimmune disease such astype 1 diabetes (20,21) or Addison’s disease (17,18), chromosomaldisorders such as Down’s (30) or Turner’s syndrome(31), and therapy with drugs such as lithium (32–34), <strong>in</strong>terferonalpha (35,36), and amiodarone (37) or excess iod<strong>in</strong>e <strong>in</strong>gestion(e.g., kelp) (38–40), TPOAb measurement may provide prognostic<strong>in</strong><strong>for</strong>mation on the risk of develop<strong>in</strong>g hypothyroidism.TSHRAb may act as a TSH agonist or antagonist (41).Thyroid stimulat<strong>in</strong>g immunoglobul<strong>in</strong> (TSI) and/or thyrotrop<strong>in</strong>b<strong>in</strong>d<strong>in</strong>g <strong>in</strong>hibitory immunoglobul<strong>in</strong> (TBII) levels,employ<strong>in</strong>g sensitive assays, should be measured <strong>in</strong> euthyroidor L-thyrox<strong>in</strong>e–treated hypothyroid pregnant womenwith a history of Graves’ disease because they are predictorsof fetal and neonatal thyrotoxicosis (42). S<strong>in</strong>ce the risk <strong>for</strong>thyrotoxicosis correlates with the magnitude of elevation ofTSI, and s<strong>in</strong>ce TSI levels tend to fall dur<strong>in</strong>g the second trimester,TSI measurements are most <strong>in</strong><strong>for</strong>mative when done<strong>in</strong> the early third trimester. The argument <strong>for</strong> measurementearlier <strong>in</strong> pregnancy is also based, <strong>in</strong> part, on determ<strong>in</strong><strong>in</strong>gwhether establish<strong>in</strong>g a surveillance program <strong>for</strong> ongo<strong>in</strong>gfetal and subsequent neonatal thyroid dysfunction isnecessary (43).<strong>Hypothyroidism</strong> may occur as a result of radioiod<strong>in</strong>e orsurgical treatment <strong>for</strong> hyperthyroidism, thyroid cancer, orbenign nodular thyroid disease and after external beam radiation<strong>for</strong> non–thyroid-related head and neck malignancies,<strong>in</strong>clud<strong>in</strong>g lymphoma. A relatively new pharmacologic causeof iatrogenic hypothyroidism is the tyros<strong>in</strong>e k<strong>in</strong>ase <strong>in</strong>hibitors,most notably sunit<strong>in</strong>ib (44,45), which may <strong>in</strong>duce hypothyroidismthrough reduction of glandular vascularity and <strong>in</strong>ductionof type 3 deiod<strong>in</strong>ase activity.Central hypothyroidism occurs when there is <strong>in</strong>sufficientproduction of bioactive TSH (46,47) due to pituitary or hypothalamictumors (<strong>in</strong>clud<strong>in</strong>g craniopharyngiomas), <strong>in</strong>flammatory(lymphocytic or granulomatous hypophysitis) or<strong>in</strong>filtrative diseases, hemorrhagic necrosis (Sheehan’s syndrome),or surgical and radiation treatment <strong>for</strong> pituitary orhypothalamic disease. In central hypothyroidism, serum TSHmay be mildly elevated, but assessment of serum free T 4 isusually low, differentiat<strong>in</strong>g it from subcl<strong>in</strong>ical primary hypothyroidism.Consumptive hypothyroidism is a rare condition that mayoccur <strong>in</strong> patients with hemangiomata and other tumors <strong>in</strong>which type 3 iodothyron<strong>in</strong>e deiod<strong>in</strong>ase is expressed, result<strong>in</strong>g<strong>in</strong> accelerated degradation of T 4 and triiodothyron<strong>in</strong>e (T 3 )(48,49).
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1207Disorders associated with hypothyroidismThe most common <strong>for</strong>m of thyroid failure has an autoimmuneetiology. Not surpris<strong>in</strong>gly, there is also an <strong>in</strong>creasedfrequency of other autoimmune disorders <strong>in</strong> this populationsuch as type 1 diabetes, pernicious anemia, primary adrenalfailure (Addison’s disease), myasthenia gravis, celiac disease,rheumatoid arthritis, systemic lupus erythematosis (17–25),and rarely thyroid lymphoma (50).Dist<strong>in</strong>ct genetic syndromes with multiple autoimmuneendocr<strong>in</strong>opathies have been described, with some overlapp<strong>in</strong>gcl<strong>in</strong>ical features. The presence of two of the threemajor characteristics is required to diagnose the syndrome ofmultiple autoimmune endocr<strong>in</strong>opathies (MAEs). The def<strong>in</strong><strong>in</strong>gmajor characteristics <strong>for</strong> type 1 MAE and type 2 MAE areas follows: Type 1 MAE: Hypoparathyroidism, Addison’s disease,and mucocutaneous candidiasis caused by mutations <strong>in</strong>the autoimmune regulator gene (AIRE), result<strong>in</strong>g <strong>in</strong>defective AIRE prote<strong>in</strong> (51). Autoimmune thyroiditis ispresent <strong>in</strong> about 10%–15% (52). Type 2 MAE: Addison’s disease, autoimmune thyroiditis,and type 1 diabetes known as Schmidt’s syndrome(53).When adrenal <strong>in</strong>sufficiency is present, the diagnosis ofsubcl<strong>in</strong>ical hypothyroidism should be deferred until afterglucocorticoid therapy has been <strong>in</strong>stituted because TSHlevels may be elevated <strong>in</strong> the presence of untreated adrenal<strong>in</strong>sufficiency and may normalize with glucocorticoid therapy(54,55) (see L-thyrox<strong>in</strong>e treatment of hypothyroidism).Signs and symptoms of hypothyroidismThe well-known signs and symptoms of hypothyroidismtend to be more subtle than those of hyperthyroidism. Dry sk<strong>in</strong>,cold sensitivity, fatigue, muscle cramps, voice changes, andconstipation are among the most common. Less commonlyappreciated and typically associated with severe hypothyroidismare carpal tunnel syndrome, sleep apnea, pituitaryhyperplasia that can occur with or without hyperprolact<strong>in</strong>emiaand galactorrhea, and hyponatremia that can occur with<strong>in</strong>several weeks of the onset of profound hypothyroidism. Although,<strong>for</strong> example, <strong>in</strong> the case of some symptoms such asvoice changes subjective (12,56) and objective (57) measuresdiffer. Several rat<strong>in</strong>g scales (56,58,59) have been used to assessthe presence and, <strong>in</strong> some cases, the severity of hypothyroidism,but have low sensitivity and specificity. While the exerciseof calculat<strong>in</strong>g cl<strong>in</strong>ical scores has been largely superseded bysensitive thyroid function tests, it is useful to have objectivecl<strong>in</strong>ical measures to gauge the severity of hypothyroidism.Early as well as recent studies strongly correlate the degree ofhypothyroidism with ankle reflex relaxation time, a measurerarely used <strong>in</strong> current cl<strong>in</strong>ical practice today (60).Normalization of a variety of cl<strong>in</strong>ical and metabolic endpo<strong>in</strong>ts <strong>in</strong>clud<strong>in</strong>g rest<strong>in</strong>g heart rate, serum cholesterol, anxietylevel, sleep pattern, and menstrual cycle abnormalities <strong>in</strong>clud<strong>in</strong>gmenometrorrhagia are further confirmatory f<strong>in</strong>d<strong>in</strong>gsthat patients have been restored to a euthyroid state (61–65).Normalization of elevated serum creat<strong>in</strong>e k<strong>in</strong>ase or othermuscle (66) or hepatic enzymes follow<strong>in</strong>g treatment ofhypothyroidism (67) are additional, less well-appreciated andalso nonspecific therapeutic endpo<strong>in</strong>ts.Measurement of T 4 and T 3T 4 is bound to specific b<strong>in</strong>d<strong>in</strong>g prote<strong>in</strong>s <strong>in</strong> serum. Theseare T 4 -b<strong>in</strong>d<strong>in</strong>g globul<strong>in</strong> (TBG) and, to a lesser extent,transthyret<strong>in</strong> or T 4 -b<strong>in</strong>d<strong>in</strong>g prealbum<strong>in</strong> and album<strong>in</strong>. S<strong>in</strong>ceapproximately 99.97% of T 4 is prote<strong>in</strong>-bound, levels ofserum total T 4 will be affected by factors that alter b<strong>in</strong>d<strong>in</strong>g<strong>in</strong>dependent of thyroid disease (Table 5) (68,69). Accord<strong>in</strong>gly,methods <strong>for</strong> assess<strong>in</strong>g (<strong>in</strong>clud<strong>in</strong>g estimat<strong>in</strong>g andmeasur<strong>in</strong>g) serum free T 4 , which is the metabolicallyavailable moiety (70), have been developed, and assessmentof serum free T 4 has now largely replaced measurement ofserum total T 4 as a measure of thyroid status. Thesemethods <strong>in</strong>clude the serum free T 4 <strong>in</strong>dex, which is derivedas the product of total T 4 and a thyroid hormone b<strong>in</strong>d<strong>in</strong>gratio, and the direct immunoassay of free T 4 after ultrafiltrationor equilibrium dialysis of serum or after addition ofanti-T 4 antibody to serum (71).A subnormal assessment of serum free T 4 serves to establisha diagnosis of hypothyroidism, whether primary, <strong>in</strong>which serum TSH is elevated, or central, <strong>in</strong> which serum TSHis normal or low (46,47). An assessment of serum free T 4(Table 6) is the primary test <strong>for</strong> detect<strong>in</strong>g hypothyroidism <strong>in</strong>antithyroid drug–treated or surgical or radioiod<strong>in</strong>e-ablatedpatients with previous hyperthyroidism <strong>in</strong> whom serum TSHmay rema<strong>in</strong> low <strong>for</strong> many weeks to months.In monitor<strong>in</strong>g patients with hypothyroidism on L-thyrox<strong>in</strong>ereplacement, blood <strong>for</strong> assessment of serum free T 4 should becollected be<strong>for</strong>e dos<strong>in</strong>g because the level will be transiently<strong>in</strong>creased by up to 20% after L-thyrox<strong>in</strong>e adm<strong>in</strong>istration (72).In one small study of athyreotic patients, serum total T 4 levels<strong>in</strong>creased above basel<strong>in</strong>e by 1 hour and peaked at 2.5 hours,while serum free T 4 levels peaked at 3.5 hours and rema<strong>in</strong>edhigher than basel<strong>in</strong>e <strong>for</strong> 9 hours (72).In pregnancy, measurement of serum total T 4 is recommendedover direct immunoassay of serum free T 4 . Becauseof alterations <strong>in</strong> serum prote<strong>in</strong>s <strong>in</strong> pregnancy, directimmunoassay of free T 4 may yield lower values based onreference ranges established with normal nonpregnant sera.Moreover, many patients will have values below the nonpregnantreference range <strong>in</strong> the third trimester, <strong>in</strong>clud<strong>in</strong>gTable 5. Factors That Alter Thyrox<strong>in</strong>eand Triiodothyron<strong>in</strong>e B<strong>in</strong>d<strong>in</strong>g <strong>in</strong> SerumIncreased TBG Decreased TBG B<strong>in</strong>d<strong>in</strong>g <strong>in</strong>hibitorsInherited Inherited SalicylatesPregnancy Androgens FurosemideNeonatal state Anabolic steroids Free fatty acidsEstrogens Glucocorticoids Phenyto<strong>in</strong>Hepatitis Severe illness Carbamazep<strong>in</strong>ePorphyria Hepatic failure NSAIDs (variable,Hero<strong>in</strong>Nephrosistransient)Methadone Nicot<strong>in</strong>ic acid Hepar<strong>in</strong>Mitotane L-Asparag<strong>in</strong>ase5-FluorouracilSERMS (e.g.,tamoxifen,raloxifene)Perphanaz<strong>in</strong>eTBG, T 4 -b<strong>in</strong>d<strong>in</strong>g globul<strong>in</strong>; SERMS, selective estrogen receptormodulators; NSAIDs, nonsteroidal anti-<strong>in</strong>flammatory drugs.
1208 GARBER ET AL.Table 6. Assessment of Free Thyrox<strong>in</strong>eTest Method CommentsFree T 4 <strong>in</strong>dex or freeT 4 estimateDirect immunoassayof free T 4Product of total T 4 and thyroid hormoneb<strong>in</strong>d<strong>in</strong>g ratio or T 3 -res<strong>in</strong> uptakeWith physical separation us<strong>in</strong>g equilibriumdialysis or ultrafiltrationDirect immunoassayof free T 4Without physical separation us<strong>in</strong>g anti-T 4antibodyNormal values <strong>in</strong> pregnancy and with alterations<strong>in</strong> TBG b<strong>in</strong>d<strong>in</strong>g;Reduced values <strong>in</strong> pregnancy compared tononpregnant reference ranges; normal values withalterations <strong>in</strong> TBG b<strong>in</strong>d<strong>in</strong>gReduced values <strong>in</strong> pregnancy compared tononpregnant reference ranges; normal values withalterations <strong>in</strong> TBG b<strong>in</strong>d<strong>in</strong>gvalues obta<strong>in</strong>ed with equilibrium dialysis (73). F<strong>in</strong>ally,method-specific and trimester-specific reference ranges <strong>for</strong>direct immunoassay of free T 4 have not been generally established.By contrast, total T 4 <strong>in</strong>creases dur<strong>in</strong>g the first trimesterand the reference range is *1.5-fold that of thenonpregnant range throughout pregnancy (73,74).As is the case with T 4 ,T 3 is also bound to serum prote<strong>in</strong>s,pr<strong>in</strong>cipally TBG, but to a lesser extent than T 4 , *99.7%.Methods <strong>for</strong> assess<strong>in</strong>g free T 3 concentration by direct immunoassayhave been developed and are <strong>in</strong> current use (71).However, serum T 3 measurement, whether total or free, haslimited utility <strong>in</strong> hypothyroidism because levels are oftennormal due to hyperstimulation of the rema<strong>in</strong><strong>in</strong>g function<strong>in</strong>gthyroid tissue by elevated TSH and to up-regulation of type 2iodothyron<strong>in</strong>e deiod<strong>in</strong>ase (75). Moreover, levels of T 3 are low<strong>in</strong> the absence of thyroid disease <strong>in</strong> patients with severe illnessbecause of reduced peripheral conversion of T 4 to T 3 and <strong>in</strong>creased<strong>in</strong>activation of thyroid hormone (76,77).Pitfalls encountered when <strong>in</strong>terpret<strong>in</strong>gserum TSH levelsMeasurement of serum TSH is the primary screen<strong>in</strong>g test<strong>for</strong> thyroid dysfunction, <strong>for</strong> evaluation of thyroid hormonereplacement <strong>in</strong> patients with primary hypothyroidism, and<strong>for</strong> assessment of suppressive therapy <strong>in</strong> patients with follicularcell–derived thyroid cancer. TSH levels vary diurnally byup to approximately 50% of mean values (78), with more recentreports <strong>in</strong>dicat<strong>in</strong>g up to 40% variation on specimensper<strong>for</strong>med serially dur<strong>in</strong>g the same time of day (79). Valuestend to be lowest <strong>in</strong> the late afternoon and highest around thehour of sleep. In light of this, variations of serum TSH valueswith<strong>in</strong> the normal range of up to 40%–50% do not necessarilyreflect a change <strong>in</strong> thyroid status.TSH secretion is exquisitely sensitive to both m<strong>in</strong>or <strong>in</strong>creasesand decreases <strong>in</strong> serum free T 4 , and abnormal TSHlevels occur dur<strong>in</strong>g develop<strong>in</strong>g hypothyroidism and hyperthyroidismbe<strong>for</strong>e free T 4 abnormalities are detectable (80).Accord<strong>in</strong>g to NHANES III (11), a disease-free population,which excludes those who self-reported thyroid disease orgoiter or who were tak<strong>in</strong>g thyroid medications, the uppernormal of serum TSH levels is 4.5 mIU/L. A ‘‘reference population’’taken from the disease-free population composed ofthose who were not pregnant, did not have laboratory evidenceof hyperthyroidism or hypothyroidism, did not havedetectable TgAb or TPOAb, and were not tak<strong>in</strong>g estrogens,androgens, or lithium had an upper normal TSH value of4.12 mIU/L. This was further supported by the Han<strong>for</strong>dThyroid Disease Study, which analyzed a cohort withoutevidence of thyroid disease, were seronegative <strong>for</strong> thyroidautoantibodies, were not on thyroid medications, and hadnormal thyroid ultrasound exam<strong>in</strong>ations (which did not disclosenodularity or evidence of thyroiditis) (81). This uppernormal value, however, may not apply to iod<strong>in</strong>e <strong>in</strong>sufficientregions even after becom<strong>in</strong>g iod<strong>in</strong>e sufficient <strong>for</strong> 20 years(82,83).More recently (84) the NHANES III reference populationwas further analyzed and normal ranges based on age, U.S.Office of Management of Budget ‘‘Race and Ethnicity’’ categories,and sex were determ<strong>in</strong>ed. These <strong>in</strong>dicated the 97.5thpercentile TSH values as low as 3.24 <strong>for</strong> African Americansbetween the ages of 30 and 39 years and as high as 7.84 <strong>for</strong>Mexican Americans ‡ 80 years of age. For every 10-year age<strong>in</strong>crease after 30–39 years, the 97.5th percentile of serum TSH<strong>in</strong>creases by 0.3 mIU/L. Body weight, anti-thyroid antibodystatus, and ur<strong>in</strong>ary iod<strong>in</strong>e had no significant impact on theseranges.The National Academy of <strong>Cl<strong>in</strong>ical</strong> Biochemists, however,<strong>in</strong>dicated that 95% of <strong>in</strong>dividuals without evidence of thyroiddisease have TSH concentrations below 2.5 mIU/L (85), and ithas been suggested that the upper limit of the TSH referencerange be lowered to 2.5 mIU/L (86). While many patients withTSH concentrations <strong>in</strong> this range do not develop hypothyroidism,those patients with AITD are much more likely todevelop hypothyroidism, either subcl<strong>in</strong>ical or overt (87) (seeTherapeutic endpo<strong>in</strong>ts <strong>in</strong> the treatment of hypothyroidism <strong>for</strong>further discussion).In <strong>in</strong>dividuals without serologic evidence of AITD, TSHvalues above 3.0 mIU/L occur with <strong>in</strong>creas<strong>in</strong>g frequency withage, with elderly ( > 80 years of age) <strong>in</strong>dividuals hav<strong>in</strong>g a23.9% prevalence of TSH values between 2.5 and 4.5 mIU/L,and a 12% prevalence of TSH concentrations above 4.5 mIU/L(88). Thus, very mild TSH elevations <strong>in</strong> older <strong>in</strong>dividuals maynot reflect subcl<strong>in</strong>ical thyroid dysfunction, but rather be anormal manifestation of ag<strong>in</strong>g. The caveat is that while thenormal TSH reference range—particularly <strong>for</strong> some subpopulations—mayneed to be narrowed (85,86), the normal referencerange may widen with <strong>in</strong>creas<strong>in</strong>g age (84). Thus, not allpatients who have mild TSH elevations are hypothyroid andthere<strong>for</strong>e would not require thyroid hormone therapy.There are other pitfalls <strong>in</strong> the <strong>in</strong>terpretation of the serumTSH because abnormal levels are observed <strong>in</strong> various nonthyroidalstates. Serum TSH may be suppressed <strong>in</strong> hospitalizedpatients with acute illness, and levels below 0.1 mIU/L <strong>in</strong>comb<strong>in</strong>ation with subnormal free T 4 estimates may be seen <strong>in</strong>critically ill patients, especially <strong>in</strong> those receiv<strong>in</strong>g dopam<strong>in</strong>e<strong>in</strong>fusions (89) or pharmacologic doses of glucocorticoids (90).In addition, TSH levels may <strong>in</strong>crease to levels above normal,
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1209but generally below 20 mIU/L dur<strong>in</strong>g the recovery phasefrom nonthyroidal illness (91). Thus, there are limitations toTSH measurements <strong>in</strong> hospitalized patients and, there<strong>for</strong>e,they should be only per<strong>for</strong>med if there is an <strong>in</strong>dex of suspicion<strong>for</strong> thyroid dysfunction (76).Serum TSH typically falls, but <strong>in</strong>frequently to below0.1 mU/L, dur<strong>in</strong>g the first trimester of pregnancy due to thethyroid stimulatory effects of human chorionic gonadotrop<strong>in</strong>and returns to normal <strong>in</strong> the second trimester (10) (seeTable 7).TSH secretion may be <strong>in</strong>hibited by adm<strong>in</strong>istration of subcutaneousoctreotide, which does not cause persistent centralhypothyroidism (92), and by oral bexarotene, which almostalways does (93). In addition, patients with anorexia nervosamay have low TSH levels <strong>in</strong> comb<strong>in</strong>ation with low levels offree T 4 (94), mimick<strong>in</strong>g what may be seen <strong>in</strong> critically ill patientsand <strong>in</strong> patients with central hypothyroidism due topituitary and hypothalamic disorders.Patients with nonfunction<strong>in</strong>g pituitary adenomas, withcentral hypothyroidism, may have mildly elevated serumTSH levels, generally not above 6 or 7 mIU/L, due to secretionof bio<strong>in</strong>active iso<strong>for</strong>ms of TSH (47). TSH levels mayalso be elevated <strong>in</strong> association with elevated serum thyroidhormone levels <strong>in</strong> patients with resistance to thyroid hormone(95). Heterophilic or <strong>in</strong>terfer<strong>in</strong>g antibodies, <strong>in</strong>clud<strong>in</strong>ghuman antianimal (most commonly mouse) antibodies,rheumatoid factor, and autoimmune anti-TSH antibodiesmay cause falsely elevated serum TSH values (96). Lastly,adrenal <strong>in</strong>sufficiency, as previously noted <strong>in</strong> Disorders associatedwith hypothyroidism, may be associated with TSH elevationsthat are reversed with glucocorticoid replacement(54,55).Other diagnostic tests <strong>for</strong> hypothyroidismPrior to the advent of rout<strong>in</strong>e validated chemical measurementsof serum thyroid hormones and TSH, tests thatcorrelated with thyroid status, but not sufficiently specific todiagnose hypothyroidism, were used to diagnose hypothyroidismand to gauge the response to thyroid hormone therapy.The follow<strong>in</strong>g are previous notable and more recentexamples: Basal metabolic rate was the ‘‘gold standard’’ <strong>for</strong> diagnosis.Extremely high and low values correlate well withmarked hyperthyroidism and hypothyroidism, respectively,but are affected by many unrelated, diverseconditions, such as fever, pregnancy, cancer, acromegaly,hypogonadism, and starvation (97,98). Decrease <strong>in</strong> sleep<strong>in</strong>g heart rate (61) Elevated total cholesterol (62,99) as well as low-densitylipoprote<strong>in</strong> (LDL) (99,100) and the highly atherogenicsubfraction Lp (a) (101) Delayed Achilles reflex time (60) Increased creat<strong>in</strong>e k<strong>in</strong>ase due to an <strong>in</strong>crease <strong>in</strong> the MMfraction, which can be marked and lead to an <strong>in</strong>crease <strong>in</strong>the MB fraction. There is a less marked <strong>in</strong>crease <strong>in</strong>myoglob<strong>in</strong> (66) and no change <strong>in</strong> tropon<strong>in</strong> levels even <strong>in</strong>the presence of an <strong>in</strong>creased MB fraction (102).Screen<strong>in</strong>g and aggressive case f<strong>in</strong>d<strong>in</strong>g<strong>for</strong> hypothyroidismCriteria <strong>for</strong> population screen<strong>in</strong>g <strong>in</strong>clude: A condition that is prevalent and an important healthproblem Early diagnosis is not usually made Diagnosis is simple and accurate Treatment is cost effective and safeDespite this seem<strong>in</strong>gly straight<strong>for</strong>ward guidance, expertpanels have disagreed about TSH screen<strong>in</strong>g of the generalpopulation (Table 8). The ATA recommends screen<strong>in</strong>g <strong>in</strong> alladults beg<strong>in</strong>n<strong>in</strong>g at age 35 years and every 5 years thereafterTable 7. Thyrotrop<strong>in</strong> Upper NormalGroup, study, society TSH upper normal CommentsNACB 2.5 When there is no evidence of thyroid diseaseNHANES III, disease free 4.5 No self-reported thyroid diseaseNot on thyroid medicationsNHANES III, reference population 4.12 No self-reported thyroid diseaseNot on thyroid medicationsNegative anti-thyroid antibodiesNot pregnantNot on estrogens, androgens, lithiumHan<strong>for</strong>d Thyroid Disease Study 4.10 No evidence of thyroid diseaseNegative anti-thyroid antibodiesNot on thyroid medicationsNormal ultrasound (no nodules or thyroiditis)Pregnancy, first trimester 2.0–2.5 See sections L-thyrox<strong>in</strong>e treatment of hypothyroidismand <strong>Hypothyroidism</strong> dur<strong>in</strong>g pregnancyPregnancy, second trimester 3.0 See sections L-thyrox<strong>in</strong>e treatment of hypothyroidismand <strong>Hypothyroidism</strong> dur<strong>in</strong>g pregnancyPregnancy, third trimester 3.5 See sections L-thyrox<strong>in</strong>e treatment of hypothyroidismand <strong>Hypothyroidism</strong> dur<strong>in</strong>g pregnancySources: Stagnaro-Green et al., 2011 (10); Hollowell et al., 2002 (11); Hamilton et al., 2008 (81); Baloch et al., 2003 (85).NACB, National Academy of <strong>Cl<strong>in</strong>ical</strong> Biochemists; NHANES, National Health and Nutrition Exam<strong>in</strong>ation Survey.
1210 GARBER ET AL.Table 8. Recommendations of Six OrganizationsRegard<strong>in</strong>g Screen<strong>in</strong>g of Asymptomatic <strong>Adults</strong><strong>for</strong> Thyroid DysfunctionOrganizationAmerican ThyroidAssociationAmerican Associationof <strong>Cl<strong>in</strong>ical</strong>Endocr<strong>in</strong>ologistsAmerican Academyof Family PhysiciansAmerican College ofPhysiciansU.S. Preventive ServicesTask ForceRoyal Collegeof Physiciansof LondonScreen<strong>in</strong>g recommendationsWomen and men > 35 yearsof age should be screenedevery 5 years.Older patients,especially women,should be screened.Patients ‡ 60 years of ageshould be screened.Women ‡ 50 years of agewith an <strong>in</strong>cidental f<strong>in</strong>d<strong>in</strong>gsuggestive of symptomaticthyroid disease should beevaluated.Insufficient evidence <strong>for</strong>or aga<strong>in</strong>st screen<strong>in</strong>gScreen<strong>in</strong>g of the healthyadult population unjustifiedSources: Bask<strong>in</strong> et al., 2002 (2); Ladenson et al., 2000 (103); AmericanAcademy of Family Physicians, 2002 (104); Helfand and Redfern,1998 (105); Vanderpump et al., 1996 (107); Helfand, 2004 (108).(103). AACE recommends rout<strong>in</strong>e TSH measurement <strong>in</strong> olderpatients—age not specified—especially women (2). TheAmerican Academy of Family Physicians recommends rout<strong>in</strong>escreen<strong>in</strong>g <strong>in</strong> asymptomatic patients older than age 60years (104), and the American College of Physicians recommendscase f<strong>in</strong>d<strong>in</strong>g <strong>in</strong> women older than 50 years (105). Incontrast, a consensus panel (106), the Royal College of Physiciansof London (107), and the U.S. Preventive Services TaskForce (108) do not recommend rout<strong>in</strong>e screen<strong>in</strong>g <strong>for</strong> thyroiddisease <strong>in</strong> adults. For recommendations <strong>in</strong> pregnancy, seeRecommendations 20.1.1 and 20.1.2.While there is no consensus about population screen<strong>in</strong>g <strong>for</strong>hypothyroidism there is compell<strong>in</strong>g evidence to support casef<strong>in</strong>d<strong>in</strong>g <strong>for</strong> hypothyroidism <strong>in</strong>: Those with autoimmune disease, such as type 1 diabetes(20,21) Those with pernicious anemia (109,110) Those with a first-degree relative with autoimmunethyroid disease (19) Those with a history of neck radiation to the thyroidgland <strong>in</strong>clud<strong>in</strong>g radioactive iod<strong>in</strong>e therapy <strong>for</strong> hyperthyroidismand external beam radiotherapy <strong>for</strong> headand neck malignancies (111–113) Those with a prior history of thyroid surgery or dysfunction Those with an abnormal thyroid exam<strong>in</strong>ation Those with psychiatric disorders (114) Patients tak<strong>in</strong>g amiodarone (37) or lithium (32–34) Patients with ICD-9 diagnoses as presented <strong>in</strong> Table 9When to treat hypothyroidismAlthough there is general agreement that patients withprimary hypothyroidism with TSH levels above 10 mIU/LTable 9. ICD-9-CM Codes to SupportThyrotrop<strong>in</strong> Test<strong>in</strong>gAdrenal <strong>in</strong>sufficiency 255.41Alopecia 704.00Anemia, unspecified deficiency 281.9Cardiac dysrhythmia, unspecified 427.9Changes <strong>in</strong> sk<strong>in</strong> texture 782.8Congestive heart failure 428.0Constipation 564.00Dementia294.8BADiabetes mellitus, type 1 250.01Dysmenorrhea 625.3Hypercholesterolemia 272.0Hypertension 401.9Mixed hyperlipidemia 272.2Malaise and fatigue 780.79Myopathy, unspecified 359.9Prolonged QT <strong>in</strong>terval 794.31Vitiligo 709.01Weight ga<strong>in</strong> 783.9MICD-9-CM, International Classification of Diseases, N<strong>in</strong>th Revision,<strong>Cl<strong>in</strong>ical</strong> Modification (www.cdc.gov/nchs/icd/icd9cm.htm).should be treated (106,115–117), which patients with TSHlevels of 4.5–10 mIU/L will benefit is less certa<strong>in</strong> (118,119). Asubstantial number of studies have been done on patientswith TSH levels between 2.5 and 4.5, <strong>in</strong>dicat<strong>in</strong>g beneficialresponse <strong>in</strong> atherosclerosis risk factors such as atherogeniclipids (120–123), impaired endothelial function (124,125), and<strong>in</strong>tima media thickness (126). This topic is further discussed <strong>in</strong>the section Cardiac benefit from treat<strong>in</strong>g subcl<strong>in</strong>ical hypothyroidism.However, there are virtually no cl<strong>in</strong>ical outcome data tosupport treat<strong>in</strong>g patients with subcl<strong>in</strong>ical hypothyroidismwith TSH levels between 2.5 and 4.5 mIU/L. The possibleexception to this statement is pregnancy because the rate ofpregnancy loss, <strong>in</strong>clud<strong>in</strong>g spontaneous miscarriage be<strong>for</strong>e 20weeks gestation and stillbirth after 20 weeks, have been reportedto be <strong>in</strong>creased <strong>in</strong> anti-thyroid antibody–negativewomen with TSH values between 2.5 and 5.0 (127).L-thyrox<strong>in</strong>e treatment of hypothyroidismS<strong>in</strong>ce the generation of biologically active T 3 by the peripheralconversion of T 4 to T 3 was documented <strong>in</strong> 1970 (128),L-thyrox<strong>in</strong>e monotherapy has become the ma<strong>in</strong>stay of treat<strong>in</strong>ghypothyroidism, replac<strong>in</strong>g desiccated thyroid and other<strong>for</strong>ms of L-thyrox<strong>in</strong>e and L-triiodothyron<strong>in</strong>e comb<strong>in</strong>ationtherapy. Although a similar quality of life (129) and circulat<strong>in</strong>gT 3 levels (130) have been reported <strong>in</strong> patients treated withL-thyrox<strong>in</strong>e compared with <strong>in</strong>dividuals without thyroid disease,other studies have not shown levels of satisfactioncomparable to euthyroid controls (131). A number of studies,follow<strong>in</strong>g a 1999 report cit<strong>in</strong>g the benefit of L-thyrox<strong>in</strong>e and L-triiodothyron<strong>in</strong>e comb<strong>in</strong>ation therapy (132), have re-addressedthe benefits of synthetic L-thyrox<strong>in</strong>e and L-triiodothyron<strong>in</strong>ecomb<strong>in</strong>ation therapy but have largely failed toconfirm an advantage of this approach to improve cognitiveor mood outcomes <strong>in</strong> hypothyroid <strong>in</strong>dividuals treated with L-thyrox<strong>in</strong>e alone (133,134).Yet several matters rema<strong>in</strong> uncerta<strong>in</strong>. What should the ratiosof L-thyrox<strong>in</strong>e and L-triiodothyron<strong>in</strong>e replacement be (133)?What is the pharmacodynamic equivalence of L-thyrox<strong>in</strong>e and
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1211L-triiodothyron<strong>in</strong>e (135)? It was previously believed to be 1:4,but a recent small study <strong>in</strong>dicated that it was approximately 1:3(135). Why do some patients prefer comb<strong>in</strong>ation therapy to L-thyrox<strong>in</strong>e monotherapy (133)? Some <strong>in</strong>sight <strong>in</strong>to the latterquestion may be ga<strong>in</strong>ed from a large-scale study of L-thyrox<strong>in</strong>eand L-triiodothyron<strong>in</strong>e comb<strong>in</strong>ation therapy <strong>in</strong> which differentresponses were observed <strong>in</strong> patients with different genetic subtypesof type 2 deiod<strong>in</strong>ase (136), despite a prior, smaller negativestudy (137). It is not known if those who responded positively toL-thyrox<strong>in</strong>e and L-triiodothyron<strong>in</strong>e comb<strong>in</strong>ation therapy willhave long-term benefit and whether genotyp<strong>in</strong>g patients withhypothyroidism who are cl<strong>in</strong>ically and biochemically euthyroidwill ultimately reliably identify patients with hypothyroidismwho are most likely to benefit from comb<strong>in</strong>ation therapy.Treatment of hypothyroidism is best accomplished us<strong>in</strong>gsynthetic L-thyrox<strong>in</strong>e sodium preparations. Because of theuniqueness of the various tablet <strong>for</strong>mulations and a recently<strong>in</strong>troduced preparation of liquid-conta<strong>in</strong><strong>in</strong>g capsules with the<strong>in</strong>active <strong>in</strong>gredients gelat<strong>in</strong>, glycer<strong>in</strong>, and water, and becauseof uncerta<strong>in</strong>ty about the sensitivity of current bioequivalenceassessment procedures to assure true <strong>in</strong>terchangability amongthe tablets, current recommendations encourage the use of aconsistent L-thyrox<strong>in</strong>e preparation <strong>for</strong> <strong>in</strong>dividual patients tom<strong>in</strong>imize variability from refill to refill (138,139).Some reports have <strong>in</strong>dicated an apparent <strong>in</strong>creased dosagerequirement <strong>for</strong> L-thyrox<strong>in</strong>e <strong>in</strong> some patients with dim<strong>in</strong>ishedgastric acid secretion (140,141). This has led to <strong>in</strong> vitrowork show<strong>in</strong>g significant differences <strong>in</strong> dissolution among L-thyrox<strong>in</strong>e preparations (142), profiles of which appear to bedependent on the pH of the solution <strong>in</strong> which the preparationswere dissolved. The liquicap preparation (Tiros<strong>in</strong>t Ò ) (143) dissolutionprofile was the least affected by changes <strong>in</strong> pH (142).The cl<strong>in</strong>ical significance of these f<strong>in</strong>d<strong>in</strong>gs rema<strong>in</strong>s unclear. Inmore recent, though short-term studies, the use of histam<strong>in</strong>e H2receptor blockers and proton pump <strong>in</strong>hibitors does not appearto <strong>in</strong>fluence cl<strong>in</strong>ical measures <strong>in</strong> L-thyrox<strong>in</strong>e tablet–treated patients(144).Desiccated thyroid has not been systematically studied (seeDietary supplements and nutraceuticals <strong>in</strong> the treatment of hypothyroidism).Absorption studies <strong>in</strong>dicate that the bioavailabilityof T 3 <strong>in</strong> desiccated thyroid is comparable to that of orally adm<strong>in</strong>isteredsynthetic L-triiodothyron<strong>in</strong>e (145). There<strong>for</strong>e, themost commonly used <strong>for</strong>m of desiccated thyroid, known asArmour Ò Thyroid, which is of porc<strong>in</strong>e orig<strong>in</strong>, may be viewedas a L-thyrox<strong>in</strong>e and L-triiodothyron<strong>in</strong>e comb<strong>in</strong>ation with aratio of approximately 4:1 by weight (145). The content ofthyroid hormone and the ratio of T 4 to T 3 may vary <strong>in</strong> desiccatedthyroid preparations depend<strong>in</strong>g on the brand employedand whether it is of porc<strong>in</strong>e or bov<strong>in</strong>e orig<strong>in</strong>.The daily dosage of L-thyrox<strong>in</strong>e is dependent on age, sex,and body size (146–151). Ideal body weight is best used <strong>for</strong>cl<strong>in</strong>ical dose calculations because lean body mass is the bestpredictor of daily requirements (152,153). A recent study,however, which did not subclassify patients on the basis oftheir <strong>in</strong>itial degree of hypothyroidism, found that while the L-thyrox<strong>in</strong>e dose per ideal body weight or degree of overweightdiffered by sex—with females hav<strong>in</strong>g a higher dose requirementthan men—it did not confirm that age was an <strong>in</strong>dependentpredictor of dosage (154).With little residual thyroid function, replacement therapyrequires approximately 1.6 lg/kg of L-thyrox<strong>in</strong>e daily(155,156). Patients who are athyreotic (after total thyroidectomyand/or radioiod<strong>in</strong>e therapy) (157) and those withcentral hypothyroidism may require higher doses (158),while patients with subcl<strong>in</strong>ical hypothyroidism (159–162)or after treatment <strong>for</strong> Graves’ disease (163) may require less.Young healthy adults may be started on full replacementdosage, which is also preferred after planned (<strong>in</strong> preparation<strong>for</strong> thyroid cancer imag<strong>in</strong>g and therapy) or short-term<strong>in</strong>advertent lapses <strong>in</strong> therapy. Start<strong>in</strong>g with full replacementversus low dosages leads to more rapid normalizationof serum TSH but similar time to symptom resolution (164).However, patients with subcl<strong>in</strong>ical hypothyroidism do notrequire full replacement doses (159). Doses of 25–75 lgdaily are usually sufficient <strong>for</strong> achiev<strong>in</strong>g euthyroid levels(160), with larger doses usually required <strong>for</strong> those present<strong>in</strong>gwith higher TSH values (161). One randomizedcontrol trial assigned L-thyrox<strong>in</strong>e doses on the basis of the<strong>in</strong>itial serum TSH values as follows: 25 lg <strong>for</strong> TSH 4.0–8.0 mIU/L, 50 lg <strong>for</strong> TSH 8–12 mIU/L, and 75 lg <strong>for</strong>TSH > 12 mIU/L. After 2 months only m<strong>in</strong>imal further adjustmentswere required to achieve euthyroidism (162).One recent study demonstrated that L-thyrox<strong>in</strong>e absorptionwith<strong>in</strong> 30 m<strong>in</strong>utes of breakfast is not as effective as when it istaken 4 hours after the last meal (165). Another study showedthat tak<strong>in</strong>g it 60 m<strong>in</strong>utes be<strong>for</strong>e breakfast on an empty stomachwas better than tak<strong>in</strong>g it with<strong>in</strong> 2 hours of the last meal of theday, which <strong>in</strong> turn was better than tak<strong>in</strong>g it with<strong>in</strong> 20 m<strong>in</strong>utesof breakfast (166). However, these two studies do not establishwhich of the two methods, L-thyrox<strong>in</strong>e taken with water 60m<strong>in</strong>utes be<strong>for</strong>e breakfast or at bedtime 4 hours after the lastmeal on an empty stomach, is superior. Although L-thyrox<strong>in</strong>eis better absorbed when taken 60 m<strong>in</strong>utes be<strong>for</strong>e a mealcompared to 30 m<strong>in</strong>utes be<strong>for</strong>e a meal, compliance may beenhanced by <strong>in</strong>struct<strong>in</strong>g patients to consistently take it withwater between 30 and 60 m<strong>in</strong>utes prior to eat<strong>in</strong>g breakfast.L-thyrox<strong>in</strong>e should be stored per product <strong>in</strong>sert at 20°C–25°C, (range, 15°C–30°C) or 68°F–77°F (range, 59°F–86°F) andprotected from light and moisture. It should not be taken withsubstances or medications (see Table 10) that <strong>in</strong>terfere with itsabsorption or metabolism. Because approximately 70% of anorally adm<strong>in</strong>istered dose of L-thyrox<strong>in</strong>e is absorbed (167–169), <strong>in</strong>dividuals unable to <strong>in</strong>gest L-thyrox<strong>in</strong>e should <strong>in</strong>itiallyreceive 70% or less of their usual dose <strong>in</strong>travenously. CrushedL-thyrox<strong>in</strong>e suspended <strong>in</strong> water should be given to patientsreceiv<strong>in</strong>g enteral feed<strong>in</strong>g through nasogastric and other tubes.For optimal absorption feed<strong>in</strong>g should be <strong>in</strong>terrupted withdoses given as long as possible after feed<strong>in</strong>g and at least 1hour be<strong>for</strong>e resum<strong>in</strong>g feed<strong>in</strong>g. Adm<strong>in</strong>ister<strong>in</strong>g <strong>in</strong>travenous L-thyrox<strong>in</strong>e solution, which is not universally available, shouldbe considered when feed<strong>in</strong>g may not be <strong>in</strong>terrupted.Dose adjustments are guided by serum TSH determ<strong>in</strong>ations4–8 weeks (156,170) follow<strong>in</strong>g <strong>in</strong>itiation of therapy, dosageadjustments, or change <strong>in</strong> the L-thyrox<strong>in</strong>e preparation(139,171). While TSH levels may decl<strong>in</strong>e with<strong>in</strong> a month of<strong>in</strong>itiat<strong>in</strong>g therapy with doses of L-thyrox<strong>in</strong>e such as 50 or 75 lg,mak<strong>in</strong>g adjustments with smaller doses may require 8 weeksor longer be<strong>for</strong>e TSH levels beg<strong>in</strong> to plateau (170,172). Incrementchanges of 12.5–25 lg/d are <strong>in</strong>itially made, but evensmaller changes may be necessary to achieve goal TSH levels.In the case of central hypothyroidism, estimates of dosagebased on 1.6 lg/kg L-thyrox<strong>in</strong>e daily and assessment of free T 4 ,not TSH, should guide therapy. Determ<strong>in</strong>ations are bestdone prior to tak<strong>in</strong>g thyroid hormone. The goal of therapy is
1212 GARBER ET AL.10.1. Interference with absorptionTable 10. Agents and Conditions Hav<strong>in</strong>g an Impact on L-thyrox<strong>in</strong>e Therapyand Interpretation of Thyroid TestsBile acid sequestrants (cholestyram<strong>in</strong>e,colestipol, colesevelam)SucralfateCation exchange res<strong>in</strong>s (Kayexelate)Oral bisphosphonatesProton pump <strong>in</strong>hibitorsRaloxifene aMultivitam<strong>in</strong>s (conta<strong>in</strong><strong>in</strong>g ferroussulfate or calcium carbonate)Ferrous sulfatePhosphate b<strong>in</strong>ders (sevelamer,alum<strong>in</strong>um hydroxide)Calcium salts (carbonate, citrate, acetate)Chromium picol<strong>in</strong>ateCharcoalOrlistat bCiprofloxac<strong>in</strong>H2 receptor antagonists aMalabsorption syndromes Celiac disease Jejunoileal bypass surgery Cirrhosis (biliary) AchlorhydriaDiet Ingestion with a meal Grapefruit juice a Espresso coffee High fiber diet Soybean <strong>for</strong>mula (<strong>in</strong>fants) Soy10.2. Thyroid gland hormone production and secretionDirect and <strong>in</strong>direct effectson the thyroid gland Iod<strong>in</strong>e uptake+ Iod<strong>in</strong>e (<strong>in</strong>clud<strong>in</strong>g kelpsupplements)+ Amiodarone+ Ethionamide+ Iod<strong>in</strong>ated contrast(ipodate, c iopanoic acid c )+ Perchlorate c Hormone production+ Iod<strong>in</strong>e (<strong>in</strong>clud<strong>in</strong>g kelpsupplements)+ Amiodarone+ Thionamides (carbimazole,methimazole, propylthiouracil)+ Iod<strong>in</strong>ated contrast(ipodate, c iopanoic acid c )+ Sulfonylureas+ Sulfonamides+ Ethionamide Secretion+ Lithium+ Iod<strong>in</strong>e (<strong>in</strong>clud<strong>in</strong>g kelpsupplements)+ Amiodarone+ Iod<strong>in</strong>ated contrast(ipodate, c iopanoic acid c ) Thyroiditis+ Induces- Amiodarone- Tyros<strong>in</strong>e k<strong>in</strong>ase <strong>in</strong>hibitors(sunit<strong>in</strong>ib, sorafenib)- Interferon alpha- Interleuk<strong>in</strong>s- Antiangiogenic(lenalidomide, thalidomide)- Lithium- Alemtuzumab- Denileuk<strong>in</strong> diftitox<strong>in</strong>+ Ameliorates (if autoimmune)- Glucocorticoids Development of Graves’+ Interferon alpha+ HAART (highly activeantiretroviral therapy)+ Alemtuzumab Amelioration of Graves’+ Glucocorticoids10.3. Direct and <strong>in</strong>direct effects on the hypothalamic–pituitary–thyroid axisTSH secretion Decrease+ Bexarotene+ Dopam<strong>in</strong>e+ Dopam<strong>in</strong>ergic agonists(bromocript<strong>in</strong>e, cabergol<strong>in</strong>e)+ Glucorticoids+ Thyroid hormone analogues+ Somatostat<strong>in</strong> analogues(octreotide, lanreotide)+ Met<strong>for</strong>m<strong>in</strong>+ Opiates (e.g., hero<strong>in</strong>)+ Interleuk<strong>in</strong>-6 Increase+ Dopam<strong>in</strong>e receptorblockers (metoclopramide)+ Hypoadrenalism+ Interleuk<strong>in</strong> 2+ Amphetam<strong>in</strong>e+ Ritonavir b+ St. John’s Wort aHypophysitis Ipilimumab10.4. Increased clearance 10.5. Peripheral metabolismPhenobarbitalPrimidonePhenyto<strong>in</strong>Carbamazep<strong>in</strong>eOxacarbazep<strong>in</strong>e bRifamp<strong>in</strong>Growth hormoneSertral<strong>in</strong>e bTyros<strong>in</strong>e k<strong>in</strong>ase <strong>in</strong>hibitors(imat<strong>in</strong>ib, b sunit<strong>in</strong>ib)Quetiap<strong>in</strong>e bStavud<strong>in</strong>e bNevirap<strong>in</strong>e a,bGlucocorticoidsAmiodaronePropylthiouracilBeta blockers (e.g., propranolol,nadolol)Iod<strong>in</strong>ated contrast (ipodate, ciopanoic acid c )Interleuk<strong>in</strong>-6Clomipram<strong>in</strong>ea Impact uncerta<strong>in</strong>.b Mechanism uncerta<strong>in</strong>.c Not presently available <strong>in</strong> the United States.
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1213generally to atta<strong>in</strong> values above the mean <strong>for</strong> assays be<strong>in</strong>gemployed, <strong>in</strong> keep<strong>in</strong>g with observations that mean values <strong>for</strong>estimates of free T 4 <strong>in</strong> patients who are treated with L-thyrox<strong>in</strong>etend to be higher than mean values observed <strong>in</strong> untreatedcontrols (150,173–175).Some cl<strong>in</strong>ical manifestations of hypothyroidism, such aschronic sk<strong>in</strong> changes, may take up to 3–6 months to resolveafter serum TSH has returned to normal (176).Once an adequate replacement dosage has been determ<strong>in</strong>edmost, but not all of us, are of the op<strong>in</strong>ion that periodicfollow-up evaluations with repeat TSH test<strong>in</strong>g at 6-month andthen 12-month <strong>in</strong>tervals are appropriate (172). Some authorsth<strong>in</strong>k that more frequent test<strong>in</strong>g is advisable to ensure andmonitor compliance with therapy.Dosage adjustments may be necessary as underly<strong>in</strong>gfunction wanes. In pregnancy thyroid hormone requirementsare <strong>in</strong>creased, then revert back to basel<strong>in</strong>e after delivery(177). Dosage adjustments are also necessary,generally when medications <strong>in</strong>fluenc<strong>in</strong>g absorption, plasmab<strong>in</strong>d<strong>in</strong>g, or metabolism are added or discont<strong>in</strong>ued. Whensuch medications are <strong>in</strong>troduced or discont<strong>in</strong>ued thyroidhormone levels should <strong>in</strong>itially be checked with<strong>in</strong> 4–8 weeksof do<strong>in</strong>g so, and tests per<strong>for</strong>med at least every 4–8 weeksuntil stable euthyroid <strong>in</strong>dices have been documented whileonthesamedoseofL-thyrox<strong>in</strong>e.Decreases<strong>in</strong>L-thyrox<strong>in</strong>erequirements occur as patients age (151) and follow<strong>in</strong>g significantweight loss. Moreover, although elderly patientsabsorb L-thyrox<strong>in</strong>e less efficiently they often require 20–-25% less per kilogram daily than younger patients, due todecreased lean body mass (152,153). Regardless of the degreeof hypothyroidism, patients older than 50–60 years, withoutevidence of coronary heart disease (CHD) may be started ondoses of 50 lg daily. Among those with known CHD, theusual start<strong>in</strong>g dose is reduced to 12.5–25 lg/day. <strong>Cl<strong>in</strong>ical</strong>monitor<strong>in</strong>g <strong>for</strong> the onset of ang<strong>in</strong>al symptoms is essential(178). Ang<strong>in</strong>al symptoms may limit the atta<strong>in</strong>ment of euthyroidism.However, optimal medical management of arterioscleroticcardiovascular disease (ASCVD) shouldgenerally allow <strong>for</strong> sufficient treatment with L-thyrox<strong>in</strong>e toboth reduce the serum TSH and ma<strong>in</strong>ta<strong>in</strong> the patient ang<strong>in</strong>afree.Emergency coronary artery bypass graft<strong>in</strong>g <strong>in</strong> patientswith unstable ang<strong>in</strong>a or left ma<strong>in</strong> coronary artery occlusionmay be safely per<strong>for</strong>med while the patient is still moderatelyto severely hypothyroid (179,180) but elective cases shouldbe per<strong>for</strong>med after the patient has become euthyroid.The exacerbation of adrenal <strong>in</strong>sufficiency was first described<strong>in</strong> cases of central hypothyroidism over 70 years ago(181). Although it rarely occurs, those with adrenal <strong>in</strong>sufficiency,either primary or central, or at risk <strong>for</strong> it, should betreated with cl<strong>in</strong>ically appropriate doses of hydrocortisoneuntil adrenal <strong>in</strong>sufficiency is ruled out (182,183). In the absenceof central hypothyroidism, elevated TSH levels may beseen <strong>in</strong> conjunction with normal T 4 levels, mak<strong>in</strong>g it <strong>in</strong>itially<strong>in</strong>dist<strong>in</strong>guishable from subcl<strong>in</strong>ical hypothyroidism. However,when due to adrenal <strong>in</strong>sufficiency elevated TSH levelsfall with glucorticoid therapy alone (54,55).Patients on high doses of L-thyrox<strong>in</strong>e ( > 200 lg/d) withpersistently or frequently elevated TSH levels may be noncompliantor have problems with L-thyrox<strong>in</strong>e absorption(171). The <strong>for</strong>mer is much more common (184). Althoughdaily dos<strong>in</strong>g of L-thyrox<strong>in</strong>e is ideal, missed doses should bemade up when the omission is recognized, even on the sameor subsequent days. In those with significant complianceproblems, weekly dos<strong>in</strong>g with L-thyrox<strong>in</strong>e results <strong>in</strong> similarcl<strong>in</strong>ical safety, outcomes, and acceptable TSH values (185).Absorption is dim<strong>in</strong>ished by meals (165,166,168,186) andcompet<strong>in</strong>g medications (see Table 10).Steps should be taken to avoid overtreatment with L-thyrox<strong>in</strong>e. This has been reported <strong>in</strong> 20% of those treated withthyroid hormone (12). The pr<strong>in</strong>cipal adverse consequences ofsubtle or frank overtreatment are cardiovascular (187–190),skeletal (191–194), and possibly affective disturbances (195–197). The elderly are particularly susceptible to atrial fibrillation,while postmenopausal women, who constitute a substantialportion of those on thyroid hormone, are prone to acceleratedbone loss.Therapeutic endpo<strong>in</strong>ts <strong>in</strong> the treatmentof hypothyroidismThe most reliable therapeutic endpo<strong>in</strong>t <strong>for</strong> the treatment ofprimary hypothyroidism is the serum TSH value. Confirmatorytotal T 4 , free T 4 , and T 3 levels do not have sufficientspecificity to serve as therapeutic endpo<strong>in</strong>ts by themselves,nor do cl<strong>in</strong>ical criteria. Moreover, when serum TSH is with<strong>in</strong>the normal range, free T 4 will also be <strong>in</strong> the normal range. Onthe other hand, T 3 levels may be <strong>in</strong> the lower reference rangeand occasionally mildly subnormal (150).The normal range <strong>for</strong> TSH values, with an upper limit of4.12 mIU/L is largely based on NHANES III (11) data, but ithas not been universally accepted. Some have proposed thatthe upper normal should be either 2.5 or 3.0 mIU/L (86) <strong>for</strong> anumber of reasons: The distribution of TSH values used to establish thenormal reference range is skewed to the right by valuesbetween 3.1 and 4.12 mIU/L. The mean and median values of approximately1.5 mIU/L are much closer to the lower limit of the reportednormal reference range than the upper limit. When risk factors <strong>for</strong> thyroid disease are excluded, theupper reference limit is somewhat lower.The counter arguments are that while many with TSH valuesbetween 2.5–3.0 and 4.12 mIU/L may have early hypothyroidism,many do not. Data to support treat<strong>in</strong>g patients <strong>in</strong> thisrange are lack<strong>in</strong>g, with the exception of data <strong>in</strong> pregnancy (seeConcurrent conditions of special significance <strong>in</strong> hypothyroidpatients—<strong>Hypothyroidism</strong> dur<strong>in</strong>g pregnancy). Though patientswithout thyroid disease have stable mean TSH values,measurements vary up to 50% above (78) and below the meanon a given day. Thus, if the upper normal of TSH were consideredto be 2.5 mIU/L, patients with mean values just abovethe mean NHANES III value of 1.5 mIU/L would frequentlybe classified as hypothyroid when they are not (78,87). Thiswould lead to more than 10 million additional diagnoses ofhypothyroidism <strong>in</strong> the United States per year—without clearcutbenefit. The controversy has not only contributed to thedebate about what TSH values should prompt treatment, butalso what the target TSH should be <strong>for</strong> patients be<strong>in</strong>g treated<strong>for</strong> hypothyroidism. Data concern<strong>in</strong>g cl<strong>in</strong>ical benefit arelack<strong>in</strong>g to support target<strong>in</strong>g to reach low normal or subnormalTSH levels <strong>in</strong> the treatment of hypothyroidism (198,199).As a result, <strong>in</strong> patients who are not pregnant, the target rangeshould be with<strong>in</strong> the normal range. If upper and lower normal
1214 GARBER ET AL.values <strong>for</strong> a third generation TSH assay are not available, therange used should be based on the NHANES III referencepopulation range of 0.45–4.12. Although there are substantialnormative data establish<strong>in</strong>g what trimester specific normalranges are <strong>for</strong> pregnancy (200–207) (see Table 7, TSH upperrange of normal), there are no prospective trials establish<strong>in</strong>goptimal target TSH ranges <strong>for</strong> patients with hypothyroidismwho are pregnant and are be<strong>in</strong>g treated with L-thyrox<strong>in</strong>e. Thelower range of normal <strong>for</strong> serum TSH <strong>in</strong> pregnancy is generally0.1–0.2 mIU/L lower than the normal range <strong>for</strong> thosewho are not pregnant (10).The appropriate target TSH values treatment <strong>for</strong> treat<strong>in</strong>gpatients with differentiated thyroid cancer, goiter, and nodularthyroid disease are beyond the scope of these guidel<strong>in</strong>es.When to consult an endocr<strong>in</strong>ologistAlthough most physicians can diagnose and treat hypothyroidism,consultation with an endocr<strong>in</strong>ologist is recommended<strong>in</strong> the follow<strong>in</strong>g situations: Children and <strong>in</strong>fants Patients <strong>in</strong> whom it is difficult to render and ma<strong>in</strong>ta<strong>in</strong> aeuthyroid state Pregnancy Women plann<strong>in</strong>g conception Cardiac disease Presence of goiter, nodule, or other structural changes <strong>in</strong>the thyroid gland Presence of other endocr<strong>in</strong>e disease such as adrenal andpituitary disorders Unusual constellation of thyroid function test results Unusual causes of hypothyroidism such as those <strong>in</strong>ducedby agents listed <strong>in</strong> Table 10.The basis <strong>for</strong> these recommendations stems from observationsthat cost-effective diagnostic evaluations and improvedoutcomes <strong>in</strong> the medical and surgical evaluation and managementof thyroid disorders such as nodular thyroid diseaseand thyroid cancer are positively correlated with the volume ofexperience a surgeon has or whether or not the patient wasevaluated by an endocr<strong>in</strong>ologist (208–210). In addition, endocr<strong>in</strong>ologistswere more knowledgeable about thyroid diseaseand pregnancy than obstetrician-gynecologists, <strong>in</strong>ternists, andfamily physicians (211). Observational studies compar<strong>in</strong>g careprovided by endocr<strong>in</strong>ologists with nonendocr<strong>in</strong>ologists <strong>for</strong>congenital, pediatric, and central hypothyroidism as well theuncommon, challeng<strong>in</strong>g cl<strong>in</strong>ical situations just listed, whichare regularly addressed by cl<strong>in</strong>ical endocr<strong>in</strong>ologists, are lack<strong>in</strong>g,and controlled studies would be unethical.Concurrent conditions of special significance<strong>in</strong> hypothyroid patients<strong>Hypothyroidism</strong> dur<strong>in</strong>g pregnancy. Overt untreated hypothyroidismdur<strong>in</strong>g pregnancy may adversely affect maternaland fetal outcomes. These adverse outcomes <strong>in</strong>clude <strong>in</strong>creased<strong>in</strong>cidences of spontaneous miscarriage, preterm delivery, preeclampsia,maternal hypertension, postpartum hemorrhage, lowbirth weight and stillbirth, and impaired <strong>in</strong>tellectual and psychomotordevelopment of the fetus (212–214). While there isevidence to suggest that subcl<strong>in</strong>ical hypothyroidism <strong>in</strong> earlypregnancy may also be associated with impaired <strong>in</strong>tellectual andpsychomotor development (215–218), and that this impairmentmay be prevented with L-thyrox<strong>in</strong>e treatment (217,218), this isnot supported by a recent randomized control trial (219). F<strong>in</strong>ally,womenwithpositiveTPOAbmayhavean<strong>in</strong>creasedrisk<strong>for</strong>firsttrimester miscarriage (220), preterm delivery (221), and <strong>for</strong> offspr<strong>in</strong>gwith impaired cognitive development (218,222). This riskmay be due to reduced thyroid functional reserve from chronicautoimmune thyroiditis lead<strong>in</strong>g to subtle hypothyroidism (223).One European study has shown that treatment with L-thyrox<strong>in</strong>ereduced the risk of miscarriage to that of TPOAb-negativeeuthyroid controls (224). A recent prospective study done <strong>in</strong>Ch<strong>in</strong>a showed that <strong>in</strong>tellectual and psychomotor developmentof offspr<strong>in</strong>g born to women with positive TPOAb and normalthyroid function who were treated with L-thyrox<strong>in</strong>e by 8 weeksof gestation had <strong>in</strong>tellectual and psychomotor developmentcomparable to controls (218). F<strong>in</strong>ally, treatment with L-thyrox<strong>in</strong>ebe<strong>for</strong>e conception has been shown to reduce the miscarriage rateand to <strong>in</strong>crease live birth rate <strong>in</strong> women with subcl<strong>in</strong>ical hypothyroidismundergo<strong>in</strong>g assisted reproduction (225).A susta<strong>in</strong>ed rise <strong>in</strong> serum total T 4 and a drop <strong>in</strong> serum TSHcharacterize the early stage of normal pregnancy. Studies offetal development and at least one outcome study done <strong>in</strong>Europe suggest that early central nervous system developmentrequires adequate transplacental T 4 transport (226–231).The offspr<strong>in</strong>g of mothers with serum T 4 levels <strong>in</strong> the lowest10th percentile of the reference range at the end of the firsttrimester have been reported to have subnormal <strong>in</strong>tellectualdevelopment even if TSH levels are normal (228–231). Basedon these f<strong>in</strong>d<strong>in</strong>gs, desiccated thyroid and L-thyrox<strong>in</strong>e/L-triiodothyron<strong>in</strong>e comb<strong>in</strong>ations, which cause lower<strong>in</strong>g ofserum T 4 levels, should not be used dur<strong>in</strong>g pregnancy. Furthermore,patients be<strong>in</strong>g treated with these preparationsshould be switched to L-thyrox<strong>in</strong>e when plann<strong>in</strong>g to conceiveand at the very latest when found to be pregnant. At this timeTSH should also be measured. A more recent study done <strong>in</strong>Greater Boston, which is iod<strong>in</strong>e sufficient, however, did notdemonstrate a relationship between fetal <strong>in</strong>tellectual developmentand maternal serum T 4 levels (232).When a woman with hypothyroidism becomes pregnant,the dosage of L-thyrox<strong>in</strong>e should be <strong>in</strong>creased as soon aspossible to ensure that serum TSH is < 2.5 mIU/L and thatserum total T 4 is <strong>in</strong> the normal reference range <strong>for</strong> pregnancy.Moreover, when a patient with a positive TPOAb test becomespregnant, serum TSH should be measured as soon aspossible and if it is >2.5 mIU/L, L-thyrox<strong>in</strong>e treatment shouldbe <strong>in</strong>itiated. Serum TSH and total T 4 measurements should bemonitored every 4 weeks dur<strong>in</strong>g the first half of pregnancy(233) and at least once between 26 and 32 weeks gestation toensure that the requirement <strong>for</strong> L-thyrox<strong>in</strong>e has not changed.Some of us would cont<strong>in</strong>ue to monitor thyroid <strong>in</strong>dices after 32weeks <strong>in</strong> order to confirm that thyroid <strong>in</strong>dices are <strong>in</strong> thenormal range. L-thyrox<strong>in</strong>e dosages should be adjusted as <strong>in</strong>dicated,aim<strong>in</strong>g <strong>for</strong> TSH levels that are with<strong>in</strong> the normalrange <strong>for</strong> that phase of pregnancy (177,200–207,234–238).Some advocate do<strong>in</strong>g so more frequently <strong>in</strong> order to ensurecompliance and the efficacy of dose adjustments, as reflectedby dropp<strong>in</strong>g TSH levels. Total T 4 <strong>in</strong>creases predictably dur<strong>in</strong>gpregnancy and, as already noted, the reference range is *1.5fold that of the nonpregnant range. Serum TSH levels decl<strong>in</strong>e<strong>in</strong> the first trimester when serum human chorionic gonadotrop<strong>in</strong>levels are high and rise after 10–12 weeks gestation.While the upper limit of normal <strong>for</strong> the first trimester is generally< 2.5 mIU/L respective upper normal values <strong>for</strong> the
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1215second and third trimesters are approximately 3.0 and3.5 mIU/L.Diabetes mellitus. Approximately 10% of patients withtype 1 diabetes mellitus will develop chronic thyroiditis (53)dur<strong>in</strong>g their lifetime, which may lead to the <strong>in</strong>sidious onset ofsubcl<strong>in</strong>ical hypothyroidism. Patients with diabetes should beexam<strong>in</strong>ed <strong>for</strong> the presence and development of a goiter.Sensitive TSH measurements should be obta<strong>in</strong>ed at regular<strong>in</strong>tervals <strong>in</strong> patients with type 1 diabetes, especially if a goiterdevelops or if evidence is found of other autoimmune disorders.In addition, postpartum thyroiditis will develop <strong>in</strong> up to25% of women with type 1 diabetes (239).Infertility. Some patients with <strong>in</strong>fertility and menstrualirregularities have underly<strong>in</strong>g chronic thyroiditis <strong>in</strong> conjunctionwith subcl<strong>in</strong>ical or overt hypothyroidism. Moreover,TPOAb-positive patients, even when euthyroid, have an excessmiscarriage rate (220,224). Typically, these patients seekmedical attention because of <strong>in</strong>fertility or a previous miscarriage,rather than hypothyroidism.A careful, comprehensive history, physical exam<strong>in</strong>ation,and appropriate laboratory evaluation can identify chronicthyroiditis. It has long been recognized that <strong>in</strong> some withpatients with overt hypothyroidism, thyroid hormone replacementtherapy may normalize the menstrual cycle andrestore normal fertility (63–65).Obesity. <strong>Hypothyroidism</strong> and obesity are often l<strong>in</strong>ked atleast <strong>in</strong> the consciousness of the lay public. However, appetite<strong>in</strong> those with marked hypothyroidism is often suppressedoffsett<strong>in</strong>g the impact of a decrease <strong>in</strong> metabolic rate, myxedemamay present with weight loss, and overt hypothyroidismdoes not appear to be more common <strong>in</strong> the obesepopulation than <strong>in</strong> the general population (240). Nonethelessthis impression dates back to early observations of significantweight loss follow<strong>in</strong>g the resolution of myxedema, an effectthat was pr<strong>in</strong>cipally the result of fluid mobilization (241). Thiswas recently confirmed <strong>in</strong> a prospective year-long study ofnewly diagnosed patients with overt hypothyroidism whosemean TSH levels at the onset of the study was 102 (242). Someobservational studies correlate TSH levels with body mass <strong>in</strong>dex(243–245) while others do not (246). However, obesity mayhave an impact on the hypothalamic–pituitary–thyroid axis asevidenced by relatively elevated TSH levels <strong>in</strong> morbidly obeseadults (247) and children (248) who have ultrasound f<strong>in</strong>d<strong>in</strong>gssuggestive of chronic thyroiditis without either elevated antithyroidantibody titers or decreased T 4 and T 3 levels. Cautionmust there<strong>for</strong>e be exercised when diagnos<strong>in</strong>g subcl<strong>in</strong>ical hypothyroidism<strong>in</strong> the sett<strong>in</strong>g of marked obesity (249).Apart from the mobilization of fluid and the ensu<strong>in</strong>g diuresis<strong>in</strong> myxedematous states, however, the impact ofthyroid hormone therapy on waist–hip ratio (250) andweight loss (242), even <strong>in</strong> cases of profound hypothyroidism,appears at most to be modest. This is despite the fact thatrest<strong>in</strong>g energy expenditure <strong>in</strong>creases significantly <strong>in</strong> <strong>in</strong>dividualswho are rendered subcl<strong>in</strong>ically hyperthyroid afterbe<strong>in</strong>g subcl<strong>in</strong>ically hypothyroid (251). Clearly behavioraland other physiological factors apart from thyroid statushave an impact on weight status. Because of the negativeimpact on nitrogen balance, cardiovascular factors, bone,and affective status, supraphysiological doses of thyroidhormone as used <strong>in</strong> the past (252,253) should not be employedas an adjunct to weight loss programs <strong>in</strong> patientswith or without hypothyroidism (254). However, it is advisableto counsel patients about the effect any change <strong>in</strong>thyroid status may have on weight control. This <strong>in</strong>cludesthyroidectomy although recent studies concern<strong>in</strong>g its effectare contradictory (255,256).Patients with normal thyroid tests. Patients with symptomsof hypothyroidism, but normal thyroid hormone levelsdo not benefit from treatment with L-thyrox<strong>in</strong>e (257). Moreover,treatment confers a substantial risk of subcl<strong>in</strong>ical orovert hyperthyroidism, which <strong>in</strong> one large-scale study wasapproximately 20% (12).Depression. The diagnosis of subcl<strong>in</strong>ical or overt hypothyroidismmust be considered <strong>in</strong> every patient with depression.In fact, a small proportion of all patients with depressionhave primary hypothyroidism—either overt or subcl<strong>in</strong>ical.Those with autoimmune disease are more likely to have depression(258) as are those with postpartum thyroiditis regardlessof whether the hypothyroidism is treated or not (259).All patients receiv<strong>in</strong>g lithium therapy require periodicthyroid evaluation because lithium may <strong>in</strong>duce goiter andhypothyroidism (32–34). Occasionally <strong>in</strong> psychiatric practice,some patients who have depression are treated not only withantidepressants but also with thyroid hormone, even thoughthey have normal thyroid function. No firm evidence hasshown that thyroid hormone treatment alone does anyth<strong>in</strong>gto alleviate depression <strong>in</strong> such patients.Substantial evidence supports the use of thyroid hormoneto treat the mood disturbances associated with hypothyroidism(114). Interest<strong>in</strong>g animal data l<strong>in</strong>k the use of bothtricyclic antidepressants (TCAs) and selective seroton<strong>in</strong> reuptake<strong>in</strong>hibitors (SSRIs) to potential changes <strong>in</strong> bra<strong>in</strong> thyroidhormone metabolism, which make the comb<strong>in</strong>ation ofL-triiodothyron<strong>in</strong>e with these an appeal<strong>in</strong>g therapeutic hypothesis(114). However, the cl<strong>in</strong>ical data from randomizedcontrolled trials evaluat<strong>in</strong>g the acceleration and augmentationof response with TCA as well as SSRI/L-triiodothyron<strong>in</strong>ecomb<strong>in</strong>ations are <strong>in</strong>consistent (114,260,261) and do not clearlysupport L-triiodothyron<strong>in</strong>e use <strong>in</strong> euthyroid depressed subjects.Nonthyroidal illness. The evaluation of thyroid function<strong>in</strong> chronically or markedly acutely ill patients may be confus<strong>in</strong>g.Medications, such as glucocorticoids (90), amiodarone(37), and dopam<strong>in</strong>e (89) may have an impact on thyroidhormone levels and <strong>in</strong> the case of amiodarone, a marked effecton thyroid status. In addition, major illness and starvationmay be accompanied by a change <strong>in</strong> thyroid hormone economy,result<strong>in</strong>g <strong>in</strong> a low serum T 3 and normal or low serum T 4and TSH levels (262,263). S<strong>in</strong>ce there is evidence that treatmentwith either L-thyrox<strong>in</strong>e (264) or L-triiodothyron<strong>in</strong>e (265)is of no benefit, patients who are not clearly hypothyroidshould not be treated until their acute medical condition hasresolved. A 2010 study showed that <strong>in</strong>fants under 5 months ofage undergo<strong>in</strong>g cardiac surgery <strong>for</strong> complex congenital heartdisease benefited from <strong>in</strong>travenous L-triiodothyron<strong>in</strong>e treatment(266), rais<strong>in</strong>g the possibility that under certa<strong>in</strong> circumstancestreat<strong>in</strong>g nonthyroidal illness with thyroid hormonemay be beneficial. In addition, patients with NYHA class III orIV heart failure with low serum T 3 levels have been shown to
1216 GARBER ET AL.benefit from <strong>in</strong>travenous L-triiodothyron<strong>in</strong>e to restore serumT 3 levels to normal (267). Evaluation of the patient by a cl<strong>in</strong>icalendocr<strong>in</strong>ologist is appropriate be<strong>for</strong>e <strong>in</strong>itiation of thyroidhormone treatment.Dietary supplements and nutraceuticals<strong>in</strong> the treatment of hypothyroidismThe majority of dietary supplements (DS) fail to meet alevel of scientific substantiation deemed necessary <strong>for</strong> thetreatment of disease (268,269). In the case of hypothyroidism,this is the case <strong>for</strong> over-the-counter products marketed<strong>for</strong> ‘‘thyroid support’’ or as a ‘‘thyroid supplement’’ orto promote ‘‘thyroid health,’’ among others. The authorsdo not recommend the use of these or any unproven therapies(269).DS are generally thought of as various vitam<strong>in</strong>s, m<strong>in</strong>erals,and other ‘‘natural’’ substances, such as prote<strong>in</strong>s, herbs, andbotanicals. The U.S. Food and Drug Adm<strong>in</strong>istration (FDA)1994 Dietary Supplement Health and Education Actexpanded the def<strong>in</strong>ition of DS as follows (270):DSHEA 1994 x3(a). ‘‘(ff) The term ‘dietary supplement’:(1) means a product (other than tobacco) that is <strong>in</strong>tendedto supplement the diet that bears or conta<strong>in</strong>s one ormore of the follow<strong>in</strong>g dietary <strong>in</strong>gredients: a vitam<strong>in</strong>, am<strong>in</strong>eral, an herb or other botanical, an am<strong>in</strong>o acid, adietary substance <strong>for</strong> use by man to supplement thediet by <strong>in</strong>creas<strong>in</strong>g the total dietary <strong>in</strong>take, or a concentrate,metabolite, constituent, extract, or comb<strong>in</strong>ationof any [of these <strong>in</strong>gredients].(2) means a product that is <strong>in</strong>tended <strong>for</strong> <strong>in</strong>gestion <strong>in</strong> [pill,capsule, tablet, or liquid <strong>for</strong>m]; is not represented <strong>for</strong>use as a conventional food or as the sole item of a mealor diet; and is labeled as a dietary supplement.’’(3) [paraphrased] <strong>in</strong>cludes products such as an approvednew drug, certified antibiotic, or licensed biologic thatwas marketed as a dietary supplement or food be<strong>for</strong>eapproval, certification, or license (unless the Secretaryof Health and Human Services waives this provision).Nutraceuticals (N), a term co<strong>in</strong>ed to reflect its ‘‘nutrition’’orig<strong>in</strong> and ‘‘pharmaceutical’’ action, do not have a ‘‘regulatorydef<strong>in</strong>ition.’’ They are dietary supplements that ‘‘conta<strong>in</strong> a concentrated<strong>for</strong>m of a presumed bioactive substance orig<strong>in</strong>allyderived from a food, but now present <strong>in</strong> a non-food matrix, andused to enhance health <strong>in</strong> dosages exceed<strong>in</strong>g those obta<strong>in</strong>ablefrom normal foods’’ (268). <strong>Guidel<strong>in</strong>es</strong> <strong>for</strong> the use of DS/N <strong>in</strong>endocr<strong>in</strong>ology have been previously published by AACE (269) .Functional foods are those foods conta<strong>in</strong><strong>in</strong>g substances hav<strong>in</strong>gphysiological actions beyond their simple nutritional value.Overlap of symptoms <strong>in</strong> euthyroidand hypothyroid personsThe symptoms of hypothyroidism are nonspecific andmimic symptoms that can be associated with variations <strong>in</strong>lifestyle, <strong>in</strong> the absence of disease, or those of many otherconditions. This is well illustrated <strong>in</strong> the Colorado thyroiddisease prevalence study (12). That study found that four ormore symptoms of hypothyroidism were present <strong>in</strong> approximately25% of those with overt hypothyroidism, 20% of thosewith subcl<strong>in</strong>ical hypothyroidism, and <strong>in</strong> 17% of euthyroidpatients. Although the differences were statistically significants<strong>in</strong>ce 88% of the population studied was euthyroid, 9%had subcl<strong>in</strong>ical hypothyroidism, and only 0.4% were overtlyhypothyroid, it is clear that there are many more euthyroidpatients with symptoms suggestive of hypothyroidism thanthose who are subcl<strong>in</strong>ically or overtly hypothyroid.A recent study compared symptoms <strong>in</strong> euthyroid patientswho underwent surgery <strong>for</strong> benign thyroid disease. Those withHashimoto’s thyroiditis, the commonest cause of hypothyroidism<strong>in</strong> iod<strong>in</strong>e sufficient regions, were more likely to compla<strong>in</strong> ofchronic fatigue, chronic irritability, chronic nervousness, andlower quality-of life than those without evidence of chronicthyroiditis (271). Nonetheless, the promulgation of claims thatsubstances other than thyroid hormone may reverse thesesymptoms or <strong>in</strong>fluence thyroid status has contributed to thewidespread use of alternative therapies <strong>for</strong> hypothyroidism.Excess iod<strong>in</strong>e <strong>in</strong>take and hypothyroidismIod<strong>in</strong>e is used as a pharmaceutical <strong>in</strong> the management ofhyperthyroidism and thyroid cancer (as radioiod<strong>in</strong>e). Kelpsupplements conta<strong>in</strong> at least 150–250 lg of iod<strong>in</strong>e per capsulecompared with the recommended daily <strong>in</strong>take of iod<strong>in</strong>e of150 lg <strong>for</strong> adults who are not pregnant or nurs<strong>in</strong>g. In euthyroidpatients, especially those with chronic thyroiditis, substantialkelp use may be associated with significant <strong>in</strong>creases<strong>in</strong> TSH levels (38). No cl<strong>in</strong>ical data exist to support the preferentialuse of stable iod<strong>in</strong>e, kelp, or other iod<strong>in</strong>e-conta<strong>in</strong><strong>in</strong>gfunctional foods <strong>in</strong> the management of hypothyroidism <strong>in</strong>iod<strong>in</strong>e-sufficient regions unless iod<strong>in</strong>e deficiency is stronglysuspected and confirmed.Adverse metabolic effects of iod<strong>in</strong>e supplementation areprimarily reported <strong>in</strong> patients with organification defects(e.g., Hashimoto’s thyroiditis) <strong>in</strong> which severe hypothyroidismensues and is referred to as ‘‘iodide myxedema’’ (39,40).Even though pregnant women may be iod<strong>in</strong>e deficient andrequire supplementation to achieve a total iod<strong>in</strong>e <strong>in</strong>take of200–300 lg/d, <strong>in</strong>gest<strong>in</strong>g kelp or other seaweed-based productsis not recommended ow<strong>in</strong>g to the variability <strong>in</strong> iod<strong>in</strong>econtent (16,272,273).Desiccated thyroidAnimal-derived desiccated thyroid (see L-thyrox<strong>in</strong>e treatmentof hypothyroidism) conta<strong>in</strong>sT 4 and T 3 .S<strong>in</strong>ceT 3 levels vary substantiallythroughout the day <strong>in</strong> those tak<strong>in</strong>g desiccated thyroid,T 3 levels cannot be easily monitored. Be<strong>in</strong>g viewed by some as anatural source of thyroid hormone has made it attractive tosome patients who may not even have biochemically confirmedhypothyroidism and wish to lose weight or <strong>in</strong>crease their senseof well-be<strong>in</strong>g (274). There are substantially more data on theuse of synthetic L-thyrox<strong>in</strong>e <strong>in</strong> the management of welldocumentedhypothyroidism, goiter, and thyroid cancer than<strong>for</strong> desiccated thyroid hormone. A PubMed computer search ofthe literature <strong>in</strong> January 2012 yielded 35 prospective randomizedcl<strong>in</strong>ical trials (PRCTs) <strong>in</strong>volv<strong>in</strong>g synthetic L-thyrox<strong>in</strong>epublished <strong>in</strong> 2007–2011, compared with no PRCTs <strong>in</strong>volv<strong>in</strong>gdesiccated thyroid extract <strong>for</strong> all years <strong>in</strong> the database. Thus,there are no controlled trials support<strong>in</strong>g the preferred use ofdesiccated thyroid hormone over synthetic L-thyrox<strong>in</strong>e <strong>in</strong> thetreatment of hypothyroidism or any other thyroid disease.
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 12173,5,3¢-Triiodothyroacetic acidAnother DS/N used <strong>for</strong> thyroid health is 3,5,3¢-triiodothyroaceticacid (TRIAC; tiratricol), an active metabolite of T 3 ,which has been sold over the counter <strong>for</strong> weight loss. TRIACappears to have enhanced hepatic and skeletal thyromimeticeffects compared with L-thyrox<strong>in</strong>e (275). The FDA scrut<strong>in</strong>izedits use because of its lack of proven benefit as well as thyrotoxicand hypothyroid side effects (276–278). It is difficult totitrate or monitor cl<strong>in</strong>ically and biochemically. Its role <strong>in</strong> thetreatment of hypothyroidism <strong>in</strong> syndromes of generalizedresistance to thyroid hormone, particularly when L-thyrox<strong>in</strong>ealone appears to be <strong>in</strong>adequate, rema<strong>in</strong>s uncerta<strong>in</strong> (279,280).There are no data support<strong>in</strong>g its use <strong>in</strong> lieu of synthetic L-thyrox<strong>in</strong>e <strong>in</strong> the treatment of hypothyroidism.Thyroid-enhanc<strong>in</strong>g preparationsL-tyros<strong>in</strong>e has been touted as a treatment <strong>for</strong> hypothyroidismby virtue of its role <strong>in</strong> thyroid hormone synthesis.There are no precl<strong>in</strong>ical or cl<strong>in</strong>ical studies demonstrat<strong>in</strong>g thatL-tyros<strong>in</strong>e has thyromimetic properties. B vitam<strong>in</strong>s, garlic,g<strong>in</strong>ger, g<strong>in</strong>gko, licorice, magnesium, manganese, meadowsweet,oats, p<strong>in</strong>eapple, potassium, saw palmetto, and valerianare <strong>in</strong>cluded <strong>in</strong> various commercially available ‘‘thyroidenhanc<strong>in</strong>gpreparations.’’ There are no precl<strong>in</strong>ical or cl<strong>in</strong>icalstudies demonstrat<strong>in</strong>g any thyromimetic properties of any ofthese DS/N. In a recent study (281), 9 out of 10 thyroid healthsupplements (marketed as ‘‘thyroid support’’) studied conta<strong>in</strong>edcl<strong>in</strong>ically significant amounts of L-thyrox<strong>in</strong>e ( > 91 lg/d)and/or L-triiodothyron<strong>in</strong>e ( > 10 lg/day). Physicians shouldspecifically engage patients regard<strong>in</strong>g all <strong>for</strong>ms of DS/N,specifically those marketed as thyroid support, and considerthe possibility that any DS/N could be adulterated with L-thyrox<strong>in</strong>e or L-triiodothyron<strong>in</strong>e.Thyromimetic preparationsSome DS/N with thyromimetic properties that have beenstudied but are of unproven cl<strong>in</strong>ical benefit <strong>in</strong>clude Asiang<strong>in</strong>seng (282), bladderwrack (283), capsaic<strong>in</strong> (284), ech<strong>in</strong>acea(285), and <strong>for</strong>skol<strong>in</strong> (286).SeleniumSelenium is an essential dietary m<strong>in</strong>eral that is part of variousselenoenzymes. These compounds are <strong>in</strong> many antioxidant,oxidation-reduction, and thyroid hormone deiod<strong>in</strong>ation pathways.It is not surpris<strong>in</strong>g that by virtue of these biochemicaleffects, selenium has been <strong>in</strong>vestigated as a modulator of autoimmunethyroid disease and thyroid hormone economy. In onestudy, selenium adm<strong>in</strong>istration was found to reduce the risk <strong>for</strong>cancer, but <strong>in</strong> a follow-up study of the study cohort, there was an<strong>in</strong>creased risk of diabetes (287). Inawell-designed,EuropeanPRCT of 2143 euthyroid women, selenium adm<strong>in</strong>istration (as200 lg/d selenomethion<strong>in</strong>e) was associated with a reduction <strong>in</strong>autoimmune thyroid disease, postpartum thyroiditis, and hypothyroidism(288). S<strong>in</strong>ce dietary selenium <strong>in</strong>take variesworldwide, these results may not be generalizable to all populations.In another PRCT <strong>in</strong>volv<strong>in</strong>g 501 patients <strong>in</strong> the UnitedK<strong>in</strong>gdom who were over age 60 years, vary<strong>in</strong>g doses of selenium(100, 200, or 300 lg/d) <strong>for</strong> 6 months were not associated withbeneficial changes <strong>in</strong> T 4 to T 3 conversion (289). Most recently, ameta-analysis was per<strong>for</strong>med of bl<strong>in</strong>ded PRCTs of patients withHashimoto’s thyroiditis receiv<strong>in</strong>g L-thyrox<strong>in</strong>e therapy (290). Theanalysis found that selenium supplementation was associatedwith decreased anti-TPO titers and improved well-be<strong>in</strong>g ormood, but there were no significant changes <strong>in</strong> thyroid glandultrasonographic morphology or L-thyrox<strong>in</strong>e dos<strong>in</strong>g. Taken together,what do these limited cl<strong>in</strong>ical data suggest? Selenium hasnotable theoretical potential <strong>for</strong> salutary effects on hypothyroidismand thyroid autoimmunity <strong>in</strong>clud<strong>in</strong>g Graves’ eye disease(291), both as a preventive measure and as a treatment.However, there are simply not enough outcome data to suggesta role at the present time <strong>for</strong> rout<strong>in</strong>e selenium use to prevent ortreat hypothyroidism <strong>in</strong> any population.QUESTIONS AND GUIDELINE RECOMMENDATIONS*When should anti-thyroid antibodies bemeasured?&RECOMMENDATION 1Anti–thyroid peroxidase antibody (TPOAb) measurementsshould be considered when evaluat<strong>in</strong>g patients with subcl<strong>in</strong>icalhypothyroidism. Grade B, BEL 1See: Epidemiology; Primary and secondary etiologies ofhypothyroidismRecommendation 1 was downgraded to B because the bestevidence is only predictive <strong>in</strong> nature. If anti-thyroid antibodiesare positive, hypothyroidism occurs at a rate of 4.3%per year versus 2.6% per year when anti-thyroid antibodiesare negative. There<strong>for</strong>e, the presence of positive TPOAb mayor may not <strong>in</strong>fluence the decision to treat.&RECOMMENDATION 2TPOAb measurement should be considered <strong>in</strong> order toidentify autoimmune thyroiditis when nodular thyroiddisease is suspected to be due to autoimmune thyroiddisease. Grade D, BEL 4See: Primary and secondary etiologies of hypothyroidism&RECOMMENDATION 3TPOAb measurement should be considered when evaluat<strong>in</strong>gpatients with recurrent miscarriage, with or without<strong>in</strong>fertility. Grade A, BEL 2See: Concurrent conditions of special significance—InfertilityRecommendation 3 was upgraded to A because of favorablerisk–benefit potential.&RECOMMENDATION 4Measurement of TSHRAbs us<strong>in</strong>g a sensitive assay shouldbe considered <strong>in</strong> hypothyroid pregnant patients with ahistory of Graves’ disease who were treated with radioactiveiod<strong>in</strong>e or thyroidectomy prior to pregnancy. Thisshould be <strong>in</strong>itially done either at 20–26 weeks of gestationor dur<strong>in</strong>g the first trimester and if they are elevated aga<strong>in</strong> at20–26 weeks of gestation. Grade A, BEL 2See: Primary and secondary etiologies of hypothyroidism*Note: When referr<strong>in</strong>g to therapy and therapeutic preparations <strong>in</strong>the recommendations and elsewhere, L-thyrox<strong>in</strong>e and L-triiodothyron<strong>in</strong>eare generally used <strong>in</strong>stead of their respective hormonalequivalents, T 4 and T 3 .
1218 GARBER ET AL.Recommendation 4 was upgraded to A because the correlationbetween a high titer of TSHRAb and the developmentof fetal or neonatal Graves’ disease is strong.What is the role of cl<strong>in</strong>ical scor<strong>in</strong>g systems<strong>in</strong> the diagnosis of patients with hypothyroidism?&RECOMMENDATION 5<strong>Cl<strong>in</strong>ical</strong> scor<strong>in</strong>g systems should not be used to diagnosehypothyroidism. Grade A, BEL 1See: Signs and symptoms of hypothyroidism; Other diagnostictests <strong>for</strong> hypothyroidismWhat is the role of diagnostic tests apart fromserum thyroid hormone levels and TSH <strong>in</strong> theevaluation of patients with hypothyroidism?&RECOMMENDATION 6Tests such as cl<strong>in</strong>ical assessment of reflex relaxation time,cholesterol, and muscle enzymes should not be used todiagnose hypothyroidism. Grade B, BEL 2See: Signs and symptoms of hypothyroidism; Other diagnostictests <strong>for</strong> hypothyroidismWhat are the preferred thyroid hormonemeasurements <strong>in</strong> addition to TSH <strong>in</strong> theassessment of patients with hypothyroidism?&RECOMMENDATION 7Apart from pregnancy, assessment of serum free T 4 shouldbe done <strong>in</strong>stead of total T 4 <strong>in</strong> the evaluation of hypothyroidism.An assessment of serum free T 4 <strong>in</strong>cludes a freeT 4 <strong>in</strong>dex or free T 4 estimate and direct immunoassay offree T 4 without physical separation us<strong>in</strong>g anti-T 4 antibody.Grade A, BEL 1See: Measurement of T 4 and T 3 ; Table 6&RECOMMENDATION 8Assessment of serum free T 4 , <strong>in</strong> addition to TSH, should beconsidered when monitor<strong>in</strong>g L-thyrox<strong>in</strong>e therapy.Grade B, BEL 1See: Measurement of T 4 and T 3Recommendation 8 was downgraded to B s<strong>in</strong>ce it shouldonly be used selectively.&RECOMMENDATION 9In pregnancy, the measurement of total T 4 or a free T 4 <strong>in</strong>dex,<strong>in</strong> addition to TSH, should be done to assess thyroidstatus. Because of the wide variation <strong>in</strong> the results of differentfree T 4 assays, direct immunoassay measurement offree T 4 should only be employed when method-specific andtrimester-specific reference ranges <strong>for</strong> serum free T 4 areavailable. Grade B, BEL 2See: Measurement of T 4 and T 3&RECOMMENDATION 10Serum total T 3 or assessment of serum free T 3 should not bedone to diagnose hypothyroidism. Grade A, BEL 2See: Measurement of T 4 and T 3Recommendation 10 was upgraded to A because of many<strong>in</strong>dependent l<strong>in</strong>es of evidence and expert op<strong>in</strong>ion.&RECOMMENDATION 11TSH measurements <strong>in</strong> hospitalized patients should bedone only if there is an <strong>in</strong>dex of suspicion <strong>for</strong> thyroiddysfunction. Grade A, BEL 2See: Measurement of T 4 and T 3 ; Pitfalls encountered when<strong>in</strong>terpret<strong>in</strong>g serum TSH levels; Concurrent conditionsof special significance <strong>in</strong> hypothyroid patients—Nonthyroidal illnessRecommendation 11 was upgraded to A because of costconsiderations and potential <strong>for</strong> <strong>in</strong>appropriate <strong>in</strong>tervention.&RECOMMENDATION 12In patients with central hypothyroidism, assessment of freeT 4 or free T 4 <strong>in</strong>dex, not TSH, should be done to diagnoseand guide treatment of hypothyroidism. Grade A, BEL 1See: Measurement of T 4 and T 3 ; L-thyrox<strong>in</strong>e treatmentof hypothyroidismWhen should TSH levels be measured <strong>in</strong> patientsbe<strong>in</strong>g treated <strong>for</strong> hypothyroidism?&RECOMMENDATION 13Patients be<strong>in</strong>g treated <strong>for</strong> established hypothyroidismshould have serum TSH measurements done at 4–8 weeksafter <strong>in</strong>itiat<strong>in</strong>g treatment or after a change <strong>in</strong> dose. Once anadequate replacement dose has been determ<strong>in</strong>ed, periodicTSH measurements should be done after 6 months andthen at 12-month <strong>in</strong>tervals, or more frequently if the cl<strong>in</strong>icalsituation dictates otherwise. Grade B, BEL 2See: L-thyrox<strong>in</strong>e treatment of hypothyroidismWhat should be considered the upper limitof the normal range of TSH values?&RECOMMENDATION 14.1The reference range of a given laboratory should determ<strong>in</strong>ethe upper limit of normal <strong>for</strong> a third generation TSH assay.The normal TSH reference range changes with age. If anage-based upper limit of normal <strong>for</strong> a third generation TSHassay is not available <strong>in</strong> an iod<strong>in</strong>e sufficient area, an upperlimit of normal of 4.12 should be considered.Grade A, BEL 1See: Pitfalls encountered when <strong>in</strong>terpret<strong>in</strong>g serum TSH levels;Therapeutic endpo<strong>in</strong>ts <strong>in</strong> the treatment of hypothyroidism;Table 7&RECOMMENDATION 14.2In pregnancy, the upper limit of the normal range should bebased on trimester-specific ranges <strong>for</strong> that laboratory. Iftrimester-specific reference ranges <strong>for</strong> TSH are not available<strong>in</strong> the laboratory, the follow<strong>in</strong>g upper normal referenceranges are recommended: first trimester, 2.5 mIU/L;second trimester, 3.0 mIU/L; third trimester, 3.5 mIU/L.Grade B, BEL 2See: Concurrent conditions of special significance <strong>in</strong>hypothyroid patients—<strong>Hypothyroidism</strong> dur<strong>in</strong>gpregnancy; Table 7
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1219Which patients with TSH levels above a givenlaboratory’s reference range should be considered<strong>for</strong> treatment with L-thyrox<strong>in</strong>e?&RECOMMENDATION 15Patients whose serum TSH levels exceed 10 mIU/L areat <strong>in</strong>creased risk <strong>for</strong> heart failure and cardiovascularmortality, and should be considered <strong>for</strong> treatment withL-thyrox<strong>in</strong>e. Grade B, BEL 1See: Areas <strong>for</strong> Future Research; When to treathypothyroidism—Cardiac benefit from treat<strong>in</strong>gsubcl<strong>in</strong>ical hypothyroidismRecommendation 15 was downgraded to B because it isnot generalizable and meta-analysis does not <strong>in</strong>clude prospective<strong>in</strong>terventional studies.&RECOMMENDATION 16Treatment based on <strong>in</strong>dividual factors <strong>for</strong> patients withTSH levels between the upper limit of a given laboratory’sreference range and 10 mIU/L should be considered particularlyif patients have symptoms suggestive of hypothyroidism,positive TPOAb or evidence of atheroscleroticcardiovascular disease, heart failure, or associated riskfactors <strong>for</strong> these diseases. Grade B, BEL 1See: Epidemiology; Primary and secondary etiologies ofhypothyroidism; Screen<strong>in</strong>g and aggressive case f<strong>in</strong>d<strong>in</strong>g<strong>for</strong> hypothyroidism; When to treat hypothyroidism; Areas<strong>for</strong> Future Research—Cardiac benefit from treat<strong>in</strong>gsubcl<strong>in</strong>ical hypothyroidism; Table 9Recommendation 16 was downgraded to B because theevidence is not fully generalizable to the stated recommendationand there are no prospective, <strong>in</strong>terventional studies.In patients with hypothyroidism be<strong>in</strong>g treatedwith L-thyrox<strong>in</strong>e, what should the target TSHranges be?&RECOMMENDATION 17In patients with hypothyroidism who are not pregnant, thetarget range should be the normal range of a third generationTSH assay. If an upper limit of normal <strong>for</strong> a thirdgeneration TSH assay is not available, <strong>in</strong> iod<strong>in</strong>e-sufficientareas an upper limit of normal of 4.12 mIU/L should beconsidered and if a lower limit of normal is not available,0.45 mIU/L should be considered. Grade B, BEL 2See: Pitfalls encountered when <strong>in</strong>terpret<strong>in</strong>g serum TSH levels;When to treat hypothyroidism; Therapeutic endpo<strong>in</strong>ts <strong>in</strong>the treatment of hypothyroidism; Table 7In patients with hypothyroidism be<strong>in</strong>g treatedwith L-thyrox<strong>in</strong>e who are pregnant, what shouldthe target TSH ranges be?&RECOMMENDATION 18In patients with hypothyroidism who are pregnant, thetarget range <strong>for</strong> TSH should be based on trimester-specificranges <strong>for</strong> that laboratory. If trimester-specific referenceranges are not available <strong>in</strong> the laboratory, the follow<strong>in</strong>gupper-normal reference ranges are recommended: firsttrimester, 2.5 mIU/L; second trimester, 3.0 mIU/L; andthird trimester, 3.5 mIU/L. Grade C, BEL 2See: Pitfalls encountered when <strong>in</strong>terpret<strong>in</strong>g serum TSH levels;When to treat hypothyroidism; Therapeutic endpo<strong>in</strong>ts<strong>in</strong> the treatment of hypothyroidism; Concurrent conditionsof special significance <strong>in</strong> hypothyroid patients—<strong>Hypothyroidism</strong> dur<strong>in</strong>g pregnancy; Table 7Recommendation 18 was downgraded to C due to lack ofprospective studies establish<strong>in</strong>g benefit.Which patients with normal serum TSH levelsshould be considered <strong>for</strong> treatment withL-thyrox<strong>in</strong>e?&RECOMMENDATION 19.1Treatment with L-thyrox<strong>in</strong>e should be considered <strong>in</strong> womenof childbear<strong>in</strong>g age with serum TSH levels between2.5 mIU/L and the upper limit of normal <strong>for</strong> a given laboratory’sreference range if they are <strong>in</strong> the first trimester ofpregnancy or plann<strong>in</strong>g a pregnancy <strong>in</strong>clud<strong>in</strong>g assisted reproduction<strong>in</strong> the immediate future. Treatment withL-thyrox<strong>in</strong>e should be considered <strong>in</strong> women <strong>in</strong> the secondtrimester of pregnancy with serum TSH levels between3.0 mIU/L and the upper limit of normal <strong>for</strong> a givenlaboratory’s reference range, and <strong>in</strong> women <strong>in</strong> the thirdtrimester of pregnancy with serum TSH levels between3.5 mIU/L and the upper limit of normal <strong>for</strong> a givenlaboratory’s reference range. Grade B, BEL 2See: When to treat hypothyroidism; Concurrent conditionsof special significance <strong>in</strong> hypothyroid patients—<strong>Hypothyroidism</strong> dur<strong>in</strong>g pregnancy; Table 7&RECOMMENDATION 19.2Treatment with L-thyrox<strong>in</strong>e should be considered <strong>in</strong> womenof childbear<strong>in</strong>g age with normal serum TSH levels whenthey are pregnant or plann<strong>in</strong>g a pregnancy, <strong>in</strong>clud<strong>in</strong>g assistedreproduction <strong>in</strong> the immediate future, if they have orhave had positive levels of serum TPOAb, particularlywhen there is a history of miscarriage or past history ofhypothyroidism. Grade B, BEL 2See: Concurrent conditions of special significance <strong>in</strong>hypothyroid patients—<strong>Hypothyroidism</strong> dur<strong>in</strong>gpregnancy; Table 7&RECOMMENDATION 19.3Women of childbear<strong>in</strong>g age who are pregnant or plann<strong>in</strong>ga pregnancy, <strong>in</strong>clud<strong>in</strong>g assisted reproduction <strong>in</strong> the immediatefuture, should be treated with L-thyrox<strong>in</strong>e if theyhave or have had positive levels of serum TPOAb and theirTSH is greater than 2.5 mIU/L. Grade B, BEL 2See: Concurrent conditions of special significance <strong>in</strong>hypothyroid patients—<strong>Hypothyroidism</strong> dur<strong>in</strong>gpregnancy; Table 7&RECOMMENDATION 19.4Women with positive levels of serum TPOAb or with a TSHgreater than 2.5 mIU/L who are not be<strong>in</strong>g treated withL-thyrox<strong>in</strong>e should be monitored every 4 weeks <strong>in</strong> thefirst 20 weeks of pregnancy <strong>for</strong> the development of hypothyroidism.Grade B, BEL 2See: Concurrent conditions of special significance <strong>in</strong>hypothyroid patients—<strong>Hypothyroidism</strong> dur<strong>in</strong>gpregnancy; Table 7
1220 GARBER ET AL.Who, among patients who are pregnant, orplann<strong>in</strong>g pregnancy, or with other characteristics,should be screened <strong>for</strong> hypothyroidism?&RECOMMENDATION 20.1.1Universal screen<strong>in</strong>g is not recommended <strong>for</strong> patients whoare pregnant or are plann<strong>in</strong>g pregnancy, <strong>in</strong>clud<strong>in</strong>g assistedreproduction. Grade B, BEL 1See: Areas <strong>for</strong> Future Research—Screen<strong>in</strong>g <strong>for</strong>hypothyroidism <strong>in</strong> pregnancyRecommendation 20.1.1 was downgraded to B becausethere are limitations to the evidence and there<strong>for</strong>e <strong>in</strong>sufficientevidence <strong>for</strong> lack of benefit.&RECOMMENDATION 20.1.2‘‘Aggressive case f<strong>in</strong>d<strong>in</strong>g,’’ rather than universal screen<strong>in</strong>g,should be considered <strong>for</strong> patients who are plann<strong>in</strong>g pregnancy.Grade C, BEL 2See: Areas <strong>for</strong> Future Research—Screen<strong>in</strong>g <strong>for</strong>hypothyroidism <strong>in</strong> pregnancyRecommendation 20.1.2 was downgraded to C becauseeven when a diagnosis of hypothyroidism is made, impact onoutcomes has not been demonstrated.&RECOMMENDATION 20.2Screen<strong>in</strong>g <strong>for</strong> hypothyroidism should be considered <strong>in</strong>patients over the age of 60. Grade B, BEL 1See: Epidemiology; Primary and secondary etiologies ofhypothyroidism; Screen<strong>in</strong>g and aggressive case f<strong>in</strong>d<strong>in</strong>g <strong>for</strong>hypothyroidism; Table 8Recommendation 20.2 was downgraded to B because thereis strong evidence that hypothyroidism is common <strong>in</strong> thisgroup but <strong>in</strong>sufficient evidence of benefit or cost effectiveness.&RECOMMENDATION 21‘‘Aggressive case f<strong>in</strong>d<strong>in</strong>g’’ should be considered <strong>in</strong> those at<strong>in</strong>creased risk <strong>for</strong> hypothyroidism. Grade B, BEL 2See: Epidemiology; Primary and secondary etiologies ofhypothyroidism; Screen<strong>in</strong>g and aggressive case f<strong>in</strong>d<strong>in</strong>g <strong>for</strong>hypothyroidism; Table 8How should patients with hypothyroidismbe treated and monitored?&RECOMMENDATION 22.1Patients with hypothyroidism should be treated withL-thyrox<strong>in</strong>e monotherapy. Grade A, BEL 1See: L-thyrox<strong>in</strong>e treatment of hypothyroidism&RECOMMENDATION 22.2The evidence does not support us<strong>in</strong>g L-thyrox<strong>in</strong>e andL-triiodothyron<strong>in</strong>e comb<strong>in</strong>ations to treat hypothyroidism.Grade B, BEL 1See: L-thyrox<strong>in</strong>e treatment of hypothyroidism; Concurrentconditions of special significance <strong>in</strong> hypothyroid patients;Dietary supplements and nutraceuticals <strong>in</strong> the treatment ofhypothyroidism; Desiccated thyroid; Areas <strong>for</strong> FutureResearch—L-thyrox<strong>in</strong>e/L-triiodothyron<strong>in</strong>e comb<strong>in</strong>ationtherapyRecommendation 22.2 was downgraded to Grade B becauseof still-unresolved issues raised by studies that report that somepatients prefer and some patient subgroups may benefit from acomb<strong>in</strong>ation of L-thyrox<strong>in</strong>e and L-triiodothyron<strong>in</strong>e.&RECOMMENDATION 22.3L-thyrox<strong>in</strong>e and L-triiodothyron<strong>in</strong>e comb<strong>in</strong>ations shouldnot be adm<strong>in</strong>istered to pregnant women or those plann<strong>in</strong>gpregnancy. Grade B, BEL 3See: Concurrent conditions of special significance <strong>in</strong>hypothyroid patients—<strong>Hypothyroidism</strong> dur<strong>in</strong>gpregnancyRecommendation 22.3 was upgraded to B because of potential<strong>for</strong> harm.&RECOMMENDATION 22.4There is no evidence to support us<strong>in</strong>g desiccated thyroidhormone <strong>in</strong> preference to L-thyrox<strong>in</strong>e monotherapy <strong>in</strong> thetreatment of hypothyroidism and there<strong>for</strong>e desiccatedthyroid hormone should not be used <strong>for</strong> the treatment ofhypothyroidism. Grade D, BEL 4See: L-thyrox<strong>in</strong>e treatment of hypothyroidism; Dietarysupplements and nutraceuticals <strong>in</strong> the treatment ofhypothyroidism; Desiccated thyroidRecommendation 22.4 was a unanimous expert op<strong>in</strong>ion.&RECOMMENDATION 22.53,5,3¢-triiodothyroacetic acid (TRIAC; tiratricol) should notbe used to treat primary and central hypothyroidism due tosuggestions of harm <strong>in</strong> the literature. Grade C, BEL 3See: Dietary supplements and nutraceuticals <strong>in</strong> the treatment ofhypothyroidism; 3,5,3¢-Triiodothyroacetic acid&RECOMMENDATION 22.6Patients resum<strong>in</strong>g L-thyrox<strong>in</strong>e therapy after <strong>in</strong>terruption(less than 6 weeks) and without an <strong>in</strong>tercurrent cardiacevent or marked weight loss may resume their previouslyemployed full replacement doses. Grade D, BEL 4See: L-thyrox<strong>in</strong>e treatment of hypothyroidismRecommendation 22.6 was a unanimous expert op<strong>in</strong>ion.&RECOMMENDATION 22.7.1When <strong>in</strong>itiat<strong>in</strong>g therapy <strong>in</strong> young healthy adults with overthypothyroidism, beg<strong>in</strong>n<strong>in</strong>g treatment with full replacementdoses should be considered. Grade B, BEL 2See: L-thyrox<strong>in</strong>e treatment of hypothyroidism&RECOMMENDATION 22.7.2When <strong>in</strong>itiat<strong>in</strong>g therapy <strong>in</strong> patients older than 50–60 yearswith overt hypothyroidism, without evidence of coronaryheart disease, an L-thyrox<strong>in</strong>e dose of 50 lg daily should beconsidered. Grade D, BEL 4See: L-thyrox<strong>in</strong>e treatment of hypothyroidismRecommendation 22.7.2 was a unanimous expert op<strong>in</strong>ion.&RECOMMENDATION 22.8In patients with subcl<strong>in</strong>ical hypothyroidism, <strong>in</strong>itialL-thyrox<strong>in</strong>e dos<strong>in</strong>g is generally lower than what is required<strong>in</strong> the treatment of overt hypothyroidism. A daily dose of25–75 lg should be considered, depend<strong>in</strong>g on the degree ofTSH elevation. Further adjustments should be guided bycl<strong>in</strong>ical response and follow-up laboratory determ<strong>in</strong>ations<strong>in</strong>clud<strong>in</strong>g TSH values. Grade B, BEL 2See: L-thyrox<strong>in</strong>e treatment of hypothyroidism
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1221&RECOMMENDATION 22.9Treatment with glucocorticoids <strong>in</strong> patients with comb<strong>in</strong>edadrenal <strong>in</strong>sufficiency and hypothyroidism should precedetreatment with L-thyrox<strong>in</strong>e. Grade B, BEL 2See: Disorders associated with hypothyroidism; Pitfallsencountered when try<strong>in</strong>g to <strong>in</strong>terpret serum TSH levels;L-thyrox<strong>in</strong>e treatment of hypothyroidism&RECOMMENDATION 23L-thyrox<strong>in</strong>e should be taken with water consistently 30–60m<strong>in</strong>utes be<strong>for</strong>e breakfast or at bedtime 4 hours after the lastmeal. It should be stored properly per product <strong>in</strong>sert andnot taken with substances or medications that <strong>in</strong>terferewith its absorption. Grade B, BEL 2See: L-thyrox<strong>in</strong>e treatment of hypothyroidism; Table 10&RECOMMENDATION 24In patients with central hypothyroidism, assessments ofserum free T 4 should guide therapy and targeted to exceedthe midnormal range value <strong>for</strong> the assay be<strong>in</strong>g used.Grade B, BEL 3See: Primary and secondary etiologies of hypothyroidism;Measurement of T 4 and T 3 ; Pitfalls encountered when<strong>in</strong>terpret<strong>in</strong>g serum TSH levels; L-thyrox<strong>in</strong>e treatmentof hypothyroidismRecommendation 24 was upgraded to B because morethan 50% of patients with central hypothyroidism adequatelytreated with L-thyrox<strong>in</strong>e have values <strong>in</strong> this range.&RECOMMENDATION 25.1In patients with hypothyroidism be<strong>in</strong>g treated withL-thyrox<strong>in</strong>e who are pregnant, serum TSH should bepromptly measured after conception and L-thyrox<strong>in</strong>edosage adjusted, with a goal TSH of less than 2.5 mIU/Ldur<strong>in</strong>g the first trimester. Grade B, BEL 2See: Therapeutic endpo<strong>in</strong>ts <strong>in</strong> the treatment of hypothyroidism;Concurrent conditions of special significance <strong>in</strong>hypothyroid patients—<strong>Hypothyroidism</strong> dur<strong>in</strong>gpregnancy; Table 7&RECOMMENDATION 25.2In patients with hypothyroidism be<strong>in</strong>g treated withL-thyrox<strong>in</strong>e who are pregnant, the goal TSH dur<strong>in</strong>gthe second trimester should be less than 3 mIU/Land dur<strong>in</strong>g the third trimester should be less than3.5 mIU/L.Grade C, BEL 2See: Therapeutic endpo<strong>in</strong>ts <strong>in</strong> the treatment of hypothyroidism;Concurrent conditions of special significance <strong>in</strong>hypothyroid patients—<strong>Hypothyroidism</strong> dur<strong>in</strong>gpregnancy; Table 7.Recommendation 25.2 was downgraded to C due to lack ofprospective studies establish<strong>in</strong>g benefit.&RECOMMENDATION 25.3Maternal serum TSH (and total T 4 ) should be monitoredevery 4 weeks dur<strong>in</strong>g the first half of pregnancy and at leastonce between 26 and 32 weeks gestation and L-thyrox<strong>in</strong>edosages adjusted as <strong>in</strong>dicated. Grade B, BEL 2See: Concurrent conditions of special significance <strong>in</strong> hypothyroidpatients—<strong>Hypothyroidism</strong> dur<strong>in</strong>g pregnancy&RECOMMENDATION 26In patients receiv<strong>in</strong>g L-thyrox<strong>in</strong>e treatment <strong>for</strong> hypothyroidism,serum TSH should be remeasured with<strong>in</strong> 4–8weeks of <strong>in</strong>itiation of treatment with drugs that decreasethe bioavailability or alter the metabolic disposition of theL-thyrox<strong>in</strong>e dose. Grade A, BEL 1See: L-thyrox<strong>in</strong>e treatment of hypothyroidism; Areas <strong>for</strong>Future Research—Agents and conditions hav<strong>in</strong>g animpact on L-thyrox<strong>in</strong>e therapy and <strong>in</strong>terpretation of thyroidtests; Tables 5 and 10.&RECOMMENDATION 27Apart from pregnant patients be<strong>in</strong>g treated withL-thyrox<strong>in</strong>e <strong>for</strong> hypothyroidism, the evidence does notsupport target<strong>in</strong>g specific TSH values with<strong>in</strong> the normalreference range. Grade B, BEL 2See: Therapeutic endpo<strong>in</strong>ts <strong>in</strong> the treatment of hypothyroidismWhen should endocr<strong>in</strong>ologists be <strong>in</strong>volved <strong>in</strong> thecare of patients with hypothyroidism?&RECOMMENDATION 28Physicians who are not endocr<strong>in</strong>ologists, but who are familiarwith the diagnosis and treatment of hypothyroidismshould be able to care <strong>for</strong> most patients with primary hypothyroidism.However, patients with hypothyroidism whofall <strong>in</strong>to the follow<strong>in</strong>g categories should be seen <strong>in</strong> consultationwith an endocr<strong>in</strong>ologist. These categories are (i) childrenand <strong>in</strong>fants, (ii) patients <strong>in</strong> whom it is difficult to render andma<strong>in</strong>ta<strong>in</strong> a euthyroid state, (iii) pregnancy, (iv) womenplann<strong>in</strong>g conception, (v) cardiac disease, (vi) presence ofgoiter, nodule, or other structural changes <strong>in</strong> the thyroidgland, (vii) presence of other endocr<strong>in</strong>e disease such as adrenaland pituitary disorders, (viii) unusual constellation ofthyroid function test results, and (ix) unusual causes of hypothyroidismsuch as those <strong>in</strong>duced by agents that <strong>in</strong>terferewith absorption of L-thyrox<strong>in</strong>e, impact thyroid glandhormone production or secretion, affect the hypothalamic–pituitary–thyroid axis (directly or <strong>in</strong>directly), <strong>in</strong>crease clearance,or peripherally impact metabolism. Grade C, BEL 3See: When to consult an endocr<strong>in</strong>ologist; Table 10Which patients should not be treated with thyroidhormone?&RECOMMENDATION 29Thyroid hormones should not be used to treat symptomssuggestive of hypothyroidism without biochemical confirmationof the diagnosis. Grade B, BEL 2See: Concurrent conditions of special significance <strong>in</strong> hypothyroidpatients—Patients with normal thyroid tests&RECOMMENDATION 30Thyroid hormones should not be used to treat obesity <strong>in</strong>euthyroid patients. Grade A, BEL 2See: Concurrent conditions of special significance <strong>in</strong>hypothyroid patients—ObesityRecommendation 30 was upgraded to Grade A because ofpotential harm.
1222 GARBER ET AL.&RECOMMENDATION 31There is <strong>in</strong>sufficient evidence to support us<strong>in</strong>g thyroid hormonesto treat depression <strong>in</strong> euthyroid patients.Grade B, BEL 2See: Concurrent conditions of special significance <strong>in</strong>hypothyroid patients—DepressionWhat is the role of iod<strong>in</strong>e supplementation, dietarysupplements, and nutraceuticals <strong>in</strong> the treatmentof hypothyroidism?&RECOMMENDATION 32.1Iod<strong>in</strong>e supplementation, <strong>in</strong>clud<strong>in</strong>g kelp or other iod<strong>in</strong>econta<strong>in</strong><strong>in</strong>gfunctional foods, should not be used <strong>in</strong> the managementof hypothyroidism <strong>in</strong> iod<strong>in</strong>e-sufficient areas.Grade C, BEL 3See: Dietary supplements and nutraceuticals <strong>in</strong> the treatmentof hypothyroidism; Excess iod<strong>in</strong>e <strong>in</strong>take andhypothyroidism&RECOMMENDATION 32.2Iod<strong>in</strong>e supplementation <strong>in</strong> the <strong>for</strong>m of kelp or other seaweed-basedproducts should not be used to treat iod<strong>in</strong>edeficiency <strong>in</strong> pregnant women. Grade D, BEL 4See: Dietary supplements and nutraceuticals <strong>in</strong> the treatmentof hypothyroidism; Excess iod<strong>in</strong>e <strong>in</strong>take andhypothyroidismRecommendation 32.2 was a unanimous expert op<strong>in</strong>ion&RECOMMENDATION 33Selenium should not be used to prevent or treat hypothyroidism.Grade B, BEL 2See: Dietary supplements and nutraceuticals <strong>in</strong> the treatment ofhypothyroidism; Selenium.&RECOMMENDATION 34Patients tak<strong>in</strong>g dietary supplements and nutraceuticals<strong>for</strong> hypothyroidism should be advised that commerciallyavailable thyroid-enhanc<strong>in</strong>g products are not aremedy <strong>for</strong> hypothyroidism and should be counseledabout the potential side effects of various preparationsparticularly those conta<strong>in</strong><strong>in</strong>g iod<strong>in</strong>e or sympathomimeticam<strong>in</strong>es as well as those marked as ‘‘thyroid support’’s<strong>in</strong>ce they could be adulterated with L-thyrox<strong>in</strong>e orL-triiodothyron<strong>in</strong>e. Grade D, BEL 4See: Dietary supplements and nutraceuticals <strong>in</strong> the treatment ofhypothyroidism; Thyroid enhanc<strong>in</strong>g preparations;Thyromimetic preparationsRecommendation 34 was a unanimous expert op<strong>in</strong>ion.AREAS FOR FUTURE RESEARCHCardiac benefit from treat<strong>in</strong>g subcl<strong>in</strong>icalhypothyroidismOvert hypothyroidism produces reversible changes <strong>in</strong>cardiovascular hemodynamics and <strong>in</strong> many of the modifiablecardiovascular risk factors <strong>for</strong> ASCVD and heart failure. Someprospective studies also <strong>in</strong>dicate that treatment of subcl<strong>in</strong>icalhypothyroidism, <strong>in</strong>clud<strong>in</strong>g groups with m<strong>in</strong>imally elevatedTSH levels, results <strong>in</strong> improvement <strong>in</strong> surrogate markers <strong>for</strong>ASCVD such as atherogenic lipids (120–123) and carotid <strong>in</strong>timamedia thickness (126).A meta-analysis of 10 longitud<strong>in</strong>al studies of subcl<strong>in</strong>icalhypothyroidism (119), which excluded patients with ASCVDat basel<strong>in</strong>e, showed a relative risk of CHD of 1.2 when allstudies were comb<strong>in</strong>ed. When only higher quality studieswere analyzed, the risk dropped to 1.02–1.08 depend<strong>in</strong>g onwhether the study design allowed <strong>for</strong> adjudicated outcomeswith or without knowledge of thyroid status. However, <strong>in</strong>studies with mean age younger than 65 years, the risk was1.51 compared with 1.05 <strong>in</strong> studies with a mean age of 65 andover. Another meta-analysis, also done <strong>in</strong> 2008, of 15 studieswith over 2500 participants with subcl<strong>in</strong>ical hypothyroidism,eight of which were also used <strong>in</strong> the a<strong>for</strong>ementioned metaanalysis,showed elevated odds ratios <strong>for</strong> the <strong>in</strong>cidence ofASCVD and cardiovascular all-cause mortality of 1.57 and1.37 <strong>for</strong> those under 65 years, but not <strong>for</strong> those over 65 years(292).A study from the Cleveland Cl<strong>in</strong>ic Preventive CardiologyCl<strong>in</strong>ic of patients at high risk <strong>for</strong> ASCVD showed that thosewith TSH levels of 6.1–10 mIU/L as well as greater than10mIU/Lwhowereunder65yearsandnottreatedwiththyroid hormone had higher all-cause mortality (118). Mostrecently a U.K. general practitioner database was analyzedto assess the impact of L-thyrox<strong>in</strong>e treatment on fatal andnonfatal cardiac events <strong>in</strong> over 3000 <strong>in</strong>dividuals with subcl<strong>in</strong>icalhypothyroidism (TSH between 5.01 and 10 mIU/L)aged between 40 and 70 years and over 1500 <strong>in</strong>dividualsolder than 70 years who were followed up <strong>for</strong> a medianof *8 years.Inthe*50% of <strong>in</strong>dividuals between 40 and 70years of age who were treated with L-thyrox<strong>in</strong>e (87.4%women) the hazard ratio <strong>for</strong> ischemic heart disease eventswas reduced compared to the *50% of untreated <strong>in</strong>dividuals(82.5% women) (0.61, CI 0.49–0.92). This reduction wasnot evident <strong>in</strong> those older than 70 years, of whom 84.6% <strong>in</strong>the treatment group and 75.6% <strong>in</strong> the untreated group werewomen (293).Yet other studies fail to show that an <strong>in</strong>creased risk ofcardiac disease <strong>in</strong> those with subcl<strong>in</strong>ical hypothyroidism isage dependent. The Cardiovascular Health Study followed3000 patients 65 years or older with subcl<strong>in</strong>ical hypothyroidismwho were <strong>in</strong>itially free of heart failure. Those withTSH levels of 10 mIU/L or greater had an <strong>in</strong>creased risk ofheart failure (294). Dur<strong>in</strong>g the 20 years of follow-up <strong>in</strong> theWhickham Survey, an association was found betweenASCVD and ASCVD-related mortality <strong>in</strong> those with subcl<strong>in</strong>icalhypothyroidism whose TSH values were between 6and 15 mIU/L <strong>in</strong>dependent of age. When those treated withL-thyrox<strong>in</strong>e were excluded, ASCVD-related morbidity andmortality were no longer evident (116). Additional large-scalestudies <strong>in</strong> those with serum TSH values of 10 mIU/L orgreater <strong>in</strong>clud<strong>in</strong>g a study of 11 prospective cohorts <strong>in</strong> theUnited States, Europe, Australia, Brazil, and Japan demonstratedan <strong>in</strong>crease <strong>in</strong> ASCVD that was <strong>in</strong>dependent of age(115) while a study of six prospective cohorts with over 2000patients had an <strong>in</strong>creased <strong>in</strong>cidence of heart failure <strong>in</strong> those upto 80 years of age (117).The absence of randomized prospective controlled trialsleaves us with several unresolved key issues perta<strong>in</strong><strong>in</strong>g tosubcl<strong>in</strong>ical hypothyroidism, <strong>in</strong>clud<strong>in</strong>g whether or not L-thyrox<strong>in</strong>e treatment will prevent the development of ASCVD
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1223or decrease the frequency of hospital admissions <strong>for</strong> heartfailure and whether age is a critical determ<strong>in</strong>ant of risk <strong>for</strong>cardiac morbidity. A prospective study to assess both of theseparameters is currently be<strong>in</strong>g planned.Cognitive benefit from treat<strong>in</strong>g subcl<strong>in</strong>icalhypothyroidismSome reports on mood, cognitive, and other objective bra<strong>in</strong>function studies <strong>in</strong> subcl<strong>in</strong>ical hypothyroidism demonstratethe presence and reversal of deficits after treatment with L-thyrox<strong>in</strong>e (295). However, other studies have not (296,297).L-thyrox<strong>in</strong>e and L-triiodothyron<strong>in</strong>e comb<strong>in</strong>ationtherapyAn important question is whether a recent study hadsufficient data to warrant revisit<strong>in</strong>g why some patientsseem to feel better on L-thyrox<strong>in</strong>e/L-triiodothyron<strong>in</strong>ecomb<strong>in</strong>ations and whether we can identify them and safelytreat them (136) with this comb<strong>in</strong>ation.L-triiodothyron<strong>in</strong>e monotherapyA potential role <strong>for</strong> L-triiodothyron<strong>in</strong>e monotherapy <strong>in</strong> lieuof L-thyrox<strong>in</strong>e monotherapy was recently raised by a smallrandomized, double-bl<strong>in</strong>d crossover <strong>in</strong>tervention study donecompar<strong>in</strong>g L-triiodothyron<strong>in</strong>e monotherapy with L-thyrox<strong>in</strong>emonotherapy <strong>in</strong> patients with hypothyroidism (298).Thrice daily dos<strong>in</strong>g was employed <strong>for</strong> each. Comparable TSHlevels were achieved. Mild weight loss and decreases <strong>in</strong> totalcholesterol, LDL cholesterol, and apolipoprote<strong>in</strong> levels wereseen without differences <strong>in</strong> cardiovascular function, <strong>in</strong>sul<strong>in</strong>sensitivity, or quality of life with L-triiodothyron<strong>in</strong>e monotherapycompared with L-thyrox<strong>in</strong>e monotherapy. The smallsize and short duration of the study as well as thrice dailydos<strong>in</strong>g presently precludes consider<strong>in</strong>g L-triiodothyron<strong>in</strong>emonotherapy as an alternative to L-thyrox<strong>in</strong>e monotherapy(298).Thyroid hormone analoguesThyroid hormone’s effects are protean, affect<strong>in</strong>g virtuallyevery organ system. Ef<strong>for</strong>ts are underway to develop andstudy analogues that have selective beneficial effects onweight control, lipoprote<strong>in</strong>s, and TSH suppression without<strong>in</strong>duc<strong>in</strong>g hypothyroidism or the most important negativeconsequences of hyperthyroidism on the heart and skeleton.Compounds studied to date <strong>in</strong>clude D-thyrox<strong>in</strong>e (299), tiratricol(275), eprotiromone (KB 2115) (300,301), and diodothyropropionicacid (302). A recent prospective Phase IIcl<strong>in</strong>ical trial of the thyroid hormone analogue eprotirome,designed to be a selective beta II receptor agonist, has beenshown to lower both total cholesterol and Lp(a) without anychange <strong>in</strong> thyroid hormone levels or untoward cardiovascularor bone effects (300). However, the development program <strong>for</strong>eprotirome has been discont<strong>in</strong>ued due to adverse f<strong>in</strong>d<strong>in</strong>gs <strong>in</strong>precl<strong>in</strong>ical studies. Further studies will be needed to confirmthe benefit and lack of side effects of these agents.Screen<strong>in</strong>g <strong>for</strong> hypothyroidism <strong>in</strong> pregnancyIt rema<strong>in</strong>s unclear if screen<strong>in</strong>g <strong>for</strong> hypothyroidism <strong>in</strong>pregnancy is beneficial. A consensus statement <strong>in</strong> 2004 (106)and cl<strong>in</strong>ical practice guidel<strong>in</strong>es <strong>in</strong> 2007 (303) and 2011 (10)found <strong>in</strong>sufficient data to support a 1999 (304) and restated2005 recommendation (305) <strong>for</strong> universal screen<strong>in</strong>g <strong>for</strong> thyroiddysfunction dur<strong>in</strong>g pregnancy, but rather recommendedaggressive case f<strong>in</strong>d<strong>in</strong>g.Arguments <strong>for</strong> screen<strong>in</strong>g <strong>in</strong>clude the follow<strong>in</strong>g: Limit<strong>in</strong>g evaluation to women <strong>in</strong> high-risk groupsmisses 30% of pregnant women with overt or subcl<strong>in</strong>icalhypothyroidism (306). A study compar<strong>in</strong>g universal screen<strong>in</strong>g to case f<strong>in</strong>d<strong>in</strong>gfound that there was a statistically significant difference<strong>in</strong> a composite endpo<strong>in</strong>t of adverse obstetric andneonatal outcomes associated with treatment of thyroiddysfunction <strong>in</strong> low-risk women who werescreened compared to those who were not (307). A cost-effectiveness model to evaluate universalscreen<strong>in</strong>g, which was predicated on the effectiveness ofthyroid hormone treatment <strong>in</strong> lower<strong>in</strong>g the <strong>in</strong>cidenceof offspr<strong>in</strong>g with <strong>in</strong>telligence quotient (IQ) < 85, concludedthat a random TSH done dur<strong>in</strong>g the first trimesterof pregnancy would ultimately save $84 perpregnancy (308). However, this has not been confirmedby a recent randomized controlled trial (219).However, questions rema<strong>in</strong> about the utility of screen<strong>in</strong>gthose at low risk <strong>for</strong> develop<strong>in</strong>g hypothyroidism (307) andwhether screen<strong>in</strong>g and <strong>in</strong>tervention earlier on <strong>in</strong> the first trimester(219) may be cost effective.The Controlled Antenatal Thyroid Study <strong>in</strong> the UnitedK<strong>in</strong>gdom and Italy exam<strong>in</strong>ed the impact at 3 years of age of L-thyrox<strong>in</strong>e treatment if free T 4 is below the 2.5th percentile or ifTSH is above the 97.5th percentile (219). Analyses failed todemonstrate a benefit when screen<strong>in</strong>g was per<strong>for</strong>med aroundthe end of the first trimester. Whether earlier <strong>in</strong>tervention,different cognitive test<strong>in</strong>g, or the same test<strong>in</strong>g per<strong>for</strong>med atage greater than 3 years would yield different results is uncerta<strong>in</strong>.‘‘A Randomized Trial of Thyrox<strong>in</strong>e Therapy <strong>for</strong> Subcl<strong>in</strong>ical<strong>Hypothyroidism</strong> or Hypothyrox<strong>in</strong>emia DiagnosedDur<strong>in</strong>g Pregnancy’’, done under the auspices of the NationalInstitute of Child Health and Human Development, is presentlystudy<strong>in</strong>g the IQ at 5 years of age follow<strong>in</strong>g a universalscreen<strong>in</strong>g versus case f<strong>in</strong>d<strong>in</strong>g program.Agents and conditions hav<strong>in</strong>g an impacton L-thyrox<strong>in</strong>e therapy and <strong>in</strong>terpretationof thyroid testsConditions such as pregnancy and malabsorption, drugs,diagnostic agents, dietary substances, and supplements canhave an impact on thyroid hormone economy, which mayor may not result <strong>in</strong> a change <strong>in</strong> thyroid status. For example,orally adm<strong>in</strong>istered estrogens <strong>in</strong>crease TBG levels. Whilethis does not alter thyroid status <strong>in</strong> euthyroid <strong>in</strong>dividualswith normal thyroid reserve, it may do so when there iseither marg<strong>in</strong>al thyroid reserve or established hypothyroidism.Drugs may have multiple effects on thyroidhormone metabolism. Notable examples <strong>in</strong>clude glucocorticoidsand amiodarone. In a number of cases, the mechanismsby which agents alter thyroid status are not known.The impact that an agent or condition has on thyroid statusmay require cl<strong>in</strong>icians to <strong>in</strong>crease monitor<strong>in</strong>g, adjust dosages,or <strong>in</strong>struct patients to change how and when they takeL-thyrox<strong>in</strong>e.
1224 GARBER ET AL.Major determ<strong>in</strong>ants of whether or not drugs and othersubstances will have an impact on thyroid status <strong>in</strong>clude thefollow<strong>in</strong>g: Dosage Duration of action Proximity to when thyroid hormone is taken Duration of treatment Iod<strong>in</strong>e content Organified Nonorganified Size of iod<strong>in</strong>e pool Autoimmune thyroid disease Nodular thyroid disease Thyroid hormone status Genetic factorsThe pr<strong>in</strong>cipal mechanisms and reasons that conditions,drugs, and other substances have an impact on thyroid statusare the follow<strong>in</strong>g: Effects on thyroid hormone metabolism:B AbsorptionB B<strong>in</strong>d<strong>in</strong>gB Peripheral metabolismB Clearance Direct and <strong>in</strong>direct effects on the hypothalamic–pituitary–thyroid axisB TSH secretionB Hypophysitis Direct and <strong>in</strong>direct effects on the thyroid glandB Iod<strong>in</strong>e uptakeB Hormone productionB Hormone secretion Thyroiditis (amelioration or development)B DestructiveB Autoimmune Amelioration or development of Graves’ diseaseTable 10 lists agents and some conditions that affect thyroidstatus—particularly if they are commonly used—and arelikely to do so or to have a profound impact on it. However,some very commonly used drugs such as sulfonylureas orsulfonamides or foodstuffs such as grapefruit juice that mayonly have a m<strong>in</strong>or impact have been <strong>in</strong>cluded. Because of theirpotential importance, some drugs, such as perchlorate, iopanoicacid, and ipodate, are also listed even though they are notgenerally available. On the other hand, some drugs that arerarely used have been omitted. Agents may appear more thanonce if there is more than one known mechanism of action. Acomprehensive review of this subject and references <strong>for</strong> eachdrug or condition is beyond the scope of these guidel<strong>in</strong>es. The<strong>in</strong>terested reader is encouraged to consult other sources <strong>for</strong>more <strong>in</strong><strong>for</strong>mation (309–311).ACKNOWLEDGMENTSWe thank Dr. Gilbert H. Daniels (Massachusetts GeneralHospital, Harvard Medical School, Boston, MA), Dr. Daniel S.Duick (Endocr<strong>in</strong>ology Associates P.A., Scottsdale, AZ, andCollege of Medic<strong>in</strong>e, University of Arizona, Phoenix andTucson, AZ), and Dr. Sheldon S. Stoffer (Endocr<strong>in</strong>e Consultant,William Beaumont Hospital, Oakland University WilliamBeaumont School of Medic<strong>in</strong>e, Oakland, CA) <strong>for</strong> theirthoughtful suggestions. Dr. Daniels reports that he has receivedconsultant fees from Genzyme Corporation. Dr. Duickreports that he has received speaker honoraria from AbbottLaboratories and consultant honoraria from Veracyte, Inc. andAsuragen, Inc. Dr. Stoffer reports that he does not have anyrelevant f<strong>in</strong>ancial relationships with any commercial <strong>in</strong>terests.AUTHOR DISCLOSURE STATEMENTJ.I.M. reports that he has received speaker and programdevelopment honoraria from Abbott Nutrition. J.R.G., R.H.C.,H.G., J.V.H., I.K., R.P.-P., P.A.S., and K.A.W. report that theydo not have any relevant f<strong>in</strong>ancial relationships with anycommercial <strong>in</strong>terests.REFERENCESNote: The authors’ EL rat<strong>in</strong>gs of the references are listed tothe right of each reference.1. S<strong>in</strong>ger PA, Cooper DS, Levy EG, Ladenson PW, EL4Braverman LE, Daniels G, Greenspan FS, McDougallIR, Nikolai TF 1995 Treatment guidel<strong>in</strong>es <strong>for</strong> patientswith hyperthyroidism and hypothyroidism.Standards of Care Committee, American ThyroidAssociation. JAMA 273:808–812.2. Bask<strong>in</strong>HJ,Cob<strong>in</strong>RH,DuickDS,GharibH,GuttlerRB, EL4Kaplan MM, Segal RL 2002 American Association of<strong>Cl<strong>in</strong>ical</strong> Endocr<strong>in</strong>ologists medical guidel<strong>in</strong>es <strong>for</strong> cl<strong>in</strong>icalpractice <strong>for</strong> the evaluation and treatment of hyperthyroidismand hypothyroidism. Endocr Pract 8:457–469.3. Garcia M, Bask<strong>in</strong> HJ, Feld S, Cob<strong>in</strong> RH, Daniels GH, EL4Davidson ET, Dickey RA, Janick JJ, Jell<strong>in</strong>ger PS, PriceWF, Rodbard HW 1995 American Association of<strong>Cl<strong>in</strong>ical</strong> Endocr<strong>in</strong>ologists cl<strong>in</strong>ical practice guidel<strong>in</strong>es<strong>for</strong> the evaluation and treatment of hyperthyroidismand hypothyroidism. Endocr Pract 1:54–62.4. Torres MS, Emerson CH 2011 Myxedema coma. In: EL4Irw<strong>in</strong> RS, Rippe JM (eds) Irw<strong>in</strong> & Rippe’s IntensiveCare Medic<strong>in</strong>e, 7th edition. Wolters Kluwer Health,Lippencott Williams and Wilk<strong>in</strong>s, Philadelphia, PA,pp 1055–1058.5. Mechanick JI, Camacho PM, Cob<strong>in</strong> RH, Garber AJ, EL4Garber JR, Gharib H, Petak SM, Rodbard HW,Trence DL 2010 American Association of <strong>Cl<strong>in</strong>ical</strong>Endocr<strong>in</strong>ologists protocol <strong>for</strong> standardized productionof cl<strong>in</strong>ical practice guidel<strong>in</strong>es—2010 update.Endocr Pract 16:270–283.6. Johnson N 1998 New approaches to the development EL4and use of treatment guidel<strong>in</strong>es. Formulary. Availableat www.highbeam.com/doc/1P3-32493644.html(accessed August 19, 2012).7. Mechanick JI, Kushner RF, Sugerman HJ, Gonzalez- EL4Campoy JM, Collazo-Clavell ML, Guven S, Spitz AF,Apovian CM, Liv<strong>in</strong>gston EH, Brol<strong>in</strong> R, Sarwer DB,Anderson WA, Dixon J 2008 American Associationof <strong>Cl<strong>in</strong>ical</strong> Endocr<strong>in</strong>ologists, The Obesity Society,and American Society <strong>for</strong> Metabolic & BariatricSurgery Medical guidel<strong>in</strong>es <strong>for</strong> cl<strong>in</strong>ical practice <strong>for</strong>the perioperative nutritional, metabolic, and nonsurgicalsupport of the bariatric surgery patient.Endocr Pract 14(Suppl 1): 1–83.8. Bahn Chair RS, Burch HB, Cooper DS, Garber JR,Greenlee MC, Kle<strong>in</strong> I, Laurberg P, McDougall IR,Montori VM, Rivkees SA, Ross DS, Sosa JA, Stan MN2011 Hyperthyroidism and other causes of thyrotox-EL4
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1225icosis: management guidel<strong>in</strong>es of the AmericanThyroid Association and American Association of<strong>Cl<strong>in</strong>ical</strong> Endocr<strong>in</strong>ologists. Thyroid 21:593–646.9. Bahn RS, Burch HB, Cooper DS, Garber JR, GreenleeMC, Kle<strong>in</strong> I, Laurberg P, McDougall IR, MontoriVM, Rivkees SA, Ross DS, Sosa JA, Stan MN 2011Hyperthyroidism and other causes of thyrotoxicosis:management guidel<strong>in</strong>es of the American ThyroidAssociation and American Association of <strong>Cl<strong>in</strong>ical</strong>Endocr<strong>in</strong>ologists. Endocr Pract 17:456–520.10. Stagnaro-Green A, Abalovich M, Alexander E, AziziF, Mestman J, Negro R, Nixon A, Pearce EN, Sold<strong>in</strong>OP, Sullivan S, Wiers<strong>in</strong>ga W 2011 <strong>Guidel<strong>in</strong>es</strong> of theAmerican Thyroid Association <strong>for</strong> the diagnosis andmanagement of thyroid disease dur<strong>in</strong>g pregnancyand postpartum. Thyroid 21:1081–1125.11. Hollowell JG, Staehl<strong>in</strong>g NW, Flanders WD, HannonWH, Gunter EW, Spencer CA, Braverman LE2002 Serum TSH, T(4), and thyroid antibodies <strong>in</strong>the United States population (1988 to 1994): NationalHealth and Nutrition Exam<strong>in</strong>ation Survey (NHANESIII). J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 87:489–499.12. Canaris GJ, Manowitz NR, Mayor G, Ridgway EC2000 The Colorado thyroid disease prevalence study.Arch Intern Med 160:526–534.13. Saw<strong>in</strong> CT, Castelli WP, Hershman JM, McNamara P,Bacharach P 1985 The ag<strong>in</strong>g thyroid. Thyroid deficiency<strong>in</strong> the Fram<strong>in</strong>gham Study. Arch Intern Med145:1386–1388.14. Vanderpump MP, Tunbridge WM, French JM, AppletonD, Bates D, Clark F, Grimley Evans J, HasanDM, Rodgers H, Tunbridge F, Young ET 1995 The<strong>in</strong>cidence of thyroid disorders <strong>in</strong> the community: atwenty-year follow-up of the Whickham Survey.Cl<strong>in</strong> Endocr<strong>in</strong>ol (Oxf ) 43:55–68.15. Vanderpump MP, Tunbridge WM 2002 Epidemiologyand prevention of cl<strong>in</strong>ical and subcl<strong>in</strong>ical hypothyroidism.Thyroid 12:839–847.16. Andersson M, de Benoist B, Delange F, Zupan J 2007Prevention and control of iod<strong>in</strong>e deficiency <strong>in</strong>pregnant and lactat<strong>in</strong>g women and <strong>in</strong> children lessthan 2-years-old: conclusions and recommendationsof the Technical Consultation. Public Health Nutr10:1606–1611.17. Nerup J 1974 Addison’s disease—cl<strong>in</strong>ical studies. Areport of 108 cases. Acta Endocr<strong>in</strong>ol (Copenh)76:127–141.18. Nerup J 1974 Addison’s disease—serological studies.Acta Endocr<strong>in</strong>ol (Copenh) 76:142–158.19. Heward J, Gough SC 1997 Genetic susceptibility tothe development of autoimmune disease. Cl<strong>in</strong> Sci(Lond) 93:479–491.20. Payami H, Joe S, Thomson G 1989 Autoimmunethyroid disease <strong>in</strong> type I diabetic families. GenetEpidemiol 6:137–141.21. Torfs CP, K<strong>in</strong>g MC, Huey B, Malmgren J, Grumet FC1986 Genetic <strong>in</strong>terrelationship between <strong>in</strong>sul<strong>in</strong>-dependentdiabetes mellitus, the autoimmune thyroiddiseases, and rheumatoid arthritis. Am J Hum Genet38:170–187.22. Walker DJ, Griffiths M, Griffiths ID 1986 Occurrenceof autoimmune diseases and autoantibodies <strong>in</strong>multicase rheumatoid arthritis families. Ann RheumDis 45:323–326.EL4EL4EL1EL1EL1EL2EL4EL4EL3EL3EL3EL3EL3EL323. Grennan DM, Dyer PA, Clague R, Dodds W,Smeaton I, Harris R 1983 Family studies <strong>in</strong> RA—theimportance of HLA-DR4 and of genes <strong>for</strong> autoimmunethyroid disease. J Rheumatol 10:584–589.24. Dittmar M, Kahaly GJ 2003 Polyglandular autoimmunesyndromes: immunogenetics and long-termfollow-up. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 88:2983–2992.25. Broadley SA, Deans J, Sawcer SJ, Clayton D,Compston DA 2000 Autoimmune disease <strong>in</strong> firstdegreerelatives of patients with multiple sclerosis. AUK survey. Bra<strong>in</strong> 123:1102–1111.26. Menconi F, Monti MC, Greenberg DA, Oashi T, OsmanR, Davies TF, Ban Y, Jacobson EM, ConcepcionES, Li CW, Tomer Y 2008 Molecular am<strong>in</strong>o acid signatures<strong>in</strong> the MHC class II peptide-b<strong>in</strong>d<strong>in</strong>g pocketpredispose to autoimmune thyroiditis <strong>in</strong> humans and<strong>in</strong> mice. Proc Natl Acad Sci USA 105:14034–14039.27. Ban Y, Greenberg DA, Davies TF, Jacobson E, ConcepcionE, Tomer Y 2008 L<strong>in</strong>kage analysis of thyroidantibody production: evidence <strong>for</strong> shared susceptibilityto cl<strong>in</strong>ical autoimmune thyroid disease. J Cl<strong>in</strong>Endocr<strong>in</strong>ol Metab 93:3589–3596.28. Huber G, Staub JJ, Meier C, Mitrache C, GuglielmettiM, Huber P, Braverman LE 2002 Prospective studyof the spontaneous course of subcl<strong>in</strong>ical hypothyroidism:prognostic value of thyrotrop<strong>in</strong>, thyroidreserve, and thyroid antibodies. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 87:3221–3226.29. Kubota S, Fujiwara M, Hagiwara H, Tsujimoto N,Takata K, Kudo T, Nishihara E, Ito M, Am<strong>in</strong>o N,Miyauchi A 2010 Multiple thyroid cysts may be acause of hypothyroidism <strong>in</strong> patients with relativelyhigh iod<strong>in</strong>e <strong>in</strong>take. Thyroid 20:205–208.30. Murdoch JC, Ratcliffe WA, McLarty DG, Rodger JC,Ratcliffe JG 1977 Thyroid function <strong>in</strong> adults withDown’s syndrome. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 44:453–458.31. Radetti G, Mazzanti L, Pagan<strong>in</strong>i C, Bernasconi S,Russo G, Rigon F, Cacciari E 1995 Frequency, cl<strong>in</strong>icaland laboratory features of thyroiditis <strong>in</strong> girls withTurner’s syndrome. The Italian Study Group <strong>for</strong>Turner’s Syndrome. Acta Paediatr 84:909–912.32. Burrow GN, Burke WR, Himmelhoch JM, SpencerRP, Hershman JM 1971 Effect of lithium on thyroidfunction. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 32:647–652.33. Bennie EH, Lazarus JH 1972 Lithium-<strong>in</strong>duced thyroiddysfunction. Lancet 2:44–45.34. Emerson CH, Dysno WL, Utiger RD 1973 Serumthyrotrop<strong>in</strong> and thyrox<strong>in</strong>e concentrations <strong>in</strong> patientsreceiv<strong>in</strong>g lithium carbonate. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab36:338–346.35. Fentiman IS, Thomas BS, Balkwill FR, Rubens RD,Hayward JL 1985 Primary hypothyroidism associatedwith <strong>in</strong>terferon therapy of breast cancer. Lancet1:1166.36. Preziati D, La Rosa L, Cov<strong>in</strong>i G, Marcelli R, RescalliS, Persani L, Del N<strong>in</strong>no E, Meroni PL, Colombo M,Beck-Peccoz P 1995 Autoimmunity and thyroidfunction <strong>in</strong> patients with chronic active hepatitistreated with recomb<strong>in</strong>ant <strong>in</strong>terferon alpha-2a. Eur JEndocr<strong>in</strong>ol 132:587–593.37. Mart<strong>in</strong>o E, Bartalena L, Bogazzi F, Braverman LE2001 The effects of amiodarone on the thyroid. EndocrRev 22:240–254.EL3EL2EL3EL3EL3EL2EL3EL3EL3EL3EL4EL2EL4EL2EL4
1226 GARBER ET AL.38. Clark CD, Bassett B, Burge MR 2003 Effects of kelpsupplementation on thyroid function <strong>in</strong> euthyroidsubjects. Endocr Pract 9:363–369.39. Braverman LE, Ingbar SH, Vagenakis AG, Adams L,Maloof F 1971 Enhanced susceptibility to iodidemyxedema <strong>in</strong> patients with Hashimoto’s disease. JCl<strong>in</strong> Endocr<strong>in</strong>ol Metab 32:515–521.40. Braverman LE, Vagenakis AG, Wang CA, Maloof F,Ingbar SH 1971 Studies on the pathogenesis of iodidemyxedema. Trans Assoc Am Physicians 84:130–138.41. Morshed SA, Latif R, Davies TF 2009 Characterizationof thyrotrop<strong>in</strong> receptor antibody-<strong>in</strong>duced signal<strong>in</strong>gcascades. Endocr<strong>in</strong>ology 150:519–529.42. Fu J, Jiang Y, Liang L, Zhu H 2005 Risk factors ofprimary thyroid dysfunction <strong>in</strong> early <strong>in</strong>fants born tomothers with autoimmune thyroid disease. ActaPaediatr 94:1043–1048.43. Laurberg P, Nygaard B, Gl<strong>in</strong>oer D, Grussendorf M,Orgiazzi J 1998 <strong>Guidel<strong>in</strong>es</strong> <strong>for</strong> TSH-receptor antibodymeasurements <strong>in</strong> pregnancy: results of an evidencebasedsymposium organized by the European ThyroidAssociation. Eur J Endocr<strong>in</strong>ol 139:584–586.44. Kappers MH, van Esch JH, Smedts FM, de KrijgerRR, Eechoute K, Mathijssen RH, Sleijfer S, Leijten F,Danser AH, van den Meiracker AH, Visser TJ 2011Sunit<strong>in</strong>ib-<strong>in</strong>duced hypothyroidism is due to <strong>in</strong>ductionof type 3 deiod<strong>in</strong>ase activity and thyroidalcapillary regression. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab96:3087–3094.45. Desai J, Yassa L, Marqusee E, George S, Frates MC,Chen MH, Morgan JA, Dychter SS, Larsen PR, DemetriGD, Alexander EK 2006 <strong>Hypothyroidism</strong> aftersunit<strong>in</strong>ib treatment <strong>for</strong> patients with gastro<strong>in</strong>test<strong>in</strong>alstromal tumors. Ann Intern Med 145:660–664.46. Utiger RD 1965 Radioimmunoassay of human plasmathyrotrop<strong>in</strong>. J Cl<strong>in</strong> Invest 44:1277–1286.47. Beck-Peccoz P, Amr S, Menezes-Ferreira MM, FagliaG, We<strong>in</strong>traub BD 1985 Decreased receptor b<strong>in</strong>d<strong>in</strong>gof biologically <strong>in</strong>active thyrotrop<strong>in</strong> <strong>in</strong> central hypothyroidism.Effect of treatment with thyrotrop<strong>in</strong>-releas<strong>in</strong>ghormone. N Engl J Med 312:1085–1090.48. Huang SA, Fish SA, Dorfman DM, Salvatore D,Kozakewich HP, Mandel SJ, Larsen PR 2002 A 21-year-old woman with consumptive hypothyroidismdue to a vascular tumor express<strong>in</strong>g type 3 iodothyron<strong>in</strong>edeiod<strong>in</strong>ase. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab87:4457–4461.49. Mouat F, Evans HM, Cutfield WS, Hofman PL,Jefferies C 2008 Massive hepatic hemangioendotheliomaand consumptive hypothyroidism. J PediatrEndocr<strong>in</strong>ol Metab 21:701–703.50. Matsuzuka F, Miyauchi A, Katayama S, NarabayashiI, Ikeda H, Kuma K, Sugawara M 1993 <strong>Cl<strong>in</strong>ical</strong>aspects of primary thyroid lymphoma: diagnosisand treatment based on our experience of 119 cases.Thyroid 3:93–99.51. Bjorses P, Aaltonen J, Horelli-Kuitunen N, Yaspo ML,Peltonen L 1998 Gene defect beh<strong>in</strong>d APECED: a newclue to autoimmunity. Hum Mol Genet 7:1547–1553.52. Meloni A, Furcas M, Cetani F, Marcocci C, Falorni A,Perniola R, Pura M, Boe Wolff AS, Husebye ES, LilicD, Ryan KR, Gennery AR, Cant AJ, Ab<strong>in</strong>un M,Spickett GP, Arkwright PD, Denn<strong>in</strong>g D, Costigan C,EL3EL3EL3EL3EL2EL4EL2EL3EL1EL2EL3EL3EL3EL4EL2Dom<strong>in</strong>guez M, McConnell V, Willcox N, Meager A2008 Autoantibodies aga<strong>in</strong>st type I <strong>in</strong>terferons as anadditional diagnostic criterion <strong>for</strong> autoimmunepolyendocr<strong>in</strong>e syndrome type I. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 93:4389–4397.53. Huber A, Menconi F, Corathers S, Jacobson EM,Tomer Y 2008 Jo<strong>in</strong>t genetic susceptibility to type 1diabetes and autoimmune thyroiditis: from epidemiologyto mechanisms. Endocr Rev 29:697–725.54. Stryker TD, Molitch ME 1985 Reversible hyperthyrotrop<strong>in</strong>emia,hyperthyrox<strong>in</strong>emia, and hyperprolact<strong>in</strong>emiadue to adrenal <strong>in</strong>sufficiency. Am J Med79:271–276.55. Abdullatif HD, Ashraf AP 2006 Reversible subcl<strong>in</strong>icalhypothyroidism <strong>in</strong> the presence of adrenal <strong>in</strong>sufficiency.Endocr Pract 12:572.56. Canaris GJ, Ste<strong>in</strong>er JF, Ridgway EC 1997 Do traditionalsymptoms of hypothyroidism correlate withbiochemical disease? J Gen Intern Med 12:544–550.57. Birkent H, Karacalioglu O, Merati AL, Akcam T,Gerek M 2008 Prospective study of the impact ofthyroid hormone replacement on objective voiceparameters. Ann Otol Rh<strong>in</strong>ol Laryngol 117:523–527.58. Billewicz WZ, Chapman RS, Crooks J, Day ME,Gossage J, Wayne E, Young JA 1969 Statisticalmethods applied to the diagnosis of hypothyroidism.Q J Med 38:255–266.59. Zulewski H, Muller B, Exer P, Miserez AR, Staub JJ1997 Estimation of tissue hypothyroidism by a newcl<strong>in</strong>ical score: evaluation of patients with variousgrades of hypothyroidism and controls. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 82:771–776.60. Lambert EH, Underdahl LO, Beckett S, Mederos LO1951 A study of the ankle jerk <strong>in</strong> myxedema. J Cl<strong>in</strong>Endocr<strong>in</strong>ol Metab 11:1186–1205.61. Bell GM, Todd WT, Forfar JC, Martyn C, WathenCG, Gow S, Riemersma R, Toft AD 1985 End-organresponses to thyrox<strong>in</strong>e therapy <strong>in</strong> subcl<strong>in</strong>ical hypothyroidism.Cl<strong>in</strong> Endocr<strong>in</strong>ol (Oxf ) 22:83–89.62. Mason RL, Hunt HM, Hurxthal, LM 1930 Blood cholesterolvalues <strong>in</strong> hyperthyroidism and hypothyroidism:their significance. N Engl J Med 203:1273–1278.63. Ha<strong>in</strong>es AL, Mussey RD 1935 Certa<strong>in</strong> menstrualdisturbances associated with low basal metabolicrates without myxedema. JAMA 105:557–560.64. Foster RC, Thornton, MJ 1939 Thyroid <strong>in</strong> the treatmentof menstrual irregularities. Endocr<strong>in</strong>ology24.383–388.65. Goldsmith RE, Sturgis SH, Lerman J, Stanbury JB1952 The menstrual pattern <strong>in</strong> thyroid disease. J Cl<strong>in</strong>Endocr<strong>in</strong>ol Metab 12:846–855.66. Kle<strong>in</strong> I, Mantell P, Parker M, Levey GS 1980 Resolutionof abnormal muscle enzyme studies <strong>in</strong> hypothyroidism.Am J Med Sci 279:159–162.67. Tajiri J, Shimada T, Naomi S, Umeda T, Sato T 1984Hepatic dysfunction <strong>in</strong> primary hypothyroidism.Endocr<strong>in</strong>ol Jpn 31:83–91.68. Surks MI, Sievert R 1995 Drugs and thyroid function.N Engl J Med 333:1688–1694.69. Oppenheimer JH, Squef R, Surks MI, Hauer H 1963B<strong>in</strong>d<strong>in</strong>g of thyrox<strong>in</strong>e by serum prote<strong>in</strong>s evaluated byequilibrium dialysis and electrophoretic techniques.Alterations <strong>in</strong> nonthyroidal illness. J Cl<strong>in</strong> Invest42:1769–1782.EL4EL3EL3EL3EL2EL3EL3EL3EL2EL3EL3EL3EL3EL3EL3EL4EL1
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 122770. Mendel CM 1989 The free hormone hypothesis: aphysiologically based mathematical model. EndocrRev 10:232–274.71. Stockigt JR 2001 Free thyroid hormone measurement.A critical appraisal. Endocr<strong>in</strong>ol Metab Cl<strong>in</strong>North Am 30:265–289.72. A<strong>in</strong> KB, Puc<strong>in</strong>o F, Shiver TM, Banks SM 1993Thyroid hormone levels affected by time of bloodsampl<strong>in</strong>g <strong>in</strong> thyrox<strong>in</strong>e-treated patients. Thyroid3:81–85.73. Lee RH, Spencer CA, Mestman JH, Miller EA, PetrovicI, Braverman LE, Goodw<strong>in</strong> TM 2009 Free T4immunoassays are flawed dur<strong>in</strong>g pregnancy. Am JObstet Gynecol 200:260 e261–266.74. Mandel SJ, Spencer CA, Hollowell JG 2005 Are detectionand treatment of thyroid <strong>in</strong>sufficiency <strong>in</strong>pregnancy feasible? Thyroid 15:44–53.75. Lum SM, Nicoloff JT, Spencer CA, Kapte<strong>in</strong> EM 1984Peripheral tissue mechanism <strong>for</strong> ma<strong>in</strong>tenance of serumtriiodothyron<strong>in</strong>e values <strong>in</strong> a thyrox<strong>in</strong>e-deficientstate <strong>in</strong> man. J Cl<strong>in</strong> Invest 73:570–575.76. Kaplan MM, Larsen PR, Crantz FR, Dzau VJ, Ross<strong>in</strong>gTH, Haddow JE 1982 Prevalence of abnormalthyroid function test results <strong>in</strong> patients with acutemedical illnesses. Am J Med 72:9–16.77. Peeters RP, Wouters PJ, Kapte<strong>in</strong> E, van Toor H,Visser TJ, Van den Berghe G 2003 Reduced activationand <strong>in</strong>creased <strong>in</strong>activation of thyroid hormone<strong>in</strong> tissues of critically ill patients. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 88:3202–3211.78. Caron PJ, Nieman LK, Rose SR, Nisula BC 1986 Deficientnocturnal surge of thyrotrop<strong>in</strong> <strong>in</strong> central hypothyroidism.J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 62:960–964.79. Karmisholt J, Andersen S, Laurberg P 2008 Variation<strong>in</strong> thyroid function tests <strong>in</strong> patients with stable untreatedsubcl<strong>in</strong>ical hypothyroidism. Thyroid 18:303–308.80. Spencer CA, LoPresti JS, Patel A, Guttler RB, EigenA, Shen D, Gray D, Nicoloff JT 1990 Applications ofa new chemilum<strong>in</strong>ometric thyrotrop<strong>in</strong> assay tosubnormal measurement. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab70:453–460.81. Hamilton TE, Davis S, Onstad L, Kopecky KJ 2008Thyrotrop<strong>in</strong> levels <strong>in</strong> a population with no cl<strong>in</strong>ical,autoantibody, or ultrasonographic evidence of thyroiddisease: implications <strong>for</strong> the diagnosis of subcl<strong>in</strong>icalhypothyroidism. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab93:1224–1230.82. Volzke H, Alte D, Kohlmann T, Ludemann J, NauckM, John U, Meng W 2005 Reference <strong>in</strong>tervals of serumthyroid function tests <strong>in</strong> a previously iod<strong>in</strong>edeficientarea. Thyroid 15:279–285.83. Volzke H, Schmidt CO, John U, Wallaschofski H,Dorr M, Nauck M 2010 Reference levels <strong>for</strong> serumthyroid function tests of diagnostic and prognosticsignificance. Horm Metab Res 42:809–814.84. Boucai L, Hollowell JG, Surks MI 2011 An approach<strong>for</strong> development of age-, gender-, and ethnicityspecificthyrotrop<strong>in</strong> reference limits. Thyroid 21:5–11.85. Baloch Z, Carayon P, Conte-Devolx B, Demers LM,Feldt-Rasmussen U, Henry JF, LiVosli VA, Niccoli-Sire P, John R, Ruf J, Smyth PP, Spencer CA, StockigtJR 2003 Laboratory medic<strong>in</strong>e practice guidel<strong>in</strong>es.EL4EL4EL3EL2EL4EL3EL2EL3EL3EL2EL3EL1EL2EL2EL1EL4Laboratory support <strong>for</strong> the diagnosis and monitor<strong>in</strong>gof thyroid disease. Thyroid 13:3–126.86. Wartofsky L, Dickey RA 2005 The evidence <strong>for</strong> anarrower thyrotrop<strong>in</strong> reference range is compell<strong>in</strong>g.J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 90:5483–5488.87. Surks MI, Goswami G, Daniels GH 2005 The thyrotrop<strong>in</strong>reference range should rema<strong>in</strong> unchanged. JCl<strong>in</strong> Endocr<strong>in</strong>ol Metab 90:5489–5496.88. Surks MI, Hollowell JG 2007 Age-specific distributionof serum thyrotrop<strong>in</strong> and antithyroid antibodies<strong>in</strong> the US population: implications <strong>for</strong> the prevalenceof subcl<strong>in</strong>ical hypothyroidism. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 92:4575–4582.89. Kapte<strong>in</strong> EM, Spencer CA, Kamiel MB, Nicoloff JT1980 Prolonged dopam<strong>in</strong>e adm<strong>in</strong>istration and thyroidhormone economy <strong>in</strong> normal and critically illsubjects. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 51:387–393.90. Sowers JR, Carlson HE, Brautbar N, Hershman JM1977 Effect of dexamethasone on prolact<strong>in</strong> and TSHresponses to TRH and metoclopramide <strong>in</strong> man. JCl<strong>in</strong> Endocr<strong>in</strong>ol Metab 44:237–241.91. Wong ET, Bradley SG, Schultz AL 1981 Elevations ofthyroid-stimulat<strong>in</strong>g hormone dur<strong>in</strong>g acute nonthyroidalillness. Arch Intern Med 141:873–875.92. Lightman SL, Fox P, Dunne MJ 1986 The effect ofSMS 201–995, a long-act<strong>in</strong>g somatostat<strong>in</strong> analogue,on anterior pituitary function <strong>in</strong> healthy male volunteers.Scand J Gastroenterol Suppl 119:84–95.93. Sherman SI, Gopal J, Haugen BR, Chiu AC, WhaleyK, Nowlakha P, Duvic M 1999 Central hypothyroidismassociated with ret<strong>in</strong>oid X receptor-selectiveligands. N Engl J Med 340:1075–1079.94. Lawson EA, Klibanski A 2008 Endocr<strong>in</strong>e abnormalities<strong>in</strong> anorexia nervosa. Nat Cl<strong>in</strong> Pract Endocr<strong>in</strong>olMetab 4:407–414.95. Gershengorn MC, We<strong>in</strong>traub BD 1975 Thyrotrop<strong>in</strong><strong>in</strong>ducedhyperthyroidism caused by selective pituitaryresistance to thyroid hormone. A new syndromeof ‘‘<strong>in</strong>appropriate secretion of TSH’’. J Cl<strong>in</strong>Invest 56:633–642.96. Halsall DJ, English E, Chatterjee VK 2009 Interferencefrom heterophilic antibodies <strong>in</strong> TSH assays.Ann Cl<strong>in</strong> Biochem 46:345–346.97. Boothby WM, Sandi<strong>for</strong>d I 1929 Normal values ofbasal or standard metabolism. A modification of theDubois standards. Am J Physiol 90:290–291.98. Werner SC 1955 Basal metabolism. In: Werner SC(ed) The Thyroid: A Fundamental and <strong>Cl<strong>in</strong>ical</strong>Text. First edition. Harper & Brothers, New York,pp 125–136.99. Tunbridge WM, Evered DC, Hall R, Appleton D,Brewis M, Clark F, Evans JG, Young E, Bird T, SmithPA 1977 The spectrum of thyroid disease <strong>in</strong> a community:the Whickham survey. Cl<strong>in</strong> Endocr<strong>in</strong>ol(Oxf ) 7:481–493.100. de Bru<strong>in</strong> TW, van Barl<strong>in</strong>gen H, van L<strong>in</strong>de-SibeniusTrip M, van Vuurst de Vries AR, Akveld MJ, ErkelensDW 1993 Lipoprote<strong>in</strong>(a) and apolipoprote<strong>in</strong> Bplasma concentrations <strong>in</strong> hypothyroid, euthyroid,and hyperthyroid subjects. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab76:121–126.101. Danese MD, Ladenson PW, Me<strong>in</strong>ert CL, Powe NR2000 <strong>Cl<strong>in</strong>ical</strong> review 115: effect of thyrox<strong>in</strong>e therapyon serum lipoprote<strong>in</strong>s <strong>in</strong> patients with mild thyroidEL4EL4EL1EL2EL2EL3EL2EL3EL3EL3EL4EL3EL4EL1EL3EL4
1228 GARBER ET AL.failure: a quantitative review of the literature. J Cl<strong>in</strong>Endocr<strong>in</strong>ol Metab 85:2993–3001.102. Ness-Abramof R, Nabriski DA, Shapiro MS, Tripto-Shkolnik L, Katz B, Weiss E, Shenkman L 2009Cardiac tropon<strong>in</strong> T is not <strong>in</strong>creased <strong>in</strong> patients withhypothyroidism. Intern Med J 39:117–120.103. Ladenson PW, S<strong>in</strong>ger PA, A<strong>in</strong> KB, Bagchi N, Bigos ST,Levy EG, Smith SA, Daniels GH, Cohen HD 2000American Thyroid Association guidel<strong>in</strong>es <strong>for</strong> detectionof thyroid dysfunction.ArchInternMed160:1573–1575.104. American Academy of Family Physicians 2002Summary of policy recommendations <strong>for</strong> periodichealth exam<strong>in</strong>ations. American Academy of FamilyPhysicians: Leawood, KS.105. Helfand M, Redfern CC 1998 <strong>Cl<strong>in</strong>ical</strong> guidel<strong>in</strong>e, part2. Screen<strong>in</strong>g <strong>for</strong> thyroid disease: an update. AmericanCollege of Physicians. Ann Intern Med 129:144–158.106. Surks MI, Ortiz E, Daniels GH, Saw<strong>in</strong> CT, Col NF,Cob<strong>in</strong> RH, Franklyn JA, Hershman JM, Burman KD,Denke MA, Gorman C, Cooper RS, Weissman NJ2004 Subcl<strong>in</strong>ical thyroid disease: scientific reviewand guidel<strong>in</strong>es <strong>for</strong> diagnosis and management.JAMA 291:228–238.107. Vanderpump MP, Ahlquist JA, Franklyn JA, ClaytonRN 1996 Consensus statement <strong>for</strong> good practice andaudit measures <strong>in</strong> the management of hypothyroidismand hyperthyroidism. The Research Unit ofthe Royal College of Physicians of London, the Endocr<strong>in</strong>ologyand Diabetes Committee of the RoyalCollege of Physicians of London, and the Society <strong>for</strong>Endocr<strong>in</strong>ology. BMJ 313:539–544.108. Helfand M 2004 Screen<strong>in</strong>g <strong>for</strong> subcl<strong>in</strong>ical thyroiddysfunction <strong>in</strong> nonpregnant adults: a summary ofthe evidence <strong>for</strong> the U.S. Preventive Services TaskForce. Ann Intern Med 140:128–141.109. Tudhope GR, Wilson GM 1962 Deficiency of vitam<strong>in</strong>B12 <strong>in</strong> hypothyroidism. Lancet 1:703–706.110. Carmel R, Spencer CA 1982 <strong>Cl<strong>in</strong>ical</strong> and subcl<strong>in</strong>icalthyroid disorders associated with pernicious anemia.Observations on abnormal thyroid-stimulat<strong>in</strong>g hormonelevels and on a possible association of bloodgroup O with hyperthyroidism. Arch Intern Med142:1465–1469.111. Glatste<strong>in</strong> E, McHardy-Young S, Brast N, Eltr<strong>in</strong>ghamJR, Kriss JP 1971 Alterations <strong>in</strong> serum thyrotrop<strong>in</strong>(TSH) and thyroid function follow<strong>in</strong>g radiotherapy<strong>in</strong> patients with malignant lymphoma. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 32:833–841.112. Const<strong>in</strong>e LS, Donaldson SS, McDougall IR, Cox RS,L<strong>in</strong>k MP, Kaplan HS 1984 Thyroid dysfunction afterradiotherapy <strong>in</strong> children with Hodgk<strong>in</strong>’s disease.Cancer 53:878–883.113. Lien<strong>in</strong>g DA, Duncan NO, Blakeslee DB, Smith DB1990 <strong>Hypothyroidism</strong> follow<strong>in</strong>g radiotherapy <strong>for</strong>head and neck cancer. Otolaryngol Head Neck Surg103:10–13.114. Hennessey JV, Jackson IMD. 1996 The <strong>in</strong>terface betweenthyroid hormones and psychiatry. Endocr<strong>in</strong>ologist6:214–223.115. Rodondi N, den Elzen WP, Bauer DC, Cappola AR,Razvi S, Walsh JP, Asvold BO, Iervasi G, ImaizumiM, Collet TH, Bremner A, Maisonneuve P, Sgarbi JA,Khaw KT, Vanderpump MP, Newman AB, CornuzJ, Franklyn JA, Westendorp RG, Vitt<strong>in</strong>ghoff E, Gus-EL3EL4EL4EL4EL4EL4EL4EL3EL3EL3EL3EL3EL4EL2sekloo J 2010 Subcl<strong>in</strong>ical hypothyroidism and therisk of coronary heart disease and mortality. JAMA304:1365–1374.116. Razvi S, Weaver JU, Vanderpump MP, Pearce SH2010 The <strong>in</strong>cidence of ischemic heart disease andmortality <strong>in</strong> people with subcl<strong>in</strong>ical hypothyroidism:reanalysis of the Whickham Survey cohort. J Cl<strong>in</strong>Endocr<strong>in</strong>ol Metab 95:1734–1740.117. Gencer B, Collet TH, Virg<strong>in</strong>i V, Bauer DC, GusseklooJ, Cappola AR, Nanchen D, den Elzen WP, Balmer P,Luben RN, Iacoviello M, Triggiani V, Cornuz J,Newman AB, Khaw KT, Jukema JW, WestendorpRG, Vitt<strong>in</strong>ghoff E, Aujesky D, Rodondi N 2012Subcl<strong>in</strong>ical thyroid dysfunction and the risk of heartfailure events: an <strong>in</strong>dividual participant data analysisfrom six prospective cohorts. Circulation126:1040–1049.118. McQuade C, Skugor M, Brennan DM, Hoar B, StevensonC, Hoogwerf BJ 2011 <strong>Hypothyroidism</strong> andmoderate subcl<strong>in</strong>ical hypothyroidism are associatedwith <strong>in</strong>creased all-cause mortality <strong>in</strong>dependent ofcoronary heart disease risk factors: a PreCIS databasestudy. Thyroid 21:837–843.119. Ochs N, Auer R, Bauer DC, Nanchen D, GusseklooJ, Cornuz J, Rodondi N 2008 Meta-analysis: subcl<strong>in</strong>icalthyroid dysfunction and the risk <strong>for</strong> coronaryheart disease and mortality. Ann Intern Med148:832–845.120. Desse<strong>in</strong> PH, Joffe BI, Stanwix AE 2004 Subcl<strong>in</strong>icalhypothyroidism is associated with <strong>in</strong>sul<strong>in</strong> resistance<strong>in</strong> rheumatoid arthritis. Thyroid 14:443–446.121. Serter R, Demirbas B, Korukluoglu B, Culha C, CakalE, Aral Y 2004 The effect of L-thyrox<strong>in</strong>e replacementtherapy on lipid based cardiovascular risk <strong>in</strong> subcl<strong>in</strong>icalhypothyroidism. J Endocr<strong>in</strong>ol Invest 27:897–903.122. Iqbal A, Jorde R, Figenschau Y 2006 Serum lipidlevels <strong>in</strong> relation to serum thyroid-stimulat<strong>in</strong>g hormoneand the effect of thyrox<strong>in</strong>e treatment on serumlipid levels <strong>in</strong> subjects with subcl<strong>in</strong>ical hypothyroidism:the Tromso Study. J Intern Med 260:53–61.123. Caraccio N, Ferrann<strong>in</strong>i E, Monzani F 2002 Lipoprote<strong>in</strong>profile <strong>in</strong> subcl<strong>in</strong>ical hypothyroidism: responseto levothyrox<strong>in</strong>e replacement, a randomized placebo-controlledstudy. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 87:1533–1538.124. Taddei S, Caraccio N, Virdis A, Dardano A, VersariD, Ghiadoni L, Salvetti A, Ferrann<strong>in</strong>i E, Monzani F2003 Impaired endothelium-dependent vasodilatation<strong>in</strong> subcl<strong>in</strong>ical hypothyroidism: beneficial effectof levothyrox<strong>in</strong>e therapy. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab88:3731–3737.125. Dardano A, Caraccio N, Monzani F 2006 Evaluationof endothelial function <strong>in</strong> subcl<strong>in</strong>ical thyroid dysfunction.Thyroid 16:200–201.126. Dardano A, Monzani F 2007 Thyroid function andcarotid artery <strong>in</strong>tima-media thickness. Circ J 71:993.127. Negro R, Schwartz A, Gismondi R, T<strong>in</strong>elli A, MangieriT, Stagnaro-Green A 2010 Increased pregnancyloss rate <strong>in</strong> thyroid antibody negative women withTSH levels between 2.5 and 5.0 <strong>in</strong> the first trimesterof pregnancy. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 95:E44–48.128. Braverman LE, Ingbar SH, Sterl<strong>in</strong>g K 1970 Conversionof thyrox<strong>in</strong>e (T4) to triiodothyron<strong>in</strong>e (T3) <strong>in</strong>athyreotic human subjects. J Cl<strong>in</strong> Invest 49:855–864.EL3EL1EL3EL1EL3EL2EL1EL2EL3EL4EL4EL2EL1
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1229129. Petersen K, Bengtsson C, Lapidus L, L<strong>in</strong>dstedt G,Nystrom E 1990 Morbidity, mortality, and quality oflife <strong>for</strong> patients treated with levothyrox<strong>in</strong>e. ArchIntern Med 150:2077–2081.130. Jonklaas J, Davidson B, Bhagat S, Sold<strong>in</strong> SJ 2008Triiodothyron<strong>in</strong>e levels <strong>in</strong> athyreotic <strong>in</strong>dividualsdur<strong>in</strong>g levothyrox<strong>in</strong>e therapy. JAMA 299:769–777.131. Saravanan P, Chau WF, Roberts N, Vedhara K,Greenwood R, Dayan CM 2002 Psychological wellbe<strong>in</strong>g<strong>in</strong> patients on ‘adequate’ doses of l-thyrox<strong>in</strong>e:results of a large, controlled community-based questionnairestudy. Cl<strong>in</strong> Endocr<strong>in</strong>ol (Oxf ) 57:577–585.132. Bunevicius R, Kazanavicius G, Zal<strong>in</strong>kevicius R,Prange AJ Jr 1999 Effects of thyrox<strong>in</strong>e as comparedwith thyrox<strong>in</strong>e plus triiodothyron<strong>in</strong>e <strong>in</strong> patientswith hypothyroidism. N Engl J Med 340:424–429.133. Escobar-Morreale HF, Botella-Carretero JI, Escobardel Rey F, Morreale de Escobar G 2005 REVIEW:Treatment of hypothyroidism with comb<strong>in</strong>ations oflevothyrox<strong>in</strong>e plus liothyron<strong>in</strong>e. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 90:4946–4954.134. Groz<strong>in</strong>sky-Glasberg S, Fraser A, Nahshoni E, WeizmanA, Leibovici L 2006 Thyrox<strong>in</strong>e-triiodothyron<strong>in</strong>ecomb<strong>in</strong>ation therapy versus thyrox<strong>in</strong>e monotherapy<strong>for</strong> cl<strong>in</strong>ical hypothyroidism: meta-analysis of randomizedcontrolled trials. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab91:2592–2599.135. Celi FS, Zemskova M, L<strong>in</strong>derman JD, Babar NI,Skarulis MC, Csako G, Wesley R, Costello R, PenzakSR, Puc<strong>in</strong>o F 2010 The pharmacodynamic equivalenceof levothyrox<strong>in</strong>e and liothyron<strong>in</strong>e: a randomized,double bl<strong>in</strong>d, cross-over study <strong>in</strong> thyroidectomizedpatients. Cl<strong>in</strong> Endocr<strong>in</strong>ol (Oxf ) 72:709–715.136. Panicker V, Saravanan P, Vaidya B, Evans J, HattersleyAT, Frayl<strong>in</strong>g TM, Dayan CM 2009 Commonvariation <strong>in</strong> the DIO2 gene predicts basel<strong>in</strong>e psychologicalwell-be<strong>in</strong>g and response to comb<strong>in</strong>ationthyrox<strong>in</strong>e plus triiodothyron<strong>in</strong>e therapy <strong>in</strong> hypothyroidpatients. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 94:1623–1629.137. Appelhof BC, Peeters RP, Wiers<strong>in</strong>ga WM, Visser TJ,Wekk<strong>in</strong>g EM, Huyser J, Schene AH, Tijssen JG,Hoogendijk WJ, Fliers E 2005 Polymorphisms <strong>in</strong> type2 deiod<strong>in</strong>ase are not associated with well-be<strong>in</strong>g,neurocognitive function<strong>in</strong>g, and preference <strong>for</strong> comb<strong>in</strong>edthyrox<strong>in</strong>e/3,5,3¢-triiodothyron<strong>in</strong>e therapy.J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 90:6296–6299.138. Hennessey JV, Malabanan AO, Haugen BR, Levy EG2010 Adverse event report<strong>in</strong>g <strong>in</strong> patients treated withlevothyrox<strong>in</strong>e: results of the pharmacovigilance task<strong>for</strong>ce survey of the American Thyroid Association,American Association of <strong>Cl<strong>in</strong>ical</strong> Endocr<strong>in</strong>ologists,and the Endocr<strong>in</strong>e Society. Endocr Pract 16:357–370.139. AACE, TES and ATA Jo<strong>in</strong>t position statement on theuse and <strong>in</strong>terchangeability of thyrox<strong>in</strong>e products.Available at https://www.aace.com/files/position-statements/aace-tes-ata-thyrox<strong>in</strong>eproducts.pdf (accessedAugust 19, 2012).140. Centanni M, Gargano L, Canettieri G, Viceconti N,Franchi A, Delle Fave G, Annibale B 2006 Thyrox<strong>in</strong>e<strong>in</strong> goiter, Helicobacter pylori <strong>in</strong>fection, and chronicgastritis. N Engl J Med 354:1787–1795.141. Sachmechi I, Reich DM, An<strong>in</strong>yei M, Wibowo F,Gupta G, Kim PJ 2007 Effect of proton pump <strong>in</strong>-EL2EL2EL2EL2EL4EL1EL2EL3EL3EL3EL4EL3EL3hibitors on serum thyroid-stimulat<strong>in</strong>g hormone level<strong>in</strong> euthyroid patients treated with levothyrox<strong>in</strong>e <strong>for</strong>hypothyroidism. Endocr Pract 13:345–349.142. Pabla D, Akhlaghi F, Zia H 2009 A comparative pHdissolutionprofile study of selected commercial levothyrox<strong>in</strong>eproducts us<strong>in</strong>g <strong>in</strong>ductively coupledplasma mass spectrometry. Eur J Pharm Biopharm72:105–110.143. U.S. Food and Drug Adm<strong>in</strong>istration 2008 Tiros<strong>in</strong>tÔ(Levothyrox<strong>in</strong>e Sodium) Capsules. Available at www.accessdata.fda.gov/drugsatfda_docs/nda/2006/021924s000TOC.cfm (accessed August 19, 2012).144. Ananthakrishnan S, Braverman LE, Lev<strong>in</strong> RM,Magnani B, Pearce EN 2008 The effect of famotid<strong>in</strong>e,esomeprazole, and ezetimibe on levothyrox<strong>in</strong>e absorption.Thyroid 18:493–498.145. LeBoff MS, Kaplan MM, Silva JE, Larsen PR 1982Bioavailability of thyroid hormones from oral replacementpreparations. Metabolism 31:900–905.146. Rosenbaum RL, Barzel US 1982 Levothyrox<strong>in</strong>e replacementdose <strong>for</strong> primary hypothyroidism decreaseswith age. Ann Intern Med 96:53–55.147. Roti E, M<strong>in</strong>elli R, Gard<strong>in</strong>i E, Braverman LE 1993 Theuse and misuse of thyroid hormone. Endocr Rev14:401–423.148. Mandel SJ, Brent GA, Larsen PR 1993 Levothyrox<strong>in</strong>etherapy <strong>in</strong> patients with thyroid disease. Ann InternMed 119:492–502.149. Toft AD 1994 Thyrox<strong>in</strong>e therapy. N Engl J Med331:174–180.150. Woeber KA 2002 Levothyrox<strong>in</strong>e therapy and serumfree thyrox<strong>in</strong>e and free triiodothyron<strong>in</strong>e concentrations.J Endocr<strong>in</strong>ol Invest 25:106–109.151. Saw<strong>in</strong> CT, Herman T, Molitch ME, London MH,Kramer SM 1983 Ag<strong>in</strong>g and the thyroid. Decreasedrequirement <strong>for</strong> thyroid hormone <strong>in</strong> older hypothyroidpatients. Am J Med 75:206–209.152. Cunn<strong>in</strong>gham JJ, Barzel US 1984 Lean body mass is apredictor of the daily requirement <strong>for</strong> thyroid hormone<strong>in</strong> older men and women. J Am Geriatr Soc32:204–207.153. Sant<strong>in</strong>i F, P<strong>in</strong>chera A, Marsili A, Ceccar<strong>in</strong>i G, CastagnaMG, Valeriano R, Giannetti M, Taddei D,Centoni R, Scartabelli G, Rago T, Mammoli C, EliseiR, Vitti P 2005 Lean body mass is a major determ<strong>in</strong>antof levothyrox<strong>in</strong>e dosage <strong>in</strong> the treatment ofthyroid diseases. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 90:124–127.154. Devdhar M, Drooger R, Pehlivanova M, S<strong>in</strong>gh G,Jonklaas J 2011 Levothyrox<strong>in</strong>e replacement doses areaffected by gender and weight, but not age. Thyroid21:821–827.155. Hennessey JV, Evaul JE, Tseng YC, Burman KD,Wartofsky L 1986 L-thyrox<strong>in</strong>e dosage: a reevaluationof therapy with contemporary preparations. AnnIntern Med 105:11–15.156. Fish LH, Schwartz HL, Cavanaugh J, Steffes MW,Bantle JP, Oppenheimer JH 1987 Replacement dose,metabolism, and bioavailability of levothyrox<strong>in</strong>e <strong>in</strong>the treatment of hypothyroidism. Role of triiodothyron<strong>in</strong>e<strong>in</strong> pituitary feedback <strong>in</strong> humans. N Engl JMed 316:764–770.157. Kabadi UM, Jackson T 1995 Serum thyrotrop<strong>in</strong> <strong>in</strong>primary hypothyroidism. A possible predictor ofEL4EL4EL2EL2EL3EL4EL4EL4EL2EL3EL3EL3EL2EL3EL2EL3
1230 GARBER ET AL.optimal daily levothyrox<strong>in</strong>e dose <strong>in</strong> primary hypothyroidism.Arch Intern Med 155:1046–1048.158. Gordon MB, Gordon MS 1999 Variations <strong>in</strong> adequatelevothyrox<strong>in</strong>e replacement therapy <strong>in</strong> patientswith different causes of hypothyroidism. EndocrPract 5:233–238.159. Rosenbaum RL, Barzel US 1981 <strong>Cl<strong>in</strong>ical</strong> hypothyroidism<strong>in</strong> the elderly—a preventable disorder? J AmGeriatr Soc 29:221–223.160. Miller MJ, Pan C, Barzel US 1990 The prevalenceof subcl<strong>in</strong>ical hypothyroidism <strong>in</strong> adults withlow-normal blood thyrox<strong>in</strong>e levels. NY State J Med90:541–544.161. Meier C, Staub JJ, Roth CB, Guglielmetti M, Kunz M,Miserez AR, Drewe J, Huber P, Herzog R, Muller B2001 TSH-controlled L-thyrox<strong>in</strong>e therapy reducescholesterol levels and cl<strong>in</strong>ical symptoms <strong>in</strong> subcl<strong>in</strong>icalhypothyroidism: a double bl<strong>in</strong>d, placebo-controlledtrial (Basel Thyroid Study). J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab86:4860–4866.162. Teixeira PF, Reuters VS, Ferreira MM, Almeida CP,Reis FA, Melo BA, Buescu A, Costa AJ, Vaisman M2008 Treatment of subcl<strong>in</strong>ical hypothyroidism reducesatherogenic lipid levels <strong>in</strong> a placebo-controlleddouble-bl<strong>in</strong>d cl<strong>in</strong>ical trial. Horm Metab Res 40:50–55.163. Bearcroft CP, Toms GC, Williams SJ, Noonan K,Monson JP 1991 Thyrox<strong>in</strong>e replacement <strong>in</strong> postradioiod<strong>in</strong>ehypothyroidism. Cl<strong>in</strong> Endocr<strong>in</strong>ol (Oxf )34:115–118.164. Roos A, L<strong>in</strong>n-Rasker SP, van Domburg RT, TijssenJP, Berghout A 2005 The start<strong>in</strong>g dose of levothyrox<strong>in</strong>e<strong>in</strong> primary hypothyroidism treatment: aprospective, randomized, double-bl<strong>in</strong>d trial. ArchIntern Med 165:1714–1720.165. Bolk N, Visser TJ, Nijman J, Jongste IJ, Tijssen JG,Berghout A 2010 Effects of even<strong>in</strong>g vs morn<strong>in</strong>g levothyrox<strong>in</strong>e<strong>in</strong>take: a randomized double-bl<strong>in</strong>dcrossover trial. Arch Intern Med 170:1996–2003.166. Bach-Huynh TG, Nayak B, Loh J, Sold<strong>in</strong> S, Jonklaas J2009 Tim<strong>in</strong>g of levothyrox<strong>in</strong>e adm<strong>in</strong>istration affectsserum thyrotrop<strong>in</strong> concentration. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 94:3905–3912.167. Hays MT 1988 Thyroid hormone and the gut. EndocrRes 14:203–224.168. Hays MT, Nielsen KR 1994 Human thyrox<strong>in</strong>e absorption:age effects and methodological analyses.Thyroid 4:55–64.169. Wenzel KW, Kirschsieper HE 1977 Aspects of theabsorption of oral L-thyrox<strong>in</strong>e <strong>in</strong> normal man. Metabolism26:1–8.170. Maeda M, Kuzuya N, Masuyama Y, Imai Y, Ikeda H1976 Changes <strong>in</strong> serum triiodothyron<strong>in</strong>e, thyrox<strong>in</strong>e,and thyrotrop<strong>in</strong> dur<strong>in</strong>g treatment with thyrox<strong>in</strong>e <strong>in</strong>severe primary hypothyroidism. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 43:10–17.171. Wiers<strong>in</strong>ga WM 2010 <strong>Hypothyroidism</strong> and myxedemacoma. In: Jameson JL, DeGroot LJ (eds) Endocr<strong>in</strong>ology:Adult and Pediatric, 6th edition.Saunders Elsevier, Philadelphia, PA, pp 1607–1622.172. Brajkovich IE, Mashiter K, Jopl<strong>in</strong> GF, Cassar J 1983Serum T4, T3, and TSH levels <strong>in</strong> primary hypothyroidismdur<strong>in</strong>g replacement therapy with thyrox<strong>in</strong>e.Metabolism 32:745–747.EL3EL3EL3EL2EL2EL3EL2EL2EL2EL4EL2EL2EL2EL4EL2173. Slawik M, Klawitter B, Meiser E, Schories M,Zwermann O, Borm K, Peper M, Lubrich B, Hug MJ,Nauck M, Olschewski M, Beuschle<strong>in</strong> F, Re<strong>in</strong>cke M2007 Thyroid hormone replacement <strong>for</strong> centralhypothyroidism: a randomized controlled trialcompar<strong>in</strong>g two doses of thyrox<strong>in</strong>e (T4) with acomb<strong>in</strong>ation of T4 and triiodothyron<strong>in</strong>e. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 92:4115–4122.174. Iverson JF, Mariash CN 2008 Optimal free thyrox<strong>in</strong>elevels <strong>for</strong> thyroid hormone replacement <strong>in</strong> hypothyroidism.Endocr Pract 14:550–555.175. Koulouri O, Auld<strong>in</strong> MA, Agarwal R, Kieffer V, RobertsonC, Falconer Smith J, Levy MJ, Howlett TA2011 Diagnosis and treatment of hypothyroidism <strong>in</strong>TSH deficiency compared to primary thyroid disease:pituitary patients are at risk of under-replacementwith levothyrox<strong>in</strong>e. Cl<strong>in</strong> Endocr<strong>in</strong>ol (Oxf )74:744–749.176. Gabrilove JL, Ludwig AW 1957 The histogenesis ofmyxedema. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 17:925–932.177. Alexander EK, Marqusee E, Lawrence J, Jarolim P,Fischer GA, Larsen PR 2004 Tim<strong>in</strong>g and magnitudeof <strong>in</strong>creases <strong>in</strong> levothyrox<strong>in</strong>e requirements dur<strong>in</strong>gpregnancy <strong>in</strong> women with hypothyroidism. N Engl JMed 351:241–249.178. Keat<strong>in</strong>g FR Jr, Park<strong>in</strong> TW, Selby JB, Dick<strong>in</strong>son LS1961 Treatment of heart disease associated withmyxedema. Prog Cardiovasc Dis 3:364–381.179. Ladenson PW, Lev<strong>in</strong> AA, Ridgway EC, Daniels GH1984 Complications of surgery <strong>in</strong> hypothyroid patients.Am J Med 77:261–266.180. Drucker DJ, Burrow GN 1985 Cardiovascular surgery<strong>in</strong> the hypothyroid patient. Arch Intern Med145:1585–1587.181. Means JH, Hertz S, Lerman J. 1940 The pituitary typeof myxedema or Simmond’s disease masquerad<strong>in</strong>g asmyxedema. Trans Assoc Am Physicians 55:32.182. Peterson RE 1958 The <strong>in</strong>fluence of the thyroid onadrenal cortical function. J Cl<strong>in</strong> Invest 37:736–743.183. Peterson RE, Wyngaarden JB 1956 The miscible pooland turnover rate of hydrocortisone <strong>in</strong> man. J Cl<strong>in</strong>Invest 35:552–561.184. A<strong>in</strong> KB, Refetoff S, Fe<strong>in</strong> HG, We<strong>in</strong>traub BD 1991Pseudomalabsorption of levothyrox<strong>in</strong>e. JAMA 266:2118–2120.185. Grebe SK, Cooke RR, Ford HC, Fagerstrom JN,Cordwell DP, Lever NA, Purdie GL, Feek CM 1997Treatment of hypothyroidism with once weeklythyrox<strong>in</strong>e. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 82:870–875.186. Lamson MJ, Pampl<strong>in</strong> CL, Rolleri RL, Kle<strong>in</strong> I 2004Quantitation of a substantial reduction <strong>in</strong> levothyrox<strong>in</strong>e(T4) reduction by food. Thyroid 14:876(abstract).187. Saw<strong>in</strong> CT, Geller A, Wolf PA, Belanger AJ, Baker E,Bacharach P, Wilson PW, Benjam<strong>in</strong> EJ, D’Agost<strong>in</strong>oRB 1994 Low serum thyrotrop<strong>in</strong> concentrations as arisk factor <strong>for</strong> atrial fibrillation <strong>in</strong> older persons. NEngl J Med 331:1249–1252.188. Shapiro LE, Sievert R, Ong L, Ocampo EL, ChanceRA, Lee M, Nanna M, Ferrick K, Surks MI 1997M<strong>in</strong>imal cardiac effects <strong>in</strong> asymptomatic athyreoticpatients chronically treated with thyrotrop<strong>in</strong>-suppressivedoses of L-thyrox<strong>in</strong>e. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 82:2592–2595.EL2EL3EL3EL2EL2EL3EL3EL3EL3EL2EL2EL3EL2EL3EL2EL3
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1231189. Biondi B, Fazio S, Cuocolo A, Sabat<strong>in</strong>i D, Nicolai E,Lombardi G, Salvatore M, Sacca L 1996 Impairedcardiac reserve and exercise capacity <strong>in</strong> patients receiv<strong>in</strong>glong-term thyrotrop<strong>in</strong> suppressive therapywith levothyrox<strong>in</strong>e. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 81:4224–4228.190. Abdulrahman RM, Delgado V, Hoftijzer HC, NgAC, Ewe SH, Marsan NA, Holman ER, Hovens GC,Corssmit EP, Romijn JA, Bax JJ, Smit JW 2011 Bothexogenous subcl<strong>in</strong>ical hyperthyroidism and shorttermovert hypothyroidism affect myocardial stra<strong>in</strong><strong>in</strong> patients with differentiated thyroid carc<strong>in</strong>oma.Thyroid 21:471–476.191. Stall GM, Harris S, Sokoll LJ, Dawson-Hughes B1990 Accelerated bone loss <strong>in</strong> hypothyroid patientsovertreated with L-thyrox<strong>in</strong>e. Ann Intern Med113:265–269.192. Faber J, Galloe AM 1994 Changes <strong>in</strong> bone massdur<strong>in</strong>g prolonged subcl<strong>in</strong>ical hyperthyroidism dueto L-thyrox<strong>in</strong>e treatment: a meta-analysis. Eur J Endocr<strong>in</strong>ol130:350–356.193. Uzzan B, Campos J, Cucherat M, Nony P, Boissel JP,Perret GY 1996 Effects on bone mass of long termtreatment with thyroid hormones: a meta-analysis. JCl<strong>in</strong> Endocr<strong>in</strong>ol Metab 81:4278–4289.194. Bauer DC, Ett<strong>in</strong>ger B, Nevitt MC, Stone KL 2001Risk <strong>for</strong> fracture <strong>in</strong> women with low serum levels ofthyroid-stimulat<strong>in</strong>g hormone. Ann Intern Med134:561–568.195. Biondi B, Fazio S, Carella C, Sabat<strong>in</strong>i D, Amato G,Cittad<strong>in</strong>i A, Bellastella A, Lombardi G, Sacca L 1994Control of adrenergic overactivity by beta-blockadeimproves the quality of life <strong>in</strong> patients receiv<strong>in</strong>g longterm suppressive therapy with levothyrox<strong>in</strong>e. J Cl<strong>in</strong>Endocr<strong>in</strong>ol Metab 78:1028–1033.196. Botella-Carretero JI, Galan JM, Caballero C, Sancho J,Escobar-Morreale HF 2003 Quality of life and psychometricfunctionality <strong>in</strong> patients with differentiatedthyroid carc<strong>in</strong>oma. Endocr Relat Cancer 10:601–610.197. Samuels MH 2008 Cognitive function <strong>in</strong> untreatedhypothyroidism and hyperthyroidism. Curr Op<strong>in</strong>Endocr<strong>in</strong>ol Diabetes Obes 15:429–433.198. Walsh JP, Ward LC, Burke V, Bhagat CI, Shiels L,Henley D, Gillett MJ, Gilbert R, Tanner M, StuckeyBG 2006 Small changes <strong>in</strong> thyrox<strong>in</strong>e dosage do notproduce measurable changes <strong>in</strong> hypothyroid symptoms,well-be<strong>in</strong>g, or quality of life: results of adouble-bl<strong>in</strong>d, randomized cl<strong>in</strong>ical trial. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 91:2624–2630.199. Boev<strong>in</strong>g A, Paz-Filho G, Radom<strong>in</strong>ski RB, Graf H,Amaral de Carvalho G 2011 Low-normal or highnormalthyrotrop<strong>in</strong> target levels dur<strong>in</strong>g treatment ofhypothyroidism: a prospective, comparative study.Thyroid 21:355–360.200. Stricker R, Echenard M, Eberhart R, Chevailler MC,Perez V, Qu<strong>in</strong>n FA 2007 Evaluation of maternalthyroid function dur<strong>in</strong>g pregnancy: the importanceof us<strong>in</strong>g gestational age-specific reference <strong>in</strong>tervals.Eur J Endocr<strong>in</strong>ol 157:509–514.201. Gilbert RM, Hadlow NC, Walsh JP, Fletcher SJ,Brown SJ, Stuckey BG, Lim EM 2008 Assessment ofthyroid function dur<strong>in</strong>g pregnancy: first-trimester(weeks 9–13) reference <strong>in</strong>tervals derived from WesternAustralian women. Med J Aust 189:250–253.EL3EL2EL3EL2EL2EL2EL3EL3EL4EL2EL2EL2EL2202. Bocos-Terraz JP, Izquierdo-Alvarez S, Bancalero-Flores JL, Alvarez-Lahuerta R, Aznar-Sauca A, Real-Lopez E, Ibanez-Marco R, Bocanegra-Garcia V,Rivera-Sanchez G 2009 Thyroid hormones accord<strong>in</strong>gto gestational age <strong>in</strong> pregnant Spanish women. BMCRes Notes 2:237.203. Haddow JE, Knight GJ, Palomaki GE, McCla<strong>in</strong> MR,Pulkk<strong>in</strong>en AJ 2004 The reference range and with<strong>in</strong>personvariability of thyroid stimulat<strong>in</strong>g hormonedur<strong>in</strong>g the first and second trimesters of pregnancy.J Med Screen 11:170–174.204. Mannisto T, Surcel HM, Ruokonen A, VaarasmakiM, Pouta A, Bloigu A, Jarvel<strong>in</strong> MR, Hartika<strong>in</strong>en AL,Suvanto E 2011 Early pregnancy reference <strong>in</strong>tervalsof thyroid hormone concentrations <strong>in</strong> a thyroid antibody-negativepregnant population. Thyroid 21:291–298.205. Marwaha RK, Chopra S, Gopalakrishnan S, SharmaB, Kanwar RS, Sastry A, S<strong>in</strong>gh S 2008 Establishmentof reference range <strong>for</strong> thyroid hormones <strong>in</strong> normalpregnant Indian women. BJOG 115:602–606.206. Panesar NS, Li CY, Rogers MS 2001 Reference <strong>in</strong>tervals<strong>for</strong> thyroid hormones <strong>in</strong> pregnant Ch<strong>in</strong>esewomen. Ann Cl<strong>in</strong> Biochem 38:329–332.207. Sold<strong>in</strong> OP, Sold<strong>in</strong> D, Sastoque M 2007 Gestationspecificthyrox<strong>in</strong>e and thyroid stimulat<strong>in</strong>g hormonelevels <strong>in</strong> the United States and worldwide. TherDrug Monit 29:553–559.208. Sosa JA, Bowman HM, Tielsch JM, Powe NR, GordonTA, Udelsman R 1998 The importance of surgeonexperience <strong>for</strong> cl<strong>in</strong>ical and economic outcomesfrom thyroidectomy. Ann Surg 228:320–330.209. Ortiz R, Hupart KH, DeFesi CR, Surks MI 1998 Effectof early referral to an endocr<strong>in</strong>ologist on efficiencyand cost of evaluation and development oftreatment plan <strong>in</strong> patients with thyroid nodules. JCl<strong>in</strong> Endocr<strong>in</strong>ol Metab 83:3803–3807.210. Kumar H, Dayk<strong>in</strong> J, Holder R, Watk<strong>in</strong>son JC,Sheppard MC, Franklyn JA 2001 An audit of managementof differentiated thyroid cancer <strong>in</strong> specialistand non-specialist cl<strong>in</strong>ic sett<strong>in</strong>gs. Cl<strong>in</strong> Endocr<strong>in</strong>ol(Oxf ) 54:719–723.211. R<strong>in</strong>aldi MD, Stagnaro-Green AS 2007 Thyroid diseaseand pregnancy: degrees of knowledge. Thyroid17:747–753.212. Davis LE, Leveno KJ, Cunn<strong>in</strong>gham FG 1988 <strong>Hypothyroidism</strong>complicat<strong>in</strong>g pregnancy. Obstet Gynecol72:108–112.213. Leung AS, Millar LK, Koon<strong>in</strong>gs PP, Montoro M,Mestman JH 1993 Per<strong>in</strong>atal outcome <strong>in</strong> hypothyroidpregnancies. Obstet Gynecol 81:349–353.214. Casey BM, Dashe JS, Wells CE, McIntire DD, ByrdW, Leveno KJ, Cunn<strong>in</strong>gham FG 2005 Subcl<strong>in</strong>icalhypothyroidism and pregnancy outcomes. ObstetGynecol 105:239–245.215. Teng W, Shan Z 2011 Pregnancy and thyroid diseases<strong>in</strong> Ch<strong>in</strong>a. Thyroid 21:1053–1055.216. Li Y, Shan Z, Teng W, Yu X, Fan C, Teng X, Guo R,Wang H, Li J, Chen Y, Wang W, Chaw<strong>in</strong>ga M,Zhang L, Yang L, Zhao Y, Hua T 2010 Abnormalitiesof maternal thyroid function dur<strong>in</strong>g pregnancyaffect neuropsychological development of theirchildren at 25–30 months. Cl<strong>in</strong> Endocr<strong>in</strong>ol (Oxf ) 72:825–829.EL3EL2EL2EL2EL2EL1EL3EL3EL3EL3EL3EL3EL2EL4EL2
1232 GARBER ET AL.217. Haddow JE, Palomaki GE, Allan WC, Williams JR,Knight GJ, Gagnon J, O’Heir CE, Mitchell ML, HermosRJ, Waisbren SE, Faix JD, Kle<strong>in</strong> RZ 1999 Maternalthyroid deficiency dur<strong>in</strong>g pregnancy andsubsequent neuropsychological development of thechild. N Engl J Med 341:549–555.218. Yu X, Shan Z, Teng W, Xue H, Li YB, Wang W, Li J,Chen Y, Li J, Fan C, Wang H, Zhang H, Guo R 2010A prospective study on impact of subcl<strong>in</strong>ical hypothyroidismdur<strong>in</strong>g pregnancy receiv<strong>in</strong>g levothyrox<strong>in</strong>etreatment or not on neuropsychologicaldevelopment of the offspr<strong>in</strong>g. ITC 2010-1037. 14thInternational Thyroid Conference, Paris, France, September11–16.219. Lazarus JH, Bestwick JP, Channon S, Paradice R,Ma<strong>in</strong>a A, Rees R, Chiusano E, John R, Guaraldo V,George LM, Perona M, Dall’Amico D, Parkes AB,Joomun M, Wald NJ 2012 Antenatal thyroidscreen<strong>in</strong>g and childhood cognitive function. N Engl JMed 366:493–501.220. Stagnaro-Green A, Roman SH, Cob<strong>in</strong> RH, el-HarazyE, Alvarez-Marfany M, Davies TF 1990 Detection ofat-risk pregnancy by means of highly sensitive assays<strong>for</strong> thyroid autoantibodies. JAMA 264:1422–1425.221. Negro R, Schwartz A, Gismondi R, T<strong>in</strong>elli A, MangieriT, Stagnaro-Green A 2011 Thyroid antibodypositivity <strong>in</strong> the first trimester of pregnancy is associatedwith negative pregnancy outcomes. J Cl<strong>in</strong>Endocr<strong>in</strong>ol Metab 96:E920–924.222. Pop VJ, de Vries E, van Baar AL, Waelkens JJ, deRooy HA, Horsten M, Donkers MM, Komproe IH,van Son MM, Vader HL 1995 Maternal thyroidperoxidase antibodies dur<strong>in</strong>g pregnancy: a markerof impaired child development? J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 80:3561–3566.223. Gl<strong>in</strong>oer D, Riahi M, Grun JP, K<strong>in</strong>thaert J 1994 Risk ofsubcl<strong>in</strong>ical hypothyroidism <strong>in</strong> pregnant women withasymptomatic autoimmune thyroid disorders. J Cl<strong>in</strong>Endocr<strong>in</strong>ol Metab 79:197–204.224. Negro R, Formoso G, Mangieri T, Pezzarossa A,Dazzi D, Hassan H 2006 Levothyrox<strong>in</strong>e treatment <strong>in</strong>euthyroid pregnant women with autoimmune thyroiddisease: effects on obstetrical complications. JCl<strong>in</strong> Endocr<strong>in</strong>ol Metab 91:2587–2591.225. Kim CH, Ahn JW, Kang SP, Kim SH, Chae HD,Kang BM 2011 Effect of levothyrox<strong>in</strong>e treatment on<strong>in</strong> vitro fertilization and pregnancy outcome <strong>in</strong> <strong>in</strong>fertilewomen with subcl<strong>in</strong>ical hypothyroidism undergo<strong>in</strong>g<strong>in</strong> vitro fertilization/<strong>in</strong>tracytoplasmicsperm <strong>in</strong>jection. Fertil Steril 95:1650–1654.226. Morreale de Escobar G, Obregon MJ, Escobar delRey F 2000 Is neuropsychological development relatedto maternal hypothyroidism or to maternalhypothyrox<strong>in</strong>emia? J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 85:3975–3987.227. Morreale de Escobar G 2001 The role of thyroidhormone <strong>in</strong> fetal neurodevelopment. J Pediatr Endocr<strong>in</strong>olMetab 14 Suppl 6:1453–1462.228. Pop VJ, Kuijpens JL, van Baar AL, Verkerk G, vanSon MM, de Vijlder JJ, Vulsma T, Wiers<strong>in</strong>ga WM,Drexhage HA, Vader HL 1999 Low maternal freethyrox<strong>in</strong>e concentrations dur<strong>in</strong>g early pregnancy areassociated with impaired psychomotor development<strong>in</strong> <strong>in</strong>fancy. Cl<strong>in</strong> Endocr<strong>in</strong>ol (Oxf ) 50:149–155.EL2EL2EL1EL2EL3EL3EL2EL2EL2EL4EL4EL3229. Pop VJ, Brouwers EP, Vader HL, Vulsma T, van BaarAL, de Vijlder JJ 2003 Maternal hypothyrox<strong>in</strong>aemiadur<strong>in</strong>g early pregnancy and subsequent child development:a 3-year follow-up study. Cl<strong>in</strong> Endocr<strong>in</strong>ol(Oxf ) 59:282–288.230. Kooistra L, Craw<strong>for</strong>d S, van Baar AL, Brouwers EP,Pop VJ 2006 Neonatal effects of maternal hypothyrox<strong>in</strong>emiadur<strong>in</strong>g early pregnancy. Pediatrics117:161–167.231. Henrichs J, Bongers-Schokk<strong>in</strong>g JJ, Schenk JJ, GhassabianA, Schmidt HG, Visser TJ, Hooijkaas H, deMu<strong>in</strong>ck Keizer-Schrama SM, Hofman A, Jaddoe VV,Visser W, Steegers EA, Verhulst FC, de Rijke YB,Tiemeier H 2010 Maternal thyroid function dur<strong>in</strong>gearly pregnancy and cognitive function<strong>in</strong>g <strong>in</strong> earlychildhood: the generation R study. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 95:4227–4234.232. Oken E, Braverman LE, Platek D, Mitchell ML, LeeSL, Pearce EN 2009 Neonatal thyrox<strong>in</strong>e, maternalthyroid function, and child cognition. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 94:497–503.233. Yassa L, Marqusee E, Fawcett R, Alexander EK 2010Thyroid hormone early adjustment <strong>in</strong> pregnancy(the THERAPY) trial. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab95:3234–3241.234. Mandel SJ, Larsen PR, Seely EW, Brent GA 1990Increased need <strong>for</strong> thyrox<strong>in</strong>e dur<strong>in</strong>g pregnancy <strong>in</strong>women with primary hypothyroidism. N Engl J Med323:91–96.235. Tamaki H, Am<strong>in</strong>o N, Takeoka K, Mitsuda N, MiyaiK, Tanizawa O 1990 Thyrox<strong>in</strong>e requirement dur<strong>in</strong>gpregnancy <strong>for</strong> replacement therapy of hypothyroidism.Obstet Gynecol 76:230–233.236. Kaplan MM 1992 Monitor<strong>in</strong>g thyrox<strong>in</strong>e treatmentdur<strong>in</strong>g pregnancy. Thyroid 2:147–152.237. Kaplan MM, Meier DA 1998 Thyroid diseases <strong>in</strong>pregnancy. In: Gleicher N (ed) Pr<strong>in</strong>ciples and <strong>Practice</strong>of Medical Therapy <strong>in</strong> Pregnancy, 3rd edition.Appleton & Lange, Stam<strong>for</strong>d, CT, pp 432–448.238. Verga U, Bergamaschi S, Cortelazzi D, Ronzoni S,Marconi AM, Beck-Peccoz P 2009 Adjustment of L-T4 substitutive therapy <strong>in</strong> pregnant women withsubcl<strong>in</strong>ical, overt or post-ablative hypothyroidism.Cl<strong>in</strong> Endocr<strong>in</strong>ol (Oxf ) 70:798–802.239. Alvarez-Marfany M, Roman SH, Drexler AJ, RobertsonC, Stagnaro-Green A 1994 Long-term prospectivestudy of postpartum thyroid dysfunction <strong>in</strong>women with <strong>in</strong>sul<strong>in</strong> dependent diabetes mellitus. JCl<strong>in</strong> Endocr<strong>in</strong>ol Metab 79:10–16.240. Glass AR, Kushner, J. 1996 Obesity, nutrition, andthe thyroid. Endocr<strong>in</strong>ologist 6:392–404.241. Plummer WA 1940 Body weight <strong>in</strong> spontaneousmyxedema. Transactions of the American Association<strong>for</strong> the Study of Goiter, pp 88–98.242. Karmisholt J, Andersen S, Laurberg P 2011 Weightloss after therapy of hypothyroidism is ma<strong>in</strong>ly causedby excretion of excess body water associated withmyxoedema. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 96:E99–103.243. Knudsen N, Laurberg P, Rasmussen LB, Bulow I,Perrild H, Ovesen L, Jorgensen T 2005 Small differences<strong>in</strong> thyroid function may be important <strong>for</strong>body mass <strong>in</strong>dex and the occurrence of obesity <strong>in</strong>the population. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 90:4019–4024.EL3EL3EL3EL2EL2EL3EL3EL3EL4EL3EL3EL4EL2EL2EL3
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1233244. Nyrnes A, Jorde R, Sundsfjord J 2006 Serum TSH ispositively associated with BMI. Int J Obes (Lond)30:100–105.245. Fox CS, Penc<strong>in</strong>a MJ, D’Agost<strong>in</strong>o RB, Murabito JM,Seely EW, Pearce EN, Vasan RS 2008 Relations ofthyroid function to body weight: cross-sectional andlongitud<strong>in</strong>al observations <strong>in</strong> a community-basedsample. Arch Intern Med 168:587–592.246. Manji N, Boelaert K, Sheppard MC, Holder RL,Gough SC, Franklyn JA 2006 Lack of associationbetween serum TSH or free T4 and body mass <strong>in</strong>dex<strong>in</strong> euthyroid subjects. Cl<strong>in</strong> Endocr<strong>in</strong>ol (Oxf ) 64:125–128.247. Michalaki MA, Vagenakis AG, Leonardou AS, ArgentouMN, Habeos IG, Makri MG, Psyrogiannis AI,Kalfarentzos FE, Kyriazopoulou VE 2006 Thyroidfunction <strong>in</strong> humans with morbid obesity. Thyroid16:73–78.248. Radetti G, Kleon W, Buzi F, Crivellaro C, PappalardoL, di Iorgi N, Maghnie M 2008 Thyroid functionand structure are affected <strong>in</strong> childhood obesity. JCl<strong>in</strong> Endocr<strong>in</strong>ol Metab 93:4749–4754.249. Rotondi M, Magri F, Chiovato L 2011 Thyroid andobesity: not a one-way <strong>in</strong>teraction. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 96:344–346.250. Razvi S, Ingoe L, Keeka G, Oates C, McMillan C,Weaver JU 2007 The beneficial effect of L-thyrox<strong>in</strong>eon cardiovascular risk factors, endothelial function,and quality of life <strong>in</strong> subcl<strong>in</strong>ical hypothyroidism:randomized, crossover trial. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab92:1715–1723.251. al-Adsani H, Hoffer LJ, Silva JE 1997 Rest<strong>in</strong>g energyexpenditure is sensitive to small dose changes <strong>in</strong>patients on chronic thyroid hormone replacement. JCl<strong>in</strong> Endocr<strong>in</strong>ol Metab 82:1118–1125.252. Gw<strong>in</strong>up G, Poucher R 1967 A controlled study ofthyroid analogs <strong>in</strong> the therapy of obesity. Am J MedSci 254:416–420.253. Rivl<strong>in</strong> RS 1975 Therapy of obesity with hormones. NEngl J Med 292:26–29.254. Kapte<strong>in</strong> EM, Beale E, Chan LS 2009 Thyroid hormonetherapy <strong>for</strong> obesity and nonthyroidal illnesses:a systematic review. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 94:3663–3675.255. Jonklaas J, Nsouli-Maktabi H 2011 Weight changes<strong>in</strong> euthyroid patients undergo<strong>in</strong>g thyroidectomy.Thyroid 21:1343–1351.256. We<strong>in</strong>reb JT, Yang Y, Braunste<strong>in</strong> GD 2011 Do patientsga<strong>in</strong> weight after thyroidectomy <strong>for</strong> thyroid cancer?Thyroid 21:1339–1342.257. Pollock MA, Sturrock A, Marshall K, Davidson KM,Kelly CJ, McMahon AD, McLaren EH 2001 Thyrox<strong>in</strong>etreatment <strong>in</strong> patients with symptoms of hypothyroidismbut thyroid function tests with<strong>in</strong> thereference range: randomised double bl<strong>in</strong>d placebocontrolled crossover trial. BMJ 323:891–895.258. Pop VJ, Maartens LH, Leus<strong>in</strong>k G, van Son MJ,Knottnerus AA, Ward AM, Metcalfe R, Weetman AP1998 Are autoimmune thyroid dysfunction and depressionrelated? J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 83:3194–3197.259. Harris B, Oretti R, Lazarus J, Parkes A, John R, RichardsC, Newcombe R, Hall R 2002 Randomisedtrial of thyrox<strong>in</strong>e to prevent postnatal depression <strong>in</strong>EL3EL2EL3EL2EL2EL4EL2EL2EL2EL4EL2EL3EL3EL2EL3EL1thyroid-antibody-positive women. Br J Psychiatry180:327–330.260. Cooper-Kazaz R, Apter JT, Cohen R, Karagichev L,Muhammed-Moussa S, Grupper D, Drori T, NewmanME, Sackeim HA, Glaser B, Lerer B 2007Comb<strong>in</strong>ed treatment with sertral<strong>in</strong>e and liothyron<strong>in</strong>e<strong>in</strong> major depression: a randomized, doublebl<strong>in</strong>d,placebo-controlled trial. Arch Gen Psychiatry64:679–688.261. Posternak M, Novak S, Stern R, Hennessey J, Joffe R,Prange A Jr, Zimmerman M 2008 A pilot effectivenessstudy: placebo-controlled trial of adjunctiveL-triiodothyron<strong>in</strong>e (T3) used to accelerate and potentiatethe antidepressant response. Int J Neuropsychopharmacol11:15–25.262. Slag MF, Morley JE, Elson MK, Crowson TW, NuttallFQ, Shafer RB 1981 Hypothyrox<strong>in</strong>emia <strong>in</strong> criticallyill patients as a predictor of high mortality.JAMA 245:43–45.263. Kapte<strong>in</strong> EM, We<strong>in</strong>er JM, Rob<strong>in</strong>son WJ, Wheeler WS,Nicoloff JT 1982 Relationship of altered thyroidhormone <strong>in</strong>dices to survival <strong>in</strong> nonthyroidal illnesses.Cl<strong>in</strong> Endocr<strong>in</strong>ol (Oxf ) 16:565–574.264. Brent GA, Hershman JM 1986 Thyrox<strong>in</strong>e therapy <strong>in</strong>patients with severe nonthyroidal illnesses and lowserum thyrox<strong>in</strong>e concentration. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 63:1–8.265. Becker RA, Vaughan GM, Ziegler MG, Seraile LG,Goldfarb IW, Mansour EH, McManus WF, Pruitt BAJr, Mason AD Jr 1982 Hypermetabolic low triiodothyron<strong>in</strong>esyndrome of burn <strong>in</strong>jury. Crit Care Med10:870–875.266. Portman MA, Slee A, Olson AK, Cohen G, Karl T,Tong E, Hast<strong>in</strong>gs L, Patel H, Re<strong>in</strong>hartz O, Mott AR,Ma<strong>in</strong>war<strong>in</strong>g R, L<strong>in</strong>am J, Danzi S 2010 Triiodothyron<strong>in</strong>eSupplementation <strong>in</strong> Infants and ChildrenUndergo<strong>in</strong>g Cardiopulmonary Bypass (TRICC): amulticenter placebo-controlled randomized trial: ageanalysis. Circulation 122:S224–233.267. P<strong>in</strong>gitore A, Galli E, Barison A, Iervasi A, Scarlatt<strong>in</strong>i M,Nucci D, L’Abbate A, Mariotti R, Iervasi G 2008 Acuteeffects of triiodothyron<strong>in</strong>e (T3) replacement therapy <strong>in</strong>patients with chronic heart failure and low-T3 syndrome:a randomized, placebo-controlled study. J Cl<strong>in</strong>Endocr<strong>in</strong>ol Metab 93:1351–1358.268. Zeisel SH 1999 Regulation of ‘‘nutraceuticals’’. Science285:1853–1855.269. Mechanick JI, Brett EM, Chausmer AB, Dickey RA,Wallach S 2003 American Association of <strong>Cl<strong>in</strong>ical</strong>Endocr<strong>in</strong>ologists medical guidel<strong>in</strong>es <strong>for</strong> the cl<strong>in</strong>icaluse of dietary supplements and nutraceuticals. EndocrPract 9:417–470.270. Scally MC, Hodge A 2000 Health supplement regulationsand consumer protection rights. South Med J93:1230–1232.271. Ott J, Promberger R, Kober F, Neuhold N, Tea M,Huber JC, Hermann M 2011 Hashimoto’s thyroiditisaffects symptom load and quality of life unrelated tohypothyroidism: a prospective case-control study <strong>in</strong>women undergo<strong>in</strong>g thyroidectomy <strong>for</strong> benign goiter.Thyroid 21:161–167.272. Zimmermann M, Delange F 2004 Iod<strong>in</strong>e supplementationof pregnant women <strong>in</strong> Europe: a reviewand recommendations. Eur J Cl<strong>in</strong> Nutr 58:979–984.EL2EL2EL3EL3EL2EL2EL2EL2EL4EL4EL4EL2EL4
1234 GARBER ET AL.273. Fumarola A, Calvanese A, D’Armiento M 2009 Iod<strong>in</strong>e<strong>in</strong>take <strong>in</strong> pregnancy. Int J Gynaecol Obstet104:147–148.274. Clarke N, Kabadi UM 2004 Optimiz<strong>in</strong>g treatment ofhypothyroidism. Treat Endocr<strong>in</strong>ol 3:217–221.275. Sherman SI, R<strong>in</strong>gel MD, Smith MJ, Kopelen HA,Zoghbi WA, Ladenson PW 1997 Augmented hepaticand skeletal thyromimetic effects of tiratricol <strong>in</strong>comparison with levothyrox<strong>in</strong>e. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 82:2153–2158.276. Chan WB, Chow CC, Cockram CS 2004 A patientwith low free T4 and low thyroid-stimulat<strong>in</strong>g hormonewithout hypopituitarism. Int J Cl<strong>in</strong> Pract58:983–984.277. Scally MC, Hodge A 2003 A report of hypothyroidism<strong>in</strong>duced by an over-the-counter fat losssupplement (Tiratricol). Int J Sport Nutr Exerc Metab13:112–116.278. Bauer BA, Elk<strong>in</strong> PL, Erickson D, Klee GG, BrennanMD 2002 Symptomatic hyperthyroidism <strong>in</strong> a patienttak<strong>in</strong>g the dietary supplement tiratricol. Mayo Cl<strong>in</strong>Proc 77:587–590.279. Messier N, Laflamme L, Hamann G, Langlois MF2001 In vitro effect of Triac on resistance to thyroidhormone receptor mutants: potential basis <strong>for</strong> therapy.Mol Cell Endocr<strong>in</strong>ol 174:59–69.280. Ueda S, Takamatsu J, Fukata S, Tanaka K, ShimizuN, Sakata S, Yamaji T, Kuma K, Ohsawa N 1996Differences <strong>in</strong> response of thyrotrop<strong>in</strong> to 3,5,3¢-triiodothyron<strong>in</strong>eand 3,5,3¢-triiodothyroacetic acid <strong>in</strong>patients with resistance to thyroid hormone. Thyroid6:563–570.281. Kang GY, Parks J, Fileta BB, Chang AS, Abdel-Rahm M, Burch HB, Bernet V 2011 Thyrox<strong>in</strong>e andtriiodothyron<strong>in</strong>e content <strong>in</strong> commercially availablethyroid health supplements. American ThyroidAssociation 81st Annual Meet<strong>in</strong>g, Indian Wells,CA, October 26–30.282. Dai X, Zhou Y, Yu X 1999 [Effect of g<strong>in</strong>seng <strong>in</strong>jection<strong>in</strong> treat<strong>in</strong>g congestive heart failure and its <strong>in</strong>fluenceon thyroid hormones]. Zhongguo Zhong Xi Yi Jie HeZa Zhi 19:209–211.283. Skibola CF 2004 The effect of Fucus vesiculosus, anedible brown seaweed, upon menstrual cycle lengthand hormonal status <strong>in</strong> three pre-menopausal women:a case report. BMC Complement Altern Med 4:10.284. Masuda Y, Haramizu S, Oki K, Ohnuki K, WatanabeT, Yazawa S, Kawada T, Hashizume S, Fushiki T2003 Upregulation of uncoupl<strong>in</strong>g prote<strong>in</strong>s by oraladm<strong>in</strong>istration of capsiate, a nonpungent capsaic<strong>in</strong>analog. J Appl Physiol 95:2408–2415.285. Barnes J, Anderson LA, Gibbons S, Phillipson JD2005 Ech<strong>in</strong>acea species (Ech<strong>in</strong>acea angustifolia (DC.)Hell., Ech<strong>in</strong>acea pallida (Nutt.) Nutt., Ech<strong>in</strong>acea purpurea(L.) Moench): a review of their chemistry,pharmacology and cl<strong>in</strong>ical properties. J PharmPharmacol 57:929–954.286. Venkateswaran A, Marsee DK, Green SH, Jhiang SM2004 Forskol<strong>in</strong>, 8-Br-3¢,5¢-cyclic adenos<strong>in</strong>e 5¢-monophosphate,and catalytic prote<strong>in</strong> k<strong>in</strong>ase A expression<strong>in</strong> the nucleus <strong>in</strong>crease radioiodide uptake and sodium/iodidesymporter prote<strong>in</strong> levels <strong>in</strong> RET/PTC1-express<strong>in</strong>g cells. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab89:6168–6172.EL4EL4EL3EL3EL3EL3EL3EL3EL3EL3EL4EL4EL4EL3287. Stranges S, Marshall JR, Natarajan R, Donahue RP,Trevisan M, Combs GF, Cappuccio FP, Ceriello A,Reid ME 2007 Effects of long-term selenium supplementationon the <strong>in</strong>cidence of type 2 diabetes: arandomized trial. Ann Intern Med 147:217–223.288. Negro R, Greco G, Mangieri T, Pezzarossa A, DazziD, Hassan H 2007 The <strong>in</strong>fluence of selenium supplementationon postpartum thyroid status <strong>in</strong>pregnant women with thyroid peroxidase autoantibodies.J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 92:1263–1268.289. Rayman MP, Thompson AJ, Bekaert B, Catterick J,Galass<strong>in</strong>i R, Hall E, Warren-Perry M, Beckett GJ 2008Randomized controlled trial of the effect of seleniumsupplementation on thyroid function <strong>in</strong> the elderly<strong>in</strong> the United K<strong>in</strong>gdom. Am J Cl<strong>in</strong> Nutr 87:370–378.290. Toulis KA, Anastasilakis AD, Tzellos TG, Goulis DG,Kouvelas D 2010 Selenium supplementation <strong>in</strong> thetreatment of Hashimoto’s thyroiditis: a systematicreview and a meta-analysis. Thyroid 20:1163–1173.291. Marcocci C, Kahaly GJ, Krassas GE, Bartalena L,Prummel M, Stahl M, Altea MA, Nardi M, Pitz S,Boboridis K, Sivelli P, von Arx G, Mourits MP, BaldeschiL, Bencivelli W, Wiers<strong>in</strong>ga W 2011 Seleniumand the course of mild Graves’ orbitopathy. N Engl JMed 364:1920–1931.292. Razvi S, Shakoor A, Vanderpump M, Weaver JU,Pearce SH 2008 The <strong>in</strong>fluence of age on the relationshipbetween subcl<strong>in</strong>ical hypothyroidism andischemic heart disease: a metaanalysis. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 93:2998–3007.293. Razvi S, Weaver JU, Butler TJ, Pearce SH 2012 Levothyrox<strong>in</strong>etreatment of subcl<strong>in</strong>ical hypothyroidism,fatal and nonfatal cardiovascular events, andmortality. Arch Intern Med. [EPub ahead of pr<strong>in</strong>t].294. Rodondi N, Bauer DC, Cappola AR, Cornuz J,Robb<strong>in</strong>s J, Fried LP, Ladenson PW, Vitt<strong>in</strong>ghoff E,Gottdiener JS, Newman AB 2008 Subcl<strong>in</strong>ical thyroiddysfunction, cardiac function, and the risk of heartfailure. The Cardiovascular Health study. J Am CollCardiol 52:1152–1159.295. Correia N, Mullally S, Cooke G, Tun TK, Phelan N,Feeney J, Fitzgibbon M, Boran G, O’Mara S, Gibney J2009 Evidence <strong>for</strong> a specific defect <strong>in</strong> hippocampalmemory <strong>in</strong> overt and subcl<strong>in</strong>ical hypothyroidism. JCl<strong>in</strong> Endocr<strong>in</strong>ol Metab 94:3789–3797.296. Jorde R, Waterloo K, Storhaug H, Nyrnes A,Sundsfjord J, Jenssen TG 2006 Neuropsychologicalfunction and symptoms <strong>in</strong> subjects with subcl<strong>in</strong>icalhypothyroidism and the effect of thyrox<strong>in</strong>e treatment.J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 91:145–153.297. Parle J, Roberts L, Wilson S, Pattison H, Roalfe A,Haque MS, Heath C, Sheppard M, Franklyn J, HobbsFD 2010 A randomized controlled trial of the effectof thyrox<strong>in</strong>e replacement on cognitive function <strong>in</strong>community-liv<strong>in</strong>g elderly subjects with subcl<strong>in</strong>icalhypothyroidism: the Birm<strong>in</strong>gham Elderly Thyroidstudy. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 95:3623–3632.298. Celi FS, Zemskova M, L<strong>in</strong>derman JD, Smith S,Dr<strong>in</strong>kard B, Sachdev V, Skarulis MC, Kozlosky M,Csako G, Costello R, Puc<strong>in</strong>o F 2011 Metabolic effectsof liothyron<strong>in</strong>e therapy <strong>in</strong> hypothyroidism: a randomized,double-bl<strong>in</strong>d, crossover trial of liothyron<strong>in</strong>eversus levothyrox<strong>in</strong>e. J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 96:3466–3474.EL1EL1EL1EL2EL2EL2EL1EL2EL2EL2EL2EL2
PRACTICE GUIDELINES FOR HYPOTHYROIDISM IN ADULTS 1235299. Strisower EH, Strisower B 1964 The separate hypolipoprote<strong>in</strong>emiceffects of dextrothyrox<strong>in</strong>e and ethylchlorophenoxyisobutyrate. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab24:139–144.300. Ladenson PW, Kristensen JD, Ridgway EC, OlssonAG, Carlsson B, Kle<strong>in</strong> I, Baxter JD, Angel<strong>in</strong> B 2010Use of the thyroid hormone analogue eprotirome <strong>in</strong>stat<strong>in</strong>-treated dyslipidemia. N Engl J Med 362:906–916.301. Berkenstam A, Kristensen J, Mellstrom K, CarlssonB, Malm J, Rehnmark S, Garg N, Andersson CM,Rudl<strong>in</strong>g M, Sjoberg F, Angel<strong>in</strong> B, Baxter JD 2008 Thethyroid hormone mimetic compound KB2115 lowersplasma LDL cholesterol and stimulates bile acidsynthesis without cardiac effects <strong>in</strong> humans. ProcNatl Acad Sci USA 105:663–667.302. Ladenson PW, McCarren M, Mork<strong>in</strong> E, EdsonRG, Shih MC, Warren SR, Barnhill JG, ChurbyL, Thai H, O’Brien T, Anand I, Warner A, HattlerB, Dunlap M, Erikson J, Goldman S 2010 Effectsof the thyromimetic agent diiodothyropropionicacid on body weight, body mass <strong>in</strong>dex, and serumlipoprote<strong>in</strong>s: a pilot prospective, randomized, controlledstudy. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 95:1349–1354.303. Abalovich M, Am<strong>in</strong>o N, Barbour LA, Cob<strong>in</strong> RH, DeGroot LJ, Gl<strong>in</strong>oer D, Mandel SJ, Stagnaro-Green A2007 Management of thyroid dysfunction dur<strong>in</strong>gpregnancy and postpartum: an Endocr<strong>in</strong>e Society<strong>Cl<strong>in</strong>ical</strong> <strong>Practice</strong> Guidel<strong>in</strong>e. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab92:S1–47.304. Gharib HC, Cob<strong>in</strong> RH, Dickey RA 1999 Subcl<strong>in</strong>icalhypothyroidism dur<strong>in</strong>g pregnancy: position statementfrom the American Association of <strong>Cl<strong>in</strong>ical</strong>Endocr<strong>in</strong>ologists. Endocr Pract 5:367–368.305. Gharib H, Tuttle RM, Bask<strong>in</strong> HJ, Fish LH, S<strong>in</strong>ger PA,McDermott MT 2005 Subcl<strong>in</strong>ical thyroid dysfunc-EL3EL1EL2EL1EL4EL4EL4tion: a jo<strong>in</strong>t statement on management from theAmerican Association of <strong>Cl<strong>in</strong>ical</strong> Endocr<strong>in</strong>ologists,the American Thyroid Association, and the Endocr<strong>in</strong>eSociety. J Cl<strong>in</strong> Endocr<strong>in</strong>ol Metab 90:581–585;discussion 586–587.306. Vaidya B, Anthony S, Bilous M, Shields B, Drury J,Hutchison S, Bilous R 2007 Detection of thyroiddysfunction <strong>in</strong> early pregnancy: universal screen<strong>in</strong>gor targeted high-risk case f<strong>in</strong>d<strong>in</strong>g? J Cl<strong>in</strong> Endocr<strong>in</strong>olMetab 92:203–207.307. Negro R, Schwartz A, Gismondi R, T<strong>in</strong>elli A, MangieriT, Stagnaro-Green A 2010 Universal screen<strong>in</strong>gversus case f<strong>in</strong>d<strong>in</strong>g <strong>for</strong> detection and treatment ofthyroid hormonal dysfunction dur<strong>in</strong>g pregnancy. JCl<strong>in</strong> Endocr<strong>in</strong>ol Metab 95:1699–1707.308. Thung SF, Funai EF, Grobman WA 2009 The costeffectivenessof universal screen<strong>in</strong>g <strong>in</strong> pregnancy <strong>for</strong>subcl<strong>in</strong>ical hypothyroidism. Am J Obstet Gynecol200:267 e261–267.309. Weiss RE, Refetoff S 2010 Thyroid function test<strong>in</strong>g.In: Jameson JL, DeGroot LJ (eds) Endocr<strong>in</strong>ology:Adult and Pediatric, 6th edition. Saunders Elsevier,Philadelphia, PA, pp 1444–1492.310. Barbes<strong>in</strong>o G 2010 Drugs affect<strong>in</strong>g thyroid function.Thyroid 20:763–770.311. Hamnvik OP, Larsen PR, Marqusee E 2011 Thyroiddysfunction from ant<strong>in</strong>eoplastic agents. J Natl CancerInst 103:1572–1578.EL2EL1EL4EL4EL4EL4Address correspondence to:Jeffrey R. Garber, M.D.Endocr<strong>in</strong>ology DivisionHarvard Vanguard Medical Associates133 Brookl<strong>in</strong>e AvenueBoston, MA 02215E-mail: jgarber@bidmc.harvard.edu