global strategy for asthma management and prevention
global strategy for asthma management and prevention
global strategy for asthma management and prevention
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
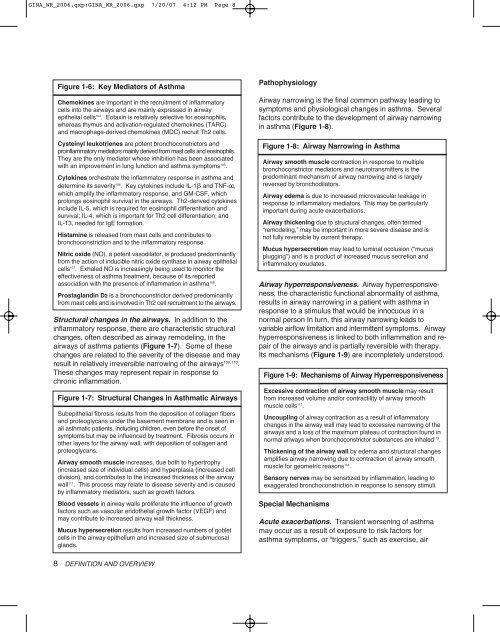
GINA_WR_2006.qxp:GINA_WR_2006.qxp 7/20/07 4:12 PM Page 8Figure 1-6: Key Mediators of AsthmaChemokines are important in the recruitment of inflammatorycells into the airways <strong>and</strong> are mainly expressed in airwayepithelial cells 104 . Eotaxin is relatively selective <strong>for</strong> eosinophils,whereas thymus <strong>and</strong> activation-regulated chemokines (TARC)<strong>and</strong> macrophage-derived chemokines (MDC) recruit Th2 cells.Cysteinyl leukotrienes are potent bronchoconstrictors <strong>and</strong>proinflammatory mediators mainly derived from mast cells <strong>and</strong> eosinophils.They are the only mediator whose inhibition has been associatedwith an improvement in lung function <strong>and</strong> <strong>asthma</strong> symptoms 105 .Cytokines orchestrate the inflammatory response in <strong>asthma</strong> <strong>and</strong>determine its severity 106 . Key cytokines include IL-1 <strong>and</strong> TNF-oc,which amplify the inflammatory response, <strong>and</strong> GM-CSF, whichprolongs eosinophil survival in the airways. Th2-derived cytokinesinclude IL-5, which is required <strong>for</strong> eosinophil differentiation <strong>and</strong>survival; IL-4, which is important <strong>for</strong> Th2 cell differentiation; <strong>and</strong>IL-13, needed <strong>for</strong> IgE <strong>for</strong>mation.Histamine is released from mast cells <strong>and</strong> contributes tobronchoconstriction <strong>and</strong> to the inflammatory response.Nitric oxide (NO), a potent vasodilator, is produced predominantlyfrom the action of inducible nitric oxide synthase in airway epithelialcells 107 . Exhaled NO is increasingly being used to monitor theeffectiveness of <strong>asthma</strong> treatment, because of its reportedassociation with the presence of inflammation in <strong>asthma</strong> 108 .Prostagl<strong>and</strong>in D2 is a bronchoconstrictor derived predominantlyfrom mast cells <strong>and</strong> is involved in Th2 cell recruitment to the airways.Structural changes in the airways. In addition to theinflammatory response, there are characteristic structuralchanges, often described as airway remodeling, in theairways of <strong>asthma</strong> patients (Figure 1-7). Some of thesechanges are related to the severity of the disease <strong>and</strong> mayresult in relatively irreversible narrowing of the airways 109, 110 .These changes may represent repair in response tochronic inflammation.Figure 1-7: Structural Changes in Asthmatic AirwaysSubepithelial fibrosis results from the deposition of collagen fibers<strong>and</strong> proteoglycans under the basement membrane <strong>and</strong> is seen inall <strong>asthma</strong>tic patients, including children, even be<strong>for</strong>e the onset ofsymptoms but may be influenced by treatment. Fibrosis occurs inother layers <strong>for</strong> the airway wall, with deposition of collagen <strong>and</strong>proteoglycans.Airway smooth muscle increases, due both to hypertrophy(increased size of individual cells) <strong>and</strong> hyperplasia (increased celldivision), <strong>and</strong> contributes to the increased thickness of the airwaywall 111 . This process may relate to disease severity <strong>and</strong> is causedby inflammatory mediators, such as growth factors.Blood vessels in airway walls proliferate the influence of growthfactors such as vascular endothelial growth factor (VEGF) <strong>and</strong>may contribute to increased airway wall thickness.Mucus hypersecretion results from increased numbers of gobletcells in the airway epithelium <strong>and</strong> increased size of submucosalgl<strong>and</strong>s.PathophysiologyAirway narrowing is the final common pathway leading tosymptoms <strong>and</strong> physiological changes in <strong>asthma</strong>. Severalfactors contribute to the development of airway narrowingin <strong>asthma</strong> (Figure 1-8).Figure 1-8: Airway Narrowing in AsthmaAirway smooth muscle contraction in response to multiplebronchoconstrictor mediators <strong>and</strong> neurotransmitters is thepredominant mechanism of airway narrowing <strong>and</strong> is largelyreversed by bronchodilators.Airway edema is due to increased microvascular leakage inresponse to inflammatory mediators. This may be particularlyimportant during acute exacerbations.Airway thickening due to structural changes, often termed“remodeling,” may be important in more severe disease <strong>and</strong> isnot fully reversible by current therapy.Mucus hypersecretion may lead to luminal occlusion (“mucusplugging”) <strong>and</strong> is a product of increased mucus secretion <strong>and</strong>inflammatory exudates.Airway hyperresponsiveness. Airway hyperresponsiveness,the characteristic functional abnormality of <strong>asthma</strong>,results in airway narrowing in a patient with <strong>asthma</strong> inresponse to a stimulus that would be innocuous in anormal person In turn, this airway narrowing leads tovariable airflow limitation <strong>and</strong> intermittent symptoms. Airwayhyperresponsiveness is linked to both inflammation <strong>and</strong> repairof the airways <strong>and</strong> is partially reversible with therapy.Its mechanisms (Figure 1-9) are incompletely understood.Figure 1-9: Mechanisms of Airway HyperresponsivenessExcessive contraction of airway smooth muscle may resultfrom increased volume <strong>and</strong>/or contractility of airway smoothmuscle cells 112 .Uncoupling of airway contraction as a result of inflammatorychanges in the airway wall may lead to excessive narrowing of theairways <strong>and</strong> a loss of the maximum plateau of contraction found innormal ariways when bronchoconstrictor substances are inhaled 113 .Thickening of the airway wall by edema <strong>and</strong> structural changesamplifies airway narrowing due to contraction of airway smoothmuscle <strong>for</strong> geometric reasons 114 .Sensory nerves may be sensitized by inflammation, leading toexaggerated bronchoconstriction in response to sensory stimuli.Special MechanismsAcute exacerbations. Transient worsening of <strong>asthma</strong>may occur as a result of exposure to risk factors <strong>for</strong><strong>asthma</strong> symptoms, or “triggers,” such as exercise, air8 DEFINITION AND OVERVIEW