global strategy for asthma management and prevention
global strategy for asthma management and prevention
global strategy for asthma management and prevention
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
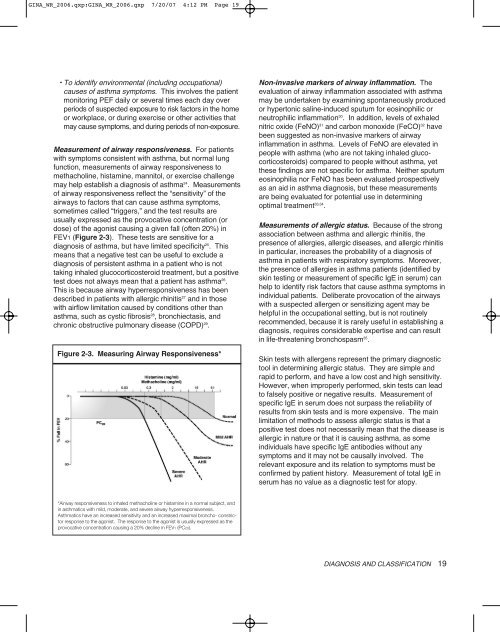
GINA_WR_2006.qxp:GINA_WR_2006.qxp 7/20/07 4:12 PM Page 19• To identify environmental (including occupational)causes of <strong>asthma</strong> symptoms. This involves the patientmonitoring PEF daily or several times each day overperiods of suspected exposure to risk factors in the homeor workplace, or during exercise or other activities thatmay cause symptoms, <strong>and</strong> during periods of non-exposure.Measurement of airway responsiveness. For patientswith symptoms consistent with <strong>asthma</strong>, but normal lungfunction, measurements of airway responsiveness tomethacholine, histamine, mannitol, or exercise challengemay help establish a diagnosis of <strong>asthma</strong> 24 . Measurementsof airway responsiveness reflect the “sensitivity” of theairways to factors that can cause <strong>asthma</strong> symptoms,sometimes called “triggers,” <strong>and</strong> the test results areusually expressed as the provocative concentration (ordose) of the agonist causing a given fall (often 20%) inFEV1 (Figure 2-3). These tests are sensitive <strong>for</strong> adiagnosis of <strong>asthma</strong>, but have limited specificity 25 . Thismeans that a negative test can be useful to exclude adiagnosis of persistent <strong>asthma</strong> in a patient who is nottaking inhaled glucocorticosteroid treatment, but a positivetest does not always mean that a patient has <strong>asthma</strong> 26 .This is because airway hyperresponsiveness has beendescribed in patients with allergic rhinitis 27 <strong>and</strong> in thosewith airflow limitation caused by conditions other than<strong>asthma</strong>, such as cystic fibrosis 28 , bronchiectasis, <strong>and</strong>chronic obstructive pulmonary disease (COPD) 29 .Figure 2-3. Measuring Airway Responsiveness*Non-invasive markers of airway inflammation. Theevaluation of airway inflammation associated with <strong>asthma</strong>may be undertaken by examining spontaneously producedor hypertonic saline-induced sputum <strong>for</strong> eosinophilic orneutrophilic inflammation 30 . In addition, levels of exhalednitric oxide (FeNO) 31 <strong>and</strong> carbon monoxide (FeCO) 32 havebeen suggested as non-invasive markers of airwayinflammation in <strong>asthma</strong>. Levels of FeNO are elevated inpeople with <strong>asthma</strong> (who are not taking inhaled glucocorticosteroids)compared to people without <strong>asthma</strong>, yetthese findings are not specific <strong>for</strong> <strong>asthma</strong>. Neither sputumeosinophilia nor FeNO has been evaluated prospectivelyas an aid in <strong>asthma</strong> diagnosis, but these measurementsare being evaluated <strong>for</strong> potential use in determiningoptimal treatment 33,34 .Measurements of allergic status. Because of the strongassociation between <strong>asthma</strong> <strong>and</strong> allergic rhinitis, thepresence of allergies, allergic diseases, <strong>and</strong> allergic rhinitisin particular, increases the probability of a diagnosis of<strong>asthma</strong> in patients with respiratory symptoms. Moreover,the presence of allergies in <strong>asthma</strong> patients (identified byskin testing or measurement of specific IgE in serum) canhelp to identify risk factors that cause <strong>asthma</strong> symptoms inindividual patients. Deliberate provocation of the airwayswith a suspected allergen or sensitizing agent may behelpful in the occupational setting, but is not routinelyrecommended, because it is rarely useful in establishing adiagnosis, requires considerable expertise <strong>and</strong> can resultin life-threatening bronchospasm 35 .Skin tests with allergens represent the primary diagnostictool in determining allergic status. They are simple <strong>and</strong>rapid to per<strong>for</strong>m, <strong>and</strong> have a low cost <strong>and</strong> high sensitivity.However, when improperly per<strong>for</strong>med, skin tests can leadto falsely positive or negative results. Measurement ofspecific IgE in serum does not surpass the reliability ofresults from skin tests <strong>and</strong> is more expensive. The mainlimitation of methods to assess allergic status is that apositive test does not necessarily mean that the disease isallergic in nature or that it is causing <strong>asthma</strong>, as someindividuals have specific IgE antibodies without anysymptoms <strong>and</strong> it may not be causally involved. Therelevant exposure <strong>and</strong> its relation to symptoms must beconfirmed by patient history. Measurement of total IgE inserum has no value as a diagnostic test <strong>for</strong> atopy.*Airway responsiveness to inhaled methacholine or histamine in a normal subject, <strong>and</strong>in <strong>asthma</strong>tics with mild, moderate, <strong>and</strong> severe airway hyperresponsiveness.Asthmatics have an increased sensitivity <strong>and</strong> an increased maximal broncho- constrictorresponse to the agonist. The response to the agonist is usually expressed as theprovocative concentration causing a 20% decline in FEV1 (PC20).DIAGNOSIS AND CLASSIFICATION 19