hipaa x12 version 5010 and ncpdp version d.0 frequently ... - eMedNY
hipaa x12 version 5010 and ncpdp version d.0 frequently ... - eMedNY
hipaa x12 version 5010 and ncpdp version d.0 frequently ... - eMedNY
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
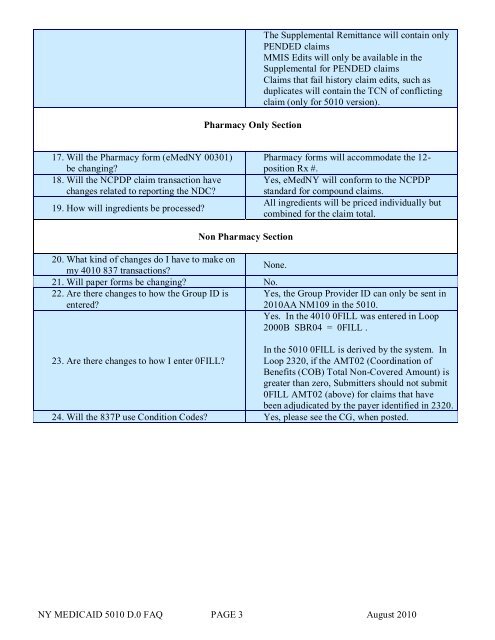
Pharmacy Only SectionThe Supplemental Remittance will contain onlyPENDED claimsMMIS Edits will only be available in theSupplemental for PENDED claimsClaims that fail history claim edits, such asduplicates will contain the TCN of conflictingclaim (only for <strong>5010</strong> <strong>version</strong>).17. Will the Pharmacy form (<strong>eMedNY</strong> 00301)be changing?18. Will the NCPDP claim transaction havechanges related to reporting the NDC?19. How will ingredients be processed?Pharmacy forms will accommodate the 12-position Rx #.Yes, <strong>eMedNY</strong> will conform to the NCPDPst<strong>and</strong>ard for compound claims.All ingredients will be priced individually butcombined for the claim total.Non Pharmacy Section20. What kind of changes do I have to make onNone.my 4010 837 transactions?21. Will paper forms be changing? No.22. Are there changes to how the Group ID is Yes, the Group Provider ID can only be sent inentered?2010AA NM109 in the <strong>5010</strong>.Yes. In the 4010 0FILL was entered in Loop2000B SBR04 = 0FILL .In the <strong>5010</strong> 0FILL is derived by the system. In23. Are there changes to how I enter 0FILL? Loop 2320, if the AMT02 (Coordination ofBenefits (COB) Total Non-Covered Amount) isgreater than zero, Submitters should not submit0FILL AMT02 (above) for claims that havebeen adjudicated by the payer identified in 2320.24. Will the 837P use Condition Codes? Yes, please see the CG, when posted.NY MEDICAID <strong>5010</strong> D.0 FAQ PAGE 3 August 2010