BCN (Retiree Faculty and Staff version) - MSU Human Resources
BCN (Retiree Faculty and Staff version) - MSU Human Resources
BCN (Retiree Faculty and Staff version) - MSU Human Resources
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
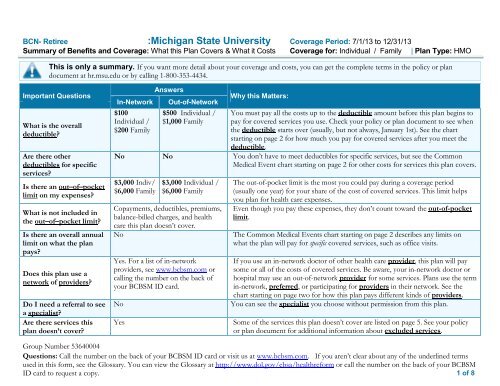
CommonMedical Event• Co-payments are fixed dollar amounts (for example, $20) you pay for covered health care, usually when you receive the service.• Co-insurance is your share of the costs of a covered service, calculated as a percent of the allowed amount for the service. For example, ifthe plan’s allowed amount for an overnight hospital stay is $1,000, your co-insurance payment of 20% would be $200. This may change ifyou haven’t met your deductible.• The amount the plan pays for covered services is based on the allowed amount. If an out-of-network provider charges more than theallowed amount, you may have to pay the difference. For example, if an out-of-network hospital charges $1,500 for an overnight stay <strong>and</strong>the allowed amount is $1,000, you may have to pay the $500 difference. (This is called balance billing.)• This plan may encourage you to use in-network providers by charging you lower deductibles, co-payments <strong>and</strong> co-insurance amounts.If you visit ahealth careprovider’s officeor clinicIf you have atestIf you needdrugs to treatyour illness orconditionFor moreinformationaboutprescriptiondrug coverage(if applicable),contact youremployer.Services You May NeedPrimary care visit to treat aninjury or illnessSpecialist visitOther practitioner office visitPreventive care/screening/immunizationDiagnostic test (x-ray, bloodwork)Imaging (CT/PET scans, MRIs)Generic or prescribed over-thecounterdrugsFormulary (preferred) br<strong>and</strong>namedrugsNonformulary (nonpreferred)br<strong>and</strong>-name drugsYour cost if you use aIn-NetworkProviderOut-of-NetworkProviderLimitations & Exceptions$20 Co-pay per visit Not Covered ---none---$20 Co-pay per visit 20% co-insurance afterdeductible---Prior authorization of out of networkprovider may be required ---$20 Co-pay per visit 20% co-insurance after Chiropractic care not covered. Priordeductibleauthorization of out of network provider maybe requiredNo Charge Not Covered Out of Network - select screenings have 20%coinsurance after deductibleNo Charge after 20% co-insurance after Prior authorization may be required. Labdeductibledeductiblecovered in full in <strong>and</strong> out-of-networkNo Charge afterdeductible$10 for 34-day supply$20 for 90-day supply$20 for 34-day supply$40 for 90-day supply$40 for 34-day supply$80 for $90-day supply20% co-insurance after Prior authorization may be requireddeductiblePrescription Drug Coverage provided through CVS/Caremark.90-daysupply only available through CVS/Caremark mail order <strong>and</strong> <strong>MSU</strong>Pharmacies.Prescription Drug Coverage provided through CVS/Caremark. Pricingis higher if generic option is available but not selected. 90-day supplyonly available via CVS/Caremark mail order or <strong>MSU</strong> PharmacyPrescription Drug Coverage provided through CVS/Caremark. Pricingis higher if generic option is available but not selected. 90-day supplyonly available via CVS/Caremark mail order or <strong>MSU</strong> Pharmacies.2 of 8
CommonMedical EventIf you haveoutpatientsurgeryIf you needimmediatemedicalattentionServices You May NeedFacility fee (e.g., ambulatorysurgery center)Physician/surgeon feesEmergency room servicesEmergency medicaltransportationUrgent careYour cost if you use aIn-Network Out-of-NetworkProviderProviderNo Charge after 20% co-insurance afterdeductibledeductibleLimitations & ExceptionsPrior authorization may be required/InNetwork weight reduction surgery 90%coinsurance after deductible up to $1000 permember; Out of Network – not covered/Infertility – 50% coinsurance after deductiblePrior authorization may be requiredNo Charge afterdeductible20% co-insurance afterdeductible$250 Co-pay $250 Co-pay Co-pay is waived if admitted or based onspecific signs <strong>and</strong> symptoms.20% co-insurance after 20% co-insurance after ---none---deductibledeductible$20 Co-pay per visit $20 Co-pay ---none---If you have ahospital stayFacility fee (e.g., hospital room)Physician/surgeon feeNo Charge afterdeductibleNo Charge afterdeductible20% co-insurance afterdeductible20% co-insurance afterdeductiblePrior authorization may be requiredPrior authorization may be requiredIf you havemental health,behavioralhealth, orsubstance abuseneedsIf you arepregnantMental/Behavioral healthoutpatient servicesMental/Behavioral healthinpatient servicesSubstance use disorder outpatientservicesSubstance use disorder inpatientservicesPrenatal <strong>and</strong> postnatal careDelivery <strong>and</strong> all inpatient servicesNo ChargeNo Charge afterdeductibleNo ChargeNo Charge afterdeductibleNo ChargeNo Charge afterdeductibleNo Charge afterdeductible20% co-insurance afterdeductible20% co-insurance afterdeductible20% co-insurance afterdeductible20% co-insurance afterdeductible20% co-insurance afterdeductiblePrior authorization may be requiredPrior authorization may be required/Additional days available beyond MedicarebenefitPrior authorization may be requiredPrior authorization may be requiredPrior authorization may be required for out ofnetwork care.Prior authorization may be required for out ofnetwork care3 of 8
CommonMedical EventIf you need helprecovering orhave otherspecial healthneedsServices You May NeedHome health careRehabilitation servicesHabilitation servicesSkilled nursing careDurable medical equipmentHospice serviceYour cost if you use aIn-Network Out-of-NetworkProviderProviderNo Charge after 20% co-insurance afterdeductibledeductible$20 Co-pay per visit 20% co-insurance afterdeductibleNot Covered Not Covered ---none---No Charge afterdeductible20% co-insurance afterdeductibleNo Charge afterdeductible20% co-insurance afterdeductibleNot coveredNo charge afterdeductibleLimitations & ExceptionsCombined in <strong>and</strong> out of network benefitslimited to 60 days per calendar year. Priorauthorization may be required out of network.Combined in <strong>and</strong> out of network benefitslimited to 60 days per calendar year. Priorauthorization may be requiredLimited to a maximum of 100 days perbenefit period. Prior authorization required.Prior authorization may be required/breastpump covered in full when authorized <strong>and</strong>obtained from Participating supplier.. Prior authorization required.If your childneeds dental oreye careEye examGlassesDental check-upNot Covered Not Covered ---none---Not Covered Not Covered ---none---Not Covered Not Covered ---none---4 of 8