Classification of Lupus Glomerulonephritis: Five Years Later
Classification of Lupus Glomerulonephritis: Five Years Later
Classification of Lupus Glomerulonephritis: Five Years Later
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
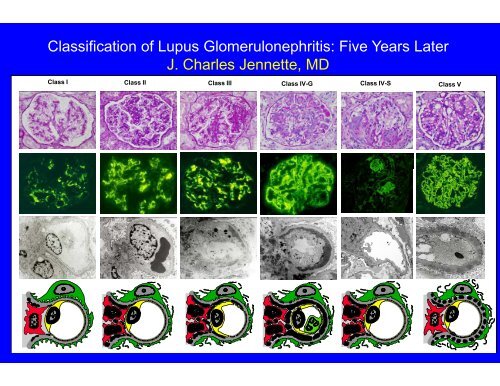
<strong>Classification</strong> <strong>of</strong> <strong>Lupus</strong> <strong>Glomerulonephritis</strong>: <strong>Five</strong> <strong>Years</strong> <strong>Later</strong>J. Charles Jennette, MDClass I Class II Class IIIClass IV-GClass IV-SClass V
Who Classified <strong>Lupus</strong> Nephritis?“Original WHO <strong>Classification</strong>”Buffalo, NY, 1974; or Geneva, 1975“Modified WHO <strong>Classification</strong>”ISKDC, Paris, 1980 (Churg and Sobin, 1982)“Modified WHO <strong>Classification</strong>”Churg 1995
Appel, Silva, Pirani, et al,Medicine 57:371-410, 1978(“according to a classificaation proposed by the WHO”)Class I. NormalNormal by LM, EM and IFClass II. Mesangial ChangesA. Minimal alterations(normal by LM, mesangial deposits by IF and EM)B. Mesangial Glomerulitis(mesangial hypercellularity)Class III. Focal and Segmental Prroliferative <strong>Glomerulonephritis</strong>l (50% glomeruli involved)Class V. Membranous <strong>Glomerulonephritis</strong>PureMixed Patterns (such as Class III associated with Class V)
Post card sent from Ed Lewis to Mel Schwrtz while Ed Lewiswas at the 1980 ISKDC Meeting
Jacob Churg, 1982 (based on modifications at the ISKDC):“WHO Morphologic <strong>Classification</strong> <strong>of</strong> <strong>Lupus</strong> Nephritis”I. Normala. Nil (by all techniques)b. Normal by LM, but deposits by EM or IFII. Pure Mesangial Alterations (Mesangiopathy)a. Mesangial widening/mild hypercellularityb. Moderate hyperrcellularityIII. Focal Segmental <strong>Glomerulonephritis</strong>a. Active necrotizing lesionsb. Active and sclerosing lesionsc. Sclerosing lesioonsIV. Diffuse <strong>Glomerulonephritis</strong>a. Without segmental lesionsb., c., and d. like a., b. and c. aboveV. Diffuse Membranous <strong>Glomerulonephritis</strong>a. Pureb. Associated withcategory IIc. Associated withcategory IIId. Associated withcategory IVVI. Advanced Sclerosing <strong>Glomerulonephritis</strong>
Jacob Churg, 1995:WHO Morphologic <strong>Classification</strong> <strong>of</strong> <strong>Lupus</strong> Nephritis (modified)I. NormalA. Nil (by all techniques)B. Normal by LM, but deposits by EM or IFII. Pure Mesangial Alterations (Mesangiopathy)A. Mesangial widening/mild hypercellularityB. Moderate hypercellularitylIII. Focal Segmental <strong>Glomerulonephritis</strong>A. Active necrotizing lesionsB. Active and scleerosing lesionsC. Sclerosing lesionsIV. Diffuse <strong>Glomerulonephritis</strong>A. Without segmeental lesionsB., C., and D. like A., B. and C. aboveV. Diffuse Membranous <strong>Glomerulonephritis</strong>A. PureB. Associated with category IIVI. Advanced Sclerosing <strong>Glomerulonephritis</strong>50% cut<strong>of</strong>f betweenIII and IVV-C and V-Ddeleted.
Problems with the WHO <strong>Lupus</strong> Nephritis <strong>Classification</strong>•Different versions with no <strong>of</strong>ficial peer-reviewed version•Lack <strong>of</strong> precise definitions <strong>of</strong> terms and criteria for different classes•Never validated for reproducibility•Unnecessary subcategorization based on mesangial hypercellularity•No guidance for classifying borderline lesions•Confusion about class III and claass IV•Uncertainty about how to classifysegmental necrotizing lesions•Different approaches to classifying mixed proliferative andmembranous lesions•Cumbersome designations for activity it and chronicityit
100Outcome <strong>of</strong> <strong>Lupus</strong> Nephritislity <strong>of</strong> Survivaal, %806040n=35WHO Class IV“WHO Class III (>50%)”Probabi202436WHOClass” Vc (>50%)” & Vd02 4 6 8 10 12 14 16 <strong>Years</strong>Korbet, Lewis, Schwartz, et al., Am J Kidney Dis 35:904-914, 2000
urvival , %Pr robabili ity <strong>of</strong> S10080604020n=352436Outcome <strong>of</strong> <strong>Lupus</strong> NephritisMost renal pathologists t would classifyall <strong>of</strong> these as class IVWHOWHO Class IV“WHO Class III (>50%)”Class” Vc (>50%)” & Vd02 4 6 8 10 121416<strong>Years</strong>Korbet, Lewis, Schwartz, et al., Am J Kidney Dis 35:904-914, 2000
ISN/RPS Working Group on the <strong>Classification</strong> <strong>of</strong> <strong>Lupus</strong><strong>Glomerulonephritis</strong>PATHOLOGISTS:Charles Alpers, U.S.A.Jan Bruijn, NetherlandsTerrence Cook, EnglandVivette D'Agati Agati, U.S.A.Franco Ferrario, ItalyAgnes Fogo, U.S.A.Gary Hill, ParisPrue Hill, AustraliaCharles Jennette, U.S.A.Lai-Ming Looi, MalaysiaLuiz Moura, BrazilMichio Nagata, JapanMelvin Schwartz, U.S.A.Surya Seshan, U.S.A.Jan J. Weening, NetherlandsCLINICIANS:Gerald Appel, U.S.A.James Balow, U.S.A.Ellen Ginzler, U.S.A.Lee Hebert, U.S.A.Norella Kong, MalaysiaPhillipe Lesavre, FranceMichael Lockshin, U.S.A.Hir<strong>of</strong>umi Makino, Japan
The <strong>Classification</strong> <strong>of</strong> <strong>Glomerulonephritis</strong> inSystemic <strong>Lupus</strong> Erythematosus RevisitedJan J. Weening, Vivette D. D’Agati, Melvin M. Schwartz, Surya V.Seshan, Charles E. Alpers, Gerald B. Appel, James E. Balow, Jan A.Bruijn, Terence Cook, Franco Ferrario, Agnes B. Fogo, Ellen M.Ginzler, Lee Hebert, Gary Hill, PrueHill, J. Charles Jennette, NorellaC. Kong, Philippe Lesavre, MichaelLockshin, Lai-Meng Looi, Hir<strong>of</strong>umiMakino21, Luiz A. Moura, Michio Nagata, on behalf <strong>of</strong> theInternational Society <strong>of</strong> Nephrologyand Renal Pathology SocietyWorking Group on the classification<strong>of</strong> lupus nephritisKidney Int 2004;65:521-530 and J Am Soc Nephrol, 2004;15:241-250
2004 ISN/RPS Consensus Conference on the <strong>Classification</strong> <strong>of</strong><strong>Lupus</strong> <strong>Glomerulonephritis</strong>Class IMinimal mesangiallupus glomerulonephritis (LGN)Class IIClass IIIClass IVMesangial proliferative LGNFocal LGN (involvinng < 50% <strong>of</strong> glomeruli)Diffuse LGN (involving 50% or > glomeruli)Class IVSClass IVGPredominantly segmentalPredoominantly globalClass VClass VIMembranous LGNAdvanced scleroticLGN (> 90% sclerotic glomeruli)
ISN/RPS <strong>Classification</strong> <strong>of</strong><strong>Lupus</strong> <strong>Glomerulonephritis</strong>Class I Class II Class IIIClass IV-GClass IV-SClass V
ISN/RPS <strong>Classification</strong> <strong>of</strong><strong>Lupus</strong> <strong>Glomerulonephritis</strong>Class I Minimal mesangial lupus glomeruloonephritis. Normal glomeruli by lightmicroscopy, but mesangial immune deposits by immun<strong>of</strong>luorescence.Normal histologyMesangial stainingfor IgGMesangial electrondense immunecomplex deposits
ISN/RPS <strong>Classification</strong> <strong>of</strong><strong>Lupus</strong> <strong>Glomerulonephritis</strong>Class II Mesangial proliferative lupus glomerulonephritis. Purely mesangialhypercellularity <strong>of</strong> any degree or mesangial matrix expansion by light microscopy, withmesangial immune deposits.There may be a few isolated subepithelial or subendothelial deposits visible byimmun<strong>of</strong>luorescence or electron microscopy,but not by light microscopy.SegmentalmesangialhypercellularityMesangial stainingfor IgGMesangial electrondense immunecomplex deposits
ISN/RPS <strong>Classification</strong> <strong>of</strong><strong>Lupus</strong> <strong>Glomerulonephritis</strong>Class III Focal lupus glomerulonephritis. Active or inactive focal, segmental orglobal endo- or extracapillary glomerulonephrritis involving
Class IV Diffuse lupus glomerulonephritis. Active or inactive diffuse, segmental or globalendo- or extracapillary glomerulonephritis involving 50% or more <strong>of</strong> all glomeruli, typically withdiffuse subendothelial immune deposits, with orwithout mesangial alterations. This class isdivided into diffuse segmental (IV-S) lupus nephritis when 50% <strong>of</strong> the involved glomeruli havesegmental lesions, and diffuse global (IV-G) lupus nephritis when 50% <strong>of</strong> the involvedglomeruli have global lesions. IV-S and IV-G aredivided into (A): active lesions, (A/C): activeand chronic lesions, and (C): chronic inactive lesions with scars.Global injury (IV-G)Extensivesubendothelialelectron denseimmune complexdepositsSegmental injury (IV-S)Less immunoglobulinMinor electronsubendothelialdense immunecomplexdeposits
ISN/RPS <strong>Classification</strong> <strong>of</strong> <strong>Lupus</strong> <strong>Glomerulonephritis</strong>Class V Membranous lupus glomerulonephritis. Global or segmental subepithelialimmune deposits or their morphologic sequelaae by light microscopy and byimmun<strong>of</strong>luorescence or electron microscopy, with or without mesangial alterations.A diagnosis <strong>of</strong> both Class III & Class V or Class IV & Class V is given when there arecombined lesions.Thick capillary wallSegmentalmesangialhypercellularityGlobal granularcapillary wallstaining for IgGSubepithelialimmune complexdeposits
ISN/RPS <strong>Classification</strong> <strong>of</strong><strong>Lupus</strong> <strong>Glomerulonephritis</strong>Class VI Advanced sclerosis lupus glomerulonephritis. 90% or more <strong>of</strong> glomeruliglobally sclerosed without residual activity. (ISN/RPS 2004)
Appel et al.78Churg82ISN/RPS04No lesion by LM,Class IClass IA No lupus GNIF or EMMesangial Class II A Class I Bdeposits but nohypercellularityMesangial Class II B Class II A,BhypercellularityFocal (50%) GNDiffuse (>50%)Proliferative GNClass IIIClass IVClass IVClass III A,B,CClass IV B,C,DMembranous Class V Class VMembranousplus ProliferativeClass V&IIIClass V&IVClass IV A,B,C,DClass VCClass VDClass IClass IIClass III A,A/C,CClass IVS A,A/C,CClass IVG A,A/C,CClass VClass III&VClass IV&V
Presenting clinical Manifestationss <strong>of</strong> Different ISN/RPS ClassesClinical I II IIIFeatureAsymptomatichematuriaAsymptomaticproteinurian=5 n=54 n=107 n=111 n=87 n=159 n=1840 19 222 4 6 5 040 42 257 6 13 0Nephrotic20 15 1740 38 65 11syndromeNephriticsyndromeAcute renalfailure0 20 3427 26 7 00 4 2Chronic renal0 0 0failureIV-G IV-S V VI18 16 2 04 8 8 89100 100 1000 100 100 100 100% % %% % % %Seshan S, Jennette JC. Renal disease in systemic lupus erythematosus with emphasis on classification<strong>of</strong> lupus glomerulonephritis: advances and implications. Arch Pathol Lab Med 2009;133:233-48.
Comparison <strong>of</strong> ISN/RPS Class IV Segmental (S) and Global (G) VariantsNajafiMittal (2004)Yokoyama(2001)(2004)# <strong>of</strong> patients 24 S 35 G 11 S 22G 6 S 17 GSC Cr S>G G>S G = SProteinuria G > S G > S G = SHTN G>S G>S NRWireloops G > S G > S NRFocal necrosis S>G S>G NRCellularity G > S G > S NRAc index G = S G = S G > SChr index S > G G = S G > SWorse outcome S > G G = S S > GTrendFollow-up 10yrs 55-38mth 95-214 mthHillSchwartzKimHiramatsu(2005) (2007) (2008) (2008)15 S 31G 22 S 22 Q39 G12 S 30G 14 S 41GG> S G=Q=S G = S G = SG > S G=Q=S G > S G > SG>S G=Q=S G=S G=SG > S G>Q>S NRS>G G>Q>S NRG > S NR G > SG > S G=Q>S G = S G = SG > S Q>S>G G = S G = SG > S Q>S>G G > S G > STrend10yrs 10yrs 10yrs 10yrs
<strong>Lupus</strong> Sever Segmental <strong>Glomerulonephritis</strong> (SSGN, similar but not identical to IV-S)veersus<strong>Lupus</strong> Diffuse Proliferatic <strong>Glomerulonephritis</strong> (DPGN, similar but not identical to IV-G)Number (%) <strong>of</strong> renal biopsy specimmens with the histologic finding:Behara VY, Whittier WL, Korbet SM, Schwartz MM, Martens M, Lewis EJ. Pathogenetic features<strong>of</strong> severe segmental lupus nephritis. Nephrol Dial Transplant. 2010;25:153-9.
<strong>Lupus</strong> Sever Segmental <strong>Glomerulonephritis</strong> (SSGN, similar but not identical to IV-S)veersus<strong>Lupus</strong> Diffuse Proliferatic <strong>Glomerulonephritis</strong> (DPGN, similar but not identical to IV-G)Percent <strong>of</strong> glomeruli per <strong>of</strong> renal biiopsy with the histologic finding:Behara VY, Whittier WL, Korbet SM, Schwartz MM, Martens M, Lewis EJ. Pathogenetic features<strong>of</strong> severe segmental lupus nephritis. Nephrol Dial Transplant. 2010;25:153-9.
<strong>Lupus</strong> Sever Segmental <strong>Glomerulonephritis</strong> (SSGN, similar but not identical to IV-S)veersus<strong>Lupus</strong> Diffuse Proliferatic <strong>Glomerulonephritis</strong> (DPGN, similar but not identical to IV-G)Peripheral IgG Staining by IFMSubendothelial Deposits by EMBehara VY, Whittier WL, Korbet SM, Schwartz MM, Martens M, Lewis EJ. Pathogenetic features<strong>of</strong> severe segmental lupus nephritis. Nephrol Dial Transplant. 2010;25:153-9.
ISN/RPS IV-S and IV-Gdoes not result in thesame classification asLewis-WHO III ≥ 50%and Lewis-WHO IVSchwartz MM, Korbet SM, Lewis EJ; Collaborative Study Group. The prognosis andpathogenesis <strong>of</strong> severe lupus glomerulonephritis. Nephrol Dial Transplant. 2008;23:1298-306.
ISN/RPS IV-S and IV-Gdoes not result in the same classification asLewis-WHO III ≥ 50%and Lewis-WHO IVRenal SurvivalISN/RPS IV-G (n=39)ISN/RPS IV-S (n=22)Lewis-WHO IIILewis “IV-Q” (n=22)≥ 50%(n=44)Schwartz MM, Korbet SM, Lewis EJ; Collaborative Study Group. The prognosis andpathogenesis <strong>of</strong> severe lupus glomerulonephritis. Nephrol Dial Transplant. 2008;23:1298-306.
Crescents are a marker <strong>of</strong> an aggressive variant <strong>of</strong> lupus GNincluding the Lewis-WHO III ≥ 50%Schwartz MM, Korbet SM, Katz RS, Lewis EJ. Evidence <strong>of</strong> concurrent immunopathologicalmechanisms determining the pathology <strong>of</strong> severe lupus nephritis. <strong>Lupus</strong> 2009;18:149-58.
Crescents are a marker <strong>of</strong> an aggressive variant <strong>of</strong> lupus GNincluding but not limited to the Lewis-WHO III ≥ 50%Schwartz et al “propose that diffuse global lupus GN with crescents is best describedas WHO class IV + WHO class III.”Schwartz MM, Korbet SM, Katz RS, Lewis EJ. Evidence <strong>of</strong> concurrent immunopathologicalmechanisms determining the pathology <strong>of</strong> severe lupus nephritis. <strong>Lupus</strong> 2009;18:149-58.
•The ISN/RPS <strong>Classification</strong>widespread acceptance and<strong>Five</strong> <strong>Years</strong> <strong>Later</strong>:System has garnereduse.•The ISN/RPS <strong>Classification</strong> System has resulted in ahigher level <strong>of</strong> interobserver reproducibility.•Multiple studies have found that lupus nephritis ISN/RPSClass IV-S has similar or better outcomes than lupusnephritis ISN/RPS Class IV-G.•Schwartz et al conclude thatt ISN/RPS class IV-S versusIV-G does not capture the major differences in prognosisand pathogenesis <strong>of</strong> severe lupus GN, and thus anotherround <strong>of</strong> classification adjustments is likely.
Anyone WHO ISN’t confusedreally doesn’t understand d thesituation.Edward R. Murrow