AT THE FOREFRONT OF OUR COMMUNITY
2011 Community Benefit Report: The University of Chicago Medical ...
2011 Community Benefit Report: The University of Chicago Medical ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
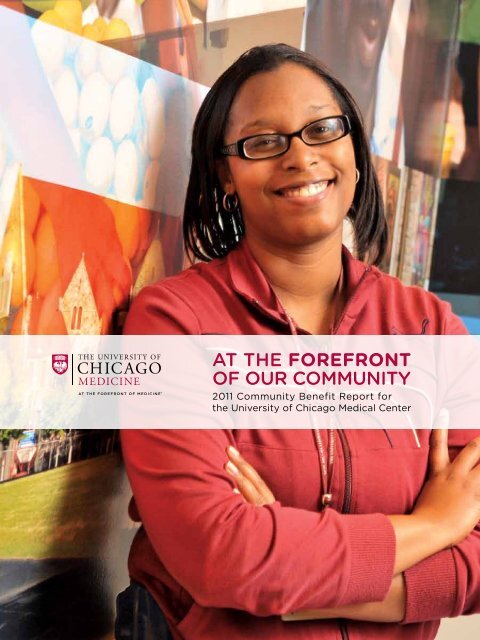
<strong>AT</strong> <strong>THE</strong> <strong>FOREFRONT</strong><strong>OF</strong> <strong>OUR</strong> <strong>COMMUNITY</strong>2011 Community Benefit Report forthe University of Chicago Medical Center
Our Commitment to the CommunityContentsAbout Us......................................................1Providing Benefits and Services...........2Creating Jobs for Chicago......................4Improving Urban Health..........................5~ Community Clinics~ Child Wellness~ Diabetes and Obesity~ Cancer PreventionVolunteering in Our Community.........15Investing in Important Research.........16Contributing to Global Health.............17We are pleased to introduce the University of Chicago Medical Center’s firstCommunity Benefit Report. This publication highlights the myriad ways wehave served the community through the clinical care we provide, as well as theprograms, medical education and research we support.The University of Chicago’s Biological Sciences Divisionand the Medical Center work together under the Universityof Chicago Medicine brand to teach and train futurephysicians, perform research and practice patient care. Ourreach and impact can be seen locally, regionally, nationallyand internationally — from the underserved residents of theSouth Side who get free flu shots to the earthquake victimsin Haiti we continue to monitor and treat.Our benefits to the community start with IRS-definedcomponents for health care providers: losses tied toMedicaid, charity care, education of health professionals,and contributions to community groups and programs.In addition, our commitment to service extends beyondthose categories. We absorb underpayments by Medicare andforgive bills for patients who are unable to pay. We supportmedical research, subsidize costly services such as ourpediatric trauma and burn units, provide volunteer work,and facilitate a number of other health-related activities.Also, each dollar spent by the University of Chicago MedicalCenter and the Biological Sciences Division supports the localeconomy. Nothing embodies both our economic impact and ourcommitment to the South Side better than the New HospitalPavilion, a 1.2 million-square-foot hospital that incorporates thelatest in technology with inpatient and operating-room design.Thanks in large part to this endeavor, the University ofChicago Medical Center has contributed tens of millionsof dollars in economic benefit as a major employer, job creatorand purchaser of goods and services. We are proud thatwomen- and minority-owned businesses have helped to buildthe New Hospital Pavilion, which is scheduled to open inJanuary 2013. We hope you will join us in the fall for a grandcelebration with our faculty and staff.We invite you to spend time reading the personal stories inthis report to learn about our many programs that may benefityou or someone you know.Sharon O’KeefePresident, University of Chicago Medical CenterKenneth S. PolonskyExecutive Vice President for Medical Affairs, University of ChicagoDean, Biological Sciences Division and Pritzker School of MedicineOn the cover: Patient advocate Semeca Johnson. Learn more about her story on Page 5.
About UsThe University of Chicago Medical Center comprises the Bernard Mitchell Hospital,Comer Children’s Hospital, the Duchossois Center for Advanced Medicine anda network of smaller clinics — all closely linked to the University of Chicago’sBiological Sciences Division and the Pritzker School of Medicine.When the University of Chicago Medical Center opened its doorsto the community in the fall of 1927, it had only two clinicaldepartments: medicine and surgery. Since then, the medicalcampus has grown to include 60 adult and 44 pediatric specialties.The Medical Center is consistently recognized as a leadingprovider of sophisticated medical care. University of Chicagophysician-scientists performed the first organ transplant andthe first bone marrow transplant in animal models, the firstsuccessful living-donor liver transplant, the first hormonetherapy for cancer and the first successful application of cancerchemotherapy. Its researchers also discovered REM sleep andwere the first to describe several of the stages of sleep. Twelveof the 87 Nobel Prize winners associated with the Universityof Chicago have received the prize for discoveries related tobiology or medicine.IN FY20119,500EmployeesINCLUDING568Licensed Beds(avg. 550 in service)74,359ER Visits700+Physicians800+Residentsand Fellows1,500Nurses146OrgansTransplanted1,572BabiesDeliveredNationally Ranked Medical CenterIn the U.S.News & World Report 2011–12 “Best Hospitals”survey, 12 adult and nine pediatric specialties at the Universityof Chicago Medical Center ranked among the top in thecountry. Those 21 top-ranked programs are more than at anyother institution in Illinois.Adult ProgramsDigestive disorders (9)Cancer (14)Pulmonology (19)Diabetes, Endocrinology (23)Kidney Disease (28)Neurology,Neurosurgery (29)Ear, Nose and Throat (30)Urology (33)Geriatrics (34)Cardiology, heart surgery (35)Gynecology (39)Orthopedics (43)Pediatric ProgramsGastroenterology (30)Neurology ,Neurosurgery (31)Neonatology (33)Pulmonology (35)Cancer (37)Urology (37)Diabetes,Endocrinology (42)Orthopedics (46)Nephrology (50)Medicaid Acute Care Daysfor Private Illinois Hospitals*1. University of Chicago Medical Center 42,7892. Northwestern Memorial Hospital 41,3113. Advocate Christ Medical Center 41,2264. Rush University Medical Center 38,0925. OSF St. Francis Medical Center (Peoria) 36,9316. Children’s Memorial Hospital 36,1607. Mount Sinai Hospital 32,7448. Loyola University Medical Center 29,0689. Resurrection St. Mary of Nazareth 22,98410. Advocate Lutheran General Hospital 21,667*Excluding normal nursery daysSource: Illinois Department of Healthcare and Family Services,for the state fiscal year ended June 30, 2010Contact usFor more information about the University of ChicagoMedicine’s programs and services or for an electronicversion of this report, please visit www.uchospitals.edu.To schedule an appointment, please call 773-702-1000.1
Providing Benefits and ServicesThe University of Chicago is home to world-class medical, research and teachingfacilities where innovation has been a hallmark and has helped position it as avaluable resource for the underserved populations of Chicago’s South Side.The University of Chicago Medical Center provides millionsof dollars in free or discounted medical care. It also subsidizesgovernment insurance programs, which reimburse at ratesmuch lower than the cost of care. In fact, nearly 56 percent ofits patients received medical coverage through governmentprograms in the fiscal year ended June 30, 2011. That’s about12 percent above the national average for the hospital industry.The University of Chicago Medical Center has formed valuablecommunity partnerships, trained future health professionalsand supported vital research to improve the health of theneighborhoods it serves. As the South Side’s largest privateemployer and one of the largest in Chicago, the university andthe medical campus add to the economic vitality of the region bycreating jobs and other opportunities for minorities and women.Altogether, the University of Chicago Medical Center and theBiological Sciences Division provided $237.1 million in totalbenefits and services to the community in fiscal 2011. Thatamounted to 21.4 percent of total operating revenues.$237.1 MILLIONCommunity benefits, services in fiscal 201121.4% of $1.11 billion total operating expensesUniversity of Chicago Medicine2MEDICAREPROGRAM LOSSES$100.7 MILLIONMedicare is a federalhealth insurance programfor people 65 and olderand for those withcertain disabilities. Thisfigure is the amountnot reimbursed by thegovernment-sponsoredprogram. As withMedicaid, Medicarepayments to health careproviders are significantlyless than the cost of care.MEDICAIDPROGRAM LOSSES*$37.7 MILLIONMedicaid is a federal-statehealth insurance programfor low-income andother needy people. Aswith Medicare, Medicaidpayments to health careproviders do not coverthe cost of care. TheUniversity of ChicagoMedical Center is oneof the top providersof Medicaid inpatientcare in Illinois.MEDICALEDUC<strong>AT</strong>ION*$44.9MILLIONTo help subsidizethe cost of trainingtomorrow’s doctors,the University ofChicago providesassistance withexpenses not coveredby tuition grantsand scholarships.MEDICALRESEARCH$23 MILLIONThis signifies theunreimbursedcost of supportingresearch on waysto prevent, detectand treat disease.CHARITYCARE*$14.4 MILLIONThis represents thecost of providingnecessary servicesto patientswith significantfinancial hardshipswho qualify for freeor discounted care.CASH AND IN-KINDCONTRIBUTIONS*$773,441This figure reflectsdonations to communityorganizations andsubsidies for services tomeet community needs.UNC<strong>AT</strong>EGORIZED<strong>COMMUNITY</strong>BENEFITS$3 MILLIONThis includes subsidizedhealth services,community activities, andsupport for volunteersand interpreters.UNRECOVERABLEP<strong>AT</strong>IENT DEBT$12.6 MILLIONHospitals absorb patientdebt when they cannotcollect expected paymentfor health services. This alsois known as “forgiven debt.”* An IRS-defined category of community benefit Components of community benefit for fiscal year 2011 (measured at cost). The numbers and data in this report wereprepared based on the Illinois Attorney General’s guidelines for fiscal year ended June 30, 2011.
In fiscal year 2011,the University ofChicago MedicalCenter and theUniversity’s BiologicalSciences Division:PROVIDED WELL-PAYING,STABLE EMPLOYMENTThe medical campus is the largestnon-government employer on theSouth Side and one of the largestin the city of Chicago.Employees: 9,565Payroll: $547 MILLIONPURCHASED GOODSAND SERVICESEach year, millions of dollars arespent on the goods and servicesneeded to provide health care.These dollars flow from themedical campus to vendors andbusinesses, spreading to the restof the local economy.Goods and Services:$341 MILLIONBUILT FOR <strong>THE</strong> FUTUREIn response to the rapid changesin medicine and technologyand to the needs of patients, theMedical Center has enhanced andupdated existing buildings, buildsnew facilities, and invests inmajor medical equipment. Theseinvestments stimulate the localeconomy through the creation ofjobs and the purchase of materials,equipment, and services.Construction and MedicalEquipment: $274 MILLIONTaylor ElectricCo. is a thirdgenerationfamily businessfounded in 1922,making it theoldest AfricanAmerican-ownedand -operatedconstructionfirm in Chicago.Martha Taylor(picturedwith NHPconstructionforeman RickTirado) servesas its presidentand CEO.SUPPORTED MINORITYAND WOMEN BUSINESSESThe New Hospital Pavilionproject is helping the MedicalCenter’s goal of granting atleast 40 percent of contracts tominority and women businessenterprises (MBEs and WBEs).That goal likely will be surpassed.Amount paid to MBEs andWBEs, as well as to womenand minority workers, on allconstruction and renovationprojects from 2001 throughJune 2011: $281.3 MILLIONSource: University of ChicagoMedical Center3
Creating Jobs for ChicagoUniversity of Chicago Medicine4For Taylor Electric Co., a family-ownedelectrical services company on theSouth Side of Chicago, the chanceto work on the University of ChicagoMedical Center’s New Hospital Pavilionwas just the kind of exposure it needed.A minority-owned business, Taylor Electric was contractedto install four emergency generators for the 1.2 millionsquare-foot,10-story hospital, which is scheduled to openin January 2013.“Working on the New Hospital Pavilion gave us a great opportunityto forge new relationships,” said Martha Taylor, president andCEO of Taylor Electric. “We were able to show the University ofChicago Medical Center what we can do, and as a result weare now working at several facilities on the medical campus.”Providing such opportunities for local businesses is acornerstone of the University of Chicago Medical Center’scommitment to strengthening the community. Capital spendingto modernize and build facilities generates millions of dollarsfor the local economy, as does purchasing goods and services.As an employer, the University of Chicago Medical Centerprovides stability and growth for the South Side, causing a rippleeffect throughout the region. More than 9,500 people workat the medical campus, which includes the Medical Centerand the University’s Biological Sciences Division (BSD). They,along with medical students, BSD undergraduates and medicalcampus visitors, add to the economic vigor of the South Side.As part of this community investment, the University ofChicago Medical Center is dedicated to creating economicopportunity for minorities and women. In 2001, it launched aninitiative to increase the number of minority- and women-ownedfirms doing business at the medical campus and to encouragethe use of minority and women workers by all contractors.Since then, through June 2011, $281.3 million has been paidon construction and renovation projects to such businesses andto minority and women contract workers.Nothing embodies this commitment more than the New HospitalPavilion, the University of Chicago’s latest major undertakingbenefiting the South Side. Since the start of construction in2009, the hospital project has encouraged and fostered theparticipation of minority and women business enterprises.“For all medical campus construction and renovation projects,we aim to grant a minimum of 40 percent of contracts tominority- and women-owned material suppliers, constructioncontractors and professional services firms,” said Joan Archie,executive director of construction compliance. “The NewHospital Pavilion will help us to meet, if not surpass, that goal forbringing economic benefit to local businesses and the economy.”ECONOMIC IMPACTThe University of Chicago commissioned AndersonEconomic Group to provide an independentassessment of how much the education, researchand patient-care activities of the BiologicalSciences Division (BSD) and the Medical Centercontributed to the local economy in fiscal year2010. The assessment included direct spending,such as on salaries, and indirect spending,as when those salaries circulate through theeconomy, but subtracted spending that wouldhave occurred even in the absence of the UCMCand BSD. Among Anderson’s findings:<strong>THE</strong> MEDICAL CENTER AND BSDUNIQUE CONTRIBUTION TO <strong>THE</strong> REGION:ST<strong>AT</strong>E<strong>OF</strong> ILCHICAGOREGION$869.9 MILLIONto the economy$260.9 MILLIONin household earningsof which$808.6 MILLIONto the economy$231.4 MILLIONin household earningsNEW HOSPITAL PAVILION WORKFORCEFrom 2009 through June 2011TOTAL: 1,809 constructionworkers earned $60.1 millionof which1,661 Illinois residentsearned $55.2 million746 minority & women workersearned $23.6 million699 Chicago residentsearned $20.8 million494 South Side residentsearned $11.1 million
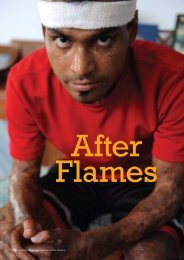
Improving Urban HealthSemeca Johnsonhelped launchthe patientadvocateprogram at theUniversity ofChicago MedicineComer Children’sHospital in 2009.Semeca Johnson understands thepeople she meets in her role as patientadvocate for the Medical Center’sadult and pediatric emergencydepartments. As a young adult with achronic disease, Johnson used to visitthe emergency room for her primarycare. Now she sees a physician closeto her home and gets regular care tobetter manage her condition.Johnson is passionate about placing patients “where theyneed to be for the best care.” On any given day, she meetsindividually with dozens of people as they wait for treatmentin the emergency department.“Many patients with chronic illnesses think of the emergencyroom as a clinic that is open 24 hours a day,” Johnson said.“We help patients understand the value of having a long-termrelationship with a regular doctor — a physician who knowsthem and can track and manage their disease or condition.”Studies show that increasing access to primary care reduces visitsto emergency rooms and hospitals. Patients who have an ongoingrelationship with a doctor generally see their health improvebecause they not only benefit from early diagnosis and treatmentbut also better understand the importance of wellness.Encouraging health and wellness and increasing access toquality care in under-resourced communities are pillarsof the Medical Center’s Urban Health Initiative (UHI).The South Side, a culturally rich and vibrant collectionof neighborhoods, has a critical need for primary care.Its population of about 869,000 people contends withdisproportionately high rates of treatable and often avoidablechronic conditions, such as diabetes, hypertension and asthma.Compounding these health disparities are difficult socioeconomiccircumstances and a widespread lack of health insurance.“We take a comprehensive and innovative approach toreducing health care disparities,” said Eric Whitaker, MD,executive vice president of strategic affiliations and associatedean for community-based research, who is responsible forleading UHI. “We believe UHI could eventually become amodel for urban health nationwide.”Using the medical campus as a hub, UHI connects residentsto health care through a coordinated network of providers.In addition to conducting community-based research,UHI also supports medical education and partners with civicleaders, faith-based groups and neighborhood organizationsto develop relationships that can foster long-term health andvitality on the South Side.When Johnson identifies someone who is visiting theemergency room with a non-urgent health issue, she seeksto connect the patient with a regular doctor. She offers toschedule an appointment at one of the clinics that partnerswith the University of Chicago Medical Center to provideprimary care and chronic disease management. Later, Johnsonwill follow up to ask how the medical visit went.“Ninety percent of the patients are pleased with the connections,”Johnson said. “They find the clinics very welcoming.”5
Improving Urban Health (continued)Family physicianDionna Brown, MD,recently beganher second yearin the REACHprogram. Sheworks at theChicago FamilyHealth Centerin Pullman.HIGHLIGHTS <strong>OF</strong> <strong>THE</strong>URBAN HEALTH INITI<strong>AT</strong>IVESouth Side Healthcare CollaborativeUHI focuses on preventive care by connecting adults andchildren with affordable, experienced doctors in the SouthSide Healthcare Collaborative, a network of more than 30community health centers, two free clinics and five localhospitals. In addition to offering routine medical services,many of the community-based health centers in the networkprovide social support, behavioral health, nutrition, dentaland pharmacy services.The University of Chicago Medical Center has implementedExtension for Community Healthcare Outcomes (ECHO),a teaching tool that uses video conferencing to train staff at theseclinics. In 2011, the Medical Center created ECHO programson treating hypertension and attention deficit hyperactivitydisorder as well as managing care for breast cancer survivors.social, cultural and civic resources available in 34 SouthSide communities. By connecting residents with services intheir neighborhoods, the Asset Census Project aims to helpparticipants learn more about services that promote wellnessand find quality health resources close to home.Repayment for Education to Alumniin Community HealthIn 2008, the University of Chicago established Repaymentfor Education to Alumni in Community Health (REACH)to encourage and enable Pritzker School of Medicinegraduates to practice on the South Side. REACH providesup to four years of financial support to help young physiciansrepay medical school debt while also making an impact inthe neighborhood where they received their education. Thedoctors work in Federally Qualified Health Centers or incommunity hospitals in the medical campus’ primary servicearea. Some also conduct research on how to improve healthcare delivery to medically underserved areas.Pipeline Programs for High Schooland College StudentsThe Pritzker School of Medicine inspires and preparestalented high school and college students to pursue careersin medicine and health-related research through fourinnovative “pipeline” initiatives: the Chicago AcademicMedicine Program, Pritzker School of Medicine Experiencein Research, Young Scientists Training Program and TrainingEarly Achievers for Careers in Health. Largely designed toattract minorities who are underrepresented in the medicaland scientific fields, these programs encourage students toaim for high levels of achievement and, eventually, to practicein medically underserved communities.South Side Health and Vitality StudiesTo better understand community health issues, the MedicalCenter and the University of Chicago have partnered withcommunity-based organizations to create the South SideHealth and Vitality Studies. This research focuses on howsocial and environmental factors in the community affecthealth and influence attitudes toward medical services.Information gathered from this project guides UHI in thedevelopment of programs, services and policies.One key study under way is the Asset Census Project, acomprehensive survey mapping all commercial, health care,$1.6MILLIONINVESTEDfor the UrbanHealth Initiative12NEIGHBORHOODSMAPPEDas part of the AssetCensus ProjectFor fiscal year ended June 30, 20112,371PEOPLECONNECTEDto a community orspecialty care clinicthrough UHI50STUDENTSINVOLVEDin pipeline programs6University of Chicago Medicine
Visit one of these locations to find a primarycare doctor. For more information, contactthe South Side Healthcare Collaborativeat 773.702.5668 or visituchospitals.edu/medicalhome6 Chicago Family HealthCenter - South Chicago9119 S. Exchange Ave. | 773.768.5000Special Services: Behavioral Health,Dentistry, OB/GYN, Pediatrics,Nutritional, AllScripts7 Chicago Family HealthCenter - Roseland120 W. 111th St. | 773.768.5000Special Services: OB/GYN,Pediatrics, Behavioral Health8 Chicago Family HealthCenter - Pullman556 E. 115th St. | 773.768.5000Special Services: Pediatrics,Dentistry, OB/GYN, AllScripts,Behavioral Health9 Christian CommunityHealth Center9718 S. Halsted St. | 773.233.4100Special Services: Behavioral Health,Dentistry, HIV, OB/GYN,Pediatrics, Podiatry10 Christian CommunityHealth Center364 Torrence Ave., Calumet City708.868.9457Special Services: OB/GYN,Pediatrics11 Frank Bearden, M.D.2011 E. 75th St., Suite 102773.752.2483Special Services: Diabetes12 Friend Family Health Center5843 S. Western Ave. | 773-434-8600Special Services: Pediatrics,Internal Medicine13 Friend Family Health Center800 E. 55th St. | 773.702.0660Special Services: Pediatrics, FamilyMedicine, Internal Medicine, OB/GYN, Confidential Teen Care,Pediatric Infectious Disease14 Friend Family Health Center5635 S. Pulaski Rd. | 773.585.3900Special Services: Pediatrics, OB/GYN19 Cottage View HealthCenter - Near North4829 S. Cottage Grove Ave.773.548.1170Special Services: Nutrition, Sub-Specialty Services (as needed)20 ACCESS South State FamilyHealth Center5050 S. State St., 2nd Floor773.624.2700Special Services: Cardiology,OB/GYN, Obstetrics21 TCA Health, Inc.1029 E. 130th St. | 773.995.6300Special Services: Optometry, Dentistry,OB/GYN, Pediatrics, Psychiatry,Behavioral Health/Substance Abuse,Internal/Family Medicine22 Mile Square Health Centerat South Shore7131 S. Jeffrey Blvd. | 312.996.2000Special Services: Adult/PediatricDentistry, Family Medicine, OB/GYN23 Mercy Family Health Center2525 S. Michigan Ave. | 312.567.2000Special Services: OB/GYN, Pediatrics,Internal Medicine24 Friend Family HealthCenter - Beethoven25 W. 47th St. | 773.702.0660Special Services: Pediatrics, InternalMedicine25 Chicago Family HealthCenter - Chicago Lawn3223 W. 63rd St. | 773.768.5000Special Services: Pediatrics, BehavioralHealth, Dentistry, OB/GYN26 Friend Family Health Center2436 W. 47th St. | 773.376.9400Special Services: Family Medicine,OB/GYN27 Chicago Family HealthCenter - East Side10536 S. Ewing Ave. | 773.768.5000Special Services: OB/GYN,Behavioral Health, Dentistry1 ACCESS Ashland FamilyHealth Center5256 S. Ashland Ave. | 773.434.92162 ACCESS Auburn-GreshamFamily Health Center8234 S. Ashland Ave. | 773.874.1400Special Services: Pediatrics,OB/GYN, Family Medicine3 Beloved CommunityFamily Wellness Center6821 S. Halsted St. | 773.651.36294 ACCESS Booker FamilyHealth Center654 E. 47th St. | 773.624.4800Special Services: Internal Medicine,OB/GYN, Family Medicine5 ACCESS Brandon FamilyHealth Center8300 S. Brandon Ave. | 773.721.7600Special Services: Family Medicine,OB/GYN, Asthma15 ACCESS Grand BoulevardFamily Health Center5401 S. Wentworth Ave.773.288.6900Special Services: Infection Control,Adult Rheumatology, Adult/Pediatric Cardiology, Adult/Pediatric Endocrinology, Adult/Pediatric Gastroenterology,Pediatric Neurology16 ACCESS at IllinoisEye Institute3241 S. Michigan Ave. | 312.949.777017 Komed Holman HealthCenter - Near North4259 S. Berkeley Ave. | 773.268.7600Special Services: Internal Medicine,Pediatric Medicine, Women’s Health,Ophthalmology, Oral Health,Podiatry18 Mile Square Health Centerat Bishop Plaza4630 S. Bishop Plz. | 312.996.2000Special Services: Family Medicine,OB/GYN, Eye Care28 Christian CommunityHealth Center901 E. Sibley Blvd., South Holland773.233.4100Special Services: Pediatrics29 CommunityHealth641 W. 63rd St. | 773.994.151530 ACCESS at Holy Cross2701 W. 68th St., 3-South773.434.4040Special Services: Behavioral Health,Family Medicine, OB/GYN,Pediatrics31 IMAN Health Clinic2744 W. 63rd St. | 773.434.4626Special Services: Family Medicine,Pediatrics32 Senior Health Center atSouth Shore7101 S. Exchange Ave. | 773.702.5700Special Services: Consultationsin Memory Center Assessment,Successful Aging for Frail Elders(SAFE) Clinic7
Improving Urban Health: Community ClinicsIn September 2010, Gwendolyn Gilmorewas one of the first patients to visitthe new CommunityHealth Englewoodclinic, just blocks from her home.“The staff here really listens to you,”said Gilmore, a 60-year-old senior careworker. “There are a lot of uninsuredpeople around here, and I tell them tocome on over.”In its first three months of operation, about 250 patientsvisited the Englewood clinic, which is open two half-days perweek and staffed predominantly by University of Chicagoresidents. In its first nine months, 1,020 uninsured patientsvisited the clinic. About a third of them were new patients.Twenty-eight of those patients were referred from theUniversity of Chicago Medical Center.During the same time, the Medical Center and theUniversity of Chicago’s Department of Medicine gave 1,302hours of resident time and 316 hours of faculty time to theEnglewood clinic, dedicated exclusively to the delivery ofdirect patient care. The services provided by the facility includehelping patients manage hypertension and diabetes — twocommon chronic conditions in the community.“We’re improving health literacy,” said Amber Pincavage, MD,then chief resident of internal medicine, now on faculty as oneof the internal medicine clerkship directors. She supervisesresidents at the clinic, a satellite site of CommunityHealth WestTown, the largest volunteer-based free clinic in Illinois. “Primarycare is a new concept for many uninsured patients who havealways relied on walk-in clinics and emergency rooms.”CommunityHealth West Town and Englewood are two offour free clinics staffed at least in part by students and medicalresidents from the University of Chicago. The other two —Washington Park Children’s Free Health Clinic and the MariaShelter — are led by Pritzker School of Medicine studentsunder the supervision of faculty volunteers.Pritzker medical students serve multiple roles in the fourclinics, such as counting medications or showing patients withdiabetes how to give themselves insulin injections, as well asconducting medical histories and physical exams overseen byfaculty volunteers. Medical residents serve as primary carephysicians to uninsured patients one half day per week.“These clinics offer uninsured or underinsured patients accessto health care they would otherwise not have,” said James1,020uninsured patients seenby University of Chicago residentsat the Englewood clinicin its first nine months4,000hours volunteeredby medical residentsat the Englewood clinic$50,000contributed by UHIto help sustain and expandthe Englewood clinicWoodruff, MD, associate dean of students for Pritzker, whooversees residents at the Englewood clinic. “You can think ofthese clinics as the safety net of the safety net.”Andrew Davis, MD, associate professor of medicine at theUniversity of Chicago and faculty adviser for the MariaShelter, views the volunteer work in clinics as a basicresponsibility for physicians in a nation where approximately50 million people don’t have access to health care.“It sensitizes students and residents to the calling of medicineand the social responsibility to promote health for all and notjust for those who can afford to pay,” Davis said.8University of Chicago Medicine
University of ChicagoMedicine volunteerphysicians and students,such as internal medicineresident James Kim,provide the bulk of medicalcare at the Community-Health Englewood clinic.Universityof ChicagoMedicineCampusS Halsted StFREE CLINICSCommunityHealthFounded in 1993, this nonprofit company is dedicatedto serving the uninsured in Chicago and its surroundingcommunities. CommunityHealth operates the West Townfacility and a satellite clinic in Englewood. The Englewoodclinic is staffed largely by residents and faculty from theUniversity of Chicago. University of Chicago students andfaculty support a weekly clinic at the West Town facility.1 West Town: 2611 W. Chicago Ave. | 773-395-99002 Englewood: 641 W. 63rd St. | 773-994-15153 Washington Park Children’sFree Health ClinicEvery Tuesday evening since 1999, a multipurpose room insidethe Chicago Youth Program headquarters has been convertedinto a clinic that provides primary and preventive care for children.5350 S. Prairie Ave. | 773-924-0220 ext. 1104 Maria Shelter ClinicEach Wednesday evening, Pritzker students and anattending physician provide medical care at the MariaShelter for homeless women and their children. The shelterwas founded in 1974 by Sister Margaret Ellen Traxler, aCatholic nun who spoke out on behalf of women’s rights.7320 S. Yale Ave. | 773-994-53509
Improving Urban Health: Child WellnessThanks to the Comer Children’s Hospital Mobile Medical Unit, nurse practitioner Pamela Beauduy is able to bringvaccinations, physical exams and education to Chicago Public Schools students who don’t have access to medical care.University of Chicago MedicineHours before children pounded downthe hallways, nurses had transformedselected Chicago Public Schoolsclassrooms into medical clinics withboxes of surgical gloves and standsof immunization-ready needles.Students tiptoed into their classrooms with crumpled consentforms in their hands to receive their shots. Some recoiled atthe sight of needles, but, in the end, they got their shots.Unvaccinated children not only run the risk of contractinga serious illness but also put schools at risks of outbreaksof preventable diseases such as measles or whooping cough,explained Kenneth Alexander, MD, professor of pediatricsand principal investigator on the Promoting AdolescentHealth at School program. Common obstructions that keepchildren from getting vaccinated include hard-to-decipherMOBILE CLINICIMPACT2010–11 SCHOOL YEARconsent forms, fears about side effects or lack of time ormoney to take children to a health care professional.Because 86 percent of Chicago Public Schools students onthe South Side come from low-income households, Alexanderdeveloped a cost-efficient, in-school immunization model tobring vaccines to South Side children. Using federal fundsalready allocated for children’s vaccines, Alexander and histeam provide state-mandated vaccines so children can stay inschool and stay healthy.“I feel that everyone should have access to in-school clinics,”said Jennifer Burns, CPNP, APN, medical director of thePediatric and Family Travel Clinic.Burns runs a different Medical Center vaccine outreachprogram. In addition to vaccinating kids, she and her teamare now providing consultation services to schools aboutcommunicative disease policies, outbreak prevention, and anumber of other topics.121SITEVISITS2,000PEDI<strong>AT</strong>RICP<strong>AT</strong>IENTS SERVED10
CHILD PROTECTIVE SERVICESIt’s Tuesday morning, and the Comer Children’s Hospital Child Protective Services (CPS)team is in the hospital’s conference room with representatives from the Illinois Department ofChildren and Family Services and the Chicago Children’s Advocacy Center. They gather eachweek to discuss potential cases of sexual and physical abuse, as well as neglect, in children.Those in attendance include Jill Glick, MD, a dedicated pediatrician and child abuse expert,who established CPS at the University of Chicago Medicine two decades ago to address theproblem of child maltreatment. As CPS medical director, Glick works alongside programmanager and social worker Lindsay Forrey, LCSW, and 10 licensed social workers to investigateand evaluate all possible child abuse and neglect cases seen in the hospital. Each year, more than400 children receive services from the CPS team.The staff also serves as a resource for the community on child welfare concerns and consultswith pediatricians on issues of abuse and neglect. The interdisciplinary team provides trainingand education for health professionals, local agencies and other community members.In 2000, Glick developed a model that called for more medical input in the assessment ofchild abuse for very young children. Because of her efforts, an expert medical review is nowmandated in Chicago for any child under age 3 with injuries that may signal abuse.This practice brings crucial expertise to community hospitals and child welfare agencies.“The program unites pediatric experts with child welfare professionals and law enforcementpersonnel to ensure all of these children receive comprehensive medical assessments, treatmentand follow-up care,” Glick said. “We want everyone involved in these cases to make the best,most informed decision.”“There’s a lot of false information out there,” Burns said.Vaccines have gotten better in the past few years, and childrenneed more vaccines to keep them safe and healthy, she added.The University of Chicago Medical Center’s mission ofpromoting wellness among children is a key element of soundpublic health practices, and its efforts extend beyond themedical campus. In addition to transforming schools intoclinics, the Medical Center uses a van to reach underinsuredand uninsured children from 2 to 18 years old.“This community outreach is rewarding because we provideservices that improve the health and future of our neighborhoodchildren and, thus, strengthen the community as a whole,” saidIcy Cade-Bell, MD, pediatrician and medical director for theMobile Medical Unit, which visits schools, day care centers,health fairs and other sites on the South Side.Felecia Morelon, CNA, senior program coordinator for themobile unit, described the 40-foot-long vehicle as a “clinic onwheels” that includes two fully equipped exam roomswhere three health care providers perform physicals,immunizations, treatment for acute injuries and illnesses,and health education sessions.During the 2010-11 school year, the mobile unit completed121 site visits and saw nearly 2,000 pediatric patients for clinicalcare and education on topics ranging from personal hygieneto sexually transmitted infections. Through the Teen Clinicand Foundations for the Future programs, 333 teens receivedconfidential adolescent services, sports physical exams, ormental health services. The Foundations for the Future programalso provides mental health education for students, parents,teachers and staff at Hyde Park Academy High School.“I have to turn down schools because we’re so in demand,”Morelon said, adding that the mobile unit has become evenmore important to families in need as the economy strugglesto recover from the recession. “For a lot of these kids, if theydidn’t see us, they wouldn’t have medical care.”400 CASESCONSULTED BY CHILD PROTECTIVESERVICES ANNUALLY2,843 CHILDRENVACCIN<strong>AT</strong>ED <strong>AT</strong> <strong>THE</strong> MEDICAL CENTER’SIMMUNIZ<strong>AT</strong>ION CLINIC AND <strong>AT</strong> SOUTH SIDESCHOOLS IN <strong>THE</strong> 2010–11 SCHOOL YEAR11
Improving Urban Health: Diabetes and ObesityReach-Outis an interactiveprogram in whichchildren learnabout goodnutritionand exercise.University of Chicago MedicineCountless campaigns have beenlaunched to steer schoolchildrentoward healthy habits, yet ratesof childhood obesity and diabetescontinue to soar. One promisingstrategy: Create programs thatare locally focused and tailored tothe culture of children who arebeing targeted.That approach inspired two child diabetes preventionprograms created by University of Chicago researchers.The two programs, Reach-Out and Power-Up, are siblingswith similar designs, goals and measures that target slightlydifferent populations and venues.To design the programs, researchers first listened to the community.The research team, led by Deborah Burnet, MD, professor ofmedicine and pediatrics, organized focus groups with overweightchildren and their parents to learn about their obstacles to improvinghealth and to gather ideas about the types of physical activityand classes that would appeal to them. The conversations laid thegroundwork for programs that would take the unique circumstancesof families on the South Side of Chicago into account.“They were good partners, they really liked working with us, andthey felt a sense of ownership,” Burnet said. “We didn’t just dropit in there; they worked with us to think about how it wouldwork in their setting.”For Reach-Out, parents and children ages 9 to 12 wererecruited to follow a 14-week program at a local YMCA, witheducation and activities that included grocery store tours,cooking classes, martial arts and yoga.For Power-Up, the program modified the Reach-Out scheduleto fit an after-school program for kindergarten through6th grade at Woodlawn Community School. Because theschool’s curriculum is structured around African heritage,traditional cultural activities such as drumming and dance wereincorporated into the course.Preliminary results from the Power-Up pilot study found asignificant drop in body mass index, frequently known as BMI,for overweight children, but not for obese kids, suggesting thatmore intense intervention may be needed. Researchers also haddifficulty reaching parents with the after-school format, andthe second pilot study incorporating text messaging to involveparents in the curriculum is under way.“There may be ways to use technology to help us personalizethings, and that’s where these programs are going,” Burnet said.12
Picture Good HealthIn the neighborhood of South Lawndale the mortalityrate from diabetes is 40 per 100,000 residents —nearly double the national rate. To reach thispredominantly Hispanic community, University ofChicago researcher Arshiya Baig, MD, decided towork through a central hub of the neighborhoodculture: the church.Picture Good Health/Imagínate una Buena Salud isan eight-week course designed to improve diabetesoutcomes for the Latino community. To educateparticipants on how to control diabetes through diet,exercise, blood-sugar monitoring and medication, theprogram uses culturally tailored materials and activities.Each session is led by a facilitator from the communitywho is trained by University of Chicago diabetes experts.The pilot study seeks to recruit 100 residents by theend of the year.“This community has high rates of diabetes and a lot ofbarriers to health care, including not being able to get into see their physician and not having health insurance,”said Baig, an assistant professor of medicine. “We thought wewould work through the churches and design a program ledby community members who are connected to resourceswithin the community. We taught trainers how to empowerpeople to change.”Kovler Diabetes CenterPart of the Kovler Diabetes Center’s mission is to help treatand prevent diabetes in South Side communities through acombination of educational, clinical and research efforts.Each year, Kovler physicians and educators reach thousandsof Chicagoans through health fairs, community seminarsand special events featuring speakers such as ChicagoBears quarterback Jay Cutler and best-selling author andTV medical expert Ian Smith, MD, a graduate of thePritzker School of Medicine.“We are delighted to have an impact at the national, regionaland local level for research and improving care of all kinds ofdiabetes,” said Lou Philipson, MD, PhD, director of the KovlerDiabetes Center and professor of medicine.Two unique clinical programs provide long-term care for youngdiabetes patients: Kovler Kids and InTransit. In addition toprograms on eating disorders and obesity, Kovler co-sponsorsseasonal farmers markets to provide access to healthy, freshfoods in urban food deserts, where grocery stores are scarce.On the research side, Kovler is part of the Diabetes Researchand Training Center, a National Institutes of Health-fundedprogram directed by Graeme Bell, PhD, professor of medicineand human genetics. This federally funded program includesan important outcomes and prevention component, which hassprouted a separate research center headed by Marshall Chinn,MD, professor of medicine.In addition, Kovler is affiliated with Improving Diabetes Careand Outcomes on the South Side of Chicago. The project isfunded by a $3.5 million grant from the Merck CompanyFoundation’s Alliance to Reduce Disparities in Diabetes and ledby Chin and Monica Peek, MD, assistant professor of medicine.The program works with six community health clinics on theSouth Side that serve primarily African-American and Hispanicpatients, including clinics in the ACCESS Community HealthNetwork. Initiatives such as the Diabetes Empowerment Program,in which educator-led classes provide culturally relevant advicefor diabetes management and care, are conducted at these clinics.Free monthly food drives and educational seminars are held incooperation with the Keep Loving Each Other Community FamilyLife Center. Another innovative pilot study uses text messaging toremind patients daily to take medication, conduct self-examinationsfor diabetes complications and check their blood sugar.“We’re trying to help people manage their diabetes wherethey are,” Peek said.NEARLY2 MILLIONAMERICANS WEREDIAGNOSED WITHTYPE 1 OR TYPE 2DIABETES IN 2010Diabetes costs willexceed $330 billionannually by 2034**Projection by Universityof Chicago research1/3<strong>OF</strong> AMERICANSARE OBESEIN <strong>THE</strong> CHICAGO AREA22% <strong>OF</strong>CHILDRENAGES 3 TO 7 ARE OBESEMORE THAN TWICE <strong>THE</strong>N<strong>AT</strong>IONAL AVERAGE.21% <strong>OF</strong> HIGH SCHOOLSTUDENTS ARE OVERWEIGHTcompared with 16% nationally.12% <strong>OF</strong> <strong>THE</strong> SOUTH SIDEPOPUL<strong>AT</strong>ION HAS DIABETEScompared with a 4% rate innon-Hispanic white neighborhoods.In some South Side communities,the rate is as high as 25%.13
Improving Urban Health: Cancer PreventionOn a drizzly Sunday afternoon undera tent on Chicago’s Southwest Side,Karen E. Kim, MD, MS, assembled ateam of volunteers to offer free flushots, blood pressure screenings andcancer education to several thousandpeople who had gathered for theChicago Latin American SoccerAssociation championship games.Spectators of all ages — from toddlers to a 104-year-oldwoman — and even some of the soccer players stopped bythe tent shared by the University of Chicago ComprehensiveCancer Center and the American Cancer Society.The event was part of a Comprehensive Cancer Centeroutreach program that offers culturally and geographicallycustomized information about cancer risk, prevention andtreatment. In fiscal year 2011, Kim’s group visited more than7,000 people at 36 community events.“Cancer is not homogeneous,” Kim said. “Not only are the risksdifferent for every racial and ethnic group, but there also aregeographic differences. For example, one out of every threecancer diagnoses in American women is breast cancer, andwe’ve found that the breast cancer death rate is much higher inChicago than in New York City or in the U.S. as a whole.”Community outreach and engagement are essential toaddressing the unequal burden of cancer carried by manyracial and ethnic groups, particularly in a major metropolitancity with a diverse population such as Chicago. Each ethnicgroup has its own health risks. Black men have an elevatedrisk of prostate cancer. Hispanic women experience a highincidence of cervical cancer. Asians and Pacific Islanders have aheightened chance of developing liver and stomach cancers.To reach the different ethnic groups, the program partnerswith community and faith-based organizations such as theApostolic Faith Church, American Indian Health Serviceof Chicago and the Asian Health Coalition. Through suchcollaborations, Kim’s group is able to not only tailor outreachefforts to each community, but also to teach communityleaders to become health advocates.Jennifer Burns, CPNP, director of the Pediatric and Family TravelClinic, administers a flu shot to a 104-year-old spectator at the2011 Chicago Latin American Soccer Association championshipgames. The free shots were part of a cancer outreach event.“Being a partner with the University of Chicago has beenan empowering experience,” said Asian Health CoalitionExecutive Director Edwin Chandrasekar. “I really appreciate thecommitment to recognizing the integral role the communityplays in the fight against cancer.”IN FISCAL YEAR 2011:DID YOU KNOW?University of Chicago Medicine36CANCEROUTREACHEVENTS7,000+<strong>COMMUNITY</strong>PARTICIPANTSEVENTSCONDUCTED IN:ENGLISHSPANISHCANTONESEKOREANVIETNAMESEAFRICAN AMERICANSare more likely to develop cancer thanany other racial or ethnic group.HISPANICShave a higher rate than whites of cancers associatedwith infection, such as uterine, cervical, liver andstomach cancers.ASIAN AMERICANShave the highest incidence of liver cancer.AMERICAN INDIANS/ALASKAN N<strong>AT</strong>IVEShave the highest kidney cancer death rate.14
Volunteering in Our CommunityMya Hardamon’s little voice wasclear over the sounds of volunteersraking planters and pulling weeds atVilla Guadalupe Senior Services onChicago’s Far South Side. “I can’tfind any worms!”“Well, they’re there,” replied Celia Hardamon, Mya’s mom.“You’ve got to dig, dig, dig.”With her husband, Antoine, who works in the Universityof Chicago Medical Center’s finance department in Darien,Hardamon and her family were just a few of the 264 volunteerswho came out in May 2011 for the ninth annual Day of Serviceand Reflection. Founded in 2002 by now-First Lady MichelleObama, the Day of Service has become a spring festival ofvolunteerism sponsored by the Office of Community Affairs,which supports the Medical Center’s external programming.This year, volunteers served at 17 South Side sites, includingsenior living facilities, food pantries and schools.The Medical Center and the Biological Sciences Divisionprovided financial and volunteer support for 53 communityevents in the fiscal year through June 2011. Key programsincluded the Day of Service and Reflection, the Bud BillikenParade, Real Men Cook and the Black Women’s Expo,which featured a booth about the South Side HealthcareCollaborative and other health topics.“We’re an important institution on the South Side of Chicago,”said Leif Elsmo, executive director for community andexternal affairs and volunteer services at the MedicalCenter. “So it’s important for us to be present in continualand meaningful ways that go beyond health care.”One way the Medical Center goes beyond conventionalmethods to tackle pressing health issues is throughCommunity Grand Rounds, which seeks to share theknowledge and research of the University of Chicago witharea residents. In the 2011 fiscal year, seven Grand Roundsevents were held in different neighborhoods, includingAuburn-Gresham, Englewood, South Chicago andWoodlawn. Each event tackled a different subject chosenby the community, such as sexual health, diabetes andasthma, or domestic violence.FAST FACTS FOR FISCAL YEAR 2011:Events53Number ofVolunteers1,272Economic Valueof Volunteers$140,965Total FinancialSupport$395,428The series kicked off in October 2010 with a production ofthe play “It Shoudda Been Me” at the Perspectives CharterSchool. Written by Doriane Miller, MD, associate professor ofmedicine and director of the Center for Community Healthand Vitality, the play addressed youth violence and depression.Miller was inspired to write a play after being struck by theresigned attitudes of her patients who had experienced youthviolence in their neighborhoods.“When I asked for information about these experiences andhow my young patients felt about them, their response madeit seem like a regular rite of passage,” Miller said. “However,many of these young people exhibited symptoms of anxietyand depression, not unlike people exposed to war.”Volunteers from the University of Chicago MedicalCenter serve up healthy samples at the 22nd RealMen Cook event celebrating Father’s Day.
Investing in Important ResearchD’Andrea Keysand her son,Joshua, interactby countingobjects andfollowing figuresin a book aspart of theThirty MillionWords project.Joshua Ryan Keys had a small devicetucked into the pocket of his shirt.It looked like a pedometer, but itcounted words he heard instead ofthe steps he took.The toddler wore the automated Language EnvironmentAnalysis system once a week as part of the Thirty Million Wordsproject led by Dana Suskind, MD, a surgeon and associateprofessor of surgery and pediatrics at the University of Chicago.The device records up to 16 hours of the words spoken to achild, verbal interaction with the child and a number of othersounds, such as those from a television.“Babies’ brains grow with language,” Suskind explained. But byage 3, children of lower socioeconomic status will have heard30 million fewer words than their more affluent counterparts.“Translational research that improves the health ofour community is our goal,” said Julian Solway, MD,director of the University of Chicago Institute forTranslational Medicine.Such community-based projects represent only one area ofthe University of Chicago’s research endeavors. At any giventime, more than 2,400 research projects are active acrossthe medical campus, ranging from finding ways to improvelanguage disparities to isolating cancer genes. University ofChicago experts conduct about 1,100 clinical trials each year,including about 400 cancer-specific trials.In addition to conducting research supported by government,industry and foundation sources, the University of ChicagoMedicine subsidized about $23 million in unreimbursedexpenses over the course of fiscal year 2011 to fund medicalresearch that benefited the community.Through the Thirty Million Words project, researchers visithomes of low-income parents to teach them more productiveways to talk with their children, empowering them to improvetheir children’s language development and educational outcomes.1,100clinical trialseach year2,400active research projectson the medical campusUniversity of Chicago MedicineSuskind’s project is one of many translational research projectson the medical campus, where researchers are turningscientific findings into programs that can help communitymembers. Translational scientists work with a variety ofexperts, including statisticians, psychologists, informaticsspecialists and others to find new ways to address health andwellness problems in neighborhoods more quickly.D’Andrea Keys, Joshua’s mother, said the Thirty MillionWords project has changed the way she interacts with her son.“Sometimes, I’ve had a long day, and I’m doing homework,and I just want to tell him to be quiet … but I don’t,” she said.“When Joshua does go on to preschool and kindergarten, he’sgoing to be an A student.”16
Contributing to Global HealthDays after a massive earthquake struckHaiti in January 2010, anesthesiologistRichard Cook bottle-fed a tiny2-week-old boy who was brought tothe University of Chicago MedicalCenter’s field hospital about 40 mileseast of Port-au-Prince. The child,whose mother was killed in the 7.0magnitude temblor, nearly died ofmalnutrition and dehydration. Hisfather had only sugar-water to feed him.During a follow-up visit in mid-2011 to the still-devastatednation, pulmonologist John Kress, MD, played with the samechild, now a toddler who has shown no lasting effects of hisnear starvation.The University of Chicago’s commitment to disaster reliefdid not end following the immediate response in 2010.“We didn’t want to jump in for the crisis and then bail out ofthe follow-up,” said disaster-medicine specialist ChristineBabcock, MD, associate professor of medicine.The Medical Center sent dozens of trained staff, including 20physicians and 16 nurses armed with 900 pounds of equipmentand supplies, to Haiti at a cost of nearly $500,000 — notincluding volunteer time. That effort continued long after theimmediate crisis, necessitating an additional investmentof more than $60,000. The second wave of outreach beganin August 2010, when volunteers returned to the countryto teach teams of Haitians how to manage health issues at adisplaced persons camp. The camp and the surrounding regionhad far fewer cholera infections and deaths than most of Haitiduring the nationwide cholera outbreak that began in October2010. Talks are under way about an ongoing clinical andeducational presence at a new hospital being built outsidePort-au-Prince by Partners in Health, a global health organization.The Medical Center’s response to such crises is coordinatedby the Global Health Initiative (GHI), which was created inJuly 2008 to tap the University of Chicago’s vast intellectualresources and apply them across the globe. GHI’s mission isto reduce health disparities and improve medical carelocally and globally.Lessons learned on the South Side of Chicago can be appliedto work with disadvantaged populations, and lessons learnedby GHI in resource-poor countries can help disadvantagedpopulations in Chicago and across the United States.For example, a project led by Funmi Olopade, MD, associatedean for global heath, compares the genetic heritage and socialstresses affecting women in Nigeria and African-Americanwomen on the South Side of Chicago to understand the roles ofnature and nurture in certain types of breast cancer. Knowledgegained from this project will be tested in a clinical trial designedto improve treatment of aggressive, early onset breast cancersthat are common on the South Side.Richard Cook, MD, professor of anesthesia and critical care, feeds a baby at the field hospital in FondParisien, Haiti. The following year, the boy’s father brought him back to the field clinic to thank theUniversity of Chicago team. The toddler is pictured (inset) with John Kress, MD, associate professorof medicine and director of the Medical Intensive Care Unit.17
address area5841 S. Maryland Ave.Chicago, IL 60637SERVING CHICAGO SINCE 1927