Greetings from the Chief Nursing Officer
Winter/Spring 2013 (PDF) - University of Chicago Hospitals
Winter/Spring 2013 (PDF) - University of Chicago Hospitals
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
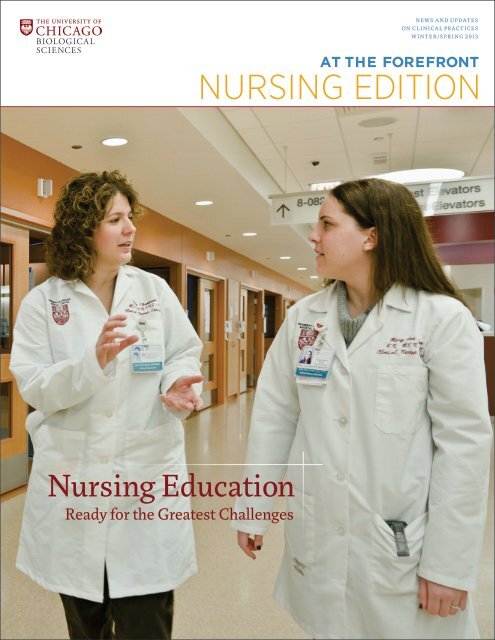
AT THE FOREFRONT NURSING EDITIONW IN T ER /SPR ING 2013 U N I V ER SI T Y OF CHICAGO MEDICIN E 3<strong>Nursing</strong> Education: Ready for <strong>the</strong> Greatest ChallengesBY AMY ALDERMAN | STAFF WRITERMonths of planning and training by<strong>the</strong> Center for <strong>Nursing</strong> ProfessionalPractice and Research (CNPPR) helpedmake for a smooth transition at <strong>the</strong>Center for Care and Discovery.From <strong>the</strong> early days of last summerthrough <strong>the</strong> weeks following <strong>the</strong>February 23 Patient Move Day, a teamof 20 in CNPPR labored to help prepare aworkforce of more than 2,300 people.“We’re a small group, but we’ve beensmall and mighty to get <strong>the</strong> job done,”said Clinical Nurse Educator Mary AnnStokas, RN, MSN, OCN.Headed by <strong>Nursing</strong> Education ManagerEmily Lowder, RN, PhD, NE-BC, andDirector of <strong>the</strong> Center for <strong>Nursing</strong>Professional Practice and ResearchKa<strong>the</strong>rine Pakieser-Reed, RN, PhD,<strong>the</strong> group of educators and specialistsdivided and conquered <strong>the</strong> technologyand infrastructure of <strong>the</strong> new hospitalpavilion based on <strong>the</strong>ir expertise.“As a group, we’re really strong toge<strong>the</strong>r,”Lowder said. “When you have newindividuals working on new equipment to30-year veterans using telemetry for <strong>the</strong>first time, nurse educators are <strong>the</strong> peoplewho are on <strong>the</strong> front line, and <strong>the</strong> pointpeople for implanting that technology.”For example, Stokas serves as a clinicalnurse educator for <strong>the</strong> Oncology CareCenter. Her experience as a consultant andmentor helped bridge <strong>the</strong> research behind<strong>the</strong> curricula and <strong>the</strong> teaching of clinicaland non-clinical staff on <strong>the</strong> new systemsat <strong>the</strong> Center for Care and Discovery.Perioperative Services Clinical NurseSpecialist Rena Thompson, APN, MSN,CNS-BC, gave employees an overview of<strong>the</strong> operating rooms, which include <strong>the</strong>new Image Stream interfacing system.Seeing clinical and non-clinical stafftake to <strong>the</strong> new systems made <strong>the</strong> workworthwhile, Thompson said.“In some of <strong>the</strong> classes, I saw people’sfaces light up,” she added. “To me, thathas been great to see.”During some sessions, nurse educators andspecialists trained 200 people per day.“We relied heavily on CNPPR to helppave <strong>the</strong> way into <strong>the</strong> Center for Care andDiscovery, and <strong>the</strong>y showed us that <strong>the</strong>ywere more than ready for <strong>the</strong> task,” saidchief nursing officer, Debra Albert, RN,MSN, MBA, NEA-BC, vice president ofPatient Care Services, and Patient MoveDay chief commanding officer.The many opportunities to walk <strong>the</strong>floors and learn about <strong>the</strong> new surroundingspaid off, said Nastassia Gurganus,RN, a procedures nurse who works inprep and recovery.“I was happy because we got moreexposure to <strong>the</strong> facility where <strong>the</strong> suppliesare, and <strong>the</strong> equipment I’ll need. That’smy priority,” she added.Outfitting clinical staff with leading-edgetechnology and skills at <strong>the</strong> new hospital isjust one of <strong>the</strong> many behind-<strong>the</strong>-scenesinitiatives that clinical nurse educatorsand clinical nurse specialists have led since<strong>the</strong>ir department centralized in 2005.<strong>Nursing</strong> education has trained nonclinicalstaff, including those <strong>from</strong> security,valet and food services, on wayfinding andon how to use equipment, such as <strong>the</strong>automated external defibrillator.“Seeing non-clinical staff understandhow to use an AED and how it doesn’t justapply to treating people at a hospital, Ithink it empowers people,” Stokas said.Outside of preparing for <strong>the</strong> newhospital, <strong>the</strong> CNPPR team spreads itsindividual strengths across <strong>the</strong> MedicalCenter, <strong>from</strong> on-boarding new staff tocompleting annual competencies of over1,500 nurses, nursing assistants and ORand ER technicians. Clinical nurseeducators constantly work in tandemwith advanced practice nurses, includingclinical nurse specialists on evidencebasedpractice in all units in inpatient,pediatrics and adult care.Emily Lowder, RN, PhD, NE-BC, center, with Michele Ackerman, RN, MA, left, Senior Hospital OperationsAdministrator, and Elise Lauderdale, RN, MSN, OCN on Patient Move Day. Photo by Harvey Tillis“You have that ability to learn <strong>from</strong>each o<strong>the</strong>r, and build resources toge<strong>the</strong>r,”Lowder said. “I think that’s where wedraw a lot of benefits.”
AT THE FOREFRONT NURSING EDITIONW IN T ER /SPR ING 2013 U N I V ER SI T Y OF CHICAGO MEDICIN E 5Great moments in our historyPhotographed are: A. J. Carlson,E. O. Jordan, Frank Billings, R. Lillie,B. C. H. Harvey, R. R. Bensley, andWilliam Rainey Harper.1892 University of Chicago opens.Founding President William RaineyHarper envisions a medical schooland a hospital.1898 Harper forms an affiliationwith Rush Medical College forclinical training of medical students.1927 Billings Hospital opens with215 beds, housing Departments ofMedicine, Surgery and Pathology.University of Chicago MedicalSchool opens October 31, forgeslinks with <strong>the</strong> University’s basicsciences departments.1930 Bobs Roberts MemorialHospital opens, with 80 pediatricbeds.1931 Chicago Lying-in Hospital, with140 beds, opens on <strong>the</strong> Universityof Chicago campus. Also, <strong>the</strong>McElwee-Hicks Hospital opens.1953ArgonneCancerResearchHospitalopens.1961 Goldblatt Pavilion opens,for outpatient services.1967 Wyler Children’s Hospitalopens with 100 beds.1977 Surgery-Brain ResearchInstitute opens; includes 17operating rooms and extensiveresearch space.1983 The Bernard A. MitchellHospital is dedicated, with 468beds. The new Chicago Lying-inHospital opens.1996 Duchossois Center forAdvanced Medicine opens.2005 Comer Children’s Hospitalopens.2009 The Gwen and Jules KnappCenter for Biomedical Discoveryopens.2013 The Center for Care andDiscovery opens to patients. Thenew hospital pavilion is <strong>the</strong> singlelargest health care investment on<strong>the</strong> South Side.Nurses on Patient Move Day: From Mitchell and DCAM to <strong>the</strong> Center for Care and Discovery
AT THE FOREFRONT NURSING EDITIONW IN T ER /SPR ING 2013 U N I V ER SI T Y OF CHICAGO MEDICIN E 7Theorists, CON T I N U ED F ROM PAGE 6Kristen Swanson, RN, PhD, FAANSwanson Theory of CaringKristen Swanson emphasizes that nursesbring with <strong>the</strong>m a body of professionalknowledge. The dean of University ofNorth Carolina at Chapel Hill School of<strong>Nursing</strong>, Swanson has investigatedpregnancy loss extensively since <strong>the</strong>1980s and has developed <strong>the</strong> SwansonTheory of Caring.Like Watson, Swanson believes <strong>the</strong>goal of a nurse is not necessarily to curepatients. Ra<strong>the</strong>r, a nurse seeks to bringabout well-being in patients by engagingin “informed caring,” in contrast to <strong>the</strong>care family and friends typically provide.That’s possible because nurses arearmed with scientific understanding andexperience in <strong>the</strong>ir field.Nurses must believe in <strong>the</strong>ir patients’ability to look forward to a meaningfulexistence, seeking to understand eventsin <strong>the</strong>ir patients’ lives through <strong>the</strong>ir eyes.They must also express to patients that<strong>the</strong>y are available, assisting in <strong>the</strong>ir careand enabling <strong>the</strong>m to help <strong>the</strong>mselves.For more information about Swanson, goto https://www.mc.vanderbilt.edu/root/vumc.php?site=evidencebasedpractice&doc=40293Virginia Henderson, RN, MANeeds TheoryVirginia Henderson frames <strong>the</strong> nurseas an extension of a patient’s will.Henderson, who passed away in 1996,maintains a considerable influence in <strong>the</strong>field of nursing: The American NursesAssociation refers to Henderson as a“modern legend” and Indianapolis is hometo <strong>the</strong> Virginia Henderson International<strong>Nursing</strong> Library.Like Orem, Henderson emphasizes <strong>the</strong>need for nurses to help patients care for<strong>the</strong>mselves once again. She lists 14 basicfunctions and activities with whichnurses assist patients, such as breathing,eating, sleeping, worship and recreation.Her definition of nursing is notable as oneof <strong>the</strong> first to gain widespread acceptance.It is <strong>the</strong> “unique function of <strong>the</strong> nurse,” shesaid, “to assist <strong>the</strong> individual, sick or well,in <strong>the</strong> performance of those activitiescontributing to health or its recovery (orto a peaceful death) that he would performunaided if he had <strong>the</strong> necessary strength,will or knowledge.” She adds that <strong>the</strong> nurseshould “do this in such a way as to help(<strong>the</strong> patient) gain independence as rapidlyas possible.”For more information about Henderson,go to http://currentnursing.com/nursing_<strong>the</strong>ory/Henderson.html.Doro<strong>the</strong>a Orem, RN, MSN EdSelf-Care Deficit <strong>Nursing</strong> TheoryThe late Doro<strong>the</strong>a Orem describes nursingas an “art,” a “helping service” and a“technology” enabling patients to take careof <strong>the</strong>mselves. Orem spent more than twodecades in <strong>the</strong> field of nursing and nursingeducation before she developed herSelf-Care Deficit <strong>Nursing</strong> Theory.According to Orem, a nurse’s rolecan be “wholly compensatory,” “partlycompensatory,” or “supportive-educative,”depending on <strong>the</strong> severity of <strong>the</strong> patient’scondition. Patients who can care for<strong>the</strong>mselves completely do not requirenurses or may only need <strong>the</strong>m to provideadvice and instructions for that care.When <strong>the</strong>y are unable to take care of<strong>the</strong>mselves, patients acquire what Oremdescribes as a “self-care deficit,” at whichpoint <strong>the</strong> nurse’s role is “compensatory,”meaning this nurse gives care to patientsthat <strong>the</strong>y would provide <strong>the</strong>mselves if<strong>the</strong>y were healthy enough to do so.Read more about Orem athttp://currentnursing.com/nursing_<strong>the</strong>ory/self_care_deficit_<strong>the</strong>ory.html
AT THE FOREFRONT NURSING EDITIONW IN T ER /SPR ING 2013 U N I V ER SI T Y OF CHICAGO MEDICIN E 8Critical Care Outreach Team Makes Early Lifesaving CallsBY AMY ALDERMAN | STAFF WRITERA group of six critical care nurses armedwith eagle-eye vision for what are oftenunrecognizable predictors of cardiac arrestamong high-risk patients are on <strong>the</strong> job at<strong>the</strong> University of Chicago Medicine.UCM has a strong history with providingrapid response to changing patientconditions. The initial team, in 2005, wasreferred to as <strong>the</strong> Medical EmergencyTeam (MET). This transitioned to <strong>the</strong>Rapid Response Team (RRT) in 2008.Now, in 2013 <strong>the</strong> team has evolved to <strong>the</strong>Critical Care Outreach (CCO) team that issolely dedicated to providing rapidresponse calls. The CCO is tasked withspotting <strong>the</strong> subtle traits of appendingcrisis and assisting nurses and physicianswith treatment before <strong>the</strong> need to call a“Dr. Cart” (A.K.A. Code Blue) arises.“We are giving nurses and physiciansano<strong>the</strong>r pair of eyes and ears,” saidPatient Care Manager Jenny Taylor, RN,BSN, MS, CCRN, RN-BC. “Respondingearly on to <strong>the</strong> changing patient condition —this affords us time for appropriateassessments and interventions that canmake a huge difference for <strong>the</strong> patient.”The Critical Care Outreach (CCO) Team’sultimate goal is to prevent cardiac arrests<strong>from</strong> happening outside <strong>the</strong> ICU.“In 2011 and 2012, 28 percent of <strong>the</strong> cardiacarrests at UCM happened outside of <strong>the</strong>ICU. We hope with <strong>the</strong> CCO nursing teamin place, we can decrease that numbersignificantly,” said Meredith Borak, RN,MSN, quality resuscitation consultant.There are triggers that nurses identifyto activate an RRT, such as increasedrespiratory rate, chest pain, or mentalstatus changes, but <strong>the</strong> CCO nurses usecriteria to round on specific patients.Those patients include ICU transfers,prior Rapid Response Team patients,and patients about whom <strong>the</strong> charge nurseis most concerned.Aside <strong>from</strong> <strong>the</strong>se triggers, nurses andphysicians should also trust <strong>the</strong>ir instinctsand call <strong>the</strong> Critical Care Outreach Team“if <strong>the</strong>y just feel something is off with <strong>the</strong>irpatients but <strong>the</strong>y can’t place what it is,”Taylor said.“I think we needed to bridge <strong>the</strong> gapbetween <strong>the</strong> ICU and general floors,” saidMiquela Duran-McConnell, RN, CCRN,who transitioned <strong>from</strong> <strong>the</strong> MICU to <strong>the</strong>Critical Care Outreach Team.Previously, rapid response calls wereanswered by patient care managers andpatient care support nurses. With <strong>the</strong>expansion of <strong>the</strong> medical center and basedon <strong>the</strong> utilization of rapid response, it wasdecided that a dedicated team shouldsupport <strong>the</strong>se 24/7 calls.Director of Critical Care Iliana Staneva,RN, MSN, MBA, CCRN, NEA-BC, whowas instrumental in getting this team inplace, said, “The need was clear.” “Weneeded a separate team,” she said. “Thesymptoms of mortality aren’t always easilyrecognizable early on. To prevent <strong>the</strong>m,you need to have a trained team to roundon patients early on.”Miquela Duran-McConnell,RN, CCRN, checks CamillaWhitaker’s lungs two daysafter <strong>the</strong> Rapid ResponseTeam was called to herroom in Mitchell when shehad difficulty breathing.Photo by Amy AldermanCritical Care Educator Pat Gwizdalski, RN,BSN, CCRN, was instrumental in <strong>the</strong>orientation process to help prepare <strong>the</strong>mfor <strong>the</strong>ir new role. Preliminary data show<strong>the</strong> team already is making a positiveimpact on patients, and critical careoutreach/rapid response calls haveincreased since <strong>the</strong> team has been in place,said Borak.“It is early, but we can already tell <strong>the</strong>difference,” Borak said. “The team is veryprofessional and adamant about explainingwhat <strong>the</strong>y feel needs to be done for <strong>the</strong>patient. When you go back and look at <strong>the</strong>steps <strong>the</strong>y’ve taken — <strong>the</strong>y’ve been spot on.”Svetlana Modylevskaya, RN, BSN, startedwith <strong>the</strong> Critical Care Outreach Team inmid-January after working for an agencyin various ICUs for several years.In addition to working with nurses andphysicians, Modylevskaya feels she is apatient advocate, intervening to help avoidcardiac arrests <strong>from</strong> happening on <strong>the</strong>floors outside of any ICUs. “I feel I amguiding my patients through a critical timeusing my critical thinking skills,” she said.To activate an RRT, dial 147 and requestan RRT/CCO to a particular room. Formore information about <strong>the</strong> team, contactTaylor at jennifer.taylor@uchospitals.edu.
AT THE FOREFRONT NURSING EDITIONW IN T ER /SPR ING 2013 U N I V ER SI T Y OF CHICAGO MEDICIN E 9Witt Honored for Excellencein Radiation Therapy<strong>Nursing</strong> AchievementsBY JEFFREY BISHKU-AYKUL AND MARY STROKASTAFF WRITERSClinical Research Nurse Mary Ellyn Witt,RN, MS, AOCN, has been named <strong>the</strong>winner of <strong>the</strong> 2013 Oncology <strong>Nursing</strong>Society’s Excellence in Radiation Therapy<strong>Nursing</strong> Award, and smiles are in order.Specializing in caring for head and neckcancer patients, Witt has focused ondental preservation for patients andsurvivors who have undergone radiation,which can cause rampant tooth decay.“I have always felt my strongest asset wasbeing a patient advocate,” said Witt, whofirst worked at <strong>the</strong> University of ChicagoMedicine <strong>from</strong> 1976 to 1981, <strong>the</strong>n cameback to stay in 1994. “I haven’t done it atMary Ellyn Witt, RN, MS, AOCN. Photo byMegan E. Doherty<strong>the</strong> bedside for many years, but it isamazing what you can do by just askingquestions and making positive changeswith your nursing practice.”In <strong>the</strong> last decade, Witt has noted,<strong>the</strong> increase in <strong>the</strong> number of head andneck cancer survivors has presented newchallenges. Among <strong>the</strong>m: ensuringthat patients who have undergonesuccessful radiation <strong>the</strong>rapy maintaina healthy mouth.“Our number of survivors has grownand so have <strong>the</strong>ir survivorship needs,”Witt said.A survey Witt conducted in 2008revealed that only about one in 10 patientsis a regular user of a nighttime fluoridetray — a mouthpiece that helps deliverextra doses of fluoride to preserve teeth.The research led her to conclude thatmerely providing patients with <strong>the</strong>written steps necessary to maintain oralhealth did not guarantee <strong>the</strong>ir compliance.Instead, “<strong>the</strong> relationship between <strong>the</strong>patient, oncology team, and <strong>the</strong> dentalhygienist should begin immediatelyfollowing a cancer diagnosis.”Her findings were published lastOctober in a continuing education articlein Registered Dental Hygienist magazine,garnering praise <strong>from</strong> dentists, as wellas hygienists.Anil Lal, executive administrator ofUniversity of Chicago Medicine’sDepartment of Radiation and CellularOncology, lauded Witt’s accomplishments.“Mary Ellyn’s work speaks for <strong>the</strong> qualityand uniqueness of our head and neckprogram,” Lal said. “The departmentis honored to have nursing that not onlyprovides good quality care but alsodevelop innovative practices andcontributes to research.”“It is amazing what youcan do by just asking questionsand making positive changeswith your nursing practice.”Mary Ellyn Witt, RN, MS, AOCNHer work has also gained internationalrecognition, leading her to present lastyear at <strong>the</strong> European Oncology <strong>Nursing</strong>Conference in Geneva, Switzerland.Despite all of <strong>the</strong> attention, Wittremains humbled.“I never thought this little survey backin 2008 would send me to Switzerland orlead to a publication in a dental hygienistjournal,” she said.Witt will receive <strong>the</strong> Excellence inRadiation Therapy <strong>Nursing</strong> Award at <strong>the</strong>38th annual ONS Congress conferenceon Thursday April 25 in Washington, D.C.
AT THE FOREFRONT NURSING EDITIONW IN T ER /SPR ING 2013 U N I V ER SI T Y OF CHICAGO MEDICIN E 10A view of a typical operating room suite inside Kiev’s heart center. Photo by Andrey Ibragimov, RN, BSN, CNORA Heart-to-Heart with Ukranian NursesBY MEGAN E. DOHERTY | STAFF WRITERA University of Chicago Medicinenurse spent some of his recent vacationtime opening bridges to his Ukrainiancounterparts. General Operating Roomnurse Andrey Ibragimov spent two daysof an October trip home to Russia touring<strong>the</strong> Ukrainian National Cardio-ThoracicCenter in Kiev, <strong>the</strong> capital of Ukraine.General operating room nurse AndreyIbragimov, RN, BSN, CNOR, stands outside<strong>the</strong> Ukranian National Cardio-Thoracic Centerduring his October visit. Photo courtesy ofAndrey IbragimovThe modern center, open in 2007,is small, specialized and instructional forboth its similarities and differences toits large American cousins. “They areactually living <strong>the</strong> lean philosophy,” saidIbragimov, RN, BSN, CNOR.Our year-old kaizen initiative isstandard practice at <strong>the</strong> Ukrainian center,he explained. “They are trying to be wisewith all <strong>the</strong>ir supplies and resources. It’senlightening that people can do so muchwith so little.”While 60 types of surgeries areroutinely performed at <strong>the</strong> University ofChicago Medical Center every day, Kiev’sis a low-volume facility, topping off at amaximum of 10 heart cases a day.Since Ukrainian nurses lack supportstaff like surgical technicians to help in<strong>the</strong> operating room or environmentalservices staff to clean rooms, <strong>the</strong> nursesdo it all. These multitaskers also toilwithout <strong>the</strong> convenience of electronicmedical health records or internal email.“In a way, it’s bare bones. The amount ofresources we have here is really amazing,”Ibragimov said.Ibragimov, 29, immigrated to <strong>the</strong> UnitedStates <strong>from</strong> Russia in 2005 to become anurse and advance his education. Hejoined <strong>the</strong> Medical Center last year andwill earn his Bachelor of Science in<strong>Nursing</strong> in 2013.While in Kiev, he fielded numerousquestions <strong>from</strong> his Ukrainian counterparts,who were curious to know howthings work in Chicago. He presented <strong>the</strong>mwith a book of U.S. thoracic surgeryguidelines as a gift.“The director of <strong>the</strong> heart center wouldlove to bring some staff here to establishsome sort of education for <strong>the</strong>m, likespending a day in one of our ORs, shadowingus and seeing how <strong>the</strong>y couldstreamline <strong>the</strong>ir own processes,”Ibragimov said. “I would love for <strong>the</strong>m tocome here, and even show <strong>the</strong>m how weconduct nursing research.”
AT THE FOREFRONT NURSING EDITIONW IN T ER /SPR ING 2013 U N I V ER SI T Y OF CHICAGO MEDICIN E 11DAISY Award WinnersHumbled by NominationsBY AMY ALDERMAN AND MEGAN E. DOHERTYSTAFF WRITERSUniversity of Chicago Medicinedirect-care nurses have been honored by<strong>the</strong>ir colleagues and patients as winnersof <strong>the</strong> Diseases Attacking <strong>the</strong> ImmuneSystem (DAISY) Foundation. One nurseis honored each month with a surprisepresentation at his or her department.Every DAISY is given a sculpture called“The Healers Touch,” a DAISY lapel pinand a certificate. Cinnamon rolls are anextra DAISY perk. The founders of <strong>the</strong>organization require all award presentationsto have cinnamon rolls, a favoritefood of J. Patrick Barnes, <strong>the</strong> founders’ lateson, who suffered <strong>from</strong> a clotting disorder,Idiopathic Thrombocytophenic Purpura.Anna “Apple” Umali, RNWhen Anna “Apple” Umali, RN, learnedthat <strong>the</strong> family of a dying man might notbe able to see him before he passed, sheraised funds and arranged for travel andfood for his family — all in one day. In amatter of hours, <strong>the</strong> patient’s family wason a train <strong>from</strong> Sou<strong>the</strong>rn Illinois toChicago, and <strong>the</strong>y were able to see him“just in <strong>the</strong> nick of time,” she said.Holding “The Healers Touch” sculpture, SayedSaad Iqbal, RN, BSN, is <strong>the</strong> December winner of<strong>the</strong> DAISY Award. Photo by Megan E. Doherty“We really helped that last moment ofhis to be full of love and family,” Umalisaid. This is one of many reasons HaroldInocencio, RN, nominated Umali for<strong>the</strong> February DAISY Award.Umali forms long-lasting relationshipswith her patients and <strong>the</strong>ir families, andshe continues to dedicate her time as avolunteer nurse across internationalborders. She volunteered in <strong>the</strong> Philippinesafter <strong>the</strong> tsunami and in orphanages inKenya and Cambodia. This June,she’ll accompany a team led by J.P. Kress,MD, associate professor of medicine anddirector of <strong>the</strong> MICU, in a clinical volunteertrip to Haiti.“She goes above and beyond her nursingduties and responsibilities,” Inocenciosaid. “She continues to touch lives andmake a difference in her family andpatients’ lives.”Syed Saad Iqbal, RN, BSNA nurse resident for a little more thanhalf a year, Syed Saad Iqbal, RN, BSN,calls work in <strong>the</strong> multispecialty unit at<strong>the</strong> University of Chicago Medicine his“home-away-<strong>from</strong>-home.”Patient Care Manager Sandra Armstrong,RN, MS, who worked with Iqbal in 3SWat <strong>the</strong> time he received his nomination,says he’s a great influence in creating ahomey atmosphere.“He’s just one of those upbeat people,”Armstrong said. “He has a great smile.He does his job very well, but I don’t thinkthat’s it. It’s that personality that winsyou over. He’s kind and a little bit funny.”Iqbal was nominated for <strong>the</strong> DAISYaward by a patient who said he made herfeel comfortable, not only through hispain management, but also through hispositive attitude.Being nominated by a patient washumbling. “I have this very emotionalattachment to this institution. Wherever Iam or whatever I am, it’s because of thisUniversity. This is my opportunity togive back,” he said.Patient Care Manager Aurika Savickaite, RN, BSN, left, celebrates with <strong>the</strong> February DAISY award winner,MICU Staff Nurse Anna “Apple” Umali, RN. Photo submitted by Ka<strong>the</strong>rine Pakieser-Reed, RN, PhD
AT THE FOREFRONT NURSING EDITIONW IN T ER /SPR ING 2013 U N I V ER SI T Y OF CHICAGO MEDICIN E 12SAVE THE DATE: APRIL 12The University Of Chicago Medicine Department Of <strong>Nursing</strong>2013 NURSING RESEARCH AND EVIDENCE-BASEDPRACTICE SYMPOSIUMGwen and Jules Knapp Center for Biomedical Discovery900 E. 57th St., Chicago, IL 60637The University of Chicago Medicine Annual <strong>Nursing</strong> Research and Evidence-BasedPractice Symposium is a forum for UCM nurses and o<strong>the</strong>r health care professionals, andnurses <strong>from</strong> external organizations. The purpose is to share research and evidence-basedpractice experiences, disseminate study findings, and network with colleagues with <strong>the</strong>ultimate goal of improving <strong>the</strong> quality and safety of patient care, and enhancing healthcare delivery.The keynote speaker,Melanie CreaganDreher, RN, PhD,FAAN, is <strong>the</strong> JohnL. and Helen KelloggDean and Professorof <strong>the</strong> College of<strong>Nursing</strong> at Rush University in Chicago. Inaddition to her role as dean, Dreher hashad a distinguished research career as <strong>the</strong>principal investigator of several community-basedstudies examining <strong>the</strong> healthand development of women and childrenin Jamaica. She will present “Creating aCulture for Evidence-based Practice.”Speaker KathleenCalzone, RN, PhD,APNG, FAAN, isa senior nursespecialist in <strong>the</strong>genetics branch of<strong>the</strong> Center for CancerResearch at <strong>the</strong> National Cancer Institutein Be<strong>the</strong>sda, Maryland. She is a pastpresident of <strong>the</strong> International Society ofNurses in Genetics. Calzone will speakon <strong>the</strong> topic “The Genomic <strong>Nursing</strong>Science Blueprint.”Click here to learn more: http://home.uchospitals.edu/pdf uch_034114.pdfThe cost to attend <strong>the</strong> symposium is $95 for University of Chicago Medicine and BiologicalSciences Division employees.Nurses WeekEvents May 6–10E ACH DAY OF T HE A N N UA LCELEBR ATORY W EEK H A S A T HEME.DETA ILS W ILL BE A N NOU NCED ONT HE IN T R A N ET HOME PAGE,http://home.uchospitals.eduMonday, May 6Unit Celebrations and RecognitionDAISY AwardTuesday, May 7Acknowledging accomplishments of <strong>the</strong> past yearNurses completing education, certifications,Publications, Conference PresentationsAPN Presenation: APN Roles: Past, Presentand FutureHuening AwardWednesday, May 8<strong>Nursing</strong> Grand RoundsHow to get started in publishingBlessing of HandsThursday, May 9Celebrating <strong>Nursing</strong> Excellence<strong>Nursing</strong> AwardsFriday, May 10Movie Day“Nurses: If Florence Could See Us Now”Discuss <strong>the</strong> NDNQI Survey With Your TeamPatient care managers are encouragedto discuss <strong>the</strong> results of <strong>the</strong> NationalDatabase of <strong>Nursing</strong> Quality Indicatorssurvey with nurses in <strong>the</strong>ir unit.Having an open discussion will addbackground to <strong>the</strong> data compiled in <strong>the</strong>NDNQI survey, said Ka<strong>the</strong>rine Pakieser-Reed, RN, PhD, director of <strong>the</strong> Centerfor <strong>Nursing</strong> Professional Practiceand Research.“That discussion is your best way ofinterpreting <strong>the</strong> survey,” Pakieser-Reedsaid. Discussing <strong>the</strong> survey results alsoprovides an opportunity for an opendialogue about <strong>the</strong> changes that havetaken place since it was conductedlast fall. Following <strong>the</strong>se discussions,patient care managers should create anaction plan based on <strong>the</strong> results andcomments <strong>from</strong> staff, Pakieser-Reed said.CongratulationsCheers to Lindsay Gregory, RN, MSN, CPN,Emily Lowder, RN, PhD, NE-BC, andFatenah Issa, MS, for having <strong>the</strong>ir abstract“There’s an App for That: Bringing <strong>Nursing</strong>Education to <strong>the</strong> Bedside” accepted for aposter presentation in April at <strong>the</strong>American Society of PeriAnes<strong>the</strong>siaNurses conference in Chicago.