Vascular Access in Hemodialysis: the 2006 KDOQI ... - Network 6
Vascular Access in Hemodialysis: the 2006 KDOQI ... - Network 6
Vascular Access in Hemodialysis: the 2006 KDOQI ... - Network 6
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Vascular</strong> <strong>Access</strong> <strong>in</strong> <strong>Hemodialysis</strong>:<strong>the</strong> <strong>2006</strong> <strong>KDOQI</strong> Guidel<strong>in</strong>es UpdateLesley C. D<strong>in</strong>widdie MSN, RN, FNP, CNNThanks to <strong>the</strong> SEKC for <strong>the</strong>gracious <strong>in</strong>vitation and honorto present <strong>the</strong> <strong>KDOQI</strong> andSurgical Aspects of:IMPROVING ARTERIALVENOUS FISTULA RATESTHROUGH AN INTEGRATEDVASCULAR ACCESS PROGRAM
Learn<strong>in</strong>g Objectives• The Learner will be able to:1. Provide an overview of <strong>the</strong> history and purposeof <strong>the</strong> <strong>KDOQI</strong> guidel<strong>in</strong>es2. Review post-operative methods to maximizematuration of AV Fistulae3. Describe how stenosis formation occurs with<strong>in</strong><strong>the</strong> access, and identify ways that it can bepreventedQ1. The <strong>KDOQI</strong> guidel<strong>in</strong>es should be<strong>in</strong>terpreted as:• A. strict protocols for cl<strong>in</strong>ical practice <strong>in</strong> <strong>the</strong> care ofall ESRD patients• B. recognized standards of cl<strong>in</strong>ical care for ESRDpatients• C. evidence-based statements to guide caregivers <strong>in</strong>cl<strong>in</strong>ical management of CKD patients• D. measures that will be used for pay forperformance• E. all of <strong>the</strong> above
Overview of <strong>the</strong> NKF-DOQI Guidel<strong>in</strong>es• In <strong>the</strong> early 1990s, <strong>the</strong> National KidneyFoundation recognized significant differences <strong>in</strong>ESRD care across <strong>the</strong> nation and around <strong>the</strong>world. Much of this care was less than optimal.Multi-discipl<strong>in</strong>ary workgroups were selected toreview <strong>the</strong> literature, build consenses of optimalcl<strong>in</strong>ical practice and create guidel<strong>in</strong>es <strong>in</strong> fourcategories of ESRD:<strong>Vascular</strong> <strong>Access</strong>Peritoneal DialysisAdequacy of Dialysis andAnemiaOverview of <strong>the</strong> <strong>KDOQI</strong> Guidel<strong>in</strong>es• The <strong>Vascular</strong> <strong>Access</strong> Multi-Discipl<strong>in</strong>aryWorkgroup started <strong>the</strong> process <strong>in</strong> 1995 with<strong>the</strong> first publication <strong>in</strong> 1997 of <strong>the</strong> DialysisOutcome Quality Initiative <strong>Vascular</strong> <strong>Access</strong>Guidel<strong>in</strong>es• These were first reviewed and revised <strong>in</strong> 2000and were published <strong>in</strong> 2001 as <strong>the</strong> KidneyDisease Outcomes Quality Initiative for<strong>Vascular</strong> <strong>Access</strong> with substantive changes <strong>in</strong><strong>the</strong> Monitor<strong>in</strong>g Section only
Overview of <strong>KDOQI</strong> Guidel<strong>in</strong>es• In <strong>the</strong> <strong>in</strong>terim, new guidel<strong>in</strong>es have been writtenfor:NutritionBone Disease ManagementChronic Kidney DiseaseCardiovascular Disease• The latest revision of <strong>the</strong> orig<strong>in</strong>al <strong>Vascular</strong><strong>Access</strong> guidel<strong>in</strong>es have been published as asupplement to <strong>the</strong> July <strong>2006</strong> AJKD and <strong>in</strong> bookform and can be viewed athttp://www.kidney.org/PROFESSIONALS/kdoqi/guidel<strong>in</strong>e_upHD_PD_VA/<strong>in</strong>dex.htm.Overview of <strong>the</strong> <strong>KDOQI</strong> Guidel<strong>in</strong>es• The format is different and <strong>the</strong> rationale is anexhaustive explication of <strong>the</strong> Work Group’sdecisions re <strong>the</strong> Guidel<strong>in</strong>es andRecommendations• Four areas of <strong>the</strong> <strong>Vascular</strong> <strong>Access</strong> Guidel<strong>in</strong>eswere <strong>in</strong>tensively reviewed and revised with <strong>the</strong>rema<strong>in</strong>der updated.
Mission Given - Limited Revision:• Select Areas of Most importance1. Role of ve<strong>in</strong> imag<strong>in</strong>g (mapp<strong>in</strong>g) <strong>in</strong> foster<strong>in</strong>g <strong>the</strong>AV fistula <strong>in</strong>itiative.2. Ca<strong>the</strong>ter <strong>in</strong>fection: Treatment and prevention3. Ca<strong>the</strong>ter dysfunction: role of thrombolytics4. Role of surveillanceMission Given - Limited Revision:• Update <strong>the</strong> literature on <strong>the</strong> o<strong>the</strong>r Guidel<strong>in</strong>es• Differentiate Guidel<strong>in</strong>es fromRecommendations• Propose Research Topics• Simplify: previous <strong>KDOQI</strong> for vascular accesshad 38 separate guidel<strong>in</strong>es with subhead<strong>in</strong>gs.
Major Changes to VA-<strong>KDOQI</strong> <strong>2006</strong>• The Previous 38 CPG were condensed <strong>in</strong>to• 7 major topics for adults (old GPG 1-28)• 1 section of cl<strong>in</strong>ical outcome goals (old 29-38)• 1 section for pediatrics (new)• Recommendations (CPR) are now separatefrom <strong>the</strong> guidel<strong>in</strong>es (to emphasize <strong>the</strong>importance of <strong>the</strong> evidence base)Major Changes to VA-<strong>KDOQI</strong> <strong>2006</strong>• Each major topic has multiple specific areasfor fur<strong>the</strong>r research studies:• Most research suggestions relate to <strong>the</strong>recommendations under each topic.• Goal is to ga<strong>the</strong>r evidence so that a guidel<strong>in</strong>e orrecommendation can be promoted or demoted(for example – access surveillance).
The evidence2892+112 +5 = 3009 articles screened59 sent for data extractionMore than half rejected24 <strong>in</strong>corporated <strong>in</strong>to evidence tablesVA 3009/58/24; HD 2749/87/23; PD 2600/101/27Q2. To be considered as a source forevidence, research articles had tograded upon:• A. study size and duration• B. applicability to <strong>the</strong> areas of review• C. results (hard outcome or surrogate)• D. methodological quality (bias avoidance)• E. all of <strong>the</strong> above
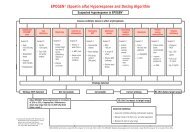
Grad<strong>in</strong>g• Study size and duration• Applicability• Results (hard outcome or surrogate)• Methodological quality (bias avoidance)A. Evidence strong that practice improves outcome.Cl<strong>in</strong>icians should follow <strong>the</strong> practice. Guidel<strong>in</strong>eB. Evidence moderately strong. Recommended thatcl<strong>in</strong>icians follow <strong>the</strong> practiceC. Weak evidence. Consider follow<strong>in</strong>g <strong>the</strong> practice.Need research. Became cl<strong>in</strong>ical practicerecommendations – (CPR)<strong>Vascular</strong> <strong>Access</strong> – <strong>KDOQI</strong> <strong>2006</strong>CPG 1. Patient Preparation for Permanent <strong>Access</strong>CPG 2. Selection and Placement of <strong>Access</strong>CPG 3. Cannulation and <strong>Access</strong>ion of <strong>Access</strong>CPG 4. Detection of <strong>Access</strong> Dysfunction:Monitor<strong>in</strong>gand Surveillance
<strong>Vascular</strong> <strong>Access</strong> - <strong>KDOQI</strong> <strong>2006</strong>CPG 5. Treatment of Autologous FistulaComplicationsCPG 6. Treatment of AV Graft ComplicationsCPG 7. Prevention and Treatment ofCa<strong>the</strong>ters/portsComplicationsCPG 8 Cl<strong>in</strong>ical Outcome GoalsCPR 8 Cl<strong>in</strong>ical Practice Recommendations for<strong>Vascular</strong> <strong>Access</strong> <strong>in</strong> Pediatric PatientsMajor Differences from <strong>the</strong> 2000Guidel<strong>in</strong>es• Clearer differentiation of guidel<strong>in</strong>es fromrecommendations based on <strong>the</strong> strength of <strong>the</strong>evidence• Proposals for fur<strong>the</strong>r research studies relat<strong>in</strong>g tospecific issues for each section – goal is to<strong>in</strong>crease <strong>the</strong> evidence base of guidel<strong>in</strong>es andespecially recommendations• Emphasis on <strong>the</strong> importance of <strong>the</strong> physicalexam: teach better practices to staff and patients
Major Differences from 2000 Guidel<strong>in</strong>es• Calls for earlier identification of/and motivationof <strong>the</strong> patient to receive a permanent accessprior to <strong>the</strong> need for dialysis (those patientsreceiv<strong>in</strong>g health care)• Emphasis on educat<strong>in</strong>g patients, staff, health caresystems; establish<strong>in</strong>g <strong>Vascular</strong> <strong>Access</strong> Teams (VAT)for shared responsibility• Data collection on access care and use of CQI.Major Focus Areas• Pre-op venous imag<strong>in</strong>g/mapp<strong>in</strong>g for plann<strong>in</strong>gAVF construction– CPG 1.3 Patients should have a functionalpermanent access at <strong>the</strong> <strong>in</strong>itiation of dialysis(criteria given)
Major Focus Areas• Monitor<strong>in</strong>g and surveillance of accesses to preventdysfunction/thrombosis• CPG 4.1 Physical exam<strong>in</strong>ation should be used todetect dysfunction <strong>in</strong> fistulae and grafts at leastmonthly by a qualified <strong>in</strong>dividual. (B)Physical Exam<strong>in</strong>ation (of <strong>the</strong> access): Inspection, palpation, andauscultation of <strong>the</strong> access. (<strong>KDOQI</strong> glossary)Major Focus Areas• Treatment/prevention of tunneled ca<strong>the</strong>ter relatedbacteremia– CPG 7.4.1 Ca<strong>the</strong>ters should be exchanged assoon as possible and with<strong>in</strong> 72 hours of<strong>in</strong>itiat<strong>in</strong>g antibiotic <strong>the</strong>rapy <strong>in</strong> most <strong>in</strong>stancesand such exchange does not require a negativeblood culture prior to <strong>the</strong> exchange. (B+)
Major Focus Areas• Treatment/prevention of tunneled ca<strong>the</strong>terrelated bacteremia– CPR7.5.3 Antibiotic lock with antibiotic towhich <strong>the</strong> organism is sensitive is <strong>in</strong>dicatedwhen follow-up cultures <strong>in</strong>dicate re<strong>in</strong>fectionwith <strong>the</strong> same organism <strong>in</strong> a patient withlimited ca<strong>the</strong>ter sites. (Op<strong>in</strong>ion)Major Focus Areas• Management of <strong>the</strong> dysfunctional tunneled ca<strong>the</strong>ter– CPG 7.3.2 Use of thrombolytics• Surveillance of accesses to prevent dysfunction/ thrombosis• CPG 4.1 Physical exam<strong>in</strong>ation should be used to detectdysfunction <strong>in</strong> fistulae and grafts at least monthly by aqualified <strong>in</strong>dividual. (B)―CPG4.2.3.1 Unstandardized dynamic venous pressures (DVP)should not be used as a surveillance technique. (A)
Patient Preparation for Long-Term <strong>Hemodialysis</strong> <strong>Access</strong> -CPG1Appropriate plann<strong>in</strong>g for dialysis <strong>the</strong>rapy allowsfor <strong>the</strong> <strong>in</strong>itiation of dialysis at <strong>the</strong> appropriatetime and with a permanent access <strong>in</strong> place at <strong>the</strong>start of dialysis <strong>the</strong>rapy.CPG 1: Preparation & Evaluation1.1 Patients with a GFR of < 30 ml/m<strong>in</strong>/1.73m2 (CKDstage IV) should be educated on all modalities ofrenal replacement <strong>the</strong>rapy <strong>in</strong>clud<strong>in</strong>g transplantationoptions so that timely referral can be made for <strong>the</strong>appropriate modality and placement of a permanentdialysis access if necessary. (A)
Q3. Ve<strong>in</strong> preservation for access<strong>in</strong>cludes:• A. all patients diagnosed with CKD• B. all peripheral arm and central vessels• C. blood draws and IV placements should befrom or <strong>in</strong> <strong>the</strong> backs of <strong>the</strong> hands• D. patient education, early and often• E. all of <strong>the</strong> aboveCPG 1: Preparation & Evaluation1.2 In patients with Stage IV or V CKD, forearm andupper arm ve<strong>in</strong>s suitable for placement of vascularaccess should not be used for venipuncture or for<strong>the</strong> placement of <strong>in</strong>travenous ca<strong>the</strong>ters, subclavianca<strong>the</strong>ters or PICC l<strong>in</strong>es. (B)
CPG 1: Preparation & Evaluation1.3 Patients should have a function<strong>in</strong>g permanentaccess at <strong>the</strong> <strong>in</strong>itiation of dialysis1.3.3 A peritoneal dialysis (PD) ca<strong>the</strong>ter should beideally placed at least 2 weeks prior to <strong>the</strong> anticipatedstart of dialysis treatments. A back-up HD access doesnot need to be placed <strong>in</strong> most patients. A PD ca<strong>the</strong>termay be used as a bridge for fistula <strong>in</strong> “appropriate”patients. (B-)1.4 Evaluations that should be performed prior toplacement of a permanent HD accessCPG2-Selection of <strong>Access</strong> Type and SiteA structured approach to <strong>the</strong> type and location of long-termHD accesses should help to optimize access survival andm<strong>in</strong>imize complications. The access should be placeddistally and <strong>in</strong> <strong>the</strong> upper extremities whenever possible.Options for fistula creation should be considered first,followed by pros<strong>the</strong>tic grafts, if fistula creation is notpossible. Ca<strong>the</strong>ters should be avoided for hemodialysis andused only when o<strong>the</strong>r options are not available.
CPG 2. Selection of <strong>Access</strong>2.1 The order of preference for placement of fistulae <strong>in</strong>patients with kidney failure who choose HD as <strong>the</strong>ir<strong>in</strong>itial mode of RRT should be:2.1.1 Preferred: fistula. (B+)2.1.1.1 A wrist (radial-cephalic) primary fistula. (A)2.1.1.2 An elbow (brachial-cephalic) primary fistula. (A)2.1.1.3 A transposed brachial basilic ve<strong>in</strong> fistula. (B)2.1.2 Acceptable: AVG of syn<strong>the</strong>tic or biological material, suchas: (B)2.1.2.1 A forearm loop graft, preferable to a straightconfiguration etc.CPG 2. Selection of <strong>Access</strong>2.1.3. Avoid if possible: Long-term ca<strong>the</strong>ters (B)2.1.3.1 Short-term ca<strong>the</strong>ters should be used for acute dialysis andfor a limited duration <strong>in</strong> hospitalized patients. Noncuffedfemoral ca<strong>the</strong>ters should be used <strong>in</strong> bed-bound patients only. (B)Although <strong>the</strong>re are no studies report<strong>in</strong>g on <strong>the</strong> safety of patients withNCCs go<strong>in</strong>g home while await<strong>in</strong>g placement at a dialysis center, <strong>the</strong>Work Group believes that <strong>the</strong> risk of <strong>in</strong>fection, <strong>in</strong>advertent removal,hemorrhage, air embolism, and patient comfort mandates that patientsafety come first. Therefore, a patient with an NCC should not bedischarged. A short-term ca<strong>the</strong>ter can be converted to a TCC if <strong>the</strong>re isno evidence of active <strong>in</strong>fection.
CPG 2. Selection of <strong>Access</strong>2.2Fistulae2.2.1. Enhanced maturation of fistulae can beaccomplished by selective obliteration of majorvenous side branches <strong>in</strong> <strong>the</strong> absence of a downstreamstenosis [B]2.3 Grafts2.3.2. There is no conv<strong>in</strong>c<strong>in</strong>g evidence to supporttapered over uniform tubes, externally supportedover unsupported grafts, thick- versus th<strong>in</strong>-walledconfigurations, or elastic versus nonelastic material.[A] .CPG 2. Selection of <strong>Access</strong>• 2.4 Ca<strong>the</strong>ters and port ca<strong>the</strong>ter systems:• 2.4.1 The preferred <strong>in</strong>sertion site for tunneled, cuffed venousdialysis ca<strong>the</strong>ters or port ca<strong>the</strong>ter systems is <strong>the</strong> right <strong>in</strong>ternaljugular ve<strong>in</strong>. O<strong>the</strong>r options <strong>in</strong>clude: <strong>the</strong> right external jugular ve<strong>in</strong>;<strong>the</strong> left <strong>in</strong>ternal and external jugular ve<strong>in</strong>s; subclavian ve<strong>in</strong>s;femoral ve<strong>in</strong>s; and translumbar and transhepatic access to <strong>the</strong> IVC.Subclavian access should be used only when no o<strong>the</strong>r upperextremityor chest-wall options are available. (A)• 2.4.2 Ultrasound should be used <strong>in</strong> <strong>the</strong> placement of ca<strong>the</strong>ters. B+2.4.3 The position of <strong>the</strong> tip of any central ca<strong>the</strong>ters should beverified radiologically. (B)
CPG3. <strong>Access</strong>ion of HD ca<strong>the</strong>tersand port ca<strong>the</strong>ter systems• The use of aseptic technique and appropriatecannulation methods, <strong>the</strong> tim<strong>in</strong>g of fistula and graftcannulation, and early evaluation of immature fistulaeare all factors that may prevent morbidity and mayprolong <strong>the</strong> survival of long-term dialysis accesses.CPG 3. Cannulation & <strong>Access</strong> Care3.1 Aseptic technique should be used for all cannulationand ca<strong>the</strong>ter accession procedures. (A)3.2 Maturation - Fistula hand-arm exercise (B)If a fistula has not matured, a fistulogram or o<strong>the</strong>rimag<strong>in</strong>g study should be obta<strong>in</strong>ed to determ<strong>in</strong>e <strong>the</strong>cause of <strong>the</strong> problem. (B+).
Exercise shouldboth enlarge <strong>the</strong>ve<strong>in</strong> by<strong>in</strong>creas<strong>in</strong>g flowand build <strong>the</strong>muscle below tomake <strong>the</strong> ve<strong>in</strong>more prom<strong>in</strong>entRule of 6s for <strong>the</strong> Fistula Maturation• Greater than 600mL per m<strong>in</strong> flow• Greater than 6 mms <strong>in</strong> diameter• Less than 6mms below sk<strong>in</strong> surfaceAND• All fistulae should be thoroughly exam<strong>in</strong>ed no laterthan 6 weeks post op• Is <strong>the</strong>re at least 6 cms of ve<strong>in</strong> to cannulate?
CPG 3. Cannulation &<strong>Access</strong> Care3.3 Cannulation of AV grafts: tutorial, use of <strong>the</strong>buttonhole3.4 Infection control measures that should be usedfor all hemodialysis ca<strong>the</strong>ters and port ca<strong>the</strong>tersystems: 4 specific statements relat<strong>in</strong>g toexam<strong>in</strong>ation, dress<strong>in</strong>gs, aseptic technique,prevention <strong>in</strong>clud<strong>in</strong>g Antimicrobial Lock<strong>in</strong>gSolutions.Q4. The Purpose of Monitor<strong>in</strong>g andSurveillance is to:• A. fill out <strong>the</strong> CPM forms correctly• B. to prospectively identify stenoses <strong>in</strong> <strong>the</strong> access• C. collect CQI data on flow rates• D. save staff time by elim<strong>in</strong>at<strong>in</strong>g physical exam• E. all of <strong>the</strong> above
CPG G 4. Detection of <strong>Access</strong> Dysfunction:Monitor<strong>in</strong>g, Surveillance, and DiagnosticTest<strong>in</strong>g• Prospective surveillance of fistulae and graftsfor hemodynamically significant stenosis, whencomb<strong>in</strong>ed with correction of <strong>the</strong> anatomicstenosis, may improve patency rates and maydecrease <strong>the</strong> <strong>in</strong>cidence of thrombosis.CPG 4. <strong>Access</strong> DysfunctionSurveillance/Monitor<strong>in</strong>g4.1. Physical exam<strong>in</strong>ation should be used todetect dysfunction <strong>in</strong> fistulae and grafts atleast monthly by a qualified <strong>in</strong>dividual. (B)4.2 Techniques, not mutually exclusive, thatshould be used <strong>in</strong> surveillance for stenosis<strong>in</strong> grafts <strong>in</strong>clude: flow, static pressure,DUS.
CPG 4. <strong>Access</strong> DysfunctionSurveillance/Monitor<strong>in</strong>g4.3 Surveillance <strong>in</strong> fistulae: flow and duplexultrasound preferred4.4. Criteria for referral for elective <strong>in</strong>terventionRecirculation and dynamic venous pressure not recommendedCPG 4. Surveillance & Monitor<strong>in</strong>g4.4 When to refer for evaluation (diagnosis) andtreatment4.4.1 One should not respond to a s<strong>in</strong>gle isolatedabnormal value. With all techniques, prospectivetrend analysis of <strong>the</strong> test parameter has greaterpower to detect dysfunction than isolated valuesalone (B).
CPG 4. Surveillance & Monitor<strong>in</strong>g4.4.2 Persistent abnormalities <strong>in</strong> any of <strong>the</strong>monitor<strong>in</strong>g or surveillance parameters shouldprompt referral for access angiography. (B)4.4.3 An access flow rate 0.5 <strong>in</strong> grafts or fistulae (B)4.4.5 An arterial segment static pressure greater than0.75 <strong>in</strong> grafts. (B)4.4.6 Ratio of dialyzer (blood pump) flow to pre-pumppressure < 1.2 <strong>in</strong> fistulae and 1.6 <strong>in</strong> grafts when us<strong>in</strong>g 15g needles. (B-)
CPG5. Treatment of Fistula ComplicationsAppropriate <strong>in</strong>terventions for access dysfunction mayresult <strong>in</strong> an <strong>in</strong>creased duration of survival of <strong>the</strong> AVF.5.1 Problems develop<strong>in</strong>g with<strong>in</strong> <strong>the</strong> first 6 monthsshould be promptly addressed [3]5.1.3. A program should be <strong>in</strong> place to detect earlyaccess dysfunction, particularly delays <strong>in</strong> maturation.The patient should be evaluated no later than 6weeks. (B)CPG5. Treatment of Fistula Complications5.2Reasons for elective <strong>in</strong>tervention (flow <strong>in</strong>adequacy,stenosis, aneurysm, ischemia)5.3A fistula with a greater than 50% stenosis <strong>in</strong> ei<strong>the</strong>r <strong>the</strong>venous outflow or arterial <strong>in</strong>flow, <strong>in</strong> conjunction withcl<strong>in</strong>ical or physiologic abnormalities, should betreated with percutaneous translum<strong>in</strong>al angioplasty orsurgical revision. (B)
CPG 5. Treatment of Fistula Complications5.4. Stenosis, as well as <strong>the</strong> cl<strong>in</strong>ical parameters used todetect it, should return to with<strong>in</strong> acceptable limitsfollow<strong>in</strong>g <strong>in</strong>tervention. (B)5.5.Thrombectomy of an Fistula should be attempted asearly as possible after thrombosis is detected but can besuccessful even after several days. (B)5.6 <strong>Access</strong> Evaluation for Ischemia: how, frequency, andwhen. [2]CPG 6. Treatment of AVG ComplicationsAppropriate management and treatment ofAVG complications may improve <strong>the</strong>function and longevity of <strong>the</strong> vascular access.6.1. Extremity Edema <strong>in</strong> <strong>Access</strong> Limb. (2)6.2. Indicators of Graft Rupture. (4)6.3. Indications for revision/repair. (4)6.4. Criteria for Action on Stenoses w/oThrombosis. (3)
CPG 6. Treatment of AVG Complications6.5. Outcomes Follow<strong>in</strong>g Treatment of Stenosis withoutThrombosis: degree of residual, change <strong>in</strong>hemodynamics or physiology, patency post<strong>in</strong>tervention (surgery vs PTAS)6.6 PTA failures and use of stents.6.7 Treatment of Thrombosis and Associated Stenosis.6.8 Outcomes Follow<strong>in</strong>g Treatment of AV GraftThrombosis.6.9. Treatment AV Graft Infection.Q5 Which statement about ca<strong>the</strong>tersis true?• A. prevention and early treatment ofcomplications should greatly reduceassociated morbidity and mortality.• B. ca<strong>the</strong>ter dysfunction is a BFR consistentlyless than 300mLs/m<strong>in</strong> <strong>in</strong> <strong>the</strong> average adult• C. strict aseptic technique should always beused when access<strong>in</strong>g a ca<strong>the</strong>ter• D. all of <strong>the</strong> above
CPG 7 Prevention and Treatment ofCa<strong>the</strong>ter and Port ComplicationsCa<strong>the</strong>ters and ports are essential tools forprovid<strong>in</strong>g urgent and, <strong>in</strong> some cases, long-termvascular access. Prevention and early treatmentof complications should greatly reduceassociated morbidity and mortality.CPG 7 Prevention and Treatment ofCa<strong>the</strong>ter and Port Complications7.1 Ca<strong>the</strong>ters and ports should be evaluated when<strong>the</strong>y become dysfunctional. Dysfunction is def<strong>in</strong>edas failure to atta<strong>in</strong> and ma<strong>in</strong>ta<strong>in</strong> an extracorporealblood flow ≥300 mL/m<strong>in</strong> at a prepump arterialpressure more negative than –250 mm Hg. (B)7.2 The exception is <strong>the</strong> pediatric or smaller adultca<strong>the</strong>ters that are not designed to have flows <strong>in</strong>excess of 300 mL/m<strong>in</strong>. (B)
CPG 7 Prevention and Treatment ofCa<strong>the</strong>ter and Port Complications7.3 Methods that should be used to treat adysfunctional or nonfunctional ca<strong>the</strong>ter or port<strong>in</strong>clude:7.3.1 Reposition<strong>in</strong>g of a malpositioned ca<strong>the</strong>ter; (B)7.3.2 Thrombolytics, us<strong>in</strong>g ei<strong>the</strong>r an <strong>in</strong>tralum<strong>in</strong>allytic, <strong>in</strong>tradialytic lock protocol or an<strong>in</strong>traca<strong>the</strong>ter thrombolytic <strong>in</strong>fusion or<strong>in</strong>terdialytic lock (B)7.3.3 Ca<strong>the</strong>ter exchange with sheath disruption whenappropriate. (B)CPG7 Prevention and Treatment ofCa<strong>the</strong>ter and Port Complications7.4 Treatment of an <strong>in</strong>fected HD ca<strong>the</strong>ter or portshould be based on <strong>the</strong> type and extent of<strong>in</strong>fection.7.4.1 All ca<strong>the</strong>ter-related <strong>in</strong>fections, except forca<strong>the</strong>ter exit-site <strong>in</strong>fections, should beaddressed by <strong>in</strong>itiat<strong>in</strong>g parenteraltreatment with an antibiotic(s) appropriate for <strong>the</strong>organism(s) suspected. (A)7.4.2 Def<strong>in</strong>itive antibiotic <strong>the</strong>rapy should be based on<strong>the</strong> organism(s) isolated. (A)
CPG7 Prevention and Treatment ofCa<strong>the</strong>ter and Port Complications7.4.3 Ca<strong>the</strong>ters should be exchanged as soon aspossible and with<strong>in</strong> 72 hours of <strong>in</strong>itiat<strong>in</strong>g antibiotic<strong>the</strong>rapy <strong>in</strong> most <strong>in</strong>stances, and such exchange doesnot require a negative blood culture prior to <strong>the</strong>exchange. (B+) Follow-up cultures are needed 1week after cessation of antibiotic <strong>the</strong>rapy (standardpractice).7.4.4 Port pocket <strong>in</strong>fections should be treated withsystemic antibiotics and irrigation, <strong>in</strong> conjunctionwith <strong>the</strong> manufacturers’ recommendations. (B)CPG 8 - Cl<strong>in</strong>ical Outcome Goals:8.1 Goals for <strong>Access</strong> Placement.8.1.1 Each center should establish a databaseand CQI process to track <strong>the</strong> types of accessescreated and <strong>the</strong> complication rates for <strong>the</strong>seaccesses (cannot accomplish without a VAT)8.1.2 The goals for <strong>in</strong>cident hemodialysis accessplacement should <strong>in</strong>clude:fistula >65%, ca<strong>the</strong>ters
CPG8 Cl<strong>in</strong>ical Outcome Goals8.3. <strong>Access</strong> complications/performance: relat<strong>in</strong>gto thrombosis rates, <strong>in</strong>fection rates overallsurvival8.4. Efficacy of Interventions: Secondary patencyfollow<strong>in</strong>g PTA or surgery w and w/othrombosis.Cl<strong>in</strong>ical Practice Recommendations for<strong>Vascular</strong> <strong>Access</strong> <strong>in</strong> Pediatric Patients8.1. Choice of <strong>Access</strong> [4]8.1.1 Permanent access <strong>in</strong> <strong>the</strong> form of a fistula orgraft is <strong>the</strong> preferred form of pediatricvascular access for ma<strong>in</strong>tenance hemodialysisfor most pediatric patients (B).
Cl<strong>in</strong>ical Practice Recommendations for<strong>Vascular</strong> <strong>Access</strong> <strong>in</strong> Pediatric Patients8.1.2 Circumstances <strong>in</strong> which a central venous ca<strong>the</strong>ter may beacceptable for pediatric chronic access <strong>in</strong>clude lack of localsurgical expertise to place permanent vascular access <strong>in</strong> smallchildren, patient size too small to support a permanentvascular access and expectation of expeditious renaltransplantation.8.1.3 If surgical expertise to place permanent access does notexist <strong>in</strong> <strong>the</strong> patient’s pediatric sett<strong>in</strong>g, efforts should be madeto consult vascular access expertise among local adultoriented surgeons to ei<strong>the</strong>r supervise or place permanentvascular access <strong>in</strong> children.Cl<strong>in</strong>ical Practice Recommendations for<strong>Vascular</strong> <strong>Access</strong> <strong>in</strong> Pediatric Patients8.1. Choice of <strong>Access</strong>8.1.4 Programs should evaluate <strong>the</strong>ir patients’ expectedwait<strong>in</strong>g times on <strong>the</strong>ir local deceased-donor kidneytransplant wait<strong>in</strong>g lists. Serious consideration shouldbe given plac<strong>in</strong>g permanent vascular access <strong>in</strong>children >20 kg <strong>in</strong> size who are expected to waitmore than 1 year for a kidney transplant. (CPR)
Cl<strong>in</strong>ical Practice Recommendations for<strong>Vascular</strong> <strong>Access</strong> <strong>in</strong> Pediatric Patients9.2 Stenosis surveillance:An AVG stenosis surveillance protocol should beestablished to detect venous anastomosis stenosis anddirect patients for surgical revisionCl<strong>in</strong>ical Practice Recommendations for<strong>Vascular</strong> <strong>Access</strong> <strong>in</strong> Pediatric Patients9.3 Ca<strong>the</strong>ter sizes, anatomical sites and configurations:Ca<strong>the</strong>ter sizes should be matched to patient sizes with<strong>the</strong> goal of m<strong>in</strong>imiz<strong>in</strong>g <strong>in</strong>tralum<strong>in</strong>al trauma andobstruction to blood flow while allow<strong>in</strong>g sufficientblood flow for adequate HD. (CPR)9.3.2 External cuffed access should be placed <strong>in</strong> <strong>the</strong><strong>in</strong>ternal jugular with <strong>the</strong> distal tip placed <strong>in</strong> <strong>the</strong> rightatrium. (C)9.3.3 The blood flow rate of an external access should bem<strong>in</strong>imally 3-5 mL/kg/m<strong>in</strong> and should be adequate todeliver <strong>the</strong> prescribed HD dose. (CPR)
It’s s always about<strong>the</strong> Patient!Thanks!– email me atlesleyd@ncnc.rr.comCPR [recommendations] 1-41CPR 1: use of ve<strong>in</strong>s on dorsum of hand, patienteducation dur<strong>in</strong>g CKD, imag<strong>in</strong>g o<strong>the</strong>r than DDU.CPR 2: what to do when a new native fistula is<strong>in</strong>filtrated, role of fistula-hand exercises prior toconstructionCPR 3: cannulation skills, self cannulation,buttonhole, manag<strong>in</strong>g extremity edemaCPR 4: monitor<strong>in</strong>g, frequency of surveillance,diagnostic test<strong>in</strong>g (what to record, how often,where, review process, by whom [VAT])
CPR [recommendations] 5-95CPR 5:• when to “mark <strong>the</strong> fistula” that is difficult to cannulate• teach<strong>in</strong>g patients to monitor <strong>the</strong>ir own fistula patencyCPR 7: ca<strong>the</strong>ter dysfunction/ca<strong>the</strong>ter ma<strong>in</strong>tenance• radiologic evaluation and <strong>in</strong>tervention; sheath stripp<strong>in</strong>g• choice and use of thrombolytics,• ca<strong>the</strong>ter ma<strong>in</strong>tenance <strong>in</strong> <strong>the</strong> patient with limited access options• use of endolum<strong>in</strong>al brushes• Manag<strong>in</strong>g <strong>in</strong>fection: when to use adjunctive antibiotics forsalvage; use of prophylactic AMLsResearch:3. Cannulation and <strong>Access</strong> Care.• Additional studies on dis<strong>in</strong>fectants, role of antibiotic locksand which patients may benefit most from CVC salvage.• Risk benefit outcomes as well as long term antibioticsusceptibility studies to detect resistance with ABLs• Does <strong>the</strong> bevel up cannulation method decrease accesscomplications? RCT• Can <strong>in</strong>creased remuneration for expert cannulators lead tobetter access outcomes?
Research:7. Ca<strong>the</strong>ters• With modern ca<strong>the</strong>ters, what is <strong>the</strong> value of <strong>the</strong>conductance (BFR/arterial pre pump pressure) <strong>in</strong>predict<strong>in</strong>g ca<strong>the</strong>ter dysfunction?• The ideal ca<strong>the</strong>ter diameter is not established. Are<strong>the</strong>re com <strong>in</strong>creased complications associated withlarger diameter ca<strong>the</strong>ters?• Comparison of lytic treatmentsResearch:7 Ca<strong>the</strong>ters (cont)• Comparison of lytic treatments• Def<strong>in</strong><strong>in</strong>g <strong>the</strong> natural history of ca<strong>the</strong>ter/port relatedcomplications <strong>in</strong> <strong>the</strong> central ve<strong>in</strong>s us<strong>in</strong>g centralvenograms• Studies to determ<strong>in</strong>e <strong>the</strong> association between<strong>in</strong>fection and fibr<strong>in</strong> sheaths <strong>in</strong> ca<strong>the</strong>ters.• Antibiotic locks: optimal use?9. Pediatrics (<strong>in</strong>f<strong>in</strong>ite number of questions)