Glucagon Diabetes mellitus Islet microcirculation
Glucagon Diabetes mellitus Islet microcirculation
Glucagon Diabetes mellitus Islet microcirculation
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
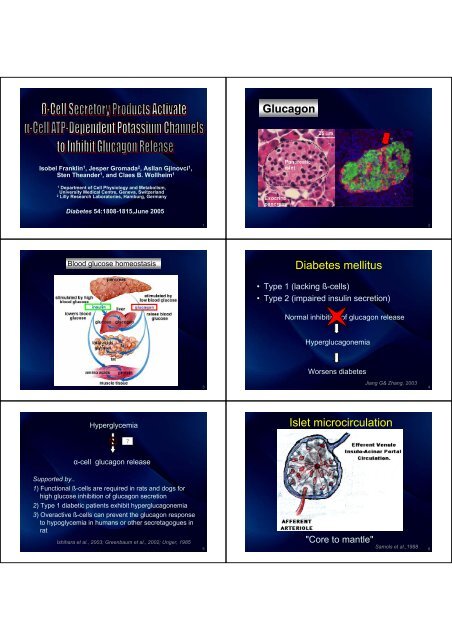
<strong>Glucagon</strong><br />
Isobel Franklin 1 , Jesper Gromada 2 , Asllan Gjinovci 1 ,<br />
Sten Theander 1 , and Claes B. Wollheim 1<br />
1<br />
Department of Cell Physiology and Metabolism,<br />
University Medical Centre, Geneva, Switzerland<br />
2<br />
Lilly Research Laboratories, Hamburg, Germany<br />
<strong>Diabetes</strong> 54:1808-1815,June 2005<br />
1<br />
2<br />
Blood glucose homeostasis<br />
<strong>Diabetes</strong> <strong>mellitus</strong><br />
• Type 1 (lacking ß-cells)<br />
• Type 2 (impaired insulin secretion)<br />
Normal inhibition of glucagon release<br />
Hyperglucagonemia<br />
3<br />
Worsens diabetes<br />
Jiang G& Zhang, 2003<br />
4<br />
Hyperglycemia<br />
<strong>Islet</strong> <strong>microcirculation</strong><br />
α-cell glucagon release<br />
Supported by..<br />
1) Functional ß-cells are required in rats and dogs for<br />
high glucose inhibition of glucagon secretion<br />
2) Type 1 diabetic patients exhibit hyperglucagonemia<br />
3) Overactive ß-cells can prevent the glucagon response<br />
to hypoglycemia in humans or other secretagogues in<br />
rat<br />
Ishihara et al., 2003; Greenbaum et al., 2002; Unger, 1985<br />
5<br />
"Core to mantle"<br />
Samols et al.,1988<br />
6
Isolation of islet cells<br />
Quantitative RT-PCR<br />
Fluorescence-activated<br />
cell sorter (FACS)<br />
purifications<br />
1 st sort, by FAD (flavine<br />
adenine dinucleotide)<br />
content<br />
ß- & α-cells<br />
2 nd sort, by NAD(P)H<br />
content of the α-cell<br />
fraction<br />
pure α- & non α-cells<br />
• Total RNA was extracted from α- and ß-<br />
cell fractions using RNeasy Mini kit ®<br />
• Converted into cDNA using Superscript<br />
reverse transcriptase<br />
• Primers were designed to amplify the<br />
insulin receptor, Kir6.2, and<br />
sulfonylurea receptor (SUR)1; glucagon,<br />
insulin and cyclophilin transcripts<br />
Pipeleers et al.,1985<br />
13<br />
• At least 4 independent experiments<br />
14<br />
• Zinc secretion assay<br />
– atomic absorption spectrophotometer<br />
• Hormone secretion assays<br />
– static incubation (triplicate)<br />
• FACS-isolated cells : 15-30 min<br />
• Dispersed islet : 60 min<br />
– radioimmunoassay<br />
• <strong>Glucagon</strong> : anti-glucagon<br />
• Insulin : anti-insulin<br />
• C-peptide : commercial kit<br />
Electrophysiology<br />
Isolated α-cell<br />
Perforated-patch whole-cell configuration<br />
Patch perforation Amphotericin B<br />
Pipette solution<br />
(in mM): K 2<br />
SO 4<br />
76,<br />
NaCl 10, KCl 10,<br />
MgCl 2<br />
1, HEPES 5<br />
(pH 7.35 with KOH)<br />
Extracellular solution<br />
(in mM): NaCl 138, KCl<br />
5.6, MgCl 2<br />
1, CaCl 2<br />
2.6,<br />
HEPES 5 (pH 7.40 with<br />
NaOH), glucose 0<br />
+ additional agents<br />
15<br />
16<br />
Electrophysiology<br />
Isolated α-cell<br />
whole-cell patch-clamp recordings of K ATP channel current activity<br />
Pipette resistance 2-6 MOhm<br />
Statistical analyses<br />
• Two-tailed, Student’s t test<br />
Pipette solution<br />
(in mM):KCl 125,<br />
KOH 30, EGTA 10,<br />
HEPES 5, MgCl 2<br />
1,<br />
Mg-ATP 0.3,<br />
K-ADP 0.3<br />
(pH 7.15)<br />
Extracellular solution<br />
(in mM):NaCl 138, KCl<br />
5.6, MgCl 2<br />
1, CaCl 2<br />
2.6, HEPES 5 (pH 7.40<br />
with NaOH), glucose<br />
0 + additional agents<br />
-60<br />
-70<br />
-80<br />
200 ms<br />
2 s<br />
17<br />
18
<strong>Islet</strong> cell<br />
High-glucose conditions<br />
Zn<br />
Isolated α-cell<br />
Zn<br />
Zn & insulin<br />
secretion<br />
<strong>Glucagon</strong> &<br />
Insulin secretion<br />
α-Cell electrical<br />
activity<br />
• α-Cells are markedly zinc sensitive<br />
• ? Zinc may inhibit glucagon secretion by preventing<br />
calcium influx<br />
25<br />
26<br />
<strong>Glucagon</strong> secretion from FACS-isolated adherent α-cells<br />
dispersed<br />
islet<br />
Membrane potential recordings from isolated α-cells<br />
using the perforated-patch whole-cell configuration<br />
Isobutylmethylxanthine (IBMX)<br />
Monomethylsuccinate Foskolin(forsk) Tolbutamide (mmsucc) Pyruvate (tolbut)(pyruv)<br />
Mean ± SE, n = 3, *P < 0.01, **P < 0.005<br />
27<br />
28<br />
Membrane potential recordings from isolated α-cells<br />
using the perforated-patch whole-cell configuration<br />
Secreted glucagon relative to basal (100%)<br />
n = 7<br />
29<br />
n = 7 *P < 0.01<br />
30
ß-cells<br />
Isolated α-cell<br />
glucagon<br />
glucagon<br />
glucagon<br />
glucagon<br />
glucagon<br />
Tolbutamide<br />
31<br />
32<br />
<strong>Glucagon</strong> secretion from isolated α-cells<br />
Whole-cell patch-clamp recordings of<br />
K ATP channel current activity in isolated α-cells<br />
Mean ± SE, n = 3, *P < 0.05<br />
33<br />
34<br />
Relative increases in K + current amplitude<br />
in response to Zn<br />
Relative transcript abundance of K ATP channel subunits<br />
Kir6.2 and SUR1 in FACS-isolated α- and ß-cells<br />
Mean ± SE, n = 7 for each point<br />
35<br />
Data are presented relative to ß-cells , n = 3, *P < 0.05<br />
36
α-cells<br />
Zinc<br />
opened K ATP channels<br />
inhibited glucose and pyruvate-stimulated<br />
glucagon secretion<br />
did not inhibit arginine-induced glucagon release<br />
… when K ATP channel activity is bypassed, Zn is unable to<br />
block hormone secretion<br />
Pancreatic ß-cell K + -ATP sensitive channel: SUR1/Kir6.2<br />
SUR1<br />
Kir6.2<br />
Transcripts encoding K ATP subunits were more<br />
abundant in α- than ß-cells (FACS-isolated)<br />
Zinc action probably results from direct activation of<br />
α-cell K ATP channels rather than inhibition of<br />
Ca 2+ channels<br />
37<br />
Site of Zn action may be located on the SUR1 subunit<br />
38<br />
Relative abundance of insulin receptor and GLP-1<br />
receptor transcripts in FACS-isolated α- and ß-cells<br />
and compared with liver<br />
Data are presented relative to ß-cells , n =3, *P < 0.05, **P < 0.01<br />
39 40<br />
Analysis of islet hormone secretion<br />
Analysis of islet hormone secretion<br />
absence<br />
Insulin antiserum<br />
presence<br />
absence<br />
presence<br />
“Zn-free”<br />
exogenous insulin<br />
absence<br />
presence<br />
exogenous insulin<br />
mean ± SE **P < 0.01<br />
41<br />
means+SE **P < 0.01<br />
42
Isolated α-cell<br />
• Insulin receptor transcript was relatively abundant in α-<br />
cells, similar to liver<br />
α-Cells are also important sites of insulin action<br />
• Transcript for GLP-1 receptor was not detected in α-cells<br />
nor did GLP-1 stimulate α-cell glucagon release<br />
in agreement with earlier studies:<br />
– cAMP levels in α-cells were unaffected by GLP-1<br />
– type 1 DM : GLP-1 had no effect on plasma glucagon levels<br />
during hyperinsulinemic-euglycemic clamp<br />
• Apparent direct inhibition by GLP-1 on glucagon secretion<br />
: paracrine factors may have mediated the suppression<br />
43<br />
44<br />
<strong>Glucagon</strong> secretion from in situ–perfused rat pancreas<br />
Membrane potential recording from an isolated α-cell<br />
using the perforated-patch whole-cell configuration<br />
Data are mean+SE of six independent perfusions<br />
45<br />
The recording is typical of six cells.<br />
46<br />
Electrical activity in response to “Zn-free" insulin was<br />
analyzed and the effect on spike frequency calculated<br />
<strong>Glucagon</strong> secretion from isolated α-cells<br />
Data are mean+ SE of six experiments<br />
47<br />
mean+SE *P < 0.05, **P < 0.005<br />
48
Loss of β-cell function<br />
α-Cell hyperactivity<br />
Glucose responsiveness in<br />
neighboring α-cells<br />
Hyperglucagonemia<br />
Worsens diabetes<br />
Greenbaum et al.,2002<br />
Other secretory products capable of<br />
influencing glucagon release in this assay<br />
would have included<br />
- Somatostatin<br />
- GABA (γ-aminobutyric acid)<br />
released from the synaptic-like<br />
microvesicles of ß-cells<br />
Design of drugs aiming at reducing<br />
postprandial α-cell activity<br />
55<br />
Brunicardi et al., 2001; Cejvan et al., 2003;<br />
Wendt et al.,2004; Franklin et al.,2004<br />
56<br />
Isolated α-cell<br />
Glucose<br />
Subjects with<br />
type 1 diabetes<br />
Stimulus-secretion coupling in<br />
the α-cell mirrors that of the ß-cell<br />
glucose<br />
Monomethylsuccinate<br />
Tolbutamide<br />
<strong>Glucagon</strong> secretion<br />
Rat pancreas perfused<br />
in retrograde direction<br />
glucose<br />
57<br />
• α-Cells express both glucokinase and GLUT1, a<br />
lower capacity isoform than GLUT2, expressed<br />
in ß-cells<br />
• Glucose oxidation in α-cells is only 30% of that<br />
in ß-cells (although steady-state glucose<br />
utilization is the same).<br />
glucose is a relatively poor substrate for<br />
mitochondrial ATP generation in α-cells.<br />
Heimberg et al.,1996, Schuit et al.,1997<br />
• An earlier study reported glucose inhibition of<br />
arginine-stimulated glucagon release from<br />
isolated α-cells<br />
Technical disparities<br />
(culture and assay conditions) Pipeleers et al.1986<br />
58<br />
Isolated rat α-cells<br />
High glucose<br />
As in ß-cells<br />
Initial ATP consumption by<br />
glucokinase<br />
Spontaneous<br />
electrical activity<br />
Tolbutamide<br />
SUR1<br />
Opening of K ATP channel<br />
transient hyperpolarization<br />
In α-cells, this could take longer (minutes rather<br />
than seconds) due to the relatively slow rate of glucose<br />
oxidation<br />
Bokvist et al.,1999; Arkhammar et al.,1987<br />
59<br />
• Tolbutamide triggers α-cell electrical activity and<br />
hormone secretion<br />
• Tolbutamide also increased circulating glucagon<br />
levels in patients with advanced type 1 diabetes<br />
Bohannon et al.,1982<br />
60
Conclusion<br />
This study demonstrates that only by<br />
removing α-cells from the repressive<br />
environment of the islet micro-organ can<br />
we begin to identify direct effectors of<br />
glucagon secretion and characterize the<br />
stimulus-secretion coupling pathways that<br />
lead to glucagon release<br />
61<br />
62<br />
63





![Integ50 MedII_KSA3 [Compatibility Mode].pdf](https://img.yumpu.com/53541610/1/190x146/integ50-medii-ksa3-compatibility-modepdf.jpg?quality=85)

