Ambulance
21hiRF8
21hiRF8
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
TODAY<br />
Spring 2016 - Issue 1 | Volume 13<br />
<strong>Ambulance</strong><br />
The global magazine for all people involved in ambulance provision<br />
Now going out globally to over 300,000 ambulance workers<br />
in partnership with NAEMT, IAED and UNISON<br />
Un<br />
This issue is supported by<br />
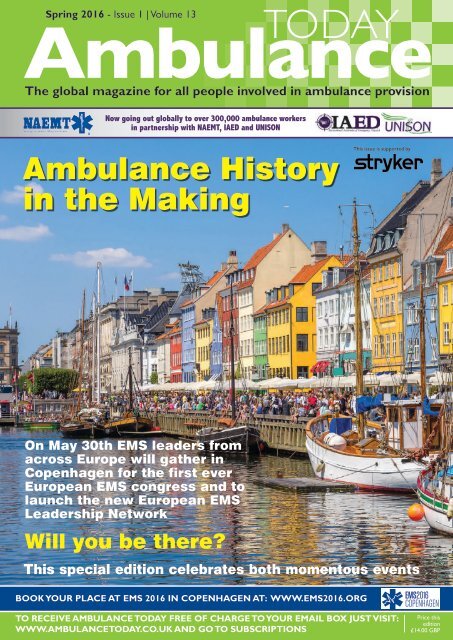
<strong>Ambulance</strong> History<br />
in the Making<br />
On May 30th EMS leaders from<br />
across Europe will gather in<br />
Copenhagen for the first ever<br />
European EMS congress and to<br />
launch the new European EMS<br />
Leadership Network<br />
Will you be there?<br />
This special edition celebrates both momentous events<br />
BOOK YOUR PLACE AT EMS 2016 IN COPENHAGEN AT: WWW.EMS2016.ORG<br />
TO RECEIVE AMBULANCE TODAY FREE OF CHARGE TO YOUR EMAIL BOX JUST VISIT:<br />
WWW.AMBULANCETODAY.CO.UK AND GO TO SUBSCRIPTIONS<br />
Price this<br />
edition<br />
£14.00 GBP
The ultimate in safe ambulance<br />
transportation for children<br />
The ACR-4 is for the safe and effective transport<br />
of infants and children in an ambulance.<br />
The <strong>Ambulance</strong> Child Restraint is now available in 4 sizes.<br />
In addition to the Small (5-12kg), Medium (10-25kg) and Large (20-45kg)<br />
sizes, this innovative, flexible and fully adjustable harnessing system now<br />
comes in an Extra Small (2-5kg) and are all colour coded for easy selection.<br />
Quick release clips dock with the ACR harness, holding the patient in place<br />
to prevent potentially dangerous movement during transportation.<br />
Features of the ACR-4<br />
• Open channel design allows complete<br />
patient access from, the airway to the<br />
waist without unrestraining the child.<br />
• The restraint tightens in the mattress<br />
of the stretcher not into the child<br />
preventing any additional injury to the<br />
patient.<br />
• Compact packaging, the ACR-4 fits<br />
into its own custom bag taking up less<br />
room in the back of an ambulance.<br />
• ACR-4 is universal will work on any<br />
stretcher or backboard without a<br />
bracket.<br />
• ACR-4 replaces the need to carry<br />
multiple devices to accomplish the task<br />
of restraining all size patients<br />
• ACR-4 has been fully crash tested<br />
under the strictest of standards<br />
• Color coded for easy size identification<br />
• Machine washable<br />
Specializing in infant and child safety<br />
XS S M L<br />
5-12 kg 10-25 kg 22-55 kg 44-99 kg<br />
<strong>Ambulance</strong><br />
Child Restraint<br />
NEXT GENERATION<br />
ParAid House, Weston Lane,<br />
Birmingham, B11 3RS, United Kingdom<br />
T: +44 (0)121 706 6744 W: www.paraid.co.uk
Guest Editor’s Comment<br />
Now is the moment to put co-operation<br />
at the heart of European EMS<br />
Freddy Lippert, MD<br />
CEO Capital Region Copenhagen<br />
and co-founder of EMS2016<br />
Produced in partnership with<br />
This issue of <strong>Ambulance</strong> Today is a historic one. It<br />
is the spring issue preceding the first European<br />
Emergency Medical Services Congress, EMS2016,<br />
which will be taking place in Copenhagen from May<br />
30th until June 1st. EMS2016 will not only be the<br />
first of its kind, it will also be a platform for obtaining<br />
further much-needed co-operation between EMSsystems.<br />
Significant things are happening in Europe right<br />
now - not only the recent terror attacks in Paris,<br />
Ankara and Brussels but also the surge of refugees<br />
moving through Europe. The tragic and worrying<br />
nature of these events should remind us all that<br />
the role of EMS is becoming increasingly more vital<br />
to the individuals and communities we serve. We<br />
experience a growing public expectation of the level<br />
of healthcare we provide to our communities 24-7.<br />
All of which means that now - more than ever - it<br />
is important that we make a special effort to share<br />
the latest knowledge and technology and to cooperate<br />
across Europe and beyond to identify best<br />
practice. This is vital if we intend to find effective new<br />
solutions to the healthcare challenges we all face.<br />
This understanding of the urgent need to share<br />
knowledge with each other is one of the primary<br />
reasons we are organizing the first European EMS<br />
congress. A European EMS Leadership Network will<br />
also be launched at EMS2016. The primary purpose<br />
of this new network will be to allow EMS countries<br />
to explore each other’s strengths and limitations<br />
and to outline a shared vision for our European<br />
emergency care system. This new European<br />
Leadership Network will come together regularly to<br />
identify and develop the strategies needed to reach<br />
both our common and local EMS goals. You can read<br />
more about our exciting new network inside this<br />
edition.<br />
The area of pre-hospital emergency care and EMS<br />
has advanced at a steady but increasingly rapid pace<br />
during the last decades. This development is due<br />
to the dedicated efforts of ardent EMS pioneers<br />
who have given careful thought to the shaping<br />
of our modern EMS systems. There is no better<br />
example of this than the person we have invited<br />
to open EMS2016. We are greatly honored that<br />
our inaugural keynote speaker will be Professor<br />
Douglas Chamberlain. Douglas is also known as the<br />
father of modern paramedic practice. He was the<br />
first to recognize the need for, and then implement,<br />
resuscitation training for British ambulance personnel.<br />
Furthermore over more than five decades he has<br />
led the way by encouraging EMS leaders globally to<br />
recognize the value of sharing good practice and<br />
innovations in pre-hospital care. Modern EMSsystems<br />
and pre-hospital medicine are now emerging<br />
further towards an evidence-based practice. But the<br />
question is: How can we best translate knowledge<br />
and science into clinical practice?<br />
This exact question was put sharply in focus when<br />
Emergency Medical Services leaders, researchers,<br />
and experts from across the world convened in<br />
June 2015 at Utstein Abbey in Norway, to address<br />
the challenge of how to increase community cardiac<br />
arrest survival and how to achieve implementation of<br />
best practices and worthwhile programs. The answer:<br />
a call to establish a Global Resuscitation Alliance as a<br />
concrete means to catalyze improvements in survival.<br />
The Global Resuscitation Alliance will provide the<br />
tools and support needed for communities to put<br />
on local programs modelled after the Resuscitation<br />
Academy and thereby promote and implement best<br />
practices.<br />
The Global Resuscitation Alliance will be established<br />
at a follow-up Utstein meeting with additional<br />
experts, preceding EMS2016 and will be announced<br />
during the congress. This is a giant achievement.<br />
The first Utstein meeting 25 years ago defined<br />
the terminology and standard for reporting results.<br />
Since then the International Liaison Committee on<br />
Resuscitation (ILCOR) are collecting, reviewing and<br />
sharing international scientific data on resuscitation<br />
and emergency care. And now the new Global<br />
Resuscitation Alliance progresses by implementation<br />
of science and best practices internationally. You can<br />
read more about the Alliance and the Resuscitation<br />
Academy in this issue. In line with this you can also<br />
read about the aspiring Scottish 2020-strategy which<br />
aims to double OHCA survival rates across Scotland.<br />
Inside this edition you will find new articles on<br />
ventilation, pain management and pre-hospital<br />
cardiac care alongside interesting articles from<br />
some of the world’s most respected and influential<br />
EMS leaders. To mention a few: articles by Dr Jeff<br />
Clawson, founder of the International Academies<br />
of Emergency Dispatch (IAED), Peter Bradley, CBE,<br />
CEO of St John New Zealand and Chuck Kearns,<br />
President of the USA’s National Association of<br />
Emergency Medical Technicians (NAEMT). The<br />
theme in this issue of <strong>Ambulance</strong> Today is that no<br />
matter how hard we all strive in our respective EMS<br />
silos, unless we make time to share our experiences<br />
and challenges and to co-operate with each<br />
other to take that vital next step forward, much<br />
of our well-intentioned effort will regrettably be<br />
wasted. Therefore, EMS2016 will provide a unique<br />
opportunity for us all to meet and network in<br />
Copenhagen and share our EMS knowledge and<br />
influence the future of EMS in Europe and abroad.<br />
Thanks to <strong>Ambulance</strong> Today for the persistent work it<br />
has done to encourage EMS groups across the world<br />
to share knowledge, forge innovation partnerships<br />
and provide an editorial platform which showcases<br />
new EMS developments to all of us who are eager<br />
to build strong EMS partnerships.<br />
On behalf of all of those who have worked tirelessly<br />
to make EMS2016 a success – particularly our hardworking<br />
team in Copenhagen and my co-founders<br />
of the congress, Dr Fionna Moore of London<br />
<strong>Ambulance</strong> Service and Jerry Overton of IAED and<br />
our Scientific Committee including Professor Lars<br />
S. Rasmussen and Professor Doris Østergaard. We<br />
should also appreciate the support we receive from<br />
our partner the Danish foundation TrygFonden, the<br />
Laerdal Foundation and our main sponsors and<br />
exhibitors who warmly welcome you all to a new<br />
and innovative congress. Be prepared for surprises<br />
and don’t miss it.<br />
Freddy Lippert, MD<br />
CEO, EMS Copenhagen, co-founder of EMS2016<br />
and co-chair of Utstein Implementation<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
3
It’s Time to Change the Way We Work<br />
WITH AN ALL TOGETHER<br />
SMARTER A&E AMBULANCE<br />
IPTS Integrated Patient Transport Systems TM<br />
KEY FACTS & FIGURES*<br />
REMOVE TAIL LIFT<br />
SAVING<br />
225kg<br />
NO SERVICING OR MAINTENANCE, SAVES £100,000<br />
APPROX PER ANNUM & LESS WEIGHT = LESS FUEL<br />
TYPICAL fleet SAVING<br />
£255K<br />
PER ANNUM ON FUEL<br />
& MAINTENANCE OR<br />
OVER VEHICLE LIFE<br />
£1.78M<br />
MEET GOVT EMISSION<br />
TARGETS BY SAVING<br />
PARAMEDIC<br />
VEHICLE<br />
PATIENT<br />
IPTS Delivers Fleet Efficiency Savings / Reduced MSK Injuries / Lighter <strong>Ambulance</strong> / Safer Environment<br />
Lower CO 2 Emissions / Improved Crew Performance / Fuel & Running Cost Reductions / Less Training<br />
Time Efficiency Savings / Better Drug Efficacy / High Value Asset Protection / Superior Communication<br />
Designed to be a leaner, better, brighter, state-of-the-art <strong>Ambulance</strong>, with all round improved<br />
equipment, ergonomics and patient experience. IPTS is available and ready for action...<br />
INTELLIGENCE<br />
ACETECH ®<br />
1.83M Co kg<br />
2<br />
PER ANNUM – A LIGHTER AMBULANCE WILL<br />
REDUCE CARBON FOOTPRINT & FUEL COSTS<br />
2 MINS LESS LOADING<br />
TASK TIME SAVING<br />
£3.25M<br />
50,000 HOURS BACK<br />
BASED ON 1,500,000 PATIENT JOURNEYS<br />
AT A UNIT HOURLY COST OF £65<br />
CATEGORY C1 DRIVER<br />
TRAINING COURSES<br />
not REQUIRED SAVING<br />
£450K<br />
BASED ON 300 COURSES PER ANNUM @ £1,500<br />
EACH & THIS DOES NOT INCLUDE RE-TESTS<br />
TAKE 10 minutes OFF<br />
MAKE READY SAVING<br />
£1.7M<br />
MODULAR SYSTEM & LESS CUPBOARDS MAKES<br />
THE AMBULANCE EASIER TO CLEAN & RESTOCK<br />
* Figures shown are based on a typical fleet of 275 vehicles, 40,000 miles per annum each @ £1.01 per litre – if you require any further information please contact us on +44 (0) 1274 851 999 or speak to the WINNER of FLEET NEWS Fleet Manager of the Year Award 2016 – Justin Wand @ SECAmb<br />
STRONGER TOGETHER<br />
FERNO.CO.UK +44(0) 1274 851 999
Issue 1, Volume 13: Spring 2016 Next Issue: Summer 2016<br />
CONTENTS<br />
www.ambulancetoday.co.uk<br />
This Issue is<br />
Supported by:<br />
VISIT OUR AMBULANCE TODAY WEBSITE AND REGISTER FOR YOUR FREE<br />
DIGITAL COPY AT: www.ambulancetoday.co.uk<br />
INSIDE YOUR SPRING EMS2016 SPECIAL:<br />
P7. Welcome to EMS2016 in<br />
Copenhagen<br />
Congress Keynote Speaker, Professor Douglas<br />
Chamberlain, looks back on the history of EMS and<br />
reminds us that we can all learn from each other<br />
Chair of Congress Host, Capital Region Copenhagen,<br />
Sophie Hæstorp Andersen reflects on the benefits of<br />
forming Europe-wide partnerships<br />
Overview of the Scientific programme, From ‘Science to Survival,’ and<br />
social highlights of Europe’s newest and largest conference for EMS<br />
leaders<br />
Founders Dr Freddy Lippert, Dr Fionna Moore and Jerry Overton offer<br />
an insight into the new EMS Leadership Network for Europe to be<br />
unveiled at EMS2016<br />
P29. Penthrox – the newest tool in the<br />
prehospital pain management kit<br />
SECamb’s Medicines Management Lead, Paul Cloves,<br />
gives an overview of how Penthrox, the newest analgesia<br />
available to EMS crews, has been received by one of<br />
Europe’s most clinically-innovative ambulance services<br />
P35. Out-of-Hospital Cardiac Arrest – Scotland’s<br />
Story<br />
HEMS Paramedic and national clinical advisor to the Scottish<br />
Government, Paul Gowens, reports on the impressive success story<br />
which has seen Scotland boost its OHCA survival rates through joinedup-working<br />
P41. Refreshing the values of EMS in<br />
New Zealand<br />
CEO of St John New Zealand, Peter Bradley, CBE,<br />
gives a run-down of the technologies boosting EMS<br />
performance in New Zealand<br />
P47. Entonox - Making the most<br />
of the basics in prehospital pain<br />
management<br />
Pain management researcher, Lucas Hawkes-<br />
Frost of London <strong>Ambulance</strong> Service reviews<br />
the contribution that ENTONOX has made to<br />
prehospital clinical care in the UK<br />
P50. Optima: Split-Second deployment decisionmaking<br />
in Dutch EMS<br />
Duncan Bänffer of Safety Region AZRR Rotterdam reports on how<br />
Optima Predict is helping develop accurate real-world simulations to<br />
improve EMS planning across the Netherlands<br />
P54. Problems associated with the Use of Self-<br />
Reforming Bags in Emergency Artificial Ventilation<br />
Professor David Baker, Emeritus Consultant Anaesthesiologist with<br />
SAMU de Paris, reviews the published evidence concerning the use of<br />
BVM in emergency care and discusses the need for better training and<br />
awareness of the associated problems<br />
P59. The Happy Haus of Baus<br />
We visited the Baus AT plant in Toruń, Poland<br />
to find out how Europe’s fastest-growing<br />
ambulance builder is expanding globally<br />
P73. Isn’t it Time that Patients Take Responsibility<br />
as Well?<br />
Dutch Correspondent, Thijs Gras, tackles the thorny question of how<br />
much legal responsibility patients should take for co-operating with their<br />
ambulance carers<br />
P76. IAED Founder Dr Jeff Clawson<br />
Welcomes new European EMS Network<br />
Joe Smith finds out about the creation and growth of the<br />
International Academies of Emergency Dispatch from its<br />
founder, Dr Jeff Clawson<br />
P79 Watson, I Presume?<br />
UMCG’s Jaap Hatenboer offers a Dutch perspective on the importance<br />
of EMS managers understanding the impact of the fourth industrial<br />
revolution on ambulance care<br />
P82. USA’s NAEMT President Chuck Kearns on<br />
Global EMT Partnership<br />
Joe Smith quizzes President, Chuck Kearns on NAEMT’s global activities<br />
and finds out how American EMS works with partners worldwide to<br />
share innovation ideas<br />
Also inside:<br />
UNISON Update<br />
Alan Lofthouse says “Keep your promise to ambulance staff!”<br />
TASC News<br />
TASC receives funding boost at ALF 2016<br />
Out & about<br />
The latest EMS news from around the world<br />
Products & Suppliers News<br />
Latest in New Products, Services & Technology<br />
Give us your feedback on this edition by emailing to: editor@ambulancetoday.co.uk<br />
EDITOR: Declan Heneghan email: editor@ambulancetoday.co.uk CORRESPONDENCE: All correspondence should be sent to: The Editor, <strong>Ambulance</strong> Today,<br />
41 Canning Street, Liverpool L8 7NN BUSINESS DEVELOPMENT MANAGER (Europe): Joseph Heneghan CALL: +31 2977 853 95 ASSISTANT-EDITOR: Joseph Smith<br />
FOR EDITORIAL CALL: +44 (0)151 708 8864 FOR ADVERTISING ENQUIRIES CALL: Advertising Sales Manager: Paul Ellis: +44 (0)151 703 0598 OR: +44 (0)7980 539 481<br />
DESIGN & Production: L1 Media email: L1media@yahoo.co.uk<br />
COPYRIGHT: All materials reproduced within are the copyright of <strong>Ambulance</strong> Today. Permission for reproduction of any images or text, in full or in part, should be sought from the Editor.<br />
PUBLISHER’S STATEMENT: <strong>Ambulance</strong> Today magazine is published by <strong>Ambulance</strong> Today Ltd, 41 Canning Street, Liverpool L8 7NN. The views and opinions expressed in this issue are not necessarily those of our Editor or <strong>Ambulance</strong> Today. No<br />
responsibility is accepted for omissions or errors. Every effort is made to ensure accuracy at all times. Advertisements placed in this publication marked “CRB Registered” with the organisation’s “CRB Registration No.” means that the Organisation/Company meets with the<br />
requirements in respect of exempted questions under the Rehabilitation of Offenders Act 1974. All applicants offered employment will be subject to a Criminal Record Check from the Criminal Records Bureau before appointment is confirmed. This will include details of<br />
cautions, reprimands or final warnings, as well as convictions and information held by the Department of Health and Education and Employment
The first European<br />
Emergency Medical Services Congress<br />
Join us for EMS2016 in Copenhagen 30th May to 1st June 2016<br />
As the first of its kind, the European Emergency<br />
Medical Services Congress - EMS 2016 in<br />
Copenhagen will bring together researchers, health care<br />
professionals and managers in the area of emergency<br />
medical services and pre-hospital care.<br />
Through innovation, involvement and a creative<br />
approach, this new congress will provide the latest<br />
knowledge, showcase the newest equipment and<br />
demonstrate best practices in the area of emergency<br />
care: From the citizen’s emergency call, through the<br />
emergency medical dispatch process, the pre-hospital<br />
care by doctors, paramedics and nurses and finally the<br />
emergency care in the emergency department.<br />
The congress will take place in the Tivoli Hotel &<br />
Congress Center 30th May to 1st June 2016 in the<br />
vibrant, progressive and green city of Copenhagen,<br />
Denmark.<br />
Get updated at EMS 2016 in Copenhagen, greet old and<br />
new friends and meet the experts.<br />
We look forward to seeing YOU in Copenhagen, where<br />
we will shape the future of emergency medical services<br />
together.<br />
Read more on our website www.ems2016.org where<br />
news will be posted continuously.<br />
Follow EMS2016 on social media<br />
o Facebook: EMS2016<br />
o Twitter: @EMS_CPH2016<br />
o Instagram: EMS_CPH2016<br />
…or use the #ems2016 or #ambulancesoftheworld<br />
Copenhagen thrives on a mixture of its beautiful<br />
medieval city centre, brave new architecture, a rich<br />
cultural life and an extraordinary culinary scene. The city<br />
is renowned for its take on biking and eco-friendly way of<br />
living.
Some thoughts from EMS2016 keynote speaker Professor Douglas Chamberlain<br />
Our European<br />
<strong>Ambulance</strong> Services:<br />
We Can Learn so much<br />
from Each Other<br />
By Professor Douglas Chamberlain, leading pioneer<br />
of paramedic practice<br />
The wish to assist the sick and wounded goes back millennia in our history. Possibly the first wellorganised<br />
attempts came in the 18th century with the formation of the Humane Societies, set up<br />
principally to save victims from drowning. The first was in Holland, but this development influenced<br />
other countries to develop similar schemes. In the 19th century, the Order of St John spread from<br />
France to many parts of the world ‘to relieve sickness and injury.’ Progressively through the 20th century,<br />
statutory ambulance services were set up wherever a sound civic structure exists. But have we continued<br />
adequately to learn from each other in our own era when communication can be rapid and effective?<br />
Systems have evolved or been developed<br />
purposefully in countries, or not infrequently<br />
in smaller areas, that vary in structure,<br />
in types of organisation, and in efficiency.<br />
Perceived local needs are generally the<br />
driving force, but other influences are<br />
sometimes powerful. Emergency services<br />
may depend on unpaid volunteers, but within<br />
professional organisations the educational<br />
background and required academic levels at<br />
entry vary widely, as do the complexity of<br />
service that can be provided. One major<br />
difference depends on whether or not<br />
physicians play a leading role, either in an<br />
advisory capacity or as active responders.<br />
Of course, there is room for variation within<br />
a service but it is likely that some structures<br />
match local requirements better than others.<br />
Few even in Europe would claim that they<br />
have the best possible system. Deficiencies<br />
may arise partly from financial constraints<br />
but there are other impediments to possible<br />
improvements. Managers, for example,<br />
may have personal reasons for accepting<br />
the status quo or simply be unaware of<br />
unnecessary shortcomings. Such problems<br />
are commonplace in all organisations, but<br />
progress within healthcare impinges strongly<br />
on the well-being and lives of individuals,<br />
and so demands our close attention.<br />
Many of us who have lived through decades<br />
of evolution in medical provision can take<br />
lessons from recent history. Knowledge<br />
within my own specialty of cardiology 50<br />
years ago was circumscribed by geography<br />
and more particularly by language. We did<br />
not dwell on the fact that progress in some<br />
areas may be well in advance of our own<br />
even in closely neighbouring countries, yet<br />
Book your place at EMS2016 now at: www.ems2016.org<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Winter 2014 | <strong>Ambulance</strong>today37
Perfect Partners<br />
Designed based on years of partnership with EMS, the LIFEPAK ® 15 monitor/defibrillator and<br />
the LUCAS ® 2 chest compression system work together to support your team in managing<br />
cardiac arrests.<br />
LUCAS ® 2 Chest Compression System<br />
LUCAS 2 is designed to provide continuous,<br />
uninterrupted compressions while helping to<br />
reduce scene complexity.<br />
LIFEPAK ® 15 Monitor/Defibrillator<br />
The 15 provides the power of 360J, plus the<br />
most advanced monitoring parameters available.<br />
For more information visit www.physio-control.com.<br />
©2015 Physio-Control, Inc. Redmond, WA, U.S.A.<br />
GDR3322999_A
Some thoughts from EMS2016 keynote speaker Professor Douglas Chamberlain<br />
<strong>Ambulance</strong> in use in Odense in 1919. Such horse-drawn<br />
ambulances were used in some provincial cities right up<br />
until the beginning of the 1940s. Source unknown.<br />
this was indeed the case. The creation of<br />
the European Society of Cardiology (ESC)<br />
led to major improvements in this regard<br />
and continues to do so. Within resuscitation<br />
medicine, a breakthrough came when the<br />
Laerdal Foundation invited members of<br />
national groups from many countries to<br />
a meeting in Stavangar where we met<br />
each other for the first time. International<br />
meetings then became commonplace. Not<br />
only did we learn from each other, but a<br />
consensus on best practice was passed<br />
on from a new international committee<br />
(ILCOR) to regional bodies that used them<br />
to create guidelines suitable for local needs.<br />
Our own regional body, within Europe, was<br />
conceived initially as a working group of<br />
the ESC, but fortunately this did not work<br />
out and instead the European Resuscitation<br />
Council (ERC) was formed. This body<br />
has considerable relevance to ambulance<br />
services because it issues important and<br />
definitive advice on the management<br />
of prehospital as well as in-hospital<br />
emergencies. But its remit does not include<br />
organisation.<br />
The question arises as to whether we<br />
need an international group devoted<br />
to ambulance services that may help<br />
them learn from each other in terms of<br />
organisation, scope, and objectives. One<br />
pattern will not suit all, but there will still<br />
be ideas that can be shared to the benefit<br />
of many. Meetings need not be frequent<br />
but occasional direct contact is essential<br />
Red Cross ambulance from the Holbaek approx. 1950.<br />
Source: The Danish Museum of Science, the Zonen<br />
Collection.<br />
so that colleagues from other countries<br />
will be known and indeed friendships built<br />
up. We do already have some national<br />
and local groups but these may have their<br />
own agendas that may not represent views<br />
of the majority of providers. It would be<br />
worth exploring the feasibility of individual<br />
administrative units having membership,<br />
despite large variations in size across nations.<br />
Whilst the intention should not be<br />
pressure to harmonise the types of service,<br />
discussions would have an influence in the<br />
medium or long term. Some principles are<br />
worth mentioning. In all advanced countries,<br />
services should be rapidly available to all<br />
through a common national or international<br />
phone number. Only one service should<br />
exist within any one region. Whilst high<br />
degrees of clinical expertise should be<br />
available, patient transport without the<br />
requirement for immediate treatment<br />
must also be provided. These leave room<br />
for other differences some of which will<br />
depend on other aspects of health care<br />
outside ambulance services; here there is<br />
room for evolution. In some areas of the<br />
United Kingdom, we have practitioners with<br />
advanced training in critical care and others<br />
in domiciliary care. How many levels of<br />
expertise are optimal? Would it be useful<br />
to discuss the criteria for non-conveyance,<br />
the maximum time on scene for different<br />
heart rhythms, the need for widespread<br />
use of emergency ultrasound, the use of<br />
mechanical compression or the availability<br />
of ECMO? In particular, we need additional<br />
<strong>Ambulance</strong> care in the UK began to develop rapidly in the<br />
late 1970S<br />
emphasis on immediate or retrospective<br />
feedback on compression quality, liaison with<br />
community first responders, the necessary<br />
skills of dispatchers, and the immediate<br />
availability of medical or other advice. The<br />
list of course does not end there.<br />
We do have an opportunity to discuss<br />
these matters at the up-coming EMS2016<br />
Congress in Copenhagen in late May. This is<br />
particularly appropriate in that colleagues in<br />
Denmark have shown not only how rapidly<br />
progress can be made but demonstrated<br />
too the impact on benefit to patients.<br />
We can all learn from each other. Let us try<br />
harder to do so.<br />
Pre-hospital cardiac care is now far more advanced<br />
Electrocardiograph patient with technician, c.1929<br />
Medical students watching an operation in theatre,<br />
c.1950-1960<br />
Book your place at EMS2016 now at: www.ems2016.org<br />
Professor<br />
Douglas<br />
Chamberlain’s<br />
keynote address entitled: The<br />
History of EMS will take place at<br />
10.30am on Monday 30th May and<br />
will open EMS2016.<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
9
AMBULANCE | FIRE | POLICE | RELIEF AGENCIES | SPECIALIST RESCUE<br />
CIVIL CONTINGENCIES | COUNTER TERROR<br />
REGISTER FOR FREE TODAY<br />
The Emergency<br />
Preparedness, Resilience<br />
and Response Event<br />
• Network with over 4,000 emergency<br />
preparedness resilience and response<br />
professionals<br />
• Visit the free-to-attend specialist conference<br />
stream chaired by Head of the Cabinet<br />
Office’s Resilience Direct programme<br />
• Explore the latest technology available to<br />
emergency preparedness resilience and<br />
response professionals<br />
Follow us on Twitter for the latest<br />
show news @Ambitionexpouk<br />
Register as a free visitor at<br />
www.ambitionexpouk.com/emergencyservices<br />
Supported by Follow us on Co-located with organised by
Welcome from the Chairman of the Regional Council of Capital Region Denmark<br />
Welcome to<br />
Copenhagen!<br />
By Sophie Hæstorp Andersen<br />
Chairman of the Regional Council of the Capital Region<br />
of Denmark<br />
In 2012 Denmark was on the cover of <strong>Ambulance</strong> Today under the headline “Let’s go Danish.” This spring<br />
Denmark is once again on the cover of the magazine due to the first European Emergency Services<br />
Congress that will be held in Copenhagen.<br />
In Europe emergency medical services<br />
are undergoing development to reflect<br />
changes in healthcare delivery with the<br />
centralization of highly specialized medical<br />
care to fewer and more specialized hospitals<br />
and emergency departments. The emphasis<br />
in the past was mainly on providing safe and<br />
comfortable transportation, rather than on<br />
delivering high-levels of acute clinical care.<br />
This change over the last two decades has<br />
led to an increased focus on pre-hospital<br />
care.<br />
It is extremely complicated and difficult to<br />
save a life. Though it may be individuals who<br />
perform CPR, attach the defibrillator, secure<br />
the airway, and administer medications,<br />
it is a system that makes it all possible.<br />
Cooperation between the dispatch center,<br />
the ambulance services and the emergency<br />
department is essential in saving lives. Lives<br />
are saved not just by highly trained EMS<br />
professionals, but by highly efficient EMS<br />
systems.<br />
There exists incredible variety and diversity<br />
among EMS systems. No two systems are<br />
the same. In Denmark there are five health<br />
care regions and even though we are a small<br />
country there are differences between the<br />
regions.<br />
In Denmark just as in all of Europe we need<br />
to address common challenges and establish<br />
cooperation. In the wake of the terrible<br />
events in both Brussells and Paris it is more<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
important than ever that we can learn from<br />
each other. This will in the end strengthen<br />
our systems and save lives.<br />
I’m incredibly proud that the first European<br />
Emergency Medical Services Congress will<br />
be held in Copenhagen from 30th May to<br />
1st June 2016. EMS2016 will bring together<br />
scientists and professionals in the areas of<br />
emergency medical services and pre-hospital<br />
care. Through innovation, involvement and a<br />
creative approach, the congress will provide<br />
the latest knowledge in the area – from the<br />
citizen’s emergency call all the way to the<br />
actual pre-hospital treatment.<br />
EMS2016 will be held in Greater<br />
Copenhagen. Greater Copenhagen is<br />
where Denmark meets Sweden and<br />
Scandinavia meets the world. It is where<br />
we cooperate and connect people, access<br />
sectors, industries, cultures and countries. It<br />
is freedom and happiness.<br />
To all the first responders, emergency<br />
medical technicians, paramedics, emergency<br />
tele-communicators, doctors, nurses and all<br />
who work in emergency medical services:<br />
Thank you for your work!<br />
I look forward to seeing you in Copenhagen.<br />
Warm regards,<br />
Sophie Hæstorp Andersen<br />
Chairman of the Regional Council of the<br />
Capital Region of Denmark<br />
Capital Region of Denmark<br />
– Some facts and figures:<br />
• 1.8 M. inhabitants<br />
• 2,561 square km - approx. 6% of Denmark<br />
• 29 municipalities<br />
• Population density five times higher than the<br />
country’s average<br />
• Approx. 40,000 employees<br />
• Total budget approx. 5 billion euros<br />
(38 billion dkk.)<br />
• The Capital Region of Denmark is one of five<br />
regional administrative units in Denmark. It<br />
provides healthcare, mental healthcare services<br />
and also carries out research and regional<br />
development for 30% of the population in<br />
Denmark.<br />
• In addition to hosting the largest health care<br />
system in Denmark, the region is also home to<br />
one of the world’s strongest life science clusters,<br />
and 70% of Denmark’s biotech companies are<br />
located in the area.<br />
• Denmark is in fourth place among the OECD<br />
countries regarding scientific publications per<br />
inhabitant and similarly in third place regarding<br />
citations. Accordingly health research in the<br />
Capital Region ranks among the best in Europe.<br />
Biography:<br />
Sophie Hæstorp Andersen<br />
Sophie Hæstorp Andersen, is a member of<br />
the Social Democratic Party and has served<br />
as chairman of the Regional Council in the<br />
Capital Region since 2014. Before that she was<br />
Chairman of the Health Committee in the<br />
Danish Parliament from 2013-2014.<br />
Sophie was born in Copenhagen in 1974,<br />
where she lives today with her spouse and<br />
their two children Rolf and Rosa. Educated as<br />
a political scientist she wrote a thesis on the<br />
Danish Quality Improvement Accreditation<br />
system in the public health care sector. She has<br />
been the Chairwoman of the management<br />
board of ‘Plejebo’ Nursing Centre since 2004<br />
and a Member of the governing body of the<br />
AIDS Foundation from 2004-2012. Sophie was<br />
officially appointed “User Friend” of the Danish<br />
Drug Users Union in 2008.<br />
Winter 2014 | <strong>Ambulance</strong>today3 11
www.kl-insurance.co.uk<br />
Kerry London is a major provider<br />
of insurance cover for the<br />
Private <strong>Ambulance</strong> Sector<br />
Our exclusive <strong>Ambulance</strong> and Medical Malpractice schemes are designed to meet your<br />
needs, offer first class cover from leading UK insurers and can cater for any size company<br />
Medical Malpractice<br />
& Extensions:<br />
Worldwide cover excluding<br />
USA/Canada<br />
Crisis Containment<br />
Employers Liability<br />
Public Liability up to £10m<br />
Professional Indemnity<br />
Interest Free Instalments<br />
available<br />
<strong>Ambulance</strong> Motor<br />
& Extensions:<br />
Blue Light Cover<br />
Event Coverage<br />
Patient/Organ Transfer<br />
Community First Responder<br />
Airside Liability<br />
Discounts are available<br />
for increased excesses<br />
or restricted driving<br />
Contact us for a no<br />
obligation quotation<br />
or for more details call<br />
tel: 020 8225 1054<br />
or email melissacroxford@kerrylondon.co.uk<br />
Kerry London Ltd is authorised and regulated<br />
by the Financial Conduct Authority. Registered Office:<br />
2nd Floor John Stow House, 18 Bevis Marks, London<br />
EC3A 7JB. Registered No. 02006558 (England).
Focus on Establishing a Global Resuscitation Alliance<br />
We Must Work Tirelessly to “Snatch<br />
Life from the Jaws of Death”<br />
A Call to Establish a Global<br />
Resuscitation Alliance<br />
In June 2015 at the Utstein Abbey near Stavanger, Norway, 36 Emergency Medical Services leaders,<br />
researchers, and experts from throughout the world convened to address the challenge of how to<br />
increase survival from out-of-hospital cardiac arrest. We have science and solutions but how do we<br />
achieve implementation of best practices? The answer: a Call to Establish a Global Resuscitation Alliance.<br />
By Freddy K. Lippert, CEO EMS Copenhagen, Denmark; Sang Do Shin, Medical Director Seoul<br />
Metropolitan Fire Department, Seoul South Korea; Tore Laerdal, Director Laerdal Foundation, Norway;<br />
Mickey Eisenberg, Director Medical Quality Improvement, King County EMS, Seattle USA.<br />
The history of Utstein<br />
In 1990 at the historic Utstein Abbey near<br />
Stavanger, Norway, international researchers<br />
and Emergency Medical Service (EMS)<br />
program and medical directors gathered<br />
to solve a problem. There was either a lack<br />
of data or inconsistencies in data about<br />
cardiac arrest survival. Attempts to measure<br />
performance with various case definitions led<br />
to inconsistencies in calculating survival rates.<br />
In short, there was insufficient data and no<br />
common terminology.<br />
The meeting resulted in a consensus<br />
recommendation on terminology and on<br />
how to report survival data. A paper was<br />
published in 1991 simultaneously in several<br />
leading scientific journals which became<br />
a landmark paper for research within<br />
resuscitation.<br />
This process of defining the essential<br />
elements of a cardiac arrest registry came to<br />
be known variously as the Utstein method,<br />
the Utstein template, the Utstein style, or<br />
merely Utstein. All resuscitation scientists<br />
have adopted it, and the original Utstein<br />
article remains one of the most cited articles<br />
in resuscitation science.<br />
Since the first Utstein meeting in 1990, 16<br />
consensus papers have been issued and<br />
25 meetings held on various topics relating<br />
to resuscitation and resuscitation research.<br />
The original paper was updated in 2004<br />
and again in 2014 and continues to have<br />
a major impact on science and reporting<br />
data.<br />
The Utstein meeting in 2015 on<br />
implementation<br />
In 2015, twenty five years after the first<br />
Utstein meeting, 36 resuscitation leaders<br />
gathered at Utstein to solve another<br />
problem – how best to implement best<br />
practices and successful strategies in<br />
managing cardiac arrest and how to spread<br />
the lessons of best practices to EMS systems<br />
and communities.<br />
Biography:<br />
Freddy K. Lippert, MD<br />
Freddy K. Lippert, MD,<br />
Associate Professor, FERC,<br />
is CEO of the Emergency<br />
Medical Services in<br />
Copenhagen, Denmark. The<br />
EMS Copenhagen covers a<br />
population of 1.7 million, i.e.<br />
one third of the Danish population. The EMS<br />
Copenhagen includes the following: Emergency<br />
Medical Dispatch, ambulance services including<br />
physician manned mobile critical care units,<br />
psychiatric mobile unit, a medical hotline 24/7,<br />
responsibility and coordination of medical<br />
preparedness on behalf of all hospitals in the<br />
Capital Region.<br />
Biography:<br />
Sang Do Shin, MD, MPH, PhD<br />
Sang Do Shin, MD, MPH, PhD,<br />
is associate professor in the<br />
Department of Emergency<br />
Medicine at the Seoul<br />
National University College<br />
of Medicine in Seoul, Korea.<br />
He’s also the director of<br />
the Laboratory of EMS at the Seoul National<br />
University Biomedical Research Institute.<br />
The results of the meeting are a call for<br />
the establishment of a Global Resuscitation<br />
Alliance in order to expand internationally<br />
the reach and utility of the Resuscitation<br />
Academy concept developed in King County,<br />
Seattle beginning in 2008. Such a global<br />
effort will promote best practices and offer<br />
help with implementation to countless<br />
communities.<br />
Biography:<br />
Tore Laerdal<br />
Tore Laerdal is Executive<br />
Director of the Laerdal<br />
Foundation, chairman of<br />
Laerdal Medical, and managing<br />
director of Laerdal Global<br />
Health. In recent years he<br />
has focused on helping<br />
reduce maternal and newborn mortality in<br />
low resource settings. For this purpose Laerdal<br />
Global Health has partnered with USAID, NIH,<br />
Save the Children, the American Academy of<br />
Pediatrics and others in the Helping Babies<br />
Breathe alliance and the Survive & Thrive<br />
alliance.<br />
Biography:<br />
Mickey Eisenberg, MD, Ph.D<br />
Mickey Eisenberg, MD, Ph.D,<br />
is Director of Medical QI at<br />
the King County Emergency<br />
Medicine Services and<br />
Professor of Medicine at the<br />
University of Washington. He<br />
has studied cardiac arrest and<br />
developed innovative programs to treat this<br />
condition for 40 years. His book, ‘Resuscitate!<br />
How your Community can Improve Survival<br />
from Sudden Cardiac Arrest – second edition’<br />
was published by University of Washington<br />
Press in 2013.<br />
Book your place at EMS2016 now at: www.ems2016.org<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Winter 2014 | <strong>Ambulance</strong>today3 13
Does he need a trauma centre<br />
or the local hospital?<br />
Twenty-year-old male in a motor vehicle accident. Airbag<br />
has deployed. Car has significant front-end damage.<br />
Is he bleeding internally? Will he need a trauma centre?<br />
These are some of the questions you need to answer on a<br />
suspected trauma call, as haemorrhage is the leading cause of death after injury. 1<br />
The new trauma parameters on the ZOLL X Series ® help you accurately and quickly<br />
assess your patients so you can feel more confident in your treatment decisions.<br />
Insight for informed decisions.<br />
www.zoll.com/uk/trauma-care<br />
1<br />
Acosta JA, et al. Journal of the American College of Surgeons. 1998;186(5):528-533.<br />
©2016 ZOLL Medical Corporation, Chelmsford, MA, USA. X Series and ZOLL are trademarks or registered trademarks of ZOLL Medical Corporation in the United States and/or other countries.<br />
MCN IP 1601 0092-05
Focus on Establishing a Global Resuscitation Alliance<br />
The famous Utstein Abbey near Stavanger in Norway<br />
This call to action declares the current<br />
situation to be unacceptable and states:<br />
• We believe communities can and must do<br />
better.<br />
• We believe, based upon current<br />
knowledge, that with adherence to<br />
and implementation of best practices<br />
communities can increase survival from<br />
cardiac arrest by 50%.<br />
• We believe the establishment of a Global<br />
Resuscitation Alliance will help educate EMS<br />
leaders about best practices and provide<br />
tools to help improve survival in their<br />
communities.<br />
Interventions that determine the<br />
outcome from cardiac arrest<br />
Several critical interventions and their<br />
timely application determine the outcome<br />
from cardiac arrest. In cardiac arrest<br />
the likelihood of surviving declines by<br />
approximately 10% for every minute. Thus<br />
the intervals from collapse to application<br />
of key interventions largely determine the<br />
likelihood of survival. The main interventions<br />
include: rapid dispatch of EMS, telephoneassisted<br />
cardiopulmonary resuscitation<br />
(T-CPR), bystander CPR, provision of high<br />
performance CPR, and early defibrillation.<br />
Both rapid time of application and high<br />
quality of these interventions define best<br />
performing EMS systems.<br />
Global Resuscitation Alliance<br />
It is now time to turn our attention to<br />
programmatic improvement. Ideally best<br />
practices should become the standard<br />
of care; thereby leading to dramatic<br />
improvements in survival. Best practice is a<br />
dynamic concept since new therapies and<br />
programs begin to define new best practices.<br />
Therein lays the power of “measure and<br />
improve”. Constant measuring enables<br />
determination of what needs improving, and<br />
demonstrates if improvement occurs - which<br />
can define new best practices.<br />
The coming decades should become the<br />
era of using measurement to help define<br />
and implement best practices. It appears<br />
from the literature that it commonly takes<br />
5-10 years before new knowledge and<br />
guidelines are generally implemented even<br />
after scientific consensus. That process<br />
must be speeded up! This requires better<br />
understanding of what factors stimulate and<br />
what factors hinder implementation of new<br />
knowledge and best practices.<br />
The establishment of a Global Resuscitation<br />
Alliance is a concrete means to catalyze<br />
progress in survival. A Global Resuscitation<br />
Alliance can provide the tools and support<br />
for communities to put on local programs<br />
modeled after the Resuscitation Academy<br />
and thereby promote best practices locally.<br />
The ongoing process, typified by the Utstein<br />
meeting on implementation, promises yet<br />
more advances in resuscitation and survival.<br />
To these individuals and to the hundreds of<br />
thousands of first responders, emergency<br />
medical technicians, paramedics, emergency<br />
tele-communicators, doctors, nurses and all<br />
Ten Steps to Improve<br />
Cardiac Arrest Survival<br />
1. Establish a cardiac arrest registry<br />
2. Begin Telephone-CPR with ongoing<br />
training and QI<br />
3. Begin high-performance EMS CPR<br />
with ongoing training and QI<br />
4. Begin rapid dispatch<br />
5. Measure professional resuscitatiion<br />
using the defibrillator recording<br />
(and voice if possible)<br />
6. Begin an AED program for first<br />
responders, including police officers,<br />
guards, and other security personnel.<br />
7. Use smart technologies to extend<br />
CPR and public access defibrillation<br />
programs to notify volunteer<br />
bystanders who can respond to nearby<br />
arrest to provide early CPR and<br />
defibrillation<br />
8. Make CPR and AED training<br />
mandatory in schools and the<br />
community<br />
9. Work toward accountability – submit<br />
annual reports to the community<br />
10. Work toward a culture of excellence<br />
Figure 2. Ten steps to improve Cardiac Arrest survival<br />
who work so tirelessly to snatch life from<br />
the jaws of death, we dedicate this call to<br />
action.<br />
EMS2016 to promote the Global<br />
Resuscitation Alliance<br />
Prior to the European EMS2016 congress a<br />
second Utstein Meeting on implementation<br />
will be held in Copenhagen with experts<br />
and representatives from major international<br />
EMS systems and international organizations.<br />
The meeting will further bring the Global<br />
Resuscitation Alliance to reality and begin to<br />
provide tools for implementation.<br />
• Cardiac arrest registry<br />
• Telephone CPR<br />
• High performance CPR<br />
• Rapid dispatch<br />
• Measurement of<br />
professional resuscitation<br />
• AED program for<br />
first responders<br />
• Smart technologies<br />
for CPR and AED<br />
• Accountability<br />
• Culture of excellence<br />
Improved<br />
Survival<br />
Figure 1. Programs and actions to implement best practices<br />
• Form a team<br />
• Select programs<br />
• Plan implementation<br />
strategy<br />
• Set specific goals<br />
• Achieve buy-in<br />
• Establish standards<br />
• Pilot the program<br />
• Consult experts<br />
• Communicate<br />
progress<br />
• Support, advocate<br />
celebrate<br />
Therefore: Join us for the 1st<br />
European Emergency Medical<br />
Services Congress to be held in<br />
Copenhagen 30th May to 1st June<br />
2016 where the results from the<br />
Utstein meeting will be presented.<br />
This short paper is based upon the full paper:<br />
Improving Survival from Out-of-Hospital<br />
Cardiac Arrest: A Call to Establish a Global<br />
Resuscitation Alliance. The full paper can be<br />
downloaded from the Resuscitation Academy<br />
homepage: www.resuscitationacademy.com<br />
www.resuscitationacademy.com/wp-content/<br />
uploads/2016/03/A-Call-to-Establish-a-Global-<br />
Resuscitation-Alliance1.pdf<br />
Citation: “It takes a system to save a<br />
life” from Resuscitation Academy<br />
Book your place at EMS2016 now at: www.ems2016.org<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Winter 2014 | <strong>Ambulance</strong>today3<br />
15
At hand when needed most.<br />
LIVOPAN®/ENTONOX® – The rapid and<br />
safe response to emergency care.<br />
LIVOPAN/ENTONOX is a ready-to-use medical gas mixture of N 2 O and O 2 that is safe<br />
and effective for both adults and children. When inhaled, LIVOPAN/ENTONOX provides<br />
a comparable opioid-like analgesic effect with rapid onset and offset of action.<br />
LIVOPAN/ENTONOX has a proven safety profile for use in both children and adults, with<br />
minimal side effects, making LIVOPAN/ENTONOX the safest option in the emergency<br />
setting where treating patient discomfort and managing cost and time pressures<br />
is essential.<br />
Linde: Living healthcare<br />
Linde AG<br />
Linde Healthcare, Seitnerstrasse 70, 82049 Pullach, Germany<br />
Phone +49.89.7446-0, www.linde-healthcare.com<br />
LIVOPAN® and ENTONOX® are registered trademarks of The Linde Group.
Focus on Resuscitation Academy<br />
Resuscitation Academy - Improving survival<br />
from out of hospital cardiac arrest through<br />
implementation of best practices<br />
Sudden cardiac arrest is the leading cause of death among adults, yet it need not be fatal. Though survival<br />
in most communities is very poor, some communities and Emergency Medical Services Systems have<br />
accomplished outstanding improvement and results. Why are some communities and EMS systems so<br />
successful when others are not? And which steps can we take to improve outcomes?<br />
These are some of the questions addressed by the Resuscitation Academy.<br />
By Ann Doll, Executive Director, Resuscitation Academy, Seattle USA: and Tom Rea, Medical Director,<br />
King County EMS, Washington USA; Mickey Eisenberg, Director, Medical QI, King County EMS,<br />
Washington USA; Sang Do Shin, Medical Director Seoul Metropolitan Fire Department, South Korea;<br />
Freddy K. Lippert, Chief Executive Director, Emergency Medical Services, Copenhagen, Denmark<br />
A leading cause of death despites<br />
advances<br />
Sudden cardiac arrest remains a leading<br />
cause of death in most modern societies,<br />
despite important advances in prevention.<br />
As disturbing as the magnitude of the<br />
problem is, the disparity in survival among<br />
communities is tremendous, even though<br />
resuscitation guidelines provide an evidencebased<br />
approach for treatment. For example<br />
there is often a 10-fold difference in survival<br />
among communities adhering to best<br />
practices compared to communities with<br />
poor adherence and some have improved<br />
considerable while others are haven’t.<br />
“It takes a system so save a life”<br />
Whether an individual lives or dies following<br />
sudden cardiac arrest is a function of many<br />
factors and circumstances. These factors<br />
may conveniently be grouped into patient<br />
factors, event factors, and system factors.<br />
Most patient and event factors, while very<br />
important, are not changeable or alterable by<br />
the responding emergency medical service<br />
personnel. What is alterable, however, is<br />
the configuration and quality of the system<br />
responding to the cardiac arrest.<br />
The chain of survival describes time-sensitive,<br />
coordinated steps in community response<br />
that need to occur to achieve the best<br />
chances of survival. If just one link is missing<br />
or weak the chances of survival decrease<br />
tremendously. Every community’s EMS<br />
system already incorporates some if not<br />
all of these system factors at least to some<br />
degree – but even these factors, although<br />
they’re necessary, are not sufficient.<br />
The history of the Resuscitation<br />
Academy<br />
The Resuscitation Academy was established<br />
in 2008 in King County, Seattle, USA with<br />
the goal to improve cardiac arrest survival.<br />
It was apparent from the first Resuscitation<br />
Academy class in 2008 that the lectures,<br />
breakout sessions and workshops could only<br />
go so far. The faculty needed to spell out<br />
the details of how to implement the various<br />
programs locally. The Resuscitation Academy<br />
Tool Kits were developed to do just this.<br />
Resuscitation Academy provides “How to?”<br />
guides, for setting up various programs<br />
Biography:<br />
Ann Doll<br />
Director, Resuscitation Academy<br />
Ann helped to create the<br />
Resuscitation Academy in<br />
2008 as a way for Seattle<br />
& King County to share<br />
best practices for improving<br />
cardiac arrest survival. Her<br />
background includes 20 years<br />
of program management and patient education.<br />
Email: Ann.Doll@kingcounty.gov<br />
Biography:<br />
Thomas D. Rea, MD, MPH<br />
Thomas D. Rea, MD, MPH<br />
Dr. Thomas Rea is Medical<br />
Program Director for King<br />
County EMS and Professor of<br />
Medicine at the University of<br />
Washington and Harborview<br />
Medical Center. He has the<br />
good fortune of spending the past decade<br />
working with the King County Medic One<br />
Paramedic group and looks forward to working<br />
more closely with the Fire Departments in<br />
King County to continue the high standard of<br />
EMS care.<br />
Email: rea123@u.washington.edu<br />
Book your place at EMS2016 now at: www.ems2016.org<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Winter 2014 | <strong>Ambulance</strong>today3 17
PARAMEDICS - SOUTH WEST<br />
£27,115 TO £35,225 (INCLUSIVE OF ENHANCEMENTS) *<br />
We understand that the better we look after you,<br />
the better equipped you’ll be to look after our patients.<br />
We are committed to providing our staff with the skills and support they need<br />
to deliver a higher level of care, enabling more patients to be treated without<br />
conveyance to hospital. And we want a better future for you too. Our career<br />
framework is designed to support your development with many existing<br />
staff being testament to our commitment to internal progression.<br />
Whether you crave a coastal location, the best of the British countryside or the<br />
historic cities of Cheltenham, Bath and Bristol (to name but a few), you really<br />
will find a better lifestyle outside of work here in the beautiful South West.<br />
• Permanent and bank<br />
opportunities available<br />
• One of the most beautiful parts<br />
of the country<br />
• Lowest conveyance rate in the UK<br />
• The most clinically advanced<br />
Trust within the UK<br />
• A better work-life balance<br />
• Structured career pathway<br />
• Up to £8,000 relocation fee package*<br />
Let us look after you better.<br />
For your next career move visit<br />
www.betterparamedic.co.uk<br />
/swasFT<br />
*Subject to qualifying criteria.<br />
Better you, Better everybody.
Focus on Resuscitation Academy<br />
within local communities . A key publication<br />
for the concept is the book: Ten Steps for<br />
Improving Survival from out-of-hospital<br />
Cardiac Arrest. The Resuscitation Academy<br />
is offered tuition-free and attendees come<br />
from throughout the world. The small class<br />
size allows for a two-way exchange of<br />
information – the faculty provides evidencebased<br />
information and tools to improve<br />
cardiac arrest survival and the attendees<br />
share the real-life challenges they face. A<br />
Resuscitation Academy session could be a<br />
two-day full course for managers and leaders<br />
looking at all components in the chain of<br />
survival or it could be a 2-4 hour workshop<br />
during a congress to focus on quality CPR<br />
for paramedics.<br />
Every community has a different<br />
constellation of culture, leadership, resources,<br />
and opportunity. The faculty of the<br />
Resuscitation Academy has learned that<br />
change is very challenging, and one should<br />
never assume that just because you present<br />
a good idea that it will be embraced and<br />
implemented next day in another setting.<br />
Impediments to change, whether they<br />
stem from habit, inertia, malaise, or lack<br />
of resources, will overwhelm the best of<br />
intentions.<br />
From Resuscitation Academy in<br />
Seattle to a Global Resuscitation<br />
Alliance<br />
The Resuscitation Academy is providing<br />
examples of best practices and at the same<br />
time tools for local implementation. This is<br />
part of its success in the USA. Resuscitation<br />
Academy as a concept has also been<br />
introduced in various countries in Europe<br />
and Asia. It is now time to ensure further<br />
implementation worldwide and to do this in<br />
an organized way. The recommendation from<br />
a recent Utstein meeting on implementation<br />
of best practices is to disseminate the<br />
concept of Resuscitation Academy<br />
internationally by establishing a Global<br />
Resuscitation Alliance.<br />
Photographs courtesy Thomas Voss<br />
This paper is a short summary of the<br />
concept of Resuscitation Academy.<br />
More information can be found and<br />
downloaded from the website of<br />
Resuscitation Academy in Seattle.<br />
Homepage of Resuscitation Academy:<br />
www.resuscitationacademy.org/<br />
Ten Steps for improving survival:<br />
www.resuscitationacademy.org/<br />
downloads/ebook/TenStepsforImproving<br />
SurvivalFromSuddenCardiacArrest-RAeBook-PDFFinal-v1_2.pdf<br />
Utstein paper on Global Resuscitation<br />
Alliance: www.resuscitationacademy.<br />
org/wp-content/uploads/2016/03/A-Call-<br />
to-Establish-a-Global-Resuscitation-<br />
Alliance1.pdf<br />
Book your place at EMS2016 now at: www.ems2016.org<br />
THE INTERNATIONAL CENTRE,<br />
TELFORD TF3 4JH<br />
7th & 8th June 2016<br />
AMBULANCE FIRE & RESCUE POLICE<br />
To register to attend this unique<br />
Fleet Exhibition showcasing over<br />
100 vehicles, technology and equipment<br />
suppliers from the <strong>Ambulance</strong>,<br />
Fire & Rescue and Police sectors please<br />
go to www.napfmevent.org.uk/visitor or<br />
contact the office for more information<br />
about attending as a delegate or exhibitor.<br />
NAPFM Event Office<br />
Mobile: +44 (0)7885 353160<br />
E: joanna@napfmevent.org.uk<br />
W: www.napfmevent.org.uk<br />
West Mercia Police & Crime Commissioner,<br />
Exchequer Services, PO Box 55<br />
Worchester WR3 8SP<br />
Including<br />
NATIONAL ASSOCIATION OF<br />
POLICE FLEET MANAGERS CONFERENCE<br />
THE NATIONAL STRATEGIC AMBULANCE FLEET<br />
GROUP MEETING<br />
MANUFACTURER UPDATE SESSIONS<br />
FOR WORKSHOP STAFF<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Winter 2014 | <strong>Ambulance</strong>today3 19
EMS2016 – Welcome from Congress Organisers<br />
Let’s shape<br />
the future for<br />
Emergency<br />
Medical<br />
Services in<br />
Europe!<br />
Pre-hospital emergency care and emergency medical services (EMS) have advanced at a steady but<br />
increasingly rapid pace during the last decades. With growing public expectations of emergency care -<br />
now - more than ever, it is important that we learn from the latest knowledge, evidence, training, and<br />
technology and that we cooperate across Europe to identify best practice and find new solutions. That’s<br />
why we are organizing the first European EMS congress.<br />
By Freddy K. Lippert, Fionna Moore and Jerry Overton<br />
The important role of EMS today<br />
Emergency medical services (EMS) have<br />
transformed over the last decades from<br />
patient transport to advanced medical care<br />
provided at scene and during transport to<br />
definitive care. Emergency medical dispatch<br />
is now the gatekeeper to emergency<br />
care in many EMS systems. The role of<br />
the emergency call and dispatch centre is<br />
more than identification, prioritizing and<br />
dispatching the right resources to the patient,<br />
now serving as an important clinical hub. In<br />
addition, it provides instruction for the lay<br />
person to begin care, the most important<br />
of which is telephone-assisted lifesaving<br />
CPR instructions. Some EMS systems are<br />
providing enhanced assessment by clinicians<br />
enabling referral to alternative appropriate<br />
pathways for patients with lower acuity<br />
symptoms. The focus is always on maintaining<br />
patient safety and using emergency resources<br />
more efficiently.<br />
Emergency medical services are also<br />
undergoing development which reflect<br />
changes in healthcare delivery with<br />
centralization of highly specialized medical<br />
care to fewer and more specialized hospitals<br />
and emergency departments and a greater<br />
emphasis on locally provided care where<br />
appropriate. This has led to an increased<br />
focus on pre-hospital care and is also why<br />
EMS plays an even more important role<br />
today.<br />
Why an EMS congress in Europe?<br />
There has been no dedicated EMS congress<br />
in Europe to address our common<br />
challenges. Therefore it is essential that<br />
we create an overview of and establish<br />
cooperation between the EMS systems in<br />
Europe. We need to explore each other’s<br />
strengths, limitations and current challenges.<br />
We need to describe a desired vision of<br />
the European emergency care system and<br />
recommend strategies to reach our goals.<br />
That is why we have organized an EMS<br />
congress in Europe – the first of its kind. The<br />
first European Emergency Medical Services<br />
Congress will be held in Copenhagen from<br />
30th May to 1st June 2016.<br />
Our ambitions – your ambitions<br />
It is our ambition that the first European<br />
EMS2016 should make such a significant<br />
impact and be such a success that it creates<br />
expectations for similar events in the future.<br />
In so doing, we aim to set the standard for<br />
future EMS congresses in Europe and for the<br />
development of a network of EMS leaders.<br />
EMS2016 will be a catalyst for future<br />
research, education and product<br />
development by disseminating<br />
existing knowledge and proposing the<br />
implementation of best practice, thus<br />
resulting in better care for the patients.<br />
EMS2016 will also have a strong focus<br />
on clinical practice, leadership and<br />
development.<br />
At EMS2016 we will create a setting where<br />
the leading experts in the field will share<br />
their experiences and where you as a<br />
participant will be given the opportunity to<br />
contribute with professional input across<br />
different fields. In the various forums you will<br />
be able to learn new practices or develop<br />
ideas for new research areas, the latest in<br />
product development as well as educational<br />
qualifications in various areas.<br />
A different Congress – for you!<br />
The congress will be characterized by its<br />
desire to encourage involvement and active<br />
participation. As a participant or exhibitor<br />
Book your place at EMS2016 now at: www.ems2016.org<br />
20 Spring 2016 | <strong>Ambulance</strong>today
EMS2016 – Welcome from Congress Organisers<br />
you will be asked to contribute as this is all<br />
for you!<br />
Through workshops, poster presentations<br />
and events– you as a participant will be<br />
asked to contribute. You will be given the<br />
opportunity to speak up and use social<br />
media at debates as well as to network and<br />
meet in small forums to develop ideas, for<br />
e.g. on product innovation and debates on<br />
specific topics.<br />
This also applies to the exhibition and<br />
the sponsors. The exhibitors will be an<br />
important part of the Congress and we<br />
are encouraging them to make their stands<br />
interactive with a focus on learning. Ideas<br />
for developing new solutions depend on<br />
interaction between clinicians, managers and<br />
exhibitors – we want to encourage this.<br />
The new Global Resuscitation<br />
Alliance<br />
EMS2016 is also proud to present and<br />
promote implementation of the new Global<br />
Resuscitation Alliance as part of the program.<br />
The Global Resuscitation Alliance is being<br />
established as a recommendation from an<br />
Utstein meeting on implementation held at<br />
Biography:<br />
Freddy K. Lippert<br />
Freddy K. Lippert, MD,<br />
Associate Professor, FERC,<br />
is CEO of the Emergency<br />
Medical Services in<br />
Copenhagen, Denmark.<br />
Freddy has served as board<br />
member of the European<br />
Resuscitation Council<br />
and as General Assembly<br />
member for years and is a founding member<br />
of the European Trauma Course. Freddy is<br />
chair of the regional Resuscitation Committee<br />
in Copenhagen, covering the Emergency<br />
Medical Services and five hospitals. Freddy is<br />
an associate professor, Faculty of Health and<br />
Medical Sciences, University of Copenhagen.<br />
Freddy has as a physician more than twenty<br />
years of experience in resuscitation, trauma<br />
care and emergency care and has published<br />
more than one hundred scientific publications<br />
and contributions to books. Recent research<br />
and publications include improved outcome<br />
from Out-of-Hospital Cardiac Arrest and<br />
implementation and use of public access<br />
defibrillation programs.<br />
Ustein near Stavanger in Norway in 2015. A<br />
follow-up meeting with international experts<br />
takes place 2 days prior to the EMS2016<br />
Congress and the result will be announced<br />
during the Congress.<br />
The new European EMS Leadership<br />
Network<br />
One of the key goals of the Congress is<br />
to establish a European EMS Leadership<br />
Network. The network will consist of initially<br />
limited numbers, but will be comprised<br />
of strongly committed CEOs, medical<br />
directors and managers from across<br />
European emergency medical services,<br />
including medical dispatch.<br />
In the wake of the recent Brussels and Paris<br />
attacks, and utilizing the learning from the<br />
recent multinational exercises (Exercise<br />
Unified Response) now more than ever<br />
– it is important that we have a highly<br />
active European EMS Leadership network.<br />
Therefore it is essential that we create<br />
an overview of and establish cooperation<br />
between the EMS systems in Europe to<br />
explore each other’s strengths, limitations<br />
and future challenges.<br />
Biography:<br />
Jerry Overton<br />
Jerry Overton serves as the<br />
Chair of the International<br />
Academies of Emergency<br />
Dispatch, the organization<br />
charged with setting<br />
standards, establishing<br />
curriculum, and conducting<br />
research for public safety<br />
dispatch worldwide.<br />
Previously, he served as the Chief Executive<br />
Officer, Richmond <strong>Ambulance</strong> Authority (RAA),<br />
Richmond, Virginia, for 18 years and had overall<br />
responsibility for the EMS system. Jerry is a<br />
Past President of the American <strong>Ambulance</strong><br />
Association, was a member of the Institute<br />
of Medicine’s Committee on the Future of<br />
Emergency Care in the U. S. Health System, and<br />
is the Treasurer for the World Association of<br />
Disaster and Emergency Medicine.<br />
He serves on the editorial boards of two<br />
leading prehospital care journals and has<br />
received numerous recognitions. As an<br />
expert in EMS system design and deployment<br />
strategies, Jerry was named one of the 20 most<br />
influential leaders in EMS by JEMS magazine<br />
This makes the timing of the unveiling of<br />
the EMS Leadership Network at EMS2016<br />
in Copenhagen very timely. The network<br />
will be dynamic and agile, responding to the<br />
changing needs and priorities of participating<br />
EMS organizations. The European EMS<br />
network will bring the future EMS congresses<br />
forward and will support the implementation<br />
of the coming Global Resuscitation Alliance.<br />
As part of EMS2016 we will have a session<br />
for you and international EMS leaders to<br />
discuss the future for EMS. At EMS2016<br />
we aim to shape the future for EMS in<br />
Europe. That is why EMS2016 will provide<br />
an unparalleled opportunity for you to have<br />
your say and to influence EMS leadership in<br />
Europe!<br />
So join us for the 1st European<br />
Emergency Medical Services<br />
Congress in Copenhagen from<br />
30th May to 1st June 2016 where<br />
together we will shape the future<br />
for emergency medical services and<br />
pre-hospital emergency care. We<br />
all look forward to seeing you all in<br />
Copenhagen!<br />
Biography:<br />
Fionna Moore<br />
Fiona Moore, MD, is<br />
Chief Executive Officer of<br />
the London <strong>Ambulance</strong><br />
Service. Fionna has been a<br />
Consultant in Emergency<br />
Medicine since 1985,<br />
holding appointments at<br />
University College Hospital,<br />
the John Radcliffe in Oxford<br />
and most recently Imperial College Healthcare<br />
Trust. She is an Honorary Consultant to<br />
London’s Air <strong>Ambulance</strong>.<br />
Fionna was appointed to Healthcare for<br />
London’s Clinical Advisory Group in 2007 and<br />
was London’s first Trauma Director from 2009.<br />
She is a member of the London Clinical Senate<br />
and the National Clinical Reference Group for<br />
Major Trauma.<br />
Fionna developed and implemented London’s<br />
Major Trauma System 2009-2013. She has an<br />
unparalleled experience in major incidents and<br />
planned events in London from 1988 and she<br />
is recognized internationally for improving pre<br />
hospital care (Gathering of Eagles award 2015).<br />
Book your place at EMS2016 now at: www.ems2016.org<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Winter 2014 | <strong>Ambulance</strong>today3 21
Focus on EMS2016 Scientific Programme<br />
EMS 2016 Scientific Programme:<br />
From Science to Survival<br />
The EMS2016 Scientific Committee has created a programme that will inspire, encourage and provide<br />
participants with the latest knowledge in the area.<br />
The programme will place strong emphasis on our shared challenges in emergency care, the sessions<br />
will focus on research and clinical practice and the speakers are leading figures within their fields.<br />
Furthermore the programme will set the scene for networking between all European EMS providers,<br />
researchers and exhibitors.<br />
The full programme can be found at: http://ems2016.org/scientific-programme/<br />
Monday, May 30, 2016<br />
10:30 AM<br />
Opening Ceremony and Keynote speaker<br />
Freddy Lippert, Douglas Chamberlain, Sophie<br />
Hæstorp Andersen, and Sophie Løhde<br />
Tivoli Hotel & Congress Center,<br />
May 30, 10:30 AM 11:30 AM<br />
11:30 AM<br />
Coffee Break<br />
Exhibition Areas<br />
May 30, 11:30 AM 12:00 PM<br />
12:00 PM<br />
Triage, referral and advice<br />
Andrew Lockey, Philipp Schuetz, Torben Wisborg,<br />
Andy Newton, and Philip D. Anderson<br />
Carstensen<br />
May 30, 12:00 PM 1:15 PM<br />
Emergency neurology<br />
Corey Slovis, M.D., Caroline L. Watkins, Hans<br />
Morten Lossius, HML, Jana Seblova, and Maren<br />
Ranhoff Hov<br />
Pjerrot<br />
May 30, 12:00 PM 1:15 PM<br />
Breakout session: Best Abstract – Oral<br />
presentationLars S. Rasmussen and Joost Bierens<br />
Akvariet 4+5,<br />
May 30, 12:00 PM 1:15 PM<br />
Workshop: Resuscitation Academy<br />
Ann Doll<br />
Karavanen 9+10<br />
May 30, 12:00 PM 1:15 PM<br />
Optimal response for the individual patient<br />
Paul Gowens, FCPara. MSc. AASI.DipIMC,RCSEd.<br />
MCMI, Gavin Perkins, Stephen Sollid, Peter<br />
Kudenchuk, and Wolfgang Voelckel<br />
Harlekin & Columbine,<br />
May 30, 12:00 PM 1:15 PM<br />
Emergency Medical Dispatch – the gatekeeper<br />
to emergency care Maaret Castrén, Marcus Ong,<br />
Jerry Overton, Leif Svensson, and Paul Sutton<br />
Tivoli Congress Hall,<br />
May 30, 12:00 PM 1:15 PM<br />
Workshop: Pre hospital quality – Nordic<br />
Collaboration on EMS data collection, quality<br />
indicators and benchmarking<br />
Erika Frischknecht Christensen and Steinar Olsen<br />
Karavanen 6<br />
May 30, 12:00 PM 1:15 PM<br />
1:15 PM<br />
Lunch Exhibition Areas<br />
1:30 PM<br />
Poster Walks<br />
Foyer, lower floor<br />
May 30, 1:30 PM - 2:20 PM<br />
2:30 PM<br />
Best Emergency Medical Service<br />
practice<br />
Fionna Moore, Marcus Ong, Freddy<br />
Lippert, and Jerry Overton<br />
Carstensen<br />
May 30, 2:30 PM - 3:45 PM<br />
Workshop: Setting focus on<br />
situational awareness in emergency care<br />
Peter Dieckmann, Rhona Flin, Stephen<br />
Sollid, Torben Wisborg, Bodil Thorsager<br />
Svendsen, and Doris Østergaard<br />
Karavanen 9+10<br />
May 30, 2:30 PM - 3:45 PM<br />
Breakout session: To be announced<br />
Akvariet 4+5<br />
May 30, 2:30 PM - 3:45 PM<br />
Major Incidents<br />
Paul Sutton, Steven Bland, and David<br />
Zideman, LVO, QHP(C), BSc, MBBS,<br />
FRCA, FRCP, FIMC, FERC<br />
Tivoli Congress Hall<br />
May 30, 2:30 PM - 3:45 PM<br />
Workshop: Essential Emergency<br />
Ultrasonography workshop<br />
Morten Thingemann Bøtker<br />
Karavanen 6<br />
May 30, 2:30 PM - 3:45 PM<br />
The elderly patient in the emergency<br />
setting<br />
Roland Bingisser, Kate Cantwell, Simon<br />
Mooijaart, MD PhD, Lars S. Rasmussen,<br />
and Caroline L. Watkins<br />
Harlekin & Columbine<br />
May 30, 2:30 PM - 3:45 PM<br />
HEMS as part of EMS<br />
David Lockey, Hans Morten Lossius, HML,<br />
and Wolfgang Voelckel<br />
Pjerrot<br />
May 30, 2:30 PM - 3:45 PM<br />
3:45 PM<br />
Coffee Break<br />
Exhibition Areas<br />
May 30, 3:45 PM - 4:15 PM<br />
4:15 PM<br />
End of first day and Keynote speaker<br />
Lars S. Rasmussen, Pierre Carli, and Hjalte Aaberg<br />
Tivoli Congress Hall<br />
May 30, 4:15 PM - 5:15 PM<br />
6:30 PM<br />
Welcome Reception<br />
Copenhagen City Hall<br />
May 30, 6:30 PM - 8:00 PM<br />
Tuesday, May 31, 2016<br />
9:00 AM<br />
Keynote speaker: Global Resuscitation Alliance<br />
Freddy Lippert<br />
Tivoli Congress Hall<br />
May 31, 9:00 AM - 10:00 AM<br />
10:00 AM<br />
Coffee Break<br />
Exhibition Areas<br />
May 31, 10:00 AM - 10:30 AM<br />
10:30 AM<br />
Safety at scene and during transport<br />
Anne Kristine Bergem, Andy Newton,<br />
Stephen Sollid, Hans Morten Lossius,<br />
HML, and Paul Gowens, FCPara. MSc.<br />
AASI.DipIMC,RCSEd.MCMI<br />
Carstensen<br />
May 31, 10:30 AM - 11:45 AM<br />
Communication when time is critical<br />
Doris Østergaard, Martine C. De Bruijne,<br />
Michaela Kolbe, Andrew Lockey, and<br />
Peter Dieckmann<br />
Harlekin & Columbine<br />
May 31, 10:30 AM - 11:45 AM<br />
EMS and the infectious patient<br />
Erika Vlieghe, MD PhD, Erika<br />
Frischknecht Christensen, Philip D.<br />
Anderson, and Steven Bland<br />
Pjerrot<br />
May 31, 10:30 AM - 11:45 AM<br />
Workshop: Cardiac arrest and<br />
emergency medical dispatching –<br />
how do you monitor and improve<br />
Tonje Søraas Birkenes, Helge Myklebust,<br />
Thea Palsgaard Møller, and Søren<br />
Viereck<br />
Karavanen 9+10<br />
May 31, 10:30 AM - 11:45 AM<br />
Workshop: Ethics and Prehospital<br />
care – questions and dilemas<br />
Jana Seblova<br />
Karavanen 6<br />
May 31, 10:30 AM - 11:45 AM<br />
Industrysponsored<br />
symposium<br />
Lumbye<br />
May 31, 10:30 AM - 11:45 AM<br />
Cardiopulmonary resuscitation<br />
David Lockey, Koen Monsieurs, Leif<br />
Svensson, Maaret Castrén, and David<br />
Zideman, LVO, QHP(C), BSc, MBBS,<br />
FRCA, FRCP, FIMC, FERC<br />
Tivoli Congress Hall<br />
May 31, 10:30 AM - 11:45 AM<br />
Cardiopulmonary resuscitation<br />
David Lockey, Koen Monsieurs, Leif<br />
Svensson, Maaret Castrén, and David<br />
Zideman, LVO, QHP(C), BSc, MBBS,<br />
FRCA, FRCP, FIMC, FERC<br />
Tivoli Congress Hall<br />
May 31, 10:30 AM - 11:45 AM<br />
11:45 AM<br />
Lunch<br />
Exhibition Areas<br />
May 31, 11:45 AM - 1:15 PM<br />
12:00 PM<br />
Poster Walks<br />
Foyer, lower floor<br />
May 31, 12:00 PM - 12:50 PM<br />
1:15 PM<br />
New perspectives on education<br />
Phaedra Boinodiris, Andy Newton,<br />
Charlotte Ringsted, Doris Østergaard,<br />
and Andrew Lockey<br />
Harlekin & Columbine<br />
May 31, 1:15 PM - 2:30 PM<br />
Workshop: Get foam´ed<br />
Sandra Rosemarie Viggers<br />
Karavanen 6<br />
May 31, 1:15 PM - 2:30 PM<br />
Breakout session: The most<br />
important EMS articles 20152016<br />
Corey Slovis, M.D., Jacob Steinmetz,<br />
Koen Monsieurs, and Paul Gowens,<br />
FCPara. MSc. AASI.DipIMC,RCSEd.MCMI<br />
Akvariet 4+5<br />
May 31, 1:15 PM - 2:30 PM<br />
The critically ill child<br />
Anne Kristine Bergem, Joost Bierens, Ian<br />
Maconochie, Lars S. Rasmussen, and<br />
22 Spring 2016 | <strong>Ambulance</strong>today
Focus on Front-Line Mental Health<br />
Gavin Perkins<br />
Carstensen<br />
May 31, 1:15 PM - 2:30 PM<br />
Workshop: Technology in Telephone<br />
CPR – To measure and improve<br />
quality<br />
Helge Myklebust, Tonje Søraas Birkenes,<br />
Thea Palsgaard Møller, and Søren<br />
Viereck<br />
Karavanen 9+10<br />
May 31, 1:15 PM - 2:30 PM<br />
CEO and Medical directors’ session<br />
Jerry Overton<br />
Pjerrot<br />
May 31, 1:15 PM - 2:30 PM<br />
Inequality in health care<br />
Mads Gilbert, Dan Brun Petersen, and<br />
Torben Wisborg<br />
Lumbye<br />
May 31, 1:15 PM - 2:30 PM<br />
2:30 PM<br />
Coffee Break<br />
Exhibition Areas<br />
May 31, 2:30 PM - 3:00 PM<br />
3:00 PM<br />
End of second day and EMS Championship finals<br />
Doris Østergaard<br />
Tivoli Congress Hall<br />
May 31, 3:00 PM - 4:30 PM<br />
6:30 PM<br />
EMS2016 Gala Dinner<br />
The Circus Building<br />
May 31, 6:30 PM - 11:59 PM<br />
Wednesday, June 01, 2016<br />
9:00 AM<br />
Keynote: Resuscitation Academy Overview<br />
Tivoli Congress Hall<br />
Jun 01, 9:00 AM - 10:00 AM<br />
10:00 AM<br />
Coffee Break<br />
Exhibition Areas<br />
Jun 01, 10:00 AM - 10:30 AM<br />
Workshop: Controlling the surge Comparing<br />
European policies to<br />
manage increasing emergency care<br />
demand<br />
Thomas Krafft, Jerry Overton, Alexandra<br />
Ziemann, Janette Turner, and Freddy<br />
Lippert<br />
Karavanen 6<br />
Jun 01, 10:30 AM - 11:45 AM<br />
Quality and patient safety<br />
Paul Gowens, FCPara. MSc.<br />
AASI.DipIMC,RCSEd.MCMI, Steinar<br />
Olsen, Erika Frischknecht Christensen,<br />
Jana Seblova, and Beth Lilja<br />
Harlekin & Columbine<br />
Jun 01, 10:30 AM - 11:45 AM<br />
Critical cardiac diseases<br />
Hideharu Tanaka, Christian Terkelsen,<br />
Leif Svensson, and Koen Monsieurs<br />
Pjerrot<br />
Jun 01, 10:30 AM - 11:45 AM<br />
Workshop: Simulation Unplugged A<br />
mass casualty triage workshop<br />
Andreas Ravn, Theo Walther Jensen,<br />
Sandra Rosemarie Viggers, and Thomas<br />
Lynge Andersen<br />
Karavanen 9+10<br />
Jun 01, 10:30 AM - 11:45 AM<br />
The global challenge in acute illness<br />
and injury<br />
Tore Laerdal, Ramana Rao, Mads Gilbert,<br />
Ian Maconochie, and Philip D. Anderson<br />
Tivoli Congress Hall<br />
Jun 01, 10:30 AM - 11:45 AM<br />
Critical decision making<br />
Peter Dieckmann, Rhona Flin, Doris<br />
Østergaard, and Torben Wisborg<br />
Carstensen<br />
Jun 01, 10:30 AM - 11:45 AM<br />
Industry sponsored symposium<br />
Akvariet 4+5<br />
Jun 01, 10:30 AM - 11:45 AM<br />
11:45 AM<br />
Lunch<br />
Exhibition Areas<br />
Jun 01, 11:45 AM - 1:15 PM<br />
12:00 PM<br />
Poster Walks<br />
Foyer, lower floor<br />
Jun 01, 12:00 PM - 12:50 PM<br />
1:15 PM<br />
Closing Ceremony and Keynote<br />
Freddy Lippert, Fionna Moore, Marcus Ong, Jerry<br />
Overton<br />
Tivoli Congress Hall<br />
Jun 01, 1:15 PM - 3:00 PM<br />
Who takes care of people helping people?<br />
Steen Visholm, Professor at the Danish University in Roskilde, specializes in group psychology<br />
and organizational psychology. In addition to his role as professor, he is a member of the<br />
international organizations ISPSO and OPUS. He has written several books and articles on<br />
organizational psychology.<br />
Steen will be preparing a study gathering all previous research on mental health in the EMS<br />
business in order to find out how to organize and manage to obtain both good mental health<br />
and performance of tasks. Steen will be presenting a pre-conference workshop at Herlev<br />
Hospital on Sunday 29th May and a shorter workshop at EMS2016 on Wednesday 1st June.<br />
Frederik Madsen, Falck’s VP Group Human Relations and Corporate Culture, will appear as a<br />
consultant at the earlier event.<br />
When interviewed about his work, a<br />
paramedic in Falck once said: “A rescuer acts<br />
upon his instincts, trusting that he is making<br />
the right decision in a split second. The<br />
reflection and contemplation happens later.<br />
It happens at night when we get back home,<br />
perhaps even after a few days when we look<br />
back. Different thoughts run through our<br />
head: ‘Could I have done anything differently?<br />
Did I do enough?’”<br />
Behind a profession of meticulous work<br />
helping others lies a spectrum of emotions.<br />
EMS front-liners are exposed to incidents<br />
that can be psychologically challenging,<br />
and some rescue officers can experience<br />
negative long-term effects physically and<br />
mentally. They take care of patients, victims,<br />
relatives and sometimes even bystanders.<br />
But who takes care of them?<br />
A review of ten recent studies reveals<br />
that about 20% of paramedics and 17%<br />
of firefighters are at risk of developing<br />
accumulated stress and PTSD (Post<br />
Traumatic Stress Disorder) where the<br />
prevalence in the normal population is 2-3%.<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
During the EMS 2016 Conference in<br />
Copenhagen, Falck wants to deal with<br />
managing front-liners in pre-hospital<br />
organisations, especially focusing on how to<br />
ensure the right managerial competencies<br />
for handling emotional and psychological<br />
health. The results of a pilot study that<br />
covers both public and private providers<br />
in the Copenhagen area will be presented<br />
by Steen Visholm, Professor MSO at<br />
Roskilde University. Additionally, at the<br />
Copenhagen Academy for Medical Education<br />
and Simulation participants will have the<br />
opportunity to discuss and reflect upon<br />
emotions and reflections within emergency<br />
services. This will take place during a precourse<br />
on Sunday 29 May.<br />
The target group for these events are<br />
researchers, managers and front liners within<br />
the EMS business interested in learning<br />
more about working with psychological and<br />
emotional health and influencing future steps<br />
in broadening knowledge and processes<br />
within this area.<br />
“We want to gather interested parties from<br />
around the world to discuss setting up a<br />
society dedicated to developing knowledge<br />
about how to manage and organise EMS<br />
organisations, specifically in connection with<br />
emotional and psychological health, and we<br />
hope to see many interested participants,”<br />
says Frederik Madsen, Vice President of<br />
Group Human Relations at Falck. The project<br />
is sponsored by the Lundbeck Foundation.<br />
Steen Visholm will host the workshop,<br />
How to Take Care of People Helping<br />
People on Sunday 29th May from 13.00<br />
to 17.00 at CAMES, Herlev Hospital,<br />
Herlev Ringvej 75, 2730 Herlev.<br />
Winter 2014 | <strong>Ambulance</strong>today3 23
O&H Vehicle Conversions are one of<br />
the leading vehicle converters in the<br />
UK.<br />
Established for over 25 years, specialising in<br />
the conversion of Patient Transport Service<br />
(PTS) <strong>Ambulance</strong>s, A&E <strong>Ambulance</strong>s, NHS<br />
Training Vehicles, Paramedic Practitioners<br />
Vehicles, Wheelchair Access Vehicles (WAV’s)<br />
& Welfare Vehicles.<br />
O&H Vehicle Conversions<br />
Tel: 01405 769867<br />
Email: sales@ohvc.co.uk<br />
Web: www. ohvc.co.uk<br />
Larsen Road,<br />
Goole, East Yorkshire,<br />
DN14 6XG<br />
www. ohvc.co.uk
Focus on EMS2016 Social Programme<br />
Social<br />
networking<br />
at EMS2016<br />
Besides the scientific programme, participants at EMS2016 will be able to network and enjoy themselves<br />
in the extensive social programme.<br />
Welcome reception<br />
- Monday evening<br />
Danish and international circus troupes. Today<br />
the Circus Building is used for professional and<br />
social events.<br />
Included in the Gala event is a welcome<br />
drink, a three course dinner with wine and<br />
beverages, a spectacular show performed by<br />
professional artists as well as the EMS2016<br />
award show.<br />
After the end of the first day EMS2016<br />
invites all participants to the official welcome<br />
reception.<br />
The reception will take place in the centre<br />
of Copenhagen at the beautiful Copenhagen<br />
City Hall on Monday the 30th May from<br />
06.30 PM - 08:00 PM.<br />
Morning run<br />
- Tuesday morning<br />
On Tuesday morning participants will be able<br />
to sign up for a guided morning run together<br />
with their fellow congress delegates. At the<br />
run participants will be able to experience<br />
Copenhagen slowly waking up while they get<br />
moving before a long day at the conference<br />
center.<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Gala dinner<br />
- Tuesday evening<br />
On the second day of the EMS2016, a<br />
Gala dinner will be held for everybody to<br />
join. The Gala dinner will take place at the<br />
famous Circus Building, right in the middle<br />
of Copenhagen. The Circus Building is the<br />
oldest of its kind in Europe. It was inaugurated<br />
with an enormous public celebration in<br />
Copenhagen on 8 May 1886. Since then, the<br />
building has played host to a wide variety of<br />
Morning swim<br />
in the Copenhagen Harbor Bath<br />
- Wednesday morning<br />
In Copenhagen, citizens are fortunate that<br />
the water in the harbor is so clean that you<br />
can swim in it. Every summer there are three<br />
harbor baths where one can take a cool dip.<br />
At EMS2016 participants will be able to<br />
get a nice refreshing start to the day when<br />
all delegates are invited to a morning swim<br />
before the last day of the congress.<br />
More information about the social<br />
programme can be found at:<br />
http://ems2016.org/social-events/<br />
Winter 2014 | <strong>Ambulance</strong>today3 25
INTRODUCING<br />
TM<br />
D10<br />
The XSLATE D10 Tablet PC<br />
Impressive on the Inside, Supremely Rugged on the Outside<br />
Emergency response is about patient care, not mobile device care. Rely on the Xplore XSLATE D10 fully<br />
rugged tablet to save lives when time matters most. Driven by Android 5.1, Lollipop and powered by an<br />
Intel Atom CPU, this bigger, stronger, and more secure tablet delivers the critical patient data to make<br />
life saving decisions at the scene.<br />
Whether in the ambulance or on foot, the XPLORE XSLATE D10 can be trusted with every mission-critical<br />
EMS need:<br />
Real-time<br />
data transmission<br />
Faster response<br />
with GPS routing<br />
Detailed, coordinated communication<br />
with receiving hospital<br />
If you would like to experience the rugged power<br />
of Xplore’s mobile computing solutions, contact us today.<br />
www.Xploretech.com/ems | +44 (0) 1926 356 560
Focus on EMS2016 Championship<br />
EMS Championship - Who will be the best<br />
under pressure?<br />
During the EMS2016 Congress in Copenhagen you will we be able to challenge yourself and your team<br />
of EMS colleagues in the competition: European EMS Championship 2016. The Championship will be a<br />
fun, challenging and educational experience for emergency medical personnel. The competition will be all<br />
about team work, skills, experience and the ability to find a solution, when challenged.<br />
By Anne Lippert and Doris Østergaard, Copenhagen Academy for Medical Education and Simulation (CAMES)<br />
The European EMS Championship<br />
introduces competitors and audiences to<br />
new techniques and technology that can<br />
be used to manage patients and settings of<br />
different levels of urgency and complexity.<br />
The competition also enables participants<br />
to share their expertise, experience,<br />
techniques and technology with EMS<br />
colleagues from all over the world.<br />
The competition will consist of scenariobased<br />
events that test each team’s ability to<br />
manage patients in various circumstances<br />
with common critical medical conditions<br />
and trauma. The teams will compete in<br />
two rounds. The first round will identify the<br />
teams to compete in the final round on<br />
Tuesday afternoon at a spectacular plenum<br />
setting in the congress hall. All scenarios<br />
will be followed by feedback from the<br />
international panel of judges.<br />
The winning team will take home the<br />
honor, the EMS Championship trophy<br />
as well as free congress passes for the<br />
EMS2017.<br />
Who can join, and what does it take?<br />
A team must consist of three people with<br />
a healthcare background; the points given<br />
will be adjusted according to their level of<br />
education. In this way, it will be possible<br />
for a team consisting of three EMT’s to<br />
compete on an equal footing with a team<br />
consisting of advanced paramedics or<br />
emergency physicians. The teams will bring<br />
their own uniform and prehospital kit/<br />
bag, while all additional equipment will be<br />
provided by the organizers.<br />
The teams will be assessed according to<br />
their demonstrated technical skills as well<br />
as non-technical skills such as teamwork,<br />
communication, and leadership.<br />
How do I get my team signed up?<br />
You can now sign up for the EMS<br />
Championship at www.ems2016.org.<br />
The number of teams is, due to logistic<br />
challenges, limited to a total of 16.<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Participation will be offered on a first-come<br />
first-served basis, the spots are nearly fully<br />
booked, so do not hesitate to sign up for<br />
this exciting event.<br />
If you have questions or any problems<br />
registering you can always contact the<br />
congress secretariat on:<br />
ems2016@regionh.dk<br />
The European EMS Championship is<br />
organized by Copenhagen Academy for<br />
Medical Education and Simulation (CAMES)<br />
and EMS Copenhagen and is sponsored by<br />
Laerdal Medical and Falck Emergency as the<br />
main sponsors for EMS2016.<br />
Biography:<br />
Dr Anne Lippert<br />
Anne Lippert, MD, FERC,<br />
is Deputy Director of the<br />
Copenhagen Academy<br />
for Medical Education and<br />
Simulation (CAMES), a<br />
position, which she has held<br />
full-time for the last 8 years.<br />
She is trained as a specialist in anaesthesiology<br />
with subspecialty in Intensive Care Medicine.<br />
Anne has been involved with simulation training<br />
for more than 18 years and has been part of<br />
the development of the current largest institute<br />
for simulation in Denmark.<br />
Anne Lippert holds a Certificate in Health<br />
Professions Education from the University<br />
of Dundee (2010). Anne has worked with<br />
Rapid Response Systems for many years and<br />
has been the author of Guidelines for the<br />
introduction of RRS in Denmark as well as a<br />
member of the Regional board for RRS and is<br />
a member of the board in International Society<br />
for Rapid Response Systems and head of the<br />
meeting committee.<br />
Start getting your team together<br />
and join us for the 1st European<br />
Emergency Medical Services<br />
Congress to be held in Copenhagen<br />
30th May to 1st June 2016, where<br />
we together will shape the future<br />
for emergency medical services<br />
and pre-hospital emergency care.<br />
We all look forward to seeing you in<br />
Copenhagen!<br />
Biography:<br />
Doris Østergaard<br />
Doris Østergaard, is Professor<br />
in Medical Education and<br />
Simulation, and Head of the<br />
Regional Simulation Center,<br />
CAMES – Copenhagen<br />
Academy for Medical<br />
Education and Simulation, in<br />
the Capital Region of Denmark.<br />
Doris is an anesthesiologist with a special<br />
interest in education. Doris works full time<br />
with medical education and simulation based<br />
training. Doris has a Master’s in Medical<br />
Education and in the last 15 years her research<br />
activities have been related to the link between<br />
patient safety, simulation based training and<br />
emergency situations. She is supervising several<br />
Ph.D. projects within these fields. She is an<br />
Associate Editor for the European Journal of<br />
Anesthesiology.<br />
Doris is a member of the Educational Board of<br />
the Danish Society for Anesthesia and Intensive<br />
Care and is responsible for the national training<br />
program for specialist training in anesthesia.<br />
Winter 2014 | <strong>Ambulance</strong>today3 27
MobiMed Smart<br />
is in service in<br />
SWASFT and<br />
SCASFT<br />
Access to Summary Care<br />
Record in ambulances<br />
Smart<br />
Smarta<br />
triage<br />
vårdkedjor<br />
Smart<br />
Monitoring<br />
Smart<br />
Documentation<br />
For the first time paramedics are able to access SCR in ambulances<br />
MobiMed Smart gives paramedics at South Central <strong>Ambulance</strong> Service NHS<br />
Foundation Trust fast and secure electronic access to SCR, giving them essential<br />
clinical patient information at the scene. It is expected to give the clinicians an<br />
increased ability/effectiveness to make informed decisions and an increased<br />
efficiency in delivering appropriate care to patients.<br />
MobiMed Smart supports the needs of a modern 21st century ambulance service.<br />
We are ISO-certified:<br />
ISO 20000<br />
IT Service Management<br />
ISO 27001<br />
Information Security<br />
Management Systems<br />
ISO 13485<br />
Quality Management System<br />
for the Design and Manufacture<br />
of Medical Devices<br />
Features<br />
• Summary Care Record (SCR)<br />
• Smart-card login<br />
• Personal Demographics Service<br />
(PDS)<br />
• Monitoring with clinical background<br />
from cardiac critical care<br />
• Easy to configure and adapt to any<br />
clinical standard, such as JRCALC,<br />
Snomed, etc<br />
• Easy to integrate with CAD,<br />
Defibrillators, information systems<br />
at hospitals, etc<br />
Ortivus Ltd | Tel: 0844 8404 999 | E-mail: sales@ortivus.com | www.ortivus.com
Clinical Focus on the use of Penthrox in Pain Management<br />
21st Century First-on-Scene Pain Relief<br />
By Paul Cloves, Medicines Management Lead,<br />
South East Coast <strong>Ambulance</strong> Service NHS Foundation Trust<br />
The effective treatment of pain is a fundamental component of quality patient care, yet in the<br />
pre-hospital setting the management of pain is a complex mix of multiple resources, medicines<br />
and techniques, which are often vastly ineffective.<br />
Below Paul Cloves reports on SECAmb’s recent introduction of new analgesia Penthrox for their pain<br />
management formulary.<br />
During 2014/15, 6.5 million patients received<br />
treatment from ambulance personnel, of<br />
which 63% required transportation to an<br />
Emergency Department in England. 1<br />
We all understand that inadequately<br />
managed pain can have psychological,<br />
physiological and socioeconomic<br />
consequences that can worsen patient<br />
suffering, clinical outcome, and increase<br />
the financial costs of healthcare 2 but in a<br />
modern health service, where resources are<br />
at a premium, how do you ensure that the<br />
right treatment is available at the right time?<br />
Until recently, the ability to provide<br />
immediate analgesia was limited to<br />
morphine sulphate for injection, with<br />
this being the most reliable, fast-acting<br />
analgesic. However, if you add in the delays<br />
for cannulation, removing morphine from<br />
secure storage and administration time, the<br />
patient still has to wait at least 10 minutes to<br />
receive effective analgesia even if we ensure<br />
a paramedic arrives on scene first. So what<br />
happens when there is no paramedic? Or in<br />
the time you wait for a paramedic to arrive?<br />
In November 2015 South East Coast<br />
<strong>Ambulance</strong> Service NHS Foundation<br />
Trust (SECAmb) introduced Penthrox<br />
(methoxyflurane) into the Trust formulary<br />
aimed at enabling non-paramedics to<br />
provide analgesia prior to paramedic arrival<br />
as well as enabling paramedics to administer<br />
an immediate analgesia while they prepare<br />
the patient for cannulation.<br />
The initial review of our first administrations<br />
is making interesting reading! On average<br />
patients present with a patient score 8.7<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
out of 10, all patients were provided with<br />
Penthrox for the immediate treatment<br />
of their pain whilst further analgesia was<br />
prepared, after one minute of Penthrox the<br />
average pain score had dropped to 4.5 out<br />
of 10.<br />
Once a patient started using Penthrox,<br />
the majority were then able to receive a<br />
further 20 minutes of analgesia before the<br />
device ran out by which time the patient<br />
was able to receive additional longer acting<br />
analgesics. Figure 1 identifies which other<br />
analgesics were administered to patients<br />
either before or after administration of<br />
Penthrox. An important observation was<br />
that 20% of patients still required Entonox<br />
despite Penthrox; digging deeper into the<br />
patient care records, this 20% represents a<br />
group of patients who were cared for and<br />
transported by non-paramedic staff, where<br />
the Penthrox device had run out leaving<br />
Entonox as the only available analgesia for<br />
the remaining journey time. For the initial<br />
introduction, patients were limited to one<br />
dose of Penthrox in an episode of trauma.<br />
Figure 1. Use of other analgesics. During<br />
this study some patients received additional<br />
analgesia after administration of Penthrox. The<br />
diagram depicts the types of analgesics used<br />
and the frequency at which each analgesia<br />
was administered.<br />
What about side effects? Understanding<br />
that the current pre-hospital analgesics all<br />
have notable side effects we were expecting<br />
to see similar for Penthrox however there<br />
were relatively few side effects and certainly<br />
none that had any clinical impact.<br />
29 3
®<br />
IP X8<br />
AN 34 2.0 02/2015/A-E<br />
C-MAC ® – Pocket Monitor<br />
Mobility is our Passion …<br />
… and Highest Requirements of Hygiene our Standard!<br />
KARL STORZ GmbH & Co. KG, Mittelstraße 8, 78532 Tuttlingen/Germany, www.karlstorz.com
Clinical Focus on the use of Penthrox in Pain Management<br />
None<br />
Vomiting<br />
Dizzy Cough Bad Taste<br />
Figure 2. Side effect profile. This diagram<br />
depicts the frequency and type of side effects<br />
experienced by patients using Penthrox.<br />
Penthrox is new to the UK however it has<br />
been used in Australasia for over 30 years.<br />
It has been used extensively in the prehospital<br />
setting and is used by the Australian<br />
<strong>Ambulance</strong> Services, Australian Defence<br />
Forces, first-aid officers, ski fields, mines and<br />
more. In Australia it is more commonly<br />
known as the ‘green whistle’ due to its<br />
characteristic green colour and shape. It is a<br />
lightweight, hand-held inhaler which is selfadministered<br />
by the patient.<br />
The safety and efficacy of Penthrox has<br />
also been assessed in a randomised,<br />
multi-centre, double-blinded, placebocontrolled<br />
study conducted in the UK. 3<br />
This study was conducted across six sites in<br />
the UK and included 300 trauma patients<br />
in the Emergency Department (ED). It<br />
demonstrated the effectiveness and safety<br />
of Penthrox for the treatment of acute pain.<br />
A total of 303 patients were screened for<br />
the study; 149 patients received inhaled<br />
methoxyflurane and 149 patients received<br />
placebo. Patients were able to request<br />
rescue analgesia, if required. The primary<br />
endpoint was the change in pain intensity<br />
as measured using a visual analogue scale<br />
[VAS] from baseline to 5, 10, 15 and 20<br />
minutes after the start of study drug<br />
inhalation. Methoxyflurane reduced pain<br />
severity significantly more than placebo<br />
(p
Focus on Improving Cardiac Arrest Survival<br />
The Danish Fairytale: more than<br />
doubling survival in a decade<br />
By Fredrik Folke, Associate Professor, Emergency Medical Services,<br />
University of Copenhagen, Denmark;<br />
Christian Torp-Pedersen, Professor, Aalborg University, Denmark;<br />
Mads Wissenberg, MD, PhD, Emergency Medical Services,<br />
University of Copenhagen, Denmark;<br />
Freddy K. Lippert, Chief Executive Director, Emergency Medical Services,<br />
University of Copenhagen, Denmark<br />
Out-of-hospital cardiac arrest (OHCA) is a major health problem in the Western World - not only in<br />
Denmark with 3500 arrests every year - but also on a worldwide level with more than 700,000 arrests in<br />
the United States and Europe with often only 5-8 % survival rate. Since 2001, Denmark has succeeded<br />
in raising bystander CPR from 19% to 65%. In the same period, survival has increased from 4% to 12%.<br />
Tripling both bystander cardiopulmonary resuscitation (CPR) and survival from OHCA in just a decade is<br />
an extraordinary improvement, and it is the result of targeted action from many stakeholders in Danish<br />
society and a number of important initiatives.<br />
A goal was set<br />
The Danish Cardiac Arrest Register<br />
documented that in 2001 bystanders<br />
provided CPR in only 19% of OHCA cases;<br />
defibrillation before ambulance arrival was<br />
anecdotal and the 30-day survival rate was<br />
merely 4%. The common culture was only<br />
to perform CPR if you had attended a first<br />
aid course, and laymen did not know what<br />
an automated external defibrillator (AED)<br />
was. It was an untenable situation. To save<br />
more lives, help from laypeople was needed.<br />
An ambitious goal was set in 2003: to get<br />
bystanders to provide CPR in more than<br />
50% of cardiac arrests and improve cardiac<br />
arrest survival. These goals were to be<br />
achieved by several national initiatives to<br />
strengthen bystander resuscitation, public<br />
access defibrillation and advanced cardiac<br />
arrest care.<br />
Danish initiatives<br />
In 2005 resuscitation training became<br />
mandatory in Danish elementary schools<br />
and from 2006 CPR courses became<br />
mandatory when taking a driver’s license.<br />
Furthermore, approximately 150,000<br />
CPR self-instruction kits were distributed<br />
between 2005 and 2010 along with an<br />
increase in CPR course certificates from<br />
175,000 annually in 2001-2004 to 300,000<br />
annually 2008-2010.<br />
The Danish AED network<br />
In 2008, the non-commercial Danish<br />
Foundation TrygFonden founded the Danish<br />
AED network where all private and public<br />
owners of an AED can register their devices<br />
and everybody can see where the nearest<br />
AED is located (www.hjertestarter.dk).<br />
Also, the Danish Resuscitation Council, The<br />
National Board of Health and TrygFonden<br />
hosted the first national AED conference. At<br />
the conference The National Board of Health<br />
launched important recommendations<br />
to all owners of AEDs. Significant<br />
recommendations are to register the AEDs<br />
in the national AED network (Hjertestarter.<br />
dk) and to place AEDs outdoors so that<br />
they are accessible 24/7. To further support<br />
bystander defibrillation, TrygFonden launched<br />
a smart-phone app in 2010 with online<br />
information on all available AEDs from the<br />
AED network (hjertestarter.dk)<br />
Role of the emergency dispatch<br />
centre<br />
The Danish emergency medical dispatch<br />
centres were given access to the AED<br />
register in 2011, allowing the dispatchers<br />
to help bystanders to the nearest available<br />
AED. In addition, the Danish emergency<br />
dispatch centres were staffed by medically<br />
trained health care professionals the<br />
same year (instead of firefighters or police<br />
officers), offering telephone assisted CPR,<br />
which increased bystander CPR even further.<br />
Post cardiac arrest treatment<br />
Along with the pre-hospital initiatives of<br />
improving OHCA resuscitation, there has<br />
been an increased focus on the in-hospital<br />
effort to improve cardiac arrest care<br />
according to the newest guidelines, including<br />
introduction of therapeutic hypothermia and<br />
early revascularization.<br />
Research as a cornerstone<br />
Four emergency medicine professors<br />
have been appointed to enhance research<br />
within the pre-hospital field. Numerous<br />
PhD-students are conducting research and<br />
winning international awards – including 2 x<br />
ERC Young Investigator Award and an AHA<br />
Young Investigator Award. Their research<br />
has been published in recognized journals<br />
like Journal of American Medical Association<br />
(JAMA), Circulation, The Journal of the<br />
American Heart Association, Resuscitation,<br />
and the journal of the European<br />
Resuscitation Council.<br />
Funding for research<br />
A main contributor to the massive change in<br />
the Danish public’s perception about CPR is<br />
TrygFonden. Only 15 years ago, the first-aidculture<br />
was articulated as something very<br />
serious and the perception in the general<br />
public was that you should only perform<br />
CPR if you had attended a first aid course;<br />
laymen did not know what an AED was.<br />
Since 2004, TrygFonden has continuously<br />
pushed these messages to the Danes: “Just<br />
do it. It is better to do something than not<br />
to do anything,” and: “you can’t do any more<br />
harm to a person who is already dead, so<br />
do your best.”<br />
32 Spring 2016 | <strong>Ambulance</strong>today
Focus on Improving Cardiac Arrest Survival<br />
Source: M. Wissenberg et. al. in JAMA 2013, “Association of National Initiatives to Improve Cardiac Arrest<br />
Management With Rates of Bystander Intervention and Patient Survival After Out-of-Hospital Cardiac Arrest”<br />
http://jama.jamanetwork.com/article.aspx?articleid=1745678<br />
The Danish experience<br />
In 2011 the ambitious goal from 2003<br />
was reached. Bystanders provided CPR in<br />
58% of all OHCA incidents. This result was<br />
presented to the Danish Public through<br />
extensive media coverage at the first<br />
‘Restart a Heart Day’ in October 2012. In<br />
2013, bystander CPR further increased to<br />
65% and OHCA survival reached 12%.<br />
Furthermore, more than 13,000 publicly<br />
available AEDs across the nation - for a<br />
population of 5.7 million - were registered at<br />
the AED network at the beginning of 2016<br />
and defibrillation by lay-first-responders<br />
before EMS arrival reached more than 12%<br />
in public locations. It is also documented that<br />
75% of cardiac arrest survivors who were<br />
at work before their cardiac arrest returned<br />
back to work after successful resuscitation.<br />
The figure below shows the temporal<br />
increase of bystander CPR (green line),<br />
the 30-day survival rate (red bars) and the<br />
increase in defibrillation before EMS arrival<br />
(blue line) from 2001-2013 in Denmark.<br />
The ugly duckling turning into a<br />
beautiful swan<br />
The case of Denmark is a story about<br />
how far you can move societal behavior<br />
within a decade by combining a high level<br />
of research, by establishing nationwide<br />
systems including community programs, by<br />
motivating citizens through communication<br />
and by changing public policy through<br />
lobbying. Through all of these interventions,<br />
Denmark has tripled both bystander CPR<br />
and survival within a period of 12 years.<br />
New goals<br />
The new ambition for Denmark is to raise<br />
bystander CPR to 85%, to further improve<br />
defibrillation before EMS arrival and to<br />
improve 30-day OHCA survival to more<br />
than 15%.<br />
To achieve this, Denmark is hosting a<br />
prestigious Utstein meeting on cardiac arrest<br />
in May where a Global Resuscitation Alliance<br />
is to be established, aiming at increasing<br />
community cardiac arrest survival by an<br />
ambitious 50%. This meeting is followed<br />
by another new and prestigious event -<br />
the first international Emergency Medical<br />
Services congress in Europe. The Danish<br />
fairy tale, its results and experiences will be<br />
presented and discussed. TrygFonden and<br />
the Laerdal Foundation are key partners for<br />
the international Utstein meeting and for<br />
EMS2016.<br />
Source: Utstein paper on Global Resuscitation Alliance: www.resuscitationacademy.org/wp-content/<br />
uploads/2016/03/A-Call-to-Establish-a-Global-Resuscitation-Alliance1.pdf<br />
You can read more about EMS2016<br />
and about the Global Resuscitation<br />
Alliance in this edition of <strong>Ambulance</strong><br />
Today.<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
33 3
NEW<br />
Advancing Acute Pain Management<br />
At last, PENTHROX ® is here...<br />
Fast, effective pain management designed<br />
for fast, efficient patient management.<br />
PENTHROX is indicated for the emergency relief of moderate to severe pain in<br />
conscious adult patients with trauma and associated pain 1<br />
Now there’s a new PCA * in a lightweight, portable, handheld inhaler for emergency relief of moderate<br />
to severe pain in conscious adults with trauma. With minimal set-up and no need for cylinders, cannulas<br />
or mandatory opioid-related A&E attendances, PENTHROX offers you the potential to reduce<br />
dedicated treatment time and improve patient management.<br />
PENTHROX 3mL inhalation vapour, liquid: Please refer to the Summary of Product Characteristics (SPC) before<br />
prescribing. Abbreviated Prescribing Information. Presentation: Each vial of PENTHROX contains 3mL of methoxyflurane<br />
99.9%, a clear, almost colourless, volatile liquid, with a characteristic fruity odour. Each PENTHROX combination pack consists of<br />
one 3mL bottle, one PENTHROX Inhaler and one Activated Carbon (AC) chamber. Indications: Emergency relief of moderate to<br />
severe pain in conscious adult patients with trauma and associated pain. Dosage and administration: PENTHROX should be selfadministered<br />
under supervision of a person trained in its administration, using the hand held PENTHROX Inhaler. Adults: One<br />
bottle of 3mL PENTHROX to be vaporised in a PENTHROX Inhaler. On finishing the 3mL dose, another 3mL may be used. The dose<br />
should not exceed 6mL in a single administration. Methoxyflurane may cause renal failure if the recommended dose is exceeded.<br />
The lowest effective dosage to provide analgesia should be used. Onset of pain relief is rapid and occurs after 6-10 inhalations.<br />
Patients are able to titrate the amount of PENTHROX inhaled and should be instructed to inhale intermittently to achieve adequate<br />
analgesia. Continuous inhalation provides analgesic relief for up to 25-30 minutes; intermittent inhalation may provide longer<br />
analgesic relief. Administration on consecutive days is not recommended and the total dose to a patient in a week should not<br />
exceed 15mL. Children: PENTHROX should not be used in children under 18 years. For detailed information on the method of<br />
administration refer to the SPC. Contraindications: Use as an anaesthetic agent. Hypersensitivity to PENTHROX or any fluorinated<br />
anaesthetic. Patients with known or genetically susceptible to malignant hyperthermia or a history of severe adverse reactions in<br />
either patient or relatives. Patients who have a history of showing signs of liver damage after previous methoxyflurane use or<br />
halogenated hydrocarbon anaesthesia. Clinically significant renal impairment. Altered level of consciousness due to any cause<br />
including head injury, drugs or alcohol. Clinically evident cardiovascular instability. Clinically evident respiratory depression.<br />
Warnings and Precautions: Methoxyflurane causes significant nephrotoxicity at high doses. Nephrotoxicity is also related to the<br />
rate of metabolism. Factors that increase the rate of metabolism such as drugs that induce hepatic enzymes can increase the risk of<br />
toxicity with methoxyflurane as well as sub-groups of people with genetic variations that may result in fast metaboliser status. The<br />
lowest effective dose should be administered, especially in the elderly or patients with other known risk factors of renal disease.<br />
Methoxyflurane should be cautiously used in patients with conditions that would pre-dispose to renal injury. Methoxyflurane is<br />
metabolised in the liver, therefore increased exposures in patients with hepatic impairment can cause toxicity. PENTHROX should<br />
be used with care in patients with underlying hepatic conditions or with risks for hepatic dysfunction. Previous exposure to<br />
halogenated hydrocarbon anaesthetics (including methoxyflurane when used as an anaesthetic agent), especially if the interval is<br />
less than 3 months, may increase the potential for hepatic injury. Cautious clinical judgement should be exercised when PENTHROX<br />
is to be used more frequently than on one occasion every 3 months. Potential effects on blood pressure and heart rate are known<br />
class-effects of high-dose methoxyflurane used in anaesthesia and other anaesthetics. Caution required in elderly due to possible<br />
reduction in blood pressure. Potential CNS effects such as sedation, euphoria, amnesia, ability to concentrate, altered sensorimotor<br />
co-ordination and change in mood are known class-effects. The CNS effects can be a risk factor for potential abuse. To reduce<br />
occupational exposure to methoxyflurane, the PENTHROX Inhaler should always be used with the AC Chamber which adsorbs<br />
exhaled methoxyflurane. Multiple use of PENTHROX Inhaler without the AC Chamber creates additional risk. Elevation of liver<br />
enzymes, blood urea nitrogen and serum uric acid have been reported in exposed maternity ward staff when methoxyflurane was<br />
used in the past at the time of labour and delivery. PENTHROX is not appropriate for providing relief of break-through pain/<br />
exacerbations in chronic pain conditions or for the relief of trauma related pain in closely repeated episodes for the same patient.<br />
Interactions: Methoxyflurane is metabolised by the CYP 450 enzymes, particularly CYP 2E1 and to some extent CYP 2A6. It is<br />
possible that enzyme inducers (such as alcohol or isoniazid for CYP 2E1 and phenobarbital or rifampicin for CYP 2A6) which increase<br />
the rate of methoxyflurane metabolism might increase its potential toxicity and they should be avoided concomitantly with<br />
methoxyflurane. Concomitant use of PENTHROX with CNS depressants, such as opioids, sedatives or hypnotics, general<br />
anaesthetics, phenothiazines, tranquillisers, skeletal muscle relaxants, sedating antihistamines and alcohol may produce additive<br />
depressant effects. If opioids are given concomitantly with PENTHROX, the patient should be observed closely. Concomitant use<br />
of methoxyflurane with medicines (eg contrast agents and some antibiotics) which are known to have a nephrotoxic effect should<br />
be avoided as there may be an additive effect on nephrotoxicity; tetracycline, gentamicin, colistin, polymyxin B and amphotericin<br />
B have known nephrotoxic potential. Sevoflurane anaesthesia should be avoided following methoxyflurane analgesia, as<br />
sevoflurane increases serum fluoride levels and methoxyflurane nephrotoxicity is associated with raised serum fluoride. When<br />
methoxyflurane was used for anaesthesia at the higher doses of 40–60mL, there were reports of drug interaction with hepatic<br />
enzyme inducers (eg barbiturates) increasing metabolism of methoxyflurane and resulting in a few reported cases of nephrotoxicity;<br />
reduction of renal blood flow and hence anticipated enhanced renal effect when used in combination with drugs (eg barbiturates)<br />
reducing cardiac output; and class effect on cardiac depression, which may be enhanced by other cardiac depressant drugs, eg<br />
intravenous practolol during cardiac surgery. Fertility, pregnancy and lactation: No clinical data on effects of methoxyflurane on<br />
fertility are available. As with all medicines care should be exercised when administered during pregnancy especially the first<br />
trimester. There is insufficient information on the excretion of methoxyflurane in human milk. Caution should be exercised when<br />
methoxyflurane is administered to a nursing mother. Effects on ability to drive and use machines: Methoxyflurane may have a<br />
minor influence on the ability to drive and use machines. Patients should be advised not to drive or operate machinery if they are<br />
feeling drowsy or dizzy. Undesirable effects: The most common non-serious reactions are CNS type reactions such as dizziness and<br />
somnolence (≥1/100 to
Focus on Scottish <strong>Ambulance</strong> Service<br />
Out of Hospital Cardiac Arrest –<br />
Scotland’s Story<br />
“Out-of-Hospital Cardiac Arrest: A Strategy for Scotland” was launched by the Minister for Public Health<br />
at the Scottish Cardiac Arrest Symposium on 27 March 2015. The strategy was produced by a broad<br />
coalition of stakeholders and sets out a commitment to improve outcomes after out-of-hospital cardiac<br />
arrest and an ambition that by 2020 Scotland will be an international leader in the management of<br />
OHCA.<br />
The strategy aims to increase survival rates<br />
after OHCA by 10% across the country<br />
within five years. Reaching this level of<br />
performance would mean around 300<br />
more lives being saved every year resulting<br />
in a total of 1,000 additional lives saved by<br />
2020. Increasing the incidence of bystander<br />
CPR is the cornerstone of improving<br />
outcomes because it can increase the<br />
likelihood of survival after OHCA by 2 or<br />
3 times. The strategy included the goal of<br />
equipping an additional 500,000 people<br />
with CPR skills by 2020.<br />
Across Scotland around 3,500 patients<br />
undergo attempted resuscitation each<br />
year after OHCA making it a significant<br />
healthcare challenge. European centres<br />
with the best survival rates return almost<br />
a quarter of OHCA victims home alive<br />
but in Scotland in 2013/14 around 1 in<br />
20 survived to hospital discharge with<br />
considerable variation in different parts of<br />
the country.<br />
In many centres around the world, including<br />
Scotland, initiatives to improve OHCA<br />
outcomes have been implemented at city<br />
level with dramatic results. Our challenge<br />
was to put in place the world’s first national<br />
programme. The key was nationwide multisector<br />
engagement including Emergency<br />
Services (Scottish <strong>Ambulance</strong> Service,<br />
Scottish Fire and Rescue and Police<br />
Scotland), key third sector organisations<br />
(including British Heart Foundation, Chest<br />
Heart and Stroke Scotland, St Andrews<br />
<strong>Ambulance</strong>, British Red Cross), and<br />
academic partners (The Resuscitation<br />
Research Group at the University of<br />
Edinburgh) and many others. We brought<br />
together both policy-makers and those at<br />
the cutting edge of operational delivery to<br />
make a difference to both delivery of care<br />
and patient outcomes.<br />
Edinburgh University’s Resuscitation<br />
Research Group helped us adapt the best<br />
evidence and inform decision-making to<br />
finalise the strategic aims. We learnt from<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
patients, academics, healthcare workers,<br />
public services, and the third sector and<br />
built on good practice from around the<br />
world. A patient story film provides vivid<br />
evidence of the impact of increasing<br />
survival rate on patients and families.<br />
One patient’s story:<br />
“It’s Not Just A Theory“<br />
https://vimeo.com/123213458<br />
A steering group with senior decision<br />
makers from a broad range of partner<br />
Biography:<br />
Paul Gowens, FCPara, MSc. PGCert.<br />
DipIMC, RCSEd. AASI. MCMI<br />
Scottish <strong>Ambulance</strong> Service<br />
Paul is a Health Foundation<br />
Fellow and currently<br />
undertaking a secondment<br />
to the Scottish Government,<br />
Health and Social Care<br />
Directorate as a national<br />
clinical advisor with portfolio<br />
including, out of hospital cardiac arrest and<br />
major trauma systems. With over twentyfive<br />
years of experience within the Scottish<br />
<strong>Ambulance</strong> Service Paul has fulfilled a number<br />
of key roles from a HEMS paramedic through<br />
to his current strategic role at Scottish<br />
Government.<br />
Biography:<br />
Karen McNee, Policy Analyst, Planning<br />
and Quality Division,<br />
Scottish Government<br />
Karen is a senior policy<br />
analyst working on health<br />
and innovation in the<br />
Strategic Planning and<br />
Clinical Priorities team within<br />
Scottish Government Health<br />
Directorates where she has<br />
been since 2013.<br />
Karen began her career in the Scottish<br />
Government in the late 1980s and has<br />
worked in a number of Departments as a<br />
social researcher. She has spent the last 9<br />
years working in Scottish Government Health<br />
Directorates; 7 years as head of the Public<br />
Health and Sport Team within Health Analytical<br />
Services Division before moving to her current<br />
policy post. She is policy lead for Out of<br />
Hospital Cardiac Arrest.<br />
organisations supported the team and<br />
enabled the input of key stakeholders as<br />
the strategy developed.<br />
At the launch of the strategy the team<br />
actively used social media to publicise the<br />
event, generating 5,000 tweets and creating<br />
3 million impressions. Scotland’s strategy for<br />
Biography:<br />
Lisa MacInnes, BSc (Hons), MSc,<br />
RGN, AFHEA<br />
Save a Life for Scotland<br />
Lisa is a nurse and member<br />
of the Resuscitation Research<br />
Group in Edinburgh She<br />
has a passion for research,<br />
education and training<br />
previously holding a teaching<br />
fellow role within medical<br />
education before joining RRG to lead on a<br />
CHSS project (live video streaming to augment<br />
decision making in COPD and OHCA). She is<br />
the National Programme Manager for Save a<br />
Life for Scotland.<br />
Biography:<br />
Dr Gareth Clegg,<br />
Resuscitation Research Group<br />
Gareth Clegg trained in<br />
Emergency Medicine in<br />
Edinburgh having completed<br />
undergraduate degrees in<br />
Medicine and Psychology. He<br />
started research work early<br />
in the course of EM training -<br />
initially looking with Professor Colin Robertson<br />
at whether the ventricular fibrillation ECG<br />
waveform could be used to guide real time<br />
resuscitation of patients in cardiac arrest.<br />
Gareth is co-founder of the Emergency<br />
Medicine Research Group in Edinburgh<br />
(EMERGE) and leads the Resuscitation<br />
Research Group, a collaborative involving<br />
Edinburgh University, the Scottish <strong>Ambulance</strong><br />
Service and NHS Lothian. Research interests<br />
include the physiology and clinical management<br />
of out-of-hospital cardiac arrest, non-technical<br />
skills in time critical resuscitation, and the<br />
physiology of fluid resuscitation. The group<br />
coordinates the TOPCAT2 project and 3RU<br />
team along with a range of other projects<br />
relating to all elements of the OHCA response<br />
‘system’ summarised in the Chain of Survival.<br />
Winter 2014 | <strong>Ambulance</strong>today3 35
Do I need to worry<br />
about respiratory failure?<br />
You’re dispatched to a 10-year-old girl having difficulty<br />
breathing. She looks terrified, audibly wheezes, and speaks in<br />
one-word sentences.<br />
This kind of patient can be very challenging to care for, and often you are presented with<br />
several reasonable diagnoses. How can you take this guesswork out of decision making?<br />
Strong assessment skills and the right technology can make all the difference in accurately<br />
diagnosing and treating the patient. The ZOLL X Series ® , with its advanced tools for CO 2<br />
and SpO 2<br />
monitoring, provides early indication of respiratory compromise, feedback on<br />
the patient’s oxygenation and ventilation status, and their responsiveness to treatments.<br />
Insight for informed decisions.<br />
www.zoll.com/uk/respiratory-care<br />
©2016 ZOLL Medical Corporation, Chelmsford, MA, USA. X Series and ZOLL are trademarks or registered trademarks of ZOLL Medical Corporation in the United States and/or other countries.<br />
MCN IP 1603 0113
Focus on Scottish <strong>Ambulance</strong> Service<br />
OHCA can be downloaded here:<br />
www.gov.scot/scottishohcastrategy<br />
There are seven key strands of work<br />
outlined in the strategy which are now<br />
being progressed: early recognition, CPR,<br />
defibrillation, pre-hospital advanced<br />
life support, post resuscitation care,<br />
rehabilitation and aftercare, culture and<br />
context. We have developed a delivery<br />
plan that sets out intermediate outcomes<br />
and related indicators to allow us to<br />
monitor and drive forward progress against<br />
these priority areas.<br />
Early results are encouraging. <strong>Ambulance</strong><br />
Control Centres across the country are<br />
prioritising cardiac arrest: the cardiac arrest<br />
8 minute response is 5% higher and triple<br />
responding is up by 15%. Overall the<br />
percentage of patients in cardiac arrest with<br />
a shockable rhythm arriving at hospital<br />
with a pulse has increased from 34% to<br />
40%.<br />
Save a Life for Scotland (SALFS)<br />
Save a Life for Scotland is the public facing<br />
strand of the OHCA strategy aimed at<br />
increasing public awareness of OHCA and<br />
encouraging people to learn CPR. It was<br />
launched at an event on Princes Street<br />
in central Edinburgh on 16th October<br />
2015, by Gregor Newton, a cardiac arrest<br />
survivor on behalf of the Resuscitation<br />
Research Group. The event was also<br />
attended by Maureen Watt, Minister<br />
of Public Health and over 20 partner<br />
organisations and industry sponsors.<br />
“This multi agency approach is great, it’s a<br />
huge marquee, All these organisations are<br />
here and the general public are coming to<br />
learn and it’s great to see this happening.”<br />
—Maureen Watt MSP<br />
The launch event was a great success<br />
with over 1400 people learning the basic<br />
skills of CPR in Edinburgh alone. Members<br />
of the public were invited into the tent<br />
to meet with volunteer CPR trainers<br />
from a wide variety of organisations and<br />
backgrounds. They received a basic ‘hands<br />
on’ introduction to CPR using Mini-Anne<br />
manikins.<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Participants were invited to signal a<br />
commitment to undertaking training in<br />
CPR and their willingness to perform<br />
basic life support should the need arise.<br />
In the SALFS photo suite many had their<br />
photograph taken and signed their name,<br />
or simply ‘I’ll do it’ across the print as<br />
their pledge. These photographs made an<br />
impressive photo wall and record of the<br />
day. Many were tweeted and are visible at<br />
the SALFS website www.savealife.scot<br />
Small cards with SALFS website information<br />
were handed to many on the streets and<br />
those who entered the marquee. Since<br />
the event we have been contacted by<br />
many organisations and individuals around<br />
Scotland requesting further information<br />
about the availability of CPR training.<br />
Launching Save a Life for Scotland<br />
around the country<br />
In addition to the Edinburgh event, over 70<br />
Fire Stations across Scotland opened their<br />
doors to the public and provided ‘hands-on’<br />
CPR training to local communities. Scottish<br />
<strong>Ambulance</strong> Service held events at National<br />
HQ, the Scottish Borders, West Lothian and<br />
Glasgow Centre. Glasgow Science Centre<br />
while Glasgow Dental School provided<br />
training in the Glasgow Science Centre.<br />
Heartstart, BASICS and Community<br />
First Responder groups provided events<br />
in Aberdeen, Neilston, Orkney, Falkirk,<br />
Dalbeattie, Bathgate, Lanarkshire and Perth.<br />
Video footage from the day can viewed at<br />
the following link: www.rrg-edinburgh.<br />
com/rrg-coordinates-save-a-life-forscotland/<br />
Plans are being developed for a<br />
similarly ambitious event in 2016.<br />
Triple Responding (3RU)<br />
The Scottish <strong>Ambulance</strong> Service is central<br />
to the delivery of high quality pre-hospital<br />
care and to improving OHCA performance<br />
and outcomes. One of the important areas<br />
they are supporting is the roll out of 3RU<br />
in urban communities across Scotland.<br />
In 2007, the Resuscitation Research Group<br />
(RRG) at the University of Edinburgh<br />
identified the need to improve the chain-ofsurvival<br />
for OHCA patients in south-east<br />
Scotland, where the national Heartstart<br />
Scotland database showed local survival to<br />
discharge rate at the time was less than 1%.<br />
The group identified the requirement to<br />
improve all elements of the local chain of<br />
survival in order to save lives. Following on<br />
from the initial TOPCAT study on OHCA,<br />
the team identified a unique opportunity<br />
to dramatically improve the quality of<br />
prehospital resuscitation practice, through<br />
defibrillator downloads, resuscitation<br />
feedback to EMS crews, simulation<br />
training and supporting resuscitation team<br />
leadership.<br />
In collaboration with the Scottish<br />
<strong>Ambulance</strong> Service, RRG set up the unique<br />
Resuscitation Rapid Response Unit (3RU).<br />
The response unit sends a specially trained<br />
3RU paramedic as a second-tier resource<br />
to lead OHCA resuscitation on-scene.<br />
The 3RU support-team consists of two<br />
doctors, 13 paramedics, a resuscitation<br />
officer, a research nurse and several medical<br />
students. The team volunteers to meet<br />
on a bi-monthly basis in their own time<br />
to maintain a high level of enthusiasm.<br />
The team was the first in the UK to<br />
pioneer a unique system of defibrillator<br />
data download and resuscitation feedback.<br />
Following every cardiac arrest, detailed<br />
resuscitation quality data is captured.<br />
The defibrillator data is analysed and<br />
fed back to the attending ambulance<br />
crew so performance can be continually<br />
improved. The team meets in the clinical<br />
simulation centre to undertake advanced<br />
Winter 2014 | <strong>Ambulance</strong>today3 37
SimMan ALS<br />
is designed to offer highly realistic training on the 10 vital first minutes of<br />
detection and stabilization of a rapidly deteriorating adult patient.<br />
@LaerdalEurope<br />
www.laerdal.com
Focus on Scottish <strong>Ambulance</strong> Service<br />
resuscitation skills training, which is open<br />
to any paramedic. This not only includes<br />
technical skills practice but all non-technical<br />
skills such as resuscitation team leadership,<br />
communication and decision-making. Video<br />
analysis is used to inform training and<br />
optimise team performance.<br />
The team communicate with regional<br />
ambulance control dispatch at the start<br />
of each shift to maintain awareness and<br />
utilisation of the 3RU resource for OHCA.<br />
The team is collaborating with Psychologists<br />
from Edinburgh University, analysing original<br />
999 calls in order to improve the uptake of<br />
telephone-assisted CPR.<br />
Having established a solid foundation in the<br />
‘basics’ of prehospital resuscitation, the 3RU<br />
team is now using a mechanical CPR device,<br />
intra-arrest ultrasound and prehospital<br />
video recording in order to provide the<br />
highest possible care and inform future<br />
development needs. The overall aim is to<br />
improve outcome from OHCA, directly<br />
saving lives.<br />
The introduction of 3RU has made a<br />
significant contribution to the improvement<br />
in the number of patients now surviving<br />
out-of-hospital cardiac arrest in Edinburgh.<br />
In 2007, the overall survival to discharge<br />
rate from OHCA in south-east Scotland<br />
was 0.7% and it is now consistently<br />
over 17%. In 2013, 24% of all OHCA in<br />
Edinburgh were discharged neurologically<br />
intact from hospital. This extraordinary<br />
improvement in survival rate translates into<br />
scores of patients, who would otherwise<br />
have died, returning home to their families.<br />
Survival from OHCA in Edinburgh is now<br />
consistently the highest in the country and<br />
amongst the highest in the UK.<br />
The Scottish <strong>Ambulance</strong> Service is now<br />
rolling out the 3RU programme across the<br />
country and if the success can be replicated,<br />
this will be an important contribution to<br />
achieving the target of saving over 300<br />
additional lives per year.<br />
There has also been interest in extending<br />
the 3RU model from further afield.<br />
<strong>Ambulance</strong> services from Wales, East<br />
Midlands, the North East and the South-<br />
East coast have all visited Edinburgh, with<br />
many adopting their own resuscitation<br />
improvement programs based on the<br />
Edinburgh-model. The RRG and 3RU team<br />
have attracted attention internationally,<br />
winning a ‘best of the best’ research prize<br />
at the European Resuscitation Council<br />
meeting in Vienna, and Emergency Team of<br />
the year from the British Medical Journal.<br />
Co-reponding<br />
We are also carrying out a national trial<br />
for co-response to OHCA. The Scottish<br />
Fire and Rescue Service are working<br />
with the Scottish <strong>Ambulance</strong> Service in 7<br />
areas of the country where firefighters in<br />
community fire and rescue stations have<br />
received enhanced training in life-support.<br />
There has been a very positive response<br />
overall with around 70 call-outs in the first<br />
6 months and at least 2 known survivors<br />
to discharge directly related to the coresponder<br />
pilot.<br />
PAD mapping<br />
Enabling prompt access to defibrillators is<br />
a key strand of the OHCA strategy and<br />
the mapping of Public Access Defibrillators<br />
is being taken forward to ensure these<br />
are made available to the public. Work is<br />
ongoing to map defibrillators and ensure<br />
interoperability with existing CAD systems.<br />
Protecting <strong>Ambulance</strong> Personnel with<br />
Body Worn Cameras<br />
The VideoBadge from Edesix offers protection from threats and abusive behaviour,<br />
and has proven to be a valuable asset for facilitating training and operational debrief.<br />
Paired with Edesix’s VideoManager software, the VideoBadge captures video and<br />
audio footage when required, and stores the data securely for future training<br />
purposes, or as court-ready evidence.<br />
“VideoBadge has made it<br />
possible to evaluate new<br />
equipment while out in<br />
the field.”<br />
Resuscitation Research<br />
Group, Edinburgh<br />
Key Benefits:<br />
w Evidential quality video and<br />
audio recording<br />
w Secure encryption and data<br />
protection controls<br />
w 8 – 14 hr recording time<br />
w Full audit tracking from camera<br />
to courtroom<br />
Free Trial<br />
If you’d like more information on the<br />
Edesix range of Body Worn Cameras,<br />
or wish to sign up for a free trial,<br />
please contact us at:<br />
sales@edesix.com<br />
quoting “AMB2” or call us on<br />
w<br />
WiFi-streaming options<br />
available<br />
0131 510 0232<br />
<strong>Ambulance</strong>-Today-Advert.indd Spring 2016 | <strong>Ambulance</strong>today<br />
1 29/03/2016 17:19 39 3
Patient Specific Linens<br />
Made in the UK<br />
Supporting the Emergency Services - as used at the Joint Response exercise, Dartford, London<br />
multi-mover<br />
ambulance linen pack<br />
Orvecare, Malmo Road,<br />
Sutton Fields Hull, HU7 0YF, UK<br />
Tel: +44 (0)1482 625333<br />
Email: service@orvecare.com<br />
Web: www.orvecare.com
Focus on Evolutionary Change within St John New Zealand<br />
Refreshing Our Values to Benefit<br />
Our Patients and Our People<br />
By Peter Bradley, CBE, CEO of St. John, New Zealand.<br />
Peter Bradley, CBE is known globally across EMS as the author of the “Bradley Report,” the groundbreaking<br />
2005 strategic review of NHS ambulance services in England, Taking Healthcare to the Patient,<br />
which was the catalyst for a major transformation in UK ambulance services. After a highly-successful<br />
decade-plus tenure as CEO of London <strong>Ambulance</strong> Service (LAS), Peter returned to New Zealand in 2012<br />
to take on the challenging role of CEO of St John New Zealand at a time of organisational change and<br />
development. The last three years have seen improvements in clinical and operational service delivery at<br />
SJNZ but, as Peter explains below, the job isn’t finished and nobody at SJNZ, least of all himself, is resting<br />
on their laurels.<br />
It’s been an interesting transition, moving<br />
from CEO of the London <strong>Ambulance</strong><br />
Service to CEO of the main ambulance<br />
service in New Zealand (NZ) – St John. I<br />
have been back here three-and-a-half years<br />
having left NZ for London in 1996.<br />
St John is a worldwide organisation<br />
operating in many countries, but we are<br />
one of only three that run the frontline<br />
emergency ambulance service – the other<br />
two are both in Australia (Western Australia<br />
and Northern Territory).<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Our five year strategy – which we have<br />
called the ‘Bigger Picture’ (a version of<br />
which appeared in a recent edition of this<br />
magazine) has five ambitions over five years<br />
and these are shown below. Most of these<br />
would align well with other ambulance<br />
services, however our fifth – ‘Partner of<br />
Choice’ focuses on our partners and reflects<br />
the much wider role that St John plays<br />
beyond running an ambulance service.<br />
- Right care right time<br />
- Local pathways<br />
- Quality care<br />
- People prepared for change<br />
- Partner of choice<br />
In terms of our ambulance service, I will start<br />
by outlining what is similar to the UK: well<br />
clearly the types of patients we see are the<br />
same, although we do get more traumarelated<br />
calls. We have similar ambulances,<br />
uniforms, kit and clinical guidelines. We<br />
have five frontline ambulance roles, starting<br />
with First Responder, then Emergency<br />
Medical Assistant (EMA), Emergency<br />
Medical Technician, Paramedic and finally<br />
Intensive Care Paramedic (ICP). All but First<br />
Responder and EMA must have an Authority<br />
to Practice (ATP), undertake annual refresher<br />
training and be exposed to a specific number<br />
of patient contacts each year to maintain<br />
their ATP. Our Medical Director has overall<br />
responsibility for approving ATP and the<br />
Clinical Procedures and Guidelines.<br />
Paramedics are not a registered health<br />
profession in NZ, however it is likely that this<br />
will happen over the next 18 to 24 months.<br />
Biography:<br />
Peter Bradley, CBE,<br />
CEO of St. John, New Zealand<br />
Peter was a paramedic<br />
in Auckland in the early<br />
stages of his career, and<br />
became Regional Director of<br />
<strong>Ambulance</strong> Services for St<br />
John New Zealand’s Northern<br />
Region before taking time<br />
out in 1995 to complete an MBA at Otago<br />
University. In 1996 he joined LAS as Director<br />
of Operations, and served as Chief Executive<br />
of the LAS from 2000 until his return to New<br />
Zealand.<br />
During his time in the UK, Peter was also the<br />
Chairman of the Association of <strong>Ambulance</strong><br />
Chief Executives (AACE), and National<br />
Director of <strong>Ambulance</strong> Services for the<br />
Department of Health in England. He led the<br />
strategic review of NHS ambulance services in<br />
England, Taking Healthcare to the Patient, which<br />
was the catalyst for a major transformation in<br />
UK ambulance services.<br />
Winter 2014 | <strong>Ambulance</strong>today3 41
Focus on Evolutionary Change within St John New Zealand<br />
- Supporting our volunteers – we expect<br />
a lot from our volunteers and they provide<br />
fantastic support. But we can’ t take this for<br />
granted and we need to ensure they feel<br />
valued and supported.<br />
- The nature of our terrain means that<br />
we sometimes don’t have the level of<br />
communications that we would like.<br />
- Taking patients to the right place first time<br />
by both road and air remains a challenge at<br />
times and is something we are working to<br />
improve.<br />
All new Paramedics must have a Bachelor’s<br />
Degree in Paramedicine and all new ICPs<br />
must have a Post-Graduate Paramedic<br />
qualification.<br />
We operate out of three Clinical Control<br />
Centres across NZ, using MPDS as our<br />
triage software and a Tri-Tech CAD system.<br />
We have an old analogue radio network and<br />
have a number of other communications<br />
challenges linked to our geography.<br />
In terms of what is different? Unlike the<br />
NHS in the UK healthcare isn’t free at the<br />
point of delivery over here so, for example,<br />
you pay around 15 pounds to see your<br />
GP and if you call an ambulance and it’s<br />
a medically-related call, patients are billed<br />
around 40 pounds. We don’t enforce<br />
payment and around 30% of patients do<br />
not pay their bills. St John is funded to about<br />
70% by the Government and the remainder<br />
is paid for through a combination of the<br />
patient’s part-charge, fundraising, sponsorship<br />
and our commercial activities. There is<br />
much debate over here as to whether or<br />
not the ambulance service should be fully<br />
funded by the Government or whether the<br />
current arrangements should remain. My<br />
own view is that there is no reason why the<br />
current funding arrangements can’t remain<br />
in place, as long as the contribution from the<br />
Government keeps pace with the cost of<br />
running the service, and this is the subject of<br />
an official review as I write this.<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Looking at some benchmarking information<br />
recently, it appears that St John costs the<br />
Government around 15 pounds per head of<br />
population in NZ, in the UK it’s around 35<br />
pounds per head and in Australia it’s around<br />
45 pounds. The reasons why St John is so<br />
much cheaper is in large part due to three<br />
things: firstly, the funding model mentioned<br />
above relies on significant support from the<br />
public. Secondly, we have a large number<br />
of volunteer ambulance staff (over 3,000)<br />
who support the day-to-day running of<br />
the service. Finally, (and surprisingly to all<br />
who read this I am sure) we are currently<br />
unable to put two staff on all our emergency<br />
ambulances. Around 100 times a day we<br />
send an ambulance out single-crewed and<br />
although the recruitment of over 150 extra<br />
ambulance staff over the last two years has<br />
improved the situation, it remains a very<br />
real risk for our staff and patients. We are<br />
committed to fully eliminating single-crewing<br />
by 2018 and are currently in discussions with<br />
the Government as to how they can help us<br />
achieve this.<br />
In addition, although we do have response<br />
time targets they are not as stringent as the<br />
UK, i.e. reaching 50% of patients in 8 minutes,<br />
and we don’t have Call Connect so the<br />
whole performance management regime<br />
feels less onerous. This doesn’t seem to have<br />
had a detrimental impact on our cardiac<br />
arrest survival-to-discharge results as our last<br />
report indicated survival-to-discharge results<br />
of 15%. We also have some control over<br />
what calls fall into what category.<br />
Challenges?<br />
- Single-crewing of emergency ambulances<br />
is the biggest single challenge facing our<br />
service with around 10% (40,000 responses<br />
a year) single-crewed. This issue has been<br />
around forever and we have seen an<br />
improvement in recent years with the extra<br />
recruitment.<br />
- Getting the baseline funding of the service<br />
to a level that means we can sustain a good<br />
service.<br />
- Taking patients with a primary care need<br />
to somewhere other than ED when it either<br />
costs the patients to go somewhere else, or<br />
where no referral pathways exist<br />
- Educating the public around the roll out<br />
of the clinical hub when they expect an<br />
ambulance.<br />
What we do well:<br />
- Virtual call-taking - our 111 (999) calls<br />
can be answered in any one of three control<br />
rooms across NZ.<br />
- We recently rolled out a national spinal<br />
cord impairment policy which allows<br />
patients in such a situation to be transported<br />
directly to one of two specialist spinal units<br />
in NZ<br />
- Our cardiac arrest survival-to-discharge<br />
results compare well with many other<br />
services<br />
- St John has been NZ’s most trusted<br />
charity for the last two years and ambulance<br />
staff and volunteers enjoy a very high level of<br />
respect in the community<br />
- We have a 24/7 Clinical Desk that all<br />
ambulance staff (including volunteers) can<br />
access for advice and information and this<br />
receives great reviews<br />
- Electronic patient report form (ePRF)<br />
– we recently rolled this out across our<br />
almost 400 ambulances in New Zealand.<br />
This is a Valentia Technologies product and I<br />
am reliably told from our current CIO Barry<br />
Thurston (who many of you will have heard<br />
of) that this is the best ePRF set up he has<br />
ever seen. The game-changer over the next<br />
Winter 2014 | <strong>Ambulance</strong>today3 43
We’re right behind you!<br />
WWW.MSIS.CO.UK<br />
In addition to our existing comprehensive Private<br />
<strong>Ambulance</strong> scheme, Miles Smith has also become the sole<br />
supplier of ambulance motor insurance for AXA insurance.<br />
Miles Smith has direct and immediate access into Lloyd’s<br />
and the London Market.<br />
With additional benefits continually being sought and<br />
added, we believe that we can offer you a scheme that is<br />
hard to match.<br />
For more information, please contact<br />
Grant Irwin at Miles Smith on<br />
020 7977 4867<br />
girwin@milessmith.co.uk<br />
MILES SMITH INSURANCE SOLUTIONS LIMITED IS AN APPOINTED REPRESENTATIVE OF MILES SMITH LIMITED WHICH IS AUTHORISED AND REGULATED BY THE FINANCIAL CONDUCT AUTHORITY FCA NO. 311273
Focus on Evolutionary Change within St John New Zealand<br />
12 months is that we will have access to a<br />
summary health care record.<br />
In the future, we aim to:<br />
- Achieve a reduction of 100,000<br />
Emergency Department presentations over<br />
5 years.<br />
- Ensure double-crewing for every<br />
ambulance in NZ.<br />
- Roll out the national major trauma system<br />
and STEMI pathway.<br />
- Introduce a national Air Desk to improve<br />
dispatching of air ambulances across NZ.<br />
- Review the call prioritisation system<br />
(MPDS) and see what system works better<br />
for us.<br />
- Really leverage the benefits of ePRF -<br />
both in terms of clinical audit and research<br />
and the summary care record.<br />
- Introduce a new set of Clinical Quality<br />
indicators.<br />
- Roll out new single stretcher ambulances.<br />
- Look to introduce a national Community<br />
First Responder scheme – much like in the<br />
UK.<br />
- Improve the equity of our service<br />
provision.<br />
- Further diversify - we are a bi-cultural<br />
nation and we need to reflect this in how<br />
we deliver our services and to ensure we<br />
provide an equitable service across the<br />
country.<br />
The above is all good bread-and-butter stuff<br />
and central to this is having a healthy culture,<br />
where our paid staff and volunteers feel wellsupported.<br />
As part of this we have recently<br />
rolled out a new set of values:<br />
- We do the Right Thing - Whakaaro Tika<br />
- We stand Side by Side - Whakakoha<br />
- We Make it Better - Whakawerohia<br />
- We have Open Minds -<br />
Whakahangahanga<br />
- We are Straight Up – Whakapono<br />
- Upgrade our current version of CAD to Our refreshed values were developed<br />
achieve ACE accreditation for our Clinical following consultations with the whole<br />
Control Centres.<br />
organisation, and we have a whole<br />
- Roll out our electronic staff appraisal programme in place over a couple of<br />
<strong>Ambulance</strong>-today-winter system.<br />
2015-132x185-v2:Layout years to make 1 these 3/12/15 values 10:56 meaningful Page and 1<br />
influence how we act and behave to towards<br />
each other.<br />
Finally, despite some of the challenges we<br />
face, we are still in a unique position of<br />
influence in the health service in NZ and we<br />
know that over the next three to five years<br />
we need to use our position to the best<br />
effect for the benefit of our patients and our<br />
people.<br />
To find out more about St. John<br />
<strong>Ambulance</strong>, please visit their website<br />
at: www.stjohn.org.nz<br />
S M A R T E L E C T R I C S F O R S M A R T V E H I C L E S<br />
carnation<br />
designs<br />
a brand of Elektron Technology<br />
Making genisys even more affordable for RRV & PTS:<br />
NEW low-cost Compact control & siren<br />
packages now available!<br />
Call +44 (0)1924 411211 for more details!<br />
genisys Compact + genisys CAN module + High quality siren amp<br />
+ +<br />
Carnation Designs has been at the forefront of ambulance power management & control for<br />
twenty-years, with proven performance in the most demanding applications.<br />
www.carnationdesigns.com +44 (0)1924 411211 info@carnationdesigns.co.uk<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Winter 2014 | <strong>Ambulance</strong>today3 45
Clinical Focus on the use of ENTONOX in Pain Management<br />
Entonox – Making the<br />
most of the basics<br />
in pre-hospital pain<br />
management<br />
By Lucas Hawkes-Frost, Paramedic<br />
and Assistant Director of Operations<br />
London <strong>Ambulance</strong> Service<br />
Entonox: the dusty weather-worn barrel bag in the side cupboard of more or less every ambulance in<br />
the UK, has been a mainstay of pre-hospital pain management since the 1970s; a loyal friend to the<br />
<strong>Ambulance</strong> Service, there at the birth of the Paramedic profession and along for the ride ever since.<br />
Nitrous oxide, a remarkable substance,<br />
used in rocket fuel among other things, has<br />
long been identified as having analgesic and<br />
anaesthetic properties with use reported<br />
for the relief of pain during labour since<br />
the 1930s, delivered at a concentration of<br />
50% in air, which delivered a useful analgesic<br />
effect with few side effects.<br />
ENTONOX as we know it today, was<br />
developed in 1961 by Dr Mike Tunstall, then<br />
an Anaesthetics Registrar at the Portsmouth<br />
and Oxford United Hospitals, who wrote<br />
to BOC asking about the feasibility of mixing<br />
oxygen and nitrous oxide together under<br />
pressure in a single gas cylinder. BOC duly<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
provided him with grey 48 cu.ft (F-size)<br />
cylinders to continue his development<br />
of portable anaesthetic machines and<br />
ENTONOX was born.<br />
The story of ENTONOX, however,<br />
was very nearly a very short one; at<br />
Oxford, a physicist to the Nuffield Dept<br />
of Anaesthetics and an anaesthetist<br />
exploring this new mix, Drs Epstein and<br />
Cole, discovered that after cooling, the<br />
gas mixture separated and was not stable,<br />
even when re-warmed. ENTONOX was<br />
regarded as being unsafe and it was felt<br />
that it had no future, until Dr Tunstall took<br />
his new development to Aberdeen in 1962<br />
as a consultant. After much development<br />
and experimentation (with the assistance<br />
of Donald’s ice-cream factory), the safety<br />
of ENTONOX was demonstrated through<br />
MRC trials and introduced for pre-hospital<br />
use by unsupervised midwives in 1965.<br />
Since then, ENTONOX has become an<br />
indispensible tool in the formulary of<br />
clinicians working in and out of hospitals,<br />
being a fast-acting, convenient and safe<br />
analgesic ideally suited to managing pain in<br />
a wide range of clinical contexts including<br />
labour, emergency care, procedural<br />
pain, wound care and of course burns.<br />
ENTONOX is especially useful in managing<br />
pain in children without the need for<br />
vascular access or other invasive procedures.<br />
One study, spanning 40 children’s and<br />
general hospitals analysed for children who<br />
received nitrous oxide as a primary sedative.<br />
In total, 1634 nitrous oxide administrations<br />
were identified in the course of the<br />
study, most of which were performed by<br />
advanced nurse practitioners or physician<br />
assistants. The study concludes that while<br />
the likelihood of vomiting increased when<br />
opioids concomitantly, the prevalence of<br />
serious adverse events was very low in the<br />
course of nitrous oxide administration.<br />
Physiologically, the analgesic effect of<br />
ENTONOX and nitrous oxide are not<br />
understood, however the prevailing<br />
evidence suggests that the action is<br />
associated with interaction between<br />
endogenous opioid substances and<br />
noradrenergic systems. This theory has been<br />
developed through observation of a number<br />
of phenomena whereby animals with a<br />
significant morphine tolerance are given<br />
nitrous oxide, the analgesic effects of nitrous<br />
oxide are equally reduced as with opiates,<br />
suggesting similar actions. Indeed, it has<br />
further been observed that the inhibition<br />
or potentiation of specific endogenous<br />
opioid receptors has a similar inhibition or<br />
potentiation of the effects of nitrous oxide<br />
Biography:<br />
Lucas Hawkes-Frost<br />
Lucas Hawkes-Frost is a<br />
Paramedic and an Assistant<br />
Director of Operations for<br />
London <strong>Ambulance</strong> Service.<br />
Professionally, Lucas has<br />
a background in clinical<br />
operations, clinical education,<br />
quality and patient safety and in addition to<br />
working within the NHS, works with a number<br />
of regulatory agencies and academic bodies<br />
nationally. Lucas has a long standing clinical<br />
interest in pain assessment and management<br />
and has spoken and published around the<br />
subject for a number of years. As a passionate<br />
advocate for the Paramedic profession, Lucas is<br />
a champion for the development of specialist<br />
clinical practice and better collaboration<br />
between professionals and agencies providing<br />
urgent and emergency care.<br />
47 3
Clinical Focus on the use of ENTONOX in Pain Management<br />
administration. Despite these observed<br />
phenomena, it remains unclear how the<br />
administration of nitrous oxide causes the<br />
release of endogenous opioids.<br />
The analgesic effects of ENTONOX are<br />
rapid, observable and reported by users<br />
after only four to five breaths. Indeed, the<br />
duration of action is very short, making<br />
the drug ideal for short procedures and of<br />
course allowing a patient to self-manage<br />
the administration of their own pain relief.<br />
In practice, ENTONOX has very few side<br />
effects or contraindications to use and is<br />
easily administered.<br />
The role of the NHS ambulance service<br />
and indeed of the Paramedic profession<br />
is developing quickly within the context<br />
of the modern NHS. In addition to<br />
NHS staff, voluntary services and other<br />
providers of urgent and emergency care<br />
are developing clinicians and indeed the<br />
resources being used to care for patients.<br />
Pain remains among the most commonly<br />
reported symptoms for the ambulance<br />
service and while the technical skill and<br />
capability of clinicians increases as well as<br />
pharmacological options for managing pain,<br />
it is important to remember that basic<br />
interventions have the potential to make a<br />
significant positive impact on the onward<br />
management of many patients in pain.<br />
Assessment and scoring of pain is an<br />
incredibly important element of treating any<br />
pain presentation, whether acute, chronic or<br />
acute on chronic. Pain assessment and basic<br />
pharmacological and non pharmacological<br />
approaches to the management of pain<br />
are important as they help not only to<br />
calm and engage a patient in the process<br />
of further assessment, but help patients to<br />
better describe symptomologies, recognise<br />
previously undisclosed pain and to better<br />
inform the clinician in crafting a care plan<br />
which meets the needs of the individual<br />
pain sufferer. ENTONOX administration<br />
provides a great opportunity, in many cases,<br />
to begin the process of pain management<br />
quickly and efficiently without the need for<br />
ancillary equipment or invasive procedures.<br />
The analgesic effect of ENTONOX may in<br />
many cases be sufficient to settle a patient<br />
adequately to better describe the illness or<br />
injury and indeed allow an attending clinician<br />
to better develop a multi-modal pain<br />
management plan which better suits the<br />
pain presentation the patient is experiencing.<br />
A significant number of pain assessment<br />
strategies exist, for children (Wong-Baker<br />
scale, FLACC), adults (Pain analogue scale,<br />
pain thermometer) and indeed those with<br />
cognitive impairment (Abbey Pain score,<br />
DOLORPLUS) and choosing the best scale<br />
is imperative in supporting a patient in<br />
identifying the nature and severity of their<br />
pain as well as supporting the clinician in<br />
best managing it.<br />
Clinically, ENTONOX administration<br />
provides patients with a fast onset and<br />
highly effective analgesia without heavy<br />
sedation, has anxiolytic and euphoric<br />
effects and supports patient relaxation<br />
and better patient engagement, providing<br />
in many cases a better opportunity for<br />
quality patient assessment and patient<br />
history. Across available literature, patients<br />
report occasional adverse effects, including<br />
nausea and vomiting, dizziness, dry mouth<br />
(most likely due to the administration of<br />
dry gas), tinnitus and rarely more significant<br />
symptoms including numbness, dreams or<br />
drowsiness the incidence of such effects<br />
ranges in literature between 0 and around<br />
30%.<br />
The efficacy of ENTONOX as a pain<br />
relieving agent and indeed quantifying actual<br />
clinical effectiveness is an area with a relative<br />
paucity of evidence. Donen et al. (1982)<br />
reviewed the cases of 240 patients to whom<br />
ENTONOX had been administered. The<br />
population studied had all presented with<br />
traumatic injuries to the chest, abdomen<br />
or back and were reporting pain. Of those<br />
reviewed, over 90% of patients reported<br />
reduced pain, with few adverse effects<br />
described.<br />
Further, in 2007, Descamps et al concluded<br />
that the administration of ENTONOX to<br />
patients presenting with acute traumatic<br />
shoulder dislocations, irrespective of the<br />
administration of a further oral analgesic,<br />
correlated strongly with markedly reduced<br />
time spent within the Accident and<br />
Emergency department in contrast to those<br />
patients to whom intravenous morphine<br />
an intravenous benzodiazepine had been<br />
administered. Descamps concluded that<br />
the use of morphine and or midazolam<br />
48 Spring 2016 | <strong>Ambulance</strong>today
Clinical Focus on the use of ENTONOX in Pain Management<br />
was linked with dramatically increased<br />
department stays; 177 minutes for<br />
intravenous morphine and / or midazolam<br />
and 77 minutes for ENTONOX alone.<br />
The paper does not explore the relative<br />
efficacy of either option in terms of pain<br />
scoring, however does underscore the fast<br />
onset and fast resolution of effects of the<br />
administration of ENTONOX as well as<br />
the clinical utility when used for traumatic<br />
injuries.<br />
Traditionally, ENTONOX has been a drug<br />
used primarily in the management of<br />
patients suffering with pain of a traumatic<br />
nature or indeed children and labour,<br />
however increasingly, evidence supports the<br />
use of ENTONOX as an analgesic option<br />
for patients suffering a range of conditions<br />
including acute heart attack.<br />
Nitrous oxide has been observed as<br />
exerting relatively minor effects on<br />
cardiovascular function in patients diagnosed<br />
with coronary artery disease. Two papers,<br />
published by Thornton et al. and Wynne<br />
et al. concluded that the administration<br />
of the nitrous oxide had very little effect<br />
on the circulatory system. Further, Wynne<br />
postulated that the weak depressant effect<br />
exerted on myocardial tissue by nitrous<br />
oxide could provide benefit in terms of<br />
improving myocardial oxygenation. This,<br />
however has not been established as fact,<br />
though ENTONOX is a credible and<br />
clinically useful option for managing patients<br />
by non-registrant clinicians without recourse<br />
to opiates and in addition to routine<br />
interventions such as nitrates, etc.<br />
Pain assessment and management is a<br />
major element of the role of the ambulance<br />
service and indeed of all those involved<br />
with the provision of urgent and emergency<br />
care in the UK. ENTONOX remains a highly<br />
credible and extremely effective means of<br />
rapid pain relief with few side effects or<br />
contraindications for use and should remain<br />
a cornerstone option for the provision of<br />
multimodal pain management in patients<br />
presenting with a range of pain conditions.<br />
From rocket fuel to pain relief in child<br />
birth, nitrous oxide as ENTONOX will<br />
likely remain a familiar tool in the side<br />
compartment of ambulances, clinics,<br />
voluntary agencies and sports clubs up and<br />
down the country.<br />
Mobile climate control for<br />
healthcare professionals<br />
Simple to use, effective in performance and reliable in operation.<br />
The Eberspächer climate control system.<br />
A WORLD OF COMFORT<br />
www.eberspacher.com – 01425 480151<br />
Spring jn1001_185x132_mobile_healthcare_atoday.indd 2016 | <strong>Ambulance</strong>today 1 09/02/2016 11:40 49 3
Focus on Performance Optimization<br />
Split-Second Deployment<br />
Decision-Making!<br />
By Duncan Bänffer, General Manager Finance & Controlling<br />
and ICT at <strong>Ambulance</strong>Zorg Rotterdam-Rijnmond (AZRR)<br />
<strong>Ambulance</strong>Zorg Rotterdam-Rijnmond (AZRR) is one of the Netherlands’ busiest ambulance services.<br />
Serving a population in excess of 1.2 M it provides urgent and emergency medical cover to the hectic<br />
Port of Rotterdam area as well as to remote rural areas. General Manager of Finance, Controlling and<br />
ICT, Duncan Bänffer was given the challenge of further developing a project to improve the deployment<br />
of front-line ambulance crews while improving response times and increasing cost-efficiencies. The start<br />
of the project was years ago in a fact finding visit of the AZRR to see Optima Live and Optima Predict<br />
working in action. The ability of Optima Live and Predict to provide accurate split-second deployment<br />
information and their popularity among dispatchers made the decision on where to seek an IT-driven<br />
solution much easier. Read on to find out what happened next…<br />
Introduction to AZRR<br />
In the Rotterdam metro area<br />
“<strong>Ambulance</strong>Zorg Rotterdam-Rijnmond”<br />
(AZRR) provides Emergency Medical<br />
Transport and Planned Medical Transport.<br />
AZRR is a cooperative of two contractors,<br />
Veiligheidsregio Rotterdam-Rijnmond (VRR),<br />
a public organisation, and the Bios Group,<br />
a private company. In total nearly 400<br />
employees are 24/7 available for medical<br />
support for approximately 1.2 million<br />
population of the Rotterdam metro area,<br />
and the tens of thousands of workers in<br />
the Port of Rotterdam and surrounding<br />
industrial areas. South of Rotterdam there<br />
is a more rural area, which is also serviced<br />
and supported by AZRR with acute and<br />
planned medical care. In 2015, AZRR<br />
handled 107.380 deployments with 85<br />
ambulance vehicles. During day time around<br />
37 ambulances are on duty.<br />
The Rotterdam-Rijnmond Dispatch Center<br />
hosts the ambulance service, fire and police<br />
departments. During the day, AZRR has six<br />
medical dispatchers on duty. Three nurses<br />
act as call-takers, one dispatcher handles<br />
low-care ambulances and two dispatchers<br />
take care of the Emergency Medical Care<br />
ambulances.<br />
First Contact with Optima<br />
The first contact with Optima dates back<br />
to 2009, resulting in a visit to Houston to<br />
see Optima Predict and Optima Live in<br />
an actual, live situation. At that moment<br />
AZRR was looking for a system to support<br />
the dispatch room in deploying the most<br />
suitable ambulance, taking into account the<br />
optimal distribution of vehicles over the area<br />
for the next 20 minutes. The dispatchers<br />
experienced a very high workload, and we<br />
envisioned Optima to decrease that. The<br />
general idea was that in hectic moments,<br />
with many simultaneous deployments to be<br />
handled by the dispatch room, dispatchers<br />
were not able to cope fully with the<br />
workload. There was not enough time for<br />
the dispatchers to get hold of the new<br />
locations of the vehicles before selecting the<br />
most suitable ones and also making sure the<br />
vehicles were distributed optimally across<br />
the service area. The mix of rural and urban<br />
settings complicated optimal deployments of<br />
vehicles and was an extra hurdle to be taken<br />
in the process. This resulted in the general<br />
idea that the solution had to be an IT-driven<br />
one, instead of increasing the number of<br />
ambulances. The costs of Optima compared<br />
to the investment and operational expenses<br />
related to adding ambulances, makes Optima<br />
the better economical choice. Although<br />
there was a lot of enthusiasm for Optima in<br />
2009, many other operational issues meant<br />
that the decision to implement Optima was<br />
delayed until 2011.<br />
What is Optima?<br />
Book your place at EMS2016 now at: www.ems2016.org<br />
Optima provides software solutions<br />
drawing on operations research to analyse<br />
historic data and providing modelling<br />
to support a range of strategic and<br />
operational decisions. Optima provides two<br />
solutions: Optima Predict and Optima Live.<br />
Both solutions are made up of a number of<br />
modules.<br />
Optima is a planning software package that<br />
statistically and dynamically determines the<br />
optimal distribution of vehicles or posts over<br />
a region. The Optima solution consists of<br />
Biography:<br />
Duncan Bänffer<br />
Duncan Bänffer is the<br />
General Manager Finance<br />
& Controlling and ICT for<br />
<strong>Ambulance</strong>Zorg Rotterdam-<br />
Rijnmond (AZRR) in the<br />
Netherlands. He oversees<br />
all financial, accounting and<br />
IT efforts of this 24/7 operational ambulance<br />
service with 400 employees. He is also the<br />
overall project manager for the Optima<br />
implementation project at AZRR. He has<br />
worked for a number of smaller and larger<br />
companies after graduating in Business<br />
Economics at the Erasmus University in<br />
Rotterdam. Duncan’s specialty is leading<br />
transition processes, supported by his<br />
combined financial and logistical expertise.<br />
50 Spring 2016 | <strong>Ambulance</strong>today
Focus on Performance Optimization<br />
two main software modules: Optima Predict<br />
and Optima Live. Optima Live is made up of<br />
four submodules.<br />
Optima Predict<br />
Optima Predict is the more static version,<br />
which predicts the response time within an<br />
area, considering the number of vehicles and<br />
posts plus historical data of deployments.<br />
By changing the variables of vehicles and<br />
posts, one can create the optimal distribution<br />
of vehicles over the area. This optimal<br />
distribution can be summarised in a post<br />
plan top 20, indicating in which order the<br />
post should be populated with ambulances.<br />
The most critical location is placed at the<br />
top.<br />
Optima Live<br />
Optima Live is a real-time decision support<br />
solution that provides an operational picture<br />
of the live situation for the service area. It<br />
can also predict how this actual situation will<br />
evolve, considering the known deployment<br />
history for the region. The Optima software’s<br />
database contains preloaded historical data.<br />
Optima Live in AZRR has for main modules:<br />
Real Time View, Look Ahead, Deployment<br />
and Dispatch. Real Time View presents the<br />
current position of each vehicle. Colour<br />
coding depicts the ability to service the<br />
patient within 15 minutes (the Dutch<br />
standard). Look Ahead shows the coverage<br />
Optima Predict is an interactive strategic<br />
planning solution that gives users the<br />
ability to generate evidence for strategic<br />
and operational decisions, quantifying the<br />
impact of any changes in response time<br />
performance, vehicle utilisation and other<br />
key operational metrics. The model uses<br />
historic data to produce a highly accurate<br />
simulation model of the operation; a<br />
user can then make changes to the<br />
operation and evaluate the impact of these<br />
changes against the general performance<br />
requirement of being on time in 95 % of<br />
the acute deployments. For example, by<br />
changing the variables of vehicles and posts,<br />
one can create the optimal distribution<br />
of vehicles over the area. This optimal<br />
distribution can be summarised in a post<br />
plan top 20, indicating in which order the<br />
post should be populated with ambulances.<br />
The most critical location is placed at the<br />
top.<br />
as it will be 20 minutes from now and<br />
indicates where to expect new incidents,<br />
based on historical data. The third module,<br />
Deployment, combines Real Time View and<br />
Look Ahead and the post plans to propose<br />
deployments while maintaining an optimal<br />
distribution of the vehicles across the region.<br />
It indicates which posts lack resources,<br />
attracting the dispatcher’s attention using a<br />
red-coloured symbol, urging the dispatcher<br />
to assign a vehicle to this location (see<br />
picture below at the left side, underresourced<br />
locations in red). The Deployment<br />
module also suggests corrective actions to<br />
restore the desired situation, by displaying<br />
action arrows.<br />
The last module, Dispatch, proposes the<br />
deployment of a specific vehicle as most<br />
suitable to respond to an incident. This<br />
deployment proposal is generated very<br />
quickly, taking all constraints, including<br />
maintaining service area coverage and<br />
response time, into account. It can directly be<br />
used for deployment.<br />
Government Funding<br />
In the Netherlands, the ambulance budget<br />
is dictated by the government. For every<br />
region, there is one organisation with an<br />
exclusive licence for the ambulance service.<br />
In our region, AZRR has obtained the<br />
licence. The budget used to be primarily<br />
output-oriented but has evolved towards<br />
a lump sum budget based on locations and<br />
performance (95% of acute deployments<br />
within 15 minutes).<br />
The picture shows a screen shot of Optima Deployment. On the left-hand side is the real-time view, showing a<br />
location in red with insufficient resourcing of vehicles. On the right-hand side, Optima’s Look Ahead is shown. It<br />
presents the situation as anticipated 20 minutes into the future, with arrows indicating the required moves to<br />
reach that goal. In this example, ambulance 116 should be moved from the location “Haringvlietdam” to the<br />
location “Goedereede”.<br />
Book your place at EMS2016 now at: www.ems2016.org<br />
Working with Optima<br />
We started working with Optima Predict<br />
in 2012, to increase our understanding of<br />
what the optimal distribution of posts and<br />
vehicles across the service area would be. In<br />
our budgeting process, it is very important to<br />
be able to recalculate the budget as granted<br />
to us by the government. The government<br />
budget dictates how many costs we are<br />
allowed to make, based on the regionspecific<br />
indicators such as demographics and<br />
infrastructural complexity, keeping in mind<br />
that 95% of the acute deployments have<br />
to be coped with within 15 minutes (12<br />
minutes driving time plus 3 minutes response<br />
time).<br />
One output from Optima Predict is a Post<br />
Plan, summarising the optimal location of<br />
posts and vehicles; this plan indicates the<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Winter 2014 | <strong>Ambulance</strong>today3 51
IS NOW<br />
Intermedix delivers technology-enabled solutions for global health and emergency response. Our solutions<br />
support and connect health care providers and emergency preparedness & response personnel. We take<br />
pride in serving our clients with extensive industry expertise and exceptional technology to back it up.<br />
Optima Live<br />
Optima Predict<br />
Optima Live brings the power of operations<br />
research to making dispatch and deployment<br />
decisions. Keep dispatchers abreast of resource<br />
statuses and locations in real time and show<br />
them how the system will look in the near future<br />
with Look Ahead. Dispatch and deployment<br />
make use of Optima’s time of day and day of<br />
week sensitive rule framework to ensure that<br />
your business rules are followed.<br />
Optima Predict enables powerful and accurate<br />
analysis, modelling and simulation for an<br />
endless range of “what if…?” scenarios. Our<br />
highly accurate strategic modelling solution<br />
offers powerful capability to model operational<br />
changes that can improve clinical and<br />
operational performance, increase efficiency,<br />
and respond to external changes, such as<br />
increasing demand or hospital reconfiguration.<br />
Improve Performance<br />
Optima Live provides the communications<br />
center with deployment recommendations<br />
for the best coverage.<br />
Make Evidence-Based Decisions<br />
Optima Predict provides a platform for<br />
effective planning and simulation of<br />
resource requirements.<br />
Increase Efficiency<br />
Optima Live allows you to minimise unnecessary<br />
moves that are taxing on crews and wastes fuel.<br />
Model Multiple Scenarios<br />
Optima Predict enables users to build scenarios<br />
that make logistical and business sense.<br />
Improve Consistency<br />
Optima Live’s rule framework ensures<br />
that deployment and dispatch procedures<br />
are always followed.<br />
Improve Operational Performance<br />
Optima Predict allows you to save time,<br />
effort and resources when changing<br />
agency operations.<br />
Contact us today to learn more and schedule a demo!<br />
info@intermedix.com | +44 1189 036 602 | www.intermedix.co.uk
Focus on Performance Optimization<br />
priority in assigning vehicles to the posts.<br />
The Post Plan is also the basis for the<br />
calculations which are being made in Optima<br />
Deployment, indicating sufficient coverage<br />
with ambulances of the various locations.<br />
The locations which are not sufficiently<br />
populated are shown in red, continuously<br />
presenting the dispatchers a clear overview<br />
of the situation. Currently, the Deployment<br />
module is going live in the dispatch room<br />
after thorough testing.<br />
Introducing Optima Live and getting<br />
the commitment of the dispatchers in<br />
Rotterdam<br />
For AZRR, it was extremely important that<br />
the decision to deploy Optima was not<br />
only made top-down but together with the<br />
people in the dispatch room, who would be<br />
working with Optima on a daily basis. For<br />
that reason there was an additional visit to<br />
the Denver location in November of 2012,<br />
to show a selected group of dispatchers<br />
an actual live working Optima solution.<br />
As a result of this visit AZRR decided to<br />
implement the first modules of Optima, with<br />
an option for the Dispatch module. Not<br />
part of the solution in Denver, we added the<br />
Deployment module. With Deployment, it is<br />
very easy to see which possible deployments<br />
maintain an optimal distribution of vehicles<br />
over the service area. And, it gives the<br />
dispatchers the possibility to look “under<br />
the hood” of the Optima software and<br />
gain a better understanding of the process<br />
leading to Optima’s results. This gives the<br />
dispatchers more comfort and trust in the<br />
calculations Optima makes. Deployment<br />
makes its calculations solely based on the<br />
AZRR Post Plan and business rules as these<br />
were previously used by the dispatchers,<br />
providing the staff with a sense of<br />
recognition. Also, we decided to take more<br />
time going through the implementation<br />
stages to give the dispatchers enough time<br />
to understand the use and the impact of<br />
Optima Live. Certainly for Optima Live<br />
Dispatch, it is important that the dispatchers<br />
are comfortable with Optima’s deployment<br />
proposals. If they are not confident with the<br />
Optima recommendations, they will keep<br />
questioning these. With the approach taken,<br />
the commitment of the workforce to the<br />
Optima solution is strengthened.<br />
Added value of Optima<br />
The Dispatch module adds significant value<br />
to our total dispatch solution and helps<br />
the dispatchers in their job. Every day we<br />
analyse our over-due deployments, and<br />
our analysis shows that especially at times<br />
with many simultaneous deployments it is<br />
difficult for the dispatcher to create and<br />
value a new mental picture of the situation<br />
and assign the most suitable vehicle while<br />
considering the optimal distribution of<br />
the ambulances across the various areas.<br />
It is normal, and human nature, that when<br />
the dispatcher has to cope with too many<br />
deployments, he reverts to a basic mode of<br />
planning, and assign the vehicle nearest to<br />
the incident. But what the dispatcher cannot<br />
do is possible with Optima Live; it can<br />
recalculate in a split second, even under the<br />
pressure of a high workload of simultaneous<br />
deployment requests. Using the Optima Live<br />
recommendations, the dispatcher can comply<br />
with our Post Plan and at the same time<br />
understand what to expect, based on the<br />
historical of deployment patterns presented<br />
by the software. As a result, we reduced<br />
the workload of the dispatchers by helping<br />
them make excellent deployments in hectic<br />
situations, allowing them time to be more<br />
supportive towards ambulance crews.<br />
The solid implementation approach starts<br />
with making a coverage plan in Optima<br />
Predict. This plan is taken to the test in the<br />
real operational environment using Optima<br />
Live modules Deployment and Dispatch,<br />
where it is fine-tuned even further. The result<br />
is a truly optimal coverage plan. This is where<br />
Optima adds real value. After thorough<br />
testing AZRR obtained good results with<br />
the Optima Live Deployment module. The<br />
next step involved the implementation of<br />
Optima Live Deployment in the production<br />
environment. In May, we plan to start<br />
implementing Optima Live Dispatch. We aim<br />
to have all Optima modules operational at<br />
the end of the year. It is needless to say that<br />
we have high expectations of using Optima<br />
and we will gladly tell you more after we<br />
have finished implementing.<br />
I would like to thank Aad Romijn and<br />
especially Willem Grool who as previous<br />
project leaders helped me to get up to speed<br />
as project leaders for Optima Dispatch. Also<br />
I would like to thank the Optima project<br />
group, Henry Oudshoorn, Hans Bontekoe,<br />
Marjolein Westerdijk and Hans Kuiper for their<br />
tremendous effort.<br />
Duncan Bänffer, Project Leader Optima<br />
Dispatch, Rotterdam 1st of April.<br />
To find out more about how the<br />
Optima solutions can help improve<br />
operational performance and<br />
dispatch effectiveness call Intermedix<br />
on: +44 (0) 1189 036 602<br />
or visit the Intermedix website at:<br />
www.intermedix.co.uk<br />
Book your place at EMS2016 now at: www.ems2016.org<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Winter 2014 | <strong>Ambulance</strong>today3 53
Clinical Focus on Emergency Artificial Ventilation<br />
Problems associated with the use<br />
of self – reforming bags in emergency<br />
artificial ventilation<br />
By Dr David J Baker, M Phil DM FRCA FRSM<br />
Emeritus Consultant Anaesthesiologist<br />
SAMU de Paris<br />
Hôpital Necker – Enfants Malades, Paris<br />
Artificial ventilation of the lungs goes back to antiquity but the modern use of bag-valve-mask (BVM)<br />
ventilation dates from the 1950s with the development of the self-reforming bag and non-return valve<br />
by the Dutch anaesthetist Henning Ruben. Since then, BVM ventilation in emergency has been widelyaccepted<br />
by emergency medical services throughout the world. The device is generally regarded as being<br />
safe and effective. This view may be related to training experience in anaesthetic rooms on patients who<br />
were asleep, had muscle relaxation and normal lung and airway characteristics. However, the use of BVM<br />
in emergency has increasingly been shown to be associated with a number of potentially serious problems<br />
including hypo - and hyperventilation, a view supported by a number of published studies. Portable<br />
gas-powered ventilators, developed over the past 40 years have been shown to deliver more consistent<br />
and effective ventilation while freeing an emergency responder from the requirement of squeezing a bag.<br />
This paper reviews the published evidence concerning the use of BVM in emergency and discusses the<br />
need for better training and awareness of the associated problems.<br />
Introduction<br />
Artificial ventilation of the lungs has long<br />
been an established part of both basic and<br />
advanced life support 1,2 . Although positive<br />
pressure ventilation has only become an<br />
integral part of medical practice over the<br />
past 60 years its origins go back to antiquity.<br />
Interest developed during the 17th and 18th<br />
centuries with experiments on ventilating<br />
animals and humans using bellows devices.<br />
At that time the essential negative pressure<br />
nature of normal breathing was not entirely<br />
understood but ventilation of the lungs<br />
was recognised as being an essential in the<br />
resuscitation of drowned persons, and led<br />
to the formation of societies such as the<br />
Royal Humane Society in London and the<br />
Society for the Resuscitation of Drowned<br />
Persons in Amsterdam. Work continued<br />
on positive pressure ventilation and the<br />
protection of the airway through intubation<br />
during the 19th century 3 . At the beginning<br />
of the 20th century the first mechanical<br />
ventilator, the Drager pulmoflator appeared.<br />
At that time however mechanical ventilation<br />
concentrated on reproducing the<br />
physiological conditions of normal breathing<br />
by creating a negative pressure around the<br />
patient. This led to the development of the<br />
cabinet ventilator (or ‘iron lung’) which was<br />
widely used in hospital ventilation until the<br />
1950s.<br />
The requirement for mass ventilation<br />
in Copenhagen during the 1952 polio<br />
epidemic overwhelmed the supply<br />
of cabinet ventilators available. The<br />
anaesthetist Bjorn Ibsen had the idea of<br />
using anaesthetic circuits containing a Boyles<br />
bag to provide intermittent positive pressure<br />
ventilation 4 . The bag was kept inflated by<br />
a positive pressure of gas within the circuit<br />
and could be squeezed by hand to provide<br />
inflation. (Figure 1) Later the bag would<br />
be modified to become self-reforming so<br />
that it could be used independently of an<br />
anaesthetic machine.<br />
Figure 1: Bjorn Ibsen and the first manual<br />
resuscitation circuit<br />
The first bag ventilation circuits used a<br />
canister of soda lime to absorb the exhaled<br />
carbon dioxide. The incorporation of a<br />
non-return valve, invented by the Dutch<br />
anaesthetist Henning Ruben 5 led to<br />
the development of the modern self –<br />
reforming bag, the first example of which<br />
was the Ambu bag in the late 1950s.<br />
Biography:<br />
Dr David J Baker<br />
M Phil DM FRCA FRSM<br />
David Baker was born in London<br />
and studied medicine at St<br />
Bartholomew’s Hospital. After<br />
qualification he served as a<br />
medical officer in the Royal Navy<br />
for nearly 20 years specializing in<br />
anaesthesia. He served in surface<br />
vessels and in the hospital ship<br />
Uganda during the Falklands War in 1982. Later he<br />
worked for several years at the United Kingdom<br />
Chemical Defence Establishment, where he conducted<br />
research on the neurophysiology of organophosphate<br />
poisoning, leading to a doctorate in medicine in 1986.<br />
After leaving the navy in 1992, David moved to France<br />
where he worked for many years as a consultant<br />
in anaesthesia for the Paris emergency medical<br />
service (SAMU) at the Necker University Hospital,<br />
specializing in the management of mass toxic incidents.<br />
From 2004 he also worked as a consultant medical<br />
toxicologist for the Centre for Radiation, Chemical<br />
and Environmental Hazards of the United Kingdom<br />
Health Protection Agency.<br />
David Baker has been a visiting professor at the<br />
Universities of Harvard and Surabaya. He has<br />
lectured in over 40 countries around the world and<br />
is the author of numerous journal articles, textbook<br />
chapters and monographs ,including the recently –<br />
published ‘Toxic Trauma: a Basic Clinical Guide. He<br />
was a Board Member of the World Association<br />
for Disaster and Emergency Medicine and has<br />
consulted for the World Health Organisation and the<br />
International Committee of the Red Cross in Geneva.<br />
Currently, he is continuing work on his long - standing<br />
interest in emergency and transport ventilation and is<br />
a consultant adviser in this area to Pneupac Ventilation,<br />
a part of Smiths Medical International.<br />
54 Spring 2016 | <strong>Ambulance</strong>today
Clinical Focus on Emergency Artificial Ventilation<br />
This device and others like it have been<br />
widely used in anaesthetic rooms and in<br />
both hospital and prehospital emergency<br />
medicine since that time 6 . In conjunction<br />
with a pharyngeal mask, the bag-valve-mask<br />
is probably the mostly widely-used device to<br />
provide positive pressure ventilation in the<br />
world today. (Figure 2)<br />
Figure 2: The BV device with the Ruben<br />
non-return valve (1) pharyngeal mask (2)<br />
filter and non-return valve (3) self-reforming<br />
bag. (Photograph by courtesy of AMBU,<br />
Copenhagen, Denmark)<br />
Perceptions of safety and<br />
effectiveness of bag valve mask<br />
ventilation<br />
There are a number of reasons for the<br />
widespread adoption of the BVM by<br />
paramedical and other emergency services<br />
which include the following:<br />
1 It had an apparent simplicity of action<br />
with either one hand holding the mask<br />
while the other squeezed the bag (single<br />
operator) or two hands holding the mask<br />
( the so-called ‘ double C ‘ position) and<br />
another person squeezing the bag 2 .<br />
2 There was a belief that in squeezing the<br />
bag manually there was a feeling of being in<br />
‘direct contact ‘ with the patient’s lungs and<br />
therefore over-ventilation would be avoided<br />
3 There was a conviction that the device<br />
was essentially safe to use and could provide<br />
effective ventilation. This was probably<br />
based upon the fact that that bag ventilation<br />
is used following the induction of general<br />
anaesthesia in the anaesthetic room on<br />
patients who are asleep, have muscle<br />
relaxation and usually an empty stomach.<br />
Many of these patients would also have<br />
normal values of airway resistance and lung<br />
compliance. It was in this environment that<br />
many paramedics first received their airway<br />
and ventilation training.<br />
4 Compared with mechanical ventilators<br />
providing BVM involved a low financial<br />
outlay. The development of disposable BVM<br />
at the end of the 20th century provided<br />
a solution to sterilisation with increasing<br />
concerns about cross-infection.<br />
Problems associated with the use of<br />
the bag-valve-mask device<br />
Despite continuing widespread use of the<br />
BVM in emergency ventilation (particularly<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
in the United States, where the adoption of<br />
alternative portable automatic ventilation<br />
has been relatively slow) there has been<br />
increasing concern over the past decade<br />
about potential serious problems that<br />
may be associated with this type of<br />
positive pressure ventilation. These may<br />
be summarised as hypo - and hyper -<br />
ventilation.<br />
Hypoventilation<br />
The BVM usually operates using air as<br />
the main gas with supplemental free-flow<br />
oxygen provided to increase the oxygen<br />
concentration. However this can cause<br />
considerable wastage of bottled oxygen due<br />
to leaks around the mask (particularly if held<br />
with only one hand). In addition, if the mask<br />
seal is not effective too low a tidal volume<br />
will be delivered to the patient leading to<br />
hypoventilation and hypoxia.<br />
Hyperventilation<br />
Inappropriate use of the BVM may cause<br />
(1) high ventilation frequency and tidal and<br />
minute volumes and (2) excessive inflation<br />
pressures. These can cause gastic insufflation,<br />
barotrauma, where weak sections of the<br />
lung parenchyma are disrupted, leading<br />
to pneumothorax and the more recently<br />
recognised problem of volutrauma,<br />
where damage is caused to the alveoli<br />
by over-distension. In addition, excessive<br />
intrathoracic inflation pressures have<br />
important haemodynamic consequences.<br />
High ventilation rates<br />
Ventilating the patient too quickly, even if the<br />
tidal volume is correct leads to an excessive<br />
minute volume and hypocapnia. Even with<br />
trained and experienced operators the<br />
stressful nature of the emergency situations<br />
where BVM are used can lead to high<br />
ventilation rates. Cooper et al 7 noted that<br />
keeping artificial ventilation rates low is<br />
difficult because the high adrenaline state of<br />
the rescuer alters time perception, and that<br />
the rapidly refilling bag provokes a reflex<br />
in which rescuers are inclined to deliver<br />
breaths as soon as the bag inflates.<br />
Aufterheide et al 8 reported a clinical<br />
study observing ventilation rates in cardiac<br />
arrest patients. They found that emergency<br />
medical services (EMS) rescuers using a bag<br />
valve device who were trained to follow<br />
the American Heart Association (AHA)<br />
guidelines were delivering on average 37±4<br />
breaths per minute, not the 10–12 breaths<br />
per minute prescribed by the guidelines.<br />
Even after the rescuers were re-trained to<br />
deliver 12 breaths per minute, they were<br />
observed delivering an average of 22±3<br />
breaths per minute.<br />
Losert et al 9 demonstrated excessive<br />
ventilation rates with BV devices even<br />
among trained intensivists, most of whom<br />
were basic or advanced life support<br />
instructors. Their study demonstrated that<br />
the respiration target rate was achieved<br />
only 18% of the time in patients receiving<br />
cardiopulmonary resuscitation, even when<br />
performed in a hospital setting. On average<br />
the guideline for correct ventilation rate was<br />
exceeded by 33%.<br />
O’Niell and Deakin 10 studied BVM in<br />
comparison with a manually triggered<br />
ventilator and an automatic transport<br />
ventilation. They found that hyperventilation<br />
was common with the BVM but mainly due<br />
to high respiratory rates (ranging from 9<br />
– 41 breaths per minute) rather than from<br />
excessive tidal volumes.<br />
Excessive inspiration pressure<br />
Several studies have demonstrated excessive<br />
inspiration pressures using bag valve devices<br />
which can cause barotrauma and gastric<br />
insufflation<br />
There has been a long-standing fear that<br />
in patients with an unprotected airway<br />
excessive airway pressure caused by<br />
squeezing the bag too hard would open<br />
the oesophageal sphincter and cause<br />
inflation of the stomach, leading to potential<br />
regurgitation and aspiration into the lungs.<br />
This was a particular concern in patients<br />
being resuscitated following cardiac arrest<br />
Updike and colleagues 11 studied the use of<br />
the BVM in comparison with a manuallytriggered<br />
ventilators and an automatic<br />
transport ventilator. All three devices<br />
delivered similar tidal volumes when used<br />
by emergency medical technicians the BV<br />
device was associated with a high PAP,<br />
mask leak and gastric insufflation. The latter<br />
problem has long been a major concern<br />
when ventilating through an unprotected<br />
airway such as a pharyngeal mask 12 – 14 . Salas<br />
et al 12 , reporting a study measuring the<br />
differences between a bag valve device and<br />
a transport ventilator used with a mask<br />
found that almost 10 times the amount<br />
of air was insufflated into the simulated<br />
stomach per breath when the subjects used<br />
a bag valve device.<br />
Haemodynamic effects of increased<br />
intra thoracic pressure when using a<br />
bag valve device<br />
There are a number of studies which<br />
have investigated the effects of excessive<br />
intrathoracic pressure on the circulation<br />
when venous return to the heart is<br />
impaired. These can have serious<br />
consequences in hypovolaemic patients<br />
following physical trauma. Cheifz et al 15<br />
noted that hyperventilation results in<br />
high intrathoracic pressure during the<br />
decompression phase of cardiopulmonary<br />
resuscitation (CPR), which decreases cardiac<br />
pre-load and cardiac output and impedes<br />
right ventricular function. Increased tidal<br />
volume is also known to adversely affect<br />
cardiac output. These authors believe that<br />
“the elevated mean intrathoracic pressures<br />
caused by excessive ventilation inhibited<br />
venous blood flow back to the right heart,<br />
as there was insufficient time to allow for<br />
55 3
Clinical Focus on Emergency Artificial Ventilation<br />
the development of negative intrathoracic<br />
pressure between compressions.”<br />
Reduced pre-load results in lower stroke<br />
volume and, ultimately, decreased cardiac<br />
output.<br />
Emergency ventilation using portable<br />
automatic ventilators<br />
The alternative to using a BV device in<br />
emergency is the portable automatic<br />
ventilator. These are widely used in some<br />
areas of the world and have a number<br />
of advantages over bag-valve devices.<br />
The International Liaison Committee on<br />
Resuscitation ( ILCOR ) reviewed the<br />
relatively limited literature about automatic<br />
ventilators in 2010 2 and produced the<br />
following observations.<br />
1 Automatic ventilators or resuscitators<br />
provide a constant flow of gas to the patient<br />
during inspiration; the volume delivered<br />
is dependent on the inspiratory time (a<br />
longer time provides a greater tidal volume).<br />
Because pressure in the airway rises<br />
during inspiration, these devices are often<br />
pressure limited to protect the lungs against<br />
barotrauma.<br />
2 An automatic ventilator can be used with<br />
either a facemask or other airway device<br />
(e.g., tracheal tube, supraglottic airway<br />
device).<br />
3 An automatic resuscitator should be set<br />
initially to deliver a tidal volume of 6–7 ml<br />
kg−1 at 10 breaths min−1. Some ventilators<br />
have co-ordinated markings on the controls<br />
to facilitate easy and rapid adjustment<br />
for patients of different sizes, and others<br />
are capable of sophisticated variation in<br />
respiratory parameters. In the presence<br />
of a spontaneous circulation, the correct<br />
setting will be determined by analysis of the<br />
patient’s arterial blood gases.<br />
4 Automatic resuscitators provide many<br />
advantages over alternative methods of<br />
ventilation.<br />
• In unintubated patients, the rescuer<br />
has both hands free for mask and airway<br />
alignment.<br />
• Cricoid pressure can be applied with one<br />
hand while the other seals the mask on the<br />
face.<br />
• In intubated patients they free the rescuer<br />
for other tasks.<br />
• Once set, they provide a constant tidal<br />
volume, respiratory rate and minute<br />
ventilation; thus, they may help to avoid<br />
excessive ventilation.<br />
• They are associated with lower peak<br />
airway pressures than manual ventilation,<br />
which reduces intrathoracic pressure and<br />
facilitates improved venous return and<br />
subsequent cardiac output.<br />
A manikin study of simulated cardiac arrest<br />
and a study involving fire-fighters ventilating<br />
the lungs of anaesthetised patients both<br />
showed a significant decrease in gastric<br />
inflation with manually triggered flow-limited<br />
oxygen-powered resuscitators and mask<br />
compared with a BVM 16,17<br />
Figure 3 shows a modern resuscitation<br />
ventilator which is currently used by a<br />
number of emergency medical services.<br />
Figure 3. The Pneupac VR1 resuscitation<br />
ventilator. This device can replace the BVM<br />
and can deliver single manually – controlled<br />
breaths during cardiopulmonary resuscitation<br />
or continuous automatic ventilation.<br />
(Photograph by courtesy of Smiths Medical International<br />
(Luton, UK)<br />
The need for more studies on<br />
automatic ventilators<br />
It is worth noting that the 2010 ILCOR<br />
guidelines cited 23 papers which studied<br />
ventilation as opposed to more than<br />
93 papers concerned with airway<br />
management. Of the ventilation papers<br />
cited, only 3 directly concerned the use<br />
of automatic ventilators. The reason for<br />
there being so few studies on manual and<br />
automatic ventilation is unclear but may be<br />
as a result of ventilation being seen as an<br />
‘obvious’ technique which does not require<br />
investigation. In this respect it is similar to<br />
suction aspiration which is an essential part<br />
of clearing the airway of secretions and<br />
vomitus but which appears never to have<br />
been the subject of a controlled trial.<br />
The evidence available shows that the use<br />
of bag-valve devices is associated with<br />
hyperventilation, in terms of both frequency<br />
and delivered tidal and minute volumes as<br />
well as the peak airway pressure delivered.<br />
The consequences of this in terms of<br />
possible gastric insufflation and barotrauma<br />
are understood. The potential dangers<br />
from volutrauma however has received less<br />
attention, although the damage caused to<br />
the lung parenchyma and subsequent acute<br />
respiratory distress syndrome (ARDS) in the<br />
intensive care setting have been recognized<br />
for many years and have led to the use of<br />
smaller tidal volumes with PEEP to keep<br />
the alveoli open, (the ‘open lung’ strategy<br />
first described by Lachmann 18 ). Given the<br />
potential vulnerability of the lungs and other<br />
organs in a patient with major trauma and<br />
shock, the question of induced volutrauma<br />
in emergency ventilation deserves greater<br />
study.<br />
Bag – valve ventilation compared<br />
with automatic ventilation<br />
There have been some studies which<br />
compare the quality of ventilation delivered<br />
by portable automatic ventilators (known<br />
as ‘automatic transport ventilators’ in US<br />
despite the fact that they are widely used<br />
in emergency ventilation as well as in the<br />
transport of a ventilator-dependent patient<br />
from one location to another).<br />
Salas et al 12 found no differences in delivered<br />
tidal volume between a bag, a valve device<br />
and an automatic ventilator (Impact 730)<br />
using a facemask in a model of adult cardiac<br />
arrest. However, as noted above, they also<br />
found less gastric insufflation and a reduced<br />
mask leak using the ventilator. Their overall<br />
conclusion was ‘that compared with the<br />
BVM the ventilator is at least as effective, is<br />
easier to use, and limits gastric insufflation.<br />
Weiss et al 19 in a study of paramedical<br />
personnel using a BVM or an automatic<br />
ventilator in cardiac arrest concluded that<br />
they were able to accomplish more tasks<br />
and provide better patient care when using<br />
the automatic ventilator. Goedeke et al 20<br />
compared ventilation with a bag valve device<br />
and the Oxylator ventilator. They found the<br />
the bag valve device delivered higher peak<br />
airway pressures and was associated with a<br />
lower SaO 2. They found no differences in<br />
the tidal volumes delivered.<br />
In another study comparing the Oxylator<br />
with bag valve ventilation Noordergraaf<br />
et al 21 found that the bag valve device was<br />
associated with better airway management<br />
and that the Oxylator in automatic<br />
mode delivered hyperventilation. They<br />
recommended that the ventilator should<br />
only be used in manual mode during<br />
resuscitation.<br />
56 Spring 2016 | <strong>Ambulance</strong>today
Clinical Focus on Emergency Artificial Ventilation<br />
The function of the automatic ventilator is<br />
important (whether the device is a pressure<br />
or a volume generator) in replacing BV<br />
ventilation. Pressure cycled ventilators<br />
have been shown to be unreliable in<br />
emergency use. L’Her and Roy 22 have<br />
conducted laboratory trials of a number of<br />
portable ventilators. They concluded that<br />
while most of the volume-cycled ventilators<br />
proved to be technically efficient and reliable<br />
pressure cycled ventilators (they examined<br />
the Oxylator EMX and the Vortran RTM)<br />
gave rise to concern since they did not<br />
deliver consistent tidal volumes and under<br />
certain conditions could be unsafe. Further<br />
comment on this is found in a review by<br />
Branson 23 .<br />
Recently, Kreft 24 has conducted bench<br />
studies using a calibrated test lung to<br />
assess BV vs automatic ventilation. Trained<br />
responders using the bag-valve device<br />
showed considerable variation in the rate<br />
and volumes of the ventilation delivered<br />
(Figures 4 and 5).<br />
Conclusions<br />
There is increasing evidence to show the<br />
variability of ventilation delivered by bag<br />
– valve devices when used in emergency<br />
ventilation. In particular, high inflation<br />
pressures and large tidal volumes may be<br />
delivered which can cause barotraumas and<br />
volutrauma, as well as gastric insufflation<br />
if the BV device is being used with a<br />
pharyngeal mask.<br />
These findings are accompanied by the<br />
scarcity of studies about emergency<br />
ventilation in the literature.<br />
There is a need for greater awareness of<br />
the potential problems of intermittent<br />
positive pressure ventilation in emergency.<br />
To achieve this better training is required<br />
for the use of the BVM and also automatic<br />
emergency ventilators.<br />
A better understanding of the limitations<br />
of the BV device and the advantages of<br />
the portable ventilator is also required.<br />
In addition more research studies are<br />
needed to provide a better evidence base<br />
for ventilation in emergency, to support<br />
international guidelines, and to bring<br />
emergency ventilation skills in line with basic<br />
and advanced airway management.<br />
Figure 4. The Ventcheck (IngMar Medical,<br />
USA) experimental set –up. Ventilation of a<br />
manikin using a BVM is monitored using an<br />
Ingmar test lung linked to a computer display<br />
of the ventilation parameters.<br />
(Photograph courtesy of Smiths Medical International (Luton,<br />
UK)<br />
Figure 5 (a) Variation in tidal volume delivered<br />
by BVM for two operators. There is significant<br />
variation from the target volume of 600 ml,<br />
both for individual ventilations and in the mean<br />
delivered ventilation over a period of 5 minutes<br />
Figure 5 (b) Ventcheck recording with the<br />
test lung ventilated by a volume targeted<br />
automatic ventilator ( Pneupac Parapac Plus)<br />
set to deliver a tidal volume of 600ml. The<br />
individual variation in tidal volume between<br />
delivered breaths is negligible compared with<br />
the bag valve recordings of tidal volume from<br />
two subjects shown above.<br />
(Photographs courtesy of Smiths Medical International<br />
(Luton, UK)<br />
References<br />
1 Koster RW, Baubin MA, Bossaert L et al. European<br />
Resuscitation Council Guidelines for Resuscitation 2010,<br />
section 2 : adult basic life support and the use of the<br />
automatic external defibrillator. Resuscitation 2010;<br />
81:1277 – 1292<br />
2 Deakin CD, Nolan JP, Soar J et al. European<br />
Resucitation Council Guidelines for Resuscitation 2010,<br />
section 4: adult advanced life support. Resuscitation 2010;<br />
81:1305 – 1352<br />
3 Wilkinson DJ. The History of Trauma Anaesthesia. In<br />
Grande CM (ed) Textbook of Trauma Anaesthesia and<br />
Critical Care, 1993; Chapter 1: 10 - 11<br />
4 Ibsen B. Aanaesthetist’s viewpoint on the treatment<br />
of respiratory complications in poliomyelitis during the<br />
epidemic in Copenhagen in 1952. Proc Roy Soc Med<br />
London 1954; 47:72 – 74<br />
5 Ruben H. A new non – rebreathing valve.<br />
Anesthesiology 1955; 16: 643.<br />
6 Ruben H. The immediate treatment of respiratory<br />
failure. Brit J Anaesth 1964; 36: 542 – 569.<br />
7 Cooper JA, Cooper JD, Cooper JM, Cardiopulmonary<br />
Resuscitation: History, Current Practice, and Future<br />
Direction, Circulation. 2006:114;2839–49.<br />
8 Aufterheide TP, Sigurdsson G, Lurie KG et<br />
al., Hyperventilation-induced hypotension during<br />
cardiopulmonary resuscitation, Circulation.<br />
2004;109:1960–65.<br />
9 Losert H, Sterz F, Koehler K et al. Quality of<br />
cardiopulmonary resusctitation among highly – trained<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
staff in an emergency department setting. Arch Intern<br />
Med 2006;166:2375 - 80<br />
10 O’Niell JF, Deakin CD. Do we hyperventilate cardiac<br />
arrest patients? Resuscitation 2007; 73: 82-85<br />
11 Updike G, Moesseno VN, Auble TE et al.<br />
Comparison of bag valve mask, manually – triggered<br />
ventilator and automatic ventilator devices used while<br />
ventilating a non – intubated mannikin model. Prehosp<br />
Emerg Care 1998; 2(1): 52 – 5<br />
12 Salas N, Wisor B, Agazio J, et al., Comparison of<br />
Ventilation and Cardiac Compressions When Utilizing<br />
the Impact Model 730 Automatic Transport Ventilator<br />
Versus Valve with a Facemask in a Model of Adult<br />
Cardiopulmonary Arrest, Resuscitation, 2007; 74(1):<br />
94–101.<br />
13 Ruben H, Knudsen EJ, Carugati G, Gastric inflation in<br />
relation to airway pressure, Acta Anaesthesiol Scand,<br />
1961;5:107–14.<br />
14 Bowman FP, Menegazzi JJ, Check BD, Duckett TM,<br />
Lower esophageal sphincter pressure during prolonged<br />
cardiac arrest and resuscitation, Ann Emerg Med,<br />
1995;26: 216–19.<br />
15 Cheiftz IM, Craig DM, Quick G, et al., Increasing tidal<br />
volumes and pulmonary over distention adversely affect<br />
pulmonary vascular mechanics and cardiac output in a<br />
pediatric swine model, Crit Care Med. 1998:26:710–16.<br />
16. Stallinger A, Wenzel V, Wagner-Berger H, et al. Effects<br />
of decreasing inspiratory flow rate during simulated basic<br />
life support ventilation of a cardiac arrest patient on<br />
lung and stomach tidal volumes. Resuscitation 2002;54:<br />
167–73.<br />
17. Noordergraaf GJ, van Dun PJ, Kramer BP, et al. Can<br />
first responders achieve and maintain normocapnia<br />
when sequentially ventilating with a bag-valve device and<br />
two oxygen-driven resuscitators? A controlled clinical<br />
trial in 104 patients. Eur J Anaesthesiol 2004;21:367–72.<br />
18 Lachman B. Open up the lung and keep it open.<br />
Intensive Care Med 1992: 18; 319 - 321<br />
19 Weiss SJ, Ernst AA Jones R et al. Automatic<br />
transport ventilator versus bag valve in the EMS setting:<br />
a prospective randomized trial. South Med J. 2005;<br />
98(10): 970 – 6.<br />
20 Goedeke A, Wenzel V, Hoermann S et al. Effects of<br />
face mask ventilation in apnoeic patients with a with<br />
resuscitation ventilator in comparison with a bag valve<br />
mask. Journal Emerg Med 2006; 30(1); 63 – 67<br />
21 Noordergraaf GJ, Van Dan DJ, Shors MP et al.<br />
Efficacy and safety in patients on an EM 100 resuscitator<br />
in comparison with a bag valve device. Am J Emerg Med<br />
2004; 22(7): 537 - 543<br />
22 L’Her E, Roy A. Bench tests of simple , handy<br />
ventilators for pandemics: performance, autonomy and<br />
ergonomy. Respiratory Care 2011; 56(6) 751 – 767.<br />
23 Branson R. Patient needs should drive ventilator<br />
selection for stockpiling; ‘handy’ ventilators may not<br />
‘lend a hand’ Respiratory Care 2011;56(6) 879<br />
24 Kreft R. 2014 Personal communication<br />
57 3
VENTILATION<br />
IN MOTION<br />
VENTILATION<br />
IN MOTION<br />
The NEW paraPAC plus ventilator from Pneupac ®<br />
Oxygen Therapy, CPAP, and Ventilation combined in one robust, compact<br />
and MRI compatible oxygen treatment platform.<br />
For more information visit www.smiths-medical.com<br />
pneupac@smiths-medical.com<br />
©2016 Smiths Medical. All rights reserved. paraPAC and the Smiths Medical design mark are trademarks of Smiths Medical.
Focus on Europe’s fastest-growing ambulance builder<br />
The Happy Haus of BAUS<br />
– Crafting Bespoke <strong>Ambulance</strong>s<br />
to Meet Growing Global EMS Demand<br />
Last year Baus AT designed and built over 800 new EMS vehicles for customers across the world. They<br />
included Medical Services Units, HDUs and Neo-Natal <strong>Ambulance</strong>s. A family-run ambulance-build<br />
company, Baus AT have been manufacturing from their Toruń-based plant in Northern Poland since 2007.<br />
But now, due to the constantly-rising demand created by their outstanding build-quality and superb<br />
after-sales support service, father, Franz, son, Uwe, and their dedicated team of 200+ workers, face the<br />
logistically demanding challenge of moving their well-organised ambulance build operation to a custombuilt<br />
new 17,000 metre square plant over twice the size of their existing facility, also in Toruń.<br />
<strong>Ambulance</strong> Today editor, Declan Heneghan, recently went out to the beautiful 12th century medieval city<br />
of Toruń, birthplace of mathematician and astronomer Copernicus, to see first-hand how Baus build their<br />
world-beating range of EMS vehicles.<br />
Photography by Isaac Heneghan<br />
Franz Baus<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Founder and the driving force behind<br />
Baus AT, German entrepreneur, Franz, is<br />
not complaining about the move one bit.<br />
Supported by Operations Director, Uwe, and<br />
their happy Polish workforce, 2016 is shaping<br />
up to be the year in which his three decades<br />
of hard work and total dedication to the<br />
craft of ambulance building is beginning to<br />
reap substantial rewards in terms of both<br />
global reputation and orders.<br />
Uwe at work<br />
When you drive into the Baus AT plant two<br />
long rows of plain-looking work units are<br />
separated by a wide tarmacked area along<br />
which rows of ambulances are parked. The<br />
decals on the sides of the vehicles tell you<br />
they are intended for customers from as<br />
far afield as Germany, the Netherlands, the<br />
UK, France, Hong Kong and all parts of the<br />
Middle East. But apart from a modest sign on<br />
the small main entrance, there’s no clue as to<br />
what exactly goes on inside any of the units.<br />
There is no reserved parking for the senior<br />
managers and cars of all makes and ages are<br />
scattered up and down. The only evidence<br />
of activity is the occasional movement of<br />
ambulances being moved from ‘A’ to ‘B’ and<br />
men in overalls walking hurriedly between<br />
each block, usually holding a clip-board or a<br />
tool of some sort.<br />
With Baus UK Managing Director, David<br />
Brophy as my initial tour guide the first stop<br />
of the day was to call in on founder and<br />
overall boss, Franz Baus, in his surprisingly<br />
modest and unfussy office. Franz was<br />
completing a phone call to Hong Kong.<br />
Aware that Baus has made a great effort to<br />
build business in the Asia-Pacific, Middle and<br />
Far East regions in recent years I inquired<br />
how things are going?<br />
“Hong Kong has been a terrific market for us<br />
in recent years. We currently have an order<br />
for about 80 units from the government<br />
Fire Brigade and we have delivered in the<br />
last 8 years more than 600 units to the<br />
Fire Brigade, also to different Power Plants,<br />
Winter 2014 | <strong>Ambulance</strong>today3 59
Focus on Europe’s fastest-growing ambulance builder<br />
St.John’s and the famous Hong Kong Hockey<br />
club. In terms of ambulance we have a<br />
100% market-share. We’re also selling well<br />
to China… about 400 units per year, in<br />
cooperation with a local manufacturer. It’s a<br />
mix of Mercedes and Vito chassis on mainly<br />
box bodies,” Franz explained.<br />
The next stop was in the Design Unit.<br />
Staffed by a group of four designers and<br />
business development managers this hectic<br />
office space is the technological nervecentre<br />
of Baus. Filled with display boards<br />
with draughtsman’s drawings it’s a case study<br />
in organised chaos. Every work surface is<br />
dominated by large computer screens and<br />
crammed with files and diagrams and every<br />
shelf is stacked with random components,<br />
such as light-boards, computer boards and<br />
even distributor caps.<br />
It is here that the design team develops<br />
the bespoke designs for each ambulance<br />
order. Baus don’t work on a ‘one-size-fitsall’<br />
business model, instead preferring to<br />
work closely with each customer so that<br />
the specification for every order precisely<br />
meets their individual needs. So even though<br />
the rudiments of the general design and<br />
build process may have large elements in<br />
common, every order will have a number<br />
of features that make it unique; whether the<br />
order is for 10 or 100 units, for a straightforward<br />
emergency care ambulance or<br />
for a complex High Dependency Unit;<br />
there may be different seating, alternative<br />
interior layouts in the patient treatment<br />
compartment, a different lifting system or<br />
a customised trolley-loading system. But as<br />
Business Development Director Robert<br />
Piotr Królikowski, explained to me: “We focus<br />
on each customer’s specific needs and then<br />
help them incorporate the latest technical<br />
innovations.” With eight years experience at<br />
Baus nothing fazes Robert. “We stay in touch<br />
with market trends in build and design and<br />
learn as much as possible about how the<br />
vehicles we build are going to be used. The<br />
more you understand their front-end use,<br />
the better you can meet the needs of your<br />
customers,” he explained. “So, for example,<br />
while we typically recommend either Sarco<br />
or Whelen light-bar fittings, we’ll look at<br />
other suppliers if the customer has a need or<br />
a preference for them.”<br />
Sat across from Robert were Project<br />
Manager, Marek Sylwestrowicz, who has<br />
been with the company 11 years and,<br />
beside him, Agnieszka Mazur, also a Project<br />
Manager who, due to her bilingual capabilities<br />
including French, is responsible for Baus’s<br />
growing presence in the French EMS<br />
market. Agnieszka is responsible for working<br />
with their French distribution partner and<br />
monitors all their builds.<br />
After the relative quiet of the Design Unit<br />
we walked into the first main build area.<br />
One production worker, Marcin, has been<br />
a tool-turner for as long as Franz Baus has<br />
been involved in ambulance-building – thirty<br />
years. Based in the busy Mounting Room,<br />
he is one of the engineers responsible<br />
for hand-crafting the numerous small but<br />
vital engine parts which form the essential<br />
bone structure of each Baus ambulance.<br />
When I caught up with him he was focusing<br />
intensely on turning an unrecognisable joint<br />
he was smoothing down for the main plinth<br />
of what I later learnt would become the<br />
main suspension supports for one of Baus’s<br />
in-house-designed under-carriages - that<br />
invisible part which support the seats in<br />
the ambulance’s driver compartment. As I<br />
looked down, I asked Marcin what he was<br />
making? “It’s a small but difficult part,” he<br />
replied. Adding with a serious look: “Each<br />
of these parts has to be crafted to within a<br />
milimetre… sometimes even more precisely.”<br />
I squinted in even closer, still trying to<br />
recognize the precise thing he was making.<br />
Sensing my lack of mechanical knowledge,<br />
he added, as if by way of further explanation.<br />
“It may appear to fit well at a glance but<br />
you have to inspect it closely. If it doesn’t fit<br />
perfectly, that’s when you get the wear-andtear…<br />
But here we build them to last.”<br />
Also guiding me around the plant was Franz’s<br />
son, Uwe. Aged just 35, it’s Operations<br />
Manager Uwe’s responsibility to know each<br />
of the company’s 200 + staff on first-name<br />
terms, exactly what their individual work<br />
manifest requires of them on a given shift<br />
and which part of each customer’s order<br />
they are charged with fulfilling that day. To<br />
achieve this daunting task he must possess an<br />
intimate knowledge of every single part of<br />
the design and build process for every one<br />
of the 800 + vehicles that rolls out of the<br />
plant each year. Despite his experience of<br />
the whole build process Uwe takes nothing<br />
for granted and consequently has nothing<br />
but admiration for Marcin and his teammates.<br />
As he explained to me: “In every ambulance<br />
we build there can be between one-to-twothousand<br />
small but essential parts, most<br />
of which are built from scratch in-house.”<br />
It’s this kind of attention to detail which<br />
marks Baus out from all other European<br />
ambulance builders. Working away next to<br />
Marcin another colleague was machining the<br />
supports that keep the gas cylinder holders<br />
in place to ensure maximum safety and,<br />
of course, total compliance with the rigid<br />
EC CEN regulations which all European<br />
ambulance builders must meet in order to<br />
make their vehicles road-worthy.<br />
Most of the Baus facility is taken up by<br />
dedicated manufacturing areas: mounting<br />
rooms, fixation rooms, furniture shop,<br />
electrical area, metal-working rooms and<br />
a huge stock management area. It’s all laid<br />
out in such a way that as you pass through<br />
each area, spread over two facing sites,<br />
you gradually get a picture of how each<br />
ambulance unit evolves. In some areas you<br />
might see a bare chassis stood next to a<br />
work-bench with a large sheet of heavy<br />
metal laid out on top and random holes<br />
drilled up and down it. Then you walk<br />
through to the next unit and see an almost<br />
identical scenario - but this time electrical<br />
engineer, Karol Pierukki, 26, is patiently<br />
threading many different-coloured lines of<br />
electrical wiring through each hole and you<br />
realize you are seeing both the inner vehicle<br />
wall and its electrical circuitry system take<br />
shape.<br />
Next we moved on to the Fixation Room<br />
where much of the stainless steel work is<br />
done – everything from the outer-skins of<br />
the ambulance body down to variouslysized<br />
brackets which hold them together<br />
are cut here. Huge and spacious it was<br />
filled with vast pallets of different grades of<br />
steel and pipes of all lengths and diameters.<br />
With its high ceiling, the high-pitched whine<br />
of a ferocious looking computer-operated<br />
cutting machines echoed off its walls; amid<br />
all the din and noise I was waved over in<br />
the most friendly of fashions by Lukas Rata<br />
60 Spring 2016 | <strong>Ambulance</strong>today
Focus on Europe’s fastest-growing ambulance builder<br />
Jczak, the metal-worker responsible for the<br />
impressively high-tech Plasma CNC-mill – a<br />
highly imposing and hugely expensive cutting<br />
machine which quite amazingly can cut up to<br />
10 large panels per shift, down to well below<br />
a milimetre’s precision. The CNC-mill can<br />
cut enough steel for the paneling for three<br />
completed vehicles in less than eight hours<br />
and, despite its furious whine, do so with the<br />
delicacy of a haute coutour cutter turning<br />
fine fabrics into a bespoke Chanel garment.<br />
Lukas, 32, has that youthful, clean-living<br />
look, common to most Polish people under<br />
about eighty, so amid all the unfamiliar noise,<br />
when I asked his age I misheard his reply<br />
and, based on his looks alone, I thought I<br />
heard ’22,’ an easy mistake to make under<br />
the circumstances. Not unsurprisingly, when<br />
he told me he had already worked for Baus<br />
for eight years, I was a little confused. Seeing<br />
my puzzlement Uwe corrected me, laughing:<br />
“No. Lukas is 32, not 22! We are dedicated,<br />
but so far we haven’t felt the need to hire<br />
children!” Uwe explained that Lukas has<br />
been with Baus for eight years and most of<br />
that time has been spent training to operate<br />
new iterations of this specific machine.”<br />
Uwe added that although the standards of<br />
apprenticeship training in Poland for crafts<br />
relevant to vehicle manufacturing, such as<br />
electrical installation and metal-working,<br />
are among the very best in Europe, making<br />
them exceptionally high by global standards<br />
– since the degree of precision required for<br />
ambulance build metal-working is higher still,<br />
mainly for infection control purposes, much<br />
of the training and development of staff like<br />
Lukas, is maintained continuously on the job.<br />
“We buy these high-tech and, to be honest,<br />
very expensive cutting devices and with the<br />
support of their manufacturers, we train<br />
our cutters to perfectly trim different types<br />
of sheet metal. Lukas knows which type<br />
of metal can be cut in a certain way and<br />
which grade is best for different elements<br />
of the ambulance’s outer or inner body.<br />
No matter how highly-skilled they might<br />
be, you couldn’t just expect another metal<br />
worker to walk in here, operate this machine<br />
and then cut the metal so precisely. All the<br />
information required is fed directly into the<br />
machine’s computer by our CAD design<br />
team and it stores the unique information<br />
for every unit we build.” Uwe finished: “One<br />
great benefit is that if an ambulance comes<br />
back to us a couple of years later and its<br />
side-wall has been written-off in a collision,<br />
we can replace it completely and identically,<br />
even using exactly the same grade of metal<br />
that was used in the original vehicle. This<br />
machine allows us to cut all major steel and<br />
aluminium components in-house, reducing<br />
waiting time for key parts.”<br />
A pattern was beginning to emerge. Even<br />
among the younger staff I had spoken with<br />
the length of service was an average eight<br />
years and, most of those over forty I had<br />
spoken to, many had worked for much<br />
longer – a few having moved to Poland<br />
from Baus’s original German base –a statistic<br />
which immediately struck me as unusual<br />
since many of the people I know who<br />
work in the ambulance-build industry move<br />
around frequently – some I have met have<br />
worked for three or four different builders<br />
during their careers! I asked Uwe why the<br />
plant seemed to be staffed with such hardworking<br />
yet apparently happy workers. “It’s<br />
because we’re a family business and we see<br />
all our staff…and their families…as part of<br />
one big family.” In what way, I wondered?<br />
“Well, for example, it’s not a big thing but<br />
every year we have a big Christmas party…<br />
local food, beer, vodka, music…and it’s not<br />
just the workers, but all their families who<br />
come along. This Christmas we had over<br />
300 at the party. We had a good time!” he<br />
replied, laughing.<br />
It was becoming clear just how Baus<br />
manage to construct such exceptionally<br />
high-quality ambulances from their<br />
unremarkable-looking base in Toruń. But as<br />
Franz stressed, the location wasn’t selected<br />
solely for the workpool of skilled vehicle<br />
engineers available in the region. “From<br />
here in Poland we can easily serve the<br />
entire European market,” he explained. We<br />
also have purchasing, sales and aftersales<br />
sites in Germany, France, the Netherlands,<br />
Finland, the UK and Ireland. We place a large<br />
emphasis on preventative maintenance and,<br />
as you saw in Lukas’s section, our engineers<br />
always make sure we have impress stock<br />
readily available for all the vehicles we supply<br />
to our global customer-base. We could<br />
be complacent about our three decades<br />
ambulance build experience, but instead<br />
we remind ourselves that a large part of<br />
our current success is based on our aftersales<br />
support set-up which means we can<br />
guarantee that our customers’ needs are<br />
always comprehensively, quickly and expertly<br />
met, regardless of where they are located in<br />
the world.”<br />
The final stop was in the furniture section<br />
where Franz again explained Baus At’s<br />
decision to locate their plant in Toruń. “It has<br />
given us a pool of exceptionally highly-skilled<br />
vehicle build workers, that I don’t believe<br />
we could find in any one other industrial<br />
location in Europe,” said Franz, looking over<br />
the busy cabinetry room. “So now, we’re<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Winter 2014 | <strong>Ambulance</strong>today3 61
Your specialist for individual<br />
rescue and patient systems<br />
Rettungsprodukte GmbH & Co. KG<br />
Rudolf-Diesel-Straße 7 • D-53859 Niederkassel-Mondorf<br />
Tel: +49 (0)228 971 18 97 • Telefax +49 (0)228 971 18 99<br />
E-Mail: info@schnitzler-rettungsprodukte.de<br />
Web: www.schnitzler-rettungsprodukte.de<br />
Vacuum mattress FALCK 01<br />
Vacuum mattress 817 K<br />
Rescue sheets Vacuum splints Rollboards<br />
Patient restraint systems for all stretchers<br />
Suitable for the<br />
transport of<br />
kids with a<br />
body weight of<br />
3,5 kg up to 22 kg<br />
Restraint systems<br />
crash tested<br />
according to<br />
EN 1789<br />
Safety requirements for all carrying systems<br />
STRYKER<br />
STOLLENWERK<br />
MEDIROL<br />
FERNO<br />
KARTSANA<br />
Obesity counseling<br />
Staircase<br />
sliding sheets<br />
Rollbords XXL<br />
Vacuum mattresses
Focus on Europe’s fastest-growing ambulance builder<br />
busy recruiting over 100 new staff, and we’re<br />
in the secure position of knowing that, even<br />
as we create these new jobs, there are still<br />
plenty of other highly-motivated and eager<br />
vehicle engineers locally who would be<br />
happy to join our growing family. One of the<br />
really impressive things about Poland is that<br />
there’s a real dedication among virtually all<br />
work-forces to working hard and doing their<br />
best. Taking pride in doing the best job you<br />
can seems to be ingrained in the national<br />
psyche. Having worked in the past with<br />
some really highly-skilled ambulance builders<br />
in different regions of Europe, I’m still<br />
amazed daily by the positive ‘can-do’ attitude<br />
of our mainly Polish work-force.”<br />
My tour ended in the boardroom over<br />
coffee and delicious locally-baked ginger<br />
biscuits. I asked Franz, Uwe, Robert and<br />
David to put my morning into context<br />
by explaining a little more about their<br />
extraordinary recent European and global<br />
growth. I asked Franz which world region<br />
they are doing best in right now?<br />
“We’re selling nearly 200 units this year in<br />
France already, which is pleasing,” he replied.<br />
“Don’t forget Switzerland, we’re selling 40-50<br />
units there and, while it’s a small market,<br />
we’ve got 50% market-share…then there’s<br />
Turkey and Romania,” Uwe reminded him.<br />
“We’re also doing very well in Germany, the<br />
United Kingdom and the Republic of Ireland,”<br />
replied Franz, pausing to add: “We sold 100<br />
ambulances in Germany last year and, thanks<br />
to David and Robert and his team, the UK/<br />
Ireland market has risen to 200 units from<br />
a standing-start two years ago, with a mix<br />
of boxes and van conversions… Which is<br />
impressive when you consider what a difficult<br />
market the UK is.”<br />
“We’re proud of the progress we’re making<br />
in the UK and Ireland”, said Robert, adding:<br />
“The growth of independent ambulance<br />
providers is the key to this. Major players<br />
such as UKSAS in England and Murray<br />
<strong>Ambulance</strong> in Ireland are highly-valued<br />
customers.<br />
“The main thing though,” said Franz quietly,<br />
“is that we’re gaining more orders in all<br />
these regions each year… but what makes<br />
us happiest is that, in every case, we’re<br />
gaining repeat orders as well. The reason<br />
that makes us so happy is that we never take<br />
our customers for granted… So when they<br />
come back we know that we’re maintaining<br />
their loyalty and trust.”<br />
Stretching his arms, Franz finished: “We all<br />
work very hard at Baus but, as you’ve seen,<br />
our success is down to having a very loyal<br />
and very committed work-force – not only<br />
here in Toruń, but in the UK, in France and<br />
everywhere else we’re busy developing. I<br />
think we achieve this because our secret<br />
ingredient is that we’re a family business…<br />
which means we have family values.”<br />
To find out more:<br />
B.A.U.S. AT SP.Z.O.o<br />
Tel : +48 662 020 072<br />
BAUS AT UK:<br />
Tel: +44 (0) 7974 940 121<br />
or visit: www.baus-at.com<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Winter 2014 | <strong>Ambulance</strong>today3 63
Focus on Global Traffic Technologies<br />
Seeing the Lights: the Traffic Signal<br />
Technology that can Save Time and Lives<br />
Tim Hall, market and development director at Global Traffic Technologies, looks at the<br />
history and technology behind the traffic systems that allow ambulances to respond to<br />
incidents more swiftly and safely<br />
When an emergency vehicle arrives at a<br />
traffic intersection, sirens blaring and lights<br />
flashing, the result can be a frightening<br />
disruption.<br />
Drivers suddenly realise they need<br />
to manoeuvre their cars to allow the<br />
emergency vehicle through. Some drivers<br />
panic, becoming confused and creating<br />
conflicts that can cause blocked lanes and<br />
emergency vehicle crashes, increasing<br />
response times.<br />
But intelligent transportation technologies<br />
that provide emergency vehicles with<br />
a green light at intersections can help<br />
minimise driver confusion, reduce collisions,<br />
and improve emergency response times.<br />
This is an emergency vehicle preemption<br />
system, or EVP. EVP systems are designed<br />
to give emergency vehicles a green light<br />
on their approach to an intersection<br />
while providing a red light to conflicting<br />
approaches.<br />
EVP systems are a simple but powerful<br />
solution that can rapidly and dramatically<br />
improve safety and response times.<br />
History of priority control systems<br />
Both Europe and North America adopted<br />
traffic light priority control in the 1960s, but<br />
developed the technology in contrasting<br />
directions.<br />
In North America, the first users of priority<br />
control were emergency services, including<br />
fire, police and ambulance companies. Public<br />
transport agencies did not take up the<br />
technology until the mid-1970s. In Europe,<br />
conversely, the public transport segment was<br />
the early adopter, followed by emergency<br />
service users.<br />
One reason for the difference is that in<br />
North America local police and fire chiefs<br />
controlled the procurement budgets<br />
for their agencies and were interested<br />
in supporting a dedicated EVP signalling<br />
system approach. Agencies in Europe at the<br />
time had a stronger focus on mass transit<br />
priority control using existing loop-based<br />
vehicle detection systems. These systems,<br />
however, were not suitable for emergency<br />
vehicle use.<br />
Another factor that may have delayed<br />
widespread introduction of emergency<br />
vehicle priority systems in the European<br />
region was the technology used to signal a<br />
preemption request to the intersection.<br />
At that time the most popular methods<br />
being used were strobe lamps, centrally<br />
activated green-corridors and sound<br />
based signalling. In North America the<br />
stroboscopic system emerged as the<br />
dominant technology. Sound-based systems<br />
had inconsistent performance, and there<br />
Similar technology is used for transit signal<br />
priority systems, which enable public<br />
transport agencies to extend or truncate<br />
green cycle times at traffic signals for more<br />
accurate schedule adherence. This means<br />
public transport vehicles — including buses,<br />
light rail trains, street cars, cable cars and<br />
trams — spend less time waiting, lowering<br />
fuel and fleet costs and reducing carbon<br />
emissions.<br />
Book your place at EMS2016 now at: www.ems2016.org<br />
64 Spring 2016 | <strong>Ambulance</strong>today
Focus on Global Traffic Technologies<br />
was a lack of communication between<br />
intersections to implement a central ‘greencorridor’<br />
system (manually providing green<br />
lights along the length of an ambulance’s<br />
route). Even with communications in place<br />
the green-corridor systems performed<br />
poorly and caused severe traffic disruptions.<br />
Strobe systems offered exceptional signalling<br />
range and consistent, reliable performance.<br />
Well suited for North America’s wide and<br />
straight streets, this line-of-sight system<br />
was less effective in Europe where curved<br />
streets and narrow roads reduce range. This<br />
limited the applications and localities suitable<br />
for emergency vehicle priority. In Europe,<br />
sound and green-corridor systems suffered<br />
from the same issues as in North America<br />
and were not widely adopted.<br />
Only with the emergence of radio/GPS<br />
based priority control systems in the early<br />
2000s was a solution developed that truly<br />
began to meet Europe’s emergency vehicle<br />
preemption requirements. Now, a properly<br />
configured EVP system can provide:<br />
• An improvement in response times of up<br />
to 25 percent<br />
• A reduction of up to 70 percent in<br />
intersection crashes involving emergency<br />
responders<br />
• A prevention of crash injuries and related<br />
costs<br />
• A reduction in property damage costs<br />
• Decreased liability for crashes with civilian<br />
motorists<br />
• A quick demonstrable recovering of the<br />
investment from the above benefits<br />
Centralised architectures<br />
EVP systems can be divided into two main<br />
categories: those that use a distributed<br />
architecture and those that implement a<br />
centralised approach to signalling for a green<br />
light.<br />
In a centralised system, the request for<br />
preemption is sent from the emergency<br />
vehicle to the intersection via a central office<br />
that controls if and when a call for a desired<br />
green phase is made.<br />
In this scenario, the equipment on the<br />
vehicle is the priority request generator. The<br />
vehicle sends its location, speed, heading<br />
and identification credentials over a radio<br />
link to the priority request server located<br />
at a central office. This server validates the<br />
identity of the sender and determines which<br />
intersection and what turning movement is<br />
being requested. The priority request server<br />
then communicates the request to the traffic<br />
controller software, which activates the signal<br />
via a wired or wireless link.<br />
Distributed architecture<br />
In a distributed EVP architecture, the priority<br />
request generator is again located on the<br />
vehicle, but each intersection now has a<br />
priority server. When preemption is desired<br />
the message is sent from the priority request<br />
generator either directly over a two-way<br />
radio link or via a cellular or trunked radio<br />
to the priority request server. The priority<br />
request server verifies the vehicle location,<br />
heading, speed and user identification.<br />
If the call is valid and meets triggering<br />
requirements, the priority server signals<br />
the traffic signal controller requesting a<br />
preemption at the intersection for the<br />
desired green phase. The priority request<br />
server may be monitored and configured<br />
by software located at the central office if<br />
communications exist between the central<br />
facility and the intersection.<br />
Advantages and disadvantages<br />
Each EVP architecture has advantages and<br />
prerequisites for proper operation.<br />
Centralised systems can leverage existing<br />
central office to intersection control of<br />
traffic signals, and require no additional<br />
equipment in the local traffic cabinet,<br />
making them an attractive proposition for<br />
European applications where traffic cabinets<br />
are either limited in space or control of<br />
the signals is centrally managed. Priority<br />
request generators on the vehicle can use<br />
existing public safety radio channels, or GPRS<br />
networks to communicate with the central<br />
office priority request server.<br />
But it’s worth remembering that centralised<br />
systems do have critical performance<br />
requirements which must be addressed<br />
if they are to be effective for EVP. Most<br />
important is the ability to accurately and<br />
consistently determine and communicate<br />
to the priority request server when the<br />
emergency vehicle (priority request<br />
generator) has reached the activation point.<br />
Inaccurate position determination, or latency<br />
in communications will cause the trip point<br />
to move forwards and backwards tens of<br />
metres. The result is preemptions that may<br />
take more side street green than is really<br />
necessary and increased traffic disruption.<br />
Book your place at EMS2016 now at: www.ems2016.org<br />
Distributed systems, as noted above, may<br />
use dedicated point-to-point or cellular<br />
radio links. Dedicated radio links ensure<br />
low latency and deterministic access to<br />
the priority server from the emergency<br />
vehicle. This is important as typically multiple<br />
vehicles will be approaching the intersection<br />
at the same time and must all be serviced<br />
with no delay. Continuous updating is also<br />
key for optimal performance. By constantly<br />
signalling the intersection priority request<br />
server, a map matching verification of the<br />
vehicles route may be obtained.<br />
Integration with TSP<br />
EVP systems can also be integrated with<br />
TSP systems, meaning users are able to use<br />
the same intersection equipment. Both EVP<br />
and TSP can be monitored and controlled<br />
using Central Management Software (CMS).<br />
This integration can prove effective in the<br />
case of large events, which are often served<br />
by park-and-ride vehicles that efficiently<br />
transport many attendees. If these public<br />
transport vehicles are equipped with<br />
priority control devices, CMS can cause red<br />
lights to turn green when they approach.<br />
However, if a high priority vehicle requires<br />
the other approach, it will override the inprogress<br />
priority control and give it to the<br />
emergency responder.<br />
This capability is also useful for disaster<br />
evacuation. Event and disaster evacuation<br />
plans may be set up in advance, ready to<br />
implement at the touch of a button.<br />
About Tim Hall and GTT:<br />
Tim Hall is the market and<br />
development director at Global<br />
Traffic Technologies (www.gtt.<br />
com). Headquartered in St. Paul,<br />
Minn., GTT is the market leader<br />
in traffic management systems,<br />
having an installation base of over<br />
70,000 intersections and 70,000<br />
vehicles with over 3,100 customers<br />
worldwide.<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Winter 2014 | <strong>Ambulance</strong>today3 65
Unison Comment<br />
UNISON Update<br />
<strong>Ambulance</strong>TODAY<br />
Keep your promise to ambulance staff<br />
There’s an <strong>Ambulance</strong> Emergency going on! As I have previously reported<br />
in <strong>Ambulance</strong> Today, the Secretary of State for Health, the Rt Hon Jeremy<br />
Hunt MP, offered ambulance staff some additional concessions in the 2015/16<br />
pay settlement for NHS Staff. These included a review of recruitment and<br />
retention issues using bandings, recruitment and retention premia, a review<br />
of the issues rising from the increase in retirement age affecting ambulance<br />
staff, and a 50:50 employer:employee contribution scheme to reduce the<br />
deductions made when taking an early pension to allow staff to retire up to 3<br />
years earlier.<br />
By Alan Lofthouse<br />
National<br />
<strong>Ambulance</strong><br />
Officer, UNISON<br />
Twelve months on and unfortunately,<br />
there’s not a lot to reassure ambulance staff.<br />
Employers have gone some way to making<br />
commitments to look at the banding for<br />
paramedics, in advance of the introduction<br />
of the BSc entry-level qualification for<br />
the HCPC register, but this is dependent<br />
on securing funding. We now have two<br />
ambulance services that pay paramedics<br />
band 6 with more in talks with their staff<br />
side. Why should Clinical Commissioning<br />
Groups fund paramedics at Band 6 when<br />
they get all the skills, responsibilities and<br />
clinical knowledge for Band 5?<br />
Retention is the key here. Pay demonstrates<br />
the value placed on the jobs people do and<br />
is a reflection of the skills and responsibilities<br />
asked of staff. Certainly, more needs to be<br />
done to improve the working conditions for<br />
ambulance staff – high demand, late finishes<br />
and missed meal breaks are the obvious<br />
ones. Just look at the East of England<br />
<strong>Ambulance</strong> service which has threatened to<br />
take draconian and unpalatable measures to<br />
ensure delivery of safe patient care! What<br />
better way to sum up the archaic approach<br />
of some ambulance services when faced<br />
with demand that outstrips capacity. Short<br />
term solutions with long term damage<br />
which will be irreparable beyond a point.<br />
Are we talking about patient care or do<br />
we really mean performance? The reality<br />
is that ambulance staff care about their<br />
patients, young or old, regardless of their<br />
background – especially the really sick ones.<br />
Their main concern is not whether their<br />
service achieves its performance targets<br />
but whether they can make a difference to<br />
someone in pain or suffering.<br />
We are at a crucial point in ambulance<br />
service history. Modernisation is happening<br />
and eyes need to be opened to what will<br />
happen next. In the rush to please the<br />
NHS Trust Development Authority, CCGs,<br />
Trust boards, NHS Improvement, Monitor,<br />
CQC… are there any more?… Trusts<br />
are forced to look at how to squeeze<br />
more from an already over burdened and<br />
stretched workforce.<br />
<strong>Ambulance</strong> staff are loyal, hardworking<br />
and diligent. They are not fools and should<br />
not be sacrificed in order to meet their<br />
Trusts’ performance targets or inspection<br />
organisations’ requirements. These are<br />
human beings doing a very human job. The<br />
problem is that demand is high and the<br />
resources are not keeping up.<br />
Where is the central leadership? Where<br />
is the government? Distracted and not<br />
listening. Our ambulance services could<br />
become world class urgent and emergency<br />
care organisations, but they are having their<br />
hands tied. Staff are feeling the frustration.<br />
The NHS 111 service is fragmented and<br />
being provided by too many different<br />
organisations. Importantly, it is out of the<br />
control of those who need it to work.<br />
Patient Transport Service contracts are<br />
awarded to the lowest private sector bidder<br />
and when contracts are not performing<br />
the CCGs throw good money after bad to<br />
keep them afloat. The provider then pulls<br />
out. Why? Because they cannot make a<br />
profit. Making money by providing a public<br />
service which caters almost exclusively for<br />
the elderly, sick and vulnerable in society<br />
is morally wrong. In all this confusion and<br />
uncertainty is it any wonder ambulance staff<br />
are leaving? The government expect more<br />
from ambulance staff than they can give,<br />
justifying their actions behind the guise of<br />
patient care, as if ambulance staff do not<br />
care about patients! I am not surprised that<br />
people are leaving.<br />
How would you feel if you worked 4<br />
consecutive 12 hour shifts with shift<br />
overruns and maybe one or two meal<br />
breaks (if you are lucky), only to be told that<br />
you are not giving enough; that you need to<br />
give more?<br />
UNISON <strong>Ambulance</strong> - there when you need us<br />
This is not the fault of staff – they are just<br />
working in difficult circumstances to help<br />
those in greatest need. I don’t even think it’s<br />
the fault of the ambulance services – they<br />
have their hands tied by central government.<br />
It’s not the fault of the patients – they are<br />
calling 999 as they are in a confusing system<br />
where they cannot get a GP appointment<br />
or access fragmented providers of urgent<br />
care. As well as this, A&E departments are<br />
full or closing. Who do they turn to? The<br />
ambulance service, because they always<br />
come.<br />
The government have been sleepwalking<br />
into this mess. The warning signs have been<br />
there for sometime but they haven’t been<br />
listening. The offer made last year was to<br />
work with us over issues of recruitment<br />
and retention but the government failed to<br />
commit any additional funding. Apparently<br />
there is no more money.<br />
Immediate action is needed to stem the<br />
exodus of staff. In the short term, bandings<br />
for ambulance staff need to be reviewed<br />
starting with paramedics. The NHS Pay<br />
Review Body recognised that this is taking<br />
too long in their 29th report. They also<br />
recognise that more needs to be done to<br />
deal with the holistic issues facing ambulance<br />
staff. The government could take the bold<br />
move to make the pension age fair for<br />
ambulance staff and bring it in line with the<br />
other emergency services.<br />
Wider, more comprehensive changes need<br />
to take place with NHS 111 and how this<br />
is commissioned to ensure it works in the<br />
right way for patients. Investment is needed<br />
to get the clinical support right for NHS 111<br />
call centres. Returning them to ambulance<br />
control will give the service the resilience<br />
to cope with surges in demand and get the<br />
right care, to the right patient, at the right<br />
time.<br />
Failure to listen and take action risks a<br />
return to industrial unrest with ambulance<br />
staff having little choice but to vote with<br />
their feet in greater numbers than before.<br />
Help them in their emergency. It’s time to<br />
keep your promises to ambulance staff!<br />
To find out more about this UNISON<br />
campaign visit: www.unison.org.<br />
uk/our-campaigns/ambulanceemergency/<br />
Alan welcomes feedback from<br />
ambulance staff and can be contacted<br />
at: a.lofthouse@unison.co.uk<br />
Facebook:<br />
Facebook.com/unisonambulance<br />
Twitter:<br />
Twitter.com/UNISON<strong>Ambulance</strong><br />
Spring 2016 | <strong>Ambulance</strong>today<br />
67 3
Focus on Cloud-Based Resource Optimization Technology<br />
EMS Operations transformed<br />
by Cloud-based platform<br />
WC EMS, the ambulance service of the Western Cape Department of Health, is one of the largest EMS<br />
services in South Africa. Covering a land area similar in size to England, it services a population of 6.2<br />
million, 3.75 million of whom live in the Cape Town metropolitan area. Operating six emergency control<br />
centres and a fleet of 460 vehicles, WC EMS attends in excess of 500,000 incidents annually. As well as<br />
emergency medical response, WC EMS comprises HealthNET, which provides non-emergency patient<br />
transport services across the Western Cape Province.<br />
Following an intensive 30-month project,<br />
WC EMS has incrementally implemented<br />
all main system components of Valentia’s<br />
CareMonX EMS Suite: Emergency CAD,<br />
Patient Transport CAD, MDT and ePCR.<br />
Also implemented are Valentia’s ERP<br />
systems covering Roster Management, Fleet<br />
Management and Operational Analytics.<br />
Together the systems are seamlessly<br />
integrated in one end-to-end platform<br />
that addresses all of WC EMS’s clinical and<br />
operational requirements.<br />
Being cloud-based and modular, CareMonX<br />
EMS Suite is highly versatile, scalable and<br />
future proofed, all of which were key<br />
selection criteria of WC EMS. All CareMonX<br />
mobility elements are operating system<br />
agnostic across Windows, iOS and Android<br />
systems. Android was selected by WC EMS<br />
as the preferred platform for all MDT and<br />
ePCR mobile devices.<br />
Implemented by Valentia in conjunction with<br />
its South African partner, Dimension Data,<br />
the solution replaced Emergency CAD and<br />
Patient Transport CAD systems used by<br />
WC EMS in all six control rooms and also<br />
introduced, for the first time, MDT, ePCR<br />
and ERP systems. The solution, which has<br />
been configured as a multi-node survivable<br />
system, is deployed in a secure private cloud<br />
environment managed by Dimension Data.<br />
Immediate benefits of CareMonX Emergency<br />
CAD included a 20% reduction in call<br />
registration times as well as a sizeable<br />
reduction in abandoned calls rates and<br />
improvements in call classifications. Average<br />
time-to-dispatch recorded a more than<br />
40% improvement from over 11 minutes<br />
to six minutes, assisted by Valentia’s<br />
location management application which<br />
provide enterprise-wide views of all vehicle<br />
locations. CareMonX Emergency CAD also<br />
incorporates international standards-based<br />
Disaster Management functionality, including<br />
rapid activation of mobile control room units<br />
that utilise multiple wireless communication<br />
technologies.<br />
CareMonX Patient Transport CAD<br />
underpins the complex daily operations of<br />
the provincial scheduled patient transport<br />
service, HealthNET, which encompasses<br />
a fleet of almost 100 vehicles plying 60<br />
routes extended across 495 collection<br />
points. CareMonX PTS CAD enables 100+<br />
treatment facilities that receive transported<br />
patients to directly enter patient transport<br />
bookings via an online portal. An SMS based<br />
e-Ticketing facility is available for use by<br />
patients, especially those living in remote or<br />
rural communities.<br />
Benefits of CareMonX MDT include<br />
improved mobilisation times resulting from<br />
electronic communication of incident data<br />
rather than via radio, shaving up to 90<br />
To find out more about Valentia Technologies’ product range visit: valentiatech.com or call them on: +353 1 299 5600<br />
68 Spring 2016 | <strong>Ambulance</strong>today
Focus on Cloud-Based Resource Optimization Technology<br />
”It has been our privilege<br />
to have worked closely<br />
with Western Cape EMS<br />
management and staff<br />
to implement our full<br />
CareMonX EMS Suite which<br />
has transformed WC EMS<br />
into one of the most joined-up EMS services<br />
anywhere in the world today.”<br />
Peter Nelson<br />
President Business Development<br />
Valentia Technologies<br />
seconds off each initial communication. Use<br />
of real-time status updates and two-way<br />
messaging has created additional benefits<br />
in the form of resource optimisation and<br />
capacity management. Additionally, intuitive<br />
navigation (map data provided by TomTom)<br />
in the MDT application has improved onscene<br />
arrival performance.<br />
records from in-field ambulances to hospital<br />
Emergency Departments where they are<br />
immediately viewable, thereby optimising<br />
use of the all-important “golden hour” for<br />
enhanced treatment outcomes. CareMonX<br />
ePCR also produces valuable operational<br />
and clinical data that contribute to improving<br />
service planning and paramedic staff skilling.<br />
“Implementation of Valentia<br />
Technologies CareMonX<br />
EMS Suite has provided<br />
Western Cape EMS with one<br />
of the most comprehensive<br />
and technologically advanced<br />
EMS business solutions in the<br />
developed world today.”<br />
Dr Shaheem De Vries<br />
Director<br />
Western Cape EMS<br />
EMS Suite<br />
Systems<br />
• Emergency CAD<br />
• Patient Transport CAD<br />
• Repatriation CAD<br />
• Major Incident CAD<br />
• Mobile Doctor/Nurse CAD<br />
• Dispatch Management<br />
• Mobilisation (MDT)<br />
• Location Management<br />
• Community Responder Apps<br />
• Electronic Patient Care Reporting (ePCR)<br />
• Roster Management<br />
• Fleet Management<br />
• Billing Management<br />
• Operational Analytics<br />
Features<br />
• Service Oriented Architecture<br />
• Cloud enabled<br />
• Survivable multi node<br />
• Multi OS enabled<br />
• 4G, 3G, Wi-Fi and TETRA enabled<br />
• Standards-based PBX integration<br />
• HL7 and health information exchange with<br />
wider health services<br />
CareMonX ePCR has enabled WC EMS to<br />
switch from manual paper recording to realtime<br />
digital capture for care interventions<br />
associated with the 500,000+ incidents<br />
responded to annually. As well as freeing up<br />
valuable paramedic time, CareMonX ePCR<br />
facilitates real-time transmission of care<br />
WESTERN<br />
CAPE<br />
Key Facts<br />
Population 6.20m<br />
Size<br />
129,462km2<br />
Population Density 45.0 per km2<br />
WC EMS<br />
Personnel 1,950<br />
Control Rooms 6<br />
Stations 55<br />
Operational Fleet 460<br />
Calls Received 735,000<br />
Incidents Attended 515,000<br />
Patients Transported 620,000<br />
PTS Transports 95,000<br />
Director<br />
Dr. Shaheem de Vries<br />
Web<br />
westerncape.gov.za<br />
As CareMonX EMS Suite includes extensive<br />
in-built healthcare data sharing capabilities<br />
that enable EMS services to integrate with<br />
wider healthcare services, the WC EMS<br />
solution has been further designed to<br />
directly support the Service’s strategy of<br />
playing an increasingly pivotal role in the<br />
continuum of community-based care across<br />
urban and rural Western Cape.<br />
About Valentia Technologies<br />
Valentia Technologies develops and<br />
implements innovative software solutions<br />
and services that transform the way<br />
healthcare is provided outside of hospital.<br />
Valentia’s integrated suite of products,<br />
spanning EMS, urgent and unplanned care,<br />
community healthcare, and homecare,<br />
enables new models of joined-up converged<br />
care that address many of the mounting<br />
challenges facing healthcare today: rising<br />
demand, escalating costs, improved quality<br />
outcomes and accountability, and the need<br />
for greater efficiency.<br />
Valentia’s solutions are implemented at scale<br />
in organisations that provide EMS services,<br />
patient transport services, urgent care<br />
services, primary care, community nursing,<br />
allied healthcare services and homecare<br />
services in countries in Europe, Australasia,<br />
the Middle East and Africa.<br />
To find out more about Valentia<br />
Technologies visit:<br />
www.valentiatech.com<br />
Or email:<br />
bizdev@valentiatech.com<br />
Telephone: +353 1 299 5600<br />
To find out more about Valentia Technologies’ product range visit: valentiatech.com or call them on: +353 1 299 5600<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Winter 2014 | <strong>Ambulance</strong>today3 69
Focus on Auxilium Systems<br />
Auxilium Systems<br />
– Personalised<br />
Health and Safety<br />
The Auxilium System is designed to assist <strong>Ambulance</strong> Staff and First Responders by providing potentially<br />
vital information about a patient which they would not usually have access to, particularly when the<br />
patient is unable to provide this information themselves.<br />
The system allows any individual to store<br />
their personal information on a website.<br />
Information such as name, home address,<br />
next of kin and key medical record data<br />
which could potentially be very useful<br />
in some situations when the patient is<br />
unable to communicate. This information<br />
can also include NHS Number, GP’s name<br />
and address, medical history, or even clear<br />
directions to get to a patient’s house. Unlike<br />
a simple medical alert system, commonly<br />
used by aged patients and people with<br />
existing medical conditions, Auxilium is a<br />
Health and Safety system intended to be<br />
used by everybody. A wide range of potential<br />
users have been consulted including schools<br />
and the construction industry to appreciate<br />
what benefits and concerns they believe<br />
such a system would provide. The system<br />
is also intended to be used for ‘one off’<br />
occasions, such as stewards at a sports or<br />
entertainment events.<br />
Each Auxilium user is provided with their<br />
own unique Auxilium Number, this number<br />
can be displayed on items carried by the<br />
user, such as Staff ID Cards, keyrings, or even<br />
displayed on their mobile phone. There is a<br />
distinctive Auxilium System logo attached to<br />
the 10-digit Auxilium number. This logo can<br />
be easily spotted by the emergency services<br />
and the public. The number can then be<br />
provided to the emergency call taker by the<br />
caller who will have access to the Auxilium<br />
Database. The operator with then use this<br />
number to access the relevant information.<br />
The simplicity of Auxilium’s system of a<br />
ten-digit number means that it is easy to<br />
understand and implement, as well as cheap<br />
(just £1 a year for an individual account).<br />
It also means that by using well-proven<br />
technology, unlike a stand-alone device, it is<br />
easily implemented into existing procedures<br />
and schemes (i.e. company ID cards, printed<br />
on sports equipment, written next to school<br />
pupils’ names on a register).<br />
The patient (Account Holder) is completely<br />
in charge of their account, they decide what<br />
information to put on the system and who<br />
has the right to view it. They are the only<br />
people that can see all of the information<br />
on their account, and there is no data about<br />
them on the database that they can’t see.<br />
The patient is responsible for providing<br />
the information which is why the Auxilium<br />
System is referred to as a ‘Personalised<br />
Health & Safety system.’ Further to this,<br />
the system is completely transparent; the<br />
Account Holder knows exactly who has<br />
viewed their data and why.<br />
The initial idea was developed by Grant<br />
Moreton, a Director of Auxilium Systems,<br />
who has a background in the construction<br />
industry (an industry where such a system<br />
would be highly applicable). Grant was<br />
motivated by the deaths of two pupils at his<br />
former school; it is hoped that in the future<br />
such incidents can be reduced by a method<br />
of organization like Auxilium. The concept<br />
was developed further with the assistance of<br />
Dr Chris Rowe, also a Director of Auxilium<br />
Systems, who has 20 years’ experience in<br />
helping individuals and companies develop<br />
innovative ideas, particularly in the medical<br />
device industry.<br />
The Auxilium system has been developed<br />
with the assistance of South Central<br />
<strong>Ambulance</strong> Service NHS Foundation<br />
Trust (SCAS) in order to have a clear<br />
understanding of what information would<br />
70 Spring 2016 | <strong>Ambulance</strong>today
Focus on Auxilium Systems<br />
be of use to the <strong>Ambulance</strong> Services.<br />
The trust has recently launched a trial<br />
of Auxilium to help to identify and treat<br />
patients at the site of an incident.<br />
Luci Stephens, Director of Operations<br />
– Clinical Coordination Centres, South<br />
Central <strong>Ambulance</strong> Service NHS<br />
Foundation Trust, said: “We are pleased to<br />
have embarked on this trial of Auxilium<br />
which we hope will prove to be of benefit<br />
to patients and staff alike. There are<br />
occasions when it would be incredibly useful<br />
to have key details about a patient which<br />
they might not be able to provide to us due<br />
to their medical condition and we hope<br />
that this trial will help demonstrate how<br />
important these details are in the event of<br />
an emergency.”<br />
Initial users are from schools and colleges,<br />
but the system is available for free to<br />
all NHS staff and 1 million numbers will<br />
be made available for free to charitable<br />
organisations for the first year. Auxilium<br />
Systems are also currently working with<br />
a range of other stakeholders from the<br />
NHS, private medical service providers<br />
and companies in order to roll out the<br />
system on a nationwide, and eventually,<br />
international scale. As well as SCAS,<br />
Auxilium Systems are seeking to work with<br />
paramedic providers from both the private<br />
and charitable sectors, as well as Account-<br />
Holder-groups from all branches of industry<br />
and walks of life.<br />
How can I buy an Auxilium<br />
Account & Number?<br />
You can buy them via a Purchasing<br />
Organisation, such as a school or<br />
company, or directly from Auxilium<br />
Systems. You will be sent a link by<br />
email to your new account so you<br />
can set a password, enter your data<br />
and select who can view your data as<br />
an Authorised Reader.<br />
How secure is Auxilium Systems?<br />
Security is of paramount importance<br />
and the system provides the same levels of<br />
security used by financial systems. All activity<br />
on your account is recorded and displayed,<br />
with email notifications if your account<br />
is viewed by an Authorised Reader or<br />
Emergency Service.<br />
How do I display my Auxilium<br />
Number?<br />
In many situations the Auxilium Number<br />
will be integrated with items you currently<br />
carry, such as work ID cards, or pupil lists for<br />
school trips. We have a website where you<br />
can download an image with your Auxilium<br />
Number and logo which can used to create<br />
a sticker or key-ring etc. via many providers.<br />
How much does it cost?<br />
For an individual Auxilium Account the cost<br />
is £1 per year, but if bought via a Purchasing<br />
Organisation the cost will depend on the<br />
number of numbers purchased. The cost of<br />
being an Authorised Reader depends on the<br />
size of the organization.<br />
What if the Account Holder<br />
is a child?<br />
It is a requirement to provide your date of<br />
birth, if you are under 18 you will need to<br />
get parental consent. Consent may also be<br />
required for other vulnerable people.<br />
To find out more contact<br />
Grant Moreton or Chris Rowe:<br />
Tel: 01865 338020<br />
Website: www.auxsys.uk<br />
Email: info@auxsys.uk<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Winter 2014 | <strong>Ambulance</strong>today3 71
Mobile technology is<br />
playing an ever more<br />
central role in the<br />
emergency services today<br />
and in some cases can<br />
enhance the performance<br />
of the emergency<br />
professional. Paramedics<br />
need to be able to rely on<br />
technology to help them<br />
seamlessly attend patient<br />
needs, access information,<br />
record Electronic Patient<br />
Report Forms, and send<br />
and receive data, transfer<br />
diagnosis and other critical<br />
details to their destination<br />
hospital in any condition,<br />
and from any location.<br />
Services like Scottish <strong>Ambulance</strong><br />
Service (SAS) are already using<br />
rugged devices from the global<br />
designer and manufacturer of<br />
rugged mobile devices, Getac,<br />
designs devices specifically for<br />
critical field performance.<br />
Focus on Mobile Technology<br />
Mobile technology<br />
when using gloves or if it’s wet,<br />
or with gloves and styluses. For<br />
added security, the laptop also<br />
offers multi-factor authentication<br />
as well as capacitive fingerprint<br />
touch technology.<br />
It is resistant to dust and water<br />
ingress, three foot drops, plus<br />
it has features that support<br />
ambulance work, such as a hotswappable<br />
battery, giving more<br />
than enough battery to support<br />
a full day’s shift. The laptop<br />
has the footprint of a business<br />
notebook but with the features<br />
of a full-rugged device, providing<br />
a combination of design,<br />
performance and versatility.<br />
Getac has just launched its latest<br />
laptop, the S410, a semi-rugged<br />
device which includes a number<br />
of features that allow emergency<br />
crews to focus on mission-critical<br />
tasks, without worrying about<br />
reliability and performance.<br />
The S410 provides the latest<br />
technologies, processors<br />
and connectivity features for<br />
improved RF coexistence<br />
and comes complete with<br />
Windows 10 support for faster<br />
and more reliable data speeds.<br />
Getac’s LumiBond technology<br />
provides a high-visibility, sunlightreadable<br />
touchscreen that works<br />
The S410 offers the<br />
functionality and reliability that<br />
the emergency services can<br />
depend upon. Tested, reliable,<br />
dependable, empowering<br />
medical professionals can do<br />
what they are trained to: save<br />
human lives.<br />
If you would like to discuss<br />
any aspect of your rugged<br />
computing solution<br />
requirements, call:<br />
01952 207 221<br />
e-mail:<br />
Sales-Getac-UK@getac.com<br />
or visit:<br />
www.getac.co.uk<br />
72 Spring 2016 | <strong>Ambulance</strong>today
Thijs Gras’ Letter from Amsterdam<br />
Isn’t it Time that Patients Take Responsibility as Well?<br />
Below our thoughtful and thought-provoking Dutch correspondent, Thijs Gras, explains the high level<br />
of legal responsibility for the patient assumed by Dutch ambulance nurses every time they go on-shift.<br />
He also asks whether or not now is the time we should finally also make patients legally responsible for<br />
co-operating with the ambulance nurse or paramedic so they can actually provide them with the high<br />
levels of patient-care that they rightly expect… but without harassment or interference!<br />
In our work we should always strive for the<br />
best in caring for a patient. This is pretty<br />
obvious - so obvious that it has almost<br />
become a hollow sentence. We know<br />
that in practice there is tension, especially<br />
when patients’ interests and colleagues’<br />
interests are conflicting. For example, a<br />
delay of several seconds when one takes<br />
over the call of another ambulance in order<br />
to prevent them doing overtime. Will the<br />
patient notice this? No. Will he or she suffer<br />
damage from this? I would say ‘no’ to this<br />
too. Maybe those seconds make it possible<br />
to take a crossing more smoothly so you<br />
make up for it.<br />
More serious are the cases where the team<br />
disagrees about how to handle a case.<br />
Luckily this is not very common. We all<br />
know we should not discuss these things in<br />
front of a patient. In our Dutch system we<br />
have a nurse and a driver, so it is clear who<br />
is medically responsible and whose decision<br />
in patient care is final.<br />
Judicially, the patient has a lot of power in<br />
our country. We are obliged to inform the<br />
patient about what we are going to do and<br />
in the end the patient decides if he is treated<br />
or transported and he or she can even<br />
indicate the hospital where he or she wants<br />
to go to. Of course there are some limits,<br />
for example because that hospital lacks the<br />
facilities or is too far away.<br />
We respect people who have indicated that<br />
they do not want to be resuscitated. These<br />
always present precarious situations and in<br />
those cases our family doctor system really<br />
helps. Patients have spoken beforehand<br />
to their doctor who generally knows the<br />
situation well and can safely tell us to stop<br />
the resuscitation attempt. We also refrain<br />
from setting IV’s if a patient really opposes<br />
it even though it deprives him or her from<br />
effective analgesia.<br />
In quite a number of cases we just advise<br />
the patients and we do not transport them<br />
to the hospital. This happens in about 25-<br />
30% of cases and this percentage is rising.<br />
The cause of this is still not clear: do people<br />
call more often? Is this<br />
due to the use of triage<br />
systems in the control<br />
room?<br />
There are a few<br />
possibilities: we were<br />
really not necessary at<br />
all (for example a young<br />
girl with abdominal pain<br />
due to her periods), we<br />
may give treatment on<br />
the scene (reviving a<br />
diabetic with glucose),<br />
we may advise people<br />
to call or visit their<br />
family doctor or we<br />
may advise them to<br />
go to the hospital with their own means of<br />
transport.<br />
In all of these cases, legally we are on thin<br />
ice because we were the last medical<br />
professionals to have seen the patient<br />
and until the next professional makes<br />
contact with the patient; this means we are<br />
responsible.<br />
But let us not only talk about the patients’<br />
rights, but also about his duties. I think<br />
more attention is needed on this aspect<br />
of patient care. First of all the patient is<br />
obliged to let us help him or her. This is<br />
sometimes quite tricky with people under<br />
the influence of alcohol, drugs or mental<br />
disorders. Then it would certainly help if he<br />
or she is polite to us. We do not deserve<br />
swearing and cursing while we help<br />
someone.<br />
And then there is the following of our<br />
advice. Who is to blame when we<br />
instructed a non-drunken, well behaved<br />
person to go to the A&E department<br />
himself and he does not do this but suffers<br />
from damage as a result? I would say it is<br />
not the ambulance crew. Who is to blame<br />
when the control room instructed a caller<br />
to call his family doctor, but he decides<br />
to wait and gets into trouble because an<br />
inflammation that could have been tackled<br />
earlier now gets the chance to do more<br />
harm? I would say it is not the control room<br />
dispatcher, though legally (according to<br />
Dutch laws) he is.<br />
It is time to write in the law something<br />
about patient duties. These involve not<br />
only behaviour, but also listening well to<br />
ambulance personnel and doing something<br />
with the advice given. If the patient refuses<br />
this, that is his or her own decision and<br />
it is his or her responsibility. For with<br />
rights come duties, with power comes<br />
responsibility. That goes for us ambulance<br />
people, but also for patients. If the doctor<br />
says you should stop smoking and you<br />
refuse this, your next heart attack cannot<br />
be blamed on the doctor.<br />
Tell Thijs what you think about this<br />
article by emailing him at:<br />
thijsgras@upcmail.nl<br />
This edition of <strong>Ambulance</strong> Today goes out to all 25 Dutch <strong>Ambulance</strong> Regions courtesy of Procentrum<br />
PROCENTRUM - LEARN TO FEEL THE DRIVE www.procentrum.eu<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
73 3
Intelligent Dispatch Solution<br />
• Easy integration<br />
• System status management<br />
• Workflow automation<br />
• Mobility<br />
• Voice communication<br />
TM<br />
IDS<br />
Meet us at EMS2016<br />
Find out more: www.logisids.com
Focus on <strong>Ambulance</strong> Leadership Forum 2016<br />
LEADERSHIP THE KEY AT ALF 2016<br />
A sense of optimism at a time of great challenges for the urgent and emergency care system merged<br />
with the resounding message that UK NHS ambulance services will need stronger leadership than ever<br />
to survive and thrive in the future, were two of the key themes to emerge from the highly successful<br />
<strong>Ambulance</strong> Leadership Forum (ALF) 2016 held in February.<br />
The event - produced annually by the<br />
Association of <strong>Ambulance</strong> Chief Executives<br />
(AACE) - is now the major place for senior<br />
ambulance staff and their colleagues in<br />
industry and from across the wider NHS<br />
and academic landscapes to meet, network<br />
and discuss the topics that are topping the<br />
agenda for today’s UK ambulance service<br />
leaders.<br />
ALF 2016 was held in Leicester and<br />
attracted over two hundred delegates<br />
over the two days, drawn from all UK<br />
NHS ambulance services and their key<br />
partners from across the health sector. The<br />
first day saw a busy series of conference<br />
presentations that sparked some lively<br />
debates across the floor.<br />
Chair of the conference – award-winning<br />
BBC and Channel 4 journalist Liz MacKean<br />
- was able to persuade the participants to<br />
provide insight and share knowledge and<br />
ideas on a range of ambulance management<br />
topics.<br />
Never far from the debate, though, was the<br />
spectre of the unprecedented and growing<br />
demand for ambulance services, combined<br />
with the stark reality of the genuine<br />
pressures being felt throughout the whole<br />
urgent and emergency care system.<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
Prof. Paresh Wankhade, one of the main speakers.<br />
Professor Keith Willet discussed this in detail<br />
and outlined what NHS England are doing<br />
to combat these issues, while simultaneously<br />
urging ambulance leaders to be brave and<br />
to adopt innovative approaches to managing<br />
their resources.<br />
Privately some audience members may<br />
have been forgiven for wondering how<br />
much more they could do and how much<br />
faster they could go to implement changes,<br />
although the mood in the room remained<br />
upbeat and Professor Willet was, as always, a<br />
most welcome and informative speaker.<br />
Regrettably, the Secretary of State Jeremy<br />
Hunt was a last minute cancellation and the<br />
audience was instead played a recorded<br />
message from Lord Prior of Brampton,<br />
Parliamentary Under Secretary of State for<br />
NHS Productivity (Minister responsible for<br />
Urgent and Emergency Care) who thanked<br />
ambulance services for the hard work being<br />
done to continue to save lives and treat<br />
patients in such challenging times.<br />
The evening saw a magnificent gala<br />
dinner - kindly sponsored by the ALF<br />
AACE Chair Anthony Marsh thanks outgoing<br />
NWAS Chief Bob Williams<br />
2016 main sponsor Ferno ® - where the<br />
AACE Outstanding Service Awards were<br />
presented to high performing staff from<br />
across England.<br />
Two other features of the evening were a<br />
charity auction that raised over £1,000 in aid<br />
of The <strong>Ambulance</strong> Services Charity (TASC<br />
- www.theAsc.org.uk) and an amusing<br />
and light-hearted send-off by AACE chair<br />
Anthony Marsh for North West <strong>Ambulance</strong><br />
Service Chief Executive Officer Bob Williams<br />
who is retiring after 36 years in the NHS.<br />
Day two provided a series of workshops<br />
where the topics were as follows: ‘Our<br />
Workforce,’ ‘Technological and Digital<br />
Enablement’ and ‘Vanguards and Innovation.’<br />
These workshops sparked more healthy<br />
debates and delegates left with new ideas<br />
and renewed vigour to take back to their<br />
trusts. The event finished with meetings of<br />
the national groups.<br />
A full report on ALF2016 and the<br />
full workshop presentation slides are<br />
available at:<br />
AACE.org.uk/ambulance-leadershipforum<br />
75 3
Exclusive Interview with IAED Founder Dr Jeff Clawson<br />
New European EMS Network will<br />
Contribute to Global EMS Improvement<br />
<strong>Ambulance</strong> Today’s Joe Smith quizzed Dr. Jeff Clawson, co-founder of the International<br />
Academies of Emergency Dispatch (IAED), and inventor of the Priority Dispatch System.<br />
Recognised globally as the Father of modern dispatch, Dr. Clawson offers his views on<br />
global partnership in EMS development and provides a fascinating insight into the<br />
amazing growth of Priority Dispatch Protocols since its formation in the late 1970s.<br />
JS: What led you to develop the<br />
first dispatch protocol for the North<br />
American EMD Network in 1978?<br />
JC: Priority Dispatch Protocols introduced<br />
into the public safety communications<br />
world in 1978 were designed for a specific<br />
purpose: to ensure that the right thing is<br />
sent to the right place, in the right way,<br />
at the right time and the right things are<br />
done over the phone until the troops<br />
arrive. This is the most important reason<br />
these protocols exist. The prioritisation of<br />
response and the orderliness of treatment is<br />
the true value of such protocol “plans.” Preplanning<br />
of emergency response is essential<br />
science in a healthcare environment that<br />
stresses efficiency of care, and the medical<br />
protocols provide a precise and detailed<br />
plan for the study of a biomedical problem<br />
or for a regimen of care.<br />
JS: When you created the North<br />
American EMD Network did you<br />
envisage the protocols for prearrival<br />
instructions for dispatchers<br />
as a purely regional EMS innovation<br />
or did you already anticipate its<br />
adoption by EMS systems globally?<br />
JC: A unified protocol model for all to<br />
use was always the goal of the Medical<br />
Priority Dispatch System (MPDS ® ), now<br />
in Version 13.0, and the same can be said<br />
of the Police Priority Dispatch System <br />
(PPDS ® ) and the Fire Priority Dispatch<br />
System (FPDS ® ), now in Versions 5.0 and<br />
6.1, respectively. A unified system of a single<br />
core protocol, modified through a scientific<br />
method process and routinely distributed<br />
to everyone ensures that every protocol<br />
benefits from the experience and research<br />
of the other users. In the same way the<br />
heart and resuscitation councils maintain<br />
a core protocol for CPR, BLS, and ACLS,<br />
the College of Fellows, a standards setting<br />
body within the International Academies<br />
of Emergency Medical Dispatch ® (IAED ),<br />
provides stability and reliability to dispatch<br />
worldwide. Importantly, the Academies<br />
continue to be a strong professional voice<br />
for emergency dispatchers and are taking<br />
an active role in the policies and politics of<br />
public safety dispatching.<br />
JS: Can you tell us more about how<br />
you developed your original priority<br />
dispatch pre-arrival instructions into<br />
three separate protocols for Medical,<br />
Fire and Police services?<br />
JC: The three sets of protocols—medical,<br />
fire, and police are based upon the same<br />
time-proven methods developed over<br />
30 years of research, testing, and quality<br />
assurance. These protocols were initiated<br />
by pre-establishing for Fire and Police,<br />
the Academy Councils of Standards, and<br />
Curriculum Boards, populated with world<br />
experts in those disciplines. Each adhered<br />
to the protocol structure objectives that we<br />
learned the hard way over many years in<br />
Medical. As with any protocols, version 1.0<br />
is simply a starting point of the evolutionary<br />
process, and with a scientific method-based<br />
process, they are guaranteed to evolve and<br />
improve if that process is maintained and<br />
supported.<br />
The FPDS started in 2000 and is now<br />
at version 6.1, while the PPDS began<br />
development in 2001 and is at version 5.0.<br />
Police is the most divergent of the three, as<br />
it requires early identification of suspect and<br />
vehicle descriptors, and quick deployment<br />
of mobile police patrollers, which puts<br />
them at significant risk. The provision of<br />
dispatch data to the mobile data computers<br />
in the cars demands a lot of special sorting,<br />
filtering, and other human engineering<br />
factors which are not as essential in the<br />
Medical and Fire disciplines. The fluidity of<br />
the events is also a differentiating factor<br />
in Police that is challenging to account<br />
accurately and safely for. The Academy<br />
more recently added a 4th pillar—ECNS <br />
(Emergency Communication Nurse<br />
System ) protocols, training, certification,<br />
and accreditation—just like the other<br />
disciplines. It is just starting to flower in a<br />
world with an ever-increasing volume of<br />
999 calls.<br />
Visit our website at www.emergencydispatch.org<br />
JS: How exactly did North American<br />
EMD grow into IAED?<br />
JC: The Network was an initial attempt to<br />
get like minds in dispatch to work together<br />
as a forum but wasn’t envisioned properly<br />
for what needed to be done, hence version<br />
2 – the Academy. Since the Academy was<br />
first formed in 1988, it was the intent<br />
of the founders to nurture and develop<br />
the organisation into an internationally<br />
recognised and standard-setting scientific<br />
and academic institution. We are an<br />
international forum for discussing standards<br />
and issues relating to medical protocol<br />
and one of several international EMS<br />
organisations dedicated to improving<br />
patient care and maximising the efficiency of<br />
EMS worldwide.<br />
JS: Since the formation of IAED<br />
how rapidly has it grown? What<br />
is its reach globally? How many<br />
countries does it reach and how<br />
many emergency service personnel<br />
globally use MPDS dispatch<br />
protocols?<br />
JC: Founded almost 30 years ago, IAED is<br />
the world’s foremost standard-setting and<br />
certification organisation for emergency<br />
communication centres with over 57,000<br />
members in 45 countries. More than<br />
3,400 communication centres use IAED’s<br />
76 Spring 2016 | <strong>Ambulance</strong>today
Exclusive Interview with IAED Founder Dr Jeff Clawson<br />
protocols and training—translated into 17<br />
languages/dialects—for medical, fire, and<br />
police dispatching. Of those, nearly 200 have<br />
become Accredited Centres of Excellence<br />
(ACE), which ensures the intent and output<br />
of the protocols are realised as designed.<br />
JS: Can you outline a few of the<br />
improvements to EMS globally that<br />
IAED has helped to bring about?<br />
JC: As medical dispatch developed, several<br />
things have become ingrained in the<br />
program and the universality of Protocol is<br />
readily apparent globally. First, emergency<br />
medical dispatch has evolved from an<br />
attempt to stop response abuse by not<br />
sending EMS when it’s not needed, to a<br />
program that prioritises response. Secondly,<br />
emergency medical dispatch has become<br />
properly viewed as part of the medical<br />
care system and as the vital first step in a<br />
multi-step process of emergency medical<br />
care. Thirdly, emergency medical dispatch<br />
has moved the dispatch centre from a point<br />
of EMS control to the earliest point of EMS<br />
assistance. Finally, the dispatcher not only<br />
assists the public, but the EMS provider as<br />
well. Studies have shown that emergency<br />
medical dispatchers, medically controlled<br />
and trained in an internationally recognised<br />
dispatcher triage system, are able to provide<br />
medical triage to incoming emergency<br />
medical calls with minimal error for undertriage<br />
of ALS runs and high selectivity for<br />
non-emergency situations. The assistance<br />
has been explicit in first founding the use<br />
of scripted PAIs throughout the history of<br />
emergency dispatch.<br />
JS: What is the importance of the<br />
partnership between good quality<br />
communications and ambulance<br />
providers in different world regions?<br />
JC: Good quality communications directly<br />
assists EMS organisations in optimising<br />
their resource use, exploring data volumes<br />
and data types, and achieving true insight<br />
and forward vision to improve operational<br />
efficiency. Partnership emphasises a<br />
commitment to encourage consistent<br />
high-quality prehospital care. For example,<br />
a major advantage is the coordination<br />
allowing dispatchers to account for ALL<br />
time intervals from the time an emergency<br />
call is answered at the emergency<br />
communication centre until the units<br />
are back in service. This can only be<br />
accomplished in the spirit of co-operation<br />
and shared vision among various types of<br />
public safety agencies poised to explore<br />
new ideas in the science of emergency<br />
medical dispatch.<br />
JS: Rightly or wrongly, it’s often<br />
claimed that despite it’s great<br />
aptitude for innovation, America is a<br />
country that is too inward-focused.<br />
Based on IAED’s global project<br />
work, do you feel that this is a fair<br />
statement in relation to EMS?<br />
JC: Considering the history of EMS<br />
and the EMS movement in the US, EMS<br />
systems overseas will unavoidably contain<br />
components in common with those in<br />
the US. And EMS, as the science of human<br />
beings in the need of emergency medical<br />
assistance, has many similarities. The US<br />
has a leadership obligation to point out<br />
problems and find the means for their<br />
actual solution. At the same time, we have<br />
to understand the limited applicability of<br />
Western systems to culturally diverse<br />
regions and, with that in mind, develop<br />
solutions in EMS that recognise a number<br />
of components universally required in<br />
every system. In other words, a global<br />
program must recognise basic prehospital<br />
elements that can be integrated into a<br />
universal system beneficial to the total<br />
prehospital care system. A unified (same<br />
core everywhere) protocol system with<br />
approved cultural modifications has been<br />
the clearly successful solution to this issue.<br />
JS: One of the founders of the<br />
EMS2016 Congress and the soon-tobe-launched<br />
European EMS Leaders’<br />
Network, is IAED’s (and <strong>Ambulance</strong><br />
Today’s) own Jerry Overton. Does<br />
Jerry’s involvement mean that IAED<br />
views the EMS Leadership Network<br />
as an opportunity for working<br />
even more closely with European<br />
<strong>Ambulance</strong> Workers?<br />
JC: Of course, particularly since the<br />
EMS Leaders’ Network was developed<br />
to produce and distribute independent<br />
research and analysis, and provide an<br />
international platform with a strong<br />
emphasis on creating global EMS solutions.<br />
Jerry Overton is a natural in the European<br />
EMS Leaders’ Network, considering his<br />
professional background contributing to<br />
his expertise in EMS system design and<br />
deployment strategies. Arguably, he is the<br />
world expert in the science of System<br />
Status Management, sometimes referred to<br />
as fluid deployment. The IAED continues<br />
to add, involve, and utilise European<br />
knowledgeable experts.<br />
JS: And finally Dr. Clawson, do<br />
you have your own vision in terms<br />
of the improvements that could<br />
be achieved if EMS leaders such<br />
as yourself could work with the<br />
European EMS Leadership Network<br />
to bring about innovations in the<br />
areas of dispatch, frontline clinical<br />
care, community medicine, and<br />
operational delivery?<br />
JC: This is an opportunity to discuss<br />
and find international solutions to critical<br />
issues in emergency response through the<br />
cooperation of EMS experts on the global<br />
stage. The EMS Leadership Network will<br />
be in the position to influence future EMS<br />
practice trends, prehospital research, and<br />
to advance quality leadership through the<br />
generations. The international scope of the<br />
Academy has fostered significant movement<br />
in the scientific evolution of dispatch<br />
stands—in protocol, curriculum, logic<br />
systems, quality improvement, and dispatch<br />
centre accreditation excellence—assuring<br />
the protocols are used as designed to get<br />
their full, envisioned effect.<br />
For more information contact the<br />
Academy on:<br />
Telephone: 0808 234 4896<br />
Or visit the IAED website at:<br />
www.emergencydispatch.org<br />
Visit our website at www.emergencydispatch.org<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
77 3
Purchase with confidence from SP Services in<br />
the knowledge that you are receiving the best<br />
value for money.<br />
Don’t leave it to chance, buy from one of<br />
the largest and long established suppliers of<br />
emergency medical supplies in the UK. You can<br />
rely on us to supply everything you need in an<br />
emergency.<br />
Benefits of SP Services<br />
• Extensive product choice<br />
• Innovative designs<br />
• Competitive prices<br />
• Dedicated sales & customer support<br />
• Prompt delivery<br />
• Leading healthcare brands<br />
• Bespoke products to your specification<br />
For more information call 01952 288 999<br />
or visit www.spservices.co.uk
Focus on <strong>Ambulance</strong> Innovation<br />
“Watson,<br />
I presume?”<br />
<strong>Ambulance</strong><br />
Care<br />
After the<br />
Fourth<br />
Industrial<br />
Revolution<br />
By Jaap Hatenboer,<br />
Strategy & Innovation Manager,<br />
UMCG <strong>Ambulance</strong>zorg,<br />
Netherlands<br />
The quote: “I know of no way of judging of the future but by the past” is from Patrick Henry. Patrick was<br />
an American attorney, planter and politician who became known as an orator during the movement for<br />
independence in Virginia in the 1770s. I suppose he meant that we are walking backwards into the future.<br />
We judge new developments using our past experiences.<br />
The title of this article is just an<br />
illustration of this fact. Interpreting<br />
the title completely depends on your<br />
past experiences. You might be a<br />
Harry Potter or a Sherlock Holmes<br />
fan. You might like expeditions to the<br />
heart of Africa. But even if you are<br />
a Sherlock Holmes fan, it matters<br />
which version you prefer or which<br />
version you recently watched. Is it<br />
Doctor John Watson or Doctor Joan<br />
Watson, is this about London or New<br />
York?... and the list goes on if you are<br />
also interested in the actors; or you<br />
might be interested in other issues<br />
and for you there is only one Watson<br />
and his first name is Paul.<br />
The simple fact is that we struggle with the<br />
future and we judge the present based on<br />
past experience combined with our age<br />
group, job, hobbies etc. Adding three letters<br />
the title becomes “IBM Watson, I presume”.<br />
Just adding IBM makes all the difference.<br />
Only then most of us would understand<br />
that this article might be about the IBM<br />
Analytics. Well it isn’t and it is.<br />
This article is an attempt to understand<br />
the relevance of the fourth industrial<br />
revolution for ambulance care. This<br />
revolution is sending some very unsettling<br />
shockwaves through society. For those<br />
who have missed it, the fourth industrial<br />
revolution is a collective term embracing<br />
a number of automation, data exchange<br />
and manufacturing technologies (https://<br />
en.wikipedia.org/wiki/Industry_4.0 ). So this<br />
is about Google, Apple, Tesla, Olaeris, Uber,<br />
Facebook, EdX, PrecisionHawk, DNV ReVolt,<br />
Precision agriculture and the list goes on<br />
and on. The fourth revolution might be on<br />
a collision course with our present way of<br />
working.<br />
Trekkies will probably remember “We are<br />
the Borg, resistance is futile, you will be<br />
assimilated.” Maybe this is the right moment<br />
to get used to this version “The fourth<br />
industrial revolution has arrived, resistance<br />
is …” Well you already know the rest. So<br />
how might this impact on ambulance care,<br />
will it actually be the end of ambulance care<br />
as we know it? Here are some initial ideas<br />
about how it might work out.<br />
Anyone who follows the car industry knows<br />
that Tesla launched some really disturbing<br />
new functionalities. You need to understand<br />
that Tesla vehicles have a lot in common<br />
with iPads and get new functionalities by<br />
software updates. The 7 series updates<br />
introduced some useful functionalities that<br />
point at the fact that vehicles increasingly<br />
will become (semi) autonomous and<br />
interconnected.<br />
Picture left:<br />
https://commons.wikimedia.org/wiki/<br />
File:Industry_4.0.png<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
79 3
Sanondaf provides a touch-less disinfection system that<br />
kills 99.99% of harmful bacteria, viruses, fungi and mould.<br />
Delivered using our innovative, leading edge hydrogen<br />
peroxide fogging and electrostatic spraying system, and<br />
combined with our patented and approved disinfectants,<br />
Sanochem is 100% environmentally friendly, non-corrosive,<br />
and poses no threat to humans, animals or plants.<br />
We specialise in the treatment of vehicles and confined<br />
spaces. Our treatment process is quick and a vehicle is<br />
readily available for use again within 30 minutes, ensuring<br />
minimum downtime.<br />
Effectively eradicates over 280 pathogens including:<br />
• MRSA<br />
• Norovirus<br />
• E-Coli<br />
• H1N1<br />
• C-Diff<br />
• Salmonella<br />
“IT’S NOT WHAT YOU SPRAY...<br />
BUT HOW YOU SPRAY IT”<br />
Sanondaf is also completely effective against high risk pathogens such as:<br />
• Hepatitis<br />
• Legionella<br />
• HIV<br />
• Polio<br />
• Ebola<br />
For more information please visit:<br />
www.sanondaf.co.uk<br />
or contact Stuart White via<br />
stuartwhite@sanondaf.co.uk<br />
or +44 (0)1236 702028<br />
+44 (0)7971 220 294
Focus on <strong>Ambulance</strong> Innovation<br />
Picture: https://www.teslamotors.com/<br />
en_GB/blog/your-autopilot-has-arrived<br />
So why still use lights and sirens if every<br />
other vehicle recognizes you as a high<br />
priority vehicle? There is already a platform<br />
available that matches location data of<br />
emergency vehicles with connected traffic<br />
apps. And by the way did you hear that<br />
Google has a US patent on an <strong>Ambulance</strong><br />
drone system? Maybe the Sky is the limit,<br />
but delivering emergency care by air will<br />
become a lot cheaper.<br />
Of course you are all familiar with Rolls<br />
Royce as a world renowned engine<br />
manufacturer. You might not have noticed<br />
that they have developed a real-time<br />
intelligent Engine Health Monitoring<br />
System. That way they keep track of the<br />
performance and health of thousands of<br />
engines flying around the world. This is all<br />
about connectivity, sensors and an awful<br />
lot of Big data. And it will also be available<br />
for everyday use in ambulances. The end<br />
result will probably be a highly connected<br />
ambulance full of sensors and IoT (Internet<br />
of Things); equipment that is monitored by<br />
fleet management and logistics.<br />
Meet YFAS - Your Friendly <strong>Ambulance</strong><br />
Station. Ever thought about an ambulance<br />
station that really takes care of you, adjusting<br />
Picture: http://www.boschpresse.de/presseforum/details.<br />
htm?txtID=6536&locale=en<br />
heating, sunshades and lights, cleaning the<br />
station, running errands, adjusting your<br />
chair and putting on your favourite music?<br />
With the smart homes concept it’s not that<br />
far-fetched. Or don’t you have an automatic<br />
vacuum cleaner at home that also acts as<br />
burglar and smoke alarm?<br />
Now you probably say, I am never at the<br />
station. It’s all driving and patient care. So<br />
let’s meet YFA, Your Friendly <strong>Ambulance</strong><br />
that is doing the same as Your Friendly<br />
<strong>Ambulance</strong> Station but now mobile. It even<br />
gives you an extra hand, called (Boston<br />
Dynamics) Spot that carries your bags and<br />
equipment.<br />
Entering the home of the patient you might<br />
already have a lot of information regarding<br />
the patient and Spot is of course carrying<br />
your Telehealth equipment and your mobile<br />
blood analysis kit. The mobile Stroke Unit<br />
is kept in the ambulance, but that has also<br />
turned into a small piece of equipment. I<br />
personally don’t think you can expect the<br />
holographic doctor soon, but you should be<br />
connected with other health professionals.<br />
Just have a look at the Telehealth system in<br />
Aachen that has been fully operational on all<br />
ambulances since 2014.<br />
Renewable energy is not for the fainthearted.<br />
It will arrive in due course and it<br />
will revolutionize the way we use energy<br />
in our fleet. Maybe it will first arrive as a<br />
hybrid, but it will at the end take over from<br />
fossil fuels. With the increasing waiting times<br />
at A&E you might not even need a fast<br />
charger to recharge your batteries. Sorry for<br />
the joke, but in E-ambulances it is all about<br />
battery charging strategies. The Tesla P90D<br />
convinced us all that lack of acceleration is<br />
not an issue.<br />
How can we best assimilate all these new<br />
possibilities? I think the approach is straightforward.<br />
We need to accept and assimilate<br />
new possibilities. And above all we need<br />
to do it together. There is no way a single<br />
organization can handle the speed and<br />
intensity of change on their own. Teamwork<br />
becomes the essential new capability of any<br />
ambulance organization. So if you want to<br />
avoid ending up as the proverbial ball in the<br />
soccer game, your only option is to act as a<br />
team player.<br />
Maybe we should all read the book Teams<br />
of Teams to better understand what lies in<br />
front of us. And for those who might think<br />
there is still plenty of time, I would strongly<br />
advise you to NOT watch the Ubulance<br />
sketch and also NOT read the article “If<br />
Uber Is Faster than an <strong>Ambulance</strong>, What’s<br />
Next for the <strong>Ambulance</strong> Industry?” by<br />
Susanna J. Smith.<br />
Tell Jaap what you think or ask for<br />
more information by emailing him<br />
at: j.hatenboer@rav.nl<br />
Want to stay in touch with global EMS developments?<br />
Get your own copy of <strong>Ambulance</strong> Today<br />
Order your own copy of <strong>Ambulance</strong> Today and we will mail you out your own copy four times a Year<br />
to the address of your choice anywhere in the world<br />
Our One Year subscription package guarantees you receive 4 consecutive quarterly editions and<br />
includes the cost of postage & packaging<br />
Sterling – £56 (within UK) – £66 (outside UK)<br />
Euros– €80 (anywhere in world)<br />
USD– $90 (anywhere in world)<br />
To make your order please visit:<br />
www.ambulancetoday.co.uk and go to: ‘subscriptions’<br />
Subscriptions can be accepted via cheques, postal orders or bank transfers made payable to:<br />
<strong>Ambulance</strong> Today Ltd<br />
For information on other payment options please either:<br />
Call: +44 (0) 151 703 0598 Or email: subscriptions@ambulancetoday.co.uk<br />
<strong>Ambulance</strong><br />
Spring 2016 - Issue 1 | Volume 13<br />
TODAY<br />
The global magazine for all people involved in ambulance provision<br />
Now going out online globally to over 275,000<br />
ambulance workers in partnership with NAEMT, IAED and UNISON<br />
<strong>Ambulance</strong> History<br />
in the Making<br />
On May 30th EMS leaders from<br />
across Europe Will gather in<br />
Copenhagen for the first ever<br />
European EMS congress and to<br />
launch the New European EMS<br />
Leadership Network<br />
Will you be there?<br />
BOOK YOUR PLACE AT EMS 2016 IN COPENHAGEN AT: WWW.EMS2016.ORG<br />
This issue i supported by<br />
This special edition celebrates both momentous events<br />
TO RECEIVE AMBULANCE TODAY FREE OF CHARGE TO YOUR EMAIL BOX JUST VISIT:<br />
WWW.AMBULANCETODAY.CO.UK AND GO TO SUBSCRIPTIONS<br />
£0.00<br />
Unison Comment<br />
A<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
81 3
FOCUS on NAEMT President Chuck Kearns<br />
“I place great<br />
value on NAEMT<br />
partnering with EMS<br />
Professionals and<br />
Agencies from around<br />
the world.”<br />
NAEMT President Chuck Kearns answers questions from <strong>Ambulance</strong> Today’s Joe Smith on<br />
what America’s leading ambulance organisation is currently doing to ensure they maintain<br />
positive links with other ambulance providers globally.<br />
JS: As President of the USA’s<br />
largest and most important body<br />
representing EMS workers, how<br />
much value do you place on working<br />
in partnership with other EMS<br />
communities from around the world?<br />
CK: I place great value in NAEMT<br />
partnering with EMS Professionals and<br />
Agencies around the world. Our training<br />
network is now established in 60 countries.<br />
We continue to reach out to EMS<br />
professionals in other countries to expand<br />
our continuing medical education programs.<br />
JS: Can you tell us more about<br />
NAEMT membership globally? I<br />
understand that your organisation<br />
has active members spread across<br />
the globe; what kind of support<br />
services do you provide for your<br />
overseas members?<br />
CK: We have 12,615 international<br />
members in 56 countries outside of the US.<br />
Here are some of the benefits that are<br />
included with NAEMT international<br />
membership:<br />
• $125 discount on registration to attend<br />
EMS World Expo<br />
• Free online CE credits and discounts on<br />
several online CE services<br />
• A voucher for up to $15 on any NAEMT<br />
course<br />
• Major discounts off rental cars from Avis,<br />
Budget and Hertz<br />
• Free on-line subscription to <strong>Ambulance</strong><br />
Today magazine, free subscription<br />
to EMS World magazine and discounts<br />
on subscriptions to many other EMS<br />
publications.<br />
• Discounts on EMS products and services<br />
• Up to 80% discount on Office Depot<br />
Office Max products<br />
• 20% discount at Wyndham Hotels<br />
JS: Much of NAEMT’s membership<br />
support focuses on education<br />
programmes. Are these influenced<br />
to any degree by your strong working<br />
links with ambulance providers in<br />
Europe and other world regions?<br />
CK: The growth of these programmes<br />
in other countries is due in large part to<br />
strong working relationships with ambulance<br />
providers and educators in these other<br />
countries. We receive requests to form new<br />
overseas partnerships almost monthly.<br />
JS: Other than providing support<br />
to overseas members are there<br />
any other activities that NAEMT<br />
is involved in which are specifically<br />
aimed at developing innovation<br />
and/or best practice with other<br />
ambulance deliverers around the<br />
globe?<br />
CK: NAEMT holds an annual World<br />
Trauma Symposium in partnership with<br />
EMS World. 300-400 attendees participate<br />
in this event each year. It is the leading<br />
trauma event for the prehospital medical<br />
care profession. We are the global leader<br />
in continuing education for prehospital<br />
practitioners, with courses offered in 60<br />
countries.<br />
JS: Arguably one of the greatest<br />
challenges for NAEMT is influencing<br />
relevant healthcare legislation in<br />
a country where laws are set to a<br />
great degree on a state-by-state<br />
basis. This must make the task<br />
of influencing federal legislation<br />
particularly difficult. It’s clear that<br />
much of NAEMT’s success in the area<br />
of influencing relevant prehospital<br />
legislation comes from helping to<br />
educate elected officials on the<br />
anticipating impact of pending<br />
federal legislation on emergency<br />
and mobile healthcare through your<br />
annual ‘EMS On the Hill Day’ – is this<br />
a model for positively influencing<br />
prehospital healthcare legislation<br />
that you would recommend to the<br />
soon-to-be launched European<br />
EMS Leaders’ Network in terms of<br />
their potential ability to positively<br />
influence EC-wide prehospital<br />
legislation?<br />
CK: Absolutely! In my experience elected<br />
officials rarely have EMS background -<br />
probably because our modern industry<br />
is still pretty young. They must be<br />
educated about our concerns and asked<br />
for their help to pass beneficial laws and<br />
82 Spring 2016 | <strong>Ambulance</strong>today
FOCUS on NAEMT President Chuck Kearns<br />
regulations. A well-organized group of EMS<br />
Practitioners in dress uniforms, armed with<br />
good educational material goes a long<br />
way in building better understanding and<br />
supportive relationships.<br />
JS: In terms of clinical dispatch<br />
and operational standards, how do<br />
you feel that American ambulance<br />
services in general compare with<br />
their cousins across the pond?<br />
CK: I have been an IAEMD-certified<br />
Advanced Emergency Medical Dispatcher<br />
for 16 years. Dispatch services vary in their<br />
staffing and effectiveness in the US. Those<br />
with good funding and training who practice<br />
some kind of “priority dispatch” method<br />
with pre-arrival medical instructions are<br />
certainly as equally effective as those in any<br />
other country.<br />
On the operational side the US has some<br />
very high performing agencies. I also think<br />
European <strong>Ambulance</strong> Agencies are far ahead<br />
in the attention to safety practices that are<br />
ingrained in the workforce.<br />
JS: There’s a great deal happening<br />
across the USA currently in terms<br />
of positively reshaping prehospital<br />
care to create an additional role for<br />
ambulance services as deliverers<br />
of community medicine. Is this a<br />
development that you envisage<br />
growing across European EMS?<br />
CK: It seems a logical and natural<br />
evolution in our industry. I do see it<br />
expanding and think it provides a new<br />
career path for EMS Practitioners who no<br />
longer want to, or are becoming unable to<br />
lift cots any more. Expanding into Mobile<br />
Integrated Healthcare can provide needed<br />
health services in a community and add<br />
years to EMS Practitioners’ careers.<br />
JS: Can you think of any examples<br />
from your own long and distinguished<br />
career that highlight the benefits of<br />
global partnerships in EMS?<br />
CK: Oh yes. Sharing ideas, best practices<br />
and building relationships are all highlight<br />
examples for me. I’ve hosted <strong>Ambulance</strong><br />
leaders from London’s LAS, Queensland,<br />
Australia, Canada, Japan and Caribbean<br />
nations.<br />
To find out more about NAEMT<br />
visit: www.NAEMT.org<br />
We’re<br />
recruiting…<br />
• Paramedics<br />
• Pre-Hospital Nurses<br />
• IHCD Technicians<br />
• First Aiders minimum FPOSi and FREC L3<br />
for venues in London, Birmingham, Coventry and Manchester<br />
Casual positions working at some of the country’s best events<br />
Apply online at: staff.showmed.com<br />
0844 888 1323 for more details<br />
or email: admin@showmed.com<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
83
.emergencyuk.com | Hall 5 | NEC | Birmingham | 21-22 September 2016 | www.emergencyuk.com | Hall 5 | NEC | Birmingham | 21-22 September 2016 | www.emergencyuk.com | Hall 5<br />
Bringing the Emergency Services<br />
together to improve public safety<br />
A unique event for everyone who works in the emergency services<br />
• Network with like-minded emergency staff<br />
• Source new kit and save money<br />
• Meet the market leaders in emergency services products<br />
• Get updated on collaboration and multi-agency plans<br />
• See the newest products on the market<br />
• Gain CPD points from our free College of Paramedics workshops<br />
• Learn from past emergency situations at the free seminars<br />
• Get up to speed on UAV technology in the Drone Zone<br />
• Watch live water rescue demo's<br />
For more information visit www.emergencyuk.com.<br />
ESS - the only show for the entire spectrum of the Emergency Services<br />
www.emergencyuk.com<br />
Show supporters and sponsors include<br />
COLLEGE OF<br />
paramedics<br />
leading the development of the paramedic profession
|<br />
Focus on The <strong>Ambulance</strong> Services Charity<br />
<strong>Ambulance</strong> Leaders Support TASC<br />
An auction at the UK’s leading conference for senior ambulance personnel raised nearly £1,500<br />
for a Coventry-based charity.<br />
TASC, The <strong>Ambulance</strong> Services Charity,<br />
attended the 2016 <strong>Ambulance</strong> Leadership<br />
Forum (ALF) for the first time since they<br />
were formed last March.<br />
The UK-wide charity helps to provide<br />
vital advice and support services to both<br />
serving and retired ambulance staff and their<br />
families.<br />
TASC Chairman Cliff Randall, Trustees<br />
Roy Norris and Mick Webb, and Director<br />
of Support Services Jean Hayes attended<br />
the annual conference at the Hinckley<br />
Island Hotel for senior ambulance staff<br />
and their colleagues from the NHS and<br />
academic institutions to network and hear<br />
presentations about topics affecting the UK’s<br />
ambulance service leaders.<br />
Over 200 delegates attended the two-day<br />
event which included a gala dinner and<br />
charity auction with £1,385 raised for TASC<br />
from the generous guests.<br />
The charity obtained a number of prizes<br />
including two hospitality tickets for a future<br />
Wasps match at the Ricoh Arena, a Land<br />
Rover Tour and Experience Day for two<br />
guests from Jaguar Land Rover Community<br />
Relations, an iPad Mini featuring the brand<br />
new ‘iCPG’ 2016 <strong>Ambulance</strong> Clinical<br />
Practice Guidelines app generously donated<br />
by Class Professional Publishing, a limited<br />
edition aviation print from SWA Fine Art<br />
Publications and two limited edition Maglite<br />
torches from SP Services.<br />
The TASC team also signed-up a number<br />
of TASC supporters to continue raising the<br />
profile and funds for the UK’s only charity<br />
From the left, Jean Hayes, Roy Norris, Mik Webb and Cliff Randall from TASC at the 2016 <strong>Ambulance</strong><br />
Leadership Forum<br />
solely focused on those working in the<br />
ambulance industry.<br />
Cliff said: “There is no doubt this is a<br />
challenging time for ambulance personnel<br />
because of the demand on the service<br />
and the presentations at the conference<br />
certainly provided some lively debates.<br />
“Attending the <strong>Ambulance</strong> Leadership<br />
Forum was an ideal opportunity to spread<br />
the message further about our work among<br />
senior personnel in the ambulance sector as<br />
well as raise a significant amount of money<br />
to continue making a difference.<br />
“The proceeds from the auction will help<br />
TASC to provide grants for rehabilitation<br />
services to help those recovering from<br />
work-related injuries, long-term illnesses<br />
or surgery, provide support to help people<br />
suffering with stress and Post Traumatic<br />
Stress Disorder following traumatic<br />
incidents at work, and bereavement<br />
support.<br />
“We signed-up a number of TASC<br />
supporters during the conference including<br />
Dr Anthony Marsh, chief executive of West<br />
Midlands <strong>Ambulance</strong> Service, Ken Wenman,<br />
the chief executive of the South Western<br />
<strong>Ambulance</strong> Service NHS Foundation Trust<br />
and Hilary Pillin, who is a consultant in<br />
healthcare response.<br />
“Their backing, along with all our other<br />
supporters, is vital in ensuring we provide<br />
the support colleagues need in times of<br />
crisis, bereavement, severe difficulty or<br />
urgent need.”<br />
For information about becoming a<br />
TASC member or supporter, please<br />
visit: www.theAsc.org.uk<br />
You can also call +44 (0)2477 987<br />
922 or the free TASC Support Line<br />
on +44 (0)800 1032 999<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
85 3
Focus on the IPTS Concept <strong>Ambulance</strong><br />
FERNO’s IPTS<br />
Concept <strong>Ambulance</strong><br />
is Ready to Go Live<br />
By Jon Ellis, MD, Ferno UK<br />
We have been sowing the seed of the Integrated Patient Transport System for over two years. Starting<br />
with ACETECH Vehicle Intelligence, then iN∫X our integrated and transport loading system and finally<br />
iN∫TRAXX our modular <strong>Ambulance</strong> interior. Information such as fuel savings, safer driving standards<br />
and a simple protocol change, making it safer for the patient and easier for the Paramedic. The whole<br />
concept gives many other major benefits from reduced total vehicle weight, improving carbon footprint,<br />
easier make-ready and asset protection.<br />
But perhaps we should tell you more of the story…<br />
Joe Bourgraf, President & CEO - Ferno<br />
Group has always had big shoes to fill for<br />
what we call the FERNO FAMILY, a group<br />
of worldwide companies and a massive<br />
distributor network which is ever-growing<br />
and was started by his father, Elroy. Our<br />
beginnings stem from making COTS (we<br />
call them Stretcher Trolleys) to move dead<br />
or injured people but innovations such as<br />
the SCOOP®, the KED® and many more<br />
soon made us the global leader and EMS<br />
specialist. Developing better products has<br />
been instrumental in developing the EMS<br />
market and ambulance industry into what it<br />
is today. Post 9/11, the American government<br />
wanted companies like FERNO to make our<br />
rescue-heroes’ lives even safer, to further<br />
innovate and take an holistic approach to the<br />
symptoms of an unsafe world that we live in<br />
today.<br />
SafePak System, iN∫TRAXX Wall and equipment mounts<br />
Joe took that challenge and with some ideas<br />
and a team of global experts formed a<br />
think tank, they put a lot of ideas down and<br />
decided that the concept needed to be in<br />
three parts:<br />
1. Technology - areas of advanced<br />
communication, information and new ideas<br />
2. Medic - making the working day/life easier<br />
and safer<br />
3. Vehicle – looking at making the<br />
environment smarter and better<br />
These three parts all wrap around the<br />
patient experience.<br />
Ideas started to form and the benefits began<br />
to hit home and then somebody came up<br />
with the idea of coining the phrase IPTS -<br />
Integrated Patient Transport System. We had<br />
concepts; we had the desire to develop and<br />
to invest to make them a reality.<br />
The Journey<br />
Millions in investment and human<br />
resource hours have been put into<br />
bringing these innovations to life. Research<br />
and Development has been very busy<br />
throughout our global operations in order<br />
to achieve our goal of bringing these exciting<br />
new innovations to market with the support<br />
of the Global Marketing Team. We all believe<br />
in the new innovations and it is an exciting<br />
time to be with FERNO as we are ready to<br />
launch the most innovative solutions to be<br />
introduced within the EMS World for over<br />
60 years!<br />
Introduction to IPTS<br />
Are you ready to take the next step? Well<br />
we know you are because it would have<br />
been remiss of us to leave it until now to find<br />
out. We developed Customer Experience<br />
Centres to showcase our initial concept IPTS<br />
components and present the FERNO vision<br />
to the global EMS industry.<br />
With IPTS you can save £millions and that’s<br />
the bottom line! FERNO can save the Whole<br />
Health Economy a fortune in terms of<br />
time and efficiency. There may be an initial<br />
increase in capital cost - bringing this kind of<br />
innovation to market doesn’t come cheap,<br />
protecting our intellectual property with<br />
patents, designing new innovations, tooling<br />
investment, then testing them to the most<br />
stringent global crash standards at 26G<br />
forces has been a global endeavor.<br />
86 Spring 2016 | <strong>Ambulance</strong>today
Focus on the IPTS Concept <strong>Ambulance</strong><br />
Hand Over of the IPTS <strong>Ambulance</strong>. From Left To Right; Jon Ellis, FERNO Managing Director UK; Justin Wand,<br />
SECAmb, Head of Fleet Operations; James Kennedy, SECAmb Chief Operating Officer; Joe Bourgraf, FERNO<br />
Group CEO and Richard Smith FERNO <strong>Ambulance</strong> Systems Manager<br />
And this is what FERNO have done<br />
We have developed a global product for a<br />
safer world and all the UK market needs to<br />
do is change the way it works – but it is for<br />
the better and it’s an easier process. In fact<br />
young children have proven how easy our<br />
IPTS systems are to operate and with less<br />
manual handling we have reduced the risk of<br />
an MSK injury considerably.<br />
iN∫X Integrated Patient Transport & Loading System<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
The first UK Beta trial of the IPTS<br />
Connected Smart <strong>Ambulance</strong> is with<br />
South East Coast <strong>Ambulance</strong> Service NHS<br />
Trust and the innovations throughout are<br />
abundant. Its WiFi communication HUB<br />
means that critical information can be<br />
accessed. The Control System monitors<br />
drug efficacy with Smart Temperature<br />
Control. The battery management system is<br />
constantly monitored and the Marine Grade<br />
Solar Panels ensure a constant power output.<br />
Asset Protect ensures no equipment is left<br />
behind at the scene. Equipment changes<br />
take minutes not hours and make-ready is a<br />
simple modular process. The whole vehicle<br />
is safer, lighter and it’s now quicker to get a<br />
patient loaded safely and administer critical<br />
care en route with the iN∫X, the most<br />
advanced patient transport and loading<br />
system ever introduced to market globally.<br />
The features, benefits and innovations are<br />
extensive and the results and feedback so<br />
far are beyond our expectations. Getting<br />
the gross vehicle weight under 3.5 tons is<br />
definitely achievable which means crews have<br />
no need to pass their Category C1 driving<br />
tests.<br />
We are ready to give you the <strong>Ambulance</strong> of<br />
the Future today:<br />
To find out more about the IPTS<br />
Concept <strong>Ambulance</strong> call Ferno UK<br />
on 01274 851 999. Ferno will also be<br />
demonstrating the ambulance at<br />
future conferences and exhibitions.<br />
These will be announced on the<br />
Ferno UK website when they are<br />
confirmed.<br />
• A CONNECTED SMART<br />
AMBULANCE Integrated Patient Transport<br />
System<br />
• NO TAIL-LIFT eliminates weight on the<br />
<strong>Ambulance</strong> and high maintenance costs<br />
• ENHANCED PATIENT EXPERIENCE<br />
improves patient outcomes<br />
• REDUCED GVW removed 250kg, saves fuel<br />
costs, servicing and maintenance reductions<br />
• TASK TIME saves at least 2 minutes using<br />
iN∫X to load and unload<br />
• UNIT HOURS phenomenal savings with less<br />
downtime and breakdowns<br />
• REGULATORY REQUIREMENTS<br />
removes the need for PUWER and LOLER<br />
• AMBULANCE AVAILABILITY keeping<br />
vehicles on the road longer<br />
• WiFi a fully connected environment to work in<br />
including emails and eLearning<br />
• 360º CONNECTION providing Supervisor<br />
support, Manager contact, clinical guidance<br />
support and connection to other healthcare<br />
providers<br />
• PAC-RAC+ Crash tested and certified to CEN<br />
EN 1789<br />
• ELIMINATING RISK ancillary equipment<br />
mounted and secured closer to the patient<br />
preventing injury and harm<br />
• WORKING PRACTICES eliminating the<br />
need to place items down on the floor because<br />
they can be mounted close to hand<br />
• MULTIPLE POSITINING OF iN∫X from<br />
“B offside position” to the “C central position” for<br />
bariatric and critical care for optimal patient care<br />
in accordance with CEN<br />
• iN∫LINE FASTENER automatic in-vehicle<br />
charger for iN∫X, crash tested and certified to<br />
CEN EN 1789<br />
• MEDIC SEAT can be orientated according to<br />
head-end of patient, allowing good airway, posture<br />
and position<br />
• iN∫TRAXX System allows for both user and<br />
vehicle configurability<br />
• FLEXIBILITY the vehicle can be configured to<br />
change rolls to suit the situation, to suit the<br />
clinician or patient need<br />
• MEDICAL EQUIPMENT you can move or<br />
change equipment easily<br />
• EQUIPMENT CHOICE provides the option<br />
to move to new technology without the need for<br />
vehicle modification and reduces downtime<br />
• INFECTION CONTROL a cleaner more<br />
clinical environment reducing the risk of cross<br />
contamination<br />
• MAKE READY an anticipated 10 minute<br />
speeding up of the “Make Ready System” saving<br />
in the region of £1.7 million<br />
• PIR MOTION SENSOR technology that<br />
controls certain aspects of the vehicle, particularly<br />
lighting, and again the Paramedic can focus on<br />
the patient rather than on the environment<br />
• SMART TEMERATURE CONTROL<br />
drives a number of functions in this vehicle, allows<br />
us to track the cooling efficacy and maintains<br />
correct temperature of the drug compartment<br />
• AUDITING OF DRUGS proves beyond<br />
reasonable doubt the optimum effectiveness of<br />
the drugs administered<br />
• ECO RUN control which means we can<br />
configure the in vehicle environment such as<br />
temperature, lighting and battery condition<br />
Winter 2014 | <strong>Ambulance</strong>today3 87
Out & About News<br />
Visit the only daily ambulance news site on the net at:<br />
www.ambulancetoday.co.uk<br />
London <strong>Ambulance</strong> Service treats over 1,000 casualties<br />
during Europe’s largest disaster training exercise<br />
Hundreds of actors - each with<br />
a different story – recently<br />
helped to make the scenario<br />
as realistic as possible and<br />
test the clinical skills of the<br />
London <strong>Ambulance</strong> Service<br />
crews responding to a four day<br />
exercise, simulating a building<br />
collapsing onto a tube train.<br />
Around 175 clinical staff attended<br />
each day including emergency<br />
ambulance crews, paramedics,<br />
advanced paramedics, and specialist<br />
staff from the Hazardous Area<br />
Response Team who are trained to<br />
provide life-saving medical care in<br />
dangerous environments.<br />
Director of Operations Paul<br />
Woodrow said: “Over four days<br />
ambulance staff treated hundreds<br />
of injuries that would be typical<br />
during an incident like this including<br />
fractures, broken limbs, head injuries,<br />
amputations, spinal injuries and<br />
respiratory conditions.<br />
“Our ambulance crews are highly<br />
trained clinicians and in the event<br />
of a major incident would be<br />
dispatched to the scene quickly start<br />
assessing and treating patients, saving<br />
lives and ensuring patients receive<br />
the treatment they need.<br />
An incident control room was<br />
opened where staff from our<br />
emergency operations centre also<br />
practiced their response to a major<br />
incident, which involves managing<br />
information from staff at the scene,<br />
ensuring that we dispatch the<br />
most appropriate resources, and<br />
coordinating where patients will be<br />
conveyed.<br />
Paramedic students and medical<br />
students are along the large number<br />
of people volunteering as casualties<br />
throughout the exercise, to make the<br />
scenario as realistic as possible for<br />
emergency teams.<br />
Paul said: “In the event of a major<br />
incident we have clear processes<br />
Determined Dermot wins WAST Management<br />
Apprentice of the Year Award<br />
A long-serving WAST<br />
paramedic has picked up a<br />
prestigious award for the<br />
lengths he has gone to further<br />
his education.<br />
Dermot O’Leary, who is based in<br />
Rhyl <strong>Ambulance</strong> Station, won the<br />
Management Apprentice of the<br />
Year Award at Coleg Llandrillo’s<br />
Apprenticeships Awards Ceremony.<br />
The father-of-two, who has worked<br />
for the Welsh <strong>Ambulance</strong> Service<br />
for 15 years, was recognised for the<br />
work he produced while studying<br />
for his ILM Level 3 Diploma in<br />
Leadership Management.<br />
Dermot, who is also a Clinical Team<br />
Leader, and supervises a team of 14<br />
colleagues, said: “I was shocked and<br />
stunned when they called out my<br />
name at the awards ceremony.<br />
SWASFT ASPIRES to develop workforce<br />
South Western <strong>Ambulance</strong><br />
NHS Foundation Trust<br />
(SWASFT) is firmly committed<br />
to the development of our<br />
workforce, ensuring fulfilling<br />
careers for those who wish<br />
to progress through the<br />
variety of clinical roles<br />
within the Trust. Additionally,<br />
progression into middle and<br />
senior management for both<br />
clinicians and support staff is<br />
also strongly encouraged.<br />
Over the past year specialist<br />
paramedic programmes have been<br />
introduced to further develop the<br />
clinical portfolio of an increased<br />
number of our operational staff. We<br />
“I thought that the other candidates<br />
were far more ahead of the game<br />
than me, and I certainly didn’t expect<br />
to win.<br />
“The diploma was tough because<br />
you’re trying to juggle your studies<br />
with a full time job, but it was so<br />
worth it and I’m glad I did it.<br />
“I was chuffed just to be nominated<br />
to be honest.”<br />
The year-long course, which Dermot<br />
completed at the Rhos-on-Sea<br />
campus, is for those who are have<br />
management responsibilities but no<br />
formal training, and are serious about<br />
developing their abilities.<br />
Sonia Thompson, the Trust’s Head<br />
of Operations in North Wales, said:<br />
“We’re delighted that Dermot has<br />
have also assisted a huge number<br />
of staff to qualify as paramedics and<br />
delivered an extensive continuing<br />
professional development (CPD)<br />
programme across a huge range of<br />
subjects.<br />
Continuing the momentum we are<br />
now proud to launch our new career<br />
portal – Aspire. Aspire is a bespoke<br />
website dedicated to supporting<br />
our staff on their career journey<br />
and providing them with tools,<br />
information and helpful hints and tips<br />
to enable them to take charge of<br />
their own development.<br />
Staff can browse this site to find<br />
information on our appraisal system<br />
‘My Career Conversation’ how this<br />
Dermot O’Leary with his award.<br />
been recognised for his dedication,<br />
which knows no bounds.<br />
“Dermot is such a worthy recipient<br />
for this award, and we’re over the<br />
moon that his commitment has been<br />
links with our talent pools and how<br />
we use our identified ‘talent’ to<br />
deliver key programmes of work<br />
whilst providing them with valuable<br />
experience of working in a new<br />
area, with new people or at a more<br />
senior level. The site also provides<br />
information on how to get the best<br />
out of applying for jobs, preparing<br />
for an interview or preparing to<br />
study for a qualification. The site also<br />
signposts staff to courses, training<br />
sessions, webinars and reading<br />
which may be of use to them in<br />
their personal and professional<br />
development.<br />
We are proud of those we employ<br />
and the vital role they play in<br />
and plans in place<br />
including an alert<br />
system for staff<br />
who have proved<br />
they are always willing to support<br />
our response - even when not on<br />
duty.<br />
“By testing our responses to an<br />
incident like this we can increase our<br />
preparedness for any major incident<br />
that affects London. It was also a<br />
great opportunity to test how we<br />
work with emergency services and<br />
all other partners across London.”<br />
recognised in such a distinguished<br />
way.”<br />
Dermot, who lives in Penmaenmawr,<br />
joined the Welsh <strong>Ambulance</strong><br />
Service in 2001 as an Emergency<br />
Medical Technician, and qualified as a<br />
Paramedic two years later.<br />
He is also one of the Trust’s road<br />
safety champions and spends much<br />
of his own time visiting schools<br />
and colleges delivering hard-hitting<br />
lessons in road safety.<br />
Justine Grew, Work-Based Learning<br />
Manager at Coleg Llandrillo, said:<br />
“Dermot is an exemplary student,<br />
going far beyond what is required.<br />
“He has demonstrated innovation<br />
and dedication to his role. His<br />
assessor and tutor are very proud<br />
of his success.”<br />
caring for our patients. We also<br />
recognise the achievements of many<br />
of our staff who have developed<br />
and progressed throughout our<br />
organisation and the launch of Aspire<br />
seeks to further develop, encourage<br />
and open doors to many more.<br />
Enjoy our daily-updated ambulance news free online at: www.ambulancetoday.co.uk<br />
88 Spring 2016 | <strong>Ambulance</strong>today
The longest Serving<br />
paramedic for North West<br />
<strong>Ambulance</strong> Service (NWAS)<br />
Steve Evans has retired after<br />
44 dedicated years in the<br />
Service.<br />
In 1971 at the age of 16, a fresh<br />
faced Steve began his career<br />
as an ambulance cadet in the<br />
Merseyside area. Steve remained<br />
in the Merseyside and Cheshire<br />
area for his entire career, becoming<br />
a paramedic in 1989 and in the<br />
last six years he has trained other<br />
paramedics across the Trust.<br />
Steve, 60, has always busied himself<br />
in undertaking a wide range of<br />
successful projects outside his<br />
commitments as a paramedic.<br />
Writing medical books and his<br />
world famous ‘Don’t Walk Away’<br />
campaign, aimed at protecting young<br />
people, saw him rewarded with<br />
an MBE in this year’s New Year’s<br />
Honours list.<br />
Saving thousands of lives over his<br />
many years in the Service and<br />
delivering 19 babies, including one<br />
on Christmas day, Steve was given a<br />
special send off by the Trust with a<br />
retirement presentation.<br />
Speaking at the retirement<br />
presentation Steve said: “It’s been<br />
an incredible experience watching<br />
the ambulance service change over<br />
the years. The main thing I’ve always<br />
wanted to do as a paramedic is<br />
to make a difference. Whether<br />
you’re out on the road saving lives<br />
or training the next generation of<br />
Out & About News<br />
Visit the only daily ambulance news site on the net at:<br />
www.ambulancetoday.co.uk<br />
NWAS’s dedicated longest serving paramedic retires after 44 years<br />
Steve Evans at the retirement presentation<br />
with NWAS Head of Driving Standards<br />
Paul Jones-Roberts.<br />
paramedics, you’re always part of a<br />
team making a huge difference to so<br />
many lives every day.<br />
“I didn’t have the qualifications to<br />
get into the police, so my Mum told<br />
me to sign up with the ambulance<br />
service. I’ve never looked back. The<br />
people in the Service are incredible<br />
and I’ll definitely miss my colleagues<br />
the most.”<br />
SECAmb Fleet success at Fleet News Awards 2016<br />
South East Coast <strong>Ambulance</strong><br />
Service NHS Foundation<br />
Trust (SECAmb) is celebrating<br />
success after winning in three<br />
categories at the Fleet News<br />
Awards.<br />
Nominated in six categories, the Trust<br />
came out top in three categories<br />
- Fleet of the Year (251 to 1000<br />
vehicles), Green Fleet of the Year<br />
and Fleet Manager of the Year where<br />
SECAmb’s Justin Wand scooped<br />
the top award. It was also Highly<br />
Commended in the Safe Fleet and<br />
Most Improved Fleet categories.<br />
About 1,500 attended the ceremony<br />
in which the SECAmb fleet team,<br />
which has been on a modernisation<br />
programme in recent years, was<br />
directly competing, not with<br />
other blue light services, but with<br />
commercial organisations.<br />
It is the third fleet awards event the<br />
Trust has been shortlisted for in the<br />
last six months. Last year SECAmb<br />
won at the Commercial Fleet Awards<br />
the Blue Light & Public Sector Fleet<br />
of the Year and was also Highly<br />
Commended at the Green Fleet<br />
Awards in a competition with 600<br />
other applicants.<br />
SECAmb’s Head of Fleet<br />
and Logistics Justin Wand<br />
said: “This recognition is a<br />
great achievement for the<br />
Trust and demonstrates<br />
Bob McGowan, Interim Head of<br />
Service for Cheshire and Merseyside<br />
said: “Steve has been a brilliant<br />
member of the team and brought a<br />
great deal of dedication, passion and<br />
enthusiasm to his roles. He will be<br />
truly missed in the Trust by colleagues<br />
up and down the North West. We<br />
all wish Steve a long and happy<br />
retirement and thank him for all his<br />
incredible work over the years.”<br />
Steve plans to spend his retirement<br />
continuing his work training street<br />
pastors and using the lawnmower he<br />
received from colleagues as a leaving<br />
gift. Steve will also by cycling Land’s<br />
End to John o’ Groats in September<br />
and will be spending the next five<br />
months training for his ‘epic’ cycle<br />
ride.<br />
the hard work the team has put<br />
in in recent years. The Fleet team<br />
plays a crucial role in ensuring the<br />
service is able to respond reliably<br />
and sustainably to our patients. I am<br />
immensely proud of all the team<br />
whose hard work is delivered day in<br />
day out and which contributes directly<br />
to patient care. I would also like to<br />
add that my personal recognition<br />
is only possible because of my own<br />
team and wider Trust support.”<br />
Alfred Bekker API Ltd<br />
Alfred Bekker API Ltd<br />
Small PTS Vehicles:<br />
5 Seats and using ECWVTA<br />
Flexi-Ramp allows the boot<br />
space to be utilised<br />
RolliBox PTS:<br />
Driffield, East Yorkshire<br />
01377 241 700<br />
info@alfredbekker.com<br />
www.alfredbekker.com<br />
Alfred Bekker specialise in<br />
the design and<br />
manufacture of PTS, Single<br />
Wheelchair PTS and Rapid<br />
Response Vehicles<br />
4 Wheelchairs, 7 Seats or<br />
any combination in between,<br />
you can also add a Stretcher<br />
Rapid Response Vehicles:<br />
Using the best base vehicles and quality electronic<br />
systems Alfred Bekker can now offer RRV’s to suit Doctors<br />
& First Response Paramedic Vehicles<br />
Spring 2016 | | <strong>Ambulance</strong>today<br />
73 89 3
Out & About News<br />
Visit the only daily ambulance news site on the net at:<br />
www.ambulancetoday.co.uk<br />
Finnish study shows high serum omega-6 polyunsaturated fatty acid<br />
concentrations linked to lower risk of type 2 diabetes<br />
A new study from the<br />
University of Eastern Finland<br />
shows that high serum<br />
omega-6 polyunsaturated fatty<br />
acid concentrations are linked<br />
to a significantly reduced<br />
risk of type 2 diabetes. The<br />
findings were published in the<br />
American Journal of Clinical<br />
Nutrition.<br />
It has been speculated that a high<br />
intake of omega-6 polyunsaturated<br />
fatty acids may increase the risk of<br />
several chronic diseases, as these<br />
fatty acids have been suggested to<br />
promote low-grade inflammation,<br />
among other things. However, studies<br />
conducted on humans have not<br />
established a link between even a<br />
high intake of omega-6 fatty acids<br />
and inflammation. Furthermore,<br />
omega-6 fatty acids have beneficial<br />
effects on, for example, glucose<br />
metabolism. Earlier research has<br />
systematically linked especially linoleic<br />
acid, which is the most common<br />
omega-6 fatty acid, to a reduced risk<br />
of cardiovascular diseases and type 2<br />
diabetes. However, scientific evidence<br />
relating to the health effects of other<br />
omega-6 polyunsaturated fatty acids<br />
is not as inconclusive.<br />
The serum fatty acid concentrations<br />
of 2,189 men aged between 42<br />
and 60 years and with no baseline<br />
type 2 diabetes diagnosis were<br />
analysed at the onset of the Kuopio<br />
Ischaemic Heart Disease Risk Factor<br />
Study, KIHD, in 1984–1989 at the<br />
University of Eastern Finland. During<br />
a follow-up of 19 years, 417 men<br />
were diagnosed with type 2 diabetes.<br />
The study found that high serum<br />
omega-6 polyunsaturated fatty acid<br />
concentrations were associated with<br />
a 46% lower risk of developing type<br />
2 diabetes during the follow-up.<br />
When analysing the independent<br />
associations of different omega-6<br />
polyunsaturated fatty acids, a similarly<br />
significant association was found<br />
between high serum linoleic and<br />
arachidonic acid concentrations<br />
and a lower risk of type 2 diabetes.<br />
However, high serum gammalinolenic<br />
and dihomo-γ-linolenic<br />
acid concentrations were linked to a<br />
higher risk.<br />
The study indicates that high<br />
serum linoleic and arachidonic<br />
acid concentrations are linked to a<br />
lower risk of type 2 diabetes. The<br />
serum linoleic acid concentration<br />
is determined by the person’s diet,<br />
and the main sources of linoleic acid<br />
are vegetable oils, nuts and seeds.<br />
Arachidonic acid is present in meat<br />
and eggs; however, the human body<br />
can also make arachidonic acid from<br />
linoleic acid.<br />
Gamma-linolenic acid and dihomoγ-linolenic<br />
acid are mainly formed<br />
in the human body from linoleic<br />
acid. Their concentrations in serum<br />
are very low in comparison to, for<br />
example, linoleic acid. The association<br />
of gamma-linolenic acid and dihomoγ-linolenic<br />
acid with a higher risk of<br />
type 2 diabetes has been observed<br />
in some earlier studies, but the<br />
underlying reason remains unknown.<br />
All in all, however, this study as well<br />
as several earlier ones suggest that<br />
polyunsaturated omega-6 fatty acids<br />
have a beneficial impact on the risk<br />
of type 2 diabetes.<br />
For further information,<br />
please contact:<br />
Jyrki Virtanen, PhD, Adjunct<br />
Professor in Nutritional<br />
Epidemiology, University of<br />
Eastern Finland Institute of<br />
Public Health and Clinical<br />
Nutrition, tel. +358294454542,<br />
jyrki.virtanen(at)uef.fi<br />
Book your place at EMS 2016 in Copenhagen at: www.ems2016.org<br />
90 Spring 2016 | <strong>Ambulance</strong>today
South Central <strong>Ambulance</strong><br />
Service NHS Foundation<br />
Trust (SCAS) are pleased to<br />
have launched a trial with<br />
Auxilium. This system aims<br />
to assist us in identifying and<br />
treating patients at the site<br />
of an incident, specifically<br />
for the patients who are<br />
incapacitated and unable to<br />
communicate this information<br />
fully themselves. It allows<br />
ambulance staff to find out<br />
valuable information about a<br />
patient even before they even<br />
reach the scene of an incident.<br />
The Auxilium<br />
system allows any<br />
individual to store<br />
their personal<br />
information<br />
on a website.<br />
Information such<br />
as name, home address, next of kin<br />
and key medical record data which<br />
could potentially be very useful in<br />
some situations when the patient is<br />
unable to communicate.<br />
Each Auxilium user is provided with<br />
their own unique Auxilium Number,<br />
this number can be displayed on<br />
items carried by the user, such as<br />
Staff ID Cards, keyrings, or even<br />
displayed on their mobile phone.<br />
There is a distinctive Auxilium<br />
System logo attached to the 10-digit<br />
Auxilium number. This logo can be<br />
easily spotted by the emergency<br />
services and the public. The number<br />
can then be provided to the<br />
emergency call taker by the caller<br />
who will have access to the Auxilium<br />
Database. The operator with then<br />
use this number to access the<br />
relevant information.<br />
Luci Stephens, Director of<br />
Operations – Clinical Coordination<br />
Centres, South Central <strong>Ambulance</strong><br />
Service NHS Foundation Trust, said<br />
“We are pleased to have embarked<br />
on this trial of Auxilium which we<br />
hope will prove to be of benefit<br />
to patients and staff alike. There<br />
Out & About News<br />
Visit the only daily ambulance news site on the net at:<br />
www.ambulancetoday.co.uk<br />
Auxilium and South Central <strong>Ambulance</strong> Service launch a new trial<br />
are occasions when it would be<br />
incredibly useful to have key details<br />
about a patient which they might not<br />
be able to provide to us due to their<br />
medical condition and we hope that<br />
this trial will help demonstrate how<br />
important these details are in the<br />
event of an emergency”.<br />
Grant Moreton, Inventor and<br />
Director of Auxilium Systems Ltd<br />
said “Some years ago I was witness<br />
to a serious incident and it at that<br />
time it occurred to me that there<br />
was a benefit of a system which<br />
would provide peoples contact<br />
details in the event of an emergency.<br />
The Auxilium system has been<br />
initially made available to members<br />
of the public in the SCAS area (as<br />
this is where the trial is taking place)<br />
to enable them to log on and fill out<br />
the details that they would want the<br />
ambulance service to have access<br />
to. Such things as contact details,<br />
current medications etc can be<br />
filled out so that staff in our control<br />
room could have access to them to<br />
pass on to responding ambulance<br />
St John New Zealand reaches ePRF milestone<br />
St John New Zealand has<br />
successfully completed the<br />
implementation of its new<br />
electronic Patient Report Form<br />
(ePRF) across its emergency<br />
ambulance service. The worldleading<br />
technology replaces<br />
paper patient records and was<br />
successfully implemented over<br />
a six month timeframe.<br />
ePRF was<br />
developed<br />
by St John in<br />
partnership<br />
with the<br />
Ministry<br />
crews. I am delighted<br />
that we have now<br />
embarked on this<br />
with SCAS to assess<br />
its effectiveness”.<br />
Auxilium is already<br />
up and running so<br />
if members of the public would like<br />
to know more they can email info@<br />
auxsys.uk membership is currently<br />
free to all schools for the first year<br />
with a £1 fee per person per year<br />
for all other members of the public.<br />
Auxilium are also offering certain<br />
charities whose members have<br />
medical conditions over 500,000<br />
AUXILIUM numbers totally free. It is<br />
the responsibility of the individual to<br />
keep the information up to date and<br />
accurate.<br />
To find out more contact<br />
Grant Moreton or Chris<br />
Rowe:<br />
Tel: 01865 338020<br />
Website: www.auxsys.uk<br />
Email: info@auxsys.uk<br />
Prof. Douglas Chamberlain ‘father of the paramedic profession’<br />
takes centre stage at EHAAT’s Clinical Governance Day<br />
The founder of the first<br />
paramedic unit in Europe,<br />
Prof. Douglas Chamberlain,<br />
spoke to an 85-strong<br />
audience of doctors,<br />
paramedics, nurses, students<br />
and other emergency services<br />
personnel at the Essex &<br />
Herts Air <strong>Ambulance</strong> Trust’s<br />
monthly Clinical Governance<br />
Day held at North Weald<br />
Airfield on Tuesday 15 March.<br />
Prof. Chamberlain, who has<br />
dedicated his career to pioneering<br />
the resuscitation techniques that are<br />
now common place amongst the<br />
emergency services and save lives<br />
every day, was invited to speak at<br />
the event hosted at North Weald<br />
Airfield - home of the Herts Air<br />
<strong>Ambulance</strong>.<br />
After giving his presentation about<br />
optimising Cardio-Pulmonary<br />
of Health’s Information Group,<br />
supported by the Accident<br />
Compensation Corporation (ACC),<br />
Valentia Technologies and Samsung<br />
Electronics.<br />
ePRF will soon allow the secure<br />
transmission of patient information<br />
between ambulances and hospital<br />
emergency departments, aligning<br />
St John records with other health<br />
records using the patient’s NHI<br />
(national health index) number.<br />
From 2017, ePRF will enable hospital<br />
staff to access ambulance care<br />
summary records directly using their<br />
computers.<br />
Resuscitation he remarked: “It was<br />
a real privilege to have come and<br />
met so many wonderful dedicated<br />
people, thank you so very much, an<br />
inspiring day for us”.<br />
EHAAT opens its doors to the<br />
wider healthcare and emergency<br />
services community on the third<br />
Tuesday of each month. All those<br />
with an interest in pre-hospital<br />
critical care are invited to share its<br />
The new technology gives<br />
paramedics access to better patient<br />
information. Currently, only details<br />
of previous ambulance call-outs can<br />
be searched, but with the future<br />
linkage of other health records, St<br />
John will be able to provide higher<br />
quality information to emergency<br />
department staff, and others in<br />
the heath sector, improving clinical<br />
practice and patient care.<br />
St John Director of Clinical<br />
Operations, Norma Lane says the<br />
roll out of ePRF is a key milestone<br />
in the modernisation of St John’s<br />
ambulance service. “Moving from<br />
governance meetings. Every event<br />
is themed around an element of<br />
emergency care and, as well as case<br />
presentations, audits and journal<br />
reviews, include presentations from<br />
expert speakers from a variety of<br />
clinical backgrounds.<br />
Laurie Phillipson, EHAAT Clinical<br />
Manager said: “Every paramedic<br />
across the country has heard of Prof.<br />
Chamberlain; in many ways he is the<br />
father of the paramedic profession<br />
and responsible for saving thousands<br />
of lives; to have him speak at one<br />
of our governance days was a real<br />
honour”.<br />
Other speakers on the day included<br />
David and Kaz Fletcher, who spoke of<br />
the influence that data downloaded<br />
from defibrillators can have on<br />
improving resuscitation, and Dr Ben<br />
Singer who presented forwardthinking<br />
presentation on Extra-<br />
pen and paper to<br />
electronic records<br />
enables us to share<br />
higher quality<br />
patient information<br />
with District Health Boards (DHBs),<br />
improving patient care. We can<br />
also now electronically analyse and<br />
audit patient records, extracting<br />
anonymised information that informs<br />
the ongoing improvement of our<br />
clinical education and practice.”<br />
For more information visit:<br />
http://www.stjohn.org.nz/<br />
News--Info/St-John-ePRF/<br />
Corporeal Membrane Oxygenation<br />
and its role in out-of-hospital cardiac<br />
arrest.<br />
Dr Alex Rosenberg , Consultant in<br />
Critical Care at the Royal Brompton<br />
and Harefield NHS Foundation Trust,<br />
and some of his colleagues attended<br />
the Governance Day. He said: “We<br />
all thought it was a really great day<br />
and thoroughly enjoyed it. I think the<br />
real take home message for me was<br />
the chaos that your team deal with<br />
day to day and how this impacts<br />
upon resuscitation.”<br />
The next Essex and Herts Air<br />
<strong>Ambulance</strong> Clinical Governance<br />
Day will be held on the 19th April<br />
2016 at North Weald Airfield. Any<br />
clinicians or emergency services<br />
personnel interested in attending<br />
should contact Geraldine.wash@<br />
ehaat.uk.com<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
91
Out & About News<br />
Visit the only daily ambulance news site on the net at:<br />
www.ambulancetoday.co.uk<br />
Essex & Herts Air <strong>Ambulance</strong> Trust signs-up to<br />
purchase its own ‘state-of-the-art’ helicopter<br />
Thanks to the support of<br />
the people and businesses of<br />
Essex and Hertfordshire, the<br />
Essex & Herts Air <strong>Ambulance</strong><br />
Trust (EHAAT) has reached<br />
a milestone in its fundraising<br />
– enabling the charity to<br />
purchase its own helicopter<br />
for the first time in its 20 year<br />
history.<br />
In March, Rob Forsyth, Chair of<br />
Trustees at EHAAT signed the<br />
contract with aircraft operator,<br />
Medical Aviation Services (MAS) to<br />
secure the purchase and operation<br />
of the £6 million Agusta Westland<br />
AW169 - the leading edge helicopter<br />
for emergency medical service<br />
operations.<br />
A 10-year contract to lease an<br />
MD902 Explorer was also approved.<br />
The life-saving Charity takes<br />
possession of both aircraft early next<br />
EEAST completes regional CAD upgrade<br />
A brand new system at the<br />
point of a 999 call to help<br />
improve the level of service to<br />
patients has been installed at<br />
the region’s ambulance service.<br />
The new computer aided dispatch<br />
system (CAD) is provided by<br />
Cleric, a company specialising in the<br />
development of computer software.<br />
Executive Officer Jon Moore said it<br />
was considered as an essential move<br />
by bosses at the East of England<br />
<strong>Ambulance</strong> Service NHS Trust<br />
(EEAST): “It was a necessary step,<br />
and an extremely positive one which<br />
year and will be ready to fly in June<br />
2017 as the leases on its current<br />
aircraft come to an end.<br />
The purchase was made possible<br />
thanks to the support given to the<br />
Charity by the people and businesses<br />
of Essex & Hertfordshire, supported<br />
by the Charity’s successful bid for<br />
£1.5 million from the Government’s<br />
Libor fund.<br />
The Agusta Westland AW169 will<br />
be the most advanced aircraft flying<br />
within the East of England region’s<br />
air ambulance services. Ideally suited<br />
to life-saving missions, it offers the<br />
maximum internal cabin space for<br />
crew, patients and equipment so that,<br />
even whilst flying, the Pre-Hospital<br />
Care Doctors and Critical Care<br />
Paramedics will have full access to<br />
the patient if necessary.<br />
It’s also capable of night flying, giving<br />
the Charity the capability, if necessary,<br />
is integral in aiding the Trust on the<br />
road to recovery.”<br />
He thanked the 450-plus-people<br />
involved in the upgrading process<br />
overall, which saw three regional<br />
emergency operation centres<br />
(EOCs) in Bedford, Norwich, and<br />
to broaden its service into the hours<br />
of darkness over the coming years.<br />
The AW169 also boasts an Auxiliary<br />
Power Unit (APU) to run clinical<br />
equipment on the ground, including<br />
the illumination of the cabin to assist<br />
crews whilst working, and Digital<br />
Automatic Flight Control to boost<br />
safety.<br />
Investment into new generation<br />
aircraft will enhance the Charity’s<br />
Air <strong>Ambulance</strong> provision both<br />
operationally and clinically and will<br />
bring huge benefits to the people of<br />
Essex, Hertfordshire and surrounding<br />
areas.<br />
Both aircraft will be flown and<br />
maintained by Medical Aviation<br />
Services (MAS) which has been<br />
working in partnership with EHAAT<br />
for the last ten years.<br />
Henk Schaeken, Managing Director<br />
of MAS, added: “EHAAT has selected<br />
Chelmsford install the new CAD in<br />
less than five months.<br />
Jon added: “It was an ambitious<br />
target we set ourselves but thanks<br />
to the tireless effort of everyone<br />
involved we have been able to<br />
deliver at an extremely period. This<br />
is one of the fastest implementations<br />
of the ambulance service.”<br />
The new system means that patients<br />
will be dispatched ambulances in a<br />
safer, more efficient, and appropriate<br />
process that is more adept at dealing<br />
with current levels of demand faced<br />
by the ambulance service.<br />
Blue Light Services launch North Yorkshire’s first Emergency<br />
First Responder scheme<br />
Fifteen retained firefighters<br />
at Pickering, Helmsley and<br />
Lythe are now responding to<br />
life-threatening emergency<br />
calls at the same time as<br />
an ambulance, thanks to<br />
the official launch of North<br />
Yorkshire’s first Emergency<br />
First Responder (EFR) scheme.<br />
The pilot scheme is a joint initiative<br />
between Yorkshire <strong>Ambulance</strong><br />
Service NHS Trust (YAS) and North<br />
Yorkshire Fire & Rescue Service<br />
(NYFRS). It follows the success of<br />
the first scheme which has been<br />
running in Humberside and the East<br />
Riding of Yorkshire for the last two<br />
years, the South Yorkshire scheme<br />
which was launched in October<br />
2015 and most recently the West<br />
Yorkshire initiative.<br />
Each EFR has been trained in basic<br />
life support, cardiopulmonary<br />
resuscitation (CPR) and oxygen<br />
therapy. They are equipped with a<br />
kit which includes oxygen and an<br />
automated external defibrillator<br />
(AED) to help patients in a medical<br />
emergency such as a heart attack,<br />
collapse or breathing difficulties.<br />
An EFR will be dispatched at<br />
the same time as an ambulance<br />
and will not replace the usual<br />
emergency medical response from<br />
YAS. However, their location within<br />
local communities could mean they<br />
are nearer to the scene in those<br />
first critical minutes of a medical<br />
emergency, delivering life-saving care<br />
until an ambulance clinician arrives.<br />
Paul Stevens, Head of Community<br />
Resilience at YAS said: “We have a<br />
responsibility to ensure we explore<br />
all available options to improve<br />
clinical outcomes for people in<br />
Yorkshire and we are delighted to be<br />
working in partnership with WYFRS<br />
on this Emergency First Responder<br />
scheme.<br />
“We have a very clear ambition<br />
to improve the survival rate for<br />
those people who suffer from a<br />
cardiac arrest in the community<br />
and we want to have world-class<br />
levels of survival. The expansion of<br />
this initiative is another important<br />
element of this.<br />
“North Yorkshire is already served by<br />
our award-winning Community First<br />
Responder teams who do a fantastic<br />
job as volunteers in their local areas.<br />
the latest and best possible aircraft<br />
available and we are delighted to<br />
be able to continue our partnership<br />
with them. The Agusta Westland<br />
AW169 will ensure the Charity’s<br />
Helicopter Emergency Medical<br />
Service (HEMS) crews will be able<br />
to provide an even greater level of<br />
service to the people of Essex and<br />
Hertfordshire.”<br />
The Agusta Westland 169 will arrive<br />
in the UK in early 2017 and will<br />
commence flying from June 2017.<br />
For more visit information on<br />
Essex & Herts Air <strong>Ambulance</strong><br />
Trust visit EHAAT.uk.com<br />
Jon said: “We are already seeing<br />
benefits which will enable us to<br />
continue our improvement in the<br />
coming months. The feedback from<br />
staff that have been trained to use<br />
the new system has been fantastic.”<br />
Want to find out more<br />
about how a 999 call works?<br />
The Trust’s Its Your Call<br />
information pages can be<br />
found here:<br />
/www.eastamb.nhs.uk/Newsand-Media/Campaigns/itsyour-call.htm<br />
The addition of Emergency First<br />
Responders has further strengthened<br />
our response in these communities<br />
and the two models work side-byside<br />
to save more lives.<br />
sponders are only available for<br />
dispatch when staffing levels at their<br />
Fire Station allow and the scheme<br />
will not have an adverse impact on<br />
fire cover. The scheme will be closely<br />
monitored throughout the pilot and<br />
fully evaluated prior to any decisions<br />
being made about the long-term<br />
future of the scheme.<br />
Head of Risk Management Owen<br />
Hayward from North Yorkshire<br />
Fire & Rescue Service said: “We are<br />
delighted to be part of this scheme<br />
and believe that it will deliver real<br />
benefits to people who require<br />
medical assistance in these rural<br />
areas.<br />
Got a special project you want to share? Please email us at: editor@ambulancetoday.co.uk<br />
92 Spring 2016 | <strong>Ambulance</strong>today
London <strong>Ambulance</strong> Service appoints new Medical Director<br />
London <strong>Ambulance</strong> Service<br />
is pleased to announce that<br />
Dr Fenella Wrigley has<br />
been appointed Medical<br />
Director following a national<br />
recruitment process.<br />
Fenella has been<br />
undertaking the role<br />
on an interim basis<br />
since January 2015.<br />
Prior to that Fenella<br />
was Deputy Medical<br />
Director, having<br />
joined the Service<br />
in 2008 as Director for Control<br />
Services.<br />
Chief Executive, Dr Fionna Moore,<br />
said: “Fenella brings a wealth of<br />
clinical experience from both the<br />
pre hospital setting and as an A&E<br />
consultant. She is committed and<br />
passionate about providing the<br />
best possible patient outcomes for<br />
Londoners.<br />
“We are delighted Fenella has<br />
accepted this role on a permanent<br />
basis.”<br />
Out & About News<br />
Visit the only daily ambulance news site on the net at:<br />
www.ambulancetoday.co.uk<br />
$1.1m investment to help half a million New Zealand<br />
children learn first aid skills<br />
Teaching Kiwi kids how to<br />
prevent injuries and ensuring<br />
they have the skills and<br />
confidence to take action in an<br />
emergency are the goals of the<br />
St John in Schools programme,<br />
formally launched in March by<br />
the Accident Compensation<br />
Corporation (ACC) Minister<br />
Nikki Kaye and St John CEO<br />
Peter Bradley at Clendon Park<br />
School in South Auckland.<br />
St John in Schools was developed by<br />
the Community Health Services arm<br />
of St John, the largest emergency<br />
ambulance service in New Zealand<br />
(population 4.47 million).<br />
It aims to improve the emergency<br />
preparedness and community<br />
resilience of the next generation, and<br />
there are numerous examples of<br />
children who have been through a St<br />
John in Schools programme making a<br />
real difference in an emergency.<br />
St John CEO, Peter Bradley says<br />
the programme was introduced in<br />
2015, with 77,000 children taking<br />
part and over 30,000 kids taught<br />
CPR. “St John in Schools improves<br />
the emergency preparedness and<br />
community resilience of the next<br />
generation,” he said.<br />
“This is exciting and significant not<br />
only for the youth of New Zealand<br />
but also for their families, friends and<br />
community who stand to benefit<br />
from their knowledge.”<br />
St John in Schools receives<br />
a significant boost through<br />
the partnership with ACC, a<br />
Government organisation that<br />
provides comprehensive, no-fault<br />
personal injury cover in New<br />
Zealand. ACC is investing $1.15<br />
million to help St John in Schools<br />
reach 480,000 children over the next<br />
five years.<br />
Around 349,000 injury claims<br />
involving children under 14 are<br />
received annually by ACC.<br />
“Giving our kids the confidence to<br />
call 111 and provide first aid could<br />
Fenella will continue to work<br />
clinically one day a week as a<br />
consultant in emergency medicine<br />
for Barts Health NHS Trust.<br />
She said: “It is a privilege to work as<br />
part of the NHS both at London<br />
<strong>Ambulance</strong> Service and for Barts<br />
Health.<br />
“The Service has had a challenging<br />
year and it is vital we continue we<br />
continue to promote excellent care<br />
and patient experience, develop all<br />
of our staff and work closely with<br />
stakeholders and the wider NHS.<br />
be the difference<br />
that saves a life or<br />
reduces the impact<br />
of the injury,” says Ms Kaye.<br />
“This initiative is another example of<br />
the extra emphasis ACC is putting<br />
on working in partnership with<br />
others to prevent injuries and make<br />
our communities safer.”<br />
The programme will also be<br />
aligned to the New Zealand<br />
School curriculum and Te Whariki,<br />
the Ministry of Education’s early<br />
childhood curriculum framework.<br />
For more information visit:<br />
http://www.stjohn.org.nz/<br />
What-we-do/Community-<br />
programmes/St-John-in-<br />
Schools-Programme/<br />
“I look forward to working together<br />
to continue to improve our clinical<br />
outcomes and develop our role as a<br />
leading mobile healthcare provider.”<br />
Fenella led on the development<br />
of urgent care within the London<br />
<strong>Ambulance</strong> Service, overseeing<br />
the introduction of a Clinical Hub<br />
in the control room. Staffed by<br />
clinicians it provides clinical support<br />
to ambulance crews at the scene<br />
as well as telephone treatment for<br />
patients.<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
93
Out & About News<br />
Visit the only daily ambulance news site on the net at:<br />
www.ambulancetoday.co.uk<br />
WAS <strong>Ambulance</strong> Technician’s tragic death<br />
inspires colleague to run London Marathon<br />
The sudden death of a longserving<br />
ambulance technician<br />
has inspired one of his<br />
colleagues to run the London<br />
Marathon in his memory.<br />
Nigel Dorsett will take on the<br />
26.2-mile challenge as a tribute<br />
to his colleague Phil Williams, an<br />
Emergency Medical Technician based<br />
in Welshpool, who died in February<br />
while on duty.<br />
Nigel’s t-shirt for the London Marathon<br />
bears Phil’s professional pin number.<br />
St John New Zealand’s second<br />
annual Out of Hospital Cardiac<br />
Arrest (OHCA) report shows<br />
the organisation maintained a<br />
strong 15% survival to hospital<br />
discharge rate for patients who<br />
are treated for cardiac arrest in<br />
the year beginning 1 July 2014.<br />
St John is New Zealand’s largest<br />
emergency ambulance service,<br />
serving around 4 million people or<br />
approximately 90% of the country’s<br />
population. Cardiac arrest is a<br />
significant public health issue in New<br />
Zealand with ischaemic heart disease<br />
being the second most prevalent<br />
cause of death; of the 38 people who<br />
are treated for cardiac arrest by St<br />
Plucky Nigel has never run a<br />
marathon before, but completed the<br />
Cardiff Half Marathon in March in<br />
preparation for his challenge in the<br />
English capital.<br />
The 54-year-old, who works for<br />
the Welsh <strong>Ambulance</strong> Service’s<br />
Patient Care Service, and is based<br />
in Newtown, said: “Until last year,<br />
I wouldn’t even run for the bus,<br />
and now I’m preparing to run a<br />
marathon.<br />
“I entered but I didn’t think I’d stand<br />
a chance of securing a place, then<br />
the letter landed on my mat and the<br />
panic set in.”<br />
Nigel signed up for the marathon<br />
last year to raise funds for Macmillan<br />
Cancer Support and the Bracken<br />
Trust, a Powys-based charity that<br />
supports those affected by cancer.<br />
Following Phil’s tragic death, he<br />
decided he also wanted to use his<br />
marathon attempt to celebrate<br />
the life of his friend and colleague,<br />
and will bear Phil’s professional pin<br />
number on his running vest.<br />
John each week, 12 are successfully<br />
resuscitated and transported to<br />
hospital and six will later survive to<br />
be discharged<br />
Published December 2015, the<br />
new OHCA data confirms St John’s<br />
clinical processes continue to be<br />
of a high standard and compare<br />
favourably with similar ambulance<br />
services internationally. The data<br />
in the report will drive important<br />
clinical improvements and processes.<br />
New Zealand’s low rate of public<br />
access to defibrillators remains an<br />
issue. While 64% of patients had<br />
bystander CPR performed, only 4%<br />
of patients were defibrillated using a<br />
public access defibrillator.<br />
He added: “Phil and I only worked<br />
together for a short time, but he was<br />
a great guy and very approachable.<br />
“This is my way of remembering Phil.<br />
Let’s hope he can get me over the<br />
finish line.”<br />
Colleagues of Phil, who was 58 and<br />
lived in Llanfechain with his partner,<br />
were offered support via the Trust’s<br />
Wellbeing Support Service following<br />
his death.<br />
Philip Pover, Clinical Team Leader at<br />
the Welsh <strong>Ambulance</strong> Service, and<br />
Phil’s manager, said: “Phil’s death came<br />
as a huge shock to us all, and we still<br />
can’t believe that he’s gone.<br />
Paramedic Phil Williams, who died suddenly<br />
in February.<br />
St John New Zealand publishes second Out of Hospital<br />
Cardiac Arrest report<br />
OHCA data also identified that<br />
Māori (New Zealand’s indigenous<br />
people) are more at risk than non-<br />
Māori. As a result the organisation<br />
has developed the ‘Marae Out<br />
of Hospital Cardiac Arrest<br />
programme’, which will see St John<br />
work with Māori communities<br />
and maraes around NZ supporting<br />
training and access to defibrillators<br />
and CPR in 2016.<br />
Demographic Findings<br />
• The most common cause of<br />
cardiac arrest was heart disease<br />
(77%)<br />
• 68% of cardiac arrests occur at<br />
home and 19% happen in public<br />
“Over the years, Phil helped<br />
hundreds if not thousands of people,<br />
many of whom would not be walking<br />
around Wales today if it wasn’t for<br />
his skill and dedication.<br />
“He was a very intelligent, kind and<br />
laid back man who had a lot of<br />
respect from his peers.<br />
“He is missed by all of us who had<br />
the pleasure of knowing him.”<br />
If you would like to sponsor<br />
Nigel’s London Marathon attempt,<br />
visit uk.virginmoneygiving.com/<br />
NigelDorsett<br />
Nigel is also organising a raffle and<br />
an auction on Saturday 14 May at<br />
the Llanerch Inn in Llandrindod Wells,<br />
the proceeds from which will be split<br />
between the two charities and Phil’s<br />
loved ones.<br />
Nigel is appealing to anyone who<br />
would like to donate a prize to<br />
the auction to get in touch via his<br />
Facebook page: ‘Nigel Marathon<br />
Dorsett’<br />
• Māori were<br />
disproportionally<br />
affected with a<br />
higher incidence<br />
of cardiac arrest (122.4) compared<br />
with all other ethnic groups (less<br />
than 90) per 100,000 person-years<br />
• Applying CPR and rapid<br />
defibrillation can increase a<br />
patient’s chances of survival by up<br />
to 40%<br />
SCAS is proud to be the provider of Non-Emergency Patient<br />
Transport Services across the Thames Valley region<br />
South Central <strong>Ambulance</strong><br />
Service NHS Foundation Trust<br />
(SCAS) is proud to announce<br />
the start of the new contract<br />
to provide the Non-Emergency<br />
Patient Transport Service<br />
(NEPTS) across the Thames<br />
Valley region from April 2016.<br />
This is a new contract which brings<br />
together three existing contracts<br />
covering Berkshire,<br />
Oxfordshire and Buckinghamshire.<br />
SCAS is the existing supplier for<br />
these three contracts.<br />
SCAS already operates the NEPTS<br />
service across many parts of the<br />
South Central region, providing<br />
transport for people who are unable<br />
to use public or other transport due<br />
to their medical condition, and are:<br />
• Attending hospital outpatient<br />
clinics<br />
• Being admitted to or discharged<br />
from hospital wards<br />
• Needing life-saving treatments<br />
such as radiotherapy, chemotherapy<br />
or renal dialysis or DVT treatment<br />
SCAS has over 40 years of<br />
experience of patient transport, and<br />
in 2014/15 undertook over 500,000<br />
patient journeys. A comprehensive<br />
mobilisation plan for the contract,<br />
managed by a dedicated project<br />
team working closely with<br />
representatives of the commissioning<br />
group, has ensured a smooth transfer<br />
to the new contract.<br />
Director of Strategy, Business<br />
Development, Communications<br />
and Engagement for SCAS, James<br />
Underhay, said: “We are really<br />
The full Out-of-Hospital<br />
Cardiac Arrest Report is<br />
available at:<br />
http://www.stjohn.org.nz/<br />
Global/18_11_15_OHCA_<br />
Report_2015_HQ_released.pdf<br />
pleased to be providing the Non-<br />
Emergency Patient Transport Service<br />
across the Thames Valley and we<br />
are determined to deliver the best<br />
possible service to patients.<br />
“I would like to thank all the people<br />
who worked so hard to ensure<br />
a smooth transition to the new<br />
contract.”<br />
The service is available to all patients<br />
who meet the eligibility criteria,<br />
which are in place to ensure that<br />
resources are available to those<br />
patients who need them most.<br />
Spread your ambulance news across the world by emailing us at: editor@ambulancetoday.co.uk<br />
94 Spring 2016 | <strong>Ambulance</strong>today
Introducing Stryker Powerload system and XPS expandable patient surface<br />
Stryker Corporation is one of<br />
the world’s leading medical<br />
technology companies<br />
Stryker’s products include<br />
implants used in joint<br />
replacement and trauma<br />
surgeries; surgical equipment<br />
and surgical navigation<br />
systems; endoscopic and<br />
communications systems;<br />
patient handling and<br />
emergency medical equipment;<br />
neurosurgical, neurovascular<br />
and spinal devices; as well as<br />
other medical device products<br />
used in a variety of medical<br />
specialties.<br />
Stryker EMS<br />
Stryker EMS is the global provider<br />
of industry-first patient transport<br />
products. If you are working in<br />
emergency services, you are at risk<br />
of injury. Whether caused by sudden,<br />
traumatic acute failure or cumulative<br />
trauma failure, injury will not only<br />
shorten careers but will also reduce<br />
operational efficiency.<br />
Having established a long<br />
term relationship with Jigsaw<br />
Medical since their inception,<br />
SP Services were keen to<br />
discuss the idea of designing<br />
some new medical bags with<br />
them.<br />
Mother & Baby Transported<br />
Together, Problem Solved - the<br />
only system on the market that<br />
allows an adult and baby to be<br />
transported safely together in<br />
one <strong>Ambulance</strong>.<br />
An emotive issue and currently<br />
incurring major cost to the NHS,<br />
FERNO KangooFix is the answer to<br />
this problem;<br />
• Cost saving – reduce number of<br />
vehicles and resources required to<br />
transport mother and baby<br />
• Safest system ever developed<br />
– baby securely harnessed to mother<br />
Stryker EMS is dedicated to<br />
delivering best-in-class solutions<br />
for real industry issues that reduce<br />
risk of injuries to the caregiver and<br />
patients alike. We have focused our<br />
efforts to address high risk injury<br />
areas including: transferring a patient<br />
up and down stairs, raising and<br />
lowering a patient on the cot, and<br />
loading and unloading into and out<br />
of an ambulance.<br />
Singular Focus. Global Reach.<br />
Stryker EMS engineering and<br />
design teams focus on continuous<br />
innovation globally with the singular<br />
goal of improving patient safety and<br />
reducing injuries among medics<br />
and caregivers. With scientifically<br />
proven results, our customers have<br />
experienced reduced Worker’s<br />
compensation costs, injuries, and<br />
lost or modified work days, while<br />
improving recruitment and retention<br />
through the development of these<br />
proven technologies.<br />
Power-LOAD System: Loading and<br />
unloading at the touch of a button<br />
Extensive discussions between<br />
senior Jigsaw Medical clinicians and<br />
the SP Parabag development team<br />
regarding the content and design<br />
of the bags resulted in a range of<br />
brand new, fully bespoke bags, made<br />
specifically for Jigsaw Medical for use<br />
on their NHS contracted ambulances<br />
and RRVs.<br />
By streamlining the equipment to<br />
only the essential items needed to<br />
provide the very best in medical<br />
care, two existing SP bags were<br />
amalgamated into one, thereby<br />
reducing the weight and load<br />
required to carry the bag by the<br />
ambulance crews. This made both<br />
the bag and Jigsaw staff more<br />
responsive in emergency situations.<br />
Additionally, with Jigsaw experiencing<br />
laid on an ambulance trolley in a<br />
vehicle<br />
• Tested and proven - dynamic<br />
tested to EN1789 (10G) and<br />
TSF2010:2 (20G), CEN compliant<br />
• Intimate contact for mother<br />
and baby – clinically proven to help<br />
in patient management and mother<br />
& baby’s condition during transfers<br />
• Snug cocoon design with<br />
integrated skull cap – keeps baby<br />
warm and secure<br />
• Lightweight and easy to<br />
store – only 1 Kg<br />
Products & Suppliers News<br />
Visit the only daily ambulance news site on the net at:<br />
www.ambulancetoday.co.uk<br />
Power-LOAD is<br />
the first automatic<br />
loading and unloading<br />
system developed<br />
by Stryker for<br />
ambulances. This<br />
eagerly awaited<br />
system operates<br />
at the touch of a<br />
button and therefore considerably<br />
reduces the risk of injury to rescue<br />
workers. The Power-LOAD System<br />
has been developed systematically in<br />
accordance with the guiding principle<br />
of reducing injuries.<br />
XPS – expandable patient<br />
surface<br />
The all-in-one solution for a variety of<br />
patients and environments.<br />
XPS is there when you need it.<br />
XPS provides an expanded patient<br />
surface area that can easily be<br />
retrofitted with compatible cots. XPS<br />
is adjustable with 7 locking positions<br />
and includes a wider mattress that<br />
reduces transfer gap and is designed<br />
with patient comfort in mind. This<br />
SP Services and Jigsaw Medical unveil bespoke medical bags<br />
Richard McManus - Jigsaw Medical Director<br />
of Clinical Services<br />
a sustained period of unrivalled<br />
growth in the industry, the bags have<br />
also been designed to custom fit<br />
their brand new ambulances that<br />
been have recently added to the<br />
Jigsaw medical fleet. SP, Jigsaw and the<br />
vehicle builder have worked together<br />
to ensure that all the bags fit the<br />
new cupboard spaces thus making<br />
everything more efficient and safer.<br />
Jigsaw Medical Director of Clinical<br />
Services, Richard McManus stated:<br />
“We are pleased to have worked so<br />
closely with a company as reputable<br />
as SP Services and we are really<br />
Ferno Kangoo Fix fixes mother & baby transport problem<br />
For more information or to<br />
trial KangooFix please call<br />
+44(0) 1274 851 999 or email;<br />
sales@ferno.co.uk<br />
solution helps address growing<br />
obesity trends and supports a variety<br />
of patients and environments.<br />
Cots with XPS meet current tip<br />
stability standards for both patient<br />
and provider safety. Engineered for<br />
durability and cleanability, with a<br />
6061-T6 aluminum core and overmold<br />
design.<br />
Certified to IEC 60601-1 for Power-<br />
PRO XT and Power-PRO TL.<br />
BS-EN 1789 for Power-PRO XT,<br />
Power-PRO TL, and Performance-<br />
PRO XT.<br />
For more information<br />
contact us at ems.info@<br />
stryker.com or visit www.<br />
strykerems.com.<br />
happy with<br />
the results. We<br />
have received<br />
nothing but<br />
positive<br />
feedback from<br />
the ambulance teams out around the<br />
country, and look forward to growing<br />
and developing our relationship with<br />
SP and Parabag in the future.<br />
For further information<br />
contact:<br />
SP Service Limited<br />
T: 01952 288 999<br />
Check out:<br />
www.spservices.co.uk,<br />
www.spservices.co.uk/<br />
facebook<br />
and www.spervices.co.uk/<br />
twitter<br />
Book your place at EMS 2016 in Copenhagen at: www.ems2016.org<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
95
Products & Suppliers News<br />
Visit the only daily ambulance news site on the net at:<br />
www.ambulancetoday.co.uk<br />
The Falck VL challenge<br />
370 vehicles. 40 stations. 900 new colleagues. 4 months.<br />
Winning a contract looks good<br />
on paper but is hardly a walk<br />
in the park. Just like Father<br />
Christmas needs his elves,<br />
behind each contract won lies<br />
many hardworking colleagues<br />
striving to put things together<br />
on time. The same was true for<br />
Falck VL in Spain.<br />
In 2015, Falck’s activities in the<br />
metropolitan area of Barcelona grew<br />
fivefold. In the span of four months,<br />
Falck had to acquire, transform and<br />
deploy more than 380 vehicles; train<br />
900 workers; contract and build 40<br />
stations; and prepare to increase<br />
capacity from managing 600 daily<br />
services to 3500. How did they<br />
do it? Why, by dividing the work<br />
into different areas of action and<br />
dedicating a team for each, of course.<br />
1 - Management and<br />
coordination<br />
This office is dedicated to the<br />
deployment process and to the<br />
control and management of start-up<br />
operations. It controls more than 300<br />
If you have a mattress tear<br />
you can now fix it properly -<br />
listening to our customers we<br />
have developed a simple tears<br />
and cuts clinical repair system,<br />
which is easy to apply and<br />
works across a range of softbased<br />
products;<br />
• <strong>Ambulance</strong> Trolley<br />
Mattresses<br />
• Vacuum Mattresses & Splints<br />
• Frac immobilisers<br />
And even as a clinical patch for<br />
torn ambulance vehicle seats<br />
different activities for the deployment<br />
and performs a continuous follow<br />
back of dates and KPI to ensure<br />
all processes, to identify critical<br />
points, areas or activities that need<br />
strengthening.<br />
2 - Human resources<br />
A specialized call centre personally<br />
welcomed employees, confirmed<br />
their personal data and informed<br />
them about a special online tool<br />
used by Falck VL. This tool allows<br />
each worker to receive meeting<br />
notifications and training courses,<br />
learn about the company and work<br />
procedures and resolve any queries.<br />
First <strong>Ambulance</strong> bus in the Netherlands<br />
On a beautiful Friday<br />
afternoon in April the very<br />
first <strong>Ambulance</strong> Bus in the<br />
Netherlands was unveiled<br />
at the international airport<br />
for the Northern part of<br />
the Netherlands, Groningen<br />
Airport Eelde.<br />
The ambulance bus is an essential<br />
element in a new strategy for<br />
handling large scale incidents in<br />
this region of the Netherlands. The<br />
ambulance bus will be jointly used<br />
by the three regional ambulance<br />
services.<br />
In 2016 the Netherlands has<br />
changed their large scale incident<br />
organizational model. One of the<br />
elements of the new model is the<br />
introduction of a “100 ambulances”<br />
standard. The Northern region had<br />
done extensive simulations based on<br />
the new standard. It quickly became<br />
obvious that the national model is<br />
not well suited for this largely rural<br />
region.<br />
The regional capacity is limited and<br />
regional hospitals would quickly<br />
reach their maximum capacity, which<br />
would result in a domino effect of<br />
ambulances driving to more remote<br />
hospitals taking them far from their<br />
designated coverage areas. This<br />
would lower regional ambulance<br />
availability for “normal incidents” to<br />
an unacceptable level.<br />
Fix it properly with FERNO CleanPatch<br />
CleanPatch comes in three different<br />
sizes and can be used for a number<br />
of applications.<br />
It patches, protects and prolongs the<br />
life of a product without having to<br />
pay for an expensive replacement,<br />
it has been put through rigorous<br />
3 - IT<br />
Falck VL has modernized its IT<br />
infrastructure. An ERP (Enterprise<br />
resource planning) tool was put<br />
in place to improve accounting,<br />
management and processing of<br />
corporate resources, a tool for<br />
managing HR and rosters, fleet<br />
management and PTS management<br />
were also put in place.<br />
4 - Stations:<br />
40 new stations meant scouting for<br />
sites, building quality facilities for<br />
workers, equipment and more. To do<br />
this, our colleagues worked with one<br />
of the most important real estate<br />
companies in Spain. They helped<br />
them with the different locations and<br />
renovation projects.<br />
5 – Patient Transport Services<br />
(PTS) Dispatch Centre:<br />
PTS operations in Falck VL represent<br />
an increase of activity by 500%.<br />
The control centre has been<br />
expanded from five positions to<br />
20, the telephone capacity has<br />
been increased, as well as back-up<br />
A large scale table top exercise<br />
confirmed the results from the<br />
simulation and confirmed the need<br />
for more onsite treatment capacity.<br />
Market research was used to check<br />
if suitable second-hand buses would<br />
be available. The answer was yes,<br />
although not in our preferred hybrid<br />
drivetrain version.<br />
A suitable second-hand bus was<br />
quickly found and bought. The actual<br />
bus had an ideal lay out for the<br />
conversion that encompassed a<br />
new interior with six fully equipped<br />
treatment stretchers. All stretcher<br />
are equipped with Corpuls monitors<br />
and the bus has a cutting edge<br />
centralised early detection system for<br />
patient deterioration.<br />
The <strong>Ambulance</strong> bus conversion<br />
was done by Visser Leeuwarden, a<br />
well-known Dutch manufacturer of<br />
ambulances and emergency services.<br />
Visser Leeuwarden is part of the<br />
clinical trials (white papers available)<br />
and is ready for immediate use, today.<br />
CleanPatch saves money and<br />
improves on infection control<br />
standards<br />
lines using digital networks and a<br />
wireless network. The Computer<br />
Aided Dispatch software is also used,<br />
which enables to automatically and<br />
intelligently schedule vehicles and<br />
services.<br />
6 – Vehicles<br />
140 emergency vehicles, 220<br />
PTS vehicles and 10 logistics<br />
and coordination vehicles were<br />
deployed - all of which were new.<br />
For their commissioning, processes<br />
of acquisition, transformation,<br />
equipment, testing and<br />
transportation had to be performed.<br />
Several audits by the regional<br />
government were also performed to<br />
ensure tender requirements.<br />
international operating Albert Ziegler<br />
GmbH & Co and is partner of the<br />
German Ambulanz Mobile.<br />
Contact:<br />
• <strong>Ambulance</strong> services<br />
• http://www.<br />
ambulancezorggroningen.nl/<br />
• http://www.rav-fryslan.nl/<br />
• http://www.<br />
umcgambulancezorg.nl/<br />
• Bus conversions<br />
• https://www.<br />
visserleeuwarden.nl/<br />
• POC Equipment<br />
• Harry Meijer, h.meijer@rav.<br />
nl<br />
• POC Large scale incident<br />
organization<br />
• Klaas Jan Hulzebos,<br />
KlaasJan.Hulsebos@<br />
ambulancezorggroningen.nl<br />
For more information call<br />
+44(0) 1274 851 999 or email;<br />
sales@ferno.co.uk<br />
96 Spring 2016 | <strong>Ambulance</strong>today
Products & Suppliers News<br />
Visit the only daily ambulance news site on the net at:<br />
www.ambulancetoday.co.uk<br />
KARL STORZ: The Leader in the field of Airway Management<br />
KARL STORZ offers a<br />
complete range of devices for<br />
Airway Management which can<br />
minimize the complications<br />
associated with difficult<br />
intubations.<br />
Designed for pre-hospital settings,<br />
the waterproof C-MAC ® PM<br />
(Pocket Monitor) is combined with<br />
highly durable reusable C-MAC ®<br />
video laryngoscope blades. The OTI<br />
(Open-To-Intubate) display gets<br />
activated automatically when the<br />
monitor is turned open.<br />
Standard shaped MAC blades<br />
for adults and MILLER blades for<br />
pediatrics are available with the<br />
Laerdal Launches SimMan ALS<br />
In an effort to improve<br />
quality and safety, training is<br />
increasingly being held in the<br />
same environment as patients<br />
would normally be treated.<br />
In situ simulation training<br />
has been found to have a<br />
positive impact on learners’<br />
performance but has presented<br />
challenges to emergency<br />
healthcare community.<br />
This is due to the fact emergency<br />
healthcare providers have to perform<br />
in many different locations, from<br />
pre-hospital, on scene assessment<br />
and management to definitive care in<br />
a hospital. Laerdal’s newest addition<br />
to their SimMan family can help fulfil<br />
these unique training requirements.<br />
SimMan ALS has a mobile, durable,<br />
and self-contained design so training<br />
can be performed wirelessly and “on<br />
the move”. Designed for complete<br />
training of ACLS and ALS courses<br />
it is especially suited to train in the<br />
rapid detection and stabilisation of a<br />
deteriorating patient.<br />
For an entry level simulator, SimMan<br />
ALS comes well prepared to make<br />
simulation more clinically relevant<br />
benefit of a low learning curve<br />
and the option to look directly if<br />
needed. The additional D-BLADE<br />
is highly curved to manage anterior<br />
airways.<br />
Part of the set is a backup battery<br />
pack for emergency situations<br />
which allows the C-MAC ® blade to<br />
be used as a direct laryngoscope.<br />
The additional BOEDEKER-<br />
MAGILL forceps adapted to the<br />
MAC blades are designed for<br />
foreign bodies removals under<br />
video view.<br />
to a wide range of healthcare<br />
disciplines. Technologies have been<br />
integrated into the simulator’s skin<br />
so that simple add-ons can be<br />
used to enhance training when<br />
needs arise. This means, ultrasound<br />
diagnostics can be included into<br />
simulation scenarios. Also, using<br />
a live defibrillator, defibrillation<br />
training events can be automatically<br />
O&H Vehicle Conversions launches ‘TITAN’ platform<br />
incorporating weight-saving technology<br />
Innovative design delivers minimum 200kg higher payload and lower converted vehicle weight, across<br />
multiple platforms<br />
The first of the Titan-based products is the new, Titan Welfare Vehicle - launching at The Commercial<br />
Vehicle Show, offering lighter-weight vehicle conversions for moving the transient workforce<br />
O&H Vehicle Conversions is<br />
claiming a first-to-market for<br />
its innovative new welfare<br />
vehicle (crew vehicle) concept<br />
– ‘Titan’ – which delivers<br />
a minimum 200kg higher<br />
payload capacity as well as<br />
lower converted-vehicle<br />
weight, across multiple<br />
platforms. Titan design uses<br />
ultra-durable, composite<br />
materials that reduce vehicle<br />
wear, improve co2 emissions<br />
and cut fuel consumption<br />
according to O&H, which is<br />
launching Titan today.<br />
The first Titan welfare vehicles have<br />
been produced for SHB and will be<br />
exhibited at this year’s Commercial<br />
Vehicle Show on the Webasto<br />
stand. In addition to this, Renault<br />
will be hosting O&H’s Renault<br />
Master Titan conversion on the<br />
Renault stand.<br />
Key features of the Titan, in addition<br />
to its weight-saving capabilities and<br />
higher capacity are a unique power<br />
re-charge facility; a larger saloon;<br />
one-piece, fully wash-down interior<br />
panels; easy-access maintenance,<br />
designed to reduce vehicle off<br />
road (VOR) time; smart electrical<br />
management and euro 6 alternator<br />
charging systems.<br />
“The Titan Welfare Vehicle is a winwin<br />
purchase for any fleet manager,<br />
Multimover-a safe patient lifting and space saving solution<br />
Orvecare’s Multimover has<br />
a unique design that ensures<br />
the safe, secure lifting and<br />
movement of patients when<br />
time and space is a restriction.<br />
Working with front line paramedics<br />
and clinicians, to gain first-hand<br />
experience of the operational<br />
difficulties, has been crucial in<br />
the development and design of<br />
Multimover.<br />
Manufactured<br />
in the UK from<br />
a lightweight,<br />
fluid resistant,<br />
latex free<br />
nonwoven<br />
material.<br />
The twelve<br />
strategically<br />
placed lifting handles ensures each<br />
patient’s weight is evenly balanced<br />
to optimise safe lifting<br />
positions and has been<br />
independently tested to<br />
have a safe lifting weight<br />
of 250kgs equivalent to<br />
40 stone.<br />
Each Multimover is<br />
individually packaged<br />
and at only 400g can be<br />
easily stored either in an equipment<br />
bag or carried on the person.<br />
The C-MAC ® PM is widely accepted<br />
and used in several air-rescue and<br />
ground based EMS systems.<br />
Contact:<br />
KARL STORZ GmbH & Co. KG<br />
Dr. Karl-Storz-Str. 34, 78532<br />
Tuttlingen, Germany<br />
Tel.: +49 7461 708-0<br />
Fax: +49 7461 708-105<br />
E-Mail: c-mac@karlstorz.com<br />
captured for assessment and debrief<br />
to ensure teams are delivering high<br />
performance CPR.<br />
All this should ensure learners’<br />
using SimMan ALS can work to<br />
improve reactions, performance, and<br />
teamwork in the environments they<br />
will have to perform.<br />
For more information,<br />
visit www.laerdal.com/<br />
SimManALS Stay in touch<br />
with Laerdal Medical on<br />
Twitter: @LaerdalEurope<br />
with the lower weight and higher<br />
capacity that our new technology<br />
delivers” says O&H Sales and<br />
Marketing Director Lee Bott.<br />
For more information on<br />
O&H Vehicle Conversions<br />
please visit:<br />
www.ohvc.co.uk<br />
or call 01405 769867<br />
For more information please<br />
contact:<br />
Tel: +44 (0) 1482 625 333<br />
Fax: +44 (0) 1482 625 355<br />
Email: service@orvec.com<br />
www.orvecare.com<br />
Spring 2016 | <strong>Ambulance</strong>today<br />
97
Products & Suppliers News<br />
Visit the only daily ambulance news site on the net at:<br />
www.ambulancetoday.co.uk<br />
Introducing the Xplore XSLATE D10 Fully Rugged<br />
Android Tablet PC for <strong>Ambulance</strong> and EMS Operations<br />
The Xplore XSLATE D10<br />
fully rugged tablet PC is<br />
uniquely designed to deliver<br />
the real-time data and rugged<br />
protection required for fast,<br />
hands-on EMS response<br />
capabilities – even in extreme<br />
conditions.<br />
Leveraging the flexibility and security<br />
of Android , the 10.1” sunlightviewable<br />
D10 works twice as fast<br />
and stores twice as much as most<br />
other rugged Android devices<br />
in support of Electronic Patient<br />
Care Reporting (ePCR) and other<br />
mobile clinical applications. It is<br />
the only device truly capable of<br />
improving quality care and records<br />
management long-term.<br />
As Body Worn Cameras<br />
(BWC) become more<br />
prominent - worn by police,<br />
front line ambulance staff,<br />
traffic wardens and security<br />
guards to name a few, we<br />
can sometimes forget the<br />
additional benefits these<br />
wearable cameras offer.<br />
Edesix provides frontline workers<br />
across the globe with tools for<br />
deterring violence, capturing<br />
evidence and convicting acts of lawbreaking,<br />
BWCs are also helping our<br />
emergency services to save lives.<br />
Alfred Bekker API Ltd<br />
specialise in the design and<br />
manufacture of Patient<br />
Transport, Rapid Response,<br />
Minibus and Wheelchair<br />
Accessible Vehicles. We convert<br />
high quality and bespoke<br />
vehicles onsite at our purpose<br />
built factory based in Driffield,<br />
East Yorkshire. We are also<br />
the sole UK distributor of the<br />
RolliBox System and API Flexi-<br />
Ramp kits.<br />
The Single wheelchair Patient<br />
Transport conversions by Alfred<br />
Bekker which has full European<br />
Whole Vehicle Type Approval utilises<br />
Whether they’re in the ambulance,<br />
treating a patient, or completing an<br />
electronic health record (EHR) enroute<br />
to the hospital, medics rely on<br />
real-time data to be effective at their<br />
jobs during a patient’s most critical<br />
moments.<br />
With eight standard I/O ports<br />
available all the time and built-in<br />
4G LTE, Wi-Fi ® and Bluetooth ® 4.0<br />
technologies, the D10 allows for fast<br />
retrieval and updating of EHRs and<br />
constant communication between<br />
incident response teams and remote<br />
healthcare advisors.<br />
Streamlined dispatch channels and<br />
built-in GPS routing get crews on-site<br />
faster, and the secure in-ambulance<br />
Body Worn Cameras – Not Just an Evidence Gathering Tool<br />
The Resuscitation Research<br />
Group, University of Edinburgh<br />
The Resuscitation Research Group<br />
(RRG) works on improving Out-of-<br />
Hospital Cardiac Arrest (OHCA)<br />
outcomes. The whole ‘Chain of<br />
Survival’ from the emergency call<br />
through to post-resuscitation care<br />
the patented Flexi-Ramp. The flat<br />
fold ramp was the first of its kind and<br />
allows the boot space to be utilised<br />
when a Wheelchair is not being<br />
transported. The conversion uses<br />
the vehicles original seats meaning<br />
that the best safety and comfort is<br />
achieved for the other passengers.<br />
Winches can be added, along with a<br />
headrest for the wheelchair user. The<br />
vehicle can be made fully wipe down<br />
to adhere to cleaning standards.<br />
The Large Patient Transport<br />
conversions offered by Alfred<br />
Bekker can utilise the unique<br />
RolliBox System. This system<br />
allows the vehicle to carry up to 4<br />
rugged tablet mounting system<br />
creates a safe, vibration-resistant<br />
transport environment.<br />
The Intel®-powered D10 boasts<br />
high field performance ratings as<br />
well. It is IP65 rated, MIL-STD-<br />
810G tested, and ATEX compliant<br />
to withstand the bumps, bruises,<br />
and constant disinfection common<br />
has to be optimised. RRG selected<br />
the Edesix VideoBadge BWC for<br />
their Resuscitation Rapid Response<br />
Unit (3RU).<br />
The Use of a BWC for<br />
Assessment and Debrief<br />
The VideoBadge is securely attached<br />
to the paramedic’s uniform,<br />
requiring only a single-touch to<br />
start recording, leaving hands and<br />
concentration free to focus on<br />
clinical tasks. Footage is encrypted<br />
on the device until it is offloaded to<br />
the VideoManager, complying with<br />
medical confidentiality.<br />
Wheelchair patient transport solutions from Alfred Bekker<br />
Wheelchairs, 7 Seated Passengers<br />
or any combination in between. A<br />
Stretcher can also be added, meaning<br />
that the system can be adjusted<br />
depending on the requirements of<br />
that particular run. The Wheelchairs<br />
places have headrests and threepoint<br />
seatbelts, whilst four-point<br />
secures fold out from the side. This<br />
keeps the system in the vehicle<br />
reducing damage and loss. This<br />
Infection control in under 10 minutes from Sanondaf<br />
Sanondaf are a specialist<br />
disinfection company who<br />
offer advanced environmental<br />
decontamination of vehicles<br />
and clinical spaces through our<br />
highly innovative fogging and<br />
electrostatic spray<br />
devices.<br />
Our process can be<br />
used in any space<br />
regardless of size and<br />
is highly suitable for<br />
vehicles as we use a<br />
dry disinfectant mist which does not<br />
cause any corrosion issues and can<br />
be used on any equipment inside the<br />
vehicle including medical devices, soft<br />
fabrics, electronics and hydraulics.<br />
A typical treatment process is carried<br />
out in under 10 minutes and a<br />
vehicle is available and back in use<br />
within 30 minutes.<br />
Sanondaf achieve a kill rate above<br />
99.99% and our process is used<br />
within NHS Trusts, laboratories, and<br />
care facilities. Sanondaf is the ideal<br />
solution for any decontamination<br />
needs and our treatments can be<br />
used to deal with an outbreak or<br />
as part of a maintenance regime<br />
to continually reduce and remove<br />
bio-burden.<br />
on the job – even in Hazardous<br />
Locations – and it will keep up with<br />
fast-paced tempo first responders<br />
must maintain regardless of the<br />
rain, bright sunshine, dust, or snow.<br />
Several data entry options are<br />
available (via touchscreen, stylus,<br />
keyboard, barcode, or camera) for<br />
real-time documentation of patient<br />
data into multiple applications – all<br />
of which will run strong for up to<br />
20 hours with the hot swappable<br />
battery option.<br />
Contact: Manjit Dosanjh<br />
+44 (0) 1926 356 560<br />
mdosanjh@xploretech.com<br />
www.xploretech.com<br />
Footage is used by the team to audit<br />
team performance, protocols and<br />
equipment to improve practice.<br />
“VideoBadge has made it possible to<br />
evaluate new equipment while out in<br />
the field. We can measure key aspects<br />
of performance in ways which were not<br />
previously possible” Dr Gareth Clegg –<br />
RRG lead.<br />
For more information on the<br />
Edesix solution, or to sign<br />
up for a free trial, contact a<br />
member of our team on<br />
0131 510 0232 quoting code<br />
‘AMB1’, today!<br />
system can also be adapted for City<br />
and Rural Patient Transport and High<br />
Dependency Vehicles.<br />
Contact:<br />
Oliver Shaw<br />
Business Development<br />
Alfred Bekker API<br />
Oli.shaw@alfredbekker.com<br />
01377 241 700<br />
07495 455 745<br />
Contact us now to arrange<br />
a demonstration and trial of<br />
the Sanondaf process. We<br />
have national coverage across<br />
the UK and internationally<br />
in Ireland, Malta, Ecuador,<br />
Mexico, Singapore and<br />
Thailand.<br />
Email:<br />
Stuartwhite@sanondaf.co.uk<br />
Telephone: 01236 702029<br />
Website: www.sanondaf.co.uk<br />
98 Spring 2016 | <strong>Ambulance</strong>today
‘Quality without Compromise”<br />
BAUS AT UK Limited<br />
Suite F1,<br />
6 Whittle Road,<br />
Ferndown Industrial Estate,<br />
Wimborne, Dorset BH21 7RU<br />
Mob: +44 (0)7974 940 121<br />
Tel: +44 (0)1425 602 999<br />
Fax: +44 (0)1425 602 602<br />
info@baus-at.co.uk<br />
www.baus-at.co.uk<br />
B.A.U.S. AT Sp. z o.o.<br />
Polna 134 - 136<br />
PL-87-100 Torun<br />
Tel: +48 728 891 442<br />
Fax: +48 56 645 3634<br />
info@baus-at.com<br />
www.baus-at.com
The Power<br />
from Stryker<br />
For more information contact us at<br />
ems.info@stryker.com<br />
www.strykerems.com<br />
A surgeon must always rely on his or her own clinical judgement when<br />
deciding which treatments and procedures to use with patients. For<br />
verifying availability of Stryker products in your area please contact your<br />
Stryker representative. Copyright © 2016 Stryker. The product shown<br />
above is CE marked. Stryker Corporation or its divisions or other corporate<br />
affiliated entities own, use or have applied for the following trademarks or<br />
Service marks: Stryker, Power-PRO XT, XPS, Power-LOAD.