You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
abstracts<br />
respectively. Giemsa staining revealed tumor cells in 60% (15/25) at baseline and in<br />
67% (8/12) after 3 rd cycle. PD-1 expression was observed in 71.4% (10/14) and 10% (1/<br />
10) (p = 0.044) <strong>of</strong> the CTC-positive patients at baseline and after the 3 rd , respectively.<br />
Conversely, PD-L1 was observed in 42,9% (6/14) and 50% (5/10) (p = 0.311) <strong>of</strong> the<br />
CTC-positive patients at baseline and after the 3 rd cycle. Among the total number <strong>of</strong><br />
detected CTCs, 47.8% were PD-1-positive at baseline and 30% after the 3 rd cycle<br />
whereas, 35.7% and 50% at baseline and after the 3 rd cycle, respectively, were<br />
PD-L1-positive.<br />
Conclusions: PD-1- and PD-L1 positive CTCs can be observed during the treatment <strong>of</strong><br />
metastatic NSCLC, suggesting that they can be used as a potential biomarker to<br />
monitor the expression <strong>of</strong> PD-L1 on tumor cells during the clinical phases <strong>of</strong> the<br />
disease and understand the mechanisms <strong>of</strong> tumor immune escape.<br />
Legal entity responsible for the study: N/A<br />
Funding: Laboratory <strong>of</strong> Translational <strong>Oncology</strong>, School <strong>of</strong> Medicine, University <strong>of</strong> Crete<br />
Disclosure: All authors have declared no conflicts <strong>of</strong> interest.<br />
Methods: Peripheral blood was collected from 124 pts with diverse staging and<br />
histology at three clinical sites prior to diagnostic biopsy, with some having follow-up<br />
draws. All nucleated cells were plated onto glass slides and circulating cells <strong>of</strong> interest<br />
identified by immun<strong>of</strong>luorescence and morphological features. Prognostic capacity <strong>of</strong><br />
PD-L1(+) cells (CK + /-, CD45-, PD-L1 + , malignant nuclear morphology) were<br />
assessed with Kaplan-Meier and Cox Proportional Hazard (PH) models.<br />
Results:<br />
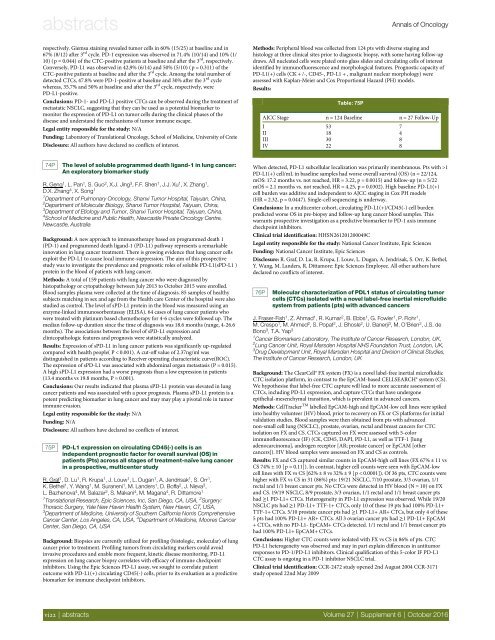
Table: 75P<br />
<strong>Annals</strong> <strong>of</strong> <strong>Oncology</strong><br />
AJCC Stage n = 124 Baseline n = 27 Follow-Up<br />
I 53 7<br />
II 18 4<br />
III 30 8<br />
IV 22 8<br />
74P<br />
The level <strong>of</strong> soluble programmed death ligand-1 in lung cancer:<br />
An exploratory biomarker study<br />
R. Geng 1 ,L.Pan 1 , S. Guo 2 , X.J. Jing 3 , F.F. Shen 1 , J.J. Xu 1 , X. Zhang 1 ,<br />
D.X. Zhang 4 , X. Song 1<br />
1 Department <strong>of</strong> Pulmonary <strong>Oncology</strong>, Shanxi Tumor Hospital, Taiyuan, China,<br />
2 Department <strong>of</strong> Molecular Biology, Shanxi Tumor Hospital, Taiyuan, China,<br />
3 Department <strong>of</strong> Etiology and Tumor, Shanxi Tumor Hospital, Taiyuan, China,<br />
4 School <strong>of</strong> Medicine and Public Health, Newcastle Private <strong>Oncology</strong> Centre,<br />
Newcastle, Australia<br />
Background: A new approach to immunotherapy based on programmed death 1<br />
(PD-1) and programmed death ligand-1 (PD-L1) pathway represents a remarkable<br />
innovation in lung cancer treatment. There is growing evidence that lung cancer cells<br />
exploit the PD-L1 to cause local immune-suppression. The aim <strong>of</strong> this prospective<br />
study was to investigate the prevalence and prognostic roles <strong>of</strong> soluble PD-L1(sPD-L1 )<br />
protein in the blood <strong>of</strong> patients with lung cancer.<br />
Methods: A total <strong>of</strong> 159 patients with lung cancer who were diagnosed by<br />
histopathology or cytopathology between July 2013 to October 2015 were enrolled.<br />
Blood samples plasma were collected at the time <strong>of</strong> diagnosis. 85 samples <strong>of</strong> healthy<br />
subjects matching in sex and age from the Health care Center <strong>of</strong> the hospital were also<br />
studied as control. The level <strong>of</strong> sPD-L1 protein in the blood was measured using an<br />
enzyme-linked immunosorbentassay (ELISA). 64 cases <strong>of</strong> lung cancer patients who<br />
were treated with platinum based chemotherapy for 4-6 cycles were followed up. The<br />
median follow-up duration since the time <strong>of</strong> diagnosis was 18.6 months (range, 4-26.6<br />
months). The associations between the level <strong>of</strong> sPD-L1 expression and<br />
clinicopathologic features and prognosis were statistically analyzed.<br />
Results: Expression <strong>of</strong> sPD-L1 in lung cancer patients was significantly up-regulated<br />
compared with health people( P < 0.001). A cut-<strong>of</strong>f value <strong>of</strong> 2.37ng/ml was<br />
distinguished in patients according to Receiver operating characteristic curve(ROC).<br />
The expression <strong>of</strong> sPD-L1 was associated with abdominal organ metastasis (P = 0.015).<br />
A high sPD-L1 expression had a worse prognosis than a low expression in patients<br />
(13.4 months vs 19.8 months, P = 0.001).<br />
Conclusions: Our results indicated that plasma sPD-L1 protein was elevated in lung<br />
cancer patients and was associated with a poor prognosis. Plasma sPD-L1 protein is a<br />
potent predicting biomarker in lung cancer and may may play a pivotal role in tumor<br />
immune evasion.<br />
Legal entity responsible for the study: N/A<br />
Funding: N/A<br />
Disclosure: All authors have declared no conflicts <strong>of</strong> interest.<br />
75P<br />
PD-L1 expression on circulating CD45(-) cells is an<br />
independent prognostic factor for overall survival (OS) in<br />
patients (Pts) across all stages <strong>of</strong> treatment-naïve lung cancer<br />
in a prospective, multicenter study<br />
R. Graf 1 ,D.Lu 1 , R. Krupa 1 , J. Louw 1 , L. Dugan 1 , A. Jendrisak 1 ,S.Orr 1 ,<br />
K. Bethel 1 ,Y.Wang 1 , M. Suraneni 1 , M. Landers 1 , D. B<strong>of</strong>fa 2 , J. Nieva 3 ,<br />
L. Bazhenova 4 , M. Salazar 2 , S. Makani 4 , M. Magana 4 , R. Dittamore 1<br />
1 Translational Research, Epic Sciences, Inc, San Diego, CA, USA, 2 Surgery:<br />
Thoracic Surgery, Yale New Haven Health System, New Haven, CT, USA,<br />
3 Department <strong>of</strong> Medicine, University <strong>of</strong> Southern California Norris Comprehensive<br />
Cancer Center, Los Angeles, CA, USA, 4 Department <strong>of</strong> Medicine, Moores Cancer<br />
Center, San Diego, CA, USA<br />
Background: Biopsies are currently utilized for pr<strong>of</strong>iling (histologic, molecular) <strong>of</strong> lung<br />
cancer prior to treatment. Pr<strong>of</strong>iling tumors from circulating markers could avoid<br />
invasive procedures and enable more frequent, kinetic disease monitoring. PD-L1<br />
expression on lung cancer biopsy correlates with efficacy <strong>of</strong> immune checkpoint<br />
inhibitors. Using the Epic Sciences PD-L1 assay, we sought to correlate patient<br />
outcome with PD-L1(+) circulating CD45(-) cells, prior to its evaluation as a predictive<br />
biomarker for immune checkpoint inhibitors.<br />
When detected, PD-L1 subcellular localization was primarily membranous. Pts with >1<br />
PD-L1(+) cell/mL in baseline samples had worse overall survival (OS) (n = 22/124,<br />
mOS: 17.2 months vs. not reached, HR = 3.22, p = 0.0015) and follow-up (n = 5/22<br />
mOS = 2.1 months vs. not reached, HR = 4.25, p = 0.0302). High baseline PD-L1(+)<br />
cell burden was additive and independent to AJCC staging in Cox PH models<br />
(HR = 2.32, p = 0.0447). Single-cell sequencing is underway.<br />
Conclusions: In a multicenter cohort, circulating PD-L1(+)/CD45(-) cell burden<br />
predicted worse OS in pre-biopsy and follow-up lung cancer blood samples. This<br />
warrants prospective investigation as a predictive biomarker to PD-1 axis immune<br />
checkpoint inhibitors.<br />
Clinical trial identification: HHSN261201200049C<br />
Legal entity responsible for the study: National Cancer Institute, Epic Sciences<br />
Funding: National Cancer Institute, Epic Sciences<br />
Disclosure: R. Graf, D. Lu, R. Krupa, J. Louw, L. Dugan, A. Jendrisak, S. Orr, K. Bethel,<br />
Y. Wang, M. Landers, R. Dittamore: Epic Sciences Employee. All other authors have<br />
declared no conflicts <strong>of</strong> interest.<br />
76P<br />
Molecular characterization <strong>of</strong> PDL1 status <strong>of</strong> circulating tumor<br />
cells (CTCs) isolated with a novel label-free inertial micr<strong>of</strong>luidic<br />
system from patients (pts) with advanced cancers<br />
J. Fraser-Fish 1 , Z. Ahmad 1 , R. Kumar 2 , B. Ebbs 1 , G. Fowler 1 , P. Flohr 1 ,<br />
M. Crespo 1 , M. Ahmed 2 , S. Popat 2 , J. Bhosle 2 , U. Banerji 3 ,M.O’Brien 2 , J.S. de<br />
Bono 3 , T.A. Yap 3<br />
1 Cancer Biomarkers Laboratory, The Institute <strong>of</strong> Cancer Research, London, UK,<br />
2 Lung Cancer Unit, Royal Marsden Hospital NHS Foundation Trust, London, UK,<br />
3 Drug Development Unit, Royal Marsden Hospital and Division <strong>of</strong> Clinical Studies,<br />
The Institute <strong>of</strong> Cancer Research, London, UK<br />
Background: The ClearCell® FX system (FX) is a novel label-free inertial micr<strong>of</strong>luidic<br />
CTC isolation platform, in contrast to the EpCAM-based CELLSEARCH® system (CS).<br />
We hypothesise that label-free CTC capture will lead to more accurate assessment <strong>of</strong><br />
CTCs, including PD-L1 expression, and capture CTCs that have undergone<br />
epithelial-mesenchymal transition, which is prevalent in advanced cancers.<br />
Methods: CellTracker TM labelled EpCAM-high and EpCAM-low cell lines were spiked<br />
into healthy volunteer (HV) blood, prior to recovery on FX or CS platforms for initial<br />
validation studies. Blood samples were then obtained from pts with advanced<br />
non-small cell lung (NSCLC), prostate, ovarian, rectal and breast cancers for CTC<br />
isolation on FX and CS. CTCs captured on FX were assessed with 5-color<br />
immun<strong>of</strong>luorescence (IF) (CK, CD45, DAPI, PD-L1, as well as TTF-1 [lung<br />
adenocarcinoma], androgen receptor [AR; prostate cancer] or EpCAM [other<br />
cancers]). HV blood samples were assessed on FX and CS as controls.<br />
Results: FX and CS captured similar counts in EpCAM-high cell lines (FX 67% ± 11 vs<br />
CS 74% ± 10 [p = 0.11]). In contrast, higher cell counts were seen with EpCAM-low<br />
cell lines with FX vs CS [62% ± 8 vs 32% ± 9 [p < 0.0001]). Of 36 pts, CTC counts were<br />
higher with FX vs CS in 31 (86%) pts: 19/21 NSCLC, 7/10 prostate, 3/3 ovarian, 1/1<br />
rectal and 1/1 breast cancer pts. No CTCs were detected in HV blood (N = 10) on FX<br />
and CS. 19/19 NSCLC, 8/9 prostate, 3/3 ovarian, 1/1 rectal and 1/1 breast cancer pts<br />
had ≥1 PD-L1+ CTCs. Heterogeneity in PD-L1 expression was observed. While 19/20<br />
NSCLC pts had ≥1 PD-L1+ TTF-1+ CTCs, only 10 <strong>of</strong> these 19 pts had 100% PD-L1+<br />
TTF-1+ CTCs. 5/10 prostate cancer pts had ≥1 PD-L1+ AR+ CTCs, but only 4 <strong>of</strong> these<br />
5 pts had 100% PD-L1+ AR+ CTCs. All 3 ovarian cancer pts had ≥1 PD-L1+ EpCAM<br />
+ CTCs, with no PD-L1- EpCAM+ CTCs detected. 1/1 rectal and 1/1 breast cancer pts<br />
had 100% PD-L1+ EpCAM+ CTCs.<br />
Conclusions: Higher CTC counts were isolated with FX vs CS in 86% <strong>of</strong> pts. CTC<br />
PD-L1 heterogeneity was observed and may in part explain differences in antitumor<br />
responses to PD-1/PD-L1 inhibitors. Clinical qualification <strong>of</strong> this 5-color IF PD-L1<br />
CTC assay is ongoing in a PD-1 inhibitor NSCLC trial.<br />
Clinical trial identification: CCR-2472 study opened 2nd August 2004 CCR-3171<br />
study opened 22nd May 2009<br />
vi22 | abstracts Volume 27 | Supplement 6 | October 2016