Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
THE MAGAZINE FOR NEW ZEALAND’S OPHTHALMIC COMMUNITY<br />
PO BOX 106 954, AUCKLAND CITY 1143<br />
Email: info@nzoptics.co.nz Website: www.nzoptics.co.nz<br />
<strong>Sep</strong>tember <strong>2015</strong><br />
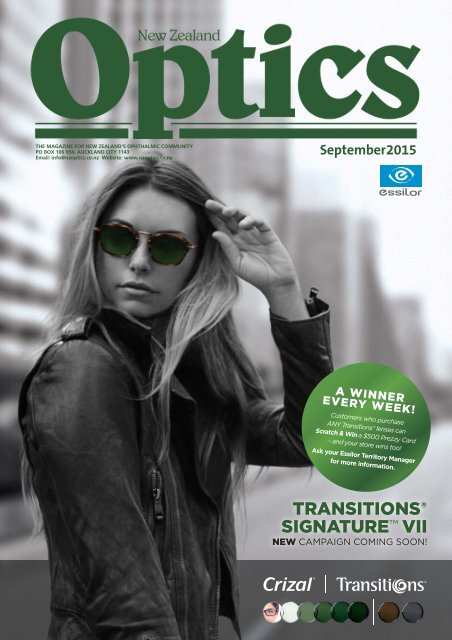
A WINNER<br />
EVERY WEEK!<br />
Customers who purchase<br />
ANY Transitions® lenses can<br />
Scratch & Win a $500 Prezzy Card<br />
- and your store wins too!<br />
Ask your Essilor Territory Manager<br />
for more information.<br />
TRANSITIONS ®<br />
SIGNATURE VII<br />
NEW CAMPAIGN COMING SOON!
Up to<br />
20<br />
hours of<br />
moisture<br />
• Mimics the natural liquid environment of your eyes 3,4<br />
• Matches the pH of healthy tears 5<br />
• <br />
disinfection system 6,7<br />
1,2<br />
1,2<br />
End of day comfort<br />
<br />
References: 1. Data on fi le, Bausch & Lomb Inc. 2. Scheuer C.A, Fridman K.M, Barniak V.L, Burke S.E, Venkatesh S: Retention of conditioning agent hyaluronan on hydrogel contact lenses. Contact Lens Anterior Eye. (2010). 3. Frescura M, Berry M, Corfi eld A, Carrington S, Easty D. Evidence of hyaluronan in human<br />
tears and secretions of conjunctival cultures. Biochem Soc Trans 1994;22:228S. 4. Lerner L, Schwartz D, Hwang D, Howes E, Stern R. Hyaluronan and CD44 in the human cornea and limbal conjunctiva: letter to the editor. Exp Eye Res 1998;67:481-4. 5. Adler’s Physiology of the Eye, 7th ed. RA Moses and WM<br />
Hart eds. Mosby: St Louis, 1987. 6. Data on File, Bausch & Lomb Inc.: Results of in vitro study following FDA/ISO Stand Alone Procedure performed with the addition of organic soil to create a more rigorous test condition. Primary criteria for effective disinfection are defi ned as a reduction in the number of bacteria by<br />
a minimum of 3 logs(99.9%) and a reduction of mold and yeast by a minimum of 1 log (90%) within the recommended disinfection time. All solutions passed FDA/ISO primary stand-alone standard testing without organic soil. Results depict mean log reduction measured after manufacturers’ recommended disinfecting<br />
time (soak only). Biotrue®, Clear Care (AO <strong>Sep</strong>t Plus), RevitaLens OcuTec, OPTI-FREE PureMoist and OPTI-FREE RepleniSH results from separate in vitro studies performed following identical test procedures.<br />
7. Barniak V, Burke S, and Venkatesh S: Comparison evaluation of multi-purpose solutions in the stabilization of tear lysozyme. Contact Lens Anterior Eye. (2010), doi:10.1016/j.clae.2010.06.011.<br />
© 2013 Bausch & Lomb Incorporated. ®/TM denote trademarks of Bausch & Lomb Incorporated and its affi liates. Other product names /brand names are trademarks of their respective owners.<br />
Bausch & Lomb (NZ) Ltd c/- Bell Gully Auckland, Vero Centre, 48 Shortland Street, Auckland 1140, New Zealand. Marketed by Radiant Health Ltd. 0508 RADIANT.<br />
2 NEW ZEALAND OPTICS <strong>Sep</strong>tember <strong>2015</strong>
Time to move over.......<br />
It’s time to say goodbye<br />
to my role as editor and<br />
publisher of New Zealand<br />
Optics. When I was<br />
first involved in purchasing<br />
the magazine from Barbara<br />
Vague some 34½ years ago<br />
I would never have guessed<br />
that I would spend more than<br />
half my life involved in the<br />
ophthalmic industry. And what<br />
a rollercoaster ride it has been!<br />
I’d like to thank all my<br />
friends and colleagues in<br />
ophthalmology, optometry,<br />
dispensing and the wider<br />
industry including the<br />
university and the many<br />
wholesalers and distributors<br />
for their trust in me and their<br />
support over the years.<br />
For a non-optometrist<br />
and ophthalmologist I feel<br />
privileged to have learnt<br />
so much about your world<br />
whether it be eye conditions,<br />
eye disease, eye surgery,<br />
ophthalmic drugs, the design<br />
of frames and lenses to name<br />
just a few. It’s also been a<br />
privilege to have been involved<br />
in the technological advances<br />
which have transformed this<br />
industry since joining it in the<br />
early 80s. One thing for sure,<br />
these changes are going to<br />
continue to happen and that’s<br />
what has made my job so<br />
exciting.<br />
I’ve had the immense<br />
pleasure to meet people all<br />
around the world associated<br />
with your professions and<br />
industry. Too many highlights<br />
to mention individually<br />
BY MARYANNE DRANSFIELD<br />
but certainly the Essilor<br />
educational conferences held in<br />
Asia would have to be up there,<br />
as well as the 40th anniversary<br />
of Silmo in France.<br />
There have been many<br />
people who have helped<br />
us to make the magazine<br />
the success it is. I’d like to<br />
single out Alan Saks who has<br />
relentlessly churned out a<br />
monthly In Contact column<br />
for over 20 years; Professor<br />
Charles McGhee for having<br />
the insight to develop the Eye<br />
on Ophthalmology column so<br />
research and developments<br />
in ophthalmology got some<br />
exposure, and for orchestrating<br />
along with Associate Professor<br />
Dipika Patel the many people<br />
who have contributed to this<br />
over the years; and Dr Sue<br />
Ormonde whose idea it was<br />
to develop the regular Focus<br />
on Research contribution.<br />
Also thank you to the various<br />
contributors of Focus on<br />
Business, a very worthwhile,<br />
topical column that plays a role<br />
in shaping your businesses.<br />
A special mention too for Dr<br />
Bruce Hadden who kindly<br />
guided the way so we could<br />
embrace ophthalmology in the<br />
magazine. Also a huge thanks<br />
to my business partner and<br />
daughter-in-law Anita who has<br />
worked with me for the past 12<br />
years. She has played a big part<br />
in growing the magazine and<br />
the Optical Information Guide.<br />
It’s the end of an era for<br />
my entire family. All three of<br />
my children have worked in<br />
The familiar faces of Maryanne and Anita Dransfield at work at<br />
ODMA|<strong>2015</strong><br />
the business at some stage<br />
and have gotten to know<br />
many of you. Now there are<br />
seven grandchildren who are<br />
mightily relieved they don’t<br />
have to become involved in<br />
sticking labels on bags or<br />
inserting copies.<br />
It’s time to explore new<br />
ventures and take a welldeserved<br />
break with some<br />
travel high on the priority list.<br />
Anita and her family are off for<br />
a year’s travel overseas later<br />
this year before their two girls<br />
start secondary school.<br />
Anita and I have handed over<br />
the reins to Lesley Springall,<br />
a very competent journalist<br />
whom I am sure will take the<br />
magazine to the next level.<br />
Simon Eskow has joined Lesley<br />
as editor. However, I can assure<br />
you that it is business as usual<br />
and we are both continuing<br />
to work with Lesley over the<br />
coming months to ensure that<br />
she is fully settled and gets<br />
a chance to meet everyone. I<br />
will also be continuing with<br />
the publication in a new role<br />
as editor-at-large, where I will<br />
continue to represent NZ Optics<br />
at various industry events<br />
and help Lesley make sure we<br />
continue to keep everyone<br />
informed of what’s going on,<br />
both here and overseas.<br />
Whatever the future holds,<br />
optics will always be close to<br />
my heart. Sincere best wishes<br />
to everyone in this stimulating<br />
and dynamic industry and<br />
thank you for the opportunity<br />
of bringing the changing world<br />
of optics to you for all these<br />
years and for the fun we have<br />
had! O<br />
Rodenstock quashes sale<br />
rumours and eyes NZ<br />
Rodenstock, one of<br />
the world’s biggest<br />
frames and lens<br />
manufacturers, is<br />
not going through any sort of<br />
official sale process, despite<br />
persistent rumours to the<br />
contrary.<br />
Tim McCann, general manager<br />
of Rodenstock Australia,<br />
quashed the rumours in an<br />
interview with NZ Optics shortly<br />
after ODMA. Hearsay is par for<br />
the course for the company<br />
given it’s owned by UK-based<br />
international private equity<br />
company Bridgepoint and a<br />
number of other financiers.<br />
Tim McCann<br />
There are strong rumours that<br />
there is an interested party, said<br />
McCann. “But we don’t know who it is at this stage. The one thing<br />
that is certain and I have an absolute emphatic response on is it’s<br />
definitely not Essilor or Hoya.”<br />
Many were speculating about Rodenstock’s potential sale at<br />
ODMA|<strong>2015</strong> this year following an article by Bloomberg Business in<br />
May, which named rival lens manufacturers Essilor International<br />
and Hoya Corp among suitors said to be weighing bids for their<br />
German competitor. Bridgepoint is said to have hired investment<br />
bank Goldman Sachs Group to look at options for the company<br />
earlier this year with any sale likely to fetch more than 500 million<br />
euros ($825 million) for Rodenstock’s shareholders.<br />
After hosting Rodenstock’s international senior management<br />
team at ODMA, McCann says the company is in a good strong<br />
position and is currently looking to expand its presence globally,<br />
including returning to its once strong position in the New Zealand<br />
market. “The strength of the company and the strength of the<br />
brand is obviously growing globally…and certainly the feeling<br />
is that our brand is quite well-recognised in New Zealand and is<br />
viewed favourably so it would make sense to do something with<br />
that and that’s what we’re hoping to do.”<br />
McCann was in New Zealand prior to ODMA, canvassing “some<br />
key opinion leaders” about what it would take to be successful<br />
again in New Zealand. He says the company’s currently weighing<br />
up its options. “There’s nothing definite about how we do it, but<br />
we’re certainly interested. We want to make sure that the quality<br />
of the brand and the reputation of the company is maintained<br />
throughout, so it won’t be anything that will be fast but when we<br />
do it, we will do it well.” O<br />
CORNEAL LENS<br />
CORPORATION N.Z. LTD<br />
ideas into practice<br />
<strong>Sep</strong>tember <strong>2015</strong><br />
NEW ZEALAND OPTICS<br />
3
Tauranga practice taps<br />
Maunganui style<br />
Standing are Karl Fischer and Susan Sharpes, with (seated, from left) Anya<br />
Fischer, and Sally Gowland, office co-ordinator<br />
The founders of a<br />
new Mt Maunganui<br />
optometry practice<br />
consciously chose the<br />
look and location of their new<br />
venture based on more than 40<br />
years combined experience in<br />
the industry.<br />
“We have seen all aspects of<br />
optics: the good, the bad and<br />
the ugly,” says Karl Fischer,<br />
who opened Fischer+Fischer<br />
Optometrists with his wife,<br />
Anya. “We decided the only<br />
way forward was to create<br />
an independent practice with<br />
a strong message of quality,<br />
workmanship, attention to<br />
detail and impeccable customer<br />
service.”<br />
The Fischers favoured a 60s,<br />
modernist aesthetic in the<br />
design of their practice and<br />
in their choice of middle to<br />
high-end frame lines. They say<br />
Mt Maunganui was a natural<br />
location for their style.<br />
“It is an up and coming area<br />
with a strong designer and<br />
art vibe, with well-travelled,<br />
discerning Kiwis in search of the<br />
EYE DOCTORS<br />
FINAL GRAND ROUND FOR <strong>2015</strong><br />
Dr Andrew Riley<br />
FRANZCO<br />
Dr Penny McAllum<br />
FRANZCO<br />
better things in life,” says Karl.<br />
The couple enlisted Stufkens<br />
and Chambers architects<br />
to create a “quirky but<br />
approachable” interior and<br />
spent months of research<br />
designing the space.<br />
“We spent a lot of time with<br />
our architect explaining the<br />
flow of our work and the<br />
patient’s journey. We wanted<br />
the feeling of space and air<br />
to permeate the practice. The<br />
rooms are generous in size, the<br />
corridors are wide enough to<br />
manoeuvre a wheelchair, and<br />
the doorways are broad.”<br />
The interior combines natural<br />
materials with polished<br />
concrete and steel, in a bluegreen<br />
palette with brown and<br />
grey highlights.<br />
Karl says they were elated by<br />
the end result, but getting there<br />
wasn’t easy. “The whole process<br />
can be at times very stressful.<br />
Always have a plan B, C and<br />
D… and then relax.”<br />
The practice opened in June<br />
with a staff of four, including<br />
the Fischers. O<br />
Dr Mark Donaldson<br />
FRANZCO<br />
Dr Shuan Dai<br />
FRANZCO<br />
Ophthalmologist wins<br />
entrepreneurial award<br />
Christchurch-based<br />
ophthalmologist Dr<br />
Rebecca Stack stood<br />
out among 130 entries<br />
in a competition recognising<br />
working mothers as successful<br />
entrepreneurs.<br />
Dr Stack won the Best<br />
Product or Service business<br />
category and was named <strong>2015</strong><br />
Supreme Mumtrepreneur of<br />
the Year winner at an event on<br />
July 22 hosted by Loyalty New<br />
Zealand, sponsor of the annual<br />
competition.<br />
The award recognised Dr<br />
Stack’s key role in establishing<br />
the Christchurch Eye Surgery,<br />
a purpose-built facility that<br />
opened in June 2014 and now Dr Rebecca Stack<br />
carries out 75 per cent of<br />
ophthalmic procedures in the<br />
Canterbury region.<br />
Dr Stack says Christchurch Eye Surgery was launched to fill a<br />
gap in the market for a dedicated facility. “Patients for eye surgery<br />
are not unwell and do not need to be in a hospital. We wanted to<br />
create a centre of excellence with the best of technology, the best<br />
trained staff and by doing so design a patient experience that<br />
would be as pleasant and non-medical as possible.”<br />
The surgery has received several awards in its own right and<br />
now includes two surgical theatres and state-of-the-art air<br />
management and patient monitoring and tracking.<br />
“The patient feedback has been overwhelmingly positive,” Dr<br />
Stack says. “The time spent on design means we have created an<br />
efficient and technologically superior facility to anything else in<br />
Christchurch.”<br />
The practice employs a staff of around 20 with nine<br />
ophthalmologists, including Drs James Borthwick, Ian Dallison,<br />
Sean Every, David Kent, Malcolm McKellar, Jo-Anne Pon, John<br />
Rawstron and Allan Simpson.<br />
Dr Stack, who earned an MBChB (distinction) and MMedSC from<br />
Otago, juggles her time among Christchurch Eye Surgery, Southern<br />
Eye Specialists and Canterbury Charity Hospital and teaches<br />
medical students and optometrists. She also a regular conference<br />
speaker, wife and mother of two.<br />
“While it is a challenge fitting in family time I do try and keep<br />
one day a week free from work commitments, especially while<br />
my children are young,” she says, while admitting that she often<br />
ends up taking work home and spending evenings and weekends<br />
attached to her laptop after the children have gone to bed.<br />
“I am lucky enough to have a tremendously supportive husband.<br />
He is a farmer and has a little more flexibility than me so often<br />
joins in school activities with the children.”<br />
As Supreme winner and category winner, Dr Stack has received<br />
40,000 Fly Buys from Loyalty New Zealand. O<br />
New campaign for Crizal Transitions<br />
Crizal Transitions<br />
has launched a new<br />
campaign offering<br />
optometrists and their<br />
customers the chance to win<br />
weekly prizes to the value of<br />
$500 for every purchase of Crizal<br />
Transitions lenses during the<br />
campaign period.<br />
The integrated campaign<br />
features stunning Canadian<br />
actress Laurence Leboeuf<br />
wearing Transitions Graphite<br />
Green lenses inspired by the<br />
iconic U.S. Navy pilot eyeglasses<br />
from the 1950s.<br />
“Transitions Graphite Green<br />
perfectly complements many<br />
frame styles and colours. From<br />
classic to cutting-edge style,<br />
customers can transform any<br />
pair of regular eyeglasses into<br />
a striking look all their own,”<br />
said Essilor, manufacturer of<br />
Crizal Transition lenses, in a<br />
statement.<br />
Also available in grey and<br />
brown and with the added<br />
benefits of Essilor’s Crizal UV,<br />
glare and scratch protection,<br />
Crizal Transitions adapt<br />
spontaneously to changing<br />
light conditions, with a fast<br />
activation in the sun in less than<br />
60 seconds.<br />
The new campaign will<br />
run from <strong>Sep</strong>tember 14th to<br />
November 27th. O<br />
Actress Laurence Leboeuf promotes Transitions Graphite Green lenses<br />
in new campaign<br />
We look forward to seeing you.<br />
28th October - Novotel, by Ascot Hospital<br />
No registration fee . CME points available<br />
Visit our website for more details<br />
or phone us on (09) 520 9689<br />
to register.<br />
Ascot Hospital (09) 520 9689 - Botany Junction (09) 277 6787<br />
www.eyedoctors.co.nz<br />
<strong>Sep</strong>tember is Save Our<br />
Sight month<br />
NZAO’s<br />
annual<br />
Save Our<br />
Sight<br />
campaign returns in<br />
<strong>Sep</strong>tember showing<br />
there is more to<br />
optometry than a<br />
new pair of glasses.<br />
The campaign<br />
is designed to<br />
reinforce the value<br />
of eye exams and to<br />
propagate positive action for eye health among the general public.<br />
This year’s campaign includes a refreshed Comprehensive<br />
Eye Exam pamphlet, which will be distributed via MediBoard<br />
receptacles at 800 GP practices throughout the country.<br />
The NZAO is also printing a special Save Our Sight issue of its GP<br />
Quarterly newsletter, which will be distributed to an additional<br />
4500 GPs, placing a number of advertisements in magazines and<br />
resurrecting its 2014 TV commercial which will show on air, TVNZ<br />
on Demand, Stuff and Trade Me.<br />
Save Our Sight month launched in 2002 with the general aim of<br />
improving eye health by encouraging people to get regular exams<br />
by optometrists, to show the connection between eye health<br />
and general health, and to broaden the perception of eye exams<br />
beyond its popular association with getting glasses whatever your<br />
age. More information is available at www.saveoursight.co.nz.<br />
NZAO conference update<br />
The NZAO says its 85th annual conference will feature a diverse<br />
range speakers and quality CPD content. The conference will be<br />
held at the Scenic Hotel Southern Cross in Dunedin from October 9<br />
to October 11.<br />
Optometrists can register from now, online, to the conference<br />
opening day. The NZAO says the total number of CPD hours to<br />
be offered has not been finalised, but the organisation expects<br />
to provide 13 hours in total. To register and to view the full<br />
programme, visit www.nzao.co.nz/nzao-conferences. O<br />
ADONZ <strong>2015</strong><br />
promises stellar<br />
lineup<br />
Dispensing opticians have until the afternoon<br />
of October 1 to register for this year’s ADONZ<br />
conference, which is hotting up to be quite an<br />
event.<br />
The conference features a solid lineup of workshop<br />
presentations, with the opportunity to earn up to 14 CPD<br />
points. Plus attendees will need to don their gladrags<br />
for a ‘Roaring ‘20s’ gala evening, celebrating the 20th<br />
anniversary of the ADONZ education service, Opti-Blocks.<br />
ADONZ <strong>2015</strong> runs from October 9 to October 11 at<br />
the Novotel Tainui in Hamilton. Speakers include wellknown<br />
optics lecturer, researcher and author Dr David<br />
Wilson and OTEN optics learning coordinator Steve Daras,<br />
both Australia-based; Elaine Grisdale, an education and<br />
marketing coordinator from the Association of British<br />
Dispensing Opticians will be giving three workshops<br />
covering the psychology of communicating with patients,<br />
smarter dispensing for presbyopes and daring to be<br />
different with bespoke eyewear. Other speakers include<br />
Dr Srechko ‘Stretch’ Kontelj, legal director for Asia Pacific<br />
with Specsavers and Clinical Professor at Deakin University<br />
School of Medicine; Stephen Caunter, ANZ business<br />
training manager; Rodney Stedall from Paterson Burn<br />
Optometrists; and Dr Stephen Guest from the Hamilton Eye<br />
Clinic, who will be talking about ‘Bugs in the Eye: ocular<br />
infections you should know about’.<br />
In addition to 13 CPD points available across ethical,<br />
cultural and technical requirements, a limited number of<br />
attendees can earn an extra CPD point for sitting in one of<br />
two sessions on Vertex Distance, though seating for this is<br />
limited.<br />
For more information, to see the full programme or to<br />
register online, go to http://conference.adonz.co.nz/. O<br />
4 NEW ZEALAND OPTICS <strong>Sep</strong>tember <strong>2015</strong>
PROMISES,<br />
PROMISES…<br />
(THE SECRET OF A SUCCESSFUL PARTNERSHIP)<br />
Why so many optical professionals have become Specsavers Partners<br />
Almost seven years ago we opened the first of our 50+ New Zealand stores,<br />
which are owned and operated by local optical professionals. Typically, y, a<br />
Specsavers store is a joint venture partnership between an Optometry Partner<br />
and a Dispensing Partner: they own all of the profits of their business and all<br />
the saleable equity too, giving them an asset to build for retirement or when<br />
it’s time to sell. As the third ‘partner’ Specsavers owns none of the profit or the<br />
saleable equity but provides a depth of support services in exchange<br />
for franchise fees.<br />
Why so much traction?<br />
Going into business for yourself is a big decision – and we have spent 30 years<br />
crafting our franchise partnership offer and support package to ensure that,<br />
once made, the decision hides no surprises for our Store Partners. We’ve found<br />
that our straightforward answers to a range of big questions – and the promises<br />
we are happy to make and be held to - are a major factor in the partnership p<br />
decision-making process…<br />
5 big questions Specsavers Others<br />
Can you promise that all your stores<br />
are available for franchise – and that<br />
you have no goal to retain a stable of<br />
company-owned stores?<br />
Can I become a store owning<br />
Partner without having to go to the<br />
bank for finance?<br />
?<br />
?<br />
Will you guarantee me a market rate<br />
Salary for the life of my franchise? ?<br />
Can you promise you’ll never reduce<br />
your marketing budget?<br />
(it’s 6.5% of sales at Specsavers)<br />
Will you take on all my accounting,<br />
back-office, payroll, accounts<br />
payable and tax compliance work as<br />
part of the fees you charge your joint<br />
venture Store Partners?<br />
?<br />
?<br />
Now let’s answer your questions…<br />
Go to<br />
spectrum-blog.com<br />
for all the current<br />
opportunities!<br />
Our Partner Recruitment team is always on hand to<br />
answer questions from aspiring franchise partners – you may be<br />
thinking about store ownership options and we would like to take you<br />
through the kind of business opportunity that Specsavers presents,<br />
from leadership development to sales and profits. We’re an open<br />
book and we’re ready to talk.<br />
Simply contact Raj Sundarjee on 0800 773 077 or<br />
raj.sundarjee@specsavers.com to get the<br />
conversation started.<br />
NZ Franchise<br />
System of<br />
the Year<br />
2014<br />
Retail<br />
Innovator<br />
of the Year<br />
2014<br />
Multichannel<br />
Retailer<br />
of the Year<br />
2014<br />
Roy Morgan<br />
Research<br />
No. 1 for eye tests<br />
2014<br />
FCA International<br />
Franchisor<br />
of the<br />
Year<br />
2014<br />
FCA Social<br />
Responsibility<br />
Award<br />
2014<br />
FCA Established<br />
Franchisor<br />
of the Year<br />
20<br />
13<br />
FCA Excellence<br />
in Marketing<br />
Award Winner<br />
2013<br />
Australian<br />
Retailer<br />
of the<br />
Year<br />
2013<br />
Australian<br />
Retail<br />
Employer<br />
of the Year<br />
2013<br />
Asia<br />
-Pacific Best<br />
Retail Training<br />
Organisation<br />
2013<br />
<strong>Sep</strong>tember embe<br />
<strong>2015</strong><br />
NEW ZEALAND AND OPTICS<br />
5
Focus<br />
on Business<br />
Aspiring to greatness<br />
BY JUANITA NEVILLE-TE RITO*<br />
I<br />
recently had an interesting discussion with a crowd<br />
of 150 people about why retail in New Zealand is so<br />
poor. This conversation took place right after I had<br />
expressed my adulation for a craft experiencing a<br />
renaissance.<br />
Internationally, retail is in a period of renaissance, but<br />
if my weekend shopping experience is anything to go by,<br />
New Zealand’s customer service alone may be enough<br />
to kill any hope of following in our overseas friends’<br />
footsteps. For instance, when a cashier asks you, “Do you<br />
have our Health 2000 loyalty card?” and you say, “No I<br />
don’t”, and they say, “Ok, then that will be $59.95”, your<br />
only response has to be, “Huh?”<br />
Many from within and outside of retail have claimed<br />
that this fine industry is dying. On its last leg. “Who is<br />
going to go shopping when the window to the world is at<br />
everyone’s fingertips?”<br />
But the cynics are being proven wrong. The only thing<br />
they had right was that mediocre retail would die—that<br />
trend continues. However, e-commerce has created a<br />
catalyst for change and a retail renaissance has emerged.<br />
In that light, I was delighted to read on the blog of one<br />
of my favourite retail gurus, Jon Bird, a post based on<br />
his visit to the recent Cannes Lions International Festival<br />
of Creativity, an annual event that this time around<br />
recognised retail as part of its overall creative love fest. If<br />
Jon’s observations are anything to go by, retailers globally<br />
are aspiring to greatness, and delivering with verve. As<br />
Bird notes in his post (http://www.newretailblog.com/<br />
retail-roars-at-the-cannes-lions/), a final awards night<br />
recognised five retail/marketing spaces as Lions winners<br />
for harnessing the power of retail in a fresh new way.<br />
Here’s what Jon Bird wrote: 1. The Gun Shop: created<br />
for the States United To Prevent Gun Violence in the<br />
US. The concept was to establish a pop-up store selling<br />
guns (both in real-life and online). Once a customer<br />
had engaged with the sales assistant, the true horrific<br />
story behind each weapon was revealed. This case is<br />
all about affecting shopper behaviour (and ultimately<br />
consumer behaviour), but by de-motivating, rather<br />
than motivating, a purchase. I thought it was brilliant.<br />
2. Monty’s Christmas: created for UK department store<br />
chain, John Lewis. The annual Christmas commercial<br />
for John Lewis is eagerly awaited by the British public.<br />
Last holiday season, ‘Monty the Penguin’ was the<br />
central character, and he was featured brilliantly, all the<br />
way from the heart-warming TV ad to a plush toy for<br />
sale on the department store shelf. This is a superbly<br />
integrated and original Christmas campaign that had<br />
both a strong cultural and sales effect. 3. Rabbit Race:<br />
created for Media Markt, Germany’s biggest electronics<br />
retailer. How do you get away from the traditional Easter<br />
retail symbols of eggs and cuddly rabbits? By turning<br />
those rabbits into red-hot racers and staging a bigger<br />
live television event than the semi-finals of the soccer<br />
World Cup. This is a great promotional spin on a seasonal<br />
retail campaign, which raised traffic to stores by more<br />
than 18 per cent. 4. Make-Up Genius: created for L’Oreal<br />
Paris. Digital both instore and out of store is now an<br />
integral part of shopper marketing. This application<br />
allowed customers to accurately try on L’Oreal makeup<br />
in a “digital mirror” (their smartphone screens),<br />
in order to increase trial and generate sales. 5. Emoji<br />
Ordering: created for Domino’s. The idea here is to enable<br />
customers to order from Domino’s via Twitter by simply<br />
using a pizza emoji. Whether it was a legitimate hit<br />
with customers or not, I am a big fan of how innovative<br />
Domino’s has become over the last few years with<br />
ordering via mobile.<br />
To read more about the Cannes winner, and to watch<br />
videos, see my full blog post called Aspiring to Greatness<br />
on http://www.retailgeek.co.nz/.<br />
*An Aussie by birth and Kiwi at<br />
heart, Juanita is CEO and founder of<br />
retail specialist Hotfoot, a smarter,<br />
nontraditional advertising and<br />
communications agency which<br />
helps transform and build NZ retail<br />
businesses. Juanita’s insights and<br />
expertise from the wonderful world that is retail have<br />
been drawn not just from a twenty year career in the<br />
industry but also from her personal passion for shopping,<br />
to which she applies the same high levels of energy,<br />
leadership and intelligence as she does to business.<br />
You can follow Juanita on Pinterest (pinterest.com/<br />
hotfootnz/) or Twitter (twitter.com/JuanitaNeville) or<br />
through her website www.retailgeek.co.nz.<br />
Paragon Care to<br />
acquire DFV<br />
Melbourne-based Paragon Care has agreed to buy<br />
three private companies, including optometry and<br />
ophthalmology distributor Designs For Vision (DFV).<br />
Paragon, a medical products and services provider,<br />
filed documents with the Australian Stock Exchange (ASX) in<br />
mid-August announcing it would raise A$44 million ($49 million)<br />
for the acquisitions, valuing the DFV purchase at A$25.5 million<br />
($28.4 million). Paragon expects to finalise the acquisitions by<br />
the end of <strong>Sep</strong>tember.<br />
The purchase of DFV is intended to “expand Paragon’s<br />
customer base by providing access to the ophthalmic market<br />
where there will be growth opportunities for some of Paragon’s<br />
existing products,” according to the ASX-filing.<br />
Based in New South Wales, DFV provides a catalogue of<br />
diagnostic equipment, ophthalmic lasers, dry eye treatments,<br />
and other products to the Australia and New Zealand markets.<br />
The private company has operated since 1978 and currently<br />
employs 55 people, including two representatives in NZ.<br />
“(Paragon) respect what we have created here in DFV and do<br />
not want to see it changed,” says DFV directors Brad Grills and<br />
Nikolas Apostolou in a co-authored statement. “The DFV brand<br />
will remain. We believe in this business and its people and in<br />
part this is why we decided to transfer the shareholding to a<br />
stronger balance sheet to build more financial strength into the<br />
DFV brand and in turn create more opportunities together for<br />
our people.”<br />
Grills adds that in NZ Keith Proctor will continue to manage its<br />
surgical business and Jared Beetham the diagnostic business. O<br />
Record turnover for<br />
Specsavers<br />
Specsavers broke the £2 billion ($4.75 billion) barrier announcing<br />
a record worldwide group revenue of £2.06 billion ($4.89 billion)<br />
for the 2014-<strong>2015</strong> financial year, a 9.1 per cent increase on 2013-<br />
2014.<br />
New Zealand also broke records, exceeding revenues of $100 million<br />
for the first time, with reported revenue across its 52 Kiwi stores of $106<br />
million, up 16.5 per cent from $91 million the previous year. Australian<br />
store numbers increased from 292 to 300, with a reported revenue<br />
of A$708 million ($791 million), an increase of 12.4 per cent over the<br />
previous year’s A$630 million despite the company relocating and<br />
refitting more than 50 stores there in the last financial year.<br />
In their introduction to Specsavers’ annual review, Specsavers founders<br />
and owners Dame Mary and Doug Perkins said the 2014-<strong>2015</strong> revenue<br />
was a ‘phenomenal landmark in Specsavers history and a ringing<br />
endorsement of the partnership model’.<br />
Charles Hornor, Specsavers’ communications director for Australia and<br />
New Zealand says the New Zealand revenue increase was ‘significantly’<br />
more than expected, with growth particularly driven by stores which<br />
expanded their number of consulting rooms from one or two to three or<br />
four in response to demand. “We have been through a big programme of<br />
opening stores since 2008, and now we’re into a phase of expanding our<br />
current stores…that’s why average store turnover has grown to around<br />
$2.1 million per year.”<br />
Specsavers has helped drive the overall size of the New Zealand<br />
market since opening here in 2008. The average New Zealander now has<br />
their eyes tested every two to three years, compared with every five to<br />
six years a decade ago, says Hornor.<br />
Record results in New Zealand are expected next year as well, boosted<br />
by strong early results from Specsavers’ Kids Go Free campaign,<br />
launched in June. Since the launch the number of kids having their eyes<br />
tested across Specsavers stores has grown by almost 70 per cent to a<br />
little over 1,000 eye tests on under 16s each week.<br />
The company launched 32 years ago and today counts 31 million<br />
customers worldwide, with 2,300 partners and more than 30,000 people<br />
working across its 1,767 stores, support offices and supply chain.<br />
Highlights in Australia and New Zealand for the year include launching<br />
450 new frame styles, increasing contact lens customers by 50,000,<br />
increasing sight tests in Australia by 10 per cent and 14.5 per cent in New<br />
Zealand, and despatching a record 3.7 million orders from its Melbourne<br />
Glazing Services lab, with only 0.2 per cent returned due to error.<br />
Specsavers also installed a self-service contact lens ordering system in<br />
its Australian and New Zealand stores, making it easier for customers<br />
to order new lenses; and raised A$700,000 ($782,000) for charities<br />
including the Grandparents Raising Grandchildren Trust in NZ.<br />
“If someone had said in New Zealand in 2008 that come <strong>2015</strong><br />
Specsavers New Zealand partners would collectively be turning over<br />
more than $100 million a year, we’d have said that’s very unlikely, but<br />
the reason it has happened is because consumers have embraced the<br />
whole concept of quality and value and that’s produced a revolution in<br />
the market,” says Hornor.<br />
Specsavers Gisborne Top Shop<br />
Specsavers Gisborne was awarded the Overall Regional Supreme Award<br />
for the Central North Island, in the annual Retail NZ Top Shop awards.<br />
Mark Johnston, Retail NZ chief executive, says Specsavers Gisborne<br />
was selected after three rounds of judging, including two in-store<br />
assessments.<br />
Speaking at the awards ceremony, Tania Richards, a dispensing<br />
optician who runs the store with optometrist Nick Whittingham, says<br />
customer service was key to the win. While Whittingham says a focus<br />
on training also contributed. “We’ve evolved into a tight-knit group.” O<br />
Optrex Actimist coming<br />
to NZ optometrists<br />
Ernest Tobia at ODMA|<strong>2015</strong><br />
EYELogic, the exclusive distributor of Optrex ActiMist products<br />
to optometry practices in Australia received the thumbs up the<br />
day before ODMA|<strong>2015</strong> to commence distributing the popular<br />
dry eye spray to New Zealand optometrists.<br />
Following the successful launch of the Optrex ActiMist range in New<br />
Zealand pharmacies, manufacturer Reckitt Benckiser NZ identified a<br />
strong desire by optometrists to also stock the product, says Ernest<br />
Tobia, founder and managing director of EYELogic.<br />
“RB actively pursued a distributor for Optrex to service the New<br />
Zealand optometry market, leading to the appointment of EYELogic due<br />
to their specialised expertise and extensive experience in the optical<br />
industry.”<br />
Tobia, an Australian optometrist and current owner of two<br />
independent practices has more than 20 years experience as an optical<br />
practitioner and practice owner. He launched EYELogic in Australia in<br />
May 2014.<br />
He has now registered EYELogic NZ, so New Zealand optometrists will<br />
soon have the opportunity to sell Optrex ActiMist, instead of referring<br />
patients to their local pharmacy, he says.<br />
“Eighty per cent of dry eye patients suffer from meibomian gland<br />
dysfunction and Optrex is the leading product that fits that space. It’s a<br />
liposomal spray, not a drop, so it’s a lot easier for patients to use.”<br />
Tobia says he’s already spoken to several Kiwi optometrists who were<br />
keen to stock it and he’ll be contacting them following EYELogic NZ’s<br />
formal launch next month. “It’s unfortunate New Zealand [optometrists]<br />
have had to wait a year longer than Australia, but now we’re here, we’re<br />
excited about it.” O<br />
Essilor buys US<br />
optometry services<br />
provider<br />
Essilor of America Inc, the American subsidiary of Essilor<br />
International, agreed to buy Vision Source, a network of<br />
optometrists with nearly 4,000 members across North<br />
America.<br />
Details of the purchase were not made public, but the<br />
acquisition is said to represent a three-fold return on investment<br />
for Vision Source’s parent company, Brazos Private Equity, a<br />
Texas-based firm that has been shedding its healthcare holdings<br />
this year.<br />
Vision Source provides glasses, contact lenses, practice<br />
management tools, marketing assistance and supply chain<br />
programmes to optometrists in its practitioner-network.<br />
The announcement came soon after Essilor International<br />
reported total revenue of 3.408 billion euros ($5.8 billion) for the<br />
first six months of <strong>2015</strong> through June 30, an increase of 22 per<br />
cent from 2.780 billion euros ($4.6 billion) reported for the same<br />
period the year prior. The company said it was on track for 8 per<br />
cent to 11 per cent growth for the full year.<br />
Essilor has been on a two-year-long acquisition track in<br />
America, spending $3.66 billion in total for polarised glasses<br />
maker Costa Inc; photochromic lens producer Transitions<br />
Optical; and Coastal Contacts Inc, an online retailer of optical<br />
products.<br />
Elsewhere in the Americas, Essilor was a sponsor of the first<br />
World Congress of Optometry in Medellin, Colombia in mid-<br />
August. The congress is the first in a series of biennial global<br />
events to encompass all aspects of optometry in order to<br />
share research knowledge, explore clinical practice, education<br />
development and technological innovations and define an<br />
agenda for the future of accessible vision health care, according<br />
to a media statement. O<br />
6 NEW ZEALAND OPTICS <strong>Sep</strong>tember <strong>2015</strong>
6 o C<br />
UV INDEX 2<br />
07:15AM<br />
transitions.com Transitions and the swirl are registered trademarks and Signature is a trademark of Transitions Optical, Inc.<br />
©<strong>2015</strong> Transitions Optical, Inc. Photochromic performance is influenced by temperature, UV exposure and lens material.<br />
Celebrate life in<br />
the best light<br />
REAL PEOPLE.<br />
REAL STORIES.<br />
Consumer campaign out now!<br />
Hear their stories at:<br />
transitions.com<br />
<strong>Sep</strong>tember <strong>2015</strong><br />
NEW ZEALAND OPTICS<br />
7
SPECIAL FEATURE: DRY EYE<br />
Driving dry eye developments<br />
Dry eye is a hot topic in ocular circles<br />
these days. Where once there was a<br />
dearth of diagnostic and treatment<br />
options, there now appears to be a<br />
plethora of new tools, drops, and recipes all aimed<br />
at helping patients with dry eye.<br />
Jennifer Craig, an associate professor with<br />
the University of Auckland’s Ophthalmology<br />
Department and vice-chair of the internationally<br />
renowned Tear Film & Ocular Society’s (TFOS’s)<br />
second dry eye Workshop (DEWSII), says the<br />
problem has always been there, but these days<br />
professionals are able to diagnose it properly and<br />
thus respond better.<br />
“Until recently the profession relied very heavily<br />
on artificial tear drops for affected patients<br />
irrespective of the cause of the dry eye and clearly<br />
that doesn’t work for everybody. Recognition of<br />
the importance of evaporative dry eye, ongoing<br />
research and industry’s increasing support<br />
through research and development in this area is<br />
now providing us with better knowledge, better<br />
diagnostic techniques and tools, and better<br />
therapies for dry eye.”<br />
Greater definition<br />
BY LESLEY SPRINGALL<br />
TFOS’s first dry eye workshop (DEWS), published<br />
eight years ago, was instrumental in bringing<br />
the problem to the fore by developing a common<br />
and accepted starting platform from which<br />
organisations could develop products.<br />
Out went the old definitions, deemed<br />
inadequate, and in came a new consensus<br />
definition:<br />
Dry eye is a multifactorial disease of the tears<br />
and ocular surface that results in symptoms<br />
of discomfort, visual disturbance and tear film<br />
instability with potential damage to the ocular<br />
surface. It is accompanied by increased osmolarity<br />
of the tear film and inflammation of the ocular<br />
surface.<br />
The chronic lack of lubrication and moisture<br />
on the surface of the eye resulting from dry eye<br />
can result in symptoms ranging from subtle but<br />
constant irritation to inflammation of the front<br />
tissues of the eye. Persistent dryness, red eyes, a<br />
feeling of scratchiness or that something’s in your<br />
eye or a burning sensation are common symptoms,<br />
as are watery eyes caused by an over-stimulation<br />
of the watery component of tears as the eye<br />
struggles to protect itself.<br />
Causes and prevalence<br />
According to the experts, there are two main forms<br />
of dry eye: aqueous-deficient dry eye, where the<br />
lacrimal gland fails to produce enough tears; and<br />
evaporative dry eye, where the tear film evaporates<br />
too quickly. The most common cause of the latter<br />
is meibomian gland dysfunction (see separate<br />
story), which is believed to be involved in about 80<br />
per cent of all dry eye cases.<br />
Nailing down the causes of either, however, is<br />
tricky because, researchers say, there are many<br />
possibilities.<br />
Age is a factor. It is estimated that more than 70<br />
per cent of women and 60 per cent of men aged<br />
over 60 have dry eye. Women are more prone due<br />
to hormonal changes, such as menopause.<br />
But dry eye is also increasing in younger people,<br />
even children, with many studies citing our<br />
addiction to screens as an exacerbating factor.<br />
“It seems to be becoming more prevalent, likely<br />
influenced by the lifestyles we lead,” says Dr<br />
Craig. “We know when people are concentrating<br />
on smartphones or tablets they tend to blink less<br />
frequently and less well than they should, often<br />
not closing their eyes fully with each blink.”<br />
Our lack of blinking is considered such a problem<br />
that TFOS commissioned a song, Blink Around the<br />
World, for its international campaign to get people<br />
to blink more.<br />
“Blink Around the World is a fun and catchy<br />
way to remind people to blink their eyes, which<br />
both exercises and protects this preciously vital<br />
organ,” said Amy Gallant Sullivan, executive<br />
director of TFOS, when the campaign launched in<br />
2013. “The simple act of blinking reduces dry eye<br />
symptoms by flushing fresh tears over the eye,<br />
re-moisturising and keeping foreign matter and<br />
irritants out.”<br />
Dry eye can be a side effect of medications,<br />
including antihistamines, antidepressants, some<br />
blood pressure drugs, Parkinson’s medications,<br />
and birth control pills. Environmental factors are<br />
also connected to dry eye. Studies have shown<br />
Some of the imagery used to launch the TFOS DEWS II<br />
higher incidence rates in densely populated (ie.<br />
heavily polluted) cities, dusty or high-altitude<br />
climates, and among those living with constant air<br />
conditioning or dry heating systems.<br />
Other factors cited include contact lens wear;<br />
eyelid diseases such as blepharitis; systemic<br />
diseases such as lupus and Sjögren’s (pronounced<br />
“show-grins”—see separate story); allergens; as an<br />
after effect of eye surgery; as well as poor diet and<br />
dehydration (see separate story).<br />
Treating dry eye<br />
The list of potential treatments and treatment<br />
regimes mirrors the list of causes. Dry eye is<br />
considered to be a chronic and typically progressive<br />
condition that may not be completely curable,<br />
though most agree it can and should be managed<br />
well to relieve symptoms as not treating dry eye<br />
can lead to damage to the ocular surface.<br />
A recent study co-authored by Professor Reza<br />
Dana, professor of ophthalmology at Harvard<br />
Medical School, also found that not treating dry<br />
eye could lead to a significant decrease in corneal<br />
endothelial cell density, lending support to those<br />
who favour treating the underlying inflammation<br />
often associated with dry eye to reduce the<br />
chances of dry eye progression.<br />
In its mildest form dry eye can be managed with<br />
eye drops and other lubricants, with some artificial<br />
tear products addressing specific tear deficiencies,<br />
such as a lack of sufficient lipids. There are also<br />
prescription eye drops; warm compresses to help<br />
melt the thickened oil in the meibomian glands;<br />
and blepharitis treatments to cleanse the lid<br />
margins and keep the controversial, microscopic<br />
and ever-so-common Demodex mite (see separate<br />
story) under control.<br />
Diet can also make a difference with a lack<br />
of vitamin A and essential fatty acids and<br />
dehydration often cited as a cause or exacerbation<br />
of dry eye (see separate story).<br />
For the aqueous deficient form of dry eye, some<br />
practitioners advocate punctal occlusion, where<br />
a small plug, either temporary or permanent, is<br />
inserted into one or more puncta in the eyes to<br />
slow tear drainage. Punctal plugs are preferred<br />
over intracanalicular plugs by some, due to<br />
the lower risk of infection and—in those with<br />
confirmed benefits from punctal occlusion—<br />
punctal cautery can be a superior long term option<br />
(see separate story).<br />
The future<br />
Our knowledge, diagnostic tools and treatment<br />
practices are getting better, says Dr Craig, but<br />
there’s still a long way to go. “We’re learning all the<br />
time. We have to remain open to understanding<br />
the different ways that dry eye can be caused and<br />
other complicating factors.” But the industry’s<br />
increased focus on meibomian gland dysfunction<br />
and its role in evaporative dry eye is certainly<br />
helping far more people with dry eye than ever<br />
before, as is improved understanding of lid hygiene<br />
and the importance of blinking.<br />
We will undoubtedly also learn more following<br />
publication of the DEWS II outcomes, but given<br />
that the workshop was only officially launched in<br />
March <strong>2015</strong>, it’s still very early days, she says.<br />
DEWSII’s sub-committees have been set up and<br />
are currently compiling the outlines of what they<br />
propose to include in their reports, which are due<br />
to have their preliminary readings at the next TFOS<br />
conference in Montpellier, France in <strong>Sep</strong>tember<br />
next year. O<br />
Dry Eye & Allergy<br />
Centre of Excellence<br />
123 Remuera Rd, Remuera<br />
0800 393 527<br />
info@eyeinstitute.co.nz<br />
Dry eye research at New Zealand’s Ocular<br />
Surface Laboratory<br />
Located within the Department of<br />
Ophthalmology at the University of<br />
Auckland, the Ocular Surface Laboratory<br />
(OSL), led by Associate Professor Jennifer<br />
Craig, provides an environment for<br />
clinical and basic science researchers to<br />
collaborate to improve understanding of the<br />
mechanisms underlying the development<br />
and propagation of ocular surface disease,<br />
particularly dry eye disease, and to develop<br />
and test new therapies for managing this<br />
prevalent and debilitating condition.<br />
We asked Dr Craig to outline some of the<br />
research projects underway at the OSL at<br />
present.<br />
BY JENNIFER CRAIG<br />
At the OSL, we continue to explore the efficacy of<br />
a number of therapies for both aqueous deficient<br />
dry eye and evaporative dry eye. Current projects<br />
include:<br />
• Recent BOptom honours and summer student<br />
projects confirmed that a microwavable<br />
seed-filled warm compress (MGDRx EyeBag)<br />
has greater predictability and heat transfer<br />
capabilities than a portable heating mask<br />
(Eyegiene). Published earlier this year, the<br />
results show that despite these differences,<br />
both devices demonstrated clinical benefits for<br />
individuals with mild MGD.<br />
• Native Manuka honey, with its intrinsic<br />
antibacterial and anti-inflammatory<br />
properties, has also been under scrutiny<br />
for its potential as a therapeutic agent for<br />
patients with lid disease. From an idea first<br />
proposed by optometrist Grant Watters,<br />
the OSL has worked in collaboration with<br />
senior lecturer and BOTU Director Dr Ilva<br />
Rupenthal; microbiologist Dr Simon Swift; and<br />
Manuka Health NZ to create a Manuka honey<br />
formulation designed for daily overnight<br />
topical application to the eyelids. Development<br />
and preclinical testing began several years ago<br />
and the clinical tolerability trial has recently<br />
been completed in healthy individuals, with<br />
the assistance of Auckland optometrist Chee<br />
Loh and trainee ophthalmologist Dr Leah Te<br />
Weehi.<br />
The next stage of the process involves testing<br />
the efficacy of the product in clinically<br />
significant blepharitis. A call will be made<br />
to clinicians in the Auckland area in coming<br />
months for patients who may wish to<br />
participate in this three month trial. This work<br />
will be coordinated by postdoctoral research<br />
fellow Dr Isabella Cheung, while evaluation of<br />
inflammatory markers is being undertaken by<br />
Auckland optometrist Varny Ganesalingam,<br />
currently working towards a MHSc on the topic<br />
of ocular surface inflammation.<br />
• Successful publication of Amy Chen’s NZAOsponsored<br />
summer studentship conducting a<br />
pilot study on the efficacy of IPL has led to a<br />
new international industry collaboration. The<br />
future project forms the basis of Ally Xue’s PhD<br />
studies, where she is delving deeper into the<br />
mechanisms of action of IPL (see associated<br />
story)<br />
• The group at the OSL has also been working<br />
in collaboration with Oculeve, a US company<br />
recently acquired by Allergan. Participation<br />
as one of the sites in Oculeve’s international<br />
multicentre trial last year created the<br />
opportunity for further collaboration with the<br />
team in the area of nasal neurostimulation,<br />
using a device which has been designed to<br />
help address aqueous deficiency.<br />
• Learning more about ocular demodecosis<br />
and seeking better tolerated and efficacious<br />
treatments for Demodex infestation has been<br />
CONTINUED ON P12<br />
8 NEW ZEALAND OPTICS <strong>Sep</strong>tember <strong>2015</strong>
Long-lasting lubrication for dry eyes<br />
that is preservative-free and completely<br />
sterile, delivered through the unique<br />
COMOD ® multi-dose application system.<br />
For severe or<br />
chronic dry eye<br />
FULLY FUNDED<br />
Special authority criteria applies *<br />
For mild to<br />
moderate dry eye<br />
The systematic approach to eye lubrication<br />
for<br />
Dry Eyes<br />
Preservative-free and phosphate-free<br />
Can be used for 6 months after opening<br />
Compatible with all types of contact lenses<br />
At least 300 measured drops per pack,<br />
or 150 treatments (both eyes)<br />
For product enquiries contact:<br />
CORNEAL LENS<br />
CORPORATION N.Z. LTD<br />
www.corneal-lens.co.nz<br />
*Special Authority criteria applies only to HYLO ® -FRESH – please refer to the New Zealand Pharmaceutical Schedule for details.<br />
HYLO ® -FRESH (Sodium hyaluronate 0.1% w/v, 10mL) and HYLO-FORTE ® (Sodium hyaluronate 0.2% w/v, 10mL) eye drops are General Sales Medicines to improve the lubrication of the eyes, in eyes that are dry, irritated and tired from external factors.<br />
Always read the label and use strictly as directed. If symptoms persist see your healthcare professional. HYLO ® -FRESH, HYLO-FORTE ® and COMOD ® are registered trademarks of URSAPHARM. AFT Pharmaceuticals, Auckland. TAPS 1535HA.<br />
22855NZO/HL/FP<br />
Health Headlines<br />
Hartley Atkinson M.Pharm, PhD<br />
Founder & CEO, AFT Pharmaceuticals<br />
www.aftpharm.com<br />
PROUDLY NEW ZEALAND OWNED<br />
<strong>Sep</strong>tember <strong>2015</strong><br />
NEW ZEALAND OPTICS<br />
9
SPECIAL FEATURE: DRY EYE<br />
Meibomian gland dysfunction and contact lenses: our challenge<br />
BY GRANT WATTERS*<br />
Awareness of meibomian gland<br />
dysfunction (MGD)—and its role in<br />
ocular surface discomfort and contact<br />
lens intolerance—has been raised by<br />
the Tear Film and Ocular Surface Society (TFOS)<br />
workshop. Working towards understanding<br />
the mechanisms contributing to MGD and the<br />
implications of MGD on ocular surface health, the<br />
TFOS came up with a definition of MGD:<br />
MGD is a chronic, diffuse abnormality of the<br />
meibomian glands, commonly characterised by<br />
terminal duct obstruction and/or qualitative/<br />
quantitative changes in the glandular secretion. It<br />
may result in alteration of the tear film, symptoms<br />
of eye irritation, clinically apparent inflammation,<br />
and ocular surface disease.<br />
Because it is well established that all types of<br />
contact lenses (CL) can disrupt the lipid layer of<br />
the tears, it stands to reason that any MGD will<br />
exacerbate the situation, and cause an increase in<br />
evaporative dry eye and contact lens intolerance.<br />
Add to this the “hostile” environment of airconditioned<br />
offices, heating in cars and at home,<br />
and a lowered blink rate during long hours of<br />
computer work and you end up with a surprising<br />
number of patients struggling, especially with<br />
the added “double whammy” of impending<br />
presbyopia.<br />
These “Peter Pan Presbyopes” want solutions.<br />
Their eyes are drying out, causing blurred vision,<br />
and their near focus is also deteriorating. CL<br />
technologies for presbyopia can still be limiting,<br />
especially as we absolutely require wettable CL<br />
materials with good stable optics. A bridge too far?<br />
To provide some sort of a solution in our practice,<br />
we have become more assertive in offering<br />
in-house MGD therapy. We recommend the<br />
purchase of an eye wheat bag to replace the use of<br />
facecloths at home for more sustained heat release<br />
and for longer heat exposure periods of four to five<br />
minutes. We perform regular in-house expression<br />
programmes: first with eye wheat bags to warm<br />
up the MG’s; then, a golf club spud for lid margin<br />
debridement of any keratin over the MG’s; and<br />
finally with MG expression using mastrota paddle<br />
tweezers. We are also considering buying an E>EYE<br />
IPL machine, which has shown great promise (see<br />
separate story). The problem is that MGD, like<br />
blepharitis, can be chronic and recurrent—two<br />
ominous words—and patients are time-poor and<br />
even lazy when it comes to doing their own home<br />
therapy. Usually when things are going better,<br />
patients tend to stop doing their home treatments<br />
and then of course things take a turn for the<br />
worse. Educating them is therefore key so they<br />
know how to get back on track.<br />
In-house MGD therapy actually achieves two<br />
things: you motivate the patient into keeping it up<br />
and you give them a “head start” for their home<br />
sessions; plus it allows you to diagnose far more<br />
accurately the degree or grade of blockage. Are<br />
the ducts completely plugged? Or, if expressible,<br />
what is the texture and colour like? Is it cloudy or<br />
creamy like tooth-paste or fairly clear? Does the<br />
patient show improvement with time? Are the lid<br />
margins looking less red and inflamed? Is there any<br />
improvement in corneal staining? I tell patients<br />
that one session in-house is the equivalent of<br />
them doing it for about two weeks at home to help<br />
motivate them.<br />
If after a month of weekly in-house and home<br />
sessions there is little or no improvement, I write<br />
to the patient’s GP to ask for additional oral<br />
doxycycline or azithromycin supply, explaining<br />
why. Most GP’s will send out a script without<br />
insisting on a consultation and the mucolytic<br />
effect of tetracyclines can often soften up the<br />
blockages, improving treatment outcomes.<br />
With a bit of effort and teamwork from us and<br />
the (motivated) patient, we can usually make good<br />
progress. Keeping them on an on-going home<br />
maintenance programme of eye wheat bag warm<br />
compresses and digital massage for 2-3 sessions a<br />
week also seems to help avoid regression.<br />
Finally, there are two other groups of CL<br />
wearers who have to have a good stable tear film:<br />
orthokeratology (OK) wearers and keratoconics.<br />
The hydraulic engineering the tear film must<br />
achieve in OK lens wearers is massively affected<br />
by marginally dry eyes. While a lot of keratoconics<br />
have little choice other than to tolerate CLs for at<br />
least 16 hours a day in all sorts of crazy conditions.<br />
I have had to “pre-treat” OK children for MGD<br />
before proceeding, as it’s much easier to do first<br />
than having to backtrack! It is also not unusual<br />
for OK kids and keratoconics to have rosacea<br />
Factors and associations thought to<br />
adversely affect MG performance<br />
• Lid hyperkeratinisation<br />
• Age<br />
• Androgen deficiency with menopause<br />
• Contact lens wear<br />
• Asian ethnicity<br />
• Rosacea<br />
• Sjögren’s syndrome<br />
• Blepharitis<br />
• Atopy<br />
• Demodex folliculorum<br />
• Antihistamines<br />
• Antidepressants<br />
which has been overlooked. Also do a little bit of<br />
investigative work to see if any of your teenage OK<br />
wearers are on Roaccutane? Plus, MGD is known to<br />
be more prevalent in the Asian population.<br />
In general we need to be more attentive to<br />
MGD therapy to help our CL patients maintain<br />
asymptomatic wear for reasonable periods. Our<br />
patients certainly enjoy their in-house “day spa”<br />
sessions and get on board with some positive<br />
education, after all “a problem shared is a problem<br />
halved!” O<br />
* Grant Watters is a qualified TPA optometrist and co-owner<br />
of Mortimer Hirst in Auckland. He specialises in keratoconus,<br />
DRY EYE TREATMENT<br />
E>Eye gets the thumbs up in latest NZ patient<br />
research<br />
More than 80 per cent of patients who received<br />
E>Eye intense pulsed light (IPL) treatments<br />
at Merivale Optical in Christchurch reported<br />
their dry eye symptoms had improved, while<br />
95.7 per cent said they would recommend the<br />
treatment to others.<br />
The results come as part of a survey of E>Eye<br />
patients at Merivale treated over a 10-month<br />
period. Of the 86 respondents, 74.4 per cent<br />
were over 60 years old, 23.3 per cent were<br />
between 20 and 40 years old and 2.3 per<br />
cent were between 20 and 40. The research<br />
was conducted by John Veale, optometrist<br />
at Merivale and New Zealand distributor for<br />
France Medical’s E>Eye machine.<br />
The E>Eye machine has been specifically<br />
designed for treating dry eye due to<br />
meibomian gland dysfunction (MGD). The<br />
device works by producing a calibrated series<br />
of IPL. These light pulses are precisely set at a<br />
specific energy and frequency to stimulate the<br />
meibomian glands and help them to recover<br />
their function.<br />
Other results from Merivale’s research<br />
include 98.5 per cent saying the treatment<br />
was “no problem” or “okay”, and 55 per cent<br />
reporting they no longer needed to use eye<br />
drops following treatment.<br />
A double-blind, placebo-controlled clinical<br />
trial of 28 patients with MGD by Associate<br />
Professor Jennifer Craig from the Ocular<br />
Normal meibomian glands<br />
Ortho-K (orthokeratology), complex contact lens fitting and<br />
management and contact lens troubleshooting. He’s also a<br />
lecturer and researcher with the Departments of Optometry and<br />
Vision Science and Ophthalmology, University of Auckland.<br />
REFERENCES:<br />
• Craig JP, Chen Y-H, Turnbull PRK. Prospective trial of<br />
intense pulsed light for the treatment of meibomian gland<br />
dysfunction. Invest Ophthal Vis Sci <strong>2015</strong>; 56(3):1965-1970.<br />
• Nichols KK et al. The International Workshop on Meibomian<br />
Gland Dysfunction: Executive Summary. Invest Ophthal Vis Sci<br />
2011; 52(4):1922-1929.<br />
• Pult H, Riede-Pult BH, Nichols JJ. Relation Between Upper and<br />
Lower Lids’ Meibomian Gland Morphology, Tear Film, and Dry<br />
Eye. Optom Vis Sci 2012; 89(3):310-315.<br />
• Kunnen C, Nichols JJ. Meibomian Gland Dysfunction: An<br />
Update. CL Spectrum <strong>2015</strong>; 30:22-27.<br />
• Efron N. Contact Lens Complications (3rd.Ed) 2012 Elsevier.<br />
Surface Laboratory in Auckland University’s<br />
Department of Ophthalmology found 82 per<br />
cent of patients showed improvement after<br />
three treatments with the E>Eye device of at<br />
least one lipid layer grade on day one with<br />
86 per cent noting reduced symptoms by day<br />
45. There was also significant improvement<br />
in non-invasive tear breakup time (NIBUT) vs<br />
controls*.<br />
For more information on the E>Eye visit:<br />
www.dryeyetreatment.co.nz. O<br />
*Source: Craig, Jennifer P., Yen-Heng Chen, and Philip RK<br />
Turnbull. “Prospective trial of intense pulsed light for the<br />
treatment of meibomian gland dysfunction.” Investigative<br />
ophthalmology & visual science 56, no. 3 (<strong>2015</strong>): 1965-1970.<br />
Current price<br />
available until<br />
October 1<br />
For more information visit our website<br />
www.dryeyesyndrome.co.nz<br />
or email us info@dryeyetreatment.co.nz<br />
Achieving<br />
great results<br />
throughout<br />
NZ<br />
I started using E►Eye in January 2014. It quickly became evident that patients<br />
were extremely happy with the results. In particular, the patients with obvious<br />
rosacea were describing huge improvements in their ocular comfort and an<br />
improvement in their conjunctival injection. For a condition that previously had<br />
limited therapeutic options, IPL is an exciting and highly eff ective new treatment<br />
modality for patients with dry eye from MGD.<br />
Dr Brendan Cronin, Ophthalmologist<br />
I invested in E►Eye with peace of mind as I would have got my money back<br />
in the fi rst three months if it was not successful.<br />
Not only my dry eye patients were happy with their IPL treatments but they<br />
also recommended their friends and relatives to get treated too and this has<br />
become a very profi table service for my business. In fact, in less than four<br />
months, I had already got the return on my investment!<br />
There is no other optometry equipment on the market with such a quick<br />
return and it defi nitely makes my practice stand out from the crowd. E►Eye is<br />
defi nitely the best piece of equipment that I have invested in.<br />
It is attracting on average three to fi ve new customers per week and these<br />
customers are now coming to buy our frames and have their eyes examined.<br />
John Veale, Optometrist<br />
My eyes felt great after three treatments and continue to improve in regards<br />
to tolerance of air conditioning and computer use, especially after a long day.<br />
Thank you for being so kind and allowing me to have the treatment. My eyes felt<br />
so much better I was fi nally encouraged to apply for a job and was successful.<br />
Sofia, dry eye sufferer from Sydney<br />
IPL research call for patients<br />
BY ALLY XUE*<br />
Artificial tears, warm compresses, manual<br />
expression, lid scrubs - the majority of<br />
current treatments for meibomian gland<br />
dysfunction (MGD) are deemed largely<br />
palliative, providing at best transient relief from<br />
dry eye symptoms. Both clinicians and affected<br />
patients frequently describe MGD therapies as<br />
disappointing and continually seek alternative<br />
management options. One alternative which has<br />
emerged in recent years is intense pulsed light (IPL)<br />
therapy, conventionally applied to reduce facial<br />
melasma, but within the last decade recognised<br />
to have positive ocular effects in MGD. Following<br />
the arrival of the E>Eye IPL device (France Medical)<br />
in New Zealand in 2013, Associate Professor<br />
Jennifer Craig and her team at the Ocular Surface<br />
Lab (OSL) conducted a Prospective Trial of Intense<br />
Pulsed Light for the Treatment of Meibomian Gland<br />
Dysfunction. Results from this randomised, doublemasked,<br />
placebo-controlled study (published<br />
in IOVS this year) demonstrated significant<br />
improvements in tear film quality and patient<br />
symptoms. Effects were cumulative, prompting<br />
Dr Craig and I to design a second IPL trial on<br />
a larger participant group, and over a longer<br />
treatment period. In addition to assessing efficacy,<br />
we will explore a range of potential therapeutic<br />
mechanisms involved in IPL therapy. We hope<br />
to better understand the applicability of IPL in<br />
different patient sub-groups in order to improve<br />
prognostic value and enable further therapeutic<br />
refinements. We will be offering IPL treatment to<br />
patients interested in participating in the research<br />
project in exchange for a few hours of their time.<br />
Recruitment of suitable dry eye patients with<br />
symptomatic MGD is due to begin shortly, with<br />
plans to commence the IPL study later this year.<br />
Practitioners are invited to mention the study to<br />
patients they think might be suitable. O<br />
*Ally Xue is a PhD student with the OSL. Practitioners and<br />
patients interested in the study can contact Ally at<br />
a.xue@auckland.ac.nz to obtain more information about the<br />
study.<br />
10 NEW ZEALAND OPTICS <strong>Sep</strong>tember <strong>2015</strong>
Topography and advanced external imaging<br />
<br />
<br />
<br />
<br />
<br />
<br />
Complete Dry Eye Assessment<br />
TF-Scan, R-scan<br />
<br />
<br />
Meibo-scan<br />
<br />
Imaging<br />
<br />
<br />
TF-Scan<br />
<br />
The Dry Eye Relief Mask, D.E.R.M., contains Silica beads which naturally<br />
attract moisture from the air and release it when microwaved. Heating the<br />
mask for 20 seconds will provide soothing moist-heat relief for 4-6 minutes.<br />
Applying a moistened cotton liner to the mask prior to heating will extend<br />
the treatment to 7-9 minutes.<br />
D.E.R.M.. is hypoallergenic and can also be used to create cold therapies<br />
for allergy relief.<br />
The Tranquileyes system incorporates two re-usable<br />
gel pack technologies to create moist-heat therapies,<br />
proven to effectively improve tear quality by providing<br />
the intensity and duration of heat required while<br />
hydrating the sensitive eyelid and surrounding skin.<br />
Tranquileyes allows patients to create soothing<br />
moist-heat compresses, ranging in temperature from<br />
101–110°F/38.33-43.33°C and lasting up to 25 minutes.<br />
May also be used for cold therapies.<br />
<br />
<br />
Meibomium Gland Expression Paddle<br />
Long Term Temporary Canalicular<br />
Inserts. Effective 60 – 180 days<br />
The most advanced silicone<br />
punctum plug available<br />
InflammaDry is a rapid, immunoassay test for<br />
the detection of elevated levels of the MMP-9<br />
protein in human tears, to aid in the diagnosis<br />
of dry eye, in conjunction with other<br />
methods of clinical evaluation.<br />
This test is intended for professional<br />
use at point-of-care sites.<br />
0800 338 800<br />
www.designsforvision.co.nz<br />
<strong>Sep</strong>tember <strong>2015</strong><br />
NEW ZEALAND OPTICS<br />
11<br />
DV765-0715
SPECIAL FEATURE: DRY EYE<br />
Diagnosing and treating dry eye disease in a specialist setting<br />
BY THE DRY EYE & ALLERGY SPECIALISTS AT EYE INSTITUTE*<br />
Diagnosis and management of dry<br />
eye disease (DED) has improved in<br />
recent years because of advances in<br />
understanding the underlying causes.<br />
Tests and equipment once considered research<br />
tools have found their way into specialist dry eye<br />
clinics here and overseas.<br />
There is no single test that is sufficiently sensitive<br />
or specific to diagnose dry eye. An accurate diagnosis<br />
of the causes of a particular patient’s DED needs to<br />
be derived from investigating several aspects of the<br />
health and integrity of the ocular surface.<br />
HISTORY AND SYMPTOMS<br />
The usual history-taking process includes asking<br />
about environmental and occupational factors, as<br />
well as noting any allergies or medications that<br />
may relate to dry eyes.<br />
Normal history-taking can be enhanced by<br />
using special questionnaires designed to detect<br />
clinically significant DED and to grade the severity<br />
of symptoms. Using validated and repeatable<br />
questionnaires also helps eliminate variability<br />
between visits and examiners. McMonnies is a good<br />
screening tool and guide to what questions to ask<br />
a patient about their dry eyes. The Ocular Surface<br />
Disease Index is suited to monitoring change over<br />
time, and SPEED evaluates both the frequency and<br />
severity of symptoms in just eight questions.<br />
After a careful history check, it is good clinical<br />
practice to continue with the least invasive tests<br />
first. Assessments of tear quality should be<br />
performed before anything is added to the tear<br />
film or the tear flow is stimulated by bright lights<br />
or eyelid manipulations. It is important to measure<br />
each eye separately, as differences between them<br />
can help in the diagnosis.<br />
Common symptoms of dry eye disease<br />
• Dry, gritty, sore eyes<br />
• Tired or heavy eyes<br />
• Foreign body sensation ‘feels like sand in<br />
my eyes’<br />
• Stinging<br />
• Burning—often associated with ocular<br />
surface or lid margin inflammation<br />
• Itching—this is more often associated<br />
with allergic eye problems, but due to<br />
languages differences a person may use<br />
this term for symptoms related to dryness<br />
• Smeared or blurry vision that improves<br />
with blinking<br />
• Light sensitivity, for example sore and<br />
watery eyes in bright sunlight<br />
• Red eyes<br />
• Not able to wear contact lenses as long as<br />
in the past<br />
• Intermittent paradoxical watering of<br />
the eyes (for example, in dry windy<br />
conditions)—this is reflex tearing in<br />
reponse to an irritated cornea, which<br />
can happen if the eyes are dry. This is a<br />
more common cause of watery eyes than<br />
blocked tear drainage.<br />
CLINICAL ASSESSMENT<br />
A simple but important part of the examination<br />
is to observe the patient’s blinking, noting if it<br />
is complete or partial, and the length of time<br />
between blinks. This should be assessed before the<br />
patient is aware they are being examined to avoid<br />
conscious alterations to the blink pattern.<br />
Analysis of the tear film lipid layer is based upon<br />
the observation of colour interference effects in zones<br />
of specular reflection at the air-lipid layer boundary.<br />
Thin lipid layers (Eye<br />
story).<br />
IN SUMMARY<br />
Once the clinical information has been gathered<br />
in a standardised way, a decision on the optimal<br />
treatment plan can follow. This will vary from<br />
patient to patient depending on the identified<br />
contributing factors and the relative contributions<br />
to the dry eye state from aqueous deficiency or<br />
excessive evaporation. O<br />
* The Eye Institute in Auckland is a provider of eye surgery and<br />
ophthalmic care, employing a team of 10 ophthalmologists and<br />
50 dedicated staff.<br />
Dry eye research at New Zealand’s Ocular Surface Laboratory<br />
CONTINUED FROM P8<br />
Donations welcome for the Ocular Surface<br />
Research Fund<br />
Running in parallel with the Ocular Surface<br />
Laboratory is the Ocular Surface Clinic, where a<br />
limited number of patients (distinct from research<br />
participants) are reviewed and treated for their<br />
ocular surface conditions. The clinic is supported by<br />
donations from patients and others to the Ocular<br />
Surface Research Fund, managed by the School<br />
of Medicine Foundation. All donations go directly<br />
towards staffing the research facility and funding<br />
activities such as upgrading and purchasing<br />
equipment and funding smaller research projects<br />
such as those conducted by Honours and summer<br />
students. Further information about the Ocular<br />
Surface Research Fund and options for donation<br />
can be found at<br />
www.givingtoauckland.org.nz/osr. O<br />
12 NEW ZEALAND OPTICS <strong>Sep</strong>tember <strong>2015</strong>
Get to the main<br />
cause of dry,<br />
irritated eyes*<br />
4UP TO<br />
HOURS<br />
RELIEF 2<br />
CLINICALLY PROVEN<br />
Optrex ActiMist – clinically proven to work<br />
How does Optrex ActiMist work?<br />
ActiMist liposomes<br />
Natural lipids<br />
Optrex ActiMist contains<br />
liposomes (tiny bubbles fi lled with<br />
moisture) that migrate across the<br />
surface of the eyelid and collect<br />
at the edges of the eye.<br />
These liposomes mix with natural<br />
lipids on the eyelid.<br />
When the eyes are open the new<br />
lipid mixture spreads over the<br />
whole tear fi lm, and helps fi ll the<br />
gaps to restore the damaged<br />
lipid layer.<br />
Hygienic. Can be used<br />
by multiple people<br />
Lasts 6 months<br />
after opening<br />
Won’t smudge<br />
make-up<br />
Convenient and<br />
portable<br />
Suitable for use<br />
with contact lenses<br />
Order stock for your practice today<br />
FREE CALL 0800 EYELOGIC (0800 393 564)<br />
www.optrex.co.nz optrex@eyelogic.com.au<br />
Always read the label. Use only as directed. If symptoms persist, see your healthcare professional. †When wearing make-up, it is recommended to apply from 20cm. *Due to disturbed lipid layer of the tear fi lm. References:<br />
1. Lee S et al. Klin Monatsbl Augenheilkd 2004; 221:1–12. 2. Khaireddin R, Schmidt KG. Klin Monatsbl Augenheilkd. 2010; 227: 128-134. 3. Pult H et al. Contact Lens Anterior Eye 2012, 35:203-207. <strong>Sep</strong>tember Reckitt Benckiser, <strong>2015</strong> NEW Auckland. ZEALAND TAPS DA1541 OPTICS<br />
13
SPECIAL FEATURE: DRY EYE<br />
AFT PHARMACEUTICALS<br />
EYELOGIC<br />
OIC<br />
The systematic<br />
approach to eye<br />
lubrication<br />
HYLO-FRESH and<br />
HYLO-FORTE eye drops<br />
provide a systematic<br />
approach for dry eye<br />
treatment through<br />
a revolutionary<br />
multi-dose device.<br />
The patented COMOD<br />
(COntinuous MOno<br />
Dose) application<br />
system protects the<br />
sodium hyaluronate solution from contaminated ambient air,<br />
and ensures the precisely measured delivery of at least 300<br />
completely sterile drops without the use of preservatives.<br />
This ingenious airless system provides long-term stability<br />
for up to 6 months after opening, and with at least 150<br />
treatments (both eyes) it provides at least five times more<br />
treatments per pack than single-use preservative-free eye<br />
drops currently available in New Zealand.*<br />
The HYLO range is also phosphate-free which is important<br />
for patients suffering pronounced damage to the corneal<br />
surface. The use of phosphate-containing eye preparations<br />
can result in corneal calcification as a result of the<br />
precipitation of calcium phosphate in patients suffering<br />
extensive corneal damage, and can be avoided through the<br />
use of the phosphate-free HYLO range.<br />
HYLO-FRESH eye drops (sodium hyaluronate 0.1% w/v,<br />
10mL) offer long-lasting lubrication for dry eyes of moderate<br />
or medium severity, and are fully funded under Special<br />
Authority criteria (see the Pharmaceutical Schedule for<br />
details).<br />
The increased sodium hyaluronate concentration in<br />
HYLO-FORTE eye drops (sodium hyaluronate 0.2% w/v,<br />
10mL) results in a higher viscosity solution for long-lasting,<br />
intensive and soothing relief of severe or chronic dry eye.<br />
Both products are also suitable for use following surgery, and<br />
can be used with all contact lenses.<br />
For enquiries about HYLO-FRESH and HYLO-FORTE eye drops<br />
contact Corneal Lens Corporation. O<br />
*Based on the largest available pack size of single use<br />
preservative-free eye drops available in New Zealand as at<br />
July 1, <strong>2015</strong>.<br />
OPTREX<br />
ACTIMIST<br />
Dry eye is<br />
described<br />
as aqueousdeficient<br />
or<br />
evaporative<br />
dry eye, the<br />
latter being<br />
the most<br />
common type<br />
(78%). 1 The<br />
Lipid layer of<br />
the tears plays<br />
an important<br />
role in inhibiting tear film evaporation. 2<br />
Optrex ActiMist is applied to the closed eyelids via a spray and<br />
supplements phospholipid-liposomes to the lid margin, where the<br />
phospholipids mix with present lipid reservoir from the meibomian<br />
glands. A certain part of the lipid reservoir spreads over the film and<br />
forms the tear film lipid layer. Improving symptoms, visual acuity,<br />
lipid layer thickness, tear film stability, eyelid margin inflammation,<br />
tear production and lid parallel conjunctival folds. 3,4<br />
The liposomal spray Optrex ActiMist is a tear film supplement<br />
containing phosphatidylcholine deriving from highly purified soylecithin.<br />
The major phospholipid, phosphatidylcholine is delivered<br />
in a stable form of liposome to the closed eyelid. From there, they<br />
migrate with blinking across the eyelid margins to combine with<br />
the tear film.<br />
Compliance is always the biggest bug bear of any practitioner<br />
dispensing a solution for the treatment of evaporative dry eye.<br />
Patients just don’t like putting in their drops. Optrex ActiMist<br />
provides a spray solution that makes the delivery of their dry eye<br />
preparation simple and easy thus improving patient compliance<br />
and addressing your patient’s dry eye symptoms. For further clinical<br />
information please contact our office at<br />
admin@eyelogic.com.au. O<br />
1. Heilgenhaus A,Koch JM,Kruse FE, Schwatz C,WaubkeTN. Diagnosis and differentiation of<br />
dry eye disorders. Der Ophthalmologe 1995:92 (1):6-11<br />
2. Mishima S,Maurice DM. The oily layer of the tear film and evaporation from the corneal<br />
surface. Experimental Eye Research 1961;1:39-45<br />
3. Craig JP, Purslow C Murphy PJ,Wolffsohn JS. Effect of a liposomal spray on the pre-ocular<br />
tear film. Contact Lens and Anterior Eye 2010;32 (2)83-7.<br />
4. Dausch D, Lee S Dausch S Kim JC, Schwert G, Michelson W. Comparative study of treatment<br />
of the dry eye syndrome due to disturbances of the tear film lipid layer with lipid containing<br />
tear substitutes. Klinische Monatsblatter furAugenheilkunde 2006;223(12):974-83<br />
OIC introduces Avenova to NZ<br />
Avenova, a new daily lid and lash<br />
cleanser that’s garnering a lot of<br />
attention in the United States,<br />
will be available in New Zealand<br />
from the end of <strong>Sep</strong>tember.<br />
The product, made by<br />
biopharmaceutical company<br />
NovaBay, is the only one<br />
to contain Neutrox, a pure,<br />
proprietary, stable formulation of<br />
hypochlorous acid (0.01 per cent)<br />
in saline. Hypochlorous acid is a naturally occurring<br />
substance produced by white blood cells to fight<br />
microbial invaders and has a very low toxicity—1000<br />
times lower than Betadine, according to NovaBay.<br />
In a recent study, Dr Arthur Epstein, director of clinical<br />
research and head of Phoenix Eye Care’s Dry Eye Center<br />
of Arizona, compared six leading lid and lash cleansers<br />
with Avenova. He found Avenova was the only one to<br />
neutralize the bacterial enzyme lipase—a major cause<br />
of blepharitis and meibomian gland dysfunction.<br />
In vitro studies of Avenova have shown the product<br />
is effective against most microorganisms commonly<br />
found on eyelids and eyelashes, including Demodex. It<br />
has an antimicrobial time-kill of less than a minute.<br />
The new product will be available from the<br />
Ophthalmic Instrument Company (OIC) from the end<br />
of <strong>Sep</strong>tember. Managing director Tim Way says he’s<br />
delighted to add Avenova to OIC’s growing list of<br />
premium Dry Eye products. “Dry Eye is a very common<br />
patient complaint, so it’s great to be able to offer them<br />
this exciting new product. Avenova has the potential<br />
to make a huge difference to a dry eye sufferers’ quality<br />
of life.”<br />
OIC’s other Dry Eye products include the Polaris, a<br />
slit lamp accessory made by Italian company CSO for<br />
advanced tear film analysis; the RPS InflammaDry<br />
Detector, the first and only rapid point-of-care test<br />
to detect MMP-9 (an inflammatory marker that is<br />
elevated in the tears of patients with dry eye disease);<br />
and the Medmont E300 USB Corneal Topographer,<br />
which has just had a comprehensive tear film package<br />
released free of charge for existing Medmont Studio<br />
Version 6 users. O<br />
NEW<br />
VISION FX<br />
S U P P O R T S<br />
H E A L T H Y<br />
V I S I O N A N D<br />
E Y E M O I S T U R E<br />
For a FREE practitioner sample*<br />
please call 0800 147 325<br />
or email ceo@realvitamins.co.nz<br />
*Limited stock: first come, first served<br />
Assessment and diagnosis of Sjögren’s syndrome<br />
A<br />
useful concept in<br />
dry eye disease<br />
management is to<br />
consider the parts that<br />
maintain the ocular surface as<br />
one unit.<br />
This “Lacrimal Functional Unit”<br />
consists of the ocular surface<br />
(cornea, conjunctiva, accessory<br />
lacrimal glands, and meibomian<br />
glands), the main lacrimal<br />
gland, and the interconnecting<br />
innervation and chemical<br />
signals between them. If any<br />
portion of this functional unit or<br />
communication is compromised,<br />
then the ocular surface can be<br />
damaged. Some diseases affect<br />
one part of this unit more than<br />
others.<br />
Sjögren’s syndrome (SS) is a<br />
chronic autoimmune problem<br />
that affects the function of the<br />
exocrine glands, including the<br />
lacrimal and salivary glands.<br />
The effect on these glands<br />
is characterised by focal,<br />
mononuclear cell infiltrates that<br />
surround the ducts and replace<br />
the secretory units. SS is usually<br />
categorised as either primary<br />
(presents by itself) or secondary,<br />
if it appears in association with<br />
other well-defined connective<br />
tissue autoimmune diseases.<br />
As you would expect from a<br />
chronic incurable condition,<br />
SS can lead to significantly<br />
degraded quality of life. As well<br />
as causing the grittiness and<br />
discomfort of dry eyes it also<br />
impacts on the quality of vision<br />
and can cause significant long<br />
term damage to the mouth.<br />
The pathogenesis of SS is<br />
still not fully understood,<br />
but is thought to involve a<br />
BY THE DRY EYE & ALLERGY SPECIALISTS AT EYE INSTITUTE*<br />
combination of genetic and<br />
exogenous factors. Studies have<br />
postulated that infection with<br />
Epstein-Barr, Coxsackie B, or<br />
cytomegalovirus, amongst other<br />
viruses, could be a trigger. SS<br />
is also known to have a higher<br />
prevalence in women and in<br />
some families.<br />
Many cases of SS are detected<br />
by a patient’s eye care provider,<br />
which perhaps comes as no<br />
surprise given that Henrik<br />
Sjögren (1899–1986), a Swedish<br />
ophthalmologist, was the first<br />
to identify a group of affected<br />
women and to connect the triad<br />
of keratoconjunctivitis sicca,<br />
xerostomia and polyarthritis.<br />
DIAGNOSIS<br />
When a GP or medical<br />
practitioner suspects SS,<br />
they should ask about<br />
dry eye symptoms.<br />
Similarly optometrists and<br />
ophthalmologists need to ask<br />
dry eye patients about any<br />
oral symptom, such as dry<br />
mouth, swollen salivary glands,<br />
or the need for liquids to aid<br />
swallowing.<br />
To confirm the diagnosis,<br />
objective criteria are needed,<br />
including tear and saliva flow,<br />
autoantibody status (including<br />
SS-A), and minor salivary gland<br />
histology.<br />
Because SS may be just one<br />
contributing factor to the dry<br />
eye status, all of the normal<br />
ocular investigations for dry<br />
eye should be performed.<br />
Meibomian gland dysfunction<br />
is not uncommon in Sjögren’s<br />
syndrome. Even if the diagnosis<br />
is aqueous deficiency secondary<br />
to Sjögren’s, a complete<br />
understanding of that patient’s<br />
Lacrimal Functional Unit helps<br />
us find ways to improve overall<br />
tear quality.<br />
Other special investigations<br />
and tests are usually coordinated<br />
by a rheumatologist.<br />
Radiographic examination of<br />
the salivary glands involves the<br />
injection of a small amount<br />
of contrast medium into the<br />
salivary duct of a single gland,<br />
followed by X-rays—called a<br />
sialogram. A biopsy of a salivary<br />
gland can be examined for<br />
lymphocytic infiltration and<br />
acinar loss, and the presence of<br />
autoantibodies can also be used<br />
as a diagnostic tool.<br />
TREATMENTS FOR<br />
DRY EYE IN SJÖGREN’S<br />
SYNDROME<br />
There are some specific<br />
considerations when treating<br />
dry eye for Sjögren’s patients.<br />
Inflammation of the ocular<br />
surface is a key feature of all dry<br />
eye disease, but especially so<br />
in severe SS, so judicious use of<br />
topical, non-preserved steroids<br />
is helpful.<br />
Secretagogues are a class<br />
of drugs that increase mucin<br />
secretion, improve tear film<br />
stability, and decrease ocular<br />
surface inflammation. Two<br />
examples of these are oral<br />
pilocarpine and cevimeline. Both<br />
stimulate secretion of lacrimal<br />
gland fluid (tears) and saliva, but<br />
have side effects of excessive<br />
sweating and cramps. More<br />
recently, topical secretagogues<br />
such as diquafosol have been<br />
developed, although these<br />
are currently commercially<br />
available only in Japan. Topical<br />
application reduces the<br />
occurrence of the side effects<br />
commonly associated with oral<br />
secretagogues.<br />
Autologous serum drops have<br />
been shown to be useful for<br />
patients with severe aqueous<br />
deficiency. They contain several<br />
key components of the tear<br />
film such as epidermal growth<br />
factor, vitamin A, and lysozyme.<br />
The use of autologous serum<br />
overseas is often limited by<br />
the challenges of frequent<br />
drawing of blood, preservation<br />
of sterility, and appropriate<br />
facilities willing to prepare<br />
them. We are fortunate here<br />
that the NZ Blood Service will<br />
make these drops from the<br />
patient’s plasma and supply<br />
them at no charge. O<br />
* The Eye Institute in Auckland is a<br />
provider of eye surgery and ophthalmic<br />
care, employing a team of 10<br />
ophthalmologists and 50 dedicated staff.<br />
REFERENCES:<br />
• Clinical Guidelines for Management<br />
of Dry Eye Associated with Sjögren<br />
Disease, THE OCULAR SURFACE /<br />
APRIL <strong>2015</strong>, VOL. 13 NO. 2 / www.<br />
theocularsurface.com<br />
• Terry G Coursey, Cintia S de<br />
PaivaClinical: Managing Sjögren’s<br />
Syndrome and non-Sjögren Syndrome<br />
dry eye with anti-inflammatory<br />
therapy, Ophthalmology 2014:8<br />
1447–1458,<br />
• http://www.ncbi.nlm.nih.gov/pmc/<br />
articles/PMC4128848/pdf/opth-8-1447.<br />
pdf<br />
• Michael Voulgarelis & Athanasios G.<br />
Tzioufa: Pathogenetic mechanisms<br />
in the initiation and perpetuation of<br />
Sjögren’s syndrome.<br />
• Nature Reviews Rheumatology 6, 529-<br />
537 (<strong>Sep</strong>tember 2010) |doi:10.1038/<br />
nrrheum.2010.118, http://www.nature.<br />
com/nrrheum/journal/v6/n9/abs/<br />
nrrheum.2010.118.html<br />
14 NEW ZEALAND OPTICS <strong>Sep</strong>tember <strong>2015</strong>
Avenova for daily lid and lash hygiene<br />
NEW<br />
Avenova with Neutrox<br />
Gentle, refreshing and soothing for<br />
everyday eyelid and eyelash cleansing<br />
Ideal as part of any lid hygiene<br />
regimen for:<br />
- Dry Eye<br />
- Blepharitis (including Demodex)<br />
- Contact lens wear<br />
- Ocular surgery and procedures<br />
Because what we do every day matters<br />
The E300 Advantage<br />
• Largest coverage of any<br />
placido ring topographer,<br />
limbus to limbus<br />
• The GOLD standard for<br />
fitting specialty lenses<br />
• Exceptional accuracy with a<br />
standard deviation of 2 µm<br />
• Comprehensive new tear film<br />
package, understand and<br />
analyse tear film break-up<br />
The RPS InflammaDry Detector is the first<br />
and only rapid, point-of-care test to detect<br />
for MMP-9, an inflammatory marker that has<br />
consistently been shown to be elevated in the<br />
tears of patients with Dry Eye disease<br />
Distributed by:<br />
phone: 09 443 0072<br />
email: <strong>Sep</strong>tember info@oic.co.nz<br />
<strong>2015</strong> NEW ZEALAND OPTICS<br />
15
SPECIAL FEATURE: DRY EYE<br />
DESIGNS FOR VISION<br />
Designs For Vision has a<br />
comprehensive range of<br />
diagnostic and therapeutic<br />
products for dry eye. The<br />
Oculus Keratograph 5M<br />
provides complete dry eye<br />
assessment with multiple<br />
scan modes and tear film<br />
analysis functionality, in<br />
addition to topography and<br />
advanced external imaging;<br />
and InflammaDry is a fast,<br />
affordable immunoassay test<br />
for the detection of dry eye<br />
indicators in human tears.<br />
Innovative treatment options<br />
include the Blephasteam<br />
moist-heat therapy system for<br />
the relief of Meibomian Gland<br />
Dysfunction and associated<br />
REAL VITAMINS<br />
A powerful new formula to<br />
support and preserve vision<br />
Eye-health research has<br />
linked proper nutrition to<br />
decreased risk of age-related<br />
macular degeneration. New<br />
Zealand company Sanderson<br />
have developed a convenient<br />
new one-a-day capsule<br />
called Vision FX in their<br />
Practitioner Series range, that<br />
combines effective levels of<br />
key nutrients identified in<br />
research like AREDS I & II as<br />
having positive benefits for<br />
eye health.<br />
Vision FX is especially<br />
notable for its high levels<br />
of Lutein and Zeaxanthin.<br />
The super antioxidant Alpha<br />
Lipoic Acid has been included<br />
to support against glaucoma<br />
• Anti-Bacterial Action<br />
• Anti-Inflammatory Action<br />
• Antiseptic Management<br />
• No Stinging<br />
• Long-Term Dry Eye Relief<br />
• Immediate Comfort and Lubrication<br />
• No Evidence of Allergic Reaction<br />
• Can be Recapped and Safely Used<br />
within 24 hours<br />
• Unit Dose Tip is Safest for Accidental<br />
Cornea Touch<br />
Distributed by:<br />
diseases. While a selection<br />
of punctum plugs from<br />
Eagle Vision and Mastrota<br />
meibomian expression paddle<br />
are available for clinical use.<br />
For ongoing patient use,<br />
Designs For Vision provides<br />
the Tranquileyes and D.E.R.M.<br />
moist-heat systems from<br />
EyeEco. These products offer<br />
safe, effective home treatment<br />
for those requiring application<br />
of regular warm or cold<br />
therapy.<br />
Optimel Antibacterial<br />
Manuka Eye Drops is now<br />
available in two strength<br />
formulations and is suitable<br />
for the treatment of chronic<br />
dry eye and blepharitis.<br />
and cataracts. Flaxseed oil<br />
has been included for its<br />
dual benefits, as a source<br />
of omega 3 as well as being<br />
beneficial for dry eyes. This<br />
comprehensive formulation<br />
means patients no longer<br />
need to take several different<br />
supplements.<br />
Each Vision FX capsule<br />
contains:<br />
* Flaxseed Oil 500mg<br />
* Vitamin A 1000iu<br />
* Vitamin C 150mg<br />
* Vitamin D3 1000iu<br />
* Lutein 20mg<br />
* Zeaxanthin 10mg<br />
* Alpha Lipoic Acid 10mg<br />
* Natural Vitamin E 200iu<br />
* Zinc 15mg<br />
* Copper 1mg<br />
Sanderson Vision<br />
T: 0800 954536<br />
E: sales@corneal-lens.co.nz<br />
NO ANTIBIOTICS<br />
NO PRESERVATIVES<br />
Oculocin Propo is a natural based dry<br />
eye drop that also treats conjunctivitis with<br />
no known side effects<br />
KEY INGREDIENTS:<br />
Propolis<br />
Aloe Vera<br />
Chamomilla<br />
The medical grade<br />
antibacterial Manuka honey<br />
is clinically proven to stabilise<br />
and improve the ocular surface<br />
health of dry eye patients. O<br />
FX is available from<br />
pharmacies, health shops<br />
and health practitioners.<br />
Ophthalmologists,<br />
optometrists and DOs are<br />
invited to request a free<br />
sample by emailing<br />
ceo@realvitamins.co.nz. O<br />
IMPORTANT ACTIVE AGENTS:<br />
• Phenols<br />
Antimicrobial properties<br />
TM<br />
NEW!<br />
OTC<br />
approved - no<br />
prescription<br />
required<br />
• Aloins and emodins<br />
Has Analgesic (painkiller) and powerful virucidal and<br />
antibacterial properties<br />
• Alfa-bisabolol and it’s oxides. Azulens*<br />
Anti-inflammatory, anti-irritant and antimicrobial properties<br />
DOSAGE:<br />
1 - 2 Drops in each eye as required or as<br />
recommended by your eyecare professional<br />
ANTI-VIRAL AND ANTI-BACTERIAL<br />
PROPERTIES<br />
*UAB ORIGMED is using high activity extract normally double in<br />
values compared to standard<br />
pharmacopeia values. For<br />
example, propolis water extracts that is normally used,<br />
holds 0.5% phenols and Oculocin -1-1.5%. Because of<br />
natural origin chemical components which are important<br />
in product activity are more than 50 active Ingredients<br />
To punctal plug or not: when<br />
surgery is the answer<br />
BY BRIAN SLOAN*<br />
The tear film on the front of the eye is a<br />
balance between tear production and<br />
tear drainage, so when tear production is<br />
limited it makes sense to look at limiting<br />
tear drainage as well. And sometimes this is a good<br />
idea, but other times it’s not.<br />
Tears drain through the lacrimal punctae at the<br />
medial (inside) end of the upper and lower eyelid.<br />
From there, very narrow passages called the upper<br />
and lower lacrimal canaliculae drain towards the<br />
nose, joining into a common canaliculus which<br />
empties into the lacrimal sac. This then drains<br />
through the nasolacrimal duct into the nose.<br />
Narrowing or blockage of the lacrimal drainage<br />
system is common, especially as we get older.<br />
The most common site of narrowing or blockage<br />
is where the nasolacrimal duct enters the nose.<br />
Blockage at this point causes stasis of tears in the<br />
lacrimal sac and, like anywhere else in the body,<br />
stasis usually leads to infection, so people with<br />
blocked tear ducts often have either a chronic low<br />
grade infection (lacrimal mucocoele) or a more<br />
severe infection called acute dacryocystitis. Either<br />
way, the tear film will often be loaded with more<br />
bacteria, their toxins and associated inflammatory<br />
mediators, which tends to make ocular surface<br />
discomfort worse. This is a form of the so-called<br />
“toxic tear syndrome” and explains why patients<br />
with a degree of dry eye may still benefit from<br />
tear duct bypass surgery (dacryocystorhinostomy<br />
or DCR) in the presence of nasolacrimal duct<br />
obstruction (NLDO).<br />
Creating or exacerbating toxic tear syndrome<br />
can happen whenever tear drainage is disrupted—<br />
partly because of stasis/infection within the<br />
residual drainage system and partly because<br />
increased evaporative tear loss increases<br />
concentrations of electrolytes and proteins in the<br />
precorneal tear film. These effects will be least if<br />
tear drainage is blocked at the lacrimal punctae,<br />
which is convenient, but when the punctae are<br />
blocked, and how, needs to be very carefully<br />
considered when deciding on which treatment to<br />
adopt.<br />
First and foremost we need to be sure that<br />
the patient has a genuine deficiency of aqueous<br />
tear production as the cause for their “dry<br />
eye” symptoms, rather than a disorder of tear<br />
film stability. Aqueous tear deficiency is quite<br />
uncommon, while secondary causes of tear film<br />
dysfunction are very common. Punctal occlusion<br />
will often improve symptoms in the former, but<br />
may make things much worse in the latter group,<br />
with inappropriate punctal occlusion potentially<br />
giving the patient symptoms of tear overflow<br />
(epiphora). Clinical assessment of aqueous tear<br />
production is notoriously variable, so multiple<br />
assessments of Schirmer’s test or Phenol Red<br />
Thread Test are helpful in establishing the<br />
diagnosis.<br />
Even in patients with proven tear production<br />
deficiency, there may be secondary factors actively<br />
destabilising the tear film, such as Meibomian<br />
gland dysfunction, lid margin inflammation etc.<br />
These problems need to be aggressively managed<br />
before punctal occlusion is considered.<br />
Lastly, the technique used for punctal occlusion<br />
needs to be determined—punctal plugs or<br />
surgical. “Punctal plugs” come in a huge variety of<br />
designs and materials, but can be considered as<br />
either temporary (dissolving) or permanent; and<br />
can be sited either at the punctum or within the<br />
canaliculae.<br />
CLC<br />
Oculocin Propo is a new product to the NZ<br />
and Australian markets targeting two key<br />
areas: chronic conjunctivitis and periodic<br />
inflammation; and dry eye.<br />
It’s a sterile, natural pharmaceutical grade<br />
extracts-based eye drop, which contains no<br />
preservatives. Other key points are:<br />
• Contains glycerin, propolis, aloe vera and<br />
chamomile extracts; is rich in phenols,<br />
aloins, amodins, alfa-bisabolols and its<br />
oxides and azulenes;<br />
• Composition is dedicated for proper<br />
lubrication, antibacterial, antiviral,<br />
antifungal, pain relief, immune boost and<br />
faster healing effects;<br />
• Works like a soft, wide-range antibiotic and<br />
NSAID together covering lubrication, easy<br />
The lacrimal drainage system<br />
Temporary plugs are most often intracanalicular<br />
and, depending on the material, will last one to<br />
four weeks. These plugs are enormously useful in<br />
determining the possible benefit from permanent<br />
punctal occlusion and assessing the risk of the<br />
patient developing epiphora.<br />
Permanent intracanalicular plugs should be<br />
avoided as they can migrate and cause infections<br />
and fistulae in the canaliculae or lacrimal sac.<br />
Permanent punctal plugs are also very useful in<br />
determining the effect of punctal occlusion for a<br />
given patient and have the added benefit of the<br />
plug being clearly visible and so easily removable.<br />
Used long term, however, they also can be<br />
associated with irritation of the punctum and the<br />
ocular surface and accumulation of biofilm on the<br />
plug itself.<br />
Surgery for punctal occlusion can be very simple<br />
(punctal cautery) or complex (conjunctival flaps<br />
used to reversibly cover the punctae). Given that<br />
most people with poor tear production have a<br />
very low chance of recovery, permanent punctal<br />
occlusion by cautery is most commonly employed.<br />
MANAGEMENT<br />
Patients with moderate/severe dry eye<br />
symptoms are best managed cooperatively by<br />
their optometrist and ophthalmologist. Careful<br />
documentation of examination findings will help<br />
secure the diagnosis (or more commonly, multiple<br />
diagnoses), allowing for aggressive management<br />
of all exacerbating factors.<br />
For a patient with significant symptoms<br />
and signs despite maximal tolerated medical<br />
management, test occlusion of one or both<br />
superior punctae can be performed with<br />
temporary or permanent punctal plugs. If this<br />
shows benefit without epiphora, permanent<br />
occlusion of the superior punctae by cautery<br />
should be performed, and medical management<br />
continued as required.<br />
For the rare patient still having significant<br />
symptoms and signs, temporary occlusion of<br />
the inferior punctae can be trialled, followed by<br />
punctal cautery as indicated. O<br />
* Dr Brian Sloan is based at the Milford<br />
Eye Clinic, consults at Milford’s<br />
Warkworth Branch once a fortnight<br />
and works half-time at Greenlane<br />
Clinical Centre. He consults in all areas<br />
of general and acute ophthalmology<br />
and specialises in oculoplastic surgery,<br />
which includes surgery for skin cancers<br />
and watery eyes.<br />
pain and spasmolytic relief properties;<br />
• Can be used long term with no potential<br />
side effects or other harm, providing<br />
symptomatic relief together with light<br />
antibacterial and anti-inflammatory<br />
action;<br />
• Can be used in the period after antibiotic<br />
or anti-inflammatory treatment when<br />
prolonged use of chemical drugs could put<br />
the patient at risk;<br />
• Can be used inconjunction with antibiotic<br />
or anti-inflammatory treatment (drop time<br />
may differ) for better effect and irritation<br />
relief; and<br />
• Due to its antibacterial properties it is a<br />
effective product for long term dry eye<br />
antiseptic management. O<br />
16 NEW ZEALAND OPTICS <strong>Sep</strong>tember <strong>2015</strong>
SPECIAL FEATURE: DRY EYE<br />
New study sheds light on Demodex<br />
role in rosacea<br />
The clinical implications of Demodex mites<br />
in rosacea was discussed at the recent<br />
annual meeting of the American Academy<br />
of Dermatology.<br />
According to a press release issued by the<br />
National Rosacea Society, which sponsored the<br />
discussion together with Galderma Laboratories,<br />
while Demodex are found on the skin of all<br />
humans, they frequently occur in greater numbers<br />
in those with rosacea.<br />
“Researchers have more recently discovered<br />
that while Demodex folliculorum and D. brevis<br />
live in the hair follicles and sebaceous glands of<br />
the facial skin, D. folliculorum is also found in the<br />
meibomian glands of ocular rosacea patients,”<br />
said Dr Frank Powell, consultant dermatologist<br />
at Mater Misericordiae Hospital in Dublin and<br />
former president of the European Academy of<br />
Dermatology and Venereology. “In the mites’ brief<br />
life span of 14 days, they live and reproduce in<br />
the pilosebaceous units, subsisting on sebum and<br />
cellular contents, and emerge from the follicles<br />
primarily at night.”<br />
The significance of the relationship between<br />
Demodex and rosacea has long been controversial,<br />
said Dr Diane Thiboutot, professor of dermatology<br />
and vice-chair for Research at Penn State<br />
University and a consultant to Galderma. “These<br />
parameters may have been superseded by more<br />
recent findings, and a recent review of 48 articles<br />
in the Archives of Dermatology concluded that the<br />
degree of Demodex infestation, as opposed to its<br />
simple presence, is an important factor in rosacea.”<br />
She pointed out that rosacea and demodicosis<br />
are currently the only diseases widely associated<br />
with increased Demodex mites, although recent<br />
evidence suggests there may be others. Dr Powell<br />
noted that increased Demodex numbers causing<br />
inflammation may be present in those whose<br />
immune systems are compromised, including<br />
individuals with malignancy, leukemia, HIV<br />
infection or pregnancy. Interestingly, he said,<br />
individuals who had significant acne when<br />
younger have often been observed to have rosacea<br />
later, supporting a possible genetic component<br />
Nourishing dry eye away<br />
BY LESLEY SPRINGALL<br />
Mitigating the effects of mild dry eye<br />
disease (DED) can be as simple as<br />
staying hydrated.<br />
We constantly lose water through<br />
urine and sweat. Of the water we lose, studies<br />
show 20 per cent is replaced by the food we eat<br />
and 80% by the fluids we drink, which is why<br />
Health authorities around the world say we should<br />
be drinking about 2 litres of water a day, or roughly<br />
eight medium-sized glasses of water. Others say<br />
we should be sipping water constantly, even when<br />
we’re not thirsty.<br />
In America 75 per cent of the population is<br />
believed to be at least mildly dehydrated, but<br />
even a small deficit can exacerbate symptoms<br />
associated with DED. The problem is made<br />
worse by our love of coffee, tea, alcohol and fizzy<br />
drinks - all diuretics that can lead to us becoming<br />
dehydrated more quickly.<br />
Plus we don’t just lose water in sweat and urine,<br />
but essential minerals such as sodium, potassium<br />
and magnesium, that enable cells to maintain<br />
their shape and to function properly, generating<br />
energy, contracting muscles and everything else<br />
they do.<br />
This has implications for the tear film because<br />
studies show it is essential for nourishing as well<br />
as lubricating the eye, with each of the three<br />
different layers—mucin, aqueous and lipid -<br />
playing a vital part in keeping our eyes healthy.<br />
Each layer is fuelled by varying concentrations of<br />
vitamins and minerals to ensure it does its job<br />
correctly.<br />
According to NTPtalk, a forum for nutritional<br />
therapists in the US, the mucin layer requires<br />
vitamin A; the lacrimal gland requires zinc,<br />
magnesium, Vitamin C, B6 and niacin; and the<br />
oily layer needs essential fatty acids—omega 3s,<br />
ZINC POTASSIUM VITAMIN A OMEGA 3 OMEGA 6 MAGNESIUM<br />
Shellfish White beans Carrots Flaxseed oil Vegetable oils Dark leafy greens<br />
Meat<br />
Dark leafy Sweet potato Seeds Nuts (walnuts) Nuts<br />
greens<br />
Wheat germ Baked<br />
Dark leafy Oily fish Seeds Seeds<br />
potato(skin on) greens<br />
Spinach Bananas Squash Tofu Meat Fish<br />
Pumpkin seeds Mushrooms Lettuce Edamame Milk<br />
Beans<br />
beans<br />
Nuts (cashews) Avocados Melon Walnuts Eggs Whole grains<br />
Cocoa Fish Dried apricots Squash Cheese Avocados<br />
Beans Yoghurt Tuna Olive oil Cereals Bananas<br />
Mushrooms Dried apricots Tropical fruit Brussel<br />
sprouts<br />
Foods rich in essential minerals and vitamins for good eye health<br />
Patient with rosacea and ocular rosacea<br />
in patients with skin that reacts to either<br />
Propionibacterium acnes or Demodex.<br />
Dr Linda Stein Gold, director of dermatology<br />
clinical research at Henry Ford Hospital, noted that<br />
microbic organisms that live on Demodex mites<br />
may also be involved, as a recent study found an<br />
unexpected diversity of such microorganisms,<br />
including a total of 92 species, 36 of which were<br />
never before recorded on humans.<br />
The roundtable participants agreed that<br />
further studies should be conducted to improve<br />
understanding of the presence of Demodex and<br />
its potential actions and interactions with other<br />
pathogenic factors in rosacea, as well as to provide<br />
knowledge for uniquely targeted therapy in clinical<br />
practice.<br />
Ocular rosacea<br />
Ocular rosacea is inflammation that causes<br />
redness, burning and itching of the eyes. It often<br />
develops in people who have rosacea, a chronic<br />
skin condition that affects the face. Sometimes<br />
ocular, or eye, rosacea is the first sign patients may<br />
later develop the facial type.<br />
Ocular rosacea primarily affects adults between<br />
30 and 50 years old and appears to develop in<br />
people who tend to blush and flush easily. O<br />
Drinking water—the simplest but most essential way<br />
to help keep dry eye at bay<br />
Evening<br />
primrose oil<br />
Dried fruit<br />
Demodex does or Demodex don’t<br />
BY LESLEY SPRINGALL<br />
There was an audible gasp in the audience<br />
as the mightily-magnified Demodex<br />
mite appeared on the screen, stubby legs<br />
waggling, long fat body wriggling.<br />
The initial shock, followed by some nervous<br />
laughing, brought a smile to Australian<br />
optometrist and director of Innovative Eye Care<br />
Lachlan Scott-Hoy, who was busily demonstrating<br />
microblepharoexfoliation using RySurg’s BlephEx<br />
to a large audience at one of ODMA’s Spotlight<br />
sessions this year.<br />
Sold in New Zealand by OptiMed, BlephEx, with<br />
an bit of extra help from some added tea tree<br />
oil – Scott-Hoy actually adds extra tea tree oil to<br />
Blephadex (the new at home and in practice lid<br />
cleanser sold in tandem with BlephEx) to increase<br />
its potency - not only cleans up the lids of patients<br />
with blepharitis, one of the most common causes<br />
of dry eye, it also kills the two species of Demodex<br />
mite (see box below) that are believed at best to be<br />
an aggravator of blepharitis and at worst to be a<br />
major cause of dry eye disease.<br />
Scott-Hoy, who said he believes Demodex is a<br />
major cause of blepharitis and dry eye, told his<br />
audience how he bought a microscope on eBay<br />
so he could see the prevalence of Demodex on his<br />
patients’ lids for himself. He was soon a convert<br />
and decided to deal with the beasties once and<br />
for all. The live Demodex pictures (transmitted<br />
straight from microscope to screen) also really help<br />
enormously with patient compliance, he laughed.<br />
Jennifer Craig, an associate professor with<br />
the University of Auckland’s Ophthalmology<br />
Department, declares a similar level of interest<br />
in Demodex and the potential role the mites<br />
play in the pathophysiology of lid disease and<br />
dry eye. Evaluation of epilated eyelashes under<br />
a microscope, from patients suspected of<br />
About Demodex<br />
Demodex mites are microscopic arachnids<br />
(relatives of spiders and ticks) that live in<br />
and on the skin of mammals—including<br />
humans. On humans they are most<br />
common on facial skin, such as the external<br />
ear canals, eyelashes, sides of the nose,<br />
cheeks and forehead.<br />
Generally the mites live out a benign<br />
coexistence with their hosts, but they<br />
are known to cause mange amongst<br />
animals and skin ailments like rosacea and<br />
blepharitis in humans.<br />
Humans host two species on their faces:<br />
Demodex folliculorum, which have the<br />
longer body, vary from about 0.3mm to<br />
0.4mm long, affect hair follicles, like the<br />
eyelashes, and feed on skin cells; and<br />
Demodex brevis, which tend to be about<br />
0.15mm to 0.2 mm long, inhabit the oil<br />
glands connected to follicles and feed on<br />
gland cells.<br />
The mites tend to be most active at night<br />
and escape deep into their follicles in bright<br />
light.<br />
Sardines: good for combating dry eye<br />
commonly found in fish oil, algae and flax seed oil,<br />
and omega 6, which comes from vegetable oils,<br />
cereals, eggs, poultry and supplements such as<br />
evening primrose oil (see table). Zinc is believed<br />
to be particularly important as the highest<br />
concentration of zinc in the entire body is in the<br />
cornea, while a lack of potassium is linked to both<br />
dehydration and DED.<br />
Adding nutrients to the diet isn’t straight<br />
forward, however.<br />
Take gamma-linolenic acid (GLA) for example, an<br />
omega 6 fatty acid shown to reduce lacrimal gland<br />
inflammation, says Jagrut Lallu of Visque Rose<br />
Optometrists in Hamilton. Or Docosahexaenoic<br />
demodecosis, is a regular occurrence in the Ocular<br />
Surface Clinic and, while patients are offered<br />
the latest evidence-based treatments, research<br />
exploring novel therapies is under way, in parallel,<br />
within the Ocular Surface Laboratory (see OSL<br />
story).<br />
In-office lid margin optimisation combined with<br />
detailed lid hygiene instruction is an integral<br />
part of Dr Craig’s management philosophy. As<br />
an advocate of the “ocular hygienist” (playing a<br />
comparable role to dentistry’s “dental hygienist”),<br />
being proactive in treating individuals affected by<br />
Demodex is no different, but she says she feels it’s<br />
important to weigh the recent hype and wave of<br />
mass hysteria against the reality that almost all<br />
adult patients, especially older patients, exhibit<br />
demodecosis, yet there are vast numbers who are<br />
asymptomatic.<br />
Dr Craig says she can report some excellent<br />
outcomes from treating individuals exhibiting<br />
lid disease associated with significant Demodex<br />
infestation, but says she’s careful to explain<br />
to patients the goal is to reduce the level of<br />
infestation rather than eradicate the mites<br />
altogether, as that would be virtually impossible.<br />
“If you have blepharitis or other lid disease or<br />
dry eye then treating Demodex is important. But<br />
what we don’t know for certain yet is whether<br />
Demodex is one of the actual causes of meibomian<br />
gland dysfunction or whether it just makes things<br />
worse.” O<br />
Lachlan Scott-Hoy demonstrating the BelphEx at<br />
ODMA|<strong>2015</strong><br />
Demodex folliculorum<br />
acid (DHA), which affects retinal cell signalling<br />
mechanisms involved in phototransduction.<br />
And eicosapentaenoic acid (EPA), a substrate of<br />
DHA, which has been linked to abnormal retinal<br />
neovascularisation, vascular permeability, and<br />
inflammation.<br />
The vast amount of research in this area shows a<br />
healthy and effective diet must contain a balance<br />
of these omega 3 and omega 6 fatty acids. Too<br />
much omega 6—typically found in animal fats<br />
and vegetable oils, heavily used in fast food—can<br />
have an inflammatory effect, as not all omega<br />
6s are created equal. On the one hand GLA<br />
reduces inflammation, but linoleic acid (LA) and<br />
arachidonic acid (AA) promote it. Yet even GLA<br />
isn’t good if taken on its own: it only acts in an<br />
inflammatory manner if converted to dihomoy-linolenic<br />
acid (DGLA), which requires other<br />
nutrients, such as magnesium, zinc, and vitamins<br />
C, B3 and B6 to happen.<br />
A balanced diet is best for treating dry eye, says<br />
Lallu. “In general if you treat dry eye systemically,<br />
then you can help alleviate a lot of the symptoms.”<br />
But every patient is different, he warns, and some<br />
nutrients can interfere with a patient’s medication.<br />
For example, omega 3 supplements can affect the<br />
action of a number of blood thinning drugs. “So<br />
you have to know about the interactions before<br />
you go, ‘here, this is great’.” O<br />
<strong>Sep</strong>tember <strong>2015</strong><br />
NEW ZEALAND OPTICS<br />
17
Focus on<br />
Eye Research<br />
The latest topics in eye research reviewed by<br />
Save Sight Society ophthalmologists<br />
Oculoplastics<br />
REVIEWED BY KATHLEEYA STANG-VELDHOUSE*<br />
RISK FACTORS FOR DEVELOPING THYROID-ASSOCIATED<br />
OPHTHALMOPATHY AMONG INDIVIDUALS WITH<br />
GRAVES’ DISEASE<br />
Stein JD et al. JAMA Ophthalmol. <strong>2015</strong>;133(3):290-296.<br />
This longitudinal cohort study evaluated health care claims data of<br />
8404 individuals who were newly diagnosed with Graves’ disease<br />
(GD). Examination of variations in exposure to medications and<br />
treatment modalities was performed in an attempt to identify<br />
modifiable risk factors predisposing patients to thyroid associated<br />
ophthalmopathy (TAO). 8.8% of patients developed TAO during the<br />
10-year follow-up period. Compared with radioactive iodine therapy<br />
alone, surgical thyroidectomy (alone or in combination with medical<br />
therapy) was associated with a 74% decreased hazard for TAO.<br />
Additionally, the use of a statin for 60 days in the preceding year was<br />
associated with a 40% decreased hazard.<br />
COMMENT: Dysthyroidism and smoking have been long associated<br />
with an increased risk of developing TAO. In 2014, Khong JJ et al.<br />
identified selenium deficiency as a possible risk factor for thyroid<br />
eye disease (TED). This study helps to identify possible preventive<br />
measures and establishes a need for prospective studies evaluating<br />
the effect of statin therapy and surgical thyroidectomy on patients<br />
with GD.<br />
THE BLICK MNEMONIC FOR CLINICAL–ANATOMICAL<br />
ASSESSMENT OF PATIENTS WITH EPIPHORA<br />
Tse DT et al. Ophthal Plast Reconstr Surg. 2014;30(6):450-458.<br />
Following a review of the literature from 1957-2014, the oculofacial<br />
plastic surgery team at Bascom Palmer Eye Institute have introduced<br />
the BLICK mnemonic to highlight less commonly considered<br />
causes of epiphora. The paper provides an overview of the lacrimal<br />
distribution system and blink cycle, and discusses under-recognised<br />
but important abnormalities that may lead to watering. BLICK stands<br />
for the following:<br />
Blink dynamics: a quick review of various conditions that alter the<br />
blink cycle are discussed, including facial nerve palsy, ichthyosis, and<br />
botulinum toxin.<br />
Lid malposition: abnormalities are classified as issues concerning<br />
anterior lamellar elasticity, apposition of the eyelid to the globe, or<br />
problems with canthal anchoring.<br />
Imbrication: the authors emphasise the significance of “a lax<br />
upper eyelid [that] overrides the lower eyelid during closure”. The<br />
contribution to epiphora is argued to be two-fold: chronic irritation<br />
of the upper palpebral conjunctiva triggers a foreign body sensation,<br />
resulting in reflex tearing; a poor eyelid-tear film apposition leads to<br />
suboptimal lacrimal distribution.<br />
Conjunctivochalasis: redundant bulbar conjunctiva may lead<br />
to poor tear distribution, while the finding of a megalocaruncle<br />
represents mechanical blockage of lacrimal outflow channels.<br />
Kissing puncta: punctal apposition in primary gaze and throughout<br />
the blink cycle can lead to disturbances in this pressure-sensitive<br />
system, preventing appropriate lacrimal drainage.<br />
COMMENT: This major review helps to remind clinicians of the<br />
complexities of tear film distribution and drainage. Further<br />
consideration of the more subtle findings on physical exam can help<br />
to elucidate the causes of epiphora in the challenging patient, as well<br />
as to point out which treatment options are more likely to succeed.<br />
EARLY RESULTS OF SURGICAL MANAGEMENT OF<br />
CONJUNCTIVAL DERMOLIPOMA: PARTIAL EXCISION AND<br />
FREE CONJUNCTIVAL AUTOGRAFT<br />
Choi YJ, et al. Br J Ophthalmol <strong>2015</strong>;99:1031–1036.<br />
This study is a retrospective analysis of 13 patients treated for<br />
conjunctival dermolipomas, which are congenital choristomas<br />
(collections of normal cells/tissue in an abnormal location). Early<br />
surgical outcomes are reported for these patients undergoing<br />
partial resection of the mass. They report acceptable cosmetic<br />
results with no significant complications (ie. diplopia, ptosis, or<br />
keratoconjunctivitis sicca) in any of the subjects. The authors<br />
attribute these results to the introduction of a free conjunctival graft<br />
harvested from the contralateral eye.<br />
COMMENT: Dermolipomas most commonly present as unilateral,<br />
subconjunctival light pink to yellow lesions noted in the lateral<br />
aspect of the palpebral fissure. Growth is common in the first two<br />
decades of life, and while they may involve the lateral rectus muscle<br />
insertion dermolipomas rarely extend into deeper orbit. Historically,<br />
surgical resection is discouraged due to the risks of complications<br />
as listed above. The technique described in this paper, which takes a<br />
page from the evolution of the pterygiectomy procedure, may make<br />
surgical excision for patients with symptomatic dermolipomas a<br />
safer and more reliable option.<br />
ABOUT THE AUTHOR<br />
* Dr Kathleeya Stang-Veldhouse is an<br />
ophthalmologist who works at the Eye Clinic at<br />
Greenlane Clinical Centre. She is board-certified<br />
with the American Board of Ophthalmology and<br />
completed her fellowship in oculoplastics, lacrimal,<br />
and orbital surgery at the University of Auckland.<br />
Cataract and refractive<br />
surgeons will head to sunny<br />
Noosa in Queensland for the<br />
<strong>2015</strong> AUSCRS conference from<br />
October 7 to October 10.<br />
The conference will take place at<br />
the Peppers Noosa Conference Centre,<br />
under the theme The Nexus. It has<br />
attracted well-known speakers in the<br />
field of refractive surgery, including<br />
two from Europe and two from the US.<br />
Dr David Kent, a New Zealand<br />
representative on the AUSCRS<br />
committee, says there are compelling<br />
reasons for cataract and refractive<br />
surgeons from here to attend the<br />
conference. “It is our local Australian<br />
and New Zealand cataract and<br />
refractive surgery meeting and it is a<br />
good way to meet and discuss cataract<br />
and refractive surgery topics with other<br />
Australasian ophthalmologists with<br />
similar interests.”<br />
Although there is a refractive surgery<br />
component at this meeting, most will<br />
be on modern cataract surgery, he says.<br />
“Another attractive component is the<br />
Vision Eye backs Chinese buyer<br />
Australian ophthalmic care<br />
provider Vision Eye Institute<br />
(VEI) has endorsed an A$1.10-<br />
a-share takeover offer by<br />
Shanghai-listed Jangho Group, effectively<br />
knocking rival Pulse Health’s bid into<br />
touch.<br />
Pulse, a small, Australian private hospital<br />
manager, which has a 15.9 per cent stake<br />
in VEI, made a hostile takeover bid for VEI<br />
in July. But the 85c a share, full scrip offer<br />
MDNZ wins friends<br />
with Professional<br />
Friend programme<br />
Macular Degeneration New Zealand (MDNZ)<br />
has had a very positive response from<br />
optometrists and ophthalmologists to its new<br />
Professional Friend programme.<br />
The programme includes free access to information for<br />
distribution to patients, a highlighted listing in the MDNZ<br />
web-directory and a quarterly newsletter.<br />
“We are working more closely with optometrists and<br />
ophthalmologists than ever before, while our key message<br />
of ‘early detection saves sight’ sends the public to the<br />
professional practices to get their eyes checked,” says<br />
MDNZ general manager Phillippa Pitcher.<br />
Pitcher says more professionals are turning up to MDNZ<br />
seminars and the strengthening connections are creating a<br />
unified message to get the public to take action to preserve<br />
their sight.<br />
The MDNZ website currently lists 23 Friend programme<br />
members from Invercargill to Whangarei, and Pitcher says<br />
more are planning to sign on soon. Check out the MDNZ<br />
website www.mdnz.org.nz for more information. Early bird<br />
signatories will be listed in the next Viewpoint newsletter.<br />
There is still an opportunity to be listed as MDNZ is<br />
committed to publishing the first 20 Ophthalmologists and<br />
the first 100 Optometrists who enlist. O<br />
event is being held at a holiday resort<br />
so it is more relaxing.”<br />
Dr Kent says he looks forward to<br />
hearing presentations by Dr Bob Cionni<br />
and Dr Eric Donnenfeld, who are two<br />
of the most renowned international<br />
speakers in their field.<br />
Dr Cionni, medical director for<br />
The Eye Institute of Utah, performs<br />
more than 2,500 operations a year,<br />
specialising in cataract surgery, lens<br />
implants, refractive surgeries such<br />
as LASIK and PRK, and refractive lens<br />
exchange. In addition to advanced<br />
technology IOLs, he utilises the LenSx<br />
femtosecond laser and ORA system<br />
with VerifEye.<br />
Dr Donnenfeld has been performing<br />
refractive surgery in the United States<br />
since 1989 and was one of the first<br />
surgeons in the world to do laser<br />
vision correction. He was involved<br />
with the initial studies that led to the<br />
approval of the excimer laser and is an<br />
experienced corneal surgeon who has<br />
performed more than 2,500 corneal<br />
transplant procedures.<br />
was swiftly rejected by VEI’s directors.<br />
Jangho, a Chinese construction material<br />
company, cemented its interest by<br />
acquiring Australian healthcare company<br />
Primary Healthcare’s 19 per cent in VEI<br />
stake last month.<br />
In explaining its decision to back<br />
Jangho’s cash offer, VEI’s directors in<br />
a statement said the bid “highlights<br />
the strategic value of our business, in<br />
particular its day surgery clinics, the<br />
Also speaking will be Dr Roberto<br />
Belluci, director of ophthalmology<br />
at the Hospital of Verona, Italy, and<br />
Dr Gilles Lesieur, a former intern of<br />
the Toulouse Hospital, France who<br />
graduated in IUD refractive surgery and<br />
phacoemulsification and is currently<br />
a scientific advisor to Bausch + Lomb<br />
and PhysIOL laboratories. Recognising<br />
the important roles support staff<br />
play in a practice, AUSCRS <strong>2015</strong><br />
also includes a practice managers/<br />
administration staff programme and a<br />
technical staff programme.<br />
The event is well supported by<br />
industry partners with Bausch +<br />
Lomb and Alcon as key sponsors, while<br />
exhibitors include Ellex Medical, BOC<br />
Ophthalmic Instruments, Lumenis,<br />
Medibroker, Designs for Vision,<br />
AcuFocus, OptiMed, Medical I.T. Best<br />
Practice Software, Spectrum Surgical,<br />
AMO Australia, IQ Medical, Bausch<br />
+ Lomb, Insight Surgical, Device<br />
Technologies, Alcon and ZEISS. For<br />
more details, visit<br />
www.auscrs<strong>2015</strong>.org.au. O<br />
program of strategic initiatives being<br />
undertaken and Vision’s strong prospects<br />
for future growth.” O<br />
A BIG (Beat Invisible<br />
Glaucoma) thank you<br />
from Glaucoma NZ<br />
Glaucoma NZ extends a big thank you to all those<br />
who supported the <strong>2015</strong> July Annual Awareness<br />
Appeal.<br />
It has been extremely encouraging to have so<br />
many regular participants willing to help out once again<br />
and also some new faces and places joining in.<br />
Optometrists and ophthalmologists responded by taking<br />
donation boxes to display at their practices, as well as<br />
some making a donation from eye and/or glaucoma<br />
examinations undertaken during July. The support<br />
nationwide of pharmacies and ASB Bank also made a<br />
significant difference, and this year we also welcomed a<br />
great number of new corporates and businesses joining in.<br />
A large amount of media exposure was generated and<br />
we were also grateful for the added support of GNZ’s<br />
ambassador Sir Richard Hadlee and his wife Lady Dianne<br />
who appeared in NZ Woman’s Weekly to support the cause.<br />
GNZ’s 0800 line was busy with enquiries from the<br />
public wanting to know more about glaucoma and early<br />
detection. Many of these people were subsequently advised<br />
to visit their local optometrist for an eye examination.<br />
The Appeal overall has been a great success, lifting the<br />
awareness of glaucoma and boosting funds.<br />
Again, Glaucoma NZ appreciates all your efforts during<br />
the <strong>2015</strong> July Annual Awareness Appeal and your<br />
continued support throughout the year working towards<br />
eliminating blindness from glaucoma. O<br />
18 NEW ZEALAND OPTICS <strong>Sep</strong>tember <strong>2015</strong>
World class eye centre opens<br />
in Solomons<br />
Fred Hollows Foundation staff from left: Lucy Dryden, Konio Szetu, Celia Parry, John Szetu, Andrew Bell, Marleen<br />
Nelisse and Craig Fisher<br />
The Hon Prime Minister Manasseh<br />
Sogavare of the Solomon Islands opened<br />
the region’s first Regional Eye Centre in<br />
the country’s capital, Honiara.<br />
The Centre provides free eye care to all citizens<br />
and doubles as a training hub for visiting eye<br />
care professionals.<br />
Officially launched on July 22, the Centre<br />
represents a partnership between the Solomon<br />
Islands, the New Zealand government and<br />
The Fred Hollows Foundation NZ. The site was<br />
designed by award winning New Zealand firm<br />
Bossley Architects and built by local contractors.<br />
The Centre’s lead ophthalmologist, Dr Claude<br />
Posala, says he is thrilled to see the facility<br />
launch after all the extensive consultation and<br />
planning.<br />
“The Centre’s design and construction is<br />
incredibly high quality. Ninety-four per cent of<br />
the Centre’s power comes from solar energy<br />
and the building materials will last 50 years. I’m<br />
proud to say we have the most advanced eye<br />
care facility in the Pacific.”<br />
Dr Posala says the Centre will help prevent<br />
avoidable blindness in the country. “In Solomon<br />
Islands, as in the wider Pacific region, four out<br />
of five people who are blind don’t need to be—<br />
their condition is preventable or treatable.”<br />
Twenty-one Solomon Island eye nurses and<br />
four eye doctors have so far graduated from The<br />
Foundation’s Pacific Eye Institute in Fiji.<br />
“The Solomon Island government has shown<br />
great commitment to building the country’s eye<br />
health systems. Their graduates are amongst the<br />
best and brightest in the Pacific, and now they<br />
have a facility befitting of their specialist skills,”<br />
says Andrew Bell, executive director for The Fred<br />
Hollows Foundation.<br />
Eye care professionals from the region can<br />
gain further specialist knowledge at the<br />
Centre, which will also run mobile clinics in<br />
neighbouring Pacific nations.<br />
In its first year alone, the Centre will double<br />
the number of sight-saving surgeries performed<br />
in the Solomon Islands. The New Zealand<br />
Government has invested more than $4.1 million<br />
in the facility, with additional funding coming<br />
from the World Diabetes Foundation, the Queen<br />
Elizabeth Diamond Jubilee Trust and The Fred<br />
Hollows Foundation NZ. O<br />
OBITUARY<br />
Sydney-based optics giant, Brien Holden<br />
Internationally renowned optics researcher<br />
and philanthropist Professor Brien Holden<br />
died on July 27, aged 73, sending ripples<br />
from his home in Sydney throughout the<br />
world of optics and beyond.<br />
Holden was a teacher, researcher and<br />
humanist, who held a lifelong interest in<br />
bringing healthcare to developing nations, a<br />
passion that resulted in the organisation that<br />
now bears his name, the Brien Holden Vision<br />
Institute (BHVI), for which he served as CEO<br />
until his death.<br />
“I have huge respect for what Brien achieved<br />
in his lifetime,” says Paul Rose, a Hamiltonbased<br />
Optometrist and contact lens developer<br />
who flew to Sydney for Holden’s funeral. “My<br />
association with Brien goes back many years<br />
now and I remember well our first encounter<br />
back in the early 70s. He will be a difficult man<br />
to replace.”<br />
Holden was known for his pioneering work<br />
in soft contact lenses, beginning in the early<br />
1970s at the School of Optometry of the<br />
University of New South Wales where he was<br />
a lecturer. There he led a team of postgraduate<br />
students in determining what was needed<br />
in contact lenses to maintain eye health.<br />
Their work drew wide interest, prompting the<br />
group to move beyond the original goal of<br />
understanding the effects of contact lenses<br />
on the cornea to all aspects of contact lenses<br />
from lens design, material properties and<br />
performance to the effects of a wide range of<br />
ocular devices, procedures and contact lens<br />
solutions on the eye.<br />
Holden is credited in the co-development<br />
of the silicone hydrogel contact lens which<br />
makes up more than half of all contacts used<br />
worldwide.<br />
He was awarded an Order of Australia Medal<br />
in 1997 for his work in eye health and vision<br />
science.<br />
BHVI today is a non-profit organisation that<br />
has established hundreds of eye care sites<br />
around the globe, provided optometric services<br />
to more than two million people and trained<br />
nearly 50,000 eye care personnel.<br />
Optometry Ball<br />
University of Auckland optometry<br />
students enjoyed a night out at<br />
Alexandra Park for the annual<br />
Optometry Student Ball. The August 6<br />
event saw students, staff, and significant others<br />
Professor Brien Holden<br />
“Brien’s efforts and achievements have<br />
been recognised, applauded and adopted<br />
worldwide,” says BHVI Chair Brian Layland.<br />
“All who have worked with him will have fond<br />
memories to cherish; all will miss him. His<br />
legacy will encourage all to strive to achieve<br />
the goals he had set.”<br />
Holden is survived by wife Yvonne, three<br />
children, and four grandchildren.<br />
BHVI appoints interim CEO<br />
The Brien Holden Vision Institute (BHVI) has<br />
appointed deputy CEO, Professor Kovin Naidoo<br />
as interim CEO. Naidoo was a co-founder of the<br />
Clear Vision Optical franchise and has served<br />
in many elected/voluntary positions including<br />
Africa Chair of the International Agency for the<br />
Prevention of Blindness. A Fulbright Scholar,<br />
Naidoo was awarded a PhD from the University<br />
of New South Wales, a Doctorate of Optometry<br />
from the Pennsylvania College of Optometry,<br />
a Masters in Public Health from Temple<br />
University and a BSc and BOptom degree from<br />
University of Durban-Westville. He was African<br />
Optometrist of the Year in 2002, International<br />
Optometrist in 2007, and was jointly awarded<br />
with Holden the Schwab Social Entrepreneur<br />
Award for Africa 2010. O<br />
dress up as pirates, with James Li and Rosa<br />
Sun taking prizes for their outfits. The event<br />
was sponsored by Specsavers, Eye Institute,<br />
NZAO, Luxottica, Designs for Vision, Optimed,<br />
CooperVision and Corneal Lens Corporation. O<br />
Prime Minister Rt Hon Manasseh Sogavare gets an<br />
explanation of the centres solar power by David<br />
Pollard from What Power Crisis?<br />
The Fred Hollows Foundation NZ Regional Eye Clinic in<br />
Honiara, Solomon Islands<br />
Health tracking in a pair of specs<br />
US-based VSP Global claims to have<br />
developed the first wearable<br />
prototype of optical frames integrated<br />
with health-tracking technologies.<br />
Project Genesis features sensor technology<br />
housed within the temple of a pair of Dragon<br />
Alliance frames, allowing the wearer to track<br />
steps, calories burned, activity time and distance<br />
travelled via an app developed in-house, and<br />
synced via Bluetooth.<br />
The app and integrated frames were developed<br />
in secret over 12 months by VSP Global’s inhouse<br />
laboratory, the SHOP, under the leadership<br />
of Jay Sales and Leslie Muller.<br />
“Eyewear has been the most successful piece<br />
of ‘wearable technology’ for over 700 years,”<br />
says Muller. “With Genesis, we’re now adding<br />
additional value into the frame, but doing so in<br />
a seamless, fully integrated design that creates a<br />
richer experience for the wearer.”<br />
SHOP is beta testing the prototype with<br />
26 VSP Global employees at the company’s<br />
Californian headquarters. Participants give<br />
real-time feedback to SHOP engineers and<br />
designers, allowing for rapid improvements to<br />
The tracking device is built into the frame’s temple<br />
the prototype’s initial hardware and software<br />
designs.<br />
“Wearable technology is exploding right now,<br />
some of it could be considered hype, some of it<br />
could be considered the start of a personalised<br />
medicine revolution,” says Sales. “The Genesis<br />
prototype is a first step at providing a deeper<br />
level of contextualised health data through<br />
a device a large portion of people are already<br />
utilising every day.” O<br />
Back row from left to right: Rahul Kumar and Sayed<br />
Shuaib; Centre: Annie Wang, Dexter Low, Janet<br />
Chung, Huimin Dai, Lexia Ahkit and Sean Mahendran.<br />
Front: Divya Anthraper and Brinda Mamidi<br />
From Left to Right: Costume prize winner Rosa Sun<br />
with Alyssa Lie, LeiLei Zhou, Jingyi Xu, and Michelle Ko<br />
(Standing, left to right) Tyler Duncan, Robert Burnie, Katarina Marcijas, Chad Walker; (middle, seated): Marna<br />
Classen, Gemima Ji, Menaga Manokoran, Alice Jackson, Sharni Killoran, Kayleigh Aspeling; and (centre, in<br />
repose) Ken Turner<br />
<strong>Sep</strong>tember <strong>2015</strong><br />
NEW ZEALAND OPTICS<br />
19
with<br />
Prof Charles McGhee<br />
& A/Prof Dipika Patel<br />
Series Editors<br />
Corneal collagen crosslinking update<br />
A<br />
B<br />
BY AKILESH GOKUL, DIPIKA PATEL, CHARLES MCHGEE*<br />
INTRODUCTION<br />
In 2003 Wollansek et al. published a nonrandomised<br />
clinical pilot study detailing the<br />
procedure for corneal collagen crosslinking<br />
(CXL) as a means to halt or slow down<br />
the progression of keratoconus. 1 Known as the<br />
Dresden protocol, the procedure requires removal<br />
of the central corneal epithelium, followed by<br />
application of riboflavin (vitamin B2) solution<br />
and irradiation with ultra-violet A (UVA) radiation<br />
(370nm).<br />
A variety of alterations to the Dresden protocol<br />
have been proposed, aimed at increasing the<br />
number of patients that can undergo CXL, in terms<br />
of time taken to perform the procedure (efficiency)<br />
and anatomical limitations (corneal thickness<br />
>400µm at the thinnest point), while maintaining<br />
safety and efficacy.<br />
This article provides an update on CXL including;<br />
variations in procedure and evidence on safety and<br />
efficacy.<br />
VARIATIONS IN PROCEDURE<br />
Accelerated Corneal Collagen Crosslinking<br />
The main differentiating factor between the<br />
Dresden and accelerated CXL procedure is the<br />
intensity of UVA utilised and its duration. The<br />
Bunsen-Roscoe law of reciprocity states that; if the<br />
irradiance (total energy received by a surface per<br />
unit area) remains constant, the photochemical<br />
effect should be similar. Thus, theoretically,<br />
increasing the intensity of UVA and reducing<br />
treatment time to keep irradiance constant should<br />
yield similar results while improving efficiency. The<br />
Dresden protocol calls for irradiation with UVA of<br />
3 mW/cm 2 for 30 minutes, total irradiance of 5.4<br />
J/cm 2 . 1 Modified protocols using UVA intensities<br />
of 9 mW/cm 2 for 10 minutes, 2 18 mW/cm 2 for 5<br />
minutes 2 and 30 mW/cm 2 for 3 minutes 2,3 (total<br />
irradiances of 5.4 J/cm 2 ) have been investigated.<br />
Transepithelial Corneal Collagen Crosslinking<br />
Removal of the central corneal epithelium in<br />
the Dresden protocol is necessary to allow<br />
riboflavin to penetrate into the corneal<br />
stroma and reach concentrations adequate<br />
for effective crosslinking to occur. However,<br />
epithelial debridement results in significant<br />
post-operative pain and carries significant risk<br />
of complications. Transepithelial CXL minimises<br />
these risks as the epithelium is not removed.<br />
However, tight junctions within the epithelium<br />
limit riboflavin penetration, thus epithelial<br />
disruption is required. Epithelial disruption can be<br />
achieved chemically using penetration enhancing<br />
agents such as benzalkonium chloride (BAK)<br />
and Ethylenediaminetetraacetic acid (EDTA),<br />
sometimes in combination. Ionotophoresis<br />
(application of a low electric gradient to the<br />
cornea to improve riboflavin penetration) 4 does<br />
not require epithelial disruption and is reported to<br />
produce higher levels of riboflavin in the stroma<br />
compared to other methods of transepithelial CXL.<br />
However this technique is not commonly used as it<br />
is more technically challenging.<br />
MICROSTRUCTURAL CHANGES<br />
In vivo confocal microscopy has been used<br />
extensively to investigate the microstructural<br />
changes that occur following CXL. Following<br />
Dresden protocol CXL; the central corneal subbasal<br />
nerve plexus is often completely obliterated<br />
and a significant decrease in anterior keratocyte<br />
density (due to apoptosis) is observed at 1-6<br />
months post-operatively with a return to the<br />
pre-operative state at 12 months. 3,5 Additionally,<br />
anterior stromal oedema with hyper-reflective<br />
cytoplasm and extracellular lacunae in a<br />
honeycomb-like appearance is observed for up to 3<br />
months postoperatively (Figure 3). 3,5 The apparent<br />
demarcation between treated and untreated<br />
stroma appears as a region where normal<br />
keratocytes transition into elongated, hyperreflective,<br />
needle-like structures and then into<br />
large hyper-reflective stromal bands. 5 Cytotoxic<br />
effects of CXL on the corneal endothelium is a<br />
major concern, however, it appears that this does<br />
not occur as long as a minimum corneal thickness<br />
of >400µm is adhered to. 3,5 Accelerated CXL with<br />
irradiances of 18 mW/cm 2 for 5 minutes 6 and 30<br />
mW/cm 2 for 3 minutes 3,4 are reported to have<br />
similar microstructural effects as the Dresden<br />
protocol, though there is some indication that<br />
the anterior microstructural changes are slightly<br />
more pronounced. 3,4,6 Generally, none to minimal<br />
disruption to the corneal microstructure occurs<br />
when transepithelial CXL is utilised. 4,6,7<br />
SAFETY AND EFFICACY<br />
Safety<br />
CXL carries the risk of a number of complications<br />
including; infection, sterile or infectious<br />
infiltrates, transient corneal haze and scarring<br />
(Figure 2), most of which are due to removal of the<br />
epithelium. Many of these risks are significantly<br />
reduced when transepithelial CXL is utilised and<br />
can be minimised with a strict regimen of topical<br />
antibiotics and corticosteroids. The Dresden<br />
protocol has reported rates of sterile infiltrates in<br />
7.6%, stromal scarring in 2.9% and loss of 2 lines<br />
of vision or more in 2.9% of cases. 8 Transient postoperative<br />
corneal haze, which fades with time in<br />
most cases, is observed in the majority of cases<br />
(up to 90%) following the Dresden protocol. 8,9<br />
Infection following CXL is a rare complication,<br />
a recent large retrospective study revealed an<br />
infection rate of 0.0017% following the Dresden<br />
protocol and no infections were reported<br />
following accelerated and transepithelial CXL. 10<br />
Efficacy<br />
Much like measuring progression in keratoconus,<br />
measuring the efficacy of CXL is challenging.<br />
The measures of a successful outcome are<br />
generally based on whether there is progression<br />
in corneal shape, refraction and visual acuity.<br />
A recent Cochrane systematic review was<br />
conducted concerning CXL as a treatment for<br />
keratoconus, which highlighted the fact that<br />
there is a shortcoming in the evidence that CXL is<br />
an effective treatment for slowing or halting the<br />
progression of keratoconus. 11 There are over 600<br />
peer-reviewed publications concerning CXL, but<br />
there are very few well conducted randomised<br />
controlled trials (RCTs). Only three RCTs were<br />
included in the final Cochrane analyses, all of<br />
which adhered to the Dresden protocol. While<br />
the quality of evidence was graded as very low<br />
(grade 1 of 4), the observations are similar to the<br />
majority of investigations concerning the efficacy<br />
of the Dresden protocol.<br />
Topography/Tomography<br />
The Cochrane review revealed that at 12 months,<br />
the mean maximal keratometry was 1.92D less<br />
than the preoperative state (Figure 1). 11 There is<br />
a significant reduction in the risk of progression<br />
(defined as an increase in maximal keratometry of<br />
1.5D or more in 12 months following treatment),<br />
relative risk of 0.12. 11 However, at 36 month<br />
follow-up and progression defined as an increase<br />
in maximal keratometry of 2D or more, the<br />
relative risk is even lower at 0.03. 11 Progression<br />
has been reported to occur in 4.8% 11 and 7.6% 8 of<br />
cases, variations in failure rates between studies<br />
is likely due to different definitions of failure.<br />
Investigations with UVA intensities of 9 mW/cm 2<br />
for 10 minutes, 2 18 mW/cm 2 for 5 minutes 2 and 30<br />
mW/cm 2 for 3 minutes 2,3 compared to the Dresden<br />
protocol, are promising and reveal flattening of<br />
the cornea at 12 months in all cases. However, it<br />
appears that the flattening affect may reduce as<br />
the intensity of UVA increases. Mean maximum<br />
keratometry at 12 months was reduced by 1.32D<br />
(Dresden protocol), 0.67D (9mW/cm 2 ),0.52D (18<br />
mW/cm 2 ) and 0.18D (30 mW/cm 2 ). 2 Failure rates<br />
of 3% were noted for the 18 mW/cm 2 and 30 mW/<br />
cm 2 groups. 2<br />
Results following the transepithelial CXL<br />
protocol with chemical disruption are less<br />
promising. On average, there was no significant<br />
increase in maximum keratometry at 12 months,<br />
however, at 24 months there was a significant<br />
increase in maximum keratometry. 12 The use of<br />
ionotophoresis in transepithelial CXL interestingly<br />
shows considerable reduction in maximum<br />
keratometry of 2.35D at 12 month follow up. 7 We<br />
should bear in mind that the aim of CXL is not to<br />
flatten the cornea but rather to prevent further<br />
steepening thus a lower flattening effect in itself<br />
does not constitute failure; however, this may<br />
carry a greater risk of failure with longer follow<br />
up.<br />
Figure 1. Anterior Axial/Sagittal Curvature. A. Pre-operative, maximum keratometry 54.1D. B. 12 months postaccelerated<br />
CXL (30mW/cm2), exceptional flattening effect, maximum keratometry 51.5D<br />
A<br />
Figure 2. Post-accelerated CXL (30mW/cm2) corneal haze. A. 16x magnification B. 25x magnification<br />
A<br />
Figure 3. Anterior keratocytes A. Pre-operative. B. 1 month post-op, hyper-reflective cytoplasm and extracellular<br />
lacunae honeycomb-like appearance<br />
A<br />
B<br />
Refraction/VA<br />
Treatment with CXL often results in a modest<br />
improvement in uncorrected (UCVA) and best<br />
corrected VA (BCVA) as well as spherical equivalent<br />
refraction (SE). For the Dresden protocol, at 12<br />
months there is an improvement of approximately<br />
2 lines in UCVA 11 and BCVA 9 and an improvement of<br />
0.65D in SE. 11 Unlike the topography/tomography<br />
B<br />
B<br />
Figure 4.<br />
Demarcation<br />
line on<br />
Anterior<br />
Segment OCT<br />
A. Shallow<br />
demarcation<br />
line B. Deep<br />
demarcation<br />
line<br />
results, the Dresden protocol, 9 mW/cm 2 , 18<br />
mW/cm 2 and 30 mW/cm 2 intensities, yielded no<br />
difference in BCVA and SE when post-operative<br />
improvements in both parameters were compared<br />
between intensities. 2, 3 Transepithelial CXL with<br />
chemical disruption resulted in an improvement<br />
in UCVA and BCVA at 12 months, however, at<br />
CONTINUED ON P21<br />
20 NEW ZEALAND OPTICS <strong>Sep</strong>tember <strong>2015</strong>
Glaucoma pharmaceutical<br />
market expected to generate<br />
$6.1B by 2020<br />
The global glaucoma<br />
pharmaceutical<br />
market is expected<br />
to climb from around<br />
US$4.7 billion ($7.2 billion)<br />
in revenues in <strong>2015</strong> to nearly<br />
US$6.1 billion ($9.3 billion) in<br />
2020 with most of the growth<br />
predicted to come from China,<br />
India, and Latin America.<br />
Although revenues have<br />
decreased in recent years<br />
as generic versions of<br />
prostaglandins have reached<br />
the market in the US, the<br />
overall market is now poised<br />
for growth, according to<br />
international market data<br />
company, Market Scope.<br />
Factors driving these changes<br />
include: aging of world<br />
populations; increasing<br />
urbanisation in emerging<br />
markets and the developing<br />
world; increasing rates of high<br />
myopia; increased access to<br />
care in the developing world,<br />
CONTINUED FROM P20<br />
24 months UCVA fell below baseline and BCVA<br />
returned to baseline. 12 Transepithelial CXL with<br />
ionotophoresis has shown an improvement in<br />
UCVA, BCVA and refractive astigmatism of 0.13<br />
LogMAR (1 line), 0.05 LogMAR (0.5 line), and 0.49D,<br />
respectively at 12 months. 7,9<br />
AS-OCT<br />
As previously mentioned, an apparent demarcation<br />
between treated and untreated corneal stroma<br />
is observable with IVCM, a similar demarcation<br />
line is observable on anterior segment optical<br />
coherence tomography (AS-OCT) (Figure 4). Though<br />
not definitively established, it is believed the<br />
demarcation line indicates how deep the crosslinking<br />
effect has occurred. If this is indeed the<br />
case, it has not yet been determined if there is<br />
an ideal or minimum depth of the demarcation<br />
that would likely result in a successful outcome.<br />
When the Dresden protocol is utilised, the depth<br />
of the demarcation is usually around 300µm. 13<br />
Accelerated CXL modalities reveal a shallower<br />
demarcation. It appears that with increasing<br />
intensity, the demarcation line is shallower and<br />
more variable. With the 18 mW/cm 2 and 30 mW/<br />
cm 2 intensities the average depth of demarcation is<br />
observed at 203µm 2 and 184-201µm, 2,4 respectively.<br />
Similar to accelerated CXL, the demarcation line is<br />
shallower following transepithelial CXL, compared<br />
to the Dresden protocol. In fact 50% of corneas<br />
treated with transepithelial CXL do not display<br />
any demarcation line, even when ionotophoresis<br />
is utilised. 4 Corneas treated with transepithelial<br />
CXL utilising ionotophoresis demonstrates a<br />
demarcation line at 212µm on average, when<br />
present. 4 As previously stated no minimum depth<br />
of demarcation for CXL to be effective has been<br />
revealed thus far hence a possible advantage<br />
of current accelerated and transepithelial CXL<br />
protocols is that they may be employed safely on<br />
corneas
Reflections<br />
Writing this edition involved much<br />
reminiscing and introspection as it<br />
marks some significant events.<br />
Maryanne and Anita Dransfield have sold New<br />
Zealand Optics to Lesley Springall who takes over<br />
as Publisher and Editor.<br />
After acquiring a fledgling NZ Optics in 1981,<br />
Maryanne moved the magazine production to a<br />
converted garage at her home in Kohimarama.<br />
From small beginnings she grew NZ Optics into<br />
the multimedia publication that it is today and it<br />
remains the only such publication in New Zealand.<br />
A colourful and energetic character Maryanne<br />
has penned millions of words covering the whole<br />
gamut of eyecare. She’s become part of the<br />
scene and fabric of New Zealand eye care and<br />
has helped organise and attended conferences,<br />
launches, functions and CPD events. She is<br />
justifiably proud of their efforts in helping to lift<br />
the profile of organisations like the NZ National<br />
Eyebank, MDNZ and Glaucoma NZ and supported<br />
fundraising efforts and events. Maryanne is<br />
pleased that the magazine has helped foster ties<br />
between optometrists and ophthalmologists<br />
and has enjoyed the challenge of embracing<br />
ophthalmology and learning fantastic things<br />
about eye disease and treatment.<br />
Most things have been dutifully recorded in word<br />
and in the thousands of photographs that serve<br />
as a documented record of the evolution of the<br />
professions. Fun times were enjoyed at many great<br />
events.<br />
At the start publishing was literally cut and<br />
paste with scissors and runny glue something<br />
NEW<br />
I too experienced in the mid ‘70s. Maryanne<br />
relates the evolution of publishing as follows: “I<br />
started by typing stories on an IBM typewriter,<br />
then Commodore computer and finally 286 &<br />
386 computers. We’d then take the stories into<br />
Parnell where they were typeset and printed out in<br />
galleys. I used to start laying up at 4pm and end at<br />
4am. I’d sleep three hours and then head back to<br />
the typesetters for corrections, headings, change<br />
of font size and have bromides made of photos.<br />
All layup was by hand; wax the galleys and paste<br />
them into place, juggling copy to fit, cutting out<br />
whole paragraphs…<br />
This went on for two to three days. It was a huge<br />
undertaking. How technology has changed things.<br />
I think it was around the late ‘80s that I was able to<br />
give a floppy disk of stories to someone who then<br />
laid them up into PageMaker. This changed my life<br />
as well as everyone in publishing. I’m pleased I had<br />
this experience as I knew what point sizes would<br />
suit and which fonts were best to use.”<br />
I first approached Maryanne in late 1994 offering<br />
my services, which resulted in my first column<br />
appearing in early 1995. This is well covered in my<br />
recent twentieth-anniversary edition.<br />
NZ Optics has also been a family affair with<br />
Maryanne’s son Kyle working with Maryanne<br />
during the 1990’s, taking NZ Optics online during<br />
this time.<br />
Anita, Maryanne’s daughter-in-law then<br />
joined up full time and has been a co-owner<br />
of the magazine for the past twelve years. Her<br />
contribution has also been immense, doing much<br />
of the layout and production, reporting on and<br />
attending numerous events.<br />
NZ Optics is always an attractive publication,<br />
with solid editorial content. Anita has also helped<br />
Built on the ACUVUE ® MOIST Platform<br />
the #1 best-selling daily disposable brand around the globe 1<br />
Her Vision Will Change.<br />
Her Experience Won’t.<br />
arrange many conferences, shared her personal<br />
experiences with Ortho-K and LASIK and been a<br />
key part of the online presence.<br />
We’ll miss their familiar faces at future events!<br />
I’ll never forget an incident when I presented the<br />
2009 BCLA Pioneers Lecture at the Royal Society of<br />
Medicine in London. I was standing in the foyer at<br />
the tea break only to catch a glimpse of Anita out<br />
of the corner of my eye. I couldn’t believe that the<br />
two of them had travelled all the way to London to<br />
surprise me with their attendance and coverage of<br />
this milestone event in the December 2009 edition.<br />
Full credit to the Dransfield’s!<br />
It’s been a pleasure working with you for the<br />
past twenty years with many great memories and<br />
sharing fantastic meals in Queenstown, Omaha<br />
and Auckland.<br />
Rest assured NZ Optics is now in the capable<br />
hands of Lesley Springall who has much experience<br />
at the pointy end of NZ journalism, writing, PR<br />
and marketing. Lesley has written for The Herald,<br />
NZ Business, and Unlimited and covered a broad<br />
range of industries along the way. A stint in the UK,<br />
with high finance and venture capital adds to her<br />
extensive biography, I am sure she will continue<br />
the fine traditions of NZ Optics while continuing<br />
its evolutionary journey onwards and upwards.<br />
We wish Lesley much luck in her new venture and<br />
I look forward to working with her.<br />
Great Mentors<br />
July marked the passing of two friends and legends<br />
in contact lenses.<br />
Trevor John Duncan RNZAF 326872 8 April 1932<br />
– 12 July <strong>2015</strong>, passed away after a brief illness.<br />
Trevor was one of the founder members of the<br />
CCLS and was active on council for over three<br />
decades. He served as secretary/treasurer 1984-<br />
1986 and as President 1991-1992. He was made a<br />
life member of the CCLS in 1993 as recognition for<br />
his sterling contribution to contact lenses and the<br />
society.<br />
He again served as secretary/treasurer from 1999<br />
to 2008, which coincided with my time on council<br />
and term as president. It was during this time that<br />
I got to know Trevor well as a fellow councillor<br />
and friend. In this period we got the CCLS online<br />
and moved the administration to computer and<br />
email. I was impressed with how Trevor took on<br />
this challenge and it did not take him long to<br />
master email, Word, electronic accounting and<br />
maintenance of the online membership database.<br />
Having Trevor on council was fantastic as he had<br />
a great sense of humour, was always calm and<br />
rational and was a real gentleman. He was also<br />
always au fait with the rules, the history and the<br />
correct procedures for elections and AGMs. We<br />
achieved many positive things during this time<br />
including the name change from the NZSCLP to<br />
the CCLS and steps needed to keep the society<br />
relevant in the ever-evolving world of contact<br />
lenses and CPD, while warding off threats to the<br />
profession. We arranged numerous conferences<br />
in this time, when most of the work was done by<br />
council; as opposed to the current situation where<br />
professional conference organisers do much of the<br />
work. This required a massive input of time and<br />
effort, many meetings and countless emails. It is<br />
credit to Trevor that some of these conferences<br />
were rated as the ‘best conferences ever’ by<br />
attending delegates.<br />
Trevor had a sterling career in practice in<br />
Hamilton as a general optometrist and contact<br />
lens specialist and provided excellent care to tens<br />
of thousands of appreciative patients over the<br />
decades.<br />
There are many people who recall with pleasure<br />
and fond memories the many dive trips that he<br />
organised in NZ and the Pacific Islands. I’ve heard<br />
stories of legendary fishing trips, where copious<br />
quantities of beer were consumed.<br />
Trevor is also remembered as the author of<br />
the notoriously politically incorrect newsletters<br />
that he regularly sent out to CCLS members.<br />
Apart from keeping the membership up to date<br />
with the goings-on of the society, these always<br />
included some humour. We kept in touch by<br />
email until shortly before his passing. I always<br />
enjoyed receiving his jokes and at times raunchy<br />
communications. He also sent these to his dear<br />
friend, ophthalmologist David Sabiston, another<br />
early CCLS member, former president and life<br />
member of the society. Trevor was instrumental in<br />
corralling David into writing the amazing history<br />
of the CCLS and one in which Trevor (and David’s)<br />
names feature dozens of times. You can read the<br />
history via this link. Search for ‘Duncan’ to gain an<br />
insight into his staunch contribution.<br />
It was friendships like the one between David<br />
and Trevor that helped foster the unique and<br />
amazing relationship between optometry and<br />
ophthalmology in the CCLS that continues to<br />
thrive.<br />
Trevor is survived by his wonderful wife,<br />
Noeleen. They were married for fifty-nine years.<br />
She supported him greatly and he took great care<br />
of her in latter years, when macula degeneration<br />
made every day life challenging.<br />
He will be fondly remembered by friends,<br />
patients, colleagues and around two-dozen<br />
children, grandchildren and great-grandchildren.<br />
RIP old friend.<br />
Last but not least, the sudden passing of the<br />
legendary and larger-than-life, Brien Anthony<br />
Holden OAM, 06.01.1942 - 27.07.<strong>2015</strong> was a shock<br />
to everyone in the eye care world. One could write<br />
pages in tribute to Brien but this is well covered in<br />
numerous places on the web so I will not repeat it<br />
here. It is strangely coincidental that Optometry<br />
and Vision Science featured his enlightening 2014<br />
Prentice Award Speech in the July <strong>2015</strong> edition.<br />
I have known Brien since the late 1970s. He<br />
was an amazing character and in my view the<br />
gold standard of presenters, who I have striven to<br />
emulate. He was one of my prime motivators, who<br />
set me on the path to doing what I do in terms or<br />
presenting and writing.<br />
Some of the highlights of my speaking career<br />
have been presenting with Brien on the same<br />
stage and our debate at the 2010 BCLA was<br />
memorable. I loved his brash Aussie style. Of<br />
course he had his detractors and he offended<br />
a good few people. Brien is however one of the<br />
most internationally respected people in the eye<br />
care world. His amazing contribution to research,<br />
founding of the CCLRU - which though its variuos<br />
iterations has garnered an astounding $1.3 billion<br />
in funding over the past five decades - is part of his<br />
legacy. Among many things, this in turn lead to the<br />
co-development of the now ubiquitous siliconehydrogel<br />
contact lenses. Today these account for<br />
the majority of soft contact lens fittings.<br />
What is arguably more important going forward<br />
is his staunch and unfailing endeavor to erradicate<br />
preventable blindness among those less fortunate.<br />
He had strong moral convictions and humanitarian<br />
beliefs. In time I believe that his vision will see<br />
to it that millions of people will have their sight<br />
restored. His commitment to Global Vision was<br />
immense and I was honoured to cover it in an<br />
article for the Optician journal.<br />
I believe his dedication to myopia control will be<br />
significant, as it’s already proving to be.<br />
There are many other projects he was involved<br />
in. The perfection and commercialisation of<br />
the restoration of accomodation project, postpresbyopia<br />
and in cataract surgery, could become a<br />
multi-billion dollar industry in its own right.<br />
I have many wonferful memories of Brien. I<br />
recall with fondness the many interactions we<br />
had at conferences around the globe. Beer-fuelled<br />
sessions in hotel rooms, with interesting people,<br />
were the venue for many significant discussions.<br />
These often went on until sunrise. We’d have a<br />
quick power nap, dust ourseleves off and be back<br />
on the podium presenting, with few any the wiser<br />
as to the shennanigans of the night before.<br />
RIP mate. There will never be another like you.<br />
Now you can continue excellent care as her vision evolves into presbyopia<br />
with 1-DAY ACUVUE ® MOIST Brand MULTIFOCAL Contact Lenses<br />
94 %<br />
of patients were successfully fit<br />
with 2 pairs of lenses or less<br />
when using the Fitting Tips.*<br />
*Up to 4 lenses total. 1 JJVC Data on File <strong>2015</strong> (Internal Analysis, based on independent third-party data)<br />
Learn more about the<br />
predictable and positive<br />
fitting experience.<br />
ACUVUE® Brand Contact Lenses are indicated for vision correction. As with any contact lens, eye problems, including corneal ulcers, can develop. Some wearers may experience<br />
mild irritation, itching or discomfort. Lenses should not be prescribed if patients have any eye infection, or experience eye discomfort, excessive tearing, vision changes, redness or<br />
other eye problems. Consult the patient information guide for more information.<br />
Johnson & Johnson Vision Care, a division of Johnson & Johnson Pacific Pty Ltd., 45 Jones Street, Ultimo NSW 2007 Australia. Phone 1-800-125-024. www.acuvue.com.au.<br />
Johnson & Johnson Vision Care, a division of Johnson & Johnson (New Zealand) Ltd., 507 Mt. Wellington Highway, Mt. Wellington, Auckland 1060, New Zealand.<br />
Phone: 0800-449-535. www.acuvue.co.nz ®TM Registered Trademark. CCP 8785/15<br />
ACUVUE® and 1-DAY ACUVUE® MOIST are trademarks of Johnson & Johnson Vision Care Companies. © Johnson & Johnson Vision Care Companies <strong>2015</strong> 10314426-A April <strong>2015</strong><br />
Change of ownership in Marton<br />
A<br />
long<br />
established optometry<br />
practice in Marton, northwest of<br />
Palmerston North, has changed<br />
hands.<br />
David Newman Optometrist has been<br />
sold to Ross Tayler and renamed the Vision<br />
Experience Optometrist. It will remain in its<br />
central Marton main street location.<br />
Newman sold the practice to retire from<br />
optics after a 35-year career, but will<br />
continue to pursue his parallel career in<br />
music.<br />
Tayler graduated from the University<br />
of Auckland in 1994 and has worked<br />
in various practices in the lower North<br />
Island. He has been a member of the ODOB<br />
board since 2014 and serves on several<br />
committees. O<br />
22 NEW ZEALAND OPTICS <strong>Sep</strong>tember <strong>2015</strong>
AAOMC conference<br />
sees heaviest<br />
attendance<br />
BY JAGRUT LALLU, VISIQUE ROSE OPTOMETRISTS<br />
Over 500 people<br />
attended the<br />
Vision by<br />
Design <strong>2015</strong><br />
annual meeting of the<br />
American Academy of<br />
Orthokeratology & Myopia<br />
Control (AAOMC), the<br />
highest attendance in its<br />
history.<br />
The assembly doubled<br />
as the fourth meeting of<br />
the International Academy<br />
of Orthokeratology (IAO),<br />
with over 40 countries<br />
from the IAO’s five regional<br />
associations represented.<br />
The IAO at the meeting<br />
launched its sixth region<br />
covering southeast Asia,<br />
India, and Africa initiated.<br />
The AAOMC meeting<br />
featured presentations<br />
on inwardly focused lens<br />
design, pharmaceutical<br />
and multifocal<br />
lens interventions,<br />
ergonomic and binocular<br />
modifications, and<br />
unique treatment options<br />
employed in China. Other<br />
panel sessions covered<br />
troubleshooting Ortho-K,<br />
scleral lens designs,<br />
practice management, and<br />
Ortho-K practice in other<br />
countries.<br />
Vision By Design also<br />
launched the first Ortho-K<br />
Mentoring event, in which<br />
new AAOMC members<br />
were paired with veterans<br />
to act as mentors through<br />
the event. Over half the<br />
attendees were firsttimers.<br />
The Orthokeratology<br />
Society of Oceania section<br />
of the IAO will hold its<br />
next international meeting<br />
in October 2016 on the<br />
Gold Coast. For more<br />
information about the<br />
Oceania society, visit<br />
www.osa.net.au or email<br />
jlallu@visique.co.nz. O<br />
Scent of Sunnies<br />
Luxury eyewear brand Oliver Peoples has partnered with<br />
Ben Gorham’s Stockholm-based fragrance house, Byredo,<br />
to explore the intersection of sight and scent.<br />
The collaboration was inspired by synesthesia, a<br />
phenomenon in which stimulation of one sense involuntarily<br />
produces an association with a different sense.<br />
The collaboration involves Byredo’s master perfumer perceiving<br />
the sights of Los Angeles through different coloured lenses, and<br />
translating them into various smells, producing a multi-faceted<br />
fragrance. The result is an original Oliver Peoples frame through<br />
which the colour of the lenses correlate with the aroma of the<br />
custom-blended fragrance by Byredo. O<br />
Banner year<br />
for Australian<br />
optometry<br />
researcher<br />
It’s been a banner year<br />
for Queensland-based<br />
Professor Nathan Efron.<br />
Efron is the recipient<br />
of the <strong>2015</strong> H Barry Collin<br />
Research Medal, awarded<br />
by Optometry Australia and<br />
considered the premier prize<br />
for optometry researchers<br />
across the ditch.<br />
Efron will deliver a medal<br />
address when he receives the<br />
medal at Optometry Australia’s<br />
Southern Regional Conference<br />
in Melbourne next March. He is<br />
the ninth researcher to receive<br />
the medal, a list that includes<br />
the late Professor Brien Holden,<br />
who won the award in 1988.<br />
Efron has received other<br />
accolades this year, recognising<br />
his ongoing contribution<br />
to eye health. He was<br />
named Companion in the<br />
General Division of the<br />
Order of Australia, for<br />
clinical optometry work<br />
in vision correction and<br />
corneal physiology, and as<br />
an academic, researcher<br />
and author. The award is<br />
bestowed by the Queen of<br />
England.<br />
Efron also received the<br />
Kenneth W Bell Medal<br />
from the Cornea and<br />
Contact Lens Society of<br />
Australia for extensive<br />
commitment and research<br />
achievements in the field<br />
of contact lenses and the<br />
anterior segment. O<br />
Professor Nathan Efron<br />
A limited edition sunglass and fragrance blend from Byredo and Oliver<br />
Peoples<br />
NEW APPOINTMENT<br />
Guy Whittaker appointed<br />
VP, global marketing for<br />
CooperVision<br />
Guy Whittaker has been<br />
appointed vice president, global<br />
marketing for CooperVision,<br />
with responsibility for<br />
advancing the company’s master and<br />
product brands, marketing its range of<br />
contacts lens products and services, and<br />
strengthening the company’s reputation<br />
worldwide with customers.<br />
A former practising optometrist, Whittaker has held<br />
management roles with CooperVision since 1998. Most<br />
recently he was general manager, Australia/New Zealand<br />
and Southeast Asia, and Vice President, Strategy, Asia-<br />
Pacific. O<br />
YOU WON’T SEE A MORE COMPREHENSIVE<br />
1-2<br />
RANGE OF SURFACE PROTECTION.<br />
Soothe, rehydrate and protect sore, dry eyes.<br />
ALWAYS READ THE LABEL. USE ONLY AS DIRECTED. IF SYMPTOMS PERSIST OR YOU EXPERIENCE SIDE EFFECTS, SEE YOUR HEALTHCARE PROFESSIONAL. KEEP OUT OF REACH OF CHILDREN.<br />
Reference: 1. Davitt WF, Bloomenstein M, Christensen M, et al. Efficacy in patients with dry eye after treatment with a new lubricant eye drop formulation. J Ocul Pharmacol Ther. 2010;26(4):<br />
347–353. 2. Christensen MT. Corneal staining reductions observed after treatment with Systane Lubricant Eye Drops. Adv Ther. 2008 Nov;25(11):1191–9. doi: 10.1007/s12325-008-0112-0.<br />
Alcon Laboratories (Australia) Pty Ltd. 10/25 Frenchs Forest Road East, Frenchs Forest NSW 2086. Distributed by Pharmaco (NZ) Ltd in New Zealand, 4 Fisher Crescent, Mt. Wellington, Auckland.<br />
Ph 0800 101 106. POPH.15106. NP4. A21507352611. TAPS.PP6917.<br />
<strong>Sep</strong>tember <strong>2015</strong><br />
NEW ZEALAND OPTICS<br />
23
SPECIALIST SHOPFITTERS & DESIGNERS TO THE OPTOMETRIC PROFESSION<br />
TEL:(09) 486-2070 MOB:(0274) 798-798<br />
Email: tony.maddocks@xtra.co.nz<br />
LOCUM OPTOMETRIST AVAILABLE<br />
Bharat Raniga. Call 021424253 or Email: bharatraniga@yahoo.com<br />
TRAINEE DISPENSING OPTICIAN<br />
We are looking for a motivated, friendly, enthusiastic team player<br />
to join our Tauranga family practice. This is an immediate start<br />
as an optical receptionist while training to qualify as a future DO.<br />
This is a full time position Monday-Friday; occasional Saturday<br />
morning cover may be required.<br />
Further information email: kmiller@visique.co.nz.<br />
TRACEY JONES OPTOMETRIST<br />
Seeking permanent position(s) in Auckland<br />
LinkedIn, 027 225 7112, traceyjonesoptometrist@gmail.com<br />
RARE OPPORTUNITY<br />
We have a lifestyle practice serving a semi-rural community<br />
for sale not far from central Auckland. Ideally suited for an<br />
optometrist wanting to work for themselves and have all the<br />
flexibility that goes with being an owner operator. Could also be<br />
ideal business opportunity for a mum wanting to return from<br />
maternity leave providing the flexibility that is needed. Double<br />
digit earnings with potential for further growth earnings.<br />
If you think this sounds like you, please apply in the strictest<br />
confidence c/- NZ Optics, info@nzoptics.co.nz Code PFSS1.<br />
LOCUM OPTOMETRIST - AUCKLAND & NZ<br />
Thomas Cheong. 021 210 8098 or cheong.thomas@gmail.com<br />
WANT YOUR OWN PRACTICE?<br />
Owner/optometrist Jan Thompson is selling her West Auckland<br />
practice, Westgate Optometrists. Those interested in taking over<br />
an independent practice that has been established in its current<br />
location for over a decade is welcome to send a confidential<br />
enquiry to westopt@ihug.co.nz or stu@opticsnz.co.nz.<br />
DO YOU SEE YOURSELF MAKING A DIFFERENCE?<br />
Does the challenge of working at the coalface excite you?<br />
You’ll want to go out of our way to find solutions for our<br />
wonderful clients? You will have great lens and dispensing<br />
skills, good technical aptitude, and enjoy sharing knowledge<br />
to coach others. Of course, you’ll understand technology and<br />
the importance of all the systems that make things happen.<br />
Combined with great communication skills, and showing care and<br />
attention to detail you could be just the person we’re looking for.<br />
Our team in South Auckland is made up of dedicated and highly<br />
motivated optometrists and support staff. Fun and friendly<br />
interactions are our specialty. You’ll enjoy the opportunity to be<br />
part of our business growth.<br />
If this sounds like you then call 0220128761 and leave your<br />
contact details and a short message.<br />
MAGNIFIERS + MORE<br />
Dear Colleagues,<br />
Thanks for sending me your low vision patients. I love<br />
helping them.<br />
I have headed offshore to observe low vision clinics and<br />
learn more about visual rehabilitation, so please keep<br />
sending those referrals, but let them know I will contact<br />
them on my return in mid-October.<br />
Greetings from the other side of the world.<br />
Naomi Meltzer<br />
Naomi Meltzer<br />
BSc, Dip Opt, P-G Dip<br />
Rehab<br />
Low Vision Consultant<br />
Optometrist<br />
P.O. Box 29021<br />
Greenwoods Corner<br />
Auckland 1347<br />
info@sightloss-services.com<br />
LOCUM OPTOMETRIST - AUCKLAND<br />
Mellissa Teh. Call 021 157 1136 or Email: hetassillem@gmail.com.<br />
OPTICAL ASSISTANT/RECEPTIONIST<br />
Mt. Albert Optometrists seeks an optical assistant / receptionist<br />
We are a longstanding small independent practice that<br />
endeavours to offer old fashioned friendly and personal service<br />
with a smile. We are seeking someone to work ideally 4 to 5<br />
weekdays per week.<br />
If you have a passion for dealing with people, an eye for detail and<br />
are self motivated we would love to hear from you. No late nights<br />
or weekends, free onsite parking.<br />
Experience with Optomate and a passion for finding the ‘perfect<br />
frame ‘ would be an advantage.<br />
All inquiries are strictly confidential . Please email expressions of<br />
interest to Christina at cherrick73@gmail.com.<br />
With growth continuing, our store teams<br />
are currently seeking optometrists to fill<br />
3-month, 6-month or permanent roles<br />
in the following NZ practice locations:<br />
• Invercargill<br />
• Timaru<br />
• Wellington CBD<br />
• Gisborne<br />
• Auckland CBD<br />
• Whangarei<br />
• Keri Keri<br />
• Albany<br />
We are currently also seeking<br />
experienced dispensers for a variety<br />
of our New Zealand stores.<br />
Alternatively, if you're interested in<br />
a move to Australia – either short or<br />
longer term, talk to us for the lowdown<br />
on possible locations in all states.<br />
To discuss any of the opportunities<br />
availalble, please contact<br />
Yvette Michael on 0800 228 417 or<br />
yvette.michael@specsavers.com<br />
NZ AND AUSTRALIAN<br />
OPPORTUNITIES!<br />
Family reunion for<br />
Curtis Vision and CLC<br />
Christchurch optometrists Curtis Vision has<br />
established a new location, sharing facilities with<br />
Corneal Lens Corporation’s laboratory in Wigram,<br />
Christchurch.<br />
The two companies sprang from the same family-owned<br />
business which has deep roots in the Canterbury region.<br />
Michael Curtis took on the optometry side and his brother<br />
Graeme runs the well-known Kiwi lens manufacturing<br />
business.<br />
“We used to be in the same building in Christchurch,<br />
but with the earthquake that site wasn’t sustainable so<br />
the Corneal Lens Corporation built in Wigram,” says Chris<br />
Clark, a director for Curtis Vision.<br />
Curtis Vision has three other shops around Christchurch,<br />
while the Wigram site operates a few days a week as a<br />
specialty practice focused on contact lenses.<br />
Clark says the site was a natural fit for Curtis Vision as<br />
Wigram has little competition, despite rapid development<br />
due to the reconstruction of Christchurch. It also fills a<br />
space Corneal Lens Corporation had set aside when it<br />
built its facility. “Michael is highly regarded in contact lens<br />
work, and working with complicated scrips, so it’s ideal for<br />
them to work together,” says Clark.<br />
Clark did not say when the Wigram site would expand<br />
beyond its part-time, contact lens work, but he says plans<br />
for the site include a full spectrum service and training for<br />
other optometrists.<br />
Curtis Vision is part of the EyePro network of<br />
independent optometrists, for which Clark also serves as a<br />
director. There are 55 optometrists associated with EyePro,<br />
located around New Zealand. O<br />
B4 eye exams serve<br />
most eligible children<br />
The government announced a record 92 per cent of eligible<br />
four-year-olds are now receiving a B4 School Check vision<br />
exam.<br />
“The B4 School Checks help to give children the best<br />
start at school by identifying and addressing any potential<br />
health or developmental problems at an early stage,” said Health<br />
Minister Jonathan Coleman in a statement. “The checks are also<br />
supporting families by connecting them to the health and support<br />
services they need.”<br />
The B4 School Check is a national programme offered to all<br />
families with children turning four. It is the final core of the<br />
Well Child/Tamariki Ora check provided free through a range of<br />
community health services. It includes hearing, eyesight, height,<br />
weight, and oral health assessments, as well as comprehensive<br />
health and development assessment, and costs the government<br />
about $10 million a year to provide. O<br />
24 NEW ZEALAND OPTICS <strong>Sep</strong>tember <strong>2015</strong>