Dry Eye 2016
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
SPECIAL FEATURE: DRY EYE<br />
Characterisation of the ocular surface microbiome<br />
BY GRANT WATTERS*<br />
Understanding and managing ocular surface<br />
disorders such as anterior blepharitis,<br />
meibomian gland dysfunction and<br />
dry eye disease remains challenging. Many of<br />
these conditions, being chronic, recurrent and<br />
debilitating, frustrate patients and clinicians alike<br />
with a plethora of treatments that are, at best,<br />
usually only partially effective¹.<br />
As in the intestine, there is a growing belief that<br />
dysregulation of the normal ocular commensal<br />
microbiota population may contribute to many of<br />
these conditions, so understanding the resident<br />
ocular surface microbiome in normal and diseased<br />
states may give us some clues as to whether we<br />
could more accurately regulate these microbe<br />
populations as a therapeutic strategy².<br />
Extensive research into the role that bacteria<br />
have in eyelid disease began with Thygeson’s work<br />
in the early half of the 20th century. He identified<br />
gram-positive (gm+) Staphylococcus aureus (S.<br />
aureus) as the organism most frequently isolated<br />
from the lid margins of blepharitis sufferers.<br />
Author(s);<br />
(year published)<br />
Albietz & Lenton<br />
(2006)<br />
Graham et al<br />
(2007)<br />
Bowman et al<br />
(1987)<br />
Dougherty &<br />
McCulley (1984)<br />
Groden et al<br />
(1991)<br />
Watters et al<br />
(<strong>2016</strong>)<br />
Country N C-N S<br />
(%)<br />
S.Aureus<br />
(%)<br />
P.acnes<br />
(%)<br />
Corynebact.<br />
sp.(%)<br />
Subsequent studies showed that while S. aureus<br />
was more common in blepharitis, coagulasenegative<br />
Staphylococcus (C-NS) was the most<br />
prevalent organism. Anaerobic gram-positive<br />
Proprionibacterium acnes (P. acnes) was also found<br />
to be more prevalent in eyes with lid disease 3,4 .<br />
We* have recently completed a study across<br />
three departments here at Auckland University<br />
to characterise the ocular surface microbiome<br />
present in New Zealanders with and without<br />
eyelid disease. Inferior lid margin swabs were<br />
collected from 157 randomly selected subjects<br />
subdivided into three categories: no lid disease<br />
(normal: n= 66); mild-to moderate lid disease (n=<br />
41), and moderate-to severe lid disese (n= 50).<br />
We also compared contact lens (CL) wearers and<br />
non-CL wearers. All subjects were analysed for<br />
aerobic isolates and 87 subjects were additionally<br />
investigated for anaerobic bacteria (P. acnes) 5 .<br />
Table 1. summarises our results in New Zealand<br />
normal eyes compared to relevant overseas<br />
studies. Of note is our sample exhibited a relatively<br />
higher percentage of individuals with S. aureus, a<br />
slightly lower incidence of C-NS, and an absence<br />
of Corynebacterium<br />
Streptococcus<br />
sp.(%)<br />
Australia* 18 84.0 6.0 22.0 6.0 0 6.0<br />
Ireland* 12 81.0 0 19.0 19.0 6.0 6.0<br />
Texas USA* 21 100.0 13.0 31.0 69.0 6.0 9.0<br />
Texas USA* 47 95.7 8.5 87.2 63.8 - -<br />
Florida USA* 160 87.5 15.6 73.7 45.0 - 4.3<br />
New<br />
Zealand*<br />
39 64.1 48.7 25.6 0 0 5.1<br />
Rubio (2004) Spain # 4366 56.8 6.4 - 30.2 7.5 6.2<br />
Hsu et al (2013)<br />
de Kaspar et al<br />
(2005)<br />
Capriotti et al<br />
(2009)<br />
Karthika et al<br />
(2014)<br />
Missouri<br />
USA #<br />
California<br />
USA #<br />
Sierra Leone<br />
(Rural) #<br />
India<br />
(Rural) #<br />
183 74.8 4.9 - 7.6 0.9 9.4<br />
162 76.0 11.7 - - 4.9 6.8<br />
276 28.6 19.9 - - - 16.0<br />
100 32.0 10.0 - 11.0 2.0 -<br />
Gm neg. rods inc.<br />
Pseudomonas (%)<br />
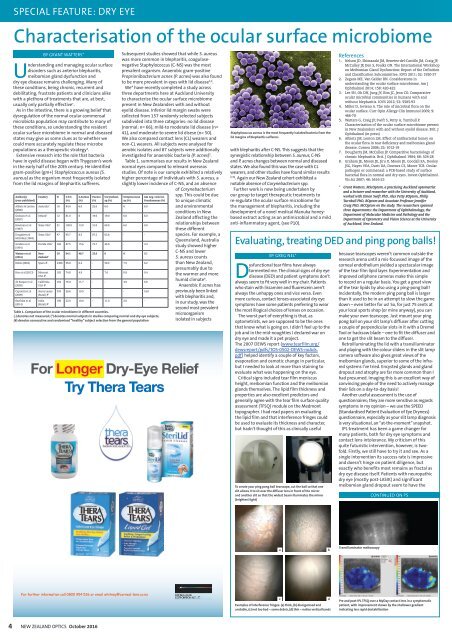
Table 1. Comparison of the ocular microbiome in different countries.<br />
(-) denotes not measured; (*) denotes normal subjects in studies comparing normal and dry eye subjects;<br />
(#) denotes consecutive and randomised “healthy” subject selection from the general population<br />
spp. This could be due<br />
to unique climatic<br />
and environmental<br />
conditions in New<br />
Zealand affecting the<br />
relationships between<br />
these different<br />
species. For example, a<br />
Queensland, Australia<br />
study showed higher<br />
C-NS and lower<br />
S. aureus counts<br />
than New Zealand,<br />
presumably due to<br />
the warmer and more<br />
humid climate 6 .<br />
Anaerobic P. acnes has<br />
previously been linked<br />
with blepharitis and,<br />
in our study, was the<br />
second most prevalent<br />
microorganism<br />
isolated in subjects<br />
For Longer <strong>Dry</strong>-<strong>Eye</strong> Relief<br />
Try Thera Tears<br />
Staphylococcus aureus is the most frequently isolated bacteria from the<br />
lid margins of blepharitis sufferers<br />
with blepharitis after C-NS. This suggests that the<br />
synergistic relationship between S. aureus, C-NS<br />
and P. acnes changes between normal and diseased<br />
states. We also found this was the case with CL<br />
wearers, and other studies have found similar results<br />
(7,8)<br />
. Again our New Zealand cohort exhibited a<br />
notable absence of Corynebacterium spp.<br />
Further work is now being undertaken by<br />
our group to target therapeutic treatments to<br />
re-regulate the ocular surface microbiome for<br />
the management of blepharitis, including the<br />
development of a novel medical Manuka honeybased<br />
extract acting as an antimicrobial and a mild<br />
anti-inflammatory agent, (see P10).<br />
BY GREG NEL*<br />
Dysfunctional tear films have always<br />
tormented me. The clinical signs of dry eye<br />
disease (DED) and patient symptoms don’t<br />
always seem to fit very well in my chair. Patients<br />
who stain with lissamine and fluorescein aren’t<br />
always the unhappy ones and vice versa. Even<br />
more curious, contact lenses-associated dry eye<br />
symptoms have some patients preferring to wear<br />
the most illogical choices of lenses on occasion.<br />
The worst part of everything is that, as<br />
optometrists, we are supposed to be the ones<br />
that know what is going on. I didn’t feel up to the<br />
job and in the mid-noughties I declared war on<br />
dry eye and made it a pet project.<br />
The 2007 DEWS report (www.tearfilm.org/<br />
dewsreport/pdfs/TOS-0502-DEWS-noAds.<br />
pdf) helped identify a couple of key factors,<br />
evaporation and osmotic change in particular,<br />
but I needed to look at more than staining to<br />
evaluate what was happening on the eye.<br />
Critical signs included tear film meniscus<br />
height, meibomian function and the meibomian<br />
glands themselves. The lipid film thickness and<br />
properties are also excellent predictors and<br />
generally agree with the tear film surface quality<br />
assessment (TFSQ) module on the Medmont<br />
topographer. I had read papers on evaluating<br />
the lipid film and that interference fringes could<br />
be used to evaluate its thickness and character,<br />
but hadn’t thought of this as clinically useful<br />
To create your ping pong ball tearscope, cut the ball so that one<br />
slit allows it to sit over the diffuser lens in front of the mirror<br />
and another slit so that the widest beam illuminates the mirror<br />
(brightest light)<br />
References<br />
1. Nelson JD, Shimazaki JM, Benetez-del-Castillo JM, Craig JP,<br />
McCulley JP, Den S, Foulks GN. The International Workshop<br />
on Meibomian Gland Dysfunction: Report of the Definition<br />
and Classification Subcommittee. IOVS 2011; 52: 1930-37<br />
2. Zegans ME, Van Gelder RN. Consideratons in<br />
understanding the ocular surface microbiome. Am J<br />
Ophthalmol 2014; 158: 420-422<br />
3. Lee SH, Oh DH, Jung JY, Kim JC, Jeon CO. Comparative<br />
ocular microbial communities in humans with and<br />
without blepharitis. IOVS 2012; 53: 5585-93<br />
4. Miller D, Iovieno A. The role of microbial flora on the<br />
ocular surface. Curr Opin Allergy Clin Immunol 2009; 9:<br />
466-70<br />
5. Watters G, Craig JP, Swift S, Petty A, Turnbull P.<br />
Characterisation of the ocular surface microbiome present<br />
in New Zealanders with and without eyelid disease. Brit. J<br />
Ophthalmol (in press)<br />
6. Albietz JM, Lenton LM. Effect of antibacterial honey on<br />
the ocular flora in tear deficiency and meibomian gland<br />
disease. Cornea 2006; 25: 1012-19<br />
7. Dougherty JM, McCulley JP. Comparitive bacteriology of<br />
chronic blepharitis. Brit. J Ophthalmol 1984; 68: 524-28<br />
8. Graham JE, Moore JE, Jiru X, Moore JE, Goodall EA, Dooley<br />
JSG, Hayes VEA, Dartt DA, Downes CS, Moore TCB. Ocular<br />
pathogen or commensal: a PCR-based study of surface<br />
bacterial flora in normal and dry eyes. Invest.Ophthalmol.<br />
Vis.Sci 2007; 48: 5616-23<br />
* Grant Watters, MScOptom, a practicing Auckland optometrist<br />
and a lecturer and researcher with the University of Auckland,<br />
worked with Simon Swift PhD, Alex Petty BOptom, Philip<br />
Turnbull PhD, BOptom and Associate Professor Jennifer<br />
Craig PhD, MCOptom on the study. The researchers spanned<br />
three departments: the Department of Ophthalmology, the<br />
Department of Molecular Medicine and Pathology and the<br />
Department of Optometry and Vision Science at the University<br />
of Auckland, New Zealand.<br />
Evaluating, treating DED and ping pong balls!<br />
because tearscopes weren’t common outside the<br />
research arena until a mis-focussed image of the<br />
corneal endothelium yielded a spectacular image<br />
of the tear film lipid layer. Experimentation and<br />
improved cellphone cameras make this simple<br />
to record on a regular basis. You get a great view<br />
of the tear lipids by also using a ping-pong ball!<br />
Incidentally, the modern ping pong ball is larger<br />
than it used to be in an attempt to slow the game<br />
down – even better for us! So, for just 75 cents at<br />
your local sports shop (or mine anyway), you can<br />
make your own tearscope. Just mount your ping<br />
pong ball on your slit lamp’s diffuser after cutting<br />
a couple of perpendicular slots in it with a Dremel<br />
Tool or hacksaw blade – one to fit the diffuser and<br />
one to get the slit beam to the diffuser.<br />
Retroilluminating the lid with a transilluminator<br />
and playing with the colour sliders in the slit lamp<br />
camera software also gives great views of the<br />
meibomian glands, superior to some of the infrared<br />
systems I’ve tried. Encysted glands and gland<br />
dropout and atrophy are far more common than I<br />
had presumed. Imaging this is an excellent way of<br />
convincing people of the need to actively manage<br />
their lids on a day-to-day basis!<br />
Another useful assessment is the use of<br />
questionnaires; they are more sensitive as regards<br />
symptoms in my opinion – we use the SPEED<br />
(Standardised Patient Evaluation of <strong>Eye</strong> <strong>Dry</strong>ness)<br />
questionnaire, especially as your slit lamp diagnosis<br />
is very situational, an “at-the-moment” snapshot.<br />
IPL treatment has been a game changer for<br />
many patients, both for dry eye symptoms and<br />
contact lens intolerance. My criticism of this<br />
quite futuristic intervention, however, is twofold.<br />
Firstly, we still have to try it and see. As a<br />
single intervention its success rate is impressive<br />
and doesn’t hinge on patient diligence, but<br />
exactly who benefits most remains as fractal as<br />
dry eye disease itself. Patients with neuropathic<br />
dry eye (mostly post-LASIK) and significant<br />
meibomian gland dropout seem to have the<br />
CONTINUED ON P5<br />
a<br />
b<br />
Transilluminator meiboscopy<br />
For further information call 0800 954 536 or email whitney@corneal-lens.co.nz<br />
c<br />
Examples of interference fringes: (a) thick, (b) disorganised and<br />
unstable, (c) not too bad – some debris, (d) thin – notice vertical bands<br />
d<br />
Pre and post-IPL TFSQ over a MyDay contact lens in a symptomatic<br />
patient, with improvement shown by the shallower gradient<br />
indicating less rapid destabilisation<br />
4 NEW ZEALAND OPTICS October <strong>2016</strong>