The Voice of Southwest Louisiana April 2018 Issue
The Voice of Southwest Louisiana News Magazine April 2018
The Voice of Southwest Louisiana News Magazine April 2018
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
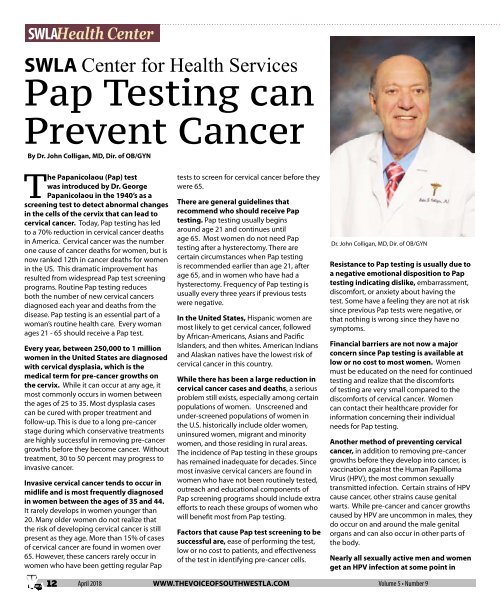
SWLA Health Center<br />
SWLA Center for Health Services<br />
Pap Testing can<br />
Prevent Cancer<br />
By Dr. John Colligan, MD, Dir. <strong>of</strong> OB/GYN<br />
<strong>The</strong> Papanicolaou (Pap) test<br />
was introduced by Dr. George<br />
Papanicolaou in the 1940’s as a<br />
screening test to detect abnormal changes<br />
in the cells <strong>of</strong> the cervix that can lead to<br />
cervical cancer. Today, Pap testing has led<br />
to a 70% reduction in cervical cancer deaths<br />
in America. Cervical cancer was the number<br />
one cause <strong>of</strong> cancer deaths for women, but is<br />
now ranked 12th in cancer deaths for women<br />
in the US. This dramatic improvement has<br />
resulted from widespread Pap test screening<br />
programs. Routine Pap testing reduces<br />
both the number <strong>of</strong> new cervical cancers<br />
diagnosed each year and deaths from the<br />
disease. Pap testing is an essential part <strong>of</strong> a<br />
woman’s routine health care. Every woman<br />
ages 21 - 65 should receive a Pap test.<br />
Every year, between 250,000 to 1 million<br />
women in the United States are diagnosed<br />
with cervical dysplasia, which is the<br />
medical term for pre-cancer growths on<br />
the cervix. While it can occur at any age, it<br />
most commonly occurs in women between<br />
the ages <strong>of</strong> 25 to 35. Most dysplasia cases<br />
can be cured with proper treatment and<br />
follow-up. This is due to a long pre-cancer<br />
stage during which conservative treatments<br />
are highly successful in removing pre-cancer<br />
growths before they become cancer. Without<br />
treatment, 30 to 50 percent may progress to<br />
invasive cancer.<br />
Invasive cervical cancer tends to occur in<br />
midlife and is most frequently diagnosed<br />
in women between the ages <strong>of</strong> 35 and 44.<br />
It rarely develops in women younger than<br />
20. Many older women do not realize that<br />
the risk <strong>of</strong> developing cervical cancer is still<br />
present as they age. More than 15% <strong>of</strong> cases<br />
<strong>of</strong> cervical cancer are found in women over<br />
65. However, these cancers rarely occur in<br />
women who have been getting regular Pap<br />
tests to screen for cervical cancer before they<br />
were 65.<br />
<strong>The</strong>re are general guidelines that<br />
recommend who should receive Pap<br />
testing. Pap testing usually begins<br />
around age 21 and continues until<br />
age 65. Most women do not need Pap<br />
testing after a hysterectomy. <strong>The</strong>re are<br />
certain circumstances when Pap testing<br />
is recommended earlier than age 21, after<br />
age 65, and in women who have had a<br />
hysterectomy. Frequency <strong>of</strong> Pap testing is<br />
usually every three years if previous tests<br />
were negative.<br />
In the United States, Hispanic women are<br />
most likely to get cervical cancer, followed<br />
by African-Americans, Asians and Pacific<br />
Islanders, and then whites. American Indians<br />
and Alaskan natives have the lowest risk <strong>of</strong><br />
cervical cancer in this country.<br />
While there has been a large reduction in<br />
cervical cancer cases and deaths, a serious<br />
problem still exists, especially among certain<br />
populations <strong>of</strong> women. Unscreened and<br />
under-screened populations <strong>of</strong> women in<br />
the U.S. historically include older women,<br />
uninsured women, migrant and minority<br />
women, and those residing in rural areas.<br />
<strong>The</strong> incidence <strong>of</strong> Pap testing in these groups<br />
has remained inadequate for decades. Since<br />
most invasive cervical cancers are found in<br />
women who have not been routinely tested,<br />
outreach and educational components <strong>of</strong><br />
Pap screening programs should include extra<br />
efforts to reach these groups <strong>of</strong> women who<br />
will benefit most from Pap testing.<br />
Factors that cause Pap test screening to be<br />
successful are, ease <strong>of</strong> performing the test,<br />
low or no cost to patients, and effectiveness<br />
<strong>of</strong> the test in identifying pre-cancer cells.<br />
Dr. John Colligan, MD, Dir. <strong>of</strong> OB/GYN<br />
Resistance to Pap testing is usually due to<br />
a negative emotional disposition to Pap<br />
testing indicating dislike, embarrassment,<br />
discomfort, or anxiety about having the<br />
test. Some have a feeling they are not at risk<br />
since previous Pap tests were negative, or<br />
that nothing is wrong since they have no<br />
symptoms.<br />
Financial barriers are not now a major<br />
concern since Pap testing is available at<br />
low or no cost to most women. Women<br />
must be educated on the need for continued<br />
testing and realize that the discomforts<br />
<strong>of</strong> testing are very small compared to the<br />
discomforts <strong>of</strong> cervical cancer. Women<br />
can contact their healthcare provider for<br />
information concerning their individual<br />
needs for Pap testing.<br />
Another method <strong>of</strong> preventing cervical<br />
cancer, in addition to removing pre-cancer<br />
growths before they develop into cancer, is<br />
vaccination against the Human Papilloma<br />
Virus (HPV), the most common sexually<br />
transmitted infection. Certain strains <strong>of</strong> HPV<br />
cause cancer, other strains cause genital<br />
warts. While pre-cancer and cancer growths<br />
caused by HPV are uncommon in males, they<br />
do occur on and around the male genital<br />
organs and can also occur in other parts <strong>of</strong><br />
the body.<br />
Nearly all sexually active men and women<br />
get an HPV infection at some point in<br />
12<br />
<strong>April</strong> <strong>2018</strong> WWW.THEVOICEOFSOUTHWESTLA.COM Volume 5 • Number 9