Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Nike & Zeiss: a new<br />
innovation<br />
SPECIALITY CL FORUM BY JACOB BENFIELD*<br />
JURASSIC PARK, CLS AND A CATARACT<br />
As the guest writer for this<br />
issue’s speciality contact lens<br />
forum, I thought I would<br />
tackle a problem I have encountered<br />
a few times and feel may become<br />
more common as we test an aging<br />
population.<br />
First we have to go back, way back,<br />
to my penultimate year at university.<br />
Sitting in a lecture about the history<br />
of contact lenses, I learned all about<br />
dental technician Eugene Hirst<br />
who brought rigid contact lenses<br />
to New Zealand around the Second<br />
World War. We heard how these<br />
lenses, made of PMMA and other<br />
old materials, took off and soon<br />
became common place. We talked<br />
about the challenges of fitting and looking after<br />
patients with hard contact lenses and how more<br />
modern materials had replaced them. Despite<br />
this, we were warned, we would still occasionally<br />
see patients who had been in hard contact lenses<br />
for several decades. They might even be PMMA or<br />
other old materials. These patients were known<br />
affectionately as ‘dinosaurs’.<br />
This leads me today’s patient, a 70-year-old<br />
female – ‘LS’ – who has been in hard contact<br />
lenses for at least 40 years. LS presented to my<br />
practice as a new patient and is a true ‘dinosaur’<br />
– not only is she a full-time wearer but she is<br />
still in PMMA. LS had noticed a reduction in<br />
vision over the past few months particularly in<br />
her right eye, and felt her contact lenses needed<br />
an update or a polish. On examination it was<br />
revealed a cataract was the underlying cause.<br />
It makes sense that these patients who have<br />
been in contact lenses for thirty or forty years<br />
may be coming in with blurry vision more often.<br />
Even if they started lens wear in their twenties<br />
they will at least be getting into their sixties<br />
now, increasing the chance of cataract, macular<br />
degeneration and other pathologies. I discussed<br />
with LS that the cataract was blurring her vision<br />
not the contact lenses and she wanted to have<br />
this dealt with. Having been short-sighted her<br />
whole life she was keen following cataract<br />
surgery to still be slightly short-sighted for<br />
the convenience of reading unaided. This got<br />
me thinking about the effect PMMA has had<br />
on her cornea and the potential effect on her<br />
prescription and final cataract outcome.<br />
PMMA and its effects on the eyes are well<br />
known to optometrists with lack of oxygen<br />
leading to oedema and corneal warpage among<br />
other things. A topography following PMMA wear<br />
shows this warpage (fig 1.) with irregular mires<br />
and an irregular surface. This is immediately<br />
noticeable to patients who switch from their<br />
lenses into spectacles and notice blurry vision.<br />
This patient has spent every waking moment<br />
in PMMA lenses for the past 40 years with no<br />
spectacle wear and hence no obvious blur. Of<br />
course older, less oxygen permeable materials<br />
have been dying off for more cornea-friendly<br />
options such as Boston XO. But even these newer<br />
materials can affect the cornea if the lens is<br />
poorly fitting or if it flexes as it ages. This change<br />
in corneal shape is of course not always bad and<br />
with new designs and materials have started the<br />
orthokeratology revolution.<br />
Back to LS then. After removing the contact<br />
lenses my initial refraction was R -7.50/ -1.50<br />
x 45 (6/12-) and L -5.75/ -2.00 x 155 (6/7.5-). I<br />
advised LS that for the best cataract outcome she<br />
will need to cease contact lens wear and wear<br />
spectacles until her corneas stabilise. I got her<br />
back after one week without contact lenses and<br />
the prescription was now quite different, at R<br />
-7.50/ -4.50 x 80 (6/21) and L -4.50/ -3.00 x 160<br />
(6/9.5+).<br />
At this stage I wasn’t happy to prescribe<br />
spectacles so I got LS back once more a week<br />
later and things were quite similar to the week<br />
before so I gave her a pair of single vision<br />
distance spectacles. This got me thinking about<br />
when was an appropriate time to review LS and<br />
when do we expect her corneas to stabilise?<br />
Fig 1: A topography showing corneal warpage<br />
Further reading made me realise the answer<br />
to this was really ‘how long is a piece of string’.<br />
A study by Wang et al 1 found the average<br />
resolution time of corneal warpage was eight<br />
weeks but this had a standard deviation of<br />
nearly seven weeks! Based on this I got LS back<br />
two months later and her prescription was now<br />
R -4.00/ -4.00 x 80 (6/12) and L -4.50/ -1.00 x 80<br />
(6/7.5-).<br />
The end was in sight! Vision was stabilising,<br />
retinoscopy reflex was good and corneas were<br />
clear on slit lamp. To be safe I got LS back<br />
once more one month later and found the<br />
prescription was stable. Success! I have since<br />
referred LS for private right cataract surgery to<br />
be followed with left cataract surgery to balance<br />
any anisometropia.<br />
There may be nothing too startling about what<br />
occurred with LS, but I think it may be a more<br />
common scenario as long-time PMMA contact<br />
lens patients (dinosaurs) develop age-related<br />
pathologies. To give the best surgical outcome<br />
we, as the optometrists, should be considering<br />
the stability of prescriptions and the stability of<br />
the cornea.<br />
The options for these patients will vary with the<br />
patients’ needs. The first step which will help in<br />
the long-term will be to change these patients<br />
to well-fitting newer materials before problems<br />
occur. The patient may not be keen to change<br />
from a winning formula but just as we change<br />
soft contact lens wearers into silicon hydrogel<br />
it seems sensible to change PMMA wearers<br />
into more modern materials. If you do end up<br />
with a patient like LS though, it is worthwhile<br />
discussing with them that they will have a few<br />
months of potentially average vision to give them<br />
a long-term positive outcome. Once out of rigid<br />
lenses patients, may decide to pursue spectacles<br />
(although we must warn them the prescription<br />
may change quickly) or soft contact lenses but<br />
these of course can be difficult with rigid wearers.<br />
I would be intrigued to find out how other<br />
optometrists deal with this problem particularly<br />
for a patient concerned with the cost of this<br />
process. There doesn’t seem to be any universal<br />
answer but it does seem certain that the<br />
number of patients in rigid lenses whether it be<br />
PMMA or modern materials are increasing in age<br />
and therefore increasing in pathology. Cataracts<br />
can affect these patients and it is our job to deal<br />
with it to give them the best vision. ▀<br />
References<br />
1. Time to Resolution of Contact Lens-Induced Corneal<br />
Warpage Prior to Refractive Surgery1 Wang, Xiaohong<br />
M.D.; McCulley, James P. M.D.; Bowman, R. Wayne M.D.;<br />
Cavanagh, H. Dwight M.D., Ph.D. CLAO Journal: October<br />
2002 - Volume 28 - Issue 4 - pp 169-171<br />
ABOUT THE AUTHOR:<br />
* Guest columnist Jacob Benefield stepped in to help while our<br />
regular speciality lens contributor<br />
Alex Petty focused on establishing<br />
his new practice in Tauranga.<br />
Benefield, an optometrist based in<br />
Palmerston North, splits his time<br />
between Visique Naylor Palmer,<br />
Bruce Little Optometrists and the<br />
glaucoma clinic at Palmerston<br />
North hospital. He too has a special<br />
interest in ortho-k and fitting hard<br />
contact lenses.<br />
For those who missed it, General Optical’s stand<br />
at last year’s Visionz conference was proudly<br />
displaying the latest partnership innovation<br />
between Nike and lens company Zeiss for Nike’s<br />
most recent Vision Running Collection.<br />
Though the companies have been working<br />
together since 1998, last year saw the development<br />
of a completely new construction method which<br />
seamlessly fuses the lens material with the frame to<br />
increase coverage and offer eyewear that is lighter<br />
than the average performance product on the market<br />
today, said the companies in a statement. The new<br />
Nike Vapourwing, Tailwind and Bandit designs were<br />
the result of two-years of collaborative development<br />
between Nike Vision, Zeiss and The Shop, VSP Global’s<br />
innovation lab, which develops technologies for the<br />
physical and digital aspects of eyewear and eye care.<br />
US-based VSP Global is the licensee owner for Nike<br />
Vision, through its global design manufacturer and<br />
distributor, <strong>March</strong>on Eyewear.<br />
“The partnership started from scratch to<br />
manufacture a new lens from a custom mould,”<br />
said Stephen Tripi, <strong>March</strong>on’s marketing director.<br />
“Once developed, the mould was refined using<br />
ultra-precise machinery with diamond-polishing<br />
technology to polish the complex lens shape down<br />
to the nanometer. The end result is a lightweight,<br />
state-of-the-art lens that maximizes coverage<br />
and provides optimum clarity to allow athletes to<br />
perform at the highest level.<br />
“To better serve our athletes, we looked to the<br />
future of sunglass design to incorporate new lens<br />
geometry and materials, as well as fit technology<br />
and design elements that haven’t been used in<br />
the performance eyewear industry before. We<br />
really wanted to elevate athletic performance by<br />
developing a better system of eyewear.”<br />
Leslie Muller, co-lead of The Shop and vice<br />
president, design for <strong>March</strong>on said his team worked<br />
side-by-side with Nike athletes to first understand<br />
the unique eyewear demands of runners. The team<br />
drew design inspiration from nature—known as<br />
biomimicry—and looked at factors like the lattice<br />
structure of bones and tendons as strong, but<br />
lightweight interactions of materials. Collaboration<br />
with Zeiss then led to breakthroughs in lens design<br />
by fusing lens materials into frames, he said.<br />
BOOK REVIEW:<br />
The Retinal Atlas, 2nd Edition<br />
by Bailey Freund, David Sarraf, William Mieler and Lawrence Yannuzzi.<br />
Published by Elsevier <strong>2017</strong>.<br />
REVIEWED BY A/PROF ANDREA VINCENT*<br />
It has been a long time since I have been seduced<br />
by a text book. But a quick flick through the pages<br />
of The Retinal Atlas quickly became an absorbing<br />
two hours.<br />
Blame it on our busy lives and the digital<br />
revolution, but we are rapidly becoming attuned<br />
to 30 second soundbites, 140 characters and<br />
e-tocs. Rapid advances in technology are<br />
constantly changing our understanding of eye<br />
diseases and the way in which we perceive and<br />
manage them, so many textbooks have a short<br />
shelf-life. The Retinal Atlas, 2nd Edition, however,<br />
is a textbook which challenges and revolts against<br />
this. As a reference textbook predominantly<br />
consisting of images of retinal disease (and<br />
optic nerve disorders for good measure), this is a<br />
diagnostician’s dream.<br />
The stellar cast of editors and contributors have<br />
ably updated Lawrence Yannuzzi’s 1st Edition.<br />
Short synopses of clinical features, epidemiology<br />
and aetiology (longer than a tweet, but succinct<br />
and concisely written) accompany a feast of<br />
images. All imaging modalities are covered, with<br />
colour codes for image type and fundus photos,<br />
including wide-field, autofluorescence, fluorescein<br />
angiography (FFA), OCT (often with a histological<br />
correlate), ICG, and occasional ancillary images of<br />
ocular or systemic associations. Post-treatment<br />
images are present where relevant. Two pages<br />
describe and illustrate OCT angiography, but FFA<br />
images predominate, with only occasional OCT-A<br />
images – notably in MacTel2 and age-related<br />
macular degeneration (AMD) - present throughout<br />
the book.<br />
Often the ‘art of medicine’ is as simple as<br />
experience and pattern recognition; that gestalt<br />
that allows us to categorise the underlying cause,<br />
eg. vascular vs inflammatory, genetic vs toxicity.<br />
Armed with a book like this, the very clearly<br />
indexed and delineated chapters enable the<br />
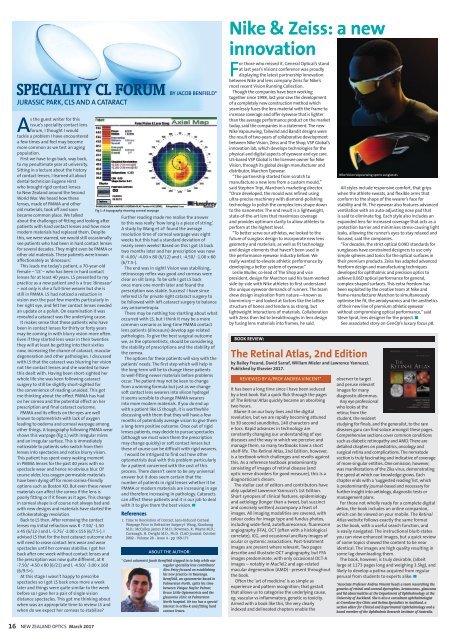
Nike Vision Vapourwing sports sunglasses<br />
All styles include responsive comfort, that grips<br />
when the athlete sweats, and flexible arms that<br />
conform to the shape of the wearer’s face for<br />
stability and fit. The eyewear also features advanced<br />
ventilation with an auto-adjusting nose pad that<br />
is said to eliminate fog. Each style also includes an<br />
expanded lens for increased coverage that acts as a<br />
protection barrier and minimises stress-causing light<br />
leaks, allowing the runner’s eyes to stay relaxed and<br />
focused, said the companies.<br />
“For decades, the strict optical 0.09D standards for<br />
sunglasses have constrained designers to use only<br />
simple spheres and torics for the optical surfaces in<br />
their premium products. Zeiss has adapted advanced<br />
freeform design and manufacturing techniques<br />
developed for ophthalmic and precision optics to<br />
achieve 0.06D optical performance for general,<br />
complex-shaped surfaces. This extra freedom has<br />
been exploited by the creative team at Nike and<br />
frame-manufacturer <strong>March</strong>on to simultaneously<br />
optimise the fit, the aerodynamics and the aesthetics<br />
of their new line of premium athletic eyewear<br />
without compromising optical performance,” said<br />
Steve Sprat, lens designer for the project. ▀<br />
See associated story on GenOp’s luxury focus p8.<br />
observer to target<br />
and peruse relevant<br />
images for many<br />
diagnostic dilemmas.<br />
Any eye professional<br />
who looks at the<br />
retina; from the<br />
student, the resident<br />
studying for finals, and the generalist, to the rare<br />
diseases guru can find solace amongst these pages.<br />
Comprehensive sections cover common conditions<br />
such as diabetic retinopathy and AMD. There are<br />
detailed chapters on paediatrics, oncology and<br />
surgical retina and complications. The nematode<br />
section is truly fascinating and indicative of coverage<br />
of more singular entities. One omission, however,<br />
was manifestations of the Zika virus, demonstrating<br />
the speed at which our knowledge grows. Each<br />
chapter ends with a ‘suggested reading’ list, which<br />
is predominantly journal-based and necessary for<br />
further insight into aetiology, diagnostic tests or<br />
management plans.<br />
For those not wholly ready for a complete digital<br />
detox, the book includes an online companion,<br />
which can be viewed on your mobile. The Retinal<br />
Atlas website follows exactly the same format<br />
as the book, with a useful search function, and<br />
is easily navigated. The instructional blurb states<br />
you can view enhanced images, but a quick review<br />
of some topics showed the content to be near<br />
identical. The images are high quality resulting in<br />
some lag downloading them.<br />
The book, however, is truly desirable, (albeit<br />
large at 1173 pages long and weighing 3.5kg), and<br />
likely to develop a patina acquired from regular<br />
perusal from students to experts alike. ▀<br />
*Associate Professor Andrea Vincent heads a team researching the<br />
genetics of retinal and corneal dystrophies, keratoconus, glaucoma<br />
and lid abnormalities at the Department of Ophthalmology at the<br />
University of Auckland. She is also a consultant ophthalmologist<br />
at Greenlane Eye Clinic and Retina Specialists in Auckland, a<br />
section editor for Clinical and Experimental Ophthalmology and a<br />
board member of the Ophthalmic Research Institute of Australia.<br />
16 NEW ZEALAND OPTICS <strong>March</strong> <strong>2017</strong>