You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
with<br />
Prof Charles McGhee<br />
& A/Prof Dipika Patel<br />
Series Editors<br />
Preoperative risk assessments to reduce<br />
cataract complications<br />
BIA Z. KIM, DIPIKA V. PATEL AND CHARLES N.J. MCGHEE<br />
Cataract surgery is highly successful but<br />
complications do occur and internationally<br />
studies report an overall complication rate of<br />
approximately 5%. Although not all complications<br />
lead to poor outcomes, the occasional severe<br />
complication can be blinding. With over 30,000<br />
cataract surgeries performed each year in New<br />
Zealand, even a small percentage of moderate<br />
adverse outcomes adds up to hundreds of patients.<br />
Numerous factors increase the risk of a<br />
complication during and after cataract surgery.<br />
Unfortunately, many of these factors are intrinsic<br />
and unavoidable but prior identification of these<br />
risk factors may allow optometrists and ophthalmic<br />
surgeons to appropriately advise patients.<br />
Subsequently, it may be possible to take appropriate<br />
perioperative precautions and adjust intraoperative<br />
techniques to try to reduce these risks.<br />
Corneal opacity<br />
One of the most apparent risk factors on slit-lamp<br />
examination is corneal scarring or haze. If the<br />
opacity is sufficient to obscure fine iris detail on<br />
slit-lamp examination, it may prove problematic<br />
during surgery. To maximise the red reflex during<br />
surgery to facilitate capsulorhexis, the eye may<br />
be manipulated into a better position and the<br />
background or direct co-axial microscope light may<br />
be altered to minimise backscatter of light from<br />
the cornea and cataract. In very severe cases of<br />
scarring, an external light pipe may occasionally<br />
be useful to illuminate structures tangentially to<br />
enable a safe capsulorhexis.<br />
White/dense/mature cataracts<br />
A dense cataract can present multiple problems<br />
during surgery. The large lens may create positive<br />
pressure and tension on the capsule and may<br />
significantly shallow the anterior chamber. The<br />
anterior capsule is also very difficult to visualise over<br />
a white or brunescent cataract, increasing the risk of<br />
a capsule tear or irregular capsulotomy.<br />
The view of the capsule can be improved using<br />
tissue staining e.g. Vision Blue (trypan blue<br />
ophthalmic solution) injected into the anterior<br />
chamber and washed out after it has stained the<br />
anterior capsule blue (Fig 1.). Furthermore, a dense<br />
cataract will require more phacoemulsification<br />
energy than a soft lens. Since total ultrasound<br />
energy can be associated with postoperative<br />
corneal oedema and intraocular inflammation, a<br />
phaco-chop technique that generally requires less<br />
energy may be preferable. 1<br />
Fig 1. Intraoperative photograph during capsulorhexis - anterior lens<br />
capsule stained with Vision Blue over congenital white cataract.<br />
Fuch’s endothelial corneal dystrophy<br />
(FECD)<br />
Other risk factors may be more subtle. Individuals<br />
with mild FECD may be asymptomatic or unaware<br />
of minor changes in vision. However, patients with<br />
FECD are at greater risk of corneal decompensation<br />
and need to be aware of the possible longer-term<br />
consequences such as a corneal transplant. Thus<br />
all corneas need to be examined carefully for signs<br />
of FECD eg. guttata and increased pachymetry<br />
(Fig 2.). A preoperative central corneal thickness<br />
12 NEW ZEALAND OPTICS <strong>Aug</strong>ust <strong>2016</strong>.indd<br />
(CCT) greater than 620µm is associated with<br />
an increased probability of requiring a corneal<br />
transplant following cataract surgery and for each<br />
10µm increase beyond 620µm, the odds of corneal<br />
decompensation increase by 1.7 times 2 .<br />
Damage to the compromised endothelium may<br />
be prevented by reducing the flow of fluids in<br />
the anterior chamber during surgery and using<br />
a ‘soft-shell’ technique (a dispersive viscoelastic<br />
device coats and protects the endothelium<br />
while a cohesive viscoelastic deepens the<br />
anterior chamber and maintains the working<br />
space) 3 . Furthermore, torsional rather than<br />
longitudinal phacoemulsification can reduce the<br />
dissipated ultrasound energy, thereby minimising<br />
endothelial injury 2 .<br />
Pseudoexfoliation syndrome<br />
Pseudoexfoliation is associated with a significant<br />
number of problems in cataract surgery, including<br />
poor pupillary dilation, zonular weakness<br />
leading to zonular dialysis or lens dislocation<br />
with vitreous loss, postoperative intraocular<br />
pressure spikes, capsular phimosis, cystoid<br />
macular oedema, prolonged inflammation, and<br />
corneal decompensation. However, the white/<br />
grey dandruff-like material mostly on the pupil<br />
margin and anterior lens surface, indicative of<br />
pseudoexfoliation, can be easily missed on casual<br />
slit-lamp examination, especially with an undilated<br />
pupil (Fig 3.). Peripupillary iris transillumination<br />
and pigmented pupillary ruff atrophy may also<br />
provide clues of underlying disease.<br />
With prior knowledge of these risk factors the<br />
patient can be better-informed and surgical<br />
planning can be modified, eg. lower anterior<br />
chamber irrigation rate, insertion of a capsular<br />
tension ring, augmented pharmacological and/<br />
or mechanical pupillary dilation (synechialysis, iris<br />
hooks). Hydrodissection and hydrodelineation of<br />
the cataract can cause further downward stress<br />
and zonular compromise, thus should be performed<br />
carefully. A zonule-friendly phaco-chop technique<br />
and a gentle two-instrument rotation of the nucleus<br />
are also helpful. It is also useful to work in the central<br />
anterior chamber with copious viscoelastic, avoiding<br />
the friable capsular periphery and shallowing of the<br />
anterior chamber. Towards the end of the surgery,<br />
thorough removal of viscoelastic is important in<br />
minimising significant postoperative IOP spikes 4 .<br />
Phacodonesis<br />
Phacodonesis is the tremulousness or subtle<br />
movement of the lens with eye movements,<br />
which may occur due to a previous eye injury,<br />
pseudoexfoliation or other causes of zonular<br />
compromise or lens subluxation. Phacodonesis may<br />
be detected by asking the patient to move their eye<br />
quickly from side-to-side and up-and-down while<br />
the clinician observes the eye on the slit-lamp. The<br />
patient may also be asked to look directly ahead<br />
while the clinician gently strikes the upright of<br />
the slit-lamp head support 2-3 times (obviously<br />
warning the patient beforehand). The transmitted<br />
energy through the head/chin rest may produce a<br />
flickering lens reflex or frank movement.<br />
Similar adjustments can be made to surgical<br />
techniques as previously highlighted in<br />
pseudoexfoliation to reduce stress on the zonules<br />
and also plan for additional techniques such as<br />
sutured capsule tension segments or rings.<br />
Anaesthetic<br />
Generally, contemporary cataract surgery is<br />
performed under regional (peri-bulbar/sub-<br />
Tenon’s anaesthesia [STA]) or topical (drop/gel)<br />
anaesthesia, with or without low-level oral or<br />
intravenous sedation. A larger volume regional<br />
anaesthesia may increase the intraocular pressure<br />
and shallow the anterior chamber, occasionally<br />
making surgery a little more difficult. Since an<br />
incision is required in the infero-nasal conjunctiva<br />
for STA it may be associated with subconjunctival<br />
haemorrhage, that on occasion may be extensive.<br />
Although not sight-threatening and self-resolving<br />
over 7-14 days, the dramatic appearance may<br />
Fig 2. Slit-lamp photograph showing corneal endothelium with guttata<br />
in Fuch’s endothelial corneal dystrophy.<br />
Fig 3. Slit-lamp photograph of white/grey pseudoexfoliative material on<br />
pupil margin.<br />
be unsettling for patients and relatives. Topical<br />
anaesthesia may avoid any injections but requires<br />
adequate patient cooperation, as the eye is able to<br />
move much more freely during the procedure.<br />
Therefore, preoperative assessments should<br />
include potential language barriers, anxiety<br />
levels, ability to lie flat for up to 30 minutes,<br />
head tremors, and antiplatelet/anticoagulant<br />
medications that may predispose to bleeding.<br />
Systemic medications<br />
Oral Doxazosin and similar alpha-blockers used<br />
for prostatic and urinary symptoms are associated<br />
with intraoperative “floppy iris syndrome” – the<br />
iris billows and has a tendency to prolapse through<br />
the surgical incisions whilst the pupil progressively<br />
constricts during surgery. This can lead to extremely<br />
complicated surgery and extensive iris damage.<br />
Unfortunately, these issues are not resolved by<br />
simply stopping the medication prior to surgery.<br />
Thus ophthalmologists may need to consider a<br />
number of strategies including: creating longer<br />
corneal incisions and maintaining the anterior<br />
chamber depth to prevent peripheral iris prolapse;<br />
augmented pharmacological pupil dilation (e.g.<br />
intra-cameral phenylephrine); and mechanical<br />
dilation/iris stabilization (e.g. iris hooks or rings).<br />
Inflammation<br />
Intraocular inflammation such as chronic anterior<br />
uveitis that is not entirely quiescent should<br />
generally be controlled and stable for around six<br />
months before embarking on cataract surgery.<br />
Perioperatively, patients may require an increased<br />
dose of corticosteroid or other immunosuppressive<br />
therapy to reduce the risk of significant<br />
postoperative inflammation and flare-ups.<br />
Risk stratification<br />
Complication rates generally decrease with<br />
increasing experience of surgeons 5 . Thus, it is<br />
imperative that cases are allocated appropriately,<br />
especially in teaching hospitals where there is a<br />
vast range of surgeon experience. Preoperative<br />
risk stratification systems have been devised to<br />
assess the risk of complications for individual<br />
patients. They may help minimise complications<br />
by identifying and allocating the higher risk cases<br />
to appropriate surgeons in a standardised manner.<br />
In a recent study in Auckland, two preoperative<br />
risk stratification systems were evaluated – one<br />
system devised by Muhtaseb et al 6 and another<br />
system used in the Buckinghamshire NHS Trust.<br />
Each system takes into account different risk factors<br />
and a final risk score is calculated by adding up the<br />
risk factors in each case (Table 1). Subsequently,<br />
the Muhtaseb system was implemented to assist<br />
allocation of cases to registrars, fellows and<br />
consultants and further analyses are underway to<br />
examine the impact on complication rates.<br />
It is imperative that risk factors are identified and<br />
documented preoperatively for such cataract risk<br />
stratification systems to work effectively. Apart<br />
from allocating cases to appropriately experienced<br />
surgeons, they support surgeons of all levels to<br />
take precautions in order to reduce complications.<br />
It also allows practitioners involved in preoperative<br />
assessments to focus discussions on specific risks<br />
with individual patients, which is critical in providing<br />
the best quality of cataract surgery, and most useful<br />
in postoperative management. ▀<br />
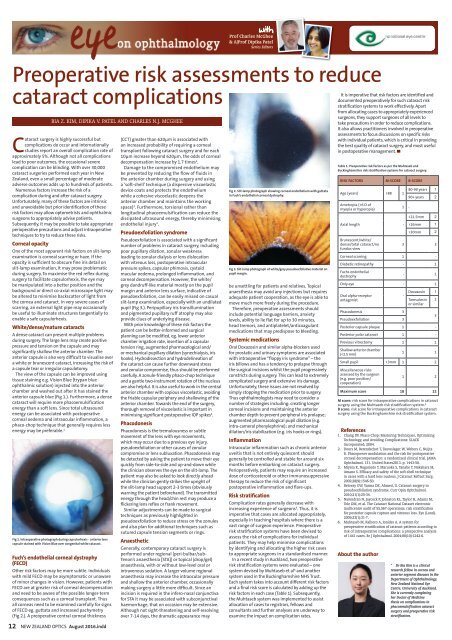
Table 1. Preoperative risk factors as per the Muhtaseb and<br />
Buckinghamshire risk stratification systems for cataract surgery.<br />
RISK FACTORS M-SCORE B-SCORE<br />
Age (years) >88 1<br />
Ametropia (>6 D of<br />
myopia or hyperopia)<br />
Axial length -<br />
Brunescent/white/<br />
dense/total cataract/no<br />
fundus view<br />
1 -<br />
80-90 years 1<br />
90+ years 2<br />
26mm 1<br />
>30mm 2<br />
3 3<br />
Corneal scarring 1 -<br />
Diabetic retinopathy - 1<br />
Fuchs endothelial<br />
dystrophy<br />
- 1<br />
Only eye - 1<br />
Oral alpha-receptor<br />
antagonist<br />
Phacodonesis 3<br />
Pseudoexfoliation 3<br />
-<br />
Doxazosin 1<br />
Tamsulosin<br />
or similar<br />
Posterior capsule plaque 1 -<br />
Posterior polar cataract 1 -<br />
Previous vitrectomy 1 1<br />
Shallow anterior chamber<br />
(